Abstract
Introduction
Cellular senescence has been linked to the pathogenesis of idiopathic pulmonary fibrosis (IPF). CCN1 is a matricellular protein that has been shown to induce cellular senescence and contribute to lung fibrosis in pre-clinical models. In this report, we determined plasma CCN1 levels in patients with IPF and its potential role in clinical outcomes.
Methods and Results
We evaluated 88 patients diagnosed with IPF at the University of Alabama at Birmingham. CCN1 levels were measured in plasma specimens by ELISA. The primary outcome measure was transplant-free survival (TFS) duration. High-CCN1 levels were associated with a lower transplant-free survival independent of %FVC and %DLCO compared to patients with low plasma CCN1 (HR = 2.15; 95%CI 1.04–4.45, p = 0.04).
Conclusion
This study demonstrates that plasma levels of CCN1 may be predictive of survival in IPF. Given the plausible role of CCN1 in cellular senescence and pathobiology of IPF, the predictive value of CCN1 in disease progression among patients with IPF warrants further investigation.
Keywords: idiopathic pulmonary fibrosis, CCN1, cellular senescence, transplant-free survival
Introduction
Idiopathic pulmonary fibrosis (IPF) is a chronic, fibrosing disease with variable disease course. IPF is a disease of aging, yet biomarkers or sub-phenotypes of the disease associated with aging biology have not been identified. Cysteine-rich protein 61 (CYR61/CCN1), a member of the cellular communication network factor (CCN) family of matricellular proteins, has been shown to induce cellular senescence (1, 2). CCN1 participates in the regulation of inflammation, wound healing and extracellular matrix remodeling (3).
Our group previously reported increased expression of CCN1 mRNA from whole lung homogenates of explants of patients with IPF when compared to control failed donor lungs, and in alveolar mesenchymal cells isolated from patients with progressive IPF (4). Additionally, in this prior study, we proposed a pro-fibrotic role of CCN1 by augmentation of transforming growth factor-β1/mothers against decapentaplegic homolog (TGF-β1/SMAD) signaling (4). In this study, we sought to determine if CCN1 could be measured in circulating plasma of IPF subjects, and whether levels of this protein was predictive of disease progression and/or survival.
Methods
Clinical data and plasma samples from a cohort of 88 subjects with well-characterized IPF based on the ATS/ERS consensus criteria (5) as discussed in our multidisciplinary conference, were analyzed. Subjects were selected based on availability of stored plasma samples, collected between January 2009 and October 2013, and with a minimum of 15-month follow-up at the University of Alabama at Birmingham (UAB). The Institutional Review Board for Human Research at UAB approved this project. Measurements of forced vital capacity (FVC) and diffusion capacity for carbon monoxide (DLCO), expressed as percentages of predicted values (%FVC and %DLCO, respectively) were obtained. CCN1 levels were measured in plasma specimens by ELISA (R&D Systems, Minneapolis, MN).
The primary endpoint of the study was transplant-free survival (TFS), defined as the interval after plasma collection that subjects underwent lung transplantation or died from any cause. Descriptive statistics are presented as means ± SD, or as proportions for categorical variables. Continuous variables were compared using t test; Chi-square was used for categorical variables. To perform survival analyses, we dichotomized the study cohort based on the median CCN1 level (0.147 ng/ml) for our cohort; subjects were categorized into “high-CCN1” (≥0.147 ng/ml) or “low-CCN1” (<0.147 ng/ml) groups. Intergroup differences in time-to-event were evaluated by Kaplan-Meier survival analyses and log-rank tests. Cox proportional-hazards regression analyses were used to assess TFS, adjusting for %FVC and %DLCO. Statistical analyses were performed using SAS software™ (SAS 9.4).
Results
There are no significant differences in baseline characteristics among subjects stratified into groups by high and low levels of plasma CCN1 (Table). The mean age of subjects in the low-CCN1 group was 64 ± 15 years compared to 67 ± 8 years (p = 0.28) in the high-CCN1 group. 72% patients were current or former smokers in both groups. There are a higher number of male subjects in the high-CCN1 group (81% vs 61%, p = 0.03). %FVC and %DLCO at baseline did not differ between the low-CCN1 and high-CCN1 groups (67 ± 21 vs 62 ± 18, p = 0.38 and 49 ± 16 vs 45 ± 18, p = 0.31 respectively).
