Abstract
Background
This study aims to compare the results of videoassisted thoracoscopic surgery and thoracotomy in the treatment of mediastinal cystic lesions.
Methods
Sixty patients (28 males, 32 females; mean age 36.1±19.4 years; range, 2 days to 82 years) who were performed thoracotomy or video-assisted thoracoscopic surgery for mediastinal cyst treatment in our clinic between January 1997 and December 2016 were retrospectively evaluated. Chest radiography and thorax computed tomography were used in all participants for diagnosis. Magnetic resonance imaging was used additionally in 23 participants.
Results
Of the patients, mediastinal cysts were localized in anteriorsuperior mediastinum in 19 (31.7%), middle mediastinum in 19 (31.7%) and posterior mediastinum in 22 (36.6%). Histopathologically, 17 bronchogenic cysts, 15 hydatid cysts, 10 pericardial cysts, seven cystic teratomas, four enteric cysts, four thymic cysts, two lymphangiomas and one thoracic duct cyst were identified. While thoracotomy was performed in 34 patients (56.7%), video-assisted thoracoscopic surgery was performed in 26 patients (43.3%). Mean duration of thoracotomies and video-assisted thoracoscopic surgeries was 123.6±24.7 minutes and 87.4±17.6 minutes, respectively (p<0.01). Mean duration of hospital stay was 8.2±4.3 days after thoracotomy and 4.3±1.2 days after video-assisted thoracoscopic surgery (p<0.01). While postoperative complications developed in four patients (two pneumothoraxes, one pleural effusion, one chylothorax), no mortality was observed in any of them.
Conclusion
Main treatment method for mediastinal cysts is surgery. Thoracoscopic approach significantly reduces patient's duration of surgical procedure and postoperative duration of hospital stay. We believe that minimally invasive approaches will be administered more frequently compared to open surgeries for mediastinal cysts in the near future.
Keywords: Cyst, mediastinum, thoracoscopy, thoracotomy
Introduction
Mediastinal cysts are round or oval benign lesions with clear boundaries that originate from different embryonic tissues and named according to their structures. These lesions can be congenital or acquired. Another way of development is cystic degeneration of a solid tumor. Although they can be seen in all age groups, they are most commonly seen in children and young adults. They are usually asymptomatic and detected incidentally on radiographs.[1]
The incidence of mediastinal cysts may vary by age. For example; foregut-derived cysts are less common in adulthood, although they form the majority of neonatal and childhood cysts. Similarly, pericardial cysts constitute about one third of adult mediastinal cysts, but are not very common in childhood.[2] Bronchogenic cysts constitute 5-10% of all mediastinal lesions and 50-60% of all mediastinal cystic pathologies.[3,4] They are mostly seen in subcarinal and paratracheal regions and rarely seen in paraesophageal and hilar regions.[5] In this study, we aimed to compare the results of video-assisted thoracoscopic surgery (VATS) and thoracotomy in the treatment of mediastinal cystic lesions.
Patients and Methods
Sixty patients (28 males, 32 females; mean age 36.1±19.4 years; range, 2 days to 82 years) who were performed thoracotomy or VATS for mediastinal cyst treatment in Atatürk University Medical School, Thorax Surgery Department between January 1997 and December 2016 were retrospectively evaluated. All patients' gender, age, admission date, complaints, medical history, physical examination findings, radiological findings, lesion localization, operation date, type and time, histopathological diagnosis, complication presence, mortality, additional treatment, postoperative duration of hospital of stay, and discharge date were recorded and evaluated.
Chest radiography and thorax computed tomography (CT) were used in all participants for diagnosis. Magnetic resonance imaging (MRI) was used additionally in 23 participants. The study protocol was approved by the Medical Faculty of Atatürk University Ethics Committee. A written informed consent was obtained from each patient. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Statistical analysis IBM SPSS version 20.0 (IBM Corp., Armonk, NY, USA) was used for statistical evaluation. Chi-square test was used to compare the categorical data for statistical evaluation of patients. Normal distribution of the numerical parameters of patients was examined by Kolmogorov Simirnov test. A t-test was used to compare parameters that fitted normal distribution, while Mann-Whitney U test was used to compare parameters that did not fit normal distribution. A p value <0.05 was considered statistically significant.
