ABSTRACT
Objectives: To compare the performance of cervical stabilizer muscles using the craniocervical flexion test (CCFT) among individuals with subacute, chronic, and asymptomatic low back pain (LBP) conditions.
Methods: Individuals with subacute (N = 23) and chronic LBP (N = 23) with their age- and gender-matched controls (N = 30) participated in this study. All recruited participants were required to perform the CCFT. The activation score (AS) and the performance index (PI) were recorded by an assessor who was blinded to the group of participants.
Results: Approximately, 74% of subacute LBP participants and 60–65% of chronic LBP participants obtained abnormal AS and PI. AS was significantly lower in participants with subacute (P = 0.0002) and chronic LBP (P = 0.0009) than the control group. Likewise, the PI was significantly lower in participants with subacute (P = 0.0002) and chronic LBP (P = 0.0036) than the control group. Participants in the subacute LBP group showed significantly greater percentages of abnormal responses on the AS (P < 0.0001) and the PI (P = 0.0001) than the control.
Discussion: Abnormal performance of cervical stabilizer muscles using the CCFT was demonstrated in a high proportion of participants with LBP. The findings highlight the plausible association in muscle control between cervical and lumbar stabilizers.
Level of Evidence: 2b.
KEYWORDS: Cervical spine, Core stabilizer muscles, craniocervical flexion test, deep neck muscles, low back pain, lumbar spine, motor control, spinal stability
Introduction
Low back pain (LBP) is a common health problem that proves an enormous financial burden for society [1–3]. Up to 80% of individuals experience at least one episode of LBP in their lifetime [4]. Several impairments have been reported in association with LBP including poor performance of lumbar core stabilizer muscles [5–8].
In the spine, core stabilizer muscles that commonly lie closed to the spine are known to provide segmental stability and stiffen the spine during function [9]. For the lumbar spine, the core stabilizer muscles consist of transversus abdominis, lumbar multifidus, diaphragm, and pelvic floor muscles [10,11]. For the cervical spine, they consist of deep cervical flexor muscles such as longus capitis and longus colli muscles [12]. In pain conditions, the functions of these muscles have been found to be impaired, decreasing and/or delaying compared with healthy individuals. During both expected and unexpected perturbations, persons with chronic LBP demonstrated delayed onset of the transversus abdominis and the deep lumbar multifidus muscles [5,13,14]. Similarly, the deep cervical flexor muscles also showed delayed onset in patients with chronic neck pain [15] and whiplash injury [16]. The reduced activation of the deeper spinal muscles is commonly associated with the increased activation of the superficial spinal muscles in people with LBP [13,17] and neck pain [18,19]. These alterations in muscle activity of the spinal muscles suggest changes in motor control of the spine [20].
Two tests commonly used in research studies and clinical settings for assessing the performance of cervical and lumbar stabilizer muscles are the craniocervical flexion test (CCFT) [12] and the abdominal drawing-in maneuver (ADIM) [10], respectively. These tests in previous studies have shown that the controls demonstrated different levels of performance from patients with neck pain [21,22] or LBP [23,24].
As the spine is a continuum of vertebral segments, it is postulated that the pain in one area might bring about pain in another area. This is evident by the coexistence of neck pain and LBP [25,26] and a significant positive correlation in degenerative changes between the cervical and the lumbar spines [27]. Individuals with comorbid LBP were also reported to have increased risk of persistent neck pain [28]. To date, there is only one study demonstrating that patients with chronic neck pain also had abnormal performance of lumbar stabilizer muscles on the ADIM even though they had no complaints concerning LBP [29]. When these patients were followed for 2 years, it was revealed that those who had abnormal ADIM were three times more likely to develop persistent or recurrent LBP [29]. However, there have been no studies assessing the possibility of the abnormal performance of cervical stabilizer muscles in persons with chronic LBP. It is also unknown whether abnormal performance would be present in a subacute LBP condition.
This study aimed to compare the performance of cervical stabilizer muscles on the CCFT among individuals with subacute, chronic, and asymptomatic LBP conditions. It was hypothesized that (1) individuals with LBP would have impaired performance of cervical stabilizer muscles and (2) individuals with subacute and chronic LBP would show lower performance of cervical stabilizer muscles than the control.
