Abstract
Very few cases of simultaneous occurrence of tibial tuberosity fracture with lower pole patella and distal patellar tendon rupture type injuries have been reported in adolescent athletic age group, but its occurrence in osteogenesis imperfecta (OI)* has not been reported to the best of our knowledge in a literature search of last 5 years in the English Language. The mechanism of avulsion injury after low-velocity trauma and the underlying pathology is a unique combination in our patient and a note on updates in general management of osteogenesis imperfecta is discussed.
Keywords: Osteogenesis imperfecta, Tibial tuberosity fracture, Patellar tendon rupture
Abbreviations: OI, Osteogenesis Imperfecta; TT, Tibial Tuberosity; PT, Patellar Tendon
1. Introduction
Over 230 cases of tibial tubercle (TT) avulsion fracture in adolescents have been reported in the past since it was first reported in 1853; a few have reported bilateral occurrence.1 The incidence of the patellar tendon (PT) rupture is rare in this age group and only a few cases have been reported.2 Over 15 cases have been reported where there is a simultaneous occurrence of the tibial tubercle and patellar tendon rupture. To the best of our knowledge, this is a first reported case of simultaneous injurty to PT and TT in a pre-pubertal case with osteogenesis imperfecta.3 We report a case of an 11 year old child having Osteogenesis imperfecta who was ambulant but not very active in sports, who sustained simultaneous TT avulsion fracture and PT rupture with a trivial trauma, its successful management and follow up. Additionally a brief review of literature on current treatment concepts in OI has been mentioned.
2. Case report
An 11-year-old male presented to the emergency department with history of pain and swelling of the left knee after minor tripping and fall following which he couldn’t walk. He had no other injuries. The patient, who was known to have OI, had a history of multiple un-displaced fractures including that of humerus, metacarpals, tibia and foot bones which were managed conservatively and healed well with good alignment in the past at a space of once in 3 years. The patient had a pixie face, blue sclera and very mild hearing loss due to otoscelrosis. The patient was not on any medical management in the form of bisphosphonates due to an extremely low rate of fractures per year in the past. The patient’s mother, maternal cousin and her son had OI. On examination, it was tender over tibial tubercle and he was not able to perform straight leg raise test.
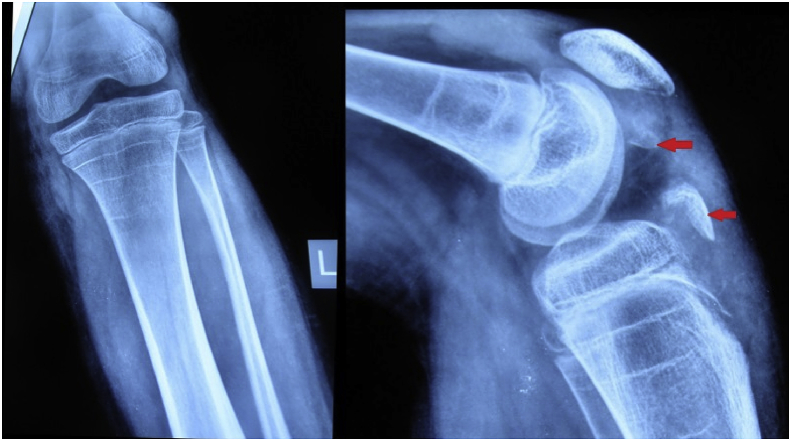
Radiograph suggestive of the tibial tubercle and lower pole patella fracture, see Fig. 1 and MRI confirmed fractures and showed a partial distal patellar tendon avulsion (Fig. 2).
Fig. 1.
Radiograph showing tibial tubercle fracture and lower pole patella fracture.
Fig. 2.
