Abstract
The perinatal period is a high-risk time for mood deterioration among women vulnerable to depression. This study examined feasibility, acceptability, and improvement associated with mindfulness-based cognitive therapy (MBCT) in perinatal women with major depressive disorder (MDD) or bipolar spectrum disorder (BSD). Following a diagnostic evaluation, 39 perinatal women with a lifetime history of MDD (n = 27) or BSD (n = 12) enrolled in an 8-week program of MBCT classes (2 h each) that incorporated meditation, yoga, and mood regulation strategies. Participants were pregnant (n = 12), planning pregnancy (n = 11), or up to 1-year postpartum (n = 16). Participants were self-referred and most had subthreshold mood symptoms. Assessments of depression, (hypo)mania, and anxiety were obtained by interview and self-report at baseline, post-treatment and at 1- and 6-month post-treatment. Women with a history of MDD were more likely to complete the classes than women with BSD. Of 32 women who completed the classes, 7 (21.9 %) had a major depressive episode during the 6-month post-treatment follow-up. On average, participants with MDD reported improvements in depression from pre- to post-treatment. Mood improvement was not observed in the BSD group. In the full sample, improvements in depression symptoms across time points were associated with increasing mindful tendency scores. This study was limited by its uncontrolled design, heterogeneous sample, and questionnaire-based assessment of mindfulness skills. MBCT may be an important component of care for perinatal women with histories of major depression. Its applicability to perinatal women with BSD is unclear.
Keywords: Meditation, Pregnancy, Postpartum, Feasibility, Acceptability, Mania, Depression
Introduction
For women with a vulnerability to mood disorders, the perinatal period—broadly defined as the interval in which women are planning pregnancy, pregnant, or postpartum—is a high-risk time for major depressive episodes. Between 8.5 and 11.0 % of women in the general population develop major or minor depression during pregnancy, and between 6.5 and 12.9 % in the first postpartum year (Gaynes et al. 2005). This risk is elevated approximately 2–3 times among women with histories of major depressive disorder (MDD; Goodman and Tully 2009). Left untreated, many women with MDD remain depressed for as long as 1 year following childbirth (Goodman 2009).
Women with bipolar spectrum disorders (BSDs; i.e., bipolar I, II or not otherwise specified disorders) are also at high risk for mood recurrences during pregnancy, and at a higher risk for recurrences in the 6-month postpartum than women with recurrent MDD (Di Florio et al. 2013; Viguera et al. 2007, 2011). These findings underscore the importance of prevention of mood episodes during the preconception, pregnancy, or postpartum periods among women with histories of depressive or bipolar disorders.
Recent efforts to prevent depressive episodes among perinatal women have evaluated an extension of the 8-week mindfulness-based cognitive therapy (MBCT) program (Segal et al. 2012). MBCT aims to interrupt the tendency to respond with strong emotions to particular thoughts or bodily sensations that occur with sad mood, through training individuals to notice and step out of habitual and automatic modes of responding with intentional, non-judgmental, and present-focused awareness. MBCT has a strong evidence base for the prevention of depressive recurrence among patients with MDD, especially those with three or more prior episodes (Piet and Hougaard 2011).
Dimidjian et al. (2014) adapted the MBCT program to be sensitive and specific to the physical and emotional experiences of pregnant women with lifetime histories of major depression. Results of a two-site open trial suggested that women reported high interest, engagement and satisfaction with MBCT classes and home practice. Moreover, there was significant improvement in depression symptoms and low rates of recurrence (18.8 %) during a 6-month postpartum interval. The current study expands upon the Dimidjian et al. trial by examining the feasibility, acceptability, and clinical benefits of MBCT in a broad and nonoverlapping sample of perinatal women (i.e. preconception, pregnant, and postpartum) with histories of depression and/or (hypo)mania.
Although originally developed as a preventive approach for individuals with recurrent MDD, studies support the extension of MBCT to individuals with BSD. In an open trial, men and women with bipolar I or II disorder who received MBCT showed significant improvement over 3 months in subthreshold depression and suicidal symptoms (Miklowitz et al. 2009). Several other open trials of MBCT have reported effects on depression or anxiety symptoms in patients with bipolar I or II disorder over 3 months (Deckersbach et al. 2012; Williams et al. 2008). The only randomized trial of MBCT in bipolar disorder, however, showed no significant benefit of the classes compared to usual care on depression or hypomania symptoms over 12-months (Perich et al. 2013).
We conducted a two site open trial of MBCT in perinatal women with lifetime diagnoses of MDD or BSD and mild/moderate current depressive symptoms. To be eligible, women had to be pregnant, planning pregnancy, or up to 1-year post-partum. We included women in the preconception phase because it is often the time when women decide whether or not to take medications while pregnant. The standard of clinical practice for treating women with bipolar disorder—especially if they have had a recent mood episode—is to continue mood stabilizers and/or second generation antipsychotics during pregnancy. However, certain standard mood stabilizers (e.g., divalproex sodium) have teratogenic effects in the first trimester (Cohen 2007). Likewise, questions have been raised about the safety of selective serotonin reuptake inhibitors in women with MDD (Bar-Oz et al. 2007). Thus, preventative psychosocial treatments are as relevant in the preconception phase as in pregnancy or the postpartum phases, especially among women with mood disorders who seek alternatives to pharmacotherapy.
The first objective of this study was to examine the feasibility of identifying and enrolling perinatal women with lifetime histories of MDD or BSD in the MBCT prevention program and evaluate its acceptability, as indicated by retention rates and post-treatment satisfaction ratings. The secondary objective was to examine whether MBCT is associated with decreases in subthreshold depressive symptoms during the 8 weeks treatment and a 1- and 6-month post-treatment follow-up. Subthreshold depressive symptoms are strong correlates of functional impairment in patients with depression and bipolar disorder and are prospectively associated with time to recurrence (e.g., Rush 2007; Judd et al. 2008). Thus, interventions that reduce residual symptoms are likely to have preventative effects on time to recurrence and degree of disability in both disorders. We hypothesized that (1) there would be improvements in self-reported depression (primary outcome) and clinician-observed depressive symptoms (secondary outcome) among perinatal women from before to after the MBCT classes, and (2) post-treatment rates of relapse would be comparable to those reported in other preventative studies with perinatal women with depression (Goodman 2009). To determine whether the effects of MBCT were specific to depression, we explored change in measures of hypomania/mania and anxiety over the same interval.
