Abstract
Introduction
The Janus kinase (JAK) inhibitor therapeutic class has shown significant clinical benefit in the treatment of rheumatoid arthritis (RA). We sought to gain insight into the mode of action and immunological effects of filgotinib, a JAK1 selective inhibitor, in active RA by analyzing secreted and cell-based biomarkers key to RA pathophysiology in two phase 2b trials of filgotinib in active RA.
Methods
Immune cell subsets and 34 serum biomarkers were analyzed longitudinally over 12 weeks using blood samples collected from patients with active RA receiving filgotinib (100 or 200 mg once daily) or placebo (PBO) in the two phase 2b trials (DARWIN 1, on a background of methotrexate, and DARWIN 2, as monotherapy).
Results
Consistently across both studies, filgotinib treatment decreased multiple immune response biomarkers that have key roles in RA for immune response, and decreased markers that promote matrix degradation, angiogenesis, leukocyte adhesion, and recruitment. Filgotinib did not significantly modulate T and natural killer (NK) lymphoid subsets, but slightly increased B cell numbers after 12 weeks. Multiple correlations were observed for changes in biomarkers with disease activity score 28-CRP. MIP1β showed modest predictivity at baseline for ACR50 response at 12 weeks in the 100 mg filgotinib dose across both studies (AUROC, 0.65 and 0.67, p < 0.05).
Conclusions
Filgotinib regulates biomarkers from multiple pathways, indicative of direct and indirect network effects on the immune system and the stromal response. These effects were not associated with reductions of major circulating lymphoid populations.
Trial Registration
ClinicalTrials.gov, NCT01888874, NCT01894516.
Electronic supplementary material
The online version of this article (10.1007/s40744-019-00192-5) contains supplementary material, which is available to authorized users.
Keywords: Biomarkers, Cytokines, DARWIN1, DARWIN2, Filgotinib, Rheumatoid arthritis
Key Summary Points
| Why carry out this study? |
| Multiple pathophysiological pathways of inflammation, immunity, tissue extracellular matrix turnover, and joint remodeling are involved in active rheumatoid arthritis. |
| Evaluation of a broad panel of circulating biomarkers representing these pathways would aid in generating a hypothesis for the mechanism of action of JAK1 inhibition by filgotinib. |
| What was learned from the study? |
| Filgotinib regulates biomarkers from multiple pathways, indicative of direct and indirect network effects on the immune system and the stromal response. These effects were not associated with reductions of major circulating lymphoid populations. |
Introduction
Rheumatoid arthritis (RA) is a debilitating, heterogeneous, autoimmune disease characterized by chronic, systemic inflammation as well as synovitis and progressive joint destruction. Despite recent advances in the treatment of RA, a considerable number of patients experience persistent disease activity manifesting as chronic synovitis, progressive destruction of articular cartilage and bone, and functional impairment and disability [1].
Both innate and adaptive immune cellular responses mediated by cytokine activity contribute to inflammation and joint injury that characterize RA pathology. Janus kinases (JAKs) are a family of four intracellular cytoplasmic tyrosine kinases that mediate cytokine signaling from membrane receptors to the nucleus via activation of the signal-transducer and activator of transcription (STAT) factors. JAK enzymes dimerize as homo- or heterodimers that interact with transmembrane receptors of the type I/II cytokine family to regulate cell expansion, hematopoiesis, and immune responses [2]. JAK1 modulates a subset of proinflammatory cytokines within the JAK-STAT pathway including interleukin-6 (IL-6). JAK1 inhibition may be primarily responsible for the therapeutic efficacy of pan-JAK inhibitors in immune-mediated diseases, supporting the use of selective inhibition of JAK1 as a therapeutic strategy [3].
Filgotinib is a once-daily, orally administered, highly selective JAK1 inhibitor small molecule in development for the treatment of inflammatory disorders, including RA, Crohn’s disease, and ulcerative colitis [4–7]. The efficacy and safety of filgotinib as both an add-on to methotrexate (MTX) and a monotherapy have been demonstrated in two 24-week phase 2b studies in adult patients with moderately-to-severely active RA and an inadequate response to MTX (MTX-IR) [5, 6]. These results were confirmed and extended in three phase 3 randomized clinical trials in MTX-IR, MTX-naïve, and biologic disease-modifying anti-rheumatic drug-IR moderately-to-severely active RA, which met 12- or 24-week primary endpoints for efficacy [8–10].
Our aim with this study was to generate a hypothesis for the mechanism of action of JAK1 inhibition in active RA by measuring a broad panel of circulating biomarkers chosen to represent multiple pathophysiological pathways of inflammation, immunity, tissue extracellular matrix turnover, and joint remodeling, in addition to circulating immune cell subsets. The selection of these biomarkers was based on several criteria. Pharmacodynamic activity of filgotinib was characterized by measuring JAK1 cytokine ligands and downstream biomarkers. Immune effects of filgotinib were also captured with key T-cell, B-cell, and innate cell cytokines and their recruiting chemokines, together with a cell-based biomarker readout of major immune cell subsets in the blood by flow cytometry immunophenotyping. Pathogenic effectors of tissue matrix damage and cross-talk between synovial fibroblasts, endothelial cells, cartilage, and bone were founded on a clinically validated panel of soluble biomarkers that associate with RA disease activity [1, 11]. Finally, several biomarkers that have been implicated in predicting clinical therapeutic response were also included [11, 12]. By using highly sensitive multiplex immunoassays that minimized sample blood volume burden to patients, we could profile serial time points for an extensive characterization of a new molecular entity in the next generation of targeted RA therapeutics.
Methods
Study Design
DARWIN1 and DARWIN2 (clinicaltrials.gov identifiers: NCT01888874 and NCT01894516) are previously reported 24-week, multicenter, randomized, double-blind, phase 2b, dose-finding studies of orally administered filgotinib or placebo (PBO) as an add-on to MTX (DARWIN1) or as monotherapy (DARWIN2) [5, 6]. Institutional review boards (IRBs)/ethics committees (ECs) from each country reviewed and approved the protocol (see Supplementary Material for a list of the IRBs or ECs). The study was performed in compliance with the ethical principles of good clinical practice and according to the ICH Harmonised Tripartite Guideline. Patients provided written informed consent to participate in the study and had the right to withdraw at any time.
Biomarker Analysis
Biomarkers were measured in available serum samples collected at baseline (BL), and at weeks 4 and 12 in the 100 mg, 200 mg, or PBO treatment groups and stored at – 80°C until analysis. The biomarker analyses and patient characteristic summaries were performed using the biomarker analysis set, comprising randomized subjects who received ≥ 1 dose of study treatment and have ≥ 1 serum biomarker with evaluable measurement available at BL. Samples were analyzed for 34 biomarkers by validated, commercially available, single- or multiplex immunoassays (Crescendo Bioscience Vectra® DA, South San Francisco, CA, USA; Merck-Millipore Milliplex high-sensitive T-cell panel immunoassay, Burlington, MA, USA; Meso Scale Discovery, Rockville, MD, USA; and R&D Systems, Minneapolis, MN, USA). The biomarkers analyzed were IL-1β, IL-2, IL-4, IL-5, IL-6, IL-7, IL-8, IL-10, IL-12-p70, IL-13, IL-17A, IL-21, IL-23, B-cell activating factor (BAFF), interferon-γ (IFNγ), epidermal growth factor (EGF), granulocyte–macrophage colony-stimulating factor (GM-CSF), vascular endothelial growth factor (VEGF), tumor necrosis factor alpha (TNFα), soluble TNF receptor type I (TNF-RI), chemokine C-X-C motif ligands (CXCL10 and CXCL13), intercellular adhesion molecule-1 (ICAM1), leptin, macrophage inflammatory proteins (MIP-1α and MIP-1β), matrix metalloproteinases (MMP1 and MMP3), monocyte chemoattractant protein-1 (MCP1), resistin, serum amyloid A (SAA), C-reactive protein (CRP), soluble glycoprotein 130 (SGP130), vascular cell adhesion molecule-1 (VCAM1), and human cartilage glycoprotein (YKL40, also known as Chitinase-3 L1). For biomarkers below the limit of quantification of the Milliplex multiplex assay (i.e., concentrations that cannot be back-calculated from standard curves), those missing values were imputed (with concentration level of the first standard/2). Values below the lower limit of quantification (LLOQ) for other immunoassays were imputed with LLOQ-1 significant digit. Biomarker data from the IL-4 assay were excluded from further analysis as less than 50% of values at BL were measurable by the Milliplex assay.
