Abstract
This paper examines the extent to which childhood circumstances contribute to health inequality in old age and how the contributions may vary across key dimensions of health. We link the China Health and Retirement Longitudinal Study (CHARLS) in 2013 and 2015 with its Life History Survey in 2014 to quantify health inequality due to childhood circumstances for which they have little control. We evaluate comprehensive dimensions of health ranging from cognitive health, mental health, physical health, self-rated health to mortality. Our analytic sample includes about 8,000 Chinese persons age above 60. Using the Shapley value decomposition approach, we first show that childhood circumstances may explain 1-23 percent of health inequality in old age across multiple health outcomes. Second, while both direct health-related circumstances and indirect health-related circumstances contribute significantly to health inequality, the latter tends to be more sizable. Our findings support the value of a life course approach in identifying the key determinants of health in old age.
Keywords: Life course approach, Inequality of opportunity, Physical health, Cognitive ability, Mental health, Mortality
1. INTRODUCTION
Population aging has become an emergent global trend. The number of older persons – those aged 60 years or over – has increased substantially in China and the world, from 125.2 million and 0.61 billion (or both 9.9% of the population) in 2000 to 209.2 million and 0.90 billion (or 15.2% and 12.3% of the population) in 2015. This growth is projected to accelerate in the coming decades, to reach almost 358.1 million and 1.40 billion (or 25.3% and 16.5% of the population) by 2030 and nearly 491.5 million and 2.09 billion (or 36.5% and 21.5% of the population) by 2050 (United Nations, 2015) in China and the world. Healthy aging has become a very important theme for society, especially in China where the population ages fast.
As a key component of human capital, strong evidence suggests that the return to health investment is the highest in early life (Cunha & Heckman 2009). The WHO Commission on the Social Determinants of Health highlights the role of childhood conditions as a primary source of unfair health inequality (Marmot et al., 2008). It is therefore important to assess the role of childhood circumstances in explaining the widening health gradient (Shen & Zeng 2014; Bor, Cohen, & Galea 2017). Growing evidence shows that a wide range of childhood circumstances could affect physical, cognitive, and mental health in old age, such as family socioeconomic status and parent’s educational attainments (Dahl & Birkelund 1997; Moody-Ayers et al. 2007; Ramos 2007; Zhang, Gu, & Hayward 2008; Katikireddi 2016; Gale et al. 2016), nutrition condition in childhood (Palloni et al. 2005; McEniry et al. 2008), health status in childhood (Sayer et al. 2004; Kuh et al. 2006; Dodds et al. 2012; Cooper et al. 2014), parenting skills (Andersson & Stevens 1993; Krause 1998), service capacity in the community (Shen 2014), social mobility (Venkataramani et al. 2016), and maternal bereavement (Black, Devereux, & Salvanes 2016; Persson & Rossin-Slater 2017). This paper aims to assess an array of key circumstances to identify the overall role of childhood circumstances on health inequality in old age.
Health inequality prevails in old age, which may originate from both early life circumstances and efforts (Thorslund & Lundberg 1994; Rueda, Artazcoz, & Navarro, 2008; Marmot et al. 2008). Inequality of Opportunity in health (IOP in health, a.k.a. health inequality due to circumstances) is beyond the realm of individuals’ choices, whereas individuals should be responsible for health inequality due to efforts (Lefranc, Pistolesi, & Trannoy, 2008). Since circumstance factors in early life are uncontrollable by the individual, childhood circumstances are largely seen as illegitimate sources of health inequalities. On the contrary, differences in health status that are due to efforts, such as lifestyle, are often seen as ethically justified by individual choice (Roemer & Trannoy 2016). Therefore, the policy implications of IOP are that actions should be taken to compensate for health inequality resulting from childhood circumstances (Roemer et al. 2003; Rosa-Dias & Jones 2007; Lefranc, Pistolesi, & Trannoy 2008; Rosa-Dias 2009; Fleurbaey & Schokkaert 2009; Trannoy et al. 2010).
It is difficult to define the exact set of childhood circumstances that contribute to health inequality. This paper classifies a comprehensive set of circumstances into eight domains most comparable to existing studies on IOP for income, such as Hufe et al. (2017). Specifically, the circumstances we measured in childhood include war, regional and urban/rural status, family socioeconomic status, parents’ health status and health behaviors, health and nutrition status, relationship with parents, friendship, and access to health care.
Using the mean logarithmic deviation (MLD) approach, this paper quantifies health inequality due to childhood circumstances (for which they have little control) that are distinguishable from health inequality due to efforts (for which they are responsible). We also measure relative contribution by domain of childhood circumstances using the Shapley value decomposition approach.
Compared to growing evidence from developed countries (Rosa-Dias 2009; Trannoy et al. 2010; Bricard et al. 2013; Lazar, 2013; Garcia-Gomez et al. 2014) and developing countries (Jusot et al. 2014; Carranza & Hojman 2015; Pal 2015; Barbosa 2016; Fajardo-Gonzalez 2016), our study may contribute to the literature in four aspects. First, we advance the literature on life course epidemiology that has mostly been limited to shorter time periods, such as a decade in Simmonds et al. (2015). In contrast, we link individuals’ health outcomes at least 50 years apart to provide novel evidence of IOP in health in old age. Second, we examine IOP in health using by far the most comprehensive set of health measures. This represents an important advance as WHO (2017) defines health as a state of complete physical, mental and social well-being, not merely the absence of diseases. In contrast, most studies, such as Trannoy et al. (2010) and Bricard et al. (2013), only evaluate a very small set of health outcomes. Third, we utilize a well-measured rich set of childhood circumstances to address the concern that poor information on childhood circumstances may undervalue IOP and therefore mislead policymakers into a false sense of complacency that health inequality is largely fair (Kanbur & Wagstaff, 2016). Fourth, we offer novel evidence of IOP in health of the Chinese elderly. As a country with the world’s largest aging population, IOP in health among Chinese elders should be of much concern.
The remainder of the paper is organized as follows. Section 2 describes the data and measurements, and lays out the conceptual framework and analytic strategy. Section 3 presents our main findings. Section 4 discusses and concludes.
2. DATA AND METHODS
2.1. Data
We match the 2013, 2015 waves of the China Health and Retirement Longitudinal Study (CHARLS), a HRS-sister survey, to its 2014 Life History Survey. The merged data set enables us to link rich information on individuals’ health status in old age with childhood circumstances in a representative sample of older adults in China.
The CHARLS national baseline survey in 2011 represented people aged 45 years or older with their spouses totaling 17,708 individuals (living in 10,287 households, 450 villages/urban communities, 150 county-level units in 28 of China’s 34 provinces).1 The 2013 follow-up survey successfully tracked 15,770 individuals from the baseline survey, while 431 individuals died in between the two surveys. The 2013 wave also added 2,834 new respondents into the survey, reaching 18,604 individuals. The 2014 life history survey recruited living respondents from both the 2011 baseline survey and the 2013 follow-up survey (Hong et al. 2017). The third wave of CHARLS was administered from mid-2015 to early 2016 and covered 12,450 households with 21,057 respondents (Strauss et al., 2018).
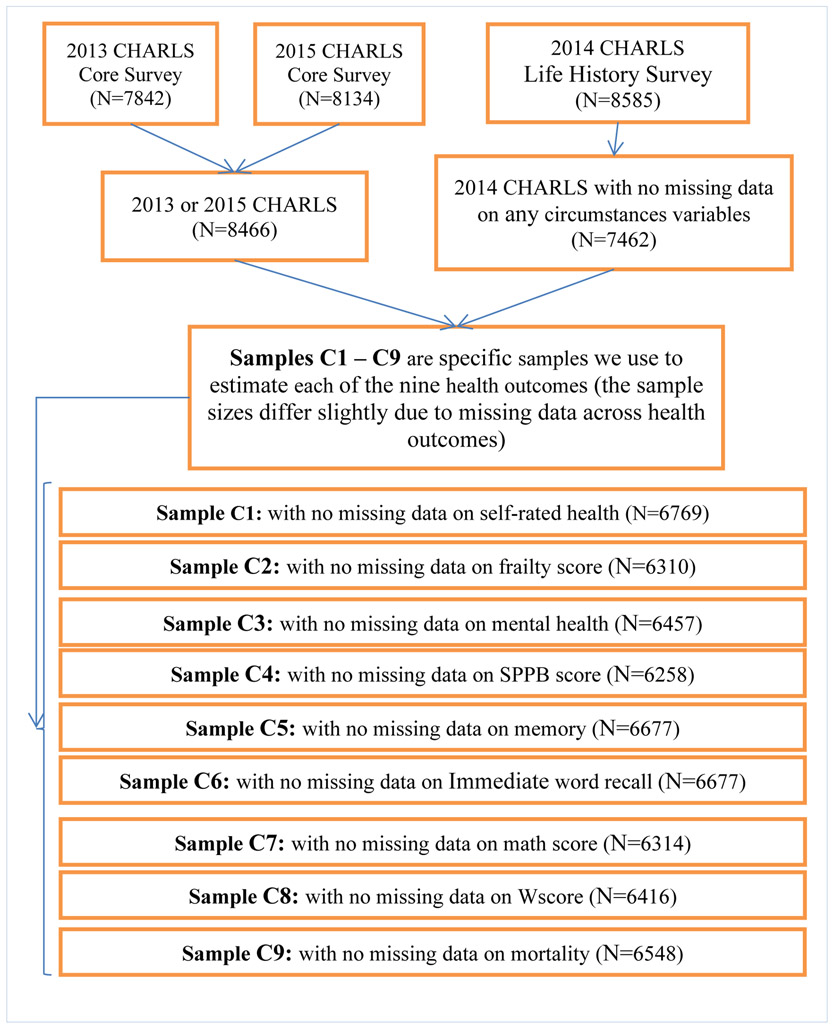
As shown in Appendix Figure 1, our sample includes 8,466 older adults born before 1953 and in either 2013 or 2015 waves of CHARLS. We measure their health in old age in multiple dimensions, i.e., physical health, self-rated health, cognitive health, mental health, and mortality. Average values are taken for health outcomes measured in both the 2013 and 2015 surveys. Meanwhile, 7,462 older adults in the 2014 CHARLS Life History Survey (LHS) have no missing value for any childhood circumstances we include in this study. Column 3 displays p-values testing statistical differences between the whole sample (Column 1) and the LHS sample with no missing value of childhood circumstances (Column 2). Reassuringly, most of childhood circumstances show no statistical difference between the two samples, especially domains of childhood circumstances that contribute more significantly to health inequality in old age.