Given the limited research on MBCT with perinatal populations, we explored these differences in symptomatic outcomes by diagnostic category (MDD, BSD), perinatal status (preconception, pregnant, and postpartum), and study site. Finally, we explored the degree of self-reported change in daily mindful tendency scores from before to after MBCT, and the association between improvement in mindful tendency scores and depressive symptoms.
Method
Participants
The trial was conducted at the University of Colorado, Boulder and the University of California, Los Angeles (UCLA) Semel Institute. Participants were women with mood disorders who responded to study advertisements posted by investigators at OB-GYN clinics and perinatal health organizations. Eligible participants met the following criteria:
Pregnant (up to 32 weeks gestation), within one year postpartum, or not pregnant but actively trying to conceive;
Diagnostic and Statistical Manual of Mental Disorders, 4th Ed., Text Rev. (DSM-IV-TR; American Psychiatric Association 2000) lifetime diagnosis of MDD or bipolar I, bipolar II, bipolar not otherwise specified (NOS), or cyclothymic disorder, as determined by the Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Patient Edition (SCID-I/P; First et al. 2002);
Current subthreshold symptoms of depression (see Table 1);
Spoke and read English, even if it was not their first language;
Age 18 or older.
Table 1.
Demographic information, perinatal status, and baseline mental health status of 39 participants by site and diagnosis
| Variable | Colorado |
UCLA |
Total |
|||
|---|---|---|---|---|---|---|
| BSDa n = 7 |
MDDb n = 10 |
BSD n = 5 |
MDD n = 17 |
BSD n = 12 |
MDD n = 27 |
|
| Mean age (SD) | 33.6 (3.3) | 34.8 (3.6) | 33.8 (3.3) | 35.5 (6.0) | 33.7 (3.1) | 35.2 (5.2) |
| Mean (SD) baseline symptom scoresc | ||||||
| BDI-II | 4.0 (1.5) | 9.3 (6.9) | 12.8 (12.6) | 17.1 (11.1) | 7.7 (8.9) | 14.2 (10.3) |
| HRSD | 3.1 (2.3) | 4.1 (3.5) | 4.6 (5.0) | 7.3 (3.5) | 3.8 (3.6) | 6.1 (4.8) |
| YMRS | 2.9 (3.4) | 0.6 (1.3) | 5.8 (4.7) | 1.8 (1.6) | 4.1 (4.1) | 1.4 (1.6) |
| STAI-C | 45.1 (3.8) | 43.9 (4.6) | 41.8 (5.8) | 42.6 (4.7) | 43.8 (4.8) | 43.1 (4.6) |
| FFMQ | 135.4 (12.6) | 115.7 (21.8) | 128.4 (27.0) | 109.1 (17.0) | 132.5 (19.1) | 111.5 (18.8) |
| Ethnicity | ||||||
| Native American | 1 | 0 | 0 | 0 | 1 | 0 |
| Asian/Pacific Islander | 0 | 0 | 1 | 1 | 1 | 1 |
| African American | 0 | 0 | 2 | 1 | 2 | 1 |
| Hispanic | 0 | 0 | 1 | 3 | 1 | 3 |
| Caucasian | 6 | 10 | 1 | 11 | 7 | 21 |
| Other | 0 | 0 | 0 | 1 | 0 | 1 |
| Education | ||||||
| Some college | 0 | 0 | 0 | 2 | 0 | 2 |
| 2-year college degree | 0 | 1 | 0 | 0 | 0 | 1 |
| 4-year college degree | 0 | 4 | 3 | 6 | 3 | 10 |
| Post-baccalaureate | 7 | 5 | 2 | 9 | 9 | 14 |
| Perinatal status | ||||||
| Pre-conception | 2 | 0 | 2 | 7 | 4 | 7 |
| Pregnant | 3 | 3 | 3 | 3 | 6 | 6 |
| Postpartum | 2 | 7 | 0 | 7 | 2 | 14 |
| Medications | ||||||
| None | 5 | 9 | 3 | 9 | 8 | 18 |
| Antidepressant | 0 | 1 | 0 | 4 | 0 | 5 |
| Antidepressant, anxiolytic | 0 | 0 | 0 | 2 | 0 | 2 |
| Antidepressant, mood stabilizer | 0 | 0 | 1 | 1 | 1 | 1 |
| Lithium | 1 | 0 | 0 | 0 | 1 | 0 |
| Lamotrigine, anxiolytic | 0 | 0 | 1 | 0 | 1 | 0 |
| Antidepressant, mood stabilizer, antipsychotic | 1 | 0 | 0 | 1 | 1 | 1 |
BSD bipolar spectrum disorder, including DSM-IV-TR cyclothymic disorder (n = 2), bipolar I disorder (n = 5), bipolar II disorder (n = 3), and bipolar disorder, not otherwise specified (n = 2)
MDD major depressive disorder (n = 27)
BDI-II Beck Depression Inventory, II; HRSD Hamilton Rating Scale for Depression; YMRS Young Mania Rating Scale; STAI-C State-Trait Anxiety Inventory, Current Status; FFMQ Five-Facet Mindfulness Questionnaire
Women who were in a current DSM-IV-TR episode of depression, mania, hypomania or mixed disorder or met current SCID-I/P criteria for substance or alcohol abuse or dependence were ineligible. There was no requirement that women take psychotropic medications or change any medications they were already taking.
