Abstract
Introduction:
A growing body of research associates childhood trauma with obsessive-compulsive disorder (OCD). The aim of this study was to investigate the relationships between childhood trauma and OCD, including both its severity and OCD patients’ comorbid impulsivity, ADHD, anxiety, and depressive symptoms.
Methods:
A convenient sample consisting of 106 patients with OCD was given the Childhood Trauma Questionnaire (CTQ), Yale-Brown Obsessive Compulsive Scale (Y-BOCS), Wender Utah Rating Scale (WURS), Hamilton Rating Scale for Depression (HAM-D), Beck Anxiety Inventory (BAI), and Barratt Impulsivity Scale-11 (BIS-11).
Results:
The results showed that childhood trauma indirectly predicts the severity of OCD and directly predicts comorbidities in OCD patients, including anxiety, ADHD, WURS, and impulsivity. Patients with childhood trauma had higher WURS, BAI, and BIS-11 scores and fewer years of education. Ongoing adult ADHD was more common in individuals with childhood trauma.
Conclusion:
A history of childhood trauma in OCD patients has indirect effects on the severity of OCD and depressive symptoms and is associated with more severe anxiety, higher levels of impulsivity, higher prevalence of ADHD, and lower levels of education. More research is needed to clarify the effects of childhood trauma on OCD severity and comorbidity.
Keywords: Anxiety, childhood trauma, depression, impulsivity behaviour, obsessive compulsive disorder, severity
INTRODUCTION
In recent years, the relationship between obsessive-compulsive disorder (OCD) and childhood trauma has attracted the attention of researchers. Although several studies have suggested that obsessive-compulsive symptoms in nonclinical populations or OCD patients may be associated with childhood trauma (1–4), few studies have focused on the relationship between the severity of OCD and childhood trauma (5). A limited number of studies have investigated the effect of childhood trauma on non-OCD obsessive-compulsive symptoms in nonclinical samples (3, 6, 7). Mathew et al. (6) found that childhood emotional abuse and physical neglect were associated with the severity of obsessive-compulsive symptoms in the general population. In another nonclinical sample recruited by Briggs et al. (8), the severity of childhood trauma was positively correlated with the severity of obsessive-compulsive symptoms, although this relationship was closely associated with depression and anxiety. Most studies of patients diagnosed with OCD have found no relationship between childhood trauma and OCD severity, although some have detected severer OCD in individuals with a history of trauma history (5, 9–12). However, the relationship between childhood trauma and the severity of OCD symptoms is unclear.
In addition to OCD, childhood traumas have recently been associated with childhood attention deficit and hyperactivity disorder (ADHD) (13). Konstenius et al. recently showed that childhood trauma may be associated with childhood ADHD (14). On the other hand, Tan et al. found no correlation between the severity of OCD and childhood ADHD severity in OCD patients (15, 16). However, to the best of our knowledge, no study has investigated childhood ADHD in OCD patients with and without childhood trauma. Similarly, the relationship between adult ADHD and symptom severity in OCD patients requires further clarification. Furthermore, it is known that impulsivity, which is a common feature of OCD and ADHD, is higher in OCD patients than in control groups (15, 17). At the same time, some studies have demonstrated a relationship between impulsivity and childhood traumas (18, 19). It is noteworthy that the two important comorbidities of impulsivity symptoms and childhood ADHD have not been investigated in OCD patients with and without childhood trauma.
Considering the scarcity of studies on the topic, we aimed to investigate the effects of childhood trauma on various aspects of OCD, such as behavioral, cognitive, affective dimensions as well symptom severity by ADHD, childhood ADHD, impulsivity, and depressive and anxiety symptoms. In addition, we sought to determine whether depression, anxiety, ADHD, childhood ADHD, and impulsivity mediate the relationship between childhood trauma and symptom severity in OCD patients. We hypothesized that childhood trauma can influence the severity of OCD symptoms and its mediating factor such as ADHD, impulsivity, anxiety and depression.
METHODS
Participants
Between January 2013 and December 2017, 228 patients were diagnosed with OCD between the ages of 18 and 65 who applied to Feneryolu Medical Center of Üsküdar University in Istanbul. A total of 122 patients were excluded from the study, because 76 were not volunteers, 33 had exclusion criteria (9 patient had neurological disease, 11 patients had psychotic disorders, 3 patients used substance, 3 patients were pregnant, and 7 patients had other exclusion criteria), and 13 had missing data. This cross-sectional study enrolled a total of 106 convenient OCD patients. Of these patients, 46 (43.4%) were female and 60 (56.6%) were male. OCD, diagnosed according to DSM-5 criteria, was the primary diagnosis, that is, the chief and most distressing psychiatric disorder during the patients’ lifetimes. The diagnosis of ADHD was made according to the DSM-5 criteria from the psychiatrist. People who had neurological disease (such as epilepsy or multiple sclerosis), people who had a history of head trauma, mental retardation, psychotic disorders, substance abuse, or cognitive dysfunctions that would prevent them from completing the questionnaires, and people who were illiterate, pregnant, or breastfeeding were excluded.
Ethics
Before the patients were enrolled in the study, the Üsküdar University Ethics Committee for Non-Interventional Studies approved the study. Patients’ rights to study are protected according to the Declaration of Helsinki, and the study was carried out in accordance with the Guidelines for Good Clinical Practice.
Procedure
Participants were assessed using the following measures.
