Abstract
Objectives:
Optical coherence tomography (OCT) is a non-invasive technique based on optical imaging with a micrometre resolution. The purpose of this study is to investigate the potential role of OCT in evaluating oral mucosa bullous diseases.
Methods:
two patients with bullous pemphigoid (BP) and one patient with pemphigus vulgaris (PV) were examined and images of their oral lesions were performed using OCT.
Results:
In OCT images, the BP blister has a clearly different morphology from the PV one compared to the blistering level.
Conclusion:
This exploratory study suggests that the OCT is able to distinguish epithelial and subepithelial layer in vivo images of healthy oral mucosa from those with bullous diseases, assisting the clinicians in differential diagnosis.The presented data are in accordance with the scientific literature, although a wider pool of cases is needed to increase statistical power. Histological examination and immunofluorescence methods remain the gold standard for the diagnosis of oral bullous diseases. In this context, the OCT can provide the clinician with a valuable aid both as an additional diagnostic tool and in the follow up of the disease.
Keywords: Optical coherence tomography, bullous pemphigoid, pemphigus vulgaris
Introduction
Oral mucosa bullous diseases are organ-specific, rare diseases characterized by autoantibodies against structural proteins that maintain cell–cell and cell–matrix adhesions in the skin and mucous membranes.1 Pemphigus vulgaris (PV) is a life-threatening, autoimmune blistering disease, characterized by intraepithelial blister formation.2 There can be molecular basis for blister formation, that would be ascribed to a loss of adhesion among epithelial cells (acantholysis), caused by circulating autoantibodies directed against intercellular adhesion structures of keratinocytes; split formation appears in the suprabasal layer, leaving a single layer of basal keratinocytes attached to the basement membrane (BM) ("row of tombstones").3 Bullous pemphigoid (BP) is the clinical phenotype of a group of rare autoimmune blistering diseases, characterized by junctional separation on the basement membrane level, causing the rise of a sub-basilar split as in other forms of pemphigoid.4 A sub-epithelial split with a chronic inflammatory infiltrate, that contains eosinophils, lymphocytes, and also neutrophils in the lamina propria5 are classical histopathological features. In a routine work, the clinical findings, integrated with histology and immunofluorescence results, represent the basis for a diagnosis. Blisters and vesicles are easy to diagnose clinically, but it can be challenging to locate the lesion with little margin of error, as well as the exact pathology of the blister. Therefore, it is important to identify the level of epidermal split for a correct diagnosis.6
In recent years, technology has developed new diagnostic techniques for the acquisition of real-time, in vivo, non-invasive images, to evaluate morphological changes in soft and hard tissue of the oral cavity. These techniques include high-frequency ultrasound,7 confocal microscopy (CM),8 and optical coherence tomography (OCT).9 Cross-sectional images of tissue can be obtained by OCT in a non-invasive way, providing high-resolution microscopic images of biological tissues,10 through the measurement of the intensity of backscattered and reflected light with axial and lateral resolution, estimated, respectively, at 13–17 and 17–22 µm. Generally, the operating mechanism of OCT is interferometer-based, with a low-coherence-length broadband light source.11 OCT can detect the light that is reflected from tissue as OCT employs infrared light, in contrast with ultrasound12 which uses sound waves. Previous studies using OCT demonstrate that it is possible to evaluate the macroscopic characteristics of epithelial, sub-epithelial, and basement membrane structures in both healthy mucous membranes and in malignant lesions.6,11
Histological and clinical characteristics of bullous diseases indicate that imaging techniques may be very helpful in providing material for early diagnosis.6,13 This group of diseases have not been extensively described, using in vivo optical imaging technologies. The purpose of the present study is to suggest that clinical diagnosis can be supported by imaging diagnosis. This preliminary study aims to explore the potential of OCT in oral mucosa bullous diseases and to examine a set of patients suffering from BP and PV, analyzing the OCT images for possible indications of the blistering level.
Methods and materials
Subjects
The Department of Oral Pathology of the “University of Campania–Luigi Vanvitelli” involved two patients with diagnosed BP and one patient with PV in the present study that has been approved by the University’s Ethical Committee. All the patients participating in the study signed a written informed consent. Three healthy volunteers (two female and one male, average age 65 ± 7,1) underwent intraoral OCT examinations in order to gather the necessary information as a reference of the normal OCT morphology of the different anatomic regions of the oral cavity.
