Abstract
Background
Stress urinary incontinence constitutes a significant health and economic burden to society. Traditional suburethral slings are surgical operations used to treat women with symptoms of stress urinary incontinence.
Objectives
To assess the effectiveness of traditional suburethral sling procedures for treating stress urinary incontinence in women; and summarise the principal findings of relevant economic evaluations.
Search methods
We searched the Cochrane Incontinence Specialised Register, which contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), as well as MEDLINE, MEDLINE In‐Process, MEDLINE Epub Ahead of Print, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), ClinicalTrials.gov, and the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP); we handsearched journals and conference proceedings (searched 27 February 2017) and the reference lists of relevant articles. On 23 January 2019, we updated this search; as a result, several additional reports of studies are awaiting classification.
Selection criteria
Randomised or quasi‐randomised trials that assessed traditional suburethral slings for treating stress or mixed urinary incontinence.
Data collection and analysis
At least two review authors independently extracted data from included trials and assessed risk of bias. When appropriate, a summary statistic was calculated: risk ratio (RR) for dichotomous data, odds ratio (OR) for continence and cure rates that were expected to be high, and mean difference (MD) for continuous data. We adopted the GRADE approach to assess the quality of evidence.
Main results
A total of 34 trials involving 3244 women were included. Traditional slings were compared with 10 other treatments and with each other.
We did not identify any trials comparing suburethral slings with no treatment or sham treatment, conservative management, anterior repair, or laparoscopic retropubic colposuspension. Most trials did not distinguish between women having surgery for primary or recurrent incontinence. One trial compared traditional slings with bladder neck needle suspension, and another trial compared traditional slings with single‐incision slings. Both trials were too small to be informative.
Traditional suburethral sling operation versus drugs
One small trial compared traditional suburethral sling operations with oxybutynin to treat women with mixed urinary incontinence. This trial did not report any of our GRADE‐specific outcomes. It is uncertain whether surgery compared with oxybutynin leads to more women being dry (83% vs 0%; OR 195.89, 95% confidence interval (CI) 9.91 to 3871.03) or having less urgency urinary incontinence (13% vs 43%; RR 0.29, 95% CI 0.09 to 0.94) because the quality of this evidence is very low.
Traditional suburethral sling versus injectables
One small trial compared traditional slings with suburethral injectable treatment. The impact of surgery versus injectables is uncertain in terms of the number of continent women (100% were dry with a traditional sling versus 71% with the injectable after the first year; OR 11.57, 95% CI 0.56 to 239.74), the need for repeat surgery for urinary incontinence (RR 0.52, 95% CI 0.05 to 5.36) or the occurrence of perioperative complications (RR 1.57, 95% CI 0.29 to 8.49), as the quality of evidence is very low.
Traditional suburethral sling versus open abdominal retropubic colposuspension
Eight trials compared slings with open abdominal retropubic colposuspension. Moderate‐quality evidence shows that the traditional suburethral sling probably leads to more continent women in the medium term (one to five years) (69% vs 59% after colposuspension: OR 1.70, 95% CI 1.22 to 2.37). High‐quality evidence shows that women were less likely to need repeat continence surgery after a traditional sling operation than after colposuspension (RR 0.15, 95% CI 0.05 to 0.42). We found no evidence of a difference in perioperative complications between the two groups, but the CI was very wide and the quality of evidence was very low (RR 1.24, 95% CI 0.83 to 1.86).
Traditional suburethral sling operation versus mid‐urethral slings
Fourteen trials compared traditional sling operations and mid‐urethral sling operations. Depending on judgements about what constitutes a clinically important difference between interventions with regard to continence, traditional suburethral slings are probably no better, and may be less effective, than mid‐urethral slings in terms of number of women continent in the medium term (one to five years) (67% vs 74%; OR 0.67, 95% CI 0.44 to 1.02; n = 458; moderate‐quality evidence). One trial reported more continent women with the traditional sling after 10 years (51% vs 32%: OR 2.22, 95% CI 1.07 to 4.61). Mid‐urethral slings may be associated with fewer perioperative complications (RR 1.74, 95% CI 1.16 to 2.60; low‐quality evidence).
One type of traditional sling operation versus another type of traditional sling operation
Nine trials compared one type of traditional sling operation with another. The different types of traditional slings, along with the number of different materials used, mean that trial results could not be pooled due to clinical heterogeneity. Complications were reported by two trials ‐ one comparing non‐absorbable Goretex with a rectus fascia sling, and the second comparing Pelvicol with a rectus fascial sling. The impact was uncertain due to the very low quality of evidence.
Authors' conclusions
Low‐quality evidence suggests that women may be more likely to be continent in the medium term (one to five years) after a traditional suburethral sling operation than after colposuspension. It is very uncertain whether there is a difference in urinary incontinence after a traditional suburethral sling compared with a mid‐urethral sling in the medium term. However, these findings should be interpreted with caution, as long‐term follow‐up data were not available from most trials. Long‐term follow‐up of randomised controlled trials (RCTs) comparing traditional slings with colposuspension and mid‐urethral slings is essential. Evidence is insufficient to suggest whether traditional suburethral slings may be better or worse than other management techniques. This review is confined to RCTs and therefore may not identify all of the adverse effects that may be associated with these procedures.
A brief economic commentary (BEC) identified three eligible economic evaluations, which are not directly comparable due to differences in methods, time horizons, and settings. End users of this review will need to assess the extent to which methods and results of identified economic evaluations may be applicable (or transferable) to their own setting.
Plain language summary
Traditional suburethral sling operations for urinary incontinence in women
Review question
How do traditional slings compare with other surgical or conservative treatments for women with stress urinary incontinence (SUI)?
Background
A traditional suburethral sling operation is one of the surgical options for treating women with SUI. Stress urinary incontinence is loss (leakage) of urine when coughing, laughing, sneezing, or exercising. It may be due to damage to the muscles that hold up the bladder neck or damage to their nerves, which often occurs during childbirth. When stress urinary incontinence occurs together with an urge to empty the bladder that is difficult to defer (urgency urinary incontinence (UUI)), this is known as mixed urinary incontinence (MUI). The traditional suburethral sling operation aims to hold up the bladder neck with a strip of material that may be biological (made from human or animal tissue) or made of non‐absorbable synthetic plastic (mesh/tape).
How up‐to‐date is this review?
The evidence is current to 27 February 2017. A further search on 23 January 2019 was not fully incorporated into the review.
Study characteristics
We found 34 randomised controlled trials (RCTs) involving 3244 women that compared traditional slings with drugs or other types of surgery (colposuspension, mid‐urethral slings, bladder neck needle suspension, single‐incision slings (mini‐slings); one type of traditional sling with another; and traditional slings with injectables. All trials included women with SUI, but some also involved women with UUI, who are said to have MUI.
We did not find any studies comparing suburethral slings with no treatment or sham treatment, conservative management such as pelvic floor exercises, anterior repair, or laparoscopic colposuspension.
Study funding sources
Few trialists reported who had funded their work.
Key results
Surgery appears to work better than drugs for treating urinary incontinence. Some evidence suggests that women had less leakage with traditional slings in the medium term (one to five years) compared with those undergoing colposuspension (a major abdominal operation), and fewer needed repeat surgery in one trial. However, information about adverse effects is lacking. It is not clear whether traditional slings were better or worse than mid‐urethral slings (synthetic tape) in the medium term, but one small trial showed that women who had a traditional sling might have less leakage 10 years later. It is not clear whether traditional slings were better or worse than injectable treatment, bladder neck needle suspension, or mini‐slings. We found insufficient information about different types of slings compared with each other, except that slings made of porcine dermis (Pelvicol) were more likely to fail than other materials. Slings made of non‐absorbable synthetic Goretex involved more complications.
Quality of the evidence
Many trials were small and used different ways of measuring success, which made combining information difficult. The quality of evidence for most outcomes was judged to be low or very low. This means that most of our conclusions about traditional slings are uncertain.
Authors' conclusions
Some evidence suggests that women had less leakage with traditional slings in the medium term (one to five years) compared with those undergoing colposuspension (a major abdominal operation), and fewer needed repeat surgery in one trial. Evidence on comparison of traditional suburethral slings with other treatments is insufficient. Three eligible economic evaluations reported similar results, but they are not directly comparable because of differences in their methods. This review is confined to randomised controlled trials (RCTs) and therefore may not identify all of the adverse effects that may be associated with these procedures.
Summary of findings
Background
Description of the condition
Urinary incontinence (UI) in women is a distressing condition that influences the physical, psychological, and social well‐being of affected individuals with considerable impact on women, carers, and health services (NICE 2013). Prevalence of urinary incontinence varies widely in different studies due to differences in definition and population but ranges from 8% to 45%, with stress urinary incontinence the most common type (Agarwal 2017). The prevalence of urinary incontinence increases with age, parity, smoking, and body mass index (BMI) (Amaral 2015; Lasserre 2009).
The International Continence Society defines urinary incontinence as involuntary loss of urine (Haylen 2010). Stress (urinary) incontinence (SUI) refers to involuntary loss of urine on effort or physical exertion (e.g. sporting activities), or on sneezing or coughing (Haylen 2010). Two mechanisms for stress incontinence are recognised: hypermobility or significant displacement of the urethra and bladder neck during exertion, and intrinsic urethral sphincter deficiency (Blaivas 1988). Among women, these mechanisms may co‐exist (O'Donnell 1994). Few clinical trials have distinguished between the two conditions, probably because no standardised and validated test is available to date (Abrams 2006; Blaivas 1988; McGuire 1993; McGuire 2004), and they are not defined by recognised terminology (Haylen 2010). Women whose incontinence may be due to either of these two mechanisms will be considered together in this review.
The diagnosis of urodynamic stress incontinence (USI) requires urodynamic investigation to exclude detrusor overactivity, in addition to history‐taking, physical examination, use of frequency/volume charts, and urine analysis. Some study authors have described women with only symptoms of stress incontinence (diagnosis made on clinical evaluation without urodynamics). Women with stress incontinence, both with and without urodynamic investigation, will be included in this review.
Urgency urinary incontinence (UUI) is the symptom of involuntary leakage of urine accompanied or immediately preceded by a sudden strong desire (urgency) to void that is difficult to delay. The woman has a sensation of urgency because the bladder is contracting too strongly. Detrusor overactivity (DO) is a urodynamic diagnosis characterised by occurrence of involuntary detrusor (bladder muscle) contractions. When a neurological cause is known, the term neurogenic detrusor overactivity is used. Idiopathic detrusor overactivity denotes absence of any identified cause (Haylen 2010). Women with both these symptoms and the urodynamic diagnosis of detrusor overactivity will be included in the review only if they have co‐existing and predominant stress urinary incontinence (mixed urinary incontinence (MUI)).
Women with mixed incontinence included in this review will have symptoms of stress and urgency urinary incontinence (diagnosed clinically), or urodynamic stress incontinence and detrusor overactivity (diagnosed via urodynamics).
Stress urinary incontinence is associated with various direct and indirect economic costs. For example, one USA‐based study found that women about to undergo Burch or fascial sling surgery for SUI had mean out‐of‐pocket costs (for supplies, laundry, and dry cleaning) equivalent to $19 USD (SD = 30) per week in today’s terms (2019 USD; converted from 2012 USD ‐ Shemilt 2010 ‐ at baseline) (Subak 2014). The women who participated in this study had an average (mean) age of 53 years (SD = 10) and an average (mean) baseline frequency of urinary UI episodes of 23 per week (SD = 21); 48% had undergone prior non‐surgical treatment for UI, and 16% had undergone prior surgery for UI. Another study estimated that in a single year (2012) in Spain alone, a national total of over 350,000 quality‐adjusted life‐years were lost due to UI among women 60 years of age and older (Villoro 2016).
Description of the intervention
Treatments for SUI include conservative, mechanical, pharmacological, and surgical interventions.
Conservative treatment centres on physical methods, including pelvic floor muscle training, electrical stimulation, biofeedback, and use of weighted cones.
Mechanical devices that prevent or reduce urinary leakage are available, such as metal plugs/patches and urethral and vaginal inserts.
Drug therapies, principally oestrogens and less often alpha‐adrenergic agents, can be used. A trial of conservative therapy is generally undertaken before surgery is undertaken.
These interventions are the topic of separate Cochrane Reviews.
Surgical procedures to remedy stress incontinence generally aim to lift and support the outlet of the bladder neck (urethrovesical junction). There is disagreement, however, regarding the precise mechanism by which continence is achieved. The choice of procedure is often influenced by co‐existent problems, surgeons' and/or women's preferences, and physical features of the person affected.
Numerous surgical methods have been described, but essentially they fall into nine categories.
Open abdominal retropubic suspension (e.g. colposuspension (Burch), Marshall‐Marchetti‐Krantz (MMK)) (Lapitan 2017).
Laparoscopic retropubic suspension (Dean 2017).
Vaginal anterior repair (anterior colporrhaphy) (Glazener 2017a).
Traditional suburethral slings (current review).
Mid‐urethral slings (retropubic or transobturator tapes) (Ford 2017).
Single‐incision slings (mini‐slings) (Nambiar 2017).
Bladder neck needle suspensions (Glazener 2017b).
Periurethral injections (Kirchin 2017).
Artificial sphincters.
This review will concentrate on traditional suburethral sling operations.
How the intervention might work
The aim of the suburethral sling operation is to restore or enhance the patient’s urethral support during sudden movement, such as that associated with coughing or sneezing. This is a achieved by lifting and supporting the urethrovesical junction with autologous or synthetic material. A traditional suburethral sling operation requires a combined abdominal and vaginal approach. Strips of material are tunnelled under the urethra and are attached to the rectus muscle or to the ileopectineal ligaments. The materials used for slings may be biological or synthetic.
Autologous biological materials include rectus fascia, fascia lata, pubococcygeal muscle, vaginal wall, aponeurosis, and pyramidalis fascia. Exogenous biological materials include ox fascia and porcine dermis (Pelvicol). Synthetic materials include Teflon, Mersilene tape in a silicon tube, lyodura, polytetrafluoroethylene (Goretex), Marlex mesh, and Silastic.
A modification of the suburethral sling procedure is the 'minimally invasive' mid‐urethral synthetic polypropylene mesh (sling/tape) applied via the retropubic or transobturator route. In this operation, a tape is inserted under the mid‐urethra with trocars but without fixation of free ends of the tape. This can be done with the patient under general or local anaesthesia (Smith 2002). These procedures have been considered in a separate Cochrane Review (Ford 2017). Only traditional sling operations using an open abdominal approach and suture fixation are included in this review.
Why it is important to do this review
The wide variety of surgical treatments for urinary incontinence suggests lack of consensus as to which procedure is best. The most robust evidence is likely to come from consideration of all well‐designed randomised controlled trials (RCTs). Hence, an easily accessible, periodically updated, comprehensive systematic review of such trials is needed to identify optimal practice and to highlight gaps in the evidence base. The findings of this review, taken in context with the findings of other continence surgery reviews, will provide women and their caregivers with the most robust evidence available to enable them to make an informed decision about whether to have surgery and, if so, what type.
Objectives
To assess the effectiveness of traditional suburethral sling procedures for treating stress urinary incontinence in women; and summarise the principal findings of relevant economic evaluations.
Methods
Criteria for considering studies for this review
Types of studies
Randomised or quasi‐randomised controlled trials of women with stress incontinence (urodynamic diagnosis) or symptoms of stress or mixed urinary incontinence (clinical diagnosis), in which at least one trial arm involves traditional suburethral sling procedures.
Types of participants
Adult women with SUI due to hypermobility and/or intrinsic sphincter deficiency, diagnosed clinically or with urodynamics, or with mixed urinary incontinence. Classification of diagnoses will be accepted as defined by the trialists.
Types of interventions
At least one arm of a study must involve traditional suburethral sling procedures to treat stress or mixed urinary incontinence. Comparison interventions may include other surgical techniques and non‐surgical interventions. The following comparisons were made for traditional suburethral sling procedures (abdominal and vaginal).
Traditional suburethral sling operation versus no treatment or sham operation.
Traditional suburethral sling operation versus conservative management (e.g. pelvic floor muscle training, electrical stimulation, cones, biofeedback).
Traditional suburethral sling operation versus drugs.
Traditional suburethral sling operation versus injectables.
Traditional suburethral sling operation versus anterior repair.
Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal).
Traditional suburethral sling operation versus open abdominal retropubic colposuspension.
Traditional suburethral sling operation versus laparoscopic colposuspension.
Traditional suburethral sling operation versus a mid‐urethral sling or tape.
Traditional suburethral sling operation versus a single‐incision sling (mini‐sling).
One type of traditional sling operation versus another type of traditional sling operation.
Types of outcome measures
Outcome measures used in this review were selected on the basis of their relevance to clinical cure or improvement in incontinence. We regard the principal measures of effectiveness as the proportion of women whose incontinence was cured following surgery and the proportion of women whose incontinence was improved.
