Graphical abstract

Keywords: Anomalous left atrial ridge, Atrial septal pouch, Atrial septum, Cardiac source of embolism, Transseptal puncture
Highlights
-
•
Left atrial ridge may affect planning of trans-septal approach for interventions.
-
•
Left atrial septal pouch may become a nidus for thrombus and source of embolus.
-
•
Complete interrogation of the atrial septum can identify these anatomic variants.
Introduction
Anomalies in the fusion of the interatrial septum may result in several anatomic variants, including atrial septal pouch, left atrial septal ridge, and a mixed anatomy that includes both a pouch and a ridge.1 Left atrial pouch is a kangaroo pocket–like structure in the interatrial septum, without an interatrial shunt, occurring because of incomplete fusion between the septum primum and septum secundum; the pocket opens into either the left atrium or, less commonly, into the right atrium.2 A left atrial ridge is a localized thickened area of tissue thought to be due to irregular fusion of the septa, typically running along the region of the fossa ovalis on the left atrial side of the septum.3 As seen in this case series, some individuals may have a combination of an atrial septal pouch with an interatrial septal ridge (mixed anatomy). The presence of a left atrial ridge may have significant clinical implications for patients undergoing catheter-based procedures that require puncture of the interatrial septum, such as percutaneous mitral valve repair or replacement, atrial fibrillation ablation, or left atrial appendage closure. Additionally, presence of a left atrial septal pouch may have clinical significance as a nidus for thrombus formation and source of intracardiac source of embolization. In this case series, we report nine cases that highlight these anatomic variants of atrial septal fusion.
Case Series Presentation
Case 1
A 41-year-old asymptomatic man with a history of bicuspid aortic valve, mildly dilated aorta, moderate to severe aortic insufficiency, coronary artery disease, reduced left ventricular function, and anomalous coronary arteries with independent origins of the left anterior descending and left circumflex coronary arteries originating from the left coronary sinus presented for preoperative transesophageal echocardiographic assessment before consideration of aortic valve replacement. On two-dimensional transesophageal echocardiography (TEE), he was found to have a pocket-like structure, consistent with a pouch, with an opening on the left atrial side of the interatrial septum (Figure 1). There was no evidence of an interatrial shunt. On further imaging characterization with three-dimensional TEE, there was also a tubular structure on the left atrial side of the interatrial septum, which was identified as an associated anomalous left atrial ridge (Figure 2). The patient underwent chest computed tomography (CT) to evaluate the size of the ascending aortic aneurysm, which also incidentally demonstrated the left atrial septal pouch and ridge with contrast seen within the pouch (Figure 3A, arrow). On retrospective review of transthoracic imaging, the abnormality could be seen in the apical four-chamber view as thickening of the left atrial side of the interatrial septum (Figure 3B). The patient underwent uncomplicated aortic root repair and repair of bicuspid aortic valve.
Figure 1.
Two-dimensional transesophageal echocardiographic images of the interatrial septum at 0° (top left), 52° (top right), and 60° (bottom), showing an anomalous left atrial septal pouch (arrow) from case 1. AV, Aortic valve; LA, left atrium, RA, right atrium.
Figure 2.

Three-dimensional transesophageal echocardiographic images from case 1 demonstrate that the left atrial septal pouch is associated with an anomalous left atrial ridge (arrow); the imaging characterizes its tubular structure on the left atrial side of the interatrial septum (en face view from left atrial perspective).
Figure 3.
Chest computed tomographic image demonstrating the left atrial septal pouch associated with anomalous left atrial ridge (black arrow) with contrast within it (A) and two-dimensional transthoracic echocardiographic image in apical four-chamber view (B) showing thickening of the interatrial septum with hint of the anomalous left atrial ridge (white arrow) from case 1.