We attempt to retain the largest possible analytical sample for each health measure in old age. Therefore, the number of observations for each estimation vary slightly across health outcome measures because of missing data. The analytical sample has a range of 6,258 – 6,769 individuals, depending on the exact health measures (Appendix Figure 1, sample C1-C9). As shown in Table 2, we find no distinguishable difference between our analytical sample C1-C9 and the whole sample for all childhood circumstance variables in domains of regional and urban/rural status, family socioeconomic status, health and nutrition conditions in childhood, friendship in childhood, as well as more than half of the variables in the other four domains. In other words, childhood circumstances that contribute the most to health variations in old age tend to be statistically indifferent between the two samples.
Table 2.
P-values of Statistical tests between the Whole Sample and Analytical Sample C1-C9
| Domain | Variable Description | Whole vs. C1 |
Whole vs. C2 |
Whole vs. C3 |
Whole vs. C4 |
Whole vs. C5 |
Whole vs. C6 |
Whole vs. C7 |
Whole vs. C8 |
Whole vs. C9 |
|---|---|---|---|---|---|---|---|---|---|---|
| Demographic factors | Gender | 0.34 | 0.24 | 0.06 | 0.28 | 0.29 | 0.29 | 0.00 | 0.31 | 0.24 |
| Ethnicity | 0.67 | 0.17 | 0.59 | 0.24 | 0.57 | 0.57 | 0.17 | 0.77 | 0.80 | |
| Birth year | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |
| War | Born in the Anti-Japan War era | 0.67 | 0.59 | 0.86 | 0.34 | 0.60 | 0.60 | 0.79 | 0.65 | 0.63 |
| Born in the Civil War era | 0.06 | 0.03 | 0.01 | 0.03 | 0.03 | 0.03 | 0.00 | 0.03 | 0.05 | |
| Parents’ health status and health behaviors | Parents’ health condition | 0.06 | 0.08 | 0.04 | 0.08 | 0.05 | 0.05 | 0.10 | 0.03 | 0.04 |
| Father has drinking problem | 0.49 | 0.41 | 0.39 | 0.45 | 0.45 | 0.45 | 0.32 | 0.35 | 0.38 | |
| Mother smokes | 0.04 | 0.02 | 0.02 | 0.02 | 0.04 | 0.04 | 0.03 | 0.06 | 0.05 | |
| Father smokes | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |
| Father’s longevity (non-response) | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |
| Father’s longevity (alive) | 0.29 | 0.27 | 0.24 | 0.31 | 0.29 | 0.29 | 0.20 | 0.19 | 0.20 | |
| Father’s longevity (low longevity) | 0.02 | 0.05 | 0.03 | 0.05 | 0.02 | 0.02 | 0.02 | 0.04 | 0.03 | |
| Father’s longevity (high longevity) | 0.02 | 0.02 | 0.00 | 0.01 | 0.01 | 0.01 | 0.00 | 0.02 | 0.03 | |
| Mother’s longevity (non-response) | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |
| Mother’s longevity (alive) | 0.29 | 0.35 | 0.12 | 0.33 | 0.25 | 0.25 | 0.11 | 0.27 | 0.37 | |
| Mother’s longevity (low longevity) | 0.13 | 0.13 | 0.12 | 0.12 | 0.12 | 0.12 | 0.09 | 0.19 | 0.09 | |
| Mother’s longevity (high longevity) | 0.02 | 0.02 | 0.01 | 0.02 | 0.01 | 0.01 | 0.00 | 0.03 | 0.03 | |
| Health & nutrition conditions in Childhood | Self-reported health status before age 15 | 0.40 | 0.39 | 0.17 | 0.46 | 0.28 | 0.28 | 0.14 | 0.33 | 0.41 |
| Ever experience hunger | 0.87 | 0.92 | 0.95 | 0.99 | 0.90 | 0.90 | 0.86 | 0.84 | 0.99 | |
| Access to health care | Received vaccination before age 15 | 0.06 | 0.02 | 0.01 | 0.02 | 0.02 | 0.02 | 0.00 | 0.04 | 0.09 |
| when ill, first visited general hospital, specialized hospital, or township health clinics? | 0.40 | 0.70 | 0.29 | 0.64 | 0.33 | 0.33 | 0.14 | 0.66 | 0.61 | |
| When ill, first visited community health centers / private clinics? | 0.59 | 0.35 | 0.61 | 0.34 | 0.56 | 0.56 | 0.42 | 0.47 | 0.50 | |
| Regional and urban/rural status | Rural or urban status at birth | 0.37 | 0.01 | 0.70 | 0.02 | 0.39 | 0.39 | 0.74 | 0.06 | 0.07 |
| Eastern China | 0.56 | 0.94 | 0.43 | 0.71 | 0.56 | 0.56 | 0.60 | 0.69 | 0.79 | |
| Central China | 0.36 | 0.93 | 0.30 | 0.93 | 0.34 | 0.34 | 0.51 | 0.41 | 0.47 | |
| Western China | 0.75 | 0.99 | 0.98 | 0.83 | 0.73 | 0.73 | 0.77 | 0.66 | 0.62 | |
| Family socioeconomic status | Parents political status | 0.83 | 0.77 | 0.50 | 0.81 | 0.68 | 0.68 | 0.36 | 0.99 | 0.98 |
| Mother’s education | 0.38 | 0.46 | 0.17 | 0.51 | 0.33 | 0.33 | 0.18 | 0.50 | 0.60 | |
| Father’s education | 0.09 | 0.19 | 0.03 | 0.11 | 0.07 | 0.07 | 0.01 | 0.17 | 0.18 | |
| Family financial status | 0.69 | 0.95 | 0.43 | 0.86 | 0.70 | 0.70 | 0.32 | 0.97 | 0.89 | |
| House type at birth | 0.59 | 0.26 | 0.73 | 0.28 | 0.64 | 0.64 | 0.86 | 0.28 | 0.30 | |
| Relationship with parents | Relationship with parents | 0.93 | 0.62 | 0.74 | 0.63 | 0.96 | 0.96 | 0.90 | 0.97 | 0.95 |
| Father ever hit you | 0.68 | 0.49 | 0.73 | 0.50 | 0.70 | 0.70 | 0.39 | 0.58 | 0.60 | |
| Mother ever hit you | 0.01 | 0.01 | 0.01 | 0.02 | 0.01 | 0.01 | 0.00 | 0.02 | 0.01 | |
| Friendship in childhood | Self-rated neighborhood willingness to help | 0.44 | 0.89 | 0.17 | 0.85 | 0.50 | 0.50 | 0.06 | 0.99 | 0.94 |
| Did you have a good friend | 0.75 | 0.78 | 0.54 | 0.88 | 0.74 | 0.74 | 0.26 | 0.83 | 0.79 |
Notes: “Whole” means the whole sample as in Table 1 column 1. The definitions of Sample C1 – C9 are in Appendix Figure 1. The variables highlighted demonstrate significant differences between the whole sample and the analytical sample C1-C9.
2.2. Measures
Descriptions of all health outcomes are provided in Appendix Table 1. Five dimensions of health status were assessed, including physical health, self-rated health, cognitive ability, mental health, and mortality. To make better use of panel data to mitigate measurement errors, we average over two consecutive waves of survey in 2013 and 2015 for almost all health outcomes (except Wscore and mortality), which are merged with the corresponding life history surveys in 2014. We take the data on health outcomes in 2013 instead of the average value both in 2013 and 2015 when there is missing data in 2015, and take the data on health outcomes in 2015 instead when there is missing data in 2013.
Self-rated health is widely used in the literature. We use the question in CHARLS, i.e. “Would you say your health is excellent, very good, good, fair, or poor?”. The five options are excellent, very good, good, fair, and poor.
Physical health is measured by short physical performance battery (SPPB) and frailty score. SPPB is an objective assessment tool to evaluate lower extremity functioning in older persons. We calculate the SPPB score involving balance ability, walk speed, and chair stand exercise according to Guralnik et al. (1994). Frailty score assesses vulnerability to an array of adverse outcomes. We follow the criteria in Fried et al. (2001) to evaluate five components of frailty, i.e. weight loss, exhaustion, low physical activity, low grip strength, and low walking speed.
Word recall, math score and Wscore are three components of cognitive ability. Word recall, a measure of episodic memory, is based on a list of 10 nouns read to the respondent who is then asked to recall as many words as possible in any order (Runge, Craig, & Jim 2015). Math score, ie Serial 7, measures working memory and is based on a task in which respondents are asked to subtract 7 from 100 and to continue subtracting 7 from each subsequent number for a total of five times (Ayyagari & Frisvold 2016). Wscore is used to standardize adaptive number series test in the 3rd wave of CHARLS in 2015, which measures a specific form of fluid intelligence related to quantitative reasoning (Strauss et al., 2018).
Mental health is measured using a 10-item Center for Epidemiological Studies Depression Scale (CES-D) (Radloff 1977). Each item scores from 0 to 3, so the total mental health score ranges from 0 to 30, with the higher score corresponding to worse mental health.
Mortality is coded as one for respondents who died between the 2014 life history survey and the 2015 follow-up survey, and zero otherwise. Around 3 percent of respondents in the 2014 life history survey died before the 2015 follow-up survey.
Since there are multi-dimension health outcomes in our study, we first analyze their correlation to show the necessity of consider comprehensive measurements on health. Appendix Table 2 shows the correlation coefficients (CC) among health outcomes. Since memory is the mean of immediate word recall and delayed word recall, the CC between Memory and Immediate word recall is 0.934, much higher than 0.6. The absolute values of CC between math score and Wscore, Frailty score and Sppb score, Mental health and Self-rated health, Memory and Wscore are 0.458, 0.451, 0.419, and 0.409, higher than 0.4, but less than 0.6. Therefore, it is necessary to use multi-dimension health outcomes to measure the comprehensive health status of the elder.