All the involved patients were non-smokers and aged over 18. Pregnant females were excluded from this work. All of the patients did not report any other systemic diseases. Clinical evaluation, incisional biopsies and direct immunofluorescence tests were performed to all patients to provide definitive histopathological diagnoses.
OCT system
OCT is a non-invasive imaging tool that can be performed in situ and in real time. It can provide a cross-sectional evaluation of tissue microstructure. In this research, a Swept Source OCT instrument (IVS-300) by Santec™ was employed, with a grip type probe of the same manufacturer. Center wavelength was 1310 (±30) nm, axial resolution of the system was ≤12 µm (in tissue); lateral resolution was 22 µm. The default native software Inner Vision™ (Windows 7 OS based) used both two-dimensional and three-dimensional imaging mode and all images were elaborated by a native OCT viewer. The scan mode was set for 5 × 5 mm on X- and Y-axis and pixel size of 500 and Z offset 24. The OCT probe was applied directly to the oral mucosa after application of ultrasound gel with a working distance of 10 mm. OCT in also able to perform more than the intensity of back-scattered and reflected light.
Results
Two BP patients (a male aged 64, and a female aged 67, named Patient 1 and Patient 2) had desquamated gingivitis, and no other blisters or erosions on oral mucosa (Figure 1a and c). Extraoral examination did not show any other cutaneous lesions; immunoblotting showed positivity for BP antibodies, BP180 (Figure 1b and d). The PV patient (female aged 63 years, named Patient 3) presented desquamated gingivitis too, with erosions on marginal gingiva (Figure 1e), and positive Nikolsky's sign associated with a bullous lesion in the cheek mucosa close to the right retromolar trigone; indirect pemphigus antibodies were positive for DSG-3 but negative for DSG-1 antibodies (Figure 1f). Final diagnosis of BP and PV were confirmed by direct immunofluorescence.
Figure 1.
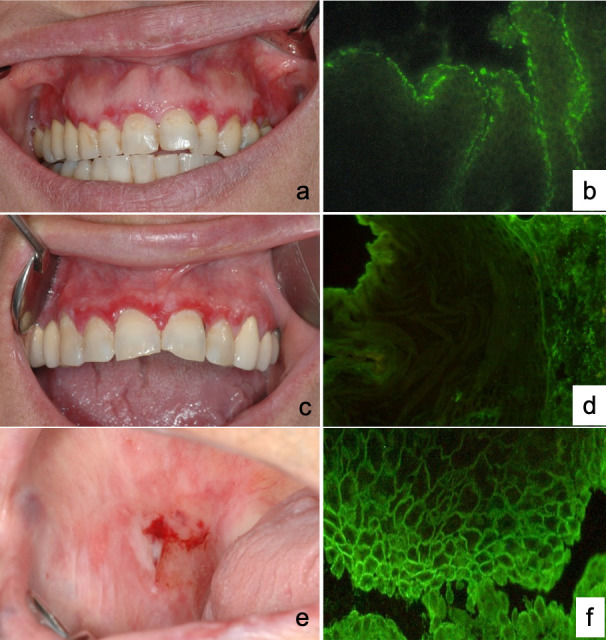
(a) Clinical photo of the BP patient (Patient 1); (b) direct immunofluorescence of the BP patient (Patient 1). (c) Clinical photo of the BP patient (Patient 2); (d) direct immunofluorescence of the BP patient (Patient 2). (e) Clinical photo of the PV patient (Patient 3); (f) direct immunofluorescence of the PV patient (Patient 3). BP, bullous pemphigoid; PV, pemphigus vulgaris.
OCT examination of healthy mucosa
The OCT examination of a healthy buccal mucosa allowed to establish clear identification of the stratified squamous epithelium (SS) along the mucosal surface, underlying the lamina propria (LP), and the transition between these tissues along basement membrane (BM) boundary. The darker appearance of the buccal mucosa epithelium is strictly related to its lower optical density and scattering properties. This is evident in a lower signal intensity. Conversely, the LP is an optically denser kind of tissue and, consequently, it appears brighter than the BM one, caused by a higher signal intensity. The thickness of the healthy epithelium is 593 ± 63 µm (Figure 2a). OCT image of the gingival mucosa slightly contrasts with its own lamina (LP) at a depth of 290 ± 29 µm. The lower contrast is typical of keratinized epithelium.11 (Figure 2b).
