Abstract
Objective:
Drug overdoses among men have historically outnumbered those among women by a large margin. Yet, U.S. research on the first wave of the opioid epidemic involving prescription opioids has found women to be at increased risk. The current study considers if the narrowing gender gap in overdose deaths, as observed during the first wave, has continued into the most recent third wave, dominated by synthetic opioid deaths. This requires consideration of interactions between gender, age, and type of drug implicated.
Method:
Drawing on 2013–2017 Delaware toxicology reports for a total of 890 overdose deaths involving opioids, we distinguished between four gender/age groups—women 15–44, women 45–64, men 15–44, and men 45–64—to calculate crude death rates, male-to-female death rate ratios, and younger-to-older death rate ratios by type of opioid.
Results:
Opioid overdose death rates during the third wave increased among both men (+102%) and women (+46%), but the larger increase among men resulted in an increase in the male-to-female death rate ratio (from 1.9 to 2.6). This trend was driven by the growing contribution of fentanyl (from 16% to 76%) and heroin overdose deaths (from 27% to 50%) compared with other opioid overdose deaths, which disproportionately affected men and younger individuals. Higher male-to-female death rate ratios were observed among older, compared with younger, individuals.
Conclusions:
Overdose deaths seem to have returned to a historically familiar pattern of dominance by younger males. Our findings suggest the gender–age distribution in deaths to specific opioid types must be considered for effective intervention.
As the opioid problem has grown in the past two decades in the United States, there are signs of a demographic shift in its fatal impact. U.S. research has historically noted the basic demographics of overdose victims are well known (Galea & Coffin, 2003), with victims typically being male (e.g., 70%+ male) and between the ages of 15 and the early 30s (Darke & Hall, 2003). The profile of opioid casualties has long fit this pattern, as most deaths have historically been among young males and attributable to heroin (Samkoff & Baker, 1982). However, women may now be at heightened risk, as the origins of the current opioid epidemic have been in prescription drugs. In fact, the rate of prescription opioid overdose death increased more rapidly for women than for men between 1999 and 2010—415% for women compared with 265% for men (Mack et al., 2013)—leading to a narrowing of the gender gap in overdose death (Lipato & Terplan, 2018) during a period the Centers for Disease Control and Prevention (CDC) (2018a) labeled the “first wave” of the opioid epidemic.
The underestimation of harms from prescription opioids may explain why women’s risk of overdose death increased more rapidly than men’s during the first wave of the crisis, which was dominated by prescription opioid deaths. Women have historically been, and continue to be, more likely to be prescribed opioids, and at higher doses, in comparison with their male counterparts (Campbell et al., 2010; Terplan, 2017). In addition, if prescription opioids are a “gateway” to other more dangerous or illegal opioids (e.g., heroin, illicitly manufactured fentanyl) as claimed (Cicero et al., 2014; National Institute on Drug Abuse, 2018), then we could expect an uptick in women’s escalation to illegal opioids and subsequent overdosing from them as well. Sharp increases in deaths involving heroin and synthetic opioids among women have indeed been reported over time (i.e., from 1999 to 2017; Van Houten et al., 2019). However, it is unclear if the reduced gender gap in overdose deaths has continued through the recent second (i.e., heroin, starting in 2010) and third (i.e., fentanyl, starting in 2013) waves of the epidemic.1
More generally, recent knowledge of the unique risk profiles of women versus men, across age group and by type of drug, is limited. Building on previous research (e.g., Calcaterra et al., 2013; Jalal et al., 2018; Rudd et al., 2016; Seth et al., 2018; Van Houten et al., 2019), this study addresses two questions: Are overdose deaths still increasing more rapidly among women than among men as the opioid epidemic wages on? To what extent are younger (i.e., childbearing age) and older women at similar risk as their male counterparts for overdose deaths, and does their risk vary by type of drug (e.g., prescription opioids, heroin, and fentanyl)?