Table:
Demographics and baseline patient characteristics
| CCN1<0.147 ng/ml | CCN1 ≥0.147 ng/ml | p-value | |
|---|---|---|---|
| Age at diagnosis (years) | 64 + 15 | 67 + 8 | 0.28 |
| Gender (male) | 61% | 81% | 0.03 |
| Race (white) | 88% | 84% | 0.84 |
| Current/Former smoker | 72% | 72% | 1.00 |
| Definite UIP on HRCT | 62% | 74% | 0.22 |
| Surgical Lung Biopsy | 60% | 58% | 0.98 |
| %predicted FVC | 67 + 21 | 62 + 18 | 0.38 |
| %predicted DLCO | 49 + 16 | 45 + 18 | 0.31 |
Values in percent or plus–minus values are means ± SD.
FEV1: forced expiratory volume in one second; FVC: forced vital capacity; DLCO: diffusing capacity for carbon monoxide; UIP: usual interstitial pneumonia; HRCT: high resolution computed tomography of chest
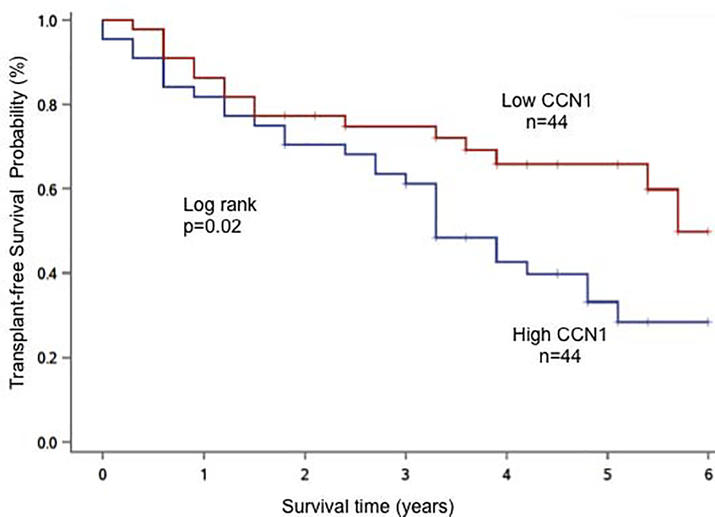
The median survival time for this IPF cohort was 4.8 years; 3.3 years for the high-CCN1 group, and 5.7 years for the low-CCN1 group. TFS was significantly worse in the high-CCN1 group compared to the low-CCN1 group (p = 0.02, log rank of Kaplan-Meier curve; Figure). Subjects with high plasma CCN1 levels had nearly a 2-fold higher risk of lung transplant or death compared to subjects with low plasma CCN1 (HR = 1.98; 95% CI 1.07–3.66, p = 0.03). Multivariate regression analyses that included adjustments for %FVC and DLCO% at the time of sample procurement similarly resulted in increased risk of lung transplant or death for the high-CCN1 group (HR = 2.15; 95%CI 1.04–4.45, p = 0.04).
Figure:
Transplant-free survival (TFS) was greater in IPF subjects with low plasma CCN1 levels compared to subjects with high plasma CCN1 levels. Cross-hatches denote censored events during the observation period.
Discussion
IPF has been increasingly recognized as a disease of aging (6). However, whether the biology of aging can inform prognosis and/or responsiveness to currently available anti-fibrotics is not known (7). The matricellular protein, CCN1, has been linked to induction of cellular senescence (1, 8). While CCN1 has consistently been shown to induce cellular senescence (1, 2), its effects have been proposed to be either anti-fibrotic (1) or pro-fibrotic (4) in pre-clinical animal models. Our own studies suggest that CCN1 may mediate its pro-fibrotic effects via enhanced TGF-β1/SMAD signaling at the cell surface (4).
The current study identifies elevated plasma levels of the matricellular protein, CCN1, among IPF patients with an increased risk of disease progression, as measured by death or requirement for lung transplantation. This observation suggests a biological role for CCN1 in IPF disease pathogenesis and progression. Whether high-CCN1 levels represent a sub-phenotype of IPF associated with accelerated aging remains to be determined; interestingly, in our cohort, mean age at time of sample collection between the low and high-CCN1 level groups was not statistically different. Of note, several recent studies have provided pre-clinical proof-of-concept that targeting cellular senescence may be beneficial in progressive lung fibrosis (9–11).
