Abstract
Background –
There is mounting evidence that long-term exposure to air pollution is related to accelerated cognitive decline in aging populations. Factors that influence individual susceptibility remain largely unknown, but may involve the apolipoprotein E genotype E4 (APOE-ε4) allele.
Objectives-
We assessed whether the association between long-term exposure to ambient air pollution and cognitive decline differed by APOE-ε4 status and cognitive risk factors.
Methods-
The Washington Heights Inwood Community Aging Project (WHICAP) is a prospective study of aging and dementia. Neuropsychological testing and medical examinations occur every 18–24 months. We used mixed-effects models to evaluate whether the association between markers of ambient air pollution (nitrogen dioxide [NO2]), fine [PM2.5], and coarse [PM10] particulate matter) and the rate of decline in global and domain-specific cognition differed across strata defined by APOE-ε4 genotypes and cognitive risk factors, adjusting for sociodemographic factors and temporal trends.
Results –
Among 4,821 participants with an average of 6 years follow-up, higher concentrations of ambient air pollution were associated with more rapid cognitive decline. This association was more pronounced among APOE-ε4 carriers (p<0.001). A one interquartile range increase in NO2 was associated with an additional decline of 0.09 standard deviations (SD) (95%CI −0.1, −0.06) in global cognition across biennial visits among APOE-ε4 positive individuals and a 0.07 SD (95%CI −0.09, −0.05) decline among APOE-ε4 negative individuals. Results for PM2.5, PM10 and cognitive domains were similar. The association between air pollutants and rate of cognitive decline also varied across strata of race-ethnicity with the association strongest among White non-Hispanic participants.
Conclusions-
These results add to the body of evidence on the adverse impact of ambient air pollution on cognitive aging and brain health and provide new insights into the genetic and behavioral factors that may impact individual susceptibility.
Keywords: Air Pollution, Cognitive Decline, Aging, Epidemiology, APOE-e4 allele, Cognitive Risk Factors
1.1. INTRODUCTION
Age-related cognitive decline is a growing public health concern as increases in life expectancy and the aging of the population are expected to substantially increase the prevalence of cognitive impairment and dementia.1,2 Approximately 5.8 million Americans live with dementia,3,4 withthe prevalence expected to rise to almost 14 million by 2050.5,6 The most common cause of dementia in older adults is Alzheimer disease (AD), accounting for between 60–70% of all dementia cases, but most patients have a mix of pathologies including AD, vascular dementia, and dementia with Lewy bodies.7–9 Poor cognitive function is the sixth leading cause of death in the United States and a key cause of disability among older adults and can have profound social, economic, and health implications.3,10 Global healthcare expenditures for cognitive impairment reached $818 billion in 2015 and are expected to reach a staggering two trillion dollars by 2030.6
The causes of dementia in the aging population are multi-faceted and are likely a combination of lifestyle, genetic, and environmental risk factors. Risk of accelerated cognitive decline increases with age, cerebrovascular disease, and the presence of traditional cardiovascular risk factors, but these factors do not fully account for risk of cognitive decline in the population. Currently, the strongest known genetic risk factor for AD and related dementias (ADRD) is the presence of the Apolipoprotein E genotype E4 (APOE-ε4) allele. There are multiple underlying mechanisms through which APOE-ε4 may impact cognitive function including neuroinflammation, amyloid-β (Aβ) plaque aggregation, and decreased vascular function.11–16
There is mounting evidence that environmental exposures including long-term exposure to ambient air pollution may have a detrimental effect on cognitive function in aging populations.17–22 In a previous publication we showed that estimates of ambient levels of nitrogen dioxide [NO2], fine [PM2.5], and coarse [PM10] particulate matter outside the residence were associated with cognitive decline in an older, multi-ethnic cohort of participants in northern Manhattan, New York City (NYC).23 As concern regarding the deleterious health effects of ambient air pollution grows, several biological mechanisms have been hypothesized to underlie the adverse effects of pollutants on the brain and cerebral vasculature, with the strongest evidence surrounding pathways of systemic inflammation and oxidative stress.24–28
Due to a shared inflammatory mechanism, a series of both animal and human studies have suggested that the effect of ambient air pollution on cognitive function may be more pronounced among individuals with the APOE-ε4 allele.26,29,30 To date, only two population-based studies have evaluated whether the association between residential air pollution and cognitive function differs by APOE-ε4, with both studies finding a stronger association among APOE-ε4 carriers.29,30 We investigated this relationship in a large, multi-ethnic cohort based in northern Manhattan, examining whether the previously observed association between ambient air pollution and rate of cognitive decline was stronger among individuals with at least one APOE-ε4 allele. We additionally examined whether the effects of ambient air pollution on rate of cognitive decline varied across strata of other established risk factors for accelerated cognitive decline.
2.1. MATERIALS AND METHODS
2.2. Study Sample.
The Washington Heights-Inwood Community Aging Project (WHICAP) is an ongoing, prospective, population-based study of aging and dementia. Established in three recruitment waves, the first wave of participants was recruited in 1992 from a random sample of Medicare-eligible adults (age ≥65 years) residing in the neighborhoods of Washington-Hamilton Heights and Inwood in northern Manhattan. The second and third waves were recruited from the same communities in 1999 and 2010, with a goal to recruit a cohort of ethnically and educationally diverse non-demented elderly based on the following goals: (1) the final sample would be equally divided among Hispanics, non-Hispanic blacks, and non-Hispanic whites, (2) the cohort would represent equal proportions of those 65–74 and ≥ 75 years old at enrollment, and (3) individuals would be excluded from participation if they had substantial cognitive problems, had been diagnosed with dementia, or did not speak English or Spanish. Participants are evaluated longitudinally every 18–24 months, with a comprehensive neuropsychological battery, medical and neurological examination, and survey about health-related behaviors, medication, comorbidities, and cardiovascular risk factors. A sub-sample of participants consented to a blood draw at enrollment and underwent genotyping to identify APOE status. The sampling strategies, recruitment outcomes, and examination methodology used in WHICAP have been published previously.31,32
To date, at least one neuropsychological examination has been collected on 6,261 older adults. The primary analytical sample for this study was comprised of individuals that, additionally: (1) consented to blood draw at enrollment for APOE genotyping, (2) had primary addresses in NYC, allowing for assessment of ambient air pollution levels at the residence, and (3) had no missing data for any of the confounding variables. These exclusion criteria resulted in a sample size of 4,821 individuals. Secondary analyses utilized individuals in the full WHICAP cohort (n=6,077), which included individuals with and without blood draw at enrollment.
All activities pertaining to WHICAP were approved by the Institutional Review Board at Columbia University Medical Center. Written informed consent was provided by each participant at enrollment.
2.3. Assessment of Residential Ambient Air Pollution.
Participants’ residential addresses at the time of the first neuropsychological evaluation (henceforth referred to as “enrollment”) were geocoded using Geosupport Batch Address Translator Desktop Edition (NYC Department of City Planning, NY, NY) (Figure 1).
Figure 1.
