Abstract
Background
Pneumonia is the most common hospital‐acquired infection affecting patients in the intensive care unit (ICU). However, current national guidelines for the treatment of hospital‐acquired pneumonia (HAP) are several years old and the diagnosis of pneumonia in mechanically ventilated patients (VAP) has been subject to considerable recent attention. The optimal duration of antibiotic therapy for HAP in the critically ill is uncertain.
Objectives
To assess the effectiveness of short versus prolonged‐course antibiotics for HAP in critically ill adults, including patients with VAP.
Search methods
We searched CENTRAL (2015, Issue 5), MEDLINE (1946 to June 2015), MEDLINE in‐process and other non‐indexed citations (5 June 2015), EMBASE (2010 to June 2015), LILACS (1982 to June 2015) and Web of Science (1955 to June 2015).
Selection criteria
We considered all randomised controlled trials (RCTs) comparing a fixed 'short' duration of antibiotic therapy with a 'prolonged' course for HAP (including patients with VAP) in critically ill adults.
Data collection and analysis
Two review authors conducted data extraction and assessment of risk of bias. We contacted trial authors for additional information.
Main results
We identified six relevant studies involving 1088 participants. This included two new studies published after the date of our previous review (2011). There was substantial variation in participants, in the diagnostic criteria used to define an episode of pneumonia, in the interventions and in the reported outcomes. We found no evidence relating to patients with a high probability of HAP who were not mechanically ventilated. For patients with VAP, overall a short seven‐ or eight‐day course of antibiotics compared with a prolonged 10‐ to 15‐day course increased 28‐day antibiotic‐free days (two studies; N = 431; mean difference (MD) 4.02 days; 95% confidence interval (CI) 2.26 to 5.78) and reduced recurrence of VAP due to multi‐resistant organisms (one study; N = 110; odds ratio (OR) 0.44; 95% CI 0.21 to 0.95), without adversely affecting mortality and other recurrence outcomes. However, for cases of VAP specifically due to non‐fermenting Gram‐negative bacilli (NF‐GNB), recurrence was greater after short‐course therapy (two studies, N = 176; OR 2.18; 95% CI 1.14 to 4.16), though mortality outcomes were not significantly different. One study found that a three‐day course of antibiotic therapy for patients with suspected HAP but a low Clinical Pulmonary Infection Score (CPIS) was associated with a significantly lower risk of superinfection or emergence of antimicrobial resistance, compared with standard (prolonged) course therapy.
Authors' conclusions
On the basis of a small number of studies and appreciating the lack of uniform definition of pneumonia, we conclude that for patients with VAP not due to NF‐GNB a short, fixed course (seven or eight days) of antibiotic therapy appears not to increase the risk of adverse clinical outcomes, and may reduce the emergence of resistant organisms, compared with a prolonged course (10 to 15 days). However, for patients with VAP due to NF‐GNB, there appears to be a higher risk of recurrence following short‐course therapy. These findings do not differ from those of our previous review and are broadly consistent with current guidelines. There are few data from RCTs comparing durations of therapy in non‐ventilated patients with HAP, but on the basis of a single study, short‐course (three‐day) therapy for HAP appears not to be associated with worse clinical outcome, and may reduce the risk of subsequent infection or the emergence of resistant organisms when there is low probability of pneumonia according to the CPIS.
Plain language summary
Short‐course versus long‐course antibiotic treatment for hospital‐acquired pneumonia in adult intensive care patients
Review question We reviewed the evidence from randomised controlled trials (RCTs) that compared the effects of a short course of antibiotics with a long course for intensive care patients with hospital‐acquired pneumonia (HAP).
Background Hospital‐acquired pneumonia is the major cause of hospital‐acquired infection in the intensive care unit (ICU). There are a number of factors that make the critically ill more likely to develop pneumonia, among which the most important is tracheal intubation performed in conjunction with mechanical ventilation; thus, the majority of ICU patients with HAP have what is termed ventilator‐associated pneumonia (VAP).
There is concern that an unnecessarily long course of antibiotic therapy may lead to patients acquiring antibiotic‐resistant organisms, which may be more difficult to recognise and treat when they cause infection and may increase drug costs. On the other hand, too short a course risks the treatment failing.
Study characteristics The evidence was current as of June 2015. We identified six RCTs, which had enrolled 1088 patients. The studies took quite different approaches to their investigations, and we found only one study that had explored the duration of antibiotic therapy for ICU patients who had HAP, but were not mechanically ventilated.
Key results For patients with VAP, our main finding was that a course of seven or eight days of antibiotics was associated with an overall decrease in antibiotic administration and reduced the recurrence of pneumonia due to resistant organisms when compared with a 10‐ to 15‐day course. Furthermore, this was achieved without any significant effect on mortality. Nevertheless, in cases when VAP was due to a particular type of organism ('non‐fermenting Gram‐negative bacillus'), which can be difficult to eradicate with antibiotics, the risk of pneumonia recurring appeared higher after a short course of treatment.
One study found that for patients with possible (but low probability) HAP a short (three‐day) course of therapy seemed to be associated with a lower chance of acquiring resistant organisms or of subsequent infections being due to a resistant organism.
Quality of evidence The quality of evidence for the main outcome measures was low to moderate. The main reasons that the quality was not high were that only a small number of studies were identified, and that there were differences in patient populations, in the nature of the interventions between studies and in the reported outcomes.
Summary of findings
Summary of findings for the main comparison. Should short‐course antibiotic therapy versus prolonged‐course antibiotic therapy be used in critically ill patients with hospital‐acquired pneumonia?
| Should short‐course antibiotic therapy versus prolonged‐course antibiotic therapy be used in critically ill patients with hospital‐acquired pneumonia? | ||||||
| Patient or population: hospital‐acquired pneumonia Settings: intensive care Intervention: short‐course antibiotic therapy Comparison: prolonged‐course antibiotic therapy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Prolonged‐course antibiotic therapy | Short‐course antibiotic therapy | |||||
| Mortality Follow‐up: 28 days | 175 per 1000 | 201 per 1000 (141 to 277) | OR 1.18 (0.77 to 1.8) | 598 (3 studies) | ⊕⊕⊕⊝ moderate1 | — |
| Mortality NF‐GNB Follow‐up: 28 days | 265 per 1000 | 255 per 1000 (123 to 450) | OR 0.95 (0.39 to 2.27) | 179 (2 studies) | ⊕⊕⊝⊝ low1,2 | — |
| Mortality MRSA Follow‐up: 28 days | 238 per 1000 | 286 per 1000 (91 to 614) | OR 1.28 (0.32 to 5.09) | 42 (1 study) | ⊕⊕⊕⊝ moderate1 | — |
| Recurrence of pneumonia Clinical and/or microbiological criteria | 180 per 1000 | 237 per 1000 (171 to 318) | OR 1.41 (0.94 to 2.12) | 733 (19 studies) | ⊕⊕⊝⊝ low1,3 | — |
| Recurrence of pneumonia NF‐GNB Clinical and/or microbiological criteria | 247 per 1000 | 417 per 1000 (272 to 577) | OR 2.18 (1.14 to 4.16) | 176 (2 studies) | ⊕⊕⊕⊝ moderate1 | — |
| Recurrence of pneumonia MRSA Clinical and/or microbiological criteria | 370 per 1000 | 479 per 1000 (66 to 920) | OR 1.56 (0.12 to 19.61) | 49 (2 studies) | ⊕⊕⊕⊝ moderate1 | — |
| 28‐day antibiotic‐free days Follow‐up: 28 days | The mean 28‐day antibiotic free days in the intervention groups was 4.02 higher (2.26 to 5.78 higher) | 431 (2 studies) | ⊕⊕⊝⊝ low1,4 | — | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MRSA: methicillin‐resistant Staphylococcus aureus; NF‐GNB: non‐fermenting Gram‐negative bacilli; OR: odds ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Low total number of events. 2Kollef et al. Multiple interventions (short versus prolonged duration, doripenem versus imipenem, extended versus standard infusion), protocol violations at several centres and premature cessation of study. 3Differences in duration of mechanical ventilation prior to episode of pneumonia and differences in bacterial aetiology. 4Presumed differences in administration of antibiotics (outside of context of study) between studies.
Background
Description of the condition
Hospital‐acquired pneumonia (HAP) is usually defined as pneumonia occurring 48 hours or more after hospital admission and not incubating at time of admission (ATS/IDSA 2005). It remains an important cause of healthcare‐associated morbidity and mortality, occurring among the general hospitalised population with a rate of 5 to 10 per 1000 hospital admissions (ATS/IDSA 2005). Patients in the intensive care unit (ICU, also referred to as intensive therapy unit, ITU) appear to be at particular risk and in this setting pneumonia is the most common cause of hospital‐acquired infection in Europe and the United States (Burgmann 2010; Richards 2000; Vincent 1995).
Over 90% of pneumonia episodes developing in ICUs occur in patients who are intubated and mechanically ventilated (ATS/IDSA 2005); ventilator‐associated pneumonia (VAP) therefore represents a very significant sub‐set of HAP occurring in ICUs. VAP has been defined as pneumonia that occurs more than 48 to 72 hours after tracheal intubation (ATS/IDSA 2005) and is thought to affect 10% to 20% patients receiving mechanical ventilation for more than 48 hours (Safdar 2005). Endotracheal intubation probably increases the risk of developing pneumonia by facilitating the growth of potential bacterial pathogens within the respiratory tract (Chastre 2002). Patients are more likely to develop VAP if they are sicker, older, have undergone prior surgery, or are admitted with neurological and/or cardiovascular failure (Blot 2013; Chastre 2002). Recently it has been suggested that 'ventilator‐associated tracheobronchitis' (VAT), i.e. ventilator‐associated respiratory tract infection in the absence of chest x‐ray changes, may be a precursor of VAP (Dallas 2011), and that antibiotic therapy may prevent an episode from developing into pneumonia (Agrafiotis 2010).
An episode of HAP has adverse consequences for the critically ill. Mortality attributable to an episode of VAP (as opposed to the severe underlying illness) has been estimated to be 4% to 13% (Bekaert 2011; Melsen 2011; Melsen 2013). Furthermore, lengths of ICU and hospital stay are significantly prolonged when VAP develops and associated costs have been estimated to range from USD 10,000 to 40,000 per patient (Rello 2002; Safdar 2005; Warren 2003).
Considerable effort has been made in recent years to refine VAP definitions, yet doubt remains as to the optimal means of identifying an episode of VAP for clinical and for surveillance purposes. Traditionally, radiological evidence of pneumonia, systemic criteria (e.g. pyrexia or abnormal white cell count) and/or pulmonary criteria (e.g. presence of bronchial breathing or worsening cough) have been required to make a diagnosis of VAP (ATS/IDSA 2005; HELICS 2004; Horan 2008). However, practically it can be very difficult to make a distinction between VAP and other conditions occurring in mechanically ventilated critically ill patients, including non‐infective processes such as atelectasis and pulmonary oedema. Quantitative culture of invasive bronchoscopic respiratory specimen (e.g. broncho‐alveolar lavage, BAL) may have particular appeal for diagnosing VAP in patient groups with greater likelihood of a non‐pulmonary cause for systemic inflammation (e.g. trauma or surgical patients, Sharpe 2015), and may reduce antibiotic prescription (Conway Morris 2011; Fagon 2000), but is not often performed in European units (Koulenti 2009). Indeed, there may be variable tendency to perform chest radiography before starting a course of antibiotics for suspected ICU‐acquired respiratory tract infection (Szakmany 2013), and disagreement on the presence or absence of radiographic signs (Wunderink 2000), or clinical pulmonary features.
The Centers for Disease Control and Prevention's National Healthcare Safety Network (CDC/NHSN) have lately attempted to improve the reliability of surveillance for ventilator‐associated morbidity in the United States, concentrating on objective criteria (i.e. changes in oxygenation, inflammatory markers, the initiation of antibiotics and positive microbiology) and introducing a classification of "ventilator‐associated events" (VAEs) (Magill 2013), of which "possible VAP [PVAP]" now represents one example. Some concern has been raised at this relatively early stage that although developing a "ventilator‐associated complication" (VAC) on the basis of worse oxygenation may predict poorer clinical outcome (Boyer 2015; Hayashi 2013; Klein Klouwenberg 2014; Muscedere 2013), the overlap between an episode of VAC (defined according to surveillance needs) and an episode of historically defined VAP (according to the radiographic, clinical and microbiological criteria) appears to be limited (Boyer 2015; Hayashi 2013; Klein Klouwenberg 2014; Muscedere 2013; Stoeppel 2014). The potential utility of these newly defined conditions with respect to antibiotic prescription at the bedside is uncertain (Kipnis 2014).
Description of the intervention
A number of strategies to guide duration of antibiotic therapy in the treatment of HAP for the critically ill have been described. Antibiotics administered according to a fixed duration is the focus of this review (Chastre 2003a; Ibrahim 2001). National guidelines published within the last decade have recommended a course of antibiotic therapy for HAP of up to eight days when there has been good response to therapy (ATS/IDSA 2005; BSAC 2008), but a prolonged course of two to three weeks if response has been poor, or when infection is due to a non‐fermenting Gram‐negative bacillus (NF‐GNB), such as Pseudomonas aeruginosa (P. aeruginosa) (ATS/IDSA 2005), an organism particularly difficult to eradicate from the respiratory tract despite in vitro sensitivity to antibiotic therapy (Dennesen 2001; Visscher 2008), and an independent risk factor for VAP recurrence and mortality (Combes 2007; Kollef 1995).
Other strategies to limit duration of antibiotic therapy were explored in a previous version of this review (Pugh 2011). Such strategies may individualise and discontinue therapy according to resolution of clinical features (Micek 2004), to microbiological criteria (e.g. quantitative reduction in culture of respiratory specimens; Mueller 2007) or to a relevant biomarker, such as procalcitonin (Bouadma 2010; Stolz 2009a). Studies of procalcitonin‐guided antibiotic therapy in critically ill patients (e.g. Bouadma 2010; Jensen 2011; Nobre 2008; Stolz 2009a) have been explored in recent dedicated systematic reviews of patients with sepsis (Kopterides 2010) and acute respiratory tract infection (Schuetz 2012a; Schuetz 2012b). Of further interest is the recently reported use of extended infusion administration (e.g. Chant 2012) and novel methods of administration, e.g. nebulisation (e.g. Niederman 2012).
How the intervention might work
Resolution of clinical abnormalities associated with VAP is often observed within the first week of antibiotic therapy (Chastre 2003a; Dennesen 2001; Kollef 2012), particularly among ICU survivors (Luna 2003). For those that have responded to treatment, further prolongation of antibiotic therapy could lead to emergence of resistant organisms (Chastre 2003a; Dennesen 2001), may increase the risk of developing Clostridium difficile (C. difficile)‐associated disease (Bignardi 1998; Dubberke 2014) and antibiotic‐related toxicity, and will increase pharmacy costs.
Why it is important to do this review
Globally, nearly three‐quarters of ICU patients receive antibiotic therapy (Vincent 2009), and when prescribed to treat infection (as opposed to prophylaxis) the focus is directed overwhelmingly at the respiratory tract (Vincent 2009). Appropriate duration of antibiotic therapy is a key consideration in the optimal antimicrobial management (or antibiotic stewardship) of critically ill patients with HAP (Kollef 2012b); too short a course of therapy risks treatment failure, whereas too long a course of therapy carries unnecessary costs and poses potential risks for the individual patient and to other patients through the emergence of resistant organisms.
The optimal duration of antibiotic therapy for HAP (including VAP) in the critically ill is uncertain. Furthermore, when HAP is due to NF‐GNB, such as P. aeruginosa, the potential risk of treatment failure following short‐course therapy may be greater.
Objectives
To assess the effectiveness of short versus prolonged‐course antibiotics for HAP in critically ill adults, including patients with ventilator‐associated pneumonia (VAP).
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) comparing a 'short' versus 'prolonged' course of antibiotic therapy for clinical and microbiological outcomes in critically ill patients with established HAP (including VAP).
Types of participants
ICU patients (16 years and older) with HAP (including VAP) diagnosed by clinical and/or radiological features and/or quantitative culture of respiratory specimens. We excluded data regarding patients with haematological malignancy, chemically induced immune suppression or HIV/AIDS where possible.
Types of interventions
RCTs comparing a fixed 'short' (eight days or less) duration of antibiotic therapy with a 'prolonged' (including standard care) course of antibiotic therapy.
Types of outcome measures
Primary outcomes
28‐day mortality.
Recurrence of pneumonia (diagnosed on the basis of clinical and/or microbiological criteria).
28‐day antibiotic‐free days.
Secondary outcomes
ICU mortality.
In‐hospital mortality.
Clinical resolution of pneumonia (according to clinical and/or microbiological criteria).
Relapse of pneumonia.
Subsequent infection due to 'resistant organisms' (for example, methicillin‐resistant Staphylococcus aureus (S. aureus) (MRSA)).
Duration of ICU stay.
Duration of hospital stay.
Duration of mechanical ventilation (where appropriate).
Mechanical ventilation‐free days (where appropriate).
Mortality attributable to HAP.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (CENTRAL 2015, Issue 5), MEDLINE (1946 to 2015), MEDLINE in‐process and other non‐indexed citations (5 June 2015), EMBASE (to June 2015), LILACS (1982 to June 2015) and Web of Science (1955 to June 2015).
We used the search strategy described in Appendix 1 to search MEDLINE and CENTRAL. We combined the MEDLINE search strategy with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximising version (2008 revision); Ovid format (Lefebvre 2011). We modified these terms to search EMBASE (Appendix 2), LILACS (Appendix 3) and Web of Science (Appendix 4). We imposed no publication or language restrictions.
