Abstract
Hypoglossal nerve stimulation (HNS) is an increasingly widespread OSA treatment. It is a non-anatomical modifying surgery able to achieve an adequate objective and subjective result with a reasonable complication rate. HNS exploits the neurostimulation to reduce upper airway collapsibility providing a multilevel upper airway improvement within a single procedure. Proper patient selection has a fundamental role in determining an adequate long-term clinical outcome. All patient candidates for HNS undergo a standard comprehensive sleep medicine assessment and upper airway surgical examination. Several features should be assessed preoperatively in order to predict patients' response to HNS treatment. In particular, the assessment of OSA severity, BMI > 32 Kg/m2, collapse pattern during drug-induced sleep endoscopy (DISE), and many other parameters, is central for a good patient selection and customization of OSA treatment. HNS is indeed one of the most promising tools in the widespread context of personalized sleep medicine. HNS is an adjustable medical device that could be titrated in order to improve HNS effectiveness, maintaining patient comfort. Moreover, HNS provides the opportunity for patients to play an active role in their own care, with a potential improvement in therapy adherence and efficacy. This review summarizes the current evidence in patient selection for HNS, highlighting the reasons behind the optimistic future of this OSA treatment in the context of personalized medicine.
Keywords: obstructive sleep apnea, hypoglossal nerve, upper airway, stimulation, personalized medicine
Introduction
Obstructive sleep apnea (OSA) is probably the most common sleep breathing disorder in the adult population.1–3 The overall prevalence ranged from 9%4 to 38%5 in some cohorts, and it is expected to increase in the near future due to the recent spreading of obesity.6,7 The most used objective measure to quantify OSA severity is the number of apneas or hypopneas per hour (apnea hypopnea index, AHI) that the patients suffer during sleep. The repeated episodes of complete (apnea) or partial (hypopnea) upper airway obstruction determine a repeated oxygen desaturation and sleep fragmentation.8 As a consequence, moderate-severe OSA determines an increased cardiovascular risk in the long-term period, and it represents an independent risk factor for all-cause mortality.9 Moreover, this chronic condition is emerging as a major health problem due to productivity loss and healthcare-associated costs.10
First-line treatment for OSA patients is continuous positive airway pressure (CPAP) regardless of OSA severity. Alternative surgical approaches may be offered depending on the patient’s risk factors, anatomy and preferences. However, although CPAP is currently the standard for OSA treatment, the low adherence in the long-term period has driven the search for new treatment options.11,12
In this context, the Hypoglossal Nerve Stimulation (HNS), first described in 2001,13 represents one of the last surgical innovation. Traditional OSA surgical approaches seek to increase upper airway patency by removing redundant soft tissue, and modifying the anatomical structures involved in the obstruction. Although a similar functional result is obtained, HNS lead to an increased upper airway patency maintaining the physiological anatomical structures.14 In particular, HNS enhances the upper airway neuromuscular tone in order to reduce the collapsibility, which is thought to be the primary pathophysiological basis for OSA.15,16 Three different systems are now available in the market. The Inspire Medical System® (Inc., Maple Grove, MN) stimulates the genioglossus muscle fibers of the tongue thanks to the placement of the stimulation lead directly over the ending hypoglossal nerve fibers. On the other hand, the ImThera® system stimulates both tongue protrusors and retractors in order to stiffen the posterior aspect of the tongue and pharyngeal walls, thanks to the more proximal location of the electrodes. Recently, the new Genio™ system (Nyxoah SA, Mont-Saint-Guibert, Belgium) has recently obtained CE Mark approval (2019) after finishing successful clinical trials.17 Its principal difference is that the energy battery is placed outside of the body and the stimulator implant (SI) is designed to be placed in the chin area, like a “saddle on a horse” on the genioglossus muscle, in contact with both branches of the hypoglossal nerve with the advantage of bilateral nerve stimulation.
HNS provides a multilevel upper airway improvement within a single procedure, similarly to extensive multilevel demolitive surgery.18 Although it remains to be proven, the mechanical coupling of the tongue to the palate and pharyngeal walls would seem to allow a retro-palatal airway opening other than the more obvious retro-lingual improvement.19
In the last years, several prospective studies on HNS have been published, and a recent meta-analysis showed that this non-anatomical modifying surgery is able to achieve an adequate long-term objective and subjective clinical outcome with reasonable complication rate.20 Moreover, this new OSA treatment is getting more and more refined thanks to the device implementation, and a better establishment of patient selection and follow-up. The main drivers directly affecting the long-term clinical outcome are therefore the careful patient selection, the accurate placement of the stimulation electrodes during surgery, and the advanced titration therapy for muscle recruitment optimization. In particular, it was demonstrated that the refinement of the inclusion criteria is able to improve the clinical outcome, increasing the surgical success rate.21 Although HNS could be modulated post-operatively, the specific assessment of patients' pre-implantation characteristics is fundamental in order to better customize OSA management and choose the correct treatment.
The purpose of this paper is to review the pre-implantation patient selection process with particular interest in the specific predictors of HNS success. In addition, we seek to describe the promising relationship between HNS and the concept of personalized medicine, now increasingly central in OSA long-term management.