The selection of circumstances variables was guided by the literature. The circumstances variables, presented in Table 1, are classified into eight domains: 1) war. Since China suffered the Anti-Japanese War, and Civil War during 1930s and 1940s, we used two dummy variables “born in the Anti-Japan War era” and “Bom in the Civil War era” to measure any overlap with those events in early life.; 2) regional and urban/rural status at birth. The economic and social conditions for urban and rural areas were vastly different between 1930s and 1950s when the respondents were in childhood; 3) family socioeconomic status in childhood, including self-rated family financial status, parental educational attainments, political status, and housing conditions; 4) parents’ health status and health behaviors in childhood, such as inability to work and/or function, excessive alcohol consumption, and use of tobacco products; 5) health and nutritional status in childhood, including self-rated health before age 15 and if hunger was experienced; 6) relationship with parents in childhood; 7) friendship in childhood; and 8) access to health care in childhood, such as vaccination status and type of doctors visited for the first time. The direct health-related circumstances in childhood refer to the circumstances directly contributing to health, including domains 4), 5) and 8). Domains 1), 2), 3), 6) and 7) are in the category of indirect health-related circumstances, which refer to the environments that may only indirectly affect health.
Table 1.
Summary Statistics of Childhood Circumstance Variables
| Domain | Variable Description | N | (1) Whole Sample |
N | (2) Sample with no missing child circumstances |
(3) Diff (1)-(2) |
|---|---|---|---|---|---|---|
| Demographic factors | Gender (1: male; 0: female) | (8585) | 0: 50.0%; 1: 50.0% | (7462) | 0: 50.6%; 1: 49.4% | 0.31 |
| Ethnicity (1: Han; 0: minority) | (7827) | 0: 6.9%; 1: 93.1% | (7462) | 0: 6.7%; 93.3% | 0.67 | |
| Birth year | (8585) | Mean: 1944; Std: 6.9 Min: 1916; Max: 1953 |
(7462) | Mean: 1945; Std: 6.4 Min: 1916; Max: 1953 |
0.00 | |
| War | Born in the Anti-Japan War era (1937-1945) (1: Yes; 0: No) | (8585) | 0: 68.7%; 1: 31.3% | (7462) | 0: 68.5%; 1: 31.5% | 0.83 |
| Born in the Civil War era (1946-1949) (1: Yes; 0: No) | (8585) | 0: 75.9%; 1: 24.1% | (7462) | 0: 74.8%; 1: 25.2% | 0.11 | |
| Parents’ health status and health behaviors | Parents’ health condition (1: long time in bed; 0: None) | (8585) | 0: 82.9%; 1: 17.1% | (7462) | 0: 81.9%; 1: 18.1% | 0.09 |
| Father has drinking problem (1: alcoholism; 0: None) | (8585) | 0: 94.2%; 1: 5.8% | (7462) | 0: 94.0%; 1: 6.0% | 0.57 | |
| Mother smokes (1: Yes; 0: None) | (8585) | 0: 90.1%; 1: 9.9% | (7462) | 0: 89.1%; 1: 10.9% | 0.03 | |
| Father smokes (1: Yes; 0: None) | (8585) | 0: 57.9%; 1: 42.1% | (7462) | 0: 55.4%; 1: 44.6% | 0.00 | |
| Father’s longevity (1: non-response; 0: others) | (8585) | 0: 76.4%; 1: 23.6% | (7462) | 0: 80.0%; 1: 20.0% | 0.00 | |
| Father’s longevity (1: alive; 0: others) | (8585) | 0: 97.1%; 1: 2.9% | (7462) | 0: 96.9%; 1: 3.1% | 0.23 | |
| Father’s longevity (1: low longevity; 0: others) | (8585) | 0: 64.0%; 1: 36.0% | (7462) | 0: 62.4%; 1: 37.6% | 0.04 | |
| Father’s longevity (1: high longevity; 0: others) | (8585) | 0: 62.5%; 1: 37.5% | (7462) | 0: 60.7%; 1: 39.3% | 0.02 | |
| Mother’s longevity (1: non-response; 0: others) | (8585) | 0: 79.6%; 1: 20.4% | (7462) | 0: 82.9%; 1: 17.1% | 0.00 | |
| Mother’s longevity (1: alive; 0: others) | (8585) | 0: 92.2%; 1: 7.8% | (7462) | 0: 91.7%; 1: 8.3% | 0.22 | |
| Mother’s longevity (1: low longevity; 0: others) | (8585) | 0: 66.4%; 1: 33.6% | (7462) | 0: 65.5%; 1: 34.5% | 0.20 | |
| Mother’s longevity (1: high longevity; 0: others) | (8585) | 0: 61.8%; 1: 38.2% | (7462) | 0: 60.0%; 1: 40.0% | 0.02 | |
| Health and nutrition conditions in Childhood | Self-reported health status before age 15 (1: much healthier; 2: somewhat healthier; 3: about average; 4: some less healthy; 5: much less healthy) | (8469) | 1: 15.3%; 2: 19.3%; 3: 52.4%;4: 7.9%; 5: 5.2% | (7462) | 1: 15.6%; 2: 19.4%; 3: 52.4%;4: 7.7%; 5: 5.0% | 0.41 |
| Ever experience hunger (1: No; 2: yes after age 5; 3: yes before age 5) | (8348) | 1: 23.6%; 2: 45.7%; 3: 30.7% | (7462) | 1: 22.9%; 2: 47.3%; 3: 29.8% | 0.79 | |
| Access to health care | Received vaccination before age 15 (1: Yes; 0: No) | (8418) | 0: 78.7%; 1: 21.3% | (7462) | 0: 80.0%; 1: 20.0% | 0.06 |
| When ill, first visited general/specialized hospital or township clinics? (1: Yes; 0: No) | (8585) | 0: 71.9%; 1: 28.1% | (7462) | 0: 71.2%; 1: 28.8% | 0.34 | |
| When ill, first visited community health centers/private clinics? (1: Yes; 0: No) | (8585) | 0: 74.2%; 25.8% | (7462) | 0: 73.9%; 1: 26.1% | 0.67 | |
| Regional and urban/rural status | Rural or urban status at birth (0: rural; 1: urban) | (8481) | 0: 90.1%; 1: 9.9% | (7462) | 0: 90.2%; 1: 9.8% | 0.86 |
| Eastern China (1: Yes; 0: No) | (8585) | 0: 73.2%; 1: 26.8% | (7462) | 0: 73.0%; 1: 27.0% | 0.70 | |
| Central China (1: Yes; 0: No) | (8585) | 0: 61.1%; 1: 38.9% | (7462) | 0: 61.8%; 1: 38.2% | 0.40 | |
| Western China (1: Yes; 0: No) | (8585) | 0: 75.6%; 1: 24.4% | (7462) | 0: 75.3%; 1: 24.7% | 0.66 | |
| Family socioeconomic status | Parents political status (1: any party member; 0: No) | (8585) | 0: 93.1%; 1: 6.9% | (7462) | 0: 92.8%; 1: 7.2% | 0.54 |
| Mother’s education (1: literate; 0: illiterate) | (8585) | 0: 94.8%; 1: 5.2% | (7462) | 0: 94.5%; 1: 5.5% | 0.41 | |
| Father’s education (1: literate; 0: illiterate) | (8585) | 0: 68.5%; 1: 31.5% | (7462) | 0: 67.4%; 1: 32.6% | 0.11 | |
| Family financial status (1: a lot better; 2: somewhat better; 3: same as; 4: somewhat worse; 5: a lot worse) | (8484) | 1: 1.2%; 2:8.1%; 3: 50.0%; 4: 15.3%; 5: 25.6% | (7462) | 1: 1.3%; 2:8.0%; 3: 50.4%; 4: 15.4%; 5: 25.0% | 0.62 | |
| House type at birth (1: concrete; 2 adobe; 3 wood or others) | (8552) | 1: 12.3%; 2: 58.6%; 3: 29.1% | (7462) | 1: 12.2%; 2: 58.6%; 3: 29.2% | 0.90 | |
| Relationship with parents | Relationship with parents (1: excellent; 2: very good; 3: good; 4: fair; 5: poor) | (7883) | 1: 27.0%; 2: 28.8%; 3: 20.1%; 4: 22.0%; 5: 2.1% | (7462) | 1: 27.0%; 2: 28.8%; 3: 20.0%; 4: 22.0%; 5: 2.2% | 0.95 |
| Father ever hit you (1: often/somewhat; 0: rarely/never) | (8585) | 0: 86.5%; 1: 13.5% | (7462) | 0: 86.1%; 1: 13.9% | 0.47 | |
| Mother ever hit you (1: often/somewhat; 0: rarely/never) | (8585) | 0: 79.3%; 1: 20.7% | (7462) | 0: 77.4%; 1: 22.6% | 0.00 | |
| Friendship in childhood | Self-rated neighborhood willingness to help (1: very/somewhat, 0: not very/not at all) | (8585) | 0: 12.2%; 1: 87.8% | (7462) | 0: 12.1%; 1: 87.9% | 0.23 |
| Did you have a good friend (1: yes; 0: no) | (8217) | 0: 56.2%; 1: 43.8% | (7462) | 0: 55.7%; 1: 44.3% | 0.57 |
Notes: Column 3 displays the tests p-values between variables in the whole sample (column 1) and the sample with no missing data on any circumstances variables (column 2, N=7,462).
We also evaluated associations between the suggested endogenous childhood circumstances (including health status before age 15, family financial status, relationship with parents, and neighborhood willingness to help) and health status in old age. We provide the pairwise correlations in Appendix Table 3. While most of these childhood circumstances and health in old age are significantly correlated at 1% level, their correlation coefficients are small, ranging between −0.112 and 0.211.
2.3. Conceptual Framework and Analytic Strategy
The main outcomes of interest in this study are health measures at the individual level. As a popular measure of the extent of health inequality, mean logarithmic deviation (MLD) of health distribution F, i.e. MLD(F), has been used to measure multiple dimensions of well-being (Haughton and Khandker 2009; Ferreira and Gignoux 2011; Ferreira and Gignoux 2013; Hufe et al. 2017; Björklund et al. 2012). It is defined as the mean deviation of lnyi from . In other words, it measures the average difference between and lnyi.
where N is the number of individuals, yi is health status of individual i. is the mean of yi. is the mean of lnyi.
