Abstract
Objective
To contrast how Brazil’s and Canada’s different jurisdictional and judicial realities have led to different types of telemedicine and how further scale and improvement can be achieved.
Composition of the committee
A subgroup of the Besrour Centre of the College of Family Physicians of Canada and Canadian telemedicine experts developed connections with colleagues in Porto Alegre, Brazil, and collaborated to undertake a between-country comparison of their respective telemedicine programs.
Methods
Following a literature review, the authors collectively reflected on their experiences in an attempt to explore the past and current state of telemedicine in Canada and Brazil.
Report
Both Brazil and Canada share expansive geographies, creating substantial barriers to health for rural patients. Telemedicine is an important part of a universal health system. Both countries have achieved telemedicine programs that have scaled up across large regions and are showing important effects on health care costs and outcomes. However, each system is unique in design and implementation and faces unique challenges for further scale and improvement. Addressing regional differences, the normalization of telemedicine, and potential alignment of telemedicine and artificial intelligence technologies for health care are seen as promising approaches to scaling up and improving telemedicine in both countries.
Résumé
Objectif
Comparer la manière dont les différentes réalités territoriales et judiciaires du Brésil et du Canada ont mené à différents types de télémédecine et déterminer comment l’expansion à plus grande échelle, ainsi que des améliorations peuvent être réalisées.
Composition du comité
Un sous-groupe du Centre Besrour du Collège des médecins de famille du Canada et des experts canadiens en télémédecine ont établi des liens avec des collègues de Porto Alegre, au Brésil, et ont collaboré pour entreprendre une comparaison entre les programmes de télémédecine des deux pays.
Méthodes
Après une revue de la documentation, les auteurs ont fait une réflexion collective sur leurs expériences afin d’explorer l’état passé et actuel de la télémédecine au Canada et au Brésil.
Rapport
Le Brésil et le Canada couvrent tous deux de vastes territoires géographiques, ce qui crée des obstacles importants à la santé des patients des zones rurales. La télémédecine est un élément important d’un système de santé universel. Les deux pays ont mis en place des programmes de télémédecine qui s’étendent sur de vastes régions et qui ont des effets importants sur les coûts des soins et la santé des populations. Toutefois, chaque système est unique dans sa conception et sa mise en œuvre et se heurte à des difficultés particulières qui entravent son expansion. La prise en compte des différences régionales, la normalisation de la télémédecine et l’harmonisation potentielle des technologies de télémédecine et d’intelligence artificielle pour les soins de santé sont considérées comme des approches prometteuses pour le développement et l’amélioration de la télémédecine dans ces deux pays.
Despite stark differences, Canada and Brazil share a common reality—that of a very expansive geography. Although Canada’s remote geography is often regarded as unique, there are striking similarities in the distribution of the populations across these countries. Residents of remote regions in Brazil and Canada face several days of travel to reach major metropolitan areas (Figure 1).1 In Canada, the geographic expanse creates a considerable barrier to health for rural patients, who make up 19% of the population and who must travel to large urban settings, where 98% of medical specialists are based, when they need specialized care.2 It is important to emphasize that this discrepancy creates risky situations and expenses. Rural areas have the highest socioeconomic burden, with fewer health services and lower use of health care than in urban areas.3 Further, the act of traveling to and from rural areas to see health providers can put one’s health at risk. In low- and middle-income countries, death from traffic injuries continues to be a substantial cause of morbidity and remains the leading cause of death among people aged 15 to 29 in Brazil.4,5 Distance also acts as a limiting factor for access to health, as well as the disproportion between demand and supply of services, resulting in considerable wait times. To solve such a complex problem, interventions that affect the health system, such as telemedicine, are necessary.
Figure 1.
Geography of Canada compared with Brazil
Data from Google.1
To better match patient needs and resources, both countries have resorted to various forms of telemedicine to improve timely access to care. While definitions vary,6,7 telemedicine can be thought of as “the use of information technology to facilitate the provision of health care across geographical, time and social barriers.”7 Telemedicine first emerged in the 1970s as a tool in high-income countries with large geographic extensions to link rural populations to large health centres.8–13 Over time, telemedicine has evolved to include a diverse set of technologies and clinical models, each with varying goals and outcomes. Although there is no consensus on classification, for this paper we have grouped telemedicine models into 4 distinct categories (Table 1).6,14,15
Table 1.
