Abstract
Background
The emergence of coronary heart disease is increased with menopause, physical inactivity and with dyslipidemia. Physical training is known to promote the improvement of cardiovascular functions.
Objective
To investigate the effects of aerobic physical training on the left ventricle in ovariectomized LDL knockout mice.
Methods
Thirty animals were divided into 6 groups (n = 5): Sedentary non-ovariectomized control; Sedentary ovariectomized control; Trained ovariectomized control; Sedentary non-ovariectomized LDL-knockout, sedentary ovariectomized LDL-knockout and trained ovariectomized LDL-knockout. We analyzed the average parameters of apparent density of collagen fibers types I and III, and metalloproteinase type 2 and type 9, were considered significant p < 0.05.
Results
The results showed that the proposed exercise protocol altered the volume of type I collagen fibers, altered collagen remodeling parameters (MMP-2), and also reduced the 8-hydroxy-2’-deoxyguanosine (8OHdG) oxidative stress parameter.
Conclusion
Moderate intensity aerobic training acts on collagen fiber volume, on collagen remodeling with the reduction of oxidative stress in the left ventricles of ovariectomized LDL-knockout mice.
Keywords: Coronary Artery Disease, Exercise, Menopause, Dyslipidemias, Motor Activity, Collagen, Oxidative Stress, Inflammation, Mice
Introduction
During the aging process, menopausal women are at increased risk of developing conditions such as dyslipidemia, hypertension, insulin resistance and changes in body composition, where lifestyle and sedentarism are associated with a higher prevalence of the development of cardiovascular disease (CD).1,2
The aging process is associated with increased oxidative stress resulting in damage of several cell macromolecules, partly due to decreased antioxidant capacity as well as reduced repair capacity, resulting in increased susceptibility to apoptosis.3,4 Particularly in menopausal women, neuroendocrine alterations affect the functionality, metabolic capacity and antioxidant activity of numerous organs, especially due to the lack of estrogen, considered a female antioxidant, resulting in an additional increase of oxidative stress.5
Lipid metabolism is also influenced by physiological changes during menopause resulting in an increase in LDL and a decrease in HDL and contributes to the emergence of cardiovascular diseases.6,7 When compared to men of the same age, postmenopausal women are at an increased risk of developing heart disease.8,9 It is one of the main causes of morbidity and mortality in this physiological stage.10
Regular physical activity relieves the effects of aging and menopause and improves aerobic fitness, maintaining body weight index of visceral fat, plasma lipid levels, increased insulin sensitivity, increased baroreflex sensitivity and improved endothelial function, capillary wall shear stress which results in increased blood flow, stimulating nitric oxide release.11-13 These factors promote a better health-related quality of life and prolong survival and can be considered essential non-pharmacological standards in the treatment of postmenopausal effects and other physiological and pathological conditions.14,15
The objective of this study is to analyze the effects of aerobic physical training on the left ventricle in ovariectomized wildtype and LDLr knockout female mice on the following parameters: volume density of types I and III collagen fibers, metalloproteinases type 2 and type 9 expression, in addition to COX2 and 8-OhdG expression.
Methods
Animals
Thirty female mice aged 10 months were used: 15 genetically modified female mice, with knockout of the low-density lipoprotein receptor (LDLr Knockout), and 15 female wildtype mice (C57BL/6J) obtained from the University of São Paulo vivarium. The animals were kept in a USJT vivarium at a controlled temperature (22-24°C) and lighting (12 hours of light cycle and 12 hours of dark) receiving commercial feed (NUVILAB CR1, Nuvital Nutrients LTDA, Curitiba, PR) and water "ad libitum". The animals were divided into 6 groups (n = 5): sedentary non-ovariectomized control (CS), sedentary ovariectomized control (COS); trained ovariectomized control (COT); non-sedentary ovariectomized LDL knockout (LDL-S), sedentary ovariectomized LDL knockout (LDL-OS) and trained ovariectomized LDL knockout (LDL-OT). The division of the animals in the groups was performed by convenicence.
