Abstract
Background
With advancing age, there is an increase in the time of and number of experiences with psychosocial stressors that may lead to the initiation and/or progression of chronic kidney disease (CKD). Our study tests whether one type of experience, everyday discrimination, predicts kidney function among middle and older adults.
Methods
The data were from 10 973 respondents (ages 52–100) in the 2006/2008 Health and Retirement Study, an ongoing biennial nationally representative survey of older adults in the United States. Estimated glomerular filtration rate (eGFR) derives from the Chronic Kidney Disease Epidemiology Collaboration equation. Our indicator of everyday discrimination is drawn from self-reports from respondents. Ordinary Least Squared regression (OLS) models with robust standard errors are applied to test hypotheses regarding the link between everyday discrimination and kidney function.
Results
Everyday discrimination was associated with poorer kidney function among respondents in our study. Respondents with higher everyday discrimination scores had lower eGFR after adjusting for demographic characteristics (B = −1.35, p < .05), and while attenuated, remained significant (B = −0.79, p < .05) after further adjustments for clinical, health behavior, and socioeconomic covariates.
Conclusions
Our study suggests everyday discrimination is independently associated with lower eGFR. These findings highlight the importance of psychosocial factors in predicting insufficiency in kidney function among middle-aged and older adults.
Keywords: Age, Discrimination, Kidney function
Aging is a complex process, believed to result in significant changes in the structure and function of the kidney (1–5). The ability of the kidney to regulate fluid and electrolytes remains relatively stable through 50 years of age, and then kidney function declines with advancing age (6–8). As individuals age, declining kidney function increase one’s susceptibility to severe cognitive impairment (9,10), loss of muscle strength (11), mobility limitations (12), and chronic kidney disease (CKD), which is defined by the presence of kidney damage (e.g., albuminuria ≥ 30 mg/g) and/or reduced glomerular filtration rate (eGFR) <60 mL/min/1.73m2. Data from the United States Renal Data System indicates that the prevalence of CKD among adults aged 60 and older is 32% (13). Other research suggests that two out of every three individuals will develop CKD in their lifetime, and CKD is one of the leading causes of death among older adults in the United States (14). Given the anticipated growth in middle age and older adults in the United States, the number of individuals above the age of 50 with CKD and CKD-related complications is expected to rise (15); which in turn, will lead to greater costs for both families and publicly funded programs.
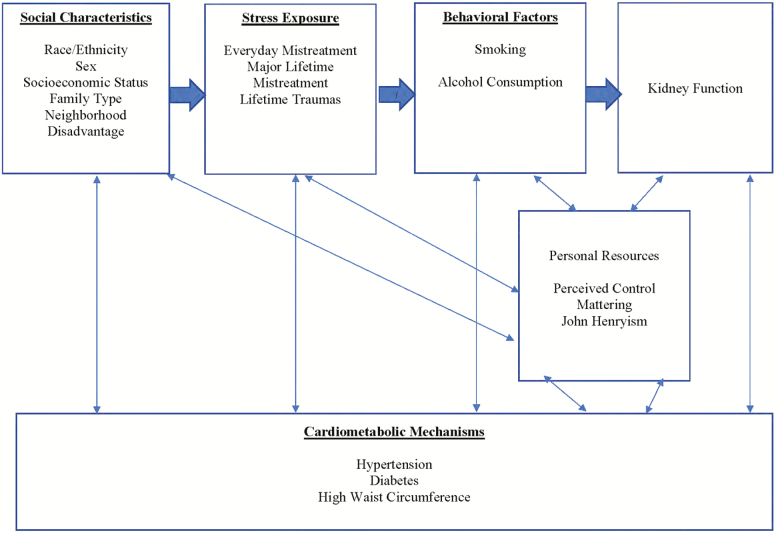
A number of risk factors are believed to contribute to insufficiency in kidney function among middle age and older adults in the United States. These factors include including hypertension (16), diabetes (17), waist circumference (18), elevated rates of inflammation (19), low socioeconomic status (20), and negative health behaviors (21). There is a reason to believe that experience with chronic stressors such as everyday discrimination (ie, minor or even trivial day-to-day hassles), which are common in late life (22), may also be a risk factor for kidney function among middle age and older adults (23). Stress theory that stressors, which often emerge from interpersonal interactions with others are patterned by social statues such as race/ethnicity, age, and sex (Figure 1). Experiences of everyday discrimination is a perceived chronic stressor that triggers a fight or flight processes that prepares one’s body for action (24). As illustrated by Figure 1 (25), advocates of this perspective contend that greater exposure to everyday discrimination overtaxes cardiovascular and metabolic systems over time, which in turn, may lead to poorer kidney function. Accordingly, a growing body of research has documented links between perceived discrimination and variations in CKD risk factors such as elevated blood pressure (26), waist circumference (27), and inflammation (25). Studies on the association between perceived discrimination and kidney function, however, are rare (28,29,30). One study found that everyday discrimination attributed to one’s gender was associated with lower levels of eGFR among respondents in the Healthy Aging in Neighborhood of Diversity Across the Life Span Study (31). A separate published study finds that a cumulative indicator of life stressors, which includes a measure everyday discrimination was negatively associated with the prevalence of CKD among respondents in the Jackson Heart Study (32).