Glossary of telemedicine models
| TERM | DEFINITION |
|---|---|
| Teleconferencing | Communication between a clinician and patient for the purpose of direct clinical care |
| Teleconsultation, eConsult | Consultation between health care providers to facilitate the diagnosis or treatment of a patient. Care is not transferred from one provider to another. The patient is usually not directly involved in the interaction |
| Telediagnosis | Use of technology to gather diagnostic information to be reviewed by a remote clinician |
| Self-management | Patients’ use of technology, including remote monitoring |
At scale, telemedicine might optimize the organization of health systems by helping to regulate the allocation of resources, enable better communication among health professionals, reduce costs of unnecessary travel, and improve patient satisfaction with care.16,17 Although these models have the potential to improve patient access to health resources while maintaining outcomes similar to in-person care,13,14 telemedicine use is not yet widely integrated into clinical practice in either country.18–20 This might partially be attributed to emerging evidence about efficacy for different conditions, including cost-benefit analyses.21,22
Given the considerable variations in telemedicine models across health jurisdictions around the world, it is useful to examine the strengths and weaknesses of telemedicine programs to facilitate improved adoption and scale to improve population health. In this article, the third in the series comparing the health systems of Brazil and Canada, we will contrast how these countries’ different jurisdictional and judicial realities have led to different types of telemedicine at different paces. Both countries have achieved telemedicine programs that have scaled up across large regions and are showing important effects on health costs and outcomes; however, each system is unique in design and implementation and faces unique challenges for further scale and improvement. This paper will first give examples of key programs in each country. We will then offer a synthesis of learnings from the comparison.
Composition of the committee
A subgroup of the Besrour Centre of the College of Family Physicians of Canada and Canadian telemedicine experts developed connections with colleagues in Porto Alegre, Brazil, and collaborated to undertake a between-country comparison of their respective tele-medicine programs.
Methods
Following a literature review, the authors collectively reflected on their experiences in an attempt to explore the past and current state of telemedicine in Canada and Brazil.
Report
Telemedicine in Canada.
Telemedicine in Canada started in the late 1970s with a clear focus on providing teleconferencing services to rural patients.13 Over the years, regional telemedicine models have been developed based on local needs, with varying support at the provincial and federal levels. In Ontario, Canada’s most populous province at 14.3 million inhabitants, the publicly funded Ontario Telemedicine Network (OTN) coordinates teleconsultation services across the province, supporting more than 896 000 visits in 2017.23 There are provincial differences in the breadth of telehealth clinic services offered across Canada. Ontario offers 72 distinct clinical areas of telehealth clinical service, as reported in the 2015 Canadian Telehealth Report.22 In contrast, other provinces are limited in the diversity of services provided, such as New Brunswick, which offers only 39 distinct areas of service.24 Despite regional differences, Canada has developed some of the most comprehensive access to acute care telemedicine in the world, with up to 75% of hospitals offering some form of telemedicine access.25 Of note, these models are supported by strong regulatory and payment frameworks, including the College of Physicians and Surgeons of Ontario’s policy on telemedicine.26 These regulations enable effective clinical integration of telemedicine with mechanisms for reimbursement that vary by province.
Telemedicine in Brazil.
Telemedicine in Brazil started later than in Canada, with the first pilot studies occurring in the mid-1990s. In 2002, the Federal Council of Medicine in Brazil officially permitted telemedicine; however, it was restricted to instances in which physicians were present at both ends of the communication.27 Indeed, teleconferencing with patients in Brazil remains illegal. This is owing to the Brazilian Federal Board of Medicine’s belief that medical consultation with the physical presence of the patient is irreplaceable.28 It is argued that, in general, the current norms of conduct, standards, and regulations for the application of telemedicine in Brazil are insufficient, and that these technologies might represent a threat to the traditional doctor-patient relationship.27
In 2007, the Ministry of Health formed the National Telehealth Program, which was expanded in 2011 and currently operates in 23 states serving 3417 cities.27 TelessaúdeRS–Universidade Federal do Rio Grande do Sul (TRU), developed in part through this funding, serves the state of Rio Grande do Sul with a strong focus on integration of telemedicine into primary care as opposed to technology development.29,30 Despite increasing use, Brazil still lacks strong guidelines around reimbursement models and regulatory frameworks for telemedicine.27 Barriers to telemedicine adoption, identified by Brazilian clinicians, include legal uncertainty, technology acquisition, and Internet connectivity.31
Specific program examples.
