Abstract
Lyme borreliosis is the object of numerous misconceptions. In this review, we revisit the fundamental manifestations of neuroborreliosis (meningitis, cranial neuritis, and radiculoneuritis), as these have withstood the test of time. We also discuss other manifestations that are less frequent. Stroke, as a manifestation of Lyme neuroborreliosis, is considered in the context of other infections. The summary of the literature regarding clinical outcomes of neuroborreliosis leads to its controversies. We also include new information on pathogenesis and on the polymicrobial nature of tick-borne diseases. In this way, we update the review that we wrote in this journal in 1995.
Lyme disease is caused by species of the genus Borrelia (B. burgdorferi, B. garinii, and B. afzelii) (Fig) and is transmitted by ticks of the genus Ixodes. Lyme disease was named for the place where it was first described in the USA, but this disorder was known in Europe for a long time as a dermatological and neurological illness in contrast to the original rheumatological presentation in the USA. The public health burden of tick-borne pathogens continues to grow substantially.1 The Centers for Disease Control and Prevention (CDC) reports approximately 30,000 cases of Lyme disease per year but estimates that the true incidence is higher.2
FIGURE 1:
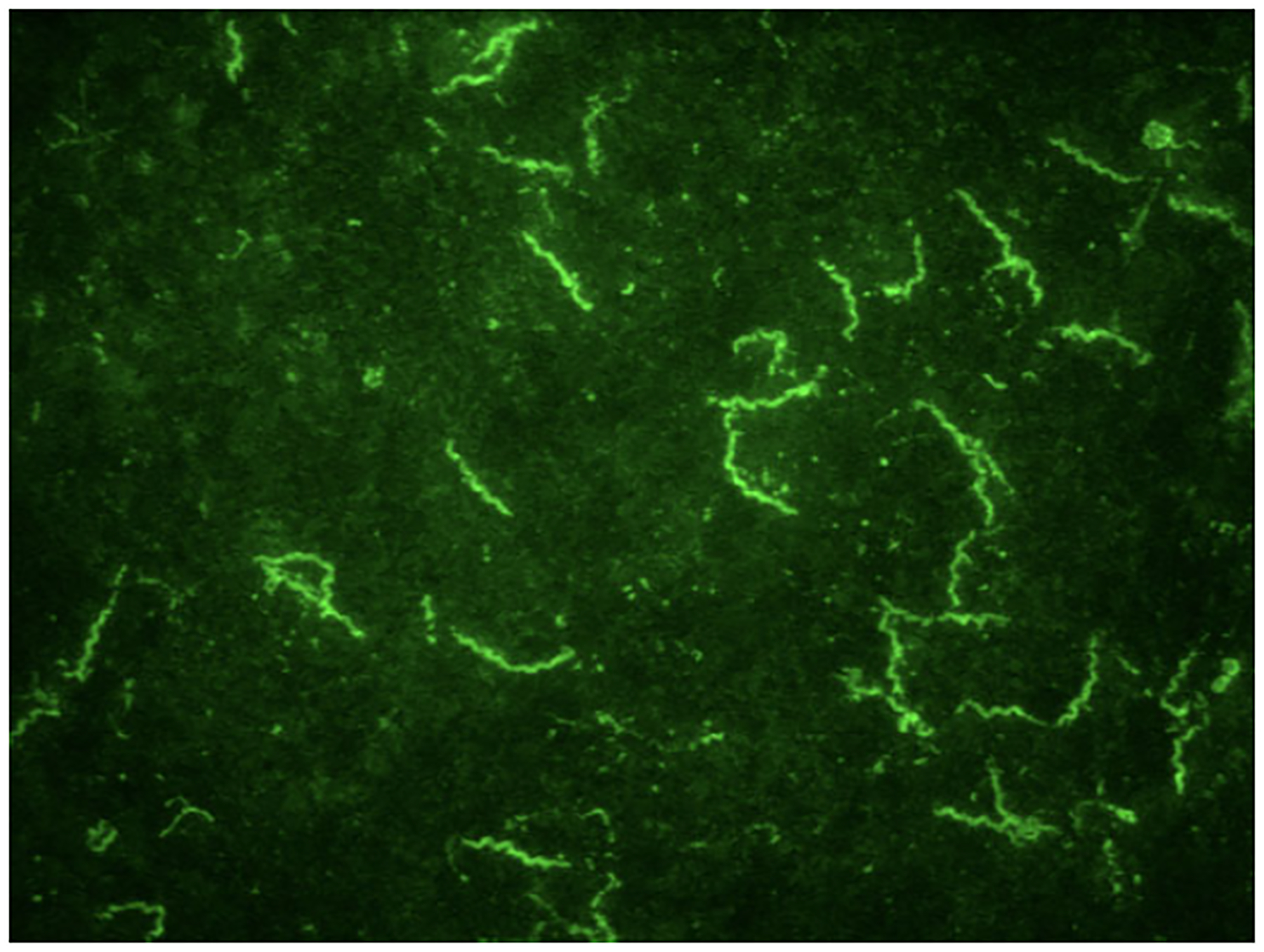
Cultured Borrelia burgdorferi stained with an IgG murine antibody to OspA followed by fluorescein isothiocyanate–labeled goat antimurine Ig; 1 cm = 5 μm.
Clinical Manifestations
The clinical course of Lyme disease is variable and begins with a skin lesion, erythema migrans, several days after a tick bite. Neurological, cardiac, chronic skin, or articular involvement develops later.3 Neurological impairment can be classified according to the location of the lesion within the neuraxis or to the time course of the disease. A chronological approach, although not always consistent, has a bearing on laboratory diagnosis. A clinical consensus currently divides Lyme disease into an acute localized (erythema migrans) and a disseminated stage, with the latter divided into early and late phases. Neurological disturbances can appear at any time within the disseminated stage and both the central nervous system (CNS) and peripheral nervous system (PNS) can be involved.4
Early Disseminated Infection
In 1922, Garin and Bujadoux described, in France, a patient with meningoradiculitis after an erythema migrans following a tick bite. Although they suspected a tick palsy, this was the first report of what we now know as Lyme neuroborreliosis (LNB). Some years later, Bannwarth described in Germany a series of patients with a similar disorder, which was recognized in Europe as Garin–Bujadoux–Bannwarth or Bannwarth syndrome.
The clinical presentations of LNB have been reviewed by us and others,5–10 but there are new population-based studies that merit mention. In a retrospective series of 431 patients with LNB from Denmark, the most common clinical manifestations were painful radiculitis (65.9%), cranial palsy (43.4%; mostly facial palsy), and headache (28.3%),11 and they all had evidence of intrathecal synthesis of antibodies. The vast majority of patients improved significantly upon antibiotic therapy within the first 4 weeks. Only 14 patients (3.2%) reported no response. This study showed similar clinical findings to those reported in Germany by Ackermann et al nearly 35 years ago in a series of 100 consecutive patients with LNB.12
Patients with Bannwarth syndrome usually have severe, migrating radicular pain that can be accompanied by peripheral nerve paresis, often combined with uni- or bilateral (one-third of cases) facial palsy, cerebrospinal fluid (CSF) pleocytosis, and a course lasting 3 to 5 months. Some patients may initially be diagnosed as having a herniated disc. Meningeal or encephalitic features are infrequent, although occasionally a confusional state and signs of CNS dysfunction such as Babinski sign may be present.6,13 Pain disappears after antibiotic treatment; however, the disorder resolves spontaneously in 5 to 6 months without therapy.14 The distribution of peripheral nerve damage is variable, in the form of single or multiple radiculitis, mononeuritis multiplex, or plexitis. Most patients with radiculitis and facial palsy have neurophysiological evidence of more widespread peripheral nerve damage, consistent with axonal injury.15,16 Nerve biopsy specimens show mononuclear cell infiltration of the vasa nervorum without evidence of necrosis of the vessel walls.15 A recent European series of 77 patients with meningoradiculitis found fewer pretreatment neurological complications than reported for Bannwarth syndrome decades ago, probably as the result of earlier recognition and prompt antibiotic treatment.17
Although these manifestations also occur in patients in the USA, where 5 cases of Bannwarth syndrome were recently reported,18 lymphocytic meningitis is the most common single, early manifestation in North America. Headache is the main complaint, and fever and meningism are mild or absent. In untreated patients, recurrent attacks of meningitis may alternate with periods of remission. CSF analysis shows lymphocytic mononuclear cell pleocytosis,4 sometimes with atypical features, resembling lymphoma.19,20 B. burgdorferi–specific oligoclonal bands can be demonstrated, usually after 4 weeks of disease, as well as intrathecal synthesis of specific antibodies.21
Less frequent manifestations have been included in Supplementary Table 1 and are grouped under the appropriate neurological disorders. They involve the CNS and PNS and may mimic other disorders (ie, herniated disc, neoplasia). Some conditions have a clear association to LNB, such as intracranial hypertension in children, and myelitis or plexitis, but the evidence of a clear link to other conditions is not compelling, such as classic motor neuron disease or dementia.