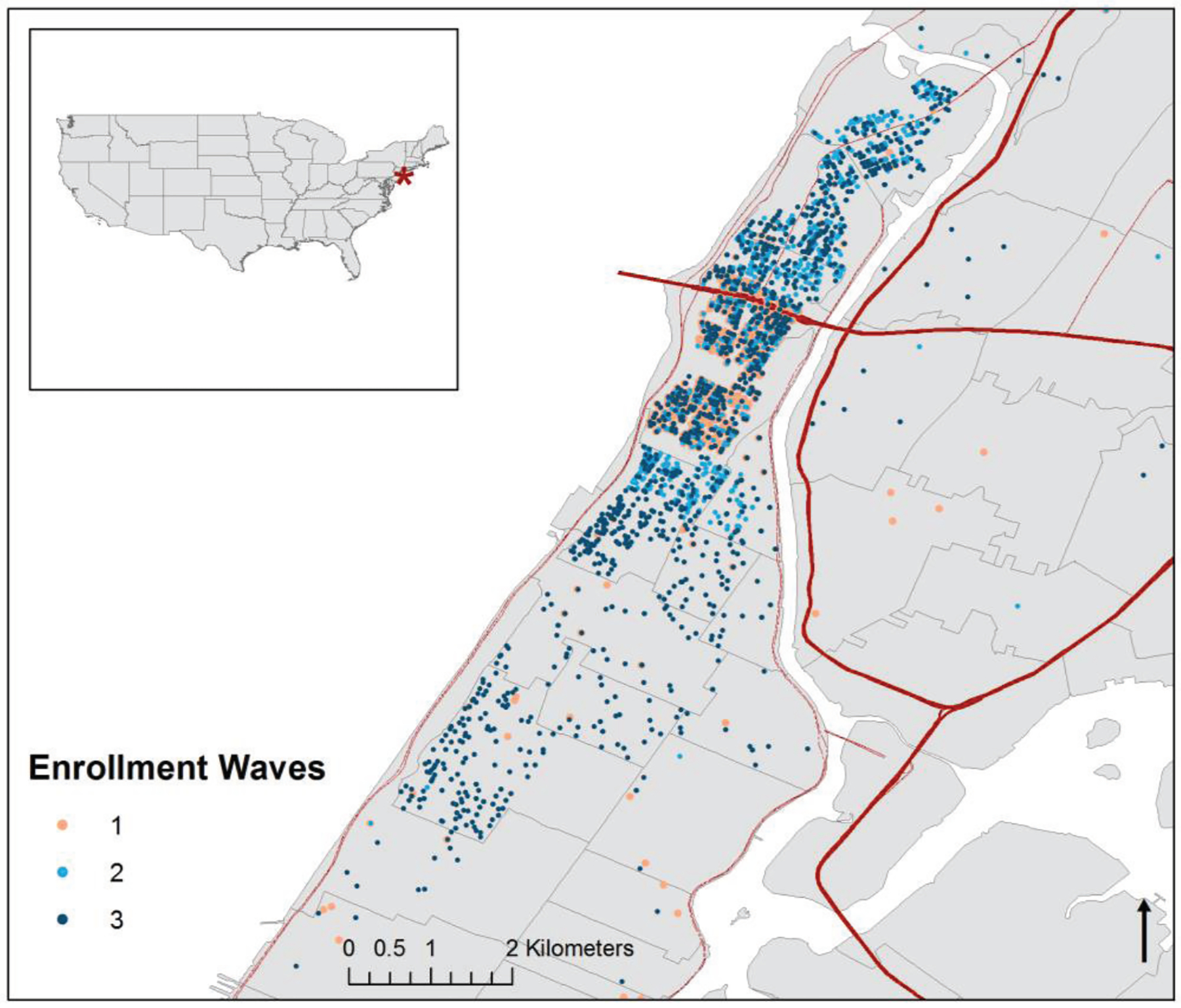
Residential Location at Enrollment of WHICAP Participants throughout Northern Manhattan, New York City.
We ascertained estimates of residential ambient air pollution levels in the calendar year prior to enrollment at each geocoded address using regionalized universal kriging models for nitrogen dioxide (NO2; ppb), fine particulate matter less than 2.5 μm in diameter (PM2.5; μg/m3), and respirable particulate matter (PM10; μg/m3), as previously described.33,34 Measurements of NO2, PM2.5, and PM10 were obtained from the U.S. Environmental Protection Agency (EPA) Air Quality System and annual average values were used in a universal kriging regression framework to predict concentrations at individual addresses. Partial least square methods were used to include geographic covariates (roadway density, population density, urban land, agricultural land, forests, bodies of water), land use, and roadway proximity to improve predictions. Additionally, the NO2 model incorporated satellite data to improve predictions.34
2.4. Outcome Ascertainment.
Neuropsychological test batteries used in WHICAP were designed to capture key cognitive domains in both English-speaking and Spanish-speaking older adults and developed to permit the calculation of domain-specific z-scores. A complete list of tests included is shown in Supplementary Table 1. As in previous studies,23 we constructed a composite global cognitive score by standardizing raw scores from all available neuropsychological tests into z-scores using cohort-specific means and standard deviations from enrollment wave. Z-scores for individual tests were then averaged to create an overall z-score. The primary outcome of this study was the change in global cognitive scores over time. We then considered the change over time in each of three individual functional domains (memory, executive function, and language), identified through factor analyses performed previously in the WHICAP Cohort.31 We expressed domain-specific scores as the mean of the individual test z-scores loading into each domain. We were unable to analyze the processing score domain as an individual functional domain because of model instability due to low response rate in tests which loaded into that domain. To enhance interpretability of the results, the global cognitive score and domain-specific scores were standard-normal transformed using means and standard deviations at enrollment, such that results reflect a change in outcome over time relative to the standard deviation of each outcome at enrollment. While some participants in this cohort had up to 13 neuropsychological examinations, given that recruitment spanned multiple waves over approximately 20 years, fewer than 10% of participants had data available from more than 6 exams. To ensure model stability, we limited our analyses to data from exams 1–6.
2.5. Covariates.
At time of enrollment, participants underwent in-person interviews in their primary language (English or Spanish) conducted by trained interviewers to assess sociodemographic characteristics, health status and risk factors using validated data collection instruments, physical, and neurological examinations.
Race-ethnicity was collected through self-identification using the format of the 2000 US Census. All individuals were first asked to report their racial group and then, in a second question, were asked whether they were of Hispanic origin. For the purpose of analysis, individuals were categorized into White non-Hispanic, Black non-Hispanic, Hispanic, and other. Education was collected through self-report as total years of education completed. Age was self-reported at time of neuropsychological assessment. We derived a summary z-score for socioeconomic status (SES) at the census tract level as a marker of neighborhood wealth, education, and occupation.35
DNA was extracted from blood samples taken at enrollment and the pattern of each individual’s APOE-ε4 isoforms was identified using the method of Hixson and Vernier, with slight modification.36,37 Individuals with one or more copies of the APOE-ε4 allele were considered to be APOE-ε4 positive, as in prior studies.38,39 Smoking status was obtained through self-report and dichotomized into never smokers versus former or current smokers for analysis.
2.6. Statistical Analysis.
Distributions of sociodemographic characteristics and cardiovascular risk factors were calculated as mean (± SD) for continuous variables and proportions (n (%)) for categorical variables. Estimates of pollutant exposure were presented as mean [interquartile range (IQR)].
We used a series of stabilized inverse probability weights (IPW) to account for possible selection bias due to both non-random selection into the sub-cohort of participants who opted in to genotyping and non-random loss to follow-up over time.40,41 To estimate IPW, we fit logistic regression models modeling selection from the full WHICAP cohort into the sub-cohort with APOE genotyping, predicting the probability that an individual would be selected into the sub-cohort. We regressed a binary indicator for study membership on a series of available time-invariant sociodemographic and health-related covariates (age, race-ethnicity, wave, dementia status at enrollment, neighborhood SES, diabetes, history of cardiac disease, and hypertension) that may have influenced an individual’s decision to undergo a blood draw at enrollment.