The Childhood Trauma Questionnaire (CTQ); includes questions that assess childhood emotional, physical, and sexual abuse and childhood physical and emotional neglect. The scale developed by Bernstein et al. is a 5-point Likert-type self-report scale that consists of 28 items (20). Turkish validity and reliability studies were conducted by Şar et al. (21). It allows the calculation of individual traumatic experience subscales and a total score. Scores for the emotional abuse subscale fall between 12 and 60, those for the physical abuse subscale fall between 7 and 35, those for the sexual abuse subscale fall between 7 and 35, those for the emotional neglect subscale fall between 16 and 80, and those for the physical neglect subscale fall between 8 and 40. The CTQ also includes three minimization questions, which address the denial of trauma and are not added to the total score. A cutoff score of 35 was suggested in the Turkish form of the scale (21); therefore, patients who have a score above 35 are regarded as having experienced childhood trauma. The cutoff scores of the subscales are as follows: 5 for sexual abuse and physical abuse, 7 for physical neglect and emotional abuse, and 12 for emotional neglect (19).
The Yale-Brown Obsessive Compulsive Scale (Y-BOCS); was used to assess the severity of OCD. It was first developed by Goodman et al. (22), and the Turkish version was developed by Karamustafalioğlu et al. (23).
The Barratt Impulsivity Scale-11 (BIS-11); is a self-report measure that evaluates the level of impulsivity. It consists of 30 items and has three subscales: attentional or cognitive impulsivity, motor impulsivity, and non-planning. The higher the total BIS-11 score, the higher the impulsivity level of the participant (24). The Turkish validity and reliability study of the BIS-11 was performed by Güleç et al. (25)
The Wender Utah Rating Scale (WURS); was developed in 1993 by Ward and colleagues to retrospectively assess the signs and symptoms of childhood ADHD in adults (26). Consisting of 25 items, the WURS is a self-report, 5-point Likert-type scale in which each item is scored between 0 and 4 (0=no, 4=extreme). The cutoff score for an ADHD diagnosis is 36. We made the diagnosis of ADHD according to the DSM-5 criteria but used the WURS to estimate the severity of childhood ADHD symptoms. It has been shown both that the WURS can distinguish ADHD patients from the control group and that ADHD patients can evaluate the results of psychopharmacological treatment. The validity and reliability study of the Turkish version of the scale was performed by Öncü et al. (27).
The Hamilton Depression Rating Scale (HAM-D); was used to measure the severity of depressive symptoms. It was first developed by Hamilton et al. (28), and the validity and reliability of the Turkish version were demonstrated by Akdemir et al. (29).
The Beck Anxiety Inventory (BAI); was used to measure the severity of anxiety. It was first developed by Beck et al. (30), and the validity and reliability of the Turkish version were demonstrated by Ulusoy et al. (31).
Statistical Analysis
Statistical analysis was performed using the SPSS 20.0 (Statistical Package for Social Sciences Inc., Chicago, IL, USA) package program. The normal distribution of variables was assessed using the Kolmogorov-Smirnov test. Student’s t-test was used to compare the continuous variables with a normal distribution, and the Mann-Whitney U test was used to compare the continuous variables without a normal distribution. Categorical data were compared using a chi-square test. Relations between parametric numerical variables and relations between nonparametric numerical variables were examined using the Pearson correlation test and the Spearman correlation test, respectively.
The multiple mediation model, which is a kind of multiple regression in the SPSS AMOS, was used to examine the hypothesis that childhood trauma affects the severity of OCD symptoms through anxiety and depression. A statistical significance limit of p≤0.05 was accepted in all analyses.
RESULTS
The comparison of categorical variables between OCD patients with and without childhood trauma is shown in Table 1. Of the 106 participants, 60 (43.4%) had a history of childhood trauma (Table 1). Gender, marital status, employment status, ongoing adult ADHD, and a past or present tic disorder did not differ significantly between those with and those without childhood trauma (Table 1). Childhood trauma was significantly more common in individuals with ADHD: of the patients with and the patients without coexisting ADHD, 78.9% (n=15) and 51.2% (n=42) had childhood trauma, respectively (p=0.028) (Table 1).
Table 1.
Comparison of categorical variables between OCD patients with and without childhood trauma
| Total | OCD patients with childhood trauma | OCD patients without childhood trauma | |||||
|---|---|---|---|---|---|---|---|
| n | % | n (%) | n (%) | X2 | df | p | |
| Total | 60 (43.4) | 46 (56.6) | |||||
| Gender | |||||||
| Female | 46 | 43.4 | 24 (52.2) | 22 (47.8) | 0.649 | 1 | a0.420 |
| Male | 60 | 56.6 | 36 (60.0) | 24 (40.0) | |||
| Marital Status | |||||||
| Married | 42 | 39.6 | 23 (54.8) | 19 (45.2) | 0.96 | 1 | a0.757 |
| Single | 64 | 60.4 | 37 (57.8) | 27 (42.2) | |||
| Employment | |||||||
| Employed | 51 | 48.6 | 30 (58.8) | 21 (41.2) | 0.114 | 1 | a0.735 |
| Unemployed | 54 | 51.4 | 30 (55.4) | 24 (44.6) | |||
| Adult ADHD | |||||||
| Yes | 19 | 18.8 | 15 (78.9) | 4 (21.1) | 4.824 | 1 | a0.028* |
| No | 82 | 81.2 | 42 (51.2) | 40 (48.8) | |||
| Tic | |||||||
| Yes | 5 | 4.9 | 4 (80.0) | 1(20.0) | 1.108 | 1 | a0.292 |
| No | 98 | 95.1 | 55 (56.1) | 43 (43.9) | |||
ADHD, attention deficit hyperactivity disorder; OCD, obsessive compulsive disorder.
Pearson Chi-Square Test.
<0.05.
The compatibility of the model test measurements was good. RMESA was <0.001 (the acceptable level is <0.05), and CMIN/DF was 0.934 (the acceptable level is <3) (Figure 1). The examination of the indirect effect of childhood trauma on symptoms severity of OCD through depressive symptoms (1.25) showed a significant relationship between them (p<0.001). Furthermore, the direct effect of childhood trauma on anxiety (0.30), ADHD (0.44), WURS (0.44), and impulsivity (0.64) was significant (p<0.05). The overall effect of childhood trauma on the severity of OCD symptoms was also significant (p<0.001).