Flow Cytometry Analysis
Immunophenotyping analysis was conducted on data from the intent-to-treat population. Whole blood was collected into BD TruCount tubes (BD Biosciences, San Jose, CA), and all testing was conducted within a centralized laboratory network with harmonized protocols. Lymphocyte subpopulations (CD3+ T cells, CD3+CD4+ T-helper cells, CD3+CD8+ cytotoxic T cells, CD19+ B cells, and CD16+CD56+ natural-killer [NK] cells) were quantified at BL, weeks 1, 2, 4, 8, and 12 by flow cytometry using the BD MultiTEST 6 Colour TBNK reagents on a BD FACSCanto. The time points for flow cytometry were conducted as part of the hematology and clinical chemistry laboratory assessments and were therefore more frequent than the biomarker collections.
Statistics
For each study, analysis of covariance model (ANCOVA) was fitted for weeks 4 and 12, respectively, to estimate the log ratio of each biomarker from BL by treatment group, after adjusting for prior biologic use and region (stratification factors), and the log-transformed BL biomarker value.
The model estimated percent change from PBO in post-BL ratio of each biomarker in filgotinib treatment arms, and the associated P values were adjusted for multiple doses per biomarker time point using Hommel’s method. Correlations between percent change in biomarkers and changes in the Disease Activity Score in 28 joints (∆DAS28)-CRP were evaluated by Spearman correlation. The area under the receiver operating characteristics curve (AUROC) was used to assess the predictive value of individual serum biomarkers at BL for treatment response (American College of Rheumatology [ACR] 20, 50, 70) at week 12. Combinations of biomarkers were also explored for identifying a predictive signature of the filgotinib treatment response by using hybrid stepwise model selection method over logistic/linear models. Wilcoxon rank-sum tests were conducted to compare the percent change of immune cells in the filgotinib-treated arm with PBO at both week 2 and week 12. All P values were reported from two-sided tests and < 0.05 were considered significant; adjustments of P values for multiplicity were not implemented, except for the ANCOVA models used to assess the treatment effect on biomarkers at multiple doses as specified above.
Results
Demographics, Baseline Disease Characteristics, and Biomarker Levels
Key demographics and BL disease characteristics were balanced across treatment groups within each study for the biomarker analysis set (411 patients) (Supplementary Table 1). Notably, BL biomarker levels were generally balanced across treatment groups within each study (Supplementary Table 2). Median biomarker levels at BL were similar in DARWIN1 and DARWIN2 (pooling all treatment groups), with the exception of IL-1β, IL-10, IL-21, GM-CSF, and TNFα, which were > 2-fold higher in DARWIN 2 (Fig. 1). The elevated cytokine levels at BL in the DARWIN2 trial were likely attributable to the absence of the immunosuppressive agent MTX.
Fig. 1.
Baseline levels (median, interquartile range) of biomarkers in DARWIN 1 (filgotinib on MTX background therapy) and DARWIN 2 (filgotinib monotherapy)
Changes from Baseline in Cytokines, Chemokines, and Markers of Tissue Degradation
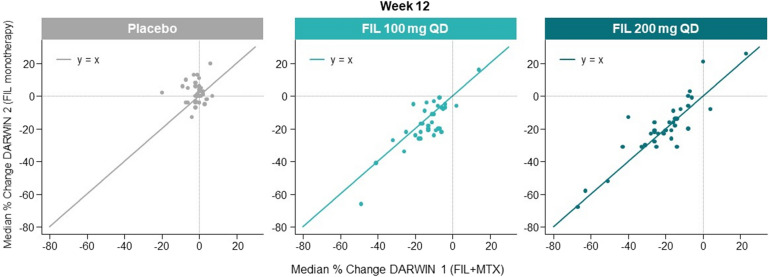
Following treatment with filgotinib, there were significant reductions in cytokines important for the expansion and activity of T-cell subsets: TH1 (IFNγ, IL-2, IL-12, and TNFα), TH2 (IL-5 [DARWIN2 only] and IL-13), TH17 (IL-1β, IL-6, IL-21, IL-23, and IL-17A [DARWIN 2 only]), B cells (CXCL13, IL-7, and IL-21), Breg/Treg (IL-10), and myeloid cells (GM-CSF) when compared with PBO (Fig. 2, Supplementary Table 3, and biomarker change from BL by treatment group in online Supplementary Figure A). The largest reductions (≥ 49% median reduction from BL in 200 mg filgotinib groups) were observed for the proinflammatory markers IL-6 and SAA. Other biomarkers with a large effect size (≥ 25% median reduction from BL in 200 mg filgotinib groups) were related to immune cell recruitment (CXCL10 and CXCL13), tissue matrix degradation (MMP1, MMP3, and YKL40), and angiogenesis (VEGF). These effects were mostly dose related, apparent at week 4, and sustained or further suppressed at week 12. Between studies, the magnitude of the percent reduction from BL to week 12 in the broad panel of cytokines was remarkably similar for filgotinib in combination with MTX or as monotherapy at both 100 mg and 200 mg once-daily doses (Fig. 3, Supplementary Table 3).
Fig. 2.

Early and sustained biomarker changes with filgotinib in DARWIN 1 and DARWIN 2 based on a model of estimated percent change from placebo in post-BL ratio of each biomarker
Fig. 3.
Percent change of biomarkers from baseline in filgotinib-treated arms were comparable in DARWIN 1 (filgotinib [FIL] + methotrexate [MTX]) and DARWIN 2 (FIL monotherapy)
Correlation Between Composite Disease Activity Measures and Individual Biomarkers
Correlations between percent change from BL in biomarker levels and ∆DAS28-CRP at week 4 or week 12 were inconsistent across the two studies, doses, and time points (Table 1). Only BAFF and ICAM1 were significant at week 12 in both studies (albeit at different doses of filgotinib). YKL40 was correlated with ∆DAS28-CRP at weeks 4 and 12 with filgotinib monotherapy. In contrast, more biomarkers were correlated with ∆DAS28-CRP in the MTX PBO group of DARWIN1. This has been previously noted, and several of these biomarkers are used in a clinically validated panel for disease activity measurement in RA [13].
Table 1.