The experimental protocol was approved by the Research Ethics Committee of Universidade São Judas Tadeu (CEP-Protocol: 058/2007) and the research was conducted according to the Principles of Laboratory Animal Care formulated by the National Institutes of Health.
Ovariectomy
At nine months of age animals underwent the ovariectomy procedure. The animals were anesthetized with a ketamine and xylazine solution (120:20 mg/Kg, im) and placed in supine position and a small incision in the lower third of the abdominal region, parallel to the line of the body, was made. The ovaries, the uterine horns, and the blood vessels were located, sectioned, and removed. After that, the musculature and the skin were sutured. Confirmation of the efficacy of the ovariectomy was determined through colpocytology of the vaginal secretion performed over four consecutive days. On the last day of analysis, euthanasia was performed on these animals.16
Training Protocol
Maximal training Test
A maximal training test was performed on all the groups at the beginning and at the end of the exercise training program. The test consists of placing the animal to run on an ergometric treadmill at 0.3 km/h for 3 minutes, and this workload was increased by 0.3 km/h every 3 minutes until the animal reached exhaustion. The time of the test and the speed of the last workload were noted and served to determine the mean value of aerobic capacity of each group.
Exercise training
Exercise training began 7 days after the ovariectomy surgery; the trained groups were subjected to a physical training protocol on an ergometric treadmill at low-moderate intensity (≈50% to 70% maximal running speed) for 1 hour a day, 5 days a week, for 4 weeks, with a gradual increase in speed from 0.3 to 1.2 km/h. The animals were adapted to the treadmill for 10 minutes on three days prior to beginning the training.
Euthanasia and tissue preparation
At the end of the training the animals were sacrificed by decapitation. A thoracotomy was performed in which the heart and atria were removed and the right and left ventricles were sectioned. Left ventricle samples were fixed in 10% buffered formalin for 24 hours. Afterwards, the tissue was transferred to a 70% ethyl alcohol solution, dehydrated in increasing ethanol series, diaphanized in xylol and embedded in paraffin. Non-serial, 5 µm thick cuts were performed in which each section received a total of 6 cuts. The sections were stained with the Picrosirius technique, for the analysis of collagen fibers I and III in the left ventricle and visualized by polarized light microscopy.
The volume density of collagen fibers I and III (Vv[fc]) expresses the fraction of the volume occupied by the collagen fibers in relation to the total volume of the analyzed image. For this analysis, the test system was used with a total of 475 points, which corresponds to 100% of the image, using the program Image J. (version 1.47 - National Intitutes of Health-(Collins).
Immunohistochemistry
For the immunohistochemical techniques, 3 to 4 micrometer thick cuts were made and mounted on slides previously silanized using 4% silane. After the slides were dewaxed, using a heating oven overnight set at 57ºC, after which they were immersed in xylol baths for 30 minutes. Afterwards, they were hydrated in ethyl alcohol with decreasing concentrations of 100%, 80% and 70%, each with a duration of 5 minutes, then washed in running water. In the next step, the antigenic recovery was performed in a water bath at 90°C, the slides were placed in citrate buffer for 30 minutes, then washed in running water. Endogenous peroxidase blockade was performed in H2O2 for 15 minutes, followed by washing in distilled running water and in PBS pH = 7.4. For each slide, a specific antibody was used, table 1, and the antibody was placed overnight in a humid chamber at 4°C. The material was washed with PBS buffer and incubated with a biotinylated secondary antibody for 30 minutes, washed again with PBS and incubated with a streptoavidin-peroxidase antibody for another 30 minutes. A chromogenic substrate, DAB (33-Diaminobenzidine) solution in the ratio of 1:1 were used for five minutes at room temperature to wash with PBS solution and to reveal the reaction. When the presence of a dark brown precipitate was observed the slides were placed in running water, after which they were counterstained with "Hematoxylin Harrys" for 2 minutes. Afterwards, they were submitted to 3 xylol baths to diafieze and to 2 alcohol baths. The slides were mounted with coverslips and Entellan®.