Figure 1.
Heuristic model of the associations between perceived discrimination, cardiometabolic risk, behavioral factors, and kidney function among older adults.
Despite ongoing interest in the relationship between everyday discrimination and kidney function, we know of no study that examines this relationship among older adults. This is important, given that experiences of everyday discrimination are common among older adults (22), and ongoing evidence that everyday discrimination is a psychosocial stressor that negatively influences the health of older adults (33). Thus, we tested the hypothesis that higher levels of exposure to everyday discrimination would be independently associated with lower levels of kidney function in middle age and older adults.
Materials and Methods
Study Population
Data derives from the Health and Retirement Study (HRS), an ongoing, nationally representative biennial longitudinal study of adults above age 50 in the United States. From its beginning in 1992, HRS oversampled racial/ethnic minority respondents. The HRS is designed, among other things, to monitor changes in the physical, functional, and cognitive health of adults as they age. In 2006, the HRS began collecting biological and psychosocial information from a random half-sample of the non-institutionalized older adults in the core biennial survey (34). Specifically, HRS interviewers collected biomarkers during the in-person interview, while self-administered psychosocial questionnaires were left with HRS respondents at the end of the in-person enhanced core interview and mailed back to the HRS. The other half of the 2006 sample received the biomarker and psychosocial assessments in 2008, and the alternating cycle repeats with the sample who received the assessments each 4 years (35). The present study pooled data from the 2006 and 2008 HRS. Our analytic sample is comprised of respondents with complete demographic information (eg, age, sex, race/ethnicity, and education), biomarker measurements, and psychosocial data were included in the analyses. Complete data was available from 10 973 respondents.
Measures
Everyday discrimination
Everyday discrimination taps into routine and relatively minor experiences of mistreatment and was assessed using the short version of the Everyday Discrimination Scale (36). The HRS asked participants how often any of the following events have happened to them in their daily life: (i) “You are treated with less courtesy or respect than other people”; (ii) “You receive poorer service than other people at restaurants or stores”; (iii) “People act as if they think you are not smart”; (iv) “People act as if they are afraid of you”; and (v) “You are threatened or harassed.” The six-point response scale to each item ranges from “never” (6) to “almost everyday” (1); the items were reverse-coded, rescaled to zero, and averaged over the number of items to produce an everyday discrimination score ranging from zero to five (Cronbach’s alpha = .80). Higher scores reflect more frequent instances of everyday discrimination.
Kidney function
Our outcome, kidney function, derives from Cystatin C. Cystatin C was assayed from dried blood spots collected during the in-home assessment. HRS interviewers collected Cystatin C from respondents by pricking participants’ finger with a sterile lancet, collecting the blood droplets, and placing them on specially treated filter paper. Because of the skewed distribution of this biomarker, the HRS took the natural log to normalize the distribution (34). We calculated eGFR from our measure of Cystatin C (eGFRcysc) using the Chronic Kidney Disease Epidemiology Collaboration Cystatin C equation (37).
