Health care expenditures and use attributed to children vary with illness severity and chronicity. We describe health care expenditures and use for children with NC-CDs.
Abstract
BACKGROUND:
Pediatric health care expenditures and use vary by level of complexity and chronic illness. We sought to determine expenditures and use for children with noncomplex chronic diseases (NC-CDs).
METHODS:
We performed a retrospective, cross-sectional analysis of Medicaid enrollees (ages 0–18 years) from January 1, 2012, through December 31, 2013, using administrative claims (the Truven MarketScan Medicaid Database). Patients were categorized by chronicity of illness by using 3M Health Information System’s Clinical Risk Groups (CRGs) as follows: without chronic diseases (WO-CDs) (CRG 1–2), NC-CDs (CRG 3–5), and complex chronic diseases (C-CDs) (CRG 6–9). Primary outcomes were medical expenditures, including total annualized population expenditure and per-member per-year expenditure (PMPY). Secondary outcomes included the number of health care encounters over the 2-year period.
RESULTS:
There were 2 424 946 children who met inclusion criteria, 53% were WO-CD; 36% had an NC-CD; and 11% had a C-CD. Children with NC-CDs accounted for 33% ($2801 PMPY) of the annual spending compared with 20% ($1151 PMPY) accounted for by children WO-CDs and 47% ($12 569 PMPY) by children with C-CDs. The median outpatient visit count by group over the 2-year period was 15 (interquartile range [IQR] 10–25) for NC-CD, 8 (IQR 5–13) WO-CD, and 34 (IQR 19–72) for C-CD.
CONCLUSIONS:
Children with NC-CDs accounted for 33% of pediatric Medicaid expenditures and have significantly higher PMPY and aggregate annual expenditures than children WO-CDs. The annual aggregate expenditures of the NC-CD group represent a significant societal cost because of the high volume of children, extrapolated to ∼$34.9 billion annually in national Medicaid expenditures.
What’s Known on This Subject:
It is widely known that care required by children with complex chronic disease is expensive despite a relatively low prevalence. Less is known about the total health care expenditures and use required to care for children with noncomplex chronic diseases.
What This Study Adds:
This retrospective, cross-sectional analysis of Medicaid administrative claims over a 2-year period highlights the prevalence of noncomplex chronic diseases. This population has frequent health care use and significant total population spending given its high prevalence.
Many health conditions affecting children are chronic in nature. A subset of these childhood chronic diseases are classified as noncomplex chronic diseases (NC-CDs). NC-CD (eg, obesity, diabetes mellitus, and asthma) is a heterogeneous group of diagnoses that affect 1 or more organ systems, last for prolonged periods of time, and may be either persistent or episodic. In contrast to complex chronic diseases (C-CDs), NC-CDs do not typically result in significant limitations of functional status or quality of life if managed properly.1
Although the epidemiologies of individual conditions that contribute to the NC-CD population are known,2–7 few data assess their cumulative societal impact on health care use and total expenditures.8,9 This is in contrast to the body of work that has detailed the individual and societal impacts of children with C-CDs.10,11 Despite their small population, children with C-CDs have disproportionally high health care use and expenditures.12–17 We hypothesize that children with NC-CDs will individually have less frequent use and lower expenditures than children with C-CDs. However, because of the high prevalence of these conditions, the aggregate NC-CD health care expenditures will approach the aggregate expenditures of the C-CD group.
The remaining children who do not fit the criteria of either NC-CD or C-CD are categorized as children without chronic diseases (WO-CDs). This group includes children who have only had normal well-child visits or brief acute illnesses. We hypothesize that children with NC-CDs will have significantly more frequent use and higher expenditures compared with children WO-CDs.
An improved understanding of children with NC-CDs and their associated health care expenditures is needed to improve health care delivery for this population and may provide opportunities for health policy interventions to reduce costs of care. Therefore, our primary objective was to describe individual and aggregate expenditures attributed to children with NC-CDs in a publicly insured population. Our secondary objective examined health care use patterns. For both objectives, we compared the NC-CD group to the WO-CD and C-CD groups.
Methods
Study Design
We performed a retrospective, cross-sectional analysis of Medicaid enrollees (0–18 years old) from January 2012 through December 2013 using the multistate Truven MarketScan Medicaid Database (Truven Health Analytics, Ann Arbor, MI).18,19 This data set contains de-identified demographic and Medicaid claims data for Medicaid fee for service and Medicaid Managed Care pooled from 7 geographically diverse states. Identification of the individual states is prohibited because of Truven’s data sharing agreement. Continuous Medicaid enrollment improves the accuracy of patient classification and identification of all health care expenditures and use associated with episodic disease. Therefore, children (ages >1 year) who did not maintain continuous enrollment in Medicaid during the study period (24 out of 24 months) were excluded.
