Abstract
Introduction
Supracondylar fracture of humerus (SFH) is frequently encountered in the immature skeleton, [1] predominantly in the non-dominant extremity.
Aim
This study compared the clinic-radiological outcome between cross pinning with lateral pinning for fixation of displaced supracondylar fracture of humerus in children.
Materials and methods
All eligible patients were randomized into two groups, group I for lateral pinning and group II for cross pinning. Before passing medial pin in group II a stab incision was given to visualise the medial epicondyle. Patients were followed up on 3 weeks, 6 weeks and 3 months. Final outcome was measured in terms of clinic-radiological union, Baumann angle, loss of reduction, stability of fracture fixation, incidence of iatrogenic nerve injury and Flynn's score. Results: There were 37 patients in group I and 40 in group II. Both groups were comparable in terms of demographic details. At the final outcome there were no difference in between the groups in terms of all radiological and clinical outcome. Two patients of group I developed delay ulnar neuritis, which resolve completely in subsequent follow-up.
Conclusion
Both techniques provide stable fixation, union and good functional outcome without iatrogenic ulnar nerve injury provided that small incision sufficient enough to identify the medial epicondyle is given with passing of medial pin.
Keywords: Pinning techniques, Paediatric supracondylar fractures, Closed reduction
1. Introduction
Supracondylar fracture of humerus (SFH) is frequently encountered in the immature skeleton,1 predominantly in the non-dominant extremity.2 The fracture in elbow extension with posterior displacement is seen in 97% of cases.2 It is commonly classified in three types as given by Gartland on the basis of displacement in coronal plane radiographs. Type I: undisplaced or minimally displaced fracture with intact anterior humeral line. Type II: small deviation, fragments in contact with intact posterior cortex, type III: complete displacement of the fracture fragments, breach in posterior cortex.3 Later on, Leitch et al., added Type IV, describing multidirectional instability.4
Most commonly used technique for surgical treatment in displaced SFH (types II, III, IV) in children is closed reduction and stabilization with percutaneous pins.5 The most common used configuration of pinning are medial and lateral crossed pinning, and lateral pinning. However, there is still controversy regarding the choice of pinning configuration6 and based primarily on the surgeons’ preference. There are two key factors when comparing these two configurations which are the mechanical stability and the risk of iatrogenic ulnar nerve injury. Cross pinning is more biomechanically stable in fixation but it has higher risk of ulnar nerve injury during insertion of medial pin.6 Although, pinning from lateral side has negligible risk of ulnar nerve injury, is considered biomechanically less stable7 and having theoretical chances of loss of reduction.
The purpose of this study is to compare the outcome and safety of two pinning techniques i.e. crossed pinning and lateral pinning in terms of radiological and functional outcome and complications if any, for fixation of displaced (Gartland type II, III and IV) SFH in children.
2. Materials and method
After approval by our Institutional Review Board, patients who qualify inclusion criteria were enrolled in this study.
Trial design: This was a prospective randomized study conducted in between March 2014 to May 2015. All the patients who presented to ER/OPD with SFH were assessed.
Participants: inclusion criteria was: a) age below twelve years, b) Gartland type II, III and IV Supracondylar fracture, c) presented to OPD/Emergency within 7 days of injury d) closed and Gustilo Grade I fractures, e) Who consented for the study. Patients with open fracture (Gustilo Grade II and III), neurovascular deficit and presenting after 7 days were excluded from the study. Patients were admitted from ER and OPD and the study was performed in Department of Orthopaedics, B.P. Koirala Institute of Health Sciences, Dharan. Total 84 patients underwent CRPP. Seven cases (five from lateral pinning and two of crossed pinning group) did not follow up after surgery as they were from remote districts of Nepal. Hence, 37 patients were recruited in lateral pinning and 40 in crossed pinning for the final analysis.