Patient Selection and Efficacy Predictors
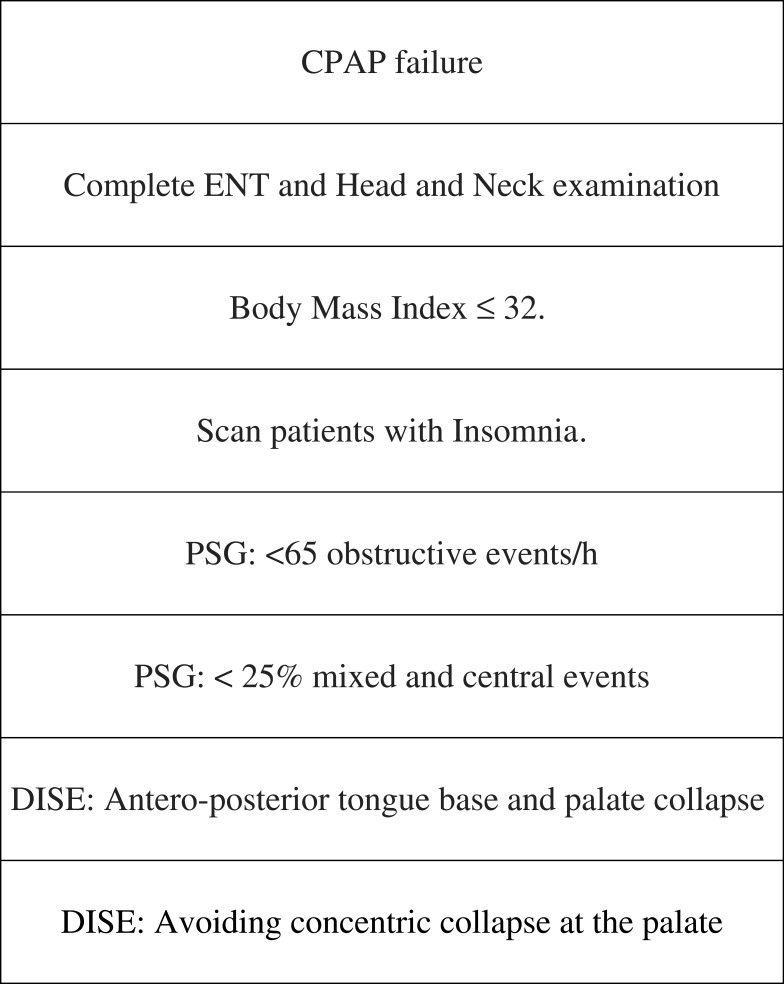
Pre-operative patient selection assumes a central role in OSA surgical management regardless of the surgical procedure (Figure 1). As a general rule, if patients are well selected and the procedures are carefully chosen, the clinical outcome could be outstanding and well tolerated in the long-term period. As already mentioned, the role of patients selection for HNS is highlighted by some feasibility studies performed with different stimulation systems. In particular, Van de Heyning et al21 implanted 20 patients with the Inspire Medical System® reporting a success rate of only 30%. Moreover, Friedman et al22 obtained a success rate of 35% in a cohort of 46 patients implanted with the ImThera® aura6000 system. If non-selected OSA patients undergo HNS, an important inter-individual difference in response to stimulation is detected.23 The reasons for HNS failure are as numerous. These are mostly related to wrong patient selection, other than inadequate placement of the stimulating electrode, having other sleep disorders like insomnia or psychological factors that do not allow for a correct establishment of the stimulating voltage of the device. Therefore, we must bear in mind that even though we might think we have the perfect candidate for HNS implantation, we might be surprised that the device does not work as well as expected. In these cases, the patient may require more counseling and follow-ups in order to better customize the treatment.
Figure 1.
“Optimum patient selection” for HNS.
All patient candidates for HNS undergo a standard comprehensive sleep medicine assessment and upper airway surgical examination. A complete evaluation of patient history, sleep comorbidities, systemic disorders, craniofacial and upper airway anatomy, and other confounding factors should be evaluated. In addition, an awake endoscopy and drug-induced sleep endoscopy (DISE) should be performed.
A definite prerequisite of patient candidate for HNS is CPAP intolerance (defined as CPAP usage lower than five nights per week-4 hrs per night) or the CPAP failure (AHI > 20 despite CPAP usage excluding central sleep apneas). In addition, some patients are unwilling to use CPAP and prefer another kind of treatment.24 Although HNS is often described as a surgical procedure for highly selected patients, the three major inclusion criteria indicated by the Food and Drug Administration (FDA) are moderate to severe OSA (AHI between 15 and 65), body mass index (BMI) <32 kg/m2, and absence of complete concentric collapse (CCC) at the soft palate level.25
Baseline AHI is a fundamental measure for OSA severity, and it should be taken into account when the treatment is chosen. The STAR trial26 used an AHI between 20 and 50 events per hour as an important inclusion criteria. Both the German Postmarket study27 and the Adhere Registry28 showed that OSA severity measured by baseline AHI is not a predictor of therapy response. If Sher criteria29 (50% reduction in AHI and overall AHI < 20) is used to define treatment response, an elevated AHI (more than 65) is not a HNS contraindication considering the reported treatment success in several studies, leading to a potential benefit for some patients with particularly severe disease.30,31 On the other hand, also patients suffering from mild OSA could potentially benefit from HNS,31 while some issues related to the invasiveness of the implanted device and the related patient discomfort should be taken into account to avoid patients' overtreatment. Moreover, HNS represents an expensive treatment with a cost of approximately 30.000 dollars per patient. As a consequence, this could raise some concerns about the treatment of patients suffering from mild OSA. On the other hand, HNS cost is certainly higher than that of other OSA treatments such as CPAP or oral appliances, but if these devices are not well tolerated, and no clinical improvement is obtained, the economic perspective assumes secondary importance.
