Abstract
Objective
This study investigated psychological characteristics of patients with chronic complex regional pain syndrome (CRPS) and examined relationships between psychosocial factors and pain severity.
Methods
In total, 76 patients with CRPS, 95 patients with other types of chronic pain, 171 healthy controls, and 66 patients with major depressive disorder (MDD) were included. Minnesota Multiphasic Personality Inventory (MMPI-2) profiles and scores on the Beck Depression Inventory and State–Trait Anxiety Inventory were calculated. Pain intensity was measured using a visual analog scale (VAS).
Results
Patients with CRPS scored higher on the Hypochondriasis (Hs), Depression (D), Hysteria (Hy), Paranoia (Pa), and Psychasthenia (Pt) scales of the MMPI-2 compared to healthy controls. The CRPS group scored lower on the D, Psychopathic deviate (Pd), Pa, Pt, Schizophrenia (Sc), and Social introversion (Si) scales compared to the MDD group. Although CRPS patients reported higher levels of pain than patients with other types of pain, the MMPI profiles of the two pain groups did not differ significantly. Linear regression analyses revealed that pain severity was significantly associated with depression and scores on the Masculinity–Femininity (Mf) scale.
Conclusion
This is the first comparative study of the psychological characteristics of chronic CRPS patients, healthy controls, and patients with MDD. The neurotic profiles of CRPS patients were more psychologically adaptable than were those of patients with MDD; however, this profile was shared by both pain groups. The present findings further showed that, although pain severity was not a major contributor to depression, patients with CRPS should be evaluated for depressive symptoms.
Keywords: pain, anxiety, depression, complex regional pain syndrome, major depressive disorder, Minnesota Multiphasic Personality Inventory-2
Introduction
Chronic pain has been defined as prolonged pain that lasts beyond tissue recovery or persistent pain that is not responsive to treatment.1 Multiple factors contribute to the pathophysiological mechanisms of chronic pain, including tissue response to acute injury, psychological characteristics, and social variables.2,3 Previous studies have reported the psychopathological characteristics of patients with chronic pain, including alexithymia, catastrophizing, anxiety, and depression, and data support the association of psychological factors with pain thresholds.3,4 Depression is one of the most common psychiatric diagnoses among patients with chronic pain,5 depression and pain frequently co-occur and influence each other in a bidirectional manner, and each is a predictor of the symptoms associated with the other.6 Comorbid depression has several adverse effects, including pain severity and disabilities in patients with chronic pain,7 whereas treatment for depression improves pain severity as well as disabilities.8 However, the association between pain and depression is complex, and the causal relationships remain unclear and vary among pain patient subgroups.
Complex regional pain syndrome (CRPS) is among the sequelae of actual or potential tissue injury after surgery or trauma; symptoms include severe pain, hyperalgesia, allodynia, changes in skin color/temperature, and abnormal motor or trophic symptoms.9 There are two subtypes of CRPS; type 1 develops in the absence of definable nerve injury, and type 2 is accompanied by a nerve lesion. The etio–pathological processes of CRPS are also poorly understood, and there have been contrasting results regarding the role of psychological factors. Previous studies have suggested that there is no association between psychological factors and CRPS.10 However, other recent research has suggested that central mechanisms are also involved in the pathophysiology of CRPS and have demonstrated associations between psychological factors and pain outcomes in patients with CRPS.11,12 Regardless, these results are not conclusive and few studies have specifically investigated this topic.13–15 Several studies that have examined psychological traits in patients with chronic pain using the Minnesota Multiphasic Personality Inventory (MMPI-2)16,17 and reported that psychological factors modulate pain sensitization by mediating physiological responses to psychological stressors.18 The MMPI-2 assesses personality traits and psychopathologies from various perspectives19 and previous research has demonstrated that the validity indicators of this tool are capable of detecting intentional exaggeration.20 However, a recent review noted the dearth of research on CRPS, despite accumulating evidence of the usefulness of the MMPI for patients with other types of pain in relation to the different aspects of personality traits, patterns of psychopathology for differential diagnostic groupings, and malingering.21 Indeed, patients with pain may exhibit exaggerated or feigned pain behaviors when they are involved in medico-legal situations.22
Thus, the present study compared the psychological characteristics of CRPS patients, including personality traits and exaggerating tendencies, with those of patients experiencing other types of chronic pain, patients with major depressive disorder (MDD), and normal controls to investigate the specific psychological traits associated with CRPS. Additionally, this study evaluated the usefulness of the MMPI-2 for elucidating the relationship between personality traits and chronic CRPS and for differentiating chronic CRPS from other types of chronic pain. The present study also examined associations between psychosocial factors and subjective experiences of pain in patients with chronic pain.
