Abstract
The genus Aeromonas belongs to the Aeromonadaceae family and comprises a group of Gram-negative bacteria widely distributed in aquatic environments, with some species able to cause disease in humans, fish, and other aquatic animals. However, bacteria of this genus are isolated from many other habitats, environments, and food products. The taxonomy of this genus is complex when phenotypic identification methods are used because such methods might not correctly identify all the species. On the other hand, molecular methods have proven very reliable, such as using the sequences of concatenated housekeeping genes like gyrB and rpoD or comparing the genomes with the type strains using a genomic index, such as the average nucleotide identity (ANI) or in silico DNA–DNA hybridization (isDDH). So far, 36 species have been described in the genus Aeromonas of which at least 19 are considered emerging pathogens to humans, causing a broad spectrum of infections. Having said that, when classifying 1852 strains that have been reported in various recent clinical cases, 95.4% were identified as only four species: Aeromonas caviae (37.26%), Aeromonas dhakensis (23.49%), Aeromonas veronii (21.54%), and Aeromonas hydrophila (13.07%). Since aeromonads were first associated with human disease, gastroenteritis, bacteremia, and wound infections have dominated. The literature shows that the pathogenic potential of Aeromonas is considered multifactorial and the presence of several virulence factors allows these bacteria to adhere, invade, and destroy the host cells, overcoming the immune host response. Based on current information about the ecology, epidemiology, and pathogenicity of the genus Aeromonas, we should assume that the infections these bacteria produce will remain a great health problem in the future. The ubiquitous distribution of these bacteria and the increasing elderly population, to whom these bacteria are an opportunistic pathogen, will facilitate this problem. In addition, using data from outbreak studies, it has been recognized that in cases of diarrhea, the infective dose of Aeromonas is relatively low. These poorly known bacteria should therefore be considered similarly as enteropathogens like Salmonella and Campylobacter.
Keywords: Aeromonas, taxonomy, epidemiology, immune response
1. Introduction
Based on the most recent edition of the Bergey’s Manual [1], the genus Aeromonas (aer-, from Greek: gas; -monas: units; i.e., gas-producing units), belongs to the class of Gammaproteobacterias, order Aeromonadales, and family Aeromonadaceae, embracing three genera: Aeromonas, Oceanimonas, and Tolumonas [1]. The members of this genus are characterized as Gram-negative bacilli (0.3–1.0 × 1.0–3.5 µm), oxidase and catalase positive, capable of degrading nitrates to nitrites, glucose fermenters and resistant with few exceptions [2] to vibriostatic factor O/129 (2,4-Diamino-6,7-di-iso-propylpteridine phosphate). This genus comprises 36 species that are considered autochthonous of aquatic environments. They are also isolated from foods, animals, and various infectious processes in humans [1,3,4,5,6].
The taxonomy of the genus Aeromonas has always been subject to change, with 22 new species added since 1992. Identification to the species level using phenotypical characterization is difficult due to the variable behavior of the strains, which has caused a lot of confusion and erroneous identifications [7]. Molecular identification methods such as the sequences of housekeeping genes and their concatenated phylogenetic analysis (i.e., multilocus phylogenetic analysis (MLPA)) have helped to correctly recognize many of the new species of the genus by overcoming the limitation of the high similarity of the 16S rRNA gene that exits among some closely related species [8,9,10,11]. In addition, the development of several tools for genome comparison and characterization has enabled analysts to recognize wrongly labeled genomes and the role of the bacteria in the environment [12,13,14].
Several species of Aeromonas are considered as emerging pathogens because they caused a wide spectrum of disease in humans, mainly gastroenteritis, wound infections, and bacteremia/septicemia, infecting immunocompromised and immunocompetent [3,4,5]. Studies have so far reported that 96.5% of the strains associated to clinical cases were identified as one of only four species: Aeromonas caviae (29.9%), Aeromonas dhakensis (26.3%), Aeromonas veronii (24.8%), and Aeromonas hydrophila (15.5%) [5,15]. In addition, other species usually linked with fish diseases, such as Aeromonas salmonicida, have also been reported in human infections [16]. Moreover, one important issue in the study of these infections is the selection of an adequate animal model or cell line that would reproduce the pathogenicity of Aeromonas [17].
The virulence of Aeromonas has been described as multifactorial and linked to the expression of genes (exoA, alt, act, etc.) that encode different toxins, structural components (flaA, maf-5, flp, etc.), secretion systems (T3SS, T6SS, etc.), and proteins associated with metals [18,19]. The presence of these virulence factors allows the bacteria to colonize, invade, and overcome the immune response mechanism of the host, resulting in an infection that generates the disease [4,5,18,20]. Several studies demonstrated the expression of different immune-related genes in the host following an Aeromonas infection, including those involved in pathogen recognition, the proteins involved in cell signaling, and apoptosis [21,22,23,24].
The aim of this review is to provide an update on the genus Aeromonas, including recently acquired knowledge of the taxonomy, ecology, epidemiology and pathogenicity of the bacteria of this genus.
2. Historic Perspective: Past and Present
The first isolates, thought to date back to 1891, were reported by Sanarelli et al. [25], who named the bacteria as Bacillus hydrophilus fuscus (now Aeromonas hydrophila). However, the International Committee of Systematic Bacteriology established the authorship of the genus to Stanier in 1943. This genus was included in the family Vibrionaceae in 1965, with the genera Vibrio and Plesiomonas. In 1986, Colwell et al. [26] carried out a sequence analysis of the 16S rRNA and 5S rRNA genes and DNA–DNA hybridization studies, and demonstrated that Aeromonas formed a different phylogenetic branch, thus creating the Aeromonadaceae family. In the mid-1970s, the species of the genus were divided into two groups based on different characteristics: mesophilic group (optimal growth at 35–37 °C) with motile isolates, responsible for several infections in humans and defined as “A. hydrophila” and a psychrophilic group (optimal growth 22–28 °C) with non-motile strains, linked to fish diseases and identified under “A. salmonicida”. However, in the last years, many studies suggested that a growth temperature greater than 22 °C induces major rearrangements in A. salmonicida, such as the loss of the type three secretion system (T3SS) which is an important virulence factor in the bacteria, resulting in non-virulent strains in fish and model hosts. This is consistent with the fact that this bacterium infects cold-water fish, including salmonids that do not survive in temperatures above 25 °C [27,28].
The genus currently comprises 36 species (Figure 1) that have been described since 1943: Aeromonas allosaccharophila [29], Aeromonas aquatica [30], Aeromonas aquatilis [31], Aeromonas australiensis [32], Aeromonas bestiarum [33], Aeromonas bivalvium [34], Aeromonas cavernicola [35], A. caviae [36], Aeromonas crassostreae [31], A. dhakensis [37], Aeromonas diversa [38], Aeromonas encheleia [39], Aeromonas enterica [31], Aeromonas eucrenophila [36], Aeromonas finlandiensis [30], Aeromonas fluvialis [40], A. hydrophila [41], Aeromonas intestinalis [31], Aeromonas jandaei [42], Aeromonas media [43], Aeromonas molluscorum [44], Aeromonas lacus, Aeromonas lusitana [2], Aeromonas piscicola [45], Aeromonas popoffii [46], Aeromonas rivipollensis [47], Aeromonas rivuli [48], A. salmonicida [49], Aeromonas sanarellii [50], Aeromonas schubertii [51], Aeromonas simiae [52], Aeromonas sobria [53], Aeromonas taiwanensis, Aeromonas tecta [54], Aeromonas trota [42], and A. veronii [55].
Figure 1.
(A) Phylogenetic tree based on the sequences of the 16S rRNA gene (1498 bp) among 36 species of Aeromonas. (B) Phylogenetic tree based on the concatenated sequences of rpoD and gyrB genes (1098) among the most similar species based on the 16S rRNA gene. The number in the nodes indicates the bootstrap values substitutions estimated by site. (C) Results (%) for the ANI (average nucleotide identity) and isDDH (in silico DNA–DNA hybridization) obtained between the genomes of the most similar species; notice that ANI and isDDH values are ≤96% and ≤70% in all cases, respectively which are the cut-off values established for delimiting Aeromonas spp.
3. Taxonomy and Identification Methods
For the description of new prokaryotic species, the International Committee on Systematics of Prokaryotes (ICSP) recommends a polyphasic study, which should include phenotypic and phylogenetic differentiation from existing species [56]. A discussion of the criteria proposed by the ICSP in relation to the genus Aeromonas is given elsewhere [57].
3.1. Phenotypic Identification
Phenotypic identification is made by physiological, morphological, and biochemical characteristics [4,56,58]. Classic phenotypic characteristics that identify the genus Aeromonas are Gram-negative staining, the presence of normally positive cytochrome oxidase, and growth in nutritive broth at 0% to grow in the presence of vibriostatic factor O/129 [4,58]. Despite that, identification to the species level using this approach is difficult due to the variable behavior of the strains. In 2010, Beaz-Hidalgo et al. [7] re-identified 119 strains, isolated mainly from diseased fish that had previously been identified phenotypically. The re-identification was carried out by molecular methods (16S rRNA-RFLP and rpoD sequences) and the results demonstrated that only 35.5% were correctly identified at the species level.
Additionally, commercial identification systems (API 20E, Vitek, BBL Crystal, MicroScan W/A, among others) have commonly been used in clinical laboratories, although several authors demonstrated that these systems had limitations [10,59]. In 2010, Lamy et al. [59] compared the accuracy of six commercial systems for Aeromonas identification, using the rpoB sequencing as a reference. Concordance was shown to be low between phylogenetic identification and the commercial identifications systems, with erroneous identification at species level. The study also ratified results of previous studies that highlighted the confusion between Aeromonas and the genus Vibrio [59,60,61]. This confusion was evidenced again in a clinical case report that identified the strain involved as Vibrio alginolyticus, while the preliminary identification at the hospital corresponded to Aeromonas spp. using API20E [20].
3.2. Molecular Identification
3.2.1. Techniques Based on the 16S rRNA Gene
The 16S rRNA gene is considered a stable molecular marker for identifying bacterial species, since its distribution is universal and allows comparison of microorganisms [56,57,62,63]. In addition, its structure presents a mosaic of variable regions, suitable in the differentiation of closely related organisms, and their conserved regions are useful for the distant organisms comparison and this allows for the design of “universal” primers [64].
In 1992, Martínez-Murcia et al. [8] sequenced the 16S rRNA gene for the first time using strains of the species described up to then; the results agreed with the DNA–DNA hybridization (DDH). In the genus Aeromonas, the 16S rRNA gene has an interspecies similarity range from 96.7–100% and the informative nucleotide positions are located mainly on region V3 [63,64].
Additionally, the presence of microheterogeneities (i.e., mutations on specific positions of the sequence of one of several copies of the 16S rRNA gene) in combination with the high similarity of the sequences for closely related species makes this gene not suitable for the Aeromonas spp. identification [64,65,66]. Figure 1 shows the phylogenetic tree derived from sequences of the 16S rRNA gene of the 36 Aeromonas species.
Matrix-assisted laser desorption/ionization time of flight mass spectrometry (MALDI-TOF MS) is a powerful method introduced to many clinical laboratories in recent years for the identification and comparison of microbial isolates [20,67]. The MALDI-TOF MS mainly detects proteins associated with the 16S rRNA gene and therefore the low resolution of this gene for the identification of closely related species of Aeromonas also impacts the resolution of this method [15].
Chen et al. [68] used the MALDI-TOF MS to characterize 217 clinical isolates previously identified by rpoB sequencing and found that 100% were correctly identified at genus level, and 97% at species level. One-year later, Shin et al. [69] re-identified 65 clinical strains previously identified by gyrB sequencing and showed 98.5% concordance at genus level, and 92.3% at the species level using the MALDI-TOF MS. These results are relatively similar to those reported by Latif-Eugenín [15] who identified 179 clinical strains from Spanish hospitals, with 98.3% correct identification at genus level, and 91.1% at species level using MALDI-TOF MS. Based on those data, they suggested that MALDI-TOF MS is a useful tool, since the identification error was <10%, while with phenotypic identification methods error can be very high. The main limitation of the latter method is the need to update the database to include the many missing Aeromonas species, such as A. dhakensis or the new species (A. intestinalis, A. crassostreae, A. enterica, and A. aquatilis). A recent study that used MALDI-TOF MS for the characterization of Aeromonas strains isolated from fish [70] demonstrated that the number of correct identifications increased after the addition of 14 new spectra in the MALDI-TOF Biotyper database.
3.2.2. Housekeeping Genes
Housekeeping genes (HKG) encode proteins with essential functions for the survival of bacteria. They were introduced for the description of new species using an MLPA because the resolution is higher than the 16S rRNA gene [56,71]. For taxonomic analysis, the ideal HKG should have the following characteristics: (1) they should not be influenced by horizontal gene transfer; (2) they should be present in all bacteria; (3) they should be single genes in the genome of the bacteria; (4) and finally they should present at least two conserved regions for the design of primers [72].
The first HKG studied of Aeromonas was the gyrB gene that encodes the subunit B of DNA gyrase [9]. Another HKG that shows a similar phylogeny to gyrB is the rpoD gene that encodes sigma factor S70 (that confers promoter-specific transcription initiation for the RNA polymerase) [10]. These genes were used to recognize and describe many species in recent years [2,30,31,32,35,37,38,40,45,47,48,50,54]. The phylogenetic tree derived from sequences of gyrB and rpoD genes of 22 highly similar Aeromonas species based on the 16S rRNA gene is presented in Figure 1. Many studies have described other HKG: rpoB, recA, dnaJ, cpn60, mdh, gyrA, dnaX, atpD, groL, gltA, metG, ppsA, dnaK, radA, tsF, and zipA [11,38,66,73,74,75,76,77]. However, the phylogeny based on the sequence of only one HKG is sometimes not conclusive and a higher resolution is obtained using the concatenated sequences of several HKG [56,57,64]. In 2011, Martínez-Murcia et al. [11] described the first MLPA of the genus Aeromonas using the concatenated sequences of seven genes (rpoD, gyrB, gyrA, atpD, recD, dnaJ, and dnaX).
3.2.3. Genotyping Methods
Different molecular methods have been employed to trace whether two isolates of Aeromonas belong, or not, to the same clone and therefore share an epidemiological relationship [20,64]. These methods are the enterobacterial repetitive intergenic consensus-PCR (ERIC-PCR), the randomly amplified polymorphic DNA-PCR (RAPD-PCR), the amplified fragment length polymorphism (AFLP), the pulsed-field gel electrophoresis (PFGE), and the multilocus sequence typing (MLST) [20,64].
The ERIC-PCR is one of the most popular methods for genotyping Aeromonas because it is easy to carry out, does not require any expensive equipment, and is highly reproducible [3,78]. Consequently, it has been used in several epidemiological studies [79,80,81,82]. In a recent study, one strain of A. caviae isolated from a sample of lettuce showed the same ERIC genotype pattern as a strain recovered from a sample of irrigation water [82]. In addition, the same genotype of A. sanarellii was recovered in samples of parsley and tomato that were irrigated with the same reclaimed water, confirming the potential health risk to humans [82].
The MLST is based on the analysis of the sequences of several genes, normally seven, to recognize allele sequences (83). This technique show to be highly discriminatory and reproducible compared with other techniques, and there is also a database to help investigators compare their results. The Bacterial Isolate Genome Sequence Database (BIGSdb) is the platform that currently manages the MLST database [83] and can be found within the PubMLST public databases. The MLST scheme is freely available and was created for Aeromonas in 2010 based on the data obtained by Martino et al. [77] using six genes (gyrB, groL, gltA, metG, ppsA, and recA). The major problem of the latter technique is the need for perfect sequences of seven housekeeping genes (450–500 bp each gene) with no ambiguities, and result comparison might be limited by the number of strains and origins available in the database, which in its last update (22 October 2019) had 751 strains, and 2817 sequences that corresponded to 652 MLST profiles (available online: https://pubmlst.org/Aeromonas/submission.shtml consulted on 22 October 2019).
3.2.4. Genomics
As of 2 September 2019, 410 Aeromonas genomes were made publicly available in the GenBank database, of which 63 are complete (available online: https://www.ncbi.nlm.nih.gov/genome/?term=Aeromonas). The size of Aeromonas genomes varies between 3.90 Mbp (A. fluvialis) and 5.18 Mbp (A. piscicola) with an average size of 4.51 Mbp [19]. Furthermore, the percentage of G + C was 60.2%, varying between 58.1% (A. australiensis) and 62.8% (A. taiwanensis).
Advances in methods of obtaining complete genomes have increased the number of available genomes in recent years. In fact, only six Aeromonas genomes were available in 2012 [84,85,86,87,88,89] and just two years later, that increased to 56 genomes representing 29 recognized or proposed species of the genus Aeromonas [90]. In 2015, using MLPA and pairwise comparison using the average nucleotide identity (ANI), Beaz-Hidalgo et al. [12] re-identified 44 genomes that were deposited in GenBank, demonstrating that 14 were wrongly labeled by using the MLPA and pairwise comparison using the ANI. The data obtained in that study showed the importance of verifying the taxonomic position of a genome, using the mentioned tools (MLPA and ANI) before submission to the NCBI or other databases. These misidentifications might also be determined using another tool based on genome comparison (i.e., in silico DNA–DNA hybridization (isDDH)) [12,58,90].
The experimental DDH is commonly used for species delineation [48]. However, this technique produces errors and takes up a lot of time. The isDDH described by Kolthoff et al. [91], using the genome-to-genome distance calculator (GGDC) developed by DSMZ (Leibniz Institute DSMZ-German Collection of Microorganisms and Cell Cultures GmbH, Braunschweig, Germany) showed to be an excellent tool for determining the genetic similarity between two bacteria genomes. The results ≥70% indicates that these two strains belong to the same species (Figure 1). Moreover, in 2009, Richter and Rosselló-Mora [92] defined the ANI as the percentage of identity that can be found in the nucleotide sequences of orthologous genes common in the two genomes (Figure 1). Based on different studies [92,93] the cut-off value was established at 95–96% and the results agreed with isDDH. There are several tools to calculate ANI values: JSpecies, ANI calculator, OrthoANI, and OrthoANI-usearch tool. The cut-off for Aeromonas was established in 2014 by Colston et al. [90]. In the study, 56 Aeromonas genomes were analyzed, suggesting that values ≥96% indicate that the two strains belong to different species. Figueras et al. [14] indicated that the ANI and the MLPA are excellent tools for verifying the identity of genomes before they are deposited in GenBank, which would prevent them from being mislabeled. In fact, Beaz-Hidalgo et al. [12] used these tools for re-identifying the genomes deposited in the NCBI, and found that 35.9% of the genomes of non-type strains of Aeromonas spp. were incorrectly labeled. Recently, different studies used the genomic indices to increase the correct identification of ambiguous Aeromonas strains, supporting the notion that these methods are essential in taxonomy [94,95,96].
4. Ecology and Epidemiology
The genus Aeromonas is widely distributed across numerous ecosystems, although it is more commonly found in various aquatic environments [4,6,32]. These microorganisms have also been isolated from several environmental and clinical samples [4,97].
4.1. Aeromonas in Aquatic Environments
Aeromonas are indigenous to aquatic environments and have been isolated from surface, underground, potable, bottled, residual, seawater, and irrigation waters [4,6,98,99,100,101,102,103]. Araujo et al. [104] established that the concentration of Aeromonas can be linked to terrestrial water effluents. In a study of rivers and lakes in Finland, 116 strains of Aeromonas were recovered, which were thought to be linked to cyanobacteria blooms [105,106] and these strains were re-identified by Beaz-Hidalgo et al. [5], thus allowing the description of three new species (A. aquatica, A. finlandiensis, and A. lacus).
The incidence of Aeromonas in wastewater is high [107,108,109,110,111]. Conventional treatments to reclaim water at wastewater treatment plants (WWTPs), such as a primary and secondary or biological treatment, do not greatly reduce the concentration of Aeromonas [6]. However, if additional tertiary treatments are carried out such as chemical (ozone, chlorination) and physical (ultraviolet radiation) treatments, Aeromonas can be completely eliminated [82,112,113,114]. Another natural tertiary treatment is lagooning. It is a process of purification which reduces the levels of Aeromonas by temporarily storing the wastewater in shallow ponds or lagoons [115,116,117]. Depending on the microbiological quality of the reclaimed water, it can be used for irrigation [32,82,113]. Irrigated waters containing Aeromonas can contaminate fruits and vegetables [82,118] and thus cause infection in humans. In fact, there is epidemiological evidence that water acts as a vehicle for the dissemination of this bacterium, because it has been possible to identify the same Aeromonas strains in drinking water samples and in the feces of individuals with diarrhea [119,120]. In another study, the same strains isolated from lettuce and tomatoes were recovered from the irrigation water [113].
There are numerous studies in which the presence of Aeromonas was detected in drinking water [3,6,100] and concentrations are related to the ability to regrow in the system [110,121], which is influenced by the amount of available nutrients, temperature, and concentration of residual chlorine [6,122]. Latif-Eugenín et al. [82] also showed the importance of culture conditions for the detection of Aeromonas in water.
Metagenomic studies of wastewater revealed Aeromonas to be one of the prevailing bacteria probably due to its capacity to regrow in the sewerage system [107].
4.2. Aeromonas in Food
Aeromonas have been isolated from fruits, vegetables, dairy products, meats and sausages, fish, and shellfish [58,123,124,125,126,127,128,129]. The temperature, salinity or pH are the factors that determine the number of Aeromonas in these foods [1]. In fact, in the case of temperature, several authors reported that Aeromonas survive in low temperatures (2–10 °C). Additionally, salt or sodium chloride (NaCl) is a common preservative for meat products and raw fish, however, Aeromonas are able to grow in NaCl concentrations of up to 4%. Finally, pH is another parameter that controls bacterial growth in food. It was demonstrated that Aeromonas can survive at pH = 5 [14,130].
Many studies have investigated the incidence of Aeromonas in meat products [128,131,132]. Based on the sequencing of HKG like rpoD and gyrB, the most prevalent species were A. veronii, A. salmonicida, A. jandaei A. simiae, A. hydrophila, and A. caviae [81,125]. In the case of fish intended for human consumption, tilapia and salmonids bare many Aeromonas spp. that after molecular identification corresponded to A. salmonicida, A. bestiarum, A. veronii, A. encheleia, A. hydrophila, A. allosaccharophila, and A. bivalvium [128,133]. In relation to shellfish, Aeromonas is often isolated from mussels, oysters, shrimps, and cockles, and based on molecular identification methods the diversity of Aeromonas species is similar to the species found in fish [128,134,135]. However, as several authors reported, Aeromonas infections are often under-diagnosed or even misdiagnosed, changing the values based on the diagnostic methods.
Different studies report the isolation of Aeromonas from fruits and vegetables, such as carrots, tomatoes, lettuces, cucumber, potatoes, onions, and celery [123,124,125]. Among the species detected A. hydrophila and A. caviae were the most prevalent clinical species [123,124,125]. These foods, together with contaminated water are the main source of infection by Aeromonas in diarrhea [128,136].