Table 1.
Antibodies used for protein detection
| Antibody | Dilution | Labeling | Function | Manufacturer |
|---|---|---|---|---|
| MMP2 | 1:250 | Cytoplasm | Collagen remodelling | sc-10736, Santa Cruz® |
| MMP9 | 1:300 | Cytoplasm | Collagen remodelling | sc-6840, Santa Cruz® |
| COX 2 | 1:100 | Cytoplasm | Inflammation | sc-1745 P, Santa Cruz® |
| 8-OHdG | 1:100 | Cytoplasm | Oxidative stress | sc-66036, Santa Cruz® |
In all the techniques, observing the presence of a dark brown precipitate, the sample was visualized under an optical microscope. A quantitative analysis of the images was performed using the program ImageLab 2000, where the brown markers were selected and the program quantified immunoexpression intensity, figure 1.
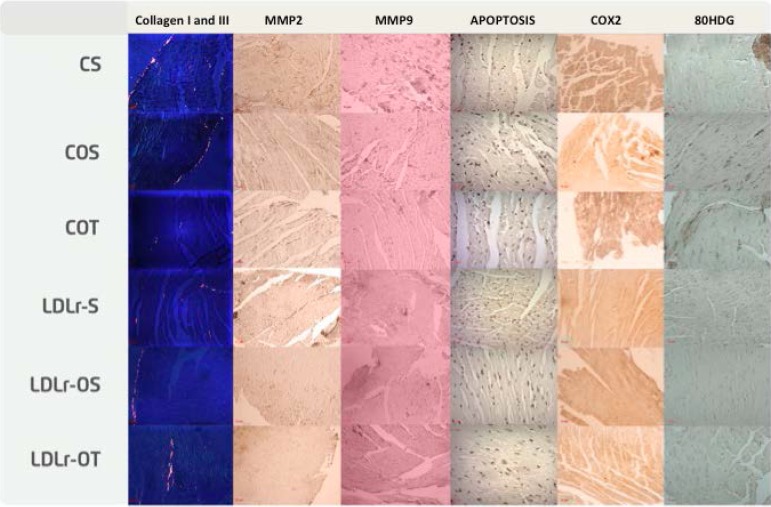
Figure 1.
Immunoexpression of proteins. CS: sedentary non-ovariectomized control; COS: sedentary ovariectomized control; COT: trained ovariectomized control; LDLr-S non-sedentary ovariectomized knockout; LLr-OS: sedentary ovariectomized LDL knockout; LDLr-OT: trained ovariectomized LDL knockout.
Statistical analysis
Absolute and relative values were used to describe the qualitative variables. For the quantitative variables with normal distribution (Shapiro-Wilk > 0.05), mean, standard deviation, minimum and maximum were used, and for the variables with non-normal distribution (Shapiro-Wilk < 0.05), median and percentiles were used. To study the diferences between the variables with the groups, the Kruskal-Wallis and ANOVA tests were used, complemented by the Dunn test or Bonferroni. For all analyzes, a confidence level of 95% was used. The program utilized for these analyzes was Stata version 11.0. (StataCorp. 2009. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP.)
Results
Our data show a significant reduction in the volume density of type I collagen fibers in the ovariectomized dyslipidemic group (LDL-OS) (-51%). The LDL-OT group showed a decrease of 100% when compared to the COS group and a significant difference in relation to the COT and LDL-S groups. Table 2 shows the association of COX-2 and MMP9 expression variables and the density of type I collagen fibers in relation to the evaluated animal group.
Table 2.