Materials and Methods
Subjects
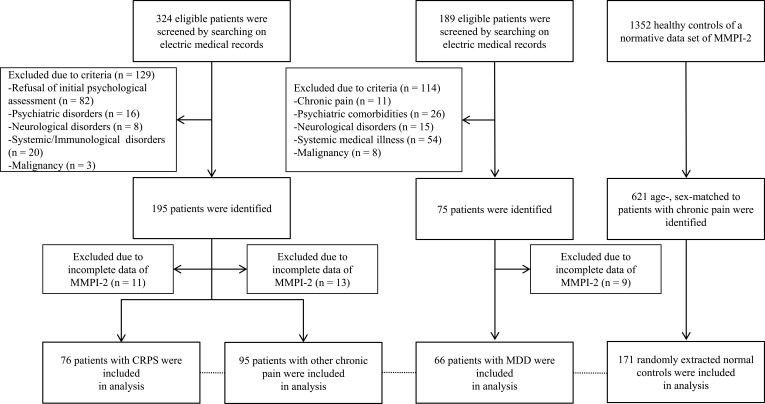
This was a retrospective study of the medical records of a sample of 324 consecutive patients with chronic back/low back or pelvis/hip or extremity pain persisting over 6 months who visited the interdisciplinary pain clinic at Seoul National University Bundang Hospital (SNUBH), Korea, between Jan. 2013 and Dec. 2018. The flow chart for the study process is presented in Figure 1 and the inclusion criteria were as follows: 1) completion of the MMPI-2 at an initial assessment at the pain clinic and 2) aged between 18 and 64 years. The exclusion criteria were as follows: 1) serious psychiatric disorders, such as bipolar disorder, psychosis, and cognitive disorder; 2) neurological disorders, such as cerebrovascular disorder, Parkinson’s disease, and epilepsy; and/or 3) systemic medical illnesses that could be responsible for the chronic pain, including malignancy and inflammatory rheumatic diseases such as Sjögren’s syndrome, systemic lupus erythematosus, rheumatoid arthritis and polymyalgia rheumatica. After the exclusion process, the final sample included 171 patients (76 CRPS patients and 95 patients with other types of chronic pain). The diagnosis of CRPS was confirmed according to the Budapest research criteria issued by International Association for the Study of Pain (IASP).23 The Structured Clinical Interview for DSM-IV axis I disorders (SCID-I) was used to identify major psychiatric disorders.24 As a comparison group for the patients with clinically significant psychopathologies, 189 patients with MDD who visited the SNUBH outpatient psychiatry clinic and completed the MMPI-2 during the same period were screened. The data of 66 patients who satisfied the inclusion and exclusion criteria were included in the comparative analysis. The inclusion criteria were the same as those for patients with chronic pain and the exclusion criteria were as follows: patients with 1) chronic pain; 2) other serious psychiatric comorbidities; 2) neurological disorders; and/or 3) systemic medical illnesses or physical symptoms that could be responsible for depression (ie, a mood disorder due to a general medical condition).
Figure 1.
Flow chart of the study process.
Abbreviations: CRPS, chronic regional pain syndrome; MDD, major depressive disorder; MMPI-2, Minnesota Multiphasic Personality Inventory-2.
We also obtained a normative data set from a study of the Korean version of MMPI-225 (permission for the use of this data set was granted by the Maumsarang Institute, Seoul, Korea) to serve as a healthy Korean control group. First, the participants were divided into age-stratified subgroups that consisted of controls that corresponded to each patient with chronic pain. Then, matched control subjects from each stratified subgroup were randomly selected for the 171 patients with chronic pain; ultimately, 171 age- and sex-matched controls from 1352 healthy participants were included in the analyses. A total of 408 subjects (76 patients with CRPS, 95 patients with other types of chronic pain, 66 patients with MDD, and 171 healthy controls) were included in the comparative analyses of the MMPI-2.
This study was conducted following the ethical standards by Helsinki Declaration (World Medical Association, 2013) and the Institutional Review Board of SNUBH approved this study protocol and waived informed consent owing to the nature of this study using a retrospective chart review (IRB No. B1907550106).
Assessments
We collected data on demographic characteristics, including age, sex, educational level, and marital status, and on clinical variables, including location and mean duration of pain, and diagnosis. A visual analog scale (VAS) was used to assess the intensity of pain (0 = “no pain” to 10 = “the worst possible pain”). Patients completed the MMPI-2, the Beck Depression Inventory-II (BDI-II),26 the State–Trait Anxiety Inventory (STAI),27 and clinical assessments during their routine diagnostic and treatment planning assessments. The BDI-II consists of 21 items assessing depressive symptoms, with higher scores indicating more severe depression. The STAI includes two 20-item scales: The State scale measures current anxiety symptoms, and the Trait scale assesses general anxiety levels. Psychological characteristics were assessed using the MMPI-2, a 567-item self-report yes/no questionnaire, and we used three validity scales (the Lie (L), Infrequency (F), and Correction (K) scales) and 10 clinical scales: 1 (Hypochondriasis, Hs), 2 (Depression, D), 3 (Hysteria, Hy), 4 (Psychopathic deviate, Pd), 5 (Masculinity-Femininity, Mf), 6 (Paranoia, Pa), 7 (Psychasthenia, Pt), 8 (Schizophrenia, Sc), 9 (Hypomania, Ma), and 10 (Social introversion, Si). Raw scale scores were converted to T scores with a mean of 50 and a standard deviation of 10. Scores over 65T imply the possibility of psychopathology.
Statistical Analysis
Pearson’s χ2 test was used to analyze categorical clinical and demographic variables, and t-tests were used to compare the two chronic pain groups with regard to continuous variables. We performed analysis of variance (ANOVA) treating MMPI-2 scores as dependent variables to compare scale scores among the four groups. We also used linear regression to analyze related psychosocial factors to the pain severity (VAS) scores of patients with chronic pain. All tests were two-tailed, and, with the exception of the comparisons involving the MMPI-2 that used an adjusted alpha level <0.0038 (0.05/13 criterion variables for each scale), p-values <0.05 were considered significant. To compare the MMPI-2 scores among the four groups, p-values adjusted for multiple corrections using an adjusted alpha and Scheffe’s post hoc tests were considered to indicate statistical significance. All analyses were performed using SPSS for Windows software (ver. 20.0; SPSS, Inc., Chicago, IL, USA).