Participants were initially screened by telephone to determine their interest level, perinatal status, diagnostic history, and current symptoms. If a study candidate was interested and appeared to be eligible, she was invited in for a full baseline assessment. Interviews were conducted by research assistants who received group or individual training in the SCID-I/P. Interrater reliability for SCID mood and psychosis items averaged .81; agreement on the diagnosis of bipolar I or II disorder or major depressive disorder was .80 (kappa statistic, 17 ratings). Participants were paid $20 for completing the baseline interview and questionnaire battery, and for each follow-up assessment.
Procedures
Mindfulness Intervention
The women participated in one of three 8-week groups conducted at UCLA or one of two 8-week groups conducted at Colorado. Two clinicians (one at UCLA and one at Colorado) led the groups, both of whom had extensive training in MBCT, including 5-day workshops with the developers of MBCT. During the trial, the Colorado clinician received MBCT supervision from a mindfulness expert and co-led one group with her. The UCLA clinician had previously been certified as an MBCT clinician and trainer. The two sites used an identical MBCT manual (Hauser et al. 2008).
The eight MBCT classes were held weekly for 2 h each. The central premise of MBCT is that individuals with histories of depression are vulnerable to recurrences during times of sadness, during which negative cognitive patterns are reactivated and can trigger new depressive episodes (Segal et al. 2012). The core skill is the ability at times of potential relapse to recognize and disengage from self-perpetuating patterns of ruminative thought that contribute to a downward spiral of moods.
In session 1, MBCT clinicians gave a general introduction to mindfulness practice and its relevance to depression and bipolar disorder. In sessions 2–4, participants began to establish a foundation for mindfulness practice through learning the skill of bringing nonjudgmental awareness to the present moment. In-session practices included the body scan, sitting meditations, mindful yoga, and the “3-min breathing space”. In sessions 5 through 8, participants learned to extend their basic mindfulness skills to become aware of relapse signs and develop depression or mania prevention plans. Participants were given multiple opportunities to engage experientially with the ways in which thoughts and emotions become engaged with rumination. The practices began with neutral and concrete targets of attention (e.g., mindful eating) and moved to more emotionally challenging and abstract targets (e.g., depression-specific thoughts). In each exercise, participants were guided to become aware of automatic thinking patterns and return their attention to immediate feelings and body sensations.
All participants received the book “The Mindful Way through Depression” (Williams et al. 2007). Although formal readings were not required, the book recapitulated many of the exercises in the classes. Between-session homework assignments usually required 45 min per day and involved mindfulness practices from standardized CDs, such as the body scan or a walking meditation.
An independent observer rated eight sessions from two of the three groups at UCLA using the MBCT Adherence Scale (Segal et al. 2002). This scale measures treatment fidelity on 17 items rated on 0 (no evidence), 1 (slight evidence) or 2 (definite evidence) scales. Examples of scale items were: use of the 3-min breathing space during sessions, providing education about the cognitive model of depression, and emphasizing commitment to mindfulness practice and relapse prevention. The independent rater observed ‘definite’ evidence for 15 of the 17 content items [mean item rating for group 1, 1.82 (SD = .53); for group 2, 1.88 (SD = .49)]. The exceptions were: using movement-based awareness exercises (rated as ‘slight’ in the first group) and use of video material about MBCT (no evidence).
Measures
Consumer Acceptability
At the post-treatment (8 weeks) assessment, participants completed the 8-item Client Satisfaction Questionnaire (CSQ-8; Larsen et al. 1979) that measures satisfaction with clinical services using 4-point scales (range 8–32).
Symptom Severity
Assessments of the severity of depressive, manic/hypomanic, and anxiety symptoms were conducted at baseline, post-treatment, and 1- and 6-month follow-ups. The 21-item self-administered Beck Depression Inventory, 2nd Ed. (BDI-II; Beck et al. 1996) and the 17-item clinician-administered Hamilton Rating Scale for Depression (HRSD; Hamilton 1960) were used to assess the frequency, duration, and severity of depressive symptoms over the prior 2 weeks. The clinician-rated Young Mania Rating Scale (YMRS; Young et al. 1978) was used to assess the frequency, duration, and severity of 11 mania or hypomania symptoms during the prior week (interrater reliability = .82 (intraclass r), minimum ten ratings). Finally, the self-report State-Trait Anxiety Inventory-Current Status Scale (STAI-C; Spielberger et al. 1983) was used to measure levels of anxiety and worry.
Recurrence of Major Depressive Episodes
The independent evaluators administered the Longitudinal Interval Follow-up Evaluation (LIFE; Keller et al. 1987) at post-treatment and at the 1 and 6 months follow-ups to determine whether participants met criteria for a recurrence of a DSM-IV-TR major depressive episode during the preceding interval. Evaluators made LIFE Psychiatric Status Ratings (PSRs) of major depression and mania/hypomania for each week of the interval. PSR ratings, which vary from 1 (absence of symptoms) to 6 (definite and severe presence of symptoms), were collapsed for simplicity to a 3-point rating where 1 indicated no or only mild symptoms, 2 indicated subthreshold symptoms, and 3 indicated syndromal symptoms that met the duration and impairment criteria for a DSM-IV-TR major depressive episode. There were no instances of DSM-IV-TR manic or mixed episodes during the trial.
Participants were classified as having a recurrence of major depression during the 6-month follow-up period if they (1) were asymptomatic or minimally symptomatic at the end of treatment (i.e., PSR ratings of depression = 1) and (2) at the 1- or 6-month follow-up, reported an increase in depressive symptoms (to a PSR rating of 3) lasting at least 2 weeks of the interval. Three raters examined the pattern of LIFE scores across the post-treatment and follow-up periods, and pairwise agreement on depression recurrences ranged from 75 to 81 %.