4.3. Aeromonas in Animals
The genus Aeromonas has been considered an animal pathogen since its first isolation from septicemias in frogs and sick fish [7,45,137]. The important fish pathogens species are A. salmonicida and A. hydrophila, which particularly affect salmonids, causing ulcers, hemorrhages, furunculosis, and septicemias [7,45]. These infections cause important financial losses in the aquaculture industry [4,7,16,45,88]. In fact, Rasmussen-Ivey et al. [138] described a hypervirulent A. hydrophila strain as a causative agent of worldwide outbreaks in warm-water fishes. Several studies have isolated other species from fish: A. veronii from catfish [139]; A. piscicola from salmonids [7,45]; A. sobria from tilapia [140]; A. schubertii from snakehead fish [141]; A. veronii, A. bestiarum, A. encheleia, and A. sobria from common carp; and A. allosaccharophila, A. dhakensis, A. caviae, A. veronii, A. hydrophila, A. jandaei, A. media, and A. trota from eel [29,39,142,143,144].
Aeromonas were isolated following outbreaks in rabbit farms as well as recovered from the feces of dogs, cats, and horses [145,146,147,148]. Several publications described Aeromonas as a pathogen of echinoderms, mollusks, and crocodiles and associated with copepods [34,44,149,150].
4.4. Aeromonas in Human Infections
Aeromonas are an emerging pathogen that cause a wide range of diseases in humans, commonly gastroenteritis, septicemia, and wound infections, and are able to infect both immunocompromised and immunocompetent patients [4,5,20].
The incidence of Aeromonas in human infections worldwide is unknown, but a study in California (1988) showed that the annual incidence of Aeromonas infections was 10.5 cases per million people [4,151]. Janda and Abbott [4] also reported that in 2004 in England, the estimated incidence of Aeromonas bacteremia was 1.5 cases per million people and in France in 2006 it was estimated that it was 0.66 cases per million [152]. Another study conducted in Taiwan between 2008 and 2010 showed that the incidence of bacteremia by Aeromonas was 76 cases per one million individuals [153]. Those studies therefore show that the incidence of diseases caused by Aeromonas vary by geographical location and can be related to bad hygiene habits in undeveloped regions [3,5,152,153,154,155,156,157,158].
A literature review describing A. dhakensis and the molecular methods used for its identification revealed that the reported prevalence of the most predominant clinical species of Aeromonas has changed over the years [3,5]. This species was described after the reclassification of A. aquariorum and A. hydrophila subsp. dhakensis. Until then A. caviae, A. veronii, and A. hydrophila were considered to be the most prevalent clinical species [3,4,5,159]. However, based on the molecular identification of 817 strains obtained from different studies around the world, 94.7% of the strains associated to clinical cases correspond to four species: A. caviae (30.5%), A. veronii (23.1%), A. dhakensis (23.0%), and A. hydrophila (18.1%) [5].
An update to the data, adding 1034 strains in more recent studies, shows that those four mentioned species represent 95.4% (1766/1852) of the Aeromonas strains linked to human infections. Table 1 shows this new evaluation with a relative abundance of the species varying slightly, with 37.26% of the strains being A. caviae, 23.49% A. veronii, 21.54% A. dhakensis, and 13.07% A. hydrophila. However, the frequency of these species also varies by country. In fact, so far A. dhakensis is the most prevalent species in tropical climates (Malaysia, Taiwan, and Australia), with clinical importance in those countries [5,68,160,161]. The current confusion between A. hydrophila and A. dhakensis may have consequences, since the latter species is more virulent and shows greater cytotoxic activity [68].
Table 1.
Distribution of Aeromonas spp. identified with molecular methods and recovered from different sites in association with human infections a.
| Species | Faeces | Wound | Blood | Respiratory Tract b | Urine | Peritoneal Dialysate | Bilis | Ascitic | Abscess | Other c Fluid | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| A. caviae | 446 | 43 | 147 | 11 | 12 | 11 | 11 | 2 | 3 | 4 | 690 (37.26) |
| A. veronii | 231 | 49 | 125 | 12 | 1 | 1 | 6 | 7 | 1 | 2 | 435 (23.49) |
| A. dhakensis d | 111 | 133 | 111 | 4 | 6 | 11 | 11 | 2 | 1 | 9 | 399 (21.54) |
| A. hydrophila | 69 | 96 | 45 | 9 | 5 | 8 | 3 | 1 | 2 | 4 | 242 (13.07) |
| A. media | 32 | 3 | 6 | 1 | 42 (2.27) | ||||||
| A. trota | 2 | 2 | 1 | 1 | 6 (0.27) | ||||||
| A. taiwanensis | 2 | 3 | 1 | 1 | 7 (0.32) | ||||||
| A. salmonicida | 1 | 2 | 1 | 4 (0.21) | |||||||
| A. jandaei | 3 | 2 | 1 | 1 | 1 | 8 (0.43) | |||||
| A. sanarellii | 1 | 4 | 5 (0.27) | ||||||||
| A. allosaccharophila | 2 | 1 | 3 (0.16) | ||||||||
| A. tecta | 2 | 2 (0.11) | |||||||||
| A. diversa | 2 | 2 (0.11) | |||||||||
| A. schubertii | 1 | 1 | 2 (0.11) | ||||||||
| A. bestiarum | 1 | 1 | 1 | 1 | 4 (0.21) | ||||||
| A. popoffii | 1 | 1 (0.05) | |||||||||
| A. intestinalise | 1 | 1 (0.05) | |||||||||
| A. enterica e | 1 | 1 (0.05) | |||||||||
| Total | 905 | 341 | 439 | 37 | 27 | 32 | 32 | 12 | 8 | 20 | 1852 |
a Adapted from Figueras and Beaz-Hidalgo [5] and Latif-Eugenín [15] that included data obtained from different studies [38,54,66,68,89,144,153,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174] and the results of 76 unpublished fecal isolates, with the addition of 865 new strains from several studies [15,175,176,177,178,179,180,181,182]. b 18 sputum strains; c Other includes: A. caviae (n = 4) of: vagina (3) and appendix (1); A. veronii (n = 2): sterile site (1) and ear fluid (1); A. dhakensis (n = 9): sterile site (6), joint fluid (1), eye (1), and bone (1); A. hydrophila (n = 4): ulcer exudate (1) and sterile site (3); A. trota (n = 1): cerebrospinal fluid (1); A. jandaei (n = 1): eye (1); d In many of the studies A. aquariorum was the name used for A. dhakensis; e Two new species of Aeromonas in the process of description.
Until now, only 16 species have been found in clinical samples [5], but two new species (A. enterica and A. intestinalis, in the process of description) isolated from human feces [31] are included in the list (Table 1). Nevertheless, the prevalence in clinical infections of the cryptic species A. rivipollensis [47], uncovered by A. media, is still not known [95].
One of the largest studies that has characterized clinical strains by molecular methods is the one performed by Latif-Eugenín [15] in her PhD thesis, who re-identified 422 isolates from Spanish hospitals using the sequences of the rpoD gene. The results showed that only 176 (41.6%) were originally correctly identified at species level. Of the 422 re-identified strains, 260 (61.6%) were identified as A. caviae, 91 (21.5%) as A. veronii, 27 (6.4%) as A. hydrophila, 19 (4.5%) as A. media, 5 (1.2%) as A. dhakensis, 2 (0.5%) as A. allosaccharophila, 2 (0.5%) as A. salmonicida, 1 (0.2%) as A. bestiarum, 2 (0.5%) as the new Aeromonas spp. mentioned above, and 13 (3.1%) did not belong to the genus Aeromonas at all. The results from that study differ from Figueras and Beaz-Hidalgo [5], and from the updated data shown in Table 1, which includes data from Latif-Eugenín [15]. In all cases, the most prevalent species was shown to be A. caviae (61.6% Spain vs. 37.26% in Table 1). A. dhakensis was less prevalent in Spain (1%) when compared with the the up-to-date reported data (21.54%). With all of the data taken together, 98% of the Aeromonas species identified in clinical cases belong to five species: A. caviae, A. dhakensis, A. veronii, A. hydrophila, and A. media (Table 1). Recently, Fernández-Bravo [20] demonstrated that human monocytes that showed the highest cell damage were coincidentally those that induced a higher expression of immune-related genes and were the most prevalent clinical species A. dhakensis, A. veronii, and A. caviae.
Aeromonas infections often involve more than one type of bacteria in the same clinical sample, which is defined as a polymicrobial or mixed infection [3,5,152,154,155,156,183]. Polymicrobial infections occur in 80% of cases of respiratory tract infections and cholangitis cases, and in 77% of cases of surgical site infections, followed by 60% of wound infections, and 30% of bacteremia [5,152,167,183]. The dominating bacteria in those mixed infections depends on the type of infection. In diarrhea cases, Aeromonas occur in combination with Campylobacter and Salmonella, while in wound infections, Staphylococcus aureus prevails [4]. Infections in which two Aeromonas strains were recovered from the same clinical sample, either two different strains of the same species or two different species, have occasionally been reported [183,184,185]; although, Mosser et al. [183] estimated a 5% incidence of dual or mixed infection. The latter authors suggested using Caenorhabditis elegans model of infection for the severity of the infections with more than one strain. Grim et al. [186] and Ponnusamy et al. [187] described complex and dynamic interactions of two strains of A. hydrophila that were isolated from an immunocompetent individual who developed necrotizing fasciitis. They suggested that the type six secretion system (T6SS) and exotoxin A (ExoA) were involved in this complex infection. Recently, using a mouse peritonitis and necrotizing fasciitis models, Fernández-Bravo et al. [188] used the mutants of T6SS and ExoA of these strains to elucidate the possible role in mixed infections and demonstrated that both virulence factors play a role after monomicrobial and polymicrobial infection.
4.5. Gastroenteritis
The first documented isolation of Aeromonas in feces dates from 1961, although Aeromonas was already isolated as a causative agent of myositis in a Jamaican woman in 1954 [189]. Several studies have associated Aeromonas with gastroenteritis [3,189,190,191,192,193,194,195]. Nausea, vomiting, fever, and abdominal cramps occur only in a fraction of patients, while colitis occurs in a third of diarrhea cases caused by Aeromonas [189]. The most frequent clinical presentation is secretory water, ranging from 75% to 89% of all cases in which this microorganism was the only associated pathogen [4,5]. Food and Drug Administration (FDA)-cleared multiplex molecular-based syndromic stool panels have replaced stool culture for bacterial pathogens in many laboratories. However, this commercial system does not detect Aeromonas [195].
Gastroenteritis caused by Aeromonas is a problem among the pediatric population, occuring mainly in children under three years with an incidence between 2.3% and 13% in countries like Taiwan and Nigeria, respectively [3,196]. However, studies by Bravo et al. [197] and Mansou et al. [194] showed a 7.5% and 1.4% incidence of Aeromonas children’s diarrhea, respectively, in Spain. Between 2–20% of gastroenteritis cases are monomicrobial and only 0–2% of children are asymptomatic carriers [198]; the diarrhea might last for one or two weeks and feces shows a liquid consistency [5,196].
The incidence in adults varies from 2% reported in Sweden, 6.9% in Hong Kong in healthy people, and 13% in immunocompromised patients [196]. Among patients in Spain with traveler’s diarrhea, Aeromonas was defined as a causative agent in 2% of cases [199], while in Japan it was isolated in 5.5% of cases, and 8.7% in Finland [196]. The infection was monomicrobial in 5.5% of the cases of traveler’s diarrhea [190,198,199].
Nowadays the enteropathogenic role of Aeromonas is clearly demonstrated in a study by Teunis and Figueras [192] using data derived from different human outbreaks [42,200,201,202,203]. It concluded that Aeromonas should be considered to be a human enteropathogen, much like Campylobacter and Salmonella. In addition, the same strain (genotype) that causes the diarrhea was isolated from water and food in several studies [82,119,120,204].
4.5.1. Wound Infections
Wounds are the second most frequent route of entry of Aeromonas to humans after the oral–fecal route [4,5,196]. Infections caused by Aeromonas can occur on any skin or mucous surface, although the extremities are the most common sites [4,205]. Most cases affect healthy people and are often associated with traumatic events and burns and scolds related to water and soil [4,5,159]. In a retrospective study of 129 cases of skin and soft tissue infections in Taiwan attributed to Aeromonas, 78% of patients had suffered previous trauma, and in 30% of cases there was exposure to water [206]. Additionally, Aeromonas was the most isolated microorganism following natural disasters such as the tsunami in Thailand in 2001 (Aeromonas accounted for 22.6% of all isolates) and Hurricane Katrina in the southeastern United States (2005), mainly associated with wound infection [207,208].
Among the Aeromonas nosocomial infections, the most common is those associated with surgical procedures, the so-called surgical site infections (SSI). Tena et al. [32,167] reviewed a series of nine cases that occurred in Spain (eight in Guadalajara and one in Zaragoza) between 1990 and 2007, together with 15 cases cited in the literature, confirming that the majority were associated with extraction of the appendix, gallbladder, and colon. In addition, the use of leech therapy lead to Aeromonas infections in 7–20% of the treatments [5,209,210]. This is due to the fact that Aeromonas are symbionts of the leeches, enabling them to digest the blood [5].
Wound infections due to Aeromonas can progress severely to necrotizing fasciitis (NF), usually in immunocompromised patients [5,211]. NF is commonly known as a flesh-eating disease that can cause hypotension, fever, necrosis, and gangrene and can be a life-threating infection [156,186,187,188,211]. A. hydrophila is the Aeromonas species most frequently associated in reported NF cases and in some cases, water was considered the source of infection [156,186,211,212,213,214]. Three studies report the complex interactions, among multiple strains of A. hydrophila that were isolated from an immunocompetent young girl who developed NF resulting in amputation of almost all the extremities [186,187,188]. The NF case involved the exposure of an open wound to river water into which the girl had fallen, and was originally considered to be a monomicrobial infection [186]. However, it was later recognized that of the four strains recovered from the wound, only two were different strains of A. hydrophila (same species) and the strains were named NF1 and NF2 [186]. Additionally, after mixed and single infections, these studies showed that exoA gene and T6SS play a role in NF developed after monomicrobial and polymicrobial infection [186,187,188].
4.5.2. Bacteremia/Septicemia
Several cases of bacteremia/septicemia due to Aeromonas are published [152,215,216,217,218]. The incidence of bacteremia can range from 0.12–3.3% and the mortality rate associated with Aeromonas bacteremia is about 30% [4,5]; although previous studies showed incidences of 25% [219,220]. Based on the data collected by Figueras [196] and Janda and Abbott [4], bacteremia associated with Aeromonas is preferably monomicrobial, acquired in the community, and mainly affecting males. Additionally, several studies demonstrated that the most prevalent species associated with blood infections were A. caviae, A. veronii, A. dhakensis, and A. hydrophila [5]. The underlying diseases found in cases of bacteremia/septicemia were most commonly malignancy, hepatobiliary disease, and diabetes [5,15,221]. Moreover, the most common symptoms associated with Aeromonas bacteremia according to Janda and Abbott [4] included fever (74–89%), jaundice (57%), abdominal pain (16–45%), septic shock (40–45%), and dyspnea (12–24%). That same study also classified the bacteremia in four groups based on the affected populations, the main one being immunocompromised individuals (>80%), followed by those who suffered a traumatic accident, then the cases that affect healthy people, and finally those that involve patients undergoing reconstructive surgery and/or leech therapy [4].
4.5.3. Other Infections
Other infections with less incidence associated with Aeromonas have been reported: (i) respiratory tract infections; (ii) urinary tract infections, and (iii) spontaneous bacterial peritonitis (SBP) [4,5,196]. Although Aeromonas pneumonia is rare, some cases have been described [5,206,222,223]. Treatment with carbapenems is effective, although some cases of pneumonia have been fatal [223]. Aeromonas were also described as a causal agent in urinary tract infections [5,224,225]. The majority of the cases were reported in patients with various underlying diseases, such as spina bifida, bilateral renal dilatation, and diabetes mellitus. Lastly, SBP occurs in 16% of patients with cirrhosis [226].
5. Virulence Factors
Aeromonas infections present a wide variety of clinical manifestations and are considered multifactorial [18,19]. Various virulence factors enable Aeromonas to overcome the host immune response and can cause infections [5,18].
5.1. Structural Components
The adhesion of bacteria to host tissues is a critical step in the initial phase of infections by many microorganisms. Bacteria adhere to host tissues and cells and alter their defense mechanisms thereby initiating colonization. The most studied structural components in Aeromonas involved in the colonization process are the flagella, pili, capsule, S layer, and lipopolysaccharides (LPS) [18,19].
Flagella are organelles responsible for bacterial mobility composed of a filament, hook, and basal body. The genus Aeromonas has a polar and lateral flagellum [18,19]. The presence of lateral flagella gives the bacteria a fast or “swarming” type of mobility that allows them to move on solid surfaces and form biofilms. The polar scourge allows mobility by “swimming” in liquid environments [18,19,227].
Pili are filamentous structures found on the surface of bacteria, with subunits known as pilin. In addition to being an adhesion organelle, this structure is also involved in other functions, such as DNA transfer, biofilm formation, cell aggregation, and invasion of host cells [19].
The LPS have three subunits: the polysaccharide O (O antigen), the core of the LPS (central polysaccharide), and lipid A, which anchors them to the outer membrane of the bacteria [19,228,229]. These play an important role in the organization and maintenance of the outer membrane and are responsible for the virulence and producing a non-specific inflammatory response [17,19]. The toll-like receptors (TLRs), TLR4 in particular, are the best known membrane protein that recognizes LPS, which induces the activation of the immune response essential for an antibacterial defense [18,21].
Capsule is a polysaccharide structure that covers the outer membrane of bacteria involved that interacts with the environment. The capsule is described as an important virulence factor that is resistant to phagocytosis and the complement system [18,19,230].
The S layer is a surface protein layer of paracrystalline that is produced by a wide range of bacteria to form the outermost cell envelope [18,19]. In addition, this layeris associated with several functions related to pathogenicity.
5.2. Extracellular Proteins
The interaction between pathogenic bacteria like Aeromonas and host cells is produced as indicated by their extracellular components and toxins that are secreted into the extracellular space, such as proteases, lipases, enterotoxins, hemolysins, and Shiga toxins, among others [4,18,19,168,198,231,232,233,234].
Cytotonic and cytotoxic enterotoxins have been described in Aeromonas [18,19]. There are two groups of cytotonic enterotoxins: thermolabile (Alt) (56 °C for 10 min), which does not react with the cholera antitoxin, and thermostable (Ast) (100 °C for 30 min), which does react with the cholera antitoxin [198]. The cytotoxic enterotoxin (act) inhibits the phagocytic activity of host cells, produces hemolysis, and increases the levels of tumor necrosis factor α (TNF-α) and interleukin (IL-1β) in the RAW 264.7 murine macrophage cell line [235].
Two types of hemolysins are defined in Aeromonas, α and β, with physiological and functional differences [236] but which are capable of forming pores in the membrane of the target cell generating their osmotic lysis [231]. Aerolysin is the prototype hemolysin of the genus, encoded by the aerA gene [19]. It was characterized in 1974 by Bernheimer and Avigad [237]. Aerolysin is secreted by the type two secretion system (T2SS), which is sec-dependent, transcribed as a pre-pro-aerolysin that undergoes various processes of maturation during its secretion to become an active 47.5 kDa aerolysin in the extracellular environment [15].
Proteases allow Aeromonas to persist in several habitats and facilitates interactions with other microorganisms. In general, proteases contribute to pathogenicity as they promote invasion by direct damage to host tissue or by proteolytic activation of toxins [18,19]. Additionally, they can also contribute to the establishment of an infection that exceeds the host initial defenses, inactivating the complement system or providing nutrients for cell proliferation [19]. Aeromonas produces at least three types of proteases: metalloprotease (ahp, aphB), acetylcholinesterase, and serine protease (aspA) [84,88].
Aeromonas, like many other pathogenic bacteria, secrete lipases to the medium that acts as hydrolases on membrane lipids [18,19]. These can provide nutrients or constitute virulence factors when interacting with human leukocytes or by affecting various functions of the immune system [18]. An important lipase in the genus Aeromonas is glycerolphospholipid: cholesterol acyltransferases (GCAT), which have the ability to digest the membranes of erythrocytes and produce their lysis [19]. In addition, gcat gene can be used for identification at genus level [60,112].
According with the literature, A. hydrophila expresses various degradative enzymes that can contribute to its virulence, among which are collagenase, elastase, and enolase. Collagenase was shown to have cytotoxicity in Vero cells [238]. Enolase, a glycolytic enzyme secreted and expressed on the surface, was identified as a virulence factor in A. dhakensis SSU, which was observed to have functions in the degradation of blood plasma proteins [239].
The function of the Shiga toxin is the inactivation of ribosomes (arrest of protein synthesis) of vascular endothelial cells, leading to cell death [19,168]. They are also encoded in bacteriophages that are normally integrated in the bacterial chromosome. When the lytic cycle is induced, large numbers of them capable of infecting other bacteria are released, acting as horizontal transmission vectors of the stx genes [240]. Recently, Shiga toxins have only been detected in strains of Aeromonas recovered from food [234].
5.3. Secretion Systems
Nowadays, six secretion systems have been described in Gram-negative bacteria, all of which are involved in the transport of virulence factors to the extracellular medium or directly into the host cell. The T2SS and type five secretion system (T5SS) are Sec or Tat dependent, which means that virulence factors secreted by these mechanisms contain signal peptides that are recognized by Sec and Tat proteins allowing their translocation, while type one secretion system (T1SS), T3SS, type four secretion system (T4SS) and T6SS are Sec independent, so they transport their proteins directly to the cell surface or host cell [241].
The T2SS is an exclusive secretion system of proteobacteria that shows a common evolutionary origin with type IV pili [19,241,242]. This secretion system is essential in the pathogenesis of various microorganisms such as Vibrio cholerae, Legionella pneumophila, Escherichia coli [242], A. hydrophila [84], and A. salmonicida [88].
The T3SS or injectosome is one of the secretion systems by which proteins can be injected directly from the bacterial cell protoplasm to the cytoplasm of the target cell or to the extracellular space [18,19,241]. In Aeromonas, T3SS genes have been extensively studied: AexT (ADP-ribolisant toxin), AopU, which inhibits the nuclear Kappa B factor involved in the activation of IkB (protein kinase), AopH (tyrosine phosphatase), AopO (serine/threonine kinase), and AexU (similar to AexT toxin) [17,19,243,244,245,246,247,248,249,250]. Studies of infections by A. salmonicida and A. hydrophila strains mutated for T3SS have shown that that they have a lower virulence than the non-mutated strains [17,247,248,249,251]. Recently, 21 Aeromonas T3SS likely effector families were described using bioinformatics tools with the experimental analysis, which will be useful in future research to identify bacterial effector proteins in other genera [252].