Results
Demographic and Clinical Characteristics
Of the 171 patients with chronic pain included in the analysis, 76 (44.4%) were diagnosed with CRPS. Of the 76 patients with CRPS, 57 (75.0%) were diagnosed with CRPS type 1, and 19 were diagnosed with CRPS type 2. Patients with CRPS were significantly younger and scored higher on the VAS compared to the other chronic pain group (Table 1). The CRPS group had a mean age of 36.05 ± 13.02 years; 41 patients were male, and the mean duration of pain was 2.65 ± 2.70 years. Patients with other chronic pain had a mean age of 41.65 ± 14.43 years; 40 patients were male, and the mean duration of pain was 3.12 ± 5.09 years.
Table 1.
Demographic and Clinical Characteristics of Patients with Chronic Pain
| Variables | CRPS (n = 76) | Other Chronic Pain (n = 95) | χ2/t | p |
|---|---|---|---|---|
| Age (years)a | 36.05 ± 13.02 | 41.65 ± 14.43 | −2.63 | 0.009 |
| Sex (Male/Female) | 41/35 | 40/55 | 2.37 | 0.123 |
| Educational levelb | 2.59 | 0.629 | ||
| Primary | 3 (3.9%) | 3 (3.2%) | 1.36 | 0.713 |
| Secondary | 5 (6.6%) | 10 (10.5%) | ||
| High level | 42 (55.3%) | 46 (48.4%) | ||
| Degree | 26 (34.2%) | 36 (37.9%) | ||
| Marital status, marriedb | 37 (48.6%) | 50 (52.3%) | 1.15 | 0.561 |
| Pain location | ||||
| Lower Extremity | 48 | 23 | ||
| Upper Extremity | 44 | 25 | ||
| Hip and Pelvis | 3 | 8 | ||
| Low back | 0 | 28 | ||
| Back | 2 | 15 | ||
| Whole body | 4 | 11 | ||
| Pain Severity (Visual Analogue Scale)a | 7.01 ± 1.76 | 5.43 ± 2.48 | 4.68 | <0.001 |
| Duration of pain symptom (years)a | 2.65 ± 2.70 | 3.12 ± 5.09 | −0.72 | 0.468 |
| Co-morbid psychiatric diagnosisb | 25 (32.9%) | 37 (38.9%) | 0.66 | 0.413 |
| Beck Depression Inventory-IIa | 24.73 ± 14.70 | 26.74 ± 13.40 | −0.89 | 0.374 |
| State-Trait Anxiety Inventory-Statea | 59.87 ± 14.31 | 59.62 ± 14.42 | 0.11 | 0.911 |
| State-Trait Anxiety Inventory-Traita | 57.36 ± 15.32 | 57.64 ± 13.27 | –0.12 | 0.903 |
Notes: aData given as mean ± standard deviation. bData given as number (%). The Student’s t-tests were applied for the comparison of means and Pearson’s χ2 tests were applied for the comparison of proportions.
Abbreviation: CRPS, chronic regional pain syndrome.
Co-morbid psychiatric disorders (including patients with more than one diagnosis) included depressive disorder (n = 25) and panic disorder (n = 2) in the CRPS group and depressive disorder (n = 30), somatoform disorder (n = 5), posttraumatic stress disorder (n = 2), generalized anxiety disorder (n = 1), and cyclothymic disorder (n = 1) in the other pain group.
The MDD group included 66 patients with a mean age of 36.45 ± 13.38 years; 32 patients were male. The mean symptom duration was 2.50 ± 2.73 years, and the mean BDI-II, STAI-State, and STAI-Trait scores were 36.03 ± 9.55, 71.95 ± 10.32, and 69.71 ± 10.21, respectively. The normal control (age- and sex-matched to patient groups) group included 171 subjects with a mean age of 39.27 ± 13.73; 81 subjects were male. There were no statistically significant differences in terms of the mean age or sex ratio among the four groups (408 participants).
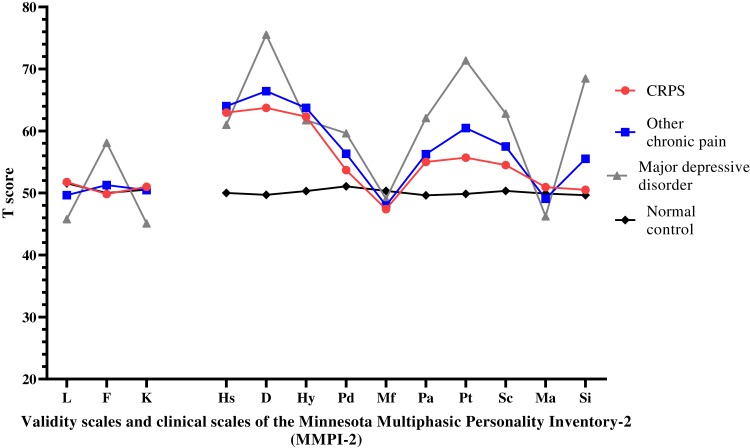
Psychological Characteristics
The mean MMPI-2 scale scores of the four groups (408 participants; CRPS, other chronic pain, MDD, and normal control groups) are presented in Table 2. As shown in Figure 2, mean scores >65T, which implies the possibility of clinically significant symptoms, were found in those with non-CRPS pain for Depression and those with MDD for Depression, Psychasthenia, and Social introversion. The results reflect significant differences among groups in psychological and psychopathological characteristics. Post hoc analyses revealed that the CRPS group scored significantly higher on the Lie (p = 0.004) and Correction (p = 0.003) scales than the MDD group and scored significantly higher on the Hypochondriasis (p < 0.001), Depression (p < 0.001), Hysteria (p < 0.001), Paranoia (p = 0.017), and Psychasthenia (p = 0.005) scales than the normal control group. In contrast, the CRPS group scored significantly lower on the Infrequency (p < 0.001), Depression (p < 0.001), Psychopathic deviate (p = 0.007), Paranoia (p = 0.021), Psychasthenia (p < 0.001), Schizophrenia (p < 0.001), and Social introversion (p < 0.001) scales than the MDD group. However, there were no significant differences between the two pain groups. These data suggest that the CRPS group experienced more psychosocial distress, depression, emotional sensitivity, and somatic sensitivity compared to the normal control group, but that they also experienced less anxiety, distress, and social withdrawal than the MDD group. However, the scores of the CRPS group were comparable to those of the other chronic pain group.