Infants (ages <1 year) were included in the study population if they were born and enrolled in Medicaid during 2012. After their initial enrollment, infants who did not maintain continuous enrollment through the remaining study period were excluded. Because birth hospitalizations do not typically represent hospitalization because of illness, birth hospitalizations were excluded from analysis (both expenditure and health care use) if they were determined to be normal newborn care as defined by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes (V30.xx-V37.xx and V39.xx), with a hospital stay of 4 days or fewer. Newborns meeting inclusion criteria were stratified into cohorts by the same criteria as older children.
This study was not considered human subjects research by the Institutional Review Board at Cincinnati Children’s Hospital Medical Center (Cincinnati, OH).
Patient Classification
By using the commercially available Clinical Risk Group (CRG) v. 1.12 software (3M Health Information Systems, Salt Lake City, Utah), all included children were assigned to 1 of 9 mutually exclusive, hierarchical chronicity groups on the basis of their historical medical claims data (ICD-9-CM, Healthcare Common Procedure Coding System, and Current Procedural Terminology codes).14,20,21 This classification algorithm incorporates the severity of both acute and chronic conditions to develop a primary chronic disease that is modified by additional comorbid conditions. By using previously defined criteria,9 we classified children as NC-CD if their CRG group was between 3 and 5. Children with a CRG <3 were considered WO-CD, and CRG groups between 6 and 9 were considered C-CD. The group of children WO-CD includes healthy children with only well-child examinations and those with acute illness such as viral respiratory infections or otitis media. Chronic diseases such as asthma, attention-deficit/hyperactivity disorder, diabetes mellitus, and depression are classified as NC-CD. The C-CD group includes combinations of significant chronic illness, such as asthma and epilepsy, and increasingly complex diagnoses, such as severe neurologic injury or cystic fibrosis (Table 1). We describe demographic characteristics for each group by prevalence, age, sex, race and ethnicity, enrollment in Medicaid Managed Care, and eligibility based on disability.
TABLE 1.
CRG Cohorts Representing Healthy Children, Children With NC-CDs, and Children With C-CDs as Grouped by Their Illness Severity and Chronicity
| WO-CD | NC-CD | C-CD |
|---|---|---|
| CRG 1: healthy | CRG 3: single minor chronic disease | CRG 6: significant chronic disease in 2 organ systems |
| CRG 2: significant acute illness | CRG 4: minor chronic disease in multiple organ systems | CRG 7: dominant chronic disease in ≥3 organ systems |
| CRG 5: episodic and lifelong chronic conditions | CRG 8: hematologic or oncologic malignancy | |
| CRG 9: catastrophic conditions | ||
| Examples: | Examples: | Examples: |
| Well-child examination | Asthma | Asthma and epilepsy |
| Upper respiratory tract infection | Attention-deficit/hyperactivity disorder | Severe neurologic injury |
| Otitis media | Diabetes mellitus | Cystic fibrosis |
| Bronchiolitis | Depression |
Outcomes
Our primary outcomes were medical expenditures reimbursed by Medicaid. A standard payment per unit service was developed by using fee-for-service claims and then applied to both fee-for-service and Medicaid managed care.22 Medical expenses were reported as the annualized aggregate expenditures and the mean per-member per-year (PMPY) expenditures. Annualized aggregate expenditures were calculated by dividing the total expenditure by 2 because of the duration of the study. Calculations were adjusted to account for the actual duration of the enrollment of included infants. Our secondary outcome was the number of health care encounters over the 2-year study period.
Expenditure and Encounter Categorization
Expenditures and encounters were categorized as inpatient, outpatient, or retail pharmacy for all 3 groups. Outpatient health care services were further subcategorized as follows: dental, outpatient laboratory testing, durable medical equipment, emergency department (ED) usage not resulting in admission, home health services, outpatient mental health and/or substance abuse treatment, outpatient therapy (including occupational, physical, and speech therapies), primary care provider visits, specialist and/or nonprimary care visits, and not otherwise specified. Expenditures and use associated with ED visits that resulted in hospital admission were attributed to the in-patient category for that episode of care. If an enrollee received more than 1 outpatient service in a single day, this was recorded as a single visit in the count of health care use, but all resulting expenditures were included.
