Abstract
Transition is an intrinsic process in the life of a patient with kidney disease and should be planned and anticipated when possible. A single therapy option might not be adequate across a patient’s entire lifespan and many patients will require a switch in their treatment modality to adapt the treatment to their clinical and psychosocial needs. There are several reasons behind changing a patient’s treatment modality, and the consequences of each decision should be evaluated, considering both short- and long-term benefits and risks. Dialysis modality transition is not only to allow for technical optimization or improved patient survival, the patient’s experience associated with the transition should also be taken into account. Transition should not be considered as treatment failure, but rather as an expected progression in the patient’s treatment options.
Keywords: home haemodialysis, integrated home dialysis model, planned transition, renal replacement therapy, transition
TRANSITION BETWEEN RENAL REPLACEMENT THERAPY OPTIONS
Every year, >120 000 Americans and ∼83 000 Europeans transition from non-dialysis-dependent chronic kidney disease to renal replacement therapy (RRT) [1–3]. A single therapy option might not be adequate across the entire lifespan of a patient with chronic kidney disease and many, especially young, patients will require a switch in modality to adapt the treatment to their clinical and psychosocial needs [4–7].
There are several reasons why a patient might change their treatment modality [1, 4–6, 8–12], including:
Previous modality failure, such as peritoneal dialysis (PD) failure or kidney graft failure
Unplanned dialysis start: patients with no pre-dialysis education who have not been informed about dialysis choices or patients who had an acute unplanned dialysis start and did not have the opportunity to initiate treatment in their chosen modality might wish to consider a different therapy option that better fits their lifestyle
Patients who have a change in lifestyle or circumstances or who wish to reconsider their initial modality choice
Medical situations that require a change in dialysis modality, such as peritonitis, vascular access problems or haemodynamic intolerance, or that require more frequent treatment prescriptions
Cessation of dialysis treatment to be replaced by kidney transplantation.
Depending on their specific circumstances, patients can switch between different RRT options, namely kidney transplantation, PD, facility haemodialysis (facility HD) and home haemodialysis (HHD), or opt for conservative management [1, 4]. The outcomes of each RRT option versus conservative management should be evaluated, considering short-term as well as long-term benefits and risks [4, 13]. In most cases, the need for a change in RRT option is predictable, thus providing an opportunity to pre-emptively prepare the patient, the family and the health care team [4, 5, 14], given that a planned transition has been associated with better patient outcomes compared with an unplanned change [1, 6, 14–16]. It is important to highlight that transition to another therapy option should not be considered as a ‘failure’ of treatment, but rather as an ‘expected progression’ in the patient’s treatment options. Transition should be considered as a ‘gradual move’ from one therapy option to another [14, 15].
It is well recognized that early kidney transplantation is the best RRT option for many patients with end-stage renal disease (ESRD). However, most patients will need to spend some time on dialysis prior to transplantation or when a transplant fails [4, 9, 10, 17, 18]. Time on the transplant waiting list can be variable, depending on the circumstances of each country. This implies that transition between dialysis modalities will be a reality for the majority of patients, especially those who face a long wait for transplantation or those for whom a kidney transplant is not possible.
The aim of this review is to address the specific situation of transition from different RRT options to HHD, emphasizing the challenges, benefits and characteristics of this transition from a previous RRT modality.
CHALLENGES IN THE TRANSITION TO HHD
Patients can experience the benefits of switching to HHD, regardless of their previous therapy. Some of these benefits are observed within the first 2–3 months of the transition, especially in patients with more intensive HD regimens [8, 19–21]. In general, most patients who want to change to HHD believe that this treatment option could offer them the opportunity to thrive, improving their freedom, flexibility and well-being [22]. However, certain aspects of HHD can lead to patient anxiety and fears at the time of transition to HHD. Therefore, when considering a change in treatment to HHD, it is important to mention not only the benefits, but also the challenges and risks that patients will face during this process [10, 13, 21–23].
It is essential to appreciate that each change (transition from pre-dialysis, facility HD or PD or due to kidney transplant failure) gives rise to different challenges and requires an individualized approach from the perspective of the patient, as well as of the health care professional, in each specific situation [4–6, 10, 11, 13, 15, 22–24].