Comparison of Cyclooxygenase-2, Volume Density of collagen fibers I and Metalloproteinase type 9, with the groups studied. clinical variables with groups
| Variables | CS | COS | COT | LDL-S | LDL-OS | LDL-OT | p* |
|---|---|---|---|---|---|---|---|
| COX-2 | 35.0 (23.9; 46.3) | 46.5 (44.2; 79.7) | 46.1 (31.3; 47.7) | 47.7 (45.8; 63.1) | 87.8 (42.5; 92.4) | 49.4 (49.1; 50.9) | 0.232 |
| Vv [fc I] | 0.21 (0.21; 0.43) | 0.43 (0.21; 0.43) | - | - | 0.21 (0.0; 0.41)A,B,C | 0.0 (0.0; 0.21)A,B,C | < 0.001 |
| MMP9 | 44.7 (40.1; 44.8) | 40.9 (39.8; 45.6) | 53.9 (48.6; 66.2) | 53.0 (38.3; 58.1) | 42.2 (27.3; 53.7) | 64.1 (45.5; 93.9) | 0.169 |
Kruskal-Wallis. Data expressed as median and 25% and 75% percentiles. COX-2: Cyclooxygenase-2; Vv [fc I]: Volume Density of collagen fibers I; MMP 9: Metalloproteinase type 9; CS: sedentary non-ovariectomized control; COS: sedentary ovariectomized control; COT: trained ovariectomized control; LDL-S: non-sedentary ovariectomized LDL knockout; LDL-OS: sedentary ovariectomized LDL knockout; LDL-OT: trained ovariectomized LDL knockout.
statistically significant difference between the studied group and the COS group;
statistically significant difference between the studied group and the TOC group;
statistically significant difference between the studied group and the LDL-S group.
Regarding metalloproteinase type 2 expression, in the control group (CS) there was a significant increase of 24% in the ovariectomized group (COS), when physical training (COT) was performed there was an increase of 72%, and with dyslipidemia (LDL-S), the increase was 92%. In the dyslipidemic group with ovariectomy (LDL-OS), the values decrease 27% in relation to the LDL-S group and 18% in relation to the COT group, but still above the values of the control groups by 42% in relation to the CS group and 14% in relation to the COS group. When the training was performed in the ovariectomized dyslipidemic group LDL-OT, the results obtained present a 15% increase in relation to the sedentary ovariectomized LDL-OS group and a 15% decrease in relation to the LDL-S group. When compared to the control group, there was an increase of 64% in relation to the CS group, 32% in relation to the COS group and a decrease of 5% in relation to the COT group.
When analyzing the oxidative stress data, evaluating 8OHdG expression, there was a decrease in the indexes for the control group (CS), in which there was a decrease of 33% in the group with ovariectomy (COT) and a 39% decrease in the trained group. When dyslipidemia was present (LDL-S), there was a 51% decrease in relation to the CS group, and in the dyslipidemic group with ovariectomy (LDL-OS) there was a decrease of 85% in relation to the CS group, 78% in relation to the COS group, 76% in relation to the COT group and 70% in relation to the LDL-S group. When training was performed in the dyslipidemic ovariectomized group (LDL-OT), the data presented a 152% increase in relation to the LDL-OS group and a decrease in relation to the control groups, with 63% for the CS group, 45% for the COS group and 40% for the COT group. For the parameters related to volume density of type III collagen fibers, metalloproteinase type 9 and inflammation (COX2), the values obtained for the control and dyslipidemic groups do not present significant differences in any parameter, table 3.
Table 3.
Comparison of the variables Metalloproteinase type 2, Anti-8-Hydroxydeoxyguanosine and Volume Density of collagen fibers III (Vv [fc III]), with the groups studied.
| Variables | CS | COS | COT | LDL-S | LDL-OS | LDL-OT | p* |
|---|---|---|---|---|---|---|---|
| MMP 2 | 28.5 (4.0) | 35.3 (9.1)A | 49.0 (3.8)A | 54.8 (52.0)A | 40.5 (9.6)A,B,C,D | 46.8 (31.0)A,B,C,E | < 0.001 |
| 8-OHDg | 105.2 (7.6) | 70.0 (10.8)A | 64.9 (4.7)A | 51.7 (0.5)A | 15.3 (7.5)A,B,C,D | 38.7 (8.4)A,B,C,E | < 0.001 |
| Vv[fc III] | 0.007 (0.037) | 0.003 (0.024) | 0.016 (0.067) | 0.015 (0.057) | 0.013 (0.062) | 0.009 (0.043) | 0.649 |
ANOVA. Data expressed as mean and standard deviation.