Stabilized inverse probability of censoring weights (IPCW) further accounted for non-random loss to follow-up in the sub-cohort over time. To estimate the IPCW, we fit pooled logistic models at each time point predicting the probability that an individual remained in the study up until that time point. At each time point we regressed a binary indicator for censorship on pollutant levels at enrollment as well as a series of available time-invariant sociodemographic covariates (sex, race-ethnicity, education, and neighborhood socioeconomic status) and a set of time-varying covariates that included age at the time of assessment and cognitive function at previous visit. The stabilized IPCW were calculated as the marginal probability of each individuals’ censorship status (yes or no) divided by the probability of each individual’s censorship status conditional on the set of time-invariant and time-varying covariates. We weighted the final analytical sample by the product of the IPW and IPCW weights. Using this method, individuals with a larger probability of not receiving genotyping and being lost to follow up would be weighted more heavily in the final analysis. The use of inverse probability weights results in a pseudo-population in which the censorship is marginally independent of treatment. IPW were created for each exposure and outcome combination to create a series of pseudo-populations for analysis. Secondary analyses completed in the full cohort were adjusted only by IPCW weights.
We used weighted linear mixed models for repeated measures to study the relationship of ambient air pollution to cognitive decline.42 We first fit separate models to estimate the associations of PM2.5, PM10, NO2, and APOE-ε4 status with longitudinal change in global cognition, memory domain scores, language domain scores, and executive function scores. All models were adjusted for visit number, visit by pollutant interaction, age, sex, race-ethnicity, education, neighborhood socioeconomic status, and an indicator for cohort wave to account for secular trends. The models, analyzed using PROC MIXED procedures, fitted participants as a random effect and used a compound symmetry covariance matrix.
To assess whether the association between ambient air pollution and cognitive decline differed across subgroups defined by APOE-ε4 status, we included three-way interaction terms between APOE-ε4 status, exposure measures, and visit number in a series of fully adjusted models for each of the four outcomes of interest. Interaction terms with a p-value <0.15 were considered potentially statistically significant. We calculated stratum-specific estimates to look at differences in the association between ambient air pollution and cognitive decline between APOE-ε4 positive and APOE-ε4 negative individuals. We further assessed whether the rate of cognitive change due to air pollution varied across subgroups of known risk factors for cognition (age, smoking status, race-ethnicity, and sex) using the same method as above. In secondary analyses, we repeated these analyses using the full WHICAP sample (n=6,077).
Previous studies have shown that the effect of the APOE-ε4 allele on the rate of cognitive decline differs by race-ethnicity.43 Since air pollution levels may also vary by race-ethnicity, in sensitivity analyses we further stratified the air pollution-cognition models by APOE-ε4 status within the race-ethnicity groups.
All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC).
3.1. RESULTS
Participants in the APOE cohort were predominately women (68%) with a median age of 76.3 (±6.6) years. Mean follow-up time for the cohort was 5.9±3.5 years. Half of participants self-identified as Hispanic (49%) and there was a high prevalence of traditional cardiovascular risk factors among participants. More than a quarter of participants (27.5%) of those genotyped carried an APOE-e4 allele, with the prevalence of the allele highest in Black non-Hispanic participants. At the end of six follow up visits, 1,743 (36%) of the cohort had died and 2,279 (47%) were censored for other reasons (Supplemental Table 2). Mean [IQR] annual estimates of ambient air pollution were 13.5 [4.42] μg/m3 for PM2.5, 21.8 [7.95] μg/m3 PM10, and 33.0 [11.2] ppb NO2 (Table 1). There were no substantial differences in characteristics of participants of the APOE cohort and the full cohort (Supplemental Table 3). Residential air pollution levels did not vary across categories of potential effect modifiers (Supplemental Figure 1).
Table 1.
Characteristics of the WHICAP APOE cohort at enrollment, stratified by APOE-e4 status
| APOE Cohort1 (n=4,821) | APOE-e4 Positive2 (n=1,327) | APOE-e4 Negative (n=3494) | |
|---|---|---|---|
| Sociodemographic Characteristics | Mean [SD] or n (%) | ||
| Age, y | 76.3 [6.6] | 75.9 [6.4] | 76.4 [6.7] |
| Men | 1555 (32.3) | 913 (31.2) | 1141 (32.7) |
| Race-ethnicity | |||
| White non-Hispanic | 1055 (21.9) | 240 (18.1) | 815 (23.3) |
| Black non-Hispanic | 1375 (28.5) | 485 (36.6) | 890 (25.5) |
| Hispanic | 2339 (48.5) | 590 (44.5) | 1749 (50.1) |
| Years of Education | 9.30 [4.95] | 9.29 [4.93] | 9.30 [4.96] |
| Census Z-Score | −3.21 [3.26] | −3.32 [3.17] | −3.17 [3.30] |
| Recruitment Wave | |||
| Wave 1 (1992) | 1457 (30.2) | 423 (31.9) | 1034 (29.6) |
| Wave 2 (1999) | 1877 (38.9) | 516 (38.9) | 1361 (39.0) |
| Wave 3 (2010) | 1487 (30.8) | 388 (29.2) | 1099 (31.5) |
| Cardiovascular Risk Factors | |||
| Smoking Status | |||
| Current or Former | 2006 (41.6) | 583 (43.9) | 1423 (40.7) |
| Never | 2815 (58.4) | 744 (56.1) | 2071 (59.3) |
| Hypertension3 | 3868 (80.2) | 1072 (80.8) | 2796 (80.0) |
| Diabetes4 | 1399 (29.0) | 331 (24.9) | 1068 (30.6) |
| History of Cardiac Disease | 1824 (37.8) | 508 (38.3) | 1316 (37.7) |
| APOE-ε4 positive5 | 1327 (27.5) | 1327 (100) | 0 (0) |
| Diagnosis of Dementia | 509 (10.6) | 178 (13.4) | 331 (9.5) |
| Residential Pollutant Levels | Mean [IQR] | ||
| NO2 (ppb) | 33.0 [11.2] | 33.4 [10.5] | 32.9 [11.4] |
| PM2.5 (μg/m3) | 13.5 [4.42] | 13.6 [4.10] | 13.4 [4.51] |
| PM10 (μg/m3) | 21.8 [7.95] | 22.2 [8.00] | 21.7 [7.97] |
IQR indicates interquartile range.
Individuals who consented to blood draw at enrollment
Individuals with at least one copy of the APOE-ε4 allele considered positive
Hypertension = systolic blood pressure > 140 mm/Hg, diastolic blood pressure recording >90 mm/Hg (based on the average of two measurements), physician diagnosis, or self-report,
Diabetes=fasting blood glucose ≥ 126 mg/dL, self-report, insulin, or hypoglycemic use
As expected, both ambient air pollution and APOE-ε4 status were associated with faster rates of cognitive decline over time (Table 2), with similar results across pollutants and cognitive domains. The association between air pollution and cognitive decline were similar in the APOE and full cohorts (Supplemental Table 4).
Table 2.