Daily Mindful Tendencies
At baseline and each follow-up visit, participants completed the Five Facet Mindfulness Questionnaire (FFMQ; Baer et al. 2008) a 39-item scale that assesses five domains: observing, describing, acting with awareness, non-judging of inner experience, and non-reactivity to inner experience. Internal reliability (alpha coefficient) of the FFMQ in this study was .75.
Statistical Analyses
First, we examined baseline differences on demographic and illness variables between women (1) from the two study sites, (2) with MDD versus BSD, and (3) who were preconception, pregnant, or postpartum. Next, we tabulated rates of treatment completion and satisfaction ratings (feasibility and acceptability). Trajectories of symptom change were examined in participants who attended at least one MBCT class (intent to treat sample) and in those who attended four or more sessions (treatment completers). Covariates included site, diagnostic status, and perinatal status. We modeled treatment response using repeated measure mixed effects models (Gueorguieva and Krystal 2004) in which symptom scores at four assessment points were treated as the repeated dependent variable, with a subject-level random effect to account for correlations among the repeated measurements. A positive treatment response was defined as a significant effect of time that remained robust when controlling for the three covariates.
Secondary mixed effect regression models were used to examine whether women who completed MBCT showed increases in FFMQ scores, whether these increases were correlated with improvements in BDI-II or HRSD scores, and whether these associations differed by site, diagnosis, or perinatal status. Our design had 56–66 % power to detect a medium effect (Cohen’s d = .50) and 91–97 % power to detect a large effect (d ≥ .80) of time (four assessment points) on symptom changes, assuming a 20 % attrition rate.
Results
Participants
Of 101 women who were screened by telephone, 39 enrolled in the study and attended at least one class (Fig. 1). The higher rate of screen failures at UCLA (41/70 or 58.6 %) compared to Colorado (11/31 or 35.5 %) reflected the larger number of non-perinatal women with depression who contacted the UCLA study seeking treatment.
Fig. 1.
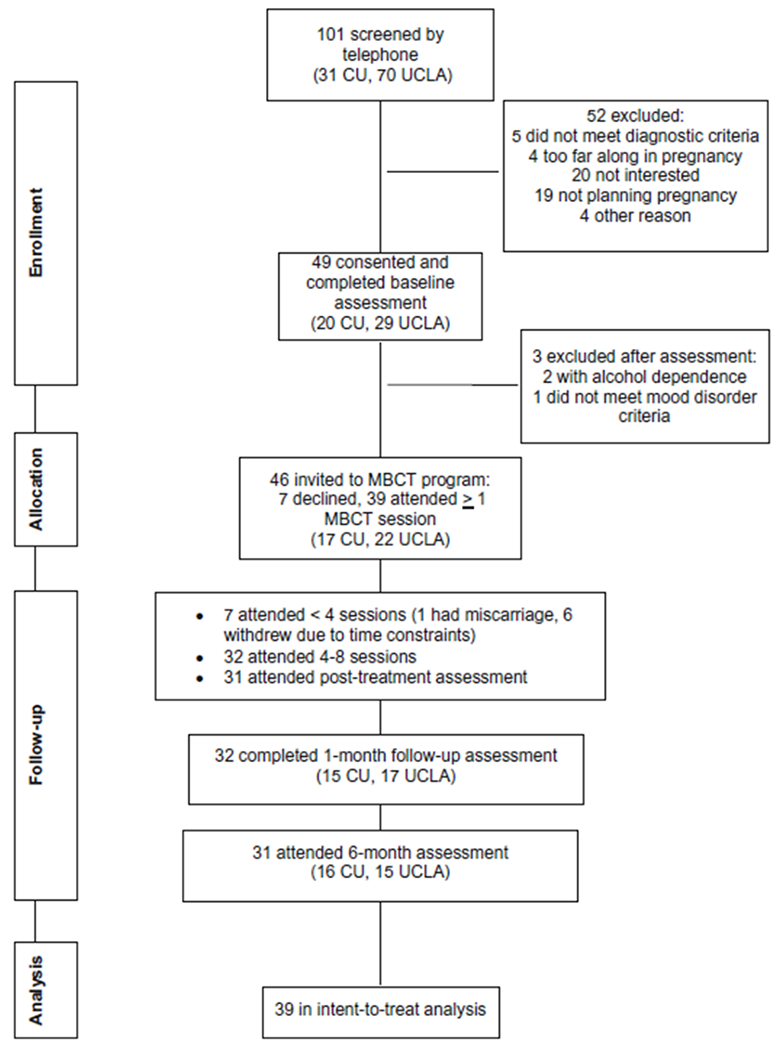
Participant enrollment and withdrawal at two study sites. MBCT mindfulness-based cognitive therapy, CU University of Colorado, UCLA University of California, Los Angeles
The 22 participants at UCLA reported significantly higher baseline levels of depression on the BDI-II [F(1,37) = 8.97, p < .005] and HRSD [F(1,37) = 4.44, p = .04] than the 17 participants at Colorado. Of 39 participants with data on prior depressive episodes, 34 (17 at Colorado, 17 at UCLA, or 85.3 %) reported at least three lifetime episodes; five of the UCLA participants reported two lifetime episodes. The small number of participants with fewer than three episodes did not allow us to examine number of episodes as a predictor.
Women in the preconception, pregnancy, or postpartum categories did not differ on baseline BDI-II or HRSD scores. There were no differences between participants at the two sites on age, baseline YMRS or STAI-C scores, or the proportion diagnosed with MDD versus BSD. Women with MDD and BSD did not differ on age or perinatal status, nor on baseline BDI-II, HRSD, or STAI-C scores. As expected, participants with BSDs had higher baseline YMRS scores (M = 4.08; SD = 4.06; n = 12) than participants with MDD (M = 1.37; SD = 1.62; n = 27) [F (1,37) = 9.08, p < .005].
