Abstract
Objective
Tuberculosis (TB) is endemic in Indian subcontinent. The paediatric osteoarticular (OA) TB is frequently confused with suppurative etiology as both can have similar clinical, radiological and laboratory presentation. It has become a health hazard due to its association with immunosuppression diseases such as HIV, chronic renal and liver diseases and use of immunosuppressive drugs. Furthermore, there is much dilemma regarding the drug choice and duration of anti tubercular treatment among practicing clinicians. This mini review briefs the reader to the classical regional and atypical tubercular clinical presentations, imaging and laboratory investigations and management for bone and joint TB.
Methods
The article details both common and atypical clinical tubercular presentations, the approach to diagnosis, drug treatment and surgical indications in paediatric OA TB.
Results
OA TB in the paediatric age group is uncommon. Diagnosis is often delayed because of diseases’ nonspecific symptoms, non-characteristic imaging findings and lack of awareness of the condition. Multidrug antitubercular chemotherapy remains the anchor sheet of tubercular treatment in children. Surgery is needed in select cases to obtain tissue, to ensure better joint movement, prevent deformities and restore neurological function.
Conclusions
TB can have varied presentation and therefore it is essential to keep tubercular infection in differential diagnosis while working up for any infective pathology. Conservative treatment produces good results in vast majority of cases. Surgery is reserved for select indications.
Keywords: Tuberculosis, Bone and joint, Pediatric, Children
1. Introduction
Osteoarticular tuberculosis (OA TB) in the paediatric age group is uncommon. It has a reported incidence of 5–6% of all paediatric extrapulmonary cases.1 More recently, there is resurgence of the disease due to its close relationship with immune compromising diseases such as HIV infection, diabetes mellitus and chronic liver or kidney failure etc. Several cases are detected late because of lack of awareness of the condition, nonspecific clinical symptoms and non-characteristic imaging findings. TB has potential to damage joints and disease sequelae may result in extensive loss of joint motion. The affection of growing physis may further lead to progressive deformities in the growth years. Multidrug antitubercular chemotherapy (ATT) remains the anchor sheet of tubercular treatment in children.
2. Difference in pathogenesis of TB in pediatric age group
There are two different mechanisms of TB infection in children.2 In infants and very young children where there is no previous exposure to TB, the lesions in bone and joints form a primary complex very similar to other bacterial infections. This variety has multiple lesions and more often is exudative. These lesions are potentially infective as well. The other mechanism is following sensitization (hypersensitivity reaction) after a solitary (primary) lesion (pulmonary or other sites). The bacilli lie dormant at various sites after an initial haematogenous spread (secondary complexes). If the host immunity weakens, these quiescent bacilli at various sites flare up, leading to isolated/multiple OA lesions.
3. Differential diagnosis and risk factors
TB can mimic various clinical conditions, infections and lesions (Fig. 1, Fig. 2, Fig. 3). Some clinical conditions which can have TB as their primary etiology are pathological fractures, non unions, dislocations, arthritis, ankylosis, instability, limb deformity, osteomyelitis, neurological deficits and avascular necrosis. Infections such as fungal, brucellosis, sarcoidisis and leprosy have several clinical features in common with TB. Risk factors include previous TB infection, immunosuppression caused by conditions such as HIV, diabetes mellitus and chronic liver or kidney failure etc.; or by immunosuppressive drugs such as long-term corticosteroids given for conditions such as kidney or pulmonary pathologies.
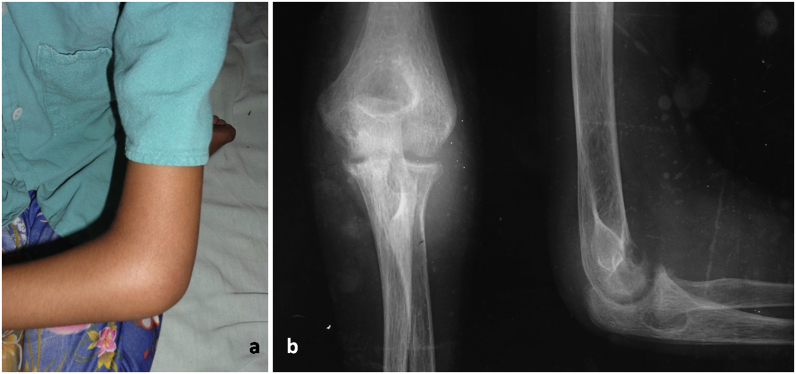
Fig. 1.