Methods
Study design
A cross-sectional study design was used [30]. Ethical approval for the study was granted by the Research Ethics Review Committee for Research Involving Human Research Participants, Health Sciences Group, Chulalongkorn University (COA No.108/2016).
Participants
Individuals aged between 20 and 45 years with normal body mass index (18.5–22.9 kg/m2) were recruited from the physical therapy clinic at the Faculty of Allied Health Sciences and from flyers posted at the university. The participants were classified into three groups including subacute LBP, chronic LBP, and age- and gender-matched control groups (±3 years). LBP was defined as pain in the region below the 12th thoracic spinous process to the inferior gluteal folds with or without lower extremity pain [31,32]. Current pain intensity was rated at least 2 on 100-mm visual analog scale. Pain that had persisted between 1 and 3 months was identified as a subacute condition, while pain that had persisted for more than 3 months was identified as a chronic condition [31,33]. All LBP participants had to have no pain or discomfort in neck area that had lasted longer than 1 day within the last 2 years. The control group had to have no pain or discomfort in all spinal areas that had lasted longer than 1 day within the last 2 years. All participants had to have no history of LBP that required intervention or limited functional abilities prior to participation in this study.
Participants were excluded if they had undergone abdominal wall or spinal surgery; had a spinal deformity such as scoliosis that had had a positive test from Adam’s forward bend test; had a neurological condition, fracture, cancer, or infectious disease of the spine; and had participated in a training program for neck or back stabilization. The participants were asked whether they were familiarized with the protocols of the CCFT or the ADIM. Those who were unable to lie prone, unable to perform the CCFT and the ADIM due to pain, and females currently menstruating or pregnant were also excluded. All participants who met the selection criteria signed the consent form before participating in the study. Twenty-three participants in each group were required. This sample size was calculated for detecting a 4 mmHg difference in the CCFT between individuals with subacute and chronic LBP and control with a standard deviation of 0.74 mmHg at 80% power and significance level of 0.05 [34].
Measures
Pain intensity
Participants with subacute and chronic LBP were asked to rate their current pain level by indicating it on a 100-mm visual analog scale. The anchor on the left end represents ‘no pain’ while that on the right represents ‘pain as bad as it can be’. This measurement was found to provide moderate-to-excellent test–retest reliability of pain measurement as reported in a previous study (ICC = 0.71–0.94) [35].
Low back pain disability
Disability from LBP was estimated by the modified Oswestry LBP disability questionnaire which contains 10 items that relate to the activities of daily life and pain [36]. Each item is scored from 0 to 5, with higher values representing greater disability. The maximum sum score of 10 items is 50 and minimum is 0 [37]. The Thai version of the modified Oswestry LBP disability questionnaire showed excellent test–retest reliability in the LBP group (ICC = 0.98) [38].
Performance of lumbar stabilizer muscles
The performance of lumbar stabilizer muscles was tested with the ADIM and a pressure biofeedback unit (PBU) (StabilizerTM, Chattanooga, Vista, CA) [10]. The PBU consists of a three-chamber air-filled pressure bag, a catheter, and a sphygmomanometer gauge. The accuracy was ±3 mmHg [39]. The participants were in a prone position with the head laying comfortably and relaxed. A deflated PBU was placed centrally beneath the lower abdomen with the lower edge in line with the anterior superior iliac spines before being inflated to 70 mmHg [10,40]. The participants were then asked to slowly draw their abdomen off the PBU and hold steadily for 10 s. During testing, a researcher palpated the thoracolumbar area so that any substitution strategies from spinal or pelvic movements were not allowed [41,42]. The maximum pressure change that could be held steadily for 10 s was recorded which was later converted to two categories: normal response (≥4 mmHg) and abnormal response (<4 mmHg) [23,41,42].
