Abstract
Acquired benign tracheoesophageal fistula (TOF) is a rare medical condition that usually results from trauma, foreign bodies or granulomatous infections. This is an unusual presentation of a male patient with a history of laryngectomy who has had over a period of several years inappropriately and vigorously used valve cleaning brushes to clean tracheal secretions, which has led to the formation of a TOF. Due to the patient’s obsessive habit, we could not manage him using conventional surgical methods. Instead, we opted for the placement of a salivary bypass tube, which yielded good results and recovery. To the best of our knowledge, no other case of similar aetiology has been published. We would like to highlight the importance of appropriate patient selection and education prior to performing a tracheoesophageal puncture to avoid developing life-threatening complications as demonstrated in our case report.
INTRODUCTION
Acquired tracheoesophageal fistula (Acquired TOF) is a challenging clinical condition, which is most commonly a result of malignancies [1, 2]. Benign acquired TOFs are rare and usually caused by trauma [1], granulomatous infection [1], foreign bodies [1], following an oesophagectomy or laryngectomy [2] and due to tracheal post-intubation injury [3]. In most cases, acquired benign TOFs are located in the upper to middle thirds of the trachea [3].
Clinical presentation of the condition can be variable amongst vary from patients [1]. The symptoms of the patient may include severe uncontrolled coughing on swallowing (Ono’s sign), acute dysphagia, shortness of breath, hoarseness, pulmonary infection and pneumonia [4]. Other clinical features include chest pain, pyrexia of unknown origin, haemoptysis and aspiration [4, 5]. In critical cases, patients can present with severe respiratory distress [1]. An acquired benign TOF can become life-threatening due to repeated tracheal soiling causing tracheobronchial contamination, which can lead to pulmonary sepsis and pneumonia, and meanwhile interfere with the patient’s nutrition [2, 4]. Spontaneous closure of TOF is exceptional, and this condition almost always requires surgical intervention [2, 6].
CASE REPORT
A 64-year-old male with a history of frequent chest infections presented to the department complaining of leakage from his speech valve and coughing on oral intake. The patient had a laryngectomy 16 years ago, following laryngeal cancer. Postoperatively, the patient was advised to care for his speech valve with a Blom–Singer voice prosthesis brush (Fig. 1). For the past 15 years, the patient had used the insight brush to clear tracheal mucous secretions rather than clearing the speech valve, as it allowed him deeper access to the trachea (Fig. 1). The patient was repeatedly advised by the medical and nursing staff to use the brush only to maintain the lifespan of his speech valve. As per the manufacturing guidelines, the brush should be used once a day only to clean the speech valve, but not to clear mucous secretions inside the trachea. After 1 month’s usage, a brush should be replaced. However, the patient went against the medical advice and used the brush vigorously several times a day to clean tracheal mucous secretions. As a result, he had mislaid voice prosthesis brushes numerous times in his bronchi or carina, which had to be removed by bronchoscopy.
Figure 1.

Image demonstrating on the left the insight voice prosthesis brush and on the right the Blom–Singer voice prosthesis brush.
On examination, the patient had no obvious abnormality in the valve puncture. The stoma site was normal except for some crusting around the edges. A marked abnormality on the tracheal wall ~6 cm inferior to the stoma site was revealed, through a flexible nasal endoscopic examination. The abnormality was later confirmed to be a TOF. The patient underwent a computed tomography (CT) scan to delineate the surrounding anatomy as to facilitate the planning of the surgery (Figs 2–4).
Figure 2.
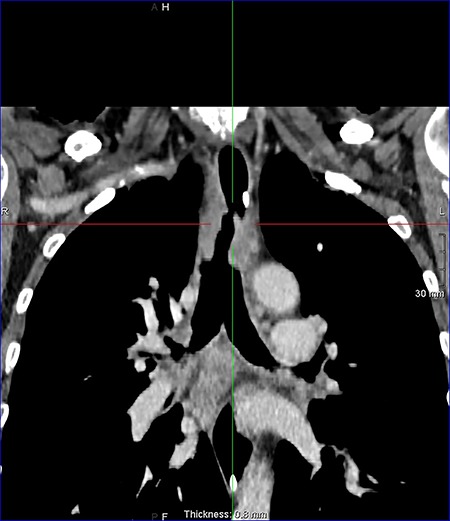
Coronal reconstruction post contrast CT neck and thorax images with 4 mm defect/tracheoesophageal fistula located 8–9 cm from tracheostomy level and 12 cm proximal to the carina.
Figure 4.

Axial reconstruction post contrast CT neck and thorax images with 4 mm defect/tracheoesophageal fistula located 8–9 cm from tracheostomy level and 12 cm proximal to the carina.
Figure 3.