An elevated BMI is known to be a negative predictor for any kind of OSA treatment,32–34 other than a risk factor for OSA development.2 A retrospective case-control study35 of 153 patients analyzed the predictive value of a BMI > 32 Kg/m2. It demonstrated that HNS is a safe and effective procedure also for higher-BMI group, obtaining comparable clinical outcome in the two cohorts. On the contrary, the Adhere Registry study highlighted a 8.5% reduced odds of treatment success for each unit increase in BMI.28 Although further data are needed to clarify this incongruence, it seems that BMI > 32 Kg/m2 represents only an indirect predictor of HNS response.36 The positive correlation between BMI and the probability of complete concentric palatal collapse has been described.37 As a consequence, if a CCC is excluded during DISE, a higher BMI has a low impact on HNS success. In particular, also patients with a BMI > 35 Kg/m2 can present a good clinical outcome if carefully selected in highly specialized centers.38
Drug-induced sleep endoscopy (DISE) is currently an essential diagnostic tool able to identify the specific site of collapse (eg, retro-palatal, retro-lingual), the pattern (concentric, anteroposterior, lateral), and the degree (complete, partial) of the obstruction.39 Moreover, DISE could be safely performed in CPAP-intolerant patients considering the almost absence of adverse events.40 During the pre-operative patient assessment, DISE is extremely useful to rule out a complete concentric collapse (CCC) at the level of the velum, probably the strongest contraindication to HNS.23,40 Furthermore, this obstruction pattern is extremely common with a prevalence of 20% to 25% in OSA patients with CPAP intolerance that are potential candidates for HNS.41 In these cases, although the other criteria allow for the device implantation, the anatomical pattern of collapse predicts the high risk of treatment failure, and these patients are excluded during DISE examination.
Patient age was not considered an exclusion criteria in clinical studies that included adults, and it seems to be not correlated with HNS failure.42 There was no difference between responders and non-responders in the German Post market study according to patients’ age (odds ratio = 0.992).43 A retrospective case-control study44 showed that patients (matched for AHI and BMI) older than 65 years presented a similar surgical success rate compared to the younger counterpart, in spite of significantly higher comorbidities. Accordingly, the Adhere Registry data36 (including 382 patients at 1 year follow-up) showed that higher age is not a predictor of HNS ineffectiveness. In particular, AHI reduction was higher in patients older than 65 years when compared to younger patients.45 These results are not fully understood, but they could partially be due to the higher adherence detected in the older population,44–46 that balance the unfavorable anatomy of these patients cohort.47,48 In addition, we highlight that several studies reporting the HNS application in children suffering from Down Syndrome have been recently published with promising results.49,50 OSA represents an important comorbidity for this population, and hopefully the device will be approved by the FDA for children in the near future.51
At present, previous OSA surgery seems to not represent a predictor of HNS response. Although a stratified analysis in the German Postmarket study revealed that a previous uvulopalatopharyngoplasty (UPPP) is associated with higher risk of being non-responders,43 but as more patients have been included this tendency has not been observed.52 A retrospective study showed that prior palatal surgery do not influence HNS clinical outcome.53,54 Another retrospective analysis found no indication for patients to routinely undergo UPPP before HNS, while palatal surgery could be suggested in case of non-adequate response to HNS after the implantation.55 Accordingly, a recent study based on the Adhere Registry data (n = 299) showed that previous surgery is not associated with HNS outcomes.52
In addition to previously described predictors, frequently used exclusion criteria are: more than 25% of central sleep apneas; positional OSA (>50% reduction in AHI between supine and non-supine positions); tonsil size greater than type 2; tongue malformations; alteration of tongue motor activity; marked salivation disorders; neuromuscular disease; hypoglossal-nerve palsy; active psychiatric disease; other non-respiratory sleep disorders; pregnancy; major systemic disorder; requirement of magnetic resonance imaging. The presence of another implantable device was usually considered an exclusion criteria in clinical studies due to the possibility of unintended interaction with the hypoglossal nerve stimulator. A recent feasibility study with fourteen patients showed that the simultaneous use of HNS (Inspire Medical System®) with transvenous Cardiac Implantable Electronic Devices (CIED) could be safe, effective and without any device–device interactions.56 Another comorbidity that should be considered during patient selection is insomnia. It has been described that 39–58% of OSA patients suffer from co-morbid insomnia and sleep apnea (COMISA).57 The coexistence of this condition is strictly related to reduced CPAP tolerance with a resultant reduced therapy adherence.58,59 As a consequence, insomnia treatment leads to an increased acceptance and use of CPAP therapy with a great benefit in the long-term period.60,61 At this time, there are no studies assessing the role of insomnia in HNS. However, it could be suspected that patients suffering from COMISA are prone to a low HNS usage. In particular, the nerve stimulation might worsen patient’s insomnia due to arousals that might be produced by tongue movements, as already shown by the Adhere Registry study that detected insomnia due to HNS in the 5% of the patients post-operatively.28 On the other hand, we have to consider that HNS titration aims to reduce arousal events, as demonstrated by the significant reduction of the arousal index at the STAR trial 5 years follow-up (27.8 ± 11.7 to 7.8 ± 9.7 events per hour).62 Although we do not currently have data quantifying the influence of insomnia in HNS compliance and usage, it is advisable to screen insomnia during HNS patient selection, and to treat this comorbidity with cognitive and behavioral therapy in order to increase long-term therapy adherence.63
Finally, although the surgical selection criteria previously described should be used in order to obtain the desired clinical outcome, the psychological component represents an important factor able to affect the surgical success rate. A pre-operative assessment of patient’s motivation should be carried out in order to predict therapy adherence and facilitate the implantation and the titration processes. In particular, patients counseling on surgical procedure, post-operative titration and expectations of therapy outcomes assumes a central role in patients’ selection for HNS.30
Hypoglossal Nerve Stimulation in the Era of Precision Medicine
In the last years, the term “precision medicine” has become widespread in several health fields and medical specialties.64–66 It is based on the fundamental concept that all individuals with the same disorder are not the same, because several factors (genetic, epigenetic, environment, etc.) contribute to each patient phenotype.67 This is particularly true for OSA patients according to several cohort studies that showed various physiologic and clinical patients' subtypes.68–70 From this perspective, OSA patients are characterized by different pathophysiological mechanisms, clinical manifestations, and different therapy response, and we should take account of these differences in our clinical practice.71,72 The possibility to distinguish different clinical phenotypes will allow to obtain a customized OSA patient management. In particular, a better understanding of a multi-level phenotypic characterization could help to determine the risk of future complications and response to different treatment options. Symptoms, polysomnographic data, airway collapse pattern, and comorbidity could, indeed, assist our clinical practice leading to an improved treatment success rate.72 The evaluation of OSA patients can no longer depend only on AHI and oxygen desaturation index (ODI) quantification.