Performance of cervical stabilizer muscles
The performance of the cervical stabilizer muscles was examined with the CCFT. The participants were positioned in supine lying with both knees bent and the cervical spine in a neutral position. The forehead and chin were aligned horizontally to the plinth surface. The PBU was placed behind the neck at the suboccipital region before being inflated to the baseline pressure of 20 mmHg [12]. They were instructed to perform a slow and controlled craniocervical flexion in a head nod action by progressively increasing the pressure in 2 mmHg increments from 20 to 30 mmHg and holding at each increment for 10 s. A 30-s rest was allowed between the successful increments. During testing, the contraction of the superficial neck flexor muscles was palpated by an assessor whose activity was kept to a minimum. A high level of activity of these superficial muscles was found to be an indicator of reduced deep cervical flexor activity.
Two data were recorded during the CCFT, i.e. the activation score (AS) and performance index (PI) [12,18]. The AS was defined as the highest pressure level change the participants could achieve and maintain steadily for 10 s. The PI which reflects the isometric endurance of the deep cervical flexor muscles was calculated by multiplying the number of times the participants could replicate the test at the AS. The highest score of the PI was set at 100 (10 repetitions at a 10 mmHg AS). Based on the previous studies in people with and without neck pain, these data were converted into a rating in which an abnormal response for the AS and the PI were ≤4 mmHg [16,43] and ≤20 scores [22,43], respectively.
Experimental procedure
Two physical therapists were involved in this study. One was responsible for recruiting participants, while the other was blinded to the assigned group and assessed the participants with the CCFT and the ADIM. All participants were required to complete two questionnaires: visual analog scale and the modified Oswestry LBP disability questionnaire. Next, they were familiarized with the testing protocol of the ADIM and the CCFT according to the established protocols until they could perform the tests. Then, they were tested first with the ADIM, followed by the CCFT. The tests began after food consumption for at least 30 min and with an empty bladder.
Statistical analysis
Data analysis was performed using the SPSS version 22.0 software (IBM, Chicago, IL, USA). The Shapiro–Wilk test found that the data of age and body mass index were normally distributed, while the AS and the PI were not normally distributed. One-way ANOVA was performed to examine whether there were significant differences among the 3 groups of participants. To test whether there were significant differences in the AS and the PI among the three groups, separate Kruskal Wallis tests were conducted. To identify which pairs were responsible for the statistical significance, the Mann–Whitney U test with the Bonferroni correction to control for Type I error was used as a post hoc analysis [30]. Chi-square analysis was used to examine whether there was a significant difference in the proportions of the participants who were classified as being of normal and abnormal performance on the AS and the PI among the three groups. The significance level was set at P < 0.0500.
Results
Seventy-six participants (36 males and 40 females) took part in this study. Each of the pain groups consisted of 23 participants, while there were 30 participants in the age- and gender-matched control group. No significant differences in age and body mass index were found among the three groups of the participants (Table 1). All LBP participants had mild level of disability as measured by the modified Oswestry LBP disability questionnaire. The majority of participants with LBP showed abnormal response on the ADIM.
Table 1.
Demographic data of subacute LBP, chronic LBP, and age- and gender-matched control groups.
| Variables | Mean (SD) |
P value | ||
|---|---|---|---|---|
| Subacute LBP group (n = 23) |
Chronic LBP group (n = 23) |
Control group (n = 30) |
||
| Gender, n (%) | ||||
| Male | 11 (47.8) | 12 (52.2) | 13 (43.3) | |
| Female | 12 (52.2) | 11 (47.8) | 17 (56.7) | |
| Age (years) | 22.7 (3.3) | 25.1 (5.4) | 24.3 (5.0) | 0.2358 |
| Body mass index (kg/m2) | 20.8 (1.5) | 20.7 (1.3) | 20.5 (1.3) | 0.6670 |
| Visual analog scale (mm) | 47.3 (18.1) | 52.4 (20.2) | – | |
| Duration of LBP (months) | 1.5 (1.7) | 21.3 (14.0) | – | |
| Modified Oswestry LBP disability questionnaire | 4.3 (3.4) | 6.4 (4.0) | – | |
| ADIM, pressure change (mmHg) (range) | 1.6 (1.0) (0–4) |
2.0 (1.4) (0–4) |
4.3 (1.8) (2–10) |
|
| ADIM, n (%) | ||||
| Normal | 2 (8.7) | 5 (21.7) | 26 (86.7) | |
| Abnormal | 21 (91.3) | 18 (78.3) | 4 (13.3) | |
The AS and the PI of the three groups are presented in Table 2. Kruskal Wallis tests showed significant differences in the AS (P = 0.0002) and the PI (P = 0.0004) of the CCFT among the three groups. Post hoc analyses with Mann–Whitney U tests revealed significantly lower AS when comparing the control group to subacute LBP (P = 0.0002) and chronic LBP groups (P = 0.0009). The PIs of the subacute LBP (P = 0.0002) and chronic LBP groups (P = 0.0036) were significantly lower than the control group. No significant differences were found between subacute and chronic LBP groups in the AS (P = 0.8893) and the PI (P = 0.7243).