Associations between Residential Levels of Ambient Air Pollutants and APOE-ε4 Status on Cognitive Decline
| NO2 | PM2.5 | PM10 | APOE-ε4 | |||||
|---|---|---|---|---|---|---|---|---|
| Change in Cognitive Scores1 | 95% CI | Change in Cognitive Scores1 | 95% CI | Change in Cognitive Scores1 | 95% CI | Change in Cognitive Scores2 | 95% CI | |
| Global Cognition | −0.075 | −0.10, −0.05 | −0.093 | −0.12, −0.07 | −0.046 | −0.06, −0.03 | −0.048 | −0.07, −0.03 |
| Memory Domain | −0.037 | −0.06, −0.01 | −0.047 | −0.08, −0.02 | −0.022 | −0.04, −0.003 | −0.049 | −0.05, −0.05 |
| Language Domain | −0.055 | −0.08, −0.03 | −0.066 | −0.10, −0.03 | −0.025 | −0.04, −0.01 | −0.059 | −0.08, −0.03 |
| Executive Function | −0.031 | −0.06, −0.01 | −0.051 | −0.08, −0.02 | −0.023 | −0.04, −0.01 | −0.040 | −0.06, −0.02 |
All models adjusted for individual (age, education, sex, race/ethnicity), neighborhood sociodemographic variables (Census based SES z-score), and a cohort indicator to adjust for secular trends. All models weighted by the product of the IPW and IPCW weights.
Expressed as a standard deviation change in the rate of decline in cognitive score associated with an IQR change in pollutant.
Expressed as a standard deviation change in the rate of decline in cognitive score associated with being APOE-ε4 positive
We assessed whether the association between air pollution and cognitive decline varied across levels of APOE-ε4 status and found that NO2, PM2.5, and PM10 were each associated with a statistically significantly faster rate of cognitive decline among APOE-ε4 positive versus negative individuals (Figure 2, Table 3). For example, an IQR shift in NO2 was associated with a decline of −0.09 SD (95% CI −0.11, −0.06) in global cognitive score across biennial visits among APOE-ε4 positive individuals and a −0.07 SD (95% CI −0.09, −0.05) decline among APOE-ε4 negative individuals (p-value for interaction: <0.001). This pattern was consistent across all measures of ambient air pollution and all cognitive function domains.
Figure 2.
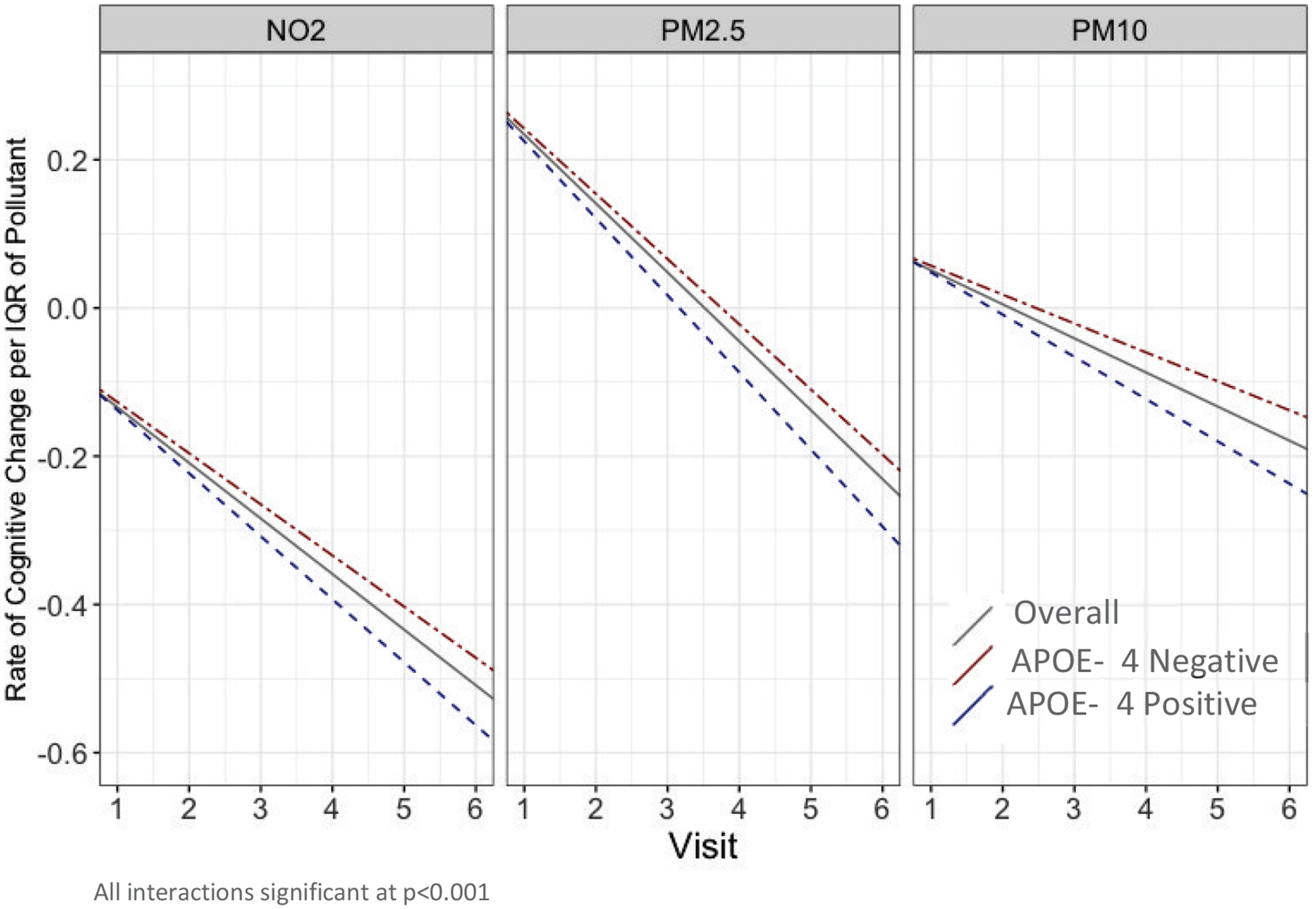
Associations between Ambient Air Pollution and Global Cognitive Decline by APOE-ε4 Status.
Table 3.
Association between Ambient Air Pollution and Cognitive Decline by APOE-ε4 status
| NO2 | PM2.5 | PM10 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Change in Cognitive Scores1 | 95% CI | p-value2 | Change in Cognitive Scores1 | 95% CI | p-value2 | Change in Cognitive Scores1 | 95% CI | p-value2 | |
| Global Cognitive Score | |||||||||
| APOE-ε4 − | −0.069 | −0.09, −0.05 | <0.001 | −0.088 | −0.12, −0.06 | <0.001 | −0.039 | −0.06, −0.02 | <0.001 |
| APOE-ε4 + | −0.085 | −0.11, −0.06 | −0.104 | −0.13, −0.08 | −0.057 | −0.07, −0.04 | |||
| Memory Domain | |||||||||
| APOE-ε4 − | −0.033 | −0.06, −0.01 | 0.03 | −0.043 | −0.07, −0.01 | 0.02 | −0.018 | −0.04, 0.001 | 0.02 |
| APOE-ε4 + | −0.043 | −0.07, −0.02 | −0.053 | −0.09, −0.02 | −0.029 | −0.05, −0.01 | |||
| Executive Function Domain | |||||||||
| APOE-ε4 − | −0.025 | −0.05, 0.001 | <0.001 | −0.047 | −0.08, −0.02 | <0.01 | −0.018 | −0.04, 0.003 | <0.001 |
| APOE-ε4 + | −0.040 | −0.07, −0.01 | −0.061 | −0.09, −0.03 | −0.033 | −0.05, −0.01 | |||
| Language Domain | |||||||||
| APOE-ε4 − | −0.046 | −0.07, −0.02 | <0.001 | −0.059 | −0.09, −0.03 | <0.001 | −0.017 | −0.04, 0.001 | <0.001 |
| APOE-ε4 + | −0.066 | −0.09, −0.04 | −0.078 | −0.11, −0.05 | −0.038 | −0.06, −0.02 | |||
All models adjusted for individual (age, education, sex, race/ethnicity), neighborhood sociodemographic variables (Census based SES z-score), and a cohort indicator to adjust for secular trends. All models weighted by the product of the IPW and IPCW weights.