Primary outcomes
-
Urinary incontinence
Number of continent (dry) women in the short term (less than 12 months), medium term (one to five years), and long term (longer than five years) as defined by women's report, quantified measures, clinician's observations, or combined measures (as defined by trialists; Table 12)
Number of women who have had repeat continence surgery
1. Definitions of cure and urinary incontinence used in included trials.
| Trial ID | Definition of outcome | Notes |
| WOMAN‐REPORTED | ||
| Albo 2007 | Overall success defined as no self‐reported symptoms of UI, no incontinence on 3‐day diary, negative stress test, no re‐treatment (combined outcome). Failure (self‐reported UI) at 5 years only (woman‐reported) | Also combined outcome before 5 years |
| Amaro 2007 | Cure defined as complete dryness with no usage of pads (woman‐reported) | |
| Arunkalaivanan 2003 | Cure of incontinence defined as a quality of life (QoL) improvement of 90% and/or patient‐determined continent status as dry (woman‐reported) | Questionnaire‐based |
| Demirci 2001 | Dry (symptom‐free) patients (woman‐reported) | |
| Guerrero 2008 | Assessment of cure not defined. Data abstracted from this trial therefore assumed to be woman‐reported | |
| Hilton 1989 | Cure stated as subjective (woman‐reported) at 24 months' follow‐up Objective (urodynamic diagnosis, pad test (clinician‐reported)) at 3 months |
Also clinician‐reported outcome at 3 months |
| Kondo 2006 | Subjective cure consistent with complete dryness or a few drops of water with strong exercises (assumed to be woman‐reported) | Also separate clinician‐reported outcome |
| Lucas 2000 | Success rate measured by recurrence of stress leakage as reported in patient questionnaire (woman‐reported) | |
| Maher 2005 | Subjective success: no or occasional (less than once a week) stress incontinence (woman‐reported) | Also separate clinician‐reported outcome |
| Sand 2000 | Cure defined as subjective (history: woman‐reported) | Also separate clinician‐reported outcome |
| Sharifiaghdas 2015 | Cure defined as of some degree of SUI at 1 year after surgery (woman‐reported) | |
| Shin 2001 | Success rate (dry) (method unspecified: assumed woman‐reported) | |
| Song 2004 | Cure rate (method unspecified: assumed woman‐reported) | |
| Viseshsindh 2003 | Stress urinary incontinence (method unspecified: assumed woman‐reported) | |
| QUANTITATIVE | ||
| Basok 2008 | Cure = dry pads, improvement = 1 wet pad, failure ≥ 1 wet pad per day (quantitative) | Satisfaction separately measured by questionnaire |
| Fischer 2001 | Subjective cure assessed via comparison between pre‐operative and postoperative Incontinence Impact Questionnaire (IIQ), Urinary Distress Inventory (UDI) (quantitative) | Also separate clinician‐reported outcome |
| Okulu 2013 | Cure defined as no pad use (quantitative) | |
| Pacetta 2005 | Subjective improvement only; subjective patient evaluations included QoL questionnaire, incontinence diary, pain and global outcome assessments (quantitative) | Also separate clinician‐reported outcome |
| Sharifiaghdas 2008 | Objective cure defined as 1‐hour pad test ≤ 2 grams (quantitative) | Also separate clinician‐reported outcome |
| Silva Filho 2006 | Women declared objectively cured when they had a postoperative pad test < 8 grams (quantitative) | |
| Zargham 2013 | Objective assessment via 48‐hour frequency volume chart, 48‐hour pad test, and standardised stress test. Surgery was considered successful when there was no postoperative SUI (patient was dry (quantitative)) | Also separate clinician‐reported outcome |
| CLINICIAN‐REPORTED | ||
| Abouhashem 2014 | No leakage of urine during stress test and urodynamic testing (clinician‐reported) | |
| Barbalias 1997 | Cure defined as complete freedom from SUI (clinician‐reported) | |
| Choe 2000 | Urine loss during cough‐stress test defined as persistent stress incontinence (clinician‐assessed) | |
| Fischer 2001 | Objective cure by stress test, voiding dysfunction by urodynamic assessment if incontinence seen (clinician‐reported) | Also separate quantitative outcome |
| Hilton 1989 | Cure stated as objective (urodynamic diagnosis, pad test (clinician‐reported)) at 3 months | Also woman‐reported outcome at 24 months |
| Kondo 2006 | Objective cure defined as complete absence of leakage during cough‐stress test with 250 or 300 mL of water in the bladder (clinician‐reported) | Also separate woman‐reported outcome |
| Maher 2005 | Objective success: no leakage due to SUI on repeat urodynamic study (clinician‐reported) | Also separate woman‐reported outcome |
| Pacetta 2005 | Objective outcome assessment: urine loss via a provocative pad test (clinician‐reported) | Also separate quantitative outcome (improvement only) |
| Sand 2000 | Cure defined as objective (urodynamic: clinician‐reported) | Also separate woman‐reported outcome |
| Sharifiaghdas 2008 | Objective cure defined as negative cough‐induced stress test with full bladder (≥ 250 mL filled) in lithotomy and standing positions (clinician‐reported) | Also separate quantitative outcome |
| Zargham 2013 | Objective assessment via 48‐hour frequency volume chart, 48‐hour pad test, and standardised stress test. Surgery considered successful when stress test was negative (clinician‐reported) and postoperative cystocoele was < grade 2 | Also separate quantitative outcome |
| COMBINED WOMAN‐ AND CLINICIAN‐REPORTED | ||
| Albo 2007 | Overall success defined as no self‐reported symptoms of UI, no incontinence on 3‐day diary, negative stress test, no re‐treatment (combined outcome). Failure (self‐reported UI) at 5 years only (woman‐reported) | Also woman‐reported outcome at 5 years |
| Al‐Azzawi 2014 | Cure of SUI defined as significant dryness as perceived by the patient, no more use of pads, negative stress test, and acceptable voiding stream (combined primary outcome) | However, no data after first week, so not useable |
| Bai 2005 | Cure defined as absence of subjective complaints of leakage and absence of urinary leakage on stress test (combined outcome) | |
| Enzelsberger 1996 | Cure defined as dry, symptom‐free without objective urine loss during stress with bladder filled to 300 mL or positive urethral‐closure pressure during stress provocation (combined outcome) | |
| Helmy 2012 | Continence defined as no urinary leakage on a 3‐day voiding diary, no self‐reported stress incontinence symptoms, and no stress incontinence surgical treatment (combined outcome) | |
| Henriksson 1978 | Cure defined as complete freedom from SUI (subjective and objective demonstrations) (combined outcome) | |
| Osman 2003 | Patients evaluated by SEAPI score (subjective and objective) after urodynamic examination before and after treatment (combined outcome) | |
| Tcherniakovsky 2009 | Cure defined as reported absence of SUI with no urinary loss during effort manoeuvres (combined outcome) | |
| Teleb 2011 | Cure defined as no leakage reported by the patient or noticed at examination (combined outcome) | |
| Wadie 2005 | Cure defined as complete dryness with no usage of pad and negative cough‐stress test (combined outcome) | |
Trials that did not report cure rates.
- Teixeira 2008: this trial did not address efficacy because it was a trial of tissue (histological) reaction to different sling materials.
- Al‐Azzawi 2014: this trial followed up women to one year and beyond but did not provide any outcome data after the first week.
Secondary outcomes
-
Women's observations
Number of women cured at one year or later (women's observations)
Number of women improved (cured or improved) in the short term (less than 12 months), medium term (one to five years), and long term (longer than five years)
Number of women satisfied
-
Quantification of symptoms
Pad changes over 24 hours (from self‐reported number of pads used)
Incontinent episodes over 24 hours (from self‐completed bladder chart)
Pad test of quantified leakage (mean weight of urine loss)
-
Clinician's observations
Numbers of women with urinary incontinence (clinician's observation) in the short term (less than 12 months), medium term (one to five years), and long term (longer than five years)
-
Surgical outcome measures
Duration of operation
Length of hospital stay
Time to return to normal activity level
Blood loss
-
Further treatment
Number of women requiring treatment for pelvic organ prolapse
-
Adverse events
Perioperative surgical complications
Bladder perforation
Urinary tract infection
Urinary urgency symptoms, urgency urinary incontinence
Detrusor overactivity (urodynamic overactivity)
Voiding dysfunction (with or without urodynamic confirmation)
Long‐term adverse effects such as mesh exposure, pelvic pain, dyspareunia, or release of sling
-
Quality of life
Condition‐specific measures to assess quality of life (e.g. Bristol Female Lower Urinary Tract Symptoms questionnaire (BFLUTS)) (Jackson 1996)
General health status measures (e.g. Short Form 36) (Ware 1993)
Main outcomes for ‘Summary of findings’ tables
We adopted the GRADE method for assessing the quality of evidence for the following five outcomes.
Number of continent (dry) women (any definition) in the medium term (1 to 5 years)
Repeat surgery for urinary incontinence.
Perioperative surgical complications.
Long‐term adverse effects such as mesh exposure, pain, and dyspareunia.
Condition‐specific quality of life.
Definition of cure and urinary incontinence
After discussion, the review authors agreed to add another outcome: women's report of cure of urinary incontinence. We identified the definitions of cure and incontinence used in each individual included trial (Table 12). However, only 14 trials used women's report of cure or incontinence to determine cure. The remainder used quantitative methods (such as whether pads were wet or dry, questionnaire scores, or diaries) (seven trials), clinician‐observed or ‐reported urine leakage (11 trials), or a combined definition without reporting the elements separately (10 trials). Some trials did report incontinence in more than one way. We therefore decided to use as our primary outcome the number of continent (dry) women, with any method used to measure or report urinary incontinence, but we added a further outcome of 'cure' as reported by women at 12 months or later.
Search methods for identification of studies
We did not impose language or other restrictions on any of these searches.
Electronic searches
Search for clinical effectiveness studies
We drew on the search strategy developed for Cochrane Incontinence. We identified relevant trials from the Cochrane Incontinence Specialised Register. For more details of the search methods used to build the Specialised Register, please see the Group's webpages, where details of the Register's development (from inception) and of the most recent searches performed to populate the Register can be found. To summarise, the Register contains trials identified by searching the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, MEDLINE In‐Process, MEDLINE Epub Ahead of Print, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), ClinicalTrials.gov, and WHO ICTRP, and by handsearching journals and conference proceedings. Many of the trials in the Cochrane Incontinence Specialised Register are also contained in CENTRAL.
The date of the last fully incorporated search was 27 February 2017.
A further updated search was conducted on 23 January 2019, the results of which were not fully incorporated into the review.
The terms used to search the Cochrane Incontinence Specialised Register are given in Appendix 1.
For previous versions of this review, one of the review authors performed extra literature searches. These are described in Appendix 2.
Search for economic evaluations
We performed additional searches of the following databases for the brief economic commentary (BEC).
MEDLINE on Ovid SP (1 January 1946 to week 5 July 2018), searched on 10 August 2018.
Embase on Ovid SP (1 January 1980 to week 32 2018), searched on 10 August 2018.
National Health Service Economic Evaluation Database (NHS EED) on Ovid SP (first quarter 2016), searched on 6 April 2017 (this database is no longer updated by the producer).
Search strategies used for the BEC are given in Appendix 3.
Searching other resources
We searched the reference lists of relevant articles for other possibly relevant trials.
Data collection and analysis
Selection of studies
At least two review authors evaluated the appropriateness of including reports of all possibly eligible studies without prior consideration of the results. We retrieved the reports of potentially eligible trials in full. We resolved any differences of opinion by discussion between the review authors.
Data extraction and management
At least three review authors undertook data extraction independently using a standard form containing pre‐specified outcomes. When data may have been collected but not reported, we sought clarification from the trialists.
Any differences of opinion related to study inclusion, data extraction, or risk of bias assessment were resolved by discussion among the review authors and, when necessary, were referred to a fourth review author for arbitration. We conducted the review using the standard Cochrane RevMan software.
Assessment of risk of bias in included studies
Each review author independently assessed risk of bias using Cochrane's 'Risk of bias' tool as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). The following questions were assessed and reported in the 'Risk of bias' tables.
Was the random sequence adequately generated (selection bias)?
Was allocation adequately concealed (selection bias)?
Were the participants or caregivers (performance bias) or outcome assessors (detection bias) blinded?
Were incomplete outcome data adequately addressed (attrition bias)?
We judged studies to be at low risk of bias if the method of blinding was adequate, or if lack of blinding could not have affected the results or could not be avoided. Each element was assessed as having low risk, high risk, or unclear risk of bias (the latter usually when no information was supplied).
Measures of treatment effect
When appropriate, we calculated a combined estimate of treatment effect across similar studies for each pre‐specified outcome, using risk ratios (RRs) for dichotomous data and mean differences (MDs) for continuous outcomes, along with 95% confidence intervals (CIs) when possible. For categorical (dichotomous) outcomes, the numbers reporting an outcome were related to the numbers at risk in each group to derive a risk ratio (RR). We have, however, used the odds ratio (OR) when reporting the number of continent or cured women, as event rates were expected to be high. For continuous variables, we used means and standard deviations to derive a mean difference (MD). We undertook a fixed‐effect approach to the analysis unless we noted evidence of heterogeneity across studies.
Unit of analysis issues
We analysed studies with multiple treatment groups by treating each pair of arms as a separate comparison, as appropriate. Studies based on a non‐standard design, such as cross‐over trials and cluster‐randomised trials, would have been analysed as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Dealing with missing data
We included data as they were reported. If women's subjective reporting of (cure of) urinary incontinence was not provided, we used the objective clinician's observations or other measures of urine leakage as surrogate data to maximise information available for the primary outcome ‐ the number of continent (dry) women (Table 12 shows data used). We did not contact authors of trials for missing data or further details for this version of the review.
Assessment of heterogeneity
We investigated differences between trials when apparent from visual inspection of the results, or when statistically significant heterogeneity was demonstrated, by using the Chi² test at the 10% probability level or assessment of the I² statistic (Higgins 2003). If we found no obvious reason for the heterogeneity (after consideration of populations, interventions, outcomes, and settings of individual trials), or if heterogeneity persisted despite removal of outlying trials, we used a random‐effects model.
Assessment of reporting biases
We would have examined publication bias through a funnel plot if 10 or more studies had been included in a meta‐analysis.
Data synthesis
We sought data on the number of participants with each outcome event by allocated treated group, irrespective of compliance and whether or not the participant was later thought to be ineligible or otherwise excluded from treatment or follow‐up, to allow an intention‐to‐treat (ITT) analysis when possible. We defined an ITT analysis to mean that all participants were analysed in their randomised groups whether or not they received the allocated intervention. We used the Mantel‐Haenszel statistical method for meta‐analysis. We used a fixed‐effect approach to the analysis, unless we found evidence of heterogeneity across studies, in which case we adopted a random‐effects model. We used a narrative review of eligible studies when statistical synthesis of data from than one study was not possible or was considered not appropriate.
Subgroup analysis and investigation of heterogeneity
We grouped trial data by type of incontinence: urodynamic stress incontinence based on a urodynamic diagnosis, or stress or mixed urinary incontinence based on symptom classification. It is unclear whether there is a clinical difference between women who had SUI alone (diagnosed by urodynamics to exclude concomitant detrusor contractions, which might be indicative of overactive bladder or urgency urinary incontinence) and women whose diagnosis of SUI was based on their report of symptoms alone. Women who have MUI (stress plus urgency) may have a worse outcome than those with SUI alone. We wished to explore whether different interventions had a differential effect among women with different types of incontinence. Quantitative synthesis was done when more than one eligible study was identified.
We also planned to examine whether findings would vary among women with primary versus recurrent SUI, or with presence or absence of prolapse, but this was not possible due to lack of information provided by the included trials.
In addition, we examined whether biological materials were associated with different outcomes compared with synthetic materials used for traditional sling arms in a separate comparison (comparison 11). It is biologically feasible that biological materials might be reabsorbed by the body tissues and thus might not be as long‐lasting as non‐absorbable synthetic materials.
Sensitivity analysis
We would have carried out sensitivity analysis based on eligibility criteria, such as by including and excluding results from abstract‐only publications or quasi‐randomised trials, if we had identified enough trials.
'Summary of findings' tables and assessing the quality of evidence
The GRADE Working Group strongly recommends including up to seven outcomes in 'Summary of findings' tables in a systematic review (Guyatt 2011a; Guyatt 2011b; Guyatt 2013a; Guyatt 2013b). We classified the primary and secondary outcomes in the Types of outcome measures as 'critical', 'important', or 'not important' for decision‐making from the patient's perspective, and we used this hierarchy to decide which outcomes should be included in the 'Summary of findings' tables. We also made judgements about which adverse events may be important to patients.
We implemented the GRADE method for assessing the quality of evidence.
Incorporating economics evidence
Following the search outlined under Search methods for identification of studies, we developed a brief economic commentary (BEC) to summarise the availability and principal findings of full economic evaluations that compare traditional sling operations for urinary incontinence in women (Shemilt 2019). This BEC encompasses full economic evaluations (i.e. cost‐effectiveness analyses, cost‐utility analyses, and cost‐benefit analyses), conducted alongside or based upon one or more RCTs included in the main review of intervention effects. This commentary focuses on the extent to which principal findings of eligible economic evaluations indicate that an intervention might be judged favourably or unfavourably from an economic perspective when implemented in different settings.
Results
Description of studies
Results of the search
We screened a total of 582 records produced by the literature search for this fourth update and retrieved 167 full‐text articles that appeared to meet the eligibility criteria for this review. After assessing the full‐text articles, we identified 115 reports of 34 included studies and 50 reports of 38 excluded studies. Additionally, we found reports of two ongoing studies (Hilton 2000; Zhu 2014). The flow of literature through the assessment process can be seen in Figure 1.
1.