Case 2
A 77-year-old man with a history of coronary artery disease, abdominal and thoracic aortic aneurysm, stroke, moderate to severe mitral regurgitation with myxomatous mitral valve leaflets, and flail anterior mitral valve leaflet (Carpentier classification type II) presented with New York Heart Association functional class III symptoms for preoperative TEE before consideration of percutaneous mitral valve repair. On TEE, he was found to have a pocket in the middle of the interatrial septum on the left atrial side that was identified as a left atrial septal pouch (Figures 4A–4C). On further imaging characterization with agitated saline contrast, there was no evidence of atrial septal defect (Figures 5A and 5B). This patient also underwent chest CT to evaluate the size of the ascending aortic aneurysm, which again demonstrated the anomalous interatrial septal anatomy with contrast seen within the pouch (Figure 6A). As in the previous case, upon retrospective review of transthoracic imaging, the pouch could be seen in the apical four-chamber view as an area of thickening of the left atrial side of the interatrial septum (Figure 6B). Further evaluation for percutaneous mitral valve repair was not pursued because of the detection of high-grade malignancy.
Figure 4.
Two-dimensional transesophageal echocardiographic images of the interatrial septum at 0° (A), 62° (B), and 118° (C) showing the left atrial septal pouch (arrow) in case 2. LA, Left atrium; RA, right atrium.
Figure 9.
Three-dimensional transesophageal echocardiographic images from case 3 demonstrate that in association with the left atrial septal pouch, there is also an anomalous left atrial ridge (arrows). Three-dimensional imaging characterizes its tubular structure on the left atrial side of the interatrial septum from case 3. (A, B) Superior and inferior plane of the interatrial septum. (C, D) En face view from left atrial side. RA, Right atrium.
Figure 5.
Saline contrast imaging in the bicaval view showing a left atrial septal pouch (arrow) and absence of an atrial septal defect both at rest (A) and with Valsalva maneuver (B) from case 2. LA, Left atrium; RA, right atrium.
Figure 6.
Chest computed tomographic image demonstrating the left atrial pouch (arrows) with contrast within it (A). Two-dimensional transthoracic echocardiographic image in apical four-chamber view shows thickening of the interatrial septum (B) but does not definitively demonstrate left atrial septal pouch seen on TEE and CT from case 2. LA, Left atrium, LV, left ventricle, RA, right atrium, RV, right ventricle.
Case 3
A 60-year-old man with a history of apical hypertrophic cardiomyopathy, apical aneurysm, and atrial fibrillation presented with fatigue and dizziness. On two-dimensional TEE, he was found to have a pouch on the left atrial side of the interatrial septum (Figures 7A–7C). On further imaging characterization with color Doppler, there appeared to be unrestricted flow within this structure but no evidence of atrial septal defect (Figures 8A and 8B). Further imaging characterization with three-dimensional TEE revealed a tubular area of thickening consistent with an anomalous left atrial ridge (Figures 9A–9D) that was associated with the left atrial septal pouch. No intracardiac thrombus was detected on TEE, and the patient underwent cardioversion without complications.
Figure 7.
Two-dimensional transesophageal echocardiographic images of the interatrial septum at 0° (A), 34° (B), and 60° (C) showing a left atrial septal pouch (arrow) from case 3. AV, Aortic valve; LA, left atrium; RA, right atrium; RV, right ventricle.
Figure 8.
Two-dimensional transesophageal echocardiographic images of the interatrial septum at 121° (A) and color Doppler imaging (B) showing a left atrial septal pouch (arrow) with color flow within it from case 3. No interatrial shunt is seen. LA, Left atrium; RA, right atrium.
Case 4
An 83-year-old woman with a history of symptomatic atrial fibrillation presented with decompensated heart failure for electrical cardioversion. She underwent TEE to rule out left atrial and left atrial appendage thrombi before electrical cardioversion. Three-dimensional imaging of the atrial septum showed a long, thick ridge extending from the superior vena cava to inferior margin of the fossa ovalis (Figure 10). No intracardiac thrombus was detected, and the patient underwent uncomplicated electrical cardioversion.
Figure 10.