Intervention and groups: After enrolment for the study, patients were randomized into two groups; group A, treated with close reduction and fixation with lateral pinning Fig. 1(b); and group B, treated with close reduction and fixation with crossed pinning (one from lateral and another from medial side) Fig. 2(a). Demographic details including age, sex, hand dominance, mechanism of injury, direction of fracture displacement, time from injury to surgery, and neurovascular status was recorded for all patients and compared between the two cohorts as shown in Table 1 Clinical examination for pain, deformity, instability distal neurovascular status of all included patients were done before surgery. Anteroposterior and lateral radiograph of elbow was taken in all patients to assess displacement and define type of fracture. Fig. 1(a)
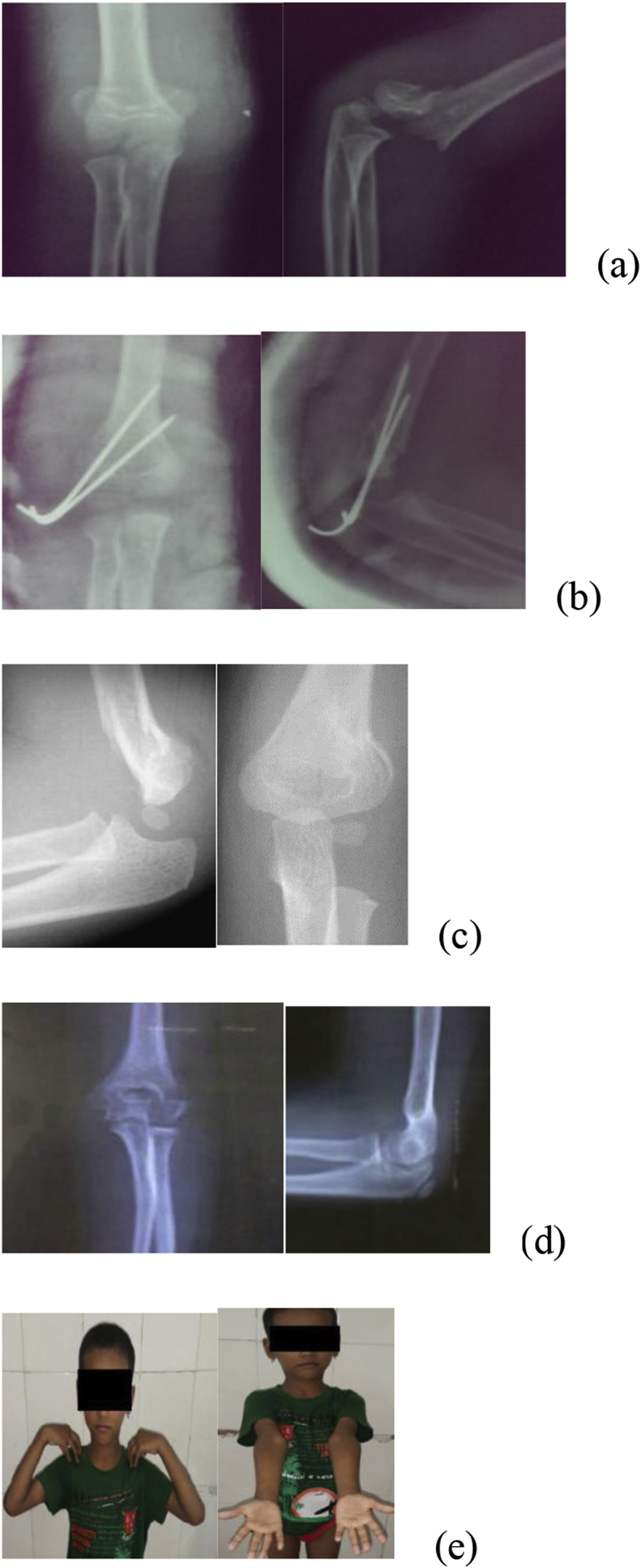
Fig. 1.
