Generic medications, which have saved billions of dollars over the past 30 years, remain vitally important as patients and payers wrestle with access and affordability in health care.
The cost of medications continues to be one of the fastest-growing health care expenses, due to increases in both price and volume: Innovative new medicines bear higher prices, while at the same time our country’s use of prescription drugs is growing in response to higher rates of chronic disease, such as diabetes and high cholesterol.
Benefit payers – the employers, labor unions, and government programs that share healthcare costs with insured individuals – can keep drug spending in check by ensuring their proper use, eliminating waste, and adopting formularies that prefer generics. Pharmacy Benefit Managers (PBMs), such as Express Scripts, a Cigna company, bring together the buying power of payers and negotiate with pharma manufacturers to include the most clinically effective and cost-effective medicines. To create the financial headroom for innovative new products, leveraging the use of generics – comprising about 90% of all prescriptions – is critical.
Beyond generic utilization, formulary management can drive dramatic savings. Express Scripts’ National Preferred Formulary, which covers more than 25 million people, has saved clients $14.5 billion in annual, incremental savings since 2014. Overall, the company’s clients spent just 0.4% more on drugs in 2018 than the prior year – and half of them spent less.
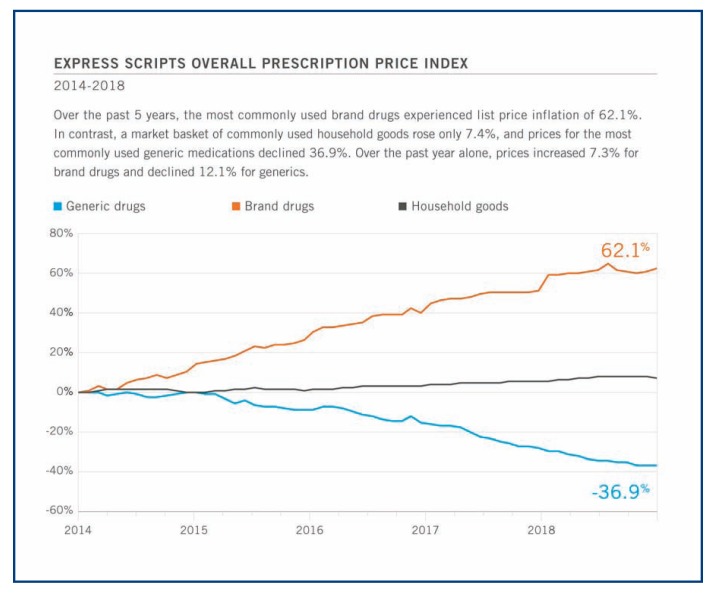
That’s despite steady increases in the cost of brand-name drugs. The average price for the most commonly used brand drugs experienced list price inflation of 62.1% between 2014–2015, more than eight times higher than the rate of inflation on a market basket of commonly used household goods. During the same period, prices for the most commonly used generic medications declined by 36.9%.
The benefits also accrue to patients. In 2018, people with Express Scripts drug coverage paid an average of $11.55 for a 30-day prescription, just 6 cents more than in 2017. And the savings realized by payers help them avoid dramatic increases in the cost to members of health care benefits.
Hurdles to Overcome
Yet the generic medication landscape does have challenges. As prices fall, so do profits for manufacturers. Generic drugs that aren’t sold in high volume are a particular challenge to the supply chain – especially when manufacturing facilities require new investments to keep up with safety standards or maintenance. Manufacturers may drop out of the market, rather than invest, leaving production of a particular drug in the hands of a single company.
In some cases, profiteers have purchased the manufacturers of single-source drugs and dramatically hiked prices.
The most notorious of these is Martin Shkreli, whose now-defunct Turing Pharmaceuticals in 2015 raised by more than 5,000% the price of a medication, Daraprim, which is used to treat a parasitic infection found in pregnant women, babies, and HIV patients. Express Scripts worked with compounding pharmacies to make an alternative generic medication for just $1 per dose, compared with $750 charged by Turing; and later implemented a program to protect payers and patients from market price shocks. Shkreli was convicted in 2017 of criminal fraud for other business practices.
Another consequence of declining generic drug manufacturing capacity is drug shortages.
In an October 2019 report, the U.S. Food and Drug Administration found that the number of ongoing drug shortages has recently been increasing, after declining from a peak in 2011, and that they are lasting longer. It analyzed 163 drugs that went into shortage between 2013 and 2017, and found that drugs most likely to run low are both older and sold at relatively low prices.
These included vital medications, such as treatments for a childhood cancer, septic shock, and palliative care in a number of forms of cancer.
Recognizing the fragility of the supply chain, Express Scripts uses proprietary algorithms to predict drug shortages, allowing the company to strategically purchase and contract for drugs from manufacturers and avoid impacts to its patients.
As overall market dynamics come into play, prices should increase to levels of sustainability for manufacturers. Global drug production also can mitigate shortages. And the FDA is recommending steps to reward manufacturers which have mature quality management systems.
The Next Generic Wave
It is important to not only protect the supply of existing generic drugs, but to encourage and support development of even more lower-cost alternatives to brand medications. A host of high-cost specialty drugs is losing patent protection, creating new opportunities to drive value and savings.
A wave of specialty oral solid generics is emerging, with FDA generic approvals representing about $14 billion in U.S. drug spending already approved and another $24 billion in opportunity expected through 2023. Prices will fall as competition is introduced into therapeutic categories long dominated by high-cost brand drugs.
Likewise, advocates including Express Scripts support the approval of biosimilars, which are clinically equivalent alternatives to injectable biologic drugs. These medications are used to treat some of the most complex and chronic disease, including rare and orphan conditions, and are among the most expensive. While the U.S. has not yet gained a significant benefit from biosimilars, it is important to note that in Europe, the biosimilar market is robust and safe, cost-effective alternatives are more broadly used. The opportunity in the U.S. is important in the overall drug pricing picture.
Biosimilars could reduce direct spending on biologic drugs by $54 billion in the next decade, according to estimates by the Rand Corporation. However, realizing that value will require regulatory changes to recognize biosimilars as interchangeable with brand originator drugs and able to compete as generics do with branded oral solid medications.
As more generics come to market, and when the potential of biosimilars is realized, payers will realize savings in drug spending that can create headroom for them to afford more new, innovative and life-saving treatments, such as gene therapy.
The U.S. spends $3.7 trillion on health care. Our challenge isn’t in finding more dollars to spend, but in using our money more wisely to afford the treatments that people need to get and stay healthy. Generic drugs are an important tool for doing so.
Footnotes
Steve Miller, MD, serves as Cigna’s Chief Clinical Officer, and leads the company’s clinical policy, quality, and performance efforts. He formerly served as Senior Vice President and Chief Medical Officer for Express Scripts and received his medical degree from the University of Missouri-Kansas City, Kansas City, Missouri.