Table 2.
The activation score (mmHg) and the performance index of subacute LBP, chronic LBP, and age- and gender-matched control groups.
| Groups | Subacute LBP (n = 23) |
Chronic LBP (n = 23) |
Control (n = 30) |
P value |
|---|---|---|---|---|
| Activation score (mmHg) | 4.4 (2.3) | 4.3 (2.7) | 6.7 (2.1) | 0.0002 |
| Minimum | 0 | 0 | 2 | |
| Maximum | 10 | 10 | 10 | |
| Performance index | 17.0 (13.7) | 21.7 (21.5) | 37.5 (18.6) | 0.0004 |
| Minimum | 0 | 0 | 4 | |
| Maximum | 50 | 80 | 80 |
In comparison to the control (4/30), the proportions of participants who showed abnormal response on the AS were significantly greater in groups of subacute LBP (17/23, P < 0.0001) and chronic LBP (15/23, P = 0.0001) (Figure 1). Regarding the PI, a significantly greater abnormal response was obtained from participants in the subacute LBP (17/23, P = 0.0001) and chronic LBP groups (14/23, P = 0.0023) than the control (6/30) (Figure 2). There were no significant differences in the proportions of participants with abnormal responses in the AS (P = 0.5216) and the PI (P = 0.3454) between subacute and chronic LBP groups.
Figure 1.
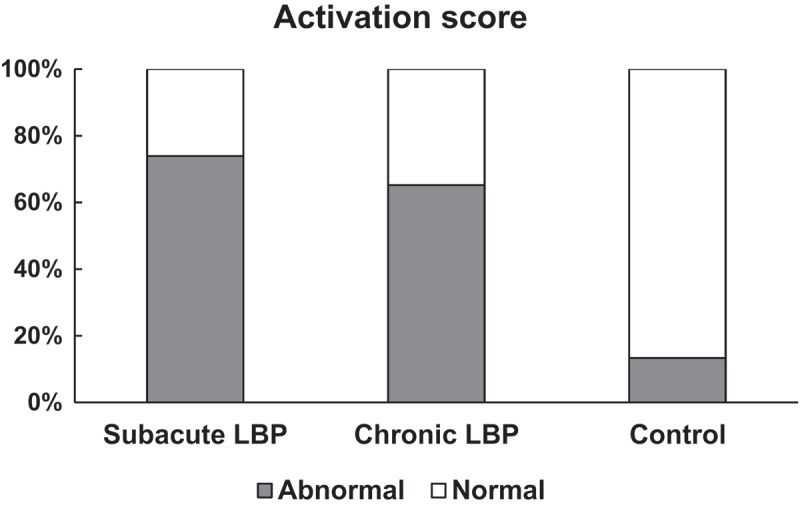
Percentages of participants in subacute LBP, chronic LBP, and control who had abnormal and normal responses on the activation score.
Figure 2.