The T4SS is the only secretion system capable of transporting DNA as well as proteins, which gives the bacterial conjugation system a homologous role [241]. This secretion system plays a crucial role in the propagation of resistance genes and virulence [18,19].
The T6SS or Vas (virulence-associated secretion) was the last secretion system to be recognized in 2006 [253]. Like the T3SS and T4SS it is able to inject protein effectors directly into the cytosol of the target cell, although this secretion system has been identified in non-pathogenic organisms or symbionts [253]. It appears to be highly conserved and can be found in one or more copies in diverse Gram-negative species, such as Vibrio cholerae, Pseudomonas aeruginosa, Yersinia pestis, E. coli, and Salmonella enterica, among others [18,19,84]. Among the secreted effector proteins, the best known are G repeat proteins (VgrG) and hemolysin-co-regulated protein (Hcp). In Aeromonas, it was first detected in 2006, following the sequencing of the complete genome of A. hydrophila [19,84], although its functionality was unknown. Suárez et al. [254] demonstrated the functional role in virulence of this secretion system in A. hydrophila. In recent years, T6SS has been reported to have an additional “antibacterial” role in polymicrobial infections, eliminating competitor bacteria [255]. In fact, Carruthers et al. [256] suggested that T6SS of Acinetobacter baumanii plays a role in the competence with other bacteria. In the same way, a different study demonstrated that the T6SS of Shigella sonnei confers an advantage to this species when it competes with Shigella flexneri and E. coli and this advantage is reduced in T6SS defective mutants [257]. Recently, the T6SS was associated with a role in the mixed infections by two A. hydrophila strains (NF1-NF2) recovered from a case of necrotizing fasciitis [187,188]. The data suggested that the expression of the effectors related to T6SS might be differentially regulated in both strains, causing a different progression of the disease following mixed infections from progression following a single infection [187,188].
5.4. Quorum Sensing
Quorum sensing (QS) it is a mechanism for regulating genetic expression in response to cell population density [19]. The cells involved produce and excrete substances, called autoinductors, which serve as a chemical signal to induce collective genetic expression. [258]. The “signal” molecule in Gram-negative bacteria is N-acyl homoserine-lactone (AHL) and in Aeromonas, the AHL is able to modulate the host immune response [19,186,259]. Several studies have shown the importance of AHLs in regulating a range of biological functions such as biofilm formation, antibiotic production, and warming motility and the different QS systems harbor differences in their influences [260,261,262,263,264,265,266]. Chan et al. [260] found in the whole genome of the strain A. veronii 159 sequences of QS-related genes, providing a model for exploring it roles in virulence and as a potential target for Aeromonas treatment. Talagrand-Reboul et al. [266] focused their review on the knowledge of the biofilm and QS in Aeromonas, explaining that biofilm provides a high cell-density that allows interaction between bacteria with the QS systems in Aeromonas. That study also reported the possible role of this biofilm formation in mixed infections and should be further studied. Recently, Liu et al. [264] showed that the infection with the asal-mutant (failed to produce the short chain AHLs signal) in a marine fish isolated of A. salmonicida affected the biofilm formation. Blöcher et al. [261]. demonstrated the development of anti-QS compounds to overcome the resistant bacteria strain A. caviae Sch3, inhibiting biofilm formation. That pilot study contributed to finding new therapies to overcome the bacterial antibiotic resistance problem. Ding et al. [262,263] demonstrated the impact of curcumin liposomes against A. sobria and A. hydrophila in biofilm formation, due to the anti-QS properties of this dietary supplement. This information might be useful to design QS inhibitors. The same occurs with tannic acid, a potent quorum quencher that regulates the biofilm formation of A. hydrophila [265].
5.5. Metal Ions
Metal ions are essential for the correct functioning of microorganisms biological process, “metallostasis” [267]. They also play an important role in the host–pathogen interaction [268]. In the course of an infection, the host restricts the accessibility of crucial metals, by inactivating the metal-dependent processes of the bacterial pathogen that compensates this limitation by generating different proteins [268,269,270].
The mechanisms for iron acquisition are known to play an important role in the development of the infection [19]. Two mechanisms are described so far: siderophore-dependent and siderophore-independent. Siderophores are peptides that present a functional group with an affinity to iron ions that need specific cell membrane-bound receptors and a cell-associated apparatus to incorporate the metal into the bacterial metabolism. The siderophore-independent mechanism consists of a bacterial outer membrane protein that binds host-specific iron. In addition, the gene expression related to the iron acquisition is regulated by protein Fur [18,19].
Other metal cofactors with a role in the pathogenicity of Aeromonas are also described, for example, copper and silver resistance genes coding for different proteins [271,272]. Recently, Fernández-Bravo et al. [273] demonstrated that the nickel-binding protein HypA in Aeromonas might play a role in acid tolerance and in the defense against macrophages.
6. Host–Pathogen Interaction
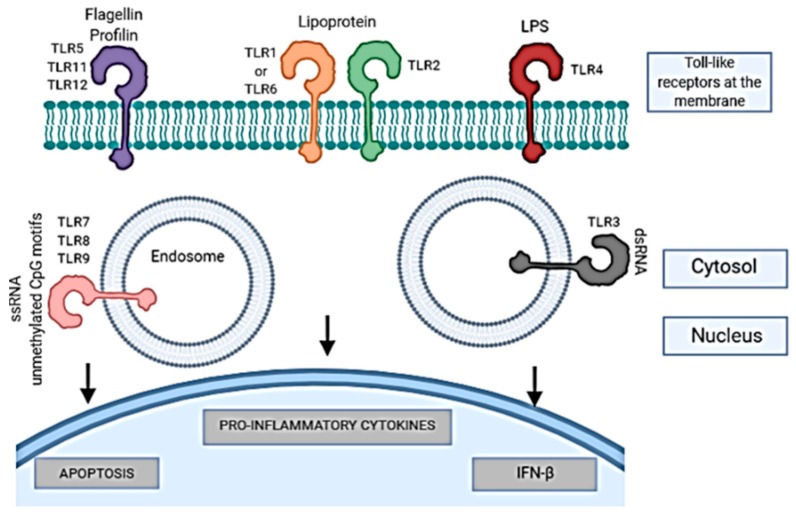
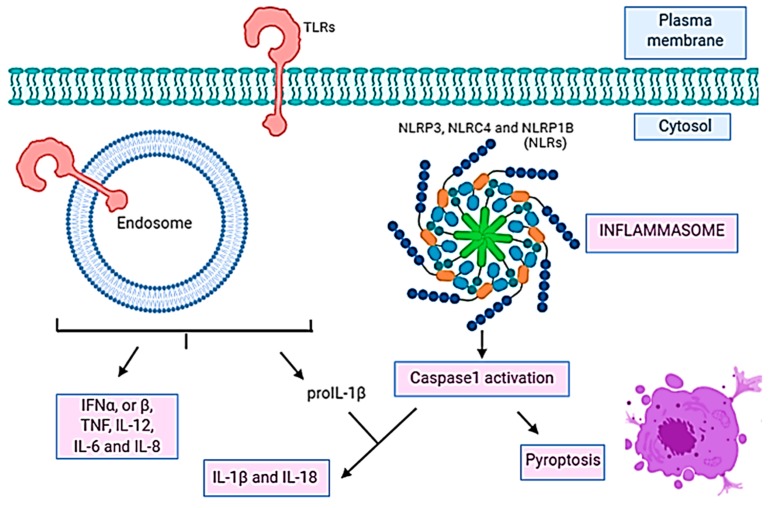
The host–pathogen interaction activates an immune response as a result of antigen exposure. Two types have been described: innate and adaptative [274]. The innate immune response is activated after recognition of structures associated with microbes named pathogen-associated molecular patterns (PAMPs) by receptors named pattern recognition receptors (PRRs) present and expressed in a variety of cells, like neutrophils, monocytes or macrophages [275,276,277]. The PRRs include TLR members, nucleotide binding, oligomerization domain-containing receptors (NOD-like receptors (NLRs)), retinoic acid-inducible gene (RIG) I-like RNA helicases, C-type lectins, and AIM2-like receptors (ALRs). The TLRs are membrane PRRs that induce the phagocytosis of the pathogen and activate the expression of cytokines in the host, initiating the inflammatory response [278]. It was also demonstrated that the TLRs recognition results in the induction of apoptosis [279] (Figure 2). NLRs are cytosolic PRRs, which activate a different type of cell death than apoptosis (programmed cell death) which is caspase-1 dependent and named pyroptosis [280,281] (Figure 3).
Figure 2.
Toll-like receptors (TLRs) pathways that induce the inflammatory response mediated by cytokines (adapted from [278]). Created with Biorender.
Figure 3.
Pyroptosis pathway with Toll-like receptors (TLRs) and Nod-like receptors (NLRs) acting in concert (adapted from [275]). Created with Biorender.
The expression of several TLR genes (TLR1, TLR2, TLR3, etc.) following Aeromonas infection has been described in the last years, as shown in Table 2. Two recent studies analyzed the expression of different TLRs following an A. hydrophila infection using a fish model [282,283]. The data obtained in these studies demonstrated that the immune response presented tissue-specific patterns. However, the higher expression of TLRs indicated that they play an important role in the innate response against A. hydrophila [282,283]. TLR4 is a transmembrane receptor of monocytes, macrophages, and dendritic cells that senses molecules such as LPS present in the cell walls of Gram-negative bacteria [284,285]. Previous studies investigated the TLR4 signaling pathway after A. hydrophila infection by using a fish model, indicating the importance of this receptor in increasing the innate immunity response to bacteria invasion. Data from two studies showed that the expression of TLR4 might be induced following an A. hydrophila infection in a minnow Gobiocypris rarus and the blunt snout bream Megalobrama amblycephala [21,286]. Similarly, an interesting study was conducted by Srivastava et al. [24] using zebrafish as a model.
Table 2.
Studies (2009–2019) that evaluate proteins and processes involved in the immune response of the animal models or cell line host after Aeromonas spp. (adapted from [20]).
| Proteins or Process Studied | Host | Aeromonas sp. | Reference |
|---|---|---|---|
| Toll-like receptors (TLRs) (TLR1, TLR2, TLR3, TLR4, TLR5, TLR7, TLR8, TLR9, TLR18, TLR19, TLR20, TLR22) | Fish, cells (EPC, HKLs, Hep-2) |
A. hydrophila, A. salmonicida, A. veronii |
[21,24,282,283,286,287,288,289,290,291,292] |
|
Cytokines (TNF-α, TNF- β, IFN-γ, IL-6, IL-8, IL-10) |
Fish, mice, cells (Hep-2, HKLs, RAW 264.7, HeLa) |
A. hydrophila, A. salmonicida, A. dhakensis, A. veronii/A. hydrophila |
[259,289,290,293,294,295,296] |
| Chemokines (CC-Chem14, CsCC-Chem20, CsCC-Chem25, CCL3, CCL5) | Fish, mice, cells (HeLa, RAW 264.7) | A. hydrophila, A. dhakensis | [259,295,297,298] |
| Transcription factors (JUN, RELA) | Fish, cells (Caco-2) |
A. hydrophila, A. salmonicida, A. veronii, A. bestiarum, A. allosaccharophila |
[299,300] |
| Apoptosis (TP53, CASP3) | Fish, mice, cells (HeLa, RAW 264.7, macrophages from fish, SLs, HKLs) |
A. hydrophila, A. veronii |
[295,301,302,303,304,305] |
|
Pyroptosis (NLRP3, NLRC4, IL-1β) |
Mice, macrophages from mice |
A. hydrophila, A. veronii |
[22,23] |
Epithelioma papulosum cyprini cell line (EPC); head kidney leukocytes (HKLs), human epithelial cell line (Hep-2); murine macrophage cell line (RAW 264.7); human epithelial type cell line (HeLa); human epithelial colorectal adenocarcinoma cell line (Caco-2); spleen leukocytes (SLs). The strains of these studies [282,283,286,292,293,294,296,297,302] were identified by non-molecular methods or lack information about the identification.
Gene expression of immune response mediators such as cytokines, tumor necrosis factor alpha and beta (TNF-α, TNF-β), interferon gamma (IFN-γ), interleukin 6, 8, and 10 (IL-6, IL-8, IL-10) among others, as well as chemokines, such as C-C ligand 3 (CCL3) induced by TLR signaling have been studied, as summarized in Table 2 [290,294,296,306]. Studies in which A. salmonicida was used to infect rainbow trout showed an upregulation of TNF-α among other cytokine genes, involved in systemic inflammation [290,306]. However, differences in expression were observed based on the tissue studied, such as the intestine or kidney [290,306]. A recent study by Kong et al. [294] established that A. hydrophila might induce an overexpression of the pro-inflammatory cytokine gene TNF-α in the intestine of fish, deteriorating the integrity of the mucosal barrier structure. Similarly, the expression of different chemokines, which are a family of small cytokines with an important role in the immune response, has been studied after A. hydrophila infection in eel and grass carp [297,298].
There are various studies on the expression of cytokines and chemokines after A. hydrophila infection using mice and several cell lines, such as murine macrophage from blood (RAW 264.7), human colon cancer cell line (HT-29), and a cancerous cell line (HeLa) (Table 2). Those studies, demonstrated, for instance, an alteration in the production of cytokines and chemokines after infection. In another study, the possible protective role of QS was evaluated using mice treated with AHL before infection by A. hydrophila [259]. Results showed a reduced level of cytokines and chemokines as well as of the bacterial load in the organs. This work suggested that the AHL pre-treatment modulated the innate immune response in mice and increased the survival of the mice following an A. hydrophila infection [259].
Table 2 shows that several studies reported that apoptosis can be induced in vitro following an Aeromonas infection, mainly with A. hydrophila, using different cell lines, such as RAW 264.7, HeLa, HT-29 or mouse BALB/C monocyte macrophage (J744). Other studies have also demonstrated the capacity of A. hydrophila and A. veronii to cause apoptosis in kidney leukocytes or head kidney macrophages obtained from fish. In relation to proteins associated with apoptosis, TP53 is a suppressor tumor protein with an important role in the programmed cell death, whose expression was studied in zebrafish after A. hydrophila infection [302]. The induction of apoptosis was also studied by evaluating the caspase 3 protein (CASP3) activation in HeLa cells [295]. The results from the study demonstrated that the AexU gene in A. hydrophila induced the apoptosis via CASP3 [295].
The inflammasome consists of a complex of caspase-1, PYCARD domain (ASC), AIM-2, and the NLR receptor. NLR subset inflammasomes, such as NLR pyrin domain containing 3 (NLRP3), NLR card domain containing 4 (NLRC4) or NLR pyrin domain containing 1 (NLRP1), promote the maturation and secretion of the pro-inflammatory cytokines, interleukin 1 beta (IL-1β) and IL-18, resulting in pyroptosis. Following an A. hydrophila infection, the activation of caspase-1, and the release of interleukin 1 beta (IL-1β), followed by the cell death called pyroptosis have been studied using macrophages as a model [23]. The results suggested that A. hydrophila induces an inflammatory response via NLRP3 inflammasome, which comprises the NLR protein (NLRP3), the adapter ASC, and caspase-1 [23]. Another study by the same Japanese group demonstrated that inflammasomes-mediated caspase-1 activation (NLRP3 and NLRC4) is involved in host defenses against systemic A. veronii infection in mice and macrophages [22,290,306] (Table 2).
The nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) is a protein complex that plays a role in the regulation of the immune response, controlling the pro-inflammatory cytokines after the stimulation of the TLRs. RelA is a protein involved in NF-κB formation and studies using fish as a model established that the overexpression of the RelA following A. hydrophila infections induced the production of several pro-inflammatory cytokines (Table 2). c-Jun is an immune modulation protein that along with c-Fos, forms the AP-1 that is also an activator of pro-inflammatory genes such as TNF-α, IL-8, and IL-6, among others. However, it has been reported that when the c-Fos acts alone, this protein induces an increase in anti-inflammatory genes such as IL-10 or IL-4, among others [307]. These genes have been studied after an infection of human epithelial colorectal adenocarcinoma (Caco-2) cells with Aeromonas observing a possible role of these transcription factors in virulence [299] (Table 2).
7. Pathogenicity Studies
7.1. In Vitro Studies
Many studies of pathogenesis and virulence in Aeromonas have been carried out in recent years using in vitro cell lines (Table 3). The ability of Aeromonas to adhere, invade, and produce cytotoxicity has been defined, mainly following A. hydrophila and A. caviae infections, using human larynx carcinoma (HEp-2) and human Caucasian colon adenocarcinoma (Caco-2) cells [289,308,309,310]. Ghatak et al. [309] analyzed the cytotoxicity of 55 strains of Aeromonas using four cell lines, African green monkey kidney (Vero), Madin Darby bovine kidney (MDBK), baby hamster kidney (BHK-21), and lymphoblast B mono lymphoblast (B95a) cells. The data obtained from that study suggested that the Vero cell line is the best model for examining and testing the cytotoxicity of Aeromonas species [309]. In 2012, Krzyminska et al. [310] demonstrated that the presence of T3SS in the Aeromonas strain tested was able to mediate cell-contact cytotoxicity, destruction of host epithelial cells, and tissue damage in different cell lines: Chinese hamster ovary (CHO), HEp-2, and Vero.
Table 3.
Studies (2009–2019) that investigate the virulence and pathogenicity of Aeromonas spp. using different cell lines (adapted from [20]).
| Cell Line | Study | Aeromonas | Reference |
|---|---|---|---|
| HEp-2, Vero | Adhesion and cytotoxicity |
A. hydrophila. A. salmonicida, A. veronii, A. bestiarum, A. schuberti, A. eucrenophila, A. encheleia, A. jandaei, A. sobria, A. caviae, A. trota, A. media |
[311] |
| HEp-2, CHO | Cell-contact cytotoxicity | A. hydrophila, A. caviae, A. veronii | [310] a |
| C2C12 | Cytotoxicity | A. hydrophila, A. dhakensis | [68] |
| HEp-2 | Adhesion, biofilm formation, and immune stimulation | A. hydrophila | [289] |
|
HEp-2, Caco-2,
T-84 |
Adhesion, invasion, and cytotoxicity | A. hydrophila, A. caviae | [308] a |
| RAW 264.7 | Role of mixed infections in Necrotizing fasciitis | A. hydrophila | [187] |
| Caco-2 | Adhesion and cytopathic effect |
A. hydrophila, A. dhakensis, A. bestiarum, A. piscicola, A. salmonicida |
[312] |
| HepG2, WLR-68 | Cytotoxicity effect of metalloprotease | A. hydrophila | [313] a |
| Caco-2 | Adhesion, invasion, and cytotoxicity | A. salmonicida | [314] |
| J744.1 | Role of metallochaperone HypA | A. hydrophila | [273] |
| RAW 264.7 | Role of mixed infections in Necrotizing fasciitis | A. hydrophila | [188] |
Human epithelial cell line (HEp-2), kidney epithelial cells from African green monkey (Vero), Chinese hamster ovary cell line (CHO), mouse myoblast cell line (C2C12), human epithelial colorectal adenocarcinoma cell line (Caco-2), human colorectal adenocarcinoma cell line (T-84), murine macrophages cell line (RAW 264.7), hepatic cell line (WLR-68). a The strains were identified by non-molecular methods (RFLP, phenotypic characteristics, virulence factors).
Moreover, Merino et al. [289] demonstrated by the generation of mutants that the flagella glycosylation in A. hydrophila plays an extremely important role in the adhesion to Hep-2 cells and in biofilm formation. In a recent study, Dos Santos et al. [308] evaluated the capacity of Aeromonas species to adhere, invade, survive, and produce cytotoxicity through the use of three different cell lines: HEp-2, Caco-2, and human colorectal adenocarcinoma (T-84). The results suggested that cytotoxicity and adhesion would depend on the type of cell line analyzed, indicating that the majority of Aeromonas strains survived in the T-84 cells.
Regarding to polymicrobial infections, Ponnusamy et al. [187] studied the mixed infections by two strains of A. hydrophila (NF1-NF2) using the murine macrophages cell line RAW 264.7. The data obtained suggested that there was a different course of the disease after mixed infection compared to the single infection.
7.2. Animal Models
Which experimental animal model to use is one of the most important questions in the study of virulence [17]. Recreating Aeromonas infections in different animal models has been the feature of some studies, and Table 4 describes the animal models used and the latest relevant studies.
Table 4.
Relevant studies (2000–2001) of virulence and pathogenicity after Aeromonas infection using different animal models (adapted from [20]).
| Model | Study | Aeromonas | Reference |
|---|---|---|---|
|
Mice (Mus musculus) |
Virulence factors, role of mixed infections in necrotizing fasciitis |
A. hydrophila, A. dhakensis, A. caviae, A. veronii, A. salmonicida |
[16,17,186,187,188,315] |
|
Catfish (Clarias gariepinus, Ictalurus punctatus, Hypophthalmichthys molitrix) |
Enterotoxic effects, virulence mechanism, transcriptome, aerolysin activity | A. hydrophila, A. veronii | [316,317,318,319] |
|
Blue gourami (Trichogaster trichopterus) |
Septicemia, immune responses | A. hydrophila | [320,321] |
|
Zebrafish (Danio rerio) |
Immune response, role of mixed infections in the virulence | A. hydrophila/A. veronii coinfection, A. hydrophila | [17,24,293] |
|
Slime mold (Trichogaster tricopterus) |
Pathogenicity | A. salmonicida, A. hydrophila | [322] |
|
Nematode (Caenorhabditis elegans) |
Virulence, immune response, necrosis |
A. hydrophila, A. dhakensis, A. veronii, A, caviae |
[183,323,324] |
In many studies, mice are considered a good model for studying pathogenicity in Aeromonas, because mice are susceptible to a similar range of microbial infections as humans [17,325]. In three recent studies by Grim et al. [186], Ponnusamy et al. [187], and Fernández-Bravo et al. [188] regarding the progression of NF, the role of the two strains of A. hydrophila involved in a mixed infection was studied using mice as the model of infection. In addition, strains were marked with a bioluminescent gene to elucidate dissemination into the peripheral organs. Another interesting study with mice was carried out by Chen et al. [315], who compared the pathogenic capacity of A. hydrophila, A. dhakensis, A. caviae, and A. veronii by the analysis of survival rates using BALB/c mice. Results suggested a variation among the most clinically prevalent species, with A. dhakensis being more virulent than A. hydrophila.
In 2016, Romero et al. [17] suggested that zebrafish larvae could be used as the host model to assess the virulence of A. hydrophila, which would enable us to stop using mice. Zebrafish were used in another study as a model of Aeromonas species co-infection [293], and showed a higher mortality rate under co-infection in relation to the single infection. Additionally, zebrafish were used to study the immune response against Aeromonas [24].
Recently, the catfish was used as a fish model to clarify the pathogenic mechanisms in A. hydrophila [317], the blocking of aerolysin activity after A. hydrophila infections [316], and the enterotoxic effects after A. hydrophila infection [318], among others.