While it would not be feasible to fully describe all telemedicine initiatives in Canada and Brazil, we have selected several programs from each country (with a focus on the provinces of Ontario and British Columbia [BC] in Canada and the state of Rio Grande do Sul in Brazil) that highlight telemedicine usage in each country (Table 2). In Ontario, all teleconferencing visits are conducted using technology supplied by the OTN. While the program initially served mostly rural patients needing consultations with urban-based specialists, such as surgeons, oncologists, and internal medicine specialists, the program now serves more people located in large urban centres who require support around mental health and addictions.32 More recently, OTN has developed a teleconsultation platform for asynchronous clinical interactions between primary care providers and specialists that has been implemented across the province. This model is focused on supporting primary care providers in maintaining care of their patients, while providing both primary care providers and specialists with a remuneration mechanism for their efforts. Before this platform’s adoption, the Champlain Building Access to Specialists through eConsultation (BASE) service launched a secure online application facilitating asynchronous e-consultations, which has undergone rigorous evaluation for usability and effects on health outcomes.32 As of July 2018, the Champlain BASE program had completed approximately 42 000 eConsult cases, providing thousands of patients with reliable and quick consultation.33 More than 1400 registered primary care providers are involved in this program, and it has been shown to be cost-effective for the provision of specialist care (cost of traditional referral to a specialist provider, on average, $133.60/case; cost of BASE eConsult service, on average, $47.35/case).34 Although begun as a small regional service based in Ottawa, Ont, the BASE eConsult service model of care has been replicated in 4 other provinces and is undergoing expansion across Ontario in partnership with OTN.
Table 2.
Examples of telemedicine projects in both countries
| NAME OF PROGRAM | TELEMEDICINE MODELS | COUNTRY | DESCRIPTION |
|---|---|---|---|
| Champlain BASE | Teleconferencing and teleconsultation | Canada (Ontario) | Contains a Web-based portal that connects primary care providers (family physicians and nurse practitioners) and specialist physicians to enable the exchange of information (eg, physician notes, test results, images) regarding patient cases |
| OTN | Teleconferencing | Canada (Ontario) | OTN organizes both e-visits and e-care. In an e-visit, physicians and patients or other physicians can engage in real-time video visits via personal computer, cellular device, or conferencing rooms in health organizations. In e-care, apps and other devices are used to monitor patients and coach them to manage their conditions at home |
| Interior Health Authority of British Columbia | Telediagnosis and self-management | Canada (British Columbia) | Patients can access videoconferencing services at their nearest medical centre to connect to specialists across the province. Specialists in other centres use imaging, electronic stethoscopes, and electronic medical records to examine the patient. The Interior Health Authority also offers a telehomecare monitoring program that allows patients with congestive heart failure to monitor and self-manage their conditions |
| Canada Health Infoway | Teleconferencing | Canada (British Columbia) | Offers in-practice and virtual clinic visits in an online setting. In-practice visits occur between primary care physicians and patients they already know. Virtual clinic visits involve new patients |
| RACE | Teleconsultation | Canada (British Columbia and Yukon) | Through this service, physicians can call one telephone number to access various specialists who can provide real-time advice. The service is available during business hours to all primary care providers in British Columbia and Yukon |
| Teleconsultation hot-line | Teleconsultation | Brazil (all-country: 26 states and 1 federal district) | Used to clarify questions (clinical and administrative) in real time. Available to all primary health care doctors and other health professionals in Brazil |
| National Telehealth Platform | Teleconsultation | Brazil (Rio Grande do Sul) | Service for primary care professionals to clarify questions (clinical and administrative) with another provider. Inquiries are answered by text within 72 h |
| RegulaSUS (Ambulatory Regulation Service) | Teleconsultation | Brazil (Rio Grande do Sul) | Organization of outpatient access to specialized services through the creation of referral protocols, classification of clinical priorities, and discussion in real time of clinical cases of patients on the waiting list |
| TelessaúdeRS-UFRGS (respiratory, ophthalmology, dermatology, stomatology) | Telediagnosis | Brazil (Rio Grande do Sul) | Allows the interpretation of clinical investigations through a digital platform. This includes the following:
|
BASE—Building Access to Specialists through eConsultation, OTN—Ontario Telemedicine Network, RACE—Rapid Access to Consultative Expertise, UFRGS—Universidade Federal do Rio Grande do Sul.