The logarithmic form comes from a natural case of the generalized entropy, a well-accepted family of inequality measures. The logarithmic form has several good features, among them the most relevant to us include: 1) it considers aversion to higher health inequality. Given the average health outcome , more unequal health status corresponds to a higher MLD;2 2) the logarithmic form enables us to mitigate the possible overinfluence of outlier values.
Let us suppose we have partitioned the population into types of individuals, each type corresponding to the set of individuals with the same value of childhood circumstances. Each type is characterized by its own health distribution. Let the type distributions be {Ft(y), t ϵ T} where T is the set of types, and let type t have frequency ft in the population and mean health outcome μt, summarized by the vectors f = f1, …, fT and μ = μ1, …, μT. We can construct a hypothetical distribution, denoted by Φ(μ, f), in which all members of each type t have the mean health outcome μt of that type. Φ(μ, f) has a cumulative distribution function that is a step function, with as many steps as types. This is often called the ‘smoothed’ distribution of F associated with the typology (f,μ). If Φ(μ, f) were the true health distribution, then all health inequality is due to childhood circumstances and none to efforts. The MLD of total inequality is decomposable as follows:
| (1) |
MLD can be fully decomposed into inequality due to childhood circumstances MLD(Φ) and efforts (Shorrocks 1980; Shorrocks 2013; Jusot et al. 2013; Wendelspiess 2014). Therefore, the ratio r measures the extent to which health inequality is due to childhood circumstances:
The conceptual model partitions the population into types by value of their childhood circumstances and takes as data the type distributions and the aggregate distribution of the outcome of interest. This non-parametric approach requires either a very large data set, or a small set of types, to ensure meaningful distribution of health outcomes by type. However, a richer set of childhood factors in our study requires us to replace the partition of the population into a typology by regression analysis. Our regression-based Shapley value decomposition approach enables us to estimate the impact of numerous childhood circumstances even in the presence of small sample and cell sizes. Following Ferreira and Gignoux (2011). The econometric specification is
where C is a vector of circumstances variables, Y is a vector of health outcomes in old age, u is the error term, and i represents individual i. We construct a parametric estimate of the smoothed distribution Φ defined earlier by replacing Y by their predictions:
Let Φ be the distribution of estimated Y. In this counterfactual, all individuals with the same childhood circumstances have the same Y. Thus, IOP, denoted by r can be rewritten as:
There is high correlation between r and R square of Yi = αCi + ui. R square makes use of variance in the measure of IOP (Ferreira & Gignoux 2013). We show the robustness test in section 3. To compute the Shapley value decomposition, we first estimate the inequality measure for all possible permutations of the circumstance variables. In a second step, the average marginal effect of each circumstance variable on the measure of IOP is computed (Juarez & Soloaga, 2014). This procedure is very computationally intensive as 2K (K= number of circumstances) must be computed. However, there are substantial advantages compared to other decomposition methods, such as being order independent, meaning that the order of circumstances for decomposition does not affect the results, and being able to add up components to the total value. Our parametric Shapley value decomposition approach has been a basic built-in toolkit in popular statistical packages, such as STATA and R, which further simplifies the analysis. Though the decomposition should not be seen as causal, it offers an idea of the relative importance of circumstances (Ferreira & Gignoux 2013). We add bootstrap standard errors to the point estimates with 50 replications.
To learn the magnitude and statistical significance of the contribution of childhood circumstances to health inequality, we jointly test multiple parameters in each domain of circumstances. Our null hypothesis is that the specific domain of childhood circumstances does not significantly contribute to health inequality in old age.
3. RESULTS
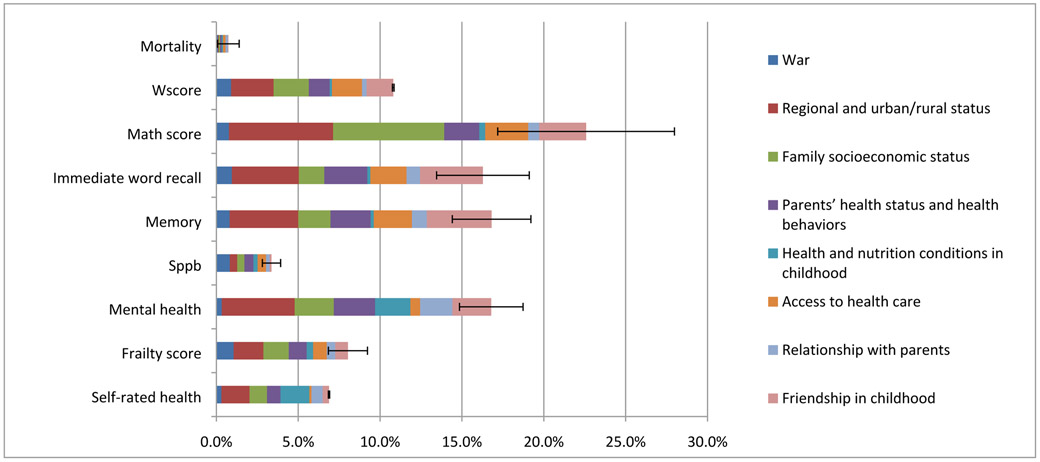
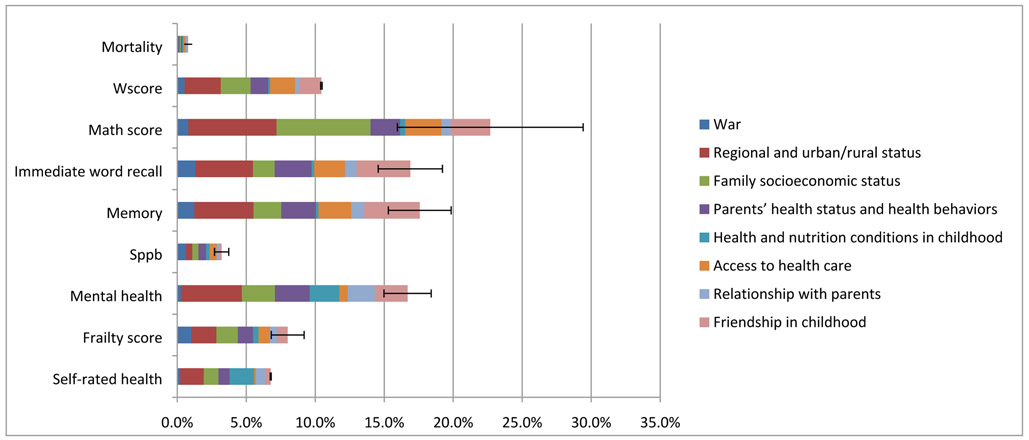
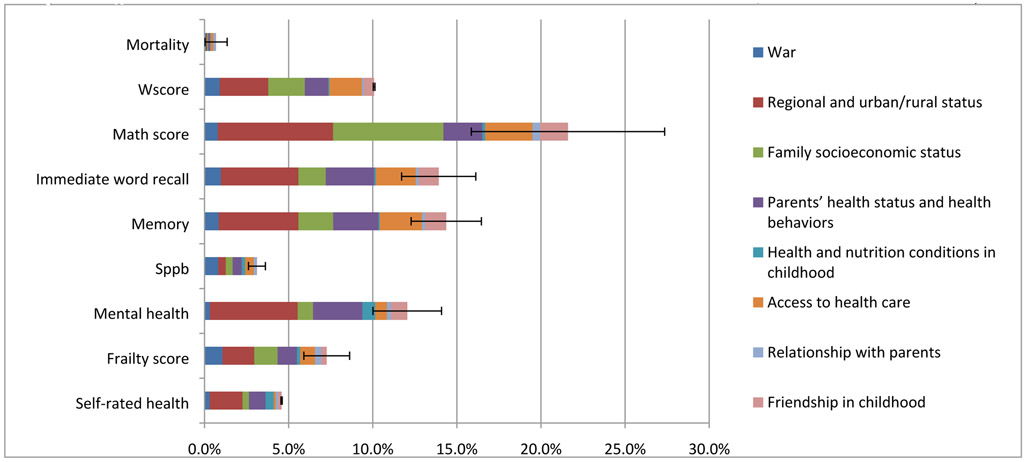
Figure 1 computes the contribution of childhood circumstances to health inequality. Results show that the share of IOP in health amounts to around 0.8% for mortality, 3.2% for SPPB, 6.8% for self-rated health, 8.0% for frailty score, 10.4% for Wscore, 16.7% for immediate word recall, 16.9% for memory and mental health, and 22.7% for math score.
Figure 1. Share of health inequality due to childhood circumstances.
Notes: The 95% confidence interval is displayed. Childhood direct health-related circumstances include three domains, i.e. parents’ health status and health behaviors, health and nutrition conditions, and access to health care. Childhood indirect health-related circumstances involve four domains, i.e. regional and urban/rural status, family socioeconomic status, relationship with parents, and friendship in childhood.