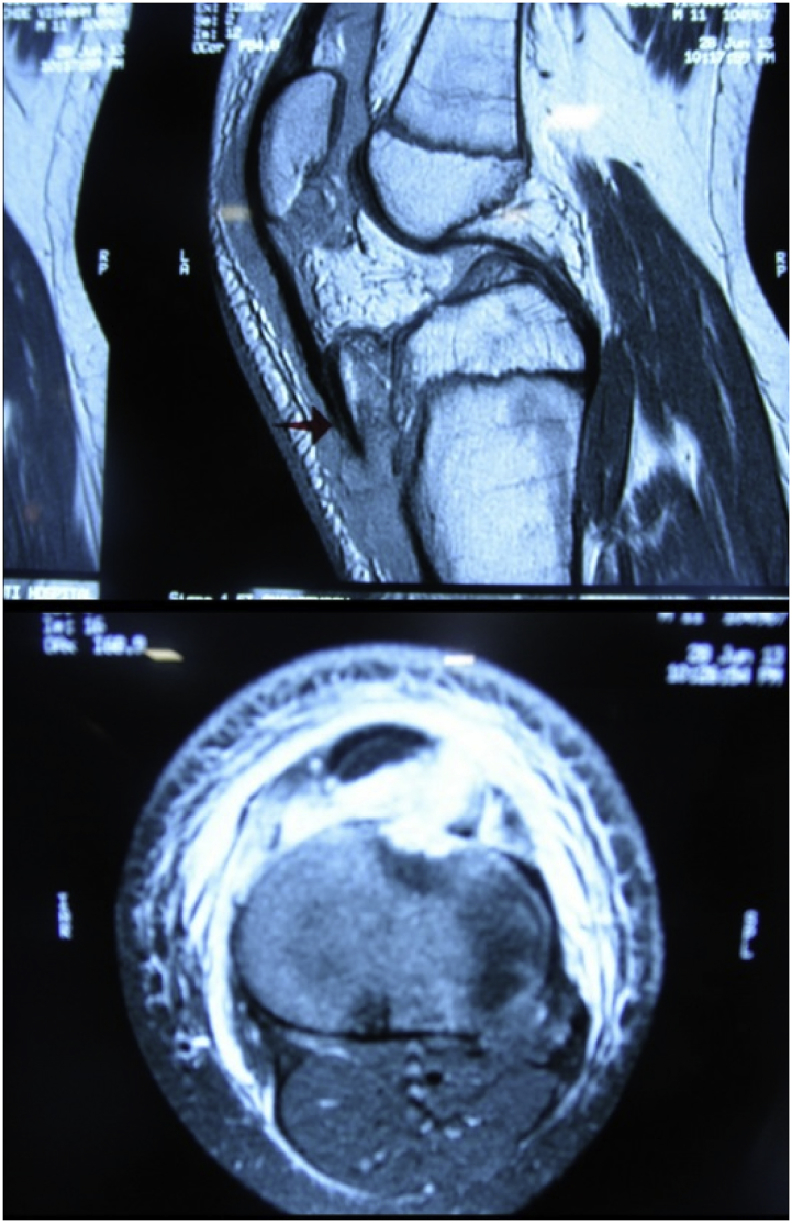
MRI scan suggestive of tibial tubercle avulsion fracture and patellar ligament avulsion.
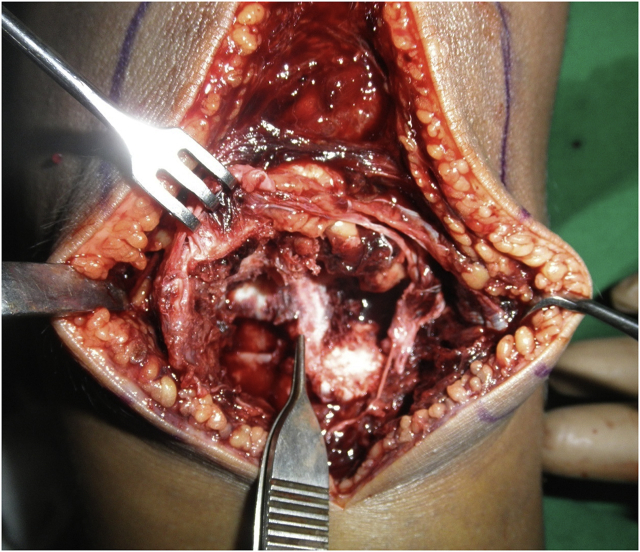
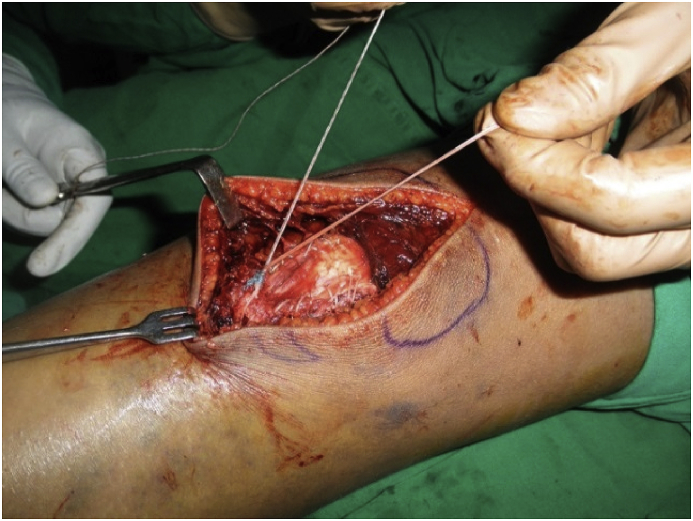
The pre-operative workup was done and he underwent open reduction and internal fixation of the fracture. Anterior approach was used with a midline incision over tibial tubercle and patellar tendon, tibial tuberosity fracture was identified (Fig. 3) and fixed with two 4.0 mm cannulated cancellous screws (Fig. 5). One fiber wire suture with Krachow stitches and anchor was used for patellar tendon rupture repair as shown in Fig. 4. The lower pole of patella fracture was treated conservatively. In the postoperative period, immobilization was given for 6 weeks and later physiotherapy was initiated to gain full range of movement by the end of 6 months.
