Abstract
Histoplasmosis is uncommon in many parts of the world, including Bangladesh, where, in recent years, cases are increasingly reported. We sought to describe the sociodemographic characteristics, clinical presentation, investigations, treatment, and outcome of histoplasmosis in Bangladesh. We conducted a retrospective data review of published literature from 1962 to 2017, containing information on histoplasmosis in and/or from Bangladesh. Unpublished, well-documented histoplasmosis cases were also included. A total of 26 male patients aged 8–75 years, with a diagnosis of histoplasmosis were included; nine were farmers, seven had diabetes, one was a renal transplant recipient, and four had HIV/AIDS. Fever (n = 20), weight loss (n = 17), anemia (n = 15), lymphadenopathy (n = 9), and hepatosplenomegaly (n = 7) were common. Eleven patients had bilateral adrenal enlargement. Diagnosis was confirmed by histo/cytopathology from skin (n = 1), oropharyngeal ulcers (n = 8), lymph nodes (n = 3), adrenal glands (n = 11), paravertebral soft tissue (n = 2), and bone marrow (n = 4). Cultures of representative samples and antibodies were detected in three and two cases, respectively. Twenty-two patients had disseminated histoplasmosis and four patients had localized oropharyngeal disease. Nine patients were prescribed anti-tuberculosis drugs empirically before establishing the diagnosis of histoplasmosis. Treatment consisted of amphotericin B and itraconazole. Six patients died in hospital, 14 patients recovered with relapse in two cases, and the outcome of the other patients could not be ascertained. Histoplasmosis is thought to be endemic in Bangladesh, but few cases are reported to date, which may be due to many asymptomatic, undiagnosed, misdiagnosed, or under-reported cases. Histoplasmosis should be considered as a differential in appropriate clinical scenarios.
Keywords: Bangladesh, Histoplasmosis, Histoplasma capsulatum
Introduction
Histoplasmosis is a systemic fungal infection caused by dimorphic fungus Histoplasma capsulatum, which is widely distributed throughout the world, but the greatest endemicity is reported in the Americas, especially along the Mississippi and Ohio river valleys.1,2 Its mycelial form is found in soil rich in bird and bat droppings.3 Airborne conidia enter into the human lungs by inhalation, where they germinate into yeast form.4,5 The host response to infection depends upon the size of the infective inoculum, the underlying health of the patient, and host immune status.1 Most infections remain asymptomatic or mild respiratory symptoms may occur in immunocompetent individuals, but in immunodeficient patients, dissemination may occur to involve various organs including the oropharynx, lymph nodes, liver, spleen, skin, and adrenal glands.2,4-11 Reactivation of latent infections may complicate recipients of solid organ transplants and patients receiving immunosuppressive therapy for other reasons.12,13 Symptoms depend upon organ involvement; fever and weight loss are common features,4-11 and the clinical presentation often mimics tuberculosis.6 Diagnosis depends on identification of the organism in culture or histopathological examination findings of tissue biopsy samples or serological tests.2
In Bangladesh, one-fifth of the population exhibited positive skin sensitivity reaction to histoplasmin,14,15 with the first case of histoplasmosis reported in 1982.16 Cases were infrequent but in recent years, a good number of cases, mostly disseminated forms, have been reported in immunodeficient and immunocompetent patients.17-31 In this systematic review, we describe the sociodemographic characteristics, clinical features, diagnostic proofs, treatment, and outcome of histoplasmosis in Bangladesh.
Methods
We systematically searched to identify all previously published English literature containing information regarding histoplasmosis in/or from Bangladesh. Searches were conducted via "PubMed" using the keywords "Bangladesh", "Histoplasma capsulatum", and "histoplasmosis". We also systematically searched through Bangladesh Journals Online (BanglaJOL) for articles published in local journals. The search engine "Google" was also used to identify articles. All literature searches were conducted up to 31 December 2017. Searches were conducted by the first two authors individually and then cross-checked by all the authors. Unpublished but well-documented cases (seven cases) were added. Cases mentioned elsewhere with inadequate information7,32,33 and possible repetitions21,34 were excluded [Figure 1].
Figure 1.
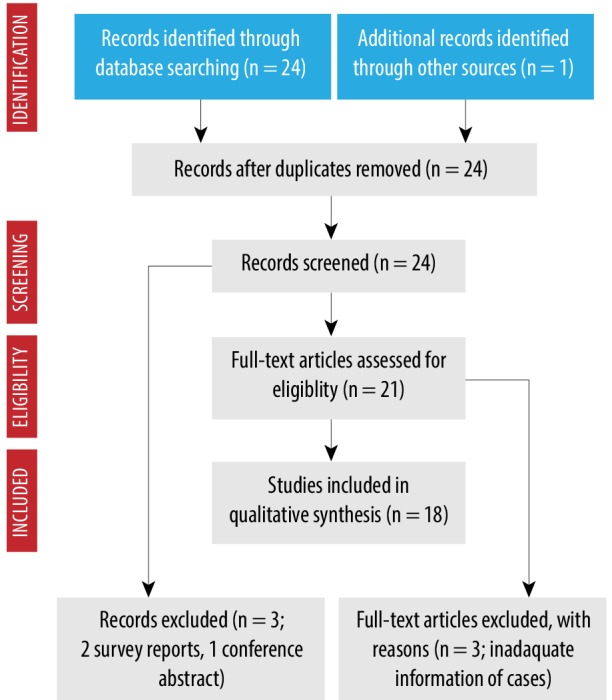
Flow diagram for histoplasmosis cases in Bangladesh.