Expressed as a standard deviation change in the rate of decline in cognitive score associated with an IQR change in pollutant
p-values for cross-product terms for interaction in the association of air pollutants and cognition
We examined whether the association between residential air pollution and cognitive function differed across subgroups of participants with other risk factors of cognitive decline, specifically age at baseline, race-ethnicity, sex, and smoking status (Table 4). Of these risk factors, the association between ambient air pollution and rate of decline in global cognitive score differed only across strata of race-ethnicity, with less rapid pollution-associated decline in global cognitive function observed among Hispanics as compared to White non-Hispanic and Black non-Hispanic participants (p-value for interaction 0.02). Results were similar across pollutants. Results were similar when considering individual functional domains, where the associations between ambient air pollution and memory and language domain-specific declines were stronger among non-Hispanic individuals. In addition, the associations between pollution and memory and language domain-specific decline were stronger among participants greater than 75 years of age. There were no significant variations across sub-groups in effect modification in the executive function domain.(Supplemental Table 5). In the full WHICAP cohort, we also saw effect measure modification by age across all cognitive domains, but saw no differences in association between ambient air pollution and cognitive decline across racial-ethnic groups (Supplemental Table 6).
Table 4.
Association between Ambient Air Pollution and Global Cognitive Decline Across Strata of Risk Factors for Cognitive Decline
| NO2 | PM2.5 | PM10 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Change in Cognitive Scores1 | 95% CI | p-value2 | Change in Cognitive Scores1 | 95% CI | p-value2 | Change in Cognitive Scores1 | 95% CI | p-value2 | |
| Age | |||||||||
| < 75 yrs old | −0.080 | −0.11, −0.05 | 0.42 | −0.115 | −0.15, −0.08 | 0.62 | −0.038 | −0.06, −0.02 | 0.22 |
| ≥ 75 yrs old | −0.083 | −0.11, −0.06 | −0.117 | −0.15, −0.09 | −0.043 | −0.06, −0.02 | |||
| Smoking Status | |||||||||
| Never Smoker | −0.076 | −0.10, −0.05 | 0.32 | −0.094 | −0.12, −0.07 | 0.61 | −0.048 | −0.07, −0.03 | 0.13 |
| Former/Current Smoker | −0.072 | −0.10, −0.05 | −0.092 | −0.12, −0.06 | −0.042 | −0.06, −0.03 | |||
| Race-ethnicity | |||||||||
| White non-Hispanic | −0.144 | −0.19, −0.09 | --- | −0.171 | −0.23, −0.11 | --- | −0.087 | −0.13, −0.05 | --- |
| Black non-Hispanic | −0.110 | −0.16, −0.06 | 0.14 | −0.136 | −0.20, −0.08 | 0.33 | −0.058 | −0.09, −0.02 | 0.26 |
| Hispanic | −0.045 | −0.08, −0.01 | 0.02 | −0.050 | −0.09, −0.01 | 0.08 | −0.029 | −0.05, −0.01 | 0.04 |
| Sex | |||||||||
| Male | −0.08 | −0.10, −0.05 | 0.27 | −0.091 | −0.12, −0.07 | 0.39 | −0.047 | −0.06, −0.03 | 0.22 |
| Female | −0.07 | −0.10, −0.05 | −0.094 | −0.12, −0.06 | −0.042 | −0.06. −0.02 | |||
All models adjusted for individual (age, education, sex, race/ethnicity), neighborhood sociodemographic variables (Census based SES z-score), and a cohort indicator to adjust for secular trends. All models weighted by the product of the IPW and IPCW weights.
Expressed as a standard deviation change in the rate of decline in cognitive score associated with an IQR change in pollutant
p-values for cross-product terms for interaction in the association of air pollutants and cognition
In sensitivity analyses where the air pollution-cognition models were stratified by APOE-ε4 status within race-ethnic groups, we found these relationships were consistent in direction overall, but varied slightly by race-ethnicity. In contrast to relationships in the overall population, we saw no effect modification between APOE-ε4 and individual pollutants among non-Hispanic Black participants. (Supplemental Table 7).
4.1. DISCUSSION
In a multiethnic prospective cohort of older residents in an urban environment, we found that residential ambient air pollution was associated with a faster rate of cognitive decline among individuals with at least one copy of the APOE-ε4 allele. Results were similar across pollutants considered and across functional domains of cognition. We also saw more rapid pollution-associated cognitive decline among non-Hispanic individuals as compared to Hispanic participants.
Several biological mechanisms behind the adverse effects of air pollution on the brain and cerebral vasculature have been proposed, with the strongest evidence surrounding pathways of systemic inflammation and oxidative stress. A series of experimental animal studies indicate that ambient Particles may affect the central nervous system either through a systemic response via the circulatory system, or intra-nasally by direct translocation to the brain through the olfactory bulb.44–46 Once in the nervous system pollutant particles activate a series of systemic inflammatory pathways leading to vascular inflammation,24–26 impaired microvascular reactivity,47 and changes in cerebral hemodynamics.48 Further evidence of these mechanisms comes from a series of studies done in Mexico City where strong histological evidence of cerebral microvascular damage, systemic inflammatory markers, and brain pathology has been observed in autopsied brains of dogs and children residing in high versus low pollutant areas.27,28
Currently, the strongest known genetic risk factor for cognitive decline and dementia is the presence of the APOE-ε4 allele. There are multiple underlying mechanisms through which APOE-ε4 may affect cognitive function. APOE-ε4 has been shown to increase the risk of atherosclerosis and stroke due to a build-up of cholesterol in the vessels, making it a risk factor for vascular impairment and dementia.11–13 Inside the brain, the APOE-ε4 protein has been shown to be less effective than APOE-ε2 and APOE-ε3 in clearing amyloid-β (Aβ) plaques, leading to Aβ aggregation and tangle formation, brain atrophy, neuroinflammation, and decreased vascular function.11–16 Due to a shared inflammatory mechanism between air pollution and APOE-ε4, a series of both animal and human studies have suggested that APOE-ε4 genotypes modify the association between ambient air pollution and cognitive function. An earlier study of autopsied brains suggested that APOE-ε4 carriers could be at higher risk for developing AD if they are exposed to higher levels of air pollutants by showing that APOE-ε4 carriers living in highly polluted areas of Mexico City had accelerated amyloid plaque accumulation as compared to non-carriers.26 Cacciottolo et al. found evidence that the detrimental effect of air pollution on both neurodegenerative changes in mice and cognitive decline in older women was stronger among carriers of the APOE-ε4 allele.29 Similar results were found in a study of older women in Germany, where exposure to air pollution was associated with poorer cognition only among APOE-ε4 carriers.30 Consistent with the results of earlier studies, we observed evidence of a differential association between air pollution and cognitive decline in models stratified by APOE-ε4 status.