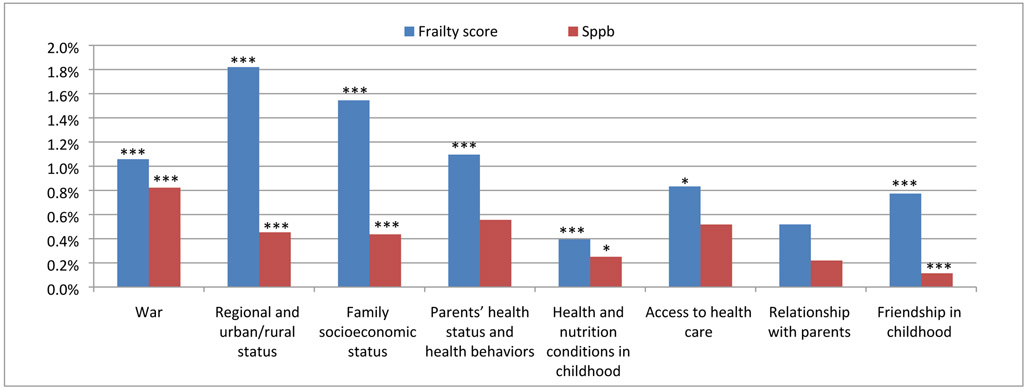
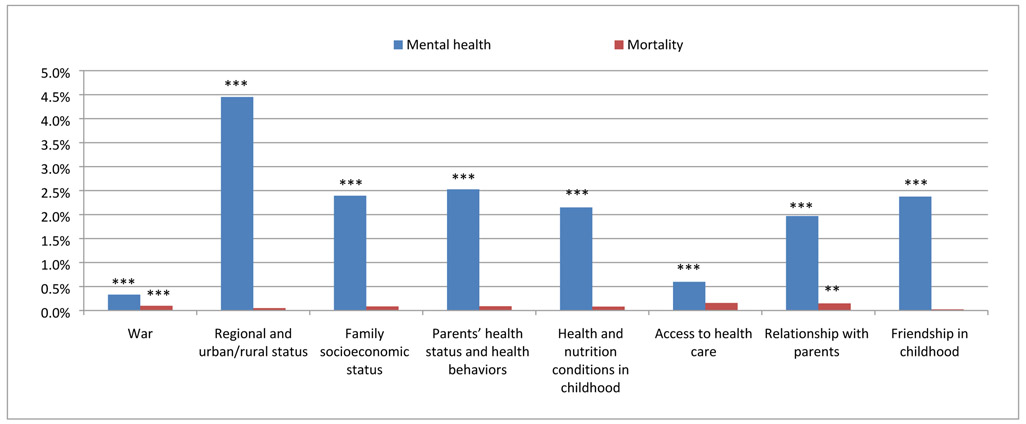
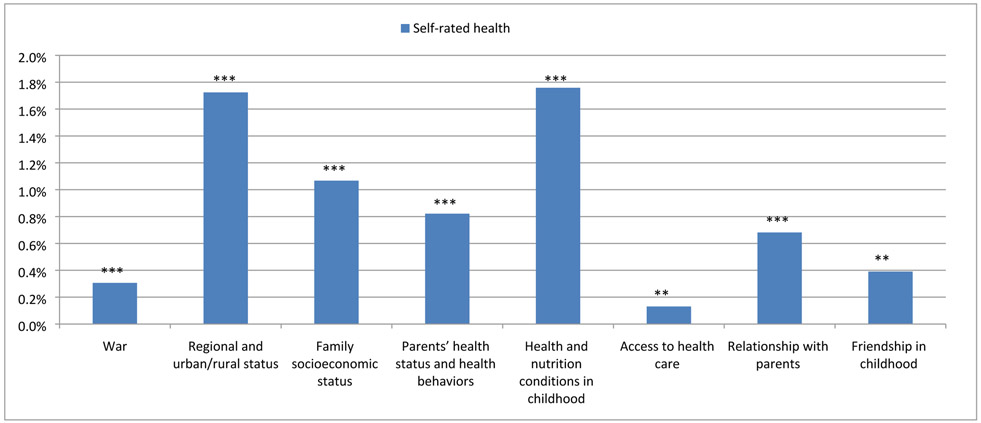
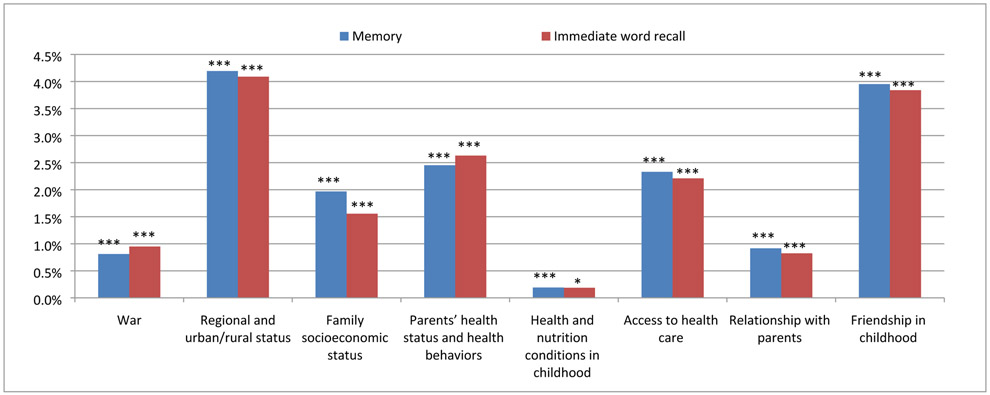
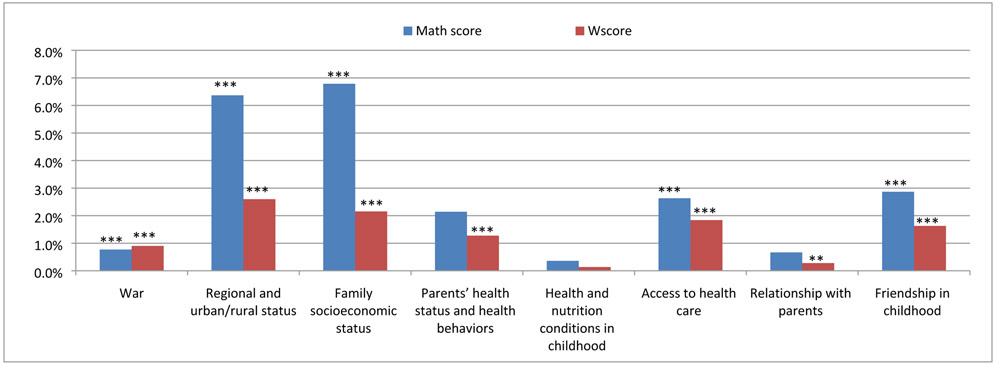
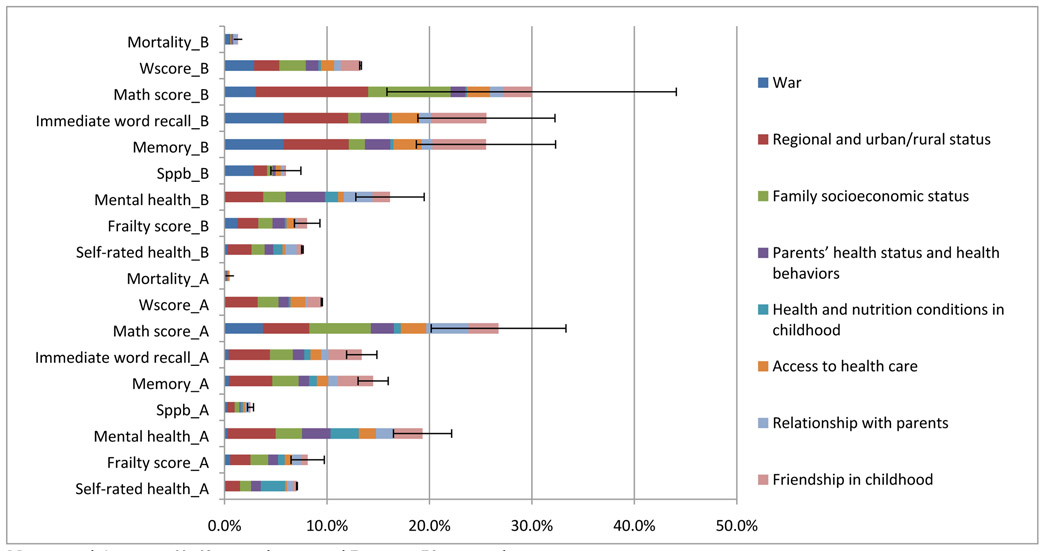
Comparisons of the magnitude and statistical significance of the contributions made by the circumstances variables in Figures 2-6 may shed light on the differential roles played by childhood direct health-related circumstances (i.e. parents’ health status and health behaviors, health and nutrition conditions in childhood, access to health care) and indirect health-related circumstances (i.e. war, regional and urban/rural status at birth, family socioeconomic status, relationship with parents, and friendship in childhood). In total, childhood direct health-related circumstances contribute to 1.3% of health inequality in SPPB, 2.3% of that in frailty score, 2.7% of that in self-rated health, 5.0% of that in memory and immediate word recall, 5.1% of that in math score, 3.2% of that in Wscore, 5.3% of that in mental health, respectively. Childhood indirect health-related circumstances contribute to 2.0% of health inequality in SPPB, 5.7% of that in frailty score, 4.2% of that in self-rated health, 11.8% of that in memory, 11.3% of that in immediate word recall, 17.5% of that in math score, 7.6% of that in Wscore, 11.5% of that in mental health, 0.4% of that in mortality. Therefore, we conclude that indirect health-related circumstances make more sizable contributions to each of the health dimensions than direct health-related circumstances.
Figure 2. The significance and contribution to inequality in physical health by domain of childhood circumstances.
Notes: *p<0.1,**p<0.05, ***p<0.01.
Figure 6. The significance and contribution to inequality in mental health and mortality by domain of childhood circumstances.
Notes: **p<0.05, ***p<0.01.
The analysis of contributions by domain of childhood circumstances could provide further insights behind the findings above. Among direct health-related circumstances, parents’ health and health behaviors contribute significantly to inequalities in almost all health dimensions, such as frailty score (1.1%) (Figure 2), self-rated health (0.8%) (Figure 3), memory (2.5%) and immediate word recall (2.6%) (Figure 4), Wscore (1.3%) (Figure 5), mental health (2.5%) (Figure 6). Health and nutrition conditions in childhood significantly account for inequalities in frailty score (0.4%) and SPPB (0.3%) (Figure 2), self-rated health (1.8%) (Figure 3), memory (0.2%) (Figure 4), mental health (2.1%) (Figure 6). The inequalities attributable to access to health care vary across health outcomes. Access to care does not saliently contribute to SPPB or mortality, but contributes 0.1% to self-rated health, 0.6% to mental health, 0.8% to frailty score, 1.8% to Wscore, 2.2% to immediate word recall, 2.3% to memory, 2.6% to math score (Figures 2-6).
Figure 3. The significance and contribution to inequality in self-rated health by domain of childhood circumstances.
Notes: **p<0.05, ***p<0.01.