Histoplasmosis cases were analyzed for selected sociodemographic characteristics including age and sex, immune status, endemicity, travel history, site(s) of disease, proof of diagnosis, treatment given, and the outcome recorded. Immunodeficiency status included patients with HIV or AIDS, those receiving immunosuppressive drugs, organ transplant recipients, patients with diabetes mellitus, and those with congenital immunodeficiency. Patients were categorized as having localized or systemic histoplasmosis. Systemic disease was characterized as single organ disease or disseminated forms. Disseminated disease was defined when a typical organism was grown in cultures or typical histopathological findings were identified from samples of extrapulmonary sites along with systemic symptoms.7,9 Endemicity was labeled where the patient had never traveled outside Bangladesh.
Results
Twenty-four articles were identified from published literature including 18 case reports, three research articles, two survey reports, and one conference abstract; and one article was identified from another source (Figure 1, Table 1, case no 22). From them, two cases were excluded because of repetition, three research articles were excluded because of inadequate information for cases (references 7,33) and presumptive diagnosis (reference 32), two skin survey reports (references 14,15), and one conference abstract was excluded. Finally, a total of 19 cases were eligible for analysis from published literature (total 18 articles) [Figure 1], to which seven unpublished but well-documented cases were added to make the total number of cases 26 [Table 1].
Table 1. Cases of histoplasmosis in/or from Bangladesh (N = 26).
| Patient number/ Journal, Year/ Reference |
Age/ Sex/ Occupation |
Immune status | Clinical presentation | Physical signs | Important laboratory and imaging findings |
Diagnostic test and form of histoplasmosis |
Treatment and outcome |
|---|---|---|---|---|---|---|---|
| 1/ BMRC Bull, 198216 |
69 years/ Male/ Not known |
Not known | Nodular lesion in oral mucosa | Submandibular lymphadenopathy Hepatosplenomegaly |
- | Histopathology from oral nodule. Disseminated histoplasmosis. |
Amphotericin B. Anti-TB prescription. Cured with relapse at 16th month. |
| 2/ JBCPS, 200535 |
41 years/ Male/ Businessman |
Positive anti-HIV | Fever Weight loss Anorexia Sore throat Loose motion |
Anemia Oral moniliasis Dehydration Cervical lymphadenopathy Hepatosplenomegaly |
Hb = 7.7 gm/dL WBC = 3800/cmm Platelets = 150 000/cmm |
Bone marrow study. Disseminated histoplasmosis. |
Itraconazole. Expired in hospital due to septic shock. |
| 3/ Transpl Infect Dis, 201017 |
60 years/ Male/ Builder |
T2DM Renal transplant recipient |
Fever Sore throat |
Skin nodules | Hb = 11.1 gm/dL WBC = 3100/cmm LDH = 256 IU/L Abnormal chest imaging (nodules) |
Biopsy and culture from skin nodule, broncho-alveolar lavage, and transbronchial biopsy. Epiglottic biopsy. Disseminated histoplasmosis. |
Lipid amphotericin B. Itraconazole for an indefinite period. History of INH prophylaxis. Cured, no recurrence up to 2 years. |
| 4/ BSMMUJ, 201018 |
45 years/ Male/ Fishing farm worker |
HIV-negative | Fever Weight loss Abdominal pain |
Anemia Generalized lymphadenopathy Growth in the oral cavity Ascites |
Hb = 9.1 gm/dL ESR = 40 mm in first hour |
Biopsy and histopathology from tongue growth and lymph node. Disseminated histoplasmosis. |
Amphotericin B. Itraconazole (planned for one year). Improved up to six weeks. |
| 5/ JHPN, 201019 |
32 years/ Male/ Storekeeper |
Diagnosed AIDS | Fever Weight loss Anorexia |
Cervical lymphadenopathy Splenomegaly Maculopapular rash |
Hb = 9.6 gm/dL Esophageal candidiasis CD4 = 19/uL |
Histopathology from lymph node. Disseminated histoplasmosis. |
Amphotericin B (0.7 mg/kg/d for 21 days). Itraconazole (200 mg 12-h). Anti-TB Not known |
| 6/ J Med, 201020 |
56 years/ Male/ Not known |
HIV-negative | Fever Cough Shortness of breath Disorientation |
Anemia | Hb = 9 gm/dL ESR = 60 mm in first hour Serum creatinine = 2.3 mg/dL Abnormal chest X-ray (infiltrates) |
Bone marrow study. Disseminated histoplasmosis. |
Amphotericin B. Anti-TB (presumptive). Expired due to aspiration pneumonia. |
| 7/ J Med, 201021 |
57 years/ Male/ Farmer |
Not known | Fever Back pain |
Anemia Generalized lymphadenopathy Hepatomegaly Spastic paraparesis |