Sagital reconstruction post contrast CT neck and thorax images with 4 mm defect/tracheoesophageal fistula located 8–9 cm from tracheostomy level and 12 cm proximal to the carina.
Initially, direct suturing under endoscopic guidance was attempted, which was initially successful but within a day the suture line had been disrupted by use of the brush. A percutaneous endoscopic gastrostomy was inserted for nutritional support. One option was to perform a right thoracotomy to disconnect the TOF and interposition an intercostal muscle flap between the oesophagus and trachea. However, due to the patient’s obsessive habit, this conventional surgical repair could predispose him to increased risk of dislodging the anastomosis and developing serious complications, such as mediastinitis. Hence as a definitive management, inserting a salivary bypass tube (SBT) was decided. The montgomery tube was positioned with the ends several centimetres above and below the fistula site. At 4 months follow-up, the SBT is still in situ, and the patient’s quality of life has improved as he is now managing oral intake, and the fistula has reduced in size but it has not fully healed.
DISCUSSION
In this case, the acquired benign TOF was caused by the long-term, intensive overuse of valve cleaning brush to clean tracheal mucosal secretions. According to the literature, this is the first reported case of a life-threatening complication resulting from inappropriate, chronic use of speech valve brushes. Voice prostheses are common mechanical aids advised to patients who have undergone tracheostomy or laryngectomy [7]. Regular cleaning of speech valve with a valve cleaning brush as per the recommended guidelines is essential. However, obsessive and inappropriate use of the valve cleaning brushes inside the trachea can have adverse effects as minor as mislaying speech valve brushes and as severe as TOF.
Spontaneous healing of a TOF is exceptional and cannot be relied upon [8]. Hence, in most cases, a surgical closure is the only definitive treatment [9]. In general, operative management of TOF involves the repair of the fistula, along with resection and reconstruction of the trachea when necessary [8]. Patients who are unfit for surgery are usually managed via endoscopic treatment, which is a valid alternative to surgery [8]. In this case study, the patient’s poor home management leads to a conclusion against any traditional surgical management. The attempt at direct suturing under endoscopic guidance was unsuccessful. As the standard operative management and endoscopic suturing failed, simpler definitive management in the form of an SBT was opted.
The SBT is ideal for patients with strictures of the cervical oesophagus or the pharynx, pharyngo-cutaneous fistulas and TOFs [10]. One of the main advantages of the SBT is oral feeding [10]. This can greatly improve the patient’s quality of life, as the patient no longer requires nasogastric tube feeding or intravenous supplementation [10]. Other than feeling a foreign body sensation, the SBT is a safe option that allows faster healing without any significant adverse complications [10]. In this case, the patient responded well to the SBT, and his condition improved at 4 months follow-up.
The awareness of this rare cause of TOF in this particular risk group should increase. Patients with speech valves should emphasize that the valve cleaning brushes are made only for cleaning the speech valves. Clearing mucous secretions inside the trachea with a valve cleaning brush can lead to severe complications, such as TOF. Using speech valve brushes of recommended size is necessary to maintain the lifespan of the speech valves. In patients with TOF, the definitive management would depend on the overall health status of the patient. As seen in this case, if surgical or endoscopic management is incongruous, placement of SBT is a safe option. Clearing excessive tracheal mucous in patients with speech valves is possible, with methods, such as adequate hydration, mucolytics (e.g. mucodyne), nebulized saline and chest physiotherapy. Carrying out respiratory exercises also supports the lung function; therefore, it would be beneficial in reducing the prevalence of chest infections.
References
- 1. Giquel J, Matadial C, Blanco YFR, Martinez-Ruiz R, Nguyen D, Candiotti K. An unusual case of tracheoesophageal fistulae. Case Rep Med 2012;2012. doi: 10.1155/2012/524687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Marulli G, Mammana M, Natale G, Rea F. Surgical treatment of acquired benign tracheoesophageal fistulas. J Visualized Surg 2018;4. doi: 10.21037/jovs.2018.06.07. [DOI] [Google Scholar]
- 3. Bibas BJ, Cardoso PFG, Minamoto H, Eloy-Pereira LP, Tamagno MFL, Terra RM et al. . Surgical management of benign acquired tracheoesophageal fistulas: a ten-year experience. Ann Thorac Surg 2016;102:1081–7. [DOI] [PubMed] [Google Scholar]
- 4. Diddee R, Shaw IH. Acquired tracheo-oesophageal fistula in adults. Contin Educ Anaesth Crit Care Pain 2006;6:105–8. [Google Scholar]
- 5. Green MS, Mathew JJ, Michos LJ, Green P, Aman MM. Using bronchoscopy to detect acquired tracheoesophageal fistula in mechanically ventilated patients. Anesthesiol Pain Med 2017;7. doi: 10.5812/aapm.57801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Osho A, Sachdeva U, Wright C, Muniappan A. Surgical management of tracheoesophageal fistula. Ann Cardiothorac Surg 2018;7:314–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kramp B, Dommerich S. Tracheostomy cannulas and voice prosthesis. GMS Curr Top Otorhinolaryngol Head Neck Surg 2009;8. doi: 10.3205/cto000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Caronia FP, Reginelli A, Santini N, Alfano R, Trovato S, Arrigo E et al. . Trans-tracheostomy repair of tracheo-esophageal fistula under endoscopic view in a 75-year-old woman. J Thorac Dis 2017;9:E176–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Muniappan A, Wain JC, Wright CD, Donahue DM, Gaissert H, Lanuti M et al. . Surgical treatment of nonmalignant tracheoesophageal fistula: a thirty-five year experience. Ann Thorac Surg 2013;95:1141–6. [DOI] [PubMed] [Google Scholar]
- 10. Punthakee X, Zaghi S, Nabili V, Knott PD, Blackwell KE. Effects of salivary bypass tubes on fistula and stricture formation. JAMA Facial Plast Surg 2013;15:219–25. [DOI] [PubMed] [Google Scholar]