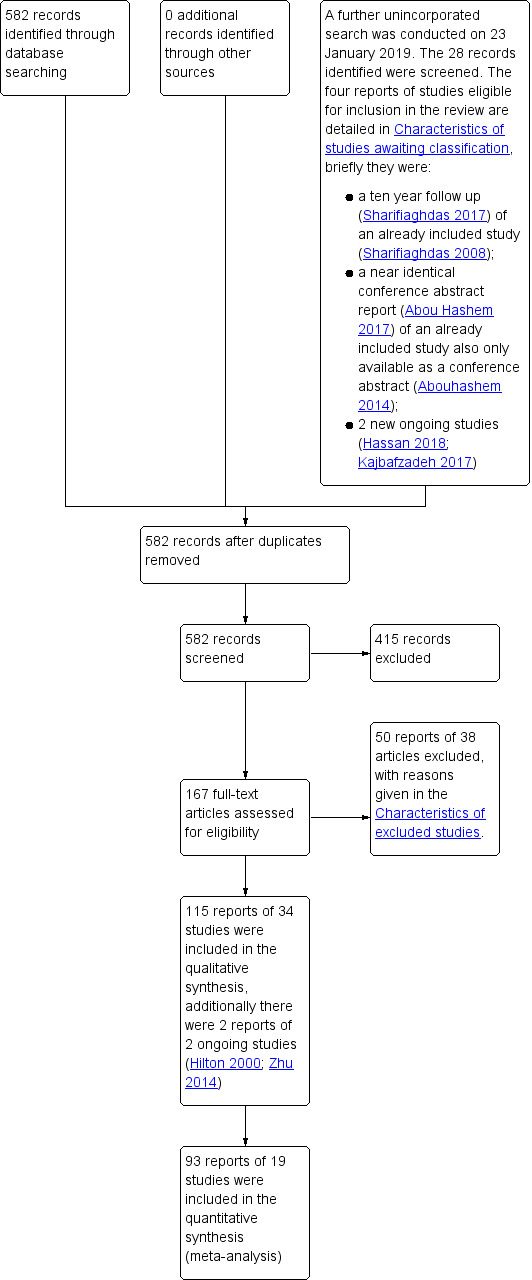
PRISMA study flow diagram ‐ search for clinical effectiveness studies.
For this update, eight new trials were included (Abouhashem 2014; Al‐Azzawi 2014; Choe 2000; Helmy 2012; Okulu 2013; Sharifiaghdas 2015; Teleb 2011; Zargham 2013). A further four have been updated with new information (Albo 2007; Amaro 2007; Guerrero 2008; Wadie 2005). In total, the review now contains 34 included trials, 38 excluded trials, and two ongoing studies.
A further updated search of the Cochrane Incontinence Specialised Register was conducted on 23 January 2019. This search was not fully incorporated into the review. A total of 28 records retrieved by the search were screened. Four reports of trials were eligible for inclusion in the review ‐ for transparency, all four eligible reports have been added to Studies awaiting classification, and details can be found under Characteristics of studies awaiting classification. In brief, the authors of Sharifiaghdas 2008 published a 10‐year update in 2017, but the data have not yet been added to the review (Sharifiaghdas 2017). Abou Hashem 2017 served as another report of the already included study (Abouhashem 2014); however, this appears to be exactly the same conference abstract as the one included study report (also a conference abstract); no new details or data are available in this additional report. Two new ongoing studies were also identified (Hassan 2018; Kajbafzadeh 2017), but their data have not yet been added to the review.
Our search for economic evaluations produced a total of 465 titles and abstracts to be screened, from which we selected four reports of three economic evaluations for further assessment (Berman 1997; Kilonzo 2004; Kumar 2017). The flow of literature through the assessment process is shown in Figure 2.
2.
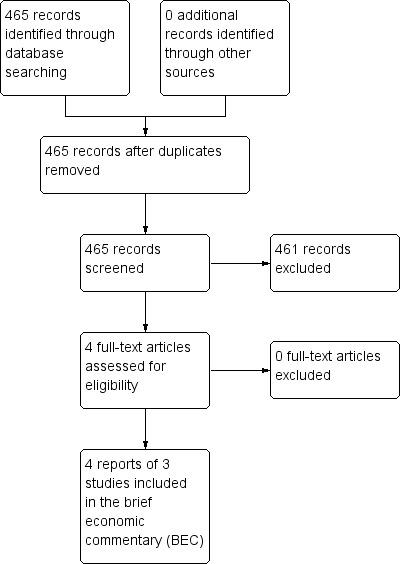
PRISMA study flow diagram ‐ search for economic evaluations for the BEC.
Included studies
We included a total of 34 RCTs, reporting data on outcomes of 3244 women, with sample sizes ranging from 20 to 655 participants. Three trials are quasi‐randomised (Choe 2000; Kondo 2006; Zargham 2013), and two are multi‐arm trials (Bai 2005; Guerrero 2008). With the exception of Albo 2007 and Sand 2000, the included trials were small and had short follow‐up.
Participants
Inclusion criteria were not always clearly defined. Ten trials included women (some or all) with stress‐predominant MUI, both stress and urgency (Al‐Azzawi 2014; Barbalias 1997; Basok 2008; Kondo 2006; Okulu 2013; Osman 2003; Sand 2000; Song 2004; Teleb 2011; Zargham 2013). Two trials involved women with self‐reported or predominant SUI (Albo 2007; Wadie 2005). All others were restricted to women with a urodynamic diagnosis of stress incontinence (USI, previously known as genuine stress incontinence). Data from two trials were insufficient, with only abstracts available (Abouhashem 2014; Helmy 2012). All trials included both pre‐menopausal and postmenopausal women, but none included women who were treated with hormone replacement therapy. One study was restricted to women with vaginal narrowing due to atrophic vaginitis or previous surgical scars (Hilton 1989).
Previous continence surgery status
Two trials included only women without previous interventions for incontinence (Henriksson 1978; Silva Filho 2006), and another included only women who had recurrent incontinence after a previous vaginal hysterectomy and at least one anterior repair (Enzelsberger 1996). The others included women with both primary and recurrent SUI but did not report outcome data separately according to previous continence surgery.
Presence or absence of pelvic organ prolapse
This information was not routinely reported in the included trials, and when it was, data were not reported separately.
Interventions
Fifteen materials were used for the traditional sling procedure across 34 studies.
Autologous biological materials
Autologous dermal graft patch (Shin 2001)
Autologous fascia lata (Song 2004)
Autologous rectus fascia (Abouhashem 2014; Al‐Azzawi 2014; Albo 2007; Amaro 2007; Bai 2005; Barbalias 1997; Demirci 2001; Guerrero 2008; Helmy 2012; Kondo 2006; Lucas 2000; Maher 2005; Osman 2003; Pacetta 2005; Sharifiaghdas 2008; Sharifiaghdas 2015; Silva Filho 2006; Tcherniakovsky 2009; Teleb 2011; Viseshsindh 2003; Wadie 2005)
Autologous vaginal wall sling (Choe 2000; Teleb 2011; Viseshsindh 2003; Zargham 2013)
Other biological materials
Cadaveric fascia lata (Basok 2008; Shin 2001)
Fortaperm (Pacetta 2005)
Lyphohilised dura matter (Enzelsberger 1996)
Porcine dermis, also known as Pelvicol (Arunkalaivanan 2003; Guerrero 2008; Hilton 1989, Teixeira 2008)
Synthetic non‐absorbable materials
Goretex sling operation (Barbalias 1997)
Polytetrafluoroethylene ‐ PTFE (Sand 2000)
Polytetrafluoroethylene impregnated with silver diacetate and chlorhexidine; Antimicrobial Mycromesh (Choe 2000)
Teflon sling (Henriksson 1978)
Ultrapro mesh: synthetic monofilament combined mesh, non‐absorbable with absorbable coating (Okulu 2013)
Prolene or prolene light mesh (Okulu 2013; Teleb 2011)
Vypro mesh: semi‐absorbable multi‐filament mesh (Okulu 2013)
One trial, reported in abstract form, did not mention the type of material used for the suburethral sling (Fischer 2001).
Comparators
The 34 included trials reported the following comparisons.
One compared traditional suburethral sling operations with oxybutynin for treating women with mixed urinary incontinence (Osman 2003).
One compared traditional suburethral sling operations with suburethral injectable treatment (Maher 2005).
One compared traditional suburethral sling operations with bladder neck needle suspension (Hilton 1989).
Eight compared traditional suburethral sling operations with open abdominal retropubic colposuspension (Albo 2007; Bai 2005; Demirci 2001; Enzelsberger 1996; Fischer 2001; Helmy 2012; Henriksson 1978; Sand 2000). There were no useable data in one of the trials identified in the updated search (Helmy 2012), and one trial was updated with new information (Albo 2007).
Fifteen trials compared traditional suburethral sling operations with mid‐urethral sling operations (Abouhashem 2014; Al‐Azzawi 2014; Amaro 2007; Arunkalaivanan 2003; Bai 2005; Basok 2008; Guerrero 2008; Kondo 2006; Sharifiaghdas 2008; Silva Filho 2006; Song 2004; Tcherniakovsky 2009; Teixeira 2008; Wadie 2005; Zargham 2013). Of these, three were added to this comparison in this version of the review (Abouhashem 2014; Al‐Azzawi 2014; Zargham 2013), but one did not provide any useable data (Abouhashem 2014). One trial did not provide data after the first week (Al‐Azzawi 2014), and further data were identified for three trials (Amaro 2007; Guerrero 2008; Wadie 2005).
One compared a traditional suburethral sling with a single‐incision sling (mini‐sling) (Sharifiaghdas 2015).
Nine trials compared one type of traditional suburethral sling with another (Barbalias 1997; Choe 2000; Guerrero 2008; Lucas 2000; Okulu 2013; Pacetta 2005; Shin 2001; Teleb 2011; Viseshsindh 2003). Of these, three are new to this comparison for this version of the review (Choe 2000; Okulu 2013; Teleb 2011), and one trial was updated with further data (Guerrero 2008).
No trials compared suburethral slings with anterior repair, laparoscopic retropubic colposuspension, or artificial sphincters.
There were seven non‐traditional sling comparators across 25 studies.
Anticholinergic (Osman 2003).
Intravaginal slingplasty (Basok 2008).
Mid‐urethral sling (Abouhashem 2014; Al‐Azzawi 2014; Amaro 2007; Arunkalaivanan 2003; Bai 2005, Guerrero 2008; Kondo 2006; Sharifiaghdas 2008; Silva Filho 2006; Song 2004; Tcherniakovsky 2009; Teixeira 2008; Wadie 2005; Zargham 2013).
Retropubic colposuspension: Burch colposuspension (Albo 2007; Bai 2005; Demirci 2001; Enzelsberger 1996; Fischer 2001; Helmy 2012; Osman 2003; Sand 2000); Marshall‐Marchetti‐Krantz (Henriksson 1978).
Stamey bladder neck (needle) suspension (Hilton 1989).
Transurethral Macroplastique (injectable material) (Maher 2005).
Single‐incision sling (mini‐sling) (Sharifiaghdas 2015).
One trial was designed to study an anticholinergic agent (oxybutynin) in comparison with surgery (Burch or sling) for women with MUI (Osman 2003). It was possible to extract only the data from sling surgery in comparison with medical treatment for inclusion in the analysis.
Outcome measures (definition of incontinence)
Outcome measures were not reported in a standardised fashion (Table 12).
Fourteen trials used women's self‐report of cure or absence of incontinence to define urinary incontinence.
Seven trials used quantitative methods (such as based on wet or dry pads, questionnaire scores, or diaries).
Eleven trials used clinician‐observed or ‐reported urine leakage (such as the stress test, or at urodynamics).
Ten trials used a combined definition without reporting the elements separately.
The primary outcome was the number of continent (dry) women using at least one of these definitions of urine leakage (32/34 trials). If woman‐reported leakage alone or clinician‐observed leakage was reported separately, those were also reported in separate outcomes. Only two trials did not report any measure of urine leakage (Al‐Azzawi 2014; Teixeira 2008).
Follow‐up
Trials varied in their reports of initial and long‐term follow‐up, reporting data on outcomes of 3244 women at last follow‐up.
Ten trialists presented their results at three‐ and/or six‐ and/or nine‐month assessment (Bai 2005; Choe 2000; Fischer 2001; Henriksson 1978; Osman 2003; Silva Filho 2006; Sand 2000; Song 2004; Teleb 2011; Viseshsindh 2003).
One trial followed up women to one year and beyond but did not provide any outcome data after the first week, such that cure data were not useable (Al‐Azzawi 2014).
Eleven trials presented follow‐up at around one year (Arunkalaivanan 2003; Basok 2008; Demirci 2001; Guerrero 2008; Lucas 2000; Maher 2005; Pacetta 2005; Sharifiaghdas 2008; Sharifiaghdas 2015; Shin 2001; Tcherniakovsky 2009).
Eleven trials described follow‐up between one and five years (Albo 2007; Amaro 2007; Arunkalaivanan 2003; Barbalias 1997; Enzelsberger 1996; Hilton 1989; Kondo 2006; Okulu 2013; Teixeira 2008; Wadie 2005; Zargham 2013).
Three trials have now reported data on the outcomes of 892 women at the last follow‐up at five years or later (Albo 2007; Guerrero 2008; Sand 2000).
For more details about the characteristics of these trials, please see Characteristics of included studies.
Excluded studies
In total, 38 studies were excluded. For further details, please see Characteristics of excluded studies.
Seventeen trials compared mid‐urethral or variant sling procedures with each other or with other operations (Amat 2007; Chong 2003; Corcos 2001; Darai 2007; Gamble 2010; Halaska 2001; Han 2001; Kocjancic 2008; Liapis 2002; Lim 2005; Naumann 2006; Oremus 2010; O'Sullivan 2000; Palomba 2008; Seo 2007; Ward 2002a; Yoo 2007). Mid‐urethral sling and open colposuspension procedures are considered in other Cochrane Reviews (Ford 2017; Lapitan 2017).
Eleven studies were not randomised (Atherton 2000; Brandt 2009; Bruschini 2005; Debodinance 1994; Giri 2004; Giri 2006; Hung 2001; Ishenko 1999; Kuo 2001; Obrink 1978; Schostak 2001).
There was uncertainty regarding the population included in two trials (Aurunkalaivanan 2001; Barrington 2003).
Five trials included some participants who did not have SUI (Debodinance 1993; Goldberg 2001; Kwon 2002; Meschia 2001; Trezza 2001).
Three trials were excluded for other reasons: Choe 2001 randomised women to having urodynamic evaluation or not; Wang 1999 randomised women to different types of anaesthetic; Lemieux 1991 compared clamping and non‐clamping of catheters after incontinence surgery.
Risk of bias in included studies
Risk of bias findings for the included trials are summarised in Figure 3 and Figure 4.
3.
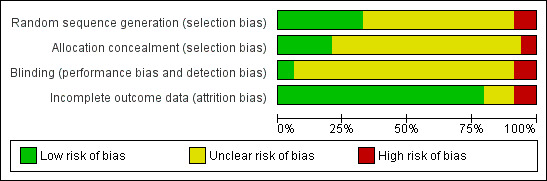
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
4.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Adequate sequence generation
Eight trials used an adequate method of sequence generation (Al‐Azzawi 2014; Albo 2007; Amaro 2007; Barbalias 1997; Guerrero 2008; Okulu 2013; Osman 2003; Sand 2000). Two trials used randomisation charts to generate the randomisation sequence without providing further information about the process (Enzelsberger 1996; Hilton 1989). Nevertheless, these were judged to be adequate. In one of these trials, one woman was randomised to one arm of the study and was compared with two women randomised to the other intervention (Barbalias 1997).
Sequence generation was inadequate in three trials, which were therefore categorised as quasi‐randomised trials. Kondo 2006 used date of birth with even dates assigned to one group and odd dates to the other. In two trials, women were randomised in alternate fashion (Choe 2000; Zargham 2013).
In the remainder, women were stated to be randomised but no other details of the process were provided.
Allocation concealment
The reported method of concealment of randomisation was secure in seven trials (Albo 2007; Amaro 2007; Guerrero 2008; Lucas 2000; Okulu 2013; Sharifiaghdas 2015; Wadie 2005). Allocation concealment was unknown for most of the remaining trials, as study authors did not record it. Another trial used sealed opaque envelopes but made no mention of numbering and thus was judged as unclear for allocation concealment (Sharifiaghdas 2008).
Inadequate allocation concealment was noted in three quasi‐randomised trials (Kondo 2006; Choe 2000; Zargham 2013).
Blinding
Masking of women or surgeons was not reported in most trials, but this is difficult to achieve in surgical trials. Only two trials attempted or reported blinding of participants or care providers (Guerrero 2008; Wadie 2005). Third party outcome assessment was not performed in any of the trials.
Incomplete outcome data
Most trials had complete outcome data at follow‐up, or losses were evenly distributed between randomised groups, and this was unlikely to have a significant effect on the final analysis. Two trials did not account for losses at follow‐up, which might potentially have been a source of bias (Demirci 2001; Fischer 2001). One trial had a differential dropout at two years' follow‐up (Wadie 2005).
Other potential sources of bias
Comparability of groups at baseline
Baseline comparisons between groups were provided in 19 trials (Albo 2007; Arunkalaivanan 2003; Bai 2005; Basok 2008; Choe 2000; Demirci 2001; Enzelsberger 1996; Hilton 1989; Kondo 2006; Lucas 2000; Maher 2005; Okulu 2013; Sand 2000; Sharifiaghdas 2008; Song 2004; Tcherniakovsky 2009; Teleb 2011; Wadie 2005; Zargham 2013). Henriksson 1978 stated that the two groups were comparable without supplying data, and the remainder did not mention baseline comparisons between groups.