Hb = 8.9 mg/dL ESR = 90 mm in first hour |
Open biopsy from paravertebral tissue. Disseminated histoplasmosis. |
Not known Not known |
| 8/ Unpublished, 2010* |
8 years/ Male/ Unknown |
Not known | Fever Anorexia Weight loss Diarrhea |
Anemia Generalized lymphadenopathy Hepatosplenomegaly |
Hb = 8.3 gm/dL WBC = 5300/cmm Platelets = 132 000/cmm ESR = 89 mm in first hour |
Lymph node culture. Disseminated histoplasmosis. |
Anti-TB Expired |
| 9/ J Med, 201122 |
65 years/ Male/ School teacher |
HIV-negative | Fever Anorexia Weight loss Abdominal pain Cough Hemoptysis Vomiting Oral ulcer |
Hepatomegaly Lung crepitation |
ALT = 81.9 IU/L AST = 83.2 IU/L Abnormal chest X-ray (reticulonodular shadow). Bilateral adrenal masses. |
FNAC from adrenal gland. Partial adrenal insufficiency. Disseminated histoplasmosis. |
Anti-TB for eight months. Not known |
| 10/ JBCPS, 201123 |
75 years/ Male/ Farmer |
HIV-negative | Fever Anorexia Weight loss |
Anemia Postural hypotension |
ERS = 41 mm in first hour. Bilateral adrenal masses. |
FNAC and culture from adrenal gland. Partial adrenal insufficiency. Disseminated histoplasmosis. |
Amphotericin B (five doses) Itraconazole (one year). Cured, no recurrence up to 27 weeks of follow-up. |
| 11/ J Med, 201224 |
60 years/ Male/ Not known |
HIV-negative | Hoarseness of voice | Ulcerative growth in vocal cord | Abnormal chest X-ray (diffuse patchy opacity). | Histopathology from vocal cord specimen. Primary vocal cord histoplasmosis. |
Amphotericin B (0.5 mg/kg EAD for 14 doses). Itraconazole (200 mg 12-h for 12 weeks). Anti-TB (two times) Improved and advised for follow-up. |
| 12/ JAFMC, 201225 |
30 years/ Male/ Brick field worker |
HIV positive | Fever Cough Bleeding from multiple sites Respiratory distress Loose stool Dis-orientation |
Anemia Mucosal ulcers rash/plaques Abnormal chest auscultation |
Pancytopenia ALT = 103 IU/L Alkaline phosphatase = 527 IU/L LDH = 1003 U/L Abnormal chest imaging (consolidation). |
PBF and bone marrow study. Disseminated histoplasmosis. |
Anti-TB for nine months (presumptive). Expired in hospital due to aspiration pneumonia. |
| 13/ JBCPS, 201226 |
42 years/ Male/ Painter |
HIV-negative | Oral ulcer Dysphagia Poor general health Diarrhea |
Anemia Bilateral submandibular lymphadenopathy |
- | Histopathology from oral ulcer. Localized to the oral cavity. |
Itraconazole (200 mg 12-h for three weeks then maintenance dose). Cured, no recurance up to 2 months of follow-up. |
| 14/ JBCPS, 201226 |
65 years/ Male/ Farmer |
HIV-negative | Oral ulcer Poor general health |
Anemia Bilateral submandibular lymphadenopathy |
- | Histopathology from oral ulcer. Localized to oral cavity. |
Itraconazole (200 mg BID for 4 weeks then maintenance dose). Cured, no recurance up to 2 months of follow-up. |
| 15/ J Gen Pract, 201327 |
32 years/ Male/ Farmer |
HIV-negative | Fever Weight loss Anorexia |
Hepatosplenomegaly | ESR = 40 mm in first hour Bilateral adrenal masses |
FNAC from adrenal gland. Disseminated histoplasmosis. |
Anti-TB Not known |
| 16/ Bang J Med. 201328 |
45 years/ Male/ Not known |
T2DM HIV positive |
Fever Cough Weight loss Orogenital ulcers |
Anemia Rash Crepitation in lung Hepatomegaly |
Hb = 8.2 gm/dL WBC = 3600/cmm Platelets = 103 000/cmm ESR = 115 mm in first hour ALT = 146 IU/L AST = 537 IU/L Alkaline phosphatase= 407 IU/L LDH = 826U/L CD4 = 4/uL |
Bone marrow study. Disseminated histoplasmosis. |
Amphotericin B Expired |
| 17/ J Med, 201329 |
62 years/ Male/ Farmer |
HIV-negative | Fever Back pain Paraplegia Bowel-bladder in-continence |
Anemia Generalized lymphadenopathy Hepatosplenomegaly Spastic paraplegia |
- | Lymph node biopsy CT-guided FNAC from paraspinal soft tissue. Disseminated histoplasmosis. |
Amphotericin B Itraconazole Neurosurgical exploration. Improved (up to one month of follow-up). |
| 18/ Mymensingh Med J, 201430 |
60 years/ Male/ Farmer |
T2DM HIV-negative |
Fever Cough Weight loss Sore throat Voice change |
- | FBG = 12 mmol/L Patchy opacity in chest X-ray |
Histopathology from vocal cord punch biopsy specimen (ulcer). Vocal cord histoplasmosis. |
Amphotericin B (0.5 mg/kg/d for six weeks). Itraconazole (200 mg for 12 weeks). Anti-TB Improved up to three months of follow-up. |
| 19/ Unpublished, 2014* |
60 years/ Male/ Farmer |
Not known | Weight loss Anorexia Weakness |
