Lightheadedness upon rapid standing is common. If systolic/diastolic blood pressure (BP) are reduced by >40/20 mm Hg this is denoted “initial orthostatic hypotension” (IOH) (Figure 1A) (1). Clinical history indicates rapid resolution of hypotension and is diagnostic of IOH. During IOH, changes in BP are rapid and are rarely detected by sphygmomanometry, requiring beat-to-beat monitoring with finger photoplethysmography. Smaller systolic BP decrements in healthy youngsters of 14 to 28 mm Hg normalize within 10 to 20 s (2). Excessive tachycardia occurs during IOH, but its extent and duration are not well-described. Thus, IOH patients are erroneously referred for postural tachycardia syndrome (POTS). We hypothesize that the magnitude and duration of tachycardia in IOH suffice to confuse IOH with POTS.
FIGURE 1. Events During IOH and ΔHR as a Function of Time.
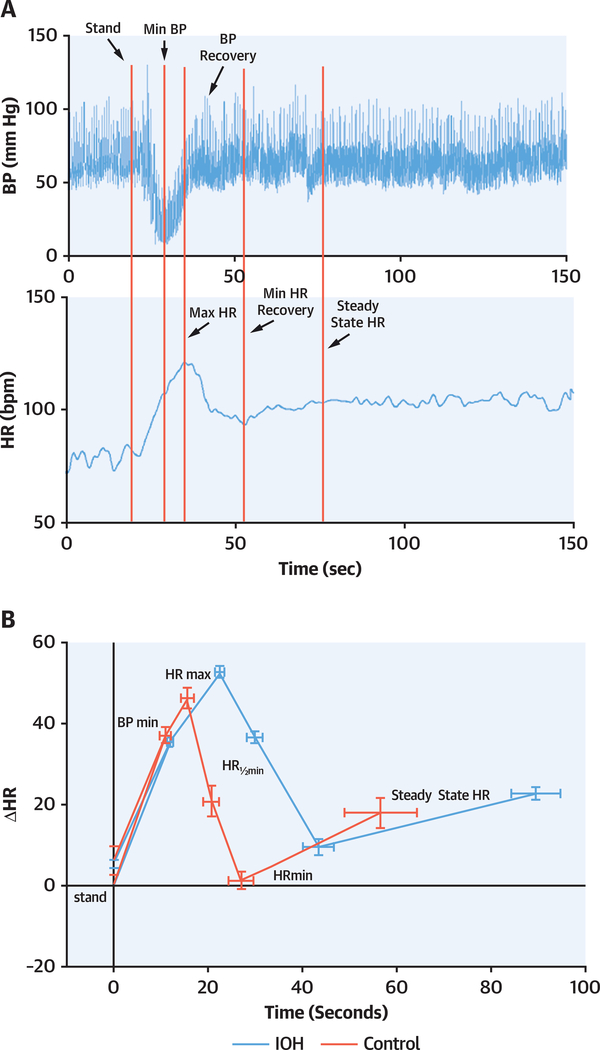
(A) Blood pressure (BP) (top) and heart rate (HR) (bottom) in a representative IOH patient. Events are demarcated. (B) Mean ΔHR in initial orthostatic hypotension (IOH) patients (red) and control subjects (blue) during the first 100 s of standing. Horizontal error bars represent SEM of event timing. HR recovery is prolonged in IOH.
To delimit the range and duration of upright tachycardia in IOH, we enrolled symptomatic IOH patients (n = 62; age 16 ± 3 years; 30 female patients) with daily orthostatic symptoms, and healthy volunteers (n = 15; age 16 ± 3 years; 8 female volunteers). Cardiac disease was ruled out in all. Exclusion criteria included systemic illness, bed rest, nicotine use, or recent past pregnancy. No subjects were taking medications, including neurally active or vasoactive drugs. Subjects refrained from xanthine-containing products for >72 h and fasted for 3 h before testing.
Subjects were instrumented for electrocardiography and for beat-to-beat blood pressure (Finometer, FMS, Amsterdam, the Netherlands) calibrated to brachial BP. Subjects free of POTS or syncope based on a 10-min 70° head-up tilt were retained and their response to a standing test was examined. After 10 min in a supine position, subjects stood for 5 min. Patients fulfilled IOH criteria during the standing test, which duplicated real-world symptoms.