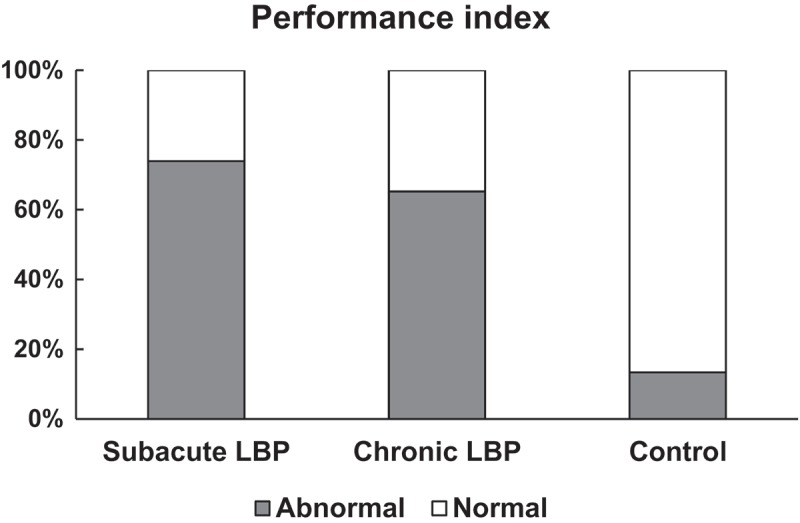
Percentages of participants in subacute LBP, chronic LBP, and control who had abnormal and normal responses on the performance index.
Discussion
This study demonstrated that a high proportion of people with LBP not only had abnormal performance of core stabilizer muscles in the lumbar spine but also in the cervical spine. The highest proportion of participants categorized as having abnormal response on the CCFT was shown among participants with subacute LBP followed by those with chronic LBP and control.
On average, pressure changes on the ADIM in subacute (1.6 ± 1.0 mmHg) and chronic (2.0 ± 1.4 mmHg) LBP groups coincided with the values of previous studies in LBP patients [10,41]. As a result, approximately 91% of subacute LBP and 78% of chronic LBP participants in this study were categorized as having abnormal response on the ADIM. These findings were found even among participants with mild disability from LBP.
It is noteworthy that the AS for the subacute and chronic LBP groups in this study was in the ranges for chronic neck pain reported in the literature. These were 3.00 ± 1.30 mmHg for chronic whiplash [16] and 4.20 ± 1.90 mmHg for chronic cervicogenic headache [43]. However, the PI for subacute and chronic LBP groups in the current study was greater than the 10.6 ± 15.3 scores reported in patients with chronic cervicogenic headaches [43]. Although these participants were free from neck pain at the time of the study, the poor performance on the CCFT suggested that they also had impaired motor control of the movement of the cervical spine. Consequently with repetitive motion, alterations in the path of normal joint movement are likely to occur and may lead to pain [44]. However, a further longitudinal study is needed to prove whether poor performance on the AS or the PI would be a predictor of the development of neck pain.
Approximately 75% of subacute LBP and 60% of chronic LBP participants showed abnormal responses on the CCFT which were shown via AS and PI being in line with a previous study that examined abnormal responses on the ADIM in chronic neck pain group [29]. These findings suggest that abnormal performance of neck stabilizer muscles could be found in subacute LBP and might continue to persist with time as there were no significant differences in the AS and the PI as well as the proportions of abnormal responses on these parameters between subacute and chronic LBP groups. To restore the performance of the cervical core stabilizer muscles, an appropriate rehabilitation protocol should be implemented [45].
The findings of the reduced performance of neck stabilizer muscles on the CCFT in LBP participants despite the participants having not had neck pain for at least 2 years prior to the study is interesting. The previous study also found a similar reduction in the performance of back stabilizer muscles on the ADIM in participants who had no LBP but did have chronic neck pain [29]. The coexistence of impairments in core stabilizer muscle performance in the neck and the back regions suggests the widespread effect of pain in the spine apart from the painful region. These results highlight that the impact of pain on muscle control is not limited to the anatomical area where pain is perceived. The mechanism that causes this phenomenon is unclear.
One study proposed that it might be related to the change in postural strategy in response to spinal pain which might pose biomechanical demands in other nonpainful spinal region [29]. In association with the decrease in lumbar lordosis and an increased anterior translation of the head which accompanied the change in sitting posture, an increase in muscle activity of the superficial neck muscles was detected [46]. Although the study reported the activity of the superficial neck muscles, alteration in the activity of the deep cervical flexor muscles is likely to occur [18]. With correct sitting posture, deep cervical flexor muscles were found to increase their activity [47,48].
