Abstract
Introduction
The Robson 10-group classification system stratifies cesarean birth rates using maternal characteristics. Our aim was to compare cesarean birth utilization in US centers with and without midwifery care using the Robson classification.
Methods
We used National Institute of Child and Human Development Consortium on Safe Labor data from 2002 to 2008. Births to women in centers with interprofessional care that included midwives (n = 48,857) were compared with births in non-interprofessional centers (n = 47,935). To compare cesarean utilization, births were classified into the Robson categories. Cesarean birth rates within each category and the contribution to the overall rate were calculated. Maternal demographics, labor and birth outcomes, and neonatal outcomes were described. Logistic regression was used to adjust for maternal comorbidities.
Results
Women were less likely to have a cesarean birth (26.1% vs 33.5%, P < .001) in centers with interprofessional care. Nulliparous women with singleton, cephalic, term fetuses (category 2) were less likely to have labor induced (11.1% vs 23.4%, P < .001), and women with a prior uterine scar (category 5) had lower cesarean birth rates (73.8% vs 85.1%, P < .001) in centers with midwives. In centers without midwives, nulliparous women with singleton, cephalic, term fetuses with induction of labor (category 2a) were less likely to have a cesarean birth compared with those in interprofessional care centers in unadjusted comparison (30.3% vs 35.8%, P < .001), but this was reversed after adjustment for maternal comorbidities (adjusted odds ratio, 1.21; 95% CI, 1.12–1.32; P < .001). Cesarean birth rates among women at risk for complications (eg, breech) were similar between groups.
Discussion
Interprofessional care teams were associated with lower rates of labor induction and overall cesarean utilization as well as higher rates of vaginal birth after cesarean. There was consistency in cesarean rates among women with higher risk for complications.
Keywords: midwife, maternity care, interprofessional, cesarean birth, vaginal birth after cesarean, induction of labor, low-risk women, Robson ten-group classification system
INTRODUCTION
Annually, nearly 4 million women give birth in the United States, 32% of them by cesarean birth.1,2 Correctly timed, indicated, and performed, cesareans save lives. In countries with fewer perinatal care resources, maternal and neonatal morbidity and mortality are increased by inadequate access to cesarean birth.3 However, in countries like the United States with higher perinatal care resources and few barriers to intervention overuse, higher cesarean rates are not associated with concomitant reductions in neonatal mortality and morbidity4 and, instead, increase maternal mortality and morbidity.5 In addition, overuse of cesarean raises health care costs; childbirth is one of the top 5 reasons for hospital admission,6 and costs and length of hospital stay for cesarean birth far exceed those for vaginal birth.7
Cesarean birth rates can be used as a perinatal care quality indicator.8 With high-quality, evidence-based care, cesarean utilization patterns should have minimal interinstitutional variation for women with similar health status.9 For example, pregnant women with an indication for surgical birth according to current practice standards (eg, breech presentation) should have high cesarean birth rates across institutions, whereas low-risk women should have consistently lower cesarean birth rates, regardless of where they labor and give birth. However, there is wide variation in cesarean utilization across US hospitals, with rates ranging from 7.1% to 69.9% for all women and from 2.4% to 36.5% among low-risk women.10 This wide institutional variation cannot be explained by maternal risk factors alone. Health care systems factors may be a primary contributor.11 One less studied factor is how the presence of midwives as members of labor and birth teams affects variation in cesarean utilization across institutions.
Midwife-Physician Interprofessional Models of Care
Interprofessional care models between midwives and physicians exhibit different practice structures. Freytsis et al define 2 types of interprofessional models: collaborative care models,12 which include both midwives and physicians as part of an integrated team, and midwifery-led models, in which midwives may collaborate with physicians but the majority of care is provided by a single midwife or team of midwives. The effect of midwifery presence in perinatal care teams is an emerging focus of research. Previous work suggests that midwifery-led models of care are associated with lower cesarean utilization. In a recent study, women who gave birth in New York hospitals with a greater proportion of midwife-attended births had reduced odds of labor induction, episiotomy, and cesarean birth compared with women who gave birth in hospitals with fewer midwife-attended births.13 In their nationwide US study, Vedam et al found that higher state-specific midwifery integration scores were associated with significantly higher rates of physiologic birth, fewer adverse neonatal outcomes, and less use of obstetric interventions, including lower rates of cesarean birth.14 Several case studies of midwife-physician interprofessional collaborative practices document primary cesarean rates ranging from 8% to 18.5%,15–20 lower than the national primary cesarean average of 21.9% when this study was conducted.21 Reduction in cesarean rates has also been noted after implementation of a midwife-physician laborist model.22 These findings suggest that midwives may affect unit-level, hospital-level utilization or regional rates of cesarean birth. Further assessment of how the composition of the perinatal care team shapes outcomes is needed to inform and improve perinatal care.
Robson 10-Group Classification System
Careful assessment of utilization of cesarean birth is an essential component of ongoing quality improvement for all intrapartum care facilities. Although the overall cesarean birth rate and the rate for nulliparous women with a singleton, term, vertex fetus are essential for appreciating patterns of cesarean utilization, they cannot offer the level of specificity regarding cesarean practices that is generated with the Robson system. To standardize assessment of cesarean utilization across facilities, the World Health Organization supports application of the Robson 10-group classification system.23 The Robson system categorizes all cesarean birth rates by 6 fixed maternal and/or fetal criteria important to perinatal care decision making: gestational age, parity, fetal lie, number of fetuses, previous cesarean birth, and onset of spontaneous labor. These characteristics are used to classify all women giving birth into 1 of 10 mutually exclusive categories (Table 1).24 This system has been used to measure cesarean birth variation among perinatal care delivery systems in several countries25,26 and allows comparison of rates within and across hospitals, health systems, and countries. Because the Robson system creates categories based on characteristics known to be associated with utilization of cesarean birth, it can be used to identify perinatal care system variation and inform interventions to improve quality and safety.27
Table 1.
