Abstract
For optimal results, facial rejuvenation procedures should address both the tissue laxity and volume deflation associated with facial aging. The lift-and-fill face lift, in which fat grafting provides volumetric rejuvenation to the face while surgical lift effectively repositions and removes ptotic and redundant tissue, has revolutionized the plastic surgeon's approach to the aged face. An understanding of the intricate anatomy of distinct facial fat compartments and a systematic method to assess areas of fat atrophy and volume depletion are keys to provide patients with a natural and youthful result. Fat grafting may be used to improve contour in any area treatable by nonautologous injectable fillers, including the temples, forehead, upper and lower orbit, cheeks, perioral region, nasolabial fold, jawline, and chin—with the benefit of a more natural contour and integration with native tissue.
Keywords: facial rejuvenation, facial aging, facial fat grafting, facial fat compartments, lift-and-fill face lift
Facial aging is a complex and dynamic process that is the result of changes to the facial skin, skeleton, and subcutaneous soft tissue. An understanding of these changes is key to properly restoring natural, attractive, and youthful facial characteristics in facial rejuvenation procedures. With age, the facial skeleton undergoes clockwise rotation of the midface in relation to the cranial base with increased size and posterior displacement of the maxilla, enlargement of the orbital aperture, and decreased size of the mandible in both horizontal and vertical planes. 1 These changes effectively shift the face's overlying retaining ligaments and soft tissue, which in turn causes deflation of distinct facial fat compartments and gives the appearance of increased skin laxity and prominent folds in the nasolabial, periorbital, and jowl regions ( Fig. 1 ). 2 3
Fig. 1.
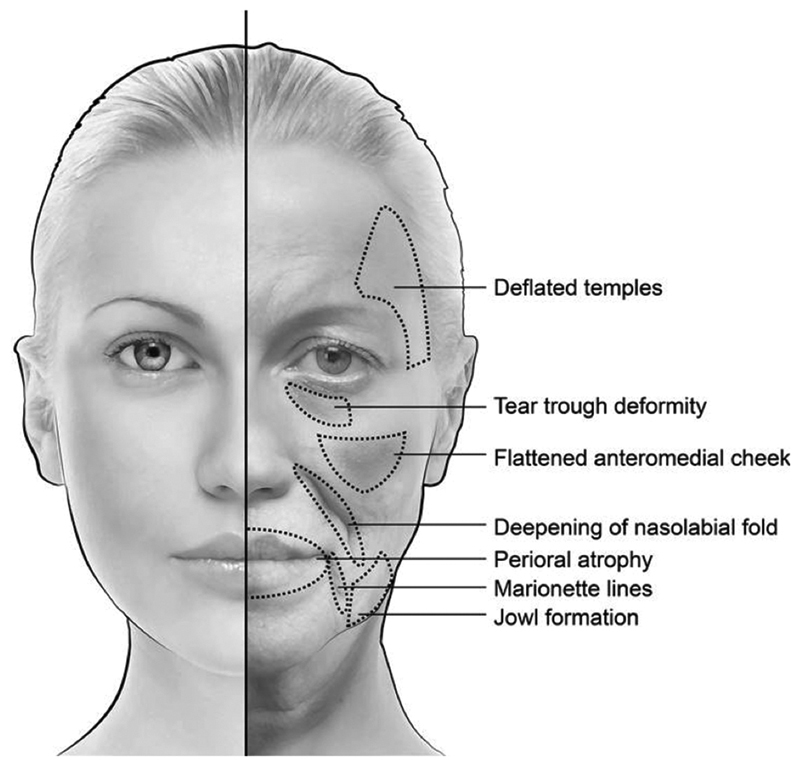
Features of the aging face. (Reproduced with permission of Baylor College of Medicine.)