Figure 2.
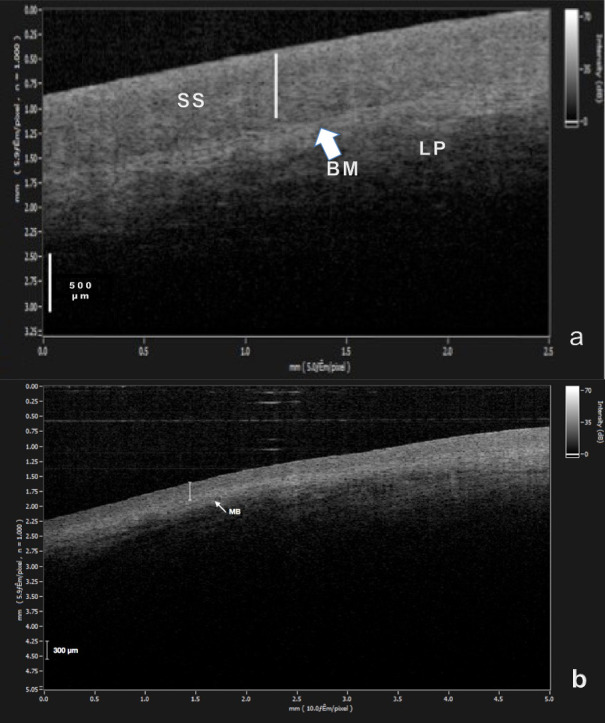
OCT images of healthy mucosa. (a) Buccal mucosa OCT image shows the stratified SS along the mucosal surface, the underlying LP and the transition between these tissues along BM boundary. Vertical bar, 500 µm. (b) Gingival mucosa OCT image shows a weak contrast with its own lamina at a depth of about 260–300 µm. The lower contrast is typical of keratinized epithelium. Vertical bar, 300 µm. BM, basement membrane; OCT, opticalcoherence tomography; LP, lamina propria; SS, squamous epithelium.
OCT examination of BP patients’ oral mucosa
OCT examination of gingival mucosa of Patient 1 shows a dark, ovoid to round, well-demarcated area due to a subepidermal blister (Figure 3a). It is circumscribed by inflammatory infiltrate (grey areas) and it is full of fluid that appears as a black area in the OCT.6
Figure 3.
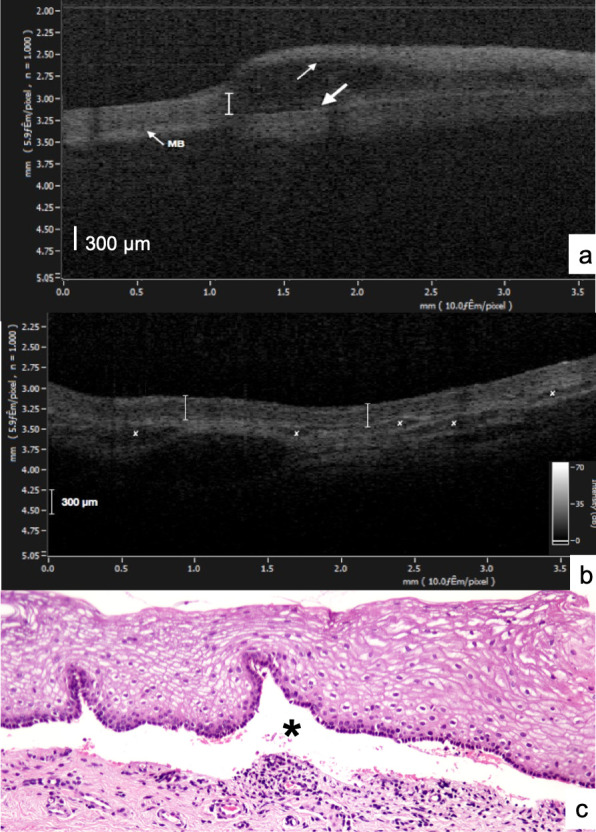
OCT images of gingival mucosa from patients with BP. (a) Subepidermal blister: epidermis is indicated by thin arrows; floor of blister by a fat arrow. A grey area at the bottom of the blister is probably due to inflammatory infiltrate. Vertical bar, 300 µm. (b) Subepidermal pattern of multiple blisters indicated by asteriks, with inflammatory infiltration as shown by the alternation of black and grey areas; the epithelial layer (300 µm), that is represented as the first horizontal band, has low contrast with the connective tissue below and seems to be well preserved. Vertical bar, 300 µm. (c) Histopathology images of the BP patient. Bulla is indicated by black asterisk. The OCT images for BP match histopathology regarding blistering and gross architecture. Magnification 10x. BP, bullous pemphigoid; OCT, optical coherence tomography.