Robson 10-Group Classification System
| Robson Category | Description |
|---|---|
| 1 | Nulliparous women with a single cephalic pregnancy, ≥37 weeks’ gestation, in spontaneous labor |
| 2 | Nulliparous women with a single cephalic pregnancy, ≥37 weeks’ gestation, who either had labor induced or gave birth by cesarean before labor |
| 2a | Nulliparous women with a single cephalic pregnancy, ≥37 weeks’ gestation, who had labor induced |
| 2b | Nulliparous women with a single cephalic pregnancy, ≥37 weeks’ gestation, who gave birth by cesarean before labor |
| 3 | Multiparous women without a previous uterine scar, with a single cephalic pregnancy, ≥37 weeks’ gestation, in spontaneous labor |
| 4 | Multiparous women without a previous uterine scar, with a single cephalic pregnancy, ≥37 weeks’ gestation, who either had labor induced or gave birth by cesarean before labor |
| 4a | Multiparous women without a previous uterine scar, with a single cephalic pregnancy, ≥37 weeks’ gestation, who had labor induced |
| 4b | Multiparous women without a previous uterine scar, with a single cephalic pregnancy, ≥37 weeks’ gestation, who gave birth by cesarean before labor |
| 5 | All multiparous women with at least one previous uterine scar, with a single cephalic pregnancy, ≥37 weeks’ gestation |
| 6 | All nulliparous women with a single breech pregnancy |
| 7 | All multiparous women with a single breech pregnancy, including women with previous uterine scars |
| 8 | All women with multiple pregnancies, including women with previous uterine scars |
| 9 | All women with a single pregnancy with a transverse or oblique lie, including women with previous uterine scars |
| 10 | All women with a single cephalic pregnancy, <37 weeks’ gestation, including women with previous uterine scars |
Source: Robson 2001.24
In the United States, there have been recent calls for greater incorporation of the Robson classification in quality improvement initiatives.28 To date, the Robson system has not been used to explore differences in cesarean rates among US perinatal care teams with and without midwife-physician interprofessional care models. The purpose of our study was to compare cesarean birth utilization between US centers with and without midwife-physician interprofessional care by applying the Robson classification system to births in the National Institute of Child and Human Development Consortium on Safe Labor (CSL) data set.
METHODS
Design
We conducted a secondary analysis of the CSL data set to describe differences in cesarean birth rates between sites with and without midwife-physician interprofessional models of care. Secondarily, labor induction utilization and common maternal and neonatal outcomes were compared between groups. The study was approved by the Colorado Multiple Institutional Review Board. Data use agreements for the CSL data for secondary analysis were obtained by all study authors from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Data Source, Population, and Independent Variable
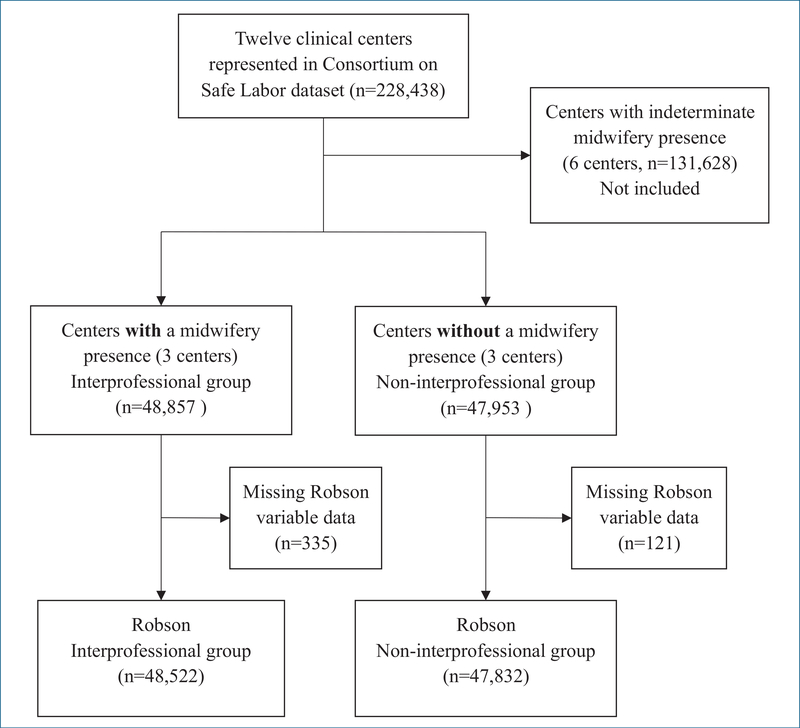
The CSL data set includes antepartum, intrapartum, and neonatal data for 228,438 births collected from 12 centers throughout the United States between 2002 and 2008.29,30 Centers in the CSL data set included academic, tertiary medical centers, community teaching hospitals, and community hospitals with around-the-clock in-house obstetricians and anesthesia services. Some centers offered midwifery care, higher-level neonatal intensive care units (NICUs), and maternal-fetal medicine specialists. The CSL data set contains 2 variables related to employment of midwives within these centers. The data set does not reliably differentiate whether a midwife was directly involved in a woman’s intrapartum care, only whether midwives were or were not intrapartum care providers at the medical center. To create the independent variable of interprofessional care compared with non-interprofessional care, centers where midwives were identified as practicing and also were identifiable as either the admitting provider or birth attendant were combined into the interprofessional care group; 3 centers met these criteria. Centers where midwives were neither an admitting provider nor birth attendant were formed into the non-interprofessional (physician-only) care group; 3 centers met these criteria. Six centers where midwifery intrapartum care was indeterminate were not included in analysis; in these centers, the variable identifying that midwives practiced in the institution indicated “yes,” but midwives were not identifiable as the admitting provider or birth attendant (Figure 1).
Figure 1.
Flowchart Depicting Creation of Robson Interprofessional and Non-Interprofessional Groups
Maternal Demographics, Birth, and Neonatal Characteristics
Maternal demographics (maternal age, body mass index [BMI], race and ethnicity, marital status, and health insurance), labor characteristics and outcomes (gestational age, cervical dilation on admission, spontaneous onset of labor, labor induction, mode of birth, postpartum hemorrhage, and maternal death), and neonatal outcomes (sex, birth weight, birth weight category, Apgar scores at 1 and 5 minutes, NICU admission, and stillbirth or neonatal death) were compared between the interprofessional and non-interprofessional groups.
Outcome
The primary outcome of interest was cesarean birth rates for each of the 10 Robson categories, compared between interprofessional and non-interprofessional groups.
Statistical Analysis
Differences between interprofessional and non-interprofessional groups for overall maternal demographics, labor processes and outcomes, and neonatal outcomes were evaluated using chi-square tests for categorical variables and Wilcoxon rank sum tests for non-normal continuous variables. We reported median values with a 95% CI for non-normal continuous variables.
After these initial comparisons between groups, each birth was placed into 1 of the 10 Robson categories using characteristics present in the CSL data.31 After sorting, frequencies and proportions were calculated for each of the Robson categories; the proportion of women who composed the Robson category in relation to the overall sample and the contribution of each Robson category to the overall cesarean birth rate were compared between the 2 groups. Chi-square tests were used to test for significant differences between groups among the Robson categories. Because important demographic and maternal comorbid differences existed between groups, cesarean rates change over time, and births occurred within different centers, logistic regression comparing cesarean birth with vaginal birth was used for each Robson category to determine if potential confounders would affect interpretation of results. In the regression, we controlled for race or ethnicity, diabetes, chronic or gestational hypertension, heart disease, renal disease, depression, anemia, BMI on admission, year of birth, and site or center. Potential covariates were identified from a review of prior studies32–36 and then selected for the model if those covariates significantly differed between the interprofessional and non-interprofessional groups. For Robson categories 2 and 4, only births with induced labor (category 2a and 4a) were included for regression analysis. Prelabor cesarean births (categories 2b and 4b) were excluded in the regression analysis. Statistical significance level was established at P less than .001 because of the large sample size. Analyses were completed using SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
Group sizes were similar, with 48,857 women in the interprofessional care group and 47,935 in the non-interprofessional care group (Table 2). Women in the interprofessional group had higher BMI on intrapartum admission and were more likely to be white, non-Hispanic, and married and have private health insurance (P < .001).
