Abstract
The aim of this study was to evaluate accuracy of seven commercial activity monitors in measuring steps in older adults with varying walking abilities and to assess monitor acceptability and usability. Forty-three participants (age = 87 ± 5.7 years) completed a gait speed assessment, two walking trials while wearing the activity monitors, and questionnaires about usability features and activity monitor preferences. The Accusplit AX2710 Accelerometer Pedometer had the highest accuracy (93.68% ±13.95%), whereas the Fitbit Charge had the lowest (39.12% ± 40.3%). Device accuracy varied based on assistive device use, and none of the monitors were accurate at gait speeds <0.08 m/s. Barriers to monitor usability included inability to apply monitor and access the step display. Monitor accuracy was rated as the most important feature, and ability to interface with a smart device was the least important feature. This study identified the limitations of the current commercial activity monitors in both step counting accuracy and usability features for older adults.
Keywords: accuracy, gait speed, pedometer, step count, walking
Physical activity is an essential part of healthy aging given the widespread, well-documented benefits for older adults (DiPietro, 2001). Despite this, older adults are the least likely group to achieve physical activity recommendations and spend the most time in sedentary behavior (Seguin et al., 2012). Commercial activity monitors that count steps may be effective in measuring and promoting physical activity in older adults as walking is a common form of exercise and light activity in this age group (Cavanaugh, Coleman, Gaines, Laing, & Morey, 2007). In addition, the knowledge of daily steps can assist older adults with behavioral change by promoting objective physical activity goals (Croteau, Richeson, Farmer, & Jones, 2007; Pelssers et al., 2013; Rosenberg et al., 2012; Talbot, Gaines, Huynh, & Metter, 2003).
Although commercial activity monitors could promote physical activity in older adults, there are several gaps in the current knowledge related to the accuracy of the monitors in counting steps. Previous studies have examined the ability of activity monitors to count steps in adults during treadmill walking (Chow, Thom, Wewege, Ward, & Parmenter, 2017; Wong, Mentis, & Kuber, 2018) or at controlled walking speeds (Singh, Farmer, Van Den Berg, Killington, & Barr, 2016), which may be different than walking over ground at an individual’s usual, selfselected gait speed (Watt et al., 2010). In addition, activity monitor validation studies in older adults have not evaluated accuracy of commonly used wrist- and shirt-worn activity monitors (Martin, Krc, Mitchell, Eng, & Noble, 2012; Webber, Magill, Schafer, & Wilson, 2014), and few studies have included older adults who use an assistive device for walking, such as a wheeled walker (Paul et al., 2015; Treacy et al., 2017; Webber et al., 2014). Finally, little is known about the usability features of the monitors and the activity monitor preferences of older adults, which are important considerations given the expectation of daily wear for physical activity promotion.
In the present report, we sought to determine the accuracy of a variety of commercially available activity monitors in measuring steps in older adults who have a range of walking speeds, to determine the accuracy of the activity monitors in measuring steps in older adults who use assistive devices for walking and those who do not use assistive devices, and to assess participants’ ratings of usability features of the activity monitors utilized in the study. We also examined the preferred characteristics of activity monitors for older adults.
Methods
Overview
This cross-sectional study assessed the accuracy of commercially available activity monitors in counting steps during walking at usual gait speed and examined the usability features of the monitors for older adults.
Subjects and Settings
Participants were recruited through informational sessions conducted at four independent living communities in the greater Pittsburgh area. After each session, interested individuals were invited to meet with an investigator to learn about the study in greater detail and schedule a study visit. To be eligible for the study, individuals had to be 65 years of age or older, be able to walk at least 100 feet with or without an assistive device, and demonstrate the ability to correctly answer basic questions about the study (study purpose and benefits/risks of study). All study visits were conducted onsite at each of the independent living communities and were administered by the principal investigator and members of the investigative team. The University of Pittsburgh Institutional Review Board approved the study, and all participants provided written informed consent before participation.
Self-Report Measures
The participants were asked about demographics; comorbid health conditions (Rigler, Studenski, Wallace, Reker, & Duncan, 2002); and use of an assistive device for walking.
Gait Speed
All participants completed an initial assessment of gait speed determined by recording the time it took for each participant to walk the central 4 m of an 8-m course at their usual pace. The gait speed was calculated as the distance (4 m) divided by the time it took to complete the 4-m walk in seconds, as meters per second (m/s) (Peel, Kuys, & Klein, 2013).
Activity Monitors
Each participant wore up to eight physical activity monitors (seven different models with one model worn at two locations) for this study. The seven models used were the Fitbit Charge (Fitbit Inc., San Francisco, CA); Garmin Vivofit (Garmin Ltd., Schaffhausen, Switzerland); Fitbit Zip (Fitbit Inc., San Francisco, CA); Yamax SW-200 Digiwalker Pedometer (Yamasa Tokei Keiki Co., Ltd., Tokyo, Japan); Accusplit AX2710 Accelerometer Pedometer (Accusplit, Inc., Livermore, CA); Yamax EX-510 Pedometer (Yamasa Tokei Keiki Co., Ltd., Tokyo, Japan); and Omron HJ- 321 Pedometer (Omron Healthcare, Inc., Lake Forest, IL). The last two devices (Yamax EX-510 and Omron HJ-321) were added during the course of the study and thus were not worn by the first 13 participants. These seven models were selected because they were widely commercially available at the time and represent a range of cost, wear locations, and usability features (Table 1). Prior to the walking tests, activity monitors were placed in a standardized manner across participants following instructions recommended by the manufacturer. The Fitbit Charge and the Garmin Vivofit were worn on separate wrists with the Fitbit Charge always worn on the participant’s dominant arm and the Garmin Vivofit worn on the opposite arm for consistency. The Fitbit Zip was attached to the shirt pocket or collar at the participant’s neckline. The Digiwalker, Accupslit, Omron, Yamax EX-510, and a second Fitbit Zip were positioned at waist level close to the anterior aspect of the thigh, but not in contact with each other, using an adjustable belt.