Figure 1.
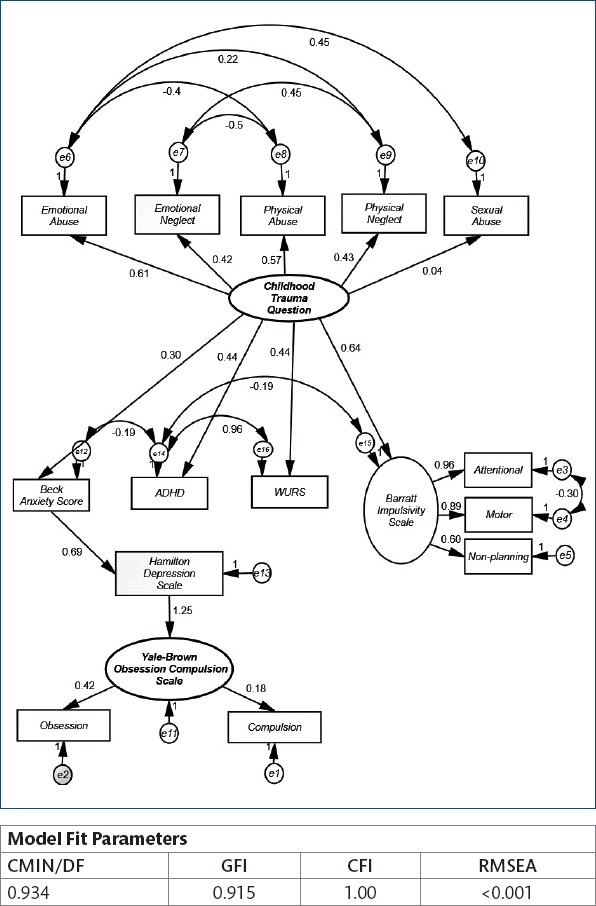
Model depicting the effect of childhood trauma, depression, anxiety and impulsivity on the severity of OCD.
The comparison of continuous variables between patients with and patients without childhood trauma is presented in Table 2. Patients with childhood trauma had significantly fewer years of education. The total score of the BIS-11 and the scores of its subscales (motor, inattention, and non-planning), BAI, and WURS were significantly higher in patients with childhood trauma. The scores of the CTQ and all its subscales were, as expected, significantly higher in the childhood trauma group. People with and people without childhood trauma did not differ significantly in age, age at onset of OCD, age at first treatment of OCD, time to first treatment of OCD, HAM-D and Y-BOCS scores, obsession, and compulsion.
Table 2.
Comparison of continuous variables between OCD patients with and without childhood trauma
| Variable | OCD patients with childhood trauma | OCD patients without childhood trauma | |||
|---|---|---|---|---|---|
| Mean±SD | Mean±SD | T/Z | p | ||
| Age | 31.37±11.03 | 31.74±10.28 | -0.316 | b0.752 | |
| Education Year | 12.47±2.90 | 14.15±2.45 | -3.378 | b0.001** | |
| OCD age of onset | 20.17±8.92 | 20.76±8.53 | -0.346 | a0.730 | |
| Age of first treatment | 24.23±8.00 | 28.48±8.68 | -0.391 | a0.697 | |
| Time without treatment | 4.06±5.23 | 4.10±7.06 | -0.741 | b0.459 | |
| BIS-11 | Total Score | 65.39±11.47 | 58.79±12.92 | -3.020 | b0.003** |
| Motor | 20.20±4.92 | 18.10±5.17 | -2.559 | b0.010** | |
| Attentional | 17.80±4.21 | 15.57±4.23 | 2.589 | a0.011* | |
| Non-planning | 27.39±5.10 | 25.12±5.77 | 2.062 | a0.042* | |
| Hamilton Depression Score | 15.25±6.76 | 13.26±8.43 | 1.348 | a0.181 | |
| Beck Anxiety Score | 23.33±12.86 | 16.20±12.58 | -2.991 | b0.003** | |
| Wender Utah Rating Scale | 34.98±18.98 | 23.02±15.12 | 3.322 | a0.001** | |
| Y-BOCS | Total Score | 22.33±6.64 | 21.91±7.29 | 0.309 | a0.758 |
| Obsession | 12.43±3.77 | 10.70±5.06 | 1.943 | a0.055 | |
| Compulsion | 9.88±4.88 | 11.02±4.36 | -1.244 | a0.216 | |
| CTQ | Total Score | 44.10±7.78 | 29.93±2.86 | -8.805 | b<0.001** |
| Emotional Neglect | 14.18±4.15 | 8.02±2.33 | 9.026 | a<0.001** | |
| Physical Neglect | 8.22±1.97 | 5.80±1.08 | 7.457 | a<0.001** | |
| Sexual Abuse | 6.30±2.49 | 5.13±0.49 | -3.546 | b<0.001** | |
| Emotional Abuse | 9.27±3.65 | 5.85±1.22 | -6.215 | b<0.001** | |
| Physical Abuse | 6.13±2.09 | 5.12±0.54 | -3.888 | b<0.001** | |
| Minimization | 0.27±0.63 | 0.80±0.88 | -3.747 | b<0.001** | |
BIS-11, Barratt impulsivity scale; CTQ, childhood trauma questionnaire; Y-BOCS, Yale-Brown obsession compulsion scale; OCD, obsessive compulsive disorder.
Student’s t test,
Mann-Whitney U Test,
p<0.05,
p<0.01.
Table 3 shows the comparison of the total Y-BOCS scores and the scores of its obsessive and compulsive subscales between individuals with a certain subtype of childhood trauma and those without this subtype. The only significant result was observed in patients with physical abuse in their childhood, who exhibited lower compulsion scores than those without this subtype of trauma (p=0.039).
Table 3.