Three-dimensional transesophageal echocardiographic image of the left side of the interatrial septum clearly shows a thick ridge (arrows) extending from the superior vena cava (SVC) to the inferior margin of the fossa ovalis (FO) in case 4. Ao, Aorta; CS, coronary sinus; MV, mitral valve.
Case 5
A 45-year-old man with a history of severe mitral regurgitation and chronic heart failure presented with fatigue and mild dyspnea on exertion. He underwent TEE for preoperative assessment before consideration of surgical mitral valve repair. On two-dimensional TEE, he was found to have a pocket on the left atrial side of the interatrial septum that was not associated with an atrial septal defect and was consistent with a left atrial septal pouch (Figures 11A and 11B). Three-dimensional imaging of the atrial septum showed a long, thick ridge extending from the superior vena cava to the inferior margin of the fossa ovalis (Figure 11C), consistent with an associated left atrial ridge. The patient will be undergoing elective mitral valve surgery and has no known complications from the atrial septal anomaly.
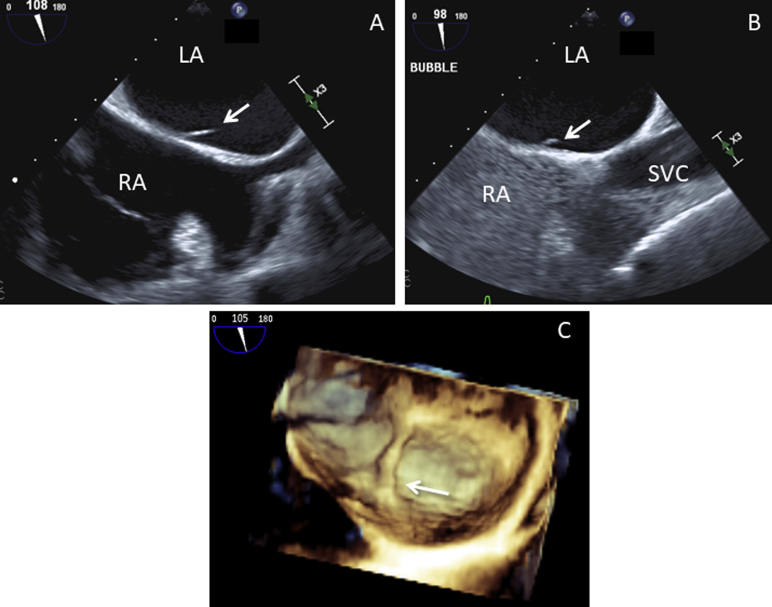
Figure 11.
Two-dimensional transesophageal echocardiographic images of the interatrial septum at 108° (A) demonstrates a left atrial septal pouch. Saline contrast study at 98° (B) demonstrates the absence of an interatrial shunt, and three-dimensional transesophageal echocardiographic image (C) demonstrates an associated anomalous left atrial ridge (arrows) from case 5. LA, Left atrium; RA, right atrium; SVC, superior vena cava.
Case 6
A 58-year-old man with a history of severe mitral regurgitation, chronic New York Heart Association functional class II symptoms, and hypercholesterolemia presented with worsening dyspnea on exertion and decreased exercise tolerance. He underwent TEE for preoperative assessment before consideration of surgical mitral valve repair. On TEE, he was found to have an area of nonfusion of the interatrial septum consistent with a left atrial septal pouch (Figure 12, top left). On further imaging characterization with color Doppler, a mosaic color Doppler signal was seen in the left atrium due to the mitral regurgitation, but there was no evidence of atrial septal defect (Figure 12, top right). Three-dimensional imaging of the atrial septum demonstrated the left atrial septal pouch (Figure 12, bottom). The patient had no known history of complications related to this anatomic finding and is planning to undergo elective mitral valve surgery.