Chen et al. [324] evaluated the nematode of C. elegans as an animal model for studying Aeromonas infections, suggesting that A. dhakensis was the most virulent species in comparison with the other most prevalent clinical species. In 2016, Chen et al. [323] also used C. elegans as a disease model for muscle necrosis following an A. dhakensis infection. In relation with the mixed infections, Mosser et al. [183] also used the C. elegans model and demonstrated that the virulence of one Aeromonas strain could be higher in the presence of another strain, so the combination of both strains caused a higher mortality rate of the nematodes than a single infection.
Other interesting animal models of infection have also been proposed, but less often studied in Aeromonas: (i) blue gourami was used to study the role of an endogenous serum lectin in the immune protection against A. hydrophila infections [320], as well as for the identification of putative virulence factors in A. hydrophila strains [321]; (ii) Dictyostelium amoebae as an alternative host model for evaluating the virulence of Aeromonas [322].
8. Antimicrobial Resistance
Resistance to antimicrobial agents is a genetic–evolutionary response mediated by the presence of genes, some of which are found in plasmids, integrons or in the genome of the bacteria. Except for a few strains and the species A. trota, Aeromonas are described as resistant to ampicillin [1,4,42]. These bacteria are also resistant to other penicillins and first-generation cephalosporins [4,199,326]. However, Aeromonas are susceptible to monobactams, carbapenems, third- and fourth-generation cephalosporins, aminoglycosides, and fluoroquinolones [327].
Ndi and Barton [328] reported an increase in resistance to beta-lactam antimicrobials (penicillins and derivatives, cephalosporines, carbapenems, and monobactams) by the presence of genes that code for the production of beta-lactamases [4]. Three mainly β-lactamases were described in Aeromonas: class B metallo-β-lactamase, class C cephalosporinase, and class D penicillinase [329]. Fosse et al. [330] characterized the β-lactamases associated with the different Aeromonas species in five groups (i–v): (i) A. hydrophila complex strains expressing class B, C, and D β-lactamases; (ii) A. caviae strains expressing class C and D β-lactamases; (iii) A. veronii strains containing class B and D lactamases; (iv) A. schubertii strains harboring class D lactamases; and (v) A. trota strains with class C β-lactamases. It also appears that many A. veronii bv. sobria isolates also produce a class C cephalosporinase [4]. In fact, Sanchez-Cespedes et al. [331] reported a case in which the patient developed cholangitis and imipenem resistance in an A. veronii biovar sobria infection, probably as result of prior antibiotic treatment.
Recently, the studies of antimicrobial profiles in Aeromonas has increased, due to the necessity of responsible use of antibiotics [181,182,332,333,334,335,336,337]. Wimalasena et al. [337] suggested that in relation to animals, pet turtles could be a health risk to humans, due to the antimicrobial resistant Aeromonas strains found in these animals. Dias et al. [332], also reported that wild animals are considered a potential public health risk because they are potential reservoirs of resistant strains of Aeromonas. Previous studies comparing clinical isolates demonstrated that the resistance genes were species- and isolation site-dependent. The resistant strains were mostly detected from peritoneal fluids [181]. In addition, Zhou et al. [182] demonstrated that clinical strains isolated from extra-intestinal infections were resistant to several antibiotics, however, third-generation cephalosphorins, fluoroquinolones, and aminoglycosides could be an option to treat these infections.
Data from other studies agree that resistance could be related to mobile genetic elements such as plasmids, insertion elements, pathogenicity islands or cassettes associated with integrons [338,339,340]. Vega-Sánchez et al. [341] showed the incidence of class 1 integron and β-lactamases genes in Aeromonas isolates from rainbow trout. In 2017, Pitowska et al. [342] studied the variety of beta-lactamases genes present in Aeromonas spp. isolated from wastewater, finding a high number of genes encoded by plasmids. They suggest that Aeromonas antibiotic resistance strains could disseminate from wastewater to other environments. Recently, Hossain et al. [334] observed a higher incidence of different antimicrobial resistance genes and class 1 integron gene cassettes in resistant Aeromonas isolates. That study was conducted to prevent the consequences of inappropriate antimicrobial use.
9. Conclusions
Many questions were addressed in this review. However, Aeromonas is an important microorganism of the aquatic system, widely distributed in the environment, and one that colonizes and can infect humans and animals. Aeromonas infections will remain a health problem in the near future, considering the increased life expectancy of humans which will result in more elderly persons with potential underlying diseases, who are more susceptible.
Although we have extensive knowledge about the genus, different questions are arising pertaining to such things as potential new species, unusual resistance mechanisms, and mixed infections with different course of diseases. Based on this, it is important to continue the studies in order to provide more precise answers to these questions.
Author Contributions
A.F.-B. and M.J.F. searched for the information and wrote the review. All authors have read and agreed to the published version of the manuscript.
Funding
The projects JPIW2013-095-C03-03 of MINECO (Spain) and AQUAVALENS of the Seventh Framework Program (FP7/2007–2013) grant agreement 311846 from the European Union supported the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Martin-Carnahan A., Joseph S.W. Order XII. Aeromonadales ord. nov. In: Brenner D.J., Krieg N.R., Staley J.T., Garrity G.M., editors. Bergey’s Manual of Systematic Bacteriology. Williams & Wilkins; Philadelphia, PA, USA: 2005. pp. 556–578. [Google Scholar]
- 2.Martínez-Murcia A., Beaz-Hidalgo R., Navarro A., Carvalho M.J., Aravena-Román M., Correia A., Figueras M.J., Saavedra M.J. Aeromonas lusitana sp. nov., isolated from untreated water and vegetables. Curr. Microbiol. 2016;72:795–803. doi: 10.1007/s00284-016-0997-9. [DOI] [PubMed] [Google Scholar]
- 3.Figueras M.J., Suarez-Franquet A., Chacon M.R., Soler L., Navarro M., Alejandre C., Grasa B., Martínez-Murcia A.J., Guarro J. First record of the rare species Aeromonas culicicola from a drinking water supply. Appl. Environ. Microbiol. 2005;71:538–541. doi: 10.1128/AEM.71.1.538-541.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Janda J.M., Abbott S.L. The genus Aeromonas: Taxonomy, pathogenicity, and infection. Clin. Microbiol. Rev. 2010;23:35–73. doi: 10.1128/CMR.00039-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Figueras M.J., Beaz-Hidalgo R. Aeromonas. Academic Press; Norfolk, UK: 2015. Aeromonas infections in humans; pp. 65–108. [Google Scholar]
- 6.Salvat M.J.F., Ashbolt N. Global Water Pathogen Project. University of Alberta; Edmonton, AB, Canada: 2019. Aeromonas . [Google Scholar]
- 7.Beaz-Hidalgo R., Alperi A., Buján N., Romalde J.L., Figueras M.J. Comparison of phenotypical and genetic identification of Aeromonas strains isolated from diseased fish. Syst. Appl. Microbiol. 2010;33:149–153. doi: 10.1016/j.syapm.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 8.Martínez-Murcia A.J., Benlloch S., Collins M.D. Phylogenetic interrelationships of members of the genera Aeromonas and Plesiomonas as determined by 16S ribosomal DNA sequencing: Lack of congruence with results of DNA-DNA hybridizations. Int. J. Syst. Bacteriol. 1992;42:412–421. doi: 10.1099/00207713-42-3-412. [DOI] [PubMed] [Google Scholar]
- 9.Yáñez M.A., Catalan V., Apráiz D., Figueras M.J., Martínez-Murcia A.J. Phylogenetic analysis of members of the genus Aeromonas based on gyrB gene sequences. Int. J. Syst. Evol. Microbiol. 2003;53:875–883. doi: 10.1099/ijs.0.02443-0. [DOI] [PubMed] [Google Scholar]
- 10.Soler L., Yáñez M.A., Chacon M.R., Aguilera-Arreola M.G., Catalan V., Figueras M.J., Martínez-Murcia A.J. Phylogenetic analysis of the genus Aeromonas based on two housekeeping genes. Int. J. Syst. Evol. Microbiol. 2004;54:1511–1519. doi: 10.1099/ijs.0.03048-0. [DOI] [PubMed] [Google Scholar]
- 11.Martínez-Murcia A.J., Monera A., Saavedra M.J., Oncina R., Lopez-Alvarez M., Lara E., Figueras M.J. Multilocus phylogenetic analysis of the genus Aeromonas. Syst. Appl. Microbiol. 2011;34:189–199. doi: 10.1016/j.syapm.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 12.Beaz-Hidalgo R., Hossain M.J., Liles M.R., Figueras M.-J. Strategies to avoid wrongly labelled genomes using as example the detected wrong taxonomic affiliation for Aeromonas genomes in the genbank database. PLoS ONE. 2015;10 doi: 10.1371/journal.pone.0115813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beaz-Hidalgo R., Laviad-Shitrit S., Shakèd T., Halpern M., Figueras M.J. Chironomid egg masses harbour the clinical species Aeromonas taiwanensis and Aeromonas sanarellii. FEMS Microbiol. Lett. 2012;337:48–54. doi: 10.1111/1574-6968.12003. [DOI] [PubMed] [Google Scholar]
- 14.Figueras M.J., Beaz-Hidalgo R., Hossain M.J., Liles M.R. Taxonomic affiliation of new genomes should be verified using average nucleotide identity and multilocus phylogenetic analysis. Genome Announc. 2014;2 doi: 10.1128/genomeA.00927-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Latif-Eugenin F.L. Aeromonas, un microorganismo ambiental de importancia en salud humana y animal. Universidad Rovira i Virgili; Tarragona, Spain: 2015. [Google Scholar]
- 16.Vincent A.T., Fernández-Bravo A., Sanchis M., Mayayo E., Figueras M.J., Charette S.J. Investigation of the virulence and genomics of Aeromonas salmonicida strains isolated from human patients. Infect. Genet. Evol. 2019;68:1–9. doi: 10.1016/j.meegid.2018.11.019. [DOI] [PubMed] [Google Scholar]
- 17.Romero A., Saraceni P.R., Merino S., Figueras A., Tomás J.M., Novoa B. The animal model determines the results of Aeromonas virulence factors. Front. Microbiol. 2016;7:1245. doi: 10.3389/fmicb.2016.01574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tomás J.M. The main Aeromonas pathogenic factors. ISRN Microbiol. 2012;2012:1–22. doi: 10.5402/2012/256261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beaz-Hidalgo R., Figueras M.J. Aeromonas spp. whole genomes and virulence factors implicated in fish disease. J. Fish Dis. 2013;36:371–388. doi: 10.1111/jfd.12025. [DOI] [PubMed] [Google Scholar]
- 20.Fernández-Bravo A. Epidemiology and pathogenic characterization of species of the genus Aeromonas. Universidad Rovira i Virgili; Tarragona, Spain: 2019. [Google Scholar]
- 21.Su J., Yang C., Xiong F., Wang Y., Zhu Z. Toll-like receptor 4 signaling pathway can be triggered by grass carp reovirus and Aeromonas hydrophila infection in rare minnow Gobiocypris rarus. Fish Shellfish. Immunol. 2009;27:33–39. doi: 10.1016/j.fsi.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 22.McCoy A.J., Koizumi Y., Higa N., Suzuki T. Differential regulation of caspase-1 activation via NLRP3/NLRC4 inflammasomes mediated by aerolysin and type III secretion system during Aeromonas veronii infection. J. Immunol. 2010;185:7077–7084. doi: 10.4049/jimmunol.1002165. [DOI] [PubMed] [Google Scholar]
- 23.McCoy A.J., Koizumi Y., Toma C., Higa N., Dixit V., Taniguchi S., Tschopp J., Suzuki T. Cytotoxins of the human pathogen Aeromonas hydrophila trigger, via the NLRP3 inflammasome, caspase-1 activation in macrophages. Eur. J. Immunol. 2010;40:2797–2803. doi: 10.1002/eji.201040490. [DOI] [PubMed] [Google Scholar]
- 24.Srivastava N., Shelly A., Kumar M., Pant A., Das B., Majumdar T., Mazumder S. Aeromonas hydrophila utilizes TLR4 topology for synchronous activation of MyD88 and TRIF to orchestrate anti-inflammatory responses in zebrafish. Cell Death Discov. 2017;3:17067. doi: 10.1038/cddiscovery.2017.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sanarelli G. Ueber einen neuen mikroorganismus des Wassers, welcher fur thiere mit veraenderlicher und konstanter temperatur pathogen ist. Zentrable Bakteriol. Parasitenkd. Infekt. Hyg. Abt. 1991;2:222–228. [Google Scholar]
- 26.Colwell R.R., McDonell M.R., Ley D.J. Proposal to recognise the family Aeromonadaceae fam. nov. Int. J. Med. Microbiol. 1986;26:19–27. [Google Scholar]
- 27.Tanaka K.H., Dallaire-Dufresne S., Daher R.K., Frenette M., Charette S.J. An insertion sequence-dependent plasmid rearrangement in Aeromonas salmonicida causes the loss of the type three secretion system. PLoS ONE. 2012;7:e33725. doi: 10.1371/journal.pone.0033725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tanaka K.H., Vincent A.T., Emond-Rheault J.-G., Adamczuk M., Frenette M., Charette S.J. Plasmid composition in Aeromonas salmonicida subsp. salmonicida 01-B526 unravels unsuspected type three secretion system loss patterns. BMC Genom. 2017;18:528. doi: 10.1186/s12864-017-3921-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martinez-Murcia A., Garay E., Collins M., Esteve C. Aeromonas allosaccharophila sp. nov., a new mesophilic member of the genus Aeromonas. FEMS Microbiol. Lett. 1992;91:199–205. doi: 10.1111/j.1574-6968.1992.tb05209.x. [DOI] [PubMed] [Google Scholar]
- 30.Beaz-Hidalgo R., Latif-Eugenin F., Hossain M., Berg K., Niemi R., Rapala J., Lyra C., Liles M., Figueras M.J. Aeromonas aquatica sp. nov., Aeromonas finlandiensis sp. nov. and Aeromonas lacus sp. nov. isolated from Finnish waters associated with cyanobacterial blooms. Syst. Appl. Microbiol. 2015;38:161–168. doi: 10.1016/j.syapm.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 31.Figueras M.J., Latif-Eugenin F., Ballester F., Pujol I., Tena D., Berg K., Hossain M.J., Beaz-Hidalgo R., Liles M.R. ‘Aeromonas intestinalis’ and ‘Aeromonas enterica’ isolated from human faeces, ‘Aeromonas crassostreae’ from oyster and ‘Aeromonas aquatilis’ isolated from lake water represent novel species. New Microbes New Infect. 2017;15:74–76. doi: 10.1016/j.nmni.2016.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aravena-Román M., Beaz-Hidalgo R., Inglis T.J.J., Riley T.V., Martínez-Murcia A.J., Chang B.J., Figueras M.J. Aeromonas australiensis sp. nov., isolated from irrigation water. Int. J. Syst. Evol. Microbiol. 2013;63:3130. doi: 10.1099/ijs.0.055368-0. [DOI] [PubMed] [Google Scholar]
- 33.Ali A., Carnahan A., Altwegg M., Luthy-Hottenstein J., Josep S.W. Aeromonas bestiarum sp. nov. (formely genomospecies DNA group 2 Aeromonas hydrophila), a new species isolated from non human sources. Med. Microbiol. Lett. 1996;5:156–165. [Google Scholar]
- 34.Miñana-Galbis D., Farfán M., Fusté M.C., Lorén J.G. Aeromonas bivalvium sp. nov., isolated from bivalve molluscs. Int. J. Syst. Evol. Microbiol. 2007;57:582–587. doi: 10.1099/ijs.0.64497-0. [DOI] [PubMed] [Google Scholar]
- 35.Martinez-Murcia A., Beaz-Hidalgo R., Svec P., Saavedra M.J., Figueras M.J., Sedlacek I. Aeromonas cavernicola sp. nov., isolated from fresh water of a brook in a cavern. Curr. Microbiol. 2013;66:197–204. doi: 10.1007/s00284-012-0253-x. [DOI] [PubMed] [Google Scholar]
- 36.Schubert R.H., Hegazi M. Aeromonas eucrenophila species nova Aeromonas caviae a later and illegitimate synonym of Aeromonas punctata. Zent. Bakteriol. Mikrobiol. Hyg. Ser. A Med. Microbiol. Infect. Dis. Virol. Parasitol. 1988;268:34–39. doi: 10.1016/S0176-6724(88)80112-3. [DOI] [PubMed] [Google Scholar]
- 37.Beaz-Hidalgo R., Martinez-Murcia A., Figueras M.J. Reclassification of Aeromonas hydrophila subsp. dhakensis Huys et al. 2002 and Aeromonas aquariorum Martinez-Murcia et al. 2008 as Aeromonas dhakensis sp. nov. comb nov. and emendation of the species Aeromonas hydrophila. Syst. Appl. Microbiol. 2013;36:171–176. doi: 10.1016/j.syapm.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 38.Miñana-Galbis D., Farfán M., Lorén J.G., Fusté M.C. Proposal to assign Aeromonas diversa sp. nov. as a novel species designation for Aeromonas group 501. Syst. Appl. Microbiol. 2010;33:15–19. doi: 10.1016/j.syapm.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 39.Esteve C., Gutierrez M.C., Ventosa A., Verdonck L., Mergaert J., Rijckaert C., Swings J., Kersters K., De Ley J. Aeromonas encheleia sp. nov., isolated from European eels. Int. J. Syst. Bacteriol. 1995;45:462–466. doi: 10.1099/00207713-45-3-462. [DOI] [PubMed] [Google Scholar]
- 40.Alperi A., Martínez-Murcia A.J., Monera A., Saavedra M.J., Figueras M.J. Aeromonas fluvialis sp. nov., isolated from a Spanish river. Int. J. Syst. Evol. Microbiol. 2010;60:1008. doi: 10.1099/ijs.0.67074-0. [DOI] [PubMed] [Google Scholar]
- 41.Stanier R.Y. A note on the taxonomy of P. hydrophilus. J. Bacteriol. 1943;46:213–214. doi: 10.1128/JB.46.2.213-214.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Carnahan A.M., Chakraborty T., Fanning G.R., Verma D., Ali A., Janda J.M., Joseph S.W. Aeromonas trota sp. nov., an ampicillin-susceptible species isolated from clinical specimens. J. Clin. Microbiol. 1991;29:1206–1210. doi: 10.1128/JCM.29.6.1206-1210.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Allen D.A., Austin B., Colwell R.R., Gavini F., Ferragut C., Izard D., Trinel P.A., Leclerc H., Lefebvre B., Mossel D.A.A. Aeromonas media, a new species isolated from river water. Int. J. Syst. Bacteriol. 1983;33:599–604. doi: 10.1099/00207713-33-3-599. [DOI] [Google Scholar]
- 44.Miñana-Galbis D. Aeromonas molluscorum sp. nov., isolated from bivalve molluscs. Int. J. Syst. Evol. Microbiol. 2004;54:2073–2078. doi: 10.1099/ijs.0.63202-0. [DOI] [PubMed] [Google Scholar]
- 45.Beaz-Hidalgo R., Alperi A., Figueras M.J., Romalde J.L. Aeromonas piscicola sp. nov., isolated from diseased fish. Syst. Appl. Microbiol. 2009;32:471–479. doi: 10.1016/j.syapm.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 46.Huys G., Kampfer P., Altwegg M., Kersters I., Lamb A., Coopman R., Lüthy-Hottenstein J., Vancanneyt M., Janssen P., Kersters K. Aeromonas popoffii sp. nov., a mesophilic bacterium isolated from drinking water production plants and reservoirs. Int. J. Syst. Bacteriol. 1997;47:1165–1171. doi: 10.1099/00207713-47-4-1165. [DOI] [PubMed] [Google Scholar]
- 47.Marti E., Balcázar J.L. Aeromonas rivipollensis sp. nov., a novel species isolated from aquatic samples. J. Basic Microbiol. 2015;55:1435–1439. doi: 10.1002/jobm.201500264. [DOI] [PubMed] [Google Scholar]
- 48.Figueras M.J., Alperi A., Beaz-Hidalgo R., Stackebrandt E., Brambilla E., Monera A., Martinez-Murcia A.J. Aeromonas rivuli sp. nov., isolated from the upstream region of a karst water rivulet. Int. J. Syst. Evol. Microbiol. 2011;61:242–248. doi: 10.1099/ijs.0.016139-0. [DOI] [PubMed] [Google Scholar]
- 49.Griffin P.J., Snieszko S.F., Friddle S.B. Pigment formation by Bacterium salmonicida. J. Bacteriol. 1953;65:652–659. doi: 10.1128/JB.65.6.652-659.1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alperi A., Martinez-Murcia A.J., Ko W.C., Monera A., Saavedra M.J., Figueras M.J. Aeromonas taiwanensis sp. nov. and Aeromonas sanarellii sp. nov., clinical species from Taiwan. Int. J. Syst. Evol. Microbiol. 2010;60:2048–2055. doi: 10.1099/ijs.0.014621-0. [DOI] [PubMed] [Google Scholar]
- 51.Hickman-Brenner F.W., Fanning G.R., Arduino M.J., Brenner D.J., Farmer J.J. Aeromonas schubertii, a new mannitol-negative species found in human clinical specimens. J. Clin. Microbiol. 1988;26:1561–1564. doi: 10.1128/JCM.26.8.1561-1564.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Harf-Monteil C., Le Flèche A., Riegel P., Prévost G., Bermond D., Grimont P.A.D., Monteil H. Aeromonas simiae sp. nov., isolated from monkey faeces. Int. J. Syst. Evol. Microbiol. 2004;54:481–485. doi: 10.1099/ijs.0.02786-0. [DOI] [PubMed] [Google Scholar]
- 53.Popoff M., Veron M. Validation of the new names and new combinations previously effectively published outside the IJSB. Int. J. Syst. Bacteriol. 1981;31:215. [Google Scholar]