Table 1.
Features of the Activity Monitors
| Activity monitor | Measures | Wear location | Cost | Mechanism | Power source | Synching capability |
|---|---|---|---|---|---|---|
| Fitbit Charge | S, D, C, SL, AM, AL | Wrist | High | Accel | Rechargeable battery | X |
| Garmin Vivofit | S, D, C | Wrist | Mid | Accel | Long-term battery | X |
| Fitbit Zip | S, D, C, AM | Waist, shirt | Mid | Accel | Rechargeable battery | X |
| Yamax SW-200 Digiwalker | S | Waist | Low | Spring | Long-term battery | |
| Accusplit Accelerometer Pedometer | S | Waist | Low | Accel | Long-term battery | |
| Omron Pedometer | S, D, C | Waist, pocket | Low | Accel | Long-term battery | |
| Yamax EX-510 Pedometer | S, D, C | Waist, pocket | Low | Accel | Long-term battery |
Note. S = steps; D = distance; C = calories; SL = sleep; AM = activity minutes; AL = altimeter; Low = <$50.00; Mid = $50.00–100.00; High = >$100.00; Accel = accelerometer; Spring = spring-lever mechanism.
100-Step Walking Test
Each participant completed two 100-step walking tests over ground while wearing all activity monitors simultaneously. For each test, participants were asked to walk 100 steps on a level surface at their usual walking pace. One investigator walked to the side and slightly behind the participant to count steps using a handheld step counter, and a second investigator was positioned on the other side of the participant to verify the step count. After the first walking test, the participant was asked to sit for 2 min while step counts were recorded from each device and the step counters were reset to zero. The procedure was repeated a second time. The accuracy was computed for each trial and also both trials combined as the percentage of investigator-counted steps that were identified by the physical activity monitor (accuracy = 100 × monitor steps/observed steps). If a monitor identified more steps than the investigator, the accuracy was penalized by subtracting the extra percentage of steps from 100%.
Usability Ratings for the Activity Monitors
After the walking trials, participants completed a questionnaire administered by the research team to assess the activity monitor usability features. The participant was provided with each activity monitor and asked to rate the usability features of the device on a scale from 1 (worst) through 5 (best). The following features were assessed: ease in applying the monitor, ease in reading the step display, comfort, and ease in accessing steps on the monitor. Participants were asked to try each feature on the monitor prior to rating the usability of the feature.
General Preferences for Activity Monitors
Using a questionnaire, participants were provided with a list of general activity monitor features and asked to rate the important features based on their personal preferences on scale from 1 (least important) to 5 (most important). The features included the accuracy of the monitor, ease with monitor application, ability to read the step display, comfort, ability to access step display, cost, power source (rechargeable battery or long-term battery), wear location, size, appearance, and ability of the monitor to synch with a smart device for added features.
Data Analyses
Appropriate summary statistics were computed to describe the participant characteristics of the sample. Accuracy was summarized both overall and by assistive device use (used assistive device and did not use assistive device) and by clinically meaningful gait speed categories (<0.6 m/s, 0.6–0.79 m/s, 0.8–1.0 m/s, and >1.0 m/s) (Cesari et al., 2005). Acceptable accuracy was defined as the activity monitor capturing ≥97% of observed steps based on industry standards (Hatano, 1993). To examine activity monitor usability ratings, the percentage of subjects indicating a favorable rating (a 4 or 5 on a scale from 1 to 5) for each feature was calculated. To determine general activity monitor preferences, mean scores were calculated for each feature based on participant ratings on a scale from 1 (least favorable) to 5 (most favorable).
Results
Based on eligibility criteria, 44 participants were recruited for the study, and of these, 43 individuals consented (M ± SD; age 87 ±5.7 years). One participant was deemed ineligible due to inability to understand the study purpose during the informed consent process. Characteristics of the participants are listed in Table 2. Participants were predominantly female (81%) and White (100%) with the majority (97.7%) completing high school. The mean body mass index was 26.1 ± 4.1 kg/m2. Average gait speed was 0.84 ± 0.24 m/s, and 21 participants (49%) used an assistive device for walking. Participants had an average of three comorbid health conditions with the most common domains being visual/hearing (98%); followed by musculoskeletal (84%); and other general (i.e., sleep, pain; 35%) health conditions.
Table 2.
Participant Characteristics (n = 43)
| Characteristic | M ± SD (Range) or n (%) |
|---|---|
| Age (years) | 86.7 ± 5.7 (69–98) |
| Female | 35 (81.4%) |
| Race | |
| White | 43 (100.0%) |
| Education | |
| elementary | 1 (2.3%) |
| high school | 23 (53.5%) |
| college | 16 (37.2%) |
| postgraduate | 3 (7.0%) |
| Comorbid conditions | |
| number of comorbidities | 3.0 ± 1.2 (1–6) |
| Comorbidity domains | |
| cardiovascular | 7 (16.3%) |
| neurological | 7 (16.3%) |
| musculoskeletal | 36 (83.7%) |
| general | 15 (34.9%) |
| visual/hearing | 42 (97.7%) |
| diabetes | 8 (18.6%) |
| cancer | 10 (23.3%) |
| lung | 5 (11.6%) |
| Height (m) | 1.61 ± 0.09 |
| Weight (kg) | 68.3 ± 13.4 |
| Body mass index (kg/m2) | 26.1 ± 4.1 |
| Gait speed (m/s) | 0.84 ± 0.24 |
| Assistive device | |
| no device | 22 (51.2%) |
| cane | 4 (9.3%) |
| wheeled walker/rollator | 17(39.5%) |
Accuracy of the Activity Monitors
Figure 1 summarizes the overall accuracy of the activity monitors. The Accusplit AX2710 Accelerometer Pedometer had the highest accuracy (93.68% ± 13.95%), followed by the Fitbit Zip worn at the waist (75.25% ± 35.56%), the Omron Pedometer (71.71% ±38.01%), the Yamax EX-510 Pedometer (71.01% ± 35.0%), the Fitbit Zip worn at the shirt collar or pocket (69.8% ± 40.35%), the Garmin Vivofit (56.95% ± 46.54%), the Digiwalker (52.83% ±37.73%), and the Fitbit Charge (39.12% ± 40.3%).