When transitioning from pre-dialysis to HHD, it is essential that the patient receives appropriate education to increase their awareness of their condition and their acceptance of the need for RRT during their lifetime, while at the same time encouraging self-care [1, 4–6]. Additionally, the creation of the vascular access for the first time is part of the challenges patient will face during this stage. Probably this could be one of the less complicated transition since the patient does not compare HHD to any other RRT so it is easier to teach them anything from the beginning, which helps to better assimilate the change. On the other hand, transitioning from facility HD requires a significantly different mindset, which is a change from a ‘passive’ to a ‘proactive’ attitude, for both the patient and the health care team. The patient must learn to take control of and manage his/her own medical condition, while health care professionals must encourage and teach the patient self-care, which will enable the latter to be in control of his/her condition. Transitioning from PD to HHD would seem easier, as the patient is already performing self-dialysis care. However, the patient is required to learn new skills which are significantly more complex than those needed for PD. The main challenge for the health care team in this situation is to encourage the patient to continue home dialysis despite the increased complexity of the technique. Finally, managing transition from kidney transplantation back to dialysis poses a different set of challenges, especially as this transition is often psychologically difficult for the patient, so health-care team needs to provide patient support for this change while promoting patient self-care and education on HHD. Table 1 shows the challenges encountered when transitioning from different RRT options to HHD, from both the patient’s and the health care team’s perspective [4, 5, 9, 10, 13, 15, 16, 22–24].
Table 1.
Aspects of patient care to be addressed before transition to HHD
| Is HHD good for me? | Discuss with the patient the advantages and disadvantages of HHD as applicable to their own circumstances |
| Facing their fears | Explore the patient’s apprehensions and misapprehensions to enable the patient to face his/her fears |
| When? | Discuss the best timing for transition to avoid complications associated with prolonged renal malfunction (pre-dialysis stage or transplant failure) or prolonged situations of inadequate dialysis dose |
| How? |
|
Before commencing the transition process, we need to address several aspects of patient care and ensure the patient is appropriately educated and prepared to transition to or start HHD (Table 2) [4–6, 10, 12, 13, 15, 16, 22]. We need to discuss with the patient the advantages and disadvantages of HHD, as applicable to the patient’s circumstances, explore the patient’s apprehensions and misconceptions about HHD in order to address these concerns and fears and ensure a timely transition in order to avoid complications associated with prolonged periods of graft failure, the pre-dialysis stage or inadequate dialysis dose. It is important that the logistics of the transition are addressed, including vascular access preparation (especially in ESRD, PD or transplanted patients with no vascular access), in addition to ensuring all necessary home adaptations are in place for this treatment (including adequate space and specific HHD equipment) as well as explaining when and how patient training will be delivered. Through appropriate planning, we can improve patient acceptance and increase the likelihood of a successful transition [12, 15, 16, 22, 23].
Table 2.
Challenges when transitioning to HHD
| Transition to HHD | Patient perspective | Health care staff perspective |
|---|---|---|
| From pre-dialysis |
Psychological acceptance:
|
|
|
| ||
| From facility HD |
Fear of:
|
Helping the patient:
|
|
| ||
| From failed PD |
Fear of:
|
Encouraging the patient to continue treatment in a home-based setting, although this change will be difficult at the beginning, given PD is a much simpler technique in all aspects, compared with HHD
|
|
| ||
| From failed transplant | Fear of:
|
|
Each change (transition from pre-dialysis, facility HD or PD or due to kidney transplant failure) gives rise to different challenges and requires an individualized approach from the different perspectives of the patient and health care professionals in each specific situation.
Therefore the health care team needs to consider not only the transition process between RRT options as a means for technical optimization or improved patient survival, but also the patient’s experience associated with this transition, always taking into account the impact of this change on the patient’s life [7].
THE ‘INTEGRATED HOME DIALYSIS MODEL’
Over the last decade there has been increasing interest in home dialysis therapies, largely due to the mounting evidence that home dialysis, including PD and HHD, represents an important alternative to facility HD that is cost effective and patient-centred, with multiple benefits related to patient outcomes, including improved quality of life and increased patient survival [8, 12, 18, 21, 25–28]. However, despite those benefits, both PD and HHD remain underused worldwide [2, 3, 16].