Demographics and Comorbidities
The present study controlled for demographic, clinical, socioeconomic, and behavioral factors that could be associated with everyday discrimination and/or kidney function among older adults. Race/ethnicity (white, black, Latino, and Other Race), age, sex, marital status, years of completed education, household income, smoking status, and drinking behaviors derive from self-reports. Our measure of diabetes combined self-reported diabetes, use of prescription diabetic medication, and an HbA1c score of 6.5% and above. Using three sitting blood pressure measurements from an automated blood pressure monitor (Omron HEM-780 Intellisense with ComFit cuff), hypertension was based on clinical outpoints (eg, average of systolic or diastolic blood pressures ≥ 140 mmHg or ≥ 90 mmHg), self-reports of hypertension, or use of anti-hypertensive prescription medication. HRS interviewers measured waist circumference by the nearest 0.1 cm with a measuring tape placed horizontally around the respondent at the narrowest part of the torso. HRS interviewers measured the respondent’s waist circumference by over undergarments or light clothing at the end of a normal exhalation. Respondents who scored in the top 25th percentile of waist circumference were coded as 1, and all else 0.
Statistical Analysis
Sample characteristics were summarized for the entire sample. Ordinary least squares (OLS) models were used to determine the association between everyday discrimination and kidney function. Model 1 examines the everyday discrimination and kidney function among older adults with adjustments for demographic covariates race/ethnicity, age, sex, and marital status. Model 2 examines the relationship between everyday discrimination and kidney function, adjusting for clinical risk factors and the covariates listed in Model 1. Model 3 includes the covariates in Model 2 as well as measures for health behaviors and socioeconomic status. Because potential overlap between race/ethnicity and experiences of everyday discrimination, interaction terms (everyday discrimination × race/ethnicity) were tested in models not shown. In each case, the interactions for blacks (p = .888), Latinos (p = .844), and those respondents of “Other Race” (p = .298) were nonsignificant.
All of these interaction terms were nonsignificant. We used sampling weights and design factors to account for non-response to the psychosocial and biomarker assessments, and for the complex study design of the HRS. All analyses were conducted using STATA 14. P-value less than .05 is considered statistically significant.
Results
Sample characteristics for the full sample are presented in Table 1. The mean eGFRcysc score among respondents in our sample is 76.1 (standard deviation [SD]: 24.6), while the average score on the everyday discrimination scale is 0.68 (SD: 0.7). Our sample is 83% white, 8% black, 6% Latino, and 2% “Other Race.” On average, respondents were 66 years of age (SD = 9.9), while a little more than half of our sample (55%) was comprised of women. Sixty-seven percent of the respondents in our study were married. Most respondents in our sample were hypertensive (66%), diabetic (64%), or have a high-risk waist circumference (61%). Forty-three percent of our sample were former smokers, while 14% currently smoke, and 57% never smoked. Respondents in our sample had an average of 12.9 (SD: 2.9) years of education and a (logged) household income of 10.64 (SD: 1.3).
Table 1.
Participant Characteristics for the Total Sample (n = 10,973)
| Total | |
|---|---|
| eGFR (mean ± SD) | 76.1 (24.6) |
| Everyday discrimination (mean ± SD) | 0.68 (0.77) |
| Demographics | |
| Race/ethnicity, % | |
| White | 83 |
| Black | 8 |
| Latino | 7 |
| Other Race | 2 |
| Age (mean ± SD) | 66.1 (9.9) |
| Female, % | 55 |
| Currently married, % | 67 |
| Clinical risk factors, % | |
| Hypertensive | 66 |
| High-risk waist circumference | 61 |
| Diabetic | 64 |
| Health behaviors, % | |
| Former smoker | 43 |
| Current smoker | 14 |
| Never smoked | 57 |
| Socioeconomic status | |
| Years of education (mean ± SD) | 13.0 (3.0) |
| Mean household income (currency, SD) | 72.72 (117.3) |
| Household income (logged) (mean ± SD) | 10.6 (1.3) |
Note: CKD = chronic kidney disease; eGFR = estimated glomerular filtration rate. Everyday discrimination ranges from 0 to 5. Source: 2006/2008 Health and Retirement Study.