British Columbia also has a long history of using teleconferencing technology to support clinical consultations for rural and remote residents and physicians. These efforts have been led by various clinical groups across the province, each with slightly different clinical goals. For example, the Interior Health Authority of BC has developed a video teleconferencing platform that allows residents of remote areas to access specialist expertise at their local health centres (if enabled with the appropriate technology).35,36 The BC Children’s Hospital is also strongly involved in virtual care to support residents in rural and remote areas. A newly evolving tele–intensive care unit strategy, complemented with more elective teleconsultations from a growing list of specialties, continues to expand. Carrier Sekani Family Services (CSFS), based in Prince George, BC, has made considerable gains in the past 8 years using telemedicine to develop a virtual primary care network to provide holistic and relationship-based services to more than a dozen very remote Indigenous communities in north-central BC. The CSFS provides videoconferencing health and coordination services to allow Indigenous community members ongoing access to primary care. Many members of the communities that participate in this program have complex health needs. In 2015, CSFS conducted approximately 1000 videoconferencing visits for remote residents in substantially underserved communities.37 Finally, a provincewide program entitled Rapid Access to Consultative Expertise (RACE) was started in 2010 to enable primary care providers access to specialty services for real-time telephone advice. It currently provides access to more than 43 specialty services and manages more than 800 calls per month.38 The program has been shown to save the provincial health care system up to $200 per call.39 All specialists and providers involved in the RACE program are satisfied and indicate that they will continue to use the service.39
In Rio Grande do Sul in Brazil, the TRU telemedicine program consists of 3 distinct streams. The first is a real-time teleconsultation hot-line that supports primary care providers (including physicians, nurses, and clinical managers) during business hours at no cost. The call is triaged and connected to the appropriate support personnel (physicians and other health professionals—the teleconsultants). These teleconsultants have considerable training and ongoing resources to support their work, including listening to previous telephone calls, technical training, and guidance on how to seek the best scientific evidence and bioethics. Professionals seeking care report their clinical doubt, and responses are based on at least 2 consolidated scientific references, remedying the problem of opinion-based informal advice that is so common in health. In 2017, 81 022 consultations were conducted. During this same period, the TRU program observed a 64% reduction in referrals to other services.40 A similar program that uses asynchronous technology, the National Telehealth Platform, with the promise of a response within 72 hours, has resulted in 27 010 teleconsultations since 2007.41
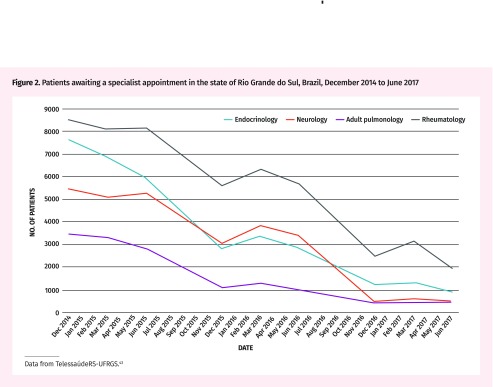
The second stream, entitled RegulaSUS, aimed to take a more proactive approach to reducing wait times for specialized services by prioritizing the care of more seriously ill patients while supporting the care of patients in primary care in their own communities.42 The program works by using a set of protocols to identify high-risk patients who likely require more immediate care and facilitating an e-consultation between primary care providers and specialists for cases that can likely be resolved virtually. Protocols were developed after an extensive literature review and peer-to-peer discussion to establish the clinical conditions that necessitate face-to-face assessment in a specialized service. Currently, this process is implemented for endocrinology, neurology, adult pulmonology, and rheumatology, and has shown a considerable reduction in waiting lists for specialist care (Figure 2).43
Figure 2.
Patients awaiting a specialist appointment in the state of Rio Grande do Sul, Brazil, December 2014 to June 2017
Data from TelessaúdeRS-UFRGS.43
The third stream focuses on the use of telediagnosis services to improve access to diagnostic examinations. Dentistry and dermatology telediagnosis services use digital photographs so that primary care providers receive timely feedback about concerning lesions (including treatment guidelines or need for referral). This has resulted in more than 2600 virtual dermatology interactions while decreasing wait times for in-person consultations.44 In addition, a network of rural spirometry clinics supported by urban respiratory specialists has resulted in 19 656 tests in 4 years to support the ongoing management of patients with asthma and chronic obstructive pulmonary disease.45
Discussion.
The results presented in this overview demonstrate different approaches to the spread and scaling of telemedicine across jurisdictions in Canada and Brazil. Of note, initial efforts in Canada were largely based on interactions between physicians and patients, resulting in service models that primarily reduce barriers to accessing specialized services, such as reduced travel costs. Therefore, many programs were developed and supported by hospital and specialist services looking to increase the reach of their services to remote areas. Over time, efforts by groups such as the OTN have managed to create impressive scale, with more than 650 000 teleconference visits conducted between 2008 and 2014 and an expanding scope of clinical services and use by both rural- and urban-based patients.31 In contrast, the lack of regulatory approval for teleconferencing services in Brazil limits the ability of clinicians to address key barriers to care access among rural patients. Given the increasing evidence of telemedicine’s benefits, including time savings, cost savings, and convenience,16,46 changes to the regulatory frameworks in the country might help drive improved access to care for the country’s large rural population.