FFMQ (daily mindful tendency) scores (M = 118.0, SD = 22.1; range 69–159) did not differ by site or perinatal status. Participants with BSD had higher FFMQ scores at baseline than participants with MDD [F(1,37) = 10.27, p = .003]. At baseline, higher FFMQ scores were associated with lower BDI-II [r(39) = −.47, p = .002] and lower HRSD scores [r(39) = −.37, p = .02]. FFMQ scores were unrelated to baseline YMRS or STAI-C scores.
Treatment Acceptability
The Colorado site conducted two consecutive 8-week groups with 9 and 8 women, respectively. The UCLA site conducted three groups with 5, 7, and 10 participants. Of 39 women who began MBCT, 32 (82.1 %) completed 50 % or more (≥4) of the sessions (“completers”; Fig. 1). Treatment completion was equally common at the two sites. Diagnosis was a strong predictor of completion: 5 of the 12 participants (41.7 %) with BSD did not complete the classes, whereas only 2 of the 27 (7.4 %) participants with MDD did not complete the classes (, p = .01). The participants who completed fewer than four classes had higher YMRS scores at entry (M = 5.86; SD = 4.18) than those who completed four or more sessions (M = 1.41; SD = 1.72) [F(1,37) = 21.42, p < .0001].
All women were classified based on their perinatal status at intake into the study, and all were retained in their original category for the longitudinal analyses. Perinatal status, age, and baseline BDI-II, HRSD, or STAI-C scores were unrelated to treatment completion. At the post-treatment assessment, the 32 completers reported high levels of satisfaction with MBCT (mean CSQ-8 score = 29.2, SD = 3.2; satisfaction scores were not obtained from women who left the course early). Treatment satisfaction scores did not differ by site, diagnosis, or perinatal status.
Changes in Depression Symptoms
A repeated measure mixed effects regression model revealed a main effect of time on self-reported depression [BDI-II; F(3,91) = 3.82, p = .013]. In the full sample (N = 39), BDI-II scores decreased significantly from baseline (M = 12.2; SD = 12.3) to post-treatment (M = 7.4; SD = 7.0) [F(1,30) = 8.10, p = .008; Cohen’s d = .52]. BDI-II scores at 1-month (M = 7.3; SD = 9.1; d = .53) and 6-month (M = 8.1; SD = 8.0; d = .45) were also lower than those at baseline (F1,31 = 7.24, p = .01 and F1,30 = 4.17, p = .05, respectively; Fig. 2). When these analyses were repeated in the 32 treatment completers, the main effect of time remained robust [F(3,86) = 3.54, p = .018; d = .57]. Changing from a mean of 12.2 to a mean of 7.4 on the BDI-II indicates moving from a mildly to a minimally depressed state.
Fig. 2.
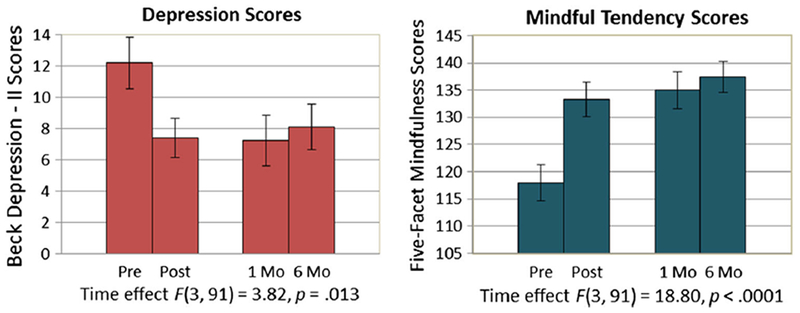
Perinatal women with lifetime histories of major depressive disorder: self-reported depression and daily mindful tendency scores from baseline to 6-month post-treatment
There was no main effect of perinatal status [F (2,85) = .85, p = .43] nor any interaction between perinatal status and time on follow-up BDI-II scores [F (6,85) = 1.56, p = .17]. There was a main effect of study site [F (1,88) = 7.68, p = .007] indicating that BDI-II scores were on average higher at the UCLA than the Colorado site. There was no study site by time interaction [F(3,88) = 1.80, p = .15], indicating that participants at the two sites had comparable improvement slopes.
Participants with MDD showed greater reductions in BDI-II scores from pre- to post-treatment and follow-up (d = .74) than participants with BSDs [d = −.27; diagnosis by time interaction, F (3,88) = 2.99, p = .035]. To determine whether this diagnostic difference was due to the higher rate of attrition in the bipolar subsample, we examined changes in BDI-II scores in the seven participants with BSD who completed MBCT. No effects of time were observed on BDI-II scores in this subgroup.
In the full sample, there were no effects of time on clinician-rated HRSD scores, nor any effects of site or perinatal status. However, a diagnosis by time interaction [F (3,91) = 3.16, p = .029] indicating that HRSD scores decreased from baseline to post-treatment in the MDD participants (d = .36), but worsened over time in the BSD participants (d = −.73). When we removed the 5 (of 12) participants with BSD who did not finish the classes, we observed an average increase in HRSD scores from baseline (M = 3.14; SD = 2.34) to post-treatment (M = 7.0; SD = 4.97; d = −.99) in the seven completers with BSD. Scores of 0–7 on the HRSD are within the normal range.
Anxiety scores (STAI-C) and YMRS scores did not change over time in the full sample or the diagnostic subgroups. There were no effects of site or perinatal status on changes in STAI-C or YMRS scores.
Recurrence Rates
Of the 32 participants who had 6 months post-treatment data, 7 met DSM-IV-TR criteria for a major depressive episode at follow-up (21.9 %). Diagnosis (MDD vs. BSD), site, and perinatal status were unrelated to the presence/absence of a depressive recurrence at follow-up. No participants reported episodes of mania or mixed disorder at follow-up, although 4 participants with BSD reported hypomanic episodes. Of these 4, 2 also had major depressive episodes at follow-up.