This is the first study, to our knowledge, that has evaluated the potential role of a senescence-associated matricellular protein in human subjects with IPF. The limitations of the current study are that the observations are from a single cohort and lack prospective, longitudinal imaging and lung function data. This preliminary report highlights the need for larger, prospective studies with stratification based on anti-fibrotic therapy to determine the potential utility of CCN1 as a biomarker of disease progression, and to identify distinct sub-phenotypes in this heterogeneous disease population. Additionally, personalized approaches to the treatment of IPF based on targeting cellular senescence and/or CCN1 deserves further study.
Highlights.
Cellular senescence is implicated in the pathogenesis of idiopathic pulmonary fibrosis
CCN1, a matricellular protein, has been shown to mediate senescence and fibrosis in preclinical animal models
High plasma levels of CCN1 protein may be associated with IPF progression
Acknowledgments
Funding source: This study was funded by National Institutes of Health grants, P01 HL114470 and R01 AG046210 (VJT), and VA Merit Award I01BX003056 (VJT)
Conflict of Interest: TK and TL have received speaker fees from Boehringer Ingelheim Pharmaceuticals, Inc, outside the submitted work. VJT has received research grants from the NIH and personal fees from Boehringer Ingelheim Pharmaceuticals, Inc, personal fees from Kadmon Corporation, grants from Genkyotex, outside the submitted work. JAD has received research grants from the NIH, Genentech, Boehringer Ingelheim, and Fibrogen; and consulting fees from Genentech, Boehringer Ingelheim, and Immuneworks, outside the submitted work. AK and YK have no conflicts of interest to disclose.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Jun JI, Lau LF. The matricellular protein CCN1 induces fibroblast senescence and restricts fibrosis in cutaneous wound healing. Nat Cell Biol 2010; 12: 676–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Du J, Klein JD, Hassounah F, Zhang J, Zhang C, Wang XH. Aging increases CCN1 expression leading to muscle senescence. Am J Physiol Cell Physiol 2014; 306: C28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim KH, Won JH, Cheng N, Lau LF. The matricellular protein CCN1 in tissue injury repair. J Cell Commun Signal 2018; 12: 273–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kurundkar AR, Kurundkar D, Rangarajan S, Locy ML, Zhou Y, Liu RM, Zmijewski J, Thannickal VJ. The matricellular protein CCN1 enhances TGF-beta1/SMAD3-dependent profibrotic signaling in fibroblasts and contributes to fibrogenic responses to lung injury. FASEB J 2016; 30: 2135–2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, Colby TV, Cordier JF, Flaherty KR, Lasky JA, Lynch DA, Ryu JH, Swigris JJ, Wells AU, Ancochea J, Bouros D, Carvalho C, Costabel U, Ebina M, Hansell DM, Johkoh T, Kim DS, King TE, Jr., Kondoh Y, Myers J, Muller NL, Nicholson AG, Richeldi L, Selman M, Dudden RF, Griss BS, Protzko SL, Schunemann HJ, Fibrosis AEJACoIP. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011; 183: 788–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thannickal VJ, Murthy M, Balch WE, Chandel NS, Meiners S, Eickelberg O, Selman M, Pardo A, White ES, Levy BD, Busse PJ, Tuder RM, Antony VB, Sznajder JI, Budinger GR. Blue journal conference. Aging and susceptibility to lung disease. Am J Respir Crit Care Med 2015; 191: 261–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thannickal VJ. Mechanistic links between aging and lung fibrosis. Biogerontology 2013; 14: 609–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jun JI, Lau LF. Cellular senescence controls fibrosis in wound healing. Aging (Albany NY) 2010; 2: 627–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hecker L, Logsdon NJ, Kurundkar D, Kurundkar A, Bernard K, Hock T, Meldrum E, Sanders YY, Thannickal VJ. Reversal of persistent fibrosis in aging by targeting Nox4-Nrf2 redox imbalance. Sci Transl Med 2014; 6: 231ra247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schafer MJ, White TA, Iijima K, Haak AJ, Ligresti G, Atkinson EJ, Oberg AL, Birch J, Salmonowicz H, Zhu Y, Mazula DL, Brooks RW, Fuhrmann-Stroissnigg H, Pirtskhalava T, Prakash YS, Tchkonia T, Robbins PD, Aubry MC, Passos JF, Kirkland JL, Tschumperlin DJ, Kita H, LeBrasseur NK. Cellular senescence mediates fibrotic pulmonary disease. Nat Commun 2017; 8: 14532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horowitz JC, Thannickal VJ. Mechanisms for the Resolution of Organ Fibrosis. Physiology (Bethesda) 2019; 34: 43–55. [DOI] [PMC free article] [PubMed] [Google Scholar]