“Ice cream scoop” appearance in TB elbow. A) The clinical presentation. B) The proximal ulnar involvement with formation of above radiological sign.
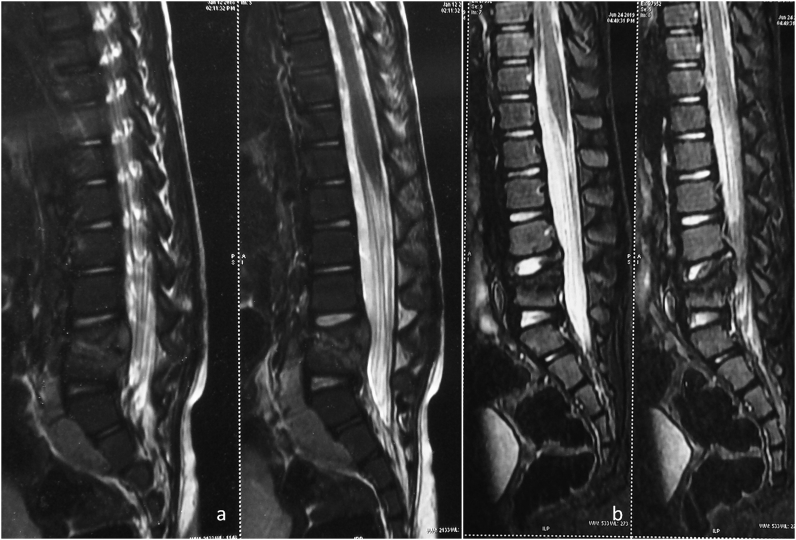
Fig. 2.
TB lumbar spine (L4, L5) in a 4 year child. A) Collapse of vertebra along with large pre and para vertebral collections. The patient was managed conservatively with rest and multidrug ATT. No surgical procedure was done. B) Post completion of ATT, bone marrow oedema reduced, the prevertebral and paravertebral collections resolved. The collapsed vertebrae and growth plates can produce spinal deformities during the growth of the child and therefore the child needs to be kept in supervised follow up.
Fig. 3.
TB osteomyelitis of left tibia in a 2 year old female child. A) Inflammation and swelling of the leg. B) Plain radiographs showing a diaphyseal involvement with sclerotic cortex on both sides and onion peel appearance. Common differential diagnosis included chronic osteomyelitis and malignancy. C) The MRI delineated the extent of the pathology, showed the soft tissue component. The tubercular diagnosis was however established by histopathology only.
4. Classical regional presentation
4.1. Shoulder
Shoulder TB is less frequent in paediatric age group. There are 2 main varieties of shoulder TB: caries exudata (abscess form) and caries sicca (dry form).3 Caries exudata manifests as cold abscess and swelling and is more common in children. Caries sicca, the uncommon variety, manifests as marked wasting and painful movement restriction. Often there is progressively deteriorating, insidious, dull, aching pain in the shoulder region and restricted movement in the latter variety. Imaging may reveal regional osteopenia and/or lytic bony lesions.
4.2. Elbow
Elbow TB is common in children and the disease is fairly advanced at the time of diagnosis. The presentation is usually exudative with abscess formation. The proximal part of the ulna is the most common site of involvement. Other site of involvement can be distal humerus, or proximal radius. An radiological ‘‘ice cream scoop’’ appearance of proximal ulna should raise suspicion for a tubercular etiology (Fig. 1).4,5
4.3. Wrist and hand
The presentation of paediatric wrist TB is usually with pain, swelling sometimes associated with abscess formation, and sinuses.6, 7, 8 TB of this region have the propensity to cause movement restrictions (pronation and supination as well) or chronic pain. There is a growing distal radial epiphysis in the vicinity which may lead to growth restrictions and deformities. Imaging usually reveals poorly defined radiolucent lesions or distinct cavities with minimal marginal sclerosis in distal radius. Sometimes with carpal involvement, there is a rheumatoid like involvement with decreased joint space.
There is an increased chance of surgery or failure of conservative treatment in paediatric wrist TB lesions if there is delay in starting of treatment beyond 10 weeks; ESR is raised more than 68 mm/h; the presentation is in form of skin ulceration or sinus or there are multiple bone lesions.6 For small ill-defined lesions, curettage and multidrug anti-tubercular chemotherapy alone results in excellent outcome. Large lytic lesions may require additional bone grafting if associated with risk of pathological fracture.7,8
The usual clinical presentation in distal hand and finger digits is a spindle shaped swelling of the joint and flexion deformity. The disease is common in young with age <5 years. Discharging sinus may or may not be present. Often multiple digits are involved or form part of multifocal presentation with lesions in other part of the body.