statistically significant difference between the studied group and the CS group;
statistically significant difference between the studied group and the COS group;
statistically significant difference between the studied group and the TOC group;
statistically significant difference between the studied group and the LDL-S group;
statistically significant difference between the studied group and the LDL-OS group.
MMP2: Metalloproteinase type 2; 8OHdG: Anti-8-Hydroxydeoxyguanosine; Vv [fc III]: Volume Density of collagen fibers III; CS: sedentary non-ovariectomized control; COS: sedentary ovariectomized control; COT: trained ovariectomized control; LDL-S: non-sedentary ovariectomized LDL knockout; LDL-OS: sedentary ovariectomized LDL knockout; LDL-OT: trained ovariectomized LDL knockout.
Discussion
Physical activity is recognized as an important non-pharmacological treatment for numerous diseases and conditions, including dyslipidemia and menopause. Studies indicate that collagen fibers are present in the process of myocardial remodeling, which occur due to aging and other factors.17,18
Our data show that in the myocardium, the expression of type III collagen fibers did not differ between groups and parameters. In relation to type I collagen, ovariectomy and training brought a decrease in the levels presented in relation to the sedentary ovariectomized control group. Results similar to those found in our study verified the same variable in animals after a period of obesity induced by a diet rich in unsaturated fat.19 Interestingly, the findings reported in this article have similar results only with the proposed physical activity. Another study where acute myocardial infarction was induced in rats, the gradual increase of types I and III collagen was observed at 4 weeks. The kinetics of collagen I/III increase, in combination with the decrease of the elastic fibers in the infarcted area after an MI, provided evidence that impaired cardiac function after an MI was due to healing or infarct scar formation, with increased rigidity and less flexibility of the heart.20
Our results suggest that the aging period in this study does not appear to interfere with the increase in the expression of collagen fibers presented in other studies.21,22 However, when evaluating the LDL-OT groups, there is a clear reduction in the volume of type I collagen fibers. This verification was obtained using the proposed training protocol (intensity or duration).23,24
Metalloproteinase type 2 and type 9 also participate in the remodeling process of cardiac tissue, and are present in several pathologies such as inflammatory and cardiovascular diseases, among other injuries.24-29 The expression of metalloproteinase type 9 did not differ between groups and parameters. Regarding metalloproteinase type 2, an increase was shown in the control group with ovariectomy and physical training even in the presence of dyslipidemia. This process explains the factor with the collagen indexes when these are not elevated, because the degradation of collagen and the extracellular matrix is peformed by the action of the metalloproteinases.25,30-32 The elevated presence of MMPs in patients with dyslipidemias found in some studies suggest their participation in the matrix degradation process in atherosclerotic plaques and in the ruptures of these and with exposure of the nucleus17,33 and are independent predictors for the progression of kidney disease and are independently associated with an increased risk of mortality.34
The expression of COX2 in our study did not present statistical significance, indicating that in all groups and parameters, there were no changes for these data. Thus, in this parameter chosen to verify inflammation, no changes are observed showing that the factors associated with the groups do not interfere in such an evaluation.
Aging, menopause and dyslipidemia are factors that also result in oxidative stress.3-5 In our research, oxidative stress was verified through the expression of 8OHdG, and ovariectomy decreased the values of this parameter in the control and dyslipidemic groups, differing from the results obtained in other studies.5,35 When physical training was performed, the values were decreased in the control group, but in the dyslipidemic group, they presented an increase. Interestingly, this marker seems to have no association with the groups proposed in this experimental model.