Statistical Analysis
In addition to descriptive statistics, χ2 tests for association were performed for categorical data, and a Kruskal-Wallis test was performed for continuous data because of non-normally distributed values. For continuous data, multiple comparisons were made by using a Dwass-Steel-Critchlow-Fligner multiple comparison procedure to control for the experiment-wise error rate. All statistical analysis was performed by using SAS 9.4 (SAS Institute, Cary, NC). P values <.05 were considered statistically significant.
Results
Demographics
Of 5 958 242 Medicaid enrollees, 2 424 946 (40.7%) children met continuous Medicaid enrollment criteria (Supplemental Fig 2). One-third of the included children were classified with NC-CDs (35.6%) compared with 53.2% WO-CDs and 11.2% with C-CDs (Table 2).
TABLE 2.
Demographic Characteristics of Children Continuously Enrolled in Truven’s Medicaid MarketScan Database From January 2012 Through December 2013
| Overall | WO-CD (CRG 1–2) | NC-CD (CRG 3–5) | C-CD (CRG 6–9) | |
|---|---|---|---|---|
| Enrollees, N (%) | 2 424 946 | 1 290 744 (53.2) | 862 811 (35.6) | 271 391 (11.2) |
| Age, y (median [IQR]) | 8 (4–12) | 6 (3–11) | 9 (4–13) | 11 (6–15) |
| Race and ethnicity, N (%) | ||||
| White, non-Hispanic | 1 051 066 (43.3) | 539 885 (41.8) | 385 239 (44.6) | 125 942 (46.4) |
| African American, non-Hispanic | 821 409 (33.9) | 449 283 (34.8) | 295 181 (34.2) | 76 945 (28.4) |
| Hispanic | 241 635 (10.0) | 148 308 (11.5) | 76 329 (8.8) | 16 998 (6.3) |
| Other | 310 836 (12.8) | 153 268 (11.9) | 106 062 (12.3) | 51 506 (19.0) |
| Sex, N (%) | ||||
| Male | 1 230 152 (50.7) | 610 303 (47.3) | 467 678 (54.2) | 152 171 (56.1) |
| Female | 1 194 794 (49.3) | 680 441 (52.7) | 395 133 (45.8) | 119 220 (43.9) |
| Managed care, N (%) | 1 564 015 (64.5) | 871 245 (67.5) | 559 817 (64.9) | 132 953 (49.0) |
| Eligible for Medicaid because of disability, N (%) | 152 707 (6.3) | 19 634 (1.5) | 56 338 (6.5) | 76 735 (28.3) |
All comparisons are significant at the P < .001 level by the Kruskal-Wallis test.
The median age for children with NC-CDs was 9 years (interquartile range [IQR] 4–13); children WO-CDs were generally younger (6 years, IQR 3–11), and children with C-CDs were older (11 years, IQR 6–15). Most enrollees (64.5%) participated in Medicaid Managed Care, including the majority of children with NC-CDs (64.9%). Rates of eligibility for Medicaid because of disability were significantly lower in children with NC-CDs (6.5%) compared with C-CDs (28.3%) (Table 2).
Expenditures
The annual expenditures for the entire cohort was $7 226 354 620 over the study period, or $3037 PMPY (Supplemental Table 5). Children with NC-CDs accounted for 35.6% of the study population and 33.1% of the annualized aggregate expenditure. Children WO-CDs accounted for 53.2% of the study population and 20.0% of annualized aggregate expenditure. Children with C-CDs accounted for 11.2% of the study population and 46.9% of the annualized aggregate expenditure (Fig 1).
FIGURE 1.