Searching other resources
We also searched the World Health Organization (WHO) International Clinical Trials Platform registers of controlled clinical trials, clinicaltrials.gov and the UK Clinical Trials Gateway (5 June 2015). We searched the Database of Abstracts of Reviews of Effects (DARE) for additional reviews. We searched reference lists of identified studies and review papers, and the OpenGrey database of grey literature. We also searched abstracts of recent conferences: International Symposium for Intensive Care and Emergency Medicine, European Society for Intensive Care Medicine, Society of Critical Care Medicine, American Thoracic Society, British Thoracic Society, European Respiratory Society, Chest, Infectious Disease Society of America and Interscience Conference on Antimicrobial Agents, and Chemotherapy.
Data collection and analysis
Selection of studies
Two review authors (RP, CG) independently analysed and reviewed the titles and abstracts of retrieved records for possible inclusion in this review. We used the following inclusion criteria: RCT, participants included ICU patients with HAP, comparison of fixed 'short' (eight days or less) duration of antibiotic therapy with 'prolonged' course antibiotic therapy, and relevant outcome data. We attempted to contact trial authors to clarify methods where indicated. We resolved any disagreements about study inclusion through consensus and, where needed, we involved a third review author (GD).
Data extraction and management
We used a standardised data extraction form. Two review authors (RP, CG) extracted data and entered these data into a Review Manager (RevMan) document (RevMan 2014). We contacted trial authors for any missing data.
Assessment of risk of bias in included studies
Two review authors (RP, GD) independently assessed the validity of studies using the Cochrane 'Risk of bias' tool (Sterne 2011). We resolved disagreements through consensus.
Measures of treatment effect
We used the following dichotomous data for measuring treatment effect:
mortality;
clinical resolution;
recurrence;
relapse;
infection with 'resistant organism'.
In addition, we collected the following continuous data:
durations of stay;
duration of mechanical ventilation;
ventilation‐ and antibiotic‐free days.
Unit of analysis issues
We did not identify significant unit of analysis issues (for example, randomisation of a group of individuals rather than an individual in a cluster‐randomised trial, or allocation of an individual to multiple interventions in a cross‐over trial).
Dealing with missing data
All studies presented data on the basis of the intention‐to‐treat (ITT) principle, i.e. all patients included in the study at the point of randomisation were analysed according to their assigned treatment group, regardless of whether or not treatment was completed.
Assessment of heterogeneity
We anticipated sources of heterogeneity relating to: participation factors (preceding durations of hospitalisation and mechanical ventilation, bacterial pathogen, prior antibiotic administration and illness severity) and intervention factors (class of antibiotic and method of administration). We anticipated that methodological diversity would be a significant source of heterogeneity. We assessed heterogeneity on the basis of the I2 statistic, interpreting a value below 40% as not suggestive of important heterogeneity (Higgins 2002).
Assessment of reporting biases
We attempted to minimise reporting bias by searching for unpublished trials and references to trial registries. Due to the small number of studies identified, we did not perform funnel plot tests for funnel plot asymmetry.
Data synthesis
We used the mean difference (MD) as a summary statistic for continuous measures and the odds ratio (OR) for dichotomous measures. We chose a random‐effects model for meta‐analysis given the clinical and methodological diversity of studies, and limited scope to explore heterogeneity through subgroup analysis.
Subgroup analysis and investigation of heterogeneity
A priori subgroups were:
duration of hospitalisation prior to development of pneumonia;
ventilator‐ and non‐ventilator‐associated HAP;
duration of mechanical ventilation prior to development of pneumonia;
administration of antibiotic therapy during hospital admission prior to development of pneumonia;
severity of illness;
chronic respiratory illness;
bacterial pathogen: NF‐GNB and MRSA;
class of antibiotic(s).
However, outcome data were insufficiently reported for individual subgroups to enable investigation of sources of heterogeneity with the exception of bacterial pathogen.
We did not perform meta‐regression owing to the low number of included studies (Deeks 2011).
Sensitivity analysis
We intended to perform sensitivity analysis if there were apparent differences in participants, interventions or methodology, irrespective of measures of study heterogeneity (I2 statistic).
The studies with which we had particular concerns in this respect were: Medina 2007 (since data has been published in abstract form only), Capellier 2012 (since participants were specifically selected for likelihood of "early‐onset" ventilator‐associated pneumonia) and Kollef 2012 (due to multiple differences between intervention measures), and on this basis, pooled results excluding data from these studies are presented in Appendix 5.
Results
Description of studies
Results of the search
The searches of CENTRAL (2015, Issue 5), MEDLINE (Ovid) from 1946 to June 2015, MEDLINE in‐process and other non‐indexed citations to June 2015, EMBASE to June 2015, LILACS to June 2015 and Web of Science to June 2015 produced 5878 results (after removal of duplicates). Further searching of DARE within The Cochrane Library 2015, Issue 5 identified 131 records. Searches of additional databases produced the following: Clinical.Trials.gov 113 results, WHO International Clinical Trials Registry Platform 83 results, UK Clinical Trials Gateway one result.
Of these, we undertook full‐text review of 12 potentially eligible studies (Capellier 2012; CCCTG 2006; Chastre 2003a; Chastre 2003b; Fagon 2000; Fekih Hassen 2009; Kim 2012; Kollef 2012; Micek 2004; Sanchez‐Nieto 1998; Singh 1998; Singh 2000). We identified five other potential studies from review articles and reference lists (Ibrahim 2001; Kollef 2005; Peery 2001; Rello 2004; Sole 2000). We found a further four studies on investigation of the 'grey literature', including relevant database searches and review of conference abstracts (Labelle 2012; Maldonado‐Ortiz 2004; Medina 2007; Wolff 2003). Review of trials registers identified three potentially relevant ongoing studies (NCT01994980; NCT00410527; NCT01554657).
Included studies
Six studies met the criteria for inclusion in this review, reporting data from a total of 1088 participants (Capellier 2012; Chastre 2003a; Fekih Hassen 2009; Kollef 2012; Medina 2007; Singh 2000). Summary data are presented in the Characteristics of included studies table. Of these, five were RCTs comparing fixed durations of antibiotic therapy in patients with VAP (Capellier 2012; Chastre 2003a; Fekih Hassen 2009; Kollef 2012; Medina 2007). The sixth study was a RCT comparing short (three‐day) course therapy with 'standard' duration therapy for patients with a low probability of HAP, of whom only 58% were mechanically ventilated. There are substantial differences between this study and the others, and data from this study are therefore not included in meta‐analysis (Singh 1998).
Of these six studies, only Kollef 2012 appears to have been blinded, though details about blinding were not available for Fekih Hassen 2009. However, as discussed below, there is a potential significant source of bias in Kollef 2012, since different antibiotic and antibiotic administration regimens were adopted for the seven‐day course (doripenem) and the 10‐day course (imipenem).
Participants
In terms of study size, the multi‐centre French Pneuma study dominates, having enrolled 401 participants (Chastre 2003a). A second multi‐centre French study (Capellier 2012) and an international multi‐centre study (Kollef 2012) recruited 225 and 274 participants, respectively, although in Kollef 2012 primary analysis is focused on the 167 participants fulfilling a "microbiological intention‐to‐treat (MITT)". A Uruguayan study, Medina 2007, recruited 77 participants and has not yet, to our knowledge, been published in a peer‐reviewed journal. A smaller single‐centre Tunisian study, which recruited 30 participants, has been published in a French language journal (Fekih Hassen 2009). The single‐centre US study by Singh 2000 enrolled 81 participants.
With respect to patient characteristics, the Pneuma study was specifically designed to compare durations of antibiotic therapy in a population likely to have a high proportion of more resistant bacteria, including NF‐GNB such as P. aeruginosa, by excluding participants with early VAP (within the first five days of mechanical ventilation) and no antimicrobial therapy within the preceding 15 days (Chastre 2003a); 33% cases of VAP were due to NF‐GNB, and 11% due to MRSA. Kollef 2012 intended to study participants with late‐onset VAP and for the "MITT" group to include only patients with Gram‐negative VAP; of this MITT group, 31% cases of VAP were due to mono‐microbial NF‐GNB; there were no cases of mono‐microbial MRSA VAP, but in 6.6% of cases MRSA was identified with another Gram‐negative organism. Higher proportions of VAP due to NF‐GNB were reported in Fekih Hassen 2009 (72%) and in Medina 2007 (64%). In contrast, Capellier 2012 intended to enrol participants with early‐onset VAP (mechanical ventilation for more than 24 hours, but less than eight days), and there were no cases of VAP due to NF‐GNB or MRSA. Lastly, Singh 2000 sought to recruit patients with a low probability of pneumonia, as determined by a Clinical Pulmonary Infection Score (CPIS, a composite score based upon high or low temperature, leukocyte count, quality of tracheal secretion, oxygenation and presence of radiographic infiltrates) of less than seven at day one and day three; pathogens associated with an episode of HAP were incompletely reported.
Antibiotics had been administered prior to the onset of VAP in 100% participants in Kollef 2012, 84% of participants in Chastre 2003a, and 68% of participants in Medina 2007. Data regarding previous antibiotic use were not provided in Fekih Hassen 2009 nor in Singh 2000, and prior antibiotic administration for pneumonia was an exclusion criterion in Capellier 2012.
Where reported, duration of mechanical ventilation prior to onset of VAP differed between studies: 14 days (Chastre 2003a), 10 days (Fekih Hassen 2009), nine days (Medina 2007), and three days (Capellier 2012). This duration was not reported in Kollef 2012, and in Singh 2000 42% participants were not mechanically ventilated at enrolment.
Presence of underlying respiratory disease was inadequately reported for comparison between studies, and for illness severity scores only limited comparison was possible; mean SAPS II (Simplified Acute Physiology Score II) scores were 45 for Chastre 2003a, 43 for Fekih Hassen 2009, and 39 for Capellier 2012; SOFA (Sequential Organ Failure Assessment) scores were mean 7.3 for Chastre 2003a and 5.8 for Kollef 2012, and median 6 for Medina 2007.
Pneumonia definitions varied between studies. All included the need for radiological and clinical features; in several studies the diagnosis of primary episode of VAP necessitated a threshold quantitative culture of broncho‐alveolar lavage (BAL; Capellier 2012; Chastre 2003a, the "MITT" cohort in Kollef 2012) or protected specimen brush (PSB) samples (Chastre 2003a). In Fekih Hassen 2009, threshold quantitative culture was permissible from endotracheal aspirate (ETA) or PSB, and in Medina 2007, quantitative culture was not required if the CPIS was above six, or blood or pleural cultures were positive. In contrast, for Singh 2000 an episode of HAP was defined according to the development of new infiltrates on chest radiography together with clinical suspicion, and microbiological confirmation was not required.
CPIS was not reported by Chastre 2003a or by Capellier 2012. However, CPIS was six or above in 92% participants in Kollef 2012 and 67% in Fekih Hassen 2009. In Singh 2000, patients with CPIS above six were excluded from study, and mean CPIS was 4.9 on day of enrolment.
Interventions
For the majority of studies, a short course of seven or eight days was compared with a prolonged course of 10 to 15 days. Capellier 2012 and Chastre 2003a allocated patients to receive either eight days or 15 days of antibiotic therapy, Fekih Hassen 2009 and Kollef 2012 to seven days or 10 days of therapy, and Medina 2007 to eight days or 12 days of therapy. Singh 2000 allocated patients whose CPIS remained less than seven on the third day of antibiotic therapy to receive either three days' antibiotic therapy or non‐fixed "standard course" therapy (typically 10 to 21 days at the start of the recruitment), as determined by the treating physician.
The most common classes of antibiotics used in Chastre 2003a were an aminoglycoside or quinolone plus beta‐lactam (91%); in Medina 2007, beta‐lactams were used in 90% of cases and aminoglycosides in 27% overall. In Capellier 2012, all participants received a beta‐lactam for the allocated duration, combined with an aminoglycoside for the first five days of therapy. Carbapenems were used in 100% cases in Kollef 2012, with doripenem in the short‐course group and imipenem in the prolonged‐therapy group. Antibiotic class data are not presented in Fekih Hassen 2009. In Singh 2000, ciprofloxacin monotherapy was used in the short‐course group, but varied widely in the standard‐therapy group (including glycopeptide, beta‐lactam, aminoglycoside and macrolide therapy).
Initial antibiotic therapy was appropriate (according to respiratory specimen culture and sensitivity results) in all cases in Capellier 2012 and Chastre 2003a (from which any patients initially treated with inappropriate antibiotics were subsequently excluded) and in Kollef 2012 (in which the pathogen's imipenem minimum inhibitory concentration, MIC, was confirmed as less than 8 μg/mL). In one case among each of the short‐course and prolonged‐therapy groups the initial antibiotic therapy was inappropriate in both Fekih Hassen 2009 and Medina 2007. Appropriateness of initial therapy is not described in Singh 2000.
Uniquely among the included studies, Kollef 2012 allocated patients in the short‐course doripenem group to receive their antibiotic therapy as a theoretically favourable four‐hour infusion every eight hours (according to pharmacokinetic/pharmacodynamic models), whereas in the prolonged‐course group imipenem was administered as a one‐hour infusion eight‐hourly.
Outcomes
Although some unambiguous outcome measures were reported in the included studies (mortality, length of stay, duration of mechanical ventilation), discussion is required regarding other measures, including 'clinical resolution', 'recurrence' and 'relapse'.
The term 'clinical resolution' used in this review refers to the outcome measures described by Capellier 2012 ('clinical cure', evaluated at day 21 according to clinical and radiographic criteria), Kollef 2012 ('clinical cure', or resolution of clinical features and improvement or lack of progression of radiographic response to therapy, evaluated at day 10 of study) and Medina 2007 ('clinical resolution', described as lessening of symptoms and signs of infection such that additional therapy is not required, evaluation day unspecified).
'Recurrence' data were presented by Capellier 2012, Chastre 2003a, Fekih Hassen 2009, and Medina 2007. In Chastre 2003a, an episode of recurrence, whether relapse (i.e. due to same initial causative organism) or super‐infection (i.e. due to other organism), again required threshold quantitative culture of BAL or PSB; distal respiratory tract sampling could be prompted by changes in oxygenation or haemodynamic status, or development of fever, purulent secretions or new infiltrates on chest radiography. For Capellier 2012, a relapse was defined as culture of original organism in conjunction with clinical or radiological signs of pneumonia or worsening SOFA score. In Fekih Hassen 2009, episodes of recurrence ('réinfection') were described in terms of infection due to initial organism or other organism, presumably using the same clinical, radiographic and microbiological criteria as for a primary episode of VAP. Medina 2007 defined episodes of recurrence according to clinical and microbiological features occurring 72 hours or more after completing an initial course of antibiotic therapy.
Excluded studies
We excluded studies if they had been published as a full paper elsewhere (Chastre 2003b; Singh 1998; Wolff 2003), were not RCTs (Ibrahim 2001; Kollef 2005; Rello 2004), investigated a diagnostic strategy (CCCTG 2006; Fagon 2000; Peery 2001; Sanchez‐Nieto 1998; Sole 2000), or used a de‐escalation or discontinuation clinical protocol (Kim 2012; Micek 2004), or biomarker (Bouadma 2010; Micek 2004; Pontet 2007; Stolz 2009a), to guide duration of therapy rather than comparing fixed durations of therapy. We also excluded two studies published in abstract form: Maldonado‐Ortiz 2004 because of inadequate outcome data and perceived risk of bias, and Labelle 2012 because fixed courses of therapy appear not to have been utilised and duration of therapy was not significantly different between groups.
Please refer to the Characteristics of excluded studies table.
Risk of bias in included studies
Risk of bias is presented in detail in the Characteristics of included studies table, presented graphically in Figure 1 and summarised in Figure 2.
1.
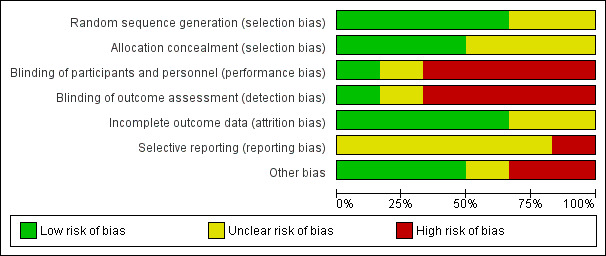
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2.
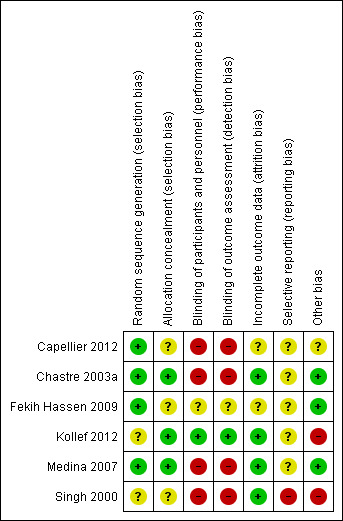
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Sequence generation was adequate in four studies (Capellier 2012; Chastre 2003a; Fekih Hassen 2009; Medina 2007), and unclear in two studies (Kollef 2012; Singh 1998). Allocation concealment was adequate in three studies (Chastre 2003a; Kollef 2012; Medina 2007), and unclear in three studies (Capellier 2012; Fekih Hassen 2009; Singh 2000).
Blinding
In only one of the studies were there efforts to blind (Kollef 2012). In one study it was unclear whether blinding had been used and contact with the authors has been unsuccessful (Fekih Hassen 2009). Four studies were unblinded (Capellier 2012; Chastre 2003a; Medina 2007; Singh 2000).