Conclusion
The data of this research indicate that physical exercise beneficially influenced the control and dyslipidemic groups in the volume density parameter of type I collagen fibers and the control group in relation to oxidative stress.
Footnotes
Sources of Funding
There were no external funding sources for this study.
Study Association
This study is not associated with any thesis or dissertation work.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Universidade de São Judas Tadeu under the protocol number 058. All the procedures in this study were in accordance with the 1975 Helsinki Declaration, updated in 2013
Author contributions
Conception and design of the research: Brianezi L, Maifrino LBM; Acquisition of data: Brianezi L, Ornelas E, Sousa LVA; Analysis and interpretation of the data: Brianezi L, Ornelas E, Gehrke FS, Fonseca FLA, Sousa LVA, Souza J, Maifrino LBM; Statistical analysis: Brianezi L, Gehrke FS, Fonseca FLA, Souza J; Writing of the manuscript: Brianezi L, Ornelas E, Gehrke FS, Fonseca FLA, Alves BCA, Sousa LVA, Maifrino LBM; Critical revision of the manuscript for intellectual content: Gehrke FS, Fonseca FLA, Alves BCA, Maifrino LBM.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Zanesco A, Antunes E. Effects of exercise training on the cardiovascular system: pharmacological approaches. Pharmacol Ther. 2007;114(3):307–317. doi: 10.1016/j.pharmthera.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 2.Coylewright M, Reckelhoff JF, Ouyang P. Menopause and hypertension: an age-old debate. Hypertension. 2008;51(4):952–959. doi: 10.1161/HYPERTENSIONAHA.107.105742. [DOI] [PubMed] [Google Scholar]
- 3.Humphreys V, Martin RM, Ratcliffe B, Duthie S, Wood S, Gunnell D, et al. Age-related increases in DNA repair and antioxidant protection: a comparison of the Boyd Orr Cohort of elderly subjects with a younger population sample. Age Ageing. 2007;36(5):521–526. doi: 10.1093/ageing/afm107. [DOI] [PubMed] [Google Scholar]
- 4.Lee HC, Wei YH. Oxidative stress, mitochondrial DNA mutation, and apoptosis in aging. Exp Biol Med (Maywood) 2007;232(5):592–606. [PubMed] [Google Scholar]
- 5.David OJ, Ocwieja M, Meiser K, Emotte C, Jakab A, Wemer J, et al. Pharmacokinetics of fingolimod (FTY720) and a combined oral contraceptive coadministered in healthy women: drug-drug interaction study results. Int J Clin Pharmacol Ther. 2012;50(8):540–544. doi: 10.5414/CP201675. [DOI] [PubMed] [Google Scholar]
- 6.Gobal FA, Mehta JL. Management of dyslipidemia in the elderly population. Ther Adv Cardiovasc Dis. 2010;4(6):375–383. doi: 10.1177/1753944710385048. [DOI] [PubMed] [Google Scholar]
- 7.Ammar T. Effects of aerobic exercise on blood pressure and lipids in overweight hypertensive postmenopausal women. J Exerc Rehabil. 2015;11(3):145–150. doi: 10.12965/jer.150204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perrella J, Berco M, Cecutti A, Gerulath A, Bhavnani BR. Potential role of the interaction between equine estrogens, low-density lipoprotein (LDL) and high-density lipoprotein (HDL) in the prevention of coronary heart and neurodegenerative diseases in postmenopausal women. Lipids Health Dis. 2003 Jun 20;2:4–4. doi: 10.1186/1476-511X-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Irigoyen MC, Paulini J, Flores LJ, Flues K, Bertagnolli M, Moreira ED, et al. Exercise training improves baroreflex sensitivity associated with oxidative stress reduction in ovariectomized rats. Hypertension. 2005;46(4):998–1003. doi: 10.1161/01.HYP.0000176238.90688.6b. [DOI] [PubMed] [Google Scholar]