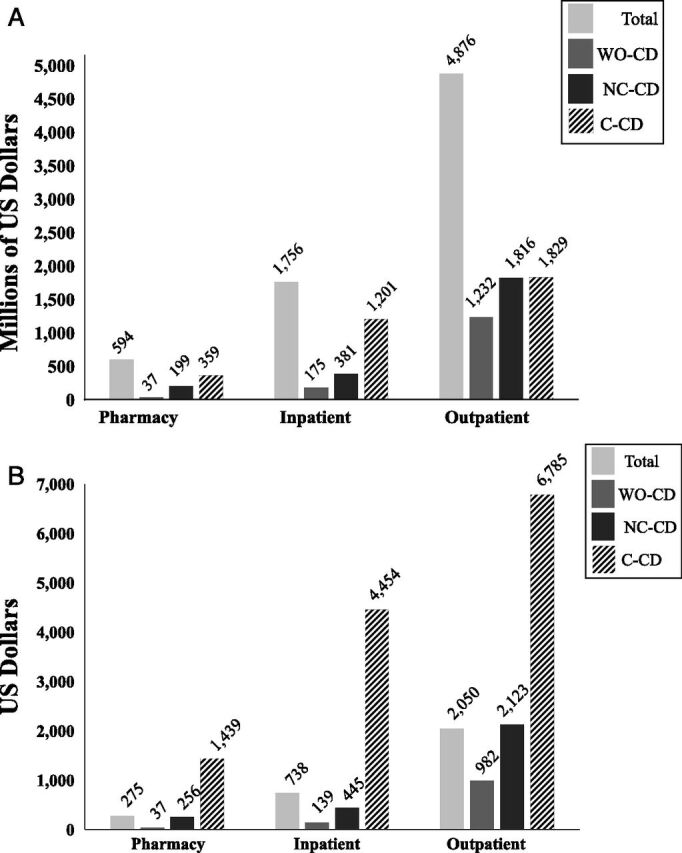
A, Annualized spending (in US dollars, millions) from January 1, 2012, to December 31, 2013, for children WO-CDs, with NC-CDs, and with C-CDs by use type. B, PMPY spending (in US dollars) from January 1, 2012, to December 31, 2013, for children WO-CDs, with NC-CDs, and with C-CDs by use type.
The total PMPY expenditure, our primary outcome, for children with NC-CDs ($2801) was significantly higher than children WO-CDs ($1151) and lower than children with C-CDs ($12 569). For both comparisons, P < .001 (Fig 1).
Inpatient
The inpatient PMPY expenditure for children with NC-CDs ($445, 15.9% of total PMPY) was higher than expenditures for children WO-CDs ($139, 12.1% of total PMPY) and lower than expenditures for children with C-CDs ($4454, 35.4% of total PMPY) (Fig 1). For both comparisons, P < .001.
Retail Pharmacy
Pharmacy expenditure, including all outpatient retail and mail order pharmacy expenditures, accounted for the smallest proportion of health care expenditures for all groups. Pharmacy PMPY for children with NC-CDs was $256 (9.1% of total PMPY). By comparison, children WO-CDs had lower expenditures ($37, 3.2% of total PMPY), and children with C-CDs had higher expenditures ($1439, 11.4% of total PMPY). For both comparisons, P < .001 (Fig 1).
Outpatient
Outpatient expenditure was the largest contributor to PMPY expenditures for all cohorts. Outpatient PMPY for children with NC-CDs was $2123 (75.8% of total PMPY). Similarly, outpatient PMPY for children WO-CDs was significantly lower ($982, 85.3% of total PMPY), whereas outpatient PMPY for children with C-CDs was significantly greater ($6758, 54.0% of total PMPY). For both comparisons, P < .001 (Fig 1).
Outpatient Expenditures by Subcategory
In all subcategories of outpatient care, children with NC-CDs had higher expenditures compared with children WO-CDs and lower expenditures than children with C-CDs (Table 3). PMPY expenditures for dental (WO-CD $185, NC-CD $223, and C-CD $231 PMPY) and primary care (WO-CD $259, NC-CD $280, and C-CD $367 PMPY) had the smallest relative difference between groups, and all comparisons were significant (P < .001). Expenditures for outpatient mental health and/or substance abuse treatment had the largest relative difference between groups (WO-CD $41, NC-CD $664, and C-CD $2565 PMPY; P < .001).
TABLE 3.
Outpatient Spending by Subcategory in PMPY Mean Values
| Overall ($) | WO-CD (CRG 1–2) ($) | NC-CD (CRG 3–5) ($) | C-CD (CRG 6–9) ($) | |
|---|---|---|---|---|
| Outpatient PMPY | 2050 | 982 | 2123 | 6785 |
| Mental health and substance abuse | 551 | 41 | 664 | 2565 |
| Specialist, nonprimary care provider | 329 | 119 | 254 | 1545 |
| Primary care provider | 278 | 259 | 280 | 367 |
| ED | 205 | 146 | 227 | 407 |
| Dental | 204 | 185 | 223 | 231 |
| Therapy, treatment | 187 | 76 | 201 | 661 |
| Testing | 150 | 97 | 149 | 399 |
| Outpatient, NOS | 53 | 25 | 50 | 191 |
| Durable medical equipment | 43 | 24 | 45 | 121 |
| Home health | 25 | 1 | 8 | 190 |
All comparisons are significant at the P < .001 level by the Kruskal-Wallis test. NOS, not otherwise specified.
