Editor,
We present a rare and challenging case of a patient presenting with ectopic variceal haemorrhage. A 57 year old man with a background of alcohol related liver cirrhosis (Child Pugh A6, MELD 10) presented with 3 episodes of frank bleeding from his umbilicus over a 4 day period. Variceal surveillance with OGD in March 2017 was negative and other significant medical history included alcohol dependence, morbid obesity, type 2 diabetes mellitus and COPD.
Abdominal examination showed caput medusae that had been oversewn in the emergency department; there was no detectable ascites or asterixis. Doppler ultrasound of liver revealed patent hepatic vasculature. Subsequent CT confirmed cirrhotic appearances of the liver with features of portal hypertension, recanalisation of the umbilical vein and varices measuring up to 2cm in diameter within an umbilical hernia (Figure 1 and 2).
Figure 1.
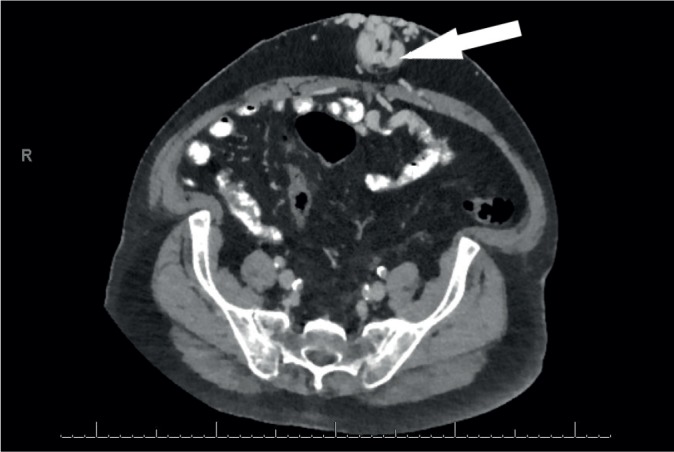
CT showing sizeable umbilical varices (white arrowhead)
Figure 2.
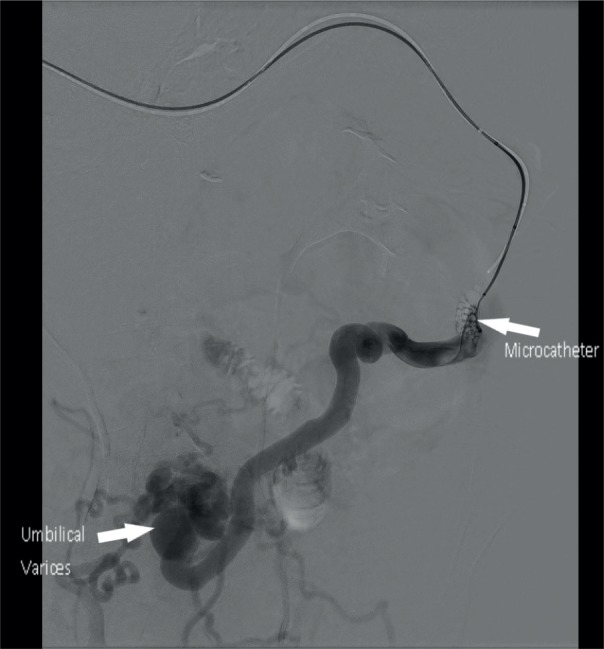
Catheterisation of umbilical varices
Following a further episode of bleeding from the umbilicus 48 hours post-admission, his haemoglobin fell from 113 g/L (130 − 180 g/L) to 62 g/L. He was managed as per gastro-intestinal variceal haemorrhage with transfusion of packed red cells, terlipressin and prophylactic antibiotics.
To prevent further bleeding a transjugular intrahepatic portosystemic shunt (TIPSS) was arranged. An echocardiogram, performed as part of a pre-TIPSS workup, established that biventricular function was normal. He remained haemodynamically stable and proceeded to TIPSS (Figure 3) which proved to be technically successful with the aid of CT fusion imaging (Figure 4). A significant hepatic venous pressure gradient in excess of 30 mmHg was recorded prior to stent deployment. Venography demonstrated a large portosystemic collateral vessel which eventually reached the level of the multiple varices at the patient's umbilicus. A microcatheter was negotiated along this allowing coiling and fibrovein foam embolisation (Figure 2). Following TIPSS and embolization (January 2018) bleeding was controlled and the patient was successfully discharged.
Figure 3.