We investigated our questions with overdose death data in Delaware. As the second smallest state in the country, Delaware currently ranks among the top 10 states with the highest overdose death rates. It was one of 23 states to witness a significant increase in those deaths between 2016 and 2017 (CDC, 2018b), and the state also ranks high in terms of prescribing long-acting or extended-release opioids, mean daily opioid dosage, and percentage of opioid prescriptions written for more than 100 morphine milligram equivalents (MMEs) per day (Paulozzi et al., 2014, 2015). For example, two of three Delaware counties ranked in the top 25% of U.S. counties in MMEs prescribed per capita in 2015 (Guy et al., 2017).
Given this level of risk, we investigated recent trends in opioid overdose death rates for younger and older women in comparison with their same-age male counterparts (i.e., women 15–44, women 45–64, men 15–44, and men 45–64). We investigated gender and age variations in overdose deaths by type of opioid (prescription opioids, fentanyl, and heroin) for a 5-year period (2013–2017). Our goal was to advance understanding of how recent increases in overdose deaths involving heroin and synthetic opioids have altered gender gaps in opioid overdose death rates, and to investigate the need to tailor prevention and harm reduction efforts to the unique needs of different demographic (i.e., Gender × Age) groups.
Method
Data
Data for this study were drawn from 2013–2017 toxicology reports for drug overdose deaths in the state of Delaware. Toxicology reports identify the presence of drugs in deaths that medical examiners conclude are due to drugs. Scientists use enzyme-linked immunosorbent assay (ELISA) for preliminary drug screens, which qualitatively distinguishes 12 drug classes: benzodiazepines, cocaine, opiates, phencyclidine (PCP), carisoprodol, methadone, amphetamine, methamphetamine, barbiturates, cannabinoids, oxycodone, and fentanyl. Cases are then coded based on the results of confirmatory tests. For example, if 6-monoacetylmorphine was confirmed as present at the time of death, then decedents are classified as heroin-involved deaths. If deaths involved multiple drugs, then the associated toxicology reports list all confirmed drug types. All overdose deaths involving opioids—accidental, unintentional, and intentional—were included (N = 1,001). Individuals age 14 years and younger and those age 65 years and older were excluded because of an insufficient number of opioid overdose deaths for stable estimates (N = 982). Because we calculated death rates based on population estimates of the resident Delaware population, cases that involved decedents with home addresses outside of the state or that were determined to be homeless were excluded from the analysis (N = 890). This study and the use of these data received Institutional Review Board approval.
Postmortem toxicology reports included information about decedent’s age, gender, and race, as well as information about drug types involved. For the purposes of our analyses, we distinguished between four gender/age groups—women 15–44, women 45–64, men 15–44, and men 45–64—and we identified three categories of opioid overdose deaths. The first category, “a prescription opioid other than fentanyl,” contained all cases involving a prescription opioid other than fentanyl, as the current methods for detection are not capable of distinguishing between prescription and illicitly manufactured fentanyl. The category “fentanyl” included those cases that were confirmed to have any fentanyl present. Last, cases in the “heroin” classification included those that were confirmed to have 6-monoacetylmorphine present. For the sake of analysis, our classifications are not mutually exclusive. For example, a case included in the heroin classification may also be included in the fentanyl classification.
Analytic strategy
Crude death rates were calculated for each year separately, and for the 5 years combined, and were expressed as the number of overdose deaths per 100,000 residents in Delaware. Population estimates by gender and age were based on the 2013–2017 National Center for Health Statistics bridged-race estimates of the July 1st resident population (CDC, 2018c). Sensitivity analyses using the more detailed 5-year age distribution as estimated for the July 1, 2013, resident Delaware population ascertained that changes in the age structure over the period 2013–2017 did not affect substantive conclusions (results available on request).
All analyses were performed with Stata software, Version 15 (StataCorp LP, College Station, TX). Because the postmortem toxicology reports concerned all overdose deaths in Delaware during that period, this is the complete research population. Considering the descriptive nature of our analysis of these population data, calculating confidence intervals or performing significance tests would be unnecessary (see, e.g., Berk et al., 1995; Cowger, 1984; Rubin, 1985).