Incomplete outcome data
Incomplete outcome data reporting was adequate in four studies (Chastre 2003a; Kollef 2012; Medina 2007; Singh 2000), and unclear in two (Capellier 2012; Fekih Hassen 2009).
Selective reporting
Selective reporting appears to have been a feature of one study (Singh 2000), and was unclear in five (Capellier 2012; Chastre 2003a; Fekih Hassen 2009; Kollef 2012; Medina 2007).
Other potential sources of bias
Interpretation of Kollef 2012 is made more difficult by there having been multiple interventions: the study compares a short course of one antibiotic administered according to theoretically favourable pharmacokinetic modelling versus a prolonged course of another antibiotic administered over a shorter, more conventional time course. Furthermore, the study was stopped early, having enrolled approximately half of the target (480) recruitment, on the basis of inferior efficacy and greater mortality in the short‐course therapy group. Lastly, data from five sites, which had enrolled 41 patients, were excluded from primary analysis because of poor compliance with agreed good clinical practice.
Singh 1998 was stopped early by an institutional review board. Results for patients managed in the 'experimental' group appear to have influenced management of patients subsequently allocated to the 'standard therapy group'.
Effects of interventions
See: Table 1
Outcomes are presented in detail (including forest plots) in the Data and analyses section below. Outcomes are summarised in Table 1 below.
Primary outcomes
1. 28‐day mortality
Twenty‐eight‐day mortality was reported in three studies and did not differ significantly between short‐course and prolonged‐course therapy groups upon meta‐analysis (odds ratio (OR) 1.18; 95% confidence interval (CI) 0.77 to 1.80; Analysis 1.1); despite differences in study characteristics, heterogeneity appeared to be low (I2 statistic = 0%) (Chastre 2003a; Fekih Hassen 2009; Kollef 2012). Twenty‐eight‐day mortality was reported as significantly greater in the small subgroup of patients in Kollef 2012 with ventilator‐associated pneumonia (VAP) due toP. aeruginosa treated with short‐course therapy (6/17 (35.3%) versus 0/10 (0.0%); 95% CI 12.6% to 58.0%; Kollef 2012). However, including data for patients with other non‐fermenting Gram‐negative bacilli (NF‐GNB) VAP (i.e. Acinetobacter spp.) from this study together with patients with NF‐GNB VAP from Chastre 2003a in meta‐analysis, there was no significant difference in 28‐day mortality between short‐ and prolonged‐course therapy (Analysis 1.1). Similarly, we identified no differences in 28‐day mortality between intervention groups for patients with VAP due to MRSA, and between groups for patients with VAP not due to MRSA/NF‐GNB, or with an unspecified organism.
1.1. Analysis.
Comparison 1 Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP, Outcome 1 28‐day mortality.
We performed sensitivity analysis to exclude data from Kollef 2012, given concerns regarding multiple interventions, premature cessation and compliance of several centres with agreed good clinical practice, but this did not lead to significant differences in 28‐day mortality on meta‐analysis (Appendix 5).
2. Recurrence of pneumonia
Recurrence data were presented in four VAP studies (Capellier 2012; Chastre 2003a; Fekih Hassen 2009; Medina 2007). Overall, there was a trend to increased recurrence following a short course of therapy (OR 1.41; 95% CI 0.94 to 2.12; Analysis 1.2; I2 statistic = 5%, suggesting low heterogeneity) in treatment of VAP. However, meta‐analysis of the two studies reporting recurrence data specifically for patients with VAP due to NF‐GNB demonstrated significantly greater recurrence for VAP due to NF‐GNB in the short‐course group (OR 2.18; 95% CI 1.14 to 4.16; P value = 0.02; Analysis 1.2; I2 statistic = 0%), though recurrence rate due to multi‐resistant organism was lower in the short‐course group in one study (OR 0.44; 95% CI 0.21 to 0.95; data from Chastre 2003a only; Analysis 1.11).
1.2. Analysis.
Comparison 1 Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP, Outcome 2 Recurrence of pneumonia.
1.11. Analysis.
Comparison 1 Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP, Outcome 11 Subsequent infection due to resistant organism.
We performed a sensitivity analysis to exclude data from Medina 2007 (data currently published in abstract form only) and from Capellier 2012 (early‐onset VAP). On exclusion of data from Medina 2007, increased recurrence following short‐course therapy for VAP due to NF‐GNB was no longer statistically significant (Appendix 5).
3. 28‐day antibiotic‐free days
Chastre 2003a and Fekih Hassen 2009 provided data on 28‐day antibiotic‐free days for patients with VAP (total number of antibiotic‐free days over the 28‐day period, which begins with onset of VAP and commencement of antibiotics). Antibiotic‐free days were significantly greater in the short‐course group (mean difference (MD) 4.02 days; 95% confidence interval (CI) 2.26 to 5.78; Analysis 1.3; I2 statistic = 68%, indicating a high degree of heterogeneity) among patients with VAP due to all organisms (two studies), and in subgroups of patients with VAP due to NF‐GNB or MRSA (one study).
1.3. Analysis.
Comparison 1 Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP, Outcome 3 28‐day antibiotic‐free days.
With regards to other measures of antibiotic exposure, for HAP patients randomised to the short‐course therapy group in Singh 2000, 28% of patients received antibiotics for more than three days, compared with 97% in the standard‐therapy group (P value = 0.0001).
Secondary outcomes
1. Intensive care unit (ICU) mortality
We identified no significant differences between short‐ and prolonged‐course antibiotic therapy with respect to ICU mortality, reported in two studies (Fekih Hassen 2009; Medina 2007) (Analysis 1.4).
1.4. Analysis.
Comparison 1 Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP, Outcome 4 ITU mortality.
2. In‐hospital mortality
We identified no significant differences between short‐ and prolonged‐course antibiotic therapy with respect to hospital mortality, reported in one study (Chastre 2003a) (Analysis 1.5).
1.5. Analysis.
Comparison 1 Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP, Outcome 5 In‐hospital mortality.
Other mortality outcomes were reported with respect to: 21 days (Capellier 2012; Analysis 1.6), 60 days (Chastre 2003a; Analysis 1.7), and 90 days (Capellier 2012; Analysis 1.8). Again, we identified no significant differences between short‐ and prolonged‐course antibiotic therapy.
1.6. Analysis.
Comparison 1 Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP, Outcome 6 21‐day mortality.
1.7. Analysis.
Comparison 1 Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP, Outcome 7 60‐day mortality.
1.8. Analysis.
Comparison 1 Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP, Outcome 8 90‐day mortality.
We separately considered data from Singh 1998, given the high proportion of non‐ventilated patients and the prerequisite that all included patients were at low risk of having pneumonia, according to Clinical Pulmonary Infection Score (CPIS). A trend towards lower 30‐day mortality was identified by the study authors in the short‐course group (OR 0.33; 95% CI 0.10 to 1.03). Outcomes for patients who were and were not mechanically ventilated were not reported separately.
3. Clinical resolution of pneumonia
Clinical resolution outcomes were reported in three studies: Capellier 2012 (evaluated at day 21), Kollef 2012 (evaluated at day 10) and Medina 2007 (unclear evaluation date). We observed a non‐significantly lower clinical resolution between treatment groups (OR 0.75; 95% CI 0.49 to 1.15; Analysis 1.9; I2 statistic = 0%) for all patients, and for the small subgroup patients with VAP due to NF‐GNB reported in one study (Kollef 2012). The authors of this last study also noted a significantly lower CPIS on day 11 among the prolonged‐therapy group compared with the short‐course group.
1.9. Analysis.
Comparison 1 Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP, Outcome 9 Clinical resolution.
4. Relapse of pneumonia
Relapse of pneumonia was non‐significantly higher following short‐course therapy for VAP among patients as a whole (OR 1.70; 95% CI 0.97 to 2.97; Analysis 1.10) and the subgroup with NF‐GNB (OR 2.08; 95% CI 0.92 to 4.70) in two studies (Capellier 2012; Chastre 2003a).
1.10. Analysis.
Comparison 1 Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP, Outcome 10 Relapse of pneumonia.
5. Subsequent infection due to 'resistant organisms'
Recurrence rate due to multi‐resistant organisms was lower in the short‐course group in one study (OR 0.44; 95% CI 0.21 to 0.95; data from Chastre 2003a only; Analysis 1.11).
Singh 2000 reported a composite measure of antibiotic resistance and/or superinfection following treatment of HAP; in the short‐course group, this adverse outcome rate was found to be significantly lower at 13% versus 33% (P value = 0.03; Analysis 2.2).
2.2. Analysis.
Comparison 2 Discontinuation of antibiotics according to Clinical Pulmonary Infection Score, Outcome 2 Episodes of superinfection or antimicrobial resistance.
6. Duration of ICU stay
Duration of ICU stay did not differ significantly between patients with VAP treated according to short‐course and prolonged‐course therapy (Analysis 1.12).
1.12. Analysis.
Comparison 1 Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP, Outcome 12 Duration of ICU stay.
Singh 2000 reported a significantly reduced mean length of ICU stay in the short‐course therapy group (9.4 versus 14.7 days; standard deviation (SD) data not presented; P value = 0.04).
7. Duration of hospital stay
Duration of hospital stay did not differ significantly between patients with VAP treated according to short‐course and prolonged‐course therapy (Analysis 1.13).
1.13. Analysis.
Comparison 1 Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP, Outcome 13 Duration of hospital stay.
8. Duration of mechanical ventilation
Duration of mechanical ventilation did not differ significantly between patients with VAP treated according to short‐course and prolonged‐course therapy (Analysis 1.14).
1.14. Analysis.
Comparison 1 Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP, Outcome 14 Duration of mechanical ventilation.
9. Mechanical ventilation‐free days
28‐day mechanical ventilation‐free days were reported in two studies, and did not differ significantly between study groups: mean 8.7 days (SD 9.1) in the short‐course and 9.1 days (SD 9.4) in the prolonged‐therapy group (Chastre 2003a), and 3.4 (SD 1.9) days in the short‐course versus 2.1 (SD 1.8) days in the prolonged‐therapy group (Fekih Hassen 2009).
10. Mortality attributable to HAP
The included trials did not report this outcome.
Discussion
Summary of main results
We identified six studies, which had enrolled a total of 1088 participants with pneumonia (92% of whom had ventilator‐associated pneumonia (VAP)) defined according to diverse radiological, clinical and microbiological criteria. There were notable differences in patient characteristics and interventions between studies, though for the most part this was not reflected in statistical heterogeneity.
Considering the five studies that compared fixed durations of antibiotic therapy for VAP (seven to eight days versus 10 to 15 days), a shorter course of therapy was associated with significantly reduced antibiotic exposure in terms of 28‐day antibiotic‐free days in two studies (mean difference (MD) 4.02 days; 95% confidence interval (CI) 2.26 to 5.78), without any significant increase in mortality, duration of mechanical ventilation or duration of hospital stay, and irrespective of pathogen (Chastre 2003a; Fekih Hassen 2009). One study reported that a shorter course of antibiotic therapy was associated with a significant reduction in VAP recurrence due to multi‐resistant organisms (odds ratio (OR) 0.44; 95% CI 0.21 to 0.95) (Chastre 2003a).
Clinical resolution of VAP was non‐significantly lower (Capellier 2012; Kollef 2012; Medina 2007) (OR 0.75; 95% CI 0.49 to 1.15) and recurrence was non‐significantly greater (Capellier 2012; Chastre 2003a; Fekih Hassen 2009; Medina 2007) (OR 1.41; 95% CI 0.94 to 2.12) for patients treated with a short course of therapy. A significant increase in recurrence was observed in the subgroup of patients with VAP due to non‐fermenting Gram‐negative bacilli (NF‐GNB) (Chastre 2003a; Medina 2007) (OR 2.18; 95% CI 1.14 to 4.16), though not for those with VAP due to methicillin‐resistant Staphylococcus aureus (MRSA). Despite this, short‐course therapy for VAP due to NF‐GNB was not associated with other significantly poorer outcomes, in terms of mortality, mechanical ventilation‐free days and length of stay (Table 1).
For critically ill patients with suspected HAP (whether mechanically ventilated or not) but a low probability of pneumonia (according to a day one and day three Clinical Pulmonary Infection Score (CPIS) below seven; Singh 2000), discontinuing antibiotic therapy at day three was associated with significantly shorter duration of antibiotic therapy (mean three days versus 9.8 days; P value = 0.0001 reported), a significantly reduced composite rate of superinfection and antimicrobial resistance (OR 0.29; 95% CI 0.09 to 0.92) and a significantly reduced duration of intensive care unit (ICU) stay.
Overall completeness and applicability of evidence
In this review, we have included only those studies using fixed durations of antibiotic therapy for hospital‐acquired pneumonia (HAP) in the critically ill; thus (unlike the previous version of our review), we have excluded studies that evaluated clinical response (e.g. Micek 2004) or a biomarker (procalcitonin; e.g. Stolz 2009a) as a guide to variable courses of antibiotic therapy. The included studies enrolled 1088 medical and surgical (including cardio‐thoracic and neuro‐surgical) critically ill adults with HAP from ICUs in Africa, Asia, Europe, and North, Central and South America. However, studies were few in number, and participants, interventions and reported outcomes varied considerably. Furthermore, we identified only one study presenting outcome data for patients with HAP who were not receiving mechanical ventilation; separate outcome data are not presented for those subgroups of patients who were and were not receiving mechanical ventilation, and indeed all of the enrolled patients were required to have 'low probability' of pneumonia according to CPIS (Singh 2000). All other included studies focused entirely on patients with VAP. This limitation is important since there may be differences in patient characteristics and in bacterial aetiology between ICU cases of nosocomial pneumonia acquired in the presence or absence of assisted mechanical ventilation (Esperatti 2010; Kohlenberg 2010); therefore, guidance that attempts to extrapolate from studies of patients with VAP to non‐ventilated patients with HAP may potentially be flawed.
For critically ill patients (not necessarily requiring mechanical ventilation) with new radiographic infiltrates and a suspicion but low probability of pneumonia (for example, according to CPIS on day of diagnosis and 72 hours later), a short course (three days) of appropriate antibiotic therapy appears to be more suitable than a prolonged (10‐ to 21‐day) course (Singh 2000), though the generalisability of empiric ciprofloxacin monotherapy may be debated. Current American (ATS/IDSA 2005), British (BSAC 2008), and Canadian (Rotstein 2008) guidelines do not make any specific recommendations for this particular scenario.
A fixed seven‐ to eight‐day course (rather than a 10‐ to 15‐day course) of antibiotic therapy appears to reduce overall antibiotic exposure and, on the basis of one study, to reduce the risk of further infection associated with resistant organisms. However, pooled data from two studies enrolling a total of 176 patients with VAP due to NF‐GNB, indicated that a fixed, short course of antibiotic therapy (seven or eight days) was associated with significantly increased risk of recurrence compared with a more prolonged course (12 or 15 days) (Chastre 2003a; Medina 2007). Outcome data for a subgroup of patients with VAP due to NF‐GNB were presented in only one other study; a trend to lower clinical resolution following short‐course therapy was seen among patients with and without VAP due to NF‐GNB, and a higher CPIS was observed at day 10 after short‐course therapy (Kollef 2012).
Given the (non‐significantly) lower clinical resolution among patients treated with short‐course therapy and significantly higher recurrence among patients with VAP due to NF‐GNB, data regarding the continued presence of bacterial pathogens (e.g. Pseudomonas sp.) in respiratory specimens during and after fixed‐duration therapy may also have been of interest but were not routinely reported in the included studies.
Diagnostic criteria for defining an episode of pneumonia were not uniform, and no study reported using the new Centers for Disease Control and Prevention (CDC) classification of ventilator‐associated events, including possible VAP (PVAP).
Unfortunately, insufficient outcome data were available to allow exploration of other subgroups of interest, for example: presence of chronic respiratory illness, illness severity, prior administration of antibiotic therapy, prior duration of mechanical ventilation (i.e. early‐ or late‐onset VAP) and class of antibiotic (including combination therapy). Durations of therapy incorporating more novel modes of administration of potential interest were confounded by multiple interventions (e.g. extended infusion versus standard infusion, doripenem versus imipenem, short course versus prolonged course) or did not meet the inclusion criteria for this review (e.g. use of nebulised antibiotics, such as Niederman 2012).
Subsequent infection due to resistant organisms was reported in only two studies (one of which reported as a composite measure only). Emergence of extra‐pulmonary infection, in particular, C. difficile‐associated disease, was surprisingly not reported at all.
Both American (ATS/IDSA 2005) and British (BSAC 2008) guidelines recommend that efforts should be made to shorten antibiotic therapy for HAP (including patients with VAP) to a duration of seven to eight days, where there has been clinical response and, in the case of American Thoracic Society/Infectious Diseases Society of America (ATS/IDSA) guidelines, where the causative organism is not P. aeruginosa. Overall, our review was broadly consistent with these guidelines; nevertheless, in the context of VAP due to NF‐GNB, short‐course therapy is unlikely to be appropriate for all patients and the optimal duration remains uncertain.
Quality of the evidence
Differences in participants, interventions and reported outcomes between studies meant that the number of studies contributing to a particular summary statistic was very small. We considered selection bias to be at low risk in three of the six included studies. Blinding occurred in only one of the six studies. We felt that there was significant other bias in two of the studies, because of multiple differences between intervention groups (Kollef 2012), and because of contamination of the control group with early termination of the study (Singh 2000). We therefore assessed the quality of evidence according to the GRADE classification as low to moderate for the main outcome measures (Table 1).