Figure 1 —
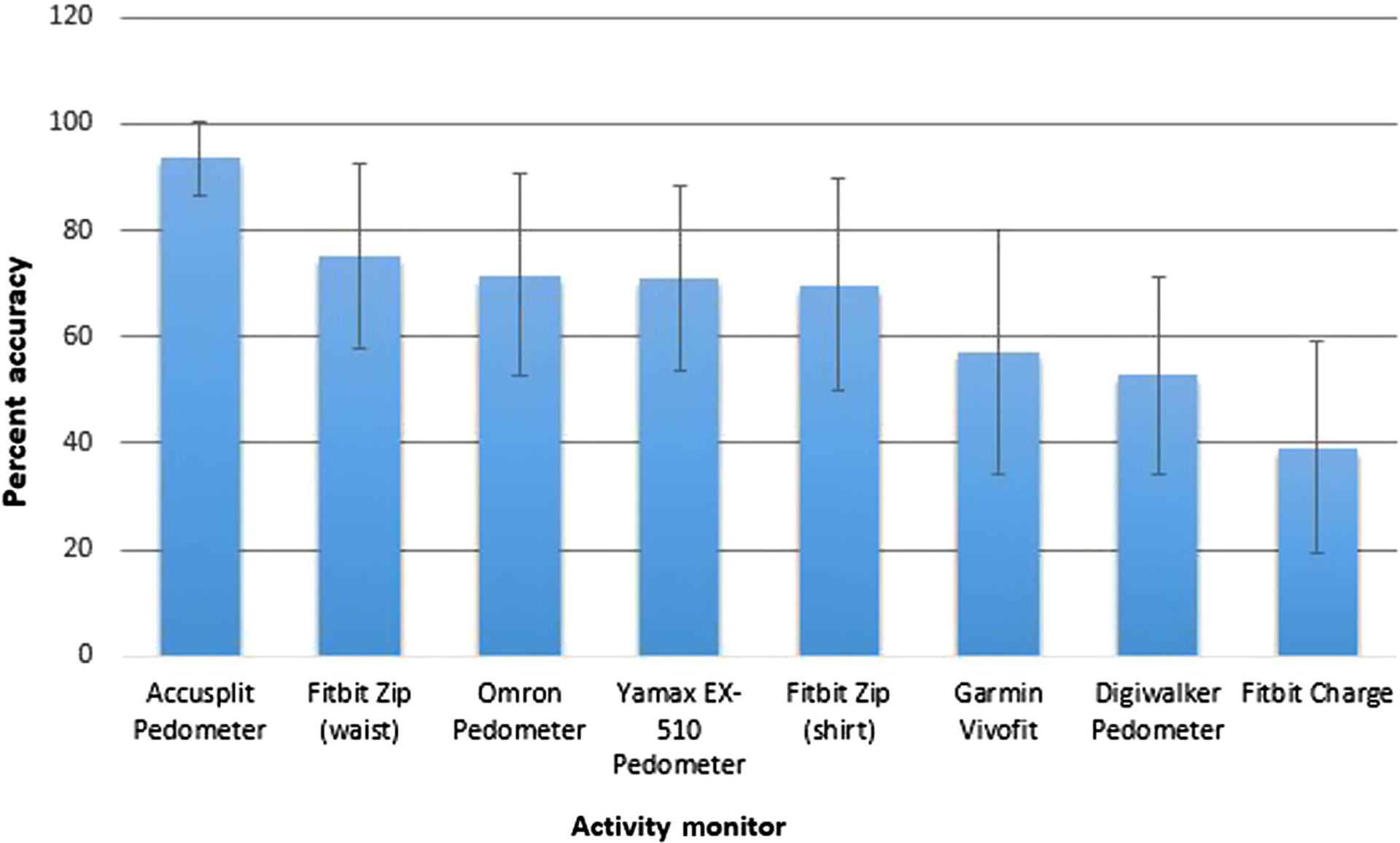
Overall percentage accuracya of activity monitors. aAccuracy was defined as monitor steps/observed steps × 100 with 100% indicating perfect accuracy.
Accuracy of Activity Monitor by Assistive Device Use
Table 3 summarizes the accuracy of the activity monitors stratified by assistive device use. Monitor accuracy varied based on assistive device use with a range of 64.12% ± 33.04% to 97.15% ± 7.44% in those not utilizing an assistance device (n = 22) and a range of 12.93% ± 29.27% to 90.04% ± 17.98% in those who used an assistive device (n = 21). None of the activity monitors were ≥97% accurate in counting steps in those who used an assistive device such as a cane, wheeled walker, or rollator. Only the Accusplit was ≥97% accurate in counting steps in those who walked without an assistive device.
Table 3.