Table 2.
Scores on the Minnesota Multiphasic Personality Inventory-2 Scales of the Three Patient Groups and Normal Control Group
| Scale | A. CRPS (n = 76) | B. Other Chronic Pain (n = 95) | C. MDD (n = 66) | D. Normal Control (n = 171) | F (df) | p | Post hoc |
|---|---|---|---|---|---|---|---|
| L | 51.77 ± 11.72 | 49.66 ± 9.34 | 45.78 ± 8.86 | 51.55 ± 10.02 | 6.00 (3, 404) | 0.001 | C < A = D |
| F | 49.82 ± 9.55 | 51.28 ± 11.62 | 58.12 ± 12.08 | 50.01 ± 9.38 | 10.66 (3, 404) | <0.001 | A = B = D < C |
| K | 51.00 ± 11.52 | 50.47 ± 10.35 | 45.12 ± 7.99 | 50.53 ± 10.05 | 5.49 (3, 404) | 0.001 | C < A = B = D |
| Hs | 62.96 ± 11.85 | 64.01 ± 10.73 | 61.00 ± 10.48 | 50.00 ± 9.85 | 49.97 (3, 404) | <0.001 | D < A = B = C |
| D | 63.73 ± 13.60 | 66.41 ± 13.79 | 75.54 ± 10.91 | 49.71 ± 9.48 | 95.66 (3, 404) | <0.001 | D < A = B < C |
| Hy | 62.30 ± 11.50 | 63.72 ± 10.55 | 61.75 ± 9.57 | 50.32 ± 10.79 | 45.01 (3, 404) | <0.001 | D < A = B = C |
| Pd | 53.69 ± 11.15 | 56.33 ± 12.15 | 59.63 ± 10.05 | 51.07 ± 11.06 | 10.85 (3, 404) | <0.001 | A < C, D < B = C |
| Mf | 47.40 ± 9.48 | 47.98 ± 10.11 | 49.04 ± 11.23 | 50.33 ± 9.45 | 2.01 (3, 404) | 0.112 | |
| Pa | 55.02 ± 13.98 | 56.25 ± 12.99 | 62.10 ± 14.37 | 49.63 ± 9.75 | 18.20 (3, 404) | <0.001 | D < A < C, D < B |
| Pt | 55.71 ± 13.03 | 60.48 ± 12.91 | 71.36 ± 11.61 | 49.87 ± 10.37 | 57.23 (3, 404) | <0.001 | D < A = B < C |
| Sc | 54.51 ± 13.70 | 57.51 ± 13.19 | 62.80 ± 11.73 | 50.34 ± 10.40 | 19.40 (3, 404) | <0.001 | A = B < C, D < B |
| Ma | 50.94 ± 10.95 | 49.07 ± 9.70 | 46.25 ± 9.73 | 49.90 ± 10.02 | 2.89 (3, 404) | 0.035 | |
| Si | 50.47 ± 13.41 | 55.53 ± 13.41 | 68.48 ± 11.22 | 49.66 ± 9.45 | 44.90 (3, 404) | <0.001 | A < C, D < B < C |
Note: Data given as mean ± standard deviation. ANOVA test was applied for the comparison of means and followed by the Scheffe’s post hoc test for multiple comparisons.
Abbreviations: CRPS, chronic regional pain syndrome; MDD, major depressive disorder; L, Lie; F, Infrequency; K, Correction; Hs, Hypochondriasis; D, Depression; Hy, Hysteria; Pd, Psychopathic deviate; Mf, Masculinity–Femininity; Pa, Paranoia; Pt, Psychasthenia; Sc, Schizophrenia; Ma, Hypomania; Si, Social introversion.
Figure 2.
Mean T scores on the Minnesota Multiphasic Personality Inventory-2 scales among 4 groups.
Abbreviations: CRPS, chronic regional pain syndrome; L, Lie; F, Infrequency; K, Correction; Hs, Hypochondriasis; D, Depression; Hy, Hysteria; Pd, Psychopathic deviate; Mf, Masculinity–– emininity; Pa, Paranoia; Pt, Psychasthenia; Sc, Schizophrenia; Ma, Hypomania; Si, Social introversion.
Factors Associated with Pain Severity
We performed multivariate linear regression analyses treating diagnosis, age, sex, educational level, marriage, symptom duration, the 13 MMPI-2 scales, the BDI-II, and the STAI as independent variables to identify variables affecting subjective pain levels. A diagnosis of CRPS was related to the level of pain and psychosocial variables were also significantly associated with pain severity (Table 3). Patients with higher levels of depression (BDI-II) and a more stereotypical gender identity (MMPI-2, Masculinity-Femininity scale), tended to report more severe pain.
Table 3.