(a) Preoperative radiograph, 1(b) immediate post-operative radiograph showing lateral pinning configuration 1(c) radiograph after removal of K-wires at 3rd weeks, 1(d) complete remodeling at 12th month 1(e) functional outcome at 12th month.
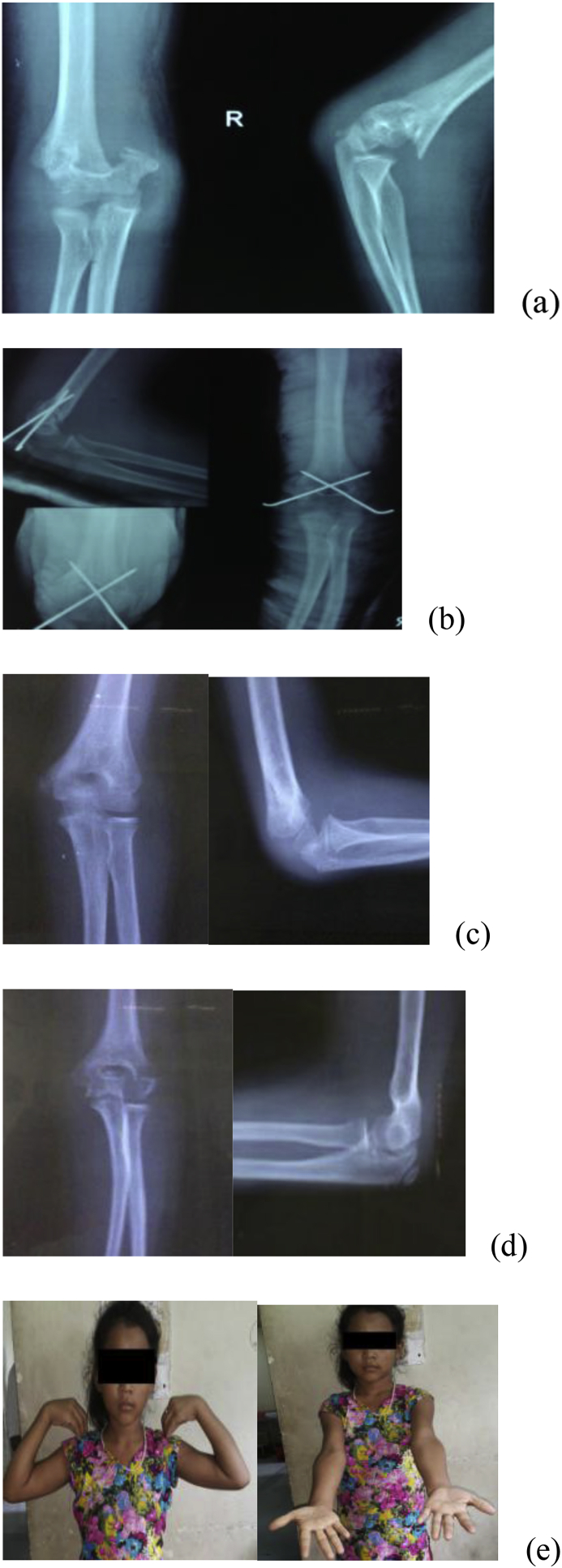
Fig. 2.
(a) Preoperative radiograph, 2(b) immediate post-operative radiograph showing cross wire configuration, 2(c) radiograph after K-wire removal, 2(d) remodeling after 12 months, 2(e) final follow-up.
Table 1.