Percentage Accuracy of Activity Monitors Stratified by Assistive Device Use
| Activity Monitor | Did Not Use Assistive Device | Used Assistive Device |
|---|---|---|
| Mean gait speed = 0.98 m/s | Mean gait speed = 0.70 m/s | |
| n = 22 | n = 21 | |
| Wrist-worn monitors | ||
| Fitbit Charge | 64.12 (33.04) | 12.93 (29.27) |
| Garmin Vivofit | 93.82 (8.23) | 18.33 (37.62) |
| Shirt-worn monitors | ||
| Fitbit Zip | 84.19 (30.07) | 54.73 (44.77) |
| Waist-worn monitors | ||
| Fitbit Zip | 89.56 (21.82) | 60.26 (41.16) |
| Digiwalker Pedometer | 74.03 (30.53) | 30.61 (31.58) |
| Accusplit Accelerometer Pedometer | 97.15 (7.44) | 90.04 (17.98) |
| Omron Pedometer | 88.35 (24.43) | 58.99 (42.11) |
| Yamax EX-510 Pedometer | 95.23 (8.00) | 52.48 (36.47) |
Note. Accuracy was defined as monitor steps/observed steps × 100 with 100% indicating perfect accuracy. Bolded value is ≥97% accurate. Data are represented as M (SD).
Accuracy of Activity Monitor by Gait Speed Category
Table 4 summarizes the accuracy of the activity monitors based on gait speed category. None of the activity monitors were accurate at gait speeds <0.8 m/s. Only the Accusplit was ≥97% accurate at gait speeds between 0.8 and 1.0 m/s, and only the Fitbit Zip, Accusplit, Omron, and Yamax EX-510 were ≥97% accurate at gait speeds >1.0 m/s. After the removal of the one participant using an assistive device in the >1.0 m/s gait speed category, the accuracy of the Garmin Vivofit increased to ≥97% accuracy.
Table 4.
Percentage Accuracy of Activity Monitors Stratified by Gait Speed Category
| Activity Monitor | <0.6 m/s | 0.60–0.79 m/s | 0.8–1.0 m/s | >1.0 m/s | >1.0 m/s (No ADa) |
|---|---|---|---|---|---|
| n = 7 | n = 12 | n = 11 | n = 13 | n = 12 | |
| Wrist-worn monitors | |||||
| Fitbit Charge | 5.85 (10.19) | 16.66 (37.80) | 43.40 (34.84) | 74.14 (28.54) | 80.32 (18.63) |
| Garmin Vivofit | 26.15 (44.75) | 45.78 (46.91) | 50.01 (48.31) | 89.73 (27.03) | 97.20 (2.08) |
| Shirt-worn monitors | |||||
| Fitbit Zip | 12.49 (19.33) | 56.37 (40.70) | 86.94 (29.65) | 98.56 (0.76) | 98.48 (0.73) |
| Waist-worn monitors | |||||
| Fitbit Zip | 28.09 (29.65) | 25.30 (36.90) | 87.55 (29.53) | 98.90 (0.67) | 98.81 (0.61) |
| Digiwalker Pedometer | 21.59 (28.46) | 38.22 (35.29) | 51.00 (33.53) | 89.33 (13.84) | 89.81 (14.43) |
| Accusplit Accelerometer Pedometer | 74.75 (25.33) | 95.19 (9.71) | 97.58 (4.16) | 99.17 (1.17) | 99.14 (1.21) |
| Omron Pedometer | 11.76 (18.56) | 80.78 (25.42) | 82.69 (31.20) | 99.16 (0.84) | 99.16 (0.84) |
| Yamax EX-510 Pedometer | 16.13 (23.87) | 81.38 (14.78) | 75.35 (31.58) | 98.87 (0.89) | 98.87 (0.89) |
Note. Accuracy was defined as monitor steps/observed steps × 100 with 100% indicating perfect accuracy. Bold values are ≥97% accurate. Data are presented as M (SD). AD = assistive device.
Percentage accuracy with the one participant who used a wheeled walker was removed.
Usability Ratings for the Activity Monitors
Figure 2 summarizes the percentage of participants who provided a favorable usability rating (rating of a 4 or 5 on a 5-point Likert scale) for the following categories: Easy to Apply Monitor, Easy to Read Steps, Comfortable to Wear, and Easy to Access Steps. In the “Easy to Apply Monitor” category, the majority of the monitors (five out of seven) received a low percentage (<75%) of favorable ratings. All monitors received a high percentage (>75%) of favorable ratings for “Easy to Read Steps” and four of the seven monitors received a high percentage (>75%) of favorable ratings for the “Comfortable to Wear” category. The Yamax EX-510 activity monitor received the highest percentage of favorable ratings in all categories, whereas the Garmin Vivofit received the lowest percentage of favorable ratings for three of the four categories (Easy to Apply, Easy to Read, and Comfortable). The Yamax Digiwalker received the lowest percentage (20%) of favorable ratings for the category of “Easy to Access Steps.”