In reviewing the less frequent manifestations of LNB, it became apparent that ischemic stroke or transient ischemic attack, likely secondary to infection-induced cerebral endarteritis,22 has been reported in a number of patients (Supplementary Table 2). Pathogenic mechanisms may be shared with syphilis and tuberculosis, where stroke is a well-known complication. Interestingly, an almost identical pattern of basilar artery enhancement on magnetic resonance imaging has been described in a child23 with LNB and in an adult with syphilis,24 in both cases suggesting infectious vasculitis. Other infections may also complicate with stroke,25 and thus suggest a common mechanism of pathogenesis. Patients with stroke without evident vascular risk factors, particularly those living in endemic areas or exposed to ticks, should be screened in serum and CSF for Lyme disease to start a proper antibiotic therapy when indicated.
Optic nerve involvement is an overlooked aspect of LNB and can have significant morbidity. Optic neuropathy may occur, although it is rare.26 A few cases of retrobulbar optic neuritis, papillitis, neuroretinitis, and ischemic optic neuropathy have been reported. Papilledema secondary to raised intracranial pressure in Lyme meningitis occurs in children, with a few adult cases reported. The main difficulty has been to prove causality in endemic areas, where prevalence of asymptomatic seropositivity to Borrelia is high. In a large retrospective review of 440 cases of optic neuropathy, 28 (6.4%) of the patients had reactive Lyme serologies.27 Among those, there was enough evidence to strongly associate the optic neuropathy to LNB in only 5 of the cases of papilledema and 1 case of papillitis.
Late Disseminated Disease
PNS Involvement.
Peripheral neuropathy in Europe has been associated with a chronic skin disorder, acrodermatitis chronica atrophicans,28 an infrequent condition in the United States. Predominantly sensory, it can be patchy or diffuse, and paresthesias or hypoesthesia are the leading symptoms. The neuropathy tends to follow the topographical distribution of the skin disease, although nonaffected extremities may also show signs of neuropathy. Nerve biopsy specimens show similar changes to those reported in meningoradiculitis, and CSF parameters can be normal.
The presence of a chronic, stocking–glove neuropathy, possibly due to a mononeuropathy multiplex, was described in 2 series of patients with late LNB in the United States in the early 1990s29,30 but is less common than initially thought.31 Patients most often complain of distal paresthesias, neurophysiology is consistent with large axonal fiber dysfunction, and the scarce neuropathologic information from sural biopsies has shown minimal changes.32 The type of nerve damage in peripheral neuropathy and meningoradiculitis appears to be similar on clinical, pathological, and neurophysiological grounds, suggesting a common disorder, perhaps with different expression in intensity and pattern of distribution, but with a common underlying pathogenic mechanism.
CNS Involvement.
Months to years after disease onset, chronic encephalomyelitis, a term coined by Ackermann in Germany in 1985, may appear.33 The precise onset of the infection was difficult to determine in this series, because some of the patients did not remember other manifestations consistent with borreliosis. Only 4 of 44 patients reported meningoradiculitis 9 months to 5 years before. Spinal or cerebral symptoms and signs predominate. Patients present with spastic paraparesis; ataxia; cranial nerve palsies, most commonly facial palsy and deafness; bladder dysfunction; and cognitive impairment of variable severity.
This chronic involvement of the CNS that is responsive to antibiotics represents a controversial feature of LNB. Its diagnosis requires an inflammatory CSF together with intrathecal synthesis of antibodies to B. burgdorferi.9,34 North American patients can also develop parenchymal CNS disease with variable illness severity.35 A diffuse encephalopathy, clinically characterized by memory problems together with a variety of cognitive dysfunctions, may occur in patients with clear evidence of Lyme disease.36 It should be stressed, however, that this condition is nonspecific, appears in patients with other infectious or metabolic disorders, and is not indicative of active infection, as indicated by the lack of CSF pleocytosis and intrathecal antibody production. Therefore, this condition does not respond to prolonged antibiotic therapy. Several controlled studies reported a comparable frequency of symptoms in patients and controls.37,38
Diagnosis
Laboratory diagnosis of infection with B. burgdorferi is done by detection of antibodies in a 2-tiered approach initially using an enzyme-linked immunoassay (EIA; whole cell lysate) followed by a Western blot to confirm the results. The immunoblot requires at least 2 of 3 signature bands for a positive IgM, and 5 of 10 signature bands for a positive IgG. Two-tier testing is not sensitive for early Lyme disease, so a negative result does not rule out infection with B. burgdorferi. Sensitivity improves with development of disseminated disease.39,40 These recommendations apply to infection acquired in the United States, because other species within the B. burgdorferi sensu lato complex can cause disease in Europe and Asia.41 Whereas most patients with erythema migrans are seronegative, most patients with neuroborreliosis should be seropositive. In addition, the demonstration of intrathecal synthesis of antibodies against B. burgdorferi in the CSF has been considered a gold standard for the diagnosis of CNS infection in Europe, where B. garinii is the species most often associated with neurologic disease. Evidence of intrathecal antibody production has been found in approximately 90% of patients with acute neuroborreliosis,42 although sensitivity may not exceed 50% in more chronic syndromes.43 Intrathecal production may persist for a long time after successful therapy.
The C6 peptide, a 26-amino-acid peptide derived from an invariant region of the lipoprotein VlsE, has been employed as the substrate for an EIA with similar sensitivity but higher specificity, as the C6 peptide, being a molecular subunit, does not cause cross-reactions. C6 peptide can also be used in European patients, as it detects responses elicited by other Borrelia genospecies.41 In some laboratories, the C6 peptide assay is replacing the whole cell EIA.40,44 A decline in the C6 antibody titer has been associated with successful antibiotic therapy.44
Treatment
The evidence-based recommendations on the treatment of LNB by a panel of the American Academy of Neurology concluded that it can be treated in adults and children with intravenous penicillin, ceftriaxone, or cefotaxime (level B recommendation). Several European studies support the use of oral doxycycline in adults with meningitis, cranial neuritis, and radiculitis (level B), reserving parenteral regimens for patients with parenchymal CNS involvement, other severe neurologic symptomatology, or failure to respond to oral regimens. They did not find compelling evidence that prolonged treatment with antibiotics has any beneficial effect in post-Lyme syndrome (level A).45
Most studies have employed 10 to 14 days of therapy with good results, although up to 28 days can be recommended with CNS involvement. The recommended regimens include intravenous (IV) penicillin (20 million U daily), IV ceftriaxone (2–4g daily), IV cefotaxime (2g every 8 hours), and oral doxycycline (200mg daily for 2 days and 100mg daily for 8 days). Doxycycline should be avoided in women who are pregnant or breastfeeding, and in children younger than 8 years. We have summarized the diagnosis and treatment recommendations in tabular form (Table 1).
TABLE 1.