Stepwise Linear Regression Analysis of the Variables Associated with the Pain Severity in Patients with Chronic Pain (n = 171)
| Variables | VAS Score | Corrected R2 | |
|---|---|---|---|
| B (SE) | p | ||
| CRPS versus other chronic pain | 2.82 (0.441) | <0.001 | 0.143 |
| BDI-II | 0.038 (0.013) | 0.005 | 0.181 |
| MMPI-2, Mf score | −0.054 (0.019) | 0.017 | 0.211 |
Note: The model is adjusted for diagnosis, age, sex, educational level, marriage, symptom duration, scores on the MMPI-2, BDI-II, and STAI.
Abbreviations: VAS, visual analog scale; CRPS, complex regional pain syndrome; BDI-II, Beck Depression Inventory-II; MMPI-2, Minnesota Multiphasic Personality Inventory-2; Mf, Masculinity–Femininity.
Discussion
To our knowledge, this is the first study to investigate the MMPI-2 profiles of patients with chronic CRPS and to compare them with those of patients with MDD as well as normal controls. In the CRPS group, no MMPI-2 scale scores exceeded the 65T threshold for clinically significant psychopathology. Moreover, the CRPS groups’ Depression, Psychopathic deviate, Paranoia, Psychasthenia, Schizophrenia, and Social introversion scale scores, which are generally considered to reflect depression, social disinhibition, interpersonal sensitivity, anxiety, apathy, cognitive disturbance, and social withdrawal, respectively, were lower than those of patients with MDD. Otherwise, the scores of patients with chronic CRPS were intermediate between those of the control and MDD groups with regard to levels of depression, anxiety, and interpersonal sensitivity.28 It has been suggested that the use of the MMPI-2 may be limited in studies investigating pain because, as a state factor, chronic pain may influence trait measurements even though the MMPI-2 is a standardized test of personality traits.29 Thus, the present study included the BDI-II and STAI in addition to the MMPI-2 to investigate, independently, the state and trait factors of depression and anxiety, respectively. The differences between groups remained after adjusting for the severities of state depression (ie, BDI-II score) and state anxiety. In fact, the MMPI-2 Depression scale has been criticized for “underreporting” underlying psychological problems because of its inclusion of items that relate to both somatic symptoms and neurotic traits; thus, patients with chronic pain may be especially sensitive to physical items.30 However, the depression scores of the CRPS group were also at an intermediate level and fell between those of the normal and MDD groups on the BDI-II. In other words, these differences in psychological traits did not simply reflect the severities of depressive and anxiety symptoms but, rather, reflected, at least in part, the differences in the personality traits of the two disease groups. The present study also observed relatively higher Lie, Correction scores and lower Infrequency scores in patients with chronic CRPS compared to patients with MDD, which implies that the CRPS patients were less likely to complain about their psychological problems than to over-report or exaggerate their symptoms. Furthermore, the scores of the CRPS patients on the validity scales did not differ from those of normal controls, which suggests that the patients with chronic CRPS did not necessarily feign their problems, as reported previously.22
These results suggest that patients with chronic CRPS experience depression, anxiety, and somatic symptoms, but these symptoms and their underlying mechanisms differ from those associated with MDD, which involves emotional dysregulation as a core mechanism. A large cohort study reported that CRPS1 patients scored in the average or below average range of psychopathology compared to both the general population and psychiatric patients.10 Recent studies have suggested that pain-induced depression differs from depressive disorder as a mental disorder in terms of symptomatology and pathophysiology. For example, the extent and enrollment of “top-down” and “bottom-up” regulations and related brain circuits vary even though there are several shared mechanisms.31–33 The present results demonstrating different personality trait profiles between chronic CRPS and MDD patients also support these previous suggestions.
However, the present results from the association analysis suggest that chronic pain and depression may have shared mechanisms that exert bidirectional effects. In this study, both pain groups reported moderate levels of depressive symptoms on the BDI-II, and depression severity was associated with subjective pain severity, as measured by the VAS. These findings are consistent with previous research on a sample of patients with chronic pain, although the conclusion was not robust.7,8,17,32,34 Previous research also reported that pain severity was associated with higher distress levels among patients with CRPS.35 However, the causal relationship between pain and depression is unclear; for example, higher levels of distress may be associated with a lower pain threshold in patients with CRPS, but it may also be caused by the pain symptoms of CRPS.36 From a biological perspective, it has been suggested that psychological factors may modulate and affect both the maintenance and the intensity of pain by altering catecholamine activity and neural circuits.37,38 Previous studies described that psychological factors, including depression and anxiety, were associated with more severe pain, more disability, and poorer long-term recovery among patients with CRPS.7,8,11 The other results of our regression analysis indicated that Mf scores were negatively associated with pain severity, which indicates that “more masculine” males and “more feminine” females may experience more severe pain. Several studies have reported that “less masculine” males and “more feminine” females tended to report more pain.39 However, these patterns are heterogenous among various societies because of ethno-sociocultural factors. Moreover, previous studies have demonstrated that both gender-associated traits and sex differences may be involved in pain modulation and subjective reports.40,41 Thus, our results suggest that the intensity of pain may be related to gender and sex, but further research is needed to clarify these relationships.