The present study has some limitations. First, participants with LBP in this study had mild levels of back disability so different proportions of abnormal response of the CCFT might be possible if the participants had moderate or severe disabilities. Second, this study was a cross-sectional design which cannot establish cause and effect regarding the abnormal response of the ADIM and the CCFT. A prospective cohort study would be required. Third, this study recruited participants who had LBP but no neck pain within the previous 2 years. A history of both neck and LBP prior to that was not recorded and any preexistence of abnormal response of the CCFT might be possible. However, the significant differences in the noncategorized CCFT data between the control and the LBP groups who had the same 2-year pain-free duration from neck pain might indicate that the differences found are truly present.
Conclusion
These results suggest that abnormal performance on the CCFT can be found in a high proportion of participants with LBP with both subacute and chronic conditions. Individuals with LBP not only had abnormal performance of core stabilizer muscles in the lumbar spine but also abnormal performance of core stabilizer muscles in the cervical spine.
Biographies
Chattrachoo Thongprasert is a physical therapist at Newton Em Physiotherapy Clinic Ratchadamri and she was a physical therapy student at time of study.
R. Kanlayanaphotporn is an assistant professor in the Undergraduate and Graduate Physical Therapy programs at Faculty of Allied Health Sciences, Chulalongkorn University. Her research interests are focused on patient outcomes, exercise therapy, and manual therapy techniques for treating musculoskeletal pathologies.
Funding Statement
This work was supported by the 90th Anniversary of Chulalongkorn University Fund (Ratchadaphiseksomphot Endowment Fund), Bangkok, Thailand under Grant [GCUGR1125594090M].
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Dagenais S, Caro J, Haldeman S.. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8:8–20. [DOI] [PubMed] [Google Scholar]
- [2].Hoy D, Brooks P, Blyth F, et al. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24:769–781. [DOI] [PubMed] [Google Scholar]
- [3].Ivanova JI, Birnbaum HG, Schiller M, et al. Real-world practice patterns, health-care utilization, and costs in patients with low back pain: the long road to guideline-concordant care. Spine J. 2011;11:622–632. [DOI] [PubMed] [Google Scholar]
- [4].Rubin DI. Epidemiology and risk factors for spine pain. Neurol Clin. 2007;25:353–371. [DOI] [PubMed] [Google Scholar]
- [5].MacDonald D, Moseley GL, Hodges PW. Why do some patients keep hurting their back? Evidence of ongoing back muscle dysfunction during remission from recurrent back pain. Pain. 2009;142:183–188. [DOI] [PubMed] [Google Scholar]
- [6].Hodges P, Coppieters M, MacDonald D, et al. New insight into motor adaptation to pain revealed by a combination of modelling and empirical approaches. Eur J Pain. 2013;17:1138–1146. [DOI] [PubMed] [Google Scholar]
- [7].van Dieën JH, Selen LP, Cholewicki J. Trunk muscle activation in low-back pain patients, an analysis of the literature. J Electromyogr Kinesiol. 2003;13:333–351. [DOI] [PubMed] [Google Scholar]
- [8].van Dieën JH, Reeves NP, Kawchuk G, et al. Motor control changes in low-back pain: divergence in presentations and mechanisms. J Orthop Sports Phys Ther. 2018. Jun 12;1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Panjabi MM. Clinical spinal instability and low back pain. J Electromyogr Kinesiol. 2003;13:371–379. [DOI] [PubMed] [Google Scholar]
- [10].Richardson C, Jull G. Muscle control–pain control. What exercises would you prescribe? Man Ther. 1995;1:2–10. [DOI] [PubMed] [Google Scholar]