Spearman correlations between percent change from baseline at weeks 4 and 12 of selected biomarkers (those with p ≤ 0.05) and ∆DAS28-CRP scores in the DARWIN 1 and DARWIN 2 studies
| Study | DARWIN 1 | DARWIN 2 | ||
|---|---|---|---|---|
| Week | Week 4 | Week 12 | Week 4 | Week 12 |
| Biomarker: rho (95% CI) | Biomarker: rho (95% CI) | Biomarker: rho (95% CI) | Biomarker: rho (95% CI) | |
| Placebo |
CXCL13: 0.35 (0.13, 0.53)† IL-1β: 0.32 (0.11, 0.51)† IL-2: 0.24 (0.02, 0.44)* IL-6: 0.34 (0.12, 0.53)† IL-21: 0.28 (0.06, 0.48)* SAA: 0.32 (0.08, 0.53)* |
CXCL13: 0.32 (0.11, 0.51)† ICAM1: 0.27 (0.05, 0.47)* IFNγ: − 0.23 (− 0.43, − 0.01)* IL-6: 0.30 (0.08, 0.49)† IL-17A: − 0.24 (− 0.44, − 0.02)* MMP1: 0.43 (0.21, 0.61)‡ VEGF: 0.27 (0.02, 0.48)* |
No biomarkers meeting criteria |
MMP1: 0.32 (0.04, 0.56)* SAA: 0.45 (0.18, 0.65)† SGP130: − 0.31 (− 0.53, − 0.07)* |
| FIL 100 mg |
Resistin: 0.31 (0.07, 0.52)* TNF-RI: 0.30 (0.05, 0.51)* |
IL-13: 0.33 (0.1, 0.53)† MMP1: 0.27 (0.02, 0.49)* SAA: 0.27 (0.02, 0.49)* TNF-RI: 0.31 (0.06, 0.52)* |
IL-17A: − 0.27 (− 0.49, − 0.03)* YKL40: 0.32 (0.04, 0.55)* |
BAFF: 0.30 (0.02, 0.53)* CXCL10: 0.36 (0.11, 0.56)† ICAM1: 0.30 (0.05, 0.52)* MIP1α: − 0.28 (− 0.5, − 0.04)* |
| FIL 200 mg |
BAFF: 0.33 (0.08, 0.55)* CXCL13: 0.31 (0.08, 0.5)† ICAM1: 0.27 (0.05, 0.47)* |
BAFF: 0.43 (0.19, 0.62)‡ CXCL13: 0.24 (0.01, 0.45)* ICAM1: 0.33 (0.11, 0.52)† MMP1: 0.28 (0.04, 0.48)* MMP3: 0.30 (0.06, 0.5)* |
No biomarkers meeting criteria | YKL40: 0.31 (0.05, 0.53)* |
Biomarkers without a statistically significant correlation are not shown
*p ≤ 0.05, †p ≤ 0.01, ‡p ≤ 0.001
Predictivity of BL Biomarker for Filgotinib Therapeutic Response
AUROC analysis demonstrated weak and inconsistent predictive values of individual serum biomarkers measured at BL for ACR20, 50, and 70 responses at week 12 (Table 2). Based on the ACR50 disease improvement measure, IL-6 (AUROC 0.65 95% CI [0.52, 0.78]) was modestly predictive for filgotinib 200 mg monotherapy and MIP1β (AUROC 0.65 95% CI [0.49, 0.8]) for 100 mg filgotinib monotherapy. IL-13 (AUROC 0.67, 95% CI [0.53, 0.8]) and MIP1β (AUROC 0.67, 95% CI [0.53, 0.8]) were significant predictors for 200 mg or 100 mg filgotinib in combination with MTX, respectively. No combination of these tested biomarkers better predicted treatment response as evaluated with any ACR responses or ∆DAS28-CRP (data not shown).
Table 2.
Predictive and prognostic performance of BL serum concentrations of selected biomarkers in DARWIN1 (FIL + MTX) and DARWIN2 (FIL monotherapy) studies for clinical outcomes at week 12
| Biomarker | Efficacy measure | Placebo | FIL 100 mg | ||||
|---|---|---|---|---|---|---|---|
| Biomarker level, median (Q1, Q3) | Biomarker level, median (Q1, Q3) | ||||||
| Responder | Non-responder | AUROC (95% CI) | P value | Responder | Non-responder | ||
| DARWIN1 | |||||||
| MIP1β | ACR20 | 31.3 (25.1, 39.1) | 31.3 (27.2, 41.3) | 0.47 (0.33, 0.6) | 0.627 | 33.4 (27.4, 43.9) | 26.3 (20.8, 31.6) |
| (pg/ml) | ACR50 | 33.8 (20.5, 41.5) | 31.3 (26.9, 39.1) | 0.48 (0.3, 0.66) | 0.864 | 35.2 (28.2, 44.7) | 31.0 (23, 35.5) |
| ACR70 | 39.1 (34.3, 47.7) | 30.3 (26.1, 39.1) | 0.72 (0.59, 0.84) | 0.06 | 41.9 (30.1, 44.8) | 31.2 (24.4, 37.0) | |
| IL-6 | ACR20 | 15.1 (9.7, 20.6) | 13.6 (8.3, 23.0) | 0.48 (0.35, 0.63) | 0.85 | 13.9 (8.2, 24.4) | 14.1 (8.2, 32.2) |
| (pg/ml) | ACR50 | 12.1 (9.7, 20.6) | 14.7 (9.1, 22.7) | 0.57 (0.4, 0.73) | 0.453 | 15.0 (6.5, 30.8) | 13.4 (10.2, 19.0) |
| ACR70 | 15.1 (10.1, 21.2) | 14.2 (8.7, 21.7) | 0.49 (0.27, 0.7) | 0.931 | 12.8 (5.9, 42.1) | 14.1 (9.5, 21.1) | |
| IL-13 | ACR20 | 10.9 (6.6, 20.1) | 8.5 (4.3, 13.6) | 0.59 (0.46, 0.72) | 0.186 | 11.6 (6.1, 23.3) | 10.5 (7.6, 14.8) |
| (pg/ml) | ACR50 | 10.6 (6.0, 13.9) | 8.8 (5.0, 16.8) | 0.51 (0.33, 0.68) | 0.935 | 10.2 (6.1, 21.4) | 10.9 (6.5, 22.1) |
| ACR70 | 11.4 (7.1, 17.4) | 8.8 (5.0, 16.6) | 0.56 (0.32, 0.79) | 0.637 | 10.2 (6.2, 22.4) | 10.7 (5.7, 22.0) | |
| ICAM1 | ACR20 | 325 (292, 394) | 328 (284, 384) | 0.49 (0.31, 0.65) | 0.889 | 357 (293, 406) | 290 (269, 370) |
| (ng/ml) | ACR50 | 379 (302, 395) | 324 (284, 384) | 0.51 (0.25, 0.76) | 0.941 | 372 (300, 406) | 322 (272, 388) |
| ACR70 | 373 (253, 387) | 326 (284, 387) | 0.45 (0.13, 0.78) | 0.747 | 388 (349, 436) | 323 (273, 390) | |
| CXCL13 | ACR20 | 130 (79, 182) | 117 (87, 143) | 0.55 (0.38, 0.73) | 0.576 | 127 (68, 182) | 103 (80, 121) |
| (pg/ml) | ACR50 | 130 (71, 182) | 119 (86, 160) | 0.59 (0.32, 0.86) | 0.427 | 116 (68, 190) | 107 (73, 142) |
| ACR70 | 182 (107, 243) | 119 (79, 163) | 0.61 (0.25, 0.93) | 0.471 | 116 (82, 186) | 107 (69, 152) | |
| DARWIN2 | |||||||
| MIP1β | ACR20 | 57.4 (44.2, 63.4) | 64.7 (49.1, 85.3) | 0.61 (0.45, 0.76) | 0.2 | 57.5 (46.5, 74.9) | 65.4 (55.5, 76.8) |
| (pg/ml) | ACR50 | 55.2 (46.1, 79.5) | 62.6 (48.6, 78.3) | 0.52 (0.26, 0.77) | 0.847 | 54.0 (43.7, 70.1) | 63.2 (54.4, 76.4) |
| ACR70 | 61.5 (44.6, 78.5) | 62.0 (49.1, 78.0) | 0.51 (0.03, 0.98) | 0.984 | 54.1 (44.3, 70.2) | 61.4 (52.6, 76.2) | |
| IL-6 | ACR20 | 28.8 (16.5, 36.0) | 29.7 (14.4, 57.0) | 0.54 (0.39, 0.68) | 0.624 | 25.2 (10.0, 52.7) | 22.0 (11.5, 44.1) |
| (pg/ml) | ACR50 | 22.8 (11.7, 30.5) | 31.1 (15.3, 57.5) | 0.66 (0.46, 0.84) | 0.175 | 25.2 (9.0, 53.1) | 22.0 (10.1, 46.8) |