In the present study, the CRPS patients scored higher on the Hs, D, Hy, Pa, and Pt MMPI-2 scales than the normal controls while the results of patients with other types of chronic pain were similar to those of the CRPS group. A previous study reported that patients with fibromyalgia scored higher on the MMPI-2 scales compared to normal controls, but the majority of the mean scores did not exceed the cutoff for psychopathology.34 It has been established that patients with chronic pain are more likely to exhibit particular MMPI-2 profiles, known as the “conversion V” or “neurotic triad”.42 Our findings that the Hypochondriasis and Hysteria scores were lower than the Depression scores are consistent with the neurotic triad pattern previously observed in patients with chronic pain.17,28 The neurotic triad pattern is related to depressive tendencies, introversion, hypochondriacal anxiety, and catastrophizing often involved in pathological conditions associated with chronic pain; it has also been associated with low tolerance for and high sensitivity to pain.43 However, few studies have investigated the specific personality traits of CRPS patients. A study of 17 patients with CRPS reported that their MMPI-2 profiles were similar to those of patients with conversion disorder.14 An earlier study noted that patients with CRPS scored lower on the Hypochondriasis, Depression, Hysteria, and Psychasthenia scales but higher on the Hypomania scale compared to myofascial pain syndrome patients.15 Similarly, a previous study reported various types of MMPI profiles within a heterogenous sample of patients with pain: disabilities, conversion V, neurotic triad, and normal.44 Consistent with previous research,45 the results observed in the two pain groups in the present study suggest that these psychological profiles may contribute to the chronicity of pain or that they may be secondary to the chronic pain itself rather than predisposing individuals to the development of CRPS. Furthermore, patients with chronic CRPS showed comparable levels of psychopathology despite significantly more intense pain. This may be attributable to CRPS patients’ difficulty with recognizing or describing emotions, a condition known as an alexithymia.35 Taken together, our results suggest that patients with chronic CRPS may have a pattern of personality traits and this pattern differs from that of healthy subjects. However, although patients with CRPS may have common patterns of personality traits, such patterns are not specific to chronic CRPS.
Because this study was retrospective and employed a case-control design, it was not possible to investigate causal relationships between psychological factors and pain/pain disorders. Additionally, this study included a modest number of participants drawn from a single pain center; thus, these results cannot be generalized. Furthermore, as only those participants who completed the MMPI-2 were included, there may have been a selection bias in that patients with relatively less pain or better functioning may have been more likely to complete the entire questionnaire. The preset study included patients with chronic pain as well as patients with chronic CRPS and, thus, the results should be interpreted cautiously as they may not be generalizable to patients in the initial phases of pain disorders. Finally, subjects in the non-CRPS pain group were heterogeneous and had a variety of diagnoses, which may have attenuated the significance of contrasts between the two pain groups.
Conclusions
The present study investigated the psychological characteristics of patients with chronic CRPS using the MMPI-2 and compared these with those of three other groups: normal controls, patients with other types of chronic pain, and patients with MDD. Patients with chronic CRPS were not more psychologically disturbed than other patients with chronic pain or patients with MDD, which may imply that patients with CRPS have relatively intact emotional regulation or that depression in patients with CRPS is different from depression in mental disorder. Also, our results showed that patients with chronic CRPS tend to deny and/or underreport psychological symptoms rather than to exaggerated or feign. However, our observation of associations between depression and pain severity suggests that CRPS patients should be evaluated and, when necessary, treated for distress even when they report relatively mild symptoms. Further studies including a large enough sample to analyze according to CRPS subtype would clarify the role of specific psychological factors in chronic pain and in pain disorders such as CRPS.
Additionally, the profile of patients with chronic pain differed from that of normal subjects and was consistent with the so-called neurotic triad, suggesting the existence of chronic pain-related personality traits. However, this pattern was not specific to CRPS patients. Thus, future prospective research studies using the MMPI will be necessary to determine whether these factors predispose individuals to chronic pain or arise during adaptation to this type of pain.
Acknowledgments
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (NRF-2017R1C1B2012733). The authors thank the Division of Statistics in Medical Research Collaborating Center at Seoul National University Bundang Hospital for statistical analyses.
Abbreviations
CRPS, complex regional pain syndrome; MDD, major depressive disorder; MMPI-2, Minnesota Multiphasic Personality Inventory-2; VAS, visual analog scale; Hs, Hypochondriasis; D, Depression; Hy, Hysteria; Pa, Paranoia; Pt, Psychasthenia; Pd, Psychopathic deviate; Sc, Schizophrenia; Si, Social introversion; Mf, Masculinity–Femininity.
Disclosure
All authors declared no conflicts of interest with respect to the present study.