Canada’s current telemedicine efforts often prioritize increasing individual patient access to care with limited focus on resource allocation across the health system. Only recently have regions in Canada made efforts to support primary care and the “medical home” through telemedicine. A policy paper from BC in 2015 included recommendations “ensuring that telemedicine visits are aligned with longitudinal primary care” priorities.47 Recent e-consultation efforts such as BASE in Ontario and RACE in BC are starting to show effects in supporting primary care across larger regions. Evaluations have indicated the growing potential of these programs.33,38 There is a need for system-wide scaling and continuous evaluation and monitoring of these programs to ensure their continued and successful reach for remote and rural populations in Canada. Additionally, targeted efforts to affect important health system issues, such as wait times, have not yet materialized but will be important for the future of telemedicine in Canada.
In contrast, efforts in Rio Grande do Sul have, from the start, focused on supporting the role of primary care health centres by facilitating interactions with specialized services. This has resulted in impressive effects on health system outcomes. The Ambulatory Regulation Service (RegulaSUS) has had a considerable effect on patient wait times for consultation with specialists. In January 2014 there were 172 373 people awaiting specialist services in the Rio Grande do Sul region, which was projected to reach 365 000 by December 2017 without a targeted intervention. However, recent numbers presented by the regulatory department of the State Health Department indicated that in December 2017, 81 881 people were waiting for consultation with specialists.48,49 However, it is difficult to identify which aspects of the service contributed to these reductions. The change might be owing to the scale of the service, including all primary care physician teams in the province, enabling the application of a strong systems lens for program development. By addressing both clinical and administrative questions about patient care, the TRU program removes several barriers to care within one program. This program demonstrates the potential of telehealth tools as an engine for strengthening health system coordination and targeting key deficits in rational health service delivery.
Both Canada and Brazil have the potential to learn from one another’s telemedicine programming to evolve telemedicine within their regions. While Canada exemplifies success in the provision of telemedicine to rural and remote populations (eg, OTN, BASE, and RACE), it lacks the focus on system-level issues that programs such as RegulaSUS in Brazil have evaluated. Monitoring and data collection for all telemedicine programs should be a priority in both countries to ensure that successes and failures are tracked and learned from. Advocacy in Brazil is required for a larger uptake of telemedicine among providers. Telemedicine has the potential to reduce several barriers for both patients and providers through remote monitoring, consultation, conferencing, and diagnostic services.
Conclusion
Although telemedicine is in an earlier stage in Brazil compared with Canada, there is still great opportunity for growth of the sector in both countries. A common theme is that regional differences are important determinants of access to consultations, examinations, and procedures. Both countries would benefit from a more intelligent and intentional regulatory system. A main obstacle in Brazil is that teleconsultation—that is, direct communication with patients—remains forbidden. Programs like RegulaSUS that have had considerable success could be even more effective if this type of communication between physicians and patients were available. To make this possible, the Federal Medical Council would have to modify the resolution prohibiting teleconsultation by medical professionals. In Canada, the lack of a uniform compensation strategy for providers who work in telemedicine is a barrier to adoption.
There are several challenges to the normalization of telemedicine in both Brazil and Canada. While regulatory constraints exist in both jurisdictions at the policy level, adoption, spread, and scale are often inadequate. The programs outlined in this paper have the potential for spread to other communities, if adequately funded and prioritized. Professional uptake of telemedicine must also be widespread to ensure adoption and implementation of the approach.
Finally, our analysis does not touch upon the development of artificial intelligence technologies that promise to transform and challenge medicine, including the patient-doctor relationships that we enjoy today. Both countries should consider the use of artificial intelligence in their jurisdictions to ensure the alignment of priorities between telemedicine and artificial intelligence for health care. A proactive approach, where the potential effects of artificial intelligence on access to health services are explored, is necessary.
Telemedicine is an important part of any health system, as many patients live in areas where health services remain physically inaccessible. Without telemedicine and the consideration of other technologies, we will not have a universal health system.
Editor’s key points
▸ This is the third paper in a series comparing the state of family medicine in Brazil and Canada.
▸ Brazil and Canada share expansive geographies, creating substantial barriers to health and health care for rural patients in both countries.
▸ Interventions such as telemedicine have been scaled up across large regions in both countries and are showing important effects on health care costs and outcomes.
Points saillants des auteurs
▸ Il s’agit du troisième d’une série d’articles qui comparent l’état de la médecine familiale dans deux pays : le Brésil et le Canada.
▸ Le Brésil et le Canada ont des territoires étendus, ce qui crée des obstacles importants à la santé et aux soins de santé pour les patients des zones rurales dans les deux pays.
▸ Des interventions comme la télémédecine ont été appliquées sur de vastes territoires dans les deux pays et démontrent des effets importants sur les coûts et les résultats des soins de santé.
