Abstract
Electronic cigarette (e-cigarette) use has recently risen to the forefront of medical discussions across the country. A significant increase in e-cigarette use by adolescents has been observed over the last decade. This article discusses the targeting of adolescents by e-cigarette companies. It looks at how teenagers are uniquely affected by nicotine and at risk for progressing to using combustible cigarettes and marijuana. Lastly, it discusses the role of physicians in combating the spread of e-cigarettes.
Introduction
Every medical student is taught the three basic questions to ask for social history. “Do you drink any alcohol? Do you do any drugs? Do you smoke cigarettes?” While these are three very important questions to help us address potential health hazards with patients, they fail to identify some of the most significant factors in the lives of adolescent patients. Specifically, vaping in adolescents poses a grave risk to patients’ health and is a topic that physicians have to confront.
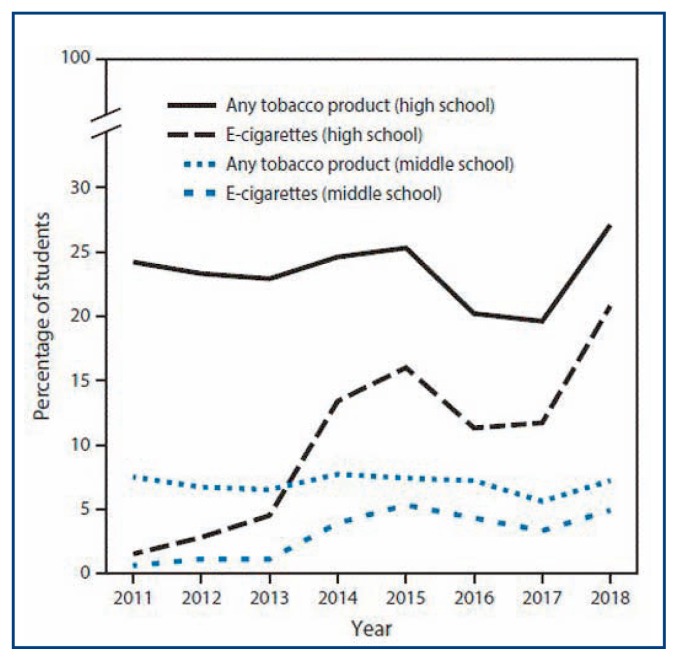
Over the last 20 years, there has been a decrease in the number of teenagers smoking combustible cigarettes. The Youth Risk Behavior Survey demonstrated a decrease in the number of teens trying combustible cigarettes from 70% in 1991 down to 58.4% in 2003 and even further down to 28.9% in 2017.1 The decrease is largely a response to exhaustive work done by physicians, advocacy groups and lawmakers. Physicians have worked diligently to improve education on the dangers of smoking and fought to pass new regulations to protect patients. The United States is seeing an explosive rise of adolescents’ vaping and the renormalization of smoking (Table 1). Recent national surveys demonstrate a drastic increase in e-cigarette use among high schoolers. An article from the New England Journal of Medicine reported a 10% increase in adolescents using e-cigarettes between 2017 and 2018 alone, which is approximately 1.3 million teenagers.2
Table 1.
The rise of adolescents’ vaping and the renormalization of smoking.
Source: Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the Field: Use of Electronic Cigarettes and Any Tobacco Products Among Middle and High School Students – United States, 2011–2018. MMWR Morb Mortal Wkly Rep 2018;67:1276–1277
Electronic cigarettes are battery-operated devices that use an electric pulse to heat and aerosolize a flavored liquid that typically contains nicotine. They were first introduced to the U.S. in 2007, and they were advertised by the tobacco companies as an adjunct method to help patients quit smoking. This claim never had evidence to support it, as studies comparing the use of electronic cigarettes, placebos, and nicotine patches demonstrated no significant differences in abstinence rates.3 But because e-cigarettes were seen as a treatment option, they were not subjected to the same regulations as combustible cigarettes. It wasn’t until 2016 that the Congress passed the Child Nicotine Poisoning Prevention Act, giving the FDA the authority to regulate e-cigarette packaging.1
Advertising Directed to Teens
Advertising for e-cigarettes has been heavily aimed at adolescents. Everything from the billboards to the packaging to the product itself has been aimed at teens. Ads on social media were widely distributed. From 2014 to 2016, advertising for vaping exploded and one study found that 78% of middle and high school students had been exposed to at least one advertisement.1 Pods come in fun packaging and the different pods are flavored to be attractive to adolescents, with everything from mint to gummi bear to frosted sugar cookie. This is especially concerning because studies have shown that flavor is one of the most important factors adolescents consider in trying e-cigarettes.4 The devices to aerosolize the pods are designed to look like anything from USBs to pens to inhalers. They can be personalized much like a cell phone case and backpacks have special pockets for the mod devices.