Figure 2 —
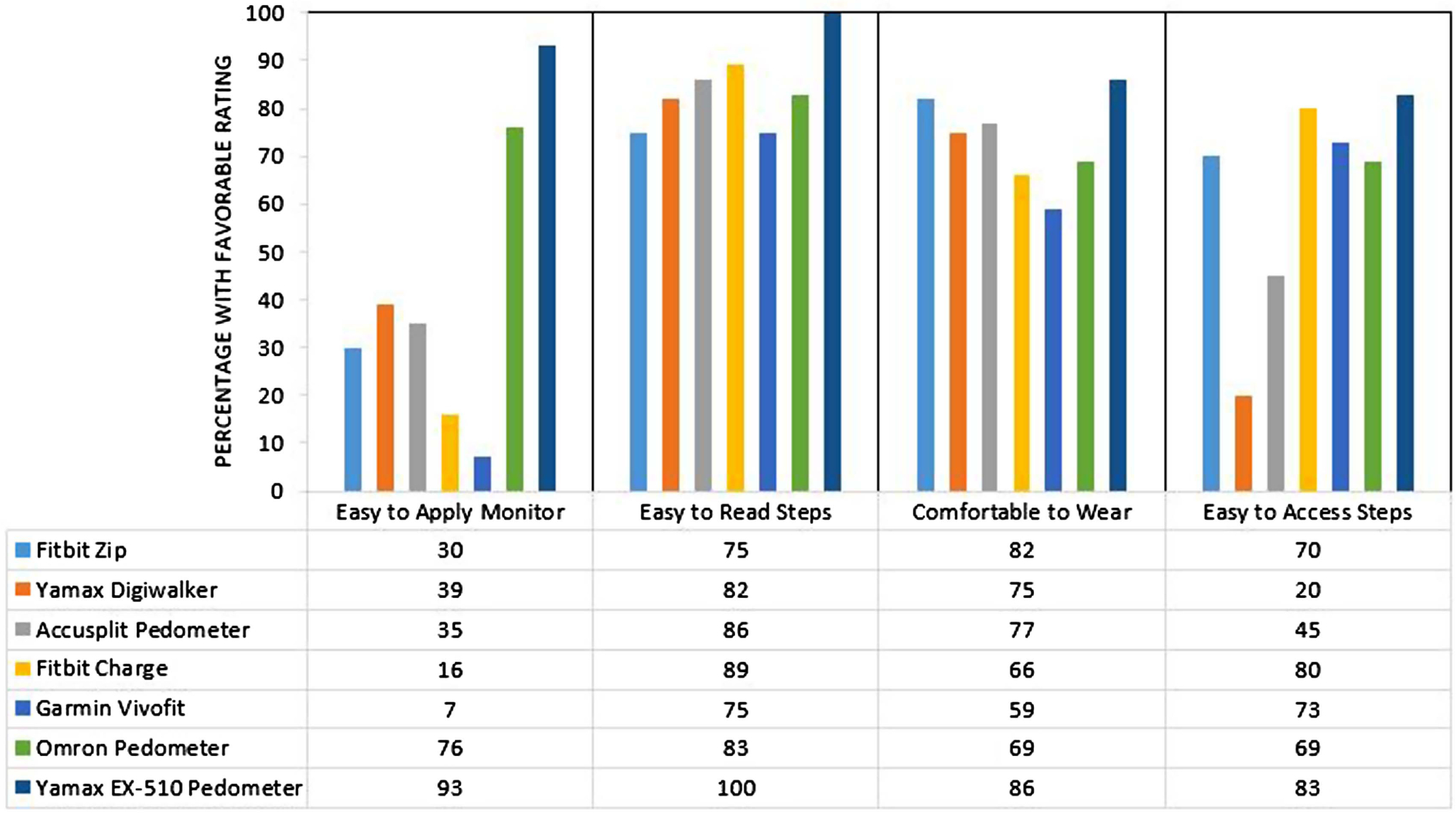
Percent of participants reporting a favorable usability rating for the activity monitor. Favorable rating = rating of a 4 or 5 on a 5-point Likert scale.
Important Features of Activity Monitors
Figure 3 summarizes participant ratings of important general features of activity monitors. Participants rated accuracy of the activity monitor as the most important feature (4.68 out of 5), followed by easy to apply monitor (4.67 out of 5), and easy to read steps (4.65 out of 5). Participants rated the ability of the activity monitor to synch with a smart device as the least important feature (1.19 out of 5).
Figure 3 —
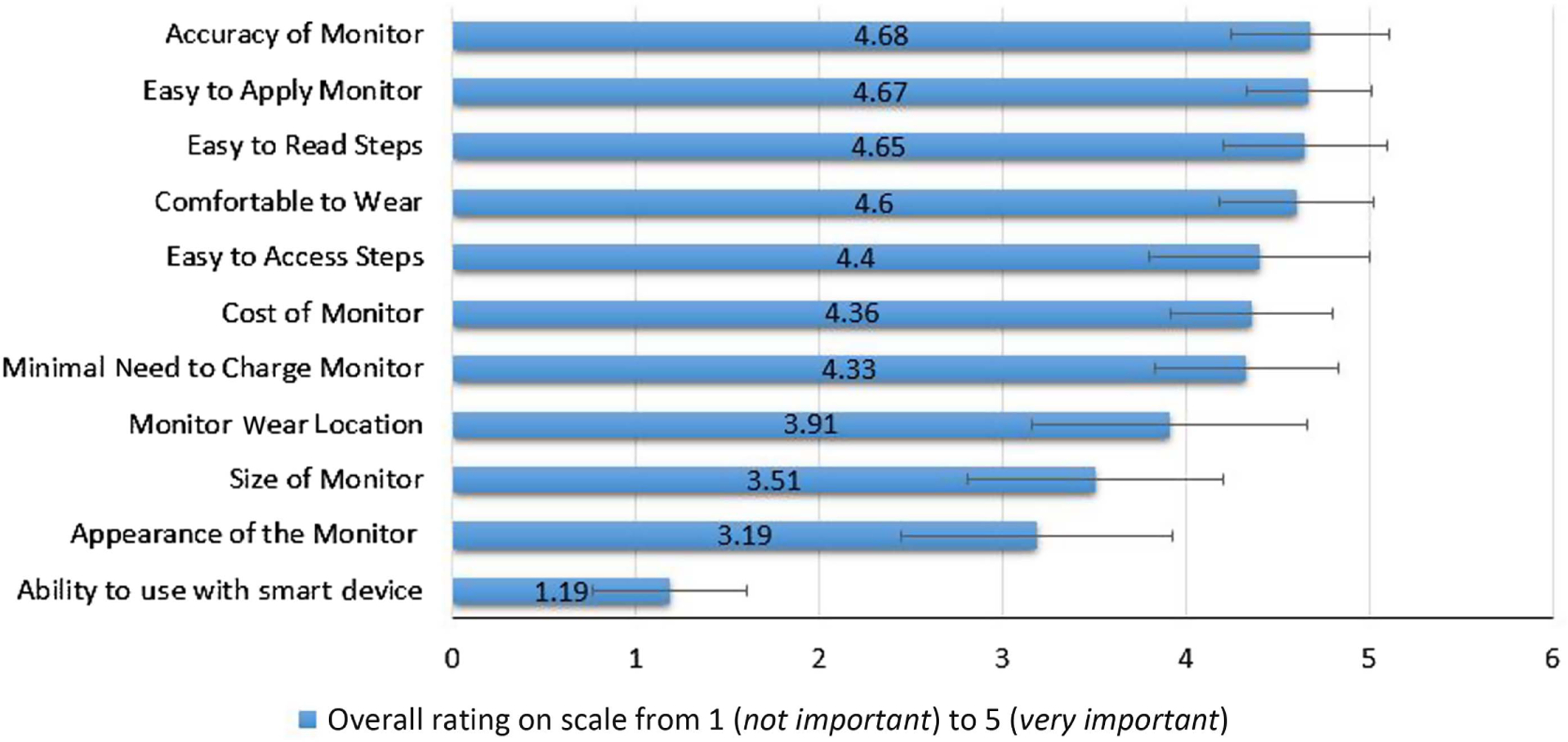
Important features of activity monitors based on participant ratings (mean rating).