Footnotes
Competing interests
None declared
References
- 1.Google . Size of Brazil in relation to Canada. Mountain View, CA: Google; 2018. [Google Scholar]
- 2.Canadian Collaborative Centre for Physician Resources [website] Canadian physician resources—2013 basic facts. Ottawa, ON: Canadian Medical Association; 2019. Available from: https://www.cma.ca/quick-facts-canadas-physicians. Accessed 2018 Jun 1. [Google Scholar]
- 3.Behrman J, Gaviria A, Székely M. Social exclusion in Latin America: introduction and overview. Washington, DC: Inter-American Development Bank; 2002. [Google Scholar]
- 4.Relatório global sobre o estado da segurança viária 2015. Geneva, Switz: World Health Organization; 2015. Organização Mundial da Saúde. Available from: www.who.int/violence_injury_prevention/road_safety_status/2015/Summary_GSRRS2015_POR.pdf. Accessed 2018 Aug 29. [Google Scholar]
- 5.Observatório Nacional de Segurança Viária . Atualização do custo total dos acidentes de trânsito no Brasil. Sao Paulo, Brazil: Observatório Nacional de Segurança Viária; 2015. Available from: http://iris.onsv.org.br/iris-beta/downloads/Atualizacao_Custos_20150416-2.pdf. Accessed 2020 Jan 10. [Google Scholar]
- 6.Craig J, Patterson V. Introduction to the practice of telemedicine. Telemed Telecare. 2005;11(1):3–9. doi: 10.1177/1357633X0501100102. [DOI] [PubMed] [Google Scholar]
- 7.Perednia DA, Allen A. Telemedicine technology and clinical applications. JAMA. 1995;273(6):483–8. [PubMed] [Google Scholar]
- 8.Gagnon MP, Godin G, Gagné C, Fortin JP, Lamothe L, Reinharz D, et al. An adaptation of the theory of interpersonal behaviour to the study of telemedicine adoption by physicians. Int J Med Inform. 2003;71(2–3):103–15. doi: 10.1016/s1386-5056(03)00094-7. [DOI] [PubMed] [Google Scholar]
- 9.Alexander M. Telemedicine in Australia. 1: The healthcare system and the development of telemedicine. J Telemed Telecare. 1995;1(4):187–95. doi: 10.1177/1357633X9500100401. [DOI] [PubMed] [Google Scholar]
- 10.Stainkey LA, Seidl IA, Johnson AJ, Tulloch GE, Pain T. The challenge of long waiting lists: how we implemented a GP referral system for non-urgent specialist’ appointments at an Australian public hospital. BMC Health Serv Res. 2010;10:303. doi: 10.1186/1472-6963-10-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marchildon GP. Canada. Health system review. Health Syst Transit. 2013;15(1):1–179. [PubMed] [Google Scholar]
- 12.Cylus J, Richardson E, Findley L, Longley M, O’Neill C, Steel D. United Kingdom. Health system review. Health Syst Transit. 2015;17(5):1–125. [PubMed] [Google Scholar]
- 13.Bashshur RL, Shannon GW. History of telemedicine: evolution, context, and transformation. New Rochelle, NY: Mary Ann Liebert, Inc; 2009. [Google Scholar]
- 14.Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015;(9):CD002098. doi: 10.1002/14651858.CD002098.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hersh WR, Hickam DH, Severance SM, Dana TL, Pyle Krages K, Helfand M. Diagnosis, access and outcomes: update of a systematic review of telemedicine services. J Telemed Telecare. 2006;12(Suppl 2):S3–31. doi: 10.1258/135763306778393117. [DOI] [PubMed] [Google Scholar]
- 16.Mair F, Whitten P. Systematic review of studies of patient satisfaction with telemedicine. BMJ. 2000;320(7248):1517–20. doi: 10.1136/bmj.320.7248.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jennett PA, Affleck Hall L, Hailey D, Ohinmaa A, Anderson C, Thomas R, et al. The socio-economic impact of telehealth: a systematic review. J Telemed Telecare. 2003;9(6):311–20. doi: 10.1258/135763303771005207. [DOI] [PubMed] [Google Scholar]
- 18.Zanaboni P, Wootton R. Adoption of routine telemedicine in Norwegian hospitals: progress over 5 years. BMC Health Serv Res. 2016;16(1):496. doi: 10.1186/s12913-016-1743-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Call VR, Erickson LD, Dailey NK, Hicken BL, Rupper R, Yorgason JB, et al. Attitudes toward telemedicine in urban, rural, and highly rural communities. Telemed J E Health. 2015;21(8):644–51. doi: 10.1089/tmj.2014.0125. Epub 2015 Apr 3. [DOI] [PubMed] [Google Scholar]