- 10.Valença CN, Nascimento Filho JM, Germano RM. Mulher no climatério: reflexões sobre desejo sexual, beleza e feminilidade. Saude Soc. 2010;19(2):273–285. [Google Scholar]
- 11.Mandarim-de-Lacerda CA, Pessanha MG. Stereology of the myocardium in embryos, fetuses and neonates of the rat. Acta Anat (Basel) 1995;154(4):261–266. doi: 10.1159/000147777. [DOI] [PubMed] [Google Scholar]
- 12.Maifrino LBM, Araújo RC, Faccini CC, Liberti EA, Gama EF, Ribeiro AA, et al. Effect of exercise training on aging-induced changes in rat papillary muscle. Arq Bras Cardiol. 2009;92(5):356–360. doi: 10.1590/s0066-782x2009000500009. 373-7. 387-92. [DOI] [PubMed] [Google Scholar]
- 13.Souza SB, Flues K, Paulini J, Mostarda C, Rodrigues B, Souza LE, et al. Role of exercise training in cardiovascular autonomic dysfunction and mortality in diabetic ovariectomized rats. Hypertension. 2007;50(4):786–791. doi: 10.1161/HYPERTENSIONAHA.107.095000. [DOI] [PubMed] [Google Scholar]
- 14.Silva AS, Zanesco A. Exercício físico, receptores: -adrenérgicos e resposta vascular. J Vasc Bras. 2010;9(2):47–56. [Google Scholar]
- 15.Morvan E, Lima NE, Machi JF, Mostarda C, De Angelis K, Irigoyen MC, et al. Metabolic, hemodynamic and structural adjustments to low intensity exercise training in a metabolic syndrome model. Cardiovasc Diabetol. 2013 Jun 18;12:89–89. doi: 10.1186/1475-2840-12-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marcondes FK, Bianchi FJ, Tanno AP. Determination of the estrous cycle phases of rats: some helpful considerations. Braz J Biol. 2002;62(4A):609–614. doi: 10.1590/s1519-69842002000400008. [DOI] [PubMed] [Google Scholar]
- 17.Biondo-Simões MLP, Alcantara EM, Dallagnol JC, Yoshizumi KO, Torres LFB, Borsato KS. Cicatrização de feridas: estudo comparativo em ratos hipertensos não tratados e tratados com inibidor da enzima conversora da angiotensina. Rev Col Bras Cir. 2006;33(2):74–78. [Google Scholar]
- 18.Tampelini FS. Efeito do exercício físico aeróbio sobre os componentes fibroelástico e colágeno da aorta de ratos normotensos e hipertensos, sedentários e treinados aorta de ratos normotensos e hipertensos. [2018 jan 12]. Internet. Disponível em: http://www.teses.usp.br/teses/disponiveis/42/42131/tde-30052008-120037/pt-br.php. [DOI]
- 19.Silva DCT, Lima-Leopoldo AP, Leopoldo AS, Campos DHS, Nascimento AF, Oliveira JSA, et al. Influência do tempo de exposição à obesidade induzida por dieta hiperlipídica sobre os colágenos Tipo I e III miocárdico. Arq Bras Cardiol. 2014;102(2):157–164. [Google Scholar]
- 20.Yu Y, Yin G, Bao S, Guo Z. Kinetic alterations of collagen and elastic fibres and their association with cardiac function in acute myocardial infarction. Mol Med Rep. 2018;17(3):3519–3526. doi: 10.3892/mmr.2017.8347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Camelliti P, Borg TK, Kohl P. Structural and functional characterization of cardiac fibroblasts. Cardiovasc Res. 2005;65(1):40–51. doi: 10.1016/j.cardiores.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 22.Masson S, Latinim R, Saliom M, Fiordaliso F. Razzaque MS. Fibrogenesis: Cellular and Molecular Basis. New York: Kluwer Academic Publishers; 2005. Cardiac fibrosis and aging; pp. 97–103. [Google Scholar]