Discussion
In this study of older adults, the accuracy of the commercially available activity monitors for counting steps ranged from 39% to 94%; thus, none of the monitors met the standard of having less than a 3% margin of error in step counting accuracy (Hatano, 1993). The Accusplit Accelerometer Pedometer, a “low-cost,” accelerometry-based, waist-worn monitor, was the most accurate of the seven monitors studied, and the Fitbit Charge, a “high-cost,” wrist-worn monitor, was the least accurate.
Activity monitors accuracy varied by use of assistive device. None of the activity monitors were ≥97% accurate in counting steps in those who used an assistive device such as a wheeled walker, rollator, or cane for walking. Furthermore, only the Accusplit Accelerometer Pedometer was accurate in counting steps in those who walked without an assistive device. The wrist-worn monitors (Fitbit Charge and Garmin Vivofit) were found to be least accurate in counting steps in those who used an assistive device and tended to grossly underestimate steps in this group by >80%. Treacy et al.(2017) reported similar findings of decreased accuracy of wrist- worn monitors in those who utilized an assistive device in a study of 166 patients in rehabilitation. Wrist-worn monitor accuracy may be impacted by the stationary placement of the upper extremity on an assistive device such as a wheeled walker, which likely impedes the device in detecting stepping motion and thus leads to a slower than those who do not use a device, which was the case in the current study. Thus, it is likely that the lack of upper extremity movement, as well as slow gait speed, influence monitor accuracy in those who use an assistive device. In those who use an assistive device for walking, wear location of the activity monitor must be considered with greater consideration given to monitors worn at the waist.
Accuracy of the monitors varied with gait speed with improved accuracy in those who walked at faster speeds. None of the activity monitors were able to count steps with sufficient accuracy in those who walked the slowest (<0.8 m/s), and most monitors significantly undercounted steps by >50% in these slower walkers. Only one of the seven monitors (Accusplit) was >97% accurate in those who walked at speeds 0.8–1.0 m/s, ad just four of the seven monitors (Fitbit Zip worn at either location, Accusplit, Omron, and Yamax EX-510) were accurate in those who walked >1.0 m/s. These findings are in agreement with other studies that have reported decreased accuracy of activity monitors in counting steps in those who walk slowly. The current study adds to these findings by reporting on the accuracy of wrist-worn devices and includes a sample of older adults who walk at slower gait speeds (Melanson et al., 2004; Storti et al., 2008). It is worth noting that the Accusplit Accelerometer Pedometer, a low-cost commercially available activity monitor, was shown to be highly accurate in those who walk at least 0.8 m/s, which is similar in accuracy to high-cost, research-grade activity monitors (Cindy Ng, Jenkins, & Hill, 2012; Grant, Dall, Mitchell, & Granat, 2008). Given the high accuracy and low cost of this monitor, the Accusplit is well suited for use by clinicians who wish to increase physical activity in older adults through the promotion of daily step counting.
Our study highlights the importance of considering the activity monitor wear location, walking speed, and assistive device use in older adults when choosing a device to monitor steps. In the faster walkers (>1.0 m/s), waist- and shirt-worn accelerometry-based monitors were more accurate in counting steps than wrist-worn monitors. However, when monitor accuracy in this walking category was examined only in those who walk without an assistive device, the accuracy of the wrist-worn Garmin Vivofit increased from 89.73% to 97.20%. This finding suggests that the use of an assistive device such as a walker in those who walk at faster gait speeds might reduce monitor accuracy and reinforces the notion that both assistive device use and gait speed exert an influence on monitor accuracy.
This study is the first to our knowledge to assess usability ratings of various activity monitors in older adults. We found most monitors were rated favorably by participants for ease in reading steps and comfort; however, participants rated most monitors as hard to apply and difficult to access the step count. Participants rated pedometers that attached with a leash cord and metal clip at the waist or pocket as most favorable for application, whereas the wrist-worn monitors were rated least favorable for application. Specifically, participants reported difficulty with applying the wrist-worn monitors and reported a preference for a wristband that required less adjustment and finger dexterity similar to a stretchable watchband. In addition, participants were noted to have difficulty with application of monitors that required management of a tight clip on the device for securing the monitor to the waist and were unable to access the step display in the pedometers that required the opening of a pedometer case to view step display. Because self-monitoring of steps depends on habitual use, these preferences should be considered in the selection and future design of activity monitors for older adults.