Results
In 2013, Delaware recorded 127 overdose deaths involving opioids among residents ages 15–64. This number increased to 235 in 2017 (results not shown), for an increase of 85%. This latter trend was driven entirely by the increase in fentanyl-involved overdose deaths (i.e., from 15.7% of opioid overdose deaths in 2013 to 76.2% in 2017) and those from heroin (from 26.8% of opioid overdose deaths in 2013 to 49.8% in 2017). Conversely, the percentage of opioid overdose deaths involving prescription opioids other than fentanyl decreased from 78% in 2013 to 40% in 2017.
Gender- and age-specific trends in opioid overdose death
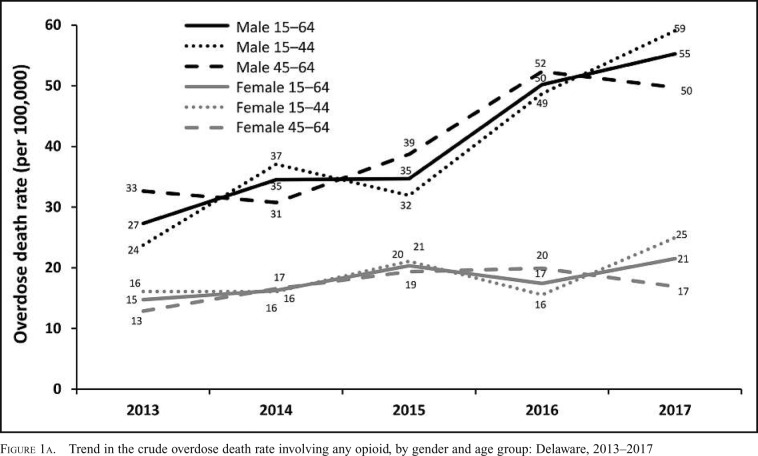
Crude overdose death rates reveal important gender differences in overdose deaths involving opioids during the study period (Figure 1A). In 2013, the opioid overdose death rate was 15/100,000 persons among women ages 15–64, and 27/100,000 persons among men ages 15–64. By 2017, these death rates had increased by 46% and 102%, respectively, resulting in an increase in the male-to-female overdose death rate ratio from 1.9 in 2013 (27.3 vs. 14.8/100,000) to 2.6 in 2017 (55.3 vs. 21.5/100,000). This indicates that the gender gap in opioid overdose deaths widened, rather than narrowed, during the third wave of the epidemic, which began in 2013.
Figure 1a.
Trend in the crude overdose death rate involving any opioid, by gender and age group: Delaware, 2013–2017
Although important, these overall trends conceal notable differences between younger and older women, and younger and older men. Among women, those ages 15–44 showed the highest overall opioid overdose death rate in 2013 (16.1/100,000 persons) and the largest increase in this death rate by 2017 (+54.8%). Women ages 45–64 had a somewhat lower rate in 2013 (12.9/100,000 persons) and a smaller increase by 2017 (+31.2%). A different trend occurred among men, as those ages 15–44 started off with a lower overall opioid overdose death rate in 2013 (23.7/100,000 persons) compared with men ages 45–64 (32.6/100,000 persons) but experienced a much steeper increase by 2017 (+149.0% vs. +52.3% for men ages 45–64). Accordingly, the overall opioid overdose death rate in 2017 was higher among those ages 15–44 compared with those ages 45–64, among both women (25.0 vs. 16.9/100,000 for women ages 45–64) and men (59.1 vs. 49.7/100,000 for men ages 45–64).