PD is being increasingly recognized as a first-choice modality of RRT. Potential advantages of a ‘PD first’ model include technique simplicity and low costs, associated not only with better the preservation of residual kidney function, but also with the protection of potential vascular access, lifestyle maintenance with minimal disruption, flexible dialysis schedules and patient outcomes equivalent or superior to conventional in-centre HD, particularly in the first 2–3 years [7, 12, 26, 29–31]. However, PD is not always feasible, due to medical contraindications or, in the majority of cases, because continuation of PD beyond the first few years is often limited by PD technique failure [10, 27, 30–32]. In these situations, HHD plays a fundamental role as the other home-based dialysis alternative, offering these patients the opportunity to begin or to remain at home. HHD is a unique modality that allows individualized treatment and, specifically, increased treatment intensity beyond what is typically feasible in the centre setting; with multiple benefits related to patient survival especially when prescribing more intensive regimens [8, 18–21, 33–36].
The integrated home dialysis model (Figure 1) involves the initiation of PD, followed by a timely transition to HHD at the time of PD completion [12, 32]. PD and HHD patients share similar profiles; both groups are used to self-care and value the benefits of home-based dialysis therapies, particularly improved quality of life, with the main difference in their treatment being the dialysis technique. This approach could represent a natural treatment evolution, with a patient first starting at home with a simple technique (PD) and subsequently needing to change over time to a more complex technique (HD), while still remaining in the same home environment.
FIGURE 1.
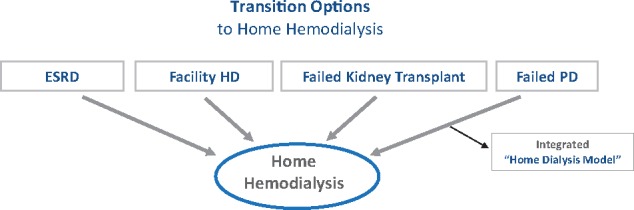
Transition options to Home Hemodialysis. Patients in HHD come from all RRT alternatives. The ‘integrated home dialysis model’ involves the initiation of PD followed by transition to HHD at the time of PD completion; thus offering an alternative to patients so they can remain at home.
There is little information on dialysis transition between home-based therapies [15, 30–32]. However, evidence has shown that, among patients undergoing RRT, those who start on PD and then transition to HHD have some of the best outcomes by maximizing the benefits from home-based dialysis therapy while still capitalizing on the putative early advantages of PD and the potential survival advantages afforded by HHD [31, 32]. Therefore HHD should be strongly considered for most PD patients in need of a new dialysis modality after PD [31], with the integrated home dialysis model as an expected progression in the patient’s treatment options, a gradual move from one therapy option to another [14]. This model should also be considered as an ideal dialysis strategy, especially if a kidney transplant is unavailable or there is a long waiting time on the kidney transplant list [7, 12, 30].
PD patients are already adapted to home dialysis and have gained prior education in self-management. Therefore it would seem natural that HHD would be a preferred modality following PD technique failure [12]. However, the actual conversion rate among patients from PD to HHD remains low, with the majority of patients transferring to facility HD when PD treatment can no longer continue [12, 30]. This fact demonstrates that we are still missing opportunities to facilitate treatment continuation at home and shows that there are still many barriers that we need to overcome to facilitate this transition [12, 16, 21, 25, 30].
CONCLUSION
Every patient with ESRD should have a life plan according to his/her individual circumstances and needs. Inherent in this approach is the understanding that patients are likely to change or transition between RRT options. Therefore these transitions should be planned and anticipated, when possible, to facilitate patient acceptance and improve patient outcomes. It is essential that the issue of potential transition between treatment modalities is introduced early in the patient’s journey, so that transition is viewed as an expected part of their therapy for renal failure rather than as a failure of treatment.
In light of all the benefits that HHD offers, we should encourage patients already using home-based therapies, such as PD, who need to transition to HD to continue treatment at home via the integrated home dialysis model, where this change should be considered as an expected progression in the patient’s treatment options. The health care team needs to consider not only the transition process between RRT options as a means for technical optimization or improved patient survival, but also the patient’s experience associated with the transition, and should understand the risks and benefits of each change, always taking into account the impact of the transition on the patient’s life.
ACKNOWLEDGEMENTS
We would like to thank Joaquin Manrique for his collaboration and contributions in reviewing this article.
CONFLICT OF INTEREST STATEMENT
All the authors are part of NxStage European Medical Advisory Board.