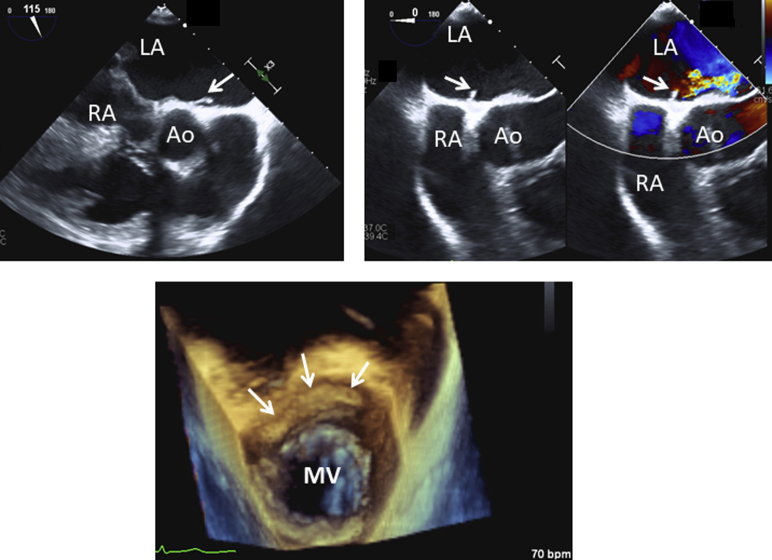
Figure 12.
Two-dimensional transesophageal echocardiographic images of the interatrial septum at 115° (top left), color Doppler at 0° (top right), and three-dimensional transesophageal echocardiographic image (bottom) showing a left atrial septal pouch from case 6 (arrows). Ao, Aorta; LA, left atrium; MV, mitral valve; RA, right atrium.
Case 7
A 38-year-old man with a history of type 2 diabetes mellitus, peripheral vascular disease, and tobacco use presented with difficulty ambulating, left lower extremity pain, and altered mental status. He was subsequently found to have an ischemic stroke in the right frontal lobe and basal ganglia and underwent TEE for evaluation of embolic source. On TEE he was found to have an area of nonfusion on the left atrial aspect of the interatrial septum, resulting in a left atrial septal pouch (Figures 13A and 13B). To evaluate for source of embolus from the aorta, he also underwent CT of the chest, which demonstrated the left atrial septal pouch (Figures 14A and 14B). Although this may potentially serve as a nidus for cardiac emboli, no intracardiac thrombus was identified in this individual. In this case, one may mistake this finding on two-dimensional imaging for cor triatriatum sinister. However, multiplane TEE and CT demonstrated that the flap of tissue was localized to the septum, unlike cor triatriatum sinister, in which a membrane divides the left atrium into superior and inferior chambers. The patient was discharged on direct oral anticoagulant therapy and aspirin.
Figure 13.
Two-dimensional transesophageal echocardiographic images of the interatrial septum at 0° (A) and 53° (B) in case 7 showing a left atrial septal pouch (arrows). LA, Left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
Figure 14.
Chest computed tomographic image demonstrating the anomalous left atrial septal pouch (arrow) with contrast within it from case 7. Axial view (A) and sagittal view (B).
Case 8
A 49-year-old man with a history of nonischemic cardiomyopathy, obstructive sleep apnea, type 2 diabetes mellitus, and atrial fibrillation presented with dyspnea on exertion and fatigue. He was found to be in atrial fibrillation with rapid ventricular rates and underwent TEE for planned electrical cardioversion. On TEE, he was found to have a severely dilated left atrium and a left atrial septal pouch (Figure 15, Figure 16A, and 16B). Cardioversion was not attempted, because of thrombus in the left atrial appendage (not shown). Approximately 1 year later, the patient presented again with acute decompensated heart failure. He was again found to be in atrial fibrillation with rapid ventricular rates. He underwent repeat TEE, which revealed that the anomalous left atrial septal pouch now contained an echodense structure seen within the pouch suggestive of thrombus, which was not seen on the prior study (Figures 16C and 16D). The patient was treated with anticoagulation.
Figure 15.