Table 2.
Maternal Characteristics by Care Group (N = 96,810)
| Characteristic | Interprofessional Groupa (n = 48,857) | Non-Interprofessional Groupb (n = 47,953) | P Value |
|---|---|---|---|
| Maternal age, median (5th–95th percentile), y | 28 (19–39) | 28 (18–39) | <.001 |
| Body mass index before pregnancy, median (5th–95th percentile), kg/m2 | 23.8 (18.3–37.6) | 23.2 (18.3–37.3) | <.001 |
| Body mass index on admission for birth,c median (5th–95th percentile), kg/m2 | 29.8 (23.2–42.8) | 29.3 (22.8–42.6) | <.001 |
| Race and ethnicity, n (%)d | |||
| White, non-Hispanic | 30,734 (62.9) | 17,794 (37.1) | <.001 |
| Black, non-Hispanic | 4967 (10.2) | 16,155 (33.7) | <.001 |
| Hispanic | 6139 (12.6) | 10,013 (20.9) | <.001 |
| Asian or Pacific Islander | 3401 (6.7) | 3000 (6.3) | <.001 |
| Other | 1044 (2.1) | 404 (.9) | <.001 |
| Unknown | 588 (1.2) | 3160 (3.3) | <.001 |
| Marital status, n (%)d | |||
| Married | 29,963 (61.3) | 28,005 (58.4) | <.001 |
| Not married | 14,971 (30.6) | 18,651 (38.9) | <.001 |
| Unknown | 3923 (8.0) | 1296 (2.7) | <.001 |
| Health insurance, n (%)d | |||
| Private | 39,613 (81.1) | 17,141 (35.8) | <.001 |
| Public | 8626 (17.7) | 17,305 (36.1) | <.001 |
| Self-pay, other | 361(0.7) | 1240 (2.6) | <.001 |
| Unknown | 257 (0.5) | 11,943 (24.9) | <.001 |
Interprofessional group includes centers with midwifery presence.
Non-interprofessional group includes centers without midwifery presence.
Values not reported for 45.8% (44,304) of women.
Percentages may not add to 100% because of rounding.
Table 3 presents comparisons between the interprofessional and non-interprofessional groups for labor, birth, and neonatal characteristics. More than half of women in both groups gave birth between 39 weeks’ gestation and 40 weeks’ and 6 days’ gestation, although there were significant differences between groups on gestational age categories, with the interprofessional group having significantly (P < .001) fewer women giving birth at early term and significantly more women giving birth at full-term, late-term, or post-term gestation. Women in the interprofessional group were admitted to the hospital with significantly greater cervical dilatation and effacement and were more likely to experience spontaneous onset of labor (P < .001). The use of labor induction differed significantly between the interprofessional and non-interprofessional groups for both nulliparous and multiparous women. The overall use of labor induction (23.6% vs 43.2%, P < .001) differed significantly between groups, with almost half as many women undergoing labor induction in the interprofessional group. The total cesarean rate was lower for women in the interprofessional care group compared with the non-interprofessional care group (26.1% vs 33.5%, P < .001), There were small, but significant, differences in neonatal characteristics, including higher birth weight, fewer NICU admissions, and fewer stillbirths or neonatal deaths in the interprofessional group compared with the non-interprofessional group.
Table 3.
Labor, Birth, and Neonatal Characteristics by Care Group (N = 96,810)
| Characteristic | Interprofessional Groupa (n = 48,857) | Non-Interprofessional Groupb (n = 47,953) | P Value |
|---|---|---|---|
| Gestational age, n (%) | |||
| Early term (37 0/7 to 38 6/7 wk) | 13,322 (30.6) | 16,239 (40.2) | <.001 |
| Full term (39 0/7 to 40 6/7 wk) | 25,213 (57.9) | 21,617 (53.5) | <.001 |
| Late term (41 0/7 to 41 6/7 wk) | 4471 (10.3) | 2357 (5.8) | <.001 |
| Post term (≥42 0/7 wk) | 510 (1.2) | 220 (0.5) | <.001 |
| Cervical dilatation on admission, mean (SD), cm | 4.2 (2.6) | 3.1 (2.2) | <.001 |
| Cervical effacement on admission, mean (SD), % | 76.9 (23.2) | 68.4 (26.2) | <.001 |
| Type of labor, n (%) | |||
| Spontaneous onset and trial of labor | 31,077 (63.6) | 18,347 (38.3) | <.001 |
| Induction and trial of labor | 11,522 (23.6) | 20,687 (43.2) | <.001 |
| Cesarean without trial of labor | 6257 (12.8) | 8835 (18.5) | <.001 |
| Mode of birth | |||
| Vaginal, spontaneous | 33,694 (69) | 29,582 (61.7) | <.001 |
| Vaginal, assisted | 2382 (4.9) | 2311 (4.8) | <.001 |
| Cesarean | 12,781 (26.1) | 16,063 (33.5) | <.001 |
| Postpartum hemorrhage, n (%) | 1329 (2.7) | 1417 (3.0) | .029 |
| Maternal death, n (%) | 0 | 2 | .245 |
| Neonatal sex, n (%) | |||
| Female | 24,032 (49.2) | 23,419 (48.8) | .445 |
| Male | 24,793 (50.8) | 24,497 (51.1) | .282 |
| Not reported | 32 (.03) | 37 (.04) | |
| Neonatal weight, mean (SD), g | 3268.5 (603.9) | 3157.1 (642.5) | <.001 |
| Birth weight categories,c n (%) | |||
| SGA (<10th percentile) | 5886 (12.3) | 5037 (10.8) | <.001 |
| AGA | 37,172 (77.6) | 37,299 (79.9) | <.001 |
| LGA (>90th percentile) | 4820 (10.1) | 4307 (9.2) | <.001 |
| Apgar score <7 at 1 min, n (%) | 3563 (7.4) | 3840 (8.1) | <.001 |
| Apgar score <7 at 5 min, n (%) | 799 (1.7) | 884 (1.8) | <.001 |
| Neonatal intensive care unit admission, n (%) | 5209 (10.7) | 6151 (12.9) | <.001 |
| Stillbirth, neonatal death, n (%) | 326 (0.7) | 423 (0.9) | <.001 |
Abbreviations: AGA, average for gestational age; LGA, large for gestational age; SGA, small for gestational age.
Interprofessional group includes centers with midwifery presence.
Non-interprofessional group includes centers without midwifery presence.