Results
The most common symptoms were chest pain in 25 (41.7%), shortness of breath in 20 (33.3%), cough in 14 (23.3%) and fatigue in five (8.3%) patients. Five patients were asymptomatic and diagnosed incidentally. Of the patients, mediastinal cysts were localized in anterior-superior mediastinum in 19 (31.7%), middle mediastinum in 19 (31.7%) and posterior mediastinum in 22 (36.6%). Histopathologically, 17 bronchogenic cysts, 15 hydatid cysts, 10 pericardial cysts, seven cystic teratomas, four enteric cysts, four thymic cysts, two lymphangiomas and one thoracic duct cyst were identified. Table 1 shows the incidence of histopathologic types in all three compartments. While thoracotomy was performed in 34 patients (56.7%) (22 right and 12 left sides), VATS was performed in 26 patients (43.3%) (19 right and 7 left sides) (Table 2, Figure 1-5). Mean duration of thoracotomies and VATSs was 123.6±24.7 min and 87.4±17.6 min, respectively (p<0.01). Mean duration of hospital stay was 8.2±4.3 days after thoracotomies and 4.3±1.2 days after VATSs (p<0.01). Postoperative complications developed in four patients (two pneumothoraxes, one pleural effusion, and one chylothorax), while no mortality was observed in any patient (Table 3).
Table 1. Mediastinal cysts and their localizations.
| Anterior/superior mediastinum | Middle mediastinum | Posterior mediastinum | ||||
| n | % | n | % | n | % | |
| Bronchogenic cyst | 4 | 21.1 | 3 | 15.8 | 10 | 45.5 |
| Hydatid cyst | 5 | 26.3 | 6 | 31.6 | 4 | 18.2 |
| Pericardial cyst | - | - | 8 | 42.1 | 2 | 9.1 |
| Cystic teratoma | 5 | 26.3 | 2 | 10.5 | - | - |
| Enteric cyst | - | - | - | - | 4 | 18.2 |
| Thymic cyst | 4 | 21.1 | - | - | - | - |
| Lymphangioma | 1 | 5.2 | - | - | 1 | 4.5 |
| Thoracic duct cyst | - | - | - | - | 1 | 4.5 |
| Total | 19 | 100 | 19 | 100 | 22 | 100 |
Table 2. Video-assisted thoracoscopic surgery and thoracotomy distribution.
| Thoracotomy | VATS | |||
| n | % | n | % | |
| Bronchogenic cyst | 9 | 26.5 | 8 | 30.7 |
| Hydatid cyst | 10 | 29.4 | 5 | 19.2 |
| Pericardial cyst | 4 | 11.8 | 6 | 23.1 |
| Cystic teratoma | 3 | 8.9 | 4 | 15.4 |
| Enteric cyst | 3 | 8.9 | 4 | 15.4 |
| Thymic cyst | 2 | 5.8 | 2 | 7.7 |
| Lymphangioma | 2 | 5.8 | - | - |
| Thoracic duct cyst | 1 | 2.9 | - | - |
| Total | 34 | 100 | 26 | 100 |
| VATS: Video-assisted thoracoscopic surgery. | ||||
Figure 1. Pericardial cyst in a 55-year-old male patient. (a) Left base opacity is present at direct radiographic image. (b) Computed tomography scan shows cystic lesion in left middle mediastinum. (c, d) Magnetic resonance imaging with high signal intensity shows a lesion that is occupying half of left hemithorax. (e) Resected cyst wall. (f) Thorocoscopy incisions are seen.