Gender- and age-specific trends by opioid type
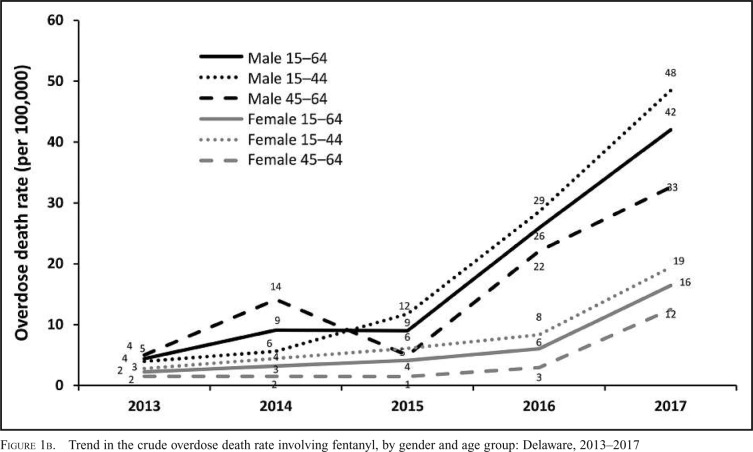
Large increases in the overall opioid overdose death rate, especially among men compared with women, but also among younger compared with older individuals, coincided with a growing contribution of fentanyl and, to a lesser extent, heroin to the overdose death rate during the third wave. Starting at a rate at or below 5/100,000 persons in 2013, the overdose death rate involving fentanyl multiplied among men ages 15–44, increased substantially among men ages 45–64, and showed more modest but nevertheless substantial increases among women ages 15–44 and 45–64 (Figure 1B).
Figure 1b.
Trend in the crude overdose death rate involving fentanyl, by gender and age group: Delaware, 2013–2017
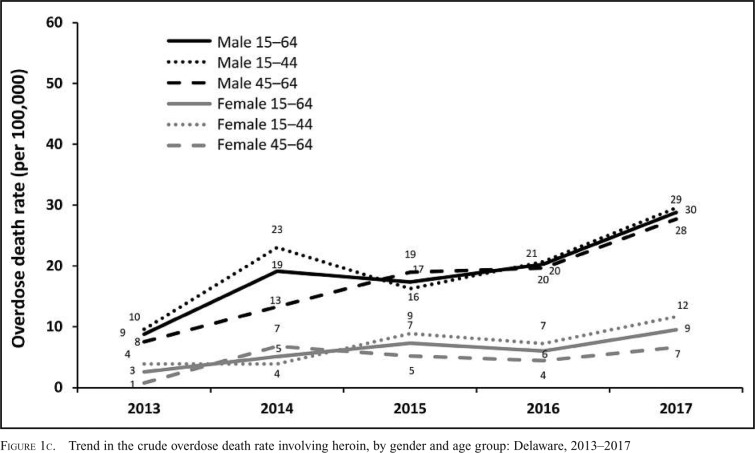
The overdose death rate involving heroin showed more variation in 2013, with the highest rate observed among men ages 15–44 and the lowest rate observed among women ages 45–64 (Figure 1C). Increases in the overdose death rate involving heroin were also smaller, yet again showed evidence of a widening gender gap over the 5-year period; much larger increases were observed among men ages 15–44 and 45–64 compared with women ages 15–44 and, even more so, women ages 45–64.
Figure 1c.