Comparison of the Y-BOCS scores between patients with and without a specific trauma subtype
| Y-BOCS Total | Y-BOCS Obsession | Y-BOCS Compulsion | ||||
|---|---|---|---|---|---|---|
| Mean±SD | p | Mean±SD | p | Mean±SD | p | |
| Emotional Neglect | ||||||
| Yes | 22.67±7.42 | a0.536 | 12.55±4.22 | a0.104 | 10.12±5.15 | a0.648 |
| No | 21.81±6.57 | 11.11±4.52 | 10.55±4.37 | |||
| Physical Neglect | ||||||
| Yes | 21.88±6.87 | a0.658 | 11.76±4.18 | a0.841 | 9.97±5.11 | a0.322 |
| No | 22.48±6.99 | 11.58±4.78 | 10.88±4.09 | |||
| Sexual Abuse | ||||||
| Yes | 22.18±6.14 | a0.980 | 12.50±3.32 | a0.257 | 9.98±4.20 | a0.360 |
| No | 22.14±7.19 | 11.38±4.76 | 10.63±4.84 | |||
| Emotional Abuse | ||||||
| Yes | 21.76±6.70 | a0.640 | 11.90±4.26 | a0.674 | 9.83±4.96 | a0.335 |
| No | 22.41±7.06 | 11.53±4.58 | 10.73±4.48 | |||
| Physical Abuse | ||||||
| Yes | 20.70±6.60 | a0.208 | 11.93±3.01 | a0.740 | 8.78±5.26 | a0.039* |
| No | 22.65±6.96 | 11.59±4.85 | 10.92±4.36 | |||
Y-BOCS, Yale-Brown obsession compulsion scale; OCD, obsessive compulsive disorder.
Student’s t test,
Mann-Whitney U Test,
p<0.05.
Table 4 compares the scores of the CTQ and its subscales between males and females. Only the scores of physical abuse differed significantly between females and males, and they were higher in the latter (p=0.021). The total score of the CTQ and the scores of neglect, physical neglect, sexual abuse, emotional abuse, and minimization were similar between the two sexes.
Table 4.
Comparison of emotional neglect, physical neglect, sexual abuse, emotional abuse, physical abuse, and minimization scores between females and males
| Females with OCD (n=46) | Males with OCD (n=60) | |||
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | T/Z | p | |
| Total CTQ | 36.52±9.06 | 39.05±9.48 | -1.385 | b0.166 |
| Emotional Neglect | 10.85±4.31 | 12.02±4.83 | 0.706 | b0.217 |
| Physical Neglect | 6.76±1.55 | 7.48±2.30 | -1.926 | a0.057 |
| Sexual Abuse | 5.78±1.61 | 5.80±2.24 | -0.154 | b0.877 |
| Emotional Abuse | 7.87±3.76 | 7.72±2.98 | -0.378 | b0.706 |
| Physical Abuse | 5.26±0.74 | 6.03±2.09 | -2.305 | b0.021* |
| Minimization | 0.52±0.78 | 0.48±0.81 | -0.327 | b0.744 |
Y-BOCS, Yale-Brown obsession compulsion scale; OCD, obsessive compulsive disorder.
Student’s t test,
Mann-Whitney U Test,
p<0.05.
Table 5 demonstrates the correlations among various data of the study. The CTQ scores are not correlated to the scores of the Y-BOCS, HAM-D, and BAI, whereas the scores of the CTQ are correlated with those of the WURS and the scores of emotional neglect are correlated with the scores of the WURS.
Table 5.
Correlations among age, Y-BOCS, HAM-D, BAI, BIS-11, WURS, and CTQ
| Age | YBOCS | YBOCS-O | YBOCS-C | HAM-D | BAI | BIS-11 | BIS-A | BIS-M | BIS-N | WURS | CTQ | EA | EN | PA | PN | SA | M | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 1 | |||||||||||||||||
| YBOCS | -0.162 | 1 | ||||||||||||||||
| YBOCS-O | -0.097 | 0.727** | 1 | |||||||||||||||
| YBOCS-C | -0.144 | 0.764** | 0.131 | 1 | ||||||||||||||
| HAM-D | -0.082 | 0.544** | 0.525** | 0.291** | 1 | |||||||||||||
| BAI | -0.051 | 0.391** | 0.349** | 0.232* | 0.659** | 1 | ||||||||||||
| BIS-11 | -0.108 | -0.084 | 0.036 | -0.178 | 0.050 | -0.007 | 1 | |||||||||||
| BIS-A | -0.188 | 0.000 | 0.151 | -0.134 | 0.147 | 0.151 | 0.799** | 1 | ||||||||||
| BIS-M | -0.096 | -0.079 | -0.052 | -0.095 | -0.067 | -0.061 | 0.784** | 0.425** | 1 | |||||||||
| BIS-N | -0.001 | -0.114 | 0.009 | -0.202* | 0.058 | -0.077 | 0.856** | 0.587** | 0.469** | 1 | ||||||||
| WURS | -0.098 | 0.059 | 0.111 | -0.014 | 0.197 | 0.389** | 0.222* | 0.339** | 0.125 | 0.107 | 1 | |||||||
| CTQ | -0.041 | -0.059 | 0.118 | -0.180 | 0.108 | 0.197* | 0.288** | 0.280** | 0.281** | 0.154 | 0.381** | 1 | ||||||
| EA | -0.213* | -0.047 | 0.027 | -0.080 | 0.099 | 0.163 | 0.242* | 0.256* | 0.267* | 0.086 | 0.297** | 0.755** | 1 | |||||
| EN | 0.005 | 0.023 | 0.173 | -0.104 | 0.152 | 0.188 | 0.198 | 0.223* | 0.160 | 0.114 | 0.353** | 0.845** | 0.461** | 1 | ||||
| PA | 0.147 | -0.150 | -0.023 | -0.191 | -0.052 | -0.007 | 0.230* | 0.177 | 0.309** | 0.082 | 0.109 | 0.535** | 0.423** | 0.263** | 1 | |||
| PN | 0.075 | -0.011 | 0.126 | -0.151 | 0.091 | 0.129 | 0.290** | 0.187 | 0.288** | 0.228* | 0.198* | 0.704** | 0.340** | 0.587** | 0.304** | 1 | ||
| SA | -0.050 | -0.113 | -0.004 | -0.154 | -0.060 | 0.092 | -0.006 | 0.040 | -0.066 | 0.017 | 0.203* | 0.296** | 0.095 | 0.046 | 0.035 | 0.091 | 1 | |
| M | -0.062 | -0.023 | -0.100 | 0.028 | 0.113 | -0.118 | 0.074 | -0.006 | 0.000 | 0.170 | -0.077 | -0.321** | -0.221* | -0.271** | -0.170 | -0.176 | -0.180 | 1 |