Does not equal 100% because of missing data.
Robson 10-Group Analysis
After initial assessment of the interprofessional and non-interprofessional samples, we categorized all 96,810 births using the Robson criteria. Data for women with any missing values for 1 of the 6 key variables (gestational age, parity, presentation, number of fetuses, mode of labor onset, prior cesarean) of the Robson classification were deleted, resulting in a loss of 456 births (0.5%) from the total sample. Each woman was placed in 1 of the 10 mutually exclusive Robson categories. Robson categories 2 and 4 were further subcategorized into 2a and 2b and 4a and 4b, differentiating prelabor cesarean from cesarean births following induced labor. For the categorized births (n = 96,354), we compared 1) the proportions of women within each of the 10 Robson categories, 2) the cesarean birth rate within each Robson category, and 3) the contribution of the cesarean rate for each Robson category to the total cesarean birth rate between the interprofessional and non-interprofessional groups (Table 4).
Table 4.
Robson Categories by Care Group Comparisons (N = 96,810)
| Interprofessional Care Groupa |
Non-interprofessional Care Groupb |
|||||||
|---|---|---|---|---|---|---|---|---|
| Robson Category | Participants n (%)c | Cesareans n (%)d | Absolute Contribution to Overall Cesarean Rate %e | Relative Contribution to Overall Cesarean Rate %f | Participants n (%)c | Cesareans n (%)d | Absolute Contribution to Overall Cesarean Rate %e | Relative Contribution to Overall Cesarean Rate %f |
| 1 | 10,581 (21.7) | 1809 (17.1) | 3.7 | 14.2 | 6070 (12.7)g | 987 (16.3) | 2.1g | 6.2g |
| 2 | 5429 (11.1) | 2265 (41.7) | 4.7 | 17.9 | 11,198 (23.4)g | 4212 (37.6)g | 8.8g | 26.3g |
| 2a | 4929 (10.2) | 1765 (35.8) | 3.6 | 13.9 | 10,022 (20.9)g | 3036 (30.3) | 6.3g | 19.0g |
| 2b | 500 (1.0) | 500 (100) | 1.0 | 3.9 | 1176 (2.5) | 1176 (100) | 2.5 | 7.3g |
| 3 | 15,446 (31.6) | 453 (2.9) | 0.9 | 3.6 | 8043 (16.8)g | 284 (3.5) | 0.6g | 1.8g |
| 4 | 5133 (10.5) | 703 (13.7) | 1.4 | 5.5 | 7989 (16.7)g | 975 (12.2) | 2.0g | 6.1 |
| 4a | 4830 (10.0) | 373 (7.7) | 0.8 | 2.9 | 7510 (15.7) | 496 (6.6) | 1.0 | 3.1 |
| 4b | 330 (0.68) | 330 (100) | 0.7 | 2.6 | 479 (1.0) | 479 (100) | 1.0 | 3.0 |
| 5 | 5311 (10.9) | 3919 (73.8) | 8.1 | 30.9 | 5697 (11.9)g | 4849 (85.1)g | 10.1g | 30.3 |
| 6 | 746 (1.5) | 731 (98.0) | 1.5 | 5.8 | 769 (1.6) | 764 (99.4) | 1.6 | 4.8g |
| 7 | 742 (1.5) | 701 (94.5) | 1.4 | 5.5 | 620 (1.3) | 596 (96.1) | 1.2 | 3.7g |
| 8 | 979 (2.0) | 638 (65.2) | 1.3 | 5.0 | 1314 (2.7)g | 972 (74.0)g | 2.0g | 6.1g |
| 9 | 34 (0.1) | 34 (100) | 0.1 | 0.3 | 64 (0.1) | 63 (98.4) | 0.1 | 0.4 |
| 10 | 4121 (8.4) | 1414 (34.3) | 2.9 | 11.2 | 6068 (12.7)g | 2318 (38.2)g | 4.8g | 14.5g |
| Total | 48,522h | 12,667 (26.1) | 26.0 | 99.9i | 47,832h | 16,020 (33.5)g | 33.3 | 100.3i |
Interprofessional group includes centers with midwifery presence.
Non-interprofessional group includes centers without midwifery presence.
Percentage = number of women in the group ÷ total number of women who gave birth in the setting × 100.
Percentage = number of cesareans in the group ÷ total number of women in the group × 100.
Percentage = number of cesareans in the group ÷ total number of women who gave birth in the setting × 100.
Percentage = number of cesareans in the group ÷ total number of cesareans in the setting × 100.
Statistically significant differences, P < .001.
Births not classified because of missing data: interprofessional, n = 335 (0.69%), non-interprofessional, n = 121 (0.25%), accounting for differences in total births in table (n = 96,354) and total births in sample (N = 96,810).
Total percentages may not add up because of rounding.
Proportions of Women Within Each of the 10 Robson Categories
There were significant differences (P < .001) between the interprofessional and non-interprofessional groups in the proportions of births to women in spontaneous labor (categories 1 and 3), in induced labor (categories 2 and 4), with a prior cesarean birth (category 5), or with a preterm birth (category 10). There were significantly more nulliparous (category 1) and multiparous (category 3) women at term gestation with a single cephalic presenting fetus experiencing spontaneous onset of labor in the interprofessional group compared with the non-interprofessional group (nulliparous, 21.7% vs 12.7%, P < .001; multiparous, 31.6% vs 16.8%, P < .001). Women experiencing prelabor cesarean birth (categories 2b and 4b) were comparatively small proportions in both groups (range, 0.68%−2.5%). The proportions of births to women with the fetus in breech presentation (categories 6 and 7), multiple gestations (category 8), and abnormal lies (category 9) were similar between the 2 groups (Table 4).
Cesarean Rates by Robson Category
Cesarean birth rates were significantly different between the care groups in Robson categories 2, 5, 8, and 10 (Table 4). Cesarean rates were significantly higher in the interprofessional care group for nulliparous women with induced labor (category 2, 41.7% vs 37.6%, P < .001) and significantly lower in the interprofessional care group for women with a previous cesarean birth (category 5, 73.8% vs 85.1%, P < .001). In the interprofessional group, cesarean rates were lower for women with multiple pregnancies (category 8, 65.2% vs 74.0%, P < .001) and women with single, cephalic, preterm fetuses (category 10, 34.3% vs 38.2%, P < .001). Prelabor cesarean births (categories 2b and 4b) were less than or equal to 1% of cesarean births in interprofessional centers, whereas in non-interprofessional centers, nulliparous prelabor cesarean births (category 2b) accounted for 2.5% of births.