- 23.Thomas DP, McCormick RJ, Zimmerman SD, Vadlamudi RK, Gosselin LE. Aging- and training-induced alterations in collagen characteristics of rat left ventricle and papillary muscle. Pt 2Am J Physiol. 1992;263(3):H778–H783. doi: 10.1152/ajpheart.1992.263.3.H778. [DOI] [PubMed] [Google Scholar]
- 24.Maifrino LBM, Araújo RC, Faccini CC, Liberti EA, Gama EF, Ribeiro AACM, et al. Efeito do treinamento físico em alterações induzidas pelo envelhecimento no musculo papilar do rato. Arq Bras Cardiol. 2009;92(5):387–392. doi: 10.1590/s0066-782x2009000500009. [DOI] [PubMed] [Google Scholar]
- 25.Polyakova V, Loeffler I, Hein S, Miyagawa S, Piotrowska I, Dammer S, et al. Fibrosis in endstage human heart failure: Severe changes in collagens metabolismo and MMP/TIMP profiles, Int. J Cardiol. 2011;151(1):18–33. doi: 10.1016/j.ijcard.2010.04.053. [DOI] [PubMed] [Google Scholar]
- 26.Nagase H, Visse R, Murphy G. Structure and function of matrix metalloproteinases and TIMPs. Cardiol Res. 2006;69:562–573. doi: 10.1016/j.cardiores.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 27.Geurts N, Opdenakker G, Van Den Steen P. Matrix Metalloproteinases as therapeutic targets in protozoan parasitic infections. Pharmacol Ther. 2012;133(3):257–279. doi: 10.1016/j.pharmthera.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 28.Kupai K, Szucs G, Cseh S, Hajdu I, Csonka C, Csont T, Ferdinandy P. Matrix metalloproteinase activity assays: Importance of zimography. J Pharmacol Toxicol Methods. 2010;61(2):205–209. doi: 10.1016/j.vascn.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 29.Viegas KAS. Ação da angiotensina II no remodelamento da matriz extracelular perivascular em camundongos. São Paulo:: Instituto de Ciências Biomédicas, Universidade de São Paulo; 2012. Tese. [Google Scholar]
- 30.Wu SY, Yu YR, Cai Y, Jia LX, Wang X, Xiao CS, et al. Endogenous aldosterone is involved in vascular calcification in rat. Exp Biol Med. 2012;237(1):31–37. doi: 10.1258/ebm.2011.011175. [DOI] [PubMed] [Google Scholar]
- 31.Parks WC, Mecham RP. Extracellular matrix degradation. New York: Springer; 2011. [Google Scholar]
- 32.Nascimento DC, Durigan RCM, Tibana RA, Durigan JLQ, Navalta JW, Prestes J. The Response of Matrix Metalloproteinase-9 and -2 to Exercise. Sports Med. 2015;45(2):269–278. doi: 10.1007/s40279-014-0265-8. [DOI] [PubMed] [Google Scholar]
- 33.Basalyga DM, Simionescu DT, Xiong W, Baxter BT, Starcher BC, Vyavahare NR. Elastin degradation and calcification in an abdominal aorta injury model: Role of matrix metalloproteinases. Circulation. 2004;110(22):3480–3487. doi: 10.1161/01.CIR.0000148367.08413.E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hsu T, Kuo K, Hung S, Huang PH, Chen JW, Tarng DC. Progression of kidney disease in non-diabetic patients with coronary artery disease: predictive role of circulating matrix metalloproteinase-2, -3, and -9. PLoS One. 2013;8(7):e70132. doi: 10.1371/journal.pone.0070132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dantas AP, Tostes RC, Forbes ZB, Costa SG, Nigro D, Carvalho MH. In vivo evidence for antioxidant potential of estrogen in microvessels of female spontaneously hypertensive rats. Pt 2Hypertension. 2002;39(2):405–411. doi: 10.1161/hy0202.102993. [DOI] [PubMed] [Google Scholar]