Increased pigmentation | Hb = 10.9 gm/dl WBC = 10 800/cmm Platelets = 189 000/cmm ESR = 47 mm in first hour ALT = 41 IU/L ACTH stimulation test: partial adrenal insufficiency Bilateral adrenal enlargement |
CT-guided FNAC from adrenal gland. Gum biopsy Anti-histoplasma antibody. Disseminated histoplasmosis. |
Itraconazole Hydrocortisone Improved up to five months of follow-up. |
| 20/ Unpublished, 2014* |
42 years/ Male/ Farmer |
Not known | Weight loss Anorexia Weakness |
Increased pigmentation | Hb = 10.6 gm/dL WBC = 9700/cmm Platelets = 230 000/cmm ESR = 53 mm in first hour ALT = 65 IU/L ACTH stimulation test: partial adrenal insufficiency Bilateral adrenal enlargement |
CT-guided FNAC from the adrenal gland. Anti-histoplasma antibody. Disseminated histoplasmosis. |
Itraconazole Hydrocortisone Improved up to three months of follow-up. |
| 21/ Unpublished, 2014* |
59 years/ Male/ School teacher |
T2DM HIV-negative |
Fever Weight loss Anorexia |
Anemia Jaundice Hepatoplenomegaly |
Hb = 9.1 gm/dL WBC = 3900/cmm Platelets = 89 000/cmm ESR = 85 mm in first hour Bilateral adrenal enlargement |
FNAC from the adrenal gland. Disseminated histoplasmosis. |
Discharged against medical advice. Not known |
| 22/ BSM Bull, 2015 |
40 years/ Male/ Not known |
HIV-negative | Fever Weight loss Cough Anorexia Weakness |
Anemia Pigmentation Hepatomegaly |
Hb = 8.9 gm/dl Bilateral adrenal mass |
USG guided FNAC from adrenal gland. Disseminated histoplasmosis. |
Lipid formulation of amphotericin B (0.5 mg/kg/d for two weeks). Itraconazole (200 mg 12-h for 12 months). Anti-TB Not known |
| 23/ Unpublished, 2015* |
72 years/ Male/ Retired government employee |
T2DM HIV-negative |
Fever Weight loss Anorexia |
Anemia | Hb = 9.6 gm/dl WBC = 6700/cmm Platelets = 165 000/cmm ESR= 67 mm in first hour HbA1c = 8.3% Bilateral adrenal enlargement |
FNAC from the adrenal gland. Disseminated histoplasmosis. |
Amphotericin B Itraconazole Improving |
| 24/ Unpublished, 2015* |
62 years/ Male/ Retired government employee |
T2DM | Fever Anorexia Weight loss Cough Convulsion |
Anemia | Hb = 8.7 gm/dl WBC = 4100/cmm Platelets = 153 000/cmm ESR = 45 mm in first hour HbA1c = 7.9% Bilateral adrenal enlargement |
FNAC from the adrenal gland MRI of brain. Disseminated histoplasmosis. |
Amphotericin B Itraconazole. Recurrence with CNS histoplasmosis (later expired). |
| 25/ Unpublished, 2016* |
42 years/ Male/ Service holder |
HIV-negative | Fever Anorexia Weight loss |
Hepatosplenomegaly | Hb = 12 gm/dl WBC = 5600/cmm Platelets = 222 000/cmm ESR = 78 mm in first hour Bilateral adrenal enlargement |
FNAC from the adrenal gland. Disseminated histoplasmosis. |
Itraconazole Anti-TB Not known |
| 26/ BIRDEM Med J, 201831 |
42 years/ Male/ Not known |
T2DM HIV-negative |
Fever Anorexia Weight loss Pigmentation |
- | Hb = 12.4 gm/dL WBC = 8300/cmm Platelets = 426 000/cmm ESR = 40 mm in first hour ALT = 91 IU/L AST = 82 IU/L HbA1c = 6.6% Bilateral adrenal enlargement |
FNAC from the adrenal gland. ACTH stimulation test: no adrenal insufficiency. Disseminated histoplasmosis. |
Amphotericin B (14 days). Itraconazole (planned for 18 months). Improved up to last (six month) visit. |
Anti-TB: anti-tuberculosis; HIV: human immune deficiency virus; Hb: hemoglobin; WBC: white blood cells; T2DM: type 2 diabetes mellitus; LDH: lactate dehydrogenase; INH: isoniazid; ESR: erythrocyte sedimentation rate; AIDS: acquired immunodeficiency syndrome; CD: cluster of differentiation; ALT: alanine aminotransferase; AST: aspartate aminotransferase; FNAC: fine-needle aspiration cytology; EAD: every alternate day; PBF: peripheral blood film; FBG: fasting blood glucose; CT: computed tomography; ACTH: adrenocorticotropic hormone; USG: ultrasonography; HbA1c: glycated hemoglobin; MRI: magnetic resonance imaging; CNS: central nervous system; BID: twice a day.
*Note: Unpublished cases were recruited from three teaching hospitals, BIRDEM General Hospital (case 8, 21, 23 and 25), Bangabandhu Sheikh Mujib Medical University (cases 19 and 20) and Dhaka Medical College (Case 24), Dhaka, Bangladesh.
Missing data: physical signs (cases 18 and 26) and value/important laboratory and imaging findings (cases 1, 13, 14 and 17).
All 26 patients were male with a mean age of 50.9 years (range 8–75) [Table 1 and Table 2]. Nine patients were farmers, and five patients had a history of smoking. Five patients had a history of traveling outside Bangladesh [Table 2].