In the context of a customized management for OSA patients, the HNS represents one of the most promising tools. The relationship between personalized medicine and HNS has become clear from different perspectives. As already outlined above, several inclusion criteria used in clinical studies are not predictors of HNS success. Only the identification of CCC during DISE seems to be an useful tool during preoperative patient selection. Although HNS success rate is promising and comparable to other accepted surgical approaches (such as UPPP or modified-UPPP), almost one third of patients are considered as a non-responder in the long-term period.20 The reason why these patients do not benefit from HNS is currently unknown. On the other hand, some patients outside baseline inclusion parameters showed an optimal clinical response.31 This clinical scenario should lead us to realize that OSA treatment could not be chosen on the basis of predetermined indications, while each patient should be assessed independently, trying to customize disease management based on several clinical aspects. HNS success is strictly dependent on a set of small factors that alone can greatly influence the clinical outcome. This is particularly true for patients' follow-up other than pre-operative selection. Although an adequate pre-operative evaluation of these patients is needed to ensure an optimal post-operative clinical outcome, the post-operative care and, in particular, the device titration has a central role in the long-term period. The follow-up of these patients has important differences compared to other OSA surgical procedure, because it extremely influences HNS long-term clinical outcome, and it could be provided in highly specialized centers with a relevant experience with this procedure.30,73
One of the fundamental advantages of HNS is that of being an adjustable medical device. Several stimulation parameters (stimulation amplitude, configuration, etc.) can be titrated in the clinical or sleep laboratory setting in order to improve HNS effectiveness, and patients' comfort. In particular, advanced titration of HNS therapy could even convert an initial non-responder into a responder in some cases.18,19 Based on the concept of personalized medicine, an adequate patient selection will lead to a proper clinical outcome only if it is supported by proper patient follow-up. We must bear in mind that OSA is a chronic condition with unavoidable long-term patient evolution that requires a longitudinal care model. Patients' follow-up should not be reduced only to a post-operative PSG assessment as usual after OSA surgical treatment. All patients should be followed through a strict protocol after HNS implantation in order to achieve a long-term clinical benefit. It could be necessary to periodically perform titration, especially during the first-year post-implantation, depending on PSG data or patient symptoms and comfort. We have to consider that HNS titration aim is to balance patient device tolerability (in order to improve therapy adherence and sleep quality) with the best PSG values reasonably achievable. As a consequence, a single night measurement could not determine AHI final outcome because some patients need to get accustomed to the device. During an in-laboratory sleep study, the device is adjusted until respiratory abnormalities are eliminated. An external programming device controlled by the physician, and composed of a tablet computer and a telemetry unit, customizes HNS settings in order to optimize OSA control and patient comfort. HNS parameters that are identified as best for the individual patient are then configured in a narrow range that could be modulated by the patient through a remote control at home. Moreover, the patient possibility to modulate these parameters (eg, voltage) within a preset range is perfectly integrated in the context of personalized medicine. HNS provides the opportunity for patients to play an active role in their own care, with a potential improvement in therapy adherence and treatment efficacy which is still to be quantified.74 Patient involvement is taking a central role in OSA management both in treatment choice24 and assessment of treatment response.75,76 In the clinical setting, some patients are satisfied with their clinical improvement, while the PSG data indicate treatment failure and classify these patients as non-responders. Although the patient may not obtain a complete improvement of the AHI, there is a justification for the implant if the quality-of-life parameters improves in the long-term period. As already mentioned, we know that we cannot base our success exclusively on the AHI, although this is the primary outcome parameter at this moment. An improvement in other features such as better sleep quality, lower glucose levels, lower blood pressure, is able to make patients feel better and happy.
In the case of a device-based treatment (eg, CPAP or HNS), the patients' compliance and device usage represents an important parameter that could assess patient satisfaction from an objective perspective.77 The possibility to quantify HNS adherence and the related patients' compliance through a remote control during the follow-up represents an indirect measure of patient satisfaction.78 Moreover, it was demonstrated that providing objective adherence data to patients with OSA could enhance treatment compliance.79
Future Developments: Transcutaneous Nerve Stimulation
Another modality of nerve stimulation proposed for OSA treatment is the transcutaneous approach (TESLA).80 This kind of stimulation is less invasive in respect to the classic HNS. In particular, transcutaneous patches are placed in the submental area in order to directly stimulate the genioglossus muscle and increase upper airway patency. No surgical approach is needed, and the stimulation intensity could be calibrated in order to reduce the risk of arousals from sleep. In 2016, Pengo et al81 published the first randomized sham-controlled trial (TESLA trial) that proved the efficacy and tolerability of the treatment. An ongoing domiciliary feasibility study (TESLA home, NCT03160456) is designed in order to quantify both clinical efficacy and therapy adherence during a three months follow-up period. Patients' selection criteria are similar to that used for HNS. Normal weight or mildly obese patients (BMI < 32 kg/m2), with an antero-posterior pharyngeal collapse during DISE, are the “classic” responders to this therapy. On the other hand, patients suffering from severe OSA, with a multi-level or concentric upper airway collapse and severe obesity, are usually excluded from clinical trials due to the elevated risk of treatment failure.82 Although some contradictory results have been published in the past, the last evidences are promising in terms of treatment efficacy and tolerability.83 In the future, new technical advances and the device refinement are expected in order to better define the role of the transcutaneous stimulation in the treatment of OSA.