Fat provides crucial structural support to the face. Therefore, age-associated soft tissue changes require both volume augmentation as well as resuspension of ptotic tissue and removal of redundant tissue. 4 Based on these principles, the lift-and-fill face lift has revolutionized the approach to the aging face in aesthetic surgery ( Table 1 ). 5 6 7 With this technique, fat grafting is performed to deep and superficial fat compartments followed by superficial musculoaponeurotic system (SMAS) and platysma manipulation. Subsequent superficial fat grafting may be performed on the forehead, temples, tear trough, oral commissure, chin, and any other regions requiring volume augmentation. Unlike nonautologous injectables, fat grafting to these regions integrates with facial tissues to yield a more seamless, natural-appearing, and long-lasting improvement in contour. The regenerative potential of adipose-derived stem cells (ADSCs) also improves the quality of overlying facial tissue, improving scars and sun damage over time. 7 8
Table 1. Sequence in the lift-and-fill face lift as described by Rohrich et al 5 .
| (1) | Fat grafting to deep and superficial fat compartments. |
| (2) | Selective skin undermining. |
| (3) | SMAS manipulation. |
| (4) | Re-draping of skin and closure. |
| (5) | Blepharoplasty (if indicated). |
Abbreviation: SMAS, superficial musculoaponeurotic system.
Precise understanding of the anatomy of the distinct facial fat compartments is critical for precision in preoperative analysis and successful rejuvenation of the aging face. Subcutaneous fat compartments of the face and their anatomic landmarks are outlined in Table 2 . 3 5
Table 2. Anatomic descriptions of the distinct subcutaneous facial fat compartments.
| Compartment | Depth | Anatomical landmarks | |
|---|---|---|---|
| Forehead | |||
| Central compartment | Superficial | Midline of forehead, bordered inferiorly by nasal dorsum. | |
| Middle temporal fat compartments | Superficial | Bordered medially/laterally by central forehead fat, inferiorly by orbicularis retaining ligament. | |
| Lateral temporal malar fat compartment | Superficial | Immediately superficial to parotid gland, connects temporal fat to cervical fat. | |
| Orbit | |||
| Superior orbital fat | Superficial | Upper orbit, bordered superiorly and laterally by orbicularis retaining ligament. | |
| Inferior orbital fat | Superficial | Immediately inferior to inferior lid tarsus, bordered inferiorly by orbicularis retaining ligament. | |
| Lateral orbital fat | Superficial | Bordered superiorly by inferior temporal septum, inferiorly by superior cheek septum. | |
| Cheek | |||
| Medial malar fat compartment a | Deep | Lateral to nasolabial fold, bordered superiorly by orbicularis retaining ligament and lateral orbital compartment. | |
| Middle malar fat compartment a | Superficial | Anterior and superficial to parotid gland, superiorly adherent to zygomaticus major. | |
| High malar fat compartment a | Superficial | Superior to middle malar fat. | |
| Nasolabial fat compartment a | Deep | Anterior to medial cheek fat, overlapping jowl fat. | |
| Jowl | Superficial | Bordered medially by lip depressor and inferiorly by platysma. | |
Fat compartments addressed first in the lift-and-fill face lift.
Preoperative Planning
Patient Selection
Although a wide variety of patients can be considered candidates for facial rejuvenation procedures, particular caution should be exercised when patients have a history of smoking, bleeding disorders, or surgical infections. 8
Assessment and Planning
Preoperative planning should include a discussion about the patient's desired postoperative outcomes and a robust facial analysis. It is often useful to examine photographs from the patient's youth to establish aesthetic goals. Facial analysis with close attention to any facial asymmetry should assess three basic parameters: midface width, facial length, and facial fullness. 9 Assessment of the patient's midface width and facial length will guide management of the SMAS after fat grafting. SMAS stacking should be performed in patients with long and narrow faces to provide a selective increase in facial fullness, while SMASectomy should be performed in patients with a short and wide face to decrease facial fullness and allow any fat-grafted compartments to appear fuller by comparison. In cases of significant asymmetry, each side of a patient's face may benefit from a different technique ( Fig. 2A,B ). 5
Fig. 2.