OCT image of the second patient’s gingival mucosa (Figure 3b) exhibits a clear subepithelial pattern of multiple blisters, with neutrophil and eosinophilic infiltration characteristics, as it is shown by the alternation of black and grey areas; the epithelial layer (300 µm), represented as the first horizontal band, has low contrast with the connective tissue below and it seems to be well preserved.
In both patients, the level at which the bullae manifests is identifiable. Accordingly, considering that the average thickness of the gingival epithelium is about 300 µm, and that the bubbles are located below this thickness, it is virtually possible to discriminate a subepithelial pathology in these patients through the OCT image.
OCT examination of PV patient’s oral mucosa
OCT image shows dark superficial cavities (clefts) within the thickness of the stratified squamous epithelium as denoted by a vertical bar (Figure 4a–b). In this case is possible to distinctly identify an intraepithelial split. These intraepithelial acantholytic blisters are possibly full of fluid. The roof of the blisters appears much thinner than the well-demarcated epithelial layer above the ones observed in patients with BP; this could be explained through the intraepithelial nature of the lesion.
Figure 4.
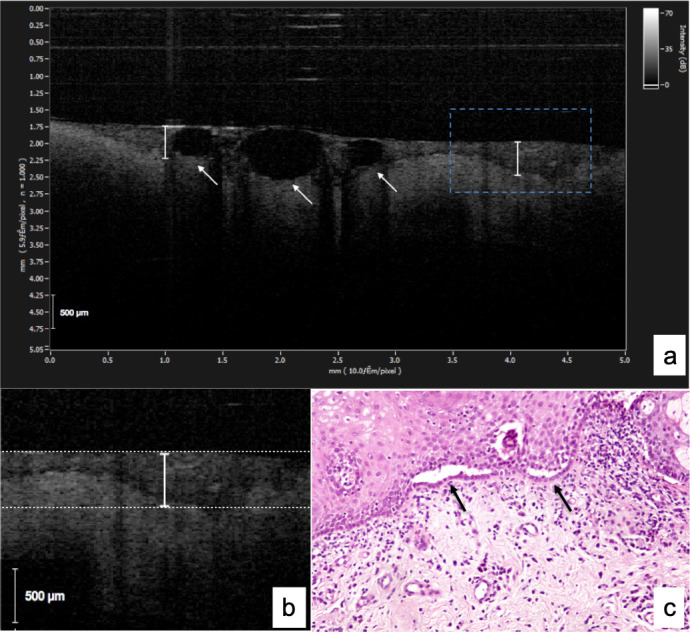
OCT images of buccal mucosa from patients with PV. (a) Intraepithelial blisters indicated by white arrows. Vertical bar, 500 µm. (b) previous image detail: some clefts within the thickness of the stratified squamous epithelium as denoted by vertical bar can be observed. Vertical bar, 500 µm. (c) Histopathology images of the PV patient. Intraepthelial blisters is indicated by black arrows, magnification 10x. OCT, optical coherence tomography; PV, pemphigus vulgaris.