Although we did not formally assess 'selective reporting' or 'other bias' (other than comparability of groups at baseline, as above), we had no concerns for these two domains across studies.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10; Table 11
Summary of findings for the main comparison. Traditional suburethral sling operation versus no treatment or sham operation.
| Traditional suburethral sling operation versus no treatment or sham operation | ||||||
| Patient or population: women with urinary incontinence Settings: secondary care Intervention: sling Comparison: no treatment or sham treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment or sham treatment | Sling | |||||
| Number of continent (dry) women (any definition) in the medium term (1 to 5 years) | Not reported | |||||
| Repeat surgery for urinary incontinence | Not reported | |||||
| Perioperative surgical complications | Not reported | |||||
| Long‐term adverse effects | Not reported | |||||
| Condition‐specific quality of life | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval. | ||||||
| GRADE Working Group grades of evidence. High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
Summary of findings 2. Traditional suburethral sling operation versus conservative management.
| Traditional suburethral sling operation versus conservative management | ||||||
| Patient or population: women with urinary incontinence Settings: secondary care Intervention: sling Comparison: conservative treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conservative treatment | Sling | |||||
| Number of continent (dry) women (any definition) in the medium term (1 to 5 years) | Not reported | |||||
| Repeat surgery for urinary incontinence | Not reported | |||||
| Perioperative surgical complications | Not reported | |||||
| Long‐term adverse effects | Not reported | |||||
| Condition‐specific quality of life | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval. | ||||||
| GRADE Working Group grades of evidence. High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
Summary of findings 3. Traditional suburethral sling operation versus drugs.
| Traditional suburethral sling operation versus drugs | ||||||
| Patient or population: women with urinary incontinence Settings: secondary care Intervention: sling Comparison: drugs | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Drugs | Sling | |||||
| Number of continent (dry) women (any definition) in the medium term (1 to 5 years) | Not reported | |||||
| Repeat surgery for urinary incontinence | Not reported | |||||
| Perioperative surgical complications | Not reported | |||||
| Long‐term adverse effects | Not reported | |||||
| Condition‐specific quality of life | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval. | ||||||
| GRADE Working Group grades of evidence. High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
Summary of findings 4. Traditional suburethral sling operation versus injectables.
| Traditional suburethral sling operation versus injectables | ||||||
| Patient or population: women with urinary incontinence Settings: secondary care Intervention: sling Comparison: injectable | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Injectable | Sling | |||||
| Number of continent (dry) women (any definition) in the medium term (1 to 5 years) | 714 per 1000 | 967 per 1000 (583 to 998) |
OR 11.57 (0.56 to 239.7) |
43 (1 study) | ⊕⊝⊝⊝ very low,a,b |
252 more women, per 1000, with traditional sling (131 fewer to 284 more) |
| Repeat surgery for urinary incontinence ‐ urodynamic stress incontinence (only) | 91 per 1000 |
47 per 1000 (5 to 487) |
RR 0.52 (0.05 to 5.36) |
43 (1 study) | ⊕⊝⊝⊝ very lowa,b |
44 fewer women, per 1000, with traditional sling (86 fewer to 396 more) |
| Perioperative surgical complications Urinary tract infection ‐ stress urinary incontinence (symptoms only) | 91 per 1000 | 143 per 1000 (26 to 772) | RR 1.57 (0.29 to 8.49) | 43 (1 study) | ⊕⊝⊝⊝ very lowa,b |
52 more women, per 1000, with traditional sling (65 fewer to 681 more) |
| Long‐term adverse effects | Not reported | |||||
| Condition‐specific quality of life | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aDowngraded one level due to serious risk of bias (unclear for sequence generation, allocation concealment, and blinding) and two levels for imprecision (95% CI very wide, 0.56 to 239.74; crosses line of no effect).
bDowngraded two levels due to very serious imprecision: single trial with small sample size.
Summary of findings 5. Traditional suburethral sling operation versus anterior repair.
| Traditional suburethral sling operation versus anterior repair | ||||||
| Patient or population: women with urinary incontinence Settings: secondary care Intervention: sling Comparison: anterior repair | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Anterior repair | Sling | |||||
| Number of continent (dry) women (any definition) in the medium term (1 to 5 years) | Not reported | |||||
| Repeat surgery for urinary incontinence | Not reported | |||||
| Perioperative surgical complications | Not reported | |||||
| Long‐term adverse effects | Not reported | |||||
| Condition‐specific quality of life | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval. | ||||||
| GRADE Working Group grades of evidence. High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
Summary of findings 6. Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal).
| Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal) | ||||||
| Patient or population: women with urinary incontinence Settings: secondary care Intervention: sling Comparison: bladder neck needle suspension | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Bladder neck needle suspension | Sling | |||||
| Number of continent (dry) women (any definition) in the medium term (1 to 5 years) | 700 per 1000 | 900 per 1000 (435 to 991) |
OR 3.86 0.33 to 45.57 |
20 (1 study) | ⊕⊝⊝⊝ very lowa |
200 more women, per 1000, with traditional sling (265 fewer to 291 more) |
| Repeat surgery for urinary incontinence | Not reported | |||||
| Perioperative surgical complications ‐ urodynamic stress incontinence (only) | 200 per 1000 | 900 per 1000 (256 to 1000) | RR 4.5 (1.28 to 15.81) | 20 (1 study) | ⊕⊝⊝⊝ very lowa |
700 more women, per 1000, with traditional sling (56 fewer to 2962 more) |
| Long‐term adverse effects | Not reported | |||||
| Condition‐specific quality of life | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aDowngraded two levels for risk of bias (evidence comes from a single trial that was judged to be unclear for allocation concealment and blinding) and two levels for imprecision (95% CI very wide).
Summary of findings 7. Traditional suburethral sling operation versus open abdominal retropubic colposuspension.
| Traditional suburethral sling operation versus open abdominal retropubic suspension | ||||||
| Patient or population: women with urinary incontinence Settings: secondary care Intervention: sling Comparison: open abdominal retropubic suspension | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Open abdominal retropubic suspension | Sling | |||||
| Number of continent (dry) women (any definition) in the medium term (1 to 5 years) | 589 per 1000 | 711 per 1000 (638 to 774) |
OR 1.70 (1.22 to 2.37) | 687 (4 RCTs) |
⊕⊕⊕⊝ moderatea |
120 more dry women, per 1000, with traditional sling (47 more to 186 more) |
| Repeat surgery for urinary incontinence‐stress urinary incontinence (symptoms only) | 119 per 1000 | 18 per 1000 (6 to 50) |
RR 0.15 (0.05 to 0.42) |
450 (1 RCT) | ⊕⊕⊕⊕ high |
101 fewer women having repeat continence surgery, per 1000, with traditional sling (113 fewer to 69 fewer) |
| Perioperative surgical complications | 95 per 1000 | 118 per 1000 (79 to 178) | RR 1.24 (0.83 to 1.86) | 792 (4 studies) | ⊕⊝⊝⊝ very lowb |
23 more women, per 1000, with traditional sling (16 fewer to 82 more) |
| Long‐term adverse effects Number of women with recurrent UTIs at > 5 years | 92 per 1000 | 94 per 1000 (52 to 167) |
RR 1.02 (0.57 to 1.82) |
453 (1 study) | ⊕⊕⊝⊝ lowc |
2 more women, per 1000, with traditional sling (39 fewer to 75 more) |
| Condition‐specific quality of life Health status measures ‐ Incontinence Impact Questionnaire (IIQ) | Mean IIQ score in the control group was 44.8 | Mean condition‐specific quality of life in the intervention groups was 1.7 higher (11.96 lower to 15.36 higher) | 453 (1 study) | ⊕⊝⊝⊝ lowd | Another trial reported no evidence of a difference between colposuspension groups and sling groups in IIQ and UDI scores but reported no actual numbers | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; IIQ: Incontinence Impact Questionnaire; OR: odds ratio; RCT: randomised controlled trial; RR: risk ratio; UDI: Urogenital Distress Inventory. | ||||||
| GRADE Working Group grades of evidence. High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aDowngraded one level due to serious risk of bias (unclear randomisation and allocation concealment in two of the smaller trials), but the trial carrying 90% of weight in the meta‐analysis was judged to have low risk of selection bias.
bDowngraded one level for risk of bias (sequence generation was unclear in one‐fourth of trials and allocation concealment was unclear in three‐quarters of trials taking part in the meta‐analysis; participants were not blinded) and one level for imprecision (95% confidence interval was very wide).
cDowngraded two levels for imprecision (95% confidence interval was very wide; 0.57 to 1.82).
dDowngraded two levels for risk of bias (sequence generation and allocation concealment were judged to be "low risk"; blinding of participants was judged to be "high risk") and two levels for imprecision (95% confidence interval was very wide; ‐11.96 to 15.36).
Summary of findings 8. Traditional suburethral sling operation versus laparoscopic colposuspension.
| Traditional suburethral sling operation versus laparoscopic colposuspension | ||||||
| Patient or population: women with urinary incontinence Settings: secondary care Intervention: sling Comparison: laparoscopic procedures | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Laparoscopic procedures | Sling | |||||
| Number of continent (dry) women (any definition) in the medium term (1 to 5 years) | Not reported | |||||
| Repeat surgery for urinary incontinence | Not reported | |||||
| Perioperative surgical complications | Not reported | |||||
| Voiding dysfunction | Not reported | |||||
| Long‐term adverse effects | Not reported | |||||
| Condition‐specific quality of life | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval. | ||||||
| GRADE Working Group grades of evidence. High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
Summary of findings 9. Traditional suburethral sling operation versus a mid‐urethral sling or tape.
| Traditional suburethral sling operation versus a mid‐urethral sling or tape | ||||||
| Patient or population: women with urinary incontinence Settings: secondary care Intervention: traditional sling Comparison: minimally invasive sling operation | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Minimally invasive sling operation | Traditional sling | |||||
| Number of continent (dry) women (any definition) in the medium term (1 to 5 years) | 737 per 1000 | 652 per 1000 (552 to 741) |
OR 0.67 (0.44 to 1.02) |
445 (6 RCTs) |
⊕⊕⊕⊝ moderate1 |
85 fewer women, per 1000, with traditional sling (185 fewer to 4 more) |
| Repeat surgery for urinary incontinence ‐ urodynamic stress incontinence (only) | One trial reported the numbers of women having repeat continence surgery at 10‐year follow‐up: traditional sling: 0/67; mid‐urethral sling: 2/69 | 136 (1 study) | ⊕⊕⊝⊝ low2 | |||
| Perioperative surgical complications | 193 per 1000 | 336 per 1000 (224 to 502) | RR 1.74 (1.16 to 2.6) | 293 (4 studies) | ⊕⊕⊝⊝ low3 |
143 more women, per 1000, with traditional sling (31 more to 309 more) |
| Long‐term adverse effects Release of sling required | 25 per 1000 | 62 per 1000 (21 to 181) | RR 2.53 (0.87 to 7.35) | 326 (3 studies) | ⊕⊝⊝⊝ very low4 |
38 more women, per 1000, with traditional sling (3 fewer to 157 more) |
| Condition‐specific quality of life IIQ‐7 ‐ stress urinary incontinence (symptoms only) | Mean IIQ‐7 score in the control group was 24.4 | Mean condition‐specific quality of life score in the intervention groups was 0.6 higher (10.17 lower to 11.37 higher) | 63 (1 study) | ⊕⊝⊝⊝ very low5 | Eight other trials reported some measure of QoL but the data were unsuitable for met‐analysis. Overall, there was no evidence of a difference between groups in QoL scores | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; IIQ‐7: Incontinence Impact Questionnaire Short Form; OR: odds ratio; QoL: quality of life; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
1Downgraded one level due to serious risk of bias: 2/6 trials had high risk of selection bias.
2Downgraded two levels due to very serious imprecision: single study with small sample size.
3Downgraded two levels for risk of bias (sequence generation and allocation concealment were high or unclear risk in all four trials taking part in the meta‐analysis).
4Downgraded two levels for risk of bias (sequence generation and allocation concealment were high or unclear risk in two of three trials taking part in the meta‐analysis) and two levels for imprecision (95% confidence interval was very wide: 0.87 to 7.35).
5Downgraded two levels for risk of bias (sequence generation was judged to be high risk, and allocation concealment was judged to be low risk; outcome data were incomplete) and two levels for imprecision (95% confidence interval was very wide: ‐10.17 to 11.37).
Summary of findings 10. Traditional suburethral sling operation versus a single‐incision sling (mini‐sling).
| Traditional suburethral sling operation versus a single‐incision sling (mini‐sling) | ||||||
| Patient or population: women with urinary incontinence Settings: secondary care Intervention: sling Comparison: another type of sling | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Number of continent (dry) women (any definition) in the medium term (1 to 5 years) | 886 per 1000 |
886 per 1000 (641 to 971) |
OR 1.00 (0.23 to 4.36) |
70 (1 study) | ⊕⊝⊝⊝ very lowa,b |
0 fewer women, per 1000, with traditional sling (245 fewer to 86 more) |
| Repeat surgery for urinary incontinence | not reported | |||||
| Perioperative surgical complications ‐ bladder perforation | 0 per 1000 |
0 per 1000 (0 to 0) |
RR 3 (0.13 to 71.22) |
70 (1 study) | ⊕⊝⊝⊝ very lowa,b | |
| Long‐term adverse effects | not reported | |||||
|
Condition‐specific quality of life IIQ |
Mean IIQ score in the control group was 42.7 | Mean condition‐specific quality of life score in the intervention groups was 50.2 higher (2.23 higher to 12.77 higher) | 70 (1 study) | ⊕⊝⊝⊝ very lowa,b | Based on mean IIQ score, quality of life was worse in the traditional sling group compared with the mini‐sling group | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; IIQ: Incontinence Impact Questionnaire; OR: odds ratio; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aDowngraded two levels due to very serious risk of bias: unclear randomisation and inadequate blinding.
bDowngraded two levels due to very serious imprecision: single trial, small sample size, wide 95% confidence intervals.
Summary of findings 11. One type of traditional sling operation versus another traditional sling operation.
| One type of traditional sling operation versus another type of traditional sling operation | ||||||
| Patient or population: women with urinary incontinence Settings: secondary care Intervention: one type of traditional sling Comparison: another type of traditional sling | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Another type of traditional sling | One type of traditional sling | |||||
| Number of continent (dry) women (any definition) in the medium term (1 to 5 years) | Not estimable | 749 (7 studies) | ⊕⊝⊝⊝ very low1 | Results not pooled (Analysis 11.2) | ||
|
Repeat surgery for urinary incontinence at first year Fascial sling vs Pelvicol sling |
196 per 1000 |
8 per 1000 (0 to 119) |
RR 0.04 (0.00 to 0.61) |
113 (1 study) | ⊕⊕⊝⊝2 low |
188 fewer women, per 1000, with fascial sling (0 fewer to 76 fewer) (Analysis 11.4 |
| Perioperative surgical complications | Not estimable | 239 (3 studies) | ⊕⊝⊝⊝ very low3 | Results not pooled (Analysis 11.14) | ||
| Long‐term adverse effects Vaginal mesh or graft exposure | Not estimable | 421 (3 studies) | ⊕⊝⊝⊝ very low4 | Results not pooled (Analysis 11.23) | ||
| Condition‐specific quality of life ICI‐Q short form UI score at 1 to 5 years | Not estimable | 282 (1 study) | ⊕⊝⊝⊝ very low5 | Results not pooled* (Analysis 11.25) | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; ICI‐Q: International Consultation on Incontinence Questionnaire; RR: risk ratio; UI: urinary incontinence. | ||||||
| GRADE Working Group grades of evidence. High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
1Downgraded two levels for imprecision (Analysis 11.2) and two levels for heterogeneity, as the trials used different materials for the traditional sling procedure.
2Downgraded two levels for imprecision (Analysis 11.4)
3Downgraded one level for risk of bias (sequence generation was judged to be at low risk of bias in two of three trials and unclear in the third trial; allocation concealment was unclear in two of three trials). Blinding (performance bias and detection bias) was judged to be unclear (two of three) or high risk (one of three). Downgraded two levels for heterogeneity, as the trials used three different materials for the traditional sling procedure, and one level for inconsistency, as 95% CIs did not overlap (Analysis 11.14).
4Downgraded two levels for heterogeneity, as the trials used four different materials for the traditional sling procedure, and one level for imprecision, as the 95% CIs were very wide (Analysis 11.23).
5Downgraded two levels for heterogeneity, as the trials used three different materials for the traditional sling procedure, and one level for inconsistency, as 95% CIs did not overlap (Analysis 11.25).
* Data from two other trials were identified and are reported narratively in the text. These two trials did not report their data in a form suitable for meta‐analysis
Comparison 1. Traditional suburethral sling operation versus no treatment or sham operation
No trials were identified.
Comparison 2. Traditional suburethral sling operation versus conservative management
No trials were identified.
Comparison 3. Traditional suburethral sling operation versus drugs
One trial included 75 women with MUI treated with surgery (either Burch colposuspension (n = 24) or rectus fascia sling (n = 26)) or oxybutynin (an anticholinergic drug treatment for urinary incontinence, overactive bladder, and detrusor overactivity ‐ not for stress incontinence; n = 25)) (Osman 2003). The type of surgery was selected according to Valsalva leak point pressure (VLPP) ‐ those with VLPP of less than 90 cm of water had rectus fascia sling, and those with VLPP of more than 90 cm of water had Burch colposuspension.