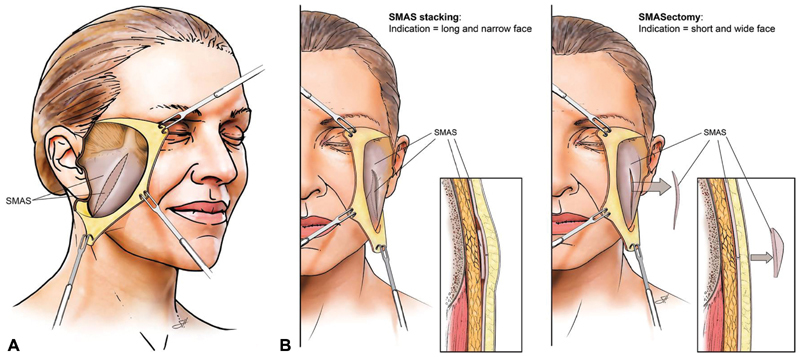
( A ) Depiction of intraoperative exposure of the SMAS during a lift-and-fill facelift. ( B ) Intraoperative depiction of SMAS stacking, as performed in patients with long and narrow faces to provide augmented fullness, and SMASectomy, as performed in patients with short and wide faces to provide a narrower facial contour. SMAS, superficial musculoaponeurotic system. (Reproduced with permission of Baylor College of Medicine.)
Evaluation of facial fullness will guide areas to be addressed with fat grafting. This may be accomplished by dividing the face into anatomical thirds and systematically assessing key features ( Fig. 3 ). Transition points between the subcutaneous and deep fat compartments will manifest as visible folds in the aging face and areas of soft tissue redundancy. It is important to identify aging features that may be addressed with fat grafting alone and those that will require accompanying surgical techniques.
Fig. 3.
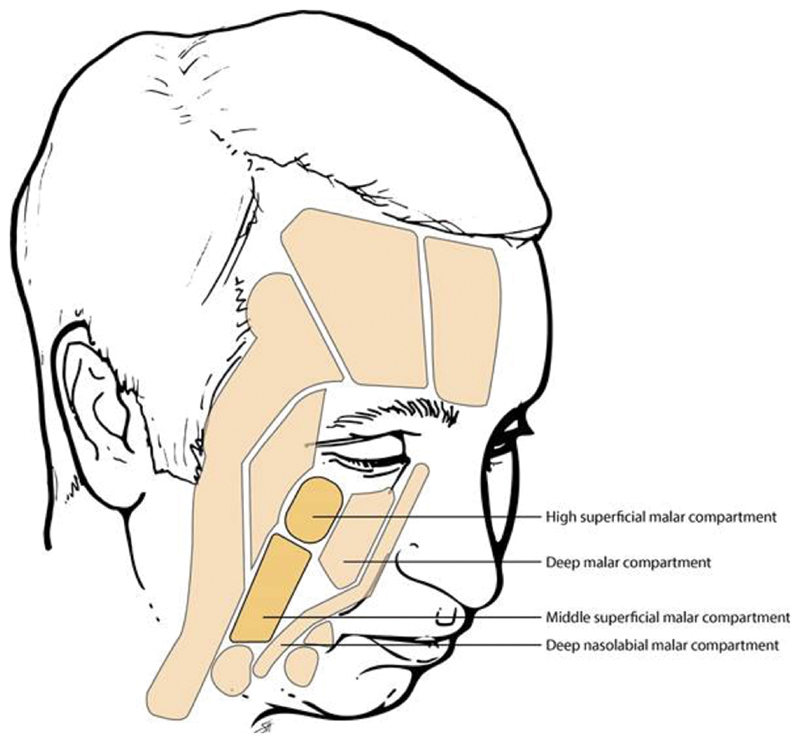
Four key mid-facial fat compartments to address with fat grafting in facial rejuvenation procedures. (Reproduced with permission from Rohrich et al, 2014. 5 )
Upper Third
Primary features of the upper third of the face that undergo significant changes with aging are the brows, upper eyelids, and temples. 2 The youthful brow and upper eyelid complex is full and convex with a lateral arch and has a smooth transition into the temple area. Aging is associated with lateral forehead hollowing and a descended lateral brow secondary to atrophy of temporal fat pads. Fat grafting to the temples and forehead can effectively restore a youthful temporal contour and lift the lateral brow, giving a more natural appearance than a surgical brow lift, which preferentially elevates the medial brow. 10 Upper lid blepharoplasty is only indicated in patients with brow ptosis. Fractionated fat injection following blepharoplasty may improve upper lid volume and stimulate dermal regeneration. 11
Middle Third
Primary features of the midface include the lower eyelid, tear trough, and malar region.