- 54.Demarta A., Küpfer M., Riegel P., Harf-Monteil C., Tonolla M., Peduzzi R., Monera A., Saavedra M.J., Martínez-Murcia A. Aeromonas tecta sp. nov., isolated from clinical and environmental sources. Syst. Appl. Microbiol. 2008;31:278–286. doi: 10.1016/j.syapm.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 55.Hickman-Brenner F.W., Macdonald K.L., Steigerwalt A.G., Fanning G.R., Brenner D.J., Farmer J.J. Aeromonas veronii, a new ornithine decarboxylase-positive species that may cause diarrhea. J. Clin. Microbiol. 1987;25:900–906. doi: 10.1128/JCM.25.5.900-906.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Stackebrandt E., Garrity G.M., Trüper H.G., Whitman W.B., Grimont P.A.D., Nesme X., Frederiksen W., Vauterin L., Kampfer P., Rosselló-Mora R., et al. Report of the ad hoc committee for the re-evaluation of the species definition in bacteriology. Int. J. Syst. Evol. Microbiol. 2002;52:1043–1047. doi: 10.1099/00207713-52-3-1043. [DOI] [PubMed] [Google Scholar]
- 57.Figueras M.J., Beaz-Hidalgo R., Collado L., Martínez-Murcia A.J. Recommendations for a new bacterial species description based on analysis of the unrelated genera Aeromonas and Arcobacter. Bull. BISMiS. 2011;2:1–16. [Google Scholar]
- 58.Abbott S.L., Cheung W.K.W., Janda J.M. The genus Aeromonas: Biochemical characteristics, atypical reactions, and phenotypic identification schemes. J. Clin. Microbiol. 2003;41:2348–2357. doi: 10.1128/JCM.41.6.2348-2357.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lamy B., Laurent F., Verdier I., Decousser J.-W., Lecaillon E., Marchandin H., Roger F., Tigaud S., De Montclos H., Kodjo A. Accuracy of 6 commercial systems for identifying clinical Aeromonas isolates. Diagn. Microbiol. Infect. Dis. 2010;67:9–14. doi: 10.1016/j.diagmicrobio.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 60.Chacón M.R., Castro-Escarpulli G., Soler L., Guarro J., Figueras M.J. A DNA probe specific for Aeromonas colonies. Diagn. Microbiol. Infect. Dis. 2002;44:221–225. doi: 10.1016/S0732-8893(02)00455-8. [DOI] [PubMed] [Google Scholar]
- 61.Soler L., Marco F., Vilá J., Chacon M.R., Guarro J., Figueras M.J. Evaluation of two miniaturized systems, MicroScan W/A and BBL Crystal E/NF, for identification of clinical isolates of Aeromonas spp. J. Clin. Microbiol. 2003;41:5732–5734. doi: 10.1128/JCM.41.12.5732-5734.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Woo P., Lau S., Teng J., Tse H., Yuen K.-Y. Then and now: Use of 16S rDNA gene sequencing for bacterial identification and discovery of novel bacteria in clinical microbiology laboratories. Clin. Microbiol. Infect. 2008;14:908–934. doi: 10.1111/j.1469-0691.2008.02070.x. [DOI] [PubMed] [Google Scholar]
- 63.Vega-Sánchez V. Caracterización fenotípica y genotípica de aislamientos de Aeromonas spp. obtenidos de trucha arcoíris (Oncorhynchus mykiss) Universidad Autónoma del Estado de México; Toluca, Mexico: 2015. [Google Scholar]
- 64.Martínez-Murcia A., Lamy B. Aeromonas. Academic Press; Norfolk, UK: 2015. Molecular diagnostics by genetic methods; pp. 155–200. [DOI] [Google Scholar]
- 65.Alperi A., Figueras M.J., Inza I., Martínez-Murcia A.J. Analysis of 16S rRNA gene mutations in a subset of Aeromonas strains and their impact in species delineation. Int. Microbiol. 2008;11:185–194. [PubMed] [Google Scholar]
- 66.Roger F., Marchandin H., Jumas-Bilak E., Kodjo A., Lamy B. Multilocus genetics to reconstruct aeromonad evolution. BMC Microbiol. 2012;12:62. doi: 10.1186/1471-2180-12-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Vavrova A., Balazova T., Sedlacek I., Tvrzova L., Sedo O. Evaluation of the MALDI-TOF MS profiling for identification of newly described Aeromonas spp. Folia Microbiol. 2015;60:375–383. doi: 10.1007/s12223-014-0369-4. [DOI] [PubMed] [Google Scholar]
- 68.Chen P.-L., Wu C.-J., Chen C.-S., Tsai P.-J., Tang H.-J., Ko W.-C., Cutler S. A comparative study of clinical Aeromonas dhakensis and Aeromonas hydrophila isolates in southern Taiwan: A. dhakensis is more predominant and virulent. Clin. Microbiol. Infect. 2014;20:O428–O434. doi: 10.1111/1469-0691.12456. [DOI] [PubMed] [Google Scholar]
- 69.Shin H.B., Yoon J., Lee Y., Kim M.S., Lee K. Comparison of MALDI-TOF MS, housekeeping gene sequencing, and 16S rRNA gene sequencing for identification of Aeromonas clinical isolates. Yonsei Med. J. 2015;56:550–555. doi: 10.3349/ymj.2015.56.2.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pérez-Sancho M., Cerdá I., Fernández-Bravo A., Domínguez L., Figueras M.J., Fernández-Garayzábal J.F., Vela A.I. Limited performance of MALDI-TOF for identification of fish Aeromonas isolates at species level. J. Fish Dis. 2018;41:1485–1493. doi: 10.1111/jfd.12837. [DOI] [PubMed] [Google Scholar]
- 71.Zhong C., Han M., Yang P., Chen C., Yu H., Wang L., Ning K. Comprehensive analysis reveals the evolution and pathogenicity of Aeromonas, viewed from both single isolated species and microbial communities. mSystems. 2019;4 doi: 10.1128/mSystems.00252-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Harayama S., Kasai H. Molecular Identification, Systematics, and Population Structure of Prokaryotes. Springer Science and Business Media; Berlin/Heidelberg, Germany: 2006. Bacterial phylogeny reconstruction from molecular sequences; pp. 105–139. [Google Scholar]
- 73.Küpfer M., Kuhnert P., Korczak B.M., Peduzzi R., Demarta A. Genetic relationships of Aeromonas strains inferred from 16S rRNA, gyrB and rpoB gene sequences. Int. J. Syst. Evol. Microbiol. 2006;56:2743–2751. doi: 10.1099/ijs.0.63650-0. [DOI] [PubMed] [Google Scholar]
- 74.Nhung P.H., Hata H., Ohkusu K., Noda M., Shah M.M., Goto K., Ezaki T. Use of the novel phylogenetic marker dnaJ and DNA-DNA hybridization to clarify interrelationships within the genus Aeromonas. Int. J. Syst. Evol. Microbiol. 2007;57:1232–1237. doi: 10.1099/ijs.0.64957-0. [DOI] [PubMed] [Google Scholar]
- 75.Sepe A., Barbieri P., Peduzzi R., Demarta A. Evaluation of recA sequencing for the classification of Aeromonas strains at the genotype level. Lett. Appl. Microbiol. 2008;46:439–444. doi: 10.1111/j.1472-765X.2008.02339.x. [DOI] [PubMed] [Google Scholar]
- 76.Miñana-Galbis D., Urbizu-Serrano A., Farfán M., Fusté M.C., Lorén J.G. Phylogenetic analysis and identification of Aeromonas species based on sequencing of the cpn60 universal target. Int. J. Syst. Evol. Microbiol. 2009;59:1976–1983. doi: 10.1099/ijs.0.005413-0. [DOI] [PubMed] [Google Scholar]
- 77.Martino M.E., Fasolato L., Montemurro F., Rosteghin M., Manfrin A., Patarnello T., Novelli E., Cardazzo B. Determination of microbial diversity of Aeromonas strains on the basis of multilocus sequence typing, phenotype, and presence of putative virulence genes. Appl. Environ. Microbiol. 2011;77:4986–5000. doi: 10.1128/AEM.00708-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Soler L., Figueras M.J., Chacón M.R., Guarro J., Martinez-Murcia A.J. Comparison of three molecular methods for typing Aeromonas popoffii isolates. Antonie Leeuwenhoek. 2003;83:341–349. doi: 10.1023/A:1023312415276. [DOI] [PubMed] [Google Scholar]
- 79.Aguilera-Arreola M.G., Hernandez-Rodriguez C., Zuniga G., Figueras M.J., Castro-Escarpulli G., Hernández-Rodríguez C. Aeromonas hydrophila clinical and environmental ecotypes as revealed by genetic diversity and virulence genes. FEMS Microbiol. Lett. 2005;242:231–240. doi: 10.1016/j.femsle.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 80.Maiti N., Mandal A., Mohanty S., Mandal R. Phenotypic and genetic characterization of Edwardsiella tarda isolated from pond sediments. Comp. Immunol. Microbiol. Infect. Dis. 2009;32:1–8. doi: 10.1016/j.cimid.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 81.Fontes M.C., Saavedra M.J., Monera A., Martins C., Martínez-Murcia A. Phylogenetic identification of Aeromonas simiae from a pig, first isolate since species description. Veter. Microbiol. 2010;142:313–316. doi: 10.1016/j.vetmic.2009.09.033. [DOI] [PubMed] [Google Scholar]
- 82.Latif-Eugenín F., Beaz-Hidalgo R., Figueras M.J. Evaluation of different conditions and culture media for the recovery of Aeromonas spp. from water and shellfish samples. J. Appl. Microbiol. 2016;121:883–891. doi: 10.1111/jam.13210. [DOI] [PubMed] [Google Scholar]
- 83.Jolley K.A., Maiden M.C. BIGSdb: Scalable analysis of bacterial genome variation at the population level. BMC Bioinform. 2010;11:595. doi: 10.1186/1471-2105-11-595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Seshadri R., Joseph S.W., Chopra A.K., Sha J., Shaw J., Graf J., Haft D., Wu M., Ren Q., Rosovitz M.J., et al. Genome sequence of Aeromonas hydrophila ATCC 7966T: Jack of all trades. J. Bacteriol. 2006;188:8272–8282. doi: 10.1128/JB.00621-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Beatson S.A., das Gracas de Luna M., Bachmann N.L., Alikhan N.F., Hanks K.R., Sullivan M.J., Wee B.A., Freitas-Almeida A.C., Dos Santos P.A., de Melo J.T., et al. Genome sequence of the emerging pathogen Aeromonas caviae. J. Bacteriol. 2011;193:1286–1287. doi: 10.1128/JB.01337-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Charette S.J., Brochu F., Boyle B., Filion G., Tanaka K.H., Derome N. Draft genome sequence of the virulent strain 01-B526 of the fish pathogen Aeromonas salmonicida. J. Bacteriol. 2012;194:722–723. doi: 10.1128/JB.06276-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Li Y., Liu Y., Zhou Z., Huang H., Ren Y., Zhang Y., Li G., Zhou Z., Wang L. Complete genome sequence of Aeromonas veronii strain B565. J. Bacteriol. 2011;193:3389–3390. doi: 10.1128/JB.00347-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Reith M.E., Singh R.K., Curtis B., Boyd J.M., Bouevitch A., Kimball J., Munholland J., Murphy C., Sarty D., Williams J., et al. The genome of Aeromonas salmonicida subsp. salmonicida A449: Insights into the evolution of a fish pathogen. BMC Genom. 2008;9:427. doi: 10.1186/1471-2164-9-427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wu C.-J., Wang H.-C., Chen C.-S., Shu H.-Y., Kao A.-W., Chen P.-L., Ko W.-C. Genome sequence of a novel human pathogen, Aeromonas aquariorum. J. Bacteriol. 2012;194:4114–4115. doi: 10.1128/JB.00621-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Colston S.M., Fullmer M.S., Beka L., Lamy B., Gogarten J.P., Graf J. Bioinformatic genome comparisons for taxonomic and phylogenetic assignments using Aeromonas as a test case. MBio. 2014;5 doi: 10.1128/mBio.02136-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Meier-Kolthoff J.P., Göker M., Spröer C., Klenk H.-P. When should a DDH experiment be mandatory in microbial taxonomy? Arch. Microbiol. 2013;195:413–418. doi: 10.1007/s00203-013-0888-4. [DOI] [PubMed] [Google Scholar]
- 92.Richter M., Rossello-Mora R. Shifting the genomic gold standard for the prokaryotic species definition. Proc. Natl. Acad. Sci. USA. 2009;106:19126–19131. doi: 10.1073/pnas.0906412106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kim M., Oh H.-S., Park S.-C., Chun J. Towards a taxonomic coherence between average nucleotide identity and 16S rRNA gene sequence similarity for species demarcation of prokaryotes. Int. J. Syst. Evol. Microbiol. 2014;64:346–351. doi: 10.1099/ijs.0.059774-0. [DOI] [PubMed] [Google Scholar]
- 94.Awan F., Dong Y., Liu J., Wang N., Mushtaq M.H., Lu C., Liu Y. Comparative genome analysis provides deep insights into Aeromonas hydrophila taxonomy and virulence-related factors. BMC Genom. 2018;19:712. doi: 10.1186/s12864-018-5100-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Talagrand-Reboul E., Roger F., Kimper J.-L., Colston S.M., Graf J., Latif-Eugenín F., Figueras M.J., Petit F., Marchandin H., Jumas-Bilak E., et al. Delineation of taxonomic species within complex of species: Aeromonas media and related species as a test case. Front. Microbiol. 2017;8:23. doi: 10.3389/fmicb.2017.00621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Vincent A.T., Charette S.J. Completion of genome of Aeromonas salmonicida subsp. salmonicida 01-B526 reveals how sequencing technologies can influence sequence quality and result interpretations. New Microbes New Infect. 2018;25:24–26. doi: 10.1016/j.nmni.2018.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pessoa R.B.G., De Oliveira W.F., Marques D.S.C., Correia M.T.D.S., De Carvalho E.V.M.M., Coelho L.C.B.B. The genus Aeromonas: A general approach. Microb. Pathog. 2019;130:81–94. doi: 10.1016/j.micpath.2019.02.036. [DOI] [PubMed] [Google Scholar]
- 98.Monfort P., Baleux B. Dynamics of Aeromonas hydrophila, Aeromonas sobria, and Aeromonas caviae in a sewage treatment pond. Appl. Environ. Microbiol. 1990;56:1999–2006. doi: 10.1128/AEM.56.7.1999-2006.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Dumontet S., Krovacek K., Baloda S., Grottoli R., Pasquale V., Vanucci S. Ecological relationship between Aeromonas and Vibrio spp. and planktonic copepods in the coastal marine environment in Southern Italy. Comp. Immunol. Microbiol. Infect. Dis. 1996;19:245–254. doi: 10.1016/0147-9571(96)00012-4. [DOI] [PubMed] [Google Scholar]
- 100.Borrell N., Figueras M.J., Guarro J. Phenotypic identification of Aeromonas genomospecies from clinical and environmental sources. Can. J. Microbiol. 1998;44:103–108. doi: 10.1139/w97-135. [DOI] [PubMed] [Google Scholar]
- 101.Montes M., Perez M.J., Nieto T.P. Numerical taxonomy of gram-negative, facultative anaerobic bacteria isolated from skin of turbot (Scophthalmus maximus) and surrounding water. Syst. Appl. Microbiol. 1999;22:604–618. doi: 10.1016/S0723-2020(99)80014-9. [DOI] [PubMed] [Google Scholar]
- 102.Egorov A.I., Best J.M.B., Frebis C.P., Karapondo M.S. Occurrence of Aeromonas spp. in a random sample of drinking water distribution systems in the USA. J. Water Heal. 2011;9:785–798. doi: 10.2166/wh.2011.169. [DOI] [PubMed] [Google Scholar]
- 103.Sharma M., Resta R., Car R. Intermolecular dynamical charge fluctuations in water: A signature of the H-bond network. Phys. Rev. Lett. 2005;95:187401. doi: 10.1103/PhysRevLett.95.187401. [DOI] [PubMed] [Google Scholar]
- 104.Araujo R.M., Parés R., Lucena F. The effect of terrestrial effluents on the incidence of Aeromonas spp. in coastal waters. J. Appl. Bacteriol. 1990;69:439–444. doi: 10.1111/j.1365-2672.1990.tb01535.x. [DOI] [PubMed] [Google Scholar]
- 105.Berg K.A., Lyra C., Sivonen K., Paulin L., Suomalainen S., Tuomi P., Rapala J. High diversity of cultivable heterotrophic bacteria in association with cyanobacterial water blooms. ISME J. 2009;3:314–325. doi: 10.1038/ismej.2008.110. [DOI] [PubMed] [Google Scholar]
- 106.Berg K.A., Lyra C., Niemi R.M., Heens B., Hoppu K., Erkomaa K., Sivonen K., Rapala J. Virulence genes of Aeromonas isolates, bacterial endotoxins and cyanobacterial toxins from recreational water samples associated with human health symptoms. J. Water Heal. 2011;9:670–679. doi: 10.2166/wh.2011.206. [DOI] [PubMed] [Google Scholar]
- 107.McLellan S.L., Huse S.M., Mueller-Spitz S.R., Andreishcheva E.N., Sogin M.L. Diversity and population structure of sewage-derived microorganisms in wastewater treatment plant influent. Environ. Microbiol. 2010;12:378–392. doi: 10.1111/j.1462-2920.2009.02075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Al-Jassim N., Ansari M.I., Harb M., Hong P.-Y. Removal of bacterial contaminants and antibiotic resistance genes by conventional wastewater treatment processes in Saudi Arabia: Is the treated wastewater safe to reuse for agricultural irrigation? Water Res. 2015;73:277–290. doi: 10.1016/j.watres.2015.01.036. [DOI] [PubMed] [Google Scholar]
- 109.Varela A.R., Nunes O.C., Manaia C.M. Quinolone resistant Aeromonas spp. as carriers and potential tracers of acquired antibiotic resistance in hospital and municipal wastewater. Sci. Total. Environ. 2016;542:665–671. doi: 10.1016/j.scitotenv.2015.10.124. [DOI] [PubMed] [Google Scholar]
- 110.Holmes P., Nicolls L.M., Sartory D.P. The Genus Aeromonas. John Wiley & Sons Ltd.; West Sussex, UK: 1996. The ecology of mesophilic Aeromonas in the aquatic environment; pp. 127–150. [Google Scholar]
- 111.Erhart R., Beimfohr C., Wagner M., Amann R. Characterization of bacterial communities from activated sludge: Culture-dependent numerical identification versus in situ identification using group- and genus-specific rRNA-targeted oligonucleotide probes. Microb. Ecol. 1996;32:101–121. doi: 10.1007/BF00185883. [DOI] [PubMed] [Google Scholar]
- 112.Latif-Eugenín F., Beaz-Hidalgo R., José F.M. A culture independent method for the detection of Aeromonas sp. from water samples. Ital. J. Food Saf. 2016;5:5489. doi: 10.4081/ijfs.2016.5489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Latif-Eugenín F., Beaz-Hidalgo R., Silvera-Simón C., Fernandez-Cassi X., Figueras M.J. Chlorinated and ultraviolet radiation -treated reclaimed irrigation water is the source of Aeromonas found in vegetables used for human consumption. Environ. Res. 2017;154:190–195. doi: 10.1016/j.envres.2016.12.026. [DOI] [PubMed] [Google Scholar]
- 114.Fernandez-Cassi X., Silvera C., Cervero-Aragó S., Rusiñol M., Latif-Eugeni F., Bruguera-Casamada C., Civit S., Araujo R.M., Figueras M.J., Gironés R., et al. Evaluation of the microbiological quality of reclaimed water produced from a lagooning system. Environ. Sci. Pollut. Res. 2016;23:16816–16833. doi: 10.1007/s11356-016-6812-0. [DOI] [PubMed] [Google Scholar]
- 115.Boussaid A., Baleux B., Hassani L., Lesne J. Aeromonas species in stabilization ponds in the arid region of Marrakesh, Morocco, and relation to fecal-pollution and climatic factors. Microb. Ecol. 1991;21:11–20. doi: 10.1007/BF02539141. [DOI] [PubMed] [Google Scholar]
- 116.Hassani L., Imziln B., Boussaid A., Gauthier M.J. Seasonal incidence of and antibiotic resistance among Aeromonas species isolated from domestic wastewater before and after treatment in stabilization ponds. Microb. Ecol. 1992;23:227–237. doi: 10.1007/BF00164098. [DOI] [PubMed] [Google Scholar]
- 117.Jjemba P.K., Weinrich L.A., Cheng W., Giraldo E., Lechevallier M.W. Regrowth of potential opportunistic pathogens and algae in reclaimed-water distribution systems. Appl. Environ. Microbiol. 2010;76:4169–4178. doi: 10.1128/AEM.03147-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Pianetti A., Bruscolini F., Sabatini L., Colantoni P. Microbial characteristics of marine sediments in bathing area along Pesaro-Gabicce coast (Italy): A preliminary study. J. Appl. Microbiol. 2004;97:682–689. doi: 10.1111/j.1365-2672.2004.02352.x. [DOI] [PubMed] [Google Scholar]
- 119.Khajanchi B.K., Fadl A.A., Borchardt M.A., Berg R.L., Horneman A.J., Stemper M.E., Joseph S.W., Moyer N.P., Sha J., Chopra A.K. Distribution of virulence factors and molecular fingerprinting of Aeromonas species isolates from water and clinical samples: Suggestive evidence of water-to-human transmission. Appl. Environ. Microbiol. 2010;76:2313–2325. doi: 10.1128/AEM.02535-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pablos M., Huys G., Cnockaert M., Rodríguez-Calleja J.M., Otero A., Santos J.A., García-López M.-L. Identification and epidemiological relationships of Aeromonas isolates from patients with diarrhea, drinking water and foods. Int. J. Food Microbiol. 2011;147:203–210. doi: 10.1016/j.ijfoodmicro.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 121.Van Der Kooij D., Martijn B., Schaap P.G., Hoogenboezem W., Veenendaal H.R., Van Der Wielen P.W. Improved biostability assessment of drinking water with a suite of test methods at a water supply treating eutrophic lake water. Water Res. 2015;87:347–355. doi: 10.1016/j.watres.2015.09.043. [DOI] [PubMed] [Google Scholar]
- 122.Sisti M., Albano A., Brandi G. Bactericidal effect of chlorine on motile Aeromonas spp. in drinking water supplies and influence of temperature on disinfection efficacy. Lett. Appl. Microbiol. 1998;26:347–351. doi: 10.1046/j.1472-765X.1998.00346.x. [DOI] [PubMed] [Google Scholar]
- 123.Chang Y.-C., Wang J.-Y., Selvam A., Kao S.-C., Yang S.-S., Shih D.Y.-C. Multiplex PCR detection of enterotoxin genes in Aeromonas spp. from suspect food samples in northern Taiwan. J. Food Prot. 2008;71:2094–2099. doi: 10.4315/0362-028X-71.10.2094. [DOI] [PubMed] [Google Scholar]