- 20.Iacono T, Stagg K, Pearce N, Hulme Chambers A. A scoping review of Australian allied health research in ehealth. BMC Health Serv Res. 2016;16(1):543. doi: 10.1186/s12913-016-1791-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mistry H, Garnvwa H, Oppong R. Critical appraisal of published systematic reviews assessing the cost-effectiveness of telemedicine studies. Telemed J E Health. 2014;20(7):609–18. doi: 10.1089/tmj.2013.0259. Epub 2014 May 12. [DOI] [PubMed] [Google Scholar]
- 22.Hailey D. The need for cost-effectiveness studies in telemedicine. J Telemed Telecare. 2005;11(8):379–83. doi: 10.1177/1357633X0501100801. [DOI] [PubMed] [Google Scholar]
- 23.Ontario Telemedicine Network . OTN annual report 2017/18. Toronto, ON: Ontario Telemedicine Network; 2018. Available from: https://otn.ca/wp-content/uploads/2017/11/otn-annual-report.pdf. Accessed 2020 Jan 13. [Google Scholar]
- 24.Canada’s Health Informatics Association . 2015 Canadian telehealth report. Public version. Toronto, ON: Canada’s Health Informatics Association; 2015. Available from: https://livecare.ca/sites/default/files/2015%20TeleHealth-Public-eBook-Final-10-9-15-secured.pdf. Accessed 2018 Aug 29. [Google Scholar]
- 25.Zelmer J, Ronchi E, Hyppönen H, Lupiáñez-Villanueva F, Codagnone C, Nøhr C, et al. International health IT benchmarking: learning from cross-country comparisons. J Am Med Inform Assoc. 2017;24(2):371–9. doi: 10.1093/jamia/ocw111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.College of Physicians and Surgeons of Ontario . Telemedicine. Toronto, ON: College of Physicians and Surgeons of Ontario; 2014. Available from: https://www.cpso.on.ca/Physicians/Policies-Guidance/Policies/Telemedicine. Accessed 2018 Nov 26. [Google Scholar]
- 27.Garcia LR, Silva E, Terra JCC. A comparison of telehealth programs between the USA and Brazil: a legal perspective. Smart Homecare Technol TeleHealth. 2015;3:139–45. [Google Scholar]
- 28.Maldonado JM, Marques AB, Cruz A. Telemedicine: challenges to dissemination in Brazil. Cad Saude Publica. 2016;32(Suppl 2):e00155615. doi: 10.1590/0102-311X00155615. Epub 2016 Nov 3. [DOI] [PubMed] [Google Scholar]
- 29.Harzheim E, Gonçalves MR, Umpierre RN, da Silva Siqueira AC, Katz N, Agostinho MR, et al. Telehealth in Rio Grande do Sul, Brazil: bridging the gaps. Telemed J E Health. 2016;22(11):938–44. doi: 10.1089/tmj.2015.0210. Epub 2016 Apr 20. [DOI] [PubMed] [Google Scholar]
- 30.Gonçalves MR, Umpierre RN, D’Avila OP, Katz N, Mengue SS, Siqueira ACS, et al. Expanding primary care access: a telehealth success story. Ann Fam Med. 2017;15(4):383. doi: 10.1370/afm.2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.De Souza CHA, Morbeck RA, Steinman M, Hors CP, Bracco MM, Kozasa EH, et al. Barriers and benefits in telemedicine arising between a high-technology hospital service provider and remote public healthcare units: a qualitative study in Brazil. Telemed J E Health. 2017;23(6):527–32. doi: 10.1089/tmj.2016.0158. Epub 2016 Dec 2. [DOI] [PubMed] [Google Scholar]
- 32.O’Gorman LD, Hogenbirk JC, Warry W. Clinical telemedicine utilization in Ontario over the Ontario Telemedicine Network. Telemed J E Health. 2016;22(6):473–9. doi: 10.1089/tmj.2015.0166. Epub 2015 Nov 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Champlain BASE eConsult [website] By the numbers. Ottawa, ON: Champlain BASE eConsult; 2018. Available from: https://www.champlainbaseeconsult.com/statistics. Accessed 2018 Nov 26. [Google Scholar]
- 34.Champlain BASE eConsult . Background. Ottawa, ON: Champlain BASE eConsult; 2018. Available from: https://221cf17f-efad-46eb-9bec-9296ed538058.filesusr.com/ugd/ac5147_1b98d08a8ef54af591840130b6f46693.pdf. Accessed 2018 Nov 26. [Google Scholar]
- 35.Canada Health Infoway [website] Telehealth programs benefit patients in remote areas of B.C. Toronto, ON: Canada Health Infoway; 2018. Available from: https://www.infowayinforoute.ca/en/what-we-do/blog/infoway/174-what-we-do/digital-health-and-you/stories/clinician-stories/388-telehealth-programs-benefit-patients-in-remote-areas-of-bc. Accessed 2020 Jan 13. [Google Scholar]