Robson Categories’ Contributions to Overall Cesarean Rate
Nulliparous women (categories 1 and 2) and women with prior cesarean birth (category 5) were the largest contributors to the overall cesarean birth rate in both groups. Together, women in Robson categories 1, 2, and 5 contributed over 50% of cesarean births in the total sample. Cesarean birth for women with a prior uterine scar (category 5) was the largest contributor to the total cesarean birth rate in both the interprofessional care group (8.0%) and the non-interprofessional care group (10.1%). The proportion of women with a previous uterine scar (category 5) were similar in interprofessional and non-interprofessional groups, comprising 11% and 12% of each group, respectively; however, the cesarean rates differed significantly, with lower rates of cesarean in the interprofessional group (74%) versus the non-interprofessional group (85%, P < .001). The contribution of women in spontaneous labor (categories 1 and 3 summed) to the total cesarean rate was lower (2.7%) in the non-interprofessional care group compared with the interprofessional care group (4.6%). Conversely, the contribution of women with induced labor (categories 2 and 4 summed) to the total cesarean birth rate was lower in the interprofessional group (6.0% vs 10.9%, P < .001). The contribution of prelabor cesarean birth to the overall cesarean rate in each group (category 2b, 1.0 % vs 2.5%, P = .02; category 4b, 0.7% vs 1.0%, P = .34) was smaller in comparison with cesarean following labor induction (category 2a, 3.6% vs 6.3%, P < .001; category 4a, 0.8% vs 1.0%, P = .03).
Multivariate Regression
Because there were differences between the interprofessional and non-interprofessional groups in maternal demographic and comorbid characteristics known to be associated with cesarean birth,32,33 we conducted logistic regression, controlling each of the variables listed in Table 5. Regression results showed that differences in overall cesarean birth rates remained significant between groups, with women in non-interprofessional care centers across all Robson categories combined more likely to experience cesarean birth (adjusted odds ratio [aOR], 1.62; 95% CI, 1.56–1.68; P < .001).
Table 5.
Unadjusted and Adjusteda Odds Ratios of Cesarean in Non-Interprofessionalb Centers Within the Robson 10 Categories
| Robson Category | Unadjusted |
Adjusteda |
||
|---|---|---|---|---|
| OR (95% CI) | P Value | aOR (95% CI) | P Value | |
| 1 | 0.94 (0.87–1.03) | .165 | 1.33 (1.18–1.5) | <.001 |
| 2ac | 0.84 (0.79–0.9) | <.001 | 1.21 (1.12–1.32) | <.001 |
| 3 | 1.21 (1.04–1.41) | .013 | 1.26 (1.00–1.57) | .05 |
| 4ac | 0.88 (0.79–0.97) | .013 | 1.23 (1.06–1.42) | .005 |
| 5 | 2.03 (1.85–2.23) | <.001 | 1.73 (1.51–1.99) | <.001 |
| 6 | NAd | NAd | ||
| 7 | NAe | NAe | ||
| 8 | 1.52 (1.27–1.82) | <.001 | 1.59 (1.23–2.06) | <.001 |
| 9 | NAf | NAf | ||
| 10 | 1.18 (1.09–1.29) | <.001 | 1.45 (1.28–1.64) | <.001 |
| Cesarean Total | 1.42 (1.38–1.46) | <.001 | 1.62 (1.56–1.68) | <.001 |
Abbreviations: aOR, adjusted odds ratio; NA, not applicable; OR, odds ratio.
Adjusted for site and center, year of birth, race and ethnicity, diabetes, chronic hypertension or gestational hypertension, heart disease, renal disease, depression, anemia, and body mass index on admission for birth.
Reference group: interprofessional group, which includes centers with midwifery presence. Non-interprofessional group includes centers without midwifery presence.
Only births with induced labor (categories 2a and 4a) were included for regression analysis. Prelabor cesarean births (2b and 4b) were excluded in the regression analysis.
Only 20 (<0.01%) vaginal births in this group among everyone.
Only 65 (<0.01%) vaginal births in this group among everyone.
Only one vaginal birth in this group among everyone.
Nulliparous women with induced labor (category 2a) were significantly more likely to have cesarean birth in the interprofessional care group (odds ratio, 0.84; 95% CI, 0.79–0.9; P < .001), but once adjusted, the differences switched direction to show a significantly higher odds of cesarean among women in the non-interprofessional care group (aOR, 1.21; 95% CI, 1.12–1.32; P < .001). Women with a prior cesarean (category 5) were significantly more likely to have a cesarean birth in a non-interprofessional care center than in an interprofessional center (aOR, 1.73; 95% CI, 1.51–1.99; P < .001).
DISCUSSION
Robson classifications provide meaningful comparisons between centers with and without interprofessional care. There were significant and clinically meaningful differences in perinatal outcomes between US academic centers with both midwife and physician care providers compared with centers with physician-only care models. Women receiving care at interprofessional centers were less likely to have labor induced and were at lower overall risk for cesarean birth. The primary driver of the lower cesarean birth rate in interprofessional centers was the higher rates of vaginal birth after cesarean (VBAC). This finding is consistent with a recent study of midwife-physician collaboration that reported lower overall cesarean birth rates and higher VBAC rates.22
Women were more likely to achieve vaginal birth when labor was induced in centers without midwives. Although this advantage of lower cesarean rates following labor induction in centers without midwives did not persist in analyses accounting for maternal demographic and comorbidity factors, the differences in vaginal birth following labor induction between groups may be related to variables not included in the Robson classification system. For example, significantly more women receiving care with interprofessional teams gave birth at full-term, late-term, or post-term gestation compared with those receiving care with non-interprofessional teams. Differences in use of labor induction between the groups may signal that in interprofessional centers, women undergoing induction of labor may be more likely to have pregnancy complications affecting their risk of needing a cesarean (eg, abnormal results of fetal testing). Future studies should assess the effects of maternal and fetal characteristics, particularly gestational age, as well as differing labor induction guidelines and practices, on the likelihood of vaginal birth following induction of labor as well as VBAC.
Our study focused on broader perinatal care team composition rather than outcomes by specific types of perinatal care providers. It is not known whether centers with midwives in the CSL had midwifery-led care or an integrated collaborative care model.12 However, the observed differences in labor processes and outcomes noted are likely not fully attributable to the care provided by specific perinatal care providers (eg, midwives vs physicians) or care models, but may be influenced by multiple system factors. For example, the presence of midwives in a hospital may shift the institution’s unit culture and approach to birth.11 Alternately, hospitals with a culture favoring vaginal birth may actively recruit and retain midwives. Understanding if midwives affect hospital-level approaches to perinatal care is an important direction for future research to identify factors that contribute to hospital-level variation in labor processes and outcomes.