Results for the surgically managed group were similar to those for the subgroup having slings. Due to small sample sizes, the data were too few to be reliable, and we therefore compared only data from oxybutynin versus sling patients in tables (Table 13).
2. Results for data from comparisons with single trials.
| Comparison 3. Traditional suburethral sling operation versus drugs | |
| Osman 2003 |
Osman 2003 included 75 women with mixed urinary incontinence treated with surgery (either Burch colposuspension (n = 24) or rectus fascia sling (n = 26)) or oxybutynin (an anticholinergic drug treatment for urinary incontinence, overactive bladder, and detrusor overactivity ‐ not for stress incontinence; n = 25) (Osman 2003). The type of surgery was selected according to Valsalva leak point pressure (VLPP) ‐ those with VLPP < 90 cm of water had rectus fascia sling, and those with VLPP > 90 cm of water had Burch colposuspension) Results for the surgically managed group were similar to those of the subgroup having slings. Due to small sample sizes, data were too few to be reliable; we therefore compared only data from oxybutynin versus sling patients provided in tables Primary outcomes Number of continent (dry) women Data suggest that, within the first year, women were significantly more likely to be continent after undergoing surgery with slings than after treatment with oxybutynin (20/24; 83% vs 0/21; OR 195.89, 95% CI 9.91 to 3871.03; n = 45; Analysis 3.1) Number of women who have repeat continence surgery Not reported Secondary outcomes Fewer women had persistent urgency urinary incontinence after traditional sling surgery (3/24; 13% vs 9/21; 43% with oxybutynin; RR 0.29, 95% CI 0.09 to 0.94; n = 45; Analysis 3.2) |
| Comparison 4. Traditional suburethral sling operation vs injectables | |
| Maher 2005 |
Maher 2005 compared slings (21) vs injectable Macroplastique (22) in 45 women. Due to the small size of the trial, the data were too few to be reliable Primary outcomes Number of continent (dry) women Short‐term: data from 1 small trial were too few to reliably identify evidence of a difference between traditional sling and injectables in the number of continent women within the first year (OR 2.79, 95% CI 0.48 to 16.33; n = 43; Maher 2005; Analysis 4.1) Medium‐term: Maher 2005 found no evidence of a difference between groups in the number of continent women after the first year (13/13; 100% continent with a traditional sling vs 10/14, 71% with the injectable; OR 11.57, 95% CI 0.56 to 239.74; n = 27; very low‐quality evidence; Analysis 4.2;Table 4) Number of women who have repeat continence surgery We found no evidence of a difference between groups in the numbers of women having repeat surgery for urinary incontinence (1 after traditional sling vs 2 after injectable: RR 0.52, 95% CI 0.05 to 5.36; n = 43; very low‐quality evidence; Maher 2005; Analysis 4.3;Table 4) Secondary outcomes Number of women cured at 1 year or later (women's observations) The trial was too small to reliably identify evidence of a difference between groups in the number of women cured after the first year (OR 11.57, 95% CI 0.56 to 239.74; n = 27; Analysis 4.4) Number of women improved Not reported Number of women satisfied Data from Maher 2005 were too few to identify a difference between groups in satisfaction rates at 6 months (P = 0.41) or at 5 years (RR 2.42, 95% CI 0.98 to 5.98; n = 27; Analysis 4.5) Quantification of symptoms Not reported Clinician's observations Data suggest there were more women with incontinence (clinician‐observed) within the first year with injectables compared with the traditional sling: 4/21 vs 20/22 (RR 0.21, 95% 0.09 to 0.21; n = 43; Maher 2005; Analysis 4.6) Surgical outcome measures Injectables were quicker to perform, involved shorter hospital stay and time to catheter removal, and led to quicker return to normal activity than after traditional sling surgery, but the data were not suitable for meta‐analysis (Maher 2005) Further treatment Not reported Adverse events Perioperative surgical complications Not reported Bladder perforation Not reported Urinary tract infection Maher 2005 reported no evidence of a difference between traditional slings and injectables in the numbers of women with urinary tract infection (RR 1.57, 95% CI 0.29 to 8.49; very low‐quality evidence; Analysis 4.7;Table 4) Urinary urgency symptoms, urgency urinary incontinence Not reported Detrusor overactivity (urodynamic overactivity) Maher 2005 reported no evidence of a difference between traditional slings and injectables in the numbers of women with de novo detrusor overactivity (RR 3.14, 95% CI 0.13 to 72.96; Analysis 4.8) Voiding dysfunction (with or without urodynamic confirmation) Maher 2005 reported no evidence of a difference between traditional slings and injectables in the numbers of women with voiding dysfunction (RR 4.19, 95% CI 0.51 to 34.50; Analysis 4.9) Long‐term adverse effects Not reported Quality of life Maher 2005 reported a significant reduction in Incontinence Impact Questionnaire (IIQ) scores compared with baseline (P < 0.01) in both groups, although he provided no data |
| Comparison 6. Traditional suburethral sling operation vs bladder neck needle suspension (abdominal and vaginal) | |
| Hilton 1989 | Only 1 trial compared porcine dermis sling vs Stamey needle suspension (Hilton 1989). This was a small trial with only 10 women in each arm. The women were unsuitable for abdominal colposuspension (the study author's preferred procedure) because they had vaginal narrowing secondary to previous interventions or atrophic vaginitis. Thus they constitute a population of women with SUI who are not typical of the majority. All women had urodynamic stress incontinence. Groups were comparable for age, parity, previous interventions, and hormonal status. Follow‐up was reported at 3 months and 24 months. Due to the small size of the trial, the data were too few to be reliable Primary outcomes Number of continent (dry) women Short‐term: within the first year after surgery, 1 small trial reported 9/10 and 8/10 continent women in the traditional sling and needle suspension groups, respectively (OR 2.25, 95% CI 0.17 to 29.77; n = 20; Hilton 1989; Analysis 6.1) Medium‐term: very low‐quality evidence from 1 trial comparing slings vs bladder neck needle suspension suggested no evidence of a difference between groups in the likelihood of being continent at 2 years after surgery (OR 3.86, 95% CI 0.33 to 45.57; n = 20; Hilton 1989; Analysis 6.2;Table 6) Long‐term: not reported Number of women who have repeat continence surgery Not reported Secondary outcomes Women's observations Number of women cured at 1 year or later (women's observations) Evidence from 1 small trial comparing slings vs bladder neck needle suspension suggests no difference between groups in cure rates at 2 years after surgery (OR 3.86, 95% CI 0.33 to 45.57; n = 20; Hilton 1989) Quantification of symptoms Pad test at 12 months and 24 months stated but not reported (Hilton 1989) Clinician's observations Not reported Surgical outcome measures Duration of operation Not reported Length of hospital stay Sling group needed an indwelling catheter for longer and more adjuvant therapy, resulting in a longer stay in hospital than those with bladder neck needle suspension (MD 13 days longer, 95% CI 5 to 21; n = 20; Hilton 1989; Analysis 6.4) Time to return to normal activity level Not reported Blood loss Not reported Further treatment Not reported Adverse events Perioperative surgical complications Nine of the 10 women who had sling operations had complications, compared with 2/10 who had needle suspension. These included pyrexia, blood loss, wound infection, and pulmonary embolus (RR 4.50, 95% CI 1.28 to 15.81; n = 20; very low‐quality evidence; Hilton 1989; Analysis 6.5;Table 6) Bladder perforation Not reported Urinary tract infection Not reported Urinary urgency symptoms, urgency urinary incontinence At 3 months: sling: 5/10, needle suspension: 3/10 (Hilton 1989; Analysis 6.6) Detrusor overactivity (urodynamic overactivity) At 3 months: sling: 2/10, needle suspension: 1/10 (Hilton 1989; Analysis 6.7) Voiding dysfunction (with or without urodynamic confirmation) At 3 months: sling: 4/10, needle suspension: 2/10 (Hilton 1989; Analysis 6.8) Long‐term adverse effects Not reported Quality of life Not reported |
| Comparison 10. Traditional suburethral sling operation vs a single‐incision sling (mini‐sling) | |
| Sharifiaghdas 2015 | One small trial compared a rectus fascia pubovaginal traditional sling vs a single‐incision sling (mini‐sling; Ophira) and included women with urodynamically diagnosed stress urinary incontinence (USI) (Sharifiaghdas 2015) Due to the small size of the trial, the data were too few to be reliable Primary outcomes Number of continent (dry) women Short‐term: not reported Medium‐term: exactly the same proportion of women were continent at 1 year after surgery (traditional sling: 31/35; mini‐sling: 31/35; very low‐quality evidence; Sharifiaghdas 2015; Analysis 10.1;Table 10) Long‐term: not reported Number of women who have repeat continence surgery Not reported Secondary outcomes Women's observations Cure For self‐report of cure at 1 year after surgery, exactly the same proportion of women were cured (traditional sling: 31/35; mini‐sling: 31/35; Sharifiaghdas 2015; Analysis 10.2) Number of women improved Not reported Number of women satisfied 10/35 women in the traditional sling group and 7/35 in the mini‐sling group reported that they were satisfied with their treatment at 1 year (RR 0.89, 95% CI 0.68 to 1.17; n = 70; Sharifiaghdas 2015; Analysis 10.3) Quantification of symptoms Not reported Clinician's observations The clinician's report of observed stress incontinence concurred with that reported by women ‐ 4 in each group (RR 1.00, 95% CI 0.27 to 3.69; n = 70; Sharifiaghdas 2015) Surgical outcome measures Not reported Further treatment Not reported Adverse effects Perioperative complications Not reported Bladder perforation One woman (of 35) had a bladder perforation in the traditional sling group compared with none (of 35) in the mini‐sling group (very low‐quality evidence; Sharifiaghdas 2008; Analysis 10.5;Table 10) Urinary tract infection Not reported Urinary urgency symptoms, urgency urinary incontinence More women in the traditional sling group reported urinary urgency incontinence (5/35) compared with the mini‐sling group (1/35) (RR 5.00, 95% CI 0.62 to 40.64; n = 70; Sharifiaghdas 2015; Analysis 10.6) Detrusor overactivity (urodynamic overactivity) Not reported Voiding dysfunction (with or without urodynamic confirmation) Not reported Long‐term adverse effects Dyspareunia: 3/35 and 4/35 in traditional sling and mini‐sling groups, respectively, reported pain with intercourse (RR 0.75, 95% CI 0.18 to 3.11; n = 70; Sharifiaghdas 2008; Analysis 10.7) Tape or mesh exposure: 1 woman in the traditional sling group and 2 in the mini‐sling group were found to have tape or mesh exposure (RR 0.50, 95% CI 0.05 to 5.27; n = 70; Sharifiaghdas 2008; Analysis 10.8) Quality of life Based on mean IIQ score, quality of life was lower in the traditional sling group compared with the mini‐sling group (MD 7.50, 95% CI 2.23 to 12.77; very low‐quality evidence; Analysis 10.9;Table 10) |
USI: urodynamically diagnosed stress urinary incontinence
VLPP: Valsalva leak point pressure
Comparison 4. Traditional suburethral sling operation versus injectables
Maher 2005 compared slings (n = 21) with injectable Macroplastique (n = 22). Based on very low‐quality evidence, we are uncertain about the impact of surgery versus injectables in terms of the number of continent women (100% were dry with a traditional sling vs 71% with the injectable after the first year; odds ratio (OR) 11.57, 95% confidence interval (CI) 0.56 to 239.74; Analysis 4.2), the need for repeat surgery for urinary incontinence (risk ratio (RR) 0.52, 95% CI 0.05 to 5.36; Analysis 4.3), or perioperative complications such as urinary tract infection (RR 1.57, 95% CI 0.29 to 8.49; Analysis 4.7).
4.2. Analysis.
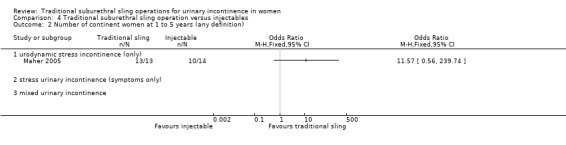
Comparison 4 Traditional suburethral sling operation versus injectables, Outcome 2 Number of continent women at 1 to 5 years (any definition).
4.3. Analysis.
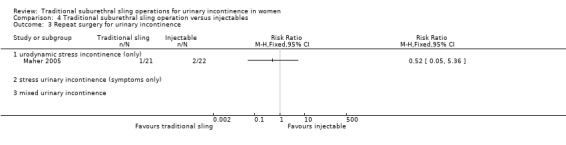
Comparison 4 Traditional suburethral sling operation versus injectables, Outcome 3 Repeat surgery for urinary incontinence.
4.7. Analysis.
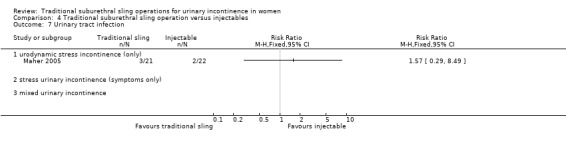
Comparison 4 Traditional suburethral sling operation versus injectables, Outcome 7 Urinary tract infection.
Due to the small size of the trial, the data were too few to be reliable (Table 4; Table 13).
Comparison 5. Traditional suburethral sling operation versus anterior repair
No trials were identified.
Comparison 6. Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal)
Only one trial compared porcine dermis sling with Stamey needle suspension (Hilton 1989). This was a small trial with only 10 women in each arm. The women were unsuitable for abdominal colposuspension (the study author's preferred procedure) because they had vaginal narrowing secondary to previous interventions or atrophic vaginitis. Thus they constitute a population of women with SUI who are not typical of the majority. All women had USI. Groups were comparable for age, parity, previous interventions, and hormonal status. Follow‐up was reported at 3 months and at 24 months.
Due to the small size of the trial, the data were too few to be reliable (Table 6; Table 13).
Comparison 7. Traditional suburethral sling operation versus open abdominal retropubic colposuspension
Eight trials compared slings with open abdominal retropubic colposuspension (Albo 2007; Bai 2005; Demirci 2001; Enzelsberger 1996; Fischer 2001; Helmy 2012; Henriksson 1978; Sand 2000). One of these trials provided no data (Helmy 2012). The extent to which the trials could be considered together was limited because of differences in procedures compared, populations studied, outcomes assessed, and length of follow‐up. Two trials involved a pubovaginal sling technique using autologous rectus fascia (Albo 2007; Demirci 2001). One trial used a lyodura sling (Enzelsberger 1996). Another trial used the Zoedler sling made of Teflon (Henriksson 1978). Still another trial used the Gortex type (Sand 2000). These were all biological materials except in two trials (Henriksson 1978; Sand 2000). Fischer 2001 did not specify the sling material used.
Only two of these trials reported follow‐up for longer than five years and presented both short‐term and long‐term data in two full reports (Albo 2007; Sand 2000).
Primary outcomes
Number of continent (dry) women
Short term
Data from four trials suggested no evidence of a difference in the likelihood of being continent within a year after treatment when comparing slings to open abdominal colposuspension (OR 2.70, 95% CI 0.69 to 10.55; n = 147; Analysis 7.1) (Bai 2005; Fischer 2001; Henriksson 1978; Sand 2000).
7.1. Analysis.
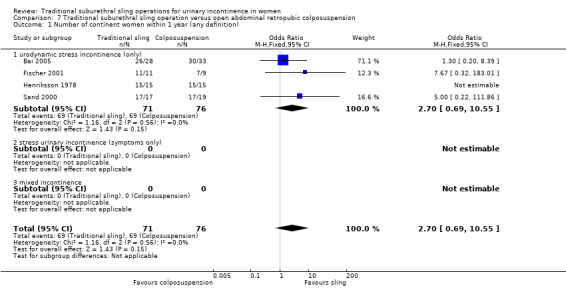
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 1 Number of continent women within 1 year (any definition).
Medium term
Moderate‐quality evidence from four trials show that women were more likely to be continent between one and five years after surgery with slings compared with open abdominal colposuspension (OR 1.70, 95% CI 1.22 to 2.37; n = 687; Analysis 7.2;Table 7) (Albo 2007; Bai 2005; Demirci 2001; Enzelsberger 1996).
7.2. Analysis.
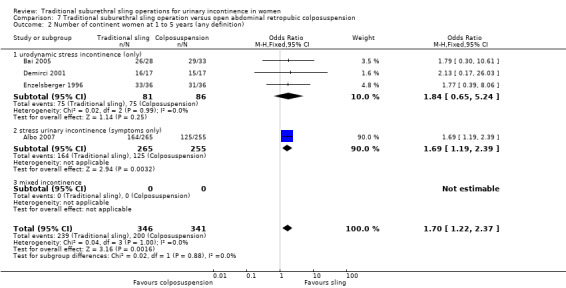
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 2 Number of continent women at 1 to 5 years (any definition).
Long term
At five years post surgery and beyond, evidence from two trials suggests that women were more likely to be continent after surgery with slings than after open abdominal colposuspension (OR 1.55, 95% CI 1.06 to 2.27; n = 190; Analysis 7.3) (Albo 2007; Sand 2000).
7.3. Analysis.
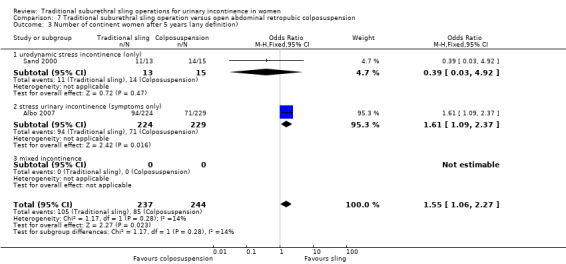
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 3 Number of continent women after 5 years (any definition).