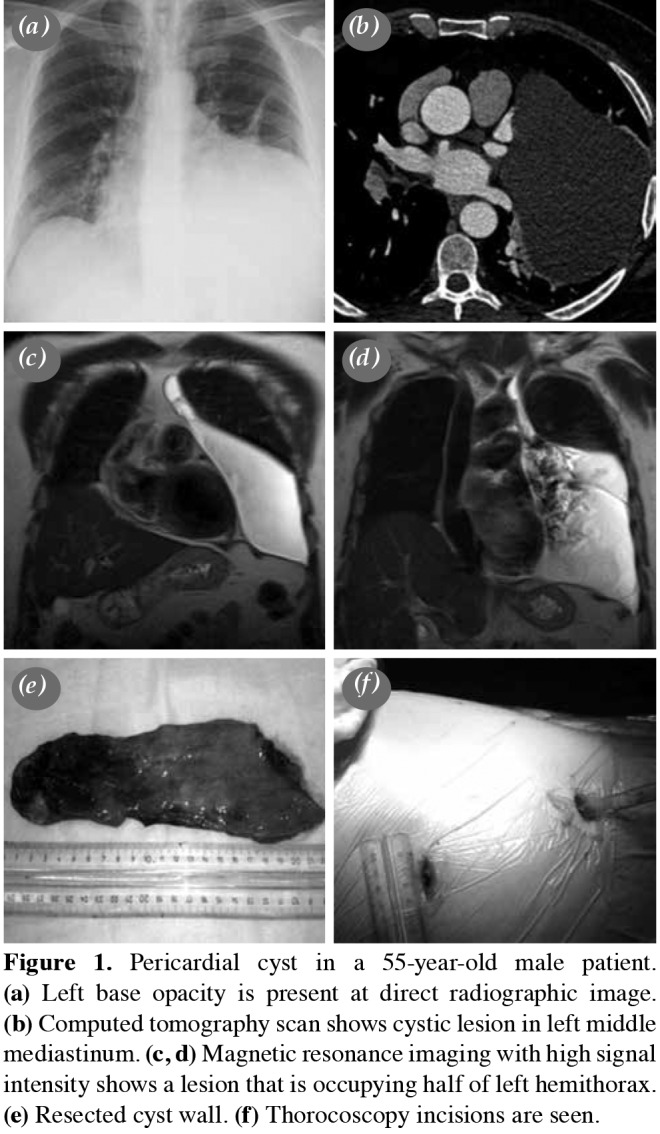
Figure 5. Enteric cyst in a 10-day-old girl patient. (a) Chest radiography shows opacity in left cardiophrenic angle. (b) Computed tomography scan shows cystic lesion in posterior mediastinum. (c) Intraoperative view of cyst and (d) excised cyst wall are seen.
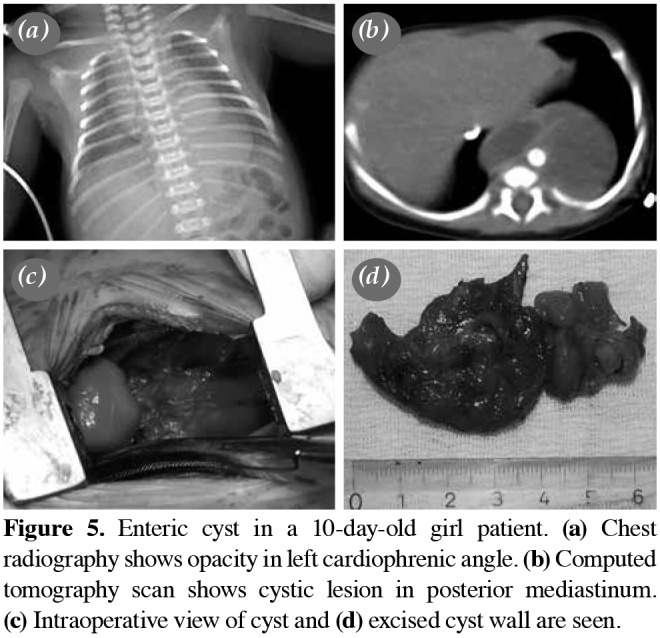
Table 3. Comparison of thoracotomy and video-assisted thoracoscopic surgery cases.