References
- 1.Harvey AM. Classification of chronic pain – descriptions of chronic pain syndromes and definitions of pain terms. Clin J Pain. 1995;11(2):163. doi: 10.1097/00002508-199506000-00024 [DOI] [Google Scholar]
- 2.Hosoi M, Molton IR, Jensen MP, et al. Relationships among alexithymia and pain intensity, pain interference, and vitality in persons with neuromuscular disease: considering the effect of negative affectivity. PAIN®. 2010;149(2):273–277. doi: 10.1016/j.pain.2010.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramond A, Bouton C, Richard I, et al. Psychosocial risk factors for chronic low back pain in primary care – a systematic review. Fam Pract. 2011;28(1):12–21. doi: 10.1093/fampra/cmq072 [DOI] [PubMed] [Google Scholar]
- 4.Dickens C, McGowan L, Dale S. Impact of depression on experimental pain perception: a systematic review of the literature with meta-analysis. Psychosom Med. 2003;65(3):369–375. doi: 10.1097/01.PSY.0000041622.69462.06 [DOI] [PubMed] [Google Scholar]
- 5.Knaster P, Karlsson H, Estlander A-M, Kalso E. Psychiatric disorders as assessed with SCID in chronic pain patients: the anxiety disorders precede the onset of pain. Gen Hosp Psychiatry. 2012;34(1):46–52. doi: 10.1016/j.genhosppsych.2011.09.004 [DOI] [PubMed] [Google Scholar]
- 6.Kroenke K, Wu J, Bair MJ, Krebs EE, Damush TM, Tu W. Reciprocal relationship between pain and depression: a 12-month longitudinal analysis in primary care. J Pain. 2011;12(9):964–973. doi: 10.1016/j.jpain.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kroenke K, Wu J, Bair MJ, Damush TM, Krebs EE, Tu W. Impact of depression on 12-month outcomes in primary-care patients with chronic musculoskeletal pain. J Musculoskelet Pain. 2012;20(1):8–17. doi: 10.3109/10582452.2011.635844 [DOI] [Google Scholar]
- 8.Kroenke K, Bair MJ, Damush TM, et al. Optimized antidepressant therapy and pain self-management in primary care patients with depression and musculoskeletal pain: a randomized controlled trial. JAMA. 2009;301(20):2099–2110. doi: 10.1001/jama.2009.723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harden RN, Bruehl SP. Diagnosis of complex regional pain syndrome: signs, symptoms, and new empirically derived diagnostic criteria. Clin J Pain. 2006;22(5):415–419. doi: 10.1097/01.ajp.0000194279.36261.3e [DOI] [PubMed] [Google Scholar]
- 10.Beerthuizenl A, Stronksl DL, Huygenl FJ, Passchierl J, Kleinl J, Van’t Spijkerl A. The association between psychological factors and the development of complex regional pain syndrome type 1 (CRPS1) – a prospective multicenter study. Eur J Pain. 2011;15(9):971–975. doi: 10.1016/j.ejpain.2011.02.008 [DOI] [PubMed] [Google Scholar]
- 11.Bean D. The Impact of Psychological Factors on Complex Regional Pain Syndrome Type-1. ResearchSpace@ Auckland; 2015. [Google Scholar]
- 12.Popkirov S, Hoeritzauer I, Colvin L, Carson AJ, Stone J. Complex regional pain syndrome and functional neurological disorders – time for reconciliation. J Neurol Neurosurg Psychiatry. 2019;90(5):608–614. doi: 10.1136/jnnp-2018-318298 [DOI] [PubMed] [Google Scholar]
- 13.Choi J, Cho S, Lim K, Han K. MMPI profiles and the other psychometric characteristics of patients with complex regional pain syndrome. Korean J Health Psychol. 2009;14(2):313–327. doi: 10.17315/kjhp.2009.14.2.006 [DOI] [Google Scholar]
- 14.Shiri S, Tsenter J, Livai R, Schwartz I, Vatine -J-J. Similarities between the psychological profiles of complex regional pain syndrome and conversion disorder patients. J Clin Psychol Med Settings. 2003;10(3):193–199. doi: 10.1023/A:1025462829059 [DOI] [Google Scholar]
- 15.Nelson DV, Novy DM. Psychological characteristics of reflex sympathetic dystrophy versus myofascial pain syndromes. Reg Anesth Pain Med. 1996;21(3):202–208. [PubMed] [Google Scholar]
- 16.Butcher JN, Graham JR, Ben-Porath YS, Tellegen A, Dahlstrom W, Kaemmer B. MMPI-2: Manual for Administration, Scoring, and Interpretation. Rev ed. Minneapolis, MN: University of Minnesota; 2001. [Google Scholar]
- 17.Nordin H, Eisemann M, Richter J. MMPI‐2 subgroups in a sample of chronic pain patients. Scand J Psychol. 2005;46(2):209–216. doi: 10.1111/sjop.2005.46.issue-2 [DOI] [PubMed] [Google Scholar]
- 18.Malin K, Littlejohn GO. Personality and fibromyalgia syndrome. Open Rheumatol J. 2012;6:273–285. doi: 10.2174/1874312901206010273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gatchel RJ, Weisberg JN. Personality Characteristics of Patients with Pain. American Psychological Association; 2000. [Google Scholar]
- 20.Bianchini KJ, Etherton JL, Greve KW, Heinly MT, Meyers JE. Classification accuracy of MMPI-2 validity scales in the detection of pain-related malingering: a known-groups study. Assessment. 2008;15(4):435–449. doi: 10.1177/1073191108317341 [DOI] [PubMed] [Google Scholar]
- 21.Piotrowski C. MMPI-related pain research through the lens of bibliometric analysis: mapping investigatory domain. N Am J Psychol. 2018;20(1):2–5. [Google Scholar]
- 22.Greve KW, Ord JS, Bianchini KJ, Curtis KL. Prevalence of malingering in patients with chronic pain referred for psychologic evaluation in a medico-legal context. Arch Phys Med Rehabil. 2009;90(7):1117–1126. doi: 10.1016/j.apmr.2009.01.018 [DOI] [PubMed] [Google Scholar]