Health Care Use
There were statistically significant differences in health care use over the 2-year study period comparing the median number of health care encounters and pharmacy prescriptions (our secondary outcome) between children with NC-CDs, WO-CDs, and with C-CDs (Table 4).
TABLE 4.
Rates of Health Care Use, Median Number of Visits by Use Type, and Median Number of Outpatient Medication Prescriptions From January 1, 2012, to December 31, 2013
| WO-CD (CRG 1–2) | NC-CD (CRG 3–5) | C-CD (CRG 6–9) | |
|---|---|---|---|
| Inpatient | |||
| Users, N (%) | 35 114 (2.7) | 58 135 (6.7) | 56 134 (20.7) |
| Median (IQR) inpatient days among patients with claims | 3 (2–5) | 3 (2–6) | 5 (2–14) |
| Pharmacy | |||
| Median (IQR) prescription medications filled | 2 (0–4) | 6 (2–12) | 16 (7–33) |
| Outpatient | |||
| Users, N (%) | 1 243 732 (96.5) | 858 004 (99.5) | 270 932 (99.8) |
| Median (IQR) visits | 8 (5–13) | 15 (10–25) | 34 (19–72) |
| Mental health and substance abuse | |||
| Users, N (%) | 106 910 (8.3) | 349 802 (40.5) | 180 723 (66.6) |
| ED | |||
| Users, N (%) | 588 412 (45.6) | 473 526 (54.9) | 174 024 (64.1) |
All comparisons are significant at the P < .001 level by the Kruskal-Wallis test.
Inpatient
Over the 2-year period, 6.7% of children with NC-CDs had an inpatient admission. Children WO-CDs were less likely to have an inpatient admission (2.7%), and children with C-CDs were more likely to have an admission (20.7%; both P < .001). Of those with an admission, the median length of stay for children with NC-CDs was 3 days (IQR 2–6). The length of stay was shortest for children WO-CDs (median 3, IQR 2–5) and longest for children with C-CDs (median 5, IQR 2–14). For both comparisons, P < .001. In other words, 25% of children admitted WO-CDs stayed in the hospital for at least 5 days versus the 6 days for children admitted with NC-CDs.
Pharmacy
The median number of outpatient medication prescriptions filled for children with NC-CDs was 6 (IQR 2–12). In comparison, 2 were filled for children WO-CDs (IQR 0–4), and 16 were filled for children with C-CDs (IQR 7–33; both P < .001).
Outpatient
Nearly all enrollees (98%) had at least 1 outpatient health care encounter during the 2-year study period. The median number of outpatient health care encounters for children with NC-CDs was 15, (IQR 10–25). Children WO-CDs had a median of 8 outpatient visits (IQR 5–13), and children with C-CDs had a median of 34 visits (IQR 19–72; both P < .001). In the 2-year study period, 54.9% of children with NC-CDs had at least 1 ED visit not associated with an inpatient admission. By comparison, 45.6% of children WO-CDs and 64.1% of children with C-CDs had at least 1 visit. For both comparisons, P < .001.
Discussion
Children with NC-CDs have significantly higher PMPY and annualized expenditures compared with children WO-CDs. As we hypothesized, the PMPY expenditures for children with NC-CDs ($2801) was significantly less than that of children with C-CDs ($12 569), but the annual aggregate expenditure for the NC-CD group represents a substantial cost because of the high prevalence of these conditions. Although outpatient use accounted for a majority of the expenditures for all cohorts, mental health services and outpatient pharmacy contributed to the large differences among cohorts for both expenditures and use, whereas primary care expenditures were only modestly different.
Our study highlights the high cost of care required for children with NC-CDs and provides evidence of the significantly greater prevalence of these conditions compared with C-CDs. Focusing efforts to reduce expenditures on the group of children with NC-CDs may be more successful than targeting the C-CD group because of the high prevalence of NC-CDs, and many conditions associated with this group are considered ambulatory sensitive (eg, attention-deficit/hyperactivity disorder, asthma, depression, and obesity).23 Smaller, individual reductions in expenditures among children with NC-CDs would cumulatively result in a larger total savings than an equal dollar amount reduction per person in the cohort of children with C-CDs. For example, a $100 reduction in the PMPY expenditures for children with NC-CDs would correlate to savings of ∼$86 million per year in our study. Extrapolating to the 35 million children in Medicaid, this reduction would result in $1.25 billion in national savings annually. In contrast, the same savings would require a reduction of $318 PMPY by children with C-CDs.