| Thoracotomy | VATS | p | |
| Surgery duration (min) | 123.6 | 87.4 | <0.01 |
| Postoperative stay (day) | 8.2 | 4.3 | <0.01 |
| Uncomplicated | 31 | 25 | 0.626 |
| Pneumothorax | 1 | 1 | |
| Pleural effusion | 1 | 0 | |
| Chylothorax | 1 | 0 | |
| Recurrence | 0 | 0 | |
| Mortality | 0 | 0 | |
| VATS: Video-assisted thoracoscopic surgery. | |||
Figure 2. Mature cystic teratoma in an eight-year-old girl patient. (a) Chest radiography shows an oval opacity on right hemidiaphragm. (b) Computed tomography scan shows anterior mediastinal cystic lesion. (c) Perioperative view of lesion. (d) Excision material and cystic liquid content are seen.
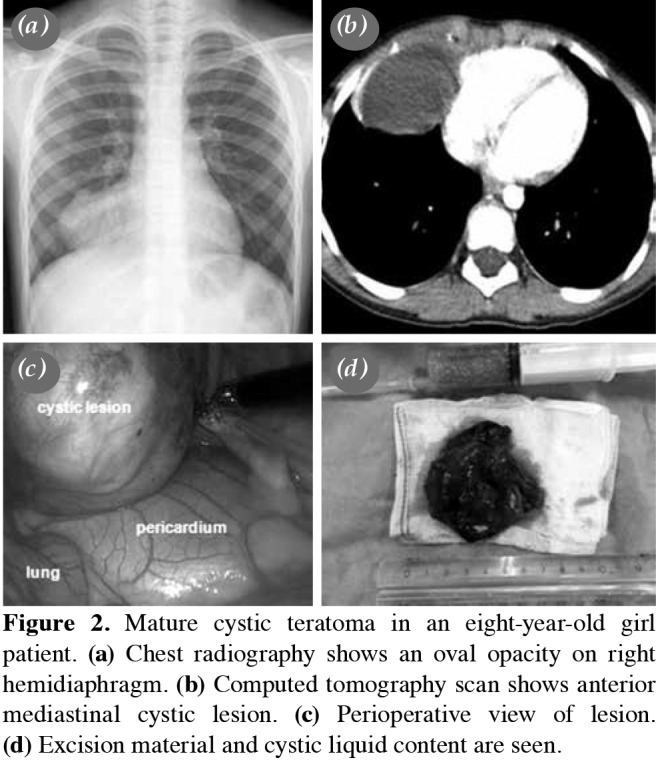
Figure 3. Bronchogenic cyst in a 20-year-old male patient. (a) Direct chest radiography shows opacity with smooth border on right hilum. (b) Computed tomography scan shows posterior mediastinal cystic lesion. (c) Axial plane magnetic resonance imaging. (d) Coronal plane magnetic resonance imaging shows cystic content of lesion.
