Abstract
New evidence raises concerns that posttraumatic stress disorder (PTSD) in preschool children is unremitting over years even with unstructured community treatment. This report presents proof of concept of the feasibility and effectiveness of a structured therapy, cognitive–behavioral therapy (CBT), for preschool PTSD that follows a range of different traumatic events. Two cases are presented, including transcribed dialogue, from a motor vehicle accident and Hurricane Katrina, respectively. Three key CBT feasibility questions were examined; it was concluded that (a) young children can cooperate meaningfully in structured, trauma-related exposure exercises; (b) they can utilize relaxation techniques successfully; and (c) highly anxious parents do not inhibit their children’s improvement per se as long as they can facilitate the manual techniques. Clinicians need to be aware of emerging evidence-based treatment for preschool children.
Preschool children historically have been underserved for mental health problems because of limited treatment studies with this population. For posttraumatic stress disorder (PTSD), the need for effective treatments is more pressing following new evidence that preschool PTSD is unremitting over 2 years even with unstructured community treatment (Scheeringa, Zeanah, Myers, & Putnam, 2005). Cognitive behavioral therapy (CBT) is well-studied for PTSD in adults, but the two prior studies with young children either did not diagnose PTSD (Cohen & Mannarino, 1996) or used a group format and included older children (Deblinger, Stauffer, & Steer, 2001), and both were restricted to sexual abuse. This report provides the first documentation of the feasibility and effectiveness of individual CBT designed for preschool PTSD from all other types of traumas. Two cases, victims of a motor vehicle accident and Hurricane Katrina, respectively, including transcribed dialogue, are presented as proof of concept to fill this gap. The CBT treatment includes both cognitive and behavioral techniques, but behavioral techniques are emphasized in these vignettes for illustrative purposes. Specifically, three questions of CBT feasibility are addressed. Can young children cooperate meaningfully in structured exposure work in the office and in vivo for homework? Can they utilize relaxation techniques successfully in these contexts? Because of young children’s dependence on the caregiving context, do highly anxious parents inhibit the progress of their children?
METHODS
Each case was treated in a trial funded by the National Institute of Mental Health to test a 12-session manualized protocol. The manual was similar to those for older children (March, Amaya-Jackson, & Murry, 1998). Sessions 1–4 teach children about posttraumatic stress symptomatology, how to self-identify and rate feelings, and several relaxation techniques. Session 5 is the “tell the story” session in which children recount in detail the traumatic experiences. Sessions 6–10 prescribe in-office exposures and out-of-office homework exposures. Session 11 focuses on relapse prevention and Session 12 is a review and graduation. All sessions include a caregiver. Pre- and post-treatment assessments of the 17 PTSD items for the children were conducted with the Preschool Age Psychiatric Assessment (Egger, Ascher, & Angold, 2002), and for parents, with the Diagnostic Interview Schedule. Weekly ratings of symptom change were assessed with parent report on the PTSD Parent–Child Weekly Rating Scale (PCWRS; Peebles &Scheeringa, 1996) that assesses 10 items for the child (sleep, irritability, fears, intrusive recollections, startle, avoidance of reminders, distress at reminders, hypervigilance, regression in developmental skills, and nightmares) and 10 items for the parent (sleep, intrusive recollections, difficulty concentrating, separation anxiety, irritability, avoidance of internal reminders, avoidance of external reminders, distress at reminders, hypervigilance, and loss of interests). Parents rate each item on a 5-point scale of change over the previous week: −2=much less severe, −1=less severe, 0=no change, 1=more severe, and 2=much more severe. The 10 child items and 10 parent items are summed to create one child score and one parent score. The possible scores range from −20 to 20, and the possible cumulative scores after 11 weeks range from −220 to 220.
RESULTS
Case 1. Dylan
Dylan was 4 1/2 years old when involved in a motor vehicle collision. His mother, 33, was driving when a speeding red pickup truck slammed into them and trapped Dylan in the back seat. He met the modified criteria for PTSD for preschool children (Scheeringa et al., 2005) with 8 items, including disabling fears of riding in cars and going past the scene of the accident. In addition, he had regressed to needing a bottle to fall asleep, would not go in his room alone at night, and feared all separations from his mother. His mother demonstrated all 17 PTSD symptoms.
Treatment began 3 months after the accident. The following transcript from Session 8 is about his homework assignment after Session 7, which was to walk up to a red truck. It illustrates Dylan’s capacity to cooperate meaningfully with homework exposures.