Trend in the crude overdose death rate involving heroin, by gender and age group: Delaware, 2013–2017
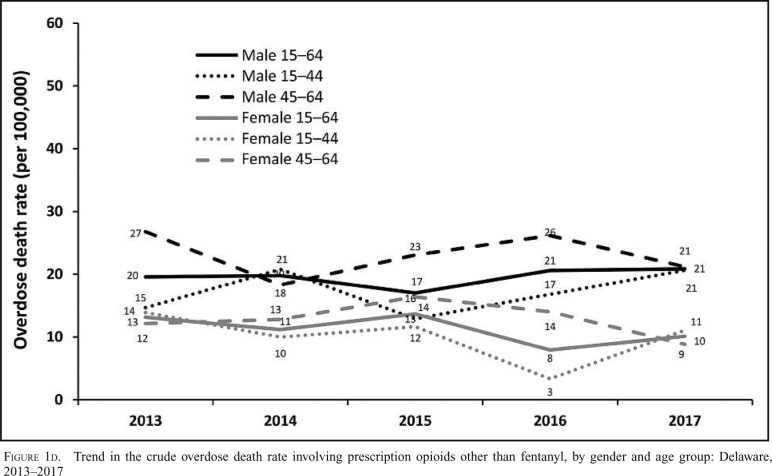
Last, overdose death rates involving prescription opioids in 2013 were much higher than those involving fentanyl and heroin (Figure 1D). However, they remained relatively stable during the period—even decreasing slightly—among women ages 15–44 and 45–64 and among men ages 45–64, although a modest increase was observed among men ages 15–44. This means that changes in overdose deaths involving prescription opioids other than fentanyl, in contrast to changes in fentanyl and heroin overdose deaths, contributed little to nothing to the widening of the gender gap in the overall opioid overdose death rate between 2013 and 2017, or during the epidemic’s third wave.
Figure 1d.
Trend in the crude overdose death rate involving prescription opioids other than fentanyl, by gender and age group: Delaware, 2013–2017
The opposing roles of prescription opioids, fentanyl, and heroin
Data for all 5 years combined (not shown here) reinforce the opposing roles of fentanyl and heroin on the one hand, and prescription opioids other than fentanyl on the other hand, in shaping gender ratios in overall opioid overdose death rates. In fact, male-to-female ratios consistently point to larger gender gaps in the fentanyl (ratios of 2.4 and 4.0, among those ages 15–44 and 45–64, respectively) and heroin (ratios of 2.8 and 3.6, among those ages 15–44 and 45–64, respectively) overdose death rate compared with the death rate involving prescription opioids other than fentanyl (ratios of 1.7 and 1.8, among those ages 15–44 and 45–64, respectively). In addition, these ratios reveal that the gender gap in overall opioid overdose death rates tends to be larger among those ages 45–64 compared with those ages 15–44—a pattern that appears to be driven by differences in fentanyl and heroin overdose death rates, as similar male-to-female ratios in prescription opioid overdose death rates were observed among those ages 15–44 and 45–64.
Discussion
The current opioid crisis plaguing the United States has now passed through three waves (first wave, prescription opioids; second wave, heroin; and third wave, synthetic opioids such as fentanyl), rendering it unique, ever more urgent, and difficult to combat. Complicating this is the changing demography of those hit hardest.
This study, focusing on third-wave deaths in Delaware, found evidence of a widening gender gap in overall opioid overdose death rates during the period 2013–2017, even as women’s overdose death rates also continued to increase. This widening gender gap in overdose deaths during the third wave appears driven by the use of illegal and synthetic drugs (i.e., fentanyl and heroin) compared with prescription opioids. Whereas all groups—women as well as men, those ages 45–64 as well as those ages 15–44—had high levels of overdose death involving prescription opioids other than fentanyl during the period 2013–2017, deaths involving fentanyl or heroin increased more dramatically (especially since 2016) among young men compared with women of any age or older men. Thus, age and drug type can help illuminate the role of gender in drug overdose.
Our findings extend previous research (Calcaterra et al., 2013; Jalal et al., 2018; Van Houten et al., 2019) reporting that gender and age intersect to shape overdose death risk profiles. Our detailed analysis of gender, age, and type of drug overdose death by year in the third wave provides nuance to the demography of current overdose death risk. To wit, we find as the types of drugs driving the epidemic have changed, so too has the demographic distribution of overdose deaths.