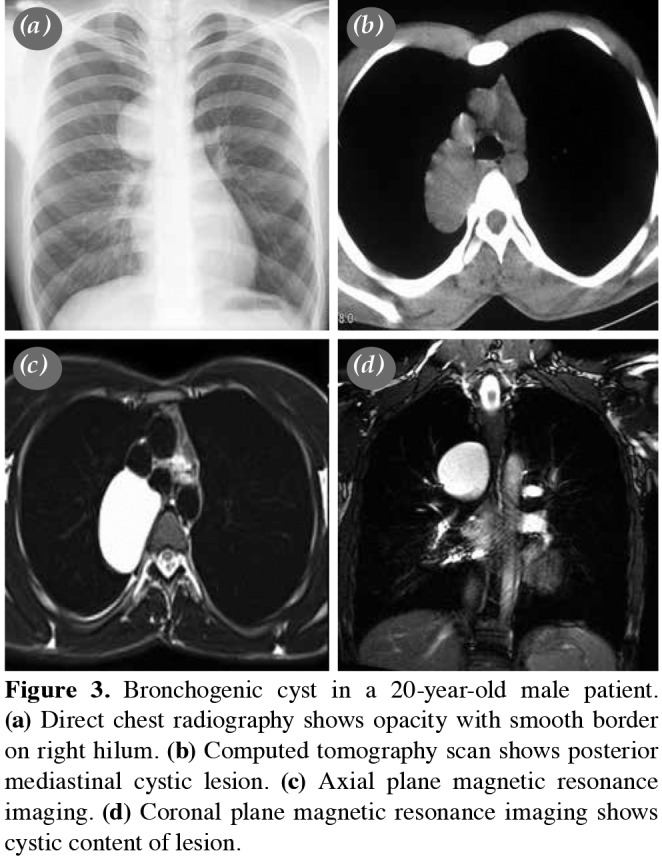
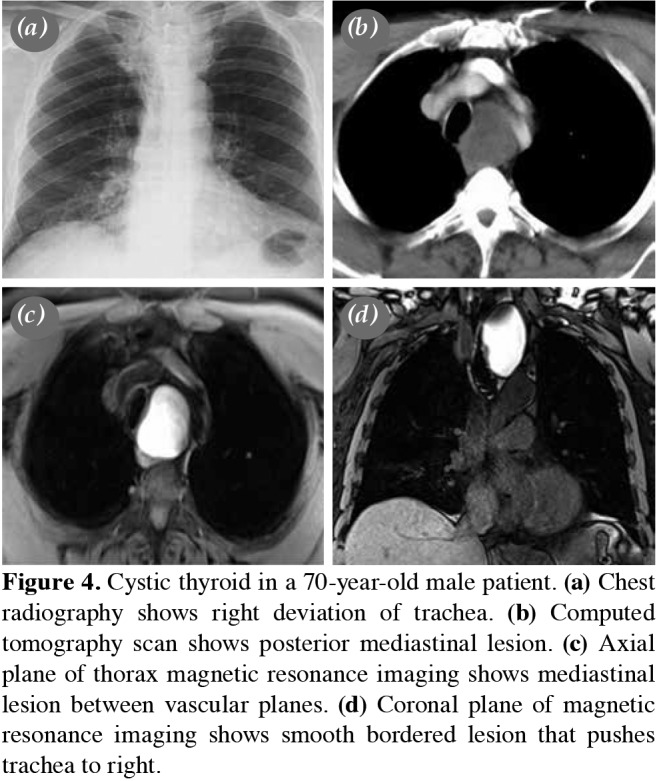
Figure 4. Cystic thyroid in a 70-year-old male patient. (a) Chest radiography shows right deviation of trachea. (b) Computed tomography scan shows posterior mediastinal lesion. (c) Axial plane of thorax magnetic resonance imaging shows mediastinal lesion between vascular planes. (d) Coronal plane of magnetic resonance imaging shows smooth bordered lesion that pushes trachea to right.
Discussion
Mediastinal cysts constitute 12-18% of mediastinal masses. Primary mediastinal cysts can be seen in all age groups, but mostly in the age range of 20-30 years and in males.[6] In our study, there were 28 males (46.7%) and 32 females (53.3%). The mean age was 36.1±19.4 years, which was above the reported mean age in the literature and 78.3% of the patients were adults.
Symptoms may vary according to the location and size of cysts. Most complaints are due to cystic compression effect or inflammatory complications. Pressure of the cysts to the tissues and organs may be life-threatening particularly in infants and may result in severe respiratory failure. Paratracheal and carinal cysts may present with symptoms such as dyspnea or cough while posterior mediastinal cysts may present with swallowing difficulty or abdominal pain.[1,6] The majority of our patients were symptomatic and the most common symptoms were chest pain, shortness of breath, and cough.
Conventional chest radiograms are the first step for examination. Mediastinal cysts are usually seen as sharp limited, round or oval opacity increases. Computed tomography is an important tool in the identification of mediastinal cysts.[2] Posteroanterior chest X-ray and chest CT were used for diagnosis in all patients in our study. Magnetic resonance imaging was used additionally in 23 cases.