Demographic data showing comparison and p-value between group I and II.
| Parameters | Group I (n = 37) (lateral pin) | Group II (n = 40) | P-value |
|---|---|---|---|
| Age | 6.8 +_ 0.9 | 7.2+_ 0.8 | 0.6 |
| Male to female | 5:4 | 2:1 | 0.3 |
| Non-dominant extremity | 23 | 27 | 0.6 |
| Injury to presentation (days) | 5.1+_0.5 | 4.9+_0.6 | 0.5 |
| Mode of injury | |||
| Fall from height | 20 | 19 | 0.9 |
| Fall while playing | 17 | 21 | 0.6 |
| Displacement | |||
| Posteromedial | 24 | 28 | 0.2 |
| Posterolateral | 13 | 12 | 0.2 |
| Ulnar nerve injury | 0 | 2 (transient) | |
| Compartment syndrome | 0 | 0 | |
| Vascular injury | 0 | 0 | |
| Infection | 3 | 2 | 0.5 |
Surgical procedure: In all patients of both group, close reduction was tried first and if failed open reduction was done. The patients who required open reduction were excluded from the study. After closed reduction acceptable in image intensifier, reduction was maintained by pinning in configuration depending upon group allocation. Patients randomized in group A, received two pins placed from the lateral side percutaneously, with bicortical purchase Fig. 1(b). It was tried to place both wire either parallel or divergent. After fixation, stability was checked, if found inadequate additional third pin was inserted. In these cases data was analysed based on the intention-to-treat principle, according to which subject in trial should be analysed in the groups to which they were allocated regardless whether they received or adhered to the allocated intervention.8 Patients allocated to the cross pinning technique group (group B) received one medially placed and laterally placed bicortical pin. The first pin was placed from the lateral side. After placement of lateral pin, medial pin was inserted percutaneously without visualization of ulnar nerve Fig. 2(a). In order to prevent ulnar nerve injury, elbow was kept at less than 45–60° of extension and wire was placed over the epicondyle, anterior to ulnar groove. If epicondyle was not palpable due to swelling a stab incision was given and was identified. Similar to the lateral-entry pin group technique, when a third pin was added from lateral side, data was analysed based on the intention-to-treat technique. All pins were cut and bent. Above elbow plaster of Paris slab was applied at the end of reduction and fixation.
Postoperative care and Rehabilitation: Duration of surgery, size and number of K-wires were noted. Assessment of iatrogenic neurovascular deficit was done in immediate postoperative period. Radiological assessment of reduction including measurement of Baumann's angle was made on radiograph (lateral view) before discharging the patient. Patients were discharged on 2nd post-operative day after checking wound dressing/pin site care with advice to keep the limb splinted, active/passive movements of joints and fingers, reporting immediately to emergency ward if excessive pain/swelling, tingling sensation, numbness or bluish discoloration of fingers occur. Repeat radiograph was done after 3 weeks following which slab and pins were removed (depending upon the evidence of union clinico-radiologically) Fig. 1, Fig. 2
The patients were evaluated as outpatients at three weeks, six weeks and twelve weeks after the surgery. Follow-up assessment of each patient was done by the same doctor throughout the trial. Necessary clinical and radiological data were noted as per proforma at every visit.
Outcomes: At 3 weeks, slab was removed on OPD basis and K wires were removed only on evidence of union seen radiologically, elbow mobilization was done by physiotherapist. Clinically: Fracture site tenderness, inflammatory features were sought. Radiologically: Evidence of callus formation, Baumann's angle was measured. At 6 weeks, Elbow ROM was assessed clinically and radiologically, Baumann's angle was measured. At 12 weeks follow-up, following information was recorded as outcome measures: (i) Loss of carrying angle and loss of total range of elbow motion based on Flynn's criteria9 (ii) Grading of loss of reduction, based on difference in the Baumann angle (degrees) between immediate post-operative radiographs and radiographs after the surgery and radiographs at 12 weeks follow-up visit according to method described by Skaggs et al.10: (1) no displacement (loss smaller than 6°), (2) moderate displacement (6–12°), and (3) large displacement (more than 12°) (iii) Final Baumann angle (degree), calculated on the radiograph of antero posterior view of elbow (iv) Incidence of nerve injury and recovery pattern (if applicable) (v) Time to union (Radiological).