Additionally, earlier work done in the WHICAP cohort indicated that the effect of the APOE-ε4 allele on cognition varied by racial-ethnic groups.43 We further stratified our analyses by race-ethnicity, acknowledging we may have had limited power to detect effects, and saw no effect modification between APOE-ε4 and individual pollutants among non-Hispanic Black participants. This is consistent with prior research which showed that differences in the APOE-ε4 genotype more strongly influenced the risk of AD in non-Hispanic White and Hispanic individuals. In addition, the overall effects of air pollution on cognitive decline were different by race-ethnicity, where the associations were strongest among non-Hispanic white participants. Differential cognitive function by race-ethnicity is not unique to this study, earlier cross-sectional studies have shown that lower mean global cognitive scores in may reflect inequalities such as educational experience, occupational opportunities, and racism that may lead to late-life differences in cognition.49–53 Similarly, in the WHICAP cohort, we saw that at baseline, white non-Hispanics had the highest global cognitive scores, followed by black non-Hispanics and Hispanics (data not shown). Consensus around the impacts of these early life experiences on cognitive decline are more heterogenous, however, with some studies showing little impact on overall cognitive function over time51,54 and others showing substantial influences on trajectories of cognitive decline.50 While we saw significant differences on the impact of ambient air pollution on cognitive decline across racial-ethnic groups, further studies should be done to assess the impact of air pollution in the broader context of these other experiences.
In addition to genetic factors like the presence of the APOE-ε4 allele, age is one of the most well known risk factors for cognitive decline.3,14,15 In our study, age also acted as an effect modifier with the association between air pollution and cognitive decline stronger among individuals greater than 75 years old at enrollment. Our results are contrary to the results of an earlier study, which found that living 50 meters from a high traffic road was associated with lower Consortium to Establish a Registry for Alzheimer’s Disease (CERAD-plus) scores only in women <74 years old, with no association in those older than 74 years old.55 A limitation of that study, however, is the sample size of women older than 74 years old living within 50 meters of a high traffic roadway was very small (n=7) and may have been due to selection bias of cognitively impaired women leaving the study.55 While our study attempted to address these limitations by using IPW weighting to adjust for selection bias, it is clear more research is needed to address whether the association between air pollution and cognitive function differs by age.
We did not find differential associations by sex or smoking status. These results are in contrast to what was found in the Health and Retirement study, in which current smokers were found to have worse cognitive function than non-smokers in specific quartiles of exposure.56 There are several substantial differences between the two studies, however, including definition and categorization of exposure and type of neuropsychological testing used that may be causing the inconsistent results. An earlier study found that smoking acted as an effect modifier between residential distance to roadway and incident ischemic stroke in the Northern Manhattan Stroke Study , where the association between proximity to roadways and ischemic stroke was significantly stronger among non-smokers.57 Air pollution has been shown to be associated with many known shared risk factors for both stroke and cognitive decline such as cardiovascular diseases58–63, greater carotid atherosclerotic burden64,65, and vascular risk factors66,67. It may also be possible that the association of air pollution and cognition are mediated through these cardiovascular mechanisms and future studies should begin to examine whether these risk factors are mediating both diseases through a similar pathway.
Our study had several important limitations. First, the study area may have limited variability in pollutant levels across the study area or across time, potentially limiting our statistical power to detect meaningful associations of smaller magnitude. In addition, we utilized regional models developed for the eastern United States and not optimized for our smaller study area. On the other hand, the urban study area is also a strength since this is one of the few studies to focus primarily on intra-urban variation in measures of ambient air pollution, perhaps reducing confounding by factors that vary between cities. In addition, although we adjusted for neighborhood and individual-level measures of SES in our analysis, we were unable to adjust for individual income levels. Second, the estimates of residential air pollution did not include data on time spent in locations outside the home or measure lifetime or occupational exposure. While the majority of participants were retired at the time of the study, there is limited data on lifetime workplace pollution exposures. Occupational exposures seem unlikely to be associated with residential outdoor levels of air pollutants, and thus unlikely to confound the analyses.
Third, similar to the prevalence in the overall population, the percentage of individuals with homozygous ε4 alleles is very low in the WHICAP cohort and therefore individuals heterozygous and homozygous for the ε4 allele were combined into a single group for the purpose of analysis, as done in prior studies.38,39 The odds of developing ADRD among heterozygous and homozygous carriers is substantially different; individuals heterozygous for the ε4 allele have between 2–4 fold increased odds of developing ADRD, while homozygous individuals have been shown to have a 5 to 34 fold increased odds of developing the disease.68,69 Within the group of APOE-ε4 positive individuals in this study, there may be heterogenous effects of the association of air pollution and cognitive function due to the differences in odds of developing dementia between individuals heterozygous and homozygous for the ε4 allele. In addition, this study analyzed the association between air pollution and cognitive decline, without including data on pathological causes of decline. Future studies should examine etiologies of dementia to further understand mechanisms of action. A final limitation is the potential for unmeasured confounders in the association between ambient air pollution and cognitive decline. We have consistently shown a stronger association between air pollution and cognitive decline in the APOE cohort as compared to the full WHICAP population despite using IPW to mitigate selection bias. We have looked extensively at potential differences between the populations and have found no substantial differences suggesting we still haven’t fully accounted for the probability of consenting to a blood draw at enrollment.
A key strength of this study is the user of a large, prospective cohort which allowed for the evaluation of multi-dimensional neuropsychological data in a diverse population in northern Manhattan as well as the use of individual assignment of air pollution measures to participants’ residential address. To our knowledge, this is the first study to test whether APOE genotypes interact with air pollution on cognition in a large, multi-ethnic population. Earlier studies have shown that prevalence of cognitive decline and dementia vary by sex and race-ethnic group,4,70 therefore it is important to have a racially and ethnically diverse population of older adults that is not limited by sex to be able to ascertain differences in higher risk segments of the population.
These results further support the current evidence on the role of air pollution on accelerated cognitive aging and brain health; however, the evidence behind effect modification of the relationship between air pollution and cognition is still very limited. Future studies should pay special attention to potential effect modifiers largely to identify potentially vulnerable populations that may be at highest risk for harmful health effects due to air pollution.
Supplementary Material
Highlights.
Ambient air pollution is associated with more rapid cognitive decline in older adults
APOE-ε4 positive individuals had more rapid pollution-associated cognitive decline
The association was also stronger among Non-Hispanic individuals
No difference in strength of association between age groups, sex, or smoking status
Acknowledgements
This manuscript has been reviewed by WHICAP investigators for scientific content and consistency of data interpretation with previous WHICAP Study publications. We acknowledge the WHICAP study participants and the WHICAP research and support staff for their contributions to this study.
FUNDING: This work was supported by the National Institutes of Health’s National Institute on Aging [PO1AG07232, R01AG037212, RF1AG054023], National Center for Advancing Translational Sciences [UL1TR001873], National Heart, Lung, and Blood Institute [T32HL134625], and National Institute of Environmental Health Sciences [R01-ES020871, P30-ES007033]; and Environmental Protection Agency Grants RD-831697 and RD-83830001. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or EPA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
REFERENCES
- 1.Ferri CP, Prince M, Brayne C, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366:2112–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9:63–75.e2. [DOI] [PubMed] [Google Scholar]
- 3.Alzheimer’s Association. 2019 Alzheimer’s Disease Facts and Figures. Alzheimers Dement. 2019;15:321–387. [Google Scholar]
- 4.Plassman BL, Langa KM, Fisher GG, et al. Prevalence of dementia in the United States: the aging, demographics, and memory study. Neuroepidemiology. Karger Publishers; 2007;29:125–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hebert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. American Academy of Neurology; 2013;80:1778–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prince M, Wimo A, Guerchet M, Ali G-C, Wu Y-T, Prina M. World Alzheimer Report 2015 The Global Impact of Dementia: An analysis of prevalence, incidence, cost and trends. London; 2015. [Google Scholar]
- 7.National Institute on Aging. What causes Alzheimer’s disease? 2017.