Findings of this study should be considered in light of certain limitations. First, our data pertain to overdose deaths and do not include data on drug use. Death rates and rate ratios as reported here likely differ from those calculated based on the population of opioid users only due to known differences in opioid use. For example, even though women have a lower prescription opioid overdose death rate (Figure 1D), they are more often prescribed opioids (Terplan, 2017) and have more frequent hospitalizations for prescription opioid overdoses (Unick et al., 2013). Second, when interpreting results, it should be kept in mind that our categories of opioid overdose deaths are not mutually exclusive. Third, we examined fentanyl separate from the category prescription opioids. Even though previous research (O’Donnell et al., 2017) has indicated that most deaths involving fentanyl involve illicitly manufactured fentanyl, some deaths could have involved pharmaceutical fentanyl, and thus findings regarding fentanyl overdose deaths should be treated with caution. The data also do not permit us to distinguish between overdoses due to medical versus nonmedical use of pharmaceutical opioids. Last, because heroin and morphine are metabolized similarly, some heroin deaths might have been misclassified as deaths involving prescription opioids other than fentanyl, leading to misclassification bias.
Footnotes
Research reported in this publication was supported by an ACCEL Jumpstart Grant (Grant no. NIH U54 GM104941; to M.C.W. Eeckhaut) and a grant from the National Institute of Justice, USDOJ (2017-IJ-CX-0016; to T. L. Anderson). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
The third wave featured a relative tie in overdose deaths between heroin and fentanyl for 2013 and 2014. In 2015, fentanyl took off and surpassed heroin.
References
- Berk R. A., Western B., Weiss R. R. Statistical inference for apparent populations. Sociological Methodology. 1995;25:421–458. doi:10.2307/271073. [Google Scholar]
- Calcaterra S., Glanz J., Binswanger I. A. National trends in pharmaceutical opioid related overdose deaths compared to other substance related overdose deaths: 1999–2009. Drug and Alcohol Dependence. 2013;131:263–270. doi: 10.1016/j.drugalcdep.2012.11.018. doi:10.1016/j.drugalcdep.2012.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell C. I., Weisner C., LeResche L., Ray G. T., Saunders K., Sullivan M. D. Von Korff M. Age and gender trends in long-term opioid analgesic use for noncancer pain. American Journal of Public Health. 2010;100:2541–2547. doi: 10.2105/AJPH.2009.180646. doi:10.2105/AJPH.2009.180646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Opioid overdose: Understanding the epidemic. 2018a Retrieved from https://www.cdc.gov/drugoverdose/epidemic/index.html. [Google Scholar]
- Centers for Disease Control and Prevention. Drug overdose deaths [data set] 2018b Retrieved from: https://www.cdc.gov/drugoverdose/data/statedeaths.html.
- Centers for Disease Control and Prevention. Bridged-race population estimates. 2018c Retrieved from https://wonder.cdc.gov/bridged-race-population.html. [Google Scholar]
- Cicero T. J., Ellis M. S., Surratt H. L., Kurtz S. P. The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71:821–826. doi: 10.1001/jamapsychiatry.2014.366. doi:10.1001/jamapsychiatry.2014.366. [DOI] [PubMed] [Google Scholar]
- Cowger C. D. Statistical significance tests: Scientific ritualism or scientific method? Social Service Review. 1984;58:358–372. doi:10.1086/644212. [Google Scholar]