- [11].Hodges PW. Is there a role for transversus abdominis in lumbo-pelvic stability? Man Ther. 1999;4:74–86. [DOI] [PubMed] [Google Scholar]
- [12].Jull GA, O’leary SP, Falla DL. Clinical assessment of the deep cervical flexor muscles: the craniocervical flexion test. J Manipulative Physiol Ther. 2008;31:525–533. [DOI] [PubMed] [Google Scholar]
- [13].MacDonald D, Moseley GL, Hodges PW. People with recurrent low back pain respond differently to trunk loading despite remission from symptoms. Spine (Phila Pa 1976). (Phila Pa 1976) 2010;35: 818–824. [DOI] [PubMed] [Google Scholar]
- [14].Knox MF, Chipchase LS, Schabrun SM, et al. Anticipatory and compensatory postural adjustments in people with low back pain: A systematic review and meta-analysis. Spine J. 2018;18:1934–1939. [DOI] [PubMed] [Google Scholar]
- [15].Falla D, Jull G, Hodges P. Feedforward activity of the cervical flexor muscles during voluntary arm movements is delayed in chronic neck pain. Exp Brain Res. 2004;157:43–48. [DOI] [PubMed] [Google Scholar]
- [16].Jull GA. Deep cervical flexor muscle dysfunction in whiplash. J Musculoskelet Pain. 2000;8:143–154. [Google Scholar]
- [17].Hodges PW. Pain and motor control: from the laboratory to rehabilitation. J Electromyogr Kinesiol. 2011;21:220–228. [DOI] [PubMed] [Google Scholar]
- [18].Jull G, Falla D. Does increased superficial neck flexor activity in the craniocervical flexion test reflect reduced deep flexor activity in people with neck pain? Man Ther. 2016;25:43–47. [DOI] [PubMed] [Google Scholar]
- [19].Johnston V, Jull G, Souvlis T, et al. Neck movement and muscle activity characteristics in female office workers with neck pain. Spine (Phila Pa 1976). 2008;33:555–563. [DOI] [PubMed] [Google Scholar]
- [20].Hodges PW, Tucker K. Moving differently in pain: A new theory to explain the adaptation to pain. Pain. 2011;152:S90–S8. [DOI] [PubMed] [Google Scholar]
- [21].Chiu TT, Law EY, Chiu TH. Performance of the craniocervical flexion test in subjects with and without chronic neck pain. J Orthop Sports Phys Ther. 2005;35:567–571. [DOI] [PubMed] [Google Scholar]
- [22].Fernandez-De-Las-Penas C, Pérez-de-Heredia M, Molero-Sánchez A, et al. Performance of the craniocervical flexion test, forward head posture, and headache clinical parameters in patients with chronic tension-type headache: a pilot study. J Orthop Sports Phys Ther. 2007;37:33–39. [DOI] [PubMed] [Google Scholar]
- [23].Hodges P, Richardson C, Jull G. Evaluation of the relationship between laboratory and clinical tests of transversus abdominis function. Physiother Res Int. 1996;1:30–40. [DOI] [PubMed] [Google Scholar]
- [24].Grooms DR, Grindstaff TL, Croy T, et al. Clinimetric analysis of pressure biofeedback and transversus abdominis function in individuals with stabilization classification low back pain. J Orthop Sports Phys Ther. 2013;43:184–193. [DOI] [PubMed] [Google Scholar]
- [25].IJzelenberg W, Burdorf A. Impact of musculoskeletal co-morbidity of neck and upper extremities on healthcare utilisation and sickness absence for low back pain. Occup Environ Med. 2004;61:806–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hagen EM, Svensen E, Eriksen HR, et al. Comorbid subjective health complaints in low back pain. Spine (Phila Pa 1976). 2006;31:1491–1495. [DOI] [PubMed] [Google Scholar]
- [27].Morishita Y, Buser Z, D’Oro A, et al. Clinical relationship of degenerative changes between the cervical and lumbar spine. Asian Spine J. 2018;12:343–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Hill J, Lewis M, Papageorgiou AC, et al. Predicting persistent neck pain: a 1-year follow-up of a population cohort. Spine (Phila Pa 1976). 2004;29:1648–1654. [DOI] [PubMed] [Google Scholar]