Sample size: During the study period, a total of 850 patients associated with elbow injury presented to our institution out of which 127 were children with supracondylar fractures of humerus. We excluded 43 patients who did not meet the eligibility criteria. Therefore total 84 patients underwent closed reduction and percutaneous pinning. Seven cases (five from lateral pinning and two of crossed pinning group) did not follow up after surgery as they were from remote districts of Nepal. Hence we analysed results of 37 cases in lateral pinning and 40 cases in crossed pinning for the final analysis.
Randomization: was done using excel random generation technique
3. Statistical analysis
Independent sample student's t-test was done to assess the parameters like age, follow-up and duration of surgery. The results and quantitative datas were expressed as mean with standard deviation. For all statistical purposes, p value was kept <0.05. Collected data was entered in Microsoft Excel 2015 and SPSS (statistical package for social sciences version 20) for statistical analysis.
4. Results
There were 98 patients reported to our OPD/Emergency of B.P. Koirala Institute of Health Sciences with SFH out of which 5 had injury of more than 7 days duration, 3 had Gustilo grade II open fractures and 6 did not give consent to take part in study. Rest 84 patients qualified the inclusion criteria and were randomized into two groups by using random number generator in Excel.
Total 84 patients underwent closed reduction and percutaneous pinning. 4 cases (3 from lateral pinning and 1 of crossed pinning group) did not follow up after surgery as they were from remote districts. We need to open reduction in 3 (1 in group A and 2 in group B). Finally, analysis was done with the results of 37 cases in group A and 40 cases in the group B.
The mean age of the patient at the time of presentation was 6.8+_0.9 years (4−12) in Group A and 7.2+_0.8 years (3−12) in Group B (P = 0.6). Male to female ratio in group A was 5:4 and in group B was 2:1 (P = 0.3). Non-dominant extremity was more in both groups. All of the patients presented with fall injury. Among them fall from height was the commonest mode of injury (extension injury) Table 1. According to Gartland classification, type III was the most common type of fracture in both group. The distribution of types of fracture and other demographic details is shown in the table. To achieve adequate stability third wire was required from medial side in 4 patients in group A, and from lateral side in 3 patients in group B.
4.1. Clinical and radiological evaluation
Baumann's angle, change in Baumann angle, loss of reduction, carrying angle, loss of carrying angle, range of motion in flexion and extension of elbow and total loss of range of motion were not significantly different at any point of time. According to Flynn's grading, 26 patient in group I and 24 patients in group II had excellent results, 7 patients in group I and 15 in group II had good result, 4 patients in group I and 1 in group II had fair result respectively. None of the patients in either group had poor results on the basis of Flynn's criteria Table 2.
Table 2.
Clinical and radiological outcome of both groups and their p-values.
| Parameters | Group I | Group II | P-value |
|---|---|---|---|
| Range of motion | 131.6+_3.4 | 131.0+_3.2 | 0.4 |
| Carrying angle | 8.9+_2.2 | 8.2+_1.6 | 0.2 |
| Loss of carrying angle | 4.4+_0.8 | 4.6+_0.9 | 0.3 |
| Baumann's angle | 78.0+_3.2 | 78.6+_3.1 | 0.4 |
| Change in Baumann's angle | 2.0+_0.7 | 2.1+_0.8 | 0.9 |
| Loss of reduction | 2.9+_0.3 | 2.9+_0.2 | 0.9 |
| Flynn's grading | |||
| Excellent | 26 | 24 | 0.9 |
| Good | 7 | 15 | 0.07 |
| Fair | 4 | 1 | 0.1 |
| Poor | 0 | 0 | 1 |
Complications: Two patients in group B developed tingling sensation and numbness in ulnar nerve distribution with intact motor function which was seen after two days of surgery. On subsequent follow up, all three patients recovered.
Three patients in group A and 2 patients in group B had pin track infection one week following surgery which was managed by dressing and oral antibiotics and responded well. None of the patients in either group developed any other complication. (P = 0.5).