Diagnosis and Treatment of Lyme Neuroborreliosis
| Diagnosis | Two-tiered approach uses an EIA as a screening test and a Western blot to confirm the results. The immunoblot requires signature bands for a positive IgM and IgG response. These recommendations apply to infection acquired in the United States. The C6 peptide, a 26-amino-acid peptide, has been employed as the substrate for an EIA with similar sensitivity but higher specificity, and may be in greater use in the future.39,41 Most patients with erythema migrans are seronegative, but as disease progresses, most patients with neuroborreliosis should be seropositive. Demonstration of intrathecal synthesis of antibodies against the appropriate Borrelia species in the CSF is a gold standard for the diagnosis of CNS infection in Europe.41,42 |
| Treatment | The evidence-based recommendations on the treatment of Lyme neuroborreliosis by a panel of the American Academy of Neurology for adults and children included IV penicillin (20 million U daily), IV ceftriaxone (2–4g daily), IV cefotaxime (2g every 8 hours), and oral doxycycline (200mg daily for 2 days and 100mg daily for 8 days). Several European studies support the use of oral doxycycline in adults with meningitis, cranial neuritis, and radiculitis (level B), reserving parenteral regimens for patients with parenchymal CNS involvement and other severe neurologic symptoms failing to respond to oral regimens. Prolonged treatment with antibiotics does not have a beneficial effect in post-Lyme syndrome (level A).45 |
CNS = central nervous system; CSF = cerebrospinal fluid; EIA = enzyme-linked immunoassay.
Outcomes
We examined and summarized 34 studies that report on long-term outcomes of LNB (Supplementary Table 3). This table was arranged in chronological order with the most recent studies first. These studies have followed American and European patients, but they are vastly different in approach and results. Some are prospective, retrospective, case–controls, or double-blind placebo studies for antibiotic therapy. Some studies followed patients for short and long periods of time after onset. Most of the studies measured outcomes through neuropsychological tests, depression, and quality of life. Importantly, these studies comprised all the known clinical manifestations of LNB. Given the differences in the design of the studies, it is difficult to generalize, but there are some salient features that merit consideration. All 34 studies had an aggregate of 2,888 patients, a sufficiently large number to draw some conclusions, with the caveat that all are fundamentally different.
Adverse outcomes were more frequently reported in the earlier studies. Five studies that reported the worst outcomes also reported delays in starting antibiotic therapy.
In 3 recent studies, adverse outcomes were associated with comorbidities.
Two studies reported that the use of corticosteroids leads to more severe outcomes.
Adverse outcomes were reported in 9 studies, and these ranged from a small number to almost half of the patients studied. The sequelae were mostly associated with the poor results of the neuropsychological tests.
Almost complete recovery of the patients was reported in 13 studies.
Studies that used antibiotic therapy as part of the clinical protocols were conclusive in their findings that additional antibiotic therapy is not useful for the treatment of adverse outcomes.
Although the general trend is that appropriately treated LNB has a long-term favorable outcome, a review of these studies indicates that a significant number of patients report low scores on neuropsychological tests, and this is at the heart of the current controversy that surrounds Lyme disease and its optimal treatment. Given the present level of controversy, mostly in the United States but rapidly spreading to Europe, it is imperative that comprehensive and identical population-based studies be conducted in parallel in both continents, and the public health agencies should give this effort a high level of urgency.
Post-Treatment Lyme Disease Syndrome
Several years ago, the first reports of what is now called “post-treatment Lyme disease syndrome” (PTLDS) were published. Today, that such a syndrome exists has been accepted by a consensus of clinicians, and the CDC has defined it as the presence of symptoms that include cognitive dysfunction, fatigue, fibromyalgialike pain, and even depression leading to poor quality of life in appropriately treated patients that can persist for >6 months and could last for years (https://www.cdc.gov/lyme/postlds/index.html). The number of patients with this syndrome has been tentatively placed at about 10%. The literature on PTLDS has increased markedly in the past few years, but despite this awareness, there is no consensus as to its cause or its treatment. Some risk factors for PTLDS have been identified and include being a female, long pretreatment period, high mononuclear cell infiltrate in the CSF, and onset of symptoms before termination of antibiotic therapy.17,46,47 PTLDS is most common in patients with LNB. An area that has not been explored is whether similar syndromes are associated with other infections, and this may be a fruitful area to gain some useful insights.
Although there is general consensus that PTLDS is a legitimate sequela of treated LNB, the controversy that surrounds it is tied to its treatment with long-term antibiotic therapy. In this aspect, the literature is unanimous in showing that long-term antibiotic therapy provides no benefits to the patients with PTLDS.48–50 Fundamentally, the inability of antibiotic therapy to improve PTLDS shows conclusively that this syndrome is not caused by a residual, treatable infection. Nonetheless, many patients insist on being prescribed (and their doctors provide) long-term antibiotic therapy. This presents a serious problem, as there have been numerous reports of harmful effects, even deaths, due to prolonged needless administration of antibiotics. This aspect is considered on the CDC website (https://www.cdc.gov/lyme/postlds/index.html).
Another problem associated with PTLDS is the notion that a condition that is generally termed as “chronic Lyme disease” is synonymous with PTLDS. The definition of PTLDS requires verifiable proof that the patient had Lyme disease, and moreover, that the disease was properly treated with antibiotics, although its symptoms are clearly subjective. Not so for chronic Lyme disease, where many patients have similar symptomatology to those with PTLDS but have no history of a rigorous clinical or laboratory diagnosis of Lyme disease. There is no consensus for chronic Lyme disease, and the use of the term is discouraged by a large majority of clinicians.51 The controversy regarding Lyme disease arises from several misconceptions: (1) patient can have Lyme disease despite repeated nonreactive serology; (2) treatment of Lyme disease requires lengthy antibiotic therapy; and (3) the clinical spectrum of Lyme disease includes nonspecific symptoms without any of the established cutaneous, cardiac, articular, and neurological manifestations. These features of the controversy belie a deep distrust of biomedical science and its researchers among segments of the population—including some health care professionals. Hence, this controversy represents a social phenomenon unlikely to be solved at either the clinic or the laboratory bench. At present, it is extremely difficult to offer solutions for this problem.
Pathogenesis
Aspects of the pathogenesis of LNB have been recreated through experimental studies using nonhuman primates (NHPs). Two models, with fundamentally similar findings, were developed. One model, using NHPs previously treated with steroids, reported positive cultures of B. burgdorferi and pleocytosis in the CSF supporting the observation that LNB is associated with direct spirochetal invasion.52 The other NHP model did not use prior immunosuppression for infection. NHPs infected by both tick bite and by needle developed pleocytosis in the CSF.53 After 6 months, a period of time representative of chronic disease, the NHPs developed nerve sheath fibrosis, focal demyelinization of the spinal cord, and peripheral neuropathy.54 Likewise, within the first 3 months of infection, NHPs developed neuritis with macrophage and B-cell infiltrates with demyelination and axonal dysfunction.55
In the absence of a mouse model for LNB,56 much information has been obtained from experimental approaches using primary cells of the nervous system and tissue explants. Early on, we demonstrated the adherence and neurotropism of Borrelia to neural cells.57–59 The overwhelming evidence is that contact of B. burgdorferi with all cells of the nervous system elicits an inflammatory response. The microglia are logical starting points, as these cells are the resident macrophages of the CNS, with clear functions in phagocytosis, scavenging, and antigen presentation. Murine microglia are efficient phagocytes and are capable of ingesting and killing spirochetes with or without opsonization.60 Inflammatory response pathways for microglia exposed to Borrelia follow the known signals that originate through Toll receptors 2 and 5, which recognize spirochetal lipoproteins and flagellin, respectively.61 Primary human microglia exposed to live B. burgdorferi and spirochetal debris resulted in phagocytosis, with the latter inducing a larger inflammatory response.62 It is not surprising that microglia respond to Borrelia as has been described, and their proinflammatory potential could be mediating some of the damage that develops in LNB. Astrocytes, the cells most likely to come in contact with the spirochetes after crossing the blood–brain barrier, secrete inflammatory mediators following exposure to these organisms.63,64 Experimental studies with oligodendroglia65 and neuronal cells ex vivo66 also indicate that Borrelia can induce inflammatory responses in these cells.