- Darke S., Hall W. Heroin overdose: Research and evidence-based intervention. Journal of Urban Health. 2003;80:189–200. doi: 10.1093/jurban/jtg022. doi:10.1093/jurban/jtg022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Coffin P. O. Drug overdose: New insights, innovative surveillance, and promising interventions. Journal of Urban Health. 2003;80:186–188. doi: 10.1093/jurban/jtg021. doi:10.1093/jurban/jtg021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy G. P., Jr., Zhang K., Bohm M. K., Losby J., Lewis B., Young R., Dowell D. Vital signs: Changes in opioid prescribing in the United States, 2006–2015. Morbidity and Mortality Weekly Report. 2017;66:697–704. doi: 10.15585/mmwr.mm6626a4. doi:10.15585/mmwr.mm6626a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalal H., Buchanich J. M., Roberts M. S., Balmert L. C., Zhang K., Burke D. S. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science. 2018;361 doi: 10.1126/science.aau1184. eaau1184. doi:10.1126/science.aau1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipato T., Terplan M. Risk factors for opioid overdose. Current Treatment Options in Psychiatry. 2018;5:323–333. doi:10.1007/s40501-018-0153-1. [Google Scholar]
- Mack K. A., Jones C. M., Paulozzi L. J. & the Centers for Disease Control and Prevention (CDC) Vital signs: Overdoses of prescription opioid pain relievers and other drugs among women—United States, 1999–2010. Morbidity and Mortality Weekly Report. 2013;62:537–542. [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. Prescription opioids and heroin. 2018. Rockville, MD: Author. Retrieved from: https://www.drugabuse.gov/publications/research-reports/relationship-between-prescription-drug-heroin-abuseprescription-opioid-use-risk-factor-heroin-use. [Google Scholar]
- O’Donnell J. K., Gladden R. M., Seth P. Trends in deaths involving heroin and synthetic opioids excluding methadone, and law enforcement drug product reports, by census region—United States, 2006–2015. Morbidity and Mortality Weekly Report. 2017;66:897–903. doi: 10.15585/mmwr.mm6634a2. doi:10.15585/mmwr.mm6634a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulozzi L. J., Mack K. A., Hockenberry J. M. & the Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control, CDC. Vital signs: Variation among states in prescribing of opioid pain relievers and benzodiazepines—United States, 2012. Morbidity and Mortality Weekly Report. 2014;63:563–568. [PMC free article] [PubMed] [Google Scholar]
- Paulozzi L. J., Strickler G. K., Kreiner P. W., Koris C. M. Controlled substance prescribing patterns—Prescription behavior surveillance system, eight states, 2013. Morbidity and Mortality Weekly Report. Surveillance Summaries. 2015;64(SS09):1–14. doi: 10.15585/mmwr.ss6409a1. doi:10.15585/mmwr.ss6409a1. [DOI] [PubMed] [Google Scholar]
- Rubin A. Significance testing with population data. Social Service Review. 1985;59:518–520. doi:10.1086/644316. [Google Scholar]
- Rudd R. A., Seth P., David F., Scholl L. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. Morbidity and Mortality Weekly Report. 2016;65:1445–1452. doi: 10.15585/mmwr.mm655051e1. doi:10.15585/mmwr.mm655051e1. [DOI] [PubMed] [Google Scholar]
- Samkoff J. S., Baker S. P. Recent trends in fatal poisoning by opiates in the United States. American Journal of Public Health. 1982;72:1251–1256. doi: 10.2105/ajph.72.11.1251. doi:10.2105/AJPH.72.11.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seth P., Scholl L., Rudd R. A., Bacon S. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. Morbidity and Mortality Weekly Report. 2018;67:349–358. doi: 10.15585/mmwr.mm6712a1. doi:10.15585/mmwr.mm6712a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terplan M. Women and the opioid crisis: Historical context and public health solutions. Fertility and Sterility. 2017;108:195–199. doi: 10.1016/j.fertnstert.2017.06.007. doi:10.1016/j.fertnstert.2017.06.007. [DOI] [PubMed] [Google Scholar]
- Unick G. J., Rosenblum D., Mars S., Ciccarone D. Intertwined epidemics: National demographic trends in hospitalizations for heroin- and opioid-related overdoses, 1993–2009. PLoS One. 2013;8(2):e54496. doi: 10.1371/journal.pone.0054496. doi:10.1371/journal.pone.0054496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Houten J. P., Rudd R. A., Ballesteros M. F., Mack K. A. Drug overdose deaths among women aged 30–64 years—United States, 1999–2017. Morbidity and Mortality Weekly Report. 2019;68:1–5. doi: 10.15585/mmwr.mm6801a1. doi:10.15585/mmwr.mm6801a1. [DOI] [PMC free article] [PubMed] [Google Scholar]