The classical radiological presentation for metacarpals and phalanges (short tubular bones) is spina ventosa. The description refers to spindle shaped expansion of the diaphyseal bone segment due to successive layering of subperiosteal bone over involved lamellae or sequestrum. Other presentation can include honey combing, diffuse infiltration or cystic lesion.
4.4. Hip
The presentation in a child is with pain, limp and restriction of movements. Sometimes the disease is brought to attention by referred pain in the knee region.
The hip disease is classically described to progress through following stages:
-
1.
Synovitis. There is pain and limping. Hip movements are restricted. The limb is the attitude of flexion, abduction and external rotation to accommodate the joint effusion. The synovitis stage requires differentiation from traumatic synovitis, rheumatoid etiology, transient synovitis, Perthes’ disease and other causes of ‘irritable hip’.
-
2.
Early arthritis. With further progress of bony destruction, the limb is in attitude of flexion, adduction and internal rotation. There is presence of apparent limb shortening. Pain is now marked and wasting may be obvious. Discharging sinuses may be present.
-
3.
Advanced arthritis. Joint destruction is now advanced. Pathological dislocation or subluxation may occur. The stage is characterized by severe restriction of joint movements, marked pain, a shortened limb.
In early pathology, the only radiological finding may be soft tissue swelling with or without rarefaction of underlying bones. The advanced radiological presentation of tubercular hip in children has classically being been described according to primary site of infection viz. acetabular roof, femoral neck, epiphysis, trochanteric apophysis, synovium, undetermined. Another commonly used method is description by Shanmugasundaram 7 types (normal, travelling acetabulum, dislocating, Perthes, protrusio-acetabuli, atrophic, mortar and pestle).9 In a retrospective study involving 27 paediatric hips, Agarwal et al. showed that there are many radiological types, not previously described, are present in children. Further, functional outcome is independent of radiological morphology of the hip in smaller children.10
4.5. Knee
The disease can affect synovium, epiphysis or metaphyseal region. The TB of knee regions commonly manifests as wasting of regional muscles, a boggy joint swelling, and effusion. Tenderness is most marked along the joint line and synovial reflections. The epiphyseal plate offers little resistance to the spread of the tubercular focus.11 Therefore epiphyseal lesions (proximal tibia and distal femur) are common in knee region. In epiphyseal variety (as compared to synovial variant), joint space is not reduced at the initial presentation unless the lesion is extensive.
4.6. Foot and ankle
Pain, limp and swelling are earliest manifestations in the ankle region. Fullness can be appreciated on the dorsum, around the malleoli and on posterior aspect on the side of Achilles tendon. There is associated plantar flexion deformity. For the ankle and joint region, much different radiological appearances are reported.12, 13, 14 In ankle joint, scalloped lesions may form on adjacent articular surfaces, giving an appearance of ‘kissing’ lesions. Coalescence of multiple intercommunicating small joints of the foot may give the appearance of a rheumatoid mass. Other described varieties are cystic, subperiosteal, and spina ventosa.
In foot, calcaneum, talus, midtarsal bones, metatarsals or phalanges may be involved. In calcaneal involvement, the child typically has antalgic gait and a ‘heel raise sign’ due to heel tenderness. Many a times, endarteritis of nutrient artery may result in formation of lytic cavity with or without a ‘coke like sequestrum’ visible on plain radiographs.