Potential biases in the review process
We attempted to minimise bias in a number of ways. Our search strategy utilised the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE. In addition, we searched review articles and the 'grey literature' to minimise reporting bias. We established inclusion criteria prior to conduct of searches and, where necessary, we contacted trial authors to clarify study eligibility. We collected data using a standardised data collection form; when not available, we contacted trial authors to provide additional relevant data. We systematically assessed internal validity using the Cochrane 'Risk of bias' tool.
The potential for study heterogeneity was evident at the planning stage of this review, for example, in terms of methodology, diagnostic criteria, illness severity and antibiotic class. We identified relevant subgroups a priori. However, outcome data were typically not presented in sufficient detail to enable adequate subgroup analysis (e.g. according to prior administration of antibiotic therapy, prior duration of mechanical ventilation, classes of antibiotic including combination therapy) and given methodological differences we used a random‐effects model for meta‐analysis.
With a very small number of included studies, we were able to meta‐analyse data from a maximum of four (and more frequently only two or three) studies per outcome. We included studies that focused on early‐onset VAP (Capellier 2012), and those that primarily recruited patients with later‐onset VAP (e.g. Chastre 2003a; Kollef 2012), with the intention of analysing according causative organism (e.g. NF‐GNB). We felt that this approach was appropriate, particularly given that the relationship between early‐ versus late‐onset VAP and the likelihood of pneumonia being due to a resistant organism has been questioned in recent reports (Gastmeier 2009; Martin‐Loeches 2015; Restrepo 2013).
Due to marked differences in participants, interventions and reported outcomes between Singh 2000 and other studies, we considered outcomes for that study separately.
We performed sensitivity analysis to exclude the results of Kollef 2012 from 28‐day mortality data, which did not produce different findings. We also performed sensitivity analysis to exclude Capellier 2012 (given its focus on early onset VAP) and Medina 2007 (since it has been published only in abstract form) from the recurrence results, which led to recurrence among the subgroup of patients with VAP due to NF‐GNB no longer being statistically significant.
Agreements and disagreements with other studies or reviews
Three systematic reviews specifically focusing on duration of antibiotic therapy for VAP have been published (Dimopoulos 2013; Dugan 2003; Grammatikos 2008). The two earlier of these reviews included observational studies and studies focused on diagnostic strategies (for example, invasive versus noninvasive diagnosis of VAP, Fagon 2000). Notably, the Dugan 2003 review also appears to have been written before publication of the Pneuma study, the largest randomised controlled trial (RCT) to date to investigate duration of therapy for VAP (Chastre 2003a). The most recently published systematic review, Dimopoulos 2013, restricted itself to RCTs as did we, but excluded Singh 2000 (presumably on the basis that it included non‐ventilated patients and all patients had a low probability of pneumonia) and Medina 2007 (since it is currently published in abstract form only). In their review, relapse was chosen as a primary outcome measure rather than recurrence.
The conclusions of Grammatikos 2008, namely that short‐course antibiotic therapy for VAP not caused by NF‐GNB does not appear to adversely affect mortality, recurrence or length of stay (Grammatikos 2008), are consistent with the findings from our review and those of Dimopoulos 2013. Dugan 2003 concluded that shorter‐course therapy may be associated with reduced antimicrobial resistance, which is consistent with Chastre 2003a. However, studies published subsequent to their review have been less supportive of the benefits of short‐course therapy in reducing ICU and hospital length of stay. Having excluded Medina 2007, the systematic review published by Dimopoulos 2013 reported a non‐significantly greater relapse in patients with VAP due to NF‐GNB treated with short‐course therapy, rather than the significantly greater recurrence that we found upon meta‐analysis.
Our finding that short‐course antibiotic therapy for VAP in the absence of NF‐GNB may be adequate, without increased risk of recurrence or mortality, is consistent with data from observational studies. Dennesen 2001 demonstrated in 27 cases of VAP treated with appropriate initial antimicrobial therapy that clinical resolution occurred within the first six days of treatment and that S. pneumoniae, H. influenzae and S. aureus were eradicated within this period. In contrast, in Dennesen's study P. aeruginosa was isolated from endotracheal aspirates in all patients 15 days after the initiation of therapy, despite a mean 12.7 days of antibiotic treatment. Similarly, after seven days' appropriate antibiotic therapy for VAP, El Solh 2007 observed a disparity between clinical response and persistent respiratory colonisation, with P. aeruginosa continuing to be cultured from broncho‐alveolar lavage (BAL) despite improvements in CPIS. This persistence may be clinically significant. Zhuo 2008 demonstrated that the bacterial load in mechanically ventilated patients colonised with P. aeruginosa but without meeting the clinical criteria for VAP may predict outcome; in their study, high P. aeruginosa load was associated with a significantly greater 28‐day mortality.
A reliable measure of clinical or microbiological response to treatment has appeal as a means of identifying those for whom a shorter course of therapy may be appropriate, particularly among those with VAP due to NF‐GNB. Kollef observed 10 days after initiation of antibiotic therapy for VAP due to Gram‐negative bacteria, that CPIS was lower among patients treated for 10 days rather than seven days (Kollef 2012). In a non‐randomised study, use of repeat BAL to guide duration of therapy for VAP in surgical/trauma patients led to a reduction in duration of therapy among patients with VAP due to NF‐GNB compared with a control group (mean 10.7 versus 14.4 days respectively) without there being any overall increase in ventilator‐free ICU days, in‐hospital mortality and VAP relapse (Mueller 2007). Bouadma 2010, Pontet 2007, and Stolz 2009a reported reductions in antibiotic exposure in patients with VAP treated according to a procalcitonin‐guided algorithm compared with standard treatment in RCTs, without observing an increase in mortality. Recurrence rates did not differ between groups in one of these studies (Pontet 2007), though outcomes for patients specifically with NF‐GNB VAP were not reported at all.
To summarise, there are very few data for non‐ventilated patients with HAP. For patients with VAP, although short‐course (seven to eight days) therapy for VAP generally appears to be safe, the increased rate of recurrence of VAP due to NF‐GNB among patients administered a fixed, short course of antibiotic therapy demonstrated in our review may reflect inadequate microbiological and/or clinical response to treatment. It would therefore appear that further work is warranted to establish the optimal duration of therapy particularly for these patients, perhaps involving strategies that enable individualisation of treatment.
Authors' conclusions
Implications for practice.
Our review identified very few data regarding the appropriate duration of antibiotic therapy for intensive care unit (ICU) patients with hospital‐acquired pneumonia (HAP) who are not mechanically ventilated. However, where HAP is suspected (in mechanically or non‐mechanically ventilated patients), but there is a low probability of pneumonia according to clinical pulmonary infection score (CPIS), a fixed three‐day course of therapy appears to significantly reduce antibiotic administration, risk of emergence of resistant organisms or superinfection, and duration of ICU stay, according to a single study.
On the basis of a very small number of studies of patients with ventilator‐associated pneumonia (VAP), adopting a seven‐ or eight‐day course of antibiotic therapy in the absence of non‐fermenting Gram‐negative bacilli (NF‐GNB) infection is associated with a significant increase in 28‐day antibiotic‐free days (two studies) and reduced VAP recurrence due to multi‐resistant organisms (one study), without adverse effects on overall recurrence or mortality, compared with a 10‐ to 15‐day course.
However, for patients with VAP due to NF‐GNB organisms, a short eight‐day course is associated with a higher rate of VAP recurrence than a prolonged 12‐ to 15‐day course, on the basis of pooled data from two studies. This greater risk of recurrence does not appear to be associated with an increased mortality, or prolonged requirement for mechanical ventilation or duration of ICU stay.
The single study utilising an extended infusion of antibiotics according to pharmaco‐dynamic/kinetic profile for Gram‐negative VAP did not demonstrate superior clinical outcomes.
There is a notable lack of data regarding emergence of C. difficile‐related infection with different antibiotic strategies.
In summary, use of short‐course (seven‐ to eight‐day) therapy for VAP is likely to reduce antibiotic exposure in the critically ill, with reduced emergence of resistant organisms, and potential for reduction in antibiotic‐associated morbidity and cost savings, but is unlikely to be appropriate for all patients with VAP due to NF‐GNB. Appreciating the current lack of data, these findings appear broadly to support current guidelines (ATS/IDSA 2005; BSAC 2008; Rotstein 2008).
Implications for research.
There are inadequate data regarding the appropriate duration of antibiotic therapy for HAP in non‐mechanically ventilated patients; characteristics differ sufficiently between this group and those with VAP for this to warrant further research. However, even for patients with VAP, there are very few randomised controlled trials (RCTs) evaluating strategies intended to limit unnecessary antibiotic treatment.
The relative merits of fixed short versus prolonged‐course antibiotic therapy have been under‐explored, and the optimal duration of therapy for patients with NF‐GNB VAP is particularly unclear. The literature on this topic is still dominated by the Pneuma study, which was published over a decade ago.
Major differences in definitions of pneumonia were evident in these studies, and arguably there is a need for greater standardisation. The relationship between a historically defined episode of ICU‐acquired pneumonia (using clinical, radiographic and microbiological criteria) and newer surveillance definitions (i.e. the new Centers for Disease Control and Prevention (CDC) ventilator‐associated event classification) appears to need further exploration. Currently, the clinical utility of these newly defined conditions is unproven and optimal antibiotic use in the context of "possible VAP" (PVAP) or infection‐related ventilator‐associated condition (I‐VAC), for example, is not clear.
Short‐course therapy does not appear to be appropriate for all patients with VAP due to NF‐GNB, and clinical response to treatment may be at variance with bacterial persistence. Further research to explore the value of continued antibiotic administration beyond seven to eight days for NF‐GNB VAP is necessary. The relationships between bacterial persistence (which in turn may be related to virulence factors), clinical response (e.g. according to Clinical Pulmonary Infection Score) and relevant biomarkers (e.g. procalcitonin) should be explored in more detail for VAP due to NF‐GNB, and ideally reported according to standardised outcome measures (e.g. 28‐day relapse, mortality, mechanical ventilation‐free days and antibiotic‐free days). There is a current lack of data regarding the emergence of C. difficile‐related disease with different antibiotic strategies in the critically ill. Furthermore, there appears to be scope to explore the appropriate duration of therapy for NF‐GNB VAP according to use of class or combination antibiotic therapy, extended administration according to pharmaco‐dynamic/kinetic profile, and novel methods of administration (e.g. nebulised therapy).
What's new
| Date | Event | Description |
|---|---|---|
| 5 June 2015 | New citation required but conclusions have not changed | Updated review. Our conclusions regarding fixed duration of therapy remain unchanged. We have not reviewed studies in this update with regards to strategies to discontinue antibiotic therapy on the basis of clinical features or a biomarker. |
| 5 June 2015 | New search has been performed | Searches updated. We included two new studies (Capellier 2012; Kollef 2012) and excluded four studies, which had previously been included in our review (Bouadma 2010; Micek 2004; Pontet 2007; Stolz 2009a). |
History
Protocol first published: Issue 1, 2009 Review first published: Issue 10, 2011
| Date | Event | Description |
|---|---|---|
| 11 January 2012 | Amended | Abstract error corrected. |
Acknowledgements
We would like again to thank Julio Medina and Julio Pontet for making available additional study data during the preparation of our original review. We are grateful to the Cochrane Acute Respiratory Infections Group editorial staff for their help with the conduct of the review, in particular to Elizabeth Dooley. We would like also to thank Sarah Thorning, Justin Clark and Susan Mahoney for their help in the design and conduct of our searches.
Appendices
Appendix 1. MEDLINE (Ovid) search strategy
1 exp Pneumonia/ 2 Respiratory Tract Infections/ 3 (respiratory adj3 infect*).tw. 4 (pneumon* or pleuropneumon* or bronchopneumon* or bronchit* or tracheobronchit*).tw. 5 or/1‐4 6 exp Cross Infection/ 7 cross infect*.tw. 8 (infection* adj3 (hospital* or nosocomial)).tw. 9 exp Intensive Care Units/ 10 ((hospital* or health care* or healthcare* or health‐care* or nosocomial* or ventilator* or icu or intensive care) adj3 (acquired or associat*)).tw. 11 exp Respiration, Artificial/ 12 exp Ventilators, Mechanical/ 13 (respirator* or ventilator*).tw. 14 or/6‐13 15 5 and 14 16 Pneumonia, Ventilator‐Associated/ 17 (hap or vap).tw. 18 15 or 16 or 17 19 exp Anti‐Bacterial Agents/ 20 antibiotic*.tw. 21 exp Glycopeptides/ 22 exp Oxazolidinones/ 23 exp Carbapenems/ 24 beta‐lactams/ or exp cephalosporins/ 25 exp Aminoglycosides/ 26 exp Fluoroquinolones/ 27 exp Polymyxins/ 28 (glycopeptide* or vancomycin* or teicoplanin* or oxazolidinone* or linezolid* or carbapenem* or meropenem* or imipenem* or doripenem or ertapenem* or beta‐lactam* or betalactam* or beta lactam* or cephalosporin* or cefuroxime* or cefotaxime* or ceftriaxone* or ceftazidime* or cefipime* or piperacillin* or aminoglycoside* or gentamicin* or amikacin* or tobramycin* or fluoroquinolone* or ciprofloxacin* or levofloxacin* or moxifloxacin* or lipoglycopeptide* or telavancin* or glycylcycline* or tigecycline* or polymyxin* or colistin*).tw,nm. 29 or/19‐28 30 18 and 29
Appendix 2. Embase.com search strategy
#25 #19 AND #24 #24 #20 OR #21 OR #22 OR #23 #23 glycopeptide*:ab,ti OR vancomycin*:ab,ti OR teicoplanin*:ab,ti OR oxazolidinone*:ab,ti OR linezolid*:ab,ti OR carbapenem*:ab,ti OR meropenem*:ab,ti OR imipenem*:ab,ti OR doripenem:ab,ti OR ertapenem*:ab,ti OR 'beta‐lactam':ab,ti OR 'beta‐lactams':ab,ti OR betalactam*:ab,ti OR 'beta lactam':ab,ti OR 'beta lactams':ab,ti OR cephalosporin*:ab,ti OR cefuroxime*:ab,ti OR cefotaxime*:ab,ti OR ceftriaxone*:ab,ti OR ceftazidime*:ab,ti OR cefipime*:ab,ti OR piperacillin*:ab,ti OR aminoglycoside*:ab,ti OR gentamicin*:ab,ti OR amikacin*:ab,ti OR tobramycin*:ab,ti OR fluoroquinolone*:ab,ti OR ciprofloxacin*:ab,ti OR levofloxacin*:ab,ti OR moxifloxacin*:ab,ti OR lipoglycopeptide*:ab,ti OR telavancin*:ab,ti OR glycylcycline*:ab,ti OR tigecycline*:ab,ti OR polymyxin*:ab,ti OR colistin*:ab,ti #22 'glycopeptide'/exp OR 'oxazolidinone derivative'/exp OR 'carbapenem derivative'/exp OR 'beta lactam'/exp OR 'cephalosporin derivative'/exp OR 'aminoglycoside antibiotic agent'/exp OR 'quinolone derivative'/exp OR 'polymyxin'/exp OR 'beta lactamase inhibitor'/exp #21 antibiotic*:ab,ti #20 'antibiotic agent'/exp #19 #16 OR #17 OR #18 #18 hap:ab,ti OR vap:ab,ti #17 'ventilator associated pneumonia'/de OR 'hospital acquired pneumonia'/de #16 #5 AND #15 #15 #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 #14 respirator*:ab,ti OR ventilator*:ab,ti #13 'mechanical ventilator'/de #12 'artificial ventilation'/exp #11 ((hospital* OR 'health care' OR healthcare* OR 'health‐care' OR nosocomial* OR ventilator* OR icu OR 'intensive care') NEAR/3 (acquired OR associat*)):ab,ti #10 'intensive care unit'/de #9 (infection* NEAR/3 (hospital* OR nosocomial)):ab,ti #8 'cross infection':ab,ti #7 'cross infection'/de #6 'hospital infection'/de OR 'healthcare associated infection'/de #5 #1 OR #2 OR #3 OR #4 #4 (respiratory NEAR/3 infect*):ab,ti #3 'respiratory tract infection'/de OR 'lower respiratory tract infection'/de OR 'lung infection'/de OR 'chest infection'/de #2 pneumon*:ab,ti OR pleuropneumon*:ab,ti OR bronchopneumon*:ab,ti OR bronchit*:ab,ti OR tracheobronchit*:ab,ti #1 'pneumonia'/exp