Counselor: So Dylan, you want to tell me how your homework was when you saw the red truck?
Child: (Holds up 10 fingers indicating the highest possible score on the stress thermometer)
Counselor: You were a 10? You must have been really scared?
Child: (Shakes head)
Counselor: Yeah. And what did you do to get not so scared?
Mom: We did our muscles. And we did breathing, huh? (referring to the relaxation techniques learned in treatment).
Child: (Shakes hands like floppy, relaxed muscles)
Counselor: Did you remember how your body felt?
Child: Yes.
Mom: He was angry. Very angry.
Child: (Nods head)
Counselor: Yeah, what do you do when you get angry?
Child: I don’t know (shrugs).
Mom: He hits. He wanted to go kick and hit the truck.
Counselor: You wanted to kick and hit the truck?
Child: (nods head)
Counselor: Did you do it?
Mom: No. Momma got a bruise from it (laughs, shows counselor her arm).
Counselor: How did momma get a bruise?
Mom: Trying to hold him back. But he was just swinging. He wanted to go hit the truck.
Child: Yeah.
Counselor: And then what did you do?
Mom: We did our breathing.
Counselor: You did your breathing? And then did you still want to hit the truck?
Mom: (Shakes head)
Child: (Nods head)
Counselor: You did?
Mom: But he didn’t swing so much.
Counselor: You weren’t swinging as much?
Mom: He kept saying it was bad, it was a bad truck.
This vignette illustrates how anger is often the main emotion rather than scared for young children. Furthermore Dylan’s physical enactment of his anger seemed to have more salience for him than cognitive mastery in the office exposures, which are not described here due to space.
His mother’s anxiety remained severe throughout treatment. At the start of treatment, she refused to drive herself or to go past the scene. She took alprazolam to enable herself to get in a taxi to come to the second session. Because she could not force herself to drive Dylan past the scene for homework exposure, she recruited her brother to drive them, but she still almost vomited. After Session 10, a minor vehicle collision occurred in front of their home. Dylan seemed fine with this unplanned naturalistic exposure, but the mom vomited in the house. Nevertheless, after Session 11 mom attempted to drive Dylan over the bridge herself, but she threw up and had to abort the attempt. The grandparents were able to step in and drove Dylan over the bridge multiple times. Despite this complication, Dylan’s symptomatology began improving dramatically after Session 8, as would be expected typically after several sessions of graded office and homework exposures (Figure 1). Posttreatment, his number of PTSD symptoms decreased to four, but his mother still had 14 PTSD symptoms.
Figure 1.
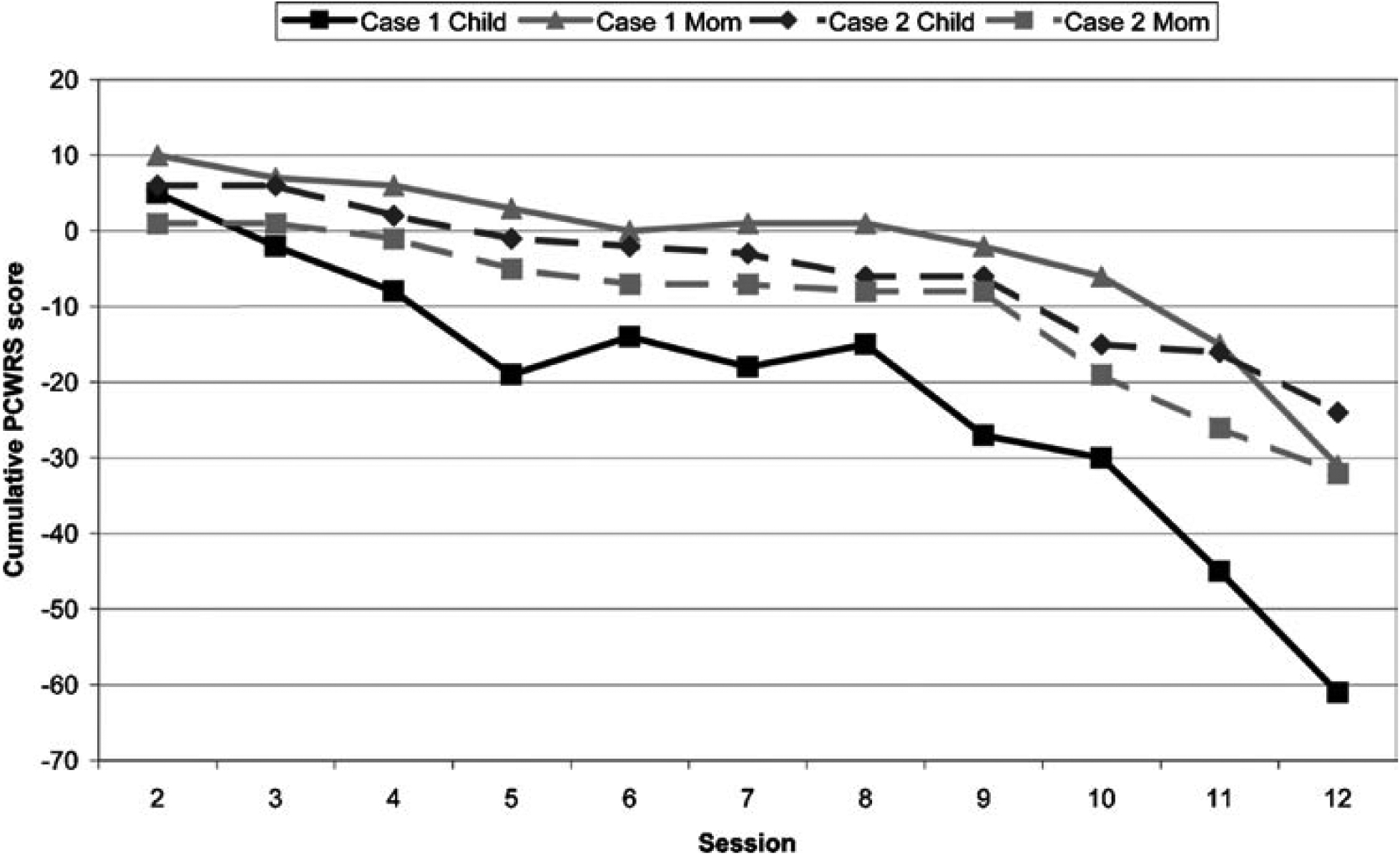