5. Discussion
Successful treatment of displaced SFH of children depends on achieving and maintaining an acceptable reduction until the fracture is healed, while avoiding complications. Controversy persists regarding the optimal pin fixation technique11 Although many configuration of pinning is described in the literature, the two most commonly used configurations are crossed and lateral entry pinning.5,12 There is a significant risk of iatrogenic ulnar nerve injury during medial pinning in crossed configuration with incidence rate of 0–6%.13 Whereas, in lateral pinning technique, there is a chance of loss of reduction due to biomechanically less stable, and most common complication of poor or loss of reduction during treatment is cubitus varus with the incidence of 3–57%.14 In order to, avoid these complication Dorgan's technique of crossed pinning from lateral side have been developed. However there is a theoretical risk of ulnar nerve injury, but in clinical situation the incidence of nerve injury is significantly less as compared to medial-lateral cross pinning.15 The problem is there is lack of data from biomechanical study, this technique has similar stability to that obtained by traditional cross pinning.7,16
In a recent meta-analysis done by Queiroz GS et al., al. regarding best method to treat SFH, concluded that percutaneous pinning with lateral wires for type II fracture and crossed wires in type III and IV fractures, with a mini-open technique for the medial wire. They also observed that if mini-open technique is not used, chances of iatrogenic ulnar nerve injury was significantly higher.17 Traditionally it was thought that ulnar nerve injury was temporary, but recent studies have contradicted this fact and is surgical exploration of nerve is required in approximately one third of the patient.18 Due to this factor most of now, mini-open and ulnar nerve exploration has become popular in practice.19 The common drawback, of mini-open surgery is longer duration of surgery and surgical scar.20 We experienced difficulty in identification of medial epicondyle which is the most important factor, while passing medial pin, usually it slips into ulnar groove, injuring the ulnar nerve. In this study, patient developed ulnar neuritis rather than iatrogenic injury which was probably due to inflammatory response of foreign body. So, to prevent that we are in favour of giving incision sufficient to identify medial epicondyle, not exploration of ulnar nerve, and have observed insignificant percentage of this complication.
There are no significant difference between the two groups in terms of radiographic outcome and loss of reductions in our and many earlier, both retrospective10,21,22 as well as prospective23 study. This contradict the fact of more biomechanical stability of crossed pinning, as observed in-vitro study. This disagreement of the results of the in-vivo and in-vitro literature are probably because of following reasons. First, the thick periosteum present in paediatric patients offers greater stability after fracture reduction, which is deficient in in-vitro models. Secondly, an osteotomy model lacks the intrinsic stability afforded by fracture interdigitation in vivo.19
As supported by some studies, it is expected that, radiographic measurements correlates well with the clinical outcome.23 Like no difference in radiographic parameter, we did not observed any clinical outcome difference in between two groups. This findings is supported by most of previously done study, including largest reported series to date and are in favour that the lateral-entry pin technique offers similar maintenance of reduction without risking iatrogenic injury to the ulnar nerve.21,22 The studies that have observed loss of reduction of the lateral entry pin technique have cited poor initial reduction and lateral reduction and technical error in pin placement as the cause.19 Similarly, in the decision tree model proposed by Lee KM et al., favoured the lateral pinning technique over the medial and lateral pinning technique in terms of the function adjusted life year, containing two comparable factors, that is, iatrogenic ulnar nerve palsy and loss of fixation represented by malunion.24 As far as Flynn score is concerned, most of the patients in both groups had good to excellent outcome similar to other studies like Vito P et al.125 and Naik LG.20
To overcome bias related to the surgeon's preference to use crossed pins for unstable fractures, we evaluated maintenance of fracture reduction in relation to fracture type and pin configuration which was considered as the strength of this study. The configuration of the pins did not appear to influence the change in the Baumann angle in either of the groups. Another strength was that the follow-up assessment of every patient was done by the same doctor during the entire study period.
5.1. Limitations
In spite of above mentioned strength, there are few limitations of this study. Firstly, the sample size, which is less because power of study was not done. Secondly, short term follow-up.