Summary
HNS is a promising OSA treatment that differs from previous surgical approaches. Pre-operative patient selection is the first step to achieve a proper clinical outcome. Although HNS is currently performed in highly selected patients, several baseline parameters seem to be not related to the post-operative outcome. According to existing data, the patients’ age, BMI, pre-implantation AHI, and previous surgeries are not directly involved in HNS success and could not be considered as useful predictors during the selection process. At this moment, the strongest contraindication to HNS is the complete concentric collapse of the soft palate detected during DISE, which is an essential assessment tool for pre-operative patient selection. In the era of “precision medicine”, the decision to perform HNS in patients suffering from moderate to severe OSA is definitely dependent on numerous factors. In this context, the most promising HNS feature is the longitudinal care model that could be provided through strict patient follow-up and device titration. The possibility to modulate HNS parameters after the implantation leads to a customized OSA management, as requested by the increasingly widespread “precision medicine”. Moreover, the participatory role of patients in their own care is consistent with the technology that is now available in sleep medicine, that will optimistically improve patients' compliance and clinical outcomes in the near future.
Funding Statement
This study received no funding.
Disclosure
All authors declare that they have no conflicts of interest.
References
- 1.Garvey JF, Pengo MF, Drakatos P, Kent BD. Epidemiological aspects of obstructive sleep apnea. J Thorac Dis. 2015;7(5):920–929. doi: 10.3978/j.issn.2072-1439.2015.04.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Senaratna CV, Perret JL, Lodge CJ, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81. doi: 10.1016/j.smrv.2016.07.002 [DOI] [PubMed] [Google Scholar]
- 3.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):136–143. doi: 10.1513/pats.200709-155MG [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma SK, Reddy EV, Sharma A, et al. Prevalence and risk factors of syndrome Z in urban Indians. Sleep Med. 2010;11(6):562–568. doi: 10.1016/j.sleep.2010.02.008 [DOI] [PubMed] [Google Scholar]
- 5.Tufik S, Santos-Silva R, Taddei JA, Bittencourt LRA. Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med. 2010;11(5):441–446. doi: 10.1016/j.sleep.2009.10.005 [DOI] [PubMed] [Google Scholar]
- 6.Report of a WHO consultation. Obesity: Preventing and Managing the Global Epidemic, Vol. 894 World Health Organ Tech Rep Ser; 2000:i–xii,1–253. [PubMed] [Google Scholar]
- 7.Twells LK, Gregory DM, Reddigan J, Midodzi WK. Current and predicted prevalence of obesity in Canada: a trend analysis. CMAJ Open. 2014;2(1):E18–E26. doi: 10.9778/cmajo.20130016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Strollo PJ, Rogers RM. Obstructive sleep apnea. N Engl J Med. 1996;334(2):99–104. doi: 10.1056/NEJM199601113340207 [DOI] [PubMed] [Google Scholar]
- 9.Marshall NS, Wong KKH, Cullen SRJ, Knuiman MW, Grunstein RR. Sleep apnea and 20-year follow-up for all-cause mortality, stroke, and cancer incidence and mortality in the Busselton Health Study cohort. J Clin Sleep Med. 2014;10(4):355–362. doi: 10.5664/jcsm.3600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chiner E, Andreu AL, Sancho-Chust JN, Sánchez-de-la-Torre A, Barbé F. The use of ambulatory strategies for the diagnosis and treatment of obstructive sleep apnea in adults. Expert Rev Respir Med. 2013;7(3):259–273. doi: 10.1586/ers.13.19 [DOI] [PubMed] [Google Scholar]
- 11.Rotenberg BW, Murariu D, Pang KP. Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg. 2016;45(1):43. doi: 10.1186/s40463-016-0156-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173–178. doi: 10.1513/pats.200708-119MG [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwartz AR, Bennett ML, Smith PL, et al. Therapeutic electrical stimulation of the hypoglossal nerve in obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 2001;127(10):1216–1223. doi: 10.1001/archotol.127.10.1216 [DOI] [PubMed] [Google Scholar]
- 14.Soose RJ, Gillespie MB. Upper airway stimulation therapy: a novel approach to managing obstructive sleep apnea. Laryngoscope. 2016;126(Suppl 7):S5–S8. doi: 10.1002/lary.26258 [DOI] [PubMed] [Google Scholar]
- 15.McGinley BM, Schwartz AR, Schneider H, Kirkness JP, Smith PL, Patil SP. Upper airway neuromuscular compensation during sleep is defective in obstructive sleep apnea. J Appl Physiol. 2008;105(1):197–205. doi: 10.1152/japplphysiol.01214.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patil SP, Schneider H, Marx JJ, Gladmon E, Schwartz AR, Smith PL. Neuromechanical control of upper airway patency during sleep. J Appl Physiol. 2007;102(2):547–556. doi: 10.1152/japplphysiol.00282.2006 [DOI] [PubMed] [Google Scholar]
- 17.Eastwood PR, Barnes M, MacKay SG, et al. Bilateral hypoglossal nerve stimulation for treatment of adult obstructive sleep apnoea. Eur Respir J. 2020;55(1):1901320. doi: 10.1183/13993003.01320-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heiser C, Maurer JT, Steffen A. Functional outcome of tongue motions with selective hypoglossal nerve stimulation in patients with obstructive sleep apnea. Sleep Breath. 2016;20(2):553–560. doi: 10.1007/s11325-015-1237-4 [DOI] [PubMed] [Google Scholar]