Appendix 3. LILACS search strategy
(mh:pneumonia OR mh:c08.381.677* OR mh:c08.730.610* OR neumonía OR pneumonia OR "Inflamación Experimental del Pulmón" OR "Inflamación del Pulmón" OR neumonitis OR "Inflamación Pulmonar" OR pneumonía OR pulmonía OR pneumonite OR "Inflamação Experimental dos Pulmões" OR "Inflamação do Pulmão" OR bronchpneumon* OR pleuropneumon* OR bronchit* OR tracheobronchit* OR mh:"Respiratory Tract Infections" OR "Infecciones del Sistema Respiratorio" OR "Infecções Respiratórias" OR "respiratory infection" OR "respiratory infections" OR "respiratory tract infection" OR "respiratory tract infections" OR "Infecciones de las Vías Respiratorias" OR "Infecciones del Tracto Respiratorio" OR "Infecciones del Aparato Respiratorio" OR "Infecciones de las Vías Respiratorias" OR "Infecciones del Tracto Respiratorio" OR "Infecciones Respiratorias" OR "Infecções das Vias Respiratórias" OR "Infecções do Trato Respiratório" OR "Infecções do Aparelho Respiratório" OR "Infecções das Vias Respiratórias" OR "Infecções das Vias Aéreas" OR "Infecções do Sistema Respiratório" OR "Infecções do Sistema Respiratório" OR "Infecções do Trato Respiratório") AND (mh:"Cross Infection" OR mh:c01.539.248* OR "hospital infections" OR "nosocomial infections" OR "Infección Hospitalaria" OR "Infecção Hospitalar" OR "Infecciones en Hospitales" OR "Infecciones Nosocomiales" OR "Infecções Nosocomiais" OR mh:"Intensive Care Units" OR "Unidades de Cuidados Intensivos" OR "Unidades de Terapia Intensiva" OR mh:n02.278.388.493* OR mh:vs3.002.001.001.005* OR "Centro de Terapia Intensiva" OR "Centros de Terapia Intensiva" OR cti OR "Unidade de Terapia Intensiva" OR uti OR hospital* OR "health care" OR "healthcare" OR "health‐care" OR nosocomial OR icu OR "intensive care" OR mh:"Respiration, Artificial" OR mh:e02.041.625* OR mh:e02.880.820* OR "Respiración Artificial" OR "Respiração Artificial" OR mh:"Ventilators, Mechanical" OR "Ventiladores Mecánicos" OR "Ventiladores Mecânicos" OR mh:e07.950* OR respirator* OR ventilator*) AND (mh:"Anti‐Bacterial Agents" OR antibiotic* OR antibacterianos OR mh:d27.505.954.122.085* OR mh:glycopeptides OR mh:d09.400.420* OR mh:d12.644.233* OR glicopéptidos OR glicopeptídeos OR mh:oxazolidinones OR mh:d03.383.129.462.600* OR oxazolidinonas mh:carbapenems OR carbapenémicos OR carbapenêmicos OR mh:d02.065.589.099.124* OR mh:d04.075.080.875.099.221.124* OR mh:"beta‐Lactams" OR "beta‐Lactamas" OR mh:d02.065.589.099* OR mh:d02.886.108* OR mh:d04.075.080.875.099.221* OR mh:aminoglycosides OR aminoglicósidos OR aminoglicosídeos OR mh:d09.408.051* OR mh:fluoroquinolones OR mh:d03.438.810.835.322* OR fluoroquinolonas OR mh:polymyxins OR mh:d04.345.566.780* OR mh:d10.477.750* OR mh:d12.644.050.600* OR mh:d12.644.641.780* OR mh:d12.776.543.695.054.600* OR polimixinas OR glycopeptide* OR vancomycin* OR teicoplanin* OR oxazolidinone* OR linezolid* OR carbapenem* OR meropenem* OR imipenem* OR doripenem OR ertapenem* OR beta‐lactam* OR betalactam* OR beta lactam* OR cephalosporin* OR cefuroxime* OR cefotaxime* OR ceftriaxone* OR ceftazidime* OR cefipime* OR piperacillin* OR aminoglycoside* OR gentamicin* OR amikacin* OR tobramycin* OR fluoroquinolone* OR ciprofloxacin* OR levofloxacin* OR moxifloxacin* OR lipoglycopeptide* OR telavancin* OR glycylcycline* OR tigecycline* OR polymyxin* OR colistin*)
Appendix 4. Web of Science search strategy
Topic=("hospital‐acquired pneumonia" or "ventilator‐associated pneumonia" or "health‐care associated pneumonia" or "nosocomial pneumonia") AND Topic=(antibiotic* or antibacterial*) Refined by: Topic=(random* or placebo* or rct or "clinical trial" or "clinical trials") Databases=SCI‐EXPANDED, CPCI‐S
Appendix 5. Sensitivity analysis
| 28‐day mortality (Analysis 1.1) | Including Kollef 2012 | Excluding Kollef 2012 |
| NF‐GNB | OR 0.95 (95% CI 0.39 to 2.27) | OR 0.71 (95% CI 0.32 to 1.56) |
| MRSA | OR 1.28 (95% CI 0.32 to 5.09) | OR 1.28 (95% CI 0.32 to 5.09) |
| Non NF‐GNB | OR 1.65 (95% CI 0.73 to 3.73) | OR 1.65 (95% CI 0.73 to 3.73) |
| Unspecified organism | OR 1.22 (95% CI 0.53 to 2.78) | OR 1.22 (95% CI 0.53 to 2.78) |
| Overall | OR 1.18 (95% CI 0.77 to 1.80) | OR 1.08 (95% CI 0.66 to 1.76) |
| Recurrence of pneumonia (Analysis 1.2) | Including Medina 2007 and Capellier 2012 | Excluding Medina 2007 | Excluding Capellier 2012 | Excluding Medina 2007 and Capellier 2012 |
| NF‐GNB | OR 2.18 (95% CI 1.14 to 4.16) | OR 2.01 (95% CI 0.94 to 4.28) | OR 2.18 (95% CI 1.14 to 4.16) | OR 2.01 (95% CI 0.94 to 4.28) |
| MRSA | OR 1.56 (95% CI 0.12 to 19.61) | OR 0.67 (95% CI 0.19 to 2.33) | OR 1.56 (95% CI 0.12 to 19.61) | OR 0.67 (95% CI 0.19 to 2.33) |
| Non NF‐GNB/ MRSA | OR 1.17 (95% CI 0.64 to 2.14) | OR 1.15 (95% CI 0.51 to 2.59) | OR 0.98 (95% CI 0.55 to 1.78) | OR 0.90 (95% CI 0.48 to 1.66) |
| Unspecified organism | OR 1.17 (95% CI 0.14 to 9.59) | OR 1.17 (95% CI 0.14 to 9.59) | OR 1.17 (95% CI 0.14 to 9.59) | OR 1.17 (95% CI 0.14 to 9.59) |
| Overall | OR 1.41 (95% CI 0.94 to 2.12) | OR 1.23 (95% CI 0.79 to 1.92) | OR 1.37 (95% CI 0.87 to 2.17) | OR 1.15 (95% CI 0.79 to 1.88) |
CI: confidence interval MRSA: methicillin‐resistant staphylococcus aureus NF‐GNB: non‐fermenting Gram‐negative bacteria OR: odds ratio
Data and analyses
Comparison 1. Short (fixed)‐course antibiotic therapy versus prolonged‐course antibiotic therapy for HAP.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 28‐day mortality | 3 | 598 | Odds Ratio (M‐H, Random, 95% CI) | 1.18 [0.77, 1.80] |
| 1.1 NF‐GNB | 2 | 179 | Odds Ratio (M‐H, Random, 95% CI) | 0.95 [0.39, 2.27] |
| 1.2 MRSA | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 1.28 [0.32, 5.09] |
| 1.3 Non NF‐GNB/MRSA | 1 | 232 | Odds Ratio (M‐H, Random, 95% CI) | 1.65 [0.73, 3.73] |
| 1.4 Unspecified organism | 2 | 145 | Odds Ratio (M‐H, Random, 95% CI) | 1.22 [0.53, 2.78] |
| 2 Recurrence of pneumonia | 4 | 733 | Odds Ratio (M‐H, Random, 95% CI) | 1.41 [0.94, 2.12] |
| 2.1 NF‐GNB | 2 | 176 | Odds Ratio (M‐H, Random, 95% CI) | 2.18 [1.14, 4.16] |
| 2.2 MRSA | 2 | 49 | Odds Ratio (M‐H, Random, 95% CI) | 1.56 [0.12, 19.61] |
| 2.3 Non NF‐GNB/MRSA | 3 | 478 | Odds Ratio (M‐H, Random, 95% CI) | 1.17 [0.64, 2.14] |
| 2.4 Unspecified organism | 1 | 30 | Odds Ratio (M‐H, Random, 95% CI) | 1.17 [0.14, 9.59] |
| 3 28‐day antibiotic‐free days | 2 | 431 | Mean Difference (IV, Random, 95% CI) | 4.02 [2.26, 5.78] |
| 3.1 NF‐GNB | 1 | 127 | Mean Difference (IV, Random, 95% CI) | 4.5 [2.25, 6.75] |
| 3.2 MRSA | 1 | 42 | Mean Difference (IV, Random, 95% CI) | 8.0 [4.14, 11.86] |
| 3.3 Non NF‐GNB/ MRSA | 1 | 232 | Mean Difference (IV, Random, 95% CI) | 3.70 [2.09, 5.31] |
| 3.4 Unspecified organism | 1 | 30 | Mean Difference (IV, Random, 95% CI) | 2.3 [1.03, 3.57] |
| 4 ITU mortality | 2 | 107 | Odds Ratio (M‐H, Random, 95% CI) | 0.85 [0.37, 1.91] |
| 5 In‐hospital mortality | 1 | 401 | Odds Ratio (M‐H, Random, 95% CI) | 1.09 [0.71, 1.68] |
| 5.1 NF‐GNB | 1 | 127 | Odds Ratio (M‐H, Random, 95% CI) | 0.75 [0.36, 1.53] |
| 5.2 MRSA | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 1.47 [0.43, 4.95] |
| 5.3 Non NF‐GNB/MRSA | 1 | 232 | Odds Ratio (M‐H, Random, 95% CI) | 1.32 [0.72, 2.42] |
| 6 21‐day mortality | 1 | 225 | Odds Ratio (M‐H, Random, 95% CI) | 1.05 [0.41, 2.69] |
| 7 60‐day mortality | 1 | 401 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.55, 1.35] |
| 7.1 NF‐GNB | 1 | 127 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.35, 1.54] |
| 7.2 MRSA | 1 | 42 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.29, 3.47] |
| 7.3 Non NF‐GNB/ MRSA | 1 | 232 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.49, 1.76] |
| 8 90‐day mortality | 1 | 198 | Odds Ratio (M‐H, Random, 95% CI) | 0.99 [0.49, 1.99] |
| 9 Clinical resolution | 3 | 472 | Odds Ratio (M‐H, Random, 95% CI) | 0.75 [0.49, 1.15] |
| 9.1 NF‐GNB | 1 | 55 | Odds Ratio (M‐H, Random, 95% CI) | 0.48 [0.16, 1.48] |
| 9.2 Unspecified organism | 3 | 417 | Odds Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.28] |
| 10 Relapse of pneumonia | 2 | 626 | Odds Ratio (M‐H, Random, 95% CI) | 1.70 [0.97, 2.97] |
| 10.1 NF‐GNB | 1 | 127 | Odds Ratio (M‐H, Random, 95% CI) | 2.08 [0.92, 4.70] |
| 10.2 MRSA | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 0.71 [0.14, 3.64] |
| 10.3 Non NF‐GNB/MRSA | 1 | 232 | Odds Ratio (M‐H, Random, 95% CI) | 1.41 [0.51, 3.92] |
| 10.4 Unspecified organism | 1 | 225 | Odds Ratio (M‐H, Random, 95% CI) | 2.92 [0.58, 14.78] |
| 11 Subsequent infection due to resistant organism | 1 | 110 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.21, 0.95] |
| 12 Duration of ICU stay | 3 | 656 | Mean Difference (IV, Random, 95% CI) | 0.15 [1.00, 1.29] |
| 12.1 NF‐GNB | 1 | 127 | Mean Difference (IV, Random, 95% CI) | 0.90 [‐5.40, 7.20] |
| 12.2 MRSA | 1 | 42 | Mean Difference (IV, Random, 95% CI) | 2.90 [‐8.39, 14.19] |
| 12.3 Non NF‐GNB/MRSA | 2 | 457 | Mean Difference (IV, Random, 95% CI) | 0.45 [‐1.02, 1.92] |
| 12.4 Unspecified organism | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐1.60 [‐4.61, 1.41] |
| 13 Duration of hospital stay | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐1.0 [‐4.11, 2.11] |
| 14 Duration of mechanical ventilation | 3 | 332 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.51, 0.54] |
Comparison 2. Discontinuation of antibiotics according to Clinical Pulmonary Infection Score.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 30‐day mortality | 1 | 81 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.10, 1.03] |
| 2 Episodes of superinfection or antimicrobial resistance | 1 | 81 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.09, 0.92] |
2.1. Analysis.
Comparison 2 Discontinuation of antibiotics according to Clinical Pulmonary Infection Score, Outcome 1 30‐day mortality.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Capellier 2012.
| Methods | Multi‐centre study, based in France. Unblinded, randomised controlled trial comparing fixed durations (8‐day versus 15‐day) of antibiotic therapy for early‐onset VAP conducted between 1998 and 2002 | |
| Participants | 225 adult patients in 13 ICUs (medical, surgical, trauma; 70% male; mean age 49; mean SAPS II score 39; no episodes due to NF‐GNB; no episodes due to MRSA). VAP diagnosis required 2 of the following: temperature of 38.3 °C or higher, white cell count > 10 x 109/L, excessive purulent secretions, and meeting radiological criteria. VAP diagnosis was confirmed with BAL culture of ≥ 104 cfu/ml. Early onset VAP was defined as pneumonia developing more than 24 hours but less than 8 days after onset of mechanical ventilation. Mean interval between hospital admission and intubation was 1.6 days, and between intubation and BAL (i.e. onset of VAP) 3.5 days. Bacterial pathogen identified on blood culture in 8% cases Exclusions: prior receipt of antibiotics for suspected pneumonia, pregnancy, immunocompromise, pulmonary abscess | |
| Interventions | 116 patients were allocated to receive an 8‐day course of beta‐lactam (from choice of 3) plus 5 days of aminoglycoside antibiotic (from choice of 3); 109 patients were allocated to receive a 15‐day course of beta‐lactam plus 5 days of aminoglycoside | |
| Outcomes | The trial was designed to show equivalence in terms of clinical cure rate Primary outcome:
Secondary outcomes (with the exception of 90‐day mortality, all evaluated at day 21):
|
|
| Notes | Appropriateness of initial antibiotic therapy was not reported. Mean duration of first‐line treatment was 7.8 days (SD 1.6) in the short course and 13.1 (SD 3.6) in the prolonged course group The interval between the end of data collection and publication was 10 years |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization is allocated in each centre by a dedicated randomisation table." |
| Allocation concealment (selection bias) | Unclear risk | "The assigned treatment arm is communicated by fax at the latest at D5 by the main investigator centre." Comment: unclear to what extent participants/investigators at main centre could have access to/have foreseen allocation according to randomisation table |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Non‐blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Non‐blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data regarding exclusions not reported. No loss to 21‐day follow‐up. However, loss to 90‐day follow‐up of 14 patients (12%) in short‐course, and of 13 (12%) in prolonged‐course group. Explanation not provided and significance not explored |
| Selective reporting (reporting bias) | Unclear risk | Antibiotic‐free days unreported |
| Other bias | Unclear risk | Follow‐up at 21‐days is relatively early compared with other studies, for assessment of, e.g. duration of ICU stay. Data were collected between 1998 and 2002. Though recently published, results will reflect critical care medicine as practised a decade earlier |
Chastre 2003a.
| Methods | The PNEUMA study, a multi‐centre study based in France. Unblinded, randomised controlled trial comparing fixed durations (8‐day versus 15‐day) of antibiotic therapy for VAP. Randomisation occurred 3 days after BAL results confirmed VAP | |
| Participants | 401 adult patients. 51 French ICUs. 72% male; mean age 61; episodes due to NF‐GNB 32.5%, MRSA 11.2%; mean SAPS II score 45; mean SOFA score 7.4 at admission. VAP was diagnosed according to the following criteria: new and persistent radiographic infiltrate, plus 1 of: purulent tracheal secretions, temperature of 38.4 °C or higher, or leukocyte count > 10,000/µL; and positive quantitative culture of 104 cfu/mL from BAL or 103 cfu/mL from PSB. Duration of mechanical ventilation prior to VAP: 13.6 days. No significant differences between groups at baseline, with the exception of significantly higher proportion of men (76.6%) in 8‐day regimen versus men in 15‐day regimen (67.6%; P value = 0.046). All patients received appropriate initial antibiotics. Exclusions included early onset pneumonia (within 5 days of commencing mechanical ventilation) in patients who had received no antimicrobial therapy in the 15 days prior to diagnosis of pneumonia, and immunocompromised state, characterised by: neutropenia, AIDS, long‐term corticosteroids or other immunosuppressant therapy | |
| Interventions | 197 patients received a fixed 8‐day course of antibiotics (chosen by treating physician); 204 patients received a 15‐day course | |
| Outcomes | The trial was designed to demonstrate the non‐inferiority of short‐course therapy in terms of all‐cause mortality and pulmonary infection recurrence, and superiority in terms of 28‐day antibiotic‐free days. It was powered to detect a 10% difference in death and pulmonary infection recurrence, and a 20% difference in 28‐day antibiotic‐free days The primary outcome measures were:
The following additional measures were reported:
|
|
| Notes | Repeat bronchoscopy was performed on the basis of fever, purulent secretions, new or progressive pulmonary infiltrates, or deterioration in respiratory or haemodynamic parameters. It was not performed routinely, e.g. on completion of 8‐day course of therapy, and consequently data regarding persistent colonisation with NF‐GNB are not available | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomisation was performed...and stratified... according to a computer‐generated random‐number table." |
| Allocation concealment (selection bias) | Low risk | "Randomisation performed centrally, using an interactive voice system... randomisation was not communicated to the investigators until day 8... On that day, investigators had to telephone the randomisation centre to receive the treatment assignment by fax." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "...Patients, medical and nursing staffs, and pharmacists remained blinded until [day 8]." However, importantly, no attempt was made to blind from day 8, i.e. the point from which allocation might make a significant difference |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "...Patients, medical and nursing staffs, and pharmacists remained blinded until [day 8]." Again, no attempt was made to blind from day 8, i.e. the point from which allocation might make a significant difference |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Following randomisation, 0 patients were lost to follow‐up. 1 patient was excluded from analysis following withdrawal of consent |
| Selective reporting (reporting bias) | Unclear risk | Study protocol not available for examination. However, outcome measures are those expected and appropriately presented within the report |
| Other bias | Low risk | There was a significantly higher proportion of men in the 8‐day group (76.6%) compared with the 15‐day group (67.6%; P value = 0.046). However, there were not significant differences in illness severity scores, prior duration of mechanical ventilation, prior antibiotic administration, micro‐organisms responsible for VAP, and antibiotic regimes to treat VAP Data regarding proportions of patients who contrary to protocol did not receive a full 8‐day or 15‐day course of antibiotics are not provided. However, absolute antibiotic‐treatment days and 28‐day antibiotic‐free day data indicate significantly less antibiotic exposure as a consequence of allocation to short or prolonged‐course therapy |
Fekih Hassen 2009.