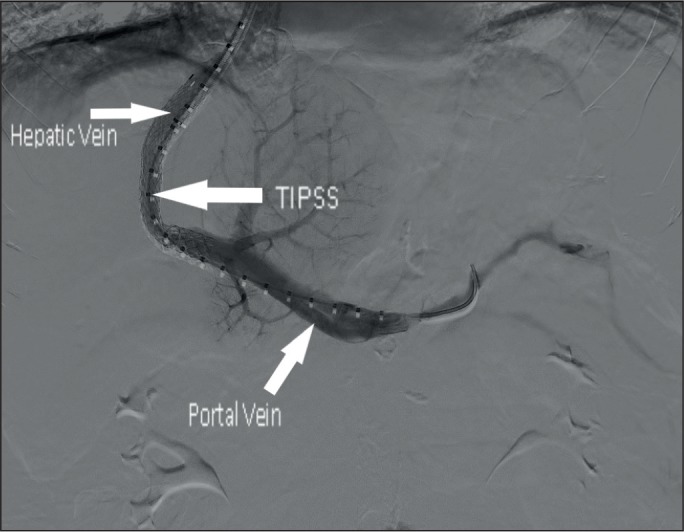
TIPSS insertion
Figure 4.
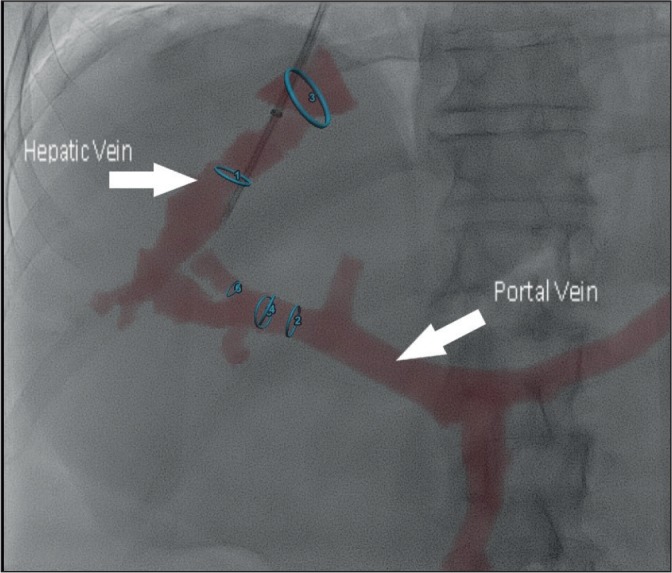
CT guided fusion imaging
To date, liver cirrhosis remains compensated with no post TIPSS hepatic encephalopathy in spite of relapse to low level alcohol consumption. He is currently Child Pugh A5 offering a 1 year survival of 95% and 2 year survival of 85%. No further variceal surveillance is required as portal hypertension has been addressed.
Gastroesophageal variceal bleeding is a common complication of patients with chronic liver disease. Bleeding from any location where there are portosystemic anastomoses and collateral vascular formation is possible.1 Variceal bleeding from locations other than the gastrointestinal tract (ectopic variceal bleeds) whilst rarely considered, account for up to 5% of all variceal bleeding. In addition, haemorrhage can be massive with mortality reaching up to 40%.2
Treatment is generally guided by local expertise due to absence of large studies. Initial interventions such as suture haemostasis and cauterisation have success for only a limited time frame. Medical treatments implemented to lower portal pressure include vasoconstrictors (terlipressin) in the acute setting and beta blockers (propranolol, carvedilol) in the chronic setting.1,2,3
Radiological interventions such as shunting (TIPSS) and percutaneous umbilical vein embolisation with sclerotherapy have been documented. A greater than 50% reduction in pressure gradient has been demonstrated to protect patients from rebleeding.1
Acknowledgments
We would like to acknowledge the IR department of RVH for their assistance with this case and the supplying of published images.
Footnotes
There was no funding for any aspect of this manuscript.
No competing interests need disclosed.
UMJ is an open access publication of the Ulster Medical Society (http://www.ums.ac.uk).
REFERENCES
- 1.Strauss C, Sivakkolunthu M, Ayantunde AA. Recurrent and Troublesome Variceal Bleeding from Parastomal Caput Medusae. The Korean Journal of Gastroenterology. 2014 doi: 10.4166/kjg.2014.64.5.290. [DOI] [PubMed] [Google Scholar]
- 2.Akhter NM, Haskal ZJ. Diagnosis and management of ectopic varices. Gastrointestinal Intervention. 2012 [Google Scholar]
- 3.Hoi KY, Mignanelli ED, Lightfoot D. Fatal haemorrhage from a caput medusae: A differential to a stabbing. Emergency Medicine Australasia. 2007 doi: 10.1111/j.1742-6723.2007.00950.x. [DOI] [PubMed] [Google Scholar]