Little is known about activity monitor features that are important to older adults and about the particular characteristics that may promote daily wear of the monitor for physical activity adoption. This study revealed that monitor accuracy was the most important feature, followed by ease in applying the monitor and ease in reading the step display. In contrast, our study revealed the least important feature of the activity monitors was the ability to interface with smart device. This finding suggests that the relatively simple “pedometer-style” activity monitors may be more appealing to older adults in spite of the trend for development of more sophisticated activity monitors that feature additional monitoring capabilities and software features.
The Yamax EX-510 pedometer was rated the highest in usability ratings, and this monitor features attachment with a leash cord and metal clip (vs. band or clip located on the monitor). In addition, the step display on this pedometer is readily available on the front of the device eliminating the need to open a case or scroll through various activity settings to access the step display. Thus, to promote more widespread adoption of activity monitors for promoting physical activity in older adults, future devices should feature simplified application features that take into account decreased hand dexterity and strength in older adults while allowing for easier access to the step display.
This study has several limitations including a small number of participants in some of the walking speed groups and the precision of our mean accuracy estimates may be less in those groups. The entire sample of participants was White, and the participants were predominantly female; therefore, our findings may not be generalizable to other populations. In addition, in monitors that consider individual characteristics of the wearer (i.e., stride length, height, and weight), we did not adjust the settings of the activity monitors for each participant. Adjusting the settings of the activity monitor may have had an influence on monitor accuracy; however, resulting errors would likely have a larger impact on other measures such as distance or energy expenditure, which were not assessed in this study. The activity monitors were presented to participants in a standardized order during testing of usability features, which may have resulted in participants providing less feedback on the later monitors due to fatigue. Finally, the criterion of 97% for acceptable accuracy was derived as a Japanese standard from a manufacturing and quality control perspective (Yamasa Tokei Keiki Co., Ltd., Tokyo, Japan). The same standard may not be appropriate from a user perspective.
Despite these limitations, our study had several strengths. We used a variety of widely available activity monitors that varied in appearance, wear location, and features. Participants represented a range of walking abilities. We solicited direct feedback from the older adults about what features of the activity monitors were important to them, which could provide essential information for individuals seeking to encourage walking activity in this population through self-monitoring of steps.
Conclusion
Commercial activity monitors have suboptimal accuracy in counting steps in older adults who walk slowly and/or use an assistive device. Of the activity monitors examined in this study, a low-cost pedometer was the most accurate for counting steps in older adults with a range of walking abilities. Wrist-worn monitors considerably undercounted steps in those who used an assistive device for ambulation. The choice of an activity monitor and wear location should be guided by the specific characteristics of the individual or group and must consider the use of an assistive device for walking and gait speed. Common barriers to activity monitor usability are the inability to apply the monitor and difficulty accessing the step display. In older adults, the ideal activity monitor is one that is accurate, easy to apply, and allows the individual to access step count without difficulty. Our results highlight the limitations of the current commercial activity monitors in both step counting accuracy and usability features for older adults.
Acknowledgments
This work was supported by the Central Research Development Fund at University of Pittsburgh, 5P30 AG024827 University of Pittsburgh Claude E. Pepper Older Americans Independence Center, and NIA K24 AG057728 Midcareer Investigator Award in Translational Patient-Oriented Research in Aging. Bethany Barone Gibbs has received grant funding to her institution from Humanscale.
References
- Cavanaugh JT, Coleman KL, Gaines JM, Laing L, & Morey MC (2007). Using step activity monitoring to characterize ambulatory activity in community-dwelling older adults. Journal of the American Geriatrics Society, 55(1), 120–124. PubMed ID: 17233695 doi: 10.1111/j.1532-5415.2006.00997.x [DOI] [PubMed] [Google Scholar]
- Cesari M, Kritchevsky SB, Penninx BW, Nicklas BJ, Simonsick EM, Newman AB, … Pahor M (2005). Prognostic value of usual gait speed in well-functioning older people—Results from the health, aging and body composition study. Journal of the American Geriatrics Society, 53(10), 1675–1680. PubMed ID: 16181165 doi: 10.1111/j.1532-5415.2005.53501.x [DOI] [PubMed] [Google Scholar]
- Chow JJ, Thom JM, Wewege MA, Ward RE, & Parmenter BJ (2017). Accuracy of step count measured by physical activity monitors: The effect of gait speed and anatomical placement site. Gait & Posture, 57, 199–203. PubMed ID: 28666177 doi: 10.1016/j.gaitpost.2017.06.012 [DOI] [PubMed] [Google Scholar]