Inflammation is an undeniable cause of neurologic damage, and it is the primary response to Borrelia in the CNS. This response is different from responses elicited by other bacteria that penetrate the nervous system and that elicit a neutrophil infiltrate. The infiltrate of the CSF in LNB is mononuclear, as is also seen in neurosyphilis and in cases of viral meningitis. Early evidence disclosed that antibody-producing cells were predominant in the CSF of patients with untreated neuroborreliosis.67 In an interesting study, CD4+ gamma interferon-producing T cells specific for Borrelia and for CNS autoantigens were demonstrated in the CSF of a patient with acute Lyme encephalitis.68 The pathogenesis of LNB appears to follow the entry of the spirochetes into the CNS.59
There is potential for spirochetal debris as agents of pathogenesis. Amorphous green fluorescence protein deposits (derived from Borrelia) were visualized in tendons and cartilage of antibiotic-treated mice, indicating that proinflammatory debris could contribute to the development of antibiotic-refractory Lyme arthritis.69 In this context, the “amber theory” for Lyme arthritis was proposed, whereby introduction of nonviable spirochetes or debris enmeshed in a host-derived fibrinous or collagenous matrix could be responsible for the joint manifestations of Lyme disease.70 Although these findings and the amber theory pertain to Lyme arthritis, it would not be inconsistent to extend them to the pathogenesis of LNB, particularly as a recent study showed that spirochetal debris is highly proinflammatory for neural cells.62 If validated, the potential for spirochetal debris as agents of pathogenesis would be unique to infection and would point to a major defect in the scavenging functions of phagocytes that are unable to “clean up” the remains of spirochetes killed by the immune response.
LNB is characterized by B-cell activation, plasma cell infiltration, and enhanced intrathecal antibody production in the CSF. The first evidence that B-cell chemoattractant, chemokine (C-X-C motif) ligand 13 (CXCL13) is expressed in the nervous system and is a definitive feature of neuroborreliosis was provided by experimental approaches using NHPs.71 CXCL13 is selective for B cells belonging to the B-1 and B-2 subsets, and interacts with its receptor CXCR5.72 CXCL13 is produced by different immune cells but preferentially by dendritic cells, and recruits B cells and also CD4+ follicular helper cells to lymphoid organs via its cognate receptor CXCR5.72 Ectopic lymphoid follicles can also form due to overexpression of CXCL13 and can lead to specific organ inflammation.73
It is now clear that the presence of CXCL13 in the CSF of patients with neuroborreliosis is important, judging by the large number of studies following the initial observation. Elevated levels of CXCL13 were found in neuroborreliosis but not in other control neurologic diseases74 and were elevated in children and adults.75 An enzyme-linked immunosorbent assay for CXCL13 had high sensitivity and specificity for acute neuroborreliosis, particularly before the antibodies are detectable, making this assay a powerful adjunct to the clinical evaluation.76 However, CXCL13 can also be detected in other manifestations of Lyme disease; patients with borrelial lymphocytoma, a skin disorder, also have high levels of serum CXCL13.77 In some other neurologic manifestations of Lyme disease, the CXCL13 assay is negative. Lyme encephalopathy, a difficult entity to diagnose, is characterized by nonspecific neurobehavioral manifestations, but levels of CXCL13 in the CSF were not elevated in patients with this syndrome.78
Increased levels of CXCL13 occur in other infections, such as in the relapsing fever borrelioses.73 Elevated levels of CXCL13 in the CSF of patients with neurosyphilis and human immunodeficiency virus infection (but not in syphilis patients without neurologic disease) were independent of T cells and declined after antibiotic treatment, making it a useful marker for diagnosis and treatment.79 Importantly, proinflammatory molecules of Borrelia species and Treponema pallidum induced production of CXCL13 from monocytes via Toll receptor signaling.80 Levels of CXCL13 decreased significantly with antibiotic therapy, suggesting a role for this chemokine as a marker for disease activity and for antibiotic effectiveness.81 Lastly, elevated levels have also been noted in patients with aseptic meningitis.82
CXCL13 in the CSF can also be a marker for noninfectious neurologic diseases. In comparative studies, CXCL13 was elevated in the CSF of all patients with borreliosis and multiple sclerosis (MS), and showed the most consistent correlation with the presence of intrathecal Ig production in the CSF.83 Anti–N-methyl-D-aspartate receptor (NMDAR) encephalitis is a severe antibody-mediated autoimmune disorder affecting children and young adults. Early stage anti-NMDAR encephalitis patients had increased levels of CXCL13 in the CSF that correlated with intrathecal NMDAR-antibody synthesis. Fluctuations in the levels of CXCL13 during relapses or following treatment was considered to be a useful measure of treatment outcome.84 CXCL13 was produced in actively demyelinating MS lesions, but not in inactive lesions. Likewise, levels of CXCL13 were elevated in the CSF of relapsing–remitting MS patients and correlated with intrathecal immunoglobulin as well as the presence of B cells. Trafficking of immune cells to MS lesions is an important feature of this disease, and CXCL13 as a chemoattractant of B cells could be a potential therapeutic target.85 CXCL13/CXCR5 are important in the homing of B cells in primary lymphoma of the CNS. Levels of CXCL13 in the CSF were elevated in patients with CNS lymphoma, and survival was tied to decreasing or lower levels of this chemokine. Higher levels are associated with a more serious course of the disease.86 Therefore, depletion of CXCL13 may be a good strategy to follow the treatment of CNS lymphoma.
Is the CXCL13/CXCR5 axis a good therapeutic target in LNB? Early disruption of the CXCL13/CXCR5 axis would help decrease the intrathecal antibody response, and hence retard recovery of the infection. If, however, there should be future evidence for an autoimmune component to neuroborreliosis, then therapeutic reduction of CXCL13 levels would be warranted. This clearly would be the case in MS, where inhibition of CXCL13 would dampen the effects of the ectopic B cell follicles and therefore the development of disease.87
The role of CXCL13 in LNB is of great interest both as a marker and as a participant in the pathogenesis of this disease. It is clear from the foregoing that B. burgdorferi induces high-level production of this B-cell chemoattractant, as befits an infection noted by strong antibody responses. Although production of CXCL13 is shared by other neurologic infections as well as other neurologic diseases, the CSF levels in neuroborreliosis are uniformly and often markedly higher than in the other diseases.88 This is useful in discriminating between LNB and other diseases. New information on the role of this chemokine is enlarging its importance in the acquired immune response as well as in vaccination, and this can generate meaningful links to neuroborreliosis and to Lyme disease in general.
Polymicrobial Infections
Since the discovery of B. burgdorferi in 1983,89–91 there has been the recognition that Lyme disease can be but one of many infections associated with ticks, particularly those caused by pathogens transmitted by Ixodes scapularis in USA and Ixodes ricinus in Europe. This tick species transmits 5 pathogens (Table 2), and 4 of these can cause neurologic disease by themselves. The impact of Ixodes-borne polymicrobial infections on neurologic disease is not known at present, but it could be synergistic, leading to a negative progression of the course of infection. In addition, Amblyomma americanum, a southern tick, has increased its range in the past decades, and this aggressive invading species is now a dominant presence in parts of the United States.92
TABLE 2.
Pathogens Transmitted by Various Tick Species
| Tick Species | Pathogens (diseases) |
|---|---|
| Ixodes scapularis/Ixodes ricinus, deer tick and black legged tick | Borrelia burgdorferi (Lyme disease), Borrelia miyamotoi (meningitis), Anaplasma phagocytophilum (anaplasmosis, meningitis), Babesia microti (babesiosis), Powassan virus lineage II (meningitis/encephalitis), tick-borne encephalitis virus |
| Amblyomma americanum, lone star tick | Ehrlichia chaffeensis (ehrlichiosis, meningitis), Rickettsia species, Francisella tularensis (tularemia) |
| Dermacentor variabilis, American dog tick | Rickettsia rickettsii (Rocky Mountain spotted fever), Francisella tularensis |
Borrelia miyamotoi was discovered in Japan in 199493 and has been documented all over the world. Of interest is that B. miyamotoi clusters genetically within the relapsing fever group of Borrelia; however, it is transmitted by the hard tick vectors of the Lyme disease Borrelias.
The clinical manifestations of B. miyamotoi infection are high fever, fatigue, severe headache, chills, and muscle and joint pain94–96 and can resolve with doxycycline therapy.97 Meningoencephalitis has been reported,98,99 and spirochetes were detected by microscopy in the CSF in a patient with lymphoma.100 Case reports suggest that infection with B. miyamotoi may be more severe than with the Lyme disease Borrelia, and the effect of coinfection on the nervous system with both Borrelia species needs to be evaluated. It is likely that this organism will be responsible for more neurological infections as new clinical series are reported. Laboratory diagnosis is based mainly upon polymerase chain reaction of acute blood samples.