Fig. 3.
Intra-operative picture showing tendon rupture and tibial tubercle fracture.
Fig. 5.
Post-operative radiograph, arrow showing healed lower pole patella fracture united with conservative treatment.
Fig. 4.
Intra-operative picture after suture anchor repair.
2.1. Follow up
The patient recovered well and gained functional recovery at the end of 6 months (Fig. 6). At about follow-up after seven years radiographs suggested united fracture and anterior tibial slope of eight degrees (Fig. 7) and clinically he had a good range of motion and a ten-degree-recurvatum was noted (Fig. 8), as the patient had no symptoms patient’s family did not want any treatment for it.
Fig. 6.
Showing functional movement at 6-month follow-up.
Fig. 7.
Radiograph after 7 years of follow-up after injury.
Fig. 8.
Clinical photographs on 7 years of follow-up after injury.
3. Discussion
Incidence of simultaneous TT avulsion fracture and PT avulsion is extremely rare. D.H.Y.Tai et al., in 2016 reported such a case that was associated with tyrosine hydroxylase deficiency and also discussed about 11 such cases.4 In 2018, Yousef MAA5 reported a case series of 3 patients with combined TT avulsion fracture and PT rupture injury. This is the first instance reported where there is simultaneous TT avulsion fracture and PT rupture injury in a patient with osteogenesis imperfecta.
Osteogenesis imperfecta or the brittle bones disease is a genetic generalized connective tissue disorder due to mutation in the genes encoding type I collagen. Patients with this disorder have osteoporotic and fragile bones increasing the risk of a long bone or spine fracture, deformities of long bones and spine. It is associated with other non-orthopedic issues like blue sclera, dental issues, hearing impairment and others symptoms as they manifest according to a range of clinical severity.6
The incidence for the occurrence of such injuries peak between the age of 12–15 and mainly associated with sports injuries where there is continued violent contraction of Quadriceps muscle even after the fracture occurred or violent flexion of the knee in opposition to hardly contracted Quadriceps muscle while the foot is fixed on the ground.5 Our patient had a history of mild osteogenesis imperfecta with a relatively high level of ambulant activity as compared to the other types. He is ambulatory without protective braces and was not given bisphosphonates due to relatively low fracture frequency per year, which could be the reason of having such injury after a trivial fall. In the review of literature, tendon rupture injury is seen less frequently although there are few reports of quadriceps, Achilles tendon rupture and mid substance PT rupture related to osteogenesis imperfecta.7
The relevance of Osteogenesis Imperfecta in this case is that the fact that mild varieties burn out by adolescence is well known. However till the skeleton fully matures : the give away occurs in the event of a traumatic force happens at a potentially weak area which in this case is the traction apophysis and hence the tuberosity got avulsed due to a violent pull.The TT avulsion fractures are classified by Ogden et al.8 into types I, II and III and subtypes A and B depending on the degree of comminution. Frankl et al.9 added a subtype C where there is associated PT rupture; this patient had a type 2C injury. These can be associated with patellar tendon avulsion, quadriceps tendon avulsion, meniscal injury and cruciate ligament injury.4
The diagnosis of PT rupture in a with TT fracture is very important where on plane radiographs Patella can be seen high riding increasing the distance between the distal pole of the patella and avulsed TT fragment, MRI helps in confirming the diagnosis.5
The treatment of these injuries has been described to consist of open reduction and internal fixation of TT fracture usually with compression screws and surgical repair of the avulsed PT. There are numerous ways described for reinsertion of PT tendon using staples, trans-osseous suturing, figure-of-eight tension band wiring, cerclage wire and suture anchor augmented with protective wire loop5. We used two compression screws with washers because of the osteoporotic bone and a suture anchor with the repair of PT ligament. The main thing one should avoid is patella baja or patella alta for which the Insall-Salvati ratio can be taken into consideration.