| ACR70 | 16.8 (9.7, 23.9) | 29.8 (15.4, 55.6) | 0.73 (0.39, 1) | 0.283 | 25.2 (7.4, 63.1) | 23.6 (10.1, 50.0) | |
| IL-13 | ACR20 | 16.6 (8.5, 28.0) | 17.6 (4.8, 24.2) | 0.42 (0.28, 0.58) | 0.355 | 23.4 (10.1, 39.7) | 15.2 (8.4, 30.0) |
| (pg/ml) | ACR50 | 7.6 (7.3, 37.8) | 17.4 (6.0, 25.8) | 0.45 (0.2, 0.69) | 0.692 | 23.9 (11.5, 39.7) | 18.2 (7.1, 34.6) |
| ACR70 | 29.3 (18.4, 40.2) | 17.2 (6.1, 25.7) | 0.64 (0.25, 0.98) | 0.53 | 20.3 (10.9, 39.4) | 23.6 (8.5, 39.2) | |
| ICAM1 | ACR20 | 408 (345, 543) | 375 (311, 454) | 0.56 (0.4, 0.72) | 0.466 | 355 (304, 438) | 390 (317, 423) |
| (ng/ml) | ACR50 | 574 (357, 636) | 378 (313, 449) | 0.67 (0.39, 0.91) | 0.151 | 399 (315, 438) | 361 (304, 423) |
| ACR70 | 507 (431, 584) | 382 (313, 454) | 0.67 (0.31, 0.98) | 0.43 | 409 (332, 446) | 359 (304, 425) | |
| CXCL13 | ACR20 | 143 (76, 226) | 138 (90, 226) | 0.49 (0.34, 0.66) | 0.924 | 114 (76, 188) | 183 (97, 261) |
| (pg/ml) | ACR50 | 102 (64, 179) | 141 (91, 234) | 0.61 (0.38, 0.84) | 0.359 | 96 (79, 200) | 157 (81, 201) |
| ACR70 | 126 (92, 161) | 138 (90, 233) | 0.6 (0.22, 0.97) | 0.641 | 84 (79, 188) | 154 (82, 203) | |
| Biomarker | Efficacy measure | FIL 100 mg | FIL 200 mg | ||||
|---|---|---|---|---|---|---|---|
| Biomarker level, median (Q1, Q3) | Biomarker level, median (Q1, Q3) | ||||||
| AUROC (95% CI) | P value | Responder | Non-responder | AUROC (95% CI) | P value | ||
| DARWIN1 | |||||||
| MIP1β | ACR20 | 0.68 (0.52, 0.82) | 0.037 | 32.9 (25.6, 38.0) | 24.5 (20.7, 34.4) | 0.65 (0.5, 0.79) | 0.054 |
| (pg/ml) | ACR50 | 0.67 (0.53, 0.8) | 0.021 | 33.1 (26.3, 38.5) | 27.9 (21.7, 34.5) | 0.62 (0.48, 0.74) | 0.089 |
| ACR70 | 0.67 (0.49, 0.84) | 0.057 | 32.2 (26.0, 33.7) | 30.7 (23.1, 39.0) | 0.52 (0.37, 0.66) | 0.8 | |
| IL-6 | ACR20 | 0.5 (0.33, 0.67) | 0.96 | 12.8 (6.1, 20.5) | 12.9 (9.1, 31.7) | 0.55 (0.4, 0.71) | 0.507 |
| (pg/ml) | ACR50 | 0.54 (0.38, 0.69) | 0.62 | 12.7 (6.3, 19.9) | 12.9 (6.3, 25.0) | 0.52 (0.39, 0.65) | 0.761 |
| ACR70 | 0.47 (0.27, 0.66) | 0.733 | 12.6 (8.2, 17.7) | 13.0 (6.1, 25.2) | 0.55 (0.42, 0.69) | 0.504 | |
| IL-13 | ACR20 | 0.54 (0.39, 0.69) | 0.64 | 12.2 (4.6, 20.1) | 8.0 (4.1, 11.2) | 0.65 (0.52, 0.76) | 0.057 |
| (pg/ml) | ACR50 | 0.54 (0.4, 0.69) | 0.604 | 16.6 (5.7, 22.3) | 7.5 (4.0, 12.6) | 0.67 (0.53, 0.8) | 0.012 |
| ACR70 | 0.52 (0.34, 0.7) | 0.798 | 16.1 (5.0, 19.2) | 8.8 (4.2, 15.7) | 0.6 (0.45, 0.74) | 0.185 | |
| ICAM1 | ACR20 | 0.78 (0.6, 0.93) | 0.01 | 324 (274, 430) | 322 (304, 420) | 0.61 (0.43, 0.78) | 0.212 |
| (ng/ml) | ACR50 | 0.58 (0.39, 0.76) | 0.394 | 339 (291, 444) | 315 (268, 378) | 0.49 (0.33, 0.66) | 0.912 |
| ACR70 | 0.64 (0.44, 0.81) | 0.188 | 313 (288, 420) | 325 (278, 427) | 0.59 (0.41, 0.74) | 0.371 | |
| CXCL13 | ACR20 | 0.76 (0.61, 0.9) | 0.02 | 135 (88, 200) | 113 (66, 194) | 0.51 (0.31, 0.69) | 0.958 |
| (pg/ml) | ACR50 | 0.67 (0.48, 0.83) | 0.076 | 153 (99, 200) | 109 (66, 189) | 0.57 (0.41, 0.73) | 0.431 |
| ACR70 | 0.55 (0.35, 0.74) | 0.626 | 175 (112, 251) | 116 (67, 189) | 0.58 (0.4, 0.75) | 0.388 | |
| DARWIN2 | |||||||
| MIP1β | ACR20 | 0.59 (0.45, 0.73) | 0.275 | 51.35 (42.5, 65.8) | 53.8 (48.2, 67.4) | 0.59 (0.44, 0.74) | 0.29 |
| (pg/ml) | ACR50 | 0.65 (0.49, 0.8) | 0.039 | 51.5 (44.4, 66.8) | 51.2 (44.4, 61.6) | 0.5 (0.36, 0.64) | 0.989 |
| ACR70 | 0.63 (0.44, 0.82) | 0.142 | 52.8 (46.7, 69.7) | 51.5 (44.4, 61.6) | 0.54 (0.34, 0.74) | 0.712 | |
| IL-6 | ACR20 | 0.52 (0.37, 0.67) | 0.811 | 22.4 (9.9, 35.2) | 29.5 (19.6, 58.4) | 0.65 (0.49, 0.78) | 0.081 |
| (pg/ml) | ACR50 | 0.53 (0.38, 0.67) | 0.722 | 18.4 (7.5, 32.8) | 25.9 (16.0, 51.6) | 0.65 (0.52, 0.78) | 0.041 |
| ACR70 | 0.52 (0.34, 0.71) | 0.809 | 25.5 (10.6, 33.4) | 23.4 (12.8, 41.0) | 0.53 (0.25, 0.7) | 0.795 | |
| IL-13 | ACR20 | 0.56 (0.4, 0.71) | 0.469 | 13.0 (4.8, 22.4) | 19.6 (8.7, 32.4) | 0.61 (0.46, 0.77) | 0.183 |
| (pg/ml) | ACR50 | 0.55 (0.41, 0.7) | 0.481 | 11.4 (4.8, 17.2) | 17.8 (7.0, 30.4) | 0.63 (0.49, 0.75) | 0.083 |
| ACR70 | 0.53 (0.36, 0.7) | 0.751 | 10.9 (7.6, 15.8) | 15.1 (6.1, 28.8) | 0.56 (0.38, 0.74) | 0.583 | |
| ICAM1 | ACR20 | 0.56 (0.4, 0.72) | 0.466 | 352 (289, 421) | 368 (329, 379) | 0.51 (0.35, 0.65) | 0.946 |
| (ng/ml) | ACR50 | 0.55 (0.4, 0.69) | 0.51 | 325 (285, 393) | 360 (308, 398) | 0.56 (0.42, 0.71) | 0.435 |
| ACR70 | 0.58 (0.41, 0.74) | 0.391 | 368 (317, 424) | 352 (288, 390) | 0.58 (0.36, 0.8) | 0.478 | |
| CXCL13 | ACR20 | 0.66 (0.51, 0.81) | 0.05 | 113 (72, 204) | 153 (97, 260) | 0.59 (0.43, 0.75) | 0.266 |
| (pg/ml) | ACR50 | 0.56 (0.41, 0.7) | 0.444 | 95 (68, 235) | 135 (91, 188) | 0.55 (0.4, 0.7) | 0.483 |
| ACR70 | 0.59 (0.41, 0.76) | 0.346 | 78 (58, 201) | 129 (78, 229) | 0.64 (0.39, 0.86) | 0.205 | |
Biomarkers not shown were not predictive at any time point in either study
Immune Cell Phenotyping
Absolute lymphocyte counts at BL were comparable across treatment arms in both studies. There were transient, dose-related increases of all lymphocyte subsets in filgotinib-treated groups in the first 2 weeks of dosing that recovered to BL levels by week 12, with the exception of a sustained increase in B-cell numbers in DARWIN1 (Fig. 4). Median and interquartile ranges for all major immune cell subsets measured (B, total T, helper T, cytotoxic T, and NK cells) remained within the reference interval throughout the study period (Supplementary Figure B).