- 23.Harden RN, Bruehl S, Stanton-Hicks M, Wilson PR. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med. 2007;8(4):326–331. doi: 10.1111/j.1526-4637.2006.00169.x [DOI] [PubMed] [Google Scholar]
- 24.Hahn OS, Ahn JH, Song SH, et al. Development of Korean version of structured clinical interview schedule for DSM-IV axis I disorder: interrater reliability. J Korean Neuropsychiatr Assoc. 2000;39(2):362–372. [Google Scholar]
- 25.Han K, Lim J, Lee J, Min B, Moon K. Validation of the Korean MMPI-2 using the Korean normative sample. Paper presented at: 40th Annual Symposium on Recent Developments in the Use of the MMPI-2/MMPI-A, Fort Lauderdale, FL; 2005. [Google Scholar]
- 26.Beck AT, Steer RA, Brown GK. Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation. 1996;78(2). [Google Scholar]
- 27.Spielberger CD. State‐Trait anxiety inventory The Corsini Encyclopedia of Psychology. Hoboken, NJ: John Wiley & Sons, Inc.; 2010. [Google Scholar]
- 28.Pérez-Pareja J, Sesé A, González-Ordi H, Palmer A. Fibromyalgia and chronic pain: are there discriminating patterns by using the Minnesota Multiphasic Personality Inventory-2 (MMPI-2)? Int J Clin Health Psychol. 2010;10(1):41–56. [Google Scholar]
- 29.Naylor B, Boag S, Gustin SM. New evidence for a pain personality? A critical review of the last 120 years of pain and personality. Scand J Pain. 2017;17(1):58–67. doi: 10.1016/j.sjpain.2017.07.011 [DOI] [PubMed] [Google Scholar]
- 30.Simonds EC, Handel RW, Archer RP. Incremental validity of the Minnesota Multiphasic Personality Inventory–2 and symptom checklist–90 – revised with mental health inpatients. Assessment. 2008;15(1):78–86. doi: 10.1177/1073191107307529 [DOI] [PubMed] [Google Scholar]
- 31.Gormsen L, Rosenberg R, Bach FW, Jensen TS. Depression, anxiety, health‐related quality of life and pain in patients with chronic fibromyalgia and neuropathic pain. Eur J Pain. 2010;14(2):127.e121–127.e128. doi: 10.1016/j.ejpain.2009.03.010 [DOI] [PubMed] [Google Scholar]
- 32.Strigo I, Matthews S, Simmons A. Decreased frontal regulation during pain anticipation in unmedicated subjects with major depressive disorder. Transl Psychiatry. 2013;3(3):e239. doi: 10.1038/tp.2013.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barthas F, Sellmeijer J, Hugel S, Waltisperger E, Barrot M, Yalcin I. The anterior cingulate cortex is a critical hub for pain-induced depression. Biol Psychiatry. 2015;77(3):236–245. doi: 10.1016/j.biopsych.2014.08.004 [DOI] [PubMed] [Google Scholar]
- 34.Vural M, Berkol TD, Erdogdu Z, Kucukserat B, Aksoy C. Evaluation of personality profile in patients with fibromyalgia syndrome and healthy controls. Mod Rheumatol. 2014;24(5):823–828. doi: 10.3109/14397595.2013.868069 [DOI] [PubMed] [Google Scholar]
- 35.Margalit D, Har LB, Brill S, Vatine -J-J. Complex regional pain syndrome, alexithymia, and psychological distress. J Psychosom Res. 2014;77(4):273–277. doi: 10.1016/j.jpsychores.2014.07.005 [DOI] [PubMed] [Google Scholar]
- 36.Bruehl S. Complex regional pain syndrome. BMJ. 2015;351:h2730. doi: 10.1136/bmj.h2730 [DOI] [PubMed] [Google Scholar]
- 37.Lumley MA, Cohen JL, Borszcz GS, et al. Pain and emotion: a biopsychosocial review of recent research. J Clin Psychol. 2011;67(9):942–968. doi: 10.1002/jclp.v67.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Doan L, Manders T, Wang J. Neuroplasticity underlying the comorbidity of pain and depression. Neural Plast. 2015;2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alabas O, Tashani O, Tabasam G, Johnson M. Gender role affects experimental pain responses: a systematic review with meta‐analysis. Eur J Pain. 2012;16(9):1211–1223. doi: 10.1002/ejp.2012.16.issue-9 [DOI] [PubMed] [Google Scholar]
- 40.Racine M, Tousignant-Laflamme Y, Kloda LA, Dion D, Dupuis G, Choinière M. A systematic literature review of 10 years of research on sex/gender and pain perception – part 2: do biopsychosocial factors alter pain sensitivity differently in women and men? Pain. 2012;153(3):619–635. doi: 10.1016/j.pain.2011.11.026 [DOI] [PubMed] [Google Scholar]
- 41.Han K, Park HI, Weed NC, Lim J, Johnson A, Joles C. Gender differences on the MMPI across American and Korean adult and adolescent normative samples. J Pers Assess. 2013;95(2):197–206. doi: 10.1080/00223891.2012.754360 [DOI] [PubMed] [Google Scholar]
- 42.Novo R, Gonzalez B, Peres R, Aguiar P. A meta-analysis of studies with the minnesota multiphasic personality inventory in fibromyalgia patients. Pers Individ Dif. 2017;116:96–108. doi: 10.1016/j.paid.2017.04.026 [DOI] [Google Scholar]
- 43.Kato F, Abe T, Kanbara K, et al. Pain threshold reflects psychological traits in patients with chronic pain: a cross-sectional study. Biopsychosoc Med. 2017;11(1):13. doi: 10.1186/s13030-017-0098-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Haggard RA, Stowell AW, Bernstein D, Gatchel RJ. Relationship between the MMPI-2 and psychosocial measures in a heterogeneous pain population. Rehabil Psychol. 2008;53:471–478. doi: 10.1037/t15120-000. [DOI]
- 45.Marinus J, Moseley GL, Birklein F, et al. Clinical features and pathophysiology of complex regional pain syndrome. Lancet Neurol. 2011;10(7):637–648. doi: 10.1016/S1474-4422(11)70106-5 [DOI] [PMC free article] [PubMed] [Google Scholar]