Everyday Discrimination and Kidney Function
The association between kidney function and everyday discrimination is displayed in Table 2. Results from Model 1 suggest that a one-unit increase in our everyday discrimination scale was associated with poorer kidney function among older adults in our sample (B = −1.35*, standard error [SE = 0.34]). Model 2 shows that adjusting for clinical risk factors reduced but did not fully attenuate the relationship between everyday discrimination and kidney function (B = −0.98*, SE = 0.34). The relationship between everyday discrimination and poorer kidney function remained significant after further controlling for health behaviors and socioeconomic status (Model 3).
Table 2.
Ordinary Least Squared Regressions of Kidney Function on Everyday Discrimination Among Older Adults (n = 10,973)
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Everyday discrimination | −1.35* (0.34) | −0.98* (0.34) | −0.83* (0.34) |
| Clinical risk factors | |||
| Hypertension | -6.11* (0.52) | -5.83* (0.52) | |
| High-risk waist circumference | -6.35* (0.50) | -6.37* (0.51) | |
| Diabetes | -1.58* (0.49) | -1.52* (0.49) | |
| Smoking status | |||
| Non-smokers | 1.00 | ||
| Former smoker | -0.63 (0.52) | ||
| Current smoker | -4.21* (0.79) | ||
| Socioeconomic status | |||
| Years of education | 0.40* (0.09) | ||
| Household income (logged) | 0.34 (0.24) | ||
| Constant | 150.95* (2.00) | 150.95* (2.00) | 155.16* (2.07) |
| R2 | 0.22 | 0.22 | 0.26 |
Notes: All models adjust for race/ethnicity, age, sex, and current marital status. Source: 2006/2008 Health and Retirement Study.
*p < .05, Robust standard errors in parentheses.
Discussion
Over the past three decades, a growing amount of research has shown that perceived discrimination tends to disfavor the health of older adults (38–42). Though important, scholarship in this area has only begun to explore how everyday discrimination relates to kidney function among older adults (25,30).To address this gap in the literature, the present study examined the interplay between everyday discrimination and kidney function among older adults. Our findings suggest that everyday mistreatment is a risk factor for lower kidney function among older adults.
Our primary goal was to assess how everyday discrimination relates to kidney function among older adults. Prior studies on the relationship between everyday discrimination and kidney function rely on convenience samples of black or white adult population in the United States (30–32). Here, we examined data from a nationally representative sample of middle age and older adults. Based on prior research, we hypothesized that higher levels of exposure to everyday discrimination would be associated with poorer levels of kidney function among older adults and demonstrated that greater exposure to everyday discrimination was associated with lower levels of kidney function among older adults in our sample. In line with the stress process model, results from our study suggest that everyday discrimination is independently associated with poorer kidney function among older adults. The association between everyday discrimination and poorer kidney function among older adults in our study is consistent with the broader research on the psychosocial dimensions of kidney function among younger and middle-aged adults.
Consistent with hypothesis, our study also shows that the association between everyday discrimination and kidney function among respondents in our sample remained significant even after adjusting for established health behaviors, socioeconomic, and even clinical risk factors (25). Across studies, not only are hypertension, diabetes, and high-risk waist circumference are strong correlates of poorer kidney function among older adults, but everyday discrimination is also associated with these clinical risk factors for poor kidney function (29, 43). Other studies have also shown that everyday discrimination predicts higher levels of engagement in unhealthy behaviors such as alcohol consumption and tobacco use (44).
The present study has a number of strengths, including our analyzation of a nationally representative sample of older adults. The large number of biopsychosocial included in the HRS also allowed us to control for many factors that were not addressed in prior research on this topic. Additionally, our use of a Cystatin C measure of kidney function offers an advantage over prior studies, given that Cystatin C is not influenced by diet and muscle mass among older adults and has been shown to play an important role in more accurately identifying kidney function decline across racial/ethnic groups among older adults (45,46). However, our study also has limitations, which include the use of cross-sectional data at one point in time to examine this association, self-report of everyday discrimination, limited data on the extent of risk factor severity/duration, and our inability to capture potential unmeasured confounders including urinary albumin excretion which was not available. Although this work is important, future studies should address the temporality issue that derives from using cross-sectional data by examining how and why the relationship between everyday discrimination and kidney function may vary over time. Second, future work should investigate whether the relationship between everyday discrimination and kidney function persists across different measures of perceived discrimination, such as major discrimination. Finally, given ongoing evidence that the improper management of comorbid conditions among older adults with CKD increases the likelihood of death (15), future studies should examine how everyday discrimination shapes both comorbid conditions and the management of these conditions among older adults.