- 8.World Health Organization. Dementia: Fact sheet. 2017.
- 9.Alzheimer’s Research UK: Dementia Statistics Hub. Different types of dementia | Dementia Statistics Hub [online]. Accessed at: https://www.dementiastatistics.org/statistics/different-types-of-dementia/. Accessed September 28, 2019. [Google Scholar]
- 10.Sosa-Ortiz AL, Acosta-Castillo I, Prince MJ. Epidemiology of dementias and Alzheimer’s disease. Arch Med Res. 2012;43:600–608. [DOI] [PubMed] [Google Scholar]
- 11.Liu C-C, Liu C-C, Kanekiyo T, Xu H, Bu G. Apolipoprotein E and Alzheimer disease: risk, mechanisms and therapy. Nat Rev Neurol. 2013;9:106–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dwyer R, Skrobot OA, Dwyer J, Munafo M, Kehoe PG. Using Alzgene-Like Approaches to Investigate Susceptibility Genes for Vascular Cognitive Impairment. J Alzheimer’s Dis. 2013;34:145–154. [DOI] [PubMed] [Google Scholar]
- 13.Sun J-H, Tan LL, Wang H-F, et al. Genetics of Vascular Dementia: Systematic Review and Meta-Analysis. J Alzheimer’s Dis. 2015;46:611–629. [DOI] [PubMed] [Google Scholar]
- 14.Daviglus ML, Plassman BL, Pirzada A, et al. Risk factors and preventive interventions for Alzheimer disease: state of the science. Arch Neurol. American Medical Association; 2011;68:1185–1190. [DOI] [PubMed] [Google Scholar]
- 15.Daviglus ML, Bell CC, Berrettini W, et al. National Institutes of Health State-of-the-Science Conference statement: preventing alzheimer disease and cognitive decline. Ann Intern Med. American College of Physicians; 2010;153:176–181. [DOI] [PubMed] [Google Scholar]
- 16.Poirier J, Bertrand P, Poirier J, et al. Apolipoprotein E polymorphism and Alzheimer’s disease. Lancet. 1993;342:697–699. [DOI] [PubMed] [Google Scholar]
- 17.Power MC, Weisskopf MG, Alexeeff SE, Coull BA, Spiro A, Schwartz J. Traffic-related air pollution and cognitive function in a cohort of older men. Environ Health Perspect. 2011;119:682–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weuve J, Puett RC, Schwartz J, Yanosky JD, Laden F, Grodstein F. Exposure to particulate air pollution and cognitive decline in older women. Arch Intern Med. 2012;172:219–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wellenius GA, Boyle LD, Coull BA, et al. Residential proximity to nearest major roadway and cognitive function in community-dwelling seniors: results from the MOBILIZE Boston Study. J Am Geriatr Soc. 2012;60:2075–2080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kioumourtzoglou M-A, Schwartz JD, Weisskopf MG, et al. Long-term PM2.5 Exposure and Neurological Hospital Admissions in the Northeastern United States. Environ Health Perspect. 2016;124:23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tzivian L, Jokisch M, Winkler A, et al. Associations of long-term exposure to air pollution and road traffic noise with cognitive function—An analysis of effect measure modification. Environ Int. 2017;103:30–38. [DOI] [PubMed] [Google Scholar]
- 22.Ailshire JA, Clarke P. Fine particulate matter air pollution and cognitive function among U.S. older adults. J Gerontol B Psychol Sci Soc Sci. Oxford University Press; 2015;70:322–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kulick ER, Wellenius GA, Boehme AK, et al. Long-term Exposure to Air Pollution and Trajectories of Cognitive Decline Among Older Adults in Northern Manhattan. Revis Neurol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Campbell A, Oldham M, Becaria A, et al. Particulate matter in polluted air may increase biomarkers of inflammation in mouse brain. Neurotoxicology. 2005;26:133–140. [DOI] [PubMed] [Google Scholar]
- 25.Levesque S, Taetzsch T, Lull ME, et al. Diesel exhaust activates and primes microglia: air pollution, neuroinflammation, and regulation of dopaminergic neurotoxicity. Environ Health Perspect. 2011;119:1149–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Calderón-Garcidueñas L, Solt AC, Henríquez-Roldán C, et al. Long-term air pollution exposure is associated with neuroinflammation, an altered innate immune response, disruption of the blood-brain barrier, ultrafine particulate deposition, and accumulation of amyloid beta-42 and alpha-synuclein in children and youn. Toxicol Pathol. SAGE Publications; 2008;36:289–310. [DOI] [PubMed] [Google Scholar]
- 27.Calderón-Garcidueñas L, Reynoso-Robles R, Vargas-Martínez J, et al. Prefrontal white matter pathology in air pollution exposed Mexico City young urbanites and their potential impact on neurovascular unit dysfunction and the development of Alzheimer’s disease. Environ Res. 2016;146:404–417. [DOI] [PubMed] [Google Scholar]
- 28.Calderón-Garcidueñas L, Mora-Tiscareño A, Styner M, et al. White matter hyperintensities, systemic inflammation, brain growth, and cognitive functions in children exposed to air pollution. J Alzheimer’s Dis. IOS Press; 2012;31:183–191. [DOI] [PubMed] [Google Scholar]
- 29.Cacciottolo M, Wang X, Driscoll I, et al. Particulate air pollutants, APOE alleles and their contributions to cognitive impairment in older women and to amyloidogenesis in experimental models. Transl Psychiatry. 2017;7:e1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schikowski T, Vossoughi M, Vierkötter A, et al. Association of air pollution with cognitive functions and its modification by APOE gene variants in elderly women. Environ Res [online serial]. 2015;142:10–16. Accessed at: https://linkinghub.elsevier.com/retrieve/pii/S001393511500184X. [DOI] [PubMed] [Google Scholar]
- 31.Manly JJ, Bell-Mcginty S, Tang M-X, Schupf N, Stern Y, Mayeux R. Implementing Diagnostic Criteria and Estimating Frequency of Mild Cognitive Impairment in an Urban Community. Arch Neurol. 2005;62:1739–1746. [DOI] [PubMed] [Google Scholar]
- 32.Tang MX, Cross P, Andrews H, et al. Incidence of AD in African-Americans, Caribbean Hispanics, and Caucasians in northern Manhattan. Neurology. Lippincott Williams & Wilkins; 2001;56:49–56. [DOI] [PubMed] [Google Scholar]
- 33.Sampson PD, Richards M, Szpiro AA, et al. A regionalized national universal kriging model using Partial Least Squares regression for estimating annual PM2.5 concentrations in epidemiology. Atmos Environ (1994). 2013;75:383–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Young MT, Bechle MJ, Sampson PD, et al. Satellite-Based NO2 and Model Validation in a National Prediction Model Based on Universal Kriging and Land-Use Regression. Environ Sci Technol. 2016;50:3686–3694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:99–106. [DOI] [PubMed] [Google Scholar]
- 36.Hixson JE. Apolipoprotein E polymorphisms affect atherosclerosis in young males. Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Research Group. Arterioscler Thromb Vasc Biol. 1991;11. [DOI] [PubMed] [Google Scholar]
- 37.Mayeux R, Ottman R, Maestre G, et al. Synergistic effects of traumatic head injury and apolipoprotein-epsilon 4 in patients with Alzheimer’s disease. Neurology [online serial]. 1995;45:555–557. Accessed at: http://www.ncbi.nlm.nih.gov/pubmed/7898715. Accessed July 25, 2019. [DOI] [PubMed] [Google Scholar]