Discussions
The aim of the current preliminary study was to evaluate the feasibility in the examination of the epithelial and sub-epithelial layer of the oral mucosa, and to distinguish intra- and sub-epithelial detachment in oral cavity lesions of PV and BP patients. The rarity of the described pathologies was the cause of the small size of the analyzed sample in this study1 as well as the difficulty in the recruitment of patients who belonged to the inclusion criteria. The data presented in this study are in line with those presented in literature.6,11 OCT has, so far, proved to be a reliable and practicable method for the determination of epithelial thickness in vivo.12 Healthy epithelium of the oral cavity varies from 75 to 550 µm in thickness, while the underlying LP extended up to 2000 µm. Prestin and co-workers11 determined average values of OCT epithelial thickness within the oral cavity that varies from 99 ± 22 µm (floor of the mouth) to 294 ± 68 µm of the buccal mucosa. In the present study, the thickness of the healthy EP was 593 ± 63 µm for the buccal region and 290 ± 29 µm on gingival mucosa. Moreover, the BM and the LP, in particular in the buccal mucosa, are easy to identify in a clear way, as reported by Mogensen et al.6 This allowed us to discriminate intraepithelial acantholysis in PV mucosa and sub-epithelial detachment in patients with BP. It should be pointed out that whereas in BP, sub-epithelial blisters appeared as colourful areas that could vary from black to grey under the elevated hyperreflective/backscattering EP, OCT images from PV showed more diffuse and less specific changes: therefore, while we were able to detect the liquid blister with a very thin roof, it was also noticed a signal-poor cavity in the context of a slightly thickened epithelial layer near the dermoepithelial junction. With its tissue penetration depth, the ergonomics of the probe and its high resolution, the imaging range of OCT technology is suitable for the oral mucosa. The OCT examination itself is non-invasive diagnostic tool as well as quick and easy to perform, and thus it is generally well accepted by patients.11 There are also other techniques for in vivo imaging of the oral cavity such as high frequency ultrasonography7 or confocal laser microscopy. A direct comparison between OCT and high frequency ultrasound performed by Vogt et al12 and by Warszawik-Hendzel et al14 highlighted that the spatial resolution of the OCT is significantly better.
Indeed, high frequency ultrasound has a penetration depth of approximately 15 mm and with a resolution of approximately 300 µm.15 At the opposite, confocal laser microscopy has a high resolution that allows distinction of fine features but possess a limited penetration depth of 0.2 mm.15 Instaed, OCT with its penetration depth of about 2 mm and resolution of 12 µm may provide an ideal balance.15 OCT imaging of oral mucosa bullous diseases exhibits the resolution necessary to evaluate fine variations in epithelial properties and has the penetration depth necessary to analyze epithelial and sub-epithelial layer.
Although all these tools have the potential to offer distinct advantages, their appropriate application and limitations remain to be determined. For instance, there still are some disadvantages in using OCT technique. The mechanical compression is certainly one of the major problems about the application of this deivce to the oral soft tissues. The application of a compression to the patients’ mucosa11 causes modifications in the optical properties of the sample, related with elasticity of different tissue layers. These changes may cause an increase in the contrast between layers and a decrease in the layer thickness, influencing the measured parameters. It would be important to control, or at least to be aware of this changes, in order to get a reference of the normal OCT morphology of the different anatomic regions of the oral cavity. The operator, in particular, should pay attention to the implication of mechanical compression for a correct interpretation of the OCT images.11 Another limitation of OCT is that the quality of the images results highly operator-linked. Moreover, as it is extremely difficult to find any definitive standards for evaluation, the interpretation of OCT images is dependent on the experience of the user.11 Despite the close agreement between OCT and histopathology scores,6,11 further studies will be necessary in order to determine the sensitivity and specificity of the OCT in the bullous lesions of the oral mucosa.
This exploratory study suggests that the OCT is an imaging device able to distinguish epithelial and sub-epithelial layer in vivo in patients affecting by oral bullous diseases, assisting the clinicians in differential diagnosis. The presented data are in accordance with the scientific literature, although a wider pool of cases is needed to increase statistical power. Histological examination and immunofluorescence methods remain the gold-standard for the diagnosis of oral bullous diseases. In this context, the OCT can provide the clinician with a valuable aid both as an additional diagnostic tool and in the follow up of the disease.
Contributor Information
Dorina Lauritano, Email: dorina.lauritano@unimib.it.
Francesca Loffredo, Email: francescaloffredo1992@gmail.com.
Enrica Gentile, Email: enrica.gentile@hotmail.it.
Alberta Lucchese, Email: alberta.lucchese@unicampania.it.