| Methods | Single‐centre study based in Tunisia. RCT comparing fixed durations (7‐day versus 10‐day) of antibiotic therapy for VAP | |
| Participants | Medical ICU. 30 adult patients (63% male; mean age 63 years; episodes due to NF‐GNB 72%; SAPS II 42.4). VAP (onset more than 48 hours after mechanical ventilation in ICU) diagnosis was suspected on the basis of: new and persistent radiographic infiltrate, purulent secretions, fever or deteriorating gas exchange or white cell count and confirmed on quantitative analysis of culture of endotracheal aspirate (> 104 cfu/ml) or protected distal respiratory specimens (>103 cfu/ml). Mean onset of VAP after institution of mechanical ventilation: 10 days. Initial antibiotics were appropriate in 94% of cases. No significant differences in baseline characteristics between the 2 groups Exclusions include: second episode of pneumonia during single hospitalisation, terminal illness, failure to isolate bacterial growth 30 patients randomised from 39 patients with clinical features of VAP: 9 not enrolled because of terminal illness or failure to isolate bacteria |
|
| Interventions | 14 patients randomised to receive 7‐day course of antibiotics; 16 patients to receive 16‐day course. Choice of antibiotic: on microbiology advice, taking into account whether early (up to including 5 days after commencing mechanical ventilation) or late‐onset VAP, and whether risk factors for multi‐resistant bacteria present, and modified according to culture/sensitivity results 94% patients received appropriate initial antibiotic therapy |
|
| Outcomes | Primary outcome measures were:
Power calculation is not reported The following additional outcome measures were presented:
|
|
| Notes | Data regarding protocol violations and patients lost to follow‐up not available. Unable to make contact with trial authors to request supplementary information | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Use of random number table |
| Allocation concealment (selection bias) | Unclear risk | Inadequately reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Inadequately reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Inadequately reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Inadequately reported |
| Selective reporting (reporting bias) | Unclear risk | Inadequately reported |
| Other bias | Low risk | No evidence of other source of bias |
Kollef 2012.
| Methods | International multi‐centre study (56 sites in 19 countries, stratified according to region as Central and Southern America, Eastern Europe and Asia, and Western Europe, North America and Australia) conducted between April 2008 and June 2011. Double‐blinded randomised controlled trial comparing a fixed 7‐day course of doripenem, with a fixed 10‐day course of imipenem‐cilastatin | |
| Participants | 274 patients (APACHE II score > 8 and < 35, baseline CPIS > 6, prior hospitalisation or management in chronic care facility for total 5 days or more within previous 90 days) with pneumonia acquired at least 48 hours after onset of mechanical ventilation. Of these, 227 (65% male, mean age 78 years, 57% APACHE II > 15, mean SOFA score 5.8) were included in the ITT analysis. Baseline characteristics of intervention groups overall appear balanced, but statistical significance of any differences not explored. VAP diagnosed on the basis of new or worsening radiographic infiltrates and at least one of: temperature > 39 °C or < 35 °C, or an increase of temperature of > 1 °C, or white blood cell count > 10 x 109/L. Among the microbiological intention‐to‐treat group (MITT; at least 1 gram‐negative pathogen identified on BAL or mini‐BAL at density of ≥ 104 cfu/mL with an imipenem MIC < 8 μg/mL), a gram‐negative pathogen was identified in 89% cases. Within this MITT group a higher proportion of the patients receiving doripenem had either Pseudomonas aeruginosa (22% versus 11%) or Acinetobacter spp. (19% versus 11%) identified. No data presented for duration of mechanical ventilation prior to onset of VAP Exclusions: pregnancy, administration of antibiotics for > 24 hours before enrolment, baseline presence of only MRSA or Stenotrophomonas maltophilia, ARDS or other condition which would hinder interpretation of VAP (including pulmonary contusion, pleural effusion, lung cancer, decompensated COPD, congestive cardiac failure, aspiration pneumonitis) and beta‐lactam sensitivity | |
| Interventions | Among the ITT group, 115 patients received a 7‐day course of doripenem 1 g administered as 4‐hour infusion every 8 hours, and 112 patients a 10‐day course of imipenem‐cilastatin 1 g as a 1‐hour infusion every 8 hours. Among the subgroup meeting the MITT criteria as above, 79 received doripenem and 88 imipenem‐cilastatin | |
| Outcomes | The study was designed to demonstrate non‐inferiority for the primary outcome measure, clinical cure (according to radiological and clinical features) at end of treatment (day 10) The following additional outcomes were reported for the MITT group:
|
|
| Notes | Study was closed prematurely because of inferior efficacy and higher mortality in 1 treatment arm Median duration of study drug therapy 9.7 days in each group, and for active drug 7.0 days in doripenem group and 10.0 days in imipenem group 5 sites (3 in Guatemala, 1 in Germany, 1 in United States) deemed to be non‐compliant with good clinical practices, and for this reason data regarding 41 patients were excluded from analysis. Note additional data published elsewhere regarding ITT patients not included in MITT analysis (Dimopoulos 2013). However, given the intention described in the original report to restrict data analysis to MITT patients, only data from these patients are included in this review The US Food and Drug Administration agency issued a warning regarding use of doripenem for ventilator‐associated pneumonia in 2014 (FDA 2014) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Treatment was randomised with use of a central interactive phone system." Comment: this implies that the randomisation process is computer‐generated, but is unclear from the text |
| Allocation concealment (selection bias) | Low risk | "Treatment was randomised with use of a central interactive phone system." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blinded. All patients received a 7‐day infusion (whether placebo or active drug) and 10‐day infusion (whether active drug or placebo) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Double‐blinded", implying outcome assessment probably blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are complete for the MITT subgroup of interest |
| Selective reporting (reporting bias) | Unclear risk | Duration of mechanical ventilation before episode of VAP not presented, which is unexpected given the intention to compare interventions in patients with late‐onset VAP In terms of outcome data, duration of mechanical ventilation and of ICU and hospital length of stay are unreported, but possibly such outcome data would have been difficult to interpret given variation in processes at such a large number of centres |
| Other bias | High risk | Unfortunately, there are multiple interventions. This study is comparing not just a short course of therapy with a prolonged course, but a short course of one antibiotic administered over a long infusion time (which may be more effective against resistant bacteria), with a long course of another antibiotic administered over a short infusion time There is a higher proportion of Pseudomonas aeruginosa and Acinetobacter spp. in the doripenem group The timing of EOT assessment (at day 10) may have favoured patients in the 10‐day therapy group rather than the 7‐day therapy group, not having allowed for relapse to have occurred in the prolonged‐therapy group |
Medina 2007.
| Methods | 2‐centre study, based in Uruguay, conducted May 2003 to December 2006. Randomised controlled study comparing fixed short (8‐day) and long (12‐day) courses of antibiotic therapy for VAP | |
| Participants | 77 patients (medical, surgical and neurosurgical; mean age 59 years, 53% male, 63.6% episodes due to NF‐GNB, 9.1% episodes due to MRSA; median APACHE II score 21, MODS score 5, SOFA score 6) with VAP. VAP was diagnosed on the basis of: new and persistent radiographic infiltrates, 2 of temperature ≥ 38.5 ºC or < 36 ºC, leukocytes ≥ 12,000/ mm3 or ≤ 4 x 103/mm3, and BAL culture ≥ 104 cfu/ml, or positive ETA plus CPIS > 6, or micro‐organism in ≥ 2 blood cultures with identical sensitivity to tracheal secretions and in the absence of other possible infection, or positive culture of pleural fluid. Mean time after commencing mechanical ventilation before onset of VAP: 9.3 days. 68% patients had received a prior course of antibiotics. In 97% cases, initial antibiotic therapy for VAP was appropriate. There were no significant differences in baseline characteristics between treatment groups Exclusion criteria: failure to meet clinical and microbiological criteria, decision not to institute antibiotic therapy, duration of therapy < 6 days, death before 6th day of treatment, onset of VAP within 48 hours of admission from other centre | |
| Interventions | 77 patients randomised to 8‐day treatment or 12‐day course on day 8 of antibiotic therapy. Antibiotic choice was that of the attending physician; in 75/77 (97%) cases, initial antibiotic therapy was appropriate. The most commonly used antibiotics were: cefoperazone‐sulbactam, carbapenem and other third‐generation cephalosporins. In 51% cases, antibiotic combinations were used | |
| Outcomes | The study was designed to demonstrate the non‐inferiority of short‐course therapy in terms of clinical resolution and non‐resolution ("therapeutic failure") of VAP The following other outcomes were also reported:
|
|
| Notes | No patients were lost to follow‐up. No patient received a shorter duration of antibiotic therapy than allocated; data are incomplete for patients who had antibiotics continued beyond the allocated duration At the time our searches were performed, this study had not been published in a peer‐reviewed journal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation using random number table |
| Allocation concealment (selection bias) | Low risk | Sealed, numbered envelopes opened sequentially |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Non‐blinded study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Non‐blinded study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No patients lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Unclear. Data incomplete for patients who had antibiotics continued beyond the allocated duration |
| Other bias | Low risk | Study appears to be free of other sources of bias |
Singh 2000.
| Methods | Single‐centre study from the USA. Randomised controlled trial comparing strategy of 3 days' ciprofloxacin monotherapy versus standard therapy (duration and antibiotic choice at the discretion of physician) for patients with pulmonary infiltrates but low‐probability pneumonia. | |
| Participants | Study entry criteria: new‐onset pulmonary infiltrate associated with possible nosocomial pneumonia. Modified Clinical Pulmonary Infection Score (CPIS) < 7 on day 1 (suggesting low probability pneumonia) 81 adult medical and surgical ICU patients; 47 (58%) receiving mechanical ventilation; mean age 66.7 years; no data on sex. APACHE III score 41.8; mean CPIS 4.9. Prior mean duration of ICU stay 8.8 days and duration of mechanical ventilation 7.6 days. Chronic obstructive airways disease present in 27% cases. 5% patients were transplant recipients. With the exception of abnormal respiration (92% experimental group versus 71% standard‐therapy group, P value = 0.016), there were no significant differences in baseline characteristics between the 2 groups, though mean duration of mechanical ventilation prior to enrolment was 10 days in the short‐course group and 5 days in the standard‐therapy group. Exclusions: HIV, chemotherapy‐induced neutropenia, concurrent antibiotic administration (other than surgical prophylaxis), flouroquinolone allergy |
|
| Interventions | Randomised at day 1 of episode of possible pneumonia. Intervention group (N = 39): 3 days' ciprofloxacin monotherapy. At day 3 if CPIS < 7, antibiotics would be discontinued; if CPIS > 6, therapy would be continued, with choice of agent and duration of therapy at the discretion of treating physician, and incorporating microbiology results Standard therapy (N = 42): choice and duration of antibiotic therapy at choice of treating physician |
|
| Outcomes | The following outcomes were reported:
Power calculation was conducted according to "worse outcome" and development of antimicrobial resistance |
|
| Notes | Pathogens associated with possible HAP were incompletely presented Outcome data for patients who were and were not mechanically ventilated are not reported separately For patients allocated to the short‐course therapy, 0 patients with CPIS < 7 at day 3 had antibiotics continued beyond 72 hours A significant decrease in duration of therapy in the "standard therapy" group was observed with time (P value = 0.0001), thought to be a result of the unblinded nature of the study. The study was terminated by institutional review board as it was deemed "unethical to continue study" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation process not described |
| Allocation concealment (selection bias) | Unclear risk | Randomisation/concealment not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Non‐blinded study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Non‐blinded study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | High risk | Microbiological data are partially reported. The components of the composite measure of "emergence of antimicrobial resistance or superinfection" are not reported |
| Other bias | High risk | Stopped early by institutional review board. Results for patients managed in "experimental" group appear to have influenced management of patients subsequently allocated to "standard therapy group" |
APACHE II score: Acute Physiology and Chronic Health Evaluation II score ARDS: acute respiratory distress syndrome BAL: broncho‐alveolar lavage cfu/ml: colony‐forming units per millilitre COPD: chronic obstructive pulmonary disease CPIS: clinical pulmonary infection score DNR order: do not resuscitate order EOT: end‐of‐treatment ETA: endo‐tracheal aspirate FiO2: fraction of inspired oxygen (in a gas mixture) HAP: hospital‐acquired pneumonia ICU: intensive care unit ITT: intention‐to‐treat ITU: intensive therapy unit MITT: microbiological intention‐to‐treat MODS: multiple organ dysfunction score MRSA: methicillin‐resistant Staphylococcus aureus NF‐GNB: non‐fermenting Gram‐negative bacilli ODIN: organ dysfunction and/or infection score PaO2: partial pressure of oxygen PSB: protected specimen brush RCT: randomised controlled trial SAPS II: Simplified Acute Physiology Score II SD: standard deviation SOFA score: Sequential Organ Failure Assessment score VAP: ventilator‐associated pneumonia
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bouadma 2010 | The PRORATA randomised controlled study investigating the utility of a procalcitonin‐guided (PCT‐guided) algorithm for antibiotic administration for intensive care patients (34% with hospital‐acquired pneumonia, of whom approximately 2/3 were mechanically ventilated). Mean duration of antibiotic therapy was significantly lower in the PCT group among patients with VAP. However, the study was excluded because interventions did not include a fixed duration of therapy |
| Cai 2001 | A randomised controlled study investigating diagnostic strategies (quantitative versus qualitative culture of respiratory tract specimens) on outcome from VAP |
| CCCTG 2006 | This 2‐by‐2 factorial randomised controlled study aiming to compare: i. invasive and non‐invasive diagnostic strategies for diagnosis of VAP, and ii. initial empiric treatment with meropenem or meropenem plus ciprofloxacin for suspected VAP. There was no significant difference in number of antibiotic‐free days between groups of patients allocated to invasive or non‐invasive strategies |
| Chastre 2003b | Data subsequently published in full (Chastre 2003a) |
| Fagon 2000 | This was a randomised study designed to compare strategies for diagnosis and selection of initial antimicrobial therapy of VAP, not duration of therapy. For groups of patients randomised to both invasive and non‐invasive diagnostic strategies, recommended duration of therapy in the presence of positive respiratory culture (i.e. confirmed pneumonia) was 14 days |
| Hochreiter 2009 | This was a randomised controlled study comparing a strategy using serial PCT measurement to guide discontinuation of antibiotic therapy for treatment of sepsis in 110 surgical intensive care patients with standard therapy. Of these patients, 43 had "pneumonia"; it is unclear what proportion had nosocomial or community‐acquired pneumonia, and what proportion of patients was receiving mechanical ventilation at time of diagnosis. Duration of antibiotic therapy was significantly shorter in the intervention (PCT‐guided) group; however, the study was excluded because interventions did not include a fixed duration of therapy |
| Ibrahim 2001 | Non‐randomised before‐and‐after study investigating a clinical guideline regarding initial treatment and subsequent discontinuation of antibiotic therapy |
| Kim 2009 | Data subsequently published in full (Kim 2012) |
| Kim 2012 | This was a single‐centre RCT investigating effectiveness of an antibiotic de‐escalation protocol for intensive care patients with HAP. 109 medical ICU patients aged 18 years and over with HAP (defined according to ACCP clinical and radiographic criteria) were randomised to the de‐escalation (DE) protocol (N = 54) or non de‐escalation (NDE) protocol (N = 55). There was no significant difference in duration of antibiotic therapy between intervention groups, and the study was excluded on the basis that fixed courses of therapy were not used |
| Kollef 2005 | Prospective observational study investigating application of previously described clinical guideline (Ibrahim 2001) for patients with suspected VAP, but negative quantitative BAL results |
| Labelle 2012 | This randomised controlled study attempted to evaluate the feasibility (and outcomes) with a treatment goal of 5 or 7 days for pneumonia in intensive care. It was excluded on consideration of a conference proceedings abstract because fixed courses of therapy appear not to have been utilised and duration of therapy was not significantly different between groups |
| Maldonado‐Ortiz 2004 | This multi‐centre randomised controlled study enrolled 65 patients in a study intended to evaluate a strategy of early discontinuation of empirical antibiotic therapy: it has been published in abstract form only. 31 patients were allocated to early (< 8 days) discontinuation of empirical therapy versus 34 patients to late discontinuation (> 9 days). Patient characteristics and diagnostic criteria were not described. Outcome data presented in the abstract were inadequate for the study's inclusion in this review, and contact with a trial author did not yield any further information. Furthermore, a highly significant risk of bias was identified: antibiotic discontinuation at day 8 was higher (70.6%) among patients allocated to late discontinuation than among patients allocated to early discontinuation (67.7%) |
| Micek 2004 | This RCT sought to evaluate the effectiveness of an antibiotic discontinuation policy for suspected VAP. Mean duration of antibiotic therapy was lower in the intervention group (6 days) compared with the standard therapy group (8 days). However, the study was excluded because interventions did not include a fixed duration of therapy |
| Nobre 2008 | This was a randomised controlled study comparing a strategy using serial measurements of procalcitonin (PCT) to guide cessation of antibiotic therapy with standard therapy in critically ill patients with sepsis or septic shock. 79 patients were randomised, of whom a total of 47 patients had sepsis of pulmonary origin. A high proportion of patients (68%) had community‐acquired sepsis. A significant proportion of patients in the PCT group (19%) had the protocol overridden to receive a longer course of antibiotics than advised by the algorithm. On intention‐to‐treat analysis, the difference in antibiotic days between control and intervention groups for all patients was not significant. The study was excluded because interventions did not include a fixed duration of therapy |
| Peery 2001 | This was a randomised study comparing diagnostic strategies for suspected VAP. It was not designed to investigate duration of therapy; there were no protocols to guide duration of antibiotic therapy |
| Pontet 2007 | This RCT compared use of a PCT‐guided algorithm with standard therapy in antibiotic treatment of VAP; the study was excluded because interventions did not include a fixed duration of therapy |
| Rello 2004 | This was an observational rather than a randomised controlled study. It investigated outcomes following introduction of a "De‐escalation" strategy which incorporated the initial administration of broad spectrum antibiotics and subsequent simplification of antibiotic treatment with culture results: 1. changing to monotherapy in absence ofPseudomonas sp; 2. shortening therapy to < 5 days if culture negative and > 48 hours of defervescence; 3. changing from a broad to narrow spectrum agent on basis of culture results |
| Sanchez‐Nieto 1998 | A randomised clinical trial comparing the effects of an invasive quantitative diagnostic strategy versus a non‐invasive strategy on management of and outcome from suspected VAP |
| Schroeder 2007 | This was a RCT comparing a procalcitonin‐guided antibiotic discontinuation strategy with standard treatment for surgical intensive care patients with severe sepsis. The study was excluded because interventions did not include a fixed duration of therapy |
| Singh 1998 | Data subsequently published in full (Singh 2000) |
| Sole 2000 | A RCT to evaluate invasive versus non‐invasive diagnostic methods on outcome from VAP |
| Stolz 2009a | The ProVAP study was a randomised controlled trial comparing a PCT‐guided algorithm with standard therapy for ICU patients with VAP. Duration of antibiotic therapy was lower in the PCT‐guided group (median 15 days versus 10 days in standard therapy group). The study was excluded because interventions did not include a fixed duration of therapy |
| Stolz 2009b | Data subsequently published in full (Stolz 2009a) |
| Svoboda 2007 | RCT evaluating PCT‐guided strategies in the management of septic illness after multiple trauma or major surgery. The study was excluded because interventions did not include a fixed duration of therapy |
| Wolff 2003 | Data subsequently published in full (Chastre 2003a) |
BAL: broncho‐alveolar lavage CPIS: clinical pulmonary infection score HAP: hospital‐acquired pneumonia ICU: intensive care unit ITU: intensive therapy unit PCT: procalcitonin RCT: randomised controlled trial VAP: ventilator‐associated pneumonia
Characteristics of ongoing studies [ordered by study ID]
NCT00410527.