Three-dimensional imaging of interatrial septum in case 8, showing a left atrial septal pouch (asterisk) from the left atrial perspective.
Figure 16.
Two-dimensional transesophageal echocardiographic images of the interatrial septum from case 8 showing the left atrial septal pouch (A, B). Repeat two-dimensional TEE 1 year later showing a mobile echodense structure arising from within the pouch suggestive of thrombus (C, D). AV, Aortic valve; LA, left atrium; RA, right atrium.
Case 9
A 69-year-old man with a history of ischemic cardiomyopathy and advanced chronic systolic heart failure on left ventricular assist device support presented with fevers and chills. Blood cultures grew Streptococcus species, and TEE was performed to evaluate for endocarditis. Two-dimensional TEE demonstrated a left atrial septal pouch (Figure 17A) and an area of thickening on the roof of the pouch that was consistent with a left atrial ridge. There was no evidence of an atrial septal defect on color Doppler imaging. Three-dimensional TEE more clearly demonstrated the left atrial ridge, as well as the left atrial septal pouch with the orifice seen on the left atrial side of the septum (Figure 17B). The pouch could be seen as an area of partial nonfusion between the septum primum and septum secundum, resulting in a “kangaroo pocket” with an opening into the left atrium. In contrast, the left atrial septal ridge could be seen as a linear region of thickened tissue on the left atrial side of the septum, running along the fossa ovalis and likely caused by irregular fusion of the septa. In this case, the patient had no known clinical sequelae from this finding.
Figure 17.
Imaging from case 9. (A) Two-dimensional TEE demonstrating a left atrial septal pouch (asterisk) and an area of thickening on the roof of the pouch that is consistent with a left atrial ridge (white arrow). Three-dimensional imaging of the interatrial septum from the left atrial perspective (B) shows the orifice of the left atrial septal pouch (solid black arrow) and the left atrial ridge (dashed black arrow). AV, Aortic valve; LA, left atrium; RA, right atrium.
Discussion
Here we report a series of patients with anomalous atrial septal fusion, an important anatomic variant as transseptal puncture is more frequently performed. In addition, the presence of a left atrial septal pouch may serve as a nidus for thrombus formation and source of embolic complications, particularly in patients with decreased cardiac function and stagnant atrial flow. The atrial septum is a blade-shaped structure with an oval-shaped fossa ovalis midway between the inferior margin and tip and constituting 28% of the total septal area.4 The atrial septum is demarcated by three borders viewed from the right atrial side: superior vena cava, inferior vena cava, and membranous septum. The left side of the atrial septum features a network of muscular trabeculations formed by remnants of the septum primum.4,5 Ridge-like structures are common in the right atrium and include well characterized structures such as the Eustachian valve and crista terminalis. Redundancy of the atrial septal membrane that forms the fossa ovalis as well as atrial septal aneurysms has previously been well described on the left atrial side of the atrial septum.4 The anomalous ridge of the left side of the interatrial septum may depend on an irregular fusion between septum primum (the floor of the fossa ovalis) and septum secundum (the folding of the atrial wall; Figure 18). The anomalous left atrial ridge is distinctly different than a prominent rim of the patent foramen ovale, where a flow signal will be seen demonstrating a shunt.
Figure 18.
Anatomic variants of the interatrial septum demonstrating different types of fusion between septum primum and septum secundum.
TEE with two-dimensional and three-dimensional imaging is a superior imaging modality to identify anatomic anomalies of the interatrial septum compared with transthoracic echocardiography, in which the anatomy may not be adequately visualized. Although atrial septal pouch can be identified on CT or cardiac magnetic resonance imaging, TEE provides better visualization of other septal abnormalities, such as patent foramen ovale or left atrial ridge. Overall, two-dimensional and three-dimensional TEE provides the most comprehensive evaluation of the interatrial septum, and further assessment of atrial septal pouches or ridges using CT is not needed in patients who have already undergone TEE. For the patients in our case series in whom CT was available, the scans were performed for other indications, and it is important that this finding be recognized when present on CT. However, in general, CT is not the first-line modality for the diagnosis of atrial septal pouch or atrial septal ridge.