Bronchogenic cysts are the most common mediastinal cystic lesions. Although bronchogenic cyst cases are congenital, they are often diagnosed in the adult age group. They are usually seen in males. In our study, there were 17 patients with bronchogenic cysts; 10 males and seven females. Lesion localizations were four in anterior, three in middle, and 10 in posterior mediastinum.
Video-assisted thoracoscopic surgery and thoracotomy are generally the preferred approaches in the treatment of mediastinal cysts. In experienced clinics, complete resection with low mortality and morbidity can be achieved in short time by VATS even with closely related bronchogenic cysts to mediastinal structures. Thoracotomy has traditionally been favored by surgeons as it enhances accessibility to the cysts and adherent tissues also surrounding tissues while enabling intervention in possible complications. Jung et al.[7] reported a 113-case study of thoracoscopic surgery in bronchogenic cysts. In this study, 109 operations were completed by VATS while four operations required changing to thoracotomy. At present, resection of bronchogenic cysts is possible also with robotic surgery with the progression of robotic surgeries in thoracic surgery. It is reported that robotic surgery allows total excision of cysts without damaging cystic capsules or adjacent structures by precise dissections.[8] In our study, nine patients of bronchogenic cysts underwent surgical intervention by thoracotomy and eight patients underwent VATS.
Mediastinal hydatid cysts constitute 0.5-1% of all hydatid cysts. Secondary mediastinal hydatid cysts are more common than primary hydatid cysts, such that they are observed as primary at a rate of 0.1%.[9,10] They can be seen at any age and frequency in paravertebral sulcus. They are more common in males. Computed tomography, MRI, complement fixation, Casoni skin test and indirect hemagglutination tests can be used during the examination phase. Symptoms are related to the size and localization of the cysts and also their relationships with neighboring structures. The most serious complication is anaphylactic shock and even death occurring by hydatid cyst material dissemination into blood after cyst rupture. In our study, a total of 15 hydatid cysts were operated including five anterior, six middle, and four posterior mediastinum localized cysts. Thoracotomy was performed in 10 patients and VATS in five patients.
Pericardial cysts are usually seen as adjacent to the right anterior cardiac angle. They can be confused with Morgagni hernias. They are usually asymptomatic and rare in children.[2,3] Five percent of pericardial cysts may be associated with pericardium. It should not be forgotten that growing pericardial cysts may have risks of hemorrhage, spontaneous rupture or cardiac tamponade.[11] There are two different opinions in the treatment of pericardial cysts; one group proposes follow-up, while the other group suggests surgery due to possible complications of cardiac pressure and rupture. However, surgical excision is in the foreground and applied with low morbidity and mortality rates. Complete excision is advocated even in asymptomatic patients. In our study, eight of the pericardial cyst cases were in middle mediastinum and two cases in posterior mediastinum. Thoracotomy was performed in four patients and VATS in six patients.
There is an important debate on the treatment of mediastinal cysts. Some authors support follow-up in asymptomatic cysts and conservative transbronchial, transesophageal or percutaneous needle aspirations accompanied by CT.[12] However, this method is debatable due to recurrence and morbidity risks. Some researchers advocate sclerosing agent application after aspiration for degeneration of epithelial debris. However, the results are not always satisfactory.[13] The traditional approach for definitive diagnosis and treatment of atypical radiological findings and symptomatic mediastinal cysts is surgical excision.[14] In non-operated patients, symptoms might develop due to growth of cysts. In these cases, operation carries higher risk of morbidity and mortality because of possible complications and malignancy developments.[15]
Although posterolateral thoracotomy is the traditional surgical procedure in the excision of mediastinal cysts, the use of VATS in cystectomy in both children and adults has increased in the last two decades. We started to use thoracoscopy in mediastinal cysts in 2008 for the first time. Since then, the use of VATS has increased. With increasing experience in our clinic, VATS has been used as the first procedure applied in mediastinal cysts.