The increasing population of adults above the age of 50 in the United States will also bring a number of challenges, including a greater number of older adults with CKD and other kidney-related problems. Results from our study indicate that greater exposure to everyday discrimination is associated with poorer kidney function among older adults. These findings highlight the need for creating policy-based interventions that center on alleviating the health-related burden associated with the life of older adults, to delay the expression of abnormal kidney-related conditions that severely affect clinical outcomes among older adults.
Acknowledgments
R. Cobb planned the study, conducted the data analysis, wrote, and revised the paper. R Thorpe Jr. contributed to revising the article. K. Norris supervised statistical analyses and contributed to revising the article.
Funding
National Center for Advancing Translational Sciences (UL1TR000124); National Institute on Aging (K02AG059140, P30AG021684 T32 AG000037 41); National Institute on Minority Health and Health Disparities (U54MD000214).
Conflict of Interest Statement
None reported.
References
- 1. Denic A, Glassock RJ, Rule AD. Structural and functional changes with the aging kidney. Adv Chronic Kidney Dis. 2016;23(1):19–28. doi: 10.1053/j.ackd.2015.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. O’Sullivan ED, Hughes J, Ferenbach DA. Renal aging: causes and consequences. J Am Soc Nephrol. 2017;28:407–420. doi: 10.1681/ASN.2015121308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zhou XJ, Rakheja D, Yu X, Saxena R, Vaziri ND, Silva FG. The aging kidney. Kidney Int. 2008;74:710–720. doi: 10.1038/ki.2008.319 [DOI] [PubMed] [Google Scholar]
- 4. Weinstein JR, Anderson S. The aging kidney: physiological changes. Adv Chronic Kidney Dis. 2010;17:302–307. doi: 10.1053/j.ackd.2010.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bowling CB, Muntner P. Epidemiology of chronic kidney disease among older adults: a focus on the oldest old. J Gerontol A Biol Sci Med Sci. 2012;67:1379–1386. doi: 10.1093/gerona/gls173 [DOI] [PubMed] [Google Scholar]
- 6. Davies DF, Shock NW. Age changes in glomerular filtration rate, effective renal plasma flow, and tubular excretory capacity in adult males. J Clin Invest. 1950;29:496–507. doi: 10.1172/JCI102286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Johnson S, Rishi R, Andone A, et al. . Determinants and functional significance of renal parenchymal volume in adults. Clin J Am Soc Nephrol. 2011;6(1):70–76. doi: 10.2215/CJN.00030110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang X, Vrtiska TJ, Avula RT, et al. . Age, kidney function, and risk factors associate differently with cortical and medullary volumes of the kidney. Kidney Int. 2014;85(3):677–685. doi: 10.1038/ki.2013.359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Burns CM, Knopman DS, Tupper DE, et al. . Prevalence and risk of severe cognitive impairment in advanced chronic kidney disease. J Gerontol A Biol Sci Med Sci. 2018;73:393–399. doi: 10.1093/gerona/glx241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zammit AR, Katz MJ, Zimmerman ME, Bitzer M, Lipton RB. Low eGFR is associated with dysexecutive and amnestic mild cognitive impairment. Alzheimers Dement (Amst). 2015;1:152–159. doi: 10.1016/j.dadm.2014.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Toyama T, van den Broek-Best O, Ohkuma T, et al. . Associations of impaired renal function with declines in muscle strength and muscle function in older men: findings from the CHAMP study. J Gerontol A Biol Sci Med Sci. 2019;74:1812–1820. doi: 10.1093/gerona/glz100 [DOI] [PubMed] [Google Scholar]
- 12. Lattanzio F, Corsonello A, Montesanto A, et al. . Disentangling the impact of chronic kidney disease, anemia, and mobility limitation on mortality in older patients discharged from hospital. J Gerontol A Biol Sci Med Sci. 2015;70:1120–1127. doi: 10.1093/gerona/glv068 [DOI] [PubMed] [Google Scholar]