- 124.Nagar V., Shashidhar R., Bandekar J.R. Prevalence, characterization, and antimicrobial resistance of Aeromonas strains from various retail food products in Mumbai, India. J. Food Sci. 2011;76:M486–M492. doi: 10.1111/j.1750-3841.2011.02303.x. [DOI] [PubMed] [Google Scholar]
- 125.Nagar V., Shashidhar R., Bandekar J.R. Characterization of Aeromonas strains isolated from Indian foods using rpoD gene sequencing and whole cell protein analysis. World J. Microbiol. Biotechnol. 2013;29:745–752. doi: 10.1007/s11274-012-1212-1. [DOI] [PubMed] [Google Scholar]
- 126.Hoel S., Vadstein O., Jakobsen A.N. Species distribution and prevalence of putative virulence factors in mesophilic Aeromonas spp. isolated from fresh retail sushi. Front. Microbiol. 2017;8:931. doi: 10.3389/fmicb.2017.00931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hoel S., Vadstein O., Jakobsen A.N. The significance of mesophilic Aeromonas spp. in minimally processed ready-to-eat seafood. Microorganisms. 2019;7:91. doi: 10.3390/microorganisms7030091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Figueras M.J., Beaz-Hidalgo R. Encyclopedia of Food Microbiology. Academic Press; London, UK: 2014. Aeromonas: Introduction, detection by cultural and modern techniques; pp. 25–30. [Google Scholar]
- 129.Hammad A.M., Moustafa A.-E.H., Mansour M.M., Fahmy B.M., Hamada M.G., Shimamoto T., Shimamoto T. Molecular and phenotypic analysis of hemolytic Aeromonas strains isolated from food in Egypt revealed clinically important multidrug resistance and virulence profiles. J. Food Prot. 2018;81:1015–1021. doi: 10.4315/0362-028X.JFP-17-360. [DOI] [PubMed] [Google Scholar]
- 130.John N., Vidyalakshmi V., Hatha A.M. Effect of pH and salinity on the production of extracellular virulence factors by Aeromonas from food sources. J. Food Sci. 2019;84:2250–2255. doi: 10.1111/1750-3841.14729. [DOI] [PubMed] [Google Scholar]
- 131.Praveen P.K., Debnath C., Shekhar S., Dalai N., Ganguly S. Incidence of Aeromonas spp. infection in fish and chicken meat and its related public health hazards: A review. Veter. World. 2016;9:6–11. doi: 10.14202/vetworld.2016.6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Shen Y., Xu C., Sun Q., Schwarz S., Ou Y., Yang L., Huang Z., Eichhorn I., Walsh T.R., Wang Y., et al. Prevalence and genetic analysis of mcr-3-positive Aeromonas species from humans, retail meat, and environmental water samples. Antimicrob. Agents Chemother. 2018;62 doi: 10.1128/AAC.00404-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Castro-Escarpulli G., Figueras M.J., Aguilera-Arreola G., Soler L., Fernández-Rendón E., Aparicio G.O., Guarro J., Chacón M.R. Characterisation of Aeromonas spp. isolated from frozen fish intended for human consumption in Mexico. Int. J. Food Microbiol. 2003;84:41–49. doi: 10.1016/S0168-1605(02)00393-8. [DOI] [PubMed] [Google Scholar]
- 134.Woodring J., Srijan A., Puripunyakom P., Oransathid W., Wongstitwilairoong B., Mason C. Prevalence and antimicrobial susceptibilities of Vibrio, Salmonella, and Aeromonas isolates from various uncooked seafoods in Thailand. J. Food Prot. 2012;75:41–47. doi: 10.4315/0362-028X.JFP-11-211. [DOI] [PubMed] [Google Scholar]
- 135.Yano Y., Hamano K., Tsutsui I., Aue-Umneoy D., Ban M., Satomi M. Occurrence, molecular characterization, and antimicrobial susceptibility of Aeromonas spp. in marine species of shrimps cultured at inland low salinity ponds. Food Microbiol. 2015;47:21–27. doi: 10.1016/j.fm.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 136.Figueras M.J., Borrego J.J. New perspectives in monitoring drinking water microbial quality. Int. J. Environ. Res. Public Heal. 2010;7:4179–4202. doi: 10.3390/ijerph7124179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Farmer J.J., Arduino M.J., Hickman-Brenner F.W. The Prokaryotes. Springer Science and Business Media; Berlin/Heidelberg, Germany: 2006. The genera Aeromonas and Plesiomonas; pp. 564–596. [Google Scholar]
- 138.Rasmussen-Ivey C.R., Hossain M.J., Odom S.E., Terhune J.S., Hemstreet W.G., Shoemaker C.A., Zhang D., Xu D.-H., Griffin M.J., Liu Y.-J., et al. Classification of a hypervirulent Aeromonas hydrophila pathotype responsible for epidemic outbreaks in warm-water fishes. Front. Microbiol. 2016;7:334. doi: 10.3389/fmicb.2016.01615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Nawaz M., Khan S.A., Khan A.A., Sung K., Tran Q., Kerdahi K., Steele R. Detection and characterization of virulence genes and integrons in Aeromonas veronii isolated from catfish. Food Microbiol. 2010;27:327–331. doi: 10.1016/j.fm.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 140.Li Y., Cai S.H. Identification and pathogenicity of Aeromonas sobria on tail-rot disease in juvenile tilapia Oreochromis niloticus. Curr. Microbiol. 2011;62:623–627. doi: 10.1007/s00284-010-9753-8. [DOI] [PubMed] [Google Scholar]
- 141.Chen Y.F., Liang R.S., Zhuo X.L., Wu X.T., Zou J.X. Isolation and characterization of Aeromonas schubertii from diseased snakehead, Channa maculata (Lacepède) J. Fish Dis. 2012;35:421–430. doi: 10.1111/j.1365-2761.2012.01362.x. [DOI] [PubMed] [Google Scholar]
- 142.Yi S.-W., You M.-J., Cho H.-S., Lee C.-S., Kwon J.-K., Shin G.-W. Molecular characterization of Aeromonas species isolated from farmed eels (Anguilla japonica) Veter. Microbiol. 2013;164:195–200. doi: 10.1016/j.vetmic.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 143.Esteve C., Gutiérrez M.C., Ventosa A. DNA Relatedness among Aeromonas allosaccharophila strains and DNA hybridization groups of the genus Aeromonas. Int. J. Syst. Bacteriol. 1995;45:390–391. doi: 10.1099/00207713-45-2-390. [DOI] [PubMed] [Google Scholar]
- 144.Esteve C., Alcaide E., Blasco M.D. Aeromonas hydrophila subsp. dhakensis isolated from feces, water and fish in Mediterranean Spain. Microbes Environ. 2012;27:367–373. doi: 10.1264/jsme2.ME12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ghenghesh K.S., Abeid S.S., Jaber M.M., Ben-Taher S.A. Isolation and haemolytic activity of Aeromonas species from domestic dogs and cats. Comp. Immunol. Microbiol. Infect. Dis. 1999;22:175–179. doi: 10.1016/S0147-9571(98)00134-9. [DOI] [PubMed] [Google Scholar]
- 146.Forga-Martel J., Gonzalez-Valle F., Weinzierl J. Infectious abortion associated with Aeromonas hydrophila in a mare. Equine Pract. 2000;22:22–24. [Google Scholar]
- 147.Waldridge B.M., Stewart A.J., Taylor D.C., Saville W.J. The incidence of Aeromonas species in the feces of nondiarrheic horses. J. Equine Veter. Sci. 2011;31:700–702. doi: 10.1016/j.jevs.2011.05.004. [DOI] [Google Scholar]
- 148.Worthing K.A., Norris J.M., Briscoe K.A. Severe acute cellulitis and sepsis caused by Aeromonas spp. in a dog on immunosuppressive therapy. J. Veter. Emerg. Crit. Care. 2019;29:444–449. doi: 10.1111/vec.12867. [DOI] [PubMed] [Google Scholar]
- 149.Gugliandolo C., Irrera G., Lentini V., Maugeri T. Pathogenic Vibrio, Aeromonas and Arcobacter spp. associated with copepods in the Straits of Messina (Italy) Mar. Pollut. Bull. 2008;56:600–606. doi: 10.1016/j.marpolbul.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 150.Pu W., Guo G., Yang N., Li Q., Yin F., Wang P., Zheng J., Zeng J. Three species of Aeromonas (A. dhakensis, A. hydrophila and A. jandaei) isolated from freshwater crocodiles (Crocodylus siamensis) with pneumonia and septicemia. Lett. Appl. Microbiol. 2019;68:212–218. doi: 10.1111/lam.13112. [DOI] [PubMed] [Google Scholar]
- 151.King G.E., Werner S.B., Kizer K.W. Epidemiology of Aeromonas infections in California. Clin. Infect. Dis. 1992;15:449–452. doi: 10.1093/clind/15.3.449. [DOI] [PubMed] [Google Scholar]
- 152.Lamy B., Kodjo A., Laurent F. Prospective nationwide study of Aeromonas infections in France. J. Clin. Microbiol. 2009;47:1234–1237. doi: 10.1128/JCM.00155-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Wu C.-J., Chen P.-L., Tang H.-J., Chen H.-M., Tseng F.-C., Shih H.-I., Hung Y.-P., Chung C.-H., Ko W.-C. Incidence of Aeromonas bacteremia in southern Taiwan: Vibrio and Salmonella bacteremia as comparators. J. Microbiol. Immunol. Infect. 2014;47:145–148. doi: 10.1016/j.jmii.2012.08.019. [DOI] [PubMed] [Google Scholar]
- 154.Mathur P., Batra P., Misra M.C. Aeromonas spp.: An emerging nosocomial pathogen. J. Lab. Physicians. 2016;8:1–4. doi: 10.4103/0974-2727.176234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Castro Escarpulli G., Pena del Barrio D., Castaneda N., Garcia Azcuaga A., Morier Dias L., Aguilera-Arreola M.G., Bravo Farias L. Virulence factors of A. caviae strains isolated from acute diarrheic disease in Cuba. Rev. Latinoam. Microbiol. 2002;44:11–13. [PubMed] [Google Scholar]
- 156.Tsai Y.-H., Shen S.-H., Yang T.-Y., Chen P.-H., Huang K.-C., Lee M.S. Monomicrobial necrotizing fasciitis caused by Aeromonas hydrophila and Klebsiella pneumoniae. Med. Princ. Pract. 2015;24:416–423. doi: 10.1159/000431094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Hochedez P., Hope-Rapp E., Olive C., Nicolas M., Beaucaire G., Cabie A. Bacteremia caused by Aeromonas species [corrected] complex in the Caribbean Islands of Martinique and Guadeloupe. Am. J. Trop. Med. Hyg. 2010;83:1123–1127. doi: 10.4269/ajtmh.2010.10-0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Su S.Y., Chao C.M., Lai C.C. Aeromonas bacteremia in southern Taiwan. Scand. J. Infect. Dis. 2013;45:728. doi: 10.3109/00365548.2012.755269. [DOI] [PubMed] [Google Scholar]
- 159.Igbinosa I.H., Igumbor E.U., Aghdasi F., Tom M., Okoh A.I. Emerging Aeromonas species infections and their significance in public health. Sci. World J. 2012;2012:1–13. doi: 10.1100/2012/625023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Aravena-Román M., Chang B.J., Riley T.V., Inglis T.J. Phenotypic characteristics of human clinical and environmental Aeromonas in Western Australia. Pathology. 2011;43:350–356. doi: 10.1097/PAT.0b013e3283463592. [DOI] [PubMed] [Google Scholar]
- 161.Puthucheary S.D., Puah S.M., Chua K.H. Molecular characterization of clinical isolates of Aeromonas species from Malaysia. PLoS ONE. 2012;7 doi: 10.1371/journal.pone.0030205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Huys G., Denys R., Albert M.J., Swings J., Kühn I., Kampfer P. Aeromonas hydrophila subsp. dhakensis subsp. nov., isolated from children with diarrhoea in Bangladesh, and extended description of Aeromonas hydrophila subsp. hydrophila (Chester 1901) Stanier 1943 (approved lists 1980) Int. J. Syst. Evol. Microbiol. 2002;52:705–712. doi: 10.1099/00207713-52-3-705. [DOI] [PubMed] [Google Scholar]
- 163.Hua H.T., Bollet C., Tercian S., Drancourt M., Raoult D. Aeromonas popoffii urinary tract infection. J. Clin. Microbiol. 2004;42:5427–5428. doi: 10.1128/JCM.42.11.5427-5428.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Al-Benwan K., Abbott S., Janda J.M., Huys G., Albert M.J. Cystitis caused by Aeromonas caviae. J. Clin. Microbiol. 2007;45:2348–2350. doi: 10.1128/JCM.00480-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Bossi-Kupfer M., Genini A., Peduzzi R., Demarta A. Tracheobronchitis caused by Aeromonas veronii biovar sobria after near-drowning. J. Med. Microbiol. 2007;56:1563–1564. doi: 10.1099/jmm.0.47202-0. [DOI] [PubMed] [Google Scholar]
- 166.Figueras M.J., Alperi A., Saavedra M.J., Ko W.-C., Gonzalo N., Navarro M., Martínez-Murcia A.J. Clinical relevance of the recently described species Aeromonas aquariorum. J. Clin. Microbiol. 2009;47:3742–3746. doi: 10.1128/JCM.02216-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Tena D., Aspiroz C., Figueras M.J., González-Praetorius A., Aldea M.J., Alperi A., Bisquert J. Surgical site infection due to Aeromonas species: Report of nine cases and literature review. Scand. J. Infect. Dis. 2009;41:164–170. doi: 10.1080/00365540802660492. [DOI] [PubMed] [Google Scholar]
- 168.Alperi A., Figueras M.J. Human isolates of Aeromonas possess Shiga toxin genes (stx1 and stx2) highly similar to the most virulent gene variants of Escherichia coli. Clin. Microbiol. Infect. 2010;16:1563–1567. doi: 10.1111/j.1469-0691.2010.03203.x. [DOI] [PubMed] [Google Scholar]
- 169.Sedláček I., Krejčí E., Andělová A., Sedláčková M., Porazilová I., Holochová P. Aeromonas hydrophila subsp. Dhakensis—A causative agent of gastroenteritis imported into the Czech Republic. Ann. Agric. Environ. Med. 2012;19:409–413. [PubMed] [Google Scholar]
- 170.Senderovich Y., Ken-Dror S., Vainblat I., Blau D., Izhaki I., Halpern M. A molecular study on the prevalence and virulence potential of Aeromonas spp. recovered from patients suffering from diarrhea in Israel. PLoS ONE. 2012;7:e30070. doi: 10.1371/journal.pone.0030070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Chen P.-L., Tsai P.-J., Chen C.-S., Lu Y.-C., Chen H.-M., Lee N.-Y., Lee C.-C., Li C.-W., Li M.-C., Wu C.-J., et al. Aeromonas stool isolates from individuals with or without diarrhea in southern Taiwan: Predominance of Aeromonas veronii. J. Microbiol. Immunol. Infect. 2015;48:618–624. doi: 10.1016/j.jmii.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 172.Morinaga Y., Yanagihara K., Eugenin F.L.L., Beaz-Hidalgo R., Kohno S., Salvat M.J.F. Identification error of Aeromonas aquariorum: A causative agent of septicemia. Diagn. Microbiol. Infect. Dis. 2013;76:106–109. doi: 10.1016/j.diagmicrobio.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 173.Shin G.-W., You M.-J., Cho H.-S., Yi S.-W., Lee C.-S. Severe sepsis due to Aeromonas aquariorum in a patient with liver cirrhosis. Jpn. J. Infect. Dis. 2013;66:519–522. doi: 10.7883/yoken.66.519. [DOI] [PubMed] [Google Scholar]
- 174.Perez-Valdespino A., Celestino-Mancera M., Villegas-Rodriguez V.L., Curiel-Quesada E. Characterization of mercury-resistant clinical Aeromonas species. Braz. J. Microbiol. 2013;44:1279–1283. doi: 10.1590/S1517-83822013000400036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Zhang H., Zou X., Zhao X., Cai L., Chen W., Yang L., Liu F., Qin D., Zeng G., Bai T., et al. Fatal Aeromonas bacteraemia in West Africa. J. Infect. 2016;72:258–260. doi: 10.1016/j.jinf.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 176.Wu C.-J., Ko W.-C., Lee N.-Y., Su S.-L., Li C.-W., Li M.-C., Chen Y.-W., Su Y.-C., Shu C.-Y., Lin Y.-T., et al. Aeromonas isolates from fish and patients in Tainan City, Taiwan: Genotypic and phenotypic characteristics. Appl. Environ. Microbiol. 2019;85 doi: 10.1128/AEM.01360-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Sinclair H.A., Heney C., Sidjabat H.E., George N.M., Bergh H., Anuj S.N., Nimmo G.R., Paterson D.L. Genotypic and phenotypic identification of Aeromonas species and CphA-mediated carbapenem resistance in Queensland, Australia. Diagn. Microbiol. Infect. Dis. 2016;85:98–101. doi: 10.1016/j.diagmicrobio.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 178.Da Silva L.C.A., Leal-Balbino T.C., De Melo B.S.T., Mendes-Marques C.L., Rezende A.M., De Almeida A.M.P., Leal N.C. Genetic diversity and virulence potential of clinical and environmental Aeromonas spp. isolates from a diarrhea outbreak. BMC Microbiol. 2017;17:179. doi: 10.1186/s12866-017-1089-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Van Zwetselaar M., Nyombi B., Sonda T., Kumburu H., Chamba N., Dekker M.C.J., Kilonzo K.G., Urasa S.J., Mmbaga B.T. Aeromonas caviae mimicking Vibrio cholerae infectious enteropathy in a cholera-endemic region with possible public health consequences: Two case reports. J. Med. Case Rep. 2018;12:71. doi: 10.1186/s13256-018-1603-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Dallagassa C.B., Surek M., Vizzotto B.S., Prediger K.C., Moriel B., Wolf S., Weiss V., Cruz L.M., Assis F.E., Paludo K.S., et al. Characteristics of an Aeromonas trota strain isolated from cerebrospinal fluid. Microb. Pathog. 2018;116:109–112. doi: 10.1016/j.micpath.2018.01.017. [DOI] [PubMed] [Google Scholar]
- 181.Khor W.C., Puah S.M., Koh T.H., Tan J.A.M.A., Puthucheary S.D., Chua K.H. Comparison of clinical isolates of Aeromonas from Singapore and Malaysia with regard to molecular identification, virulence, and antimicrobial profiles. Microb. Drug Resist. 2018;24:469–478. doi: 10.1089/mdr.2017.0083. [DOI] [PubMed] [Google Scholar]
- 182.Zhou Y., Yu L., Nan Z., Zhang P., Kan B., Yan D., Su J. Taxonomy, virulence genes and antimicrobial resistance of Aeromonas isolated from extra-intestinal and intestinal infections. BMC Infect. Dis. 2019;19:158. doi: 10.1186/s12879-019-3766-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Mosser T., Talagrand-Reboul E., Colston S.M., Graf J., Figueras M.J., Jumas-Bilak E., Lamy B. Exposure to pairs of Aeromonas strains enhances virulence in the Caenorhabditis elegans infection model. Front. Microbiol. 2015;6:3785. doi: 10.3389/fmicb.2015.01218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Joseph S.W., Carnahan A.M., Brayton P.R., Fanning G.R., Almazan R., Drabick C., Trudo E.W., Colwell R.R. Aeromonas jandaei and Aeromonas veronii dual infection of a human wound following aquatic exposure. J. Clin. Microbiol. 1991;29:565–569. doi: 10.1128/JCM.29.3.565-569.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Shak J.R., Whitaker J.A., Ribner B.S., Burd E.M. Aminoglycoside-resistant Aeromonas hydrophila as part of a polymicrobial infection following a traumatic fall into freshwater. J. Clin. Microbiol. 2011;49:1169–1170. doi: 10.1128/JCM.01949-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Grim C.J., Kozlova E.V., Ponnusamy D., Fitts E.C., Sha J., Kirtley M.L., Van Lier C.J., Tiner B.L., Erova T.E., Joseph S.J., et al. Functional genomic characterization of virulence factors from necrotizing fasciitis-causing strains of Aeromonas hydrophila. Appl. Environ. Microbiol. 2014;80:4162–4183. doi: 10.1128/AEM.00486-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Ponnusamy D., Kozlova E.V., Sha J., Erova T.E., Azar S.R., Fitts E.C., Kirtley M.L., Tiner B.L., Andersson J.A., Grim C.J., et al. Cross-talk among flesh-eating Aeromonas hydrophila strains in mixed infection leading to necrotizing fasciitis. Proc. Natl. Acad. Sci. USA. 2016;113:722–727. doi: 10.1073/pnas.1523817113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Fernández-Bravo A., Kilgore P.B., Andersson J.A., Blears E., Figueras M.J., Hasan N.A., Colwell R.R., Sha J., Chopra A.K. T6SS and ExoA of flesh-eating Aeromonas hydrophila in peritonitis and necrotizing fasciitis during mono- and polymicrobial infections. Proc. Natl. Acad. Sci. USA. 2019;116:24084–24092. doi: 10.1073/pnas.1914395116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Von Graevenitz A. The role of Aeromonas in diarrhea: A Review. Infection. 2007;35:59–64. doi: 10.1007/s15010-007-6243-4. [DOI] [PubMed] [Google Scholar]
- 190.Ottaviani D., Leoni F., Rocchegiani E., Santarelli S., Masini L., D’Annibale M.L., Pianetti A., Carraturo A. A severe case of Aeromonas veronii biovar sobria travellers’ diarrhoea characterized by Vibrio parahaemolyticus co-isolation. J. Med. Microbiol. 2013;62:161–164. doi: 10.1099/jmm.0.044743-0. [DOI] [PubMed] [Google Scholar]
- 191.Qamar F.N., Nisar M.I., Quadri F., Shakoor S., Sow S.O., Nasrin D., Blackwelder W.C., Wu Y., Farag T., Panchalingham S., et al. Aeromonas-associated diarrhea in children under 5 Years: The GEMS experience. Am. J. Trop. Med. Hyg. 2016;95:774–780. doi: 10.4269/ajtmh.16-0321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Teunis P., Figueras M.J. Reassessment of the enteropathogenicity of mesophilic Aeromonas species. Front. Microbiol. 2016;7:643. doi: 10.3389/fmicb.2016.01395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Figueras M.J., Horneman A.J., Martinez-Murcia A., Guarro J. Controversial data on the association of Aeromonas with diarrhoea in a recent Hong Kong study. J. Med. Microbiol. 2007;56:996–998. doi: 10.1099/jmm.0.47062-0. [DOI] [PubMed] [Google Scholar]
- 194.Mansour A.M., Abd Elkhalek R., Shaheen H.I., El Mohammady H., Refaey S., Hassan K., Riddle M., Sanders J.W., Sebeny P.J., Young S.Y., et al. Burden of Aeromonas hydrophila-associated diarrhea among children younger than 2 years in rural Egyptian community. J. Infect. Dev. Ctries. 2012;6:842–846. doi: 10.3855/jidc.2390. [DOI] [PubMed] [Google Scholar]
- 195.Schuetz A.N. Emerging agents of gastroenteritis: Aeromonas, Plesiomonas, and the diarrheagenic pathotypes of Escherichia coli. Semin. Diagn. Pathol. 2019;36:187–192. doi: 10.1053/j.semdp.2019.04.012. [DOI] [PubMed] [Google Scholar]