Anaplasma phagocytophilum and Ehrlichia chaffeensis are obligate intracellular bacteria (Rickettsiales) that invade neutrophils and monocytes, respectively. Anaplasma is transmitted by Ixodes scapularis. Thus, A. phagocytophilum and B. burgdorferi can be transmitted simultaneously and cause a double infection. E. chaffeensis is transmitted by Amblyomma americanum and is not cotransmitted with other pathogens. Both organisms cause a febrile disease and can also cause neurological illness. One percent of anaplasmosis patients develop meningitis.101 In contrast, meningitis has been reported in 5% of patients with ehrlichiosis.102 This disparity has an interesting biological basis; whereas E. chaffeensis–infected monocytes readily transmigrate human brain microvasculature, A. phagocytophilum suppresses neutrophil transmigration.103 The reason is that Anaplasma-infected neutrophils downregulate the surface expression of P and L selectins, thereby decreasing their ability to cross vasculature.104
The neurologic manifestations have been better studied in ehrlichiosis. The intracellular morulae (bacterial cell aggregates) of E. chaffeensis were detected in the CSF of a patient with meningitis.105 The most common CSF abnormalities are a lymphocytic pleocytosis with elevated proteins and decreased glucose. Four (19%) of the 21 patients with Ehrlichia meningitis died.106 The PNS is less frequently involved.107 Given the rapid spread of its vector tick, more cases of ehrlichiosis are likely to occur. The effect of coinfections with Borrelia and Anaplasma on the prevalence or severity of neurological manifestations is not clear.
Entering this polymicrobial milieu is Powassan virus (POWV), a flavivirus member of the tick-borne encephalitis virus (TBEV) group, first isolated in 1958 in Canada.108 Since then, >100 cases have been reported in the USA, with a death rate of 11%,109 underscoring its severity.110
POWV is composed of 2 lineages, lineage I (prototype POWV) and lineage II (LII), first identified as deer tick virus.111 POWV (lineage I) is transmitted through an Inocybe cookei–woodchuck cycle. LII virus circulates in an I. scapularis–white-footed mouse cycle, and it is precisely in this cycle that this virus can become a part of the polymicrobial group of pathogens. Evidence is mounting for this virus being responsible for human disease, with 3 fatal cases of encephalitis reported. In one case of necrotizing meningoencephalitis, deer tick virus was identified in large neurons in the brainstem, cerebellum, basal ganglia, thalamus, and spinal cord.112 One fatal case of LII virus in a patient with lymphoma113 and another in a patient without predisposing factors114 were described recently. LII virus is widespread in ticks in the same geographic areas as Lyme disease.115 Serologic evidence of infection and exposure was obtained in a retrospective study of patients suspected of having Lyme disease, indicating broad exposure to the virus that can cause subclinical infection as well as serious neurologic manifestations.116
The occurrence of TBEV and Borrelia in Europe parallels that of the USA with LII. Almost 4% of patients in a series with acute lymphocytic meningitis had double infections with TBEV and B. burgdorferi.117 Patients with lymphocytic meningitis or meningoencephalitis from areas endemic for both TBEV and LNB can yield both virus and spirochete isolations from the CSF.118 Lymphocytic infiltrate of CSF is higher in patients with neuroborreliosis than in those with TBEV.119 However, a prospective study of children diagnosed with TBEV had more long-term and higher frequency of neurologic deficits than children diagnosed with LNB.120
Given the geographic and vector overlap of tick-borne viruses with Lyme disease, the possibility of double infections of patients with Borrelia species and tick-borne encephalitis viruses in both continents should be evaluated. In addition to the geographic overlap of TBEV and LII virus with borreliosis in Europe and the United States, there are clinical and laboratory similarities between the infections with the viruses and with Borrelia species, particularly with less severe exposures to the viral agents. Whether there is a clinical neurological correlate to double infections and the extent of their impact on the occurrence and severity of disease remain to be determined.56
Summary
In the intervening 2 decades since our first review, the main manifestations of LNB remain mostly as initially described on both continents. There are infrequent cases of neurologic complications that remind us how severe this infection can be. We have also seen the documentation for the unexplained condition of PTLDS, which could be a unique complication of neuroborreliosis. Importantly, this sequela can be confused with a condition “chronic Lyme disease,” a term mostly used in the lay networks, and carries the negative impact of excessive antibiotic therapy.
We look forward to some needed research. The etiology of PTLDS is top on our list. Coordinated population-based epidemiological studies on both continents could answer decisively some of the lingering questions on the medical and microbiologic diversity of Lyme disease on both continents. Lastly, research on the pathogenesis of, for example, facial nerve palsy, which is a condition seen in widely different infections such as herpes and Borrelia, would provide new perspectives.
Supplementary Material
Acknowledgment
This study was supported by the National Institute of Allergy and Infectious Diseases NIH (AI-027044-28).
Footnotes
Additional supporting information can be found in the online version of this article.
Potential Conflicts of Interest
Nothing to report.
References
- 1.Paules CI, Marston HD, Bloom ME, Fauci AS. Tickborne diseases—confronting a growing threat. N Engl J Med 2018;379:701–703. [DOI] [PubMed] [Google Scholar]
- 2.Rosenberg R, Lindsey NP, Fischer M, et al. Vital signs: trends in reported vectorborne disease cases—United States and territories, 2004–2016. MMWR Morb Mortal Wkly Rep 2018;67:496–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steere AC, Strle F, Wormser GP, et al. Lyme borreliosis. Nat Rev Dis Primers 2016;2:16090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pachner AR, Steere AC. The triad of neurologic manifestations of Lyme disease: meningitis, cranial neuritis, and radiculoneuritis. Neurology 1985;35:47–53. [DOI] [PubMed] [Google Scholar]
- 5.Garcia-Monco JC, Benach JL. Lyme neuroborreliosis. Ann Neurol 1995;37:691–702. [DOI] [PubMed] [Google Scholar]
- 6.Kristoferitsch W. Neurological manifestations of Lyme borreliosis: clinical definition and differential diagnosis. Scand J Infect Dis Suppl 1991;77:64–73. [PubMed] [Google Scholar]
- 7.Marques AR. Lyme neuroborreliosis. Continuum (Minneap Minn) 2015;21(6 Neuroinfectious Disease):1729–1744. [DOI] [PubMed] [Google Scholar]
- 8.Pachner AR, Steiner I. Lyme neuroborreliosis: infection, immunity, and inflammation. Lancet Neurol 2007;6:544–552. [DOI] [PubMed] [Google Scholar]
- 9.Stanek G, Wormser GP, Gray J, Strle F. Lyme borreliosis. Lancet 2012;379:461–473. [DOI] [PubMed] [Google Scholar]
- 10.Halperin JJ, Garcia-Monco JC. The human borreliosis: Lyme neuroborreliosis and relapsing fever In: Garcia-Monco JC, ed. CNS infections: a clinical approach. London, UK: Springer, 2017. [Google Scholar]
- 11.Knudtzen FC, Andersen NS, Jensen TG, Skarphedinsson S. Characteristics and clinical outcome of Lyme neuroborreliosis in a high endemic area, 1995–2014: a retrospective cohort study in Denmark. pp 233–249. Clin Infect Dis 2017;65:1489–1495. [DOI] [PubMed] [Google Scholar]