Figure 4. The significance and contribution to inequality in word recall by domain of childhood circumstances.
Notes: *p<0.1,***p<0.01.
Figure 5. The significance and contribution to inequality in math score by domain of childhood circumstances.
Notes: **p<0.05, ***p<0.01.
Among indirect health-related circumstances, regional and urban/rural status at birth makes the most sizable and significant contribution to each of the health dimensions (Figures 2-6), such as mental health (4.5%), memory (4.2%), immediate word recall (4.1%), Wscore (2.6%), frailty score (1.8%), self-rated health (1.7%), and SPPB (0.5%) (Figure 2-6). Family socioeconomic status contribute significantly to inequalities in almost all health outcome variables, such as math score (6.8%), mental health (2.4%), Wscore (2.2%), memory (2.0%), immediate word recall (1.6%), frailty score (1.5%), self-rated health (1.1%), and SPPB (0.4%) (Figure 2-6). War contributes significantly to inequalities in all health outcomes variables, such as frailty score (1.1%), immediate word recall (0.9%), Wscore (0.9%), SPPB (0.8%), memory (0.8%), math score (0.8%), mental health (0.3%), self-rated health (0.3%), and mortality (0.1%). Friendship in childhood significantly accounts for inequalities in frailty score (0.8%) and SPPB (0.1%) (Figure 2), self-rated health (0.4%) (Figure 3), memory (4.0%) and immediate word recall (3.8%) (Figure 4), math score (2.9%) and Wscore (1.6%) (Figure 5), and mental health (2.4%) (Figure 6). Relationship with parents in early life only plays a small role in explaining health inequality in self-rated health (0.7%) (Figure 3), memory (0.9%) and immediate word recall (0.8%) (Figures 4), Wscore (0.3%) (Figure 5), mental health (2.0%) and mortality (0.1%) (Figure 5).
Our estimates so far using the MLD are robust to the Variance approach. We perform the Chi-square test between the two approaches to compare the overall size of health inequality attributable to childhood circumstances. The p-value of Chi-square test is 0.97 and the correlation coefficient is 0.57, suggesting no significant difference in overall size of contribution between the MLD approach and the Variance approach. Further checking the size of contribution to health inequality by domain of childhood circumstances, we show in Appendix Table 4 the p-values of Chi-square tests comparing the MLD approach and the Variance approach. Since all p-values of Chi-square tests are close to 1, no significant difference in size of contribution by domain of childhood circumstances is found between the two approaches.
We also evaluate the robustness of the age specification in addition to our linear age form in the main model. First, controlling for a set of age bin dummy variables each representing 5 years of age, i.e. 60-64, 65-69, 70-74, 75-79, 80-84, 85-89, 90-94, 95-99, we show in Appendix Figure 2 that the results are robust. Second, we test results by subsample, i.e. age 60-70 in panel A and age over 70 in panel B of Appendix Figure 3. Compared to main results displayed in Figure 1, the results on total and relative contributions of childhood circumstances by age cohort are also robust.
Finally, in Appendix Figure 4 we remove four self-rated measures of childhood circumstances more susceptible to recall bias and endogeneity concern, including health status before age 15, family financial status, relationship with parents, and neighborhood willingness to help. While the total contribution of childhood circumstances to health in old age slightly declines, the relative contribution by domain of childhood circumstances remains largely robust. Moreover, the relative contributions of direct versus indirect health-related circumstances are also robust to this change.
4. CONCLUSION AND DISCUSSIONS
This paper quantifies the extent to which overall childhood circumstances influence health inequality in old age and evaluates the importance of each domain of circumstances in contributing to health inequality. First, our results show that the total contribution of childhood circumstances to health inequality in old age can be substantial, ranging from 1% to 22% of health inequality across health outcomes. This is smaller than the 21% value of health inequalities in adulthood due to IOP in the UK (Rosa-Dias 2009) except for math score, but much smaller than the value in France where IOP amounts to 45% (Jusot, Tubeuf, and Trannoy 2013).
Second, while both direct and indirect health-related circumstances contribute significantly to health inequality in old age, the latter tends to contribute more. This finding lends support to studies in developed countries that also show a significant effect of indirect health-related circumstances on health in later life (Rosa-Dias & Jones 2007; Trannoy et al. 2010; Bricard et al. 2013). Because social determinants often play an important role beyond health care in promoting population health and health equity, and because countries such as the U.S. and China have been spending an increasingly large portion of national income on health care without the expected gain in population health, our study suggests that more attention should be given to how and to what extent indirect health-related circumstances contribute to health and health inequality.
Third, Specifically, regional and urban/rural status contributes substantially to inequality in almost all health outcomes; while family socioeconomic status makes sizable contribution to inequalities in cognitive ability and mental health.
We also demonstrate the value of life course approach in identifying key determinants of health among older people. To improve the health of older persons, further studies are needed to develop and evaluate successful interventions. Distinguishing sources of health inequality and rectifying inequality due to key circumstances should be the basis of policy that promotes health equity.
Further work is required to identify if IOP in the health of older persons is driven directly by childhood circumstances or through intergenerational transmission of unhealthy lifestyle patterns. The former would largely require policies compensating for poorer initial circumstances, while the latter may call for policies reducing social reproduction and the intergenerational transmission of unhealthy lifestyle. However, substantive equality of opportunity requires compensating for the influence of family and social origins on individual health outcomes, regardless of the channel through which it operates, as childhood circumstances lie beyond individual responsibility and choices (Roemer 1993; Lefranc, Pistolesi, & Trannoy 2008).
This paper focuses on the contributions of different types of circumstances on IOP in health. The main strengths of this study include: we provide one of the first evidence of IOP in health in old age, especially the first such evidence from a developing country; introduce a new method – the Shapley Value Decomposition – to quantify the size of health inequality due to circumstances; apply a newly released high-quality life history data; advance the life course epidemiology via exploring a more than 60-year long time window; and measure comprehensive dimensions of health outcomes.
This study also has limitations for improvement. First, this observational study does not aim to offer a causal interpretation of the link between a specific early life environment and health in old age. As an initial step towards understanding the relative contribution of a rich set of early life environments, we isolate the statistical variations in health attributable to each domain of childhood circumstances with recognition of limitations including endogeneity of recalled circumstances and both overestimation (due to overfitting) and underestimation (due to unobserved childhood circumstances). Based on our findings, future studies will investigate causal inference for specific key circumstances that may lead to eventual interventions. Second, because childhood conditions in the life history survey are based on recall, they may suffer from reporting errors. Third, in addition to considering early life exposures to key historical events like wars and recessions, future studies may improve the measurement of exposures, for example, by considering the length and intensity of early life exposures, as both the extensive margin and the intensive margin may take a toll on older persons.
Acknowledgements
Dr. Yan is supported by the Natural Science Foundation of China (71974097, 71503129), the Fundamental Research Funds for the Central Universities (KJQN201628) and the Fundamental Research Funds for the Central Universities (SKCX2019006), a project funded by the Priority Academic Program Development of Jiangsu Higher Education Institute (PAPD), a research grant by China Center for Food Security Studies at Nanjing Agricultural University, and Jiangsu Center of Agricultural Modernization. We are grateful to Maya Mahin for research assistance. The authors declare that there is no conflict of interest regarding the preparation of this manuscript. Dr. Gill is the recipient of an Academic Leadership Award (K07AG043587) from the National Institute on Aging. Drs. Gill and Chen are supported by the Yale Claude D. Pepper Older Americans Independence Center (P30AG21342). Dr. Chen acknowledges financial support from the James Tobin Research Fund at Yale Economics Department, NIH/NIA grants (R03AG048920; K01AG053408), and faculty research grant awarded by Yale Macmillan Center (2017-2019).
Appendix
Appendix Table 1.
Summary Statistics of Health Outcome Measures
| Dimensions and Measures of Health | Obs | Mean | SD | Min | Max | Variable Description | |
|---|---|---|---|---|---|---|---|
| Self-rated health | Self-rated health | 8255 | 3.9 | 0.8 | 1 | 5 | Would you say your health is excellent, very good, good, fair, or poor? 1. excellent, 2. very good, 3. good, 4. fair, 5. poor. The average value of self-rated health between 2013 and 2015, |
| Physical health | SPPB score | 7479 | 9.6 | 2.6 | 0 | 12 | The average value of SPPB score between 2013 and 2015, |
| Chair stand score | 7705 | 3.0 | 1.2 | 0 | 4 | The ability and time to complete 5 repeated risings from chair exercise (0: cannot complete; 1: more than 16.6 seconds; 2: more than 13.6 seconds but less than 16.6 seconds; 3: more than 11.1 seconds but less than 13.6 seconds; 4: less than 11.1 seconds.) | |
| Balance score | 7538 | 3.6 | 1.0 | 0 | 4 | The ability and time to complete side-by-side or the full tandem exercise of the balance test (0: cannot complete the 10 seconds side-by-side exercise of the balance test; 1: less than 10 seconds to do side-by-side;2: less than 3 seconds to do full tandem exercise; 3: more than 3 seconds but less than 10 seconds to do full tandem exercise; 4: more than 10 seconds to do full tandem exercise) | |
| Walk speed score | 7684 | 2.9 | 1.1 | 0 | 4 | The ability and time to walk 5 meters (0: cannot complete or not qualified; 1: more than 11.4 seconds; 2: more than 8.2 seconds but less than 11.4 seconds; 3: more than 6.4 seconds but less than 8.2 seconds; 4: less than 6.4 seconds.) | |
| Frailty score | 7552 | 2.0 | 1.0 | 0 | 5 | ||
| Low grip strength | 7552 | 0.3 | 0.4 | 0 | 1 | stratified by gender and body mass index quantiles with cutoffs (0: more than the cutoff; 1: no more than the cutoff) | |
| Slow walk speed | 7604 | 0.7 | 0.4 | 0 | 1 | stratified by gender and height with cutoffs (0: no more than the cutoff; 1: more than the cutoff) | |
| Weight loss | 7682 | 0.4 | 0.4 | 0 | 1 | “Have you involuntarily lost 5 or more kilograms in the past year?” | |
| Exhaustion | 8266 | 0.3 | 0.4 | 0 | 1 | Two CES-D questions are used. (a) I felt everything I did was an effort; (b) I could not get “going”. The question is asked “how you have felt and behaved during the last week?” 1=rarely or none of the time (<1 day) 2=some or a little of the time (1-2 days) 3=occasionally or a moderate amount of the time (3-4 days) 4=most or all of the time (5-7 days). Subjects answering “3” or “4” to either of these questions are categorized as exhausted | |
| Low physical activity | 8266 | 0.3 | 0.4 | 0 | 1 | If elders whose SPPB=0; or if one can get up from a chair after sitting for a long time; or if one can get into or out of bed by oneself. | |
| Cognitive ability | Math score | 7408 | 2.6 | 1.9 | 0 | 5 | Based on a task in which respondents are asked to subtract 7 from 100 and to continue subtracting 7 from each subsequent number for a total of five times. The score is the count of correct subtractions across the five trials. |
| Wscore | 7888 | 447.1 | 102.6 | 299 | 635 | Wscore is used to standardize adaptive number series test in 2015 | |
| Memory | 8042 | 2.8 | 1.7 | 0 | 10 | The average value of immediate word recall and delay word recall | |
| Immediate Word Recall | 8042 | 3.3 | 1.7 | 0 | 10 | A list of 10 nouns read to the respondent who is asked to recall as many words as possible in any order. The score is the count of the number of words correctly recalled that ranges from 0 to 10. | |
| Mental health | Depressive symptoms | 7667 | 8.5 | 5.8 | 0 | 30 | The Center for Epidemiological Studies Depression Scale (CES-D) 10-item version; each item scores from 0 to 3; the total mental health score is from 0 to 30. |
| Mortality | Alive in 2015 or not | 8134 | 0.03 | 0.16 | 0 | 1 | Alive in 2015 or not (0: alive; 1: died) |
Notes:The cutoffs for low grip strength (kg) are 29 (males, BMI<=24), 30 (male, 24<BMI<=28), 32 (male, BMI>28), 17 (female, MBI<=23), 17.3 (female, 23<BMI<=26), 18 (female, 26<BMI<=29), 21 (female, BMI>29). The cutoffs for low walk speed are 0.65m/s (male, height<=173 cm; female, height<=159 cm), and 0.76m/s (male, height>173 cm; female, height>159 cm).