4.7. Spine
A persistent stiff spine or backache in a child requires investigation for TB spine. The gait may be cautious or the child may use of hands to support the head or trunk if there is spine involvement. Sometimes very obvious paraspinal abscess and or sinuses are present. A knuckle deformity with or without associated neurological involvement is another common presentation for TB spine in our country. The radiological appearance will depend on number of vertebrae involved, and type of lesion (paradiscal, central, anterior, appendicular or skip lesions). Higher imaging (CT and MRI) is often needed to delineate lesion in junctional areas like occipitocervical, cervicodorsal and lumbosacral regions. In junctional spinal tuberculosis, the role of MRI in diagnosis is more informative than CT scan in the early stages. The spinal TB in children is a different disease entity than in adults. The vertebral bodies in children are cartilaginous. Hence, whenever a tubercular infection affects the vertebral bodies, the cartilage loss occurs rapidly and consecutively, severe deformities occur within a short period of time (Fig. 2). Younger the child, more severe is the expected deformity. Several reports now recommend use of instrumentation along with debridement and fusion in acute stage of disease.15,16
5. Atypical TB presentations in pediatric age group
5.1. Acute presentation
The acute presentation of TB match the duration (days-weeks) and the systemic signs of an acute suppurative infection.17 Differentiating this variety from septic arthritis and acute pyogenic infections is difficult as these are also common in this age group. The diagnosis is commonly missed on typical aerobic and anaerobic cultures, if tubercular etiology is not suspected. Many a time, the acute abscess has been incised and drained in the mistaken diagnosis of acute suppurative infection.
The acute presentation of TB is generally a hypersensitivity reaction to a previous exposure. As such, many of these patients may exhibit scar marks of old healed TB. There is involvement of superficial bones and joints such as phalanges, metacarpals, clavicle, sternum, shoulder joint etc. The abscess/collection is therefore, manifested early, clinically. The condition warrants awareness of this atypical form, a precise and methodical clinical assessment and support of dedicated laboratory facility to aid in diagnosis. When the suspicion is high (clinical manifestation as above) or in areas where TB is present in endemic proportions, it is suggested that samples, FNAC, aspirate be sent for Ziehl–Neelsen staining/specialized tubercular testing prior to drainage/debridement procedure. A smear positive for acid fast bacteria reveals the diagnosis early in many cases. In some patients with an identifiable radiological lesion, FNAC/trocar biopsy can decompress an abscess and obtain tissue for diagnosis. Not to mention here, that sometimes the tubercular pathogenesis is made entirely retrospectively on culture or histopathology report.
5.2. Multifocal presentation
Multifocal presentation accounts for 5–10% of all OA cases.18 Lesions may demonstrate different stages of destruction/healing. All lesions may not be symptomatic. This reason is interplay between the virulence of the bacilli and local/general immunity of the host. The number of osseous lesions usually is 4–6. Treatment for multifocal presentation is similar to that for solitary lesions.
5.3. Epiphyseal and metaepiphyseal tubercular osteomyelitis
Typical osseous lesions of pediatric OA TB are usually situated in the metaphyseal region. However, rarely the lesion can cross the physeal plate and lie in the epiphysis (especially the knee region). This happens especially in small children where the transphyseal vascular canals are open.19 Being uncommon and less symptomatic, the diagnosis is often delayed. The epiphyseal lesions prompts several other differential diagnosis such as primary epiphyseal or apophyseal subacute osteomyelitis (PEASAO), chronic osteomyelitis, cartilaginous tumours, osteoid osteoma, simple and aneurismal bone cysts, haematological disease, and certain malignant tumours.
5.4. Cystic TB
Erol et al. reported 8 children with histologically proven solitary cystic TB of the proximal tibia and distal femur.20 Average age at presentation was 4 years (range, 2–6 years). A primary diagnosis of a bony tumor was made before referral to author’s institution. The lesions were metaphyseal but crossed epiphysis in 3 patients. The condition was treated with curettage without bone grafting. A follow up of 4 years showed a preserved epiphyseal growth in the particular series.
6. Diagnosis
6.1. Imaging
Imaging findings are non-specific in OA paediatric TB. Plain radiographs, USG, CT scan, MRI, bone scans, PET or other imaging modalities can be used to detect and delineate a probable lesion. However, imaging is indispensable in providing the extent of involvement, soft tissue component, skip lesions, investigation of difficult areas e.g. pelvic or vertebral region and to obtain a guided biopsy (Fig. 3).
Both suppurative and tubercular lesions can have similar radiological presentation. The joint space may be normal or increased following an effusion. Associated periarticular soft tissue swelling signify oedematous tissues/and collections. Concomitant osteomyelitis changes in adjacent bones may also be present.
As infection progresses, regional osteopenia, decrease in joint space and articular erosions may become manifest. Sometimes, the presentation can be in form of complications e.g. subluxation and dislocation.
6.2. Laboratory
The hematological investigations for OA TB are again nonspecific. Serial estimations of haemogram, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), liver and kidney function test are used to monitor the disease activity and general well being of the patient while on antitubercular treatment. Estimation of Anti TB antibodies (IgM and IgG) are not considered useful for diagnostic evaluation in OA TB. The various other commonly used laboratory tests for extrapulmonary TB are listed in Table 1. More recently, molecular analysis test such as Xpert MTB/RIF assay are being increasingly used because of their comparable diagnostic efficacy and faster results.21
Table 1.