With age, hollowing of the infraorbital region, laxity of the orbital retaining ligament, and loss of volume in the anterior cheek create a deep tear trough deformity. Patients with fat herniation at the inferior orbital rim may require a blepharoplasty prior to any fat transfer to achieve a smooth transition from the lower eyelid to the cheek. 12 Blending of the lid-cheek junction and correction of orbital hollowing are best addressed with fractionated fat grafting. 13
There are four key fat compartments that should be addressed in volume augmentation of the malar region: the deep malar (medial) compartment, deep nasolabial malar compartment, the high lateral superficial malar compartment, and the middle superficial malar compartment ( Fig. 2 ). The deep malar compartment (the “workhorse” in midface volume restoration) should be addressed first, followed by the superficial high and middle malar compartments. 5 Fat grafting to the cheek produces a softer improvement in malar contour than that achieved with implant placement. Any notable, pre-existing malar asymmetry is also easily corrected. The buccal fat pad is an often-overlooked component to the youthful midface and should be complementarily reconstituted after malar augmentation to prevent a hollowed appearance. 12 14
Lower Third
Primary features of the lower third of the face include the nasolabial fold, labiomandibular fold (marionette lines), prejowl sulcus (geniomandibular groove), labiomental sulcus, lips, and chin. Deepening of the nasolabial fold occurs with deflation of the cheek. Therefore, filling of the malar fat compartments should effectively lift the nasolabial fold and be performed before any nasolabial augmentation to avoid overcorrection.
Jowls are the result of dentate mandible expansion and relative prejowl concavity. 15 16 17 While a youthful, angular jaw contour may be achieved with fat grafting along the lateral mandible posterior to the jowl, significant jowling requires surgical cervicofacial rhytidectomy 2 ; however, surgical lift of the jowl cannot address the geniomandibular groove. Fat grafting is necessary in this region to create a smooth line from the chin to posterior mandible. 7
With age, the lips become thin and lose crispness along the philtral columns. These changes, in conjunction with subcutaneous fat atrophy, manifests as perioral rhytids that cannot be addressed with surgical rhytidectomy alone. Resurfacing techniques alone are ineffective in correcting perioral pucker lines. Instead, fat grafting to superficial compartments near the vermillion-cutaneous junction is necessary to achieve volume augmentation of an atrophied perioral region. 18 Filling of the white roll and vermillion, however, should be done with injectables, as fat graft take in these areas is unpredictable. 18
Age-related volume depletion in the chin results in loss of chin projection and vertical height as well as deepening of the labiomental crease. Fat grafting effectively restores a youthful lower lip contour and refined chin in patients with soft tissue descent and small asymmetries or imperfections, such as bifid chin or microgenia. 19 Patients requiring more than 3 mL of augmentation per side may benefit from chin implants to avoid a globular appearance. 7
Surgical Technique
Preoperative Facial Marking
The patient's face should be preoperatively marked with the patient in an upright position, allowing dependent tissues to fully accentuate facial highlights and shadows. 2 After all markings have been made, the patient's face should be photographed again to serve as an intraoperative reference. 7
Anesthesia
Face lift procedures accompanied by fat transfer are generally performed under general anesthesia, allowing for optimal patient comfort and operative efficiency. Heavier sedation also enables large volume fat harvesting and the ability to access multiple donor sites, should the need arise. 8 20
Technique
The Coleman technique is a popular fat grafting technique that has been applied and improved upon since the early 1990s. This technique involves gentle fat harvesting to preserve parcel structure, fat refinement through centrifugation to remove nonviable components, and to concentrate the adipose tissue, and delivery of the fat in small aliquots to ensure satisfactory blood supply and increased likelihood of graft take. 21 22
Fat Harvesting