- 13. Saran R, Robinson B, Abbott KC, et al. . US renal data system 2017 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2018;71(3, Supplement 1):A7. doi: 10.1053/j.ajkd.2018.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Grams ME, Chow EKH, Segev DL, Coresh J. Lifetime incidence of CKD stages 3–5 in the United States. Am J Kidney Dis. 2013;62(2):245–252. doi: 10.1053/j.ajkd.2013.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hall RK, Zhou H, Reynolds K, Harrison TN, Bowling CB. A novel approach to developing a discordance index for older adults with chronic kidney disease. The Journals of Gerontology: Series A. 2019. doi: 10.1093/gerona/glz248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Young JH, Klag MJ, Muntner P, Whyte JL, Pahor M, Coresh J. Blood pressure and decline in kidney function: findings from the systolic hypertension in the elderly program (SHEP). J Am Soc Nephrol. 2002;13:2776–2782. doi: 10.1097/01.asn.0000031805.09178.37 [DOI] [PubMed] [Google Scholar]
- 17. Lee LT, Alexandrov AW, Howard VJ, et al. . Race, regionality and pre-diabetes in the reasons for geographic and racial differences in stroke (REGARDS) study. Prev Med. 2014;63:43–47. doi: 10.1016/j.ypmed.2014.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kramer H, Gutiérrez OM, Judd SE, et al. . Waist circumference, body mass index, and ESRD in the REGARDS (reasons for geographic and racial differences in stroke) study. Am J Kidney Dis. 2016;67:62–69. doi: 10.1053/j.ajkd.2015.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Amdur RL, Feldman HI, Dominic EA, et al. ; CRIC Study Investigators Use of measures of inflammation and kidney function for prediction of atherosclerotic vascular disease events and death in patients with CKD: findings from the CRIC study. Am J Kidney Dis. 2019;73:344–353. doi: 10.1053/j.ajkd.2018.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Nicholas SB, Kalantar-Zadeh K, Norris KC. Socioeconomic disparities in chronic kidney disease. Adv Chronic Kidney Dis. 2015;22:6–15. doi: 10.1053/j.ackd.2014.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schrauben SJ, Hsu JY, Wright Nunes J, et al. ; CRIC Study Investigators Health behaviors in younger and older adults with CKD: results from the CRIC study. Kidney Int Rep. 2019;4:80–93. doi: 10.1016/j.ekir.2018.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Luo Y, Xu J, Granberg E, Wentworth WM. A longitudinal study of social status, perceived discrimination, and physical and emotional health among older adults. Res Aging. 2012;34(3):275–301. doi: 10.1177/0164027511426151 [DOI] [Google Scholar]
- 23. Bruce MA, Beech BM, Crook ED, et al. . Association of socioeconomic status and CKD among African Americans: the Jackson Heart Study. Am J Kidney Dis. 2010;55:1001–1008. doi: 10.1053/j.ajkd.2010.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Turner RJ. Understanding health disparities: the relevance of the stress process model. Society and Mental Health. 2013;3(3):170–186. doi: 10.1177/2156869313488121 [DOI] [Google Scholar]
- 25. Bruce MA, Griffith DM, Thorpe RJ Jr. Stress and the kidney. Adv Chronic Kidney Dis. 2015;22:46–53. doi: 10.1053/j.ackd.2014.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lewis TT, Barnes LL, Bienias JL, Lackland DT, Evans DA, Mendes de Leon CF. Perceived discrimination and blood pressure in older African American and white adults. J Gerontol A Biol Sci Med Sci. 2009;64:1002–1008. doi: 10.1093/gerona/glp062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Stephan Y, Sutin AR, Terracciano A. How old do you feel? The role of age discrimination and biological aging in subjective age. PLoS One. 2015;10:e0119293. doi: 10.1371/journal.pone.0119293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lewis TT, Cogburn CD, Williams DR. Self-reported experiences of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Annu Rev Clin Psychol. 2015;11:407–440. doi: 10.1146/annurev-clinpsy-032814-112728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004;130:601–630. doi: 10.1037/0033-2909.130.4.