REFERENCES
- 1. Kalantar-Zadeh K, Kovesdy CP, Streja E. et al. Transition of care from pre-dialysis prelude to renal replacement therapy: the blueprints of emerging research in advanced chronic kidney disease. Nephrol Dial Transplant 2017; 32: ii91–ii98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kramer A, Pippias M, Noordzij M. et al. The European Renal Association–European Dialysis and Transplant Association (ERA-EDTA) Registry Annual Report 2016: a summary. Clin Kidney J 2019; 12: 702–720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Saran R, Robinson B, Abbott KC. et al. US Renal Data System 2018 Annual Data Report: epidemiology of kidney disease in the United States. Am J Kidney Dis 2019; 73: A7–A8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Covic A, Bammens B, Lobbedez T. et al. Educating end-stage renal disease patients on dialysis modality selection: clinical advice from the European Renal Best Practice (ERBP) Advisory Board. Nephrol Dial Transplant 2010; 25: 1757–1759 [DOI] [PubMed] [Google Scholar]
- 5. Moist LM, Lok CE.. Incident dialysis access in patients with end-stage kidney disease: what needs to be improved. Semin Nephrol 2017; 37: 151–158 [DOI] [PubMed] [Google Scholar]
- 6. Chan CT, Blankestijn PJ, Dember LM. et al. Dialysis initiation, modality choice, access, and prescription: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int 2019; 96: 37–47 [DOI] [PubMed] [Google Scholar]
- 7. Lambie M, Davies SJ.. Transition between home dialysis modalities: another piece in the jigsaw of the integrated care pathway. Nephrol Dial Transplant 2015; 30: 1781–1783 [DOI] [PubMed] [Google Scholar]
- 8. Lockridge R, Cornelis T, Van Eps C.. Prescriptions for home hemodialysis. Hemodial Int 2015; 19(Suppl 1): S112–S127 [DOI] [PubMed] [Google Scholar]
- 9. Molnar MZ, Ichii H, Lineen J. et al. Timing of return to dialysis in patients with failing kidney transplants. Semin Dial 2013; 26: 667–674 [DOI] [PubMed] [Google Scholar]
- 10. Walker RC, Blagg CR, Mendelssohn DC.. Systems to cultivate suitable patients for home dialysis. Hemodial Int 2015; 19 (Suppl 1): S52–S58 [DOI] [PubMed] [Google Scholar]
- 11. Bowman B, Zheng S, Yang A. et al. Improving incident ESRD care via a transitional care unit. Am J Kidney Dis 2018; 72: 278–283 [DOI] [PubMed] [Google Scholar]
- 12. McCormick BB, Chan CT, Group OHDR. Striving to achieve an integrated home dialysis system: a report from the Ontario Renal Network Home Dialysis Attrition Task Force. Clin J Am Soc Nephrol 2018; 13: 468–470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bennett PN, Schatell D, Shah KD.. Psychosocial aspects in home hemodialysis: a review. Hemodial Int 2015; 19(Suppl 1): S128–S134 [DOI] [PubMed] [Google Scholar]
- 14. Burkart J. Transitions from PD are expected. Why not continue at home? Perit Dial Int 2007; 27: 645–646 [PubMed] [Google Scholar]
- 15. Chan C, Combes G, Davies S. et al. Transition between different renal replacement modalities: gaps in knowledge and care–the Integrated Research Initiative. Perit Dial Int 2019; 39: 4–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chan CT, Wallace E, Golper TA. et al. Exploring barriers and potential solutions in home dialysis: an NKF-KDOQI Conference outcomes report. Am J Kidney Dis 2019; 73: 363–371 [DOI] [PubMed] [Google Scholar]
- 17. Gill JS, Rose C, Pereira BJ. et al. The importance of transitions between dialysis and transplantation in the care of end-stage renal disease patients. Kidney Int 2007; 71: 442–447 [DOI] [PubMed] [Google Scholar]
- 18. Miller AJ, Perl J, Tennankore KK.. Survival comparisons of intensive vs. conventional hemodialysis: pitfalls and lessons. Hemodial Int 2018; 22: 9–22 [DOI] [PubMed] [Google Scholar]