Commonly used laboratory tests for extrapulmonary tuberculosis.
| Test | Sensitivity | Time taken | Remarks |
|---|---|---|---|
| AFB staining | 10–30% | – | Non tubercular bacteria may stain similarly |
| Conventional solid media (LJ) | 30–80% | 6–8 weeks | Gold standard |
| Mycobacterial Growth Indicator tube (MGIT) 960 | 97% | 2–4 weeks | Gold standard |
| Histopathology | 72–97% | Tissue processing required | Gold standard |
| Interferon gamma release assay: QuantiFERON –TB; T SPOT | 60–83% | 24 h | Indicate cellular response to specific microbial antigens. ATT based on these tests is not warranted. |
| Molecular analysis e.g. PCR, Xpert MTB/RIF assay | 61–83% | 24 h | Extraction and amplification of target gene and DNA. ATT based on PCR is investigational and clinical/histopathology correlation is advised |
Sample collection: The clinician should try to obtain as much pathological material while planning a biopsy from a probable tubercular lesion. An image guided biopsy may yield better tissue for diagnosis. Possible tissues can be skin edge, pus, granulation tissue, soft tissue, bone curetting, lymph nodes, joint fluid, synovial tissue, and other involved sites. Whenever feasible, these samples should be subjected to multiple laboratory tests (acid fast staining, culture, histopathological examination, molecular analysis etc.). The entire sample should be processed for the laboratory investigations.
6.3. Clinico-radiological diagnosis
In developing countries in general, the diagnosis of OA TB can be reliably made on clinical and radiological examinations.1 However where possible, all patients should have a biopsy of the lesion to provide a specimen for culture to confirm the diagnosis and perform drug susceptibility testing, and to rule out other diagnoses.
7. Treatment
The main treatment for extrapulmonary TB is multidrug antitubercular chemotherapy (ATT) (Fig. 2). Analgesics, rest, immobilization, splintage, braces are also necessary in early stages. As soon as inflammation and pain is controlled, patients should be encouraged to start joint mobilization to regain/retain useful range of motion. Tubercular osteomyelitis, if advanced, requires protection to prevent pathological fractures. Most patients also require nutritional/built up therapy. The indications of surgical intervention in OA TB are detailed below.
While prescribing the treatment for TB, it is necessary to ensure that the patient receives the right (genuine) drug in right (correct) dosage, the combination of antitubercular drugs used is right (sensitive drugs), drugs are given for the right (total) duration and the entire course is completed uninterrupted. According to Index TB Guidelines 2016, the following treatment regime is recommended for extra pulmonary TB (including bone and joint TB): a 2-month intensive phase consisting of four drugs (isoniazid, rifampicin, pyrazinamide and ethambutol), followed by a continuation phase lasting a minimum 10 months [2RHZE/10RHE] (which is extendable to 18 months on a case by case basis, depending on the site of disease and the patient’s clinical response).22
According to the previous guidelines, drug treatment for drug sensitive TB was an intermittent regimen with 2 categories of treatment: an Intensive phase (IP) for 2–3 months followed by Continuation phase (CP) for 4–5 months. Drugs were to be taken three times a week. Dose administration under supervision was one of the key components of these old guidelines. There has been a paradigm shift in technical and operational guidelines for Tuberculosis Control Programme in India, 2016.23 In the revised guidelines, a daily dosing schedule according to appropriate weight band has been incorporated. The duration of the treatment in bone and joint TB has been extended to minimum 1 year. There is more emphasis on follow up (both clinical and laboratory investigations) and a long term monitoring up to 2 years has been added.
7.1. Role of surgery
A surgical procedure may be indicated in TB primarily to obtain a tissue and establish correct diagnosis. The procedure be imaging guided for regions with a difficult assess e.g. spine, deep joints etc. The tissue obtained can also help determine bacterial sensitivity and permit administration of appropriate antibiotics. In some situations, the surgical requirement may be emergent e.g. to decompress a bulky abscess (difficulty in breathing or swallowing as might occur in presence of large cervical TB collections, impending bursts in any region etc.). Surgery is also indicated if patient is not responding after 4–5 months of supervised chemotherapy, again to establish diagnosis or determine bacterial sensitivity.22
Spinal TB holds a peculiar position as far as surgical procedures are concerned.22 Surgical intervention may be needed if there is gross neurological deficit at presentation, neurological deficit is of very recent origin, there is evidence of instability or when the neurological deficit interferes with patient mobilization/nursing (e.g. quadriplegia or paraplegia). With advancement in spinal stabilization instrumentation and subtraction techniques, surgery is also indicated for correction of post tubercular kyphotic or scoliotic deformities, both in acute and late stages. Late onset neurological deteriorations often also need surgical decompressions.