6. Conclusion
There is no significant difference between lateral pinning and crossed pinning in terms of functional outcome, stability, union and other surgical complications. Therefore, it is concluded that both the techniques provide stable fixation, union and good functional outcome without iatrogenic ulnar nerve injury provided that small incision sufficient enough to identify the medial epicondyle is given with passing of medial pin.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2019.01.013.
Financial support and sponsorship
Nil
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Davis R.T., Gorczyca Pugh K. Supracondylar humerus fractures in children. Comparison of operative treatment methods. Clin Orthop Relat Res. 2000;376:49–55. [PubMed] [Google Scholar]
- 2.Wilkins K.E. Fractures and dislocations of the elbow region. In: Rockwood C.A., King R.E., Wilkins K.E., editors. Fractures in Children. third ed. JB Lippincott; New York: 1991. pp. 526–617. [Google Scholar]
- 3.Gartland J.J. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet. 1959;109(2):145–154. [PubMed] [Google Scholar]
- 4.Leitch K.K., Kay R.M., Femino J.D., Tolo V.T., Storer S.K., Skaggs D.L. Treatment of multidirectionally unstable supracondylar humeral fractures in children. A modified Gartland type -IV fracture. J Bone Surg Am. 2006;88(5):980–985. doi: 10.2106/JBJS.D.02956. [DOI] [PubMed] [Google Scholar]
- 5.Buturovic S. Medicinski Fakultet. 2006. Komparacija rezultata lijeèenja preloma distralnog humerusa kod djece prema indikaciji za konzervativno ili operativno rjesenje: doktorska? disertacija. Sarajevo: univerzitet u Sarajevu. [Google Scholar]
- 6.Larson L., Firoozbakhsh K., Passarelli R., Bosch P. Biomechanical analysis of pinning techniques for pediatric supracondylar humerus fractures. J Pediatr Orthop. 2006 Sep 1;26(5):573–578. doi: 10.1097/01.bpo.0000230336.26652.1c. [DOI] [PubMed] [Google Scholar]
- 7.Eberhardt O., Fernandez F., Ilchmann T., Parsch K. Cross pinning of supracondylar fractures from a lateral approach. Stabilization achieved with safety. Journal of children's orthopaedics. 2007 Mar 1;1(2):127–133. doi: 10.1007/s11832-007-0011-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baumann E. Beitrage zur Kenntnis der Frakturen am Ellbogengelenk unter besonderer Berucksichtigung der Spatfolgen: allgemeines und Fractura supracondylica. Bietr Klin Chir. 1929;146:1–50. [Google Scholar]
- 9.Flynn J.C., Matthews J.G., Benoit R.L. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years' experience with longterm follow-up. J Bone Joint Surg Am. 1974;56:263–272. [PubMed] [Google Scholar]
- 10.Skaggs D.L., Hale J.M., Bassett J., Kaminsky C., Kay R.M., Tolo V.T. Operative treatment of supracondylar fractures of the humerus in children. The consequences of pin placement. J Bone Joint Surg Am. 2001;83:735–740. [PubMed] [Google Scholar]
- 11.Brauer C.A., Lee B.M., Bae D.S., Waters P.M., Kocher M.S. A systematic review of medial and lateral entry pinning versus lateral entry pinning for supracondylar fractures of the humerus. Journal of Pediatric Orthopaedics:March. 2007;27(2):181–186. doi: 10.1097/bpo.0b013e3180316cf1. [DOI] [PubMed] [Google Scholar]