Table 2. Selected sociodemographic, clinical, and laboratory characteristics of Bangladeshi patients with histoplasmosis (N = 26).
| Characteristics | Frequency | Percentage | Mean | Range |
|---|---|---|---|---|
| Age, years | - | - | 50.9 | 8–75 |
| Sex, male | 26 | 100 | - | - |
| Occupation, farmer | 9 | 34.6 | - | - |
| Habit, smoker | 5 | 19.2 | - | - |
| History of traveling outside Bangladesh | ||||
| No | 21 | 80.8 | - | - |
| Yes | 5 | 19.2 | - | - |
| Underlying condition | ||||
| Diabetes mellitus | 7 | 26.9 | - | - |
| Kidney transplant recipient | 1 | 3.8 | - | - |
| HIV/AIDS status | ||||
| Positive | 4 | 15.4 | - | - |
| Negative | 15 | 57.7 | - | - |
| Not known | 7 | 26.9 | - | - |
| Clinical presentation | ||||
| Fever | 20 | 76.9 | - | - |
| Weight loss | 17 | 65.4 | - | - |
| Anorexia | 14 | 53.8 | - | - |
| Cough | 7 | 26.9 | - | - |
| Oral ulcer | 8 | 30.8 | - | - |
| Hyperpigmentation | 3 | 11.5 | - | - |
| Anemia | 15 | 57.7 | - | - |
| Cervical lymphadenopathy | 5 | 19.2 | - | - |
| Generalized lymphadenopathy | 4 | 15.4 | - | - |
| Skin rash/nodule | 4 | 15.4 | - | - |
| Hepatomegaly | 3 | 11.5 | - | - |
| Hepatosplenomegaly | 7 | 26.9 | - | - |
| Splenomegaly | 1 | 3.8 | - | - |
| Major organ involvement | ||||
| Lung | 6 | 23.1 | - | - |
| Liver/spleen | 9 | 34.6 | - | - |
| Adrenal glands | 11 | 42.3 | - | - |
| Skin | 7 | 26.9 | - | - |
| Gastrointestinal tract | 8 | 30.8 | - | - |
| Bone marrow | 4 | 15.4 | - | - |
| Lymph nodes | 9 | 34.6 | - | - |
| Form of histoplasmosis | ||||
| Disseminated histoplasmosis | 22 | 84.6 | - | - |
| Localized oropharyngeal disease | 4 | 15.4 | - | - |
| Treatment | ||||
| Amphotericin B (initial) | 14 | 53.8 | - | - |
| Itraconazole (continuation/only) | 17 | 65.5 | - | - |
| Anti-TB treatment, empiric | 9 | 34.6 | - | - |
| Follow-up and outcome | ||||
| Cured/improving up to the last follow-up | 14 (recurred in 2) | 53.8 | - | - |
| Death | 6 | 23.1 | - | - |
| Recurred | 2 (1 later expired) | 7.7 | - | - |
| Not known | 6 | 23.1 | - | - |
HIV: human immunodeficiency virus; AIDS: acquired immunodeficiency syndrome; TB: tuberculosis.
Among the patients, one was a known case of AIDS, and disseminated histoplasmosis was the presenting feature of AIDS in another three cases [Table 2]. The CD4 counts in one patient with AIDS was 19/µL and 4/µL in another patient [Table 1]. Seven patients had diabetes, one was a renal transplant recipient, and another had AIDS. HIV was negative in 15 cases and the HIV status was not known in the rest of the cases [Table 2]. No other history suggestive of immunosuppression was found among the patients.
Fever (n = 20) and weight loss (n = 17) were the two most common clinical presentations. Other features were oral ulcer, anorexia, skin rash and nodules, cough, abdominal pain, diarrhea, and bleeding [Table 1]. Common physical findings included anemia, lymphadenopathy, hepatosplenomegaly, oral candidiasis, and abnormal lung findings [Table 2].
Fifteen patients had anemia, including pancytopenia in two patients. Three (reports available for six patients) patients had abnormal liver biochemistry, and two (reports available for three patients) patients had raised lactate dehydrogenase (LDH). Abnormal chest radiograph and bilateral adrenal enlargement were present in six and 11 cases, respectively [Table 2]. Esophageal moniliasis was found in three patients. Diagnosis was confirmed by histopathological examination of tissue from oropharyngeal ulcers (n = 8) and bone marrow (n = 4), and fine-needle aspiration cytology from adrenal glands (n = 11), lymph nodes (n = 3), and skin (n = 1) [Table 1]. Culture from lymph nodes and adrenal glands aspirates and skin nodule revealed growth of Histoplasma in one case each. Disseminated histoplasmosis was diagnosed in 22 cases and localized oropharyngeal disease in four cases. In six cases, diagnosis was confirmed from more than one site.
Treatment consisted of amphotericin B and itraconazole with wide variations in doses and durations [Table 1 and Table 2]. Nine patients were prescribed anti-tuberculosis (anti-TB) drugs during disease course empirically or without definitive proof, and three patients had a history of tuberculosis/anti-TB prophylaxis [Table 1]. Six patients with disseminated histoplasmosis died in hospital, 14 patients recovered with relapse in two cases (one patient later died in hospital), and the outcome of the other six cases could not be ascertained [Table 1].