Changes in Five Facet Mindfulness Questionnaire Scores
Baseline FFMQ total scores (sample mean = 118.0, SD = 22.1; range 69–159) did not differ by site or perinatal status. FFMQ scores increased with time in the full sample [F (3,91) = 18.80, p < .0001; Fig. 2]. There was no interaction between study site and time, nor between perinatal status and time in predicting changes in FFMQ scores. However, there was an interaction between diagnosis and time on FFMQ scores [F (3,88) = 2.81, p = .04], indicating that women with MDD showed greater increases in FFMQ scores from baseline to 6 months (mean increase 24.88, SD = 19.69) than women with BSDs (mean increase 9.57, SD = 9.14) (d = 1.0).
The majority of the change in FFMQ and BDI-II scores occurred between the baseline and post-treatment (8 weeks) assessments (Fig. 2). A mixed effects regression model revealed a main effect of FFMQ change scores [F (48,24) = 2.61, p = .007], no effect of time [F(2,24) = 1.46, p = .25], and an interaction of FFMQ change scores and time [F(19,24) = 2.06, p = .048] on BDI-II scores at follow-up. This interaction indicated that participants who reported increases in mindful tendency scores also showed decreases in depression scores across time. The correlation of FFMQ change scores and BDI-II change scores did not differ in magnitude across the MDD and BSD groups.
Discussion
This study examined the feasibility, acceptability, and short-term benefits of an 8-session MBCT program in a heterogeneous sample of perinatal women with MDD or BSD. Together with a recent trial of MBCT for pregnant women with depression (Dimidjian et al. 2014), we conclude that MBCT is a promising treatment for perinatal women with MDD, including those who are planning pregnancy or within 1 year postpartum. Perinatal women with MDD reported high levels of treatment satisfaction and most (92.6 %) completed the classes. Further, participants with MDD reported significant decreases in self-rated depressive symptoms.
The rate of depressive recurrence observed over 6 months, 21.9 %, is comparable to the rate observed in the Dimidjian et al. (2014) trial (18 %), and lower than the 30 % rate in 6 months reported in naturalistic studies of perinatal women with depression histories (Goodman and Tully 2009). The women in the present study may have been a treatment-responsive subpopulation because most (85 %) had had three or more depressive episodes prior to treatment. In a meta-analysis of mindfulness trials for men and women with MDD, MBCT was associated with a 34 % reduction in recurrence rates over an average of 14 months, and a 43 % reduction among participants with three or more depressive episodes (Piet and Hougaard 2011).
On the clinician-rated HRSD, MDD participants showed a modest level of improvement from baseline to 6-month (d = .36). Most had scores within the normal range when they began treatment (M = 6.1, SD = 4.8) and had little room to improve. In contrast, we did not observe symptomatic improvements among the women with BSD on either the BDI-II or the HRSD. Women with BSD also were less likely to stay in the program (58.3 %) than women with MDD (92.6 %). The lack of significant improvement among women with BSD contrasts with results from open trials that have found positive effects of MBCT on depression or anxiety symptoms in bipolar disorder (Weber et al. 2010; Miklowitz et al. 2009; Deckersbach et al. 2012; Ives-Deliperi et al. 2013; Williams et al. 2008). Our findings are, however, consistent with the single randomized trial of adults with bipolar disorder that found no effects of MBCT compared to usual care on depression or hypomania symptoms over 12-months (Perich et al. 2013).
Several design limitations deserve mention. First, because of the small sample and the participants’ symptomatic heterogeneity, we cannot conclude that MBCT is ineffective or contraindicated among perinatal women with BSD. Second, although MBCT was administered by clinicians who had substantial training and supervision, treatment fidelity ratings were only available for one of the two sites. Thus, we cannot be certain that fidelity scores were equivalent across sites or diagnostic subgroups. Third, there are other unmeasured variables that could have affected the trajectory of depression scores, such as the length of time that participants had been trying to conceive, distress levels in the spousal relationship, or hormonal changes during the pregnancy or postpartum.
Our findings underscore the importance of studying the balance of risks and benefits associated with MBCT for patients with BSD or MDD. The persisting symptom states of many individuals with BSD, even during remission, can include labile energy, mood instability, rapid thinking, inattention, and impulsive responding (Townsend and Altshuler 2012). These symptoms may make daily meditation practice and nonjudgmental self-observation much more difficult than for remitted individuals with MDD. Possibly, perinatal women with BSD would engage more easily with mindfulness practices that are briefer, varied, and more directly linked to the immediate physical and emotional experiences of pregnancy and the postpartum. Such questions should be addressed in studies focused specifically on pregnant women with BSD, given the complexities associated with pharmacological management of bipolar disorder during pregnancy and the increased risk, relative to non-clinical populations and women with MDD, for mood disturbance and psychosis to emerge during the postpartum period (Di Florio et al. 2013; Ward and Wisner 2007).
Approximately half of the women in this study (53.8 %) were taking antidepressants, mood stabilizers, or antipsychotic medications during the classes or at follow-up. Without a randomly assigned medication-only condition, we cannot determine whether some women with depression histories can remain off maintenance medications during pregnancy or the postpartum and substitute MBCT (with self-guided meditation practice) to maintain mood stability. A randomized trial of maintenance antidepressants, MBCT, and placebo in remitted depressed patients found that among unstable remitters (i.e., those with periods of symptom exacerbation during remission), antidepressants and MBCT were both associated with lower rates of recurrence than placebo (Segal et al. 2010). A similar study has not been conducted among perinatal women with MDD.