Cesarean Rates and Unit Culture
Our findings demonstrate that the presence of midwives as part of intrapartum care teams is associated with significant reductions in rates of labor induction and cesarean birth as well as significant increases in VBAC rates. It is possible that these results reflect the influence of midwifery training and values. The midwifery philosophy of care places value on minimizing the use of intervention, and the American College of Nurse-Midwives (ACNM) hallmarks of midwifery promote nonintervention in physiologic processes.37 ACNM advocates for increased access to VBAC38 and supports recent moves to increase in-hospital access to trial of labor after a previous cesarean birth.39
In unadjusted analysis, results also demonstrated that care provided by physician-only intrapartum teams was more frequently associated with vaginal birth among women whose labors were induced. The Robson approach does not evaluate reasons for induction of labor, so our results do not identify if labor inductions differed by indication between the groups. Until the 2018 release of a large trial regarding labor induction versus expectant management,40 evidence suggested that induction of labor without medical indication was associated with an increased rate of cesarean birth.41 Future research examining the effect of labor induction practices and cultures of perinatal care in broader populations, including understanding the effect of interprofessional versus non-interprofessional teams, is essential for informing safe and effective labor induction practices.
Although perinatal care researchers have examined maternal risk factors for cesarean birth, such as maternal age or BMI, evidence suggests that organizational or unit-level factors contribute to a large variation in cesarean birth rates.9,10,42 Variation in cesarean rates between institutions may relate to differences in approaches to labor and birth management within an organization. Examples include perinatal care providers’ approaches to antenatal decision making regarding elective cesarean birth,43 characteristics of birth settings,11,44 differing perinatal care models,36,45,46 and social interaction effects that normalize intervention rates among neighboring hospitals.47
Other aspects of birth culture known to affect the likelihood of cesarean include use of intervention during uncomplicated labors,48 allowance of sufficient time for labor to progress,49 use of universal electronic fetal monitoring,50 and differences in care provided by labor and birth unit nurses.51 As our findings suggest, differences in perinatal care providers’ approaches to labor and birth management may affect cesarean birth utilization, use of labor induction, and effectiveness of trial of labor after cesarean. It is difficult to determine if unit culture is shaped by on-the-ground care providers or by the administrative leadership that recruits, trains, and retains nurses, staff, midwives, and physicians.
Limitations
This was a secondary analysis of data from a data set collected between 2002 and 2008. In the time since these data were collected, there has been considerable change in cesarean birth practice patterns. The available midwifery care variables in this data set could not be used to distinguish the role midwives played in specific women’s intrapartum care, and therefore 6 centers with indeterminate documentation of midwifery unit-level presence could not be included in the analysis. The study sample of predominately urban, university-affiliated hospitals likely has different labor and birth practices, including providing access to VBAC, than rural or community hospital practice settings, thus reducing generalizability across birth settings. Within our sample, maternal characteristics were different between the interprofessional and non-interprofessional groups, particularly race and insurance status, which are known to be associated with differences in outcomes. However, our results remained significant when these factors were controlled in the adjusted logistic regression analyses, only switching direction among nulliparous women with induced labor (category 2a).
A significant limitation is that the CSL does not include other variables related to differences in unit culture, in particular, the nursing care environment. Other factors that contribute to unit culture, such as attitudes of nurses, midwives, and physicians toward vaginal birth or the ratio of nurses to laboring women, likely have a significant effect on use of labor interventions and cesarean birth.
Although our analysis, using the Robson categories, facilitated identification of differences in cesarean rates and of which Robson category populations contributed most to the overall rate, we did not identify the indications for cesarean. However, prior studies using the CSL data indicated that the diagnosis of labor dystocia in early stages of dilation and nonreassuring fetal status were the primary indications for cesarean birth among nulliparous women whose labors were induced.29
Implications for Research and Policy
Future research is needed to elucidate differences in labor processes and outcomes between interprofessional and non-interprofessional perinatal care provider teams and hospitals. This research would provide valuable information to assist clinicians, administrators, and policy makers in developing strategies for lowering cesarean rates. One impediment to the study of midwifery care is that perinatal care data often only include the provider of record for birth.12 If a woman is referred by a midwife to a physician at any point in the childbearing cycle, midwifery care becomes invisible within most large databases. In addition, the professional background of a woman’s prenatal care provider is almost never identified in perinatal care data sets, limiting analysis of the dose of midwifery care in relationship to perinatal outcomes.12 In the future, data sets should include information to identify women’s exposure to different provider types throughout their perinatal care.
In the United States, midwives are increasingly part of interprofessional health care provider teams. A recent study showed that nearly 30% of obstetricians reported working with midwives in some capacity and that more reported an intention to hire midwives in the future.52 Better understanding of the composition of perinatal care teams and dose of midwifery care also carries policy relevance. The proportion of midwife-attended births varies widely by state, ranging from 0.6% to 27%,53 and may be underreported in state vital statistics.54 State-level health care policy and regulation greatly influence the prevalence and boundaries of midwifery practice.14 Midwives are an integral part of intrapartum care for many US women, yet the scope and influence of midwifery care in the United States remains limited in many states.14 Our findings suggest that policies supporting increased integration of midwifery care a cross the United States, which includes eliminating the systematic barriers to independent midwifery practice, could improve overall cesarean rates and greatly improve rates of VBAC.
The attitudes and beliefs of perinatal care providers toward interventions, such as induction of labor and cesarean birth, affect their utilization.11 Future research may benefit from further exploration of the not easily quantifiable, yet ever-present, effect of differences in philosophical approach to birth that may separate midwives from most other perinatal care providers in the United States. We speculate that drivers of cesarean birth variation are attributable to the attitudes not only of the individual provider11 but of the team as a whole, including nurses, midwives, and physicians. For future research, we recommend 1) clear identification of the type of health care providers involved in each component of perinatal care, 2) evaluation of the regulatory environment for midwifery practice in a given state or hospital,14 and 3) consideration of how the beliefs and practices of individuals, professional groups, and teams within an organization may influence women’s labors and birth outcomes, including a description of how interprofessional perinatal care teams influence unit, hospital, or system-level processes and outcomes.55
CONCLUSION
Our findings demonstrate a benefit of midwifery presence for safe cesarean reduction. There is also evidence that when labor is induced, physician teams may be more successful in achieving vaginal birth overall, but less successful when maternal demographic and comorbid factors are considered. It is possible that cultural drivers within perinatal care teams shape choices with regard to inducing labor or awaiting labor onset, efficacy of achieving vaginal birth during induced labor, and efficacy of achieving VBAC. Identifying these cultural drivers is an essential step to creating health care systems that can uniformly replicate the most effective approaches to perinatal care in all hospital settings. Such findings may guide future research and policy in the pursuit of optimizing the use of cesarean birth for women and neonates most likely to benefit from this intervention.5
Quick Points.
The Robson 10-group classification system can be used to compare differences in cesarean birth utilization among women with similar perinatal characteristics.
Women, particularly women seeking vaginal birth after cesarean, receiving intrapartum care in hospitals with midwives more frequently began labor spontaneously and were more likely to achieve vaginal birth.
Health systems should investigate adding midwives to their intrapartum care teams to decrease overall cesarean birth rates and increase rates of vaginal birth after cesarean.