Fig. 4.
Box plots of percentage changes from baseline in absolute lymphocyte subpopulation counts at weeks 2 and 12 in the DARWIN 1 and DARWIN 2 studies
Discussion
In this study, we assessed the effects of a selective JAK1 inhibitor on an array of circulating immune and tissue biomarkers in active RA. Treatment of RA patients with filgotinib resulted in significant reductions in the levels of a broad range of biomarkers involved in multiple pathophysiological pathways (Fig. 5). Despite important differences in the study populations with regard to the presence (DARWIN1) or absence (DARWIN2) of MTX as background therapy, we demonstrated remarkably similar biomarker modulations over 12 weeks of filgotinib treatment, comparable to the efficacious clinical responses (Fig. 3). A greater relative reduction of some TH1- (IL-2, IFNγ, and IL-12) and TH2-related (IL-5 and IL-13) cytokines by filgotinib monotherapy in DARWIN2 (Fig. 2) may reflect the lack of background MTX in this study compared to DARWIN1 (Supplementary Table 3). It is interesting to note that although MTX reduces IL-6 in MTX-naïve patients [14], in the setting of MTX-IR, the JAK inhibitor (JAKinib) class retains the ability to markedly lower systemic levels of this key pathogenic mediator in RA [15, 16].
Fig. 5.
Overview of the cytokine-mediated regulation of synovial interactions.
Adapted from Ref. [37]
Filgotinib treatment induced a dose-dependent and significant decrease in a variety of biomarkers implicated in RA pathogenesis. The reduction in cytokines was significant by 4 weeks of treatment, consistent with the early onset of clinical efficacy in these phase 2b studies [5, 6]. The biomarkers that include SAA, IL-6, MMP3, CXCL10, and CXCL13 were biomarkers that showed a median reduction from BL levels ≥ 20% at both dose levels in both studies. The diversity of affected biomarkers establishes that filgotinib moderates cell activation proximally through JAK1 signaling (e.g., IL-6) and distally by reducing downstream biomarkers subsequently produced by impacted cells that go on to signal via non–JAK pathways (e.g., MMP3, CXCL10, TNFα, IL-17, and IL-1β). This process has been referred to as a network effect on immune responses [17].
The highest magnitude reductions were seen with IL-6 and its downstream targets, SAA, and probably also CXCL10, MMP1, and MMP3 [18], indicative of inhibition of JAK1 signaling and cellular biomarker output. IL-6, a key pathogenic mediator in RA, is produced by immune cells (T and B lymphocytes, macrophages), with a substantial contribution by stromal fibroblast-like synoviocytes (FLS) that involves a newly described leukemia inhibitory factor-JAK1-TYK2 autocrine amplification of IL-6 [19–21]. IL-6 was predictive of 200 mg filgotinib monotherapy ACR50 clinical response; however, this was not the case for filgotinib in combination with MTX, indicating that the serum concentration of IL-6 (either BL or post-treatment reduction) was not the sole determinant of filgotinib efficacy.
We noted significant reductions in markers that have important functional roles for activated B cells including the B-cell chemoattractant CXCL13, survival and activation marker BAFF, and biomarkers that direct germinal center and plasma-cell differentiation (IL-2, IL-5, IL-7, and IL-21). These observations are despite an increase in circulating B-cell number following filgotinib treatment. Down-modulation of BAFF may also impact the activation, proliferation, and cytokine production of other pathogenic cells in the joint, including macrophages, dendritic cells, CD4+ T cells, and FLS [22].
We observed decreases in several immune cell recruitment biomarkers (CXCL10, CXCL13, VCAM, and ICAM1). Reduced serum CXCL10 [23, 24] and CXCL13 [24, 25] levels were reported following treatment with other RA therapeutics, and CXCL10 was also reduced locally in the synovium of RA patients in response to the pan-JAK inhibitor, tofacitinib [23]. Reductions in biomarkers previously associated with the stromal response (ICAM1, VCAM, MMP1, and MMP3) have been demonstrated in the synovium after treatment with other effective RA therapies [23, 26]. Together with the significant decrease in VEGF by filgotinib, these effects could act to decrease infiltration of leukocytes at sites of synovial inflammation. Collectively, our data show that filgotinib displays effects on immune factors that are common to other treatments with demonstrated efficacy in RA. Furthermore, these findings also support a network effect of JAK1 inhibition that contributes to filgotinib mechanism of action.
Individual biomarkers in this study were modestly associated with disease activity or clinical response when using the standard composite scores, ∆DAS28-CRP and ACR response (Tables 1 and 2). The predictive ability of BL levels of IL-6 or MIP1β for filgotinib monotherapy and IL-13 or MIP-1 for filgotinib with MTX will need to be reproduced in follow-up studies for these therapeutic regimens. Multivariate analysis of biomarker combinations did not reveal predictors of clinical response for 12 weeks of filgotinib treatment. These data are consistent with other investigations seeking predictive biomarkers for RA, and, to date, there are no clinically valid predictors of response to any therapeutic. Recently, the levels of serum ICAM1 and CXCL13 have been shown as potential BL predictors of TNFα inhibitor, tocilizumab (anti–IL-6), or therapeutic response, respectively [12, 27]. We explored the impact of filgotinib on these biomarkers using a similar approach, but failed to demonstrate any predictive value for response in our MTX-IR population. Conspicuously, neither serum IL-6 nor TNFα are predictive for treatment response to targeted therapies that specifically block these cytokines [28]. We conclude that the heterogeneous and complex pathophysiology of RA, in addition to the composite clinical scores used as the outcome measure, continue to challenge the search for a predictive biomarker panel.
Mild, transient increases in total lymphocyte count, T cells (CD3, CD4, CD8), and NK cells were largely confined to the first 2 weeks of treatment with filgotinib. Significant elevation of B-cell numbers was sustained through to 12 weeks of treatment in the setting of MTX co-therapy, and a trend was evident also with filgotinib monotherapy. In the absence of major numerical changes in the examined lymphoid subsets, the observed cytokine changes could reflect a down-modulation of the pathogenic activity of these cell subsets. Furthermore, peripheral blood cytokine levels may be influenced by inflammatory activity localized to affected joints. Conversely, arthritic disease expression may be dominated by paracrine cytokine activity, which may not be fully apparent in peripheral blood [29].