Donor site selection for fat grafting should account for donor site aesthetics, patient preference, surgical positioning, quantity of fat needed, and quantity of fat available. 23 The lower abdomen and inner thighs—sites with a high concentration of ADSCs—are the preferred harvesting sites for facial augmentation procedures. An average of 30 mL of fat is required for most facial rejuvenation and contouring cases. 24
The technique of choice for fat harvesting is syringe aspiration with a 10-mL Luer-Lok syringe attached to a harvesting cannula. A modified multihole Coleman cannula increases harvesting efficiency by creating a negative pressure when the plunger of the syringe is pulled back. 2 8 The face is a volume-sensitive recipient site, so a small cannula (12 gauge) with small holes (1 × 1 mm) should be used to ensure that appropriately sized lobules of fat are harvested. 25 Entry sites for cannula insertion should be made in discreet areas such as the umbilicus (for harvest from the lower abdomen) or inguinal line (for harvest from the medial thigh). Deep passage of the cannula should be avoided to prevent damage to the rectus fascia and harvest fat uniformly to ensure a smooth postprocedure contour. 2
Fat Refinement and Purification
Centrifugation is often the preferred method of fat refinement. 2 Centrifugation permits separation and concentration of ruptured fat cells (the oil fraction) and blood and local anesthetic (the water fraction) from intact fat cells. Unprocessed fat is loaded into a centrifuge and spun minimally (no longer than 1 minute at 2,250 rpm). 7 26 Blood-tinged water and oil fractions are discarded, and a Telfa strip (Telfa Strip) or Codman neuropad (Codman, Neuro) is placed inside of the barrel to absorb any residual oil. 8 Fractionated fat requires mechanical emulsification after centrifugation by pushing fat between two syringes connected by a Luer-Lok connecter. 13 Processed fat can subsequently be transferred into 1-mL syringes for precise injection. Higher density fat demonstrates better graft take than lower density fat and should be preferentially utilized. 27
Fat Placement
A small volume of fat should be administered with each injection to maximize control of fat delivery and to minimize complications such as fibrosis, calcification, infections, or oil cyst formation. 24 With each pass, no more than 0.5 to 1 mL of fat should be injected per second, and injections should be performed within multiple tissue planes and in multiple directions, with awareness of the cannula tip at all times. 4 28 29 Additionally, care should be taken to avoid nearby vessels and nerves. When injecting smaller facial regions such as the periorbital region, a smaller cannula should be utilized for greater control over the volume placed. 24 As fat is injected, facial augmentation will be readily apparent. If volume-restrictive factors, such as fibrotic adhesions or a tight skin envelope, are suspected, dissection with an 18-gauge needle or forked tip cannula may be indicated. 24 Guidelines for fat injection to specific treatment areas are shown in Table 3 . 7 13 24 Deep compartments are accessed just lateral to the alar-cheek junction. 30
Table 3. Commonly fat grafted areas of the face, along with their injection entry point and typical fat volume required.
| Treated area | Injection site | Volume required |
|---|---|---|
| Forehead | Crease in the mid-forehead or within the hairline | 10–15 mL |
| Temples | Within temporal hairline | 2–7 mL |
| Tear trough and periorbital region | Inferior to medial orbit in mid-cheek | 3 mL |
| Cheek (nasolabial and deep malar compartments, superficial superior and inferior malar compartments) | Adjacent to alar base | 1–3 mL per compartment |
| Buccal region | Intraoral or medial lower cheek | 2–5 mL |
| Geniomandibular groove | Over mandibular border | 1–3 mL |
| Chin | Intersection of the oral commissure and lateral canthus | 1–3 mL |
| Perioral region | Adjacent to oral commissures | 1–2 mL |
| Mandible | Anterior to mandibular angle | 1–3 mL |
Fat injection should proceed from deep to superficial, and the depth of fat placement should be tailored to achieve desired patient outcomes. Placement in the intradermal or subdermal layers can improve the appearance of wrinkles, overall facial complexion, and overall skin quality. 31 Superficial fat placement should be performed with care as irregularities are more apparent. Deeper placement of fat in the intermediate subcutaneous layers can rejuvenate facial proportions, and placement against the bony periosteum can change how the overlying soft tissue envelope encases the facial bony structure. 8 Fat necrosis and resorption may be minimized by ensuring that there is no molding of placed fat. After grafting is complete, the infusion sites can be closed with interrupted sutures. Small, concentrated volumes of approximately 0.2 to 0.3 mL can be placed into the closed incisions to facilitate incisional healing. 8