Session-by-session change in severity of posttraumatic symptomatology for the children and moms in Cases 1 and 2.
PCWRS=PTSD Parent–Child Weekly Rating Scale.
Case 2. Chris
Chris was 3 years 7 months old when Hurricane Katrina struck. Floodwater rose to the ceiling of the first floor of their house. The family spent two terrifying nights in a dark, hot, suffocating attic. They finally left in their own boat, slept one night on a highway, then spent two nights at the Convention Center before being evacuated by bus to Houston.
Chris met the modified criteria for PTSD in preschool children (Scheeringa et al., 2005). He had 6 items of PTSD, plus he started urinating on himself one week after the flood when they were in Houston and it lasted 2 months before spontaneously resolving. His 28-year-old mom demonstrated 8 of the symptoms of PTSD.
Chris was 4 years 1 month old when treatment started. Typical of most 4-year-old children, he had difficulty self-rating his negative feelings in the Session 3 exercises, but was quite capable of narrating key aspects of his story in Session 5. For example, he recalled that he was scared when he was responsible for holding their dog during the boat evacuation, a point that his mom had forgotten.
After the third week of exposure work (after Session 8), Chris had one recurrence of daytime enuresis, which made us question whether the pace of therapy was too fast. Rather than back down to a lower anxiety-provoking exposure, which could decrease the therapeutic potency, the next week’s homework (Session 9) was to go back to the gutted house for the first time, and we discussed with his mom ways to build in more comfort during the homework exposures. This exposure seemed successful for increasing his mastery of the anxiety and there were no recurrences of enuresis. In fact, his symptoms started to improve dramatically after this homework (Figure 1).
The transcript from Session 12 describes the homework exposure after Session 11. They were still not living in their old house, but their exposure task was to climb back into the attic of the gutted house for the first time. The child showed limited awareness that it was important in therapy to talk about the homework, or perhaps he was avoiding the topic, but it was evident that the homework exposure itself was enormously salient.
Counselor: Can you tell me about your homework? Where did you go?
Child: The blue house.
Mom: What did we do in the blue house?
Child: Sitting down.
Mom: Where were we sitting down?
Child: Up the stairs.
Mom: Where up the stairs?
Child: You were with me momma (implying that he didn’t want to be questioned when mom already knew the answers).
Counselor: Tell me. I wasn’t with you.
Mom: Tell her what happened.
Counselor: Did you sit on the stairs?
Child: Yeah.
Counselor: Did you feel scared?