S.T. Nathan10 reported a case with 25° of recurvatum after open reduction and internal fixation of TT fracture as a complication because of injury to the growth plate. Similarly, when the patient in our report came for follow up after seven years, it was noted that the patient had ten degrees of recurvatum and reason is thought to damage of the growth plate at time of initial injury. Also an eight-degree-anterior tibial slope is noted in our case which suggests it is a bony deformity. In contrast to the case reported by Nathan, the recurvatum was left alone as he was asymptomatic.
3.1. Review of current treatment options from paediatric orthopedics point of view for osteogenesis imperfecta
Osteogenesis imperfecta is a genetic disorder of quantitative or qualitative synthesis of collagen 1 which has a widespread distribution in normal individuals. Because of this, there are several skeletal and extra-skeletal manifestations. It can be classified in number of ways and is controversial. The genetic classification includes the classical Sillence type I to type IV which was described in 1979, and the list has grown unto 18 types as new mutations are still being discovered. It can also be classified depending upon the grade of severity as mild (type I), moderate (type IV), severe (type III) and extremely severe (type II).11,12
The diagnosis of osteogenesis imperfecta is dependent on clinical and radiological features and is generally done by experts based on the study of radiographs of long bones and skull in addition to evaluation of dentition. The general signs include short stature, relative asymmetric macrocephaly, blue-sclera, typical facial and thoracic configuration, hearing impairment, scoliosis and sarcopenia.12
The treatment of osteogenesis imperfecta essentially depends on its type, age of the patient and should be multi-disciplinary.13 There is no cure for this disease and the main aim of treatment is to optimise the current health status and treat the symptoms and its complications. When dealing with extremely severe or lethal form the disease which is picked up as one or more fractures prenatally on ultrasonography the main aim is to provide supportive treatment as it is a life-threatening condition and majority of neonates with this condition perish in – weeks. Pre-implantation diagnosis is available for couples with strong positive family history.12
When a patient has moderate to severe osteogenesis imperfecta the main problems are multiple fractures, deformities, disabilities and pain. This calls for an expert multidisciplinary team approach which includes professionals from paediatrics, orthopaedics, physiotherapy, orthotics, genetics, dentistry and otology and individualised delivery of care suitable for the patient. While a patient with a mild disease seldom has deformities, but has issues of fractures that are generally treated conservatively except when a fracture occurs at the same place twice or more. From Orthopaedics point of view treatment can be Non-surgical, surgical and Pharmacological.13
The surgical management is indicated in cases of recurrent fractures and severe deformities in moderate to severe osteogenesis imperfecta for upper limb, lower limb and spine and is combined with pharmacotherapy and pre and post-surgery rehabilitation. Intramedullary nails fixed length or with a telescoping mechanism such as the Bailey-Dubow, Sheffield and Fassier-Duval nails have been described to be used as plate and screw constructs are not suitable biomechanically.6 The usual principles of deformity corrections are applicable viz osteotomy to be placed at the apex of deformity, number of apices decide the number of osteotomies and depend on severity of deformity it can be performed by percutaneous or open approach. Despite modern surgical techniques and new improved implants, the re-operation rates have not changed much and the important cause can be listed as nail migration in joint, jamming of telescoping mechanism and bending of nails. Having said this it is noted that the overall activity level of these patients has improved as they can walk a short distance and manage transfer.14
Until the mutated allele is modified by gene therapy the main aim of Pharmacotherapy would be to improve bone density, alleviate pain and increase growth velocity. Amongst the agents employed currently that include bisphosphonates, denosumab, RANKL-inhibitory antibodies or cathepsin k inhibitors; bisphosphonates are considered to be standard of care. Although bisphosphonates improve bone mass they are thought not to improve the fragility of bone.15 There is no fixed regime of bisphosphonates and is controversial, Elena Monti et al. suggested cycle of three days intravenous pamidronate (dose 9 mg/kg/year) every two to four months (annual).13
4. Conclusion
Concomitant TT avulsion fracture and PT rupture is very rare, a high degree of suspicion has to be kept in mind as such diagnosis can be missed. Open reduction and internal fixation is necessary with the repair of the extensor mechanism with the restoration of the patellar height. Recurvatum can be seen after tibial tuberosity injury in a growing bone and has to be dealt with according to its severity.