Number of women who had repeat continence surgery
High‐quality evidence from one trial shows that the risk of required repeat continence surgery was lower after traditional slings compared to after open abdominal colposuspension (RR 0.15, 95% CI 0.05, 0.42; n = 450; Analysis 7.4; Table 7) (Albo 2007).
7.4. Analysis.
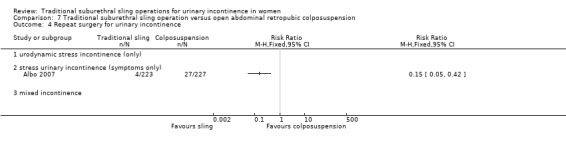
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 4 Repeat surgery for urinary incontinence.
Secondary outcomes
Women's observations
Number of women cured at one year or later (women's observations)
Data from three trials suggest that women undergoing surgery with slings were more likely to report subjective cure than women having open abdominal colposuspension (OR 1.56, 95% CI 1.07 to 2.28; n = 221; Analysis 7.5) (Albo 2007; Demirci 2001; Sand 2000).
7.5. Analysis.
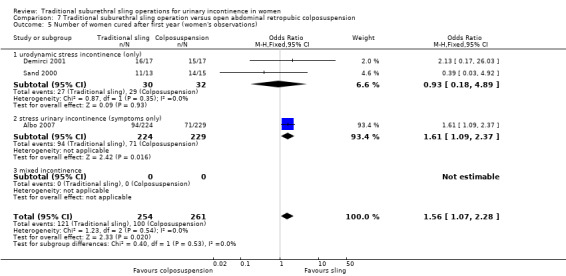
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 5 Number of women cured after first year (women's observations).
Number of women improved
This was not reported.
Number of women satisfied
Data from one trial indicate that more women were likely to be satisfied with surgery with slings than with open abdominal colposuspension (RR 1.14, 95% CI 1.02 to 1.27; n = 352; Analysis 7.6) (Albo 2007).
7.6. Analysis.
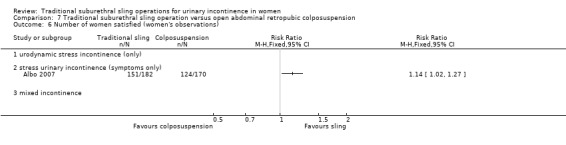
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 6 Number of women satisfied (women's observations).
Quantification of symptoms
This was not reported.
Clinician's observations
Number of women with urinary incontinence (clinician's observations)
Short term
This was not reported.
Medium term and long term
Researchers found no evidence of a difference between slings and open abdominal colposuspension in the numbers of women with urinary incontinence at one to five years (RR 0.88, 95% CI 0.59 to 1.31; n = 626; Analysis 7.8) (Albo 2007; Demirci 2001; Enzelsberger 1996). Depending on judgements about what constitutes a clinically important difference between interventions with regard to continence, traditional suburethral slings are probably no worse, and may be slightly more effective, than colposuspension beyond five years (RR 0.90, 95% CI 0.80 to 1.01, n = 461; Analysis 7.9) (Albo 2007; Sand 2000).
7.8. Analysis.
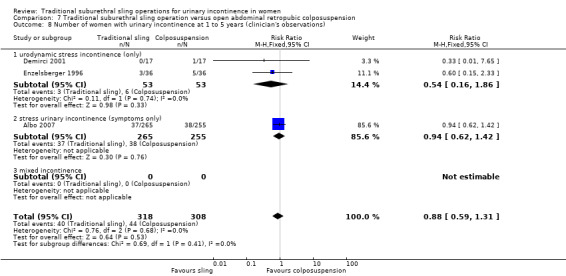
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 8 Number of women with urinary incontinence at 1 to 5 years (clinician's observations).
7.9. Analysis.
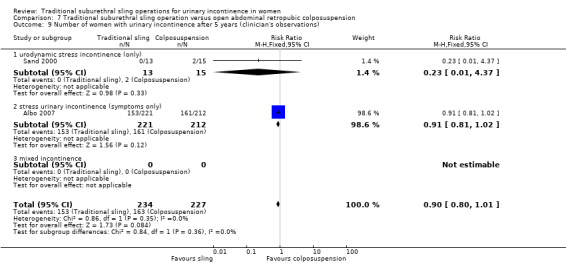
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 9 Number of women with urinary incontinence after 5 years (clinician's observations).
Surgical outcome measures
Duration of operation
One trial was too small to reliably detect a difference in operating times between slings (61 minutes) and open abdominal colposuspension (55 minutes) (mean difference (MD) 6.02, 95% CI ‐0.52 to 12.56; Analysis 7.10) (Demirci 2001). Moreover, the difference in the duration of operation time observed was too small to be of clinical importance.
7.10. Analysis.
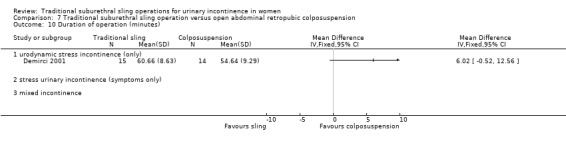
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 10 Duration of operation (minutes).
Length of hospital stay/time to catheter removal
Data from three trials suggest that women undergoing surgery with slings had longer hospital stays than women having open abdominal colposuspension (MD 2.03 days, 95% CI 1.47 to 2.59; n = 137; Analysis 7.11) (Demirci 2001; Enzelsberger 1996; Sand 2000). This may have been due in part to a difference in the time of catheter use after surgery (women in the sling group used a sling for eight days longer (MD) after sling than after colposuspension; 95% CI 6.84 to 9.18, n = 108; Analysis 7.12). However, it is unclear if this was due to the procedures themselves or to differences in hospital policies.
7.11. Analysis.
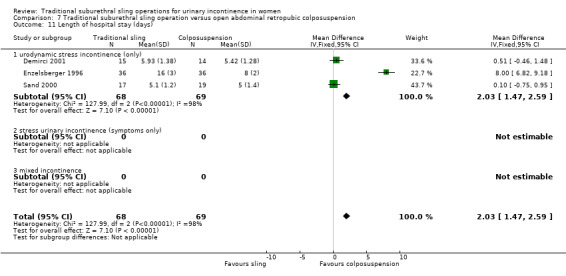
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 11 Length of hospital stay (days).
7.12. Analysis.
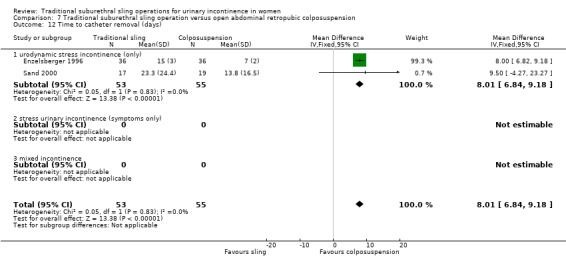
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 12 Time to catheter removal (days).
Time to return to normal activity level
This was not reported.
Blood loss
This was not reported.
Further treatment
Three trials reported that significantly more women required treatment for a new or recurrent prolapse after open colposuspension (12/282; 4.3%) compared to after a sling procedure (2/277; 0.7%; RR 0.20, 95% CI 0.05 to 0.77; n = 559; Analysis 7.14) (Albo 2007; Demirci 2001; Enzelsberger 1996). However, trial authors provided no information about subsequent surgery for prolapse in any trial.
7.14. Analysis.
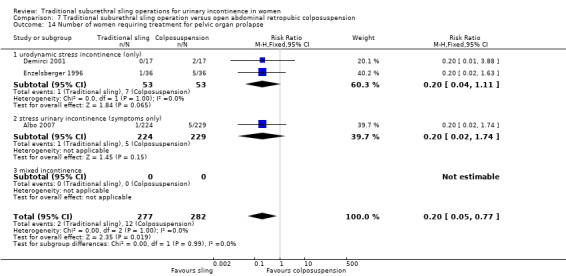
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 14 Number of women requiring treatment for pelvic organ prolapse.
Adverse events
Perioperative surgical complications
Four trials reported similar numbers of perioperative complications in the groups (47/394; 12% vs 38/398; 10%; RR 1.24, 95% CI 0.83 to 1.86; n = 792; low‐quality evidence; Analysis 7.15;Table 7) (Albo 2007; Demirci 2001; Enzelsberger 1996; Sand 2000).
7.15. Analysis.
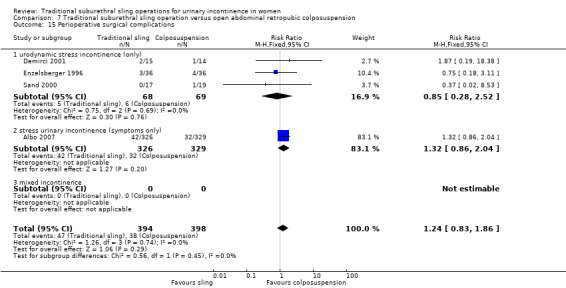
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 15 Perioperative surgical complications.
Bladder perforation
One large trial reported significantly lower risk of bladder perforation with the sling procedure (RR 0.20, 95% CI 0.04 to 0.91; Analysis 7.16) (Albo 2007).
7.16. Analysis.
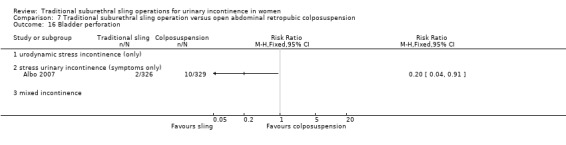
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 16 Bladder perforation.
Urinary tract infection
Researchers reported significantly more urinary tract infections with the sling procedure soon after surgery compared with colposuspension (RR 1.50, 95% CI 1.33 to 1.70; n = 655; Analysis 7.17). However, the risk of recurrent urinary tract infection (UTI) was not statistically different at five years or later (RR 1.02, 95% CI 0.57 to 1.82; n = 453; low‐quality evidence; Analysis 7.18;Table 7) (Albo 2007).
7.17. Analysis.
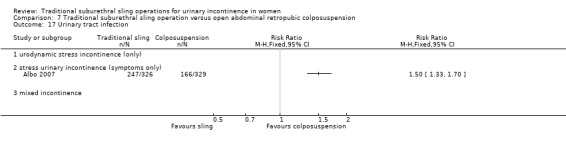
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 17 Urinary tract infection.
7.18. Analysis.
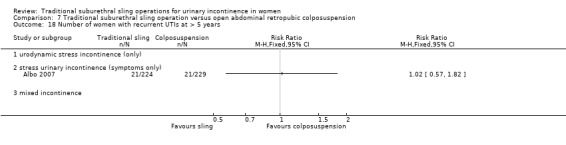
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 18 Number of women with recurrent UTIs at > 5 years.
Urinary urgency symptoms; urgency urinary incontinence
Two trials reported data on de novo urgency symptoms or incontinence: the evidence was insufficient to identify whether there was a difference between sling and colposuspension groups (RR 1.10, 95% CI 0.74 to 1.64; Analysis 7.19) (Albo 2007; Enzelsberger 1996).
7.19. Analysis.
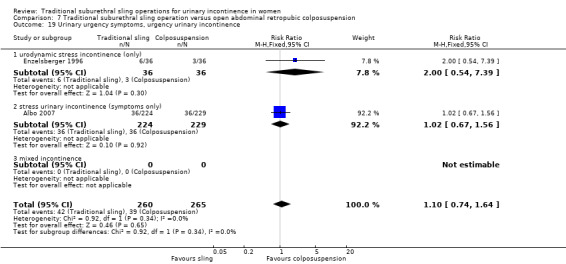
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 19 Urinary urgency symptoms, urgency urinary incontinence.
Detrusor overactivity (urodynamic overactivity)
Evidence from four small trials was insufficient to show whether there was a difference in detrusor overactivity between sling and colposuspension groups (RR 1.42, 95% CI 0.52 to 3.87; Analysis 7.20) (Bai 2005; Demirci 2001; Enzelsberger 1996; Sand 2000).
7.20. Analysis.
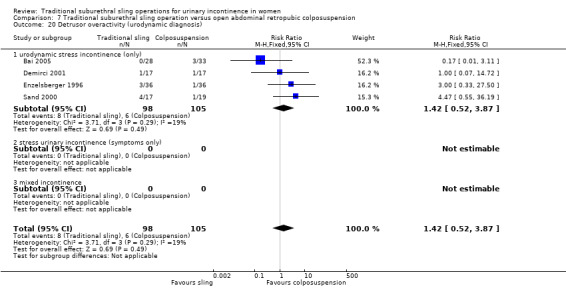
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 20 Detrusor overactivity (urodynamic diagnosis).
Voiding dysfunction (with or without urodynamic confirmation)
Pooled data from five trials show that significantly more women had voiding dysfunction after sling (13% vs 2% after open colposuspension; RR 6.08, 95% CI 3.10 to 11.95; moderate‐quality evidence; Analysis 7.21) (Albo 2007; Bai 2005; Demirci 2001; Enzelsberger 1996; Sand 2000). One trial reported long‐term voiding dysfunction at five years or later (Albo 2007). Very few women still reported this complication (seven after sling vs one after colposuspension).
7.21. Analysis.
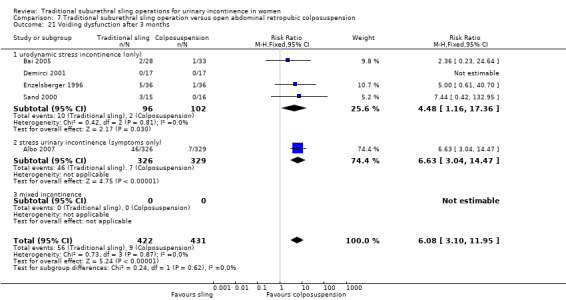
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 21 Voiding dysfunction after 3 months.
Long‐term adverse effects
This was not reported.
Quality of life
Data were reported in different formats; thus meta‐analysis was not possible.
One trial reported quality of life scores at over five years (Albo 2007). Women reported better quality of life after the sling surgery on one scale (Urogenital Distress Inventory (UDI)) (MD ‐10, 95% CI ‐18.91 to ‐1.09) but no difference on another scale (Incontinence Impact Questionnaire (IIQ)) (MD 1.70, 95% CI ‐11.96 to 15.36; very low‐quality evidence; Table 7).
One trial reported no significant difference in IIQ and UDI scores between the colposuspension group and the sling group, although actual numbers were not reported (Fischer 2001).
Comparison 8. Traditional suburethral sling operation versus laparoscopic colposuspension
No trials were identified.
Comparison 9. Traditional suburethral sling operation versus mid‐urethral sling or tape
Fifteen trials addressed this comparison (Abouhashem 2014; Al‐Azzawi 2014; Amaro 2007; Arunkalaivanan 2003; Bai 2005; Basok 2008; Guerrero 2008; Kondo 2006; Sharifiaghdas 2008; Silva Filho 2006; Song 2004; Tcherniakovsky 2009; Teixeira 2008; Wadie 2005; Zargham 2013). Two new trials were added in this update (Abouhashem 2014; Zargham 2013). However, one of the new trials did not provide any useable data (Abouhashem 2014). Three trials were updated (Amaro 2007; Guerrero 2008; Wadie 2005).
Primary outcomes
Number of continent (dry) women
Short term
Data from 11 trials suggest there was no evidence of a difference between traditional slings and mid‐urethral slings in the likelihood of being continent within one year (73% vs 75%; OR 0.94, 95% CI 0.67 to 1.32; n = 841; Analysis 9.1) (Amaro 2007; Arunkalaivanan 2003; Bai 2005; Basok 2008; Guerrero 2008; Kondo 2006; Sharifiaghdas 2008; Song 2004; Tcherniakovsky 2009; Wadie 2005; Zargham 2013).
9.1. Analysis.
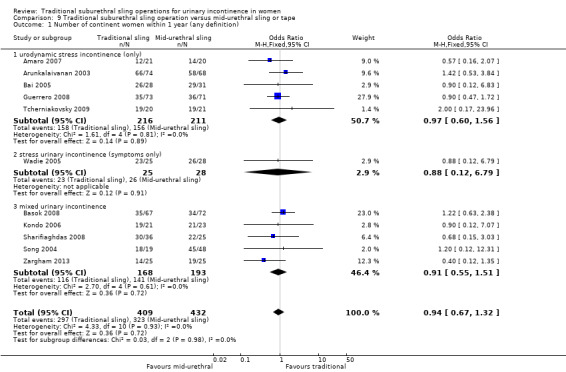
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 1 Number of continent women within 1 year (any definition).
Medium term
Depending on judgements about what constitutes a clinically important difference between interventions with regard to continence, traditional suburethral slings are probably no better, and may be less effective, than mid‐urethral slings in terms of number of women continent in the medium term (one to five years). However, the results were not statistically significant (67% vs 74%, OR 0.67, 95% CI 0.44 to 1.02; n = 458; moderate‐quality evidence); Analysis 9.2;Table 9) (Amaro 2007; Arunkalaivanan 2003; Bai 2005; Guerrero 2008; Kondo 2006; Zargham 2013).