Child: Yeah.
Counselor: Yeah? How scared? None, a little, or a whole lot scared?
Child: A whole lot scared.
Counselor: Whole lot scared. OK. I’m glad you can tell us you feel a whole lot scared.
Mom: We went in the attic.
Counselor: Can you tell me more about it?
Mom: When we first got there, he was alright. When we first sat upstairs in the attic, it was hot. I asked him was he scared. He was like no.
Counselor: Did he remember that? (meaning the original experience during the flood).
Mom: Well, I don’t know. So I asked dad to close the door. Some of the ceiling was gone so he could still watch us. So I asked him to close the stairs up. And I asked Chris, let’s practice your breathing in case you get scared you’ll know that you’ll be relaxed. I asked him to do that first. Then I asked him to close his eyes and picture us up in the attic in the darkness and he did that and I asked him was he scared. He said yes. We needed to end the exercise. I said let’s do your breathing.
Counselor: That’s right.
Mom: We did that for two cycles and that’s when we came down.
Counselor: OK. Was he scared afterwards, after he did it two times?
Mom: No. After we went downstairs and he was out of the attic he was OK with it.
Post-treatment, Chris’s number of PTSD symptoms had decreased to 2, and his mother decreased slightly to 6. Later, while noting with the mom that both she and Chris had improved with therapy, the counselor asked mom whether she felt that she improved first or if Chris improved first. The mom replied that once she saw that Chris had become calmer overall, then she was able to relax.
DISCUSSION
These two cases provide proof of concept from actual preschool children with PTSD that CBT techniques can be applied in a feasible and effective fashion for different types of life-threatening experiences. Even though young children are still developing the capacities to self-reflect and cooperate in treatment, they can engage in structured therapy, cooperate with exposure exercises, and voluntarily use relaxation techniques for a targeted end.
The traditional thinking about parent–child relationships is that mothers have to control their own anxieties to some degree to become better protective shields for their children, which will then enable children to control their own anxieties. However, these cases indicate that the children made improvements despite high ongoing anxiety levels in their moms. In one case, the mom reported directly that her child improved first, allowing her to calm down. This suggests that what counselors need to teach parents is not that parents need to relax per se, but that they need to endure their own anxiety enough to help their children to confront their fears. This then will help their children improve, which then will help the parents to relax.
In conclusion, PTSD in young children is too often underrecognized and ineffectively treated, but these cases provide some of the earliest evidence that an effective treatment modality exists and warrants wider implementation.
Contributor Information
Michael S. Scheeringa, Department of Psychiatry and Neurology, Tulane University, New Orleans, LA
Alison Salloum, School of Social Work, University of South Florida, Tampa, FL.
Ruth A. Arnberger, Department of Psychiatry and Neurology, Tulane University, New Orleans, LA
Carl F. Weems, Department of Psychology, University of New Orleans, New Orleans, LA
Lisa Amaya-Jackson, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center, Center for Child and Family Health, Durham, NC.
Judith A. Cohen, Department of Psychiatry, Drexel University College of Medicine, Allegheny General Hospital, Pittsburgh, PA
REFERENCES
- Cohen J, & Mannarino A (1996). A treatment outcome study for sexually abused preschool children: Initial findings. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 42–50. [DOI] [PubMed] [Google Scholar]
- Deblinger E, Stauffer L, & Steer R (2001).Comparative efficacies of supportive and cognitive behavioral group therapies for young children who have been sexually abused and their nonoffending mothers. Child Maltreatment, 6, 332–343. [DOI] [PubMed] [Google Scholar]
- Egger H, Ascher B, & Angold A (2002). Preschool Age Psychiatric Assessment. Durham, NC: Duke University Medical Center. [Google Scholar]
- March J, Amaya-Jackson L, & Murry M (1998). Cognitive–behavioral psychotherapy for children and adolescents with posttraumatic stress disorder after a single-incident stressor. Journal of the American Academy of Child and Adolescent Psychiatry, 37, 585–593. [DOI] [PubMed] [Google Scholar]
- Peebles C, & Scheeringa M (1996). PTSD Parent–Child Weekly Rating Scale. New Orleans, LA. [Google Scholar]
- Scheeringa M, Zeanah C, Myers L, & Putnam F (2005). Predictive validity in a prospective follow-up of PTSD in preschool children. Journal of the American Academy of Child and Adolescent Psychiatry, 44, 899–906. [DOI] [PubMed] [Google Scholar]