Discussion
The first histoplasmosis survey was done in Bangladesh in 1961 (then East Pakistan), which revealed that 12–23% of people had a positive skin reaction to histoplasmin.14 A second survey among patients attending different clinics revealed almost similar results in 1968–1969.15 We also found similar results reported among people living along the banks of the river Jamuna near Delhi, India, in a survey in 1960.36 In endemic areas, more than half of the population exhibit positive skin reaction to histoplasmin.1 The first histoplasmosis case in Bangladesh was reported in 198216 and the second case in 2005.35 Cases are increasingly reported nowadays.17-31 All were males, reflecting that males are possibly more at risk of exposure to soil due to occupational or recreational activities. A male predominance of histoplasmosis cases was also reported from India6,7 and Brazil.37
Common presenting features were fever, weight loss, oropharyngeal ulcer, lymphadenopathy, and hepatosplenomegaly. Bilateral adrenal enlargement was also common. Similar findings were reported among patients from Panama,9 Brazil,37 Australia,10 Europe,11 Africa,8 South-East Asia,5 and India6,7 irrespective of patients’ immune status. Disseminated forms were more common than the localized disease in the current study, even in immunocompetent patients. In immunocompetent patients, adrenal enlargements were more common as was seen in an Australian series,10 but less than two Indian series.6,7 Increased steroid concentration within the adrenal glands promotes the growth of H. capsulatum.38
Cytopenias, elevated hepatic enzymes, and LDH are established features of disseminated histoplasmosis in HIV infected patients.9,28 Among the three patients in whom LDH reports were available, two had raised LDH, and both had HIV/AIDS. Among the 26 cases reported here, only in the first case authors reported the possibility of histoplasmosis during diagnostic work-up. Among the seven unpublished cases (cases 8, 19–21, 23–25) reported here, in six (except case 8) adrenal histoplasmosis was a deferential diagnosis during diagnostic work-up (primary data; by personal communication); but few other cases reported here were diagnosed incidentally (cases 6, 7, 9, 11, 16, 17 and 26 by personal communication with the corresponding authors) when tissue samples were sent for histopathological examination or culture. A similar observation was reported in a South-East Asian series.5
Treatment of reported histoplasmosis cases consisted mostly of amphotericin B followed by oral itraconazole. In localized oral cases, itraconazole can be curative. Regarding the outcome of histoplasmosis cases, six patients with disseminated disease died, and 14 patients improved with relapse in two cases. Treatment monitoring is important. Urine antigen can be used for treatment monitoring and possible disease recurrence.39,40 In Bangladesh, currently there is no facility for such a test.
As histoplasmosis is an uncommon diagnosis in Bangladesh, diagnostic work-up and management strategies varied widely among the cases reported. We do not have any definite working diagnostic algorithms for many diseases, including histoplasmosis, and diagnostic work-ups are performed on a case-by-case basis and also depend upon the availability of diagnostic facilities. The 2007 Update by the Infectious Diseases Society of America recommends initial amphotericin B treatment followed by itraconazole in moderately severe to severe progressive disseminated histoplasmosis cases and in less severe cases oral itraconazole.41 Patients with HIV may require life-long therapy depending upon CD4 counts and the status of anti-retroviral therapy.41 Physicians should adhere to standard protocols41 for managing histoplasmosis cases and as the cases are increasing in Bangladesh, especially in the last two decades [Table 1], it should be evaluated for possible "emerging disease" and also whether it should be considered a "notifiable" one.
Our literature search was confined to "PubMed," "BanglaJOL," and "Google" and we did not search through other databases. Treatment detail and outcome data were not available for all the cases reported.
Conclusion
Despite high skin sensitivity test results, only a small number of cases (mostly from 2010 and onwards) were reported over a three-decade period in Bangladesh. It may indicate that a good number of cases remain asymptomatic or minimally symptomatic. There may be cross-reactivity to some other fungus with histoplasmin. Under-reporting of cases and improper diagnosis, especially tuberculosis, is not impossible. Clinicians should be aware of the condition and histoplasmosis should be suspected in an appropriate clinical setting. A further survey may be done in farm areas and among persons working on poultry farms.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