ACKNOWLEDGMENTS
The data included in this article were obtained from the Consortium on Safe Labor, supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), National Institutes of Health. Institutions involved in the Consortium include, in alphabetical order, Baystate Medical Center, Springfield, MA; Cedars-Sinai Medical Center Burnes Allen Research Center, Los Angeles, CA; Christiana Care Health System, Newark, DE; Georgetown University Hospital, MedStar Health, Washington, DC; Indiana University Clarian Health, Indianapolis, IN; Intermountain Healthcare and the University of Utah, Salt Lake City, UT; Maimonides Medical Center, Brooklyn, NY; MetroHealth Medical Center, Cleveland, OH; Summa Health System, Akron City Hospital, Akron, OH; The EMMES Corporation, Rockville, MD (Data Coordinating Center); University of Illinois at Chicago, Chicago, IL; University of Miami, Miami, FL; and University of Texas Health Science Center at Houston, Houston, TX. The authors alone are responsible for the views expressed in this article, which does not necessarily represent the decisions or the stated policy of the NICHD. We would like to thank the Principal Investigators who conducted the original Consortium of Safe Labor study, as well as the NICHD for funding the study and the NICHD Data and Specimen Hub for providing us with the data.
We would like to acknowledge Kasey Abrahamson, MPH, for his statistical assistance.
Footnotes
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Martin JA, Hamilton BE, Osterman MJ, Driscoll AK, Mathews TJ. Births: final data for 2015. Natl Vital Stat Rep. 2017;66(1):1. [PubMed] [Google Scholar]
- 2.Martin JA, Hamilton BE, Osterman MJ, Curtin SC, Matthews TJ. Births: final data for 2013. Natl Vital Stat Rep. 2015;64(1):1–65. [PubMed] [Google Scholar]
- 3.Gibbons L, Belizan JM, Lauer JA, Betran AP, Merialdi M, Althabe F. Inequities in the use of cesarean section deliveries in the world. Am J Obstet Gynecol. 2012;206(4):331.e1–e19. [DOI] [PubMed] [Google Scholar]
- 4.Ye J, Zhang J, Mikolajczyk R, Torloni MR, Gulmezoglu AM, Betran AP. Association between rates of caesarean section and maternal and neonatal mortality in the 21st century: a worldwide population-based ecological study with longitudinal data. BJOG. 2016;123(5):745–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller S, Abalos E, Chamillard M, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet. 2016;388(10056):2176–2192. [DOI] [PubMed] [Google Scholar]
- 6.Torio C, Moore B. National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2013. Healthcare Cost and Utilization Project (HCUP) Statistical Brief 204. Rockville, MD: Agency for Healthcare Research and Quality; 2016. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb204-Most-Expensive-Hospital-Conditions.pdf. Accessed July 11, 2018. [PubMed] [Google Scholar]
- 7.Truven Health Analytics. The Cost of Having a Baby in the United States. Truven Health Analytics Marketscan Study Prepared for Childbirth Connection, Catalyst for Payment Reform, and the Center for Healthcare Quality and Payment Reform. Ann Arbor, MI: Truven Health Analytics; 2013. http://transform.childbirthconnection.org/wp-content/uploads/2013/01/Cost-of-Having-a-Baby.pdf. Accessed July 11, 2018. [Google Scholar]
- 8.Gibson K, Bailit JL. Cesarean delivery as a marker for obstetric quality. Clin Obstet Gynecol. 2015;58(2):211–216. [DOI] [PubMed] [Google Scholar]
- 9.Main EK. Clues for understanding hospital variation among obstetric services. Am J Obstet Gynecol. 2015;213(4):443–444. [DOI] [PubMed] [Google Scholar]
- 10.Kozhimannil KB, Law MR, Virnig BA. Cesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Aff (Millwood). 2013;32(3):527–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.White VanGompel E, Main EK, Tancredi D, Melnikow J. Do provider birth attitudes influence cesarean delivery rate: a cross-sectional study. BMC Pregnancy Childbirth. 2018;18(1):184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Freytsis M, Phillippi JC, Cox KJ, Romano A, Cragin L. The American College of Nurse-Midwives Clarity in Collaboration Project: describing midwifery care in interprofessional collaborative care models. J Midwifery Womens Health. 2017;62(1):101–108. [DOI] [PubMed] [Google Scholar]
- 13.Attanasio L, Kozhimannil KB. Relationship between hospital-level percentage of midwife-attended births and obstetric procedure utilization. J Midwifery Womens Health. 2018;63(1):14–22. [DOI] [PubMed] [Google Scholar]
- 14.Vedam S, Stoll K, MacDorman M, et al. Mapping integration of midwives across the United States: impact on access, equity, and outcomes. PLoS One. 2018;13(2):e0192523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Angelini DJ, O’Brien B, Singer J, Coustan DR. Midwifery and obstetrics: twenty years of collaborative academic practice. Obstet Gynecol Clin North Am. 2012;39(3):335–346. [DOI] [PubMed] [Google Scholar]
- 16.Hutchison MS, Ennis L, Shaw-Battista J, et al. Great minds don’t think alike: collaborative maternity care at San Francisco General Hospital. Obstet Gynecol. 2011;118(3):678–682. [DOI] [PubMed] [Google Scholar]
- 17.Darlington A, McBroom K, Warwick S. A northwest collaborative practice model. Obstet Gynecol. 2011;118(3):673–677. [DOI] [PubMed] [Google Scholar]
- 18.Nielsen PE, Munroe M, Foglia L, et al. Collaborative practice model: Madigan Army Medical Center. Obstet Gynecol Clin North Am. 2012;39(3):399–410. [DOI] [PubMed] [Google Scholar]
- 19.Shaw-Battista J, Fineberg A, Boehler B, Skubic B, Woolley D, Tilton Z. Obstetrician and nurse-midwife collaboration: successful public and private partnership. Obstet Gynecol. 2011;118(3):663–672. [DOI] [PubMed] [Google Scholar]
- 20.DeJoy S, Burkman RT, Graves BW, et al. Making it work: successful collaborative practice. Obstet Gynecol. 2011;118(3):683–686. [DOI] [PubMed] [Google Scholar]
- 21.Osterman MJ, Martin JA. Trends in low-risk cesarean delivery in the United States, 1990–2013. Natl Vital Stat Rep. 2014;63(6):1–16. [PubMed] [Google Scholar]
- 22.Rosenstein MG, Nijagal M, Nakagawa S, Gregorich SE, Kuppermann M. The association of expanded access to a collaborative midwifery and laborist model with cesarean delivery rates. Obstet Gynecol. 2015;126(4):716–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Betran AP, Torloni MR, Zhang JJ, Gulmezoglu AM; WHO Working Group on Caesarean Section. WHO statement on caesarean section rates. BJOG. 2016;123(5):667–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robson MS. Classification of caesarean sections. Fetal Matern Med Rev. 2001;12(1):23–39. [Google Scholar]
- 25.Hehir MP, Ananth CV, Siddiq Z, Flood K, Friedman AM, D’Alton ME. Cesarean delivery in the United States 2005 through 2014: a population-based analysis using the Robson 10-group classification system. Am J Obstet Gynecol. 2018;219(1):105.e1–105.e11. [DOI] [PubMed] [Google Scholar]
- 26.Pasko DN. 879: Comparison of cesarean deliveries in a multicentre U.S. cohort using the WHO Robson 10-group classification system. Am J Obstet Gynecol. 2018;218(suppl 1):S523. [Google Scholar]
- 27.Robson M, Murphy M, Byrne F. Quality assurance: the 10-group classification system (Robson classification), induction of labor, and cesarean delivery. Int J Gynaecol Obstet. 2015;131(suppl 1):S23–S27. [DOI] [PubMed] [Google Scholar]
- 28.Robson MS. The 10-group classification system - a new way of thinking. Am J Obstet Gynecol. 2018;219(1):1–4. [DOI] [PubMed] [Google Scholar]
- 29.Zhang J, Landy HJ, Branch DW, et al. ; Consortium on Safe Labor. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2010;116(6):1281–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Consortium on Safe Labor (CSL). Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Data and Specimen Hub (DASH) website. https://dash.nichd.nih.gov/study/2331. Accessed November 2, 2018.