BAI, Beck anxiety inventory; BIS-11, Barratt impulsivity scale; BIS-A, attentional subscale of Barratt impulsivity scale; BIS-M, motor impulsivity subscale of Barratt impulsivity scale; BIS-N, non-planning subscale of Barratt impulsivity scale; CTQ, childhood trauma questionnaire; HAM-D, Hamilton depression rating scale-17 items; Y-BOCS, Yale-Brown obsessive compulsive scale; YBOCS-O, obsession subscale of Yale-Brown obsessive compulsive scale; YBOCS-C, compulsion subscale of Yale-Brown obsessive compulsive scale; WURS, Wender Utah rating scale; EA, emotional abuse subscale of childhood trauma questionnaire; EN, emotional neglect subscale of childhood trauma questionnaire; PA, physical abuse subscale of childhood trauma questionnaire; PN, psychical neglect subscale of childhood trauma questionnaire; SA, sexual abuse subscale of childhood trauma questionnaire; M, minimization subscale of childhood trauma questionnaire.
p<0.05,
p<0.01.
Table 6 reveals that OCD patients with ongoing adult ADHD had significantly higher total CTQ scores (p=0.026) and significantly higher emotional abuse scores (p=0.003) than did those without ADHD.
Table 6.
Comparison of total CTQ, emotional neglect, physical neglect, sexual abuse, emotional abuse, physical abuse and minimization between OCD patients with and without ongoing adult ADHD
| OCD patients with adult ADHD (n=82) | OCD patients without adult ADHD (n=19) | |||
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | T/Z | p | |
| Total CTQ | 41.79±9.51 | 36.76±8.78 | -2.227 | b0.026* |
| Emotional Neglect | 13.16±5.52 | 10.98±4.35 | -1.591 | b0.112 |
| Physical Neglect | 7.42±1.83 | 7.07±2.10 | 0.665 | a0.508 |
| Sexual Abuse | 5.95±1.84 | 5.79±2.08 | -0.198 | b0.843 |
| Emotional Abuse | 9.53±3.79 | 7.23±2.73 | 3.052 | a0.003** |
| Physical Abuse | 5.74±1.28 | 5.68±1.77 | -0.662 | b0.508 |
| Minimization | 0.42±0.69 | 0.54±0.83 | -0.484 | b0.629 |
OCD, obsessive compulsive disorder; CTQ, childhood trauma questionnaire.
Student’s t test,
Mann-Whitney U Test,
p<0.05,
p<0.01.
DISCUSSION
The study’s most important finding is that childhood trauma causes increased severity of OCD symptoms through anxiety and depression. In patients with OCD, this is that showed childhood trauma predict severe OCD and that showed it predicts severe anxiety and depression. In addition, this study showed that OCD patients with a history of childhood trauma had severer anxiety, higher levels of impulsivity, higher levels of childhood ADHD, higher prevalence of ongoing adult ADHD, and fewer years of education than did patients without a history of childhood trauma. To the best of our knowledge, this is the first study to identify the ways in which childhood traumas affect the severity of OCD in a clinical sample.
Moreover, recent studies showed that there is a relationship between childhood trauma and the severity of psychiatric disorders, such as anxiety disorder (32), depression (33), psychosis (34), bipolar disorder (35), somatization (36), suicide attempts (37) and conversion disorder (38). On the other hand, although one study detected high OCD scores in individuals with childhood trauma compared to those without it (5), most previous studies of OCD found no significant relationship between childhood trauma and OCD severity (9–12). Two studies estimated only weak correlations between OCD severity and childhood trauma (2, 39), and this was true only for the severity of obsessions in one of them (2). In two studies conducted on nonclinical samples, no association between the severity of obsessive-compulsive symptoms and childhood trauma was observed by either Mathew et al. (6) or Briggs et al. (8), who controlled for depression and anxiety. It is also known that childhood trauma has an effect on anxiety and depression in OCD patients (6, 8). Moreover, the severity of anxiety and that of depression symptoms were shown to increase the severity of OCD symptoms (40). Regarding this point, our study showed that childhood psychiatric traumas increased the severity of anxiety and depression symptoms in OCD patients and that this effect caused an increase in the severity of OCD symptoms. The reason for the lack of a direct effect of childhood trauma on the severity of OCD symptoms is that the severity of such symptoms can be explained by the complex and generalized effect of childhood trauma on anxiety and depression. In light of all this information, our results provide sufficient evidence to explain the relationship between childhood trauma and OCD symptoms.
We found that OCD patients with childhood trauma had higher levels of anxiety but a similar severity of depressive symptoms in comparison to those without childhood trauma. This lack of a relationship between childhood trauma and depression is not surprising in view of the existing literature. According to the model of our study, anxiety symptoms affect depressive symptoms. Ay and Erbay detected similar levels of anxiety and depressive symptoms in OCD patients with and those without childhood trauma (5). Selvi et al. observed no correlation between the severities of depression and trauma (9). Visser et al. found that trauma was associated with the comorbidity of affective disorders but not with that of anxiety disorders. (11) Hemmings et al. offered a slightly lower, though marginally significant, score of physical neglect in obsessive-compulsives with comorbid depression than in those without depression (41).