In the literature, VATS and thoracotomy are usually compared between bronchogenic and mediastinal cysts. Some known difficulties of VATS include pericystic intense adhesions, tracheobronchial or esophageal neighborhoods with cyst, difficulties in bleeding control, and failure to eradicate the entire cystic wall. In addition, cyst size, depth, and neighborhoods with major vascular structures, tracheobronchial, and esophageal structures may cause converting to thoracotomy. There are similar excision difficulties, possible complications and recurrences within thoracotomy and VATS; however, VATS provides a marked postoperative superiority when compared with thoracotomy.[16-18] Most of these studies showed that VATS did not increase surgery-related complications, intraoperative bleeding, intensive care unit stay, postoperative complications, or incomplete resection risk.[19] Moreover, as with our study, it was shown that the duration of operation and hospitalization were shorter with VATS.[19,20] The mean duration of VATSs was 87.4±17.6 min, while it was 123.6±24.7 min with surgeries performed with thoracotomy. Furthermore, postoperative duration of hospital stay after thoracotomies was mean 8.2 days, while it was 4.3 days after VATSs. The difference between durations of operation and postoperative hospital stay was statistically significant. All these results suggest that VATS cystectomy is an effective and safe method for treatment of mediastinal cysts.
Our study has some limitations; it is retrospective study, age population is vary, there are a lot of different histopathological types, and lesions show varied settlements.
In c onclusion, it is generally accepted that mediastinal cyst aspiration is an inadequate treatment for mediastinal cysts and excision should be performed for all mediastinal cysts regardless of their origin. Thoracoscopy is preferred to thoracotomy due to its superiority in duration of surgery, postoperative pain, pulmonary complications, costs, and duration of hospital stay. Our findings show that both video-assisted thoracoscopic surgery and thoracotomy are suitable approaches for the treatment of mediastinal cysts. However, considering its perioperative results, videoassisted thoracoscopic surgery seems to be superior.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Gochi F, Omasa M, Yamada T, Sato M, Menju T, Aoyama A, et al. Factors affecting the preoperative diagnosis of anterior mediastinal cysts. Gen Thorac Cardiovasc Surg. 2015;63:349–353. doi: 10.1007/s11748-015-0530-2. [DOI] [PubMed] [Google Scholar]
- 2.Aydin Y, Araz O, Ozgokce M, Ince I, Alper F, Eroglu A. Video-Assisted Thoracoscopic Surgery of Mediastinal Cysts: Report of 13 Cases. Indian J Surg. 2015;77:236–239. doi: 10.1007/s12262-012-0782-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aydin Y, Ogul H, Turkyilmaz A, Eroglu A. Surgical treatment of mediastinal cysts: report on 29 cases. Acta Chir Belg. 2012;112:281–286. [PubMed] [Google Scholar]
- 4.Xu S, Liu B, Wang X, Meng H, Wang T, Wang S. Robotic thoracic surgery of the anterior superior mediastinal bronchogenic cyst. Ann Transl Med. 2015;3:57–57. doi: 10.3978/j.issn.2305-5839.2015.03.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jiang JH, Yen SL, Lee SY, Chuang JH. Differences in the distribution and presentation of bronchogenic cysts between adults and children. J Pediatr Surg. 2015;50:399–401. doi: 10.1016/j.jpedsurg.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 6.Takeda S, Miyoshi S, Minami M, Ohta M, Masaoka A, Matsuda H. Clinical spectrum of mediastinal cysts. Chest. 2003;124:125–132. doi: 10.1378/chest.124.1.125. [DOI] [PubMed] [Google Scholar]