- 19.Heiser C, Edenharter G, Bas M, Wirth M, Hofauer B. Palatoglossus coupling in selective upper airway stimulation. Laryngoscope. 2017;127(10):E378–E383. doi: 10.1002/lary.26487 [DOI] [PubMed] [Google Scholar]
- 20.Costantino A, Rinaldi V, Moffa A, et al. Hypoglossal nerve stimulation long-term clinical outcomes: a systematic review and meta-analysis. Sleep Breath. Epub 2019 Aug 15. doi: 10.1007/s11325-019-01923-2 [DOI] [PubMed] [Google Scholar]
- 21.Van de Heyning PH, Badr MS, Baskin JZ, et al. Implanted upper airway stimulation device for obstructive sleep apnea. Laryngoscope. 2012;122(7):1626–1633. doi: 10.1002/lary.23301 [DOI] [PubMed] [Google Scholar]
- 22.Friedman M, Jacobowitz O, Hwang MS, et al. Targeted hypoglossal nerve stimulation for the treatment of obstructive sleep apnea: six-month results. Laryngoscope. 2016;126(11):2618–2623. doi: 10.1002/lary.25909 [DOI] [PubMed] [Google Scholar]
- 23.Vanderveken OM, Maurer JT, Hohenhorst W, et al. Evaluation of drug-induced sleep endoscopy as a patient selection tool for implanted upper airway stimulation for obstructive sleep apnea. J Clin Sleep Med. 2013;9(5):433–438. doi: 10.5664/jcsm.2658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liao W-J, Song L-J, Yi H-L, et al. Treatment choice by patients with obstructive sleep apnea: data from two centers in China. J Thorac Dis. 2018;10(3):1941–1950. doi: 10.21037/jtd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strohl MM, Yamauchi M, Peng Z, Strohl KP. Insights since FDA approval of hypoglossal nerve stimulation for the treatment of obstructive sleep apnea. Curr Sleep Med Rep. 2017;3(3):133–141. doi: 10.1007/s40675-017-0088-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Strollo PJ, Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139–149. doi: 10.1056/NEJMoa1308659 [DOI] [PubMed] [Google Scholar]
- 27.Heiser C, Maurer JT, Hofauer B, Sommer JU, Seitz A, Steffen A. Outcomes of upper airway stimulation for obstructive sleep apnea in a multicenter German Postmarket Study. Otolaryngol Head Neck Surg. 2017;156(2):378–384. doi: 10.1177/0194599816683378 [DOI] [PubMed] [Google Scholar]
- 28.Thaler E, Schwab R, Maurer J, et al. Results of the ADHERE upper airway stimulation registry and predictors of therapy efficacy. Laryngoscope. Epub 2019 Sep 14. doi: 10.1002/lary.28286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sher AE, Schechtman KB, Piccirillo JF. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep. 1996;19(2):156–177. doi: 10.1093/sleep/19.2.156 [DOI] [PubMed] [Google Scholar]
- 30.Thaler ER, Schwab RJ. Single-institution experience and learning curve with upper airway stimulation. Laryngoscope. 2016;126(Suppl 7):S17–S19. doi: 10.1002/lary.26178 [DOI] [PubMed] [Google Scholar]
- 31.Sarber KM, Chang KW, Ishman SL, Epperson MV, Dhanda Patil R. Hypoglossal nerve stimulator outcomes for patients outside the U.S. FDA recommendations. Laryngoscope. Epub 2019 Jul 10. doi: 10.1002/lary.28175 [DOI] [PubMed] [Google Scholar]
- 32.Miljeteig H, Hoffstein V. Determinants of continuous positive airway pressure level for treatment of obstructive sleep apnea. Am Rev Respir Dis. 1993;147(6 Pt 1):1526–1530. doi: 10.1164/ajrccm/147.6_Pt_1.1526 [DOI] [PubMed] [Google Scholar]
- 33.Vicente E, Marín JM, Carrizo S, Naya MJ. Tongue-base suspension in conjunction with uvulopalatopharyngoplasty for treatment of severe obstructive sleep apnea: long-term follow-up results. Laryngoscope. 2006;116(7):1223–1227. doi: 10.1097/01.mlg.0000224498.09015.d9 [DOI] [PubMed] [Google Scholar]
- 34.Camacho M, Liu SY, Certal V, Capasso R, Powell NB, Riley RW. Large maxillomandibular advancements for obstructive sleep apnea: an operative technique evolved over 30 years. J Craniomaxillofac Surg. 2015;43(7):1113–1118. doi: 10.1016/j.jcms.2015.05.015 [DOI] [PubMed] [Google Scholar]
- 35.Huntley C, Steffen A, Doghramji K, Hofauer B, Heiser C, Boon M. Upper airway stimulation in patients with obstructive sleep apnea and an elevated body mass index: a multi-institutional review. Laryngoscope. 2018;128(10):2425–2428. doi: 10.1002/lary.27426 [DOI] [PubMed] [Google Scholar]
- 36.Steffen A. What makes the responder to upper airway stimulation in obstructive sleep apnea patients with positive airway pressure failure? J Thorac Dis. 2018;10(Suppl 26):S3131–S3134. doi: 10.21037/jtd.2018.07.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vroegop AV, Vanderveken OM, Boudewyns AN, et al. Drug-induced sleep endoscopy in sleep-disordered breathing: report on 1249 cases. Laryngoscope. 2014;124(3):797–802. doi: 10.1002/lary.24479 [DOI] [PubMed] [Google Scholar]
- 38.Heiser C, Knopf A, Bas M, Gahleitner C, Hofauer B. Selective upper airway stimulation for obstructive sleep apnea: a single center clinical experience. Eur Arch Otorhinolaryngol. 2017;274(3):1727–1734. doi: 10.1007/s00405-016-4297-6 [DOI] [PubMed] [Google Scholar]
- 39.De Vito A, Carrasco Llatas M, Ravesloot MJ, et al. European position paper on drug-induced sleep endoscopy: 2017 update. Clin Otolaryngol. 2018;43(6):1541–1552. doi: 10.1111/coa.13213 [DOI] [PubMed] [Google Scholar]