Ideally, the presence of a chronic illness would result in substantially more primary care visits for the management of both acute and chronic problems; yet, we found there were only modest differences in outpatient spending attributed to primary care visits between the groups. Furthermore, our study demonstrates larger differences in expenditures between the groups for urgent and emergency care. These findings are consistent with previous reporting of limited primary care spending for children enrolled in Medicaid, and “spending on primary care rises modestly compared with other health services” among children with high resource use.22 Because of the ambulatory nature of the conditions in the NC-CD group, increased primary care use may prevent more expensive urgent care and ED use.15 Unlike children with C-CDs, who frequently establish their medical home at hospital-based academic medical centers, we expect broader community access for children with NC-CDs. Children with chronic illnesses may gain the most benefit from comprehensive care coordination and managed care; yet, the NC-CD and C-CD groups were less likely to participate in Medicaid Managed Care than children WO-CDs. Wider implementation of managed care that emphasizes care coordination and increased emphasis on the primary care physician as a medical home for the pediatric Medicaid population with chronic illnesses may result in improved health and limit the growth of health care expenditures.24–27
We found higher mental health care expenditures and use for children with NC-CDs and C-CDs (Table 3) when compared with children WO-CDs, which is similar to previous reports.22,28,29 Children with a primary diagnosis of mental health disorders that independently result in higher CRG classification and children with chronic physical conditions with comorbid mental health disorders are likely both captured in the NC-CD and C-CD groups.30 Both groups result in increased expenditures and use. For instance, anxiety and mood disorders comorbid to pediatric and adolescent asthma are associated with increases in use, expenditures, and self-reported symptoms compared with those without mental illness.31–33 Integrating mental health services within the primary medical home may help improve access and reduce disparities that are present among children with NC-CDs and C-CDs.34
Finally, we note that children with C-CDs and NC-CDs are older than children WO-CDs, which is consistent with reports of both increasing medical complexity and high resource use.10,22,28,35 Certainly, some of the difference in age is due to the advancement of diseases and life-prolonging therapies. However, the increased age for children with NC-CDs and C-CDs may reflect the accumulation of specific diagnoses that affect classification but may not represent true progression of diseases.
Our findings should be interpreted in the context of several limitations. First, the study population included only those enrolled in Medicaid. Our outcomes of expenditures and use reflect both access to and reimbursement for services provided by Medicaid. Limitations in coverage for services, including durable medical equipment and mental health services, may prevent these results from being generalizable to all payer populations. Our large sample size is likely to be representative of the 35 million publicly insured children nationally.36 The annual aggregate expenditures for the care of children with NC-CDs represents a significant societal cost, extrapolating our study results to national pediatric Medicaid expenditures results in ∼$34.9 billion in annual spending. Second, although the Truven MarketScan Medicaid database aggregates de-identified data from 7 geographically diverse states, this large sample does not ensure that our study population is a representative sample of the national Medicaid population. Third, we excluded 59% of our study population for not maintaining continuous Medicaid enrollment over the 2-year study period. Although the 2-year period of continuous enrollment improved accuracy of patient classification, this inclusion criterion may have created a bias toward children with chronic illness. Families of children with chronic illnesses requiring increased health care use may have a financial incentive to maintain enrollment and, therefore, be more risk averse to lapses in insurance coverage than families of children WO-CDs. Fourth, although the classification method has previously demonstrated good to excellent specificity in identifying children WO-CDs, with NC-CDs, and with C-CDs by using CRGs in a full 3 years of Medicaid data, there is a risk of misclassification of patient complexity when using the CRG algorithm.14 As with any classification system based on billing encounters, only those who have encounters that code a chronic condition will be identified as such. Thus, children with well-controlled chronic conditions that may not result in health care use, such as developmental delay or learning disorders, may be undercounted.14 Fifth, some members of CRG-6 (included in the C-CD group) may not be complex and may have similarities with the NC-CD group. Our study design was intended to exclude children with complexity from the NC-CD group; thus, the prevalence and use of the NC-CD group may be greater than reported. Finally, our data set did not allow for the assessment of qualified medical home penetrance among our population. Therefore, we are unable to make a clear assessment of the potential benefit of this intervention.