Baseline data (mean ± SD) were similar in IOH compared with control subjects: BP 110 ± 17/56 ± 9 mm Hg; heart rate (HR) 68 ± 11 beats/min versus BP 111 ± 9/54 ± 5 mm Hg; HR 73 ± 5 beats/min. Three variables—heart rate change (ΔHR), BP, and time—were dependent on events defined as minimum BP, BP recovery, peak HR, HR minimum, and steady state (Figure 1A). IOH and control over events were analyzed by repeated measures analysis of variance. We evaluated a group-by-period interaction term to determine whether response patterns differed between IOH and control subjects.
Comparing IOH with control subjects: peak HR was similar (121 ± 13 beats/min vs. 120 ± 12 beats/min), BP nadir was reduced (p < 0.001; 66 ± 15/30 ± 10 mm Hg vs. 86 ± 14/42 ± 7 mm Hg), and peak BP was the same (132 ± 19/65 ± 13 mm Hg vs. 137 ± 22/63 ± 12 mm Hg). There were no group differences in HR or BP at events except for BP at its nadir (by definition of IOH).
The time (seconds) at which events occur was, however, significantly (p < 0.005) different for IOH and control subjects (Figure 1B). Beginning at peak HR, events occur later in IOH patients compared with control subjects. Figure 1B depicts ΔHR versus time presented as averages ± SEM. Comparing IOH with control, time to minimum BP (nadir) = 12.0 ± 0.6 s versus 11.0 ± 1.0 s (p = 0.5); time to Peak HR = 22.5.0 ± 0.7 s versus 15.7 ± 1.3 s (p < 0.01); time to BP recovery = 26.4 ± 0.9 s vs. 20.7 ± 2.5 s (p < 0.025); time to HR recovery = 42.8 ± 3.3 s versus 27.0 ± 2.6 s (p < 0.025); and time to steady state = 89.5 ± 5.2 s versus 55.0 ± 7.8 s (p < 0.005).
Mean HR was excessively increased (ΔHR >40 beats/min) in IOH and control subjects. However, while ΔHR >40 beats/min was present in 7 of 15 (47%) of control subjects for an average of 5 s, ΔHR >40 beats/min was present in 54 of 62 (87%) of IOH patients for nearly 30 s.
IOH has been regarded as an expected consequence of physiological changes in response to rapid shifts of blood by gravity. IOH patients have decreased nadir BP and prolonged time to BP recovery, suggesting deficits in adrenergic vasoconstriction or hypovolemia (3). The most striking finding is overall reduced “speed of heart rate recovery in response to orthostatic challenge” considered to be deficient parasympathetic control, a predictor of mortality in adults (4). We infer that reduced speed of HR recovery in young IOH patients also implies parasympathetic autonomic dysfunction not previously considered (5).
Acknowledgments
Please note: Funding for this project was provided by grants RO1 HL 112736 and RO1 HL 134674 from the National Heart, Lung, and Blood Institute. The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
REFERENCES
- 1.Wieling W, Krediet CT, van Dijk N, Linzer M, Tschakovsky ME. Initial orthostatic hypotension: review of a forgotten condition. Clin Sci 2007;112:157–65. [DOI] [PubMed] [Google Scholar]
- 2.Tanaka H, Thulesius O, Borres M, Yamaguchi H, Mino M. Blood pressure responses in Japanese and Swedish children in the supine and standing position. Eur Heart J 1994;15:1011–9. [DOI] [PubMed] [Google Scholar]
- 3.van Wijnen VK, Hove DT, Finucane C, et al. Hemodynamic mechanisms underlying initial orthostatic hypotension, delayed recovery and orthostatic hypotension. J Am Med Dir Assoc 2018;19:786–92. [DOI] [PubMed] [Google Scholar]
- 4.McCrory C, Berkman LF, Nolan H, O’Leary N, Foley M, Kenny RA. Speed of heart rate recovery in response to orthostatic challenge. Circ Res 2016;119: 666–75. [DOI] [PubMed] [Google Scholar]
- 5.Stewart JM, Clarke D. “He’s dizzy when he stands up”: an introduction to initial orthostatic hypotension. J Pediatr 2011;158:499–504. [DOI] [PMC free article] [PubMed] [Google Scholar]