- 12.Ackermann R, Horstrup P, Schmidt R. Tick-borne meningopolyneuritis (Garin-Bujadoux, Bannwarth). Yale J Biol Med 1984;57:485–490. [PMC free article] [PubMed] [Google Scholar]
- 13.Kruger H, Reuss K, Pulz M, et al. Meningoradiculitis and encephalomyelitis due to Borrelia burgdorferi: a follow-up study of 72 patients over 27 years. J Neurol 1989;236:322–328. [DOI] [PubMed] [Google Scholar]
- 14.Kruger H, Kohlhepp W, Konig S. Follow-up of antibiotically treated and untreated neuroborreliosis. Acta Neurol Scand 1990;82:59–67. [DOI] [PubMed] [Google Scholar]
- 15.Camponovo F, Meier C. Neuropathy of vasculitic origin in a case of Garin-Boujadoux-Bannwarth syndrome with positive borrelia antibody response. J Neurol 1986;233:69–72. [DOI] [PubMed] [Google Scholar]
- 16.Vallat JM, Hugon J, Lubeau M, et al. Tick-bite meningoradiculoneuritis: clinical, electrophysiologic, and histologic findings in 10 cases. Neurology 1987;37:749–753. [DOI] [PubMed] [Google Scholar]
- 17.Ogrinc K, Lusa L, Lotric-Furlan S, et al. Course and outcome of early European Lyme neuroborreliosis (Bannwarth syndrome): clinical and laboratory findings. Clin Infect Dis 2016;63:346–353. [DOI] [PubMed] [Google Scholar]
- 18.Shah A, O’Horo JC, Wilson JW, et al. An unusual cluster of neuroinvasive Lyme disease cases presenting with Bannwarth syndrome in the Midwest United States. Open Forum Infect Dis 2018;5:ofx276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garcia-Monco JC, Beldarrain MG, Zabalza I. Infectious meningitis with atypical cerebrospinal fluid cells. Eur J Neurol 1997;4:188–191. [DOI] [PubMed] [Google Scholar]
- 20.Garcia-Monco JC, Gomez Beldarrain M, Estrade L. Painful lumbosacral plexitis with increased ESR and Borrelia burgdorferi infection. Neurology 1993;43:1269. [DOI] [PubMed] [Google Scholar]
- 21.Henriksson A, Link H, Cruz M, Stiernstedt G. Immunoglobulin abnormalities in cerebrospinal fluid and blood over the course of lymphocytic meningoradiculitis (Bannwarth’s syndrome). Ann Neurol 1986;20:337–345. [DOI] [PubMed] [Google Scholar]
- 22.Garkowski A, Zajkowska J, Zajkowska A, et al. Cerebrovascular manifestations of Lyme neuroborreliosis—a systematic review of published cases. Front Neurol 2017;8:146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lebas A, Toulgoat F, Saliou G, et al. Stroke due to Lyme neuroborreliosis: changes in vessel wall contrast enhancement. J Neuroimaging 2012;22:210–212. [DOI] [PubMed] [Google Scholar]
- 24.Ruisanchez A, Vicente-Olabarria I, Escalza-Cortina I, et al. Role of MRI in early detection of stroke secondary to neurosyphilis in an elderly patient coinfected with HIV. Neurol Clin Pract 2017;7: e12–e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ionita CC, Siddiqui AH, Levy EI, et al. Acute ischemic stroke and infections. J Stroke Cerebrovasc Dis 2011;20:1–9. [DOI] [PubMed] [Google Scholar]
- 26.Traisk F, Lindquist L. Optic nerve involvement in Lyme disease. Curr Opin Ophthalmol 2012;23:485–490. [DOI] [PubMed] [Google Scholar]
- 27.Sibony P, Halperin J, Coyle PK, Patel K. Reactive Lyme serology in optic neuritis. J Neuroophthalmol 2005;25:71–82. [DOI] [PubMed] [Google Scholar]
- 28.Kristoferitsch W, Sluga E, Graf M, et al. Neuropathy associated with acrodermatitis chronica atrophicans. Clinical and morphological features. Ann N Y Acad Sci 1988;539:35–45. [DOI] [PubMed] [Google Scholar]
- 29.Logigian EL, Kaplan RF, Steere AC. Chronic neurologic manifestations of Lyme disease. N Engl J Med 1990;323:1438–1444. [DOI] [PubMed] [Google Scholar]
- 30.Halperin JJ. Lyme disease and the peripheral nervous system. Muscle Nerve 2003;28:133–143. [DOI] [PubMed] [Google Scholar]
- 31.Wormser GP, Strle F, Shapiro ED, et al. A critical appraisal of the mild axonal peripheral neuropathy of late neurologic Lyme disease. Diagn Microbiol Infect Dis 2017;87:163–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Halperin JJ, Little BW, Coyle PK, Dattwyler RJ. Lyme disease: cause of a treatable peripheral neuropathy. Neurology 1987;37: 1700–1706. [DOI] [PubMed] [Google Scholar]
- 33.Ackermann R, Gollmer E, Rehse-Kupper B. Progressive Borrelia encephalomyelitis. Chronic manifestation of erythema chronicum migrans disease of the nervous system [in German]. Dtsch Med Wochenschr 1985;110:1039–1042. [DOI] [PubMed] [Google Scholar]
- 34.Mygland A, Ljostad U, Fingerle V, et al. EFNS guidelines on the diagnosis and management of European Lyme neuroborreliosis. Eur J Neurol 2010;17:8–16, e1–e4. [DOI] [PubMed] [Google Scholar]
- 35.Halperin JJ, Luft BJ, Anand AK, et al. Lyme neuroborreliosis: central nervous system manifestations. Neurology 1989;39:753–759. [DOI] [PubMed] [Google Scholar]
- 36.Halperin JJ, Krupp LB, Golightly MG, Volkman DJ. Lyme borreliosis-associated encephalopathy. Neurology 1990;40: 1340–1343. [DOI] [PubMed] [Google Scholar]
- 37.Shadick NA, Phillips CB, Sangha O, et al. Musculoskeletal and neurologic outcomes in patients with previously treated Lyme disease. Ann Intern Med 1999;131:919–926. [DOI] [PubMed] [Google Scholar]
- 38.Cerar D, Cerar T, Ruzic-Sabljic E, et al. Subjective symptoms after treatment of early Lyme disease. Am J Med 2010;123:79–86. [DOI] [PubMed] [Google Scholar]
- 39.Branda JA, Strle K, Nigrovic LE, et al. Evaluation of modified 2-tiered serodiagnostic testing algorithms for early Lyme disease. Clin Infect Dis 2017;64:1074–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moore A, Nelson C, Molins C, et al. Current guidelines, common clinical pitfalls, and future directions for laboratory diagnosis of Lyme disease, United States. Emerg Infect Dis 2016;22(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marques AR. Laboratory diagnosis of Lyme disease: advances and challenges. Infect Dis Clin North Am 2015;29:295–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hammers-Berggren S, Hansen K, Lebech AM, Karlsson M. Borrelia burgdorferi-specific intrathecal antibody production in neuroborreliosis: a follow-up study. Neurology 1993;43:169–175. [DOI] [PubMed] [Google Scholar]
- 43.Steere AC, Berardi VP, Weeks KE, et al. Evaluation of the intrathecal antibody response to Borrelia burgdorferi as a diagnostic test for Lyme neuroborreliosis. J Infect Dis 1990;161:1203–1209. [DOI] [PubMed] [Google Scholar]
- 44.Philipp MT, Wormser GP, Marques AR, et al. A decline in C6 antibody titer occurs in successfully treated patients with culture-confirmed early localized or early disseminated Lyme borreliosis. Clin Diagn Lab Immunol 2005;12:1069–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Halperin JJ, Shapiro ED, Logigian E, et al. Practice parameter: treatment of nervous system Lyme disease (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2007;69:91–102. [DOI] [PubMed] [Google Scholar]
- 46.Eikeland R, Mygland A, Herlofson K, Ljostad U. Risk factors for a non-favorable outcome after treated European neuroborreliosis. Acta Neurol Scand 2013;127:154–160. [DOI] [PubMed] [Google Scholar]
- 47.Ljostad U, Mygland A. Remaining complaints 1 year after treatment for acute Lyme neuroborreliosis; frequency, pattern and risk factors. Eur J Neurol 2010;17:118–123. [DOI] [PubMed] [Google Scholar]
- 48.Berende A, ter Hofstede HJ, Vos FJ, et al. Randomized trial of longer-term therapy for symptoms attributed to Lyme disease. N Engl J Med 2016;374:1209–1220. [DOI] [PubMed] [Google Scholar]
- 49.Krupp LB, Hyman LG, Grimson R, et al. Study and treatment of post Lyme disease (STOP-LD): a randomized double masked clinical trial. Neurology 2003;60:1923–1930. [DOI] [PubMed] [Google Scholar]