Conclusions
The percentage of children enrolled in Medicaid with NC-CDs is substantial (35.6%). The group of children with NC-CDs requires expensive care, accounting for 33% of Medicaid pediatric expenditures. The majority of these expenditures take place in the outpatient setting, with these children having a median of 15 outpatient encounters over the 2-year study period. Extrapolating to the 35 million children with Medicaid nationally, the NC-CD population accounts for $34.9 billion in annual Medicaid spending. Given the high prevalence of children with NC-CDs, it would require a smaller PMPY reduction in the NC-CD population compared with children with C-CDs to achieve similar results.
Supplementary Material
Glossary
- C-CD
complex chronic disease
- CRG
Clinical Risk Group
- ED
emergency department
- IQR
interquartile range
- NC-CD
noncomplex chronic disease
- PMPY
per member per year
- WO-CD
without chronic disease
Footnotes
Drs Hoefgen and Auger conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript; Drs Andrews, Hall, Neff, Macy, Bettenhausen, and Shah conceptualized and designed the study and reviewed and revised the manuscript; Dr Richardson conceptualized and designed the study, conducted the initial analyses, and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FUNDING: Dr Auger's research is funded by a grant from the Agency for Healthcare Research and Quality (K08-HS024735-01A1).
References
- 1.Simon TD, Cawthon ML, Stanford S, et al. ; Center of Excellence on Quality of Care Measures for Children with Complex Needs (COE4CCN) Medical Complexity Working Group . Pediatric medical complexity algorithm: a new method to stratify children by medical complexity. Pediatrics. 2014;133(6). Available at: www.pediatrics.org/cgi/content/full/133/6/e1647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akinbami LJ, Simon AE, Rossen LM. Changing trends in asthma prevalence among children. Pediatrics. 2016;137(1):1–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cizza G, Brown RJ, Rother KI. Rising incidence and challenges of childhood diabetes. A mini review. J Endocrinol Invest. 2012;35(5):541–546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pulgaron ER, Delamater AM. Obesity and type 2 diabetes in children: epidemiology and treatment. Curr Diab Rep. 2014;14(8):508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Froehlich TE, Lanphear BP, Epstein JN, Barbaresi WJ, Katusic SK, Kahn RS. Prevalence, recognition, and treatment of attention-deficit/hyperactivity disorder in a national sample of US children. Arch Pediatr Adolesc Med. 2007;161(9):857–864 [DOI] [PubMed] [Google Scholar]
- 6.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee JM, Sundaram V, Sanders L, Chamberlain L, Wise P. Health care utilization and costs of publicly-insured children with diabetes in California. J Pediatr. 2015;167(2):449–454.e6 [DOI] [PubMed] [Google Scholar]
- 8.Roehrig C. Mental disorders top the list of the most costly conditions in the United States: $201 billion. Health Aff (Millwood). 2016;35(6):1130–1135 [DOI] [PubMed] [Google Scholar]
- 9.Neff JM, Clifton H, Popalisky J, Zhou C. Stratification of children by medical complexity. Acad Pediatr. 2015;15(2):191–196 [DOI] [PubMed] [Google Scholar]
- 10.Newacheck PW, Strickland B, Shonkoff JP, et al. An epidemiologic profile of children with special health care needs. Pediatrics. 1998;102(1, pt 1):117–123 [DOI] [PubMed] [Google Scholar]
- 11.Burns KH, Casey PH, Lyle RE, Bird TM, Fussell JJ, Robbins JM. Increasing prevalence of medically complex children in US hospitals. Pediatrics. 2010;126(4):638–646 [DOI] [PubMed] [Google Scholar]
- 12.Berry JG, Hall M, Hall DE, et al. Inpatient growth and resource use in 28 children’s hospitals: a longitudinal, multi-institutional study. JAMA Pediatr. 2013;167(2):170–177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agrawal R, Smith T, Li Y, Cartland J. Rate of spending on chronic conditions among Medicaid and CHIP recipients. Pediatrics. 2014;134(1). Available at: www.pediatrics.org/cgi/content/full/134/1/e80 [DOI] [PubMed] [Google Scholar]