- 196.Figueras M.J. Clinical relevance of Aeromonas sM503. Rev. Med. Microbiol. 2005;16:145–153. doi: 10.1097/01.revmedmi.0000184410.98677.8a. [DOI] [Google Scholar]
- 197.Bravo L., Fernandez A., Nunez F.A., Rivero L.A., Ramirez M., Aguila A., Ledo Y., Cruz Y., Hernandez J. Aeromonas spp asociated to acute diarrheic disease in Cuba: Case-control study. Rev. Chil. Infectol. 2012;29:44–48. doi: 10.4067/S0716-10182012000100008. [DOI] [PubMed] [Google Scholar]
- 198.Chopra A.K., Houston C.W. Enterotoxins in Aeromonas-associated gastroenteritis. Microbes Infect. 1999;1:1129–1137. doi: 10.1016/S1286-4579(99)00202-6. [DOI] [PubMed] [Google Scholar]
- 199.Vila J., Ruiz J., Gallardo F., Vargas M., Soler L., Figueras M.J., Gascón J. Aeromonas spp. and traveler’s diarrhea: Clinical features and antimicrobial resistance. Emerg. Infect. Dis. 2003;9:552–555. doi: 10.3201/eid0905.020451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Granum P.E., O’Sullivan K., Tomas J.M., Ormen O. Possible virulence factors of Aeromonas spp. from food and water. FEMS Immunol. Med. Microbiol. 1998;21:131–137. doi: 10.1111/j.1574-695X.1998.tb01158.x. [DOI] [PubMed] [Google Scholar]
- 201.Krovacek K., Dumontet S., Eriksson E., Baloda S.B. Isolation, and Virulence Profiles, of Aeromonas hydrophila implicated in an outbreak of food poisoning in Sweden. Microbiol. Immunol. 1995;39:655–661. doi: 10.1111/j.1348-0421.1995.tb03253.x. [DOI] [PubMed] [Google Scholar]
- 202.Zhang Q., Shi G.-Q., Tang G.-P., Zou Z.-T., Yao G.-H., Zeng G. A foodborne outbreak of Aeromonas hydrophila in a college, Xingyi City, Guizhou, China, 2012. West. Pac. Surveill. Response J. 2012;3:39–43. doi: 10.5365/wpsar.2012.3.4.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Morgan D.R., Johnson P.C., Dupont H.L., Satterwhite T.K., Wood L.V. Lack of correlation between known virulence properties of Aeromonas hydrophila and enteropathogenicity for humans. Infect. Immun. 1985;50:62–65. doi: 10.1128/IAI.50.1.62-65.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Altwegg M., Lucchini G.M., Lüthy-Hottenstein J., Rohrbach M. Aeromonas-associated gastroenteritis after consumption of contaminated shrimp. Eur. J. Clin. Microbiol. Infect. Dis. 1991;10:44–45. doi: 10.1007/BF01967100. [DOI] [PubMed] [Google Scholar]
- 205.Janda J.M., Abbott S.L. Evolving concepts regarding the genus Aeromonas: An expanding panorama of species, disease presentations, and unanswered questions. Clin. Infect. Dis. 1998;27:332–344. doi: 10.1086/514652. [DOI] [PubMed] [Google Scholar]
- 206.Chao C.-M., Lai C.-C., Gau S.-J., Hsueh P.-R. Skin and soft tissue infection caused by Aeromonas species in cancer patients. J. Microbiol. Immunol. Infect. 2013;46:144–146. doi: 10.1016/j.jmii.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 207.Hiransuthikul N., Tantisiriwat W., Lertutsahakul K., Vibhagool A., Boonma P. Skin and soft-tissue infections among tsunami survivors in Southern Thailand. Clin. Infect. Dis. 2005;41:93–96. doi: 10.1086/497372. [DOI] [PubMed] [Google Scholar]
- 208.Presley S.M., Rainwater T.R., Austin G.P., Platt S.G., Zak J.C., Cobb G.P., Marsland E.J., Tian K., Zhang B., Anderson T.A., et al. Assessment of pathogens and toxicants in New Orleans, LA following Hurricane Katrina. Environ. Sci. Technol. 2006;40:468–474. doi: 10.1021/es052219p. [DOI] [PubMed] [Google Scholar]
- 209.Etemadi J., Ardalan M.R., Motavali R., Tubbs R.S., Shoja M.M. Thrombotic microangiopathy as a complication of medicinal leech therapy. South. Med. J. 2008;101:845–847. doi: 10.1097/SMJ.0b013e31817e30ca. [DOI] [PubMed] [Google Scholar]
- 210.Sartor C., Bornet C., Guinard D., Fournier P.-E. Transmission of Aeromonas hydrophila by leeches. Lancet. 2013;381:1686. doi: 10.1016/S0140-6736(13)60316-5. [DOI] [PubMed] [Google Scholar]
- 211.Spadaro S., Berselli A., Marangoni E., Romanello A., Colamussi M.V., Ragazzi R., Zardi S., Volta C.A. Aeromonas sobria necrotizing fasciitis and sepsis in an immunocompromised patient: A case report and review of the literature. J. Med. Case Rep. 2014;8:315. doi: 10.1186/1752-1947-8-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Furusu A., Yoshizuka N., Abe K., Sasaki O., Miyazaki K., Miyazaki M., Hirakata Y., Ozono Y., Harada T., Kohno S. Aeromonas hydrophila necrotizing fasciitis and gas gangrene in a diabetic patient on haemodialysis. Nephrol. Dial. Transplant. 1997;12:1730–1734. doi: 10.1093/ndt/12.8.1730. [DOI] [PubMed] [Google Scholar]
- 213.Joseph S.W., Daily O.P., Hunt W.S., Seidler R.J., Allen D.A., Colwell R.R. Aeromonas primary wound infection of a diver in polluted waters. J. Clin. Microbiol. 1979;10:46–49. doi: 10.1128/JCM.10.1.46-49.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Sever R., Lee Goldstein A., Steinberg E., Soffer D. Trauma with a touch of fresh water: Necrotizing fasciitis caused by Aeromonas hydrophila after a motorcycle accident. Am. Surg. 2013;79:E326–E328. [PubMed] [Google Scholar]
- 215.Pampin F., Bou G., Galeiras R., Freire D., Bouza M.T., Zuniga Mdel C. Aeromonas and meningitis: An unusual presentation. Neurocirugia. 2012;23:200–202. doi: 10.1016/j.neucir.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 216.Tang H.-J., Lai C.-C., Lin H.-L., Chao C.-M. Clinical manifestations of bacteremia caused by Aeromonas species in southern Taiwan. PLoS ONE. 2014;9:e91642. doi: 10.1371/journal.pone.0091642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Wu C.-J., Chen P.-L., Hsueh P.-R., Chang M.-C., Tsai P.-J., Shih H.-I., Wang H.-C., Chou P.-H., Ko W.-C. Clinical implications of species identification in monomicrobial Aeromonas bacteremia. PLoS ONE. 2015;10:e0117821. doi: 10.1371/journal.pone.0117821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Ohta T. A Case of severe sepsis presenting marked decrease of neutrophils and interesting findings on dynamic CT. Am. J. Case Rep. 2015;16:322–327. doi: 10.12659/AJCR.893351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Cordingley F.T., Rajanayagam A. Aeromonas hydrophila bacteraemia in haematological patients. Med. J. Aust. 1981;1:364–365. doi: 10.5694/j.1326-5377.1981.tb135636.x. [DOI] [PubMed] [Google Scholar]
- 220.Janda J.M., Guthertz L.S., Kokka R.P., Shimada T. Aeromonas species in septicemia: Laboratory characteristics and clinical observations. Clin. Infect. Dis. 1994;19:77–83. doi: 10.1093/clinids/19.1.77. [DOI] [PubMed] [Google Scholar]
- 221.Shizuma T., Tanaka C., Mori H., Fukuyama N. Investigation of bacteremia due to Aeromonas species and comparison with that due to enterobacteria in patients with liver cirrhosis. Gastroenterol. Res. Pract. 2011;2011:1–4. doi: 10.1155/2011/930826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Kao H.-T., Huang Y.-C., Lin T.-Y. Fatal bacteremic pneumonia caused by Aeromonas hydrophila in a previously healthy child. J. Microbiol. Immunol. Infect. 2003;36:209–211. [PubMed] [Google Scholar]
- 223.Nagata K., Takeshima Y., Tomii K., Imai Y. Fulminant fatal bacteremic pneumonia due to Aeromonas hydrophila in a non-immunocompromised woman. Intern. Med. 2011;50:63–65. doi: 10.2169/internalmedicine.50.4192. [DOI] [PubMed] [Google Scholar]
- 224.Tena D., González-Praetorius A., Gimeno C., Pérez-Pomata M.T., Bisquert J. Extraintestinal infection due to Aeromonas spp.: Review of 38 cases. Enferm. Infecc. Microbiol. Clín. 2007;25:235–241. doi: 10.1157/13100463. [DOI] [PubMed] [Google Scholar]
- 225.Mandal J., Dhodapkar R., Acharya N.S., Sastry A., Parija S.C. Urinary tract infection due to Aeromonas spp., a lesser known causative bacterium. J. Infect. Dev. Ctries. 2010;4:679–681. doi: 10.3855/jidc.1052. [DOI] [PubMed] [Google Scholar]
- 226.Garrido E., Sanromán A.L., Rodríguez-Gandía M.A., Rivero M., Royuela A., Moreira V., Milicua J.M. Optimized protocol for diagnosis of acute ileitis. Clin. Gastroenterol. Hepatol. 2009;7:1183–1188. doi: 10.1016/j.cgh.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 227.Lowry R., Balboa S., Parker J.L., Shaw J.G. Aeromonas flagella and colonisation mechanisms. Adv. Microb. Physiol. 2014;65:203–256. doi: 10.1016/bs.ampbs.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 228.Nazarenko E.L., Crawford R.J., Ivanova E.P. The structural diversity of carbohydrate antigens of selected gram-negative marine bacteria. Mar. Drugs. 2011;9:1914–1954. doi: 10.3390/md9101914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Heiss C., Wang Z., Thurlow C.M., Hossain M.J., Sun D., Liles M.R., Saper M.A., Azadi P. Structure of the capsule and lipopolysaccharide O-antigen from the channel catfish pathogen, Aeromonas hydrophila. Carbohydr. Res. 2019;486:107858. doi: 10.1016/j.carres.2019.107858. [DOI] [PubMed] [Google Scholar]
- 230.Merino S., Tomás J. Bacterial capsules and evasion of immune responses. eLS. 2010 doi: 10.1002/9780470015902.a0000957.pub4. [DOI] [Google Scholar]
- 231.Galindo C.L., Gutierrez C., Jr., Chopra A.K. Potential involvement of galectin-3 and SNAP23 in Aeromonas hydrophila cytotoxic enterotoxin-induced host cell apoptosis. Microb. Pathog. 2006;40:56–68. doi: 10.1016/j.micpath.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 232.Merino S., Rubires X., Knøchel S., Tomás J.M. Emerging pathogens: Aeromonas spp. Int. J. Food Microbiol. 1995;28:157–168. doi: 10.1016/0168-1605(95)00054-2. [DOI] [PubMed] [Google Scholar]
- 233.Janda J.M. Molecular Medical Microbiology. Academic Press; Cambridge, MA, USA: 2001. Aeromonas and Plesiomonas; pp. 1237–1270. [Google Scholar]
- 234.Palma-Martínez I., Guerrero-Mandujano A., Ruiz-Ruiz M.J., Hernández-Cortez C., Molina-López J., Bocanegra-García V., Castro-Escarpulli G. Active Shiga-like toxin produced by some Aeromonas spp., isolated in Mexico City. Front. Microbiol. 2016;7:4496. doi: 10.3389/fmicb.2016.01522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Chopra A.K., Xu X.-J., Ribardo D., Gonzalez M., Kuhl K., Peterson J.W., Houston C.W. The cytotoxic enterotoxin of Aeromonas hydrophila induces proinflammatory cytokine production and activates arachidonic acid metabolism in macrophages. Infect. Immun. 2000;68:2808–2818. doi: 10.1128/IAI.68.5.2808-2818.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Singh D.V., Sanyal S.C. Haemolysin and enterotoxin production by Aeromonas caviae isolated from diarrhoeal patients, fish and environment. J. Diarrhoeal Dis. Res. 1992;10:16–20. [PubMed] [Google Scholar]
- 237.Bernheimer A.W., Avigad L.S. Partial characterization of aerolysin, a lytic exotoxin from Aeromonas hydrophila. Infect. Immun. 1974;9:1016–1021. doi: 10.1128/IAI.9.6.1016-1021.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Sha J., Erova T.E., Alyea R.A., Wang S., Olano J.P., Pancholi V., Chopra A.K. Surface-expressed enolase contributes to the pathogenesis of clinical isolate SSU of Aeromonas hydrophila. J. Bacteriol. 2009;191:3095–3107. doi: 10.1128/JB.00005-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Huang L., Qin Y., Yan Q., Lin G., Huang L., Huang B., Huang W. MinD plays an important role in Aeromonas hydrophila adherence to Anguilla japonica mucus. Gene. 2015;565:275–281. doi: 10.1016/j.gene.2015.04.031. [DOI] [PubMed] [Google Scholar]
- 240.Herold S., Karch H., Schmidt H. Shiga toxin-encoding bacteriophages-genomes in motion. Int. J. Med. Microbiol. 2004;294:115–121. doi: 10.1016/j.ijmm.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 241.Tseng T.-T., Tyler B.M., Setubal J.C. Protein secretion systems in bacterial-host associations, and their description in the Gene Ontology. BMC Microbiol. 2009;9:S2. doi: 10.1186/1471-2180-9-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Cianciotto N.P. Type II secretion: A protein secretion system for all seasons. Trends Microbiol. 2005;13:581–588. doi: 10.1016/j.tim.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 243.Burr S.E., Stuber K., Wahli T., Frey J. Evidence for a type III secretion system in Aeromonas salmonicida subsp. salmonicida. J. Bacteriol. 2002;184:5966–5970. doi: 10.1128/JB.184.21.5966-5970.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Chacon M.R., Soler L., Groisman E.A., Guarro J., Figueras M.J. Type III secretion system genes in clinical Aeromonas isolates. J. Clin. Microbiol. 2004;42:1285–1287. doi: 10.1128/JCM.42.3.1285-1287.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Sha J., Wang S., Suarez G., Sierra J., Fadl A., Erova T., Foltz S., Khajanchi B., Silver A., Graf J., et al. Further characterization of a type III secretion system (T3SS) and of a new effector protein from a clinical isolate of Aeromonas hydrophila—Part I. Microb. Pathog. 2007;43:127–146. doi: 10.1016/j.micpath.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 246.Tan Y.W., Yu H.B., Leung K.Y., Sivaraman J., Mok Y.-K. Structure of AscE and induced burial regions in AscE and AscG upon formation of the chaperone needle-subunit complex of type III secretion system in Aeromonas hydrophila. Protein Sci. 2008;17:1748–1760. doi: 10.1110/ps.036798.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Vilches S., Jimenez N., Merino S., Tomás J.M. The Aeromonas dsbA mutation decreased their virulence by triggering type III secretion system but not flagella production. Microb. Pathog. 2012;52:130–139. doi: 10.1016/j.micpath.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 248.Vilches S., Urgell C., Merino S., Chacón M.R., Soler L., Castro-Escarpulli G., Figueras M.J., Tomás J.M. Complete type III secretion system of a mesophilic Aeromonas hydrophila strain. Appl. Environ. Microbiol. 2004;70:6914–6919. doi: 10.1128/AEM.70.11.6914-6919.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Vilches S., Wilhelms M., Yu H.B., Leung K.Y., Tomás J.M., Merino S. Aeromonas hydrophila AH-3 AexT is an ADP-ribosylating toxin secreted through the type III secretion system. Microb. Pathog. 2008;44:1–12. doi: 10.1016/j.micpath.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 250.Yu H.B., Rao P.S.S., Lee H.C., Vilches S., Merino S., Tomas J.M., Leung K.Y. A Type III secretion system is required for Aeromonas hydrophila AH-1 pathogenesis. Infect. Immun. 2004;72:1248–1256. doi: 10.1128/IAI.72.3.1248-1256.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Burr S.E., Frey J. Analysis of type III effector genes in typical and atypical Aeromonas salmonicida. J. Fish Dis. 2007;30:711–714. doi: 10.1111/j.1365-2761.2007.00859.x. [DOI] [PubMed] [Google Scholar]
- 252.Rangel L.T., Marden J., Colston S., Setubal J.C., Graf J., Gogarten J.P. Identification and characterization of putative Aeromonas spp. T3SS effectors. PLoS ONE. 2019;14:e0214035. doi: 10.1371/journal.pone.0214035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Bingle L.E., Bailey C.M., Pallen M.J. Type VI secretion: A beginner’s guide. Curr. Opin. Microbiol. 2008;11:3–8. doi: 10.1016/j.mib.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 254.Suarez G., Sierra J.C., Sha J., Wang S., Erova T.E., Fadl A.A., Foltz S.M., Horneman A.J., Chopra A.K. Molecular characterization of a functional type VI secretion system from a clinical isolate of Aeromonas hydrophila. Microb. Pathog. 2008;44:344–361. doi: 10.1016/j.micpath.2007.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.English G., Trunk K., Rao V.A., Srikannathasan V., Hunter W.N., Coulthurst S.J. New secreted toxins and immunity proteins encoded within the type VI secretion system gene cluster of Serratia marcescens. Mol. Microbiol. 2012;86:921–936. doi: 10.1111/mmi.12028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Carruthers M.D., Nicholson P.A., Tracy E.N., Munson R.S. Acinetobacter baumannii utilizes a type VI secretion system for bacterial competition. PLoS ONE. 2013;8:e59388. doi: 10.1371/annotation/7aa1688c-56c8-46ca-82ea-f86697f3c4fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Anderson M.C., Vonaesch P., Saffarian A., Marteyn B.S., Sansonetti P.J. Shigella sonnei encodes a functional T6SS used for interbacterial competition and niche occupancy. Cell Host Microbe. 2017;21:769–776. doi: 10.1016/j.chom.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 258.Miller M.B., Bassler B.L. Quorum sensing in bacteria. Annu. Rev. Microbiol. 2001;55:165–199. doi: 10.1146/annurev.micro.55.1.165. [DOI] [PubMed] [Google Scholar]
- 259.Khajanchi B.K., Kirtley M.L., Brackman S.M., Chopra A.K. Immunomodulatory and protective roles of quorum-sensing signaling molecules N-Acyl homoserine lactones during infection of mice with Aeromonas hydrophila. Infect. Immun. 2011;79:2646–2657. doi: 10.1128/IAI.00096-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Chan X.-Y., How K.-Y., Yin W.-F., Chan K.-G. N-Acyl homoserine lactone-mediated quorum sensing in Aeromonas veronii biovar sobria strain 159: Identification of LuxRI homologs. Front. Microbiol. 2016;6:5772. doi: 10.3389/fcimb.2016.00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Blöcher R., Ramírez A.R., Castro-Escarpulli G., Curiel-Quesada E., Reyes-Arellano A. design, synthesis, and evaluation of Alkyl-Quinoxalin-2(1H)-one derivatives as anti-quorum sensing molecules, inhibiting biofilm formation in Aeromonas caviae Sch3. Molecules. 2018;23:3075. doi: 10.3390/molecules23123075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Ding T., Li T., Li J. Impact of curcumin liposomes with anti-quorum sensing properties against foodborne pathogens Aeromonas hydrophila and Serratia grimesii. Microb. Pathog. 2018;122:137–143. doi: 10.1016/j.micpath.2018.06.009. [DOI] [PubMed] [Google Scholar]
- 263.Ding T., Li T., Wang Z., Li J. Curcumin liposomes interfere with quorum sensing system of Aeromonas sobria and in silico analysis. Sci. Rep. 2017;7:8612. doi: 10.1038/s41598-017-08986-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Liu L., Yan Y., Feng L., Zhu J. Quorum sensing asaI mutants affect spoilage phenotypes, motility, and biofilm formation in a marine fish isolate of Aeromonas salmonicida. Food Microbiol. 2018;76:40–51. doi: 10.1016/j.fm.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 265.Patel B., Kumari S., Banerjee R., Samanta M., Das S. Disruption of the quorum sensing regulated pathogenic traits of the biofilm-forming fish pathogen Aeromonas hydrophila by tannic acid, a potent quorum quencher. Biofouling. 2017;33:1–11. doi: 10.1080/08927014.2017.1336619. [DOI] [PubMed] [Google Scholar]
- 266.Talagrand-Reboul E., Jumas-Bilak E., Lamy B. The social life of Aeromonas through biofilm and quorum sensing systems. Front. Microbiol. 2017;8:449. doi: 10.3389/fmicb.2017.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Waldron K.J., Rutherford J.C., Ford D., Robinson N.J. Metalloproteins and metal sensing. Nature. 2009;460:823–830. doi: 10.1038/nature08300. [DOI] [PubMed] [Google Scholar]
- 268.Capdevila D.A., Wang J., Giedroc D.P. Bacterial strategies to maintain zinc metallostasis at the host-pathogen interface. J. Boil. Chem. 2016;291:20858–20868. doi: 10.1074/jbc.R116.742023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.O’Halloran T.V., Culotta V.C. Metallochaperones, an intracellular shuttle service for metal ions. J. Boil. Chem. 2000;275:25057–25060. doi: 10.1074/jbc.R000006200. [DOI] [PubMed] [Google Scholar]
- 270.Palmer L.D., Skaar E.P. Transition metals and virulence in bacteria. Annu. Rev. Genet. 2016;50:67–91. doi: 10.1146/annurev-genet-120215-035146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Fones H., Preston G.M. The impact of transition metals on bacterial plant disease. FEMS Microbiol. Rev. 2013;37:495–519. doi: 10.1111/1574-6976.12004. [DOI] [PubMed] [Google Scholar]
- 272.Francki K.T., Chang B.J., Mee B.J., Collignon P.J., Susai V., Keese P.K. Identification of genes associated with copper tolerance in an adhesion-defective mutant of Aeromonas veronii biovar sobria. FEMS Immunol. Med. Microbiol. 2000;29:115–121. doi: 10.1111/j.1574-695X.2000.tb01513.x. [DOI] [PubMed] [Google Scholar]
- 273.Fernandez-Bravo A., Lopez-Fernandez L., Figueras M.J. The metallochaperone encoding gene hypA is widely distributed among pathogenic Aeromonas spp. and its expression is increased under acidic pH and within macrophages. Microorganisms. 2019;7:415. doi: 10.3390/microorganisms7100415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Janeway C.A., Jr. How the immune system protects the host from infection. Microbes Infect. 2001;3:1167–1171. doi: 10.1016/S1286-4579(01)01477-0. [DOI] [PubMed] [Google Scholar]