Prior studies have observed effects of MBCT on mindfulness and self-compassion scores in patients with MDD or bipolar disorder (Deckersbach et al. 2012; Kuyken et al. 2010; Williams et al. 2014). In the present study, improvements in FFMQ scores (e.g., maintaining a non-judgmental and non-reactive stance toward inner experience) were observed in both diagnostic groups, but were greater in women with MDD than in women with BSD, perhaps because the former group started from a lower baseline. In the full sample, improvements in mindfulness were correlated with decreases in depressive symptoms over 6 months. Because daily mindful tendencies and depression were measured at the same assessment points, we do not know whether improvements in mindfulness lead to improvements in mood, improvements in mood lead to increases in mindful tendencies, or changes in both result from the natural progression of mood disorders. Further, Grossman et al. (2011) and Davidson (2010) have voiced concerns about the reliability and conceptual validity of self-report mindfulness scales. We acknowledge the importance of examining whether (1) participants’ reports of increased mindful competencies are reflected in their daily behavior, (2) changes in mindfulness antedate changes in depressed mood, and (3) whether these causal pathways to symptom change are specific to mindfulness therapies.
In summary, MBCT is a promising treatment for perinatal women with major depression, with high rates of treatment completion and satisfaction, low rates of recurrence, and improvement in self-reported depression scores. Further research is needed to evaluate whether and under what circumstances the reduction in symptoms observed among perinatal women with depression extends to perinatal women with BSDs. We recommend studies that systematically compare the responses to MBCT of perinatal women who are versus are not taking antidepressants or mood stabilizers. Additionally, there may be intervals within the reproductive transitions of pre-conception, pregnancy, and postpartum during which women with mood disorders are most likely to integrate and implement the coping strategies recommended in mindfulness treatments.
Acknowledgments
Conflict of Interest This study was supported by grants from the Danny H. Alberts Foundation and the Attias Family Foundation, and Grant R01-MH093676 from the National Institute of Mental Health (NIMH) (Miklowitz, PI). Author D. Miklowitz lists the following financial relationships: NIMH, Carl and Roberta Deutsch Foundation, Kayne Family Foundation, Knapp Foundation, Danny H. Alberts Foundation, and Attias Family Foundation; and book royalties from Guilford Press and John Wiley and Sons. Author S. Dimidjian receives research funding from the NIMH and book royalties from Guilford Press. Authors R. Semple, D. Elkun, and M. Weintraub have no financial or other relationships that would create a conflict of interest regarding this manuscript.
Footnotes
Informed Consent All procedures performed in studies involving human participants were in accordance with the ethical standards of each institution’s research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all participants after they received a full explanation of the study procedures. The protocol was reviewed and approved by the Human Subject Review Boards of the University of Colorado and the UCLA School of Medicine.
Animal Rights No animals studies were carried out by the authors for this paper.
Clinical Trials Registration: .
References
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders, (text revision) (DSM-IV-TR) (4th ed.). Washington, DC: American Psychiatric Press. [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, et al. (2008). Construct validity of the Five Facet Mindfulness Questionnaire in meditating and nonmeditating samples. Assessment, 15, 329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Bar-Oz B, Einarson T, Einarson A, Boskovic R, O’Brien L, Malm H, et al. (2007). Paroxetine and congenital malforma tions: Meta-analysis and consideration of potential confounding factors. Clinical Therapeutics, 29(5), 918–926. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck Depression Inventory-II. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Cohen LS (2007). Treatment of bipolar disorder during pregnancy. Journal of Clinical Psychiatry, 68(Suppl 9), 4–9. [PubMed] [Google Scholar]
- Davidson RJ (2010). Empirical explorations of mindfulness: Conceptual and methodological conundrums. Emotion, 10(1), 8–11. doi: 10.1037/a0018480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deckersbach T, Hölzel BK, Eisner LR, Stange JP, Peckham AD, Dougherty DD, et al. (2012). Mindfulness-based cognitive therapy for nonremitted patients with bipolar disorder. CNS Neuroscience & Therapeutics, 18(2), 133–141. doi: 10.1111/j.1755-5949.2011.00236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Florio A, Forty L, Gordon-Smith K, Heron J, Jones L, Craddock N, et al. (2013). Perinatal episodes across the mood disorder spectrum. JAMA Psychiatry, 70(2), 168–175. doi: 10.1001/jamapsychiatry.2013.279. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Goodman SH, Felder JN, Gallop R, Brown AP, & Beck A (2014). An open trial of mindfulness-based cognitive therapy for the prevention of perinatal depressive relapse/recurrence. Archives of Women’s Mental Health, 18(1), 85–94. doi: 10.1007/s00737-014-0468-x. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Miriam G, & Williams JBW (2002). Structured Clinical Interview for DSM-IV-TR Axis I disorders, research version, patient edition with psychotic screen (SCID-I/P W/PSY SCREEN). New York: Biometrics Department, New York State Psychiatric Institute. [Google Scholar]
- Gaynes BN, Gavin N, Meltzer-Brody S Lohr KN, Swinson T, Gartlehner G, et al. (2005). Perinatal depression: prevalence, screening accuracy, and screening outcomes Evidence Report/Technology Assessment No. 119. (Prepared by the RTI-University of North Carolina Evidence-based Practice Center, under Contract No. 290-02-0016.) AHRQ Publication No. 05-E006-2. Rockville, MD: Agency for Healthcare Research and Quality. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH (2009). Depression in mothers. Annual Review of Clinical Psychology, 3, 107–135. [DOI] [PubMed] [Google Scholar]