- 50.Klempner MS, Baker PJ, Shapiro ED, et al. Treatment trials for post-Lyme disease symptoms revisited. Am J Med 2013;126:665–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Feder HM Jr, Johnson BJ, O’Connell S, et al. A critical appraisal of “chronic Lyme disease”. N Engl J Med 2007;357:1422–1430. [DOI] [PubMed] [Google Scholar]
- 52.Pachner AR, Delaney E, O’Neill T, Major E. Inoculation of nonhuman primates with the N40 strain of Borrelia burgdorferi leads to a model of Lyme neuroborreliosis faithful to the human disease. Neurology 1995;45:165–172. [DOI] [PubMed] [Google Scholar]
- 53.Philipp MT, Aydintug MK, Bohm RP Jr, et al. Early and early disseminated phases of Lyme disease in the rhesus monkey: a model for infection in humans. Infect Immun 1993;61:3047–3059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Roberts ED, Bohm RP Jr, Cogswell FB, et al. Chronic lyme disease in the rhesus monkey. Lab Invest 1995;72:146–160. [PubMed] [Google Scholar]
- 55.Roberts ED, Bohm RP Jr, Lowrie RC Jr, et al. Pathogenesis of Lyme neuroborreliosis in the rhesus monkey: the early disseminated and chronic phases of disease in the peripheral nervous system. J Infect Dis 1998;178:722–732. [DOI] [PubMed] [Google Scholar]
- 56.Garcia-Monco JC, Benach JL. A disconnect between the neurospirochetoses in humans and rodent models of disease. PLoS Pathog 2013;9:e1003288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Garcia-Monco JC, Fernandez Villar B, Szczepanski A, Benach JL. Cytotoxicity of Borrelia burgdorferi for cultured rat glial cells. J Infect Dis 1991;163:1362–1366. [DOI] [PubMed] [Google Scholar]
- 58.Garcia-Monco JC, Fernandez-Villar B, Benach JL. Adherence of the Lyme disease spirochete to glial cells and cells of glial origin. J Infect Dis 1989;160:497–506. [DOI] [PubMed] [Google Scholar]
- 59.Garcia-Monco JC, Villar BF, Alen JC, Benach JL. Borrelia burgdorferi in the central nervous system: experimental and clinical evidence for early invasion. J Infect Dis 1990;161:1187–1193. [DOI] [PubMed] [Google Scholar]
- 60.Kuhlow CJ, Garcia-Monco JC, Coleman JL, Benach JL. Murine microglia are effective phagocytes for Borrelia burgdorferi. J Neuroimmunol 2005;168:183–187. [DOI] [PubMed] [Google Scholar]
- 61.Parthasarathy G, Philipp MT. Inflammatory mediator release from primary rhesus microglia in response to Borrelia burgdorferi results from the activation of several receptors and pathways. J Neuroinflammation 2015;12:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Greenmyer JR, Gaultney RA, Brissette CA, Watt JA. Primary human microglia are phagocytically active and respond to Borrelia burgdorferi with upregulation of chemokines and cytokines. Front Microbiol 2018;9:811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ramesh G, Alvarez AL, Roberts ED, et al. Pathogenesis of Lyme neuroborreliosis: Borrelia burgdorferi lipoproteins induce both proliferation and apoptosis in rhesus monkey astrocytes. Eur J Immunol 2003;33:2539–2550. [DOI] [PubMed] [Google Scholar]
- 64.Brissette CA, Kees ED, Burke MM, et al. The multifaceted responses of primary human astrocytes and brain microvascular endothelial cells to the Lyme disease spirochete, Borrelia burgdorferi. ASN Neuro 2013;5:221–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ramesh G, Benge S, Pahar B, Philipp MT. A possible role for inflammation in mediating apoptosis of oligodendrocytes as induced by the Lyme disease spirochete Borrelia burgdorferi. J Neuroinflammation 2012;9:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Myers TA, Kaushal D, Philipp MT. Microglia are mediators of Borrelia burgdorferi-induced apoptosis in SH-SY5Y neuronal cells. PLoS Pathog 2009;5:e1000659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Baig S, Olsson T, Link H. Predominance of Borrelia burgdorferi specific B cells in cerebrospinal fluid in neuroborreliosis. Lancet 1989;2: 71–74. [DOI] [PubMed] [Google Scholar]
- 68.Lunemann JD, Gelderblom H, Sospedra M, et al. Cerebrospinal fluid-infiltrating CD4+ T cells recognize Borrelia burgdorferi lysine-enriched protein domains and central nervous system autoantigens in early Lyme encephalitis. Infect Immun 2007;75:243–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bockenstedt LK, Gonzalez DG, Haberman AM, Belperron AA. Spirochete antigens persist near cartilage after murine Lyme borreliosis therapy. J Clin Invest 2012;122:2652–2660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wormser GP, Nadelman RB, Schwartz I. The amber theory of Lyme arthritis: initial description and clinical implications. Clin Rheumatol 2012;31:989–994. [DOI] [PubMed] [Google Scholar]
- 71.Narayan K, Dail D, Li L, et al. The nervous system as ectopic germinal center: CXCL13 and IgG in Lyme neuroborreliosis. Ann Neurol 2005;57:813–823. [DOI] [PubMed] [Google Scholar]
- 72.Legler DF, Loetscher M, Roos RS, et al. B cell-attracting chemokine 1, a human CXC chemokine expressed in lymphoid tissues, selectively attracts B lymphocytes via BLR1/CXCR5. J Exp Med 1998; 187:655–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lalor SJ, Segal BM. Lymphoid chemokines in the CNS. J Neuroimmunol 2010;224:56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rupprecht TA, Pfister HW, Angele B, et al. The chemokine CXCL13 (BLC): a putative diagnostic marker for neuroborreliosis. Neurology 2005;65:448–450. [DOI] [PubMed] [Google Scholar]
- 75.Wutte N, Berghold A, Loffler S, et al. CXCL13 chemokine in pediatric and adult neuroborreliosis. Acta Neurol Scand 2011;124: 321–328. [DOI] [PubMed] [Google Scholar]
- 76.Schmidt C, Plate A, Angele B, et al. A prospective study on the role of CXCL13 in Lyme neuroborreliosis. Neurology 2011;76: 1051–1058. [DOI] [PubMed] [Google Scholar]
- 77.Mullegger RR, Means TK, Shin JJ, et al. Chemokine signatures in the skin disorders of Lyme borreliosis in Europe: predominance of CXCL9 and CXCL10 in erythema migrans and acrodermatitis and CXCL13 in lymphocytoma. Infect Immun 2007;75:4621–4628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Eckman EA, Pacheco-Quinto J, Herdt AR, Halperin JJ. Neuroimmunomodulators in neuroborreliosis and Lyme encephalopathy. Clin Infect Dis 2018;67:80–88. [DOI] [PubMed] [Google Scholar]
- 79.Marra CM, Tantalo LC, Sahi SK, et al. CXCL13 as a cerebrospinal fluid marker for neurosyphilis in HIV-infected patients with syphilis. Sex Transm Dis 2010;37:283–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rupprecht TA, Kirschning CJ, Popp B, et al. Borrelia garinii induces CXCL13 production in human monocytes through Toll-like receptor 2. Infect Immun 2007;75:4351–4356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Senel M, Rupprecht TA, Tumani H, et al. The chemokine CXCL13 in acute neuroborreliosis. J Neurol Neurosurg Psychiatry 2010;81: 929–933. [DOI] [PubMed] [Google Scholar]
- 82.Fujimori J, Nakashima I, Kuroda H, et al. Cerebrospinal fluid CXCL13 is a prognostic marker for aseptic meningitis. J Neuroimmunol 2014;273:77–84. [DOI] [PubMed] [Google Scholar]
- 83.Kowarik MC, Cepok S, Sellner J, et al. CXCL13 is the major determinant for B cell recruitment to the CSF during neuroinflammation. J Neuroinflammation 2012;9:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Leypoldt F, Hoftberger R, Titulaer MJ, et al. Investigations on CXCL13 in anti-N-methyl-D-aspartate receptor encephalitis: a potential biomarker of treatment response. JAMA Neurol 2015;72: 180–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Krumbholz M, Theil D, Cepok S, et al. Chemokines in multiple sclerosis: CXCL12 and CXCL13 up-regulation is differentially linked to CNS immune cell recruitment. Brain 2006;129(pt 1):200–211. [DOI] [PubMed] [Google Scholar]