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nguyen AW, Hamler TC, Cobb RJ. Discrimination and chronic kidney disease among Caribbean blacks: the effects of immigration and social status. Race Soc Probl. 2018;10:248–258. doi: 10.1007/s12552-018-9234-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Beydoun MA, Poggi-Burke A, Zonderman AB, Rostant OS, Evans MK, Crews DC. Perceived discrimination and longitudinal change in kidney function among urban adults. Psychosom Med. 2017;79:824–834. doi: 10.1097/PSY.0000000000000478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lunyera J, Davenport CA, Bhavsar NA, et al. . Nondepressive psychosocial factors and CKD outcomes in black Americans. Clin J Am Soc Nephrol. 2018;13:213–222. doi: 10.2215/CJN.06430617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Keith VM. Chapter 5: stress, discrimination, and coping in late life. In: Handbook of Minority Aging. Springer Publishing; 2013. https://www.springerpub.com/handbook-of-minority-aging-9780826109637.html/. Accessed February 21, 2019. [Google Scholar]
- 34. Crimmins E, Guyer H, Langa K, Ofstedal M, Wallace R, Weir D. Documentation of physical measures, anthropometrics and blood pressure in the health and retirement study. 2008.
- 35. Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, Weir DR. Cohort profile: the health and retirement study (HRS). Int J Epidemiol. 2014;43:576–585. doi: 10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shariff-Marco S, Breen N, Landrine H, et al. . Measuring everyday racial/ethnic discrimination in health surveys: how best to ask the questions, in one or two stages, across multiple racial/ethnic groups? Du Bois Rev. 2011;8:159–177. doi: 10.1017/S1742058X11000129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Inker LA, Schmid CH, Tighiouart H, et al. ; CKD-EPI Investigators Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med. 2012;367:20–29. doi: 10.1056/NEJMoa1114248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Li LW, Dong X. Self-reported discrimination and depressive symptoms among older Chinese adults in Chicago. J Gerontol A Biol Sci Med Sci. 2017;72(suppl_1):S119–S124. doi: 10.1093/gerona/glw174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ong AD, Williams DR, Nwizu U, Gruenewald TL. Everyday unfair treatment and multisystem biological dysregulation in African American adults. Cultur Divers Ethnic Minor Psychol. 2017;23:27–35. doi: 10.1037/cdp0000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dong X, Chen R, Simon MA. Experience of discrimination among U.S. Chinese older adults. J Gerontol A Biol Sci Med Sci. 2014;69(Suppl_2):S76–S81. doi: 10.1093/gerona/glu150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cobb RJ, Parker LJ, Thorpe RJ. Self-reported instances of major discrimination, race/ethnicity, and inflammation among older adults: evidence from the health and retirement study. J Gerontol A Biol Sci Med Sci. 2018. doi: 10.1093/gerona/gly267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Haroun MK, Jaar BG, Hoffman SC, Comstock GW, Klag MJ, Coresh J. Risk factors for chronic kidney disease: a prospective study of 23,534 men and women in Washington County, Maryland. J Am Soc Nephrol. 2003;14:2934–2941. doi: 10.1097/01.asn.0000095249.99803.85 [DOI] [PubMed] [Google Scholar]
- 44. Sutin AR, Terracciano A. Perceived weight discrimination and high-risk health-related behaviors. Obesity (Silver Spring). 2017;25:1183–1186. doi: 10.1002/oby.21845 [DOI] [PubMed] [Google Scholar]
- 45. Canney M, Sexton DJ, O’Connell MDL, Kenny RA, Little MA, O’Seaghdha CM. Kidney function estimated from cystatin C, but not creatinine, is related to objective tests of physical performance in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2017;72:1554–1560. doi: 10.1093/gerona/glx039 [DOI] [PubMed] [Google Scholar]
- 46. Peralta CA, Katz R, DeBoer I, et al. . Racial and ethnic differences in kidney function decline among persons without chronic kidney disease. J Am Soc Nephrol. 2011;22:1327–1334. doi: 10.1681/ASN.2010090960 [DOI] [PMC free article] [PubMed] [Google Scholar]