- Goodman SH, & Tully EC (2009). Recurrence of depression during pregnancy: Psychosocial and personal functioning correlates. Depression and Anxiety, 26, 557–567. doi: 10.1002/da.20421. [DOI] [PubMed] [Google Scholar]
- Grossman P, et al. (2011). Defining mindfulness by how poorly I think I pay attention during everyday awareness and other intractable problems for psychology’s (re)invention of mindful ness: Comment on Brown et al. (2011). Psychological Assessment, 23, 1034–1040. doi: 10.1037/a0022713. [DOI] [PubMed] [Google Scholar]
- Gueorguieva R, & Krystal JH (2004). Move over ANOVA: Progress in analyzing repeated-measures data and its reflection in papers published in the Archives of General Psychiatry. Archives of General Psychiatry, 61, 310–317. [DOI] [PubMed] [Google Scholar]
- Hamilton M (1960). A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry, 12, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser M, Miklowitz DJ, & Dimidjian S (2008). Treatment manual for mindfulness-based cognitive therapy for bipolar disorder. Unpublished University of Colorado, Boulder, CO. [Google Scholar]
- Ives-Deliperi VL, Howells F, Stein DJ, Meintjes EM, & Horn N (2013). The effects of mindfulness-based cognitive therapy in patients with bipolar disorder: A controlled functional MRI investigation. Journal of Affective Disorders, 150(3), 1152–1157. doi: 10.1016/j.jad.2013.05.074. [DOI] [PubMed] [Google Scholar]
- Judd LL, Schettler PJ, Akiskal HS, Coryell W, Leon AC, Maser JD, et al. (2008). Residual symptom recovery from major affective episodes in bipolar disorders and rapid episode relapse/recurrence. Archives of General Psychiatry, 65(4), 386–394. doi: 10.1001/archpsyc.65.4.386. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, et al. (1987). The longitudinal interval follow-up evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry, 44, 540–548. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Watkins E, Holden E, White K, Taylor RS, Byford S, et al. (2010). How does mindfulness-based cognitive therapy work? Behavior Research and Therapy, 48(11), 1105–1112. doi: 10.1016/j.brat.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, & Nguyen TD (1979). Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning, 2, 197–207. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Alatiq Y, Goodwin GM, Geddes JR, Fennell MVF, Dimidjian S, et al. (2009). A pilot study of mindfulness-based cognitive therapy for bipolar disorder. International Journal of Cognitive Therapy, 2(4), 373–382. doi: 10.1521/ijct.2009.2.4.373. [DOI] [Google Scholar]
- Perich T, Manicavasagar V, Mitchell PB, Ball JR, & Hadzi-Pavlovic D (2013). A randomized controlled trial of mind-fulness-based cognitive therapy for bipolar disorder. Acta Psychiatrica Scandinavaca, 127(5), 333–343. doi: 10.1111/acps.12033. [DOI] [PubMed] [Google Scholar]
- Piet J, & Hougaard E (2011). The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: A systematic review and meta-analysis. Clinical Psychology Review, 31, 1032–1040. doi: 10.1016/j.cpr.2011.05.002. [DOI] [PubMed] [Google Scholar]
- Rush AJ (2007). STAR*D: What have we learned? American Journal of Psychiatry, 164(2), 201–204. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Bieling P, Young T, Macqueen G, Cooke R, Martin L, et al. (2010). Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depresssion. Archives of General Psychiatry, 67, 1256–1264. doi: 10.1001/archgenpsychiatry.2010.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Teasdale JD, Williams JM, & Gemar MC (2002). The Mindfulness-Based Cognitive Therapy Adherence Scale: Inter-rater reliability, adherence to protocol and treatment distinctiveness. Clinical Psychology and Psychotherapy, 9, 131–138. [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD, & Kabat-Zin J (2012). Mindfulness-based cognitive therapy for depression (2nd ed.). New York: Guilford Press. [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene PR, Vagg PR, & Jacobs AG (1983). Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Townsend J, & Altshuler LL (2012). Emotion processing and regulation in bipolar disorder: A review. Bipolar Disorders, 14(4), 326–339. doi: 10.1111/j.1399-5618.2012.01021.x. [DOI] [PubMed] [Google Scholar]
- Viguera AC, Tondo L, Koukopoulos AE, Reginaldi D, Lepri B, & Baldessarini RJ (2011). Episodes of mood disorders in 2,252 pregnancies and postpartum periods. American Journal of Psychiatry, 168(11), 1179–1185. doi: 10.1176/appi.ajp.2011.11010148. [DOI] [PubMed] [Google Scholar]
- Viguera AC, Whitfield T, Baldessarini RJ, Newport DJ, Stowe Z, Reminick A, et al. (2007). Risk of recurrence in women with bipolar disorder during pregnancy: Prospective study of mood stabilizer discontinuation. American Journal of Psychiatry, 164(12), 1817–1824. [DOI] [PubMed] [Google Scholar]
- Ward S, & Wisner KL (2007). Collaborative management of women with bipolar disorder during pregnancy and postpartum: Pharmacologic considerations. Journal of Midwifery and Women’s Health, 52(1), 3–13. [DOI] [PubMed] [Google Scholar]
- Weber B, Jermann F, Gex-Fabry M, Nallet A, Bondolfi G, & Aubry JM (2010). Mindfulness-based cognitive therapy for bipolar disorder: A feasibility trial. European Psychiatry, 25(6), 334–337. doi: 10.1016/j.eurpsy.2010.03.007. [DOI] [PubMed] [Google Scholar]
- Williams JM, Alatiq Y, Crane C, Barnhofer T, Fennell MJ, Duggan DS, et al. (2008). Mindfulness-based Cognitive Therapy (MBCT) in bipolar disorder: Preliminary evaluation of immediate effects on between-episode functioning. Journal of Affective Disorders, 107(1–3), 275–279. doi: 10.1016/j.jad.2007.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams MJ, Dalgleish T, Karl A, & Kuyken W (2014). Examining the factor structures of the Five Facet Mindfulness Questionnaire and the self-compassion scale. Psychological Assessment, 26(2), 407–418. doi: 10.1037/a0035566. [DOI] [PubMed] [Google Scholar]
- Williams M, Teasdale J, Segal Z, & Kabat-Zinn J (2007). The mindful way through depression: Freeing yourself from chronic unhappiness. New York: The Guilford Press. [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, & Meyer DA (1978). A rating scale for mania: reliability, validity and sensitivity. The British Journal of Psychiatry, 133(5), 429–435. [DOI] [PubMed] [Google Scholar]