- 12.Madjar-Simic I., Talic- Tanovic A., Hadziahmetovic Z., Sarac- Hadzihalilovic A. Radiographic assessment in the treatment of supracondylar humerus fractures in children. Acta Inf Med. 2012;20(3):154–159. doi: 10.5455/aim.2012.20.154-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krusche-Mandl I., Aldrian S., Köttstorfer J., Seis A., Thalhammer G., Egkher A. Crossed pinning in paediatric supracondylar humerus fractures: a retrospective cohort analysis. Int Orthop. 2012;36(9):1893–1898. doi: 10.1007/s00264-012-1582-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Green D.W., Widmann R.F., Frank J.S., Gardner M.J. Low incidence of ulnar nerve injury with crossed pin placement for pediatric supracondylar humerus fractures using a mini-open technique. J Orthop Trauma. 2005;19:158–163. doi: 10.1097/00005131-200503000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Memisoglu K., Kesemenli C.C., Atmaca H. Does the technique of lateral cross-wiring (Dorgan's technique) reduce iatrogenic ulnar nerve injury? Int Orthop. 2011 Mar 1;35(3):375–378. doi: 10.1007/s00264-010-1090-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Queally J.M., Paramanathan N., Walsh J.C., Cathal J., Moran C.J., Fintan J. Dorgan's lateral cross-wiring of supracondylar fractures of the humerus in children: a retrospective review. Injury. 2010;41:568–571. doi: 10.1016/j.injury.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 17.Patriota G.S., Assunção Filho C.A., Assunção C.A. What is the best fixation technique for the treatment of supracondylar humerus fractures in children? Revista brasileira de ortopedia. 2017 Aug;52(4):428–434. doi: 10.1016/j.rboe.2017.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rudicel S., Esdaile J. The randomized clinical trial in orthopaedics: obligation or option?. The Journal of bone and joint surgery. American volume. 1985 Oct;67(8):1284–1293. [PubMed] [Google Scholar]
- 19.Gaston R.G., Cates T.B., Devito D. Medial and lateral pin versus lateral-entry pin fixation for Type 3 supracondylar fractures in children: a prospective, surgeon-randomized study. J Pediatr Orthop. 2010 Dec 1;30(8):799–806. doi: 10.1097/BPO.0b013e3181f73d59. [DOI] [PubMed] [Google Scholar]
- 20.Naik L.G., Sharma G.M., Badgire K.S., Qureshi F., Waghchoure C., Jain V. Cross pinning versus lateral pinning in the management of type III supracondylar humerus fractures in children. J Clin Diagn Res: JCDR. 2017 Aug;11(8):RC01. doi: 10.7860/JCDR/2017/28481.10351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen R.S., Liu C.B., Lin X.S., Feng X.M., Zhu J.M., Ye F.Q. Supracondylar extension fracture of the humerus in children: manipulative reduction, immobilisation and fixation using a U-shaped plaster slab with the elbow in full extension. Bone & Joint Journal. 2001 Aug 1;83(6):883–887. doi: 10.1302/0301-620x.83b6.11705. [DOI] [PubMed] [Google Scholar]
- 22.Gordon J.E., Patton C.M., Luhmann S.J., Bassett G.S., Schoenecker P.L. Fracture stability after pinning of displaced supracondylar distal humerus fractures in children. J Pediatr Orthop. 2001 May 1;21(3):313–318. [PubMed] [Google Scholar]
- 23.Mehserle W.L., Meehan P.L. Treatment of the displaced supracondylar fracture of the humerus (type III) with closed reduction and percutaneous cross-pin fixation. Journal of pediatric orthopedics. 1991;11(6):705–711. doi: 10.1097/01241398-199111000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Lee K.M., Chung C.Y., Gwon D.K. Medial and lateral crossed pinning versus lateral pinning for supracondylar fractures of the humerus in children: decision analysis. J Pediatr Orthop. 2012 Mar 1;32(2):131–138. doi: 10.1097/BPO.0b013e3182471931. [DOI] [PubMed] [Google Scholar]
- 25.Pavone V., Riccioli M., Testa G. Surgical treatment of displaced supracondylar pediatric humerus fractures: comparison of two pinning techniques. Journal of Functional Morphology and Kinesiology. 2016 Jan 8;1(1):39–47. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.