Immunophenotyping of the major immune cell populations also allows indirect comparison with the reported effects of JAK inhibitors of different selectivities. Total lymphocyte count is also transiently increased by other JAK inhibitors [14, 30–33]. Sustained B-cell increases of similar magnitude to week 24 have been noted with baricitinib (JAK1/2 inhibitor) [33], while tofacitinib (JAK1/2/3 inhibitor) increased B cells in healthy subjects, and subjects with RA or psoriasis after 12 weeks of therapy, but this effect was not evident at week 24 in longer duration studies in RA [34–36]. The numerical increase in B-cell numbers is as of yet unexplained, and our data indicate that B-cell increases are not due to cytokine-driven enhanced survival or expansion, as key factors in these processes were down-regulated (IL-7 and BAFF) with treatment. Transient increases in T cells that return to pre-dose levels occur with filgotinib and tofacitinib, in contrast to the progressive reduction of total T-cell count to week 24 with baricitinib [33, 35, 36]. The differential effects on NK-cell numbers provide the most striking differences amongst JAK inhibitors. Other JAK inhibitors have decreased NK-cell numbers by week 12 of treatment; in contrast, filgotinib relatively spared NK-cell count [14, 31, 35, 36]. The decrease in NK-cell numbers with tofacitinib therapy was also associated with attenuation of functional activity, which was not investigated in our studies [36]. It is not clear why NK-cell counts were not significantly altered by filgotinib, but the counts likely reflect a balance of JAK selectivity, potency, and duration of inhibition that differs between JAK inhibitors.
There were several limitations in this study, including the approach of measuring systemic cytokine levels as a surrogate for local processes in the arthritic joint and immunophenotyping that was confined to major immune cell populations (with no further B-cell or T-cell subset analysis or cell function studies). Additionally, earlier time points may help identify key drivers of the observed network effects. Despite these limitations, blood-based biomarker panels, including the markers we analyzed in this report, have been correlated with contemporaneous clinical disease activity measures in RA (with some RA therapies), supporting mechanistic understanding of disease from selective profiling of the systemic compartment [13]. Further, as a systemic disease, with multiple organ involvement in subgroups of patients, profiling the immune status in the periphery remains a relevant analysis and may serve to better characterize the disease.
The strength of this work is the reproducibility in findings over two large, independent, placebo-controlled, randomized clinical studies. The robustness of these findings has in part been achieved by minimizing analytical variability by conducting biomarker testing at the same central laboratories using identical assays and platforms within a short time period. This is the first time that such a wide range of disease-relevant biomarkers have been profiled for a targeted synthetic disease-modifying antirheumatic drug and could set the standard for mechanistic profiling for new medications in active RA.
Conclusions
Our data demonstrate the ability of selective JAK1 inhibition to down-modulate several key inflammatory mediators of signaling pathways in RA, independent of MTX background therapy. This confirms the strong network effects (on JAK1 and downstream non–JAK pathways) of the JAK1 node in autoimmunity, matrix and cartilage degradation, angiogenesis, and leukocyte adhesion and recruitment (Fig. 5). Such broad profiling of cytokines may provide insight into the optimal JAK inhibition profile for effective treatment of RA and other autoimmune diseases.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank all the patients who participated in the DARWIN1 and DARWIN2 trials and provided samples for this analysis. PCT would like to acknowledge support by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre (BRC) and by AR UK.
Funding
This study was funded by Gilead Sciences, Inc., and Galapagos NV. Gilead Sciences, Inc., and Galapagos NV funded the Rapid Service Fee.
Medical Writing and Editorial Assistance
Writing and editorial support was provided by Beth Sesler, PhD, of Impact Communication Partners and funded by Gilead Sciences, Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Prior Presentation
Portions of the work have been presented at recent meetings:
Taylor PC, Westhovens R, Meuleners L, et al. The JAK1-selective inhibitor filgotinib displays an anti-inflammatory biomarker signature in rheumatoid arthritis patients [abstract]. Arthritis Rheumatol. 2016;68(suppl 10). https://acrabstracts.org/abstract/the-jak1-selective-inhibitor-filgotinib-displays-an-anti-inflammatory-biomarker-signature-in-rheumatoid-arthritis-patients/.
Genovese M, Li W, Goyal L, et al. Effects of the JAK1-selective inhibitor filgotinib on multibiomarker disease activity scores in patients with active rheumatoid arthritis and an inadequate response to methotrexate. Annals of the Rheumatic Diseases. 2017;76:281.
Kavanaugh A, Van der Aa A, Jamoul C, et al. Monotherapy with the JAK1-selective inhibitor filgotinib displays an anti-inflammatory biomarker profile in rheumatoid arthritis patients. Annals of the Rheumatic Diseases. 2017;76:270–271.
Taylor P, Westhovens R, Van der Aa A, et al. The JAK1-selective inhibitor filgotinib reduces multiple markers of inflammation linked to various pathologic cell types and processes in rheumatoid arthritis patients. Annals of the Rheumatic Diseases. 2017;76:281–282.
Genovese MC, Galien R, Pan Y, et al. Correlation of multi-biomarker disease activity score with clinical disease activity measures for the JAK1-selective inhibitor filgotinib as monotherapy and in combination with methotrexate in rheumatoid arthritis patients [abstract]. Arthritis Rheumatol. 2017;69(suppl 10). https://acrabstracts.org/abstract/correlation-of-multi-biomarker-disease-activity-score-with-clinical-disease-activity-measures-for-the-jak1-selective-inhibitor-filgotinib-as-monotherapy-and-in-combination-with-methotrexate-in-rheumat/.
Taylor PC, Galien R, Van der Aa A, et al. Monotherapy with filgotinib, a JAK1-selective inhibitor, reduces disease-related biomarkers in rheumatoid arthritis patients [abstract]. Arthritis Rheumatol. 2017;69(suppl 10). https://acrabstracts.org/abstract/monotherapy-with-filgotinib-a-jak1-selective-inhibitor-reduces-disease-related-biomarkers-in-rheumatoid-arthritis-patients/.
Disclosures
Jacqueline M. Tarrant is an employee of Gilead Sciences, Inc. Lovely Goyal is an employee of Gilead Sciences, Inc. Yang Pan is an employee of Gilead Sciences, Inc. Rachael Hawtin is an employee of Gilead Sciences, Inc. Wangyin Li is currently an employee of MyoKardia and was employed by Gilead Sciences, Inc., at the time the research was conducted. René Galien is an employee of Galapagos SASU. Annegret van der Aa is an employee of OCTIMET Oncology and was employed by Galapagos NV, Mechelen, Belgium at the time the research was conducted. Peter C. Taylor receives research grants from Galapagos and Eli Lilly; and receives consultancy fees from Eli Lilly, AbbVie, Gilead Sciences, Inc., Galapagos, and Pfizer.
Compliance with Ethics Guidelines
Institutional review boards (IRBs)/ethics committees (ECs) from each country reviewed and approved the protocol (see Supplementary Material for a list of the IRBs or ECs). The study was performed in compliance with the ethical principles of good clinical practice and according to the ICH Harmonised Tripartite Guideline. Patients provided written informed consent to participate in the study and had the right to withdraw at any time.
Data Availability
The data supporting the authors’ conclusions are included in the article and additional file.
Footnotes
Enhanced Digital Features
To view enhanced digital features for this article go to: 10.6084/m9.figshare.11324111.