- [29].Moseley GL. Impaired trunk muscle function in sub-acute neck pain: etiologic in the subsequent development of low back pain? Man Ther. 2004;9:157–163. [DOI] [PubMed] [Google Scholar]
- [30].Portney LG, Watkins MP. Foundations of clinical research: applications to practice. 3rd ed. Essex: Pearson Education Limited; 2014. [Google Scholar]
- [31].Delitto A, George SZ, Van Dillen LR, et al. Low back pain: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American physical therapy association. J Orthop Sports Phys Ther. 2012;42:A1–A57. [DOI] [PubMed] [Google Scholar]
- [32].Krismer M, Van Tulder M. Low back pain (non-specific). Best Pract Res Clin Rheumatol. 2007;21:77–91. [DOI] [PubMed] [Google Scholar]
- [33].Von MK. Studying the natural history of back pain. Spine (Phila Pa 1976). 1994;19:2041S–6S. [DOI] [PubMed] [Google Scholar]
- [34].Jørgensen R, Ris I, Falla D, et al. Reliability, construct and discriminative validity of clinical testing in subjects with and without chronic neck pain. BMC Musculoskelet Disord. 2014;15:408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Hawker GA, Mian S, Kendzerska T, et al. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S240–S52. [DOI] [PubMed] [Google Scholar]
- [36].Fritz JM, Irrgang JJ. A comparison of a modified Oswestry low back pain disability questionnaire and the Quebec back pain disability scale. Phys Ther. 2001;81:776–788. [DOI] [PubMed] [Google Scholar]
- [37].Fairbank JC, Pynsent PB. The Oswestry disability index. Spine (Phila Pa 1976). 2000;25:2940–2953. [DOI] [PubMed] [Google Scholar]
- [38].Sakulsriprasert P, Vachalathiti R, Vongsirinavarat M, et al. Cross-cultural adaptation of modified Oswestry low back pain disability questionnaire to Thai and its reliability. J Med Assoc Thai. 2006;89:1694–1701. [PubMed] [Google Scholar]
- [39].Chattanooga Group of Encore Medical LP Stabilizer pressure bio-feedback operating instruction. Hixson, USA: Chattanooga Group Inc.; 2005. [Google Scholar]
- [40].Von Garnier K, Köveker K, Rackwitz B, et al. Reliability of a test measuring transversus abdominis muscle recruitment with a pressure biofeedback unit. Physiotherapy. 2009;95:8–14. [DOI] [PubMed] [Google Scholar]
- [41].Cairns MC, Harrison K, Wright C. Pressure biofeedback: a useful tool in the quantification of abdominal muscular dysfunction? Physiotherapy. 2000;86:127–138. [Google Scholar]
- [42].Ramos LAV, Callegari B, Fjr F, et al. Comparison between transcutaneous electrical nerve stimulation and stabilization exercises in fatigue and transversus abdominis activation in patients with lumbar disk herniation: A randomized study. J Manipulative Physiol Ther. 2018;41:323–331. [DOI] [PubMed] [Google Scholar]
- [43].Jull G, Barrett C, Magee R, et al. Further clinical clarification of the muscle dysfunction in cervical headache. Cephalalgia. 1999;19:179–185. [DOI] [PubMed] [Google Scholar]
- [44].Sahrmann SA. Movement system impairment of the extremities, cervical and thoracic spines. Missouri: Elsevier Mosby; 2011. [Google Scholar]
- [45].Kim JY, Kwag KI. Clinical effects of deep cervical flexor muscle activation in patients with chronic neck pain. J Phys Ther Sci. 2016;28:269–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Falla D, Jull G, Russell T, et al. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther. 2007;87:408–417. [DOI] [PubMed] [Google Scholar]
- [47].Beer A, Treleaven J, Jull G. Can a functional postural exercise improve performance in the cranio-cervical flexion test?–A preliminary study. Man Ther. 2012;17:219–224. [DOI] [PubMed] [Google Scholar]
- [48].Falla D, O’Leary S, Fagan A, et al. Recruitment of the deep cervical flexor muscles during a postural-correction exercise performed in sitting. Man Ther. 2007;12:139–143. [DOI] [PubMed] [Google Scholar]