| Trial name or title | 'Effectiveness of short‐course versus standard antibiotic therapy in ICU patients' |
| Methods | Randomised controlled trial |
| Participants | ICU patients (not necessarily mechanically ventilated) aged 18 years and older with pulmonary infiltrates on chest radiography, but low probability of pneumonia according to CPIS of 6 or less |
| Interventions | 3‐day course of meropenem versus standard course (8 days or more) of antibiotic therapy |
| Outcomes | Identification of resistant organisms in respiratory specimen; duration of antibiotic therapy; duration of ICU and hospital length of stay |
| Starting date | August 2006 |
| Contact information | Not available |
| Notes | https://clinicaltrials.gov/ct2/show/study/NCT00410527 |
NCT01554657.
| Trial name or title | 'Five versus seven day antibiotic course for the treatment of pneumonia in the Intensive Care Unit' |
| Methods | Randomised controlled trial |
| Participants | Medical and surgical patients aged 18 years and over with pneumonia |
| Interventions | 5 days of antibiotic therapy versus 7 days of antibiotic therapy |
| Outcomes | Length of antibiotic therapy, 28‐day mortality, 28‐day hospital length of stay, 28‐day development of C. difficile‐related diarrhoea, identification of MDR bacteria from lower respiratory tract specimen |
| Starting date | January 2011 |
| Contact information | Not available |
| Notes | https://clinicaltrials.gov/ct2/show/study/NCT01554657 |
NCT01994980.
| Trial name or title | 'Duration of antibiotic treatment for early VAP (Date) trial' |
| Methods | Randomised controlled trial |
| Participants | Surgical patients aged 18 years and older with VAP, defined according to CPIS and BAL threshold culture |
| Interventions | 4 days of antibiotic therapy versus 8 days of antibiotic therapy |
| Outcomes | Clinical outcomes (CPIS); microbiological outcome (BAL culture); biomarker response (procalcitonin) |
| Starting date | December 2013 |
| Contact information | Maria Rodil, Denver Medical Health Centre, Denver, Colorado, United States 80204 maria.rodil@dhha.org |
| Notes | https://clinicaltrials.gov/ct2/show/NCT01994980 |
BAL: broncho‐alveolar lavage CPIS: Clinical Pulmonary Infection Score CRP: C‐reactive protein ICU: intensive care unit MDR: multi‐drug resistant pathogen PCT: procalcitonin SIRS: systemic inflammatory response syndrome VAP: ventilator‐associated pneumonia
Differences between protocol and review
Our original intention was to exclude trials enrolling patients with haematological malignancy, chemically induced immune‐suppression or HIV/AIDS; we subsequently revised this to: "We intended to exclude data from patients with haematological malignancy, chemically induced immune‐suppression or HIV/AIDS where possible."
Anticipating potential variation in outcome reporting, other modifications to outcome measures included: separation of non‐resolution and recurrence outcomes and the addition of ICU mortality and duration of mechanical ventilation.
Since publication of the previous version of the review in 2011, use of procalcitonin to guide duration of antibiotic therapy in acute respiratory tract infection has been the subject of a dedicated Cochrane review (Schuetz 2012b), and we subsequently took the decision to focus this review on interventions involving a fixed duration of therapy.
Given the greater reporting of measures of 'Clinical resolution' rather than the reciprocal 'Non‐resolution', we selected clinical resolution as a preferable outcome measure in this version of the review.
Contributions of authors
Ged Dempsey (GD) conceived the idea for the systematic review. Richard Pugh (RP), Chris Grant (CG), Richard Cooke (RC) and GD contributed to the drafting of the protocol and final review. RP and CG were responsible for study selection, quality assessment and data extraction. GD assisted in resolution of any disagreement over study selection and quality assessment. RC and GD provided content expertise.
Sources of support
Internal sources
No sources of support supplied
External sources
-
Cochrane Acute Respiratory Infections Group, Australia.
Development and conduct of literature search, and editorial support.
Declarations of interest
There were no sources of funding for this review.
Richard Pugh: none known. Chris Grant: none known. Richard PD Cooke: none known. Ged Dempsey: none known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Capellier 2012 {published data only}
- Capellier G, Mockly H, Charpentier C, Annane D, Blasco G, Desmettre T, et al. Early‐onset ventilator‐associated pneumonia in adults randomized clinical trial: comparison of 8 versus 15 days of antibiotic treatment. PloS One 2012;7(8):e41290. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chastre 2003a {published data only}
- Chastre J, Wolff M, Fagon JY, Chevret S, Thomas F, Wermert D, et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator‐associated pneumonia in adults: a randomized trial. JAMA 2003;290(19):2588‐98. [DOI] [PubMed] [Google Scholar]
Fekih Hassen 2009 {published data only}
- Fekih Hassen M, Ayed S, Ben Sik Ali H, Gharbi R, Marghli S, Elatrous S. Duration of antibiotic therapy for ventilator‐associated pneumonia: comparison of 7 and 10 days. A pilot study. Annales Françaises d'Anesthésie et de Réanimation 2009;28(1):16‐23. [DOI] [PubMed] [Google Scholar]
Kollef 2012 {published data only}
- Kollef M, Chastre J, Restrepo M, Michiels B, Kaniga K, Cirillo I, et al. A randomized trial of 7‐day doripenem versus 10‐day imipenem‐cilastatin for ventilator‐associated pneumonia. Critical Care 2012;16:R218. [DOI] [PMC free article] [PubMed] [Google Scholar]
Medina 2007 {published and unpublished data}
- Medina JC, Perez Protto SE, Paciel D, Pontet J, Saldun P, Berro M. Antibiotic treatment for the ventilator‐associated pneumonia: 8 vs. 12 days randomized trial preliminary data. Annual Interscience Conference on Antimicrobial Agents and Chemotherapy, Chicago, IL. 2007.
Singh 2000 {published data only}
- Singh N, Rogers P, Atwood CW, Wagener MM, Yu VL. Short‐course empiric antibiotic therapy for patients with pulmonary infiltrates in the intensive care unit. A proposed solution for indiscriminate antibiotic prescription. American Journal of Respiratory and Critical Care Medicine 2000;162:505‐11. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bouadma 2010 {published data only}
- Bouadma L, Luyt CE, Tubach F, Cracco C, Alvarez A, Schwebel C, et al. Use of procalcitonin to reduce patients' exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet 2010;375(9713):463‐74. [DOI] [PubMed] [Google Scholar]
Cai 2001 {published data only}
- Cai S, Zhang J, Qian G. Impact of quantitative and qualitative pathogen culture on the outcome of ventilator‐associated pneumonia. Zhonghua Jie He He Hu Xi Za Zhi 2001;24(8):494‐7. [PubMed] [Google Scholar]
CCCTG 2006 {published data only}
- Canadian Critical Care Trials Group. A randomized trial of diagnostic techniques for ventilator‐associated pneumonia. New England Journal of Medicine 2006;355(25):2619‐30. [DOI] [PubMed] [Google Scholar]
Chastre 2003b {published data only}
- Chastre J, Wolff M, Fagon JY, Chevret S. Comparison of two durations of antibiotic therapy to treat ventilator‐associated pneumonia (VAP). American Thoracic Society Meeting, Seattle, Washington. 2003:A015.
Fagon 2000 {published data only}
- Fagon JY, Chastre J, Wolff M, Gervais C, Parer‐Aubas S, Stéphan F, et al. Invasive and noninvasive strategies for management of suspected ventilator‐associated pneumonia. A randomized trial. Annals of Internal Medicine 2000;132(8):621‐30. [DOI] [PubMed] [Google Scholar]
Hochreiter 2009 {published data only (unpublished sought but not used)}
- Hochreiter M, Köhler T, Schweiger AM, Keck FS, Bein B, von Spiegel T, et al. Procalcitonin to guide duration of antibiotic therapy in intensive care patients: a randomized prospective controlled trial. Critical Care 2009;13(3):R83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ibrahim 2001 {published data only}
- Ibrahim EH, Ward S, Sherman G, Schaiff R, Fraser VJ, Kollef MH. Experience with a clinical guideline for the treatment of ventilator‐associated pneumonia. Critical Care Medicine 2001;29(6):1109‐15. [DOI] [PubMed] [Google Scholar]
Kim 2009 {published data only}
- Kim JW, Chung J, Jang HJ, Hong SB, Lim CM, Koh Y. De‐escalation of antibiotics in critically ill patients with hospital‐acquired pneumonia. Respirology. 2009; Vol. 14:A129.
Kim 2012 {published data only}
- Kim JW, Chung J, Choi SH, Jang HJ, Hong SB, Lim CM, et al. Early use of imipenem/cilastatin and vancomycin followed by de‐escalation versus conventional antimicrobials without de‐escalation for patients with hospital‐acquired pneumonia in a medical ICU: a randomized clinical trial. Critical Care 2012;16(1):R28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kollef 2005 {published data only}
- Kollef MH, Kollef KE. Antibiotic utilization and outcomes for patients with clinically suspected ventilator‐associated pneumonia and negative quantitative BAL culture results. Chest 2005;128:2706‐13. [DOI] [PubMed] [Google Scholar]
Labelle 2012 {unpublished data only}
- Labelle AJ, Schoenberg N, Skrupky L, Kollef M. Five versus seven day antibiotic course for the treatment of pneumonia in the intensive care unit. American Journal of Respiratory and Critical Care Medicine. 2012; Vol. 185:A6078.
Maldonado‐Ortiz 2004 {unpublished data only}
- Maldonado‐Ortiz EA, Niederman MS, Nacul F, Rodríguez A, Ceballos S, Osorio J. How long is enough to treat ventilator associated pneumonia? A randomized pilot study: the Latinoamerican experience. Chest 2004;126(Suppl 4):717. [Google Scholar]
Micek 2004 {published data only}
- Micek ST, Ward S, Fraser VJ, Kollef MH. A randomized controlled trial of an antibiotic discontinuation policy for clinically suspected ventilator‐associated pneumonia. Chest 2004;125(5):1791‐9. [DOI] [PubMed] [Google Scholar]
Nobre 2008 {published data only}
- Nobre V, Harbarth S, Graf JD, Rohner P, Pugin J. Use of procalcitonin to shorten antibiotic treatment duration in septic patients: a randomized trial. American Journal of Respiratory and Critical Care Medicine 2008;177(5):498‐505. [DOI] [PubMed] [Google Scholar]
Peery 2001 {published data only}
- Peery C, Chendrasekhar A, Moorman DW, Timberlake GA. Ventilator‐associated pneumonia therapy: protected specimen brushing versus tracheal aspirate data. Journal of Applied Research 2001;1(2):1. [Google Scholar]
Pontet 2007 {published and unpublished data}
- Pontet J, Paciel D, Olivera W, Bentancourt S, Cancela M, Gervas J. Procalcitonin (PCT) guided antibiotic treatment in ventilator associated pneumonia (VAP). Multi‐centre, clinical prospective, randomized‐controlled study. American Thoracic Society International Conference, San Francisco, California, USA. 2007:A76.
Rello 2004 {published data only}
- Rello J, Vidaur L, Sandiumenge A, Rodríguez A, Gualis B, Boque C, et al. De‐escalation therapy in ventilator‐associated pneumonia. Critical Care Medicine 2004;32(11):2183‐90. [DOI] [PubMed] [Google Scholar]
Sanchez‐Nieto 1998 {published data only}
- Sanchez‐Nieto JM, Torres A, Garcia‐Cordoba F, El‐Ebiary M, Carrillo A, Ruiz J, et al. Impact of invasive and noninvasive quantitative culture sampling on outcome of ventilator‐associated pneumonia: a pilot study. American Journal of Respiratory and Critical Care Medicine 1998;157(2):371‐6. [DOI] [PubMed] [Google Scholar]
Schroeder 2007 {published data only (unpublished sought but not used)}
- Schroeder S, Hochreiter M, Koehler T, Schweiger AM, Bein B, Keck FS, et al. Procalcitonin (PCT)‐guided algorithm reduces length of antibiotic treatment in surgical intensive care patients with severe sepsis: results of a prospective randomized study. Langenbeck's Archives of Surgery 2009;394:221‐6. [DOI] [PubMed] [Google Scholar]
Singh 1998 {published data only}
- Singh N. Short‐course empiric antibiotic therapy for suspected nosocomial pneumonia: a proposed solution for indiscriminate antibiotic prescription for pulmonary infiltrates in the ICU. Annual Meeting of the Infectious Disease Society of America, Denver, Colorado. 1998.
Sole 2000 {published data only}
- Sole VJ, Fernandez JA, Benitez AB, Cardenosa Cendrero JA, Rodriguez de CF. Impact of quantitative invasive diagnostic techniques in the management and outcome of mechanically ventilated patients with suspected pneumonia. Critical Care Medicine 2000;28(8):2737‐41. [DOI] [PubMed] [Google Scholar]
Stolz 2009a {published and unpublished data}
- Stolz D, Smyrnios N, Eggimann P, Pargger H, Thakkar N, Siegemund M, et al. Procalcitonin for reduced antibiotic exposure in ventilator‐associated pneumonia: a randomised study. European Respiratory Journal 2009;34(6):1364‐75. [DOI] [PubMed] [Google Scholar]
Stolz 2009b {published data only}
Svoboda 2007 {published data only}
- Svoboda P, Kantorová I, Scheer P, Radvanova J, Radvan M. Can procalcitonin help us in timing of re‐intervention in septic patients after multiple trauma or major surgery?. Hepatogastroenterology 2007;54:359‐63. [PubMed] [Google Scholar]
Wolff 2003 {published data only}
- Wolff M, Chastre J, Fagon JY, Chevret S. Comparison of two durations of antibiotic therapy for ventilator‐associated pneumonia (VAP) caused by non‐fermenting gram negative bacilli (NF‐GNB). American Thoracic Society Meeting Seattle, Washington. 2003:A860.
References to ongoing studies
NCT00410527 {published data only}
- Effectiveness of short‐course versus standard antibiotic therapy in ICU patients. http://clinicaltrials.gov/ct2/show/study/NCT00410527 2006 (accessed 5 June, 2015).
NCT01554657 {published data only}
- Five versus seven day antibiotic course for the treatment of pneumonia in the intensive care unit. https://clinicaltrials.gov/show/NCT01554657 2012 (accessed 5 June, 2015).
NCT01994980 {published data only}
- Duration of antibiotic treatment for early VAP. http://clinicaltrials.gov/show/NCT01994980 2013 (accessed 5 June, 2015).