References
- 1.Centola M, Cavet G, Shen Y, Ramanujan S, Knowlton N, Swan KA, Turner M, Sutton C, Smith DR, Haney DJ, Chernoff D, Hesterberg LK, Carulli JP, Taylor PC, Shadick NA, Weinblatt ME, Curtis J. R Development of a multi-biomarker disease activity test for rheumatoid arthritis. PLoS One. 2013;8(4):e60635. doi: 10.1371/journal.pone.0060635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O’Shea JJ, Holland SM, Staudt LM. JAKs and STATs in immunity, immunodeficiency, and cancer. N Engl J Med. 2013;368(2):161–170. doi: 10.1056/NEJMra1202117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haan C, Rolvering C, Raulf F, Kapp M, Druckes P, Thoma G, Behrmann I, Zerwes HG. JAK1 has a dominant role over JAK3 in signal transduction through gamma c-containing cytokine receptors. Chem Biol. 2011;18(3):314–323. doi: 10.1016/j.chembiol.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 4.Ito H, Takazoe M, Fukuda Y, Hibi T, Kusugami K, Andoh A, Matsumoto T, Yamamura T, Azuma J, Nishimoto N, Yoshizaki K, Shimoyama T, Kishimoto T. A pilot randomized trial of a human anti-interleukin-6 receptor monoclonal antibody in active Crohn’s disease. Gastroenterology. 2004;126(4):989–996. doi: 10.1053/j.gastro.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 5.Kavanaugh A, Kremer J, Ponce L, Cseuz R, Reshetko OV, Stanislavchuk M, Greenwald M, Van der Aa A, Vanhoutte F, Tasset C, Harrison P. Filgotinib (Glpg0634/Gs-6034), an oral selective JAK1 inhibitor, is effective as monotherapy in patients with active rheumatoid arthritis: results from a randomised, dose-finding study (Darwin 2) Ann Rheum Dis. 2017;76(6):1009–1019. doi: 10.1136/annrheumdis-2016-210105. [DOI] [PubMed] [Google Scholar]
- 6.Westhovens R, Taylor PC, Alten R, Pavlova D, Enriquez-Sosa F, Mazur M, Greenwald M, Van der Aa A, Vanhoutte F, Tasset C, Harrison P. Filgotinib (Glpg0634/Gs-6034), an oral JAK1 selective inhibitor, is effective in combination with methotrexate (Mtx) in patients with active rheumatoid arthritis and insufficient response to MTX: results from a randomised, dose-finding study (Darwin 1) Ann Rheum Dis. 2017;76(6):998–1008. doi: 10.1136/annrheumdis-2016-210104. [DOI] [PubMed] [Google Scholar]
- 7.Vainchenker W, Dusa A, Constantinescu SN. Jaks in pathology: role of Janus kinases in hematopoietic malignancies and immunodeficiencies. Semin Cell Dev Biol. 2008;19(4):385–393. doi: 10.1016/j.semcdb.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 8.Combe B, Kivitz A, Tanaka Y, van der Heijde D, Matzkies F, Bartok B, Ye L, Guo Y, Tasset C, Sundy J, Mozaffarian N, Landewé RBM, Bae S-C, Keystone EC, Nash P. Lb0001 efficacy and safety of filgotinib for patients with rheumatoid arthritis with inadequate response to methotrexate: Finch1 primary outcome results. Ann Rheum Dis. 2019;78(Suppl 2):77–78. [Google Scholar]
- 9.Westhovens R, Rigby W, van der Heijde D, Ching D, Bartok B, Matzkies F, Yin Z, Guo Y, Tasset C, Sundy J, Mozaffarian N, Messina O, Landewé RBM, Atsumi T, Burmester GR. Lb0003 efficacy and safety of filgotinib for patients with rheumatoid arthritis naïve to methotrexate therapy: Finch3 primary outcome results. Ann Rheum Dis. 2019;78(Suppl 2):259–261. [Google Scholar]
- 10.Genovese MC, Kalunian K, Gottenberg J-C, Mozaffarian N, Bartok B, Matzkies F, Gao J, Guo Y, Tasset C, Sundy JS, de Vlam K, Walker D, Takeuchi T. Effect of filgotinib vs placebo on clinical response in patients with moderate to severe rheumatoid arthritis refractory to disease-modifying antirheumatic drug therapy: the Finch 2 randomized clinical trial effect of filgotinib in rheumatoid arthritis refractory to disease-modifying antirheumatic drugs effect of filgotinib in rheumatoid arthritis refractory to disease-modifying antirheumatic drugs. JAMA. 2019;322(4):315–325. doi: 10.1001/jama.2019.9055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Han BK, Kuzin I, Gaughan JP, Olsen NJ, Bottaro A. Baseline CXCL10 and CXCL13 levels are predictive biomarkers for tumor necrosis factor inhibitor therapy in patients with moderate to severe rheumatoid arthritis: a pilot, prospective study. Arthritis Res Ther. 2016;18:93. doi: 10.1186/s13075-016-0995-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dennis G, Jr, Holweg CT, Kummerfeld SK, Choy DF, Setiadi AF, Hackney JA, Haverty PM, Gilbert H, Lin WY, Diehl L, Fischer S, Song A, Musselman D, Klearman M, Gabay C, Kavanaugh A, Endres J, Fox DA, Martin F, Townsend MJ. Synovial phenotypes in rheumatoid arthritis correlate with response to biologic therapeutics. Arthritis Res Ther. 2014;16(2):R90. doi: 10.1186/ar4555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bakker MF, Cavet G, Jacobs JW, Bijlsma JW, Haney DJ, Shen Y, Hesterberg LK, Smith DR, Centola M, van Roon JA, Lafeber FP, Welsing PM. Performance of a multi-biomarker score measuring rheumatoid arthritis disease activity in the camera tight control study. Ann Rheum Dis. 2012;71(10):1692–1697. doi: 10.1136/annrheumdis-2011-200963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kremer JM, Emery P, Camp HS, Friedman A, Wang L, Othman AA, Khan N, Pangan AL, Jungerwirth S, Keystone EC. A phase IIb study of ABT-494, a selective JAK-1 inhibitor, in patients with rheumatoid arthritis and an inadequate response to anti-tumor necrosis factor therapy. Arthritis Rheumatol. 2016;68(12):2867–2877. doi: 10.1002/art.39801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hodge JA, Kawabata TT, Krishnaswami S, Clark JD, Telliez JB, Dowty ME, Menon S, Lamba M, Zwillich S. The mechanism of action of tofacitinib—an oral Janus kinase inhibitor for the treatment of rheumatoid arthritis. Clin Exp Rheumatol. 2016;34(2):318–328. [PubMed] [Google Scholar]
- 16.Murakami K, Kobayashi Y, Uehara S, Suzuki T, Koide M, Yamashita T, Nakamura M, Takahashi N, Kato H, Udagawa N, Nakamura Y. A JAK1/2 inhibitor, baricitinib, inhibits osteoclastogenesis by suppressing Rankl expression in osteoblasts in vitro. PLoS One. 2017;12(7):e0181126. doi: 10.1371/journal.pone.0181126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moodley D, Yoshida H, Mostafavi S, Asinovski N, Ortiz-Lopez A, Symanowicz P, Telliez JB, Hegen M, Clark JD, Mathis D, Benoist C. Network pharmacology of JAK inhibitors. Proc Natl Acad Sci USA. 2016;113(35):9852–9857. doi: 10.1073/pnas.1610253113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Araki Y, Tsuzuki Wada T, Aizaki Y, Sato S, Yokota K, Fujimoto K, Kim YT, Oda H, Kurokawa R, Mimura T. Histone methylation and STAT-3 differentially regulate interleukin-6–induced matrix metalloproteinase gene activation in rheumatoid arthritis synovial fibroblasts. Arthritis Rheumatol. 2016;68(5):1111–1123. doi: 10.1002/art.39563. [DOI] [PubMed] [Google Scholar]