Appendix Table 2.
Correlation among Health Outcome Measures
| Self-rated health | Frailty score | Mental health | Sppb | Memory | Immediate word recall | Math score | Wscore | |
|---|---|---|---|---|---|---|---|---|
| Self-rated health | 1.000 | |||||||
| Frailty score | 0.247* | 1.000 | ||||||
| Mental health | 0.419* | 0.367* | 1.000 | |||||
| Sppb | −0.203* | −0.451* | −0.214* | 1.000 | ||||
| Memory | −0.123* | −0.241* | −0.216* | 0.260* | 1.000 | |||
| Immediate word recall | −0.118* | −0.233* | −0.206* | 0.258* | 0.934* | 1.000 | ||
| Math score | −0.081* | −0.169* | −0.195* | 0.231* | 0.357* | 0.350* | 1.000 | |
| Wscore | −0.073* | −0.178* | −0.176* | 0.255* | 0.409* | 0.409* | 0.458* | 1.000 |
Notes: since people who died during 2014 life history survey and 2015 follow-up survey have no information on other health outcomes, there is no correlation between died2015 with other 8 health outcomes. Star * means significance level at 1%.
Appendix Table 3.
Pairwise correlations between self-reported health status in childhood and in old age
| Self-rated health | Frailty score | Mental health | SPPB | Memory | Immediate word recall | Math score | Wscore | |
|---|---|---|---|---|---|---|---|---|
| self-rated health before age 15 | 0.140* | 0.062* | 0.130* | −0.042* | −0.070* | −0.060* | −0.041* | −0.043* |
| self-rated family financial status in childhood | 0.106* | 0.074* | 0.148* | −0.006 | −0.079* | −0.079* | −0.068* | −0.072* |
| relationship with parents | 0.073* | 0.011 | 0.086* | −0.012 | −0.076* | −0.078* | −0.027 | −0.045* |
| neighborhood willingness to help | −0.062* | −0.061* | −0.112* | −0.006 | 0.211* | 0.209* | 0.100* | 0.148* |
Note: indicates statistical significance at 1% level, SPPB= Short Physical Performance Battery, Wscore is used to standardize adaptive number series test in the 3rd wave of CHARLS in 2015, which measures a specific form of fluid intelligence related to quantitative reasoning (Strauss et al., 2018).
Appendix Table 4.
Chi-square tests between MLD and Variance approaches across health outcomes
| Self-rated health | Frailty score | Mental health | SPPB | Memory | Immediate word recall | Math score | Wscore | Mortality | |
|---|---|---|---|---|---|---|---|---|---|
| P value of Chi square test | 0.96 | 0.94 | 1.00 | 0.98 | 1.00 | 1.00 | 0.97 | 1.00 | 0.92 |
Note: MLD = Mean Logarithmic Deviation. SPPB= Short Physical Performance Battery, Wscore is used to standardize adaptive number series test, which measures a specific form of fluid intelligence related to quantitative reasoning (Strauss et al., 2018).
Appendix Figure 1:
Flow chart of study sample
Appendix Figure 2.
Share of health inequality due to childhood circumstances (Including a set of dummy variables representing age bins, each age bin is five years of age) (95% confidence interval)
Appendix Figure 3. Share of health inequality due to childhood circumstances cross cohorts.
Note: panel A means 60-69 age cohort, panel B means 70+ age cohort.
Appendix Figure 4. Share of health inequality due to childhood circumstances (omitting four self-rated childhood circumstances measures in the main estimations, 95% confidence interval).
Note: The four self-rated childhood circumstances omitted include health status before age 15, family financial status, relationship with parents, and neighborhood willingness to help.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The 150 county-level units were randomly selected using probability proportional to size (PPS) and stratified by region, urban/rural and county-level gross domestic product (GDP). Within each county-level unit, three village-level units (villages in rural areas and urban communities in urban areas) were randomly selected using PPS as primary sampling units (PSUs). Within each PSU, 80 dwellings were randomly selected from a complete list of dwelling units generated from a mapping or listing operation, using augmented Google Earth maps (Google Inc) along with considerable ground checking. In scenarios with more than one age-eligible household in a dwelling unit, one was randomly selected. From this sample for each PSU, the proportion of households with age-eligible members was determined, as was the proportion of empty residences. From these proportions and an assumed response rate, we selected households from our original PSU frame to obtain a target number of 24 age-eligible households per PSU. Thus, the final household sample size in a PSU depended on the PSU age-eligibility and empty residence rates. In each household, one person aged 45 years or older was randomly chosen as the main respondent, and the individual’s spouse was automatically included. On the basis of this sampling procedure, 1 or 2 individuals in each household were interviewed depending on the marital status of the main respondent.
Let us suppose there are two individuals with logarithmic values of health outcome lux1 and lnx2, respectively. According to Jensen's Inequality, MLD increases with inequality –(lnx1 +lnx2)/2 > – ln [(x1 + x2)/2]. The MLD is nonnegative, takes the value zero when everyone has the same health status, and takes larger positive values as health becomes more unequal.
Contributor Information
Binjian Yan, College of Economics and Management, Nanjing Agricultural University and Department of Health Policy and Management, Yale School of Public Health.
Xi Chen, Department of Health Policy and Management, Yale School of Public Health and Department of Economics, Yale University.
Thomas M. Gill, Department of Internal Medicine, School of Medicine, Yale University.