- Cindy Ng LW, Jenkins S, & Hill K (2012). Accuracy and responsiveness of the stepwatch activity monitor and ActivPAL in patients with COPD when walking with and without a rollator. Disability and Rehabilitation, 34(15), 1317–1322. PubMed ID: 22200080 doi: 10.3109/09638288.2011.641666 [DOI] [PubMed] [Google Scholar]
- Croteau KA, Richeson NE, Farmer BC, & Jones DB (2007). Effect of a pedometer-based intervention on daily step counts of community-dwelling older adults. Research Quarterly for Exercise and Sport, 78(5), 401–406. PubMed ID: 18274211 doi: 10.1080/02701367.2007.10599439 [DOI] [PubMed] [Google Scholar]
- DiPietro L (2001). Physical activity in aging: Changes in patterns and their relationship to health and function. The Journals of Gerontology: Series A, 56(Suppl. 2), 13–22. doi: 10.1093/gerona/56.suppl_2.13 [DOI] [PubMed] [Google Scholar]
- Grant PM, Dall PM, Mitchell SL, & Granat MH (2008). Activitymonitor accuracy in measuring step number and cadence in community-dwelling older adults. Journal of Aging and Physical Activity, 16(2), 201–214. doi: 10.1123/japa.16.2.201 [DOI] [PubMed] [Google Scholar]
- Hatano Y (1993). Use of the pedometer for promoting daily walking exercise. Journal of the International Committee on Health, Physical Education and Recreation, 29(4), 4–8. [Google Scholar]
- Martin JB, Krc KM, Mitchell EA, Eng JJ, & Noble JW (2012).Pedometer accuracy in slow walking older adults. International Journal of Therapy & Rehabilitation, 19(7), 387–393. doi: 10.12968/ijtr.2012.19.7.387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melanson EL, Knoll JR, Bell ML, Donahoo WT, Hill J, Nysse LJ, … Levine JA (2004). Commercially available pedometers: considerations for accurate step counting. Preventive Medicine, 39(2), 361–368. PubMed ID: 15226047 doi: 10.1016/j.ypmed.2004.01.032 [DOI] [PubMed] [Google Scholar]
- Paul SS, Tiedemann A, Hassett LM, Ramsay E, Kirkham C, Chagpar S, & Sherrington C (2015). Validity of the Fitbit activity tracker for measuring steps in community-dwelling older adults. BMJ Open Sport & Exercise Medicine, 1(1), e000013. doi: 10.1136/bmjsem-2015-000013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peel NM, Kuys SS, & Klein K (2013). Gait speed as a measure in geriatric assessment in clinical settings: A systematic review. The Journals of Gerontology, Series A: Biological Sciences and Medical Science, 68(1), 39–46. doi: 10.1093/gerona/gls174 [DOI] [PubMed] [Google Scholar]
- Pelssers J, Delecluse C, Opdenacker J, Kennis E, Van Roie E, & Boen F (2013). “Every step counts!”: Effects of a structured walking intervention in a community-based senior organization. Journal of Aging and Physical Activity, 21(2), 167–185. PubMed ID:22898451doi: 10.1123/japa.21.2.167 [DOI] [PubMed] [Google Scholar]
- Rigler SK, Studenski S, Wallace D, Reker DM, & Duncan PW (2002). Co-morbidity adjustment for functional outcomes in community-dwelling older adults. Clinical Rehabilitation, 16(4), 420–428. PubMed ID: 12061477 doi: 10.1191/0269215502cr515oa [DOI] [PubMed] [Google Scholar]
- Rosenberg DE, Kerr J, Sallis JF, Norman GJ, Calfas K, & Patrick K (2012). Promoting walking among older adults living in retirement communities. Journal of Aging and Physical Activity, 20(3), 379– 394. PubMed ID: 22186798 doi: 10.1123/japa.20.3.379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seguin R, Lamonte M, Tinker L, Liu J, Woods N, Michael YL, … Lacroix AZ (2012). Sedentary behavior and physical function decline in older women: Findings from the women’s health initiative. Journal of Aging Research, 2012, 271589 PubMed ID: 22675631 doi: 10.1155/2012/271589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh AK, Farmer C, Van Den Berg ML, Killington M, & Barr CJ (2016). Accuracy of the FitBit at walking speeds and cadences relevant to clinical rehabilitation populations. Disability and Health Journal, 9(2), 320–323. PubMed ID: 26905972 doi: 10.1016/j.dhjo.2015.10.011 [DOI] [PubMed] [Google Scholar]
- Storti KL, Pettee KK, Brach JS, Talkowski JB, Richardson CR,& Kriska AM (2008). Gait speed and step-count monitor accuracy in community-dwelling older adults. Medicine & Science in Sports & Exercise, 40(1), 59–64. PubMed ID: 18091020 doi: 10.1249/mss. 0b013e318158b504 [DOI] [PubMed] [Google Scholar]
- Talbot LA, Gaines JM, Huynh TN, & Metter EJ (2003). A home based pedometer-driven walking program to increase physical activity in older adults with osteoarthritis of the knee: A preliminary study. Journal of the American Geriatrics Society, 51(3), 387–392. PubMed ID: 12588583 doi: 10.1046/j.1532-5415.2003.51113.x [DOI] [PubMed] [Google Scholar]
- Treacy D, Hassett L, Schurr K, Chagpar S, Paul SS, & Sherrington C (2017). Validity of different activity monitors to count steps in an inpatient rehabilitation setting. Physical Therapy, 97(5), 581–588. PubMed ID: 28339904 doi: 10.1093/ptj/pzx010 [DOI] [PubMed] [Google Scholar]
- Watt JR, Franz JR, Jackson K, Dicharry J, Riley PO, & Kerrigan DC (2010). A three-dimensional kinematic and kinetic comparison of overground and treadmill walking in healthy elderly subjects. Clinical Biomechanics (Bristol, Avon), 25(5), 444–449. doi: 10.1016/j.clinbiomech.2009.09.002 [DOI] [PubMed] [Google Scholar]
- Webber SC, Magill SM, Schafer JL, & Wilson KC (2014). GT3X+ accelerometer, Yamax pedometer and SC-StepMX pedometer step count accuracy in community-dwelling older adults. Journal of Aging and Physical Activity, 22(3), 334–341. PubMed ID: 23921227 doi: 10.1123/JAPA.2013-0002 [DOI] [PubMed] [Google Scholar]
- Wong CK, Mentis HM, & Kuber R (2018). The bit doesn’t fit: Evaluation of a commercial activity-tracker at slower walking speeds. Gait & Posture, 59, 177–181. PubMed ID: 29049964 doi: 10.1016/j.gaitpost.2017.10.010 [DOI] [PubMed] [Google Scholar]