Treatment of osteogenesis imperfecta is multidisciplinary and is tailored as per individual patient. The treatment is indicated in patients with symptoms or who have complications following treatment. Fractures are treated conservatively, the intramedullary nails are used for the treatment of recurrent fractures and severe deformities. Intravenous Pamidronate is used to improve bone mass and rehabilitation.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Rujuta Mehta: Conceptualization, Resources, Writing - review & editing, Project administration. Uday Mahajan: Writing - original draft, Visualization.
Acknowledgements
None.
Contributor Information
Rujuta Mehta, Email: rujutabos@gmail.com.
Uday Mahajan, Email: dr.mahajanuday@gmail.com.
References
- 1.Khodadadyan-Klostermann c, Morren R., Raschke M., Haas N. Simultaneous bilateral tibial tubercle avulsion fractures in a boy with osteogenesis imperfecta. Eur J Trauma. 2003 June;29(3):164–167. [Google Scholar]
- 2.Yousef M.A.A., Rosenfeld S. Acute traumatic rupture of the patellar tendon in pediatric population: case series and review of the literature. Injury. 2017 Nov;48(11):2515–2521. doi: 10.1016/j.injury.2017.08.069. [DOI] [PubMed] [Google Scholar]
- 3.Behery O.A., Feder O.I., Beutel B.G., Godfried D.H. Combined tibial tubercle fracture and patellar tendon avulsion: surgical technique and case report. J Orthop Case Rep. 2018 May- June;8(3):18–22. doi: 10.13107/jocr.2250-0685.1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tai D.H.Y., Lee K.B., Wong K.F. Tibial tuberosity avulsion fracture and patellar tendon avulsion: a case report. 2016 December. 21(1), 44-47. [DOI]
- 5.Yousef M.A.A. Combined avulsion fracture of the tibial tubercle and patellar tendon rupture in pediatric population: case series and review of literature. Eur J Orthop Surg Traumatol. 2018;28(2):317–323. doi: 10.1007/s00590-017-2048-z. [DOI] [PubMed] [Google Scholar]
- 6.Frazone J.M., Shah S.A., Wallace M.J., Kruse R.W. Osteogenesis imperfecta: a pediatric orthopedic perspective. Orthop Clin N Am. 2019 April;50(2):193–209. doi: 10.1016/j.ocl.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Jansen J.A., Haddad F.S. Distal patellar tendon avulsion fracture in a football player with osteogenesis imperfecta. Knee Surg Sports Traumatol Arthrosc. 2012 Feb;20(2):327–330. doi: 10.1007/s00167-011-1595-9. [DOI] [PubMed] [Google Scholar]
- 8.Ogden J.A., Tross R.B., Murphy M.J. Fractures of tibial tuberosity in adolescents. J Bone Joint Surg Am. 1980;62:205–215. [PubMed] [Google Scholar]
- 9.Frankl U., Wasilewski S.A., Healy W.L. Avulsion fracture of tibial tubercle with avulsion of the patellar ligament report of two cases. J Bone Joint Surg Am. 1990;72:1411–1413. [PubMed] [Google Scholar]
- 10.Nathan S.T., Parikh S.N. Genu recurvatum after tibial tuberosity fracture. Case Rep Orthop. 2013 April:5. doi: 10.1155/2013/952978. 2013: 952978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Dijk F.S., Sillence D.O. Osteogenesis imperfecta: clinical Diagnosis,Nomenclature and severity assessment. Am J Med Genet. 2014 June;164(6):1470–1481. doi: 10.1002/ajmg.a.36545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marini J.C., Forlino A., Bächinge H.P. Osteogenesis imperfecta. Nat Rev Dis Primers. 2018 August;3:17052. doi: 10.1038/nrdp.2017.52. [DOI] [PubMed] [Google Scholar]
- 13.Monti E., Mottes M., Fraschini P. Current and emerging treatments for the management of osteogenesis imperfecta. Therapeut Clin Risk Manag. 2010 September;7(6):367–381. doi: 10.2147/tcrm.s5932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wirth T. The orthopaedic management of long bone deformities in genetically and acquired generalized bone weakening conditions. J Child Orthop. 2019 February;13(1):12–21. doi: 10.1302/1863-2548.13.180184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marom R., Lee Y.C., Grafe I., Lee B. Pharmacological and biological therapeutic strategies for osteogenesis imperfecta. Am J Med Genet C Semin Med Genet. 2016 Decembe;172(4):367–383. doi: 10.1002/ajmg.c.31532. [DOI] [PubMed] [Google Scholar]