Overcorrection should not be performed in the face, as intercompartmental membranes are elastic and can accommodate the graft volume. In addition, overcorrection can easily create an unattractive and unnaturally overfilled facial contour. 5
Postoperative Care
Surgeons should advise all facial fat grafting patients that some degree of bruising and swelling is to be expected for up to 6 weeks postoperatively. 8 12 Pigmentation of the lower eyelids, or “tea staining,” may persist for several months to a year until the overlying skin thickens. 8 After facial fat grafting, cool compresses may be applied to minimize bruising, swelling, and patient discomfort. Deep massage should be avoided to prevent fat migration or necrosis and any shear force or trauma to the area may compromise graft survival. 8
Patients should be counseled prior to their initial fat grafting operation that additional procedures are almost always necessary to achieve an ideal result. Grafted volume will often decrease by up to 50 to 90%. 8 Repeat facial fat grafting operations should be performed at least 6 months to a year after the initial operation to allow for resolution of the inflammatory response and proper assessment of the surgical outcome. 8 12 In addition, volume loss secondary to facial aging is expected to continue, and additional augmentation will likely be desired regardless of graft take. 12
Counseling should also include an approximate timeline of expected outcomes. Immediately after the operation, restoration of facial volume is obvious. Overlying skin thickening and softening, scar improvement, and wrinkle reduction take place more gradually and become increasingly apparent over the course of a few months. After a year, improved complexion of aging or sun-damaged skin may be noted ( Figs. 4A,B and 5 ). 8
Fig. 4.

( A ) Frontal and lateral pre- and postoperative photographs of a lift-and-fill face lift patient. Center panels labeled to show the location and amount of fat grafting. ( B ) Oblique views of the same patient. (Reproduced with permission from Rohrich et al, 2014. 5 )
Fig. 5.

Frontal and lateral pre- and postoperative photographs of a lift-and-fill face lift patient. Center panels labeled to show the location and amount of fat grafting. (Reproduced with permission from Rohrich et al, 2014. 5 )
Complications
The most common complication after fat grafting is minor aesthetic irregularity or asymmetry. Palpable lumps may occur secondary to fat placement too superficially or in large aliquots that results in fat necrosis. Treatment of these irregularities is relatively straightforward, requiring suction lipectomy, direct open excision, or the use of Lipodissolve. 8 Fat necrosis may also present as postoperative subcutaneous nodules and can be addressed with simple excision if the patient desires. 24
Other complications include infection, fat embolism, hematoma, and nerve injury. Although infection is rare, proper care should be taken to minimize this risk. Areas such as the lips that may be contaminated with oral flora should be injected last, and patients with any history of cold sores should receive prophylactic acyclovir. 8 Preinjection of planned recipient sites with 1% lidocaine with 1:200,000 epinephrine is recommended to minimize the risk of intravascular fat injection and subsequent embolic event. 24
Conclusion
Fat grafting has been demonstrated to address the volume deflation and skin changes associated with facial aging. When performed in conjunction with surgical rhytidectomy, blepharoplasty, neuromodulator application, injectable fillers, and laser/light therapies, facial fat grafting provides optimal results in achieving a youthful aesthetic. 2 Careful preoperative facial analysis with attention to each facial component is necessary to formulate a proper surgical plan and identify beneficial adjunctive procedures.
Acknowledgments
The authors would like to thank Scott Holmes, CMI, a member of the Michael E. DeBakey Department of Surgery Research Core at Baylor College of Medicine, for his assistance preparing several illustrations for publication in this manuscript.
Conflicts of Interest None declared.
Financial Disclosure
R.J.R receives book royalties from Thieme Medical Publishers.