- 40.Ong AA, Murphey AW, Nguyen SA, et al. Efficacy of upper airway stimulation on collapse patterns observed during drug-induced sedation endoscopy. Otolaryngol Head Neck Surg. 2016;154(5):970–977. doi: 10.1177/0194599816636835 [DOI] [PubMed] [Google Scholar]
- 41.Steffen A, Frenzel H, Wollenberg B, König IR. Patient selection for upper airway stimulation: is concentric collapse in sleep endoscopy predictable? Sleep Breath. 2015;19(4):1373–1376. doi: 10.1007/s11325-015-1277-9 [DOI] [PubMed] [Google Scholar]
- 42.Heiser C, Hofauer B. Predictive success factors in selective upper airway stimulation. ORL J Otorhinolaryngol Relat Spec. 2017;79(1–2):121–128. doi: 10.1159/000455728 [DOI] [PubMed] [Google Scholar]
- 43.Steffen A, Sommer JU, Hofauer B, Maurer JT, Hasselbacher K, Heiser C. Outcome after one year of upper airway stimulation for obstructive sleep apnea in a multicenter German post-market study. Laryngoscope. 2018;128(2):509–515. doi: 10.1002/lary.26688 [DOI] [PubMed] [Google Scholar]
- 44.Zhu Z, Hofauer B, Wirth M, et al. Selective upper airway stimulation in older patients. Respir Med. 2018;140:77–81. doi: 10.1016/j.rmed.2018.06.002 [DOI] [PubMed] [Google Scholar]
- 45.Withrow K, Evans S, Harwick J, Kezirian E, Strollo P. Upper airway stimulation response in older adults with moderate to severe obstructive sleep apnea. Otolaryngol Head Neck Surg. 2019;161(4):714–719. doi: 10.1177/0194599819848709 [DOI] [PubMed] [Google Scholar]
- 46.Heiser C, Steffen A, Boon M, et al. Post-approval upper airway stimulation predictors of treatment effectiveness in the ADHERE registry. Eur Respir J. 2019;53(1):1801405. doi: 10.1183/13993003.01405-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fei T, Polacco RC, Hori SE, et al. Age-related differences in tongue-palate pressures for strength and swallowing tasks. Dysphagia. 2013;28(4):575–581. doi: 10.1007/s00455-013-9469-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Irvine LE, Yang Z, Kezirian EJ, Nimni ME, Han B. Hyoepiglottic ligament collagen and elastin fiber composition and changes associated with aging. Laryngoscope. 2018;128(5):1245–1248. doi: 10.1002/lary.27094 [DOI] [PubMed] [Google Scholar]
- 49.Diercks GR, Wentland C, Keamy D, et al. Hypoglossal nerve stimulation in adolescents with down syndrome and obstructive sleep apnea. JAMA Otolaryngol Head Neck Surg. 2018;144(1):37–42. doi: 10.1001/jamaoto.2017.1871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Caloway CL, Diercks GR, Keamy D, et al. Update on hypoglossal nerve stimulation in children with down syndrome and obstructive sleep apnea. Laryngoscope. Epub 2019 Jun 20. doi: 10.1002/lary.28138 [DOI] [PubMed] [Google Scholar]
- 51.Ishman SL, Chang KW, Kennedy AA. Techniques for evaluation and management of tongue-base obstruction in pediatric obstructive sleep apnea. Curr Opin Otolaryngol Head Neck Surg. 2018;26(6):409–416. doi: 10.1097/MOO.0000000000000489 [DOI] [PubMed] [Google Scholar]
- 52.Kezirian EJ, Heiser C, Steffen A, et al. Previous surgery and hypoglossal nerve stimulation for obstructive sleep apnea. Otolaryngol Head Neck Surg. 2019;161(5):897–903. doi: 10.1177/0194599819856339 [DOI] [PubMed] [Google Scholar]
- 53.Huntley C, Vasconcellos A, Doghramji K, Hofauer B, Heiser C, Boon M. Upper airway stimulation in patients who have undergone unsuccessful prior palate surgery: an initial evaluation. Otolaryngol Head Neck Surg. 2018;159(5):938–940. doi: 10.1177/0194599818792191 [DOI] [PubMed] [Google Scholar]
- 54.Mahmoud AF, Thaler ER. Upper airway stimulation therapy and prior airway surgery for obstructive sleep apnea. Laryngoscope. 2018;128(6):1486–1489. doi: 10.1002/lary.26956 [DOI] [PubMed] [Google Scholar]
- 55.Steffen A, Abrams N, Suurna MV, Wollenberg B, Hasselbacher K. Upper-airway stimulation before, after, or without uvulopalatopharyngoplasty: a two-year perspective. Laryngoscope. 2018;129(2):514–518. doi: 10.1002/lary.27357 [DOI] [PubMed] [Google Scholar]
- 56.Parikh V, Thaler E, Kato M, et al. Early feasibility of hypoglossal nerve upper airway stimulator in patients with cardiac implantable electronic devices and continuous positive airway pressure-intolerant severe obstructive sleep apnea. Heart Rhythm. 2018;15(8):1165–1170. doi: 10.1016/j.hrthm.2018.04.016 [DOI] [PubMed] [Google Scholar]
- 57.Luyster FS, Buysse DJ, Strollo PJ. Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med. 2010;6(2):196–204. doi: 10.5664/jcsm.27772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wickwire EM, Smith MT, Birnbaum S, Collop NA. Sleep maintenance insomnia complaints predict poor CPAP adherence: a clinical case series. Sleep Med. 2010;11(8):772–776. doi: 10.1016/j.sleep.2010.03.012 [DOI] [PubMed] [Google Scholar]
- 59.Pieh C, Bach M, Popp R, et al. Insomnia symptoms influence CPAP compliance. Sleep Breath. 2013;17(1):99–104. doi: 10.1007/s11325-012-0655-9 [DOI] [PubMed] [Google Scholar]
- 60.Lichstein KL, Justin Thomas S, Woosley JA, Geyer JD. Co-occurring insomnia and obstructive sleep apnea. Sleep Med. 2013;14(9):824–829. doi: 10.1016/j.sleep.2013.02.008 [DOI] [PubMed] [Google Scholar]
- 61.Sweetman AM, Lack LC, Catcheside PG, et al. Developing a successful treatment for co-morbid insomnia and sleep apnoea. Sleep Med Rev. 2017;33:28–38. doi: 10.1016/j.smrv.2016.04.004 [DOI] [PubMed] [Google Scholar]