REFERENCES
- 1.Ishii K. Importance of serological tests in diagnosis of autoimmune blistering diseases. J Dermatol 2015; 42: 3–10. doi: 10.1111/1346-8138.12703 [DOI] [PubMed] [Google Scholar]
- 2.Lucchese A, Mittelman A, Tessitore L, Serpico R, Sinha AA, Kanduc D. Proteomic definition of a desmoglein linear determinant common to pemphigus vulgaris and pemphigus foliaceous. J Transl Med 2006; 4: 37. doi: 10.1186/1479-5876-4-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mihai S, Sitaru C. Immunopathology and molecular diagnosis of autoimmune bullous diseases. J Cell Mol Med 2007; 11: 462–81. doi: 10.1111/j.1582-4934.2007.00033.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hammers CM, Stanley JR. Mechanisms of disease: pemphigus and bullous pemphigoid. Annu Rev Pathol 2016; 11: 175–97. doi: 10.1146/annurev-pathol-012615-044313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bruch-Gerharz D, Hertl M, Ruzicka T. Mucous membrane pemphigoid: clinical aspects, immunopathological features and therapy. Eur J Dermatol 2007; 17: 191–200. doi: 10.1684/ejd.2007.0148 [DOI] [PubMed] [Google Scholar]
- 6.Mogensen M. Morsy H a, Nurnberg BM, Jemec GBE. optical coherence tomography imaging of bullous diseases. J. Eur. Acad. Dermatol. Venereol 2008; 22: 1458–64. [DOI] [PubMed] [Google Scholar]
- 7.Di Stasio D, Lauritano D, Paparella R, Franco R, Montella M, Serpico R, et al. Ultrasound imaging of oral fibroma: a case report. J Biol Regul Homeost Agents 2017; 31(2 Suppl 1): 23–6. [PubMed] [Google Scholar]
- 8.Lucchese A, Scivetti M, Pilolli GP, Favia G. Analysis of ghost cells in calcifying cystic odontogenic tumors by confocal laser scanning microscopy. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 2007; 104: 391–4. doi: 10.1016/j.tripleo.2006.09.005 [DOI] [PubMed] [Google Scholar]
- 9.García-Hernández A, Roldán-Marín R, Iglesias-Garcia P, Malvehy J. In Vivo Noninvasive Imaging of Healthy Lower Lip Mucosa: A Correlation Study between High-Definition Optical Coherence Tomography, Reflectance Confocal Microscopy, and Histology. Dermatol Res Pract 2013; 2013: 1–8. doi: 10.1155/2013/205256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kirillin MY, Agrba PD, Kamensky VA. In vivo study of the effect of mechanical compression on formation of OCT images of human skin. J Biophotonics 2010; 3: 752–8. doi: 10.1002/jbio.201000063 [DOI] [PubMed] [Google Scholar]
- 11.Gentile E, Maio C, Romano A, Laino L, Lucchese A. The potential role of in vivo optical coherence tomography for evaluating oral soft tissue: a systematic review. J. Oral Pathol. Med 2017;: 1–13. [DOI] [PubMed] [Google Scholar]
- 12.Vogt M, Knüttel A, Hoffmann K, Altmeyer P, Ermert H. Comparison of high frequency ultrasound and optical coherence tomography as modalities for high resolution and non invasive skin imaging. Biomed. Tech 2003; 48: 116–21. [DOI] [PubMed] [Google Scholar]
- 13.Di Stasio D, Lauritano D, Romano A, Salerno C, Minervini G, Minervini G, et al. In vivo characterization of oral pemphigus vulgaris by optical coherence tomography. J Biol Regul Homeost Agents 2015; 29(3 Suppl 1): 39–41. [PubMed] [Google Scholar]
- 14.Warszawik-Hendzel O, Olszewska M, Maj M, Rakowska A, Czuwara J, Rudnicka L. Non-Invasive diagnostic techniques in the diagnosis of squamous cell carcinoma. J Dermatol Case Rep 2015; 9: 89–97. doi: 10.3315/jdcr.2015.1221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mamalis A, Ho D, Jagdeo J. Optical coherence tomography imaging of normal, chronologically aged, photoaged and photodamaged skin: a systematic review. Dermatol Surg 2015; 41: 1–1005. doi: 10.1097/DSS.0000000000000457 [DOI] [PMC free article] [PubMed] [Google Scholar]