References
- 1.Farkas J P, Pessa J E, Hubbard B, Rohrich R J. The science and theory behind facial aging. Plast Reconstr Surg Glob Open. 2013;1(01):e8–e15. doi: 10.1097/GOX.0b013e31828ed1da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glasgold R, Glasgold M, Lam S. Berlin, Heidelberg: Springer; 2018. Complementary fat grafting; pp. 321–332. [Google Scholar]
- 3.Rohrich R JPJ, Pessa J E.The fat compartments of the face: anatomy and clinical implications for cosmetic surgery Plast Reconstr Surg 2007119072219–2227., discussion 2228–2231 [DOI] [PubMed] [Google Scholar]
- 4.Coleman S R.Structural fat grafting: more than a permanent filler Plast Reconstr Surg 2006118(3, Suppl):108S–120S. [DOI] [PubMed] [Google Scholar]
- 5.Rohrich R J, Ghavami A, Constantine F C, Unger J, Mojallal A. Lift-and-fill face lift: integrating the fat compartments. Plast Reconstr Surg. 2014;133(06):756e–767e. doi: 10.1097/01.prs.0000436817.96214.7e. [DOI] [PubMed] [Google Scholar]
- 6.DeFatta R J, Williams E F., IIIFat transfer in conjunction with facial rejuvenation procedures Facial Plast Surg Clin North Am 20081604383–390., v [DOI] [PubMed] [Google Scholar]
- 7.Marten T J, Elyassnia D. Fat grafting in facial rejuvenation. Clin Plast Surg. 2015;42(02):219–252. doi: 10.1016/j.cps.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 8.Coleman S R, Katzel E B.Fat grafting for facial filling and regeneration Clin Plast Surg 20154203289–300., vii [DOI] [PubMed] [Google Scholar]
- 9.Rohrich R J, Ghavami A, Lemmon J A, Brown S A. The individualized component face lift: developing a systematic approach to facial rejuvenation. Plast Reconstr Surg. 2009;123(03):1050–1063. doi: 10.1097/PRS.0b013e31819c91b0. [DOI] [PubMed] [Google Scholar]
- 10.Chiu C H. Objective evaluation of eyebrow position after autologous fat grafting to the temple and forehead. Aesthetic Plast Surg. 2017;41(06):1342–1350. doi: 10.1007/s00266-017-0881-4. [DOI] [PubMed] [Google Scholar]
- 11.Rohrich R J, Villanueva N L, Afrooz P N. Refinements in upper blepharoplasty: the five-step technique. Plast Reconstr Surg. 2018;141(05):1144–1146. doi: 10.1097/PRS.0000000000004439. [DOI] [PubMed] [Google Scholar]
- 12.Glasgold M, Glasgold R, Lam S. Autologous fat grafting for midface rejuvenation. Clin Plast Surg. 2015;42(01):115–121. doi: 10.1016/j.cps.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 13.Rohrich R J, Mahedia M, Shah N, Afrooz P, Vishvanath L, Gupta R K. RK G. Role of fractionated fat in blending the lid-cheek junction. Plast Reconstr Surg. 2018;142(01):56–65. doi: 10.1097/PRS.0000000000004526. [DOI] [PubMed] [Google Scholar]
- 14.Cohen S R, Fireman E, Hewett S, Saad A. Buccal fat pad augmentation for facial rejuvenation. Plast Reconstr Surg. 2017;139(06):1273e–1276e. doi: 10.1097/PRS.0000000000003384. [DOI] [PubMed] [Google Scholar]
- 15.Mendelson B, Wong C H. Changes in the facial skeleton with aging: implications and clinical applications in facial rejuvenation. Aesthetic Plast Surg. 2012;36(04):753–760. doi: 10.1007/s00266-012-9904-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pecora N G, Baccetti T, McNamara J A., Jr The aging craniofacial complex: a longitudinal cephalometric study from late adolescence to late adulthood. Am J Orthod Dentofacial Orthop. 2008;134(04):496–505. doi: 10.1016/j.ajodo.2006.11.022. [DOI] [PubMed] [Google Scholar]