9.2. Analysis.
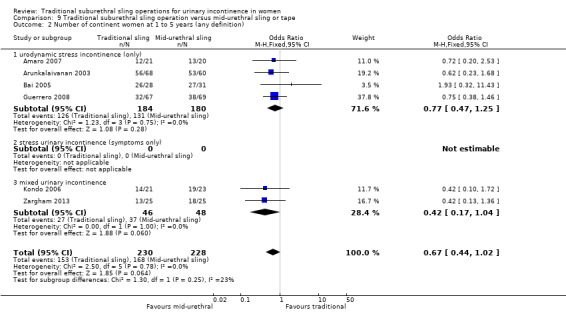
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 2 Number of continent women at 1 to 5 years (any definition).
Long term
Data from one small trial suggest that women undergoing traditional sling operations were nearly twice as likely to be continent at five years after traditional sling surgery as women who had received a mid‐urethral sling (51% vs 32%; OR 2.22, 95% CI 1.07 to 4.61; n = 124; Analysis 9.3) (Guerrero 2008).
9.3. Analysis.
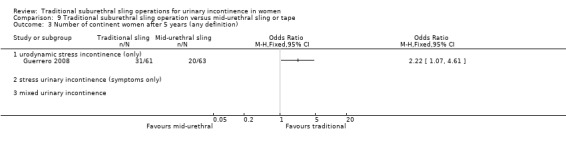
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 3 Number of continent women after 5 years (any definition).
Number of women who had repeat continence surgery
Low‐quality evidence from one trial reported the numbers of women having repeat continence surgery; no women in either arm required repeat surgery (traditional sling: 0/67; mid‐urethral sling: 0/69; Analysis 7.4;Table 9) (Guerrero 2008). By 10 years, 2 of 63 women still being followed‐up after a mid‐urethral sling had required repeat continence surgery compared to none in the traditional sling group.
Secondary outcomes
Women's observations
Number of women cured after the first year (women's observations)
Four trials provided no evidence of a difference between traditional slings and mid‐urethral slings in the likelihood of cure at one year or later (OR 1.06, 95% CI 0.65 to 1.72; n = 337; Analysis 9.5) (Amaro 2007; Arunkalaivanan 2003; Guerrero 2008; Kondo 2006).
9.5. Analysis.
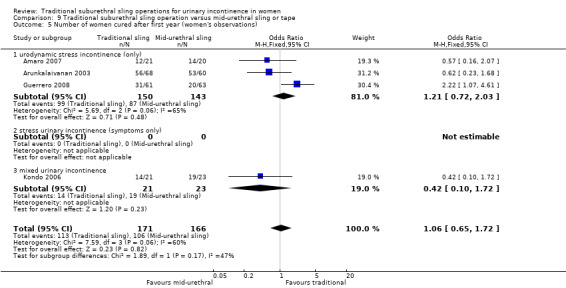
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 5 Number of women cured after first year (women's observations).
Number of women improved or cured
Trials provided no evidence of a difference between traditional slings and mid‐urethral slings in the likelihood of improvement or cure:
within one year (OR 1.33, 95% CI 0.74 to 2.39; n = 425; Analysis 9.6) (Arunkalaivanan 2003; Basok 2008; Guerrero 2008);
at one to five years (OR 0.76, 95% CI 0.31 to 1.87; n = 264; (Analysis 9.7) (Arunkalaivanan 2003; Guerrero 2008); or
after five years (OR 1.13, 95% CI 0.51 to 2.54; n = 124; Analysis 9.8) (Guerrero 2008).
9.6. Analysis.
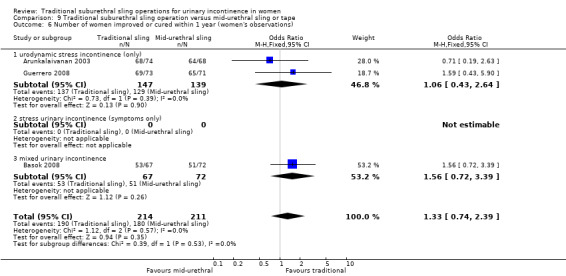
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 6 Number of women improved or cured within 1 year (women's observations).
9.7. Analysis.
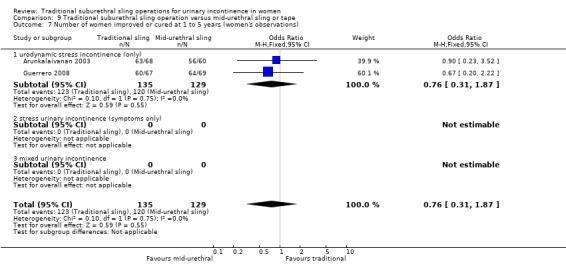
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 7 Number of women improved or cured at 1 to 5 years (women's observations).
9.8. Analysis.
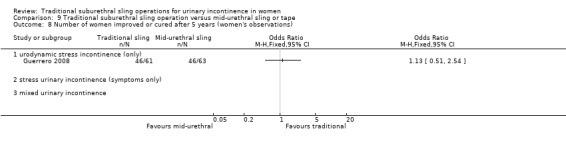
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 8 Number of women improved or cured after 5 years (women's observations).
Number of women satisfied
No evidence suggests a difference between traditional slings and mid‐urethral slings in the likelihood of women being satisfied (RR 1.09, 95% CI 0.89 to 1.33; n = 163; Analysis 9.9) (Amaro 2007; Guerrero 2008).
9.9. Analysis.
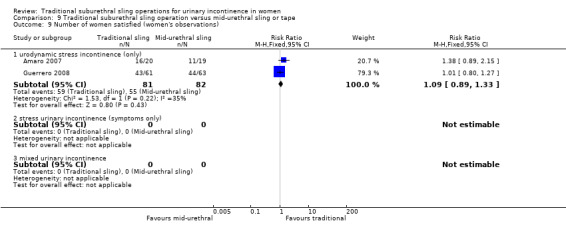
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 9 Number of women satisfied (women's observations).
Quantification of symptoms
Pad changes over 24 hours (from self‐reported number of pads used)
This was not reported.
Incontinent episodes over 24 hours (from self‐completed bladder chart)
This was not reported.
Pad test of quantified leakage (mean weight of urine loss)
One small trial reported the mean weight of urine on a pad test (Silva Filho 2006). Data show less incontinence in the traditional sling group compared with the mid‐urethral sling group (MD ‐31.00 grams, 95% CI ‐57.53 to ‐4.47; n = 20; Analysis 9.10).
9.10. Analysis.
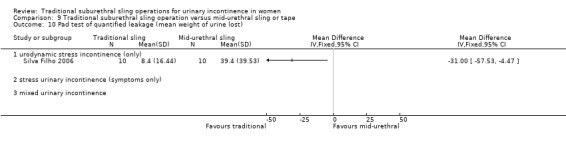
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 10 Pad test of quantified leakage (mean weight of urine lost).
Clinician's observations
Number of women with urinary incontinence
Short term
Clinician‐reported incontinence within one year, defined as complete absence of urinary leakage during a cough‐stress test, was assessed in two small trials (Kondo 2006; Sharifiaghdas 2008), which provided no evidence of a difference between the two groups (RR 1.29, 95% CI 0.45 to 3.71; Analysis 9.11).
9.11. Analysis.
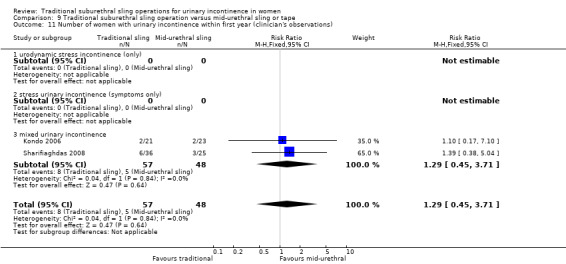
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 11 Number of women with urinary incontinence within first year (clinician's observations).
One trial further addressed objective cure after the first year, but again the evidence was insufficient to reveal whether there was a difference between groups, as the confidence interval was wide (RR 1.72, 95% CI 0.82 to 3.61; n = 44; Analysis 9.12) (Kondo 2006).
9.12. Analysis.
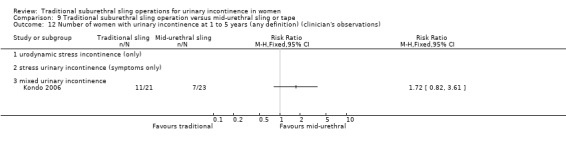
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 12 Number of women with urinary incontinence at 1 to 5 years (any definition) (clinician's observations).
Surgical outcome measures
Duration of operation
Traditional suburethral sling operations took significantly longer to complete (MD 57.08 minutes, 95% CI 54.67 to 59.49; Analysis 9.13). There was statistically significant heterogeneity that could not be explained by differences in populations, interventions, or settings of the individual trials. This heterogeneity persisted even after sensitivity analysis was performed. This excludes the largest trial, which showed a much longer operating time for the traditional sling operation than was seen in the other trials (Song 2004). It also excludes another trial in which women also had concomitant prolapse surgery in both arms, and in the mid‐urethral sling arm, an additional mesh kit was used to repair the prolapse (Zargham 2013). Because of heterogeneity in trials that included women with MUI, some of whom also had concomitant prolapse surgery, a sensitivity analysis was performed excluding the four trials (Al‐Azzawi 2014; Kondo 2006; Song 2004; Zargham 2013). The mean difference in operative time was 44 minutes longer for traditional sling surgery (95% CI 40 to 48; analysis not shown).
9.13. Analysis.
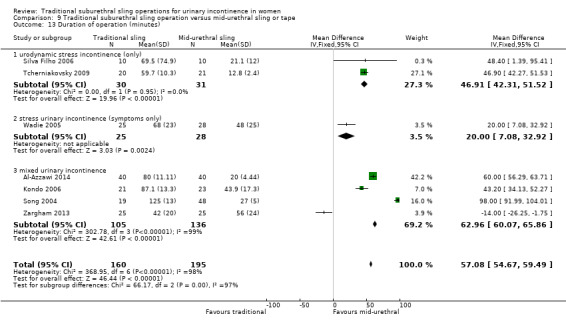
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 13 Duration of operation (minutes).
Length of hospital stay and duration of catheterisation
In four small trials, the length of hospital stay was longer after traditional sling operations (RR 0.74 days, 95% CI 0.55 to 0.93; Analysis 9.14) (Al‐Azzawi 2014; Kondo 2006; Silva Filho 2006; Zargham 2013). Two trials reported no evidence of a difference between groups in length of time to catheter removal (MD 0.11 days, 95% ‐0.07 to 0.30; Analysis 9.15) (Kondo 2006; Wadie 2005).
9.14. Analysis.
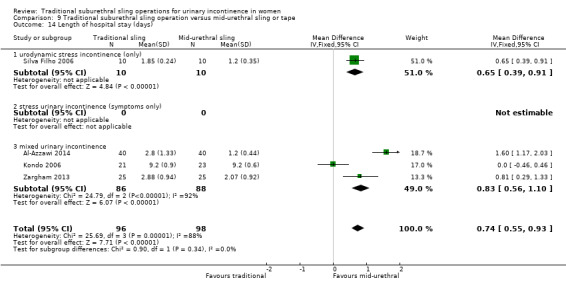
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 14 Length of hospital stay (days).
9.15. Analysis.
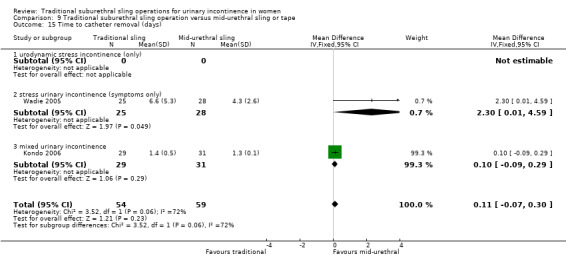
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 15 Time to catheter removal (days).
Time to return to normal activity level
This was not reported.
Blood loss
This was not reported.
Further treatment
This was not reported.
Adverse events
Perioperative complications
Low‐quality evidence from four trials was insufficient to identify whether risk of perioperative complications was higher after traditional sling operations (49/148; 33.1% vs 28/145; 19.3% after a mid‐urethral sling; RR 1.74, 95% CI 1.16 to 2.60; n = 293; Analysis 9.16;Table 9) (Arunkalaivanan 2003; Kondo 2006; Tcherniakovsky 2009; Zargham 2013).
9.16. Analysis.
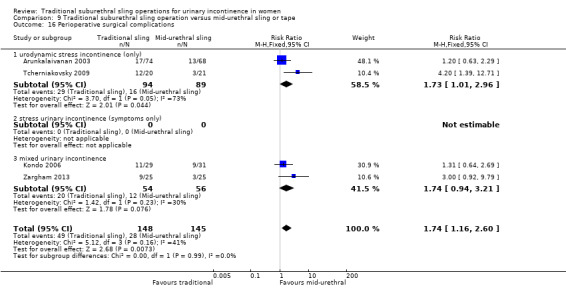
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 16 Perioperative surgical complications.
Bladder perforation
Evidence from 10 RCTs shows that traditional slings may have fewer bladder perforations compared with mid‐urethral slings. However, whilst there is no evidence of a statistical difference in the number of bladder perforations, the confidence interval may rule out clinically important reductions for mid‐urethral slings (17/414; 4.1% vs 30/430; 6.9%; RR 0.59, 95% CI 0.34 to 1.01; n = 844; Analysis 9.17) (Al‐Azzawi 2014; Arunkalaivanan 2003; Bai 2005; Guerrero 2008; Kondo 2006; Sharifiaghdas 2008; Song 2004; Tcherniakovsky 2009; Wadie 2005; Zargham 2013).
9.17. Analysis.
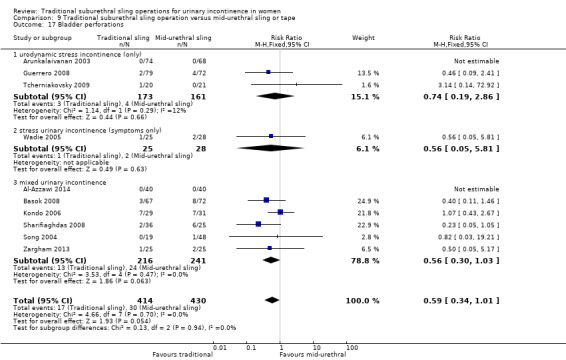
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 17 Bladder perforations.
Urinary tract infection
Trials provided no evidence of a difference between traditional slings and mid‐urethral slings in the number of women with urinary tract infections (RR 1.00, 95% CI 0.22 to 4.49; n = 50; Analysis 9.20) (Zargham 2013).
9.20. Analysis.
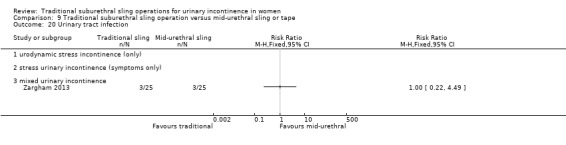
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 20 Urinary tract infection.
Urinary urgency symptoms; urgency urinary incontinence
Combined results from four trials were insufficient to show whether there was a difference between traditional slings and mid‐urethral slings in the number of women with urinary urgency symptoms (RR 1.50, 95% CI 0.58 to 3.88; Analysis 9.22) (Guerrero 2008; Kondo 2006; Sharifiaghdas 2008; Zargham 2013).
9.22. Analysis.
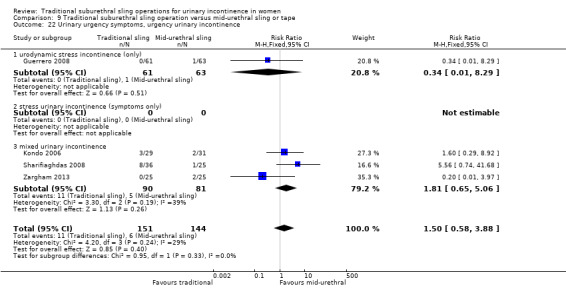
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 22 Urinary urgency symptoms, urgency urinary incontinence.
Detrusor overactivity (urodynamic overactivity)
Data from four trials suggest higher risk of detrusor overactivity after traditional sling operations than after mid‐urethral sling operations (RR 2.61, 95% CI 1.17 to 5.84; n = 325; Analysis 9.23) (Al‐Azzawi 2014; Bai 2005; Basok 2008; Wadie 2005). This was principally due to the higher weighting given to the largest trial (Basok 2008).
9.23. Analysis.
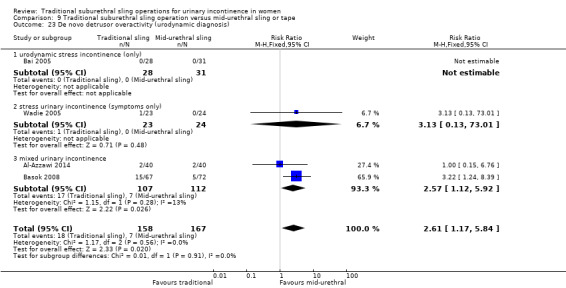
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 23 De novo detrusor overactivity (urodynamic diagnosis).
Voiding dysfunction
Very low‐quality evidence from eight trials suggests no difference between traditional slings and mid‐urethral slings in the number of women with voiding dysfunction (RR 1.34, 95% CI 0.85 to 2.12; n = 629; Table 9) (Al‐Azzawi 2014; Arunkalaivanan 2003; Bai 2005; Guerrero 2008; Kondo 2006; Sharifiaghdas 2008; Wadie 2005; Zargham 2013).