- 275.Bergsbaken T., Fink S.L., Cookson B.T. Pyroptosis: Host cell death and inflammation. Nat. Rev. Genet. 2009;7:99–109. doi: 10.1038/nrmicro2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Kumar H., Kawai T., Akira S. Pathogen recognition by the innate immune system. Int. Rev. Immunol. 2011;30:16–34. doi: 10.3109/08830185.2010.529976. [DOI] [PubMed] [Google Scholar]
- 277.Mahla R.S., Reddy M.C., Prasad D.V.R., Kumar H. Sweeten PAMPs: Role of sugar complexed PAMPs in innate immunity and vaccine biology. Front. Immunol. 2013;4:248. doi: 10.3389/fimmu.2013.00248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Kawai T., Akira S. TLR signaling. Semin. Immunol. 2007;19:24–32. doi: 10.1016/j.smim.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 279.Shrestha N., Bahnan W., Wiley D.J., Barber G., Fields K.A., Schesser K. Eukaryotic initiation factor 2 (eIF2) signaling regulates proinflammatory cytokine expression and bacterial invasion. J. Boil. Chem. 2012;287:28738–28744. doi: 10.1074/jbc.M112.375915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Lamkanfi M., Dixit V.M. Inflammasomes: Guardians of cytosolic sanctity. Immunol. Rev. 2009;227:95–105. doi: 10.1111/j.1600-065X.2008.00730.x. [DOI] [PubMed] [Google Scholar]
- 281.Saxena M., Yeretssian G. NOD-Like receptors: Master regulators of inflammation and cancer. Front. Immunol. 2014;5:327. doi: 10.3389/fimmu.2014.00327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Zhang X.-T., Zhang G.-R., Shi Z.-C., Yuan Y.-J., Zheng H., Lin L., Wei K.-J., Ji W. Expression analysis of nine Toll-like receptors in yellow catfish (Pelteobagrus fulvidraco) responding to Aeromonas hydrophila challenge. Fish Shellfish. Immunol. 2017;63:384–393. doi: 10.1016/j.fsi.2017.02.021. [DOI] [PubMed] [Google Scholar]
- 283.Gong Y., Feng S., Li S., Zhang Y., Zhao Z., Hu M., Xu P., Jiang Y. Genome-wide characterization of Toll-like receptor gene family in common carp (Cyprinus carpio) and their involvement in host immune response to Aeromonas hydrophila infection. Comp. Biochem. Physiol. Part D Genom. Proteom. 2017;24:89–98. doi: 10.1016/j.cbd.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 284.Takeuchi O., Kawai T., Sanjo H., Copeland N., Gilbert D., Jenkins N., Takeda K., Akira S. TLR6: A novel member of an expanding toll-like receptor family. Gene. 1999;231:59–65. doi: 10.1016/S0378-1119(99)00098-0. [DOI] [PubMed] [Google Scholar]
- 285.Takeda K. Toll-like receptor. Jpn. J. Clin. Immunol. 2005;28:309–317. doi: 10.2177/jsci.28.309. [DOI] [PubMed] [Google Scholar]
- 286.Lai R.F., Jakovlic I., Liu H., Wei J., Zhan F.B., Yang P.H., Wang W.M. Characterization and expression of Megalobrama amblycephala toll-like receptor 22 involved in the response to Aeromonas hydrophila. J. Fish Biol. 2017;90:803–818. doi: 10.1111/jfb.13199. [DOI] [PubMed] [Google Scholar]
- 287.Basu M., Swain B., Sahoo B.R., Maiti N.K., Samanta M. Induction of toll-like receptor (TLR) 2, and MyD88-dependent TLR- signaling in response to ligand stimulation and bacterial infections in the Indian major carp, mrigal (Cirrhinus mrigala) Mol. Biol. Rep. 2012;39:6015–6028. doi: 10.1007/s11033-011-1415-9. [DOI] [PubMed] [Google Scholar]
- 288.Basu M., Swain B., Maiti N., Routray P., Samanta M. Inductive expression of toll-like receptor 5 (TLR5) and associated downstream signaling molecules following ligand exposure and bacterial infection in the Indian major carp, mrigal (Cirrhinus mrigala) Fish Shellfish. Immunol. 2012;32:121–131. doi: 10.1016/j.fsi.2011.10.031. [DOI] [PubMed] [Google Scholar]
- 289.Merino S., Wilhelms M., Tomás J.M. Role of Aeromonas hydrophila flagella glycosylation in adhesion to Hep-2 cells, biofilm formation and immune stimulation. Int. J. Mol. Sci. 2014;15:21935–21946. doi: 10.3390/ijms151221935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Brietzke A., Korytář T., Jaros J., Köllner B., Goldammer T., Seyfert H.-M., Rebl A. Aeromonas salmonicida infection only moderately regulates expression of factors contributing to toll-like receptor signaling but massively activates the cellular and humoral branches of innate immunity in rainbow trout (Oncorhynchus mykiss) J. Immunol. Res. 2015;2015:1–16. doi: 10.1155/2015/901015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Reyes-Becerril M., Ascencio-Valle F., Hirono I., Kondo H., Jirapongpairoj W., Esteban M.A., Alamillo E., Angulo C., Valadez C.E.A. TLR21’s agonists in combination with Aeromonas antigens synergistically up-regulate functional TLR21 and cytokine gene expression in yellowtail leucocytes. Dev. Comp. Immunol. 2016;61:107–115. doi: 10.1016/j.dci.2016.03.012. [DOI] [PubMed] [Google Scholar]
- 292.Zhang J., Li L., Kong X., Wu F., Zhou C., Nie G., Li X. Expression patterns of Toll-like receptors in natural triploid Carassius auratus after infection with Aeromonas hydrophila. Veter. Immunol. Immunopathol. 2015;168:77–82. doi: 10.1016/j.vetimm.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 293.Chandrarathna H., Nikapitiya C., Dananjaya S., Wijerathne C., Wimalasena S., Kwun H.J., Heo G.-J., Lee J., De Zoysa M. Outcome of co-infection with opportunistic and multidrug resistant Aeromonas hydrophila and A. veronii in zebrafish: Identification, characterization, pathogenicity and immune responses. Fish Shellfish. Immunol. 2018;80:573–581. doi: 10.1016/j.fsi.2018.06.049. [DOI] [PubMed] [Google Scholar]
- 294.Kong W.-G., Chen X.-X., Huang Y.-Q., Wu Z.-X., Li S.-S., Tang Y. A study of the damage of the intestinal mucosa barrier structure and function of Ctenopharyngodon idella with Aeromonas hydrophila. Fish Physiol. Biochem. 2017;43:1223–1235. doi: 10.1007/s10695-017-0366-z. [DOI] [PubMed] [Google Scholar]
- 295.Sierra J.C., Suárez G., Sha J., Baze W.B., Foltz S.M., Chopra A.K. Unraveling the mechanism of action of a new type III secretion system effector AexU from Aeromonas hydrophila. Microb. Pathog. 2010;49:122–134. doi: 10.1016/j.micpath.2010.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Xu Q.Q., Xu P., Zhou J.W., Pan T.S., Tuo R., Ai K., Yang D.Q. Cloning and expression analysis of two pro-inflammatory cytokines, IL-1beta and its receptor, IL-1R2, in the Asian swamp eel Monopterus albus. Mol. Biol. 2016;50:760–774. doi: 10.1134/S0026893316030122. [DOI] [PubMed] [Google Scholar]
- 297.Arockiaraj J., Bhatt P., Kumaresan V., Dhayanithi N.B., Arshad A., Harikrishnan R., Arasu M.V., Al-Dhabi N.A. Fish chemokines 14, 20 and 25: A comparative statement on computational analysis and mRNA regulation upon pathogenic infection. Fish Shellfish. Immunol. 2015;47:221–230. doi: 10.1016/j.fsi.2015.09.015. [DOI] [PubMed] [Google Scholar]
- 298.Liao Z., Wan Q., Xiao X., Ji J., Su J. A systematic investigation on the composition, evolution and expression characteristics of chemokine superfamily in grass carp Ctenopharyngodon idella. Dev. Comp. Immunol. 2018;82:72–82. doi: 10.1016/j.dci.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 299.Hayes S., Waltmann M., Donohue M., Lye D., Vesper S. Predicting virulence of Aeromonas isolates based on changes in transcription of c-jun and c-fos in human tissue culture cells. J. Appl. Microbiol. 2009;107:964–969. doi: 10.1111/j.1365-2672.2009.04276.x. [DOI] [PubMed] [Google Scholar]
- 300.Tian L., Zhou X.-Q., Jiang W.-D., Liu Y., Wu P., Jiang J., Kuang S.-Y., Tang L., Tang W.-N., Zhang Y.-A., et al. Sodium butyrate improved intestinal immune function associated with NF-κB and p38MAPK signalling pathways in young grass carp (Ctenopharyngodon idella) Fish Shellfish. Immunol. 2017;66:548–563. doi: 10.1016/j.fsi.2017.05.049. [DOI] [PubMed] [Google Scholar]
- 301.Banerjee C., Goswami R., Verma G., Datta M., Mazumder S. Aeromonas hydrophila induced head kidney macrophage apoptosis in Clarias batrachus involves the activation of calpain and is caspase-3 mediated. Dev. Comp. Immunol. 2012;37:323–333. doi: 10.1016/j.dci.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 302.Lu A.J., Hu X.C., Wang Y., Zhu A.H., Shen L.L., Tian J., Feng Z.Z., Feng Z.J. Skin immune response in the zebrafish, Danio rerio (Hamilton), to Aeromonas hydrophila infection: A transcriptional profiling approach. J. Fish Dis. 2015;38:137–150. doi: 10.1111/jfd.12214. [DOI] [PubMed] [Google Scholar]
- 303.Ni P.-J., Jiang W.-D., Wu P., Liu Y., Kuang S.-Y., Tang L., Tang W.-N., Zhang Y.-A., Zhou X.-Q., Feng L. Dietary low or excess levels of lipids reduced growth performance, and impaired immune function and structure of head kidney, spleen and skin in young grass carp (Ctenopharyngodon idella) under the infection of Aeromonas hydrophila. Fish Shellfish. Immunol. 2016;55:28–47. doi: 10.1016/j.fsi.2016.03.163. [DOI] [PubMed] [Google Scholar]
- 304.Reyes-Becerril M., Sanchez V., Delgado K., Guerra K., Velazquez E., Ascencio F., Angulo C. Caspase -1, -3, -8 and antioxidant enzyme genes are key molecular effectors following Vibrio parahaemolyticus and Aeromonas veronii infection in fish leukocytes. Immunobiology. 2018;223:562–576. doi: 10.1016/j.imbio.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 305.Shelly A., Banerjee C., Saurav G.K., Ray A., Rana V.S., Raman R., Mazumder S. Aeromonas hydrophila-induced alterations in cytosolic calcium activate pro-apoptotic cPKC-MEK1/2-TNFα axis in infected headkidney macrophages of Clarias gariepinus. Dev. Comp. Immunol. 2017;76:392–402. doi: 10.1016/j.dci.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 306.Mulder I., Wadsworth S., Secombes C. Cytokine expression in the intestine of rainbow trout (Oncorhynchus mykiss) during infection with Aeromonas salmonicida. Fish Shellfish. Immunol. 2007;23:747–759. doi: 10.1016/j.fsi.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 307.Hop H.T., Arayan L.T., Huy T.X.N., Reyes A.W.B., Vu S.H., Min W., Lee H.J., Rhee M.H., Chang H.H., Kim S. The key role of c-Fos for immune regulation and bacterial dissemination in Brucella infected macrophage. Front. Microbiol. 2018;8 doi: 10.3389/fcimb.2018.00287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Dos Santos P.A., Pereira A.C.M., Ferreira A.F., Alves M.A.D.M., Rosa A.C.P., Freitas-Almeida A.C., De Freitas-Almeida A.C. Adhesion, invasion, intracellular survival and cytotoxic activity of strains of Aeromonas spp. in HEp-2, Caco-2 and T-84 cell lines. Antonie Leeuwenhoek. 2015;107:1225–1236. doi: 10.1007/s10482-015-0416-4. [DOI] [PubMed] [Google Scholar]
- 309.Ghatak S., Agarwal R., Bhilegaonkar K. Comparative study of cytotoxicity of Aeromonas spp. on four different cell lines. Comp. Immunol. Microbiol. Infect. Dis. 2006;29:233–241. doi: 10.1016/j.cimid.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 310.Krzyminska S., Mokracka J., Koczura R., Cwiertnia A., Kaznowski A. Aeromonas spp.-mediated cell-contact cytotoxicity is associated with the presence of type III secretion system. Antonie Leeuwenhoek. 2012;101:243–251. doi: 10.1007/s10482-011-9627-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Ottaviani D., Parlani C., Citterio B., Masini L., Leoni F., Canonico C., Sabatini L., Bruscolini F., Pianetti A. Putative virulence properties of Aeromonas strains isolated from food, environmental and clinical sources in Italy: A comparative study. Int. J. Food Microbiol. 2011;144:538–545. doi: 10.1016/j.ijfoodmicro.2010.11.020. [DOI] [PubMed] [Google Scholar]
- 312.Albarral V., Sanglas A., Palau M., Miñana-Galbis D., Fusté M.C. Potential pathogenicity of Aeromonas hydrophila complex strains isolated from clinical, food, and environmental sources. Can. J. Microbiol. 2016;62:296–306. doi: 10.1139/cjm-2015-0466. [DOI] [PubMed] [Google Scholar]
- 313.Abdallah M.M. The cytotoxicity effect of metalloprotease produced and isolated from Aeromonas spp. Iraqi J. Vet. Med. 2019;42:41–45. [Google Scholar]
- 314.Dias C., Ribeiro M., Correia-Branco A., Domínguez-Perles R., Martel F., Saavedra M.J., Simões M. Virulence, attachment and invasion of Caco-2 cells by multidrug-resistant bacteria isolated from wild animals. Microb. Pathog. 2019;128:230–235. doi: 10.1016/j.micpath.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 315.Chen P.-L., Wu C.-J., Tsai P.-J., Tang H.-J., Chuang Y.-C., Lee N.-Y., Lee C.-C., Li C.-W., Li M.-C., Chen C.-C., et al. Virulence diversity among bacteremic Aeromonas isolates: Ex vivo, animal, and clinical evidences. PLoS ONE. 2014;9 doi: 10.1371/journal.pone.0111213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Dong Y., Yang Y., Liu J., Awan F., Lu C., Liu Y. Inhibition of Aeromonas hydrophila-induced intestinal inflammation and mucosal barrier function damage in crucian carp by oral administration of Lactococcus lactis. Fish Shellfish. Immunol. 2018;83:359–367. doi: 10.1016/j.fsi.2018.09.041. [DOI] [PubMed] [Google Scholar]
- 317.Peatman E., Mohammed H., Kirby A., Shoemaker C.A., Yildirim-Aksoy M., Beck B.H. Mechanisms of pathogen virulence and host susceptibility in virulent Aeromonas hydrophila infections of channel catfish (Ictalurus punctatus) Aquaculture. 2018;482:1–8. doi: 10.1016/j.aquaculture.2017.09.019. [DOI] [Google Scholar]
- 318.Sellegounder D., Gupta Y.R., Murugananthkumar R., Senthilkumaran B. Enterotoxic effects of Aeromonas hydrophila infection in the catfish, Clarias gariepinus: Biochemical, histological and proteome analyses. Veter. Immunol. Immunopathol. 2018;204:1–10. doi: 10.1016/j.vetimm.2018.08.008. [DOI] [PubMed] [Google Scholar]
- 319.Wang W., Tan S., Luo J., Shi H., Zhou T., Yang Y., Jin Y., Wang X., Niu D., Yuan Z., et al. GWAS analysis indicated importance of NF-κB signaling pathway in host resistance against motile Aeromonas septicemia disease in catfish. Mar. Biotechnol. 2019;21:335–347. doi: 10.1007/s10126-019-09883-0. [DOI] [PubMed] [Google Scholar]
- 320.Fock W., Chen C., Lam T., Sin Y. Roles of an endogenous serum lectin in the immune protection of blue gourami, Trichogaster trichopterus (Pallus) against Aeromonas hydrophila. Fish Shellfish. Immunol. 2001;11:101–113. doi: 10.1006/fsim.2000.0297. [DOI] [PubMed] [Google Scholar]
- 321.Yu H.B., Zhang Y.L., Lau Y.L., Yao F., Vilches S., Merino S., Tomas J.M., Howard S.P., Leung K.Y. Identification and characterization of putative virulence genes and gene clusters in Aeromonas hydrophila PPD134/91. Appl. Environ. Microbiol. 2005;71:4469–4477. doi: 10.1128/AEM.71.8.4469-4477.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Froquet R., Cherix N., Burr S.E., Frey J., Vilches S., Tomas J.M., Cosson P. Alternative host model to evaluate Aeromonas virulence. Appl. Environ. Microbiol. 2007;73:5657–5659. doi: 10.1128/AEM.00908-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Chen P.L., Chen Y.W., Ou C.C., Lee T.M., Wu C.J., Ko W.C., Chen C.S. A disease model of muscle necrosis caused by Aeromonas dhakensis infection in Caenorhabditis elegans. Front. Microbiol. 2016;7:2058. doi: 10.3389/fmicb.2016.02058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Chen Y.-W., Ko W.-C., Chen C.-S., Chen P.-L. Evaluating virulence and pathogenesis of Aeromonas infection in a Caenorhabditis elegans model. J. Vis. Exp. 2018:e58768. doi: 10.3791/58768. [DOI] [PubMed] [Google Scholar]
- 325.Buer J., Balling R. Mice, microbes and models of infection. Nat. Rev. Genet. 2003;4:195–205. doi: 10.1038/nrg1019. [DOI] [PubMed] [Google Scholar]
- 326.Aravena-Roman M., Inglis T.J., Henderson B., Riley T.V., Chang B.J. Antimicrobial susceptibilities of Aeromonas strains isolated from clinical and environmental sources to 26 antimicrobial agents. Antimicrob. Agents Chemother. 2012;56:1110–1112. doi: 10.1128/AAC.05387-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Codjoe F.S., Donkor E.S. Carbapenem resistance: A review. Med. Sci. 2017;6:1. doi: 10.3390/medsci6010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Ndi O.L., Barton M.D. Incidence of class 1 integron and other antibiotic resistance determinants in Aeromonas spp. from rainbow trout farms in Australia. J. Fish Dis. 2011;34:589–599. doi: 10.1111/j.1365-2761.2011.01272.x. [DOI] [PubMed] [Google Scholar]
- 329.Dias C., Serra C.R., Simoes L.C., Simões M., Martinez-Murcia A., Saavedra M.J. Extended-spectrum β-lactamase and carbapenemase-producing Aeromonas species in wild animals from Portugal. Veter. Rec. 2014;174:532. doi: 10.1136/vr.101803. [DOI] [PubMed] [Google Scholar]
- 330.Fosse T., Giraud-Morin C., Madinier I. Phenotypes of beta-lactam resistance in the genus Aeromonas. Pathol. Boil. 2003;51:290–296. doi: 10.1016/S0369-8114(03)00027-0. [DOI] [PubMed] [Google Scholar]
- 331.Cespedes J.S., Figueras M.J., Aspiroz C., Aldea M.J., Toledo M., Alperi A., Marco F., Vilá J. Development of imipenem resistance in an Aeromonas veronii biovar sobria clinical isolate recovered from a patient with cholangitis. J. Med. Microbiol. 2009;58:451–455. doi: 10.1099/jmm.0.47804-0. [DOI] [PubMed] [Google Scholar]
- 332.Dias C., Borges A., Saavedra M.J., Simoes M. Biofilm formation and multidrug-resistant Aeromonas spp. from wild animals. J. Glob. Antimicrob. Resist. 2018;12:227–234. doi: 10.1016/j.jgar.2017.09.010. [DOI] [PubMed] [Google Scholar]
- 333.Hossain S., De Silva B., Dahanayake P., Heo G.-J. Characterization of virulence properties and multi-drug resistance profiles in motile Aeromonas spp. isolated from zebrafish (Danio rerio) Lett. Appl. Microbiol. 2018;67:598–605. doi: 10.1111/lam.13075. [DOI] [PubMed] [Google Scholar]
- 334.Hossain S., De Silva B., Wickramanayake M., Dahanayake P., Wimalasena S., Heo G. Incidence of antimicrobial resistance genes and class 1 integron gene cassettes in multidrug-resistant motile Aeromonas sp. isolated from ornamental guppy (Poecilia reticulata) Lett. Appl. Microbiol. 2019;69:2–10. doi: 10.1111/lam.13162. [DOI] [PubMed] [Google Scholar]
- 335.Ramadan H., Ibrahim N., Samir M., El-Moaty A.A., Gad T. Aeromonas hydrophila from marketed mullet (Mugil cephalus) in Egypt: PCR characterization of β -lactam resistance and virulence genes. J. Appl. Microbiol. 2018;124:1629–1637. doi: 10.1111/jam.13734. [DOI] [PubMed] [Google Scholar]
- 336.Scarano C., Piras F., Virdis S., Ziino G., Nuvoloni R., Dalmasso A., De Santis E., Spanu C. Antibiotic resistance of Aeromonas ssp. strains isolated from Sparus aurata reared in Italian mariculture farms. Int. J. Food Microbiol. 2018;284:91–97. doi: 10.1016/j.ijfoodmicro.2018.07.033. [DOI] [PubMed] [Google Scholar]
- 337.Wimalasena S.H.M.P., Shin G.-W., Hossain S., Heo G.-J. Potential enterotoxicity and antimicrobial resistance pattern of Aeromonas species isolated from pet turtles and their environment. J. Veter. Med. Sci. 2017;79:921–926. doi: 10.1292/jvms.16-0493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Cattoir V., Poirel L., Aubert C., Soussy C.-J., Nordmann P. Unexpected occurrence of plasmid-mediated quinolone resistance determinants in environmental Aeromonas spp. Emerg. Infect. Dis. 2008;14:231–237. doi: 10.3201/eid1402.070677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Cespedes J.S., Blasco M.D., Marti S., Alba V., Alcalde E., Esteve C., Vila J. Plasmid-mediated QnrS2 determinant from a clinical Aeromonas veronii isolate. Antimicrob. Agents Chemother. 2008;52:2990–2991. doi: 10.1128/AAC.00287-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Piotrowska M., Popowska M. Insight into the mobilome of Aeromonas strains. Front. Microbiol. 2015;6:494. doi: 10.3389/fmicb.2015.00494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Vega-Sánchez V., Latif-Eugenín F., Soriano-Vargas E., Beaz-Hidalgo R., Figueras M.J., Aguilera-Arreola M.G., Castro-Escarpulli G. Re-identification of Aeromonas isolates from rainbow trout and incidence of class 1 integron and β-lactamase genes. Veter. Microbiol. 2014;172:528–533. doi: 10.1016/j.vetmic.2014.06.012. [DOI] [PubMed] [Google Scholar]
- 342.Piotrowska M., Przygodzińska D., Matyjewicz K., Popowska M. Occurrence and variety of β-Lactamase genes among Aeromonas spp. isolated from urban wastewater treatment plant. Front. Microbiol. 2017;8:863. doi: 10.3389/fmicb.2017.00863. [DOI] [PMC free article] [PubMed] [Google Scholar]