TB can result in many sequelae and surgery may be indicated in late stages to correct limb deformities, restore joint functions (e.g. to produce a sound ankylosis, excision arthroplasty of hip or elbow etc.).1
7.2. Non-responders
There is a certain percentage (5–10%) of patients who do not respond to standard treatment for TB.1 Possible causes of deterioration on treatment or failure to improve on treatment include poor adherence to ATT, drug resistance, paradoxical reaction (an initial improvement, followed by deterioration), immune reconstitution syndrome associated with HIV, alternative diagnosis – patient does not have TB or has two diagnoses.22 A patient is generally labeled as non-responder if he/she has not shown expected clinico-radiological response after completing at least 5 months’ ATT, there is persistence or worsening of local and systemic symptoms and signs, there is no improvement, or deterioration of the lesion on repeat imaging, new lesions (non-healing ulcer/sinus/abscesses/lymphadenopathy) appear while the patient is on ATT or there is wound dehiscence post-operatively. Such patients require a multispecialty workup preferably in consultation with an infectious disease expert. Ensuring a good general health and diet, intake of genuine medications, correct medicine dosage and right combination of drugs can aid in treatment of such patients.
7.3. Healed status and outcome
The healed status in OA TB is judged clinico-radiologically. The pathology is considered healed after if the patient has completed the designated course of ATT and there is no relapse of disease at 2 years’ follow up.22 Clinically, fever, night sweats, weight loss (if initially present) and sinuses/ulcers (if initially present) should resolve. Radiological signs of bone healing include remineralisation of affected bone and sharpening of joint/vertebral margins. On MRI, healing is manifested as resolution of marrow oedema, fatty replacement in marrow and no contrast enhancement of the lesion.
In general, the shorter is the symptom treatment time, better is the prognosis. Pure synovial involvement and early or low grade arthritis also have more favourable prognosis than advanced disease stages.
8. Conclusions
TB is endemic in Indian subcontinent. TB can have varied presentation and therefore it is essential to keep tubercular infection in differential diagnosis while working up for any infective pathology. Where possible, all patients should have a biopsy of the lesion to provide a specimen for culture to confirm the diagnosis and perform drug susceptibility testing, and to rule out other diagnoses. The main treatment for paediatric OA TB is non-operative and possible with multidrug antitubercular chemotherapy.
Financial conflicts
Nil.
Declaration of competing interest
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
References
- 1.Tuli S.M. General principles of osteoarticular tuberculosis. Clin Orthop Relat Res. 2002;398:11–19. doi: 10.1097/00003086-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Campos O.P. Bone and joint tuberculosis and its treatment. J Bone Joint Surg Am. 1955;37-A:937–966. [PubMed] [Google Scholar]
- 3.Agarwal A., Kumar A., Shaharyar A., Bhat M.S. Shoulder tuberculosis in children: a report of two cases. J Orthop Surg (Hong Kong) 2015;23:398–401. doi: 10.1177/230949901502300330. [DOI] [PubMed] [Google Scholar]
- 4.Agarwal A., Mumtaz I., Kumar P., Khan S., Qureshi N.A. Tuberculosis of the elbow joint in children: a review of ten patients who were managed nonoperatively. J Bone Joint Surg Am. 2010;92:436–441. doi: 10.2106/JBJS.I.00805. [DOI] [PubMed] [Google Scholar]
- 5.Agarwal A., Rastogi A. Tuberculosis of the elbow region in pediatric age group - experiences from a single centre. J Hand Surg Asian Pac. 2017;22:457–463. doi: 10.1142/S0218810417500502. [DOI] [PubMed] [Google Scholar]