- 19. Cherukuri S, Bajo M, Colussi G. et al. Home hemodialysis treatment and outcomes: retrospective analysis of the Knowledge to Improve Home Dialysis Network in Europe (KIHDNEy) cohort. BMC Nephrol 2018; 19: 262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. François K, Ghazan-Shahi S, Chan CT.. Modalities and prescribing strategies in intensive home hemodialysis: a narrative review. Minerva Urol Nefrol 2015; 67: 75–84 [PubMed] [Google Scholar]
- 21. Karkar A, Hegbrant J, Strippoli GF.. Benefits and implementation of home hemodialysis: a narrative review. Saudi J Kidney Dis Transpl 2015; 26: 1095–1107 [DOI] [PubMed] [Google Scholar]
- 22. Walker RC, Hanson CS, Palmer SC. et al. Patient and caregiver perspectives on home hemodialysis: a systematic review. Am J Kidney Dis 2015; 65: 451–463 [DOI] [PubMed] [Google Scholar]
- 23. Rioux JP, Marshall MR, Faratro R. et al. Patient selection and training for home hemodialysis. Hemodial Int 2015; 19(Suppl 1): S71–S79 [DOI] [PubMed] [Google Scholar]
- 24. Jayanti A, Foden P, Mitra S. et al. Multidisciplinary staff attitudes to home haemodialysis therapy. Clin Kidney J 2017; 10: 269–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pommer W, Wagner S, Müller D. et al. Attitudes of nephrologists towards assisted home dialysis in Germany. Clin Kidney J 2018; 11: 400–405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ghaffari A, Kalantar-Zadeh K, Lee J. et al. PD first: peritoneal dialysis as the default transition to dialysis therapy. Semin Dial 2013; 26: 706–713 [DOI] [PubMed] [Google Scholar]
- 27. Trinh E, Hanley JA, Nadeau-Fredette AC. et al. A comparison of technique survival in Canadian peritoneal dialysis and home hemodialysis patients. Nephrol Dial Transplant 2019. 10.1093/ndt/gfz075 [DOI] [PubMed] [Google Scholar]
- 28. Perl J, Dember LM, Bargman JM. et al. The use of a multidimensional measure of dialysis adequacy-moving beyond small solute kinetics. Clin J Am Soc Nephrol 2017; 12: 839–847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nadeau-Fredette AC, Hawley CM, Pascoe EM. et al. An incident cohort study comparing survival on home hemodialysis and peritoneal dialysis (Australia and New Zealand Dialysis and Transplantation Registry). Clin J Am Soc Nephrol 2015; 10: 1397–1407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nadeau-Fredette AC, Hawley C, Pascoe E. et al. Predictors of transfer to home hemodialysis after peritoneal dialysis completion. Perit Dial Int 2016; 36: 547–554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nadeau-Fredette AC, Bargman JM, Chan CT.. Clinical outcome of home hemodialysis in patients with previous peritoneal dialysis exposure: evaluation of the integrated home dialysis model. Perit Dial Int 2015; 35: 316–323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nadeau-Fredette AC, Chan CT, Cho Y. et al. Outcomes of integrated home dialysis care: a multi-centre, multi-national registry study. Nephrol Dial Transplant 2015; 30: 1897–1904 [DOI] [PubMed] [Google Scholar]
- 33. McCullough PA, Chan CT, Weinhandl ED. et al. Intensive hemodialysis, left ventricular hypertrophy, and cardiovascular disease. Am J Kidney Dis 2016; 68(5 Suppl 1): S5–S14 [DOI] [PubMed] [Google Scholar]
- 34. Morfin JA, Fluck RJ, Weinhandl ED. et al. Intensive hemodialysis and treatment complications and tolerability. Am J Kidney Dis 2016; 68(5 Suppl 1): S43–S50 [DOI] [PubMed] [Google Scholar]
- 35. Copland M, Komenda P, Weinhandl ED. et al. Intensive hemodialysis, mineral and bone disorder, and phosphate binder use. Am J Kidney Dis 2016; 68(5 Suppl 1): S24–S32 [DOI] [PubMed] [Google Scholar]
- 36. Tennankore KK, Kim SJ, Baer HJ. et al. Survival and hospitalization for intensive home hemodialysis compared with kidney transplantation. J Am Soc Nephrol 2014; 25: 2113–2120 [DOI] [PMC free article] [PubMed] [Google Scholar]