We found that the prevalence of ongoing adult ADHD and the severity of childhood ADHD symptoms (measured by the WURS) were higher in patients with childhood trauma than in those without it. The severity of childhood ADHD symptoms was correlated, though weakly, to the total severity of trauma, emotional abuse, and emotional neglect. The severity of childhood ADHD was not correlated with that of OCD. The positive correlation between childhood ADHD and childhood trauma severities is compatible with the literature (42, 43). A recent prospective twin study on a rather large sample revealed a strong association between ADHD and abuse or neglect in childhood; nevertheless, into young adulthood, neither abuse or neglect was associated with ADHD (13). The fact that OCD could interact with childhood trauma as well as ADHD independently might account for the high prevalence of adult ADHD in our traumatized group; in other words, an increase in the risk of comorbid adult ADHD might be mediated through OCD even if trauma did not play a role. Moreover, impulsivity, which is known to be high in both OCD and ADHD patients, may lead to potentially risky situations that expose children to traumatic events. The comparison of our adult patients with and those without current, ongoing ADHD with respect to trauma history revealed that those with ADHD were more severely traumatized. When trauma subtypes were compared separately, only emotional abuse, but not other subtypes of trauma, was significantly severer in individuals with ADHD than in people without it.
Indeed, it has been suggested that impulsivity, which accompanies both ADHD and OCD, is an outcome of childhood trauma (15, 44, 45). As one might expect, our obsessive-compulsive patients with a history of childhood trauma exhibited higher total, attentional, motor, and non-planning impulsivity than did those without trauma. Furthermore, we observed several significant, though weak, correlations between various subscales of impulsivity and trauma. Previous studies have shown that OCD patients had high impulsivity compared to controls (15, 46, 47). It seems that trauma further increases impulsivity levels in patients already afflicted with high impulsivity.
We demonstrated a relationship between childhood trauma and fewer years of education. The educational disadvantage of people who underwent childhood adversities is well-established (48), Another study, which investigated the impact of childhood trauma on education in patients with OCD, achieved results consistent with the present study (5). Furthermore, it is reasonable that ADHD, which was much more frequent in our traumatized patients than in those who had not suffered trauma, might have contributed to educational problems in the sample under investigation.
One of the limitations of the current study is its cross-sectional design. The cross-sectional correlational properties of the data do not allow for propositions regarding the causal mechanisms of the relationships. The evaluation of childhood trauma using a self-report survey might be another limitation of the present study; however, for obvious reasons, measures other than self-report are rarely administered in studies focusing on childhood trauma. In addition, the fact that the study was carried out in one center may be an obstacle to the generalization of our results.
CONCLUSION
A history of trauma can commonly be detected in the childhood of OCD patients. Comorbid ADHD, anxiety, depression, and severe symptoms should call to mind that these patients probably experienced various kinds of trauma when they were children. Adults with a history of trauma suffer higher anxiety and depressive symptoms, thus aggravating the clinical picture as a whole. Although trauma does not affect future employment and marital status, traumatized children with OCD are less educated. The educational disadvantages, coexisting ADHD, high impulsivity, and severe anxiety associated with childhood trauma may have further impacts on obsessive-compulsive individuals not investigated in the current study, and these impacts remain to be illuminated. Whether psychotherapy that targets OCD should not only employ classical exposure and response prevention but also handle past trauma represents an interesting question that could be profitably addressed by clinicians.
Footnotes
Ethics Committee Approval: The Üsküdar University Ethics Committee approved this study.
Informed Consent: Patients’ rights to study are protected according to the Declaration of Helsinki, and the study was carried out in accordance with the Guidelines for Good Clinical Practice.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - AÇ, OT; Design - AÇ, OT; Supervision - OT; Resource - AÇ; Materials: AÇ, OT; Data Collection and/ or Processing - AÇ, OT; Analysis and/or Interpretation - AÇ, OT; Literature Search - AÇ; Writing - AÇ, OT; Critical Reviews - AÇ, OT.
Conflict of Interest: Authors have declared that they have no conflict of interest.
Financial Disclosure: None
REFERENCES
- 1.Lochner C, du Toit PL, Zungu Dirwayi N, Marais A, van Kradenburg J, Seedat S, Niehaus DJ, Stein DJ. Childhood trauma in obsessive compulsive disorder, trichotillomania, and controls. Depress Anxiety. 2002;15:66–68. doi: 10.1002/da.10028. [DOI] [PubMed] [Google Scholar]
- 2.Carpenter L, Chung MC. Childhood trauma in obsessive compulsive disorder:the roles of alexithymia and attachment. Psychol Psychother. 2011;84:367–388. doi: 10.1111/j.2044-8341.2010.02003.x. [DOI] [PubMed] [Google Scholar]