- 36.Interior Health Authority of British Columbia [website] Telehealth services. Connecting patients to health care through technology. Kelowna, BC: Interior Health Authority of British Columbia; 2018. Available from: https://www.interiorhealth.ca/YourCare/telehealth/Pages/default.aspx. Accessed 2020 Jan 13. [Google Scholar]
- 37.Holyk T, Pawlovich J, Ross C, Hooper A. The role of telehealth in improving continuity of care: the Carrier Sekani Family Services primary care model. B C Med J. 2017;59(9):459–64. [Google Scholar]
- 38.RACE Rapid Access to Consultative Expertise [website] What is RACE? Vancouver, BC: RACE Rapid Access to Consultative Expertise; 2018. Available from: http://www.raceconnect.ca/about-race/what-is-race. Accessed 2018 Nov 26. [Google Scholar]
- 39.Wilson M, Mazowita G, Ignaszewski A, Levin A, Barber C, Thompson D, et al. Family physician access to specialist advice by telephone. Reduction in unnecessary specialist consultations and emergency department visits. Can Fam Physician. 2016;62:e668–76. Available from: www.cfp.ca/content/cfp/62/11/e668.full.pdf. Accessed 2020 Jan 13. [PMC free article] [PubMed] [Google Scholar]
- 40.TelessaúdeRS-UFRGS . Base de dados própria: equipe de estatística: 08006446543. Porto Alegre, Brazil: TelessaúdeRS-UFRGS; 2018. [data bank]. [Google Scholar]
- 41.TelessaúdeRS-UFRGS . Base de dados própria: equipe de estatística: Plataforma Nacional de Telessaúde. Porto Alegre, Brazil: TelessaúdeRS-UFRGS; 2018. [data bank]. [Google Scholar]
- 42.Katz N. Porto Alegre, Brazil: Universidade Federal do Rio Grande do Sul; 2016. Avaliação da efetividade da realização de teleconsultorias na qualificação dos referenciamentos entre atenção primária e atenção especializada para pacientes portadores de condições crônicas em endocrinologia. [dissertation]. [Google Scholar]
- 43.TelessaúdeRS-UFRGS . Série histórica: filas de espera RegulaSUS. Porto Alegre, Brazil: TelessaúdeRS-UFRGS; 2018. [Google Scholar]
- 44.Secretaria Municipal de Saúde de Porto Alegre [website] Com telemedicina, prefeitura zera fila por consulta dermatológica. Porto Alegre, Brazil: Secretaria Municipal de Saúde de Porto Alegre; 2017. Available from: www2.portoalegre.rs.gov.br/portal_pmpa_novo/default.php?p_noticia=999194266&COM. Accessed 2018 Jun 1. [Google Scholar]
- 45.TelessaúdeRS-UFRGS . Base de dados própria: equipe de estatística: RespiraNet. Porto Alegre, Brazil: TelessaúdeRS-UFRGS; 2018. [data bank]. [Google Scholar]
- 46.Canada Health Infoway . Virtual visits in British Columbia: 2015 patient survey and physician intervention study. Summary of results. Toronto, ON: Canada Health Infoway; 2015. Available from: https://www.infoway-inforoute.ca/en/what-we-do/news-events/webinars/3105-virtual-visits-in-british-columbia-2015-patient-survey-and-physician-interview-study/view-document. Accessed 2018 Aug 29. [Google Scholar]
- 47.British Columbia Ministry of Health . Primary and community care in B.C.: a strategic policy framework. Executive summary. Vancouver, BC: British Columbia Ministry of Health; 2015. Available from: https://www.health.gov.bc.ca/library/publications/year/2015_a/primary-and-community-care-policy-paper-exec.pdf. Accessed 2018 Jun 1. [Google Scholar]
- 48.TelessaúdeRS-UFRGS . Relatório de indicadores de estrutura, processo e resultado do convênio 150/2014: Projeto RegulaSUS integração da clínica ao processo regulatório ambulatorial da Secretaria Estadual de Saúde do Rio Grande do Sul por meio de ferramentas de telessaúde aplicadas na atenção primária à saúde/atenção básica. Porto Alegre, Brazil: TelessaúdeRS-UFRGS; 2017. [Google Scholar]
- 49.Secretaria da Saúde do Estado do Rio Grande do Sul . Central Estadual de Regulação Ambulatorial (CRA-RS). Lista de espera para consultas médicas em Porto Alegre (POA)—não residentes. Porto Alegre, Brazil: Secretaria da Saúde do Estado do Rio Grande do Sul; 2018. [Google Scholar]