Health Risks for Adolescents
This targeted marketing of e-cigarettes is particularly harmful given the significant health risks these products pose to teens. Many people know that nicotine causes lots of problems for the developing brain. However, it is not widely recognized that many e-cigarettes contain higher concentrations of nicotine than combustible cigarettes. JUUL is the most common e-cigarette brand used in the U.S.; it is so popular that teens use JUULing as a verb.1 JUUL pods contain 5%, or 59mg/ml, of nicotine.5 This is approximately equal to the nicotine contained in 20 combustible cigarettes.6 To make this more concerning, one study demonstrated that 39% of adolescents did not consider JUULs to be e-cigarettes at all.6 Another survey suggested that 63% of adolescents did not know that JUUL pods contained nicotine at all.7
Many studies, primarily based on the use of combustible cigarettes, have demonstrated the adverse health effects of nicotine. Adolescent brains are still developing, and nicotine exposure has been linked with cognitive deficits and impairment in memory and executive function. Electronic cigarettes have been connected with increased impulsivity, with one animal study demonstrating that exposure to e-cigarette vapor during times of rapid brain growth (like during adolescence) can cause hyperactivity and impulsive behavior changes.4 Another study looking specifically at the teen population found increased risks of physical fighting, attempted suicide, and alcohol/marijuana use when comparing non-users to teens who smoked or vaped.8
Nicotine Addiction in Teens
There has also been evidence that suggests e-cigarette use increases an individual’s chance of using combustible cigarettes. Adolescents who use e-cigarettes are 3.6 times more likely to report using combustible cigarettes later in life.9 Teens have also been shown to be more susceptible to addiction. We know that nicotine addiction often originates in adolescence with studies showing that close to 90% of adult daily smokers started before the age of 18.10 Thus, e-cigarettes are effectively helping to create a new generation addicted to nicotine.
Gateway to Marijuana Use
Many vaping devices can also be used to inhale cannabinoids. One study demonstrated that teens who use nicotine liquid in e-cigarettes were 3.6 to 4 times more likely to use marijuana in the next two years.1 Another study demonstrated that 1 in 10 seniors in high school vape cannabis.6 This should be extremely distressing to physicians and medical providers because it is known that marijuana is extremely harmful to the development of the adolescent brain and studies have actually shown changes in brain structure. As a result, deficits in attention, learning, and memory associated with cannabis use in adolescents has been reported.11 One study demonstrated that high schoolers who use marijuana were four times more likely to have multiple sexual partners when compared to students who only use tobacco or alcohol.12 A sizable portion of adolescents who use marijuana report symptoms of paranoia, anxiety and hallucinations.13. Adverse effects from marijuana use, including cannabis hyperemesis syndrome have become common among pediatric patients.14
Flavors and Additives
Beyond the nicotine, the flavoring chemicals and additives present their own danger. Currently there are no federal laws to ensure that the labels on e-cigarettes are accurate. Until August 2018 they did not even have to include the nicotine concentration on labels. Testing has demonstrated different carcinogens in e-cigarettes including aldehydes, metals, and polycyclic aromatic hydrocarbons.6 One recent study looking at the different additives found that that vapes containing cinnamaldehyde for cinnamon flavor were associated with impaired mucociliary function in bronchial epithelial cells. Biopsies from chronic vapers demonstrate structural changes in lung tissue.1
Education
Physicians caring for adolescent patients are quickly realizing the health hazards associated with vaping and are looking for ways to combat the epidemic. First and foremost is education for both the teen and their parents. Teens obtain most of their knowledge on e-cigarettes from social media and their peers. One in three adolescents in the U.S. still consider electronic cigarettes to be less harmful than traditional combustible cigarettes.4 It is imperative that teens are given accurate information on e-cigarettes.
Unfortunately, parents often face the same challenges in finding resources for vaping education as their children. They rely on schools to educate both the parent and their child on e-cigarettes, yet studies have shown that most parents receive little communication from their school on the topic.15 This is an area where physicians can help fill the knowledge gap. One study found that while parents understood that nicotine exposure is detrimental for teens, most did not know that JUUL pods contain nicotine. Less than half of the middle school and high school parents could identify a JUUL mod in a picture.15 Most parents were concerned about the use of e-cigarettes in teens but only two in five were concerned about use in their own child.15 Parents who do not feel that their children are at risk are less likely to talk to their children about the risks associated with vaping. It is imperative that physicians encourage parents to discuss vaping with their teens and provide tools to facilitate that discussion.