- 3.Demirci K. The investigation of relationship between childhood trauma and obsessive-compulsive symptoms. J Mood Disord. 2016;6:7–13. [Google Scholar]
- 4.Gershuny BS, Baer L, Parker H, Gentes EL, Infield AL, Jenike MA. Trauma and posttraumatic stress disorder in treatment resistant obsessive compulsive disorder. Depress Anxiety. 2008;25:69–71. doi: 10.1002/da.20284. [DOI] [PubMed] [Google Scholar]
- 5.Ay R, Erbay LG. Relationship between childhood trauma and suicide probability in obsessive-compulsive disorder. Psychiatry Res. 2018;261:132–136. doi: 10.1016/j.psychres.2017.12.054. [DOI] [PubMed] [Google Scholar]
- 6.Mathews CA, Kaur N, Stein MB. Childhood trauma and obsessive compulsive symptoms. Depress Anxiety. 2008;25:742–751. doi: 10.1002/da.20316. [DOI] [PubMed] [Google Scholar]
- 7.Nelson EC, Heath AC, Madden PA, Cooper ML, Dinwiddie SH, Bucholz KK, Glowinski A, McLaughlin T, Dunne MP, Statham DJ, Martin NG. Association between self-reported childhood sexual abuse and adverse psychosocial outcomes:results from a twin study. Arch Gen Psychiatry. 2002;59:139–145. doi: 10.1001/archpsyc.59.2.139. [DOI] [PubMed] [Google Scholar]
- 8.Briggs ES, Price IR. The relationship between adverse childhood experience and obsessive-compulsive symptoms and beliefs:the role of anxiety, depression, and experiential avoidance. J Anxiety Disord. 2009;23:1037–1046. doi: 10.1016/j.janxdis.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Selvi Y, Besiroglu L, Aydin A, Gulec M, Atli A, Boysan M, Celik C. Relations between childhood traumatic experiences, dissociation, and cognitive models in obsessive compulsive disorder. Int J Psychiatry Clin Pract. 2012;16:53–59. doi: 10.3109/13651501.2011.617458. [DOI] [PubMed] [Google Scholar]
- 10.Belli H, Ural C, Yesilyurt S, Vardar M, Akbudak M, Oncu F. Childhood trauma and dissociation in patients with obsessive compulsive disorder. West Indian Med J. 2013;62:39–44. [PubMed] [Google Scholar]
- 11.Visser HA, van Minnen A, van Megen H, Eikelenboom M, Hoogendoorn A, Kaarsemaker M, Balkom AJ, van Oppen P. The relationship between adverse childhood experiences and symptom severity, chronicity, and comorbidity in patients with obsessive-compulsive disorder. J Clin Psychiatry. 2014;75:1034–1039. doi: 10.4088/JCP.13m08825. [DOI] [PubMed] [Google Scholar]
- 12.Shavitt RG, Valério C, Fossaluza V, da Silva EM, Cordeiro Q, Diniz JB, Belotto-Silva C, Cordioli AV, Mari J, Miguel EC. The impact of trauma and post-traumatic stress disorder on the treatment response of patients with obsessive-compulsive disorder. J Clin Psychiatry. 2010;260:91–99. doi: 10.1007/s00406-009-0015-3. [DOI] [PubMed] [Google Scholar]
- 13.Stern A, Agnew-Blais J, Danese A, Fisher HL, Jaffee SR, Matthews T, Polanczyk GV, Arseneault L. Associations between abuse/neglect and ADHD from childhood to young adulthood:a prospective nationally-representative twin study. Child Abuse Negl. 2018;81:274–285. doi: 10.1016/j.chiabu.2018.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Konstenius M, Leifman A, van Emmerik-van Oortmerssen K, van de Glind G, Franck J, Moggi F, Ramos-Quiroga JA, Levin FR, Carpentier PJ, Skutle A, Bu ET, Kaye S, Demetrovics Z, Barta C, Auriecomb M, Fatséas M, Johnson B, Faraone SV, Allsop S, Carruthers S, Schoevers RA, Verspreet S, Dom G, Koeter MWJ, van den Brink W. Childhood trauma exposure in substance use disorder patients with and without ADHD. Addict Behav. 2017;65:118–124. doi: 10.1016/j.addbeh.2016.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tan O, Metin B, Metin S. Obsessive-compulsive adults with and without childhood ADHD symptoms. Atten Defic Hyperact Disord. 2016;8:131–138. doi: 10.1007/s12402-016-0196-3. [DOI] [PubMed] [Google Scholar]
- 16.Abramovitch A, Dar R, Mittelman A, Wilhelm S. Comorbidity between attention deficit/hyperactivity disorder and obsessive-compulsive disorder across the lifespan:a systematic and critical review. Harv Rev Psychiatry. 2015;23:245–262. doi: 10.1097/HRP.0000000000000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tan O, Koroglu AF. Smoking Prevalence, Nicotine Dependence, and Impulsivity in Obsessive-Compulsive Disorder. Int J Ment Health Addict. 2018 [Google Scholar]
- 18.Evren C, Cınar O, Evren B, Ulku M, Karabulut V, Umut G. The mediator roles of trait anxiety, hostility, and impulsivity in the association between childhood trauma and dissociation in male substance-dependent inpatients. Compr Psychiatry. 2013;54:158–166. doi: 10.1016/j.comppsych.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 19.Erel Ö, Gölge ZB. The relationship between risky behaviors and childhood abuse, impulsivity and risky behaviors in university students. Anat J Psychiatry. 2015;16:189–197. [Google Scholar]
- 20.Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, Sapareto E, Ruggiero J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151:1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- 21.Şar V, Öztürk PE, İkikardeş E. Validity and Reliability of the Turkish Version of the Childhood Trauma Questionnaire. Turkiye Klinikleri J Med Sci. 2012;32:1054–1063. [Google Scholar]
- 22.Goodman W, Price L, Rasmussen S, Mazure C, Fleischmann R, Hill C, Heninger G, Charney D. Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 23.Karamustafalıoğlu K, Üçışık A, Ulusoy M, Erkmen H. Validity and Reliability of the Turkish Version of the Yale-brown obsessive compulsive scale. Bursa: SavaşOfset; 1993. p. 86. [Google Scholar]