- 62.Woodson BT, Strohl KP, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: 5-year outcomes. Otolaryngol Head Neck Surg. 2018;159(1):194–202. doi: 10.1177/0194599818762383 [DOI] [PubMed] [Google Scholar]
- 63.Sweetman A, Lack L, Catcheside PG, et al. Cognitive and behavioral therapy for insomnia increases the use of continuous positive airway pressure therapy in obstructive sleep apnea participants with co-morbid insomnia: a randomized clinical trial. Sleep. 2019;42(12):zsz178. doi: 10.1093/sleep/zsz178 [DOI] [PubMed] [Google Scholar]
- 64.Hamburg MA, Collins FS. The path to personalized medicine. N Engl J Med. 2010;363(4):301–304. doi: 10.1056/NEJMp1006304 [DOI] [PubMed] [Google Scholar]
- 65.Rubin MA. Health: make precision medicine work for cancer care. Nature. 2015;520(7547):290–291. doi: 10.1038/520290a [DOI] [PubMed] [Google Scholar]
- 66.Khoury MJ. Planning for the future of epidemiology in the era of big data and precision medicine. Am J Epidemiol. 2015;182(12):977–979. doi: 10.1093/aje/kwv228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.König IR, Fuchs O, Hansen G, von Mutius E, Kopp MV. What is precision medicine? Eur Respir J. 2017;50:4. doi: 10.1183/13993003.00391-2017 [DOI] [PubMed] [Google Scholar]
- 68.Ye L, Pien GW, Ratcliffe SJ, et al. The different clinical faces of obstructive sleep apnoea: a cluster analysis. Eur Respir J. 2014;44(6):1600–1607. doi: 10.1183/09031936.00032314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kim J, Keenan BT, Lim DC, Lee SK, Pack AI, Shin C. Symptom-based subgroups of Koreans with obstructive sleep apnea. J Clin Sleep Med. 2018;14(3):437–443. doi: 10.5664/jcsm.6994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Keenan BT, Kim J, Singh B, et al. Recognizable clinical subtypes of obstructive sleep apnea across international sleep centers: a cluster analysis. Sleep. 2018;41(3). doi: 10.1093/sleep/zsx214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pien GW, Ye L, Keenan BT, et al. Changing faces of obstructive sleep apnea: treatment effects by cluster designation in the icelandic sleep apnea cohort. Sleep. 2018;41(3). doi: 10.1093/sleep/zsx201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zinchuk AV, Gentry MJ, Concato J, Yaggi HK. Phenotypes in obstructive sleep apnea: a definition, examples and evolution of approaches. Sleep Med Rev. 2017;35:113–123. doi: 10.1016/j.smrv.2016.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Murphey AW, Baker AB, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: the surgical learning curve. Laryngoscope. 2016;126(2):501–506. doi: 10.1002/lary.25537 [DOI] [PubMed] [Google Scholar]
- 74.Pack AI. Further development of P4 approach to obstructive sleep apnea. Sleep Med Clin. 2019;14(3):379–389. doi: 10.1016/j.jsmc.2019.05.004 [DOI] [PubMed] [Google Scholar]
- 75.Lim JH, Park P, Wee JH, et al. Evaluation of the success of obstructive sleep apnea surgery using criteria based on long-term symptoms and incident hypertension. Eur Arch Otorhinolaryngol. 2018;275(4):1015–1022. doi: 10.1007/s00405-018-4894-7 [DOI] [PubMed] [Google Scholar]
- 76.Goh YH, Mark I, Fee WE. Quality of life 17 to 20 years after uvulopalatopharyngoplasty. Laryngoscope. 2007;117(3):503–506. doi: 10.1097/MLG.0b013e31802d83bd [DOI] [PubMed] [Google Scholar]
- 77.Broström A, Ulander M, Nilsen P, Svanborg E, Arestedt KF. The attitudes to CPAP treatment inventory: development and initial validation of a new tool for measuring attitudes to CPAP treatment. J Sleep Res. 2011;20(3):460–471. doi: 10.1111/jsr.2011.20.issue-3 [DOI] [PubMed] [Google Scholar]
- 78.Hofauer B, Steffen A, Knopf A, Hasselbacher K, Heiser C. Patient experience with upper airway stimulation in the treatment of obstructive sleep apnea. Sleep Breath. 2019;23(1):235–241. doi: 10.1007/s11325-018-1689-4 [DOI] [PubMed] [Google Scholar]
- 79.Kuna ST, Shuttleworth D, Chi L, et al. Web-based access to positive airway pressure usage with or without an initial financial incentive improves treatment use in patients with obstructive sleep apnea. Sleep. 2015;38(8):1229–1236. doi: 10.5665/sleep.4898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pengo MF, Steier J. Emerging technology: electrical stimulation in obstructive sleep apnoea. J Thorac Dis. 2015;7(8):1286–1297. doi: 10.3978/j.issn.2072-1439.2014.04.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pengo MF, Xiao S, Ratneswaran C, et al. Randomised sham-controlled trial of transcutaneous electrical stimulation in obstructive sleep apnoea. Thorax. 2016;71(10):923–931. doi: 10.1136/thoraxjnl-2016-208691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.He B, Al-Sherif M, Nido M, et al. Domiciliary use of transcutaneous electrical stimulation for patients with obstructive sleep apnoea: a conceptual framework for the TESLA home programme. J Thorac Dis. 2019;11(5):2153–2164. doi: 10.21037/jtd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bisogni V, Pengo MF, De Vito A, et al. Electrical stimulation for the treatment of obstructive sleep apnoea: a review of the evidence. Expert Rev Respir Med. 2017;11(9):711–720. doi: 10.1080/17476348.2017.1358619 [DOI] [PubMed] [Google Scholar]