Additional references
Agrafiotis 2010
- Agrafiotis M, Siempos II, Falagas ME. Frequency, prevention, outcome and treatment of ventilator‐associated tracheobronchitis: systematic review and meta‐analysis. Respiratory Medicine 2010;104:325‐36. [DOI] [PubMed] [Google Scholar]
ATS/IDSA 2005
- American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital‐acquired, ventilator‐associated, and healthcare‐associated pneumonia. American Journal of Respiratory and Critical Care Medicine 2005;171(4):388‐416. [DOI] [PubMed] [Google Scholar]
Bekaert 2011
- Bekaert M, Timsit JF, Vansteelandt S, Depuydt P, Vésin A, Garrouste‐Orgeas M, et al. Attributable mortality of ventilator‐associated pneumonia: a reappraisal using causal analysis. American Journal of Respiratory and Critical Care Medicine 2011;184(10):133‐9. [DOI] [PubMed] [Google Scholar]
Bignardi 1998
- Bignardi GE. Risk factors for Clostridium difficile infection. Journal of Hospital Infection 1998;40(1):1‐15. [DOI] [PubMed] [Google Scholar]
Blot 2013
- Blot S, Koulenti D, Dimopoulos G, Martin C, Komnos A, Krueger WA, et al. Prevalence, risk factors, and mortality for ventilator‐associated pneumonia in middle‐aged, old, and very old critically ill patients. Critical Care Medicine 2014;42:601‐9. [DOI] [PubMed] [Google Scholar]
Boyer 2015
- Boyer AF, Schoenberg N, Babcock H, McMullen KM, Micek ST, Kollef MH. A prospective evaluation of ventilator‐associated conditions and infection‐related ventilator‐associated conditions. Chest 2015;147:68‐81. [DOI] [PubMed] [Google Scholar]
BSAC 2008
- Masterton RG, Galloway A, French G, Street M, Armstrong J, Brown E, et al. Guidelines for the management of hospital‐acquired pneumonia in the UK: report of the working party on hospital‐acquired pneumonia of the British Society for Antimicrobial Chemotherapy. Journal of Antimicrobial Chemotherapy 2008;62(1):5‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burgmann 2010
- Burgmann H, Hiesmayer J, Savey A, Bauer P, Metnitz B, Metnitz P. Impact of nosocomial infections on clinical outcome and resource consumption in critically ill patients. Intensive Care Medicine 2010;36:1597‐601. [DOI] [PubMed] [Google Scholar]
Chant 2012
- Chant C, Leung A, Friedrich JO. Optimal dosing of antibiotics in critically ill patients by using continuous/extended infusions: a systematic review and meta‐analysis. Critical Care 2012;17:R279. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chastre 2002
- Chastre J, Fagon JY. Ventilator‐associated pneumonia. American Journal of Respiratory and Critical Care Medicine 2002;165:867‐903. [DOI] [PubMed] [Google Scholar]
Combes 2007
- Combes A, Luyt CE, Fagon JY, Wolff M, Trouillet JL, Chastre J. Early predictors for infection recurrence and death in patients with ventilator‐associated pneumonia. Critical Care Medicine 2007;35(1):146‐54. [DOI] [PubMed] [Google Scholar]
Conway Morris 2011
- Morris AC, Kefala K, Simpson AJ, Wilkinson TS, Everingham K, Kerslake D, et al. Evaluation of the effect of diagnostic methodology on the reported incidence of ventilator‐associated pneumonia. Thorax 2011;64:516‐22. [DOI] [PubMed] [Google Scholar]
Dallas 2011
- Dallas J, Skrupky L, Abebe N, Boyle W, Kollef M. Ventilator‐associated tracheobronchitis in a mixed surgical and medical ICU population. Chest 2011;139:513‐8. [DOI] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Dennesen 2001
- Dennesen PJ, Ven AJ, Kessels AG, Ramsay G, Bonten MJ. Resolution of infectious parameters after antimicrobial therapy in patients with ventilator‐associated pneumonia. American Journal of Respiratory and Critical Care Medicine 2001;163(6):1371‐5. [DOI] [PubMed] [Google Scholar]
Dimopoulos 2013
- Dimopoulos G, Poulakou G, Pneumatikos IA, Armaganidis A, Kollef MH, Matthaiou DK. Short‐ versus long‐duration antibiotic regimens for ventilator‐associated pneumonia: a systematic review and meta‐analysis. Chest 2013;144:1759‐67. [DOI] [PubMed] [Google Scholar]
Dubberke 2014
- Dubberke E, Carling P, Carrico R, Donskey C, Loo V, McDonald L, et al. Strategies to prevent Clostridium difficile infections in acute care hospitals: 2014 Update. Infection Control and Hospital Epidemiology 2014;35:628‐45. [DOI] [PubMed] [Google Scholar]
Dugan 2003
- Dugan HA, MacLaren R, Jung R. Duration of antimicrobial therapy for nosocomial pneumonia: possible strategies for minimizing antimicrobial use in intensive care units. Journal of Clinical Pharmacy and Therapeutics 2003;28(2):123‐9. [DOI] [PubMed] [Google Scholar]
El Solh 2007
- Solh AA, Choi G, Schultz MJ, Pineda LA, Mankowski C. Clinical and hemostatic responses to treatment in ventilator‐associated pneumonia: role of bacterial pathogens. Critical Care Medicine 2007;35(2):490‐6. [DOI] [PubMed] [Google Scholar]
Esperatti 2010
- Esperatti M, Ferrer M, Theessen A, Liapikou A, Valencia M, Saucedo L, et al. Nosocomial pneumonia in the intensive care unit acquired by mechanically ventilated versus nonventilated patients. American Journal of Respiratory and Critical Care Medicine 2010;182:1533‐9. [DOI] [PubMed] [Google Scholar]
FDA 2014
- US Food, Drug Administration. FDA approves label changes for antibacterial Doribax (doripenem) describing increased risk of death for ventilator patients with pneumonia. FDA Drug Safety Communication 2014:http://www.fda.gov/Drugs/DrugSafety/ucm387971.htm (accessed 4 May 2015).
Gastmeier 2009
- Gastmeier P, Sohr D, Geffers C, Rüden H, Vonberg R, Welte T. Early‐ and late‐onset pneumonia: is this still a useful classification?. Antimicrobial Agents and Chemotherapy 2009;53:2714‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grammatikos 2008
- Grammatikos AP, Siempos II, Michalopoulos A, Falagas ME. Optimal duration of the antimicrobial treatment of ventilator‐acquired pneumonia. Expert Review of Anti‐infective Therapy 2008;6(6):861‐6. [DOI] [PubMed] [Google Scholar]
Hayashi 2013
- Hayashi Y, Morisawa K, Klompas M, Jones M, Bandeshe H, Boots R, et al. Toward improved surveillance: the impact of ventilator‐associated complications on length of stay and antibiotic use in patients in intensive care units. Clinical Infectious Disease 2013;56:471‐7. [DOI] [PubMed] [Google Scholar]
HELICS 2004
- Hospital in Europe Link for Infection Control through Surveillance (HELICS). Surveillance of Nosocomial infections in intensive care units, Protocol Version 6.1. http://ecdc.europa.eu/en/activities/surveillance/HAI/Documents/0409_IPSE_ICU_protocol.pdf 2004 (accessed 9 January 2015).
Higgins 2002
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21:1539‐58. [DOI] [PubMed] [Google Scholar]
Horan 2008
- Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care‐associated infection and criteria for specific types of infections in the acute care setting. American Journal of Infection Control 2008;36:309‐32. [DOI] [PubMed] [Google Scholar]
Jensen 2011
- Jensen JU, Hein L, Lundgren B, Bestle MH, Mohr TT, Andersen MH, et al. Procalcitonin‐guided interventions against infections to increase early appropriate antibiotics and improve survival in the intensive care unit: a randomized trial. Critical Care Medicine 2011;39:2048‐58. [DOI] [PubMed] [Google Scholar]
Kipnis 2014
- Kipnis E, Nseir S. Ventilator‐associated events (VAEs): VAE Victis? (Woe to the conquered?)*. Critical Care Medicine 2014;42(8):1949‐50. [DOI] [PubMed] [Google Scholar]
Klein Klouwenberg 2014
- Klein Klouwenberg P, Mourik M, Ong D, Horn J, Schultz M, Cremer O, et al. Electronic implementation of a novel surveillance paradigm for ventilator‐associated events. Feasibility and validation. American Journal of Respiratory and Critical Care Medicine 2014;189:947‐55. [DOI] [PubMed] [Google Scholar]
Kohlenberg 2010
- Kohlenberg A, Schwab F, Behnke M, Geffers C, Gastmeier P. Pneumonia associated with invasive and noninvasive ventilation: an analysis of the German nosocomial infection surveillance system database. Intensive Care Medicine 2010;36(6):971‐8. [DOI] [PubMed] [Google Scholar]
Kollef 1995
- Kollef MH, Silver P, Murphy DM, Trovillion E. The effect of late‐onset ventilator‐associated pneumonia in determining patient mortality. Chest 1995;108(6):1655‐62. [DOI] [PubMed] [Google Scholar]
Kollef 2012b
- Kollef MH, Micek ST. Antimicrobial stewardship programs: mandatory for all ICUs. Critical Care 2012;16(6):179. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kopterides 2010
- Kopterides P, Siempos II, Tsangaris I, Tsantes A, Armaganidis A. Procalcitonin‐guided algorithms of antibiotic therapy in the intensive care unit: a systematic review and meta‐analysis of randomized controlled trials. Critical Care Medicine 2010;38(11):2229‐41. [DOI] [PubMed] [Google Scholar]
Koulenti 2009
- Koulenti D, Lisboa T, Brun‐Buisson C, Krueger W, Macor A, Sole‐Violan J, et al. Spectrum of practice in the diagnosis of nosocomial pneumonia in patients requiring mechanical ventilation in European intensive care units. Critical Care Medicine 2009;37:2360‐8. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6. Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Luna 2003
- Luna CM, Blanzaco D, Niederman MS, Matarucco W, Baredes NC, Desmery P, et al. Resolution of ventilator‐associated pneumonia: prospective evaluation of the clinical pulmonary infection score as an early clinical predictor of outcome. Critical Care Medicine 2003;31(3):676‐82. [DOI] [PubMed] [Google Scholar]
Magill 2013
- Magill S, Klompas M, Balk R, Burns SM, Deutschman C, Diekema D, et al. Developing a new, national approach to surveillance for ventilator‐associated events. Critical Care Medicine 2013;41:2467‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martin‐Loeches 2015
- Martin‐Loeches I, Torres A, Rinaudo M, Terraneo S, Rosa F, Ramirez P, et al. Resistance patterns and outcomes in intensive care unit (ICU)‐acquired pneumonia. Validation of European Centre for Disease Prevention and Control (ECDC) and the Centers for Disease Control and Prevention (CDC) classification of multidrug resistant organisms. Journal of Infection 2015;70:213‐22. [DOI] [PubMed] [Google Scholar]
Melsen 2011
- Melsen WG, Rovers MM, Koeman M, Bonten MJ. Estimating the attributable mortality of ventilator‐associated pneumonia from randomized prevention studies. Critical Care Medicine 2011;39(12):2736‐42. [DOI] [PubMed] [Google Scholar]
Melsen 2013
- Melsen WG, Rovers MM, Groenwold RH, Bergmans DC, Camus C, Bauer TT, et al. Attributable mortality of ventilator‐associated pneumonia: a meta‐analysis of individual patient data from randomised prevention studies. Lancet Infectious Diseases 2013;13(8):665‐71. [DOI] [PubMed] [Google Scholar]
Mueller 2007
- Mueller EW, Croce MA, Boucher BA, Hanes SD, Wood GC, Swanson JM, et al. Repeat bronchoalveolar lavage to guide antibiotic duration for ventilator‐associated pneumonia. Journal of Trauma 2007;63(6):1329‐37. [DOI] [PubMed] [Google Scholar]
Muscedere 2013
- Muscedere J, Sinuff T, Heyland D, Dodek P, Keenan S, Wood G, et al. The clinical impact and preventability of ventilator‐associated conditions in critically ill patients who are mechanically ventilated. Chest 2013;144:1453‐60. [DOI] [PubMed] [Google Scholar]
Niederman 2012
- Niederman MS, Chastre J, Corkery K, Fink JB, Luyt CE, García MS. BAY41‐6551 achieves bactericidal tracheal aspirate amikacin concentrations in mechanically ventilated patients with Gram‐negative pneumonia. Intensive Care Medicine 2012;38:263‐71. [DOI] [PubMed] [Google Scholar]
Rello 2002
- Rello J, Ollendorf DA, Oster G, Vera‐Llonch M, Bellm L, Redman R, et al. Epidemiology and outcomes of ventilator‐associated pneumonia in a large US database. Chest 2002;122:2115‐21. [DOI] [PubMed] [Google Scholar]
Restrepo 2013
- Restrepo M, Peterson J, Fernandez J, Qin Z, Fisher A, Nicholson S. Comparison of the bacterial etiology of early‐onset and late‐onset ventilator‐associated pneumonia in subjects enrolled in 2 large clinical studies. Respiratory Care 2013;58:1220‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Richards 2000
- Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in combined medical‐surgical intensive care units in the United States. Infection Control and Hospital Epidemiology 2000;21(8):510‐5. [DOI] [PubMed] [Google Scholar]
Rotstein 2008
- Rotstein C, Evans G, Born A, Grossman R, Light RB, Magder S, et al. Clinical practice guidelines for hospital‐acquired pneumonia and ventilator‐associated pneumonia in adults. Canadian Journal of Infectious Diseases and Medical Microbiology 2008;19(1):19‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Safdar 2005
- Safdar N, Dezfulian C, Collard HR, Saint S. Clinical and economic consequences of ventilator‐associated pneumonia: a systematic review. Critical Care Medicine 2005;33:2184‐93. [DOI] [PubMed] [Google Scholar]
Schuetz 2012a
- Schuetz P, Briel M, Christ‐Crain M, Stolz D, Bouadma L, Wolff M, et al. Procalcitonin to guide initiation and duration of antibiotic treatment in acute respiratory infections: an individual patient data meta‐analysis. Clinical Infectious Diseases 2012;55:651‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schuetz 2012b
- Schuetz P, Müller B, Christ‐Crain M, Stolz D, Tamm M, Bouadma L, et al. Procalcitonin to initiate or discontinue antibiotics in acute respiratory tract infections. Cochrane Database of Systematic Reviews 2012, Issue 9. [DOI: 10.1002/14651858.CD007498.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sharpe 2015
- Sharpe JP, Magnotti LJ, Weinberg JA, Swanson JM, Schroeppel TJ, Clement LP, et al. Adherence to an established diagnostic threshold for ventilator‐associated pneumonia contributes to low false‐negative rates in trauma patients. Journal of Trauma and Acute Care Surgery 2015;78(3):468‐73. [DOI] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D (editors). Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Stoeppel 2014
- Stoeppel CM, Eriksson EA, Hawkins K, Eastman A, Wolf S, Minei J, et al. Applicability of the National Healthcare Safety Network's surveillance definition of ventilator‐associated events in the surgical intensive care unit: a 1‐year review. Journal of Trauma and Acute Care Surgery 2014;77:934‐7. [DOI] [PubMed] [Google Scholar]
Szakmany 2013
- Szakmany T, Harrison W, Roberts H, Scholey G, Pugh R. Surveillance for ventilator‐associated pneumonia (VAP) in Wales: is HELICS the best way?. Critical Care Medicine 2013;41(Suppl 12):46. [Google Scholar]
Vincent 1995
- Vincent JL, Bihari DJ, Suter PM, Bruining HA, White J, Nicolas‐Chanoin MH, et al. The prevalence of nosocomial infection in intensive care units in Europe. Results of the European Prevalence of Infection in Intensive Care (EPIC) Study. EPIC International Advisory Committee. JAMA 1995;274(8):639‐44. [PubMed] [Google Scholar]
Vincent 2009
- Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA 2009;302(21):2323‐9. [DOI] [PubMed] [Google Scholar]
Visscher 2008
- Visscher S, Schurink CA, Melsen WG, Lucas PJ, Bonten MJ. Effects of systemic antibiotic therapy on bacterial persistence in the respiratory tract of mechanically ventilated patients. Intensive Care Medicine 2008;34(4):692‐9. [DOI] [PubMed] [Google Scholar]
Warren 2003
- Warren DK, Shukla SJ, Olsen MA, Kollef MH, Hollenbeak CS, et al. Outcome and attributable cost of ventilator‐associated pneumonia among intensive care unit patients in a suburban medical center. Critical Care Medicine 2003;31:1312‐7. [DOI] [PubMed] [Google Scholar]
Wunderink 2000
- Wunderink R. Radiologic diagnosis of ventilator‐associated pneumonia. Chest 117;117(Suppl):188‐90. [DOI] [PubMed] [Google Scholar]
Zhuo 2008
- Zhuo H, Yang K, Lynch SV, Dotson RH, Glidden DV, Singh G, et al. Increased mortality of ventilated patients with endotracheal Pseudomonas aeruginosa without clinical signs of infection. Critical Care Medicine 2008;36(9):2495‐503. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Pugh 2009
- Pugh R, Grant C, Cooke RPD, Dempsey G. Short‐course versus prolonged‐course antibiotic therapy for hospital‐acquired pneumonia in critically ill adults. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD007577] [DOI] [Google Scholar]
Pugh 2011
- Pugh R, Grant C, Cooke RPD, Dempsey G. Short‐course versus prolonged‐course antibiotic therapy for hospital‐acquired pneumonia in critically ill adults. Cochrane Database of Systematic Reviews 2011, Issue 10. [DOI: 10.1002/14651858.CD007577.pub2] [DOI] [PubMed] [Google Scholar]