- 19.Calabrese LH, Rose-John S. IL-6 biology: implications for clinical targeting in rheumatic disease. Nat Rev Rheumatol. 2014;10(12):720–727. doi: 10.1038/nrrheum.2014.127. [DOI] [PubMed] [Google Scholar]
- 20.Firestein GS, Alvaro-Gracia JM, Maki R. Quantitative analysis of cytokine gene expression in rheumatoid arthritis. J Immunol. 1990;144(9):3347–3353. doi: 10.4049/jimmunol.144.9.3347. [DOI] [PubMed] [Google Scholar]
- 21.Nguyen HN, Noss EH, Mizoguchi C, Huppertz KS, Wei G, Watts FM, Brenner MB. Autocrine loop involving IL-6 family F member LIF, LIF receptor, and STAT4 drives sustained fibroblast production of inflammatory mediators. Immunity. 2017;46(2):220–232. doi: 10.1016/j.immuni.2017.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wei F, Chang Y, Wei W. The role of BAFF in the progression of rheumatoid arthritis. Cytokine. 2015;76(2):537–544. doi: 10.1016/j.cyto.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 23.Boyle DL, Soma K, Hodge J, Kavanaugh A, Mandel D, Mease P, Shurmur R, Singhal AK, Wei N, Rosengren S, Kaplan I, Krishnaswami S, Luo Z, Bradley J, Firestein GS. The JAK inhibitor tofacitinib suppresses synovial JAK1-STAT signalling in rheumatoid arthritis. Ann Rheum Dis. 2015;74(6):1311–1316. doi: 10.1136/annrheumdis-2014-206028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Han BK, Kuzin I, Gaughan JP, Olsen NJ, Bottaro B. Baseline Cxcl10 and Cxcl13 levels are predictive biomarkers for tumor necrosis factor inhibitor therapy in patients with moderate to severe rheumatoid arthritis: a pilot, prospective study. Arthritis Res Ther. 2016;18(1):93. doi: 10.1186/s13075-016-0995-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gabay C, Msihid J, Zilberstein M, Paccard C, Lin Y, Graham NMH, Boyapati A. Identification of sarilumab pharmacodynamic and predictive markers in patients with inadequate response to TNF inhibition: a biomarker substudy of the phase 3 target study. RMD Open. 2018;4(1):e000607. doi: 10.1136/rmdopen-2017-000607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kraan MC, Reece RJ, Barg EC, Smeets TJ, Farnell J, Rosenburg R, Veale DJ, Breedveld FC, Emery P, Tak PP. Modulation of inflammation and metalloproteinase expression in synovial tissue by leflunomide and methotrexate in patients with active rheumatoid arthritis. Findings in a prospective, randomized, double-blind, parallel-design clinical trial in thirty-nine patients at two centers. Arthritis Rheum. 2000;43(8):1820–1830. doi: 10.1002/1529-0131(200008)43:8<1820::AID-ANR18>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 27.Folkersen L, Brynedal B, Diaz-Gallo LM, Ramskold D, Shchetynsky K, Westerlind H, Sundstrom Y, Schepis D, Hensvold A, Vivar N, Eloranta ML, Ronnblom L, Brunak S, Malmstrom V, Catrina A, Moerch UG, Klareskog L, Padyukov L, Berg L. Integration of known DNA, RNA and protein biomarkers provides prediction of anti-TNF response in rheumatoid arthritis: results from the combine study. Mol Med. 2016;22:322–328. doi: 10.2119/molmed.2016.00078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang J, Bansal AT, Martin M, Germer S, Benayed R, Essioux L, Lee JS, Begovich A, Hemmings A, Kenwright A, Taylor KE, Upmanyu R, Cutler P, Harari O, Marchini J, Criswell LA, Platt A. Genome-wide association analysis implicates the involvement of eight loci with response to tocilizumab for the treatment of rheumatoid arthritis. Pharmacogenom J. 2013;13(3):235–241. doi: 10.1038/tpj.2012.8. [DOI] [PubMed] [Google Scholar]
- 29.Orr C, Vieira-Sousa E, Boyle DL, Buch MH, Buckley CD, Canete JD, Catrina AI, Choy EHS, Emery P, Fearon U, Filer A, Gerlag D, Humby F, Isaacs JD, Just SA, Lauwerys BR, Le Goff B, Manzo A, McGarry T, McInnes IB, Najm A, Pitzalis C, Pratt A, Smith M, Tak PP, Thurlings R, Fonseca JE, Veale DJ, Tas SW. Synovial tissue research: a state-of-the-art review. Nat Rev Rheumatol. 2017;13(8):463–475. doi: 10.1038/nrrheum.2017.115. [DOI] [PubMed] [Google Scholar]
- 30.Wollenhaupt J, Silverfield J, Lee EB, Curtis JR, Wood SP, Soma K, Nduaka CI, Benda B, Gruben D, Nakamura H, Komuro Y, Zwillich SH, Wang L, Riese RJ. Safety and efficacy of tofacitinib, an oral Janus kinase inhibitor, for the treatment of rheumatoid arthritis in open-label, long-term extension studies. J Rheumatol. 2014;41(5):837–852. doi: 10.3899/jrheum.130683. [DOI] [PubMed] [Google Scholar]
- 31.Genovese MC, Kremer J, Zamani O, Ludivico C, Krogulec M, Xie L, Beattie SD, Koch AE, Cardillo TE, Rooney TP, Macias WL, de Bono S, Schlichting DE, Smolen JS. Baricitinib in patients with refractory rheumatoid arthritis. N Engl J Med. 2016;374(13):1243–1252. doi: 10.1056/NEJMoa1507247. [DOI] [PubMed] [Google Scholar]
- 32.Dougados M, van der Heijde D, Chen YC, Greenwald M, Drescher E, Liu J, Beattie S, Witt S, de la Torre I, Gaich C, Rooney T, Schlichting D, de Bono S, Emery P. Baricitinib in patients with inadequate response or intolerance to conventional synthetic Dmards: results from the RA-BUILD study. Ann Rheum Dis. 2017;76(1):88–95. doi: 10.1136/annrheumdis-2016-210094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Emery P, McInnes I, Genovese MC, Smolen JS, Kremer J, Dougados M, Schlichting DE, Rooney T, Issa M, de Bono S, Macias WL, Rogai V, Zuckerman SH, Taylor PC. Characterization of changes in lymphocyte subsets in baricitinib-treated patients with rheumatoid arthritis in two phase 3 studies [Abstract] Arthritis Rheumatol. 2015;67(suppl 10):1364–1366. [Google Scholar]
- 34.Rizzi M, Lorenzetti R, Fischer K, Staniek J, Janowska I, Troilo A, Strohmeier V, Erlacher M, Kunze M, Bannert B, Kyburz D, Voll R, Venhoff E, Thiel J. Impact of tofacitinib treatment on human B-cells in vitro and in vivo. J Autoimmun. 2017;77:55–66. doi: 10.1016/j.jaut.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 35.Strober B, Buonanno B, Clark JD, Kawabata T, Tan H, Wolk R, Valdez H, Langley RG, Harness J, Menter A, Papp K. Effect of tofacitinib, a Janus kinase inhibitor, on haematological parameters during 12 weeks of psoriasis treatment. Br J Dermatol. 2013;169(5):992–999. doi: 10.1111/bjd.12517. [DOI] [PubMed] [Google Scholar]
- 36.Weinhold KJ, Bukowski JF, Brennan TV, Noveck RJ, Staats JS, Lin L, Stempora L, Hammond C, Wouters A, Mojcik CF, Cheng J, Collinge M, Jesson MI, Hazra A, Biswas P, Lan S, Clark JD, Hodge JA. Reversibility of peripheral blood leukocyte phenotypic and functional changes after exposure to and withdrawal from tofacitinib, a Janus kinase inhibitor, in healthy volunteers. Clin Immunol. 2018;191:10–20. doi: 10.1016/j.clim.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McInnes IB, Schett G. Cytokines in the pathogenesis of rheumatoid arthritis. Nat Rev Immunol. 2007;7:429–442. doi: 10.1038/nri2094. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data supporting the authors’ conclusions are included in the article and additional file.