References
- 1.Wheat LJ. Histoplasmosis: a review for clinicians from non-endemic areas. Mycoses 2006. Jul;49(4):274-282. 10.1111/j.1439-0507.2006.01253.x [DOI] [PubMed] [Google Scholar]
- 2.Kauffman CA. Histoplasmosis: a clinical and laboratory update. Clin Microbiol Rev 2007. Jan;20(1):115-132. 10.1128/CMR.00027-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wheat LJ, Kauffman CA. Histoplasmosis. Infect Dis Clin North Am 2003. Mar;17(1):1-19, vii. 10.1016/S0891-5520(02)00039-9 [DOI] [PubMed] [Google Scholar]
- 4.Oladele RO, Ayanlowo OO, Richardson MD, Denning DW. Histoplasmosis in Africa: An emerging or a neglected disease? PLoS Negl Trop Dis 2018. Jan;12(1):e0006046. 10.1371/journal.pntd.0006046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang TL, Cheah JS, Holmberg K. Case report and review of disseminated histoplasmosis in South-East Asia: clinical and epidemiological implications. Trop Med Int Health 1996. Feb;1(1):35-42. 10.1046/j.1365-3156.1996.d01-10.x [DOI] [PubMed] [Google Scholar]
- 6.Gopalakrishnan R, Nambi PS, Ramasubramanian V, Abdul Ghafur K, Parameswaran A. Histoplasmosis in India: truly uncommon or uncommonly recognised? J Assoc Physicians India 2012. Oct;60:25-28. [PubMed] [Google Scholar]
- 7.Subramanian S, Abraham OC, Rupali P, Zachariah A, Mathews MS, Mathai D. Disseminated histoplasmosis. J Assoc Physicians India 2005. Mar;53:185-189. [PubMed] [Google Scholar]
- 8.Loulergue P, Bastides F, Baudouin V, Chandenier J, Mariani-Kurkdjian P, Dupont B, et al. Literature review and case histories of Histoplasma capsulatum var. duboisii infections in HIV-infected patients. Emerg Infect Dis 2007. Nov;13(11):1647-1652. 10.3201/eid1311.070665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gutierrez ME, Canton A, Sosa N, Puga E, Talavera L. Disseminated histoplasmosis in patients with AIDS in Panama: a review of 104 cases. Clin Infect Dis 2005. Apr;40(8):1199-1202. 10.1086/428842 [DOI] [PubMed] [Google Scholar]
- 10.McLeod DS, Mortimer RH, Perry-Keene DA, Allworth A, Woods ML, Perry-Keene J, et al. Histoplasmosis in Australia: report of 16 cases and literature review. Medicine (Baltimore) 2011. Jan;90(1):61-68. 10.1097/MD.0b013e318206e499 [DOI] [PubMed] [Google Scholar]
- 11.Antinori S, Magni C, Nebuloni M, Parravicini C, Corbellino M, Sollima S, et al. Histoplasmosis among human immunodeficiency virus-infected people in Europe: report of 4 cases and review of the literature. Medicine (Baltimore) 2006. Jan;85(1):22-36. 10.1097/01.md.0000199934.38120.d4 [DOI] [PubMed] [Google Scholar]
- 12.Gajurel K, Dhakal R, Deresinski S. Histoplasmosis in transplant recipients. Clin Transplant 2017. Oct;31(10). 10.1111/ctr.13087 [DOI] [PubMed] [Google Scholar]
- 13.Blanchard E, Truchetet ME, Machelart I, Séneschal J, Raherison-Semjen C. Respiratory infections associated with anti-TNFα agents. Med Mal Infect 2017. Oct;47(6):375-381. 10.1016/j.medmal.2017.05.002 [DOI] [PubMed] [Google Scholar]
- 14.Islam N, Islam M, Muazzam MG. A histoplasmosis survey in East Pakistan. Trans R Soc Trop Med Hyg 1962;56(3):246-249 . 10.1016/0035-9203(62)90162-1 [DOI] [Google Scholar]
- 15.Islam N, Sobhan MA. Sensitivity to histoplasmin, coccidioidin, blastomycin, and tuberculin in East Pakistan. Am J Trop Med Hyg 1971. Jul;20(4):621-624. 10.4269/ajtmh.1971.20.621 [DOI] [PubMed] [Google Scholar]
- 16.Islam N, Chowdhury NA. Histoplasmosis from Bangladesh : a case report. Bangladesh Med Res Counc Bull 1982. Jun;8(1):21-24. [PubMed] [Google Scholar]
- 17.Rappo U, Beitler JR, Faulhaber JR, Firoz B, Henning JS, Thomas KM, et al. Expanding the horizons of histoplasmosis: disseminated histoplasmosis in a renal transplant patient after a trip to Bangladesh. Transpl Infect Dis 2010. Apr;12(2):155-160. 10.1111/j.1399-3062.2009.00466.x [DOI] [PubMed] [Google Scholar]
- 18.Ahmed S, Shazzad MN, Rahman MF, Kader MA, Azad MA, Haq SA. Disseminated histoplasmosis without pulmonary involvement in an immunocompetent host – a case report. BSMMU J 2010;3(1):44-46 . 10.3329/bsmmuj.v3i1.5515 [DOI] [Google Scholar]
- 19.Pervez MM, Cobb B, Matin N, Shahrin L, Ford ER, Pietroni M. Disseminated histoplasmosis in a patient with advanced HIV disease–lessons learnt from Bangladesh. J Health Popul Nutr 2010. Jun;28(3):305-307. 10.3329/jhpn.v28i3.5561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahbub MS, Ahsan MN, Miah MT, Alam MB, Gupta RD, Arif KM, et al. Disseminated histoplasmosis. J Med 2010;11:70-73 . 10.3329/jom.v11i1.4278 [DOI] [Google Scholar]