- 17.Shaw R B, Jr, Katzel E B, Koltz P F, Kahn D M, Girotto J A, Langstein H N. Aging of the mandible and its aesthetic implications. Plast Reconstr Surg. 2010;125(01):332–342. doi: 10.1097/PRS.0b013e3181c2a685. [DOI] [PubMed] [Google Scholar]
- 18.Pezeshk R A, Stark R Y, Small K H, Unger J G, Rohrich R J. Role of autologous fat transfer to the superficial fat compartments for perioral rejuvenation. Plast Reconstr Surg. 2015;136(03):301e–309e. doi: 10.1097/PRS.0000000000001506. [DOI] [PubMed] [Google Scholar]
- 19.Rohrich R J, Sanniec K, Afrooz P N. Autologous fat grafting to the chin: a useful adjunct in complete aesthetic facial rejuvenation. Plast Reconstr Surg. 2018;142(04):921–925. doi: 10.1097/PRS.0000000000004817. [DOI] [PubMed] [Google Scholar]
- 20.Chen H H, Williams E F. Lipotransfer in the upper third of the face. Curr Opin Otolaryngol Head Neck Surg. 2011;19(04):289–294. doi: 10.1097/MOO.0b013e32834896a0. [DOI] [PubMed] [Google Scholar]
- 21.Coleman S. The technique of periorbital lipoinfiltration. Operat Tech Plast Reconstr Surg. 1994;1:120–126. [Google Scholar]
- 22.Coleman S R. Long-term survival of fat transplants: controlled demonstrations. Aesthetic Plast Surg. 1995;19(05):421–425. doi: 10.1007/BF00453875. [DOI] [PubMed] [Google Scholar]
- 23.Khan H A, Keyhan S O. Fat grafting in facial aesthetic units. Atlas Oral Maxillofac Surg Clin North Am. 2018;26(01):15–23. doi: 10.1016/j.cxom.2017.10.001. [DOI] [PubMed] [Google Scholar]
- 24.Pu L LQ.Fat grafting for facial rejuvenation and contouring: a rationalized approach Ann Plast Surg 201881(6S, Suppl 1):S102–S108. [DOI] [PubMed] [Google Scholar]
- 25.Del Vecchio D, Rohrich R J. A classification of clinical fat grafting: different problems, different solutions. Plast Reconstr Surg. 2012;130(03):511–522. doi: 10.1097/PRS.0b013e31825dbf8a. [DOI] [PubMed] [Google Scholar]
- 26.Rohrich R J, Durand P D, Dayan E. The lift-and-fill facelift: superficial musculoaponeurotic system manipulation with fat compartment augmentation. Clin Plast Surg. 2019;46(04):515–522. doi: 10.1016/j.cps.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 27.Allen R J, Jr, Canizares O, Jr, Scharf C et al. Grading lipoaspirate: is there an optimal density for fat grafting? Plast Reconstr Surg. 2013;131(01):38–45. doi: 10.1097/PRS.0b013e3182729cc6. [DOI] [PubMed] [Google Scholar]
- 28.Lee J H, Kirkham J C, McCormack M C, Nicholls A M, Randolph M A, Austen W G., Jr The effect of pressure and shear on autologous fat grafting. Plast Reconstr Surg. 2013;131(05):1125–1136. doi: 10.1097/PRS.0b013e3182879f4a. [DOI] [PubMed] [Google Scholar]
- 29.Xie Y, Zheng D N, Li Q F et al. An integrated fat grafting technique for cosmetic facial contouring. J Plast Reconstr Aesthet Surg. 2010;63(02):270–276. doi: 10.1016/j.bjps.2008.11.016. [DOI] [PubMed] [Google Scholar]
- 30.Rohrich R J, Afrooz P N. Finesse in facial lifting: the role of facial fat compartment augmentation in facial rejuvenation. Plast Reconstr Surg. 2019;143(01):98–101. doi: 10.1097/PRS.0000000000005165. [DOI] [PubMed] [Google Scholar]
- 31.Mojallal A, Lequeux C, Shipkov C et al. Improvement of skin quality after fat grafting: clinical observation and an animal study. Plast Reconstr Surg. 2009;124(03):765–774. doi: 10.1097/PRS.0b013e3181b17b8f. [DOI] [PubMed] [Google Scholar]