- 7.Jung HS, Kim DK, Lee GD, Sim HJ, Choi SH, Kim HR, et al. Video-assisted thoracic surgery for bronchogenic cysts: is this the surgical approach of choice. Interact Cardiovasc Thorac Surg. 2014;19:824–829. doi: 10.1093/icvts/ivu228. [DOI] [PubMed] [Google Scholar]
- 8.Toker A, Ayalp K, Grusina-Ujumaza J, Kaba E. Resection of a bronchogenic cyst in the first decade of life with robotic surgery. Interact Cardiovasc Thorac Surg. 2014;19:321–323. doi: 10.1093/icvts/ivu113. [DOI] [PubMed] [Google Scholar]
- 9.Eroğlu A, Aydın Y, Altuntaş B, Ulaş AB. Surgical management of primary mediastinal hydatid cysts: a 30-year experience. Turk Gogus Kalp Dama. 2016;24:495–500. [Google Scholar]
- 10.Eroğlu A, Kürkçüoğlu C, Karaoğlanoğlu N, Tekinbaş C, Kaynar H, Onbaş O. Primary hydatid cysts of the mediastinum. Eur J Cardiothorac Surg. 2002;22:599–601. doi: 10.1016/s1010-7940(02)00398-6. [DOI] [PubMed] [Google Scholar]
- 11.Shiraishi I, Yamagishi M, Kawakita A, Yamamoto Y, Hamaoka K. Acute cardiac tamponade caused by massive hemorrhage from pericardial cyst. Circulation. 2000;101:196–197. doi: 10.1161/01.cir.101.19.e196. [DOI] [PubMed] [Google Scholar]
- 12.Okubo K, Chino M, Fuse J, Yo S, Nishimura F. Life-saving needle aspiration of a cardiac-compressing pericardial cyst. Am J Cardiol. 2000;85:521–521. doi: 10.1016/s0002-9149(99)00788-2. [DOI] [PubMed] [Google Scholar]
- 13.Westcott JL. Percutaneous needle aspiration of hilar and mediastinal masses. Radiology. 1981;141:323–329. doi: 10.1148/radiology.141.2.7291553. [DOI] [PubMed] [Google Scholar]
- 14.Smail H, Baste JM, Melki J, Peillon C. Mediastinal Bronchogenic Cyst With Acute Cardiac Dysfunction: Two- Stage Surgical Approach. Ann Thorac Surg. 2015;100:79–80. doi: 10.1016/j.athoracsur.2015.06.059. [DOI] [PubMed] [Google Scholar]
- 15.Zambudio AR, Lanzas JT, Calvo MJ, Fernández PJ, Paricio PP. Non-neoplastic mediastinal cysts. Eur J Cardiothorac Surg. 2002;22:712–716. doi: 10.1016/s1010-7940(02)00484-0. [DOI] [PubMed] [Google Scholar]
- 16.Weber T, Roth TC, Beshay M, Herrmann P, Stein R, Schmid RA. Video-assisted thoracoscopic surgery of mediastinal bronchogenic cysts in adults: a single-center experience. Ann Thorac Surg. 2004;78:987–991. doi: 10.1016/j.athoracsur.2004.03.092. [DOI] [PubMed] [Google Scholar]
- 17.Jung HS, Kim DK, Lee GD, Sim HJ, Choi SH, Kim HR, et al. Video-assisted thoracic surgery for bronchogenic cysts: is this the surgical approach of choice. Interact Cardiovasc Thorac Surg. 2014;19:824–829. doi: 10.1093/icvts/ivu228. [DOI] [PubMed] [Google Scholar]
- 18.Esme H, Eren S, Sezer M, Solak O. Primary mediastinal cysts: clinical evaluation and surgical results of 32 cases. Tex Heart Inst J. 2011;38:371–374. [PMC free article] [PubMed] [Google Scholar]
- 19.Tölg C, Abelin K, Laudenbach V, de Heaulme O, Dorgeret S, Lipsyc ES, et al. Open vs thorascopic surgical management of bronchogenic cysts. Surg Endosc. 2005;19:77–80. doi: 10.1007/s00464-003-9328-x. [DOI] [PubMed] [Google Scholar]
- 20.Guo C, Mei J, Liu C, Deng S, Pu Q, Lin F, et al. Videoassisted thoracic surgery compared with posterolateral thoracotomy for mediastinal bronchogenic cysts in adult patients. J Thorac Dis. 2016;8:2504–2511. doi: 10.21037/jtd.2016.08.29. [DOI] [PMC free article] [PubMed] [Google Scholar]