- 6.Prakash J., Mehtani A. Hand and wrist tuberculosis in paediatric patients - our experience in 44 patients. J Pediatr Orthop B. 2017;26:250–260. doi: 10.1097/BPB.0000000000000325. [DOI] [PubMed] [Google Scholar]
- 7.Agarwal A., Qureshi N.A., Kumar P., Khan S. Tubercular osteomyelitis of metacarpals and phalanges in children. Hand Surg. 2011;16:19–27. doi: 10.1142/S0218810411005011. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal A., Kant K.S., Kumar A., Shaharyar A., Verma I., Suri T. Lytic lesions of distal radius in children: a rare tubercular presentation. Hand Surg. 2014;19:369–374. doi: 10.1142/S0218810414500294. [DOI] [PubMed] [Google Scholar]
- 9.Shanmugasundaram T.K. Kothandaram and Co.; Madras: 1983. Bone and Joint Tuberculosis. [Google Scholar]
- 10.Agarwal A., Suri T., Verma I., Kumar S.K., Gupta N., Shaharyar A. Tuberculosis of the hip in children: a retrospective analysis of 27 patients. Indian J Orthop. 2014;48:463–469. doi: 10.4103/0019-5413.139852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kant K.S., Agarwal A., Suri T., Gupta N., Verma I., Shaharyar A. Tuberculosis of knee region in children: a series of eight cases. Trop Doct. 2014;44 doi: 10.1177/0049475513512633. 29-3. [DOI] [PubMed] [Google Scholar]
- 12.Mittal R., Gupta V., Rastogi S. Tuberculosis of the foot. J Bone Joint Surg Br. 1999;81:997–1000. doi: 10.1302/0301-620x.81b6.9925. [DOI] [PubMed] [Google Scholar]
- 13.Rasool M.N. Osseous manifestations of tuberculosis in children. J Pediatr Orthop. 2001;21:749–755. [PubMed] [Google Scholar]
- 14.Dhillon M.S., Nagi O.N. Tuberculosis of the foot and ankle. Clin Orthop Relat Res. 2002;398:107–113. doi: 10.1097/00003086-200205000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Hu X., Zhang H., Yin X., Chen Y., Yu H., Zhou Z. One-stage posterior focus debridement, fusion, and instrumentation in the surgical treatment of lumbar spinal tuberculosis with kyphosis in children. Childs Nerv Syst. 2016;32:535–539. doi: 10.1007/s00381-015-2948-3. [DOI] [PubMed] [Google Scholar]
- 16.Hu J., Li D., Kang Y. Active thoracic and lumbar spinal tuberculosis in children with kyphotic deformity treated by one-stage posterior instrumentation combined anterior debridement: preliminary study. Eur J Orthop Surg Traumatol. 2014;24(Suppl 1):S221–S229. doi: 10.1007/s00590-014-1440-1. [DOI] [PubMed] [Google Scholar]
- 17.Agarwal A. Acute suppurative presentation of osteoarticular tuberculosis in children. Indian J Tubercul. 2011;58:66–71. [PubMed] [Google Scholar]
- 18.Agarwal A., Khan S.A., Qureshi N.A. Multifocal osteoarticular tuberculosis in children. J Orthop Surg (Hong Kong) 2011;19:336–340. doi: 10.1177/230949901101900315. [DOI] [PubMed] [Google Scholar]
- 19.Agarwal A., Gupta N., Mishra M., Agrawal N., Kumar D. Primary epiphyseal and metaepiphyseal tubercular osteomyelitis in children A series of 8 case. Acta Orthop Belg. 2016;82:797–805. [PubMed] [Google Scholar]
- 20.Erol B., Topkar M.O., Basar H., Caliskan E., Okay E. Solitary cystic tuberculosis of the distal femur and proximal tibia in children. J Pediatr Orthop B. 2015;24:315–320. doi: 10.1097/BPB.0000000000000193. [DOI] [PubMed] [Google Scholar]
- 21.Held M., Laubscher M., Mears S. Diagnostic accuracy of the Xpert MTB/RIF assay for extrapulmonary tuberculosis in children with musculoskeletal infections. Pediatr Infect Dis J. 2016;35:1165–1168. doi: 10.1097/INF.0000000000001271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ministry of Health & Family Welfare-Government of India . 2016. Index TB Guidelines.https://tbcindia.gov.in/showfile.php?lid=3245 [Google Scholar]
- 23.Chaudhuri A.D. Recent changes in technical and operational guidelines for tuberculosis control programme in India - 2016: a paradigm shift in tuberculosis control. J Assoc Chest Physicians. 2017;5:1–9. [Google Scholar]