- 31.CSL Linked by Pregnancy DatasetAll Sites. In: Consortium on Safe Labor (CSL). Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Data and Specimen Hub (DASH) website. https://dash.nichd.nih.gov/study/2331. Accessed May 3, 2019.
- 32.Murphy PA, Fullerton JT. Development of the Optimality Index as a new approach to evaluating outcomes of maternity care. J Obstet Gynecol Neonatal Nurs. 2006;35(6):770–778. [DOI] [PubMed] [Google Scholar]
- 33.Kominiarek MA, VanVeldhuisen P, Gregory K, Fridman M, Kim H, Hibbard JU. Intrapartum cesarean delivery in nulliparas: risk factors compared by two analytical approaches. J Perinatol. 2015;35(3): 167–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Neal JL, Carlson NS, Phillippi JC, et al. Midwifery presence in United States medical centers and labor care and birth outcomes among low-risk nulliparous women: a Consortium on Safe Labor study [published online November 11, 2018]. Birth. 10.1111/birt.12407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carlson NS, Neal JL, Tilden EL, et al. Influence of midwifery presence in United States centers on labor care and outcomes of low-risk parous women: a Consortium on Safe Labor study [published online November 9, 2018]. Birth. 10.1111/birt.12405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carlson NS, Corwin EJ, Hernandez TL, Holt E, Lowe NK, Hurt KJ. Association between provider type and cesarean birth in healthy nulliparous laboring women: a retrospective cohort study. Birth. 2018;45(2):159–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.American College of Nurse-Midwives. Core Competencies for Basic Midwifery Practice. Silver Spring, MD: American College of Nurse-Midwives; 2012. [Google Scholar]
- 38.American College of Nurse-Midwives. Care for women desiring vaginal birth after cesarean. J Midwifery Womens Health. 2011;56(5): 517–525. [DOI] [PubMed] [Google Scholar]
- 39.Committee on Practice Bulletins – Obstetrics, American College of Obstetricians and Gynecologists. Practice bulletin no. 184: Vaginal birth after cesarean delivery. Obstet Gynecol. 2017;130(5):e217–e233. [DOI] [PubMed] [Google Scholar]
- 40.Grobman WA, Rice MM, Reddy UM, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379(6):513–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ehrenthal DB, Jiang X, Strobino DM. Labor induction and the risk of a cesarean delivery among nulliparous women at term. Obstet Gynecol. 2010;116(1):35–42. [DOI] [PubMed] [Google Scholar]
- 42.Barber EL, Lundsberg L, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Contributing indications to the rising cesarean delivery rate. Obstet Gynecol. 2011;118(1):29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sinnott SJ, Brick A, Layte R, Cunningham N, Turner MJ. National variation in caesarean section rates: a cross sectional study in Ireland. PLoS One. 2016;11(6):e0156172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Snowden JM, Tilden EL, Snyder J, Quigley B, Caughey AB, Cheng YW. Planned out-of-hospital birth and birth outcomes. N Engl J Med. 2015;373(27):2642–2653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nijagal MA, Kuppermann M, Nakagawa S, Cheng Y. Two practice models in one labor and delivery unit: association with cesarean delivery rates. Am J Obstet Gynecol. 2015;212(4):491. e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Srinivas SK, Small DS, Macheras M, Hsu JY, Caldwell D, Lorch S. Evaluating the impact of the laborist model of obstetric care on maternal and neonatal outcomes. Am J Obstet Gynecol. 2016;215(6): 770.e1–e9. [DOI] [PubMed] [Google Scholar]
- 47.Guccio C, Lisi D. Thus do all. Social interactions in inappropriate behavior for childbirth services in a highly decentralized healthcare system. Reg Sci Urban Econ. 2016;61:1–17. [Google Scholar]
- 48.Kennedy HP, Shannon MT. Keeping birth normal: research findings on midwifery care during childbirth. J Obstet Gynecol Neonatal Nurs. 2004;33(5):554–560. [DOI] [PubMed] [Google Scholar]
- 49.Carlson NS, Lowe NK. A concept analysis of watchful waiting among providers caring for women in labour. J Adv Nurs. 2014;70(3): 511–522. [DOI] [PubMed] [Google Scholar]
- 50.Goodrick E, Salancik GR. Organizational discretion in responding to institutional practices: hospitals and cesarean births. Adm Sci Q. 1996;41(1):1–28. [Google Scholar]
- 51.Edmonds JK, O’Hara M, Clarke SP, Shah NT. Variation in cesarean birth rates by labor and delivery nurses. J Obstet Gynecol Neonatal Nurs. 2017;46(4):486–493. [DOI] [PubMed] [Google Scholar]
- 52.Farrow VA, Lawrence H, Schulkin J. Women’s healthcare providers’ range of services and collaborative care. J Healthc Qual. 2014;36 (2):39–49. [DOI] [PubMed] [Google Scholar]
- 53.Declercq E Midwife-attended births in the United States, 1990–2012: results from revised birth certificate data. J Midwifery Womens Health. 2015;60(1):10–15. [DOI] [PubMed] [Google Scholar]
- 54.Biscone ES, Cranmer J, Lewitt M, Martyn KK. Are CNM-attended births in Texas hospitals underreported? J Midwifery Womens Health. 2017;62(5):614–619. [DOI] [PubMed] [Google Scholar]
- 55.Blomberg M Avoiding the first cesarean section - results of structured organizational and cultural changes. Acta Obstet Gynecol Scand. 2016;95(5):580–586. [DOI] [PubMed] [Google Scholar]