- 38.Cosentino S, Scarmeas N, Helzner E, et al. APOE epsilon 4 allele predicts faster cognitive decline in mild Alzheimer disease. Neurology. 2008;70:1842–1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsapanou A, Scarmeas N, Gu Y, et al. Data from a cross-sectional study on Apolipoprotein E (APOE-ε4) and snoring/sleep apnea in non-demented older adults. Data Br. 2015;5:351–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Howe CJ, Cole SR, Lau B, Napravnik S, Eron JJ. Selection Bias Due to Loss to Follow Up in Cohort Studies. Epidemiology. 2016;27:91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hernán MA, McAdams M, McGrath N, Lanoy E, Costagliola D. Observation plans in longitudinal studies with time-varying treatments. Stat Methods Med Res. 2009;18:27–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Laird NM, Ware JH. Random-Effects Models for Longitudinal Data Author(s). Biometrics. 1982;38:963–974. [PubMed] [Google Scholar]
- 43.Tang M-X, Maestre G, Tsai W-Y, et al. Relative Risk of Alzheimer Disease and Age-at-Onset Distributions, Based on APOE Genotypes among Elderly African Americans, Caucasians, and Hispanics in New York City. Am J Hum Genet. 1996;58:574–584. [PMC free article] [PubMed] [Google Scholar]
- 44.Oberdörster G, Sharp Z, Atudorei V, et al. Translocation of inhaled ultrafine particles to the brain. Inhal Toxicol. Taylor & Francis; 2004;16:437–445. [DOI] [PubMed] [Google Scholar]
- 45.Oberdörster G, Utell MJ. Ultrafine particles in the urban air: to the respiratory tract--and beyond? Environ Health Perspect. 2002;110:A440–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peters A, Veronesi B, Calderón-Garcidueñas L, et al. Translocation and potential neurological effects of fine and ultrafine particles a critical update. Part Fibre Toxicol. BioMed Central; 2006;3:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Adar SD, Klein R, Klein BEK, et al. Air Pollution and the microvasculature: a cross-sectional assessment of in vivo retinal images in the population-based multi-ethnic study of atherosclerosis (MESA). PLoS Med. Public Library of Science; 2010;7:e1000372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wellenius GA, Boyle LD, Wilker EH, et al. Ambient fine particulate matter alters cerebral hemodynamics in the elderly. Stroke. 2013;44:1532–1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zahodne LB, Manly JJ, Azar M, Brickman AM, Glymour MM. Racial Disparities in Cognitive Performance in Mid- and Late Adulthood: Analyses of Two Cohort Studies. J Am Geriatr Soc [online serial]. 2016;64:959–964. Accessed at: http://doi.wiley.com/10.1111/jgs.14113. Accessed March 31, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Melrose RJ, Brewster P, Marquine MJ, et al. Early life development in a multiethnic sample and the relation to late life cognition. Journals Gerontol - Ser B Psychol Sci Soc Sci. Gerontological Society of America; 2015;70:519–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sisco S, Gross AL, Shih RA, et al. The role of early-life educational quality and literacy in explaining racial disparities in cognition in late life. Journals Gerontol - Ser B Psychol Sci Soc Sci. Gerontological Society of America; 2015;70:557–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schwartz BS, Glass TA, Bolla KI, et al. Disparities in cognitive functioning by race/ethnicity in the Baltimore Memory Study. Environ Health Perspect. 2004;112:314–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liu SY, Glymour MM, Zahodne LB, Weiss C, Manly JJ. Role of Place in Explaining Racial Heterogeneity in Cognitive Outcomes among Older Adults. J Int Neuropsychol Soc [online serial]. 2017;21:677–687. Accessed at: https://www.cambridge.org/core/services/aop-cambridge-core/content/view/283311DE1BF88F9B37277DD1F41DC85B/S1355617715000806a.pdf/role_of_place_in_explaining_racial_heterogeneity_in_cognitive_outcomes_among_older_adults.pdf. Accessed April 24, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Weuve J, Barnes LL, Mendes De Leon CF, et al. Cognitive Aging in Black and White Americans: Cognition, Cognitive Decline, and Incidence of Alzheimer Disease Dementia. Epidemiology. Lippincott Williams and Wilkins; 2018;29:151–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ranft U, Schikowski T, Sugiri D, Krutmann J, Krämer U. Long-term exposure to traffic-related particulate matter impairs cognitive function in the elderly. Environ Res. 2009;109:1004–1011. [DOI] [PubMed] [Google Scholar]
- 56.Ailshire JA, Crimmins EM. Fine particulate matter air pollution and cognitive function among older US adults. Am J Epidemiol. 2014;180:359–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kulick ER, Wellenius GA, Boehme AK, Sacco RL, Elkind MS. Residential proximity to major roadways and risk of incident ischemic stroke in the Northern Manhattan Study. Stroke. 2018;49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hart JE, Puett RC, Rexrode KM, Albert CM, Laden F. Effect Modification of Long-Term Air Pollution Exposures and the Risk of Incident Cardiovascular Disease in US Women. J Am Heart Assoc. 2015;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hoffmann B, Weinmayr G, Hennig F, et al. Air quality, stroke, and coronary events: results of the Heinz Nixdorf Recall Study from the Ruhr Region. Dtsch Arztebl Int. 2015;112:195–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hoffmann B, Moebus S, Stang A, et al. Residence close to high traffic and prevalence of coronary heart disease. Eur Heart J. 2006;27:2696–2702. [DOI] [PubMed] [Google Scholar]
- 61.Tonne C, Melly S, Mittleman M, Coull B, Goldberg R, Schwartz J. A Case–Control Analysis of Exposure to Traffic and Acute Myocardial Infarction. Environ Health Perspect. 2016;115:53–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Van Hee VC, Adar SD, Szpiro AA, et al. Exposure to traffic and left ventricular mass and function: the Multi-Ethnic Study of Atherosclerosis. Am J Respir Crit Care Med. 2009;179:827–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dominici F, Peng RD, Bell ML, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory disease. JAMA. American Medical Association; 2006;295:1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Adar SD, Sheppard L, Vedal S, et al. Fine particulate air pollution and the progression of carotid intima-medial thickness: a prospective cohort study from the multi-ethnic study of atherosclerosis and air pollution. PLoS Med. 2013;10:e1001430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kaufman JD, Adar SD, Allen RW, et al. Prospective study of particulate air pollution exposures, subclinical atherosclerosis, and clinical cardiovascular disease. Am J Epidemiol. 2012;176:825–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Samet J, Krewski D. Health effects associated with exposure to ambient air pollution. J Toxicol Environ Health A. 2007;70:227–242. [DOI] [PubMed] [Google Scholar]
- 67.Park SK, Adar SD, O’Neill MS, et al. Long-term exposure to air pollution and type 2 diabetes mellitus in a multiethnic cohort. Am J Epidemiol. 2015;181:327–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Farrer LA, Cupples LA, Haines JL, et al. Effects of Age, Sex, and Ethnicity on the Association Between Apolipoprotein E Genotype and Alzheimer Disease. JAMA. 1997;278:1349. [PubMed] [Google Scholar]
- 69.Kukull WA, Schellenberg GD, Bowen JD, et al. Apolipoprotein E in Alzheimer’s disease risk and case detection: a case-control study. J Clin Epidemiol. 1996;49:1143–1148. [DOI] [PubMed] [Google Scholar]
- 70.Manly JJ, Mayeux R. Ethnic Differences in Dementia and Alzheimer’s Disease. Crit Perspect Racial Ethn Differ Heal Late Life. National Academies Press (US); 2004. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