- 21.Parvin R, Amin R, Mahbub MS, Hasnain M, Arif KM, Miah MT, et al. Deep fungal infection- an emerging problem in Bangladesh. J Med 2010;11:170-175 . 10.3329/jom.v11i2.5466 [DOI] [Google Scholar]
- 22.Amin MR, Shumi F, Khan H, Abdullah SA, Alam S, Hussain AR, et al. Disseminated histoplasmosis in an elderly man presented with fever, weight loss, abdominal pain and haemoptysis – a case report with literature review. J Med 2011;12(1):81-85 . 10.3329/jom.v12i1.6745 [DOI] [Google Scholar]
- 23.Alam AS, Hasan Z, Khan MA, Zulkifl MA, Samdani AT, Islam MT, et al. Chronic disseminated histoplasmosis in an immunocompetent man presented as bilateral adrenal masses with partial adrenocortical insufficiency- a rare condition. J Bangladesh Coll Phys Surg 2011;29(4):235-240 . 10.3329/jbcps.v29i4.11345 [DOI] [Google Scholar]
- 24.Habib SK, Patwary SA, Khan MA, Miah MT, Gupta RD, Ahasan HA. Primary histoplasmosis of vocal cord in an immunocompetent elderly man- a case report with literature review. J Med 2012;13(1):77-81 . 10.3329/jom.v13i1.10080 [DOI] [Google Scholar]
- 25.Bhuiyan MN, Giti S, Islam MS, Uddin MN. Disseminated histoplasmosis in a patient with AIDS- a case report and review of literature. JAFMC 2012;8(2):81-86. [Google Scholar]
- 26.Sadat SM, Rita SN, Kahhar MA. Oral histoplasmosis: report of two cases. J Bangladesh Coll Phys Surg 2012;30(4):229-233 . 10.3329/jbcps.v30i4.14768 [DOI] [Google Scholar]
- 27.Parvin R, Uddin AK. Bilateral adrenal histoplasmosis in an immunocompetent man. J Gen Pract (Los Angel) 2013;1:103 . 10.4172/2329-9126.1000103 [DOI] [Google Scholar]
- 28.Yasmin R, Rahim MA, Haque HF, Dewan P, Ahmed JU, Ahmed AS, et al. Disseminated histoplasmosis as presenting feature of acquired immunodeficiency syndrome: a case report. Bangladesh J Medicine 2013;24(2):78-81 . 10.3329/bjmed.v24i2.20221 [DOI] [Google Scholar]
- 29.Singha CK, Biswas E, Jahan F, Biswas PK. Histoplasmosis – an unusual cause of spastic paraplegia in an immunocompetent host in Bangladesh. J Med 2013;14(2):201-203 . 10.3329/jom.v14i2.19688 [DOI] [Google Scholar]
- 30.Masud MK, Ahmad SM, Ferdouse F, Bhuiyan MR, Paul SK, Litu MA, et al. Laryngeal histoplasmosis. Mymensingh Med J 2014. Jul;23(3):566-571. [PubMed] [Google Scholar]
- 31.Afsana F, Hossain KN, Tareque A, Amin MF, Pathan MF. A Case of adrenal histoplasmosis. BIRDEM Med J 2018;8(1):77-80 . 10.3329/birdem.v8i1.35046 [DOI] [Google Scholar]
- 32.Shahrin L, Leung DT, Matin N, Pervez MM, Azim T, Bardhan PK, et al. Characteristics and predictors of death among hospitalized HIV-infected patients in a low HIV prevalence country: Bangladesh. PLoS One 2014. Dec;9(12):e113095. 10.1371/journal.pone.0113095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gugnani HC, Denning DW, Rahim R, Sadat A, Belal M, Mahbub MS. Burden of serious fungal infections in Bangladesh. Eur J Clin Microbiol Infect Dis 2017. Jun;36(6):993-997. 10.1007/s10096-017-2921-z [DOI] [PubMed] [Google Scholar]
- 34.Sadat SM, Robin MA, Rita SN, Akhter F, Uddin AF. Oral histoplasmosis with previously treated pulmonary tuberculosis: a case report. Med Today (Karachi) 2013;25(2):99-102 . 10.3329/medtoday.v25i2.17931 [DOI] [Google Scholar]
- 35.Rahman MM, Hossain SM, Dewanjee AK, Sultan MT, Faiz MA, Rahman J. Disseminated histoplasmosis in acquired immunodeficiency syndrome – a case report. J Bangladesh Coll Phys Surg 2005;23:43-45. [Google Scholar]
- 36.Viswanathan R, Chakravarty SC, Randhawa HS, Demonte AJ. Pilot histoplasmosis survey in Delhi area. Br Med J 1960. Feb;1(5170):399-400. 10.1136/bmj.1.5170.399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Faiolla RC, Coelho MC, Santana RdeC, Martinez R. Histoplasmosis in immunocompetent individuals living in an endemic area in the Brazilian Southeast. Rev Soc Bras Med Trop 2013. Jul-Aug;46(4):461-465. 10.1590/0037-8682-0124-2013 [DOI] [PubMed] [Google Scholar]
- 38.Angeli A, Masera RG, Gatti G. [Mycoses and adrenocortical function. New pathogenetic aspects of adrenal hypofunction]. Recenti Prog Med 1991. Dec;82(12):652-660. [PubMed] [Google Scholar]
- 39.Wheat LJ. Histoplasmosis in Indianapolis. Clin Infect Dis 1992. Mar;14(Suppl 1):S91-S99. 10.1093/clinids/14.Supplement_1.S91 [DOI] [PubMed] [Google Scholar]
- 40.Wheat LJ, Connolly-Stringfield P, Blair R, Connolly K, Garringer T, Katz BP, et al. Effect of successful treatment with amphotericin B on Histoplasma capsulatum variety capsulatum polysaccharide antigen levels in patients with AIDS and histoplasmosis. Am J Med 1992. Feb;92(2):153-160. 10.1016/0002-9343(92)90106-L [DOI] [PubMed] [Google Scholar]
- 41.Wheat LJ, Freifeld AG, Kleiman MB, Baddley JW, McKinsey DS, Loyd JE, et al. Infectious Diseases Society of America Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis 2007. Oct;45(7):807-825. 10.1086/521259 [DOI] [PubMed] [Google Scholar]