The presence of the atrial septal pouch has been reported in several studies.2,6, 7, 8 This anomaly occurs because of incomplete fusion of the septum primum and septum secundum, resulting in a pouch without an interatrial shunt. The majority of atrial septal pouches are left sided; in an autopsy series, 39% of hearts were found to have left atrial septal pouches, whereas only 4% were found to have right-sided septal pouches.2 Although the relationship between stroke risk and left atrial septal pouch remains controversial, several studies have reported that left atrial septal pouch is associated with increased risk for stroke.6, 7, 8 In our case series, we observed the development of thrombus in the left atrial septal pouch in a patient with severely reduced left ventricular systolic function (case 8). This observation raises the possibility that left atrial septal pouch might become a nidus for thrombus formation in patients with low flow states. Further investigation is needed to further clarify the role the left atrial septal pouch may play in the risk for embolic stroke, as well of the impact of coexisting factors that may contribute to a thrombotic milieu. However, the available observations suggest that evaluation for left atrial septal pouch and comprehensive imaging to assess for associated thrombus should be undertaken in patients who are being evaluated for cardiac source of embolus.
Five of our cases as well as one previously reported case document a prominent ridge forming along the fossa ovalis.3 In our case series, the majority of left atrial ridge findings occurred in the presence of a left atrial septal pouch. Recognition of the left atrial ridge is important so as to not mistake it for a mass, tumor, or cor triatriatum. This anatomic variant has clinical implications given the growing use of transseptal puncture for percutaneous structural interventions. It has been noted that thickening of the interatrial septal may present technical challenges for transseptal puncture.9 With complete imaging and appropriate planning, the interventionalist can avoid crossing the ridge, which may be difficult to puncture or may require crossing both the interatrial septum and the additional ridge tissue. Furthermore, the ridge may interfere with the navigation of guidewires and catheters in the left atrium via the transseptal approach.10,11 This is not just a theoretical concern, as it was previously reported that a double atrial septum altered the placement of transseptal puncture in a patient undergoing pulmonary vein isolation for atrial fibrillation.12,13
We note that in five of the nine cases, other structural cardiac abnormalities were also present: aortic regurgitation in the setting of a bicuspid aortic valve and aortopathy in case 1, myxomatous flail mitral valve and aortic aneurysm in case 2, hypertrophic cardiomyopathy in case 3, and mitral regurgitation in cases 5 and 6. However, it has previously been observed that the presence of a left atrial septal pouch is quite common in the general population2 and thus does not appear to be specifically associated with other congenital cardiac anomalies. Whether the presence of a left atrial ridge is associated with other congenital abnormalities remains unknown.
Conclusion
These cases of anomalous interatrial septal fusion highlight the importance of complete interrogation of the interatrial septum, particularly in patients being considered for catheter-based procedures that will require a transseptal approach and in patients being evaluated for intracardiac thrombus. TEE provides comprehensive imaging of the atrial septal anatomy, and the use of three-dimensional imaging allows more detailed assessment of the anatomic features of the septum. Three-dimensional TEE is particularly useful for identifying atrial septal ridge, which may have implications in patients undergoing structural interventions that require transseptal puncture. Although CT is generally not required for evaluation of atrial septal abnormalities, findings such as a left atrial pouch can be easily identified on CT with contrast imaging. For example, in patients who are undergoing evaluation for percutaneous structural interventions, TEE and/or CT is often used for procedural planning, and attention should be paid to the atrial septal anatomy in cases in which transseptal puncture is anticipated. Likewise, many patients who are being evaluated for cardiac source of embolus undergo TEE, and in such patients, assessment of the atrial septal anatomy, beyond assessment for interatrial shunt, may provide useful information.
Footnotes
Conflicts of interest: The authors reported no actual or potential conflicts of interest relative to this document.