- 14.Neff JM, Sharp VL, Muldoon J, Graham J, Myers K. Profile of medical charges for children by health status group and severity level in a Washington State Health Plan. Health Serv Res. 2004;39(1):73–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berry JG, Hall M, Neff J, et al. Children with medical complexity and Medicaid: spending and cost savings. Health Aff (Millwood). 2014;33(12):2199–2206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen E, Berry JG, Camacho X, Anderson G, Wodchis W, Guttmann A. Patterns and costs of health care use of children with medical complexity. Pediatrics. 2012;130(6). Available at: www.pediatrics.org/cgi/content/full/130/6/e1463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peltz A, Hall M, Rubin DM, et al. Hospital utilization among children with the highest annual inpatient cost. Pediatrics. 2016;137(2):e20151829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mark TL, Axelsen KJ, Mucha L, Sadkova Y. Racial differences in switching, augmentation, and titration of lipid-lowering agents by Medicare/Medicaid dual-eligible patients. Am J Manag Care. 2007;13(suppl 3):S72–S79 [PubMed] [Google Scholar]
- 19.Amendah DD, Grosse SD, Bertrand J. Medical expenditures of children in the United States with fetal alcohol syndrome. Neurotoxicol Teratol. 2011;33(2):322–324 [DOI] [PubMed] [Google Scholar]
- 20.Hughes JS, Averill RF, Eisenhandler J, et al. Clinical Risk Groups (CRGs): a classification system for risk-adjusted capitation-based payment and health care management. Med Care. 2004;42(1):81–90 [DOI] [PubMed] [Google Scholar]
- 21.Neff J, Clifton H, Park KJ, et al. Identifying children with lifelong chronic conditions for care coordination by using hospital discharge data. Acad Pediatr. 2010;10(6):417–423 [DOI] [PubMed] [Google Scholar]
- 22.Kuo DZ, Hall M, Agrawal R, et al. Comparison of health care spending and utilization among children with Medicaid insurance. Pediatrics. 2015;136(6). Available at: www.pediatrics.org/cgi/content/full/136/6/1521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lu S, Kuo DZ. Hospital charges of potentially preventable pediatric hospitalizations. Acad Pediatr. 2012;12(5):436–444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mosquera RA, Avritscher EB, Samuels CL, et al. Effect of an enhanced medical home on serious illness and cost of care among high-risk children with chronic illness: a randomized clinical trial. JAMA. 2014;312(24):2640–2648 [DOI] [PubMed] [Google Scholar]
- 25.Raphael JL, Cooley WC, Vega A, et al. Outcomes for children with chronic conditions associated with parent- and provider-reported measures of the medical home. J Health Care Poor Underserved. 2015;26(2):358–376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baker LC, Afendulis C. Medicaid managed care and health care for children. Health Serv Res. 2005;40(5, pt 1):1466–1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Healy-Collier K, Jones WJ, Shmerling JE, Robertson KR, Ferry RJ Jr. Medicaid managed care reduces readmissions for youths with type 1 diabetes. Am J Manag Care. 2016;22(4):250–256 [PubMed] [Google Scholar]
- 28.Kuo DZ, Melguizo-Castro M, Goudie A, Nick TG, Robbins JM, Casey PH. Variation in child health care utilization by medical complexity. Matern Child Health J. 2015;19(1):40–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agrawal R, Hall M, Cohen E, et al. Trends in health care spending for children in Medicaid with high resource use. Pediatrics. 2016;138(4):e20160682. [DOI] [PubMed] [Google Scholar]
- 30.Neff JM, Sharp VL, Muldoon J, Graham J, Popalisky J, Gay JC. Identifying and classifying children with chronic conditions using administrative data with the clinical risk group classification system. Ambul Pediatr. 2002;2(1):71–79 [DOI] [PubMed] [Google Scholar]
- 31.Richardson LP, Lozano P, Russo J, McCauley E, Bush T, Katon W. Asthma symptom burden: relationship to asthma severity and anxiety and depression symptoms. Pediatrics. 2006;118(3):1042–1051 [DOI] [PubMed] [Google Scholar]
- 32.Richardson LP, Russo JE, Lozano P, McCauley E, Katon W. The effect of comorbid anxiety and depressive disorders on health care utilization and costs among adolescents with asthma. Gen Hosp Psychiatry. 2008;30(5):398–406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sztein DM, Lane WG. Examination of the comorbidity of mental illness and somatic conditions in hospitalized children in the United States using the kids’ inpatient database, 2009. Hosp Pediatr. 2016;6(3):126–134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Njoroge WF, Hostutler CA, Schwartz BS, Mautone JA. Integrated behavioral health in pediatric primary care. Curr Psychiatry Rep. 2016;18(12):106. [DOI] [PubMed] [Google Scholar]
- 35.Simon TD, Berry J, Feudtner C, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Department of Health and Human Services . Medicaid & CHIP: April 2016 monthly applications, eligibility determinations and enrollment report. 2016. Available at: https://www.medicaid.gov/medicaid/program-information/downloads/june-2016-enrollment-report.pdf. Accessed July 27, 2016
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