- 24.Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 25.Güleç H, Tamam L, Yazıcı M, Turhan M, Karakuş G, Zengin M, Stanford MS. Psychometric Properties of the Turkish Version of the Barratt Impulsiveness Scale-11. Bull Clin Psychopharmacol. 2008;18:251–258. [Google Scholar]
- 26.Ward MF, Wender PH, Reimherr FW. The Wender Utah Rating Scale:an aid in the retrospective diagnosis of childhood attention deficit hyperactivity disorder. Am J Psychiatry. 1993;150:885–890. doi: 10.1176/ajp.150.6.885. Available at: https://pdfs.semanticscholar.org/d519/805d656c84366927a0c1d17632dbf13f6f42.pdf . [DOI] [PubMed] [Google Scholar]
- 27.Öncü B, Ölmez Ş, Şentürk V. Validity And Reliability of the Turkish Version of the Wender Utah Rating Scale for Attention-Deficit/ Hyperactivity Disorder in Adults. Turk Psikiyatri Derg. 2005;16:252–259. [PubMed] [Google Scholar]
- 28.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Akdemir A, Örsel S, Dağ İ, Türkçapar H, İşcan N, Özbay H. Clinical Use and Validity and Reliability of the Turkish Version of the Hamilton Depression Rating Scale. Psikiyatri Psikoloji Psikofarmakoloji Derg. 1996;4:251–259. [Google Scholar]
- 30.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety:psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 31.Ulusoy M, Sahin NH, Erkmen H. Turkish Version of the Beck Anxiety Inventory:Psychometric Properties. Int J Cogn Ther. 1998;12:163–172. [Google Scholar]
- 32.Gül A, Gül H, Özen NE, Battal S. The relationship between anxiety, depression, and dissociative symptoms on the basis of childhood traumas. J Mood Disord. 2016;6:107–115. [Google Scholar]
- 33.Bülbül F, Çakır Ü, Ülkü C, Üre I, Karabatak O, Alpak G. Childhood trauma in recurrent and first episode depression. Anat J Psychiatry. 2013;14:93–99. [Google Scholar]
- 34.Üçok A, Bıkmaz S. The effects of childhood trauma in patients with first episode schizophrenia. Acta Psychiatr Scand. 2007;116:371–377. doi: 10.1111/j.1600-0447.2007.01079.x. [DOI] [PubMed] [Google Scholar]
- 35.Erten E, Uney AFK, Fıstıkcı N. Bipolar Disorder and Childhood Trauma. Curr Appr Psychiatry. 2015;7:157–165. [Google Scholar]
- 36.Altıntaş E, Göksel BK, Sarıtürk Ç, Taşkıntuna N. Evaluation of relationship between childhood maltreatment and medication overuse headache. Arch Neuropsychiatr. 2015;52:267–271. doi: 10.5152/npa.2015.8833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yildirim F, Küçükgöncü S, Beştepe EE, Yildirim MS. The relationship of childhood abuse and neglect with suicide attempts in an adult unipolar depression sample. Arch Neuropsychiatr. 2014;51:133–140. doi: 10.4274/npa.y6802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Akyüz F, Gökalp PG, Erdiman S, Oflaz S, Karşidağ Ç. Conversion disorder comorbidity and childhood trauma. Arch Neuropsychiatr. 2017;54:15–20. doi: 10.5152/npa.2017.19184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Semiz UB, Inanc L, Bezgin CH. Are trauma and dissociation related to treatment resistance in patients with obsessive-compulsive disorder? Soc Psychiatry Psychiatr Epidemiol. 2014;49:1287–1296. doi: 10.1007/s00127-013-0787-7. [DOI] [PubMed] [Google Scholar]
- 40.Altıntaş E, Taşkıntuna N. Factors associated with depression in obsessive-compulsive disorder:a cross-sectional study. Arch Neuropsychiatr. 2015;52:346–353. doi: 10.5152/npa.2015.7657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hemmings SMJ, Lochner C, van der Merwe L, Cath DC, Seedat S, Stein DJ. BDNF Val66Met modifies the risk of childhood trauma on obsessive-compulsive disorder. J Psychiatr Res. 2013;47:1857–1863. doi: 10.1016/j.jpsychires.2013.08.012. [DOI] [PubMed] [Google Scholar]
- 42.Rucklidge JJ, Brown DL, Crawford S, Kaplan BJ. Retrospective reports of childhood trauma in adults with ADHD. J Atten Disord. 2006;9:631–641. doi: 10.1177/1087054705283892. [DOI] [PubMed] [Google Scholar]
- 43.Brown NM, Brown SN, Briggs RD, Germán M, Belamarich PF, Oyeku SO. Associations between adverse childhood experiences and ADHD diagnosis and severity. Acad Pediatr. 2017;17:349–355. doi: 10.1016/j.acap.2016.08.013. [DOI] [PubMed] [Google Scholar]
- 44.Matthies SD, Philipsen A. Common ground in attention deficit hyperactivity disorder (ADHD) and borderline personality disorder (BPD)-Review of recent findings. Borderline Personal Disord Emot Dysregul. 2014;1:3. doi: 10.1186/2051-6673-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Richard-Lepouriel H, Kung A-L, Hasler R, Bellivier F, Prada P, Gard S, Ardu S, Kahn J-P, Dayer A, Henry C, Aubry JM, Leboyer M, Perroud N, Etain B. Impulsivity and its association with childhood trauma experiences across bipolar disorder, attention deficit hyperactivity disorder and borderline personality disorder. J Affect Disord. 2018;244:33–41. doi: 10.1016/j.jad.2018.07.060. [DOI] [PubMed] [Google Scholar]
- 46.Benatti B, Dell'Osso B, Arici C, Hollander E, Altamura AC. Characterizing impulsivity profile in patients with obsessive-compulsive disorder. Int J Psychiatry Clin Pract. 2014;18:156–160. doi: 10.3109/13651501.2013.855792. [DOI] [PubMed] [Google Scholar]
- 47.Demirci E, Özmen S, Öztop DB. Relationship between impulsivity and serum oxytocin in male children and adolescents with attention-deficit and hyperactivity disorder:A preliminary study. Arch Neuropsychiatr. 2016;53:291–295. doi: 10.5152/npa.2015.10284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Veldman K, Bültmann U, Almansa J, Reijneveld SA. Childhood adversities and educational attainment in young adulthood:the role of mental health problems in adolescence. J Adolesc Health. 2015;57:462–467. doi: 10.1016/j.jadohealth.2015.08.004. [DOI] [PubMed] [Google Scholar]