References
- 1.Faletra F.F., Leo L.A., Paiocchi V.L., Schlossbauer S.A., Pedrazzini G., Moccetti T. Revisiting anatomy of the interatrial septum and its adjoining atrioventricular junction using noninvasive imaging techniques. J Am Soc Echocardiogr. 2019;32:580–592. doi: 10.1016/j.echo.2019.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Krishnan S.C., Salazar M. Septal pouch in the left atrium—a new anatomical entity with potential for embolic complications. J Am Coll Cardiol Intv. 2010;3:98–104. doi: 10.1016/j.jcin.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 3.Shizukuda Y., Muth J., Chaney C., Attari M. Anomalous ridge on the left atrial side of the atrial septum. Ann Card Anaesth. 2012;15:161–162. doi: 10.4103/0971-9784.95083. [DOI] [PubMed] [Google Scholar]
- 4.Sweeney L.J., Rosenquist G.C. The normal anatomy of the atrial septum in the human heart. Am Heart J. 1979;98:194–199. doi: 10.1016/0002-8703(79)90221-7. [DOI] [PubMed] [Google Scholar]
- 5.Mommersteeg M.T., Hoogaars W.M., Prall O.W., de Gier-de Vries C., Wiese C., Clout D.E. Two distinct pools of mesenchyme contribute to the development of the atrial septum. Circ Res. 2006;99:351–353. doi: 10.1161/01.RES.0000238360.33284.a0. [DOI] [PubMed] [Google Scholar]
- 6.Holda M.K., Karawczyk-Ozog A., Koziej M., Aorysz D., Holda J., Dudek D. Left-sided atrial septal pouch is a risk factor for cryptogenic stroke. J Am Soc Echocardiogr. 2018;31:771–776. doi: 10.1016/j.echo.2018.01.023. [DOI] [PubMed] [Google Scholar]
- 7.Tuzcu A., Okajim K., Jin Z., Rundek T., Sacco R.L., Elkind M.S.V. Septal pouch in the left atrium and risk of ischemic stroke. J Am Coll Cardiol Img. 2010;3:1276–1283. doi: 10.1016/j.jcmg.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun J.P., Meng F., Yang X.S., Lee A.P., Chen M., Zhang B. Prevalence of atrial septal pouch and risk of ischemic stroke. Int J Cardiol. 2016;214:37–40. doi: 10.1016/j.ijcard.2016.03.119. [DOI] [PubMed] [Google Scholar]
- 9.Alkhouli M., Rihal C.S., Holmes D.R. Transseptal techniques for emerging structural heart interventions. J Am Coll Cardiol Intv. 2016;9:2465–2480. doi: 10.1016/j.jcin.2016.10.035. [DOI] [PubMed] [Google Scholar]
- 10.Faletra F.F., Nucifora G., Ho S.Y. Imaging the atrial septum using real-time three-dimensional transesophageal echocardiography: technical tips, normal anatomy, and its role in transseptal puncture. J Am Soc Echocardiogr. 2011;24:593–599. doi: 10.1016/j.echo.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 11.Pushparajah K., Miller O.I., Simpson J.M. 3D echocardiography of the atrial septum: anatomical features and landmarks for the echocardiographer. J Am Coll Cardiol Img. 2010;3:981–984. doi: 10.1016/j.jcmg.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 12.Harding J.D., Grzywacz E., Sangrigoli R. Double atrial septum and transseptal puncture: an unusual obstacle to pulmonary vein isolation. Heart Rhythm. 2011;8:1457–1458. doi: 10.1016/j.hrthm.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 13.Gold B.M., Parekh D.R., Kearney D.L., Silva G.V., Fish R.O., Stainback R.F. Forme fruste cor triatriatum dexter by transesophageal echocardiogrpahy and its impact on percutaneous heart procedures: a case series. Cardiovasc Imaging Case Rep. 2019;3:189–199. doi: 10.1016/j.case.2019.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]