- 86.Rubenstein JL, Wong VS, Kadoch C, et al. CXCL13 plus interleukin 10 is highly specific for the diagnosis of CNS lymphoma. Blood 2013;121:4740–4748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sellebjerg F, Bornsen L, Khademi M, et al. Increased cerebrospinal fluid concentrations of the chemokine CXCL13 in active MS. Neurology 2009;73:2003–2010. [DOI] [PubMed] [Google Scholar]
- 88.van Burgel ND, Bakels F, Kroes AC, van Dam AP. Discriminating Lyme neuroborreliosis from other neuroinflammatory diseases by levels of CXCL13 in cerebrospinal fluid. J Clin Microbiol 2011;49: 2027–2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Benach JL, Bosler EM, Hanrahan JP, et al. Spirochetes isolated from the blood of two patients with Lyme disease. N Engl J Med 1983; 308:740–742. [DOI] [PubMed] [Google Scholar]
- 90.Burgdorfer W, Barbour AG, Hayes SF, et al. Lyme disease—a tick-borne spirochetosis? Science 1982;216:1317–1319. [DOI] [PubMed] [Google Scholar]
- 91.Steere AC, Grodzicki RL, Kornblatt AN, et al. The spirochetal etiology of Lyme disease. N Engl J Med 1983;308:733–740. [DOI] [PubMed] [Google Scholar]
- 92.Sonenshine DE. Range expansion of tick disease vectors in North America: implications for spread of tick-borne disease. Int J Environ Res Public Health 2018;15 pii: E478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Fukunaga M, Takahashi Y, Tsuruta Y, et al. Genetic and phenotypic analysis of Borrelia miyamotoi sp. nov., isolated from the ixodid tick Ixodes persulcatus, the vector for Lyme disease in Japan. Int J Syst Bacteriol 1995;45:804–810. [DOI] [PubMed] [Google Scholar]
- 94.Molloy PJ, Telford SR III, Chowdri HR, et al. Borrelia miyamotoi disease in the northeastern United States: a case series. Ann Intern Med 2015;163:91–98. [DOI] [PubMed] [Google Scholar]
- 95.Platonov AE, Karan LS, Kolyasnikova NM, et al. Humans infected with relapsing fever spirochete Borrelia miyamotoi, Russia. Emerg Infect Dis 2011;17:1816–1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Jiang BG, Jia N, Jiang JF, et al. Borrelia miyamotoi Infections in humans and ticks, northeastern China. Emerg Infect Dis 2018;24: 236–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Krause PJ, Fish D, Narasimhan S, Barbour AG. Borrelia miyamotoi infection in nature and in humans. Clin Microbiol Infect 2015;21: 631–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Boden K, Lobenstein S, Hermann B, et al. Borrelia miyamotoi-associated neuroborreliosis in immunocompromised person. Emerg Infect Dis 2016;22:1617–1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hovius JW, de Wever B, Sohne M, et al. A case of meningoencephalitis by the relapsing fever spirochaete Borrelia miyamotoi in Europe. Lancet 2013;382:658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gugliotta JL, Goethert HK, Berardi VP, Telford SR III. Meningoencephalitis from Borrelia miyamotoi in an immunocompromised patient. N Engl J Med 2013;368:240–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dahlgren FS, Heitman KN, Drexler NA, et al. Human granulocytic anaplasmosis in the United States from 2008 to 2012: a summary of national surveillance data. Am J Trop Med Hyg 2015;93:66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dahlgren FS, Heitman KN, Behravesh CB. Undetermined human ehrlichiosis and anaplasmosis in the United States, 2008–2012: a catch-all for passive surveillance. Am J Trop Med Hyg 2016;94: 299–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Park J, Choi KS, Grab DJ, Dumler JS. Divergent interactions of Ehrlichia chaffeensis- and Anaplasma phagocytophilum-infected leukocytes with endothelial cell barriers. Infect Immun 2003;71: 6728–6733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Choi KS, Garyu J, Park J, Dumler JS. Diminished adhesion of Anaplasma phagocytophilum-infected neutrophils to endothelial cells is associated with reduced expression of leukocyte surface selectin. Infect Immun 2003;71:4586–4594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Dunn BE, Monson TP, Dumler JS, et al. Identification of Ehrlichia chaffeensis morulae in cerebrospinal fluid mononuclear cells. J Clin Microbiol 1992;30:2207–2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ratnasamy N, Everett ED, Roland WE, et al. Central nervous system manifestations of human ehrlichiosis. Clin Infect Dis 1996;23: 314–319. [DOI] [PubMed] [Google Scholar]
- 107.Davis LE, Paddock CD, Childs JE. Ehrlichiosis and the nervous system In: Davis LE, Kennedy PGE, eds. Infectious diseases of the nervous system. Oxford, UK: Butterworth-Heinemann, 2000:499–520. [Google Scholar]
- 108.McLean DM, Donohue WL. Powassan virus: isolation of virus from a fatal case of encephalitis. Can Med Assoc J 1959;80:708–711. [PMC free article] [PubMed] [Google Scholar]
- 109.Krow-Lucal ER, Lindsey NP, Fischer M, Hills SL. Powassan virus disease in the United States, 2006–2016. Vector Borne Zoonotic Dis 2018;18:286–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Piantadosi A, Rubin DB, McQuillen DP, et al. Emerging cases of Powassan virus encephalitis in New England: clinical presentation, imaging, and review of the literature. Clin Infect Dis 2016;62: 707–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Telford SR III, Armstrong PM, Katavolos P, et al. A new tick-borne encephalitis-like virus infecting New England deer ticks, Ixodes dammini. Emerg Infect Dis 1997;3:165–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Tavakoli NP, Wang H, Dupuis M, et al. Fatal case of deer tick virus encephalitis. N Engl J Med 2009;360:2099–2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Solomon IH, Spera KM, Ryan SL, et al. Fatal Powassan encephalitis (deer tick virus, lineage II) in a patient with fever and orchitis receiving rituximab. JAMA Neurol 2018;75:746–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Cavanaugh CE, Muscat PL, Telford SR III, et al. Fatal deer tick virus infection in Maine. Clin Infect Dis 2017;65:1043–1046. [DOI] [PubMed] [Google Scholar]
- 115.Dupuis AP Jr, Peters RJ, Prusinski MA, et al. Isolation of deer tick virus (Powassan virus, lineage II) from Ixodes scapularis and detection of antibody in vertebrate hosts sampled in the Hudson Valley, New York State. Parasit Vectors 2013;6:185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Frost HM, Schotthoefer AM, Thomm AM, et al. Serologic evidence of Powassan virus infection in patients with suspected Lyme disease. Emerg Infect Dis 2017;23:1384–1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cimperman J, Maraspin V, Lotric-Furlan S, et al. Concomitant infection with tick-borne encephalitis virus and Borrelia burgdorferi sensu lato in patients with acute meningitis or meningoencephalitis. Infection 1998;26:160–164. [DOI] [PubMed] [Google Scholar]
- 118.Cimperman J, Maraspin V, Lotric-Furlan S, et al. Double infection with tick borne encephalitis virus and Borrelia burgdorferi sensu lato. Wien Klin Wochenschr 2002;114:620–622. [PubMed] [Google Scholar]
- 119.Holub M, Kluckova Z, Beran O, et al. Lymphocyte subset numbers in cerebrospinal fluid: comparison of tick-borne encephalitis and neuroborreliosis. Acta Neurol Scand 2002;106:302–308. [DOI] [PubMed] [Google Scholar]
- 120.Engman ML, Lindstrom K, Sallamba M, et al. One-year follow-up of tick-borne central nervous system infections in childhood. Pediatr Infect Dis J 2012;31:570–574. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