References
- Andersson L, Stevens N (1993). Associations between early experiences with parents and well-being in old-age. Journals of Gerontology,Series B: Psychological Sciences and Social Sciences, 48(3), P109–P116. [DOI] [PubMed] [Google Scholar]
- Ayyagari P, Frisvold D (2016). The impact of social security income on cognitive function at older ages. American Journal of Health Economics, 2, 463–488. [Google Scholar]
- Barbosa E (2016). Overall unfair inequality in health care: an application to Brazil PhD thesis, University of York. [Google Scholar]
- Bjorklund A, Jantti M, Roemer J (2012). Equality of Opportunity and the Distribution of Long-run income in Sweden. Social Choice and Welfare, 39, 675–696. [Google Scholar]
- Black S, Devereux P, Salvanes K (2016) Does grief transfer across generations? Bereavements during Pregnancy and Child Outcomes. American Economic Journal: Applied Economics, 8(1), 193–223. [Google Scholar]
- Bor J, Cohen G, Galea S (2017). Population health in an era of rising income inequality: USA, 1980–2015. The Lancet, 389, 1475–1490. [DOI] [PubMed] [Google Scholar]
- Bricard D, Jusot F, Trannoy A, Tubeuf S (2013). Inequality of opportunity in health and the principle of natural reward: evidence from European Countries. Research on Economic Inequality, 21, 335–370. [Google Scholar]
- Carpantier J, Sapata C(2013). An ex-post view of inequality of opportunity in France and its regions. Journal of Labor Research, 34, 281–311. [Google Scholar]
- Carranza R,Hojman D (2015). Inequality of opportunity in health and cognitive abilities: the case of Chile Serie de documentos, University of Chile, Santiago. [Google Scholar]
- Cooper R, Hardy R, Bann D et al. (2014) Body mass index from age 15 years onwards and muscle mass, strength and quality in early old age. Journal of Gerontology, Series A: Biological Sciences and Medical Sciences,69, 1253–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunha F, Heckman J (2009). The economics and psychology of inequality and human development. Journal of the European Economic Association, 7, 320–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl E, Birkelund G (1997). Health inequalities in later life in a social democratic welfare state. Social Science & Medicine, 44, 871–881. [DOI] [PubMed] [Google Scholar]
- Dodds R, Denison HJ, Ntani G et al. (2012). Growth in early life and muscle strength: a systematic review and meta-analysis. Journal of Nutrition, Health &Aging, 16: 609–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fajardo-Gonzalez J(2016). Inequality of opportunity in adult health in Colombia. Minnesota Population Center, University of Minnesota, Working Paper No.2016–2. [Google Scholar]
- Ferreira F, Gignoux J, 2011. The measurement of inequality of opportunity: theory and an application to Latin American, Review of Income and Wealth 57(4): 622–657. [Google Scholar]
- Ferreira F, Gignoux J (2013). The measurement of educational inequality: achievement and opportunity. World Bank Economic Review, 28, 210–246. [Google Scholar]
- Fleurbaey M, Schokkaert E(2009). Unfair inequalities in health and health care. Journal of Health Economics, 28(1), 73–90. [DOI] [PubMed] [Google Scholar]
- Fried L, Tangen C, Walston J, Newman A, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop W, Burke G, McBurnie M (2001). Frailty in Older Adults: Evidence for a Phenotype. Journal of Gerontology, Series A: Biological Sciences and Medical Sciences, 56(3), M146–M156. [DOI] [PubMed] [Google Scholar]
- Gale C, Booth T, Starr J, Deary I (2016). Intelligence and socioeconomic position in childhood in relation to frailty and cumulative allostatic load in later life: the Lothian Birth Cohort 1936. Journal of Epidemiology and Community Health, 70, 576–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Gomez P, Schokkaert E, Ourti T, dUva T (2014). Inequity in the face of death. Health Economics, 24, 1348–1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill T, Gahbauer E, Allore H, Han L(2006). Transitions between frailty states among community-living older persons. Archives of Internal Medicine, 166, 418–423. [DOI] [PubMed] [Google Scholar]
- Guralnik J, Simonsick E, Ferrucci L, Glynn R, Berkman L, Blazer D, Scherr P, Wallace R(1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology, Series A:Medical Sciences, 49(2), M85–M94. [DOI] [PubMed] [Google Scholar]
- Haughton J and Khandker SR 2009. Handbook on Poverty and Inequality. Washington, DC: World Bank; http://documents.worldbank.org/curated/en/488081468157174849/Handbook-on-poverty-and-inequality [Google Scholar]
- Hong Y, Zhou Z, Fang Y, Shi L (2017). The digital divide and health disparities in China: evidence from a national survey and policy implications. J Med Internet Res, 19(9): e317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hufe P, Peichl A, Roemer J, Ungerer M(2017). Inequality of income acquisition:the role of childhood circumstances. Social Choice and Welfare, 49, 1–46. [Google Scholar]
- Juarez F, Soloaga I (2014). IOP: Estimating ex-ante inequality of opportunity. The Stata Journal, 14, 830–846. [Google Scholar]
- Jusot F, Mage S, Menendez M(2014). Inequality of opportunity in health in Indonesia. Document De Travail, DT/2014-06, UMR DIAL 225. [Google Scholar]
- Jusot F, Tubeuf S, Trannoy A (2013). Circumstances and Efforts: how important is their correlation for the measurement of inequality of opportunity in Health? Health Economics, 22, 1470–1495. [DOI] [PubMed] [Google Scholar]
- Kanbur R, and Wagstaff A (2016). How Useful Is Inequality of Opportunity as a Policy Construct?In Inequality and Growth: Patterns and Policy, Volume 1: Concepts and Analysis, ed. Kaushik Basu and Stiglitz Joseph E., 131–148. London: Palgrave McMillan. [Google Scholar]
- Katikireddi S(2016). Economic Opportunity: a determinant of health? Lancet Public Health, 1, E4–E5. [DOI] [PubMed] [Google Scholar]
- Krause N (1998). Early parental loss, recent life events, and changes in health among older adults. Journal of Aging and Health, 10, 395–421. [DOI] [PubMed] [Google Scholar]
- Kuh D, Hardy R, Butterworth S, Okell L et al. (2006) Developmental origins of midlife grip strength: findings from a birth cohort cohort study. Journal of Gerontology, Series A: Biological Sciences and Medical Sciences, 61, 702–06. [DOI] [PubMed] [Google Scholar]
- Lazar A(2013). Ex-ante and Ex-post measurement of inequality of opportunity in health: evidence from Israel In Dias Pedro Rosa, O’Donnell Owen, editors, Health and Inequality (Research on Economic Inequality, vo.21), Emerald Group Publishing Limited, 371–395. [Google Scholar]
- Lefranc A, Pistolesi N, Trannoy A (2008) Inequality of opportunities VS inequality of outcomes: are western societies all alike? Review of Income and Wealth, 54, 513–546. [Google Scholar]
- Marmot M, Friel S, Bell R, Houweling T, Taylor S (2008). Closing the gap in a generation: health equity through action on the social determinants of health. The Lancet, 372, 1661–1669. [DOI] [PubMed] [Google Scholar]
- McEniry M, Palloni A, Davila A, Gurucharri A (2008). Early life exposure to poor nutrition and infectious diseases and its effects on the health of older Puerto Rican adults. Journal of Gerontology, Series B: Psychological Sciences and Social Sciences, 63(6), S337–S348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moody-Ayers S, Lindquist K, Sen S, Covinsky K(2007). Childhood social and economic well-being and health in older age. American Journal of Epidemiology, 166, 1059–1067. [DOI] [PubMed] [Google Scholar]
- Pal R(2015). Inequality in maternal health care utilization in India: a Shapley decomposition analysis. Journal of International Development, 27(7), 1141–1152. [Google Scholar]
- Palloni A, McEniry M, Davila A, Gurucharri A (2005). The influence of early conditions on health status among elderly Puerto Ricans. Social Biology, 52(3-4), 132–163. [DOI] [PubMed] [Google Scholar]
- Persson P, Rossin-Slater M (2017). Family ruptures, stress, and the mental health of the next generation. American Economic Review, forthcoming. [PubMed] [Google Scholar]
- Ramos M (2007). Impact of socioeconomic status on Brazilian elderly health. Revista De Saude Publica, 41, 616–624. [DOI] [PubMed] [Google Scholar]
- Roemer J (1993). A Pragmatic Theory of Responsibility for the Egalitarian Planner. Philosophy and Public Affairs, 22, 146–66. [Google Scholar]
- Roemer J, Aaberge R, Colombino U, Fritzell J, Jenkins S, Lefranc A, Marx I, Page M, Pommer E, Ruiz-Castillo J, Segundo M, Tranaes T, Trannoy A, Wagner G, Zubiri I (2003). To what extent do fiscal regimes equalize opportunities for income acquisition among citizens? Journal of Public Economics, 87, 539–565. [Google Scholar]
- Roemer J, Trannoy A (2016). Equality of Opportunity: theory and measurement. Journal of Economic Literature, 54, 1288–1332. [Google Scholar]
- Rosa-Dias P (2009). Inequality of opportunity in Health: evidence from a UK cohort study. Health Economics, 18, 1057–1074. [DOI] [PubMed] [Google Scholar]
- Rosa-Dias R, Jones A (2007). Giving equality of opportunity a fair innings. Health Economics, 16(2), 109–112. [DOI] [PubMed] [Google Scholar]
- Rueda S, Artazcoz L, Navarro V (2008). Health inequalities among the elderly in Western Europe. Journal of Epidemiology & Community Health, 62, 492–498. [DOI] [PubMed] [Google Scholar]
- Runge S, Craig B, Jim H (2015). Word recall: cognitive performance within internet surveys. Journal of Medical Internet Research Mental Health, 2(2), e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayer AA, Syddall HE, Gilbody HJ, Dennison EM, Cooper C. (2004). Does sarcopenia originate in early life? Findings from the Hertfordshire Cohort Study. Journal of Gerontology, Series A: Biological Sciences and Medical Sciences,59, M930–M934. [DOI] [PubMed] [Google Scholar]
- Shen K, Zeng Y (2014). Direct and indirect effects of childhood conditions on survival and health among male and female elderly in China, Social Science & Medicine, 119, 207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen Y (2014). Community building and mental health in mid-life and older life: evidence from China. Social Science & Medicine, 107, 209–216. [DOI] [PubMed] [Google Scholar]
- Shorrocks AF 1980. The Class of Additively Decomposable Inequality Measures". Econometrica. 48 (3): 613–625. [Google Scholar]
- Shorrocks A (2013). Decomposition procedures for distributional analysis: a unified framework based on the Shapley value. Journal of Economic Inequality, 11(1), 99–126. [Google Scholar]
- Simmonds SJ, Syddall HE, Westbury LD, Dodds RM, Cooper C, Sayer AA. (2015). Grip strength among community-dwelling older people predicts hospital admission during the following decade. Age Ageing, 44, 954–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss J, Witoelar F, Meng Q, Chen X, Zhao Y, Sikoki B, Wang Y, 2018, Cognition and SES relationships among the Mid-aged and elderly: a comparison of China and Indonesia, NBER Working Paper 24583. [Google Scholar]
- Thorslund M, Lundberg O (1994). Health and Inequalities among the oldest old. Journal of Aging Health, 6, 51–69. [DOI] [PubMed] [Google Scholar]
- Tomasetti C, Li L, Vogelstein B (2017). Stem cell divisions, somatic mutations, cancer etiology, and cancer prevention. Science, 355, 1330–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trannoy A, Tubeuf S, Jusot F, Devaux M (2010). Inequality of opportunities in Health in France: a First Pass. Health Economics, 19, 921–938. [DOI] [PubMed] [Google Scholar]
- United Nations Department of Economic and Social Affairs Population Division (2015). World Population Ageing 2015 (ST/ESA/SER.A/390). [Google Scholar]
- Venkataramani A, Brigell R, O’Brien R, Chatterjee P, Kawachi I, Tsai A (2016). Economic opportunity health behaviours and health outcomes in the USA: a population-based cross-sectional study. Lancet Public Health, 18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wendelspiess Chávez Juárez F, Soloaga I. 2014. iop: Estimating ex-ante inequality of opportunity. Stata J. 14(4): 830–46. [Google Scholar]
- World Health Organization. (2017). Constitution of WHO: principles. http://www.who.int/about/mission/. [Google Scholar]
- Zhang Z, Gu D, Hayward M (2008). Early life influences on cognitive impairment among oldest old Chinese. Journal of Gerontology, Series B: Psychological Sciences and Social Sciences, 63(1), S25–S33. [DOI] [PubMed] [Google Scholar]
- Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. (2014). Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol,43(1):61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]