Advocacy
The other way physicians can help address vaping in adolescents is by participating in advocacy at a local, state or national level. Currently in the state of Missouri, e-cigarettes are not included in the definition of “Tobacco Products” and thus are not subject to the same restrictions as combustible cigarettes. The sale of e-cigarettes to those under 18 years of age is prohibited, just as with tobacco. But the only regulation in place for e-cigarette packaging is that the liquid must be in child-resistant containers. The American Academy of Pediatrics is currently advocating for Missouri to include e-cigarettes in smoke-free laws and to increase the minimum age to purchase electronic cigarettes to 21 years.16 Organizations like the American Academy of Pediatrics and the American College of Physicians have both released position papers on vaping and offer further ways to join the fight. It is time for physicians to ask their adolescent patients about vaping and to provide education to the child and parents on the dangers of vaping. Physicians have the responsibility to be advocates for their patients working with medical organizations, state and local governments to address the adolescent vaping epidemic.
Footnotes
Kristen Jones, DO, (left ), is a Pediatrics Resident in Internal Medicine; Gary A. Salzman, MD, (right), MSMA member since 2007, is Professor of Medicine; University of Missouri-Kansas City School of Medicine, Kansas City, Missouri.
Contact: salzmang@umkc.edu
Disclosure
None reported.
References
- 1.Slekman J. Vaping: It’s all a smokescreen. Pediatric Nursing. 2019;45(1):12–15. 35. [Google Scholar]
- 2.Zainab, et al. The Adolescent Vaping Epidemic in the United States - How It Happened and Where We Go From Here. JAMA Otolaryngology - Head & Neck Surgery. 2019 Aug 22; doi: 10.1001/jamaoto.2019.2410. [DOI] [PubMed] [Google Scholar]
- 3.Huey SW, Granitto MH. Smoke screen. Journal of the American Association of Nurse Practitioners. 2019;1 doi: 10.1097/jxx.0000000000000234. [DOI] [PubMed] [Google Scholar]
- 4.Tobore TO. On the potential harmful effects of E-Cigarettes (EC) on the developing brain: The relationship between vaping-induced oxidative stress and adolescent/young adults social maladjustment. Journal of Adolescence. 2019;76:202–209. doi: 10.1016/j.adolescence.2019.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Morean ME, Bold KW, Kong G, et al. Adolescents’ awareness of the nicotine strength and e-cigarette status of JUUL e-cigarettes. Drug and Alcohol Dependence. 2019;204:107512. doi: 10.1016/j.drugalcdep.2019.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morean ME, Bold KW, Kong G, et al. Adolescents’ awareness of the nicotine strength and e-cigarette status of JUUL e-cigarettes. Drug and Alcohol Dependence. 2019;204:107512. doi: 10.1016/j.drugalcdep.2019.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fadus MC, Smith TT, Squeglia LM. The rise of e-cigarettes, pod mod devices, and JUUL among youth: Factors influencing use, health implications, and downstream effects. Drug and Alcohol Dependence. 2019;201:85–93. doi: 10.1016/j.drugalcdep.2019.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Demissie Z, Jones SE, Clayton HB, King BA. Adolescent Risk Behaviors and Use of Electronic Vapor Products and Cigarettes. Pediatrics. 2017;139(2) doi: 10.1542/peds.2016-2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jenssen BP, Wilson KM. What is new in electronic-cigarettes research? Current Opinion in Pediatrics. 2019;31(2):262–266. doi: 10.1097/mop.0000000000000741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kong G, Krishnan-Sarin S. A call to end the epidemic of adolescent E-cigarette use. Drug and Alcohol Dependence. 2017;174:215–221. doi: 10.1016/j.drugalcdep.2017.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jacobus J, Bava S, Cohen-Zion M, Mahmood O, Tapert S. Functional consequences of marijuana use in adolescents. Pharmacology Biochemistry and Behavior. 2009;92(4):559–565. doi: 10.1016/j.pbb.2009.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Green KM, Musci RJ, Matson PA, Johnson RM, Reboussin BA, Ialongo NS. Developmental Patterns of Adolescent Marijuana and Alcohol Use and Their Joint Association with Sexual Risk Behavior and Outcomes in Young Adulthood. Journal of Urban Health. 2017;94(1):115–124. doi: 10.1007/s11524-016-0108-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levy S, Weitzman ER. Acute Mental Health Symptoms in Adolescent Marijuana Users. JAMA Pediatrics. 2019;173(2):185. doi: 10.1001/jamapediatrics.2018.3811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chadi N, Levy S. Understanding the Highs and Lows of Adolescent Marijuana Use. Pediatrics. 2017;140(6) doi: 10.1542/peds.2017-3164. [DOI] [PubMed] [Google Scholar]
- 15.Patel M, Czaplicki L, Perks SN, et al. Parents’ Awareness and Perceptions of JUUL and Other E-Cigarettes. American Journal of Preventive Medicine. 2019;57(5):695–699. doi: 10.1016/j.amepre.2019.06.012. [DOI] [PubMed] [Google Scholar]
- 16.Jenssen BP, Walley SC. E-Cigarettes and Similar Devices. Pediatrics. 2019;143(2) doi: 10.1542/peds.2018-3652. [DOI] [PMC free article] [PubMed] [Google Scholar]