Long‐term adverse effects
Wound pain
Three trials reported that more women had long‐term wound pain in the traditional sling groups (17/126 vs 2/131; RR 6.40, 95% CI 1.94 to 21.12; n = 257; Analysis 9.25) (Al‐Azzawi 2014; Guerrero 2008; Wadie 2005).
9.25. Analysis.
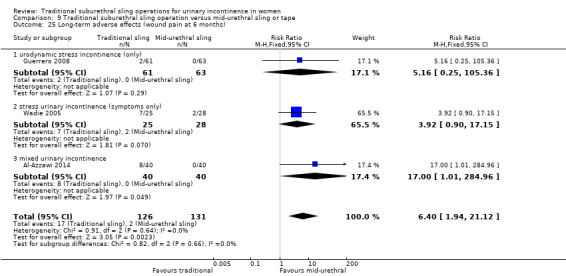
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 25 Long‐term adverse effects (wound pain at 6 months).
Mesh exposure
Evidence from five trials was insufficient to reveal whether there was a difference in vaginal exposure (RR 0.28, 95% CI 0.05 to 1.65; n = 348; Analysis 9.26) (Al‐Azzawi 2014; Guerrero 2008; Tcherniakovsky 2009; Wadie 2005; Zargham 2013). Only four cases of mesh exposure (from 177 women) were reported in the mid‐urethral sling group compared with none among 171 women in the traditional sling arms. The five trials all used a biological graft as traditional sling material.
9.26. Analysis.
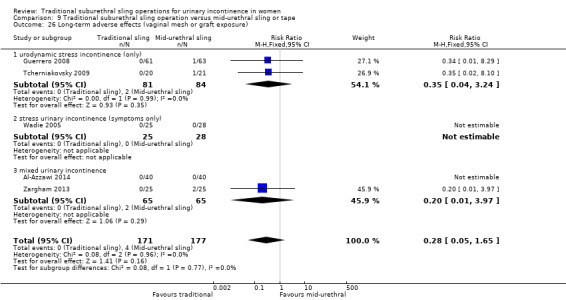
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 26 Long‐term adverse effects (vaginal mesh or graft exposure).
Release of sling
Very low‐quality evidence from three trials suggests no difference between traditional slings and mid‐urethral slings in the numbers of women requiring release of sling (11/164; 6.7% vs 4/162; 2.5%: RR 2.53, 95% CI 0.87 to 7.35; n = 326; Analysis 9.24;Table 9) (Arunkalaivanan 2003; Guerrero 2008; Kondo 2006).
9.24. Analysis.
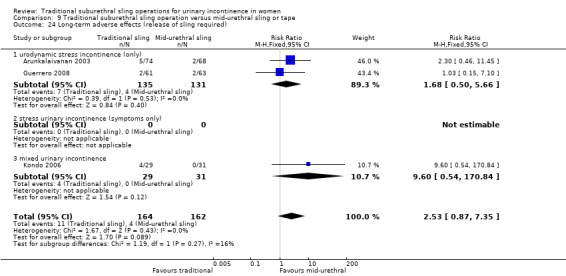
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 24 Long‐term adverse effects (release of sling required).
Other adverse effects
One trial further reported urethral injury alone, which suggests no evidence of a difference between groups (RR 0.36, 95% CI 0.02 to 8.39) (Kondo 2006).
Finally, one small trial reported vaginal bleeding and UTI (Analysis 9.19;Analysis 9.20) (Zargham 2013). Results show no significant difference in the risk of vaginal bleeding (RR 1.67, 95% CI 0.45 to 6.24).
9.19. Analysis.
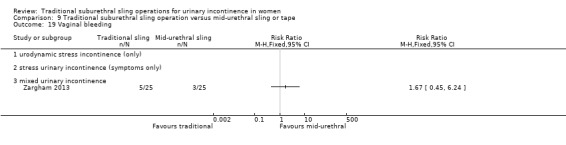
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 19 Vaginal bleeding.
Quality of life
Quality of life (QoL) was assessed in nine trials (Amaro 2007; Arunkalaivanan 2003; Basok 2008; Guerrero 2008; Kondo 2006; Okulu 2013; Sharifiaghdas 2008; Silva Filho 2006; Wadie 2005). Data were reported in different ways; thus meta‐analysis was not possible and individual results are reported below. In this section, results are reported qualitatively according to how trialists reported their findings. Therefore, use of 'statistically significant' is as reported in the trials ‐ not as interpreted by the review authors ‐ and we have not changed this.
Amaro 2007 used the Portuguese version of King's Health Questionnaire (KHQ), reporting no statistically significant differences between groups in general health condition; impact of incontinence; role, physical, and social limitations; personal relationships; emotions; sleep; and severity perception of urinary incontinence at 36 months.
A 10‐point questionnaire‐based assessment was used by Arunkalaivanan 2003. The mean score was 8.03 for mid‐urethral synthetic suburethral slings and 8.05 for traditional slings, with a median score of 9 for both groups.
A subjective 10‐point patient satisfaction questionnaire was used by Basok 2008, which provided no evidence of a difference between groups, with satisfaction rates of 82% and 87.5% with the traditional sling and the mid‐urethral sling, respectively.
Trialists found no significant difference in any domain of the Bristol Female Lower Urinary Tract Symptom (BFLUTS) score, as assessed in Guerrero 2008.
Statistically significant improvement was noted postoperatively on the IIQ Short Form (IIQ‐7) and the UDI Short Form (UDI‐6) within both groups, but no significant difference in the degree of improvement was evident between groups (Kondo 2006).
One study assessed quality of life using the ICIQ‐Short form score. While there was improvement from baseline in all groups, there were no significant differences between randomised groups (Okulu 2013).
IIQ score was also used by Sharifiaghdas 2008 to determine subjective cure. Means were reported as 44.3 (range 35.2 to 61.5) for the mid‐urethral procedure and 48.5 (range 38.5 to 69.7) for the sling operation (P = 0.46). A score less than 50 represents good quality of life, between 50 and 70 moderate quality of life, and greater than 70 poor quality of life. There was no significant difference in QoL between groups; 15 (72%) in the mid‐urethral group and 20 (55%) in the sling group were satisfied with the operation (P = 0.3, as reported by trialists).
The KHQ was used in Silva Filho 2006 to show significantly greater improvement in those who underwent the traditional suburethral sling operation in the following domains: general health perception; physical, social, and role limitations; emotions and severity measures. There were no significant differences in incontinence impact, personal relationships, sleep, and energy domains.
In one small trial (Wadie 2005), researchers reported UDI‐6 and IIQ‐7 scores, which show no statistically significant differences between trial arms (Analysis 9.27;Analysis 9.28
9.27. Analysis.
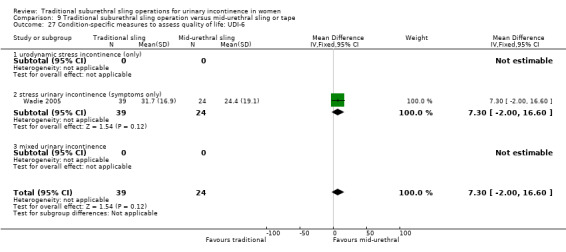
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 27 Condition‐specific measures to assess quality of life: UDI‐6.
9.28. Analysis.
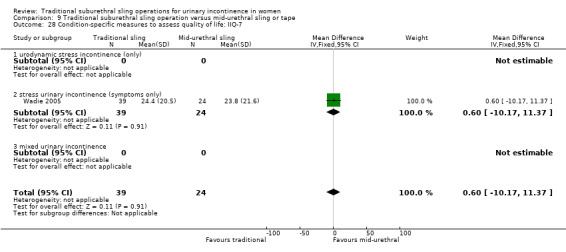
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 28 Condition‐specific measures to assess quality of life: IIQ‐7.
Comparison 10. Traditional suburethral sling operation versus single‐incision sling (mini‐sling)
One small trial compared a rectus fascia pubovaginal traditional sling with a single‐incision sling (mini‐sling; Ophira) and included women with urodynamically diagnosed stress urinary incontinence (USI) (Sharifiaghdas 2015).
Due to the small size of the trial, the data were too few to be reliable (Table 13).
Comparison 11. One type of traditional sling operation versus another type of traditional sling operation
Nine trials addressed this comparison (Barbalias 1997; Choe 2000; Guerrero 2008; Lucas 2000; Okulu 2013; Pacetta 2005; Shin 2001; Teleb 2011; Viseshsindh 2003). Three of these were newly added in this update (Choe 2000; Okulu 2013; Teleb 2011). One was updated (Guerrero 2008).
The traditional slings in this comparison used the following materials to suspend the urethra.
Autologous biological materials: rectus fascial sling (Barbalias 1997; Guerrero 2008; Lucas 2000; Teleb 2011); dermal graft patch (Shin 2001); tissue removed from the vaginal wall (Choe 2000; Teleb 2011; Viseshsindh 2003).
Other biological materials: cadaveric fascia lata (Shin 2001); Fortaperm porcine collagen matrix (Pacetta 2005); Pelvicol (Guerrero 2008).
Synthetic materials: Goretex (Barbalias 1997); antimicrobial MycroMesh (Choe 2000); Vypro, Ultrapro, and Prolene (Okulu 2013); Prolene (Teleb 2011).
Some trials compared three different materials: these have been presented as pair‐wise comparisons. One trial compared the same material (autologous rectus fascia) but with different lengths of the material used (Lucas 2000). It is not possible to pool data from any of these trials because different materials were compared, and each individual trial was too small for findings to be conclusive.
Primary outcomes
Number of continent (dry) women
Short term
Five trials reported the number of continent women within the first year after surgery (Guerrero 2008; Lucas 2000; Okulu 2013; Pacetta 2005; Viseshsindh 2003). A total of 437 women studied within the first 12 months after surgery showed similar incontinence rates between traditional sling operations using biological or synthetic materials. However, the confidence intervals were wide (Analysis 11.1).
11.1. Analysis.
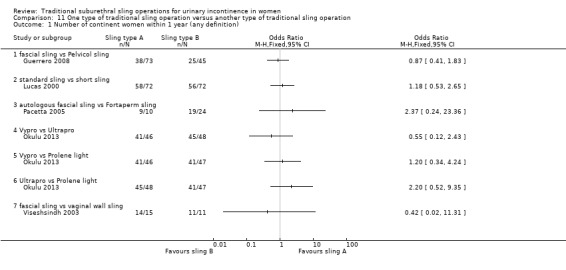
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 1 Number of continent women within 1 year (any definition).
Medium term
Seven trials reported the number of continent women from one to five years after surgery (Barbalias 1997; Choe 2000; Guerrero 2008; Lucas 2000; Okulu 2013; Shin 2001; Teleb 2011). Again, it is not possible to pool any of these trials because different materials were compared. With one exception, none of the comparisons suggest any evidence of a difference between different materials. One small trial suggests that women were more likely to be continent with autologous fascial sling operations than with Pelvicol graft (OR 3.29, 95% 1.41 to 7.69; n = 113; Analysis 11.2.1; Table 11) (Guerrero 2008). This effect was evident early and led to premature closure of the Pelvicol arm.
11.2. Analysis.
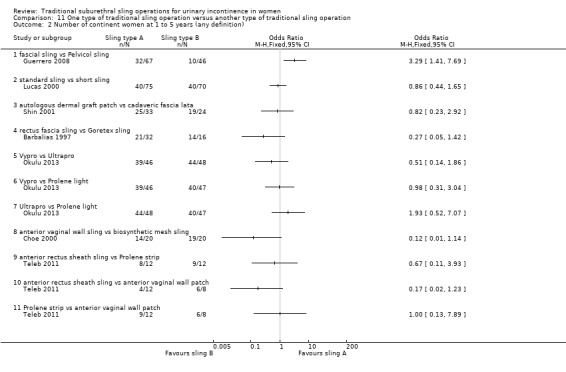
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 2 Number of continent women at 1 to 5 years (any definition).
Long term
One trial measured continence rates at six years after surgery and found no evidence of a difference between a standard (long) sling and a short sling (31/73 and 35/69 continent women, respectively) (OR 0.72, 95% CI 0.37 to 1.39, n = 142; Analysis 11.3) (Lucas 2000).
11.3. Analysis.
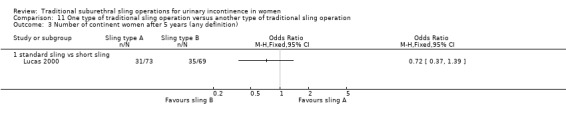
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 3 Number of continent women after 5 years (any definition).
Number of women who had repeat continence surgery
One trial reported the number of women requiring repeat continence surgery at 1 year and at 10 years (Guerrero 2008). Only women who received the biological material Pelvicol required any repeat surgery (9/46; 20%; RR 0.04, 95% CI 0.00 to 0.61; Analysis 11.4; Table 11) compared to 0 of 67 women in the rectus fascia group requiring repeat surgery 10 years later. This was statistically significant in favour of the traditional sling with rectus fascia; as a result, Pelvicol is no longer used in traditional sling surgery.
11.4. Analysis.
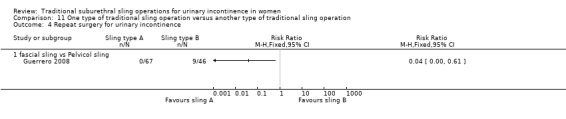
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 4 Repeat surgery for urinary incontinence.
Secondary outcomes
Women's observations
Number of women cured at one year or later (women's observations)
Three trials reported women's perception of cure of incontinence (Guerrero 2008; Lucas 2000; Shin 2001). Only one reported any evidence of a difference between groups; fascial slings were significantly better than Pelvicol slings (OR 3.29, 95% CI 1.41 to 7.69; Analysis 11.5.1) (Guerrero 2008).
11.5. Analysis.
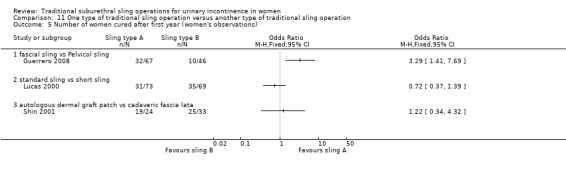
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 5 Number of women cured after first year (women's observations).
Number of women improved
Short term
Three trials reported women’s perception of improvement within one year (Barbalias 1997; Guerrero 2008; Pacetta 2005). Only one reported a difference between groups; women having fascial slings were more likely to perceive themselves as improved compared to women having Pelvicol slings (69/73 vs 33/34; OR 6.27, 95% CI 1.88 to 20.94; Analysis 11.6.1) (Guerrero 2008).
11.6. Analysis.
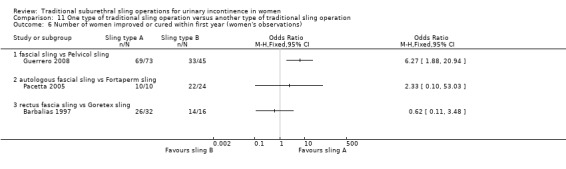
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 6 Number of women improved or cured within first year (women's observations).
Medium term
Four trials reported women’s perception of improvement after one year (Barbalias 1997; Guerrero 2008; Shin 2001; Teleb 2011). Only one reported a difference between groups; women having fascial slings were more likely to perceive themselves as improved compared to women having Pelvicol slings (60/67 vs 28/46; RR 1.47, 95% CI 1.15 to 1.88; Analysis 11.7.1) (Guerrero 2008).
11.7. Analysis.
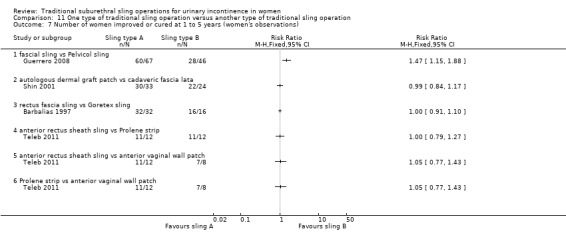
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 7 Number of women improved or cured at 1 to 5 years (women's observations).
Long term
This was not reported.
Number of women satisfied
Three trials reported satisfaction, but results could not be combined and individually, numbers were too small to be conclusive (Analysis 11.8) (Choe 2000; Guerrero 2008; Okulu 2013). Study authors provided no evidence of a difference between groups in any comparison.
11.8. Analysis.
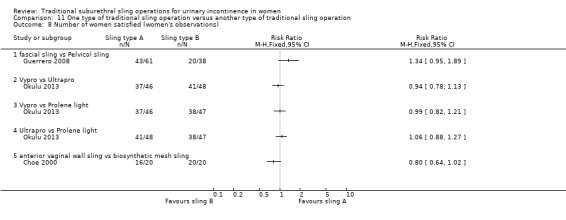
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 8 Number of women satisfied (women's observations).
Quantification of symptoms
Two trials reported data on mean weight of urine on a pad test (Analysis 11.9) (Lucas 2000; Okulu 2013).
11.9. Analysis.
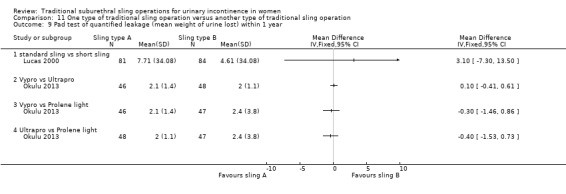
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 9 Pad test of quantified leakage (mean weight of urine lost) within 1 year.
In the short term, trials provided no reliable evidence of a difference between groups (Analysis 11.9), but after one year, one trial showed that Ultrapro was better than both Vypro and Prolene light for this outcome (Analysis 11.10) (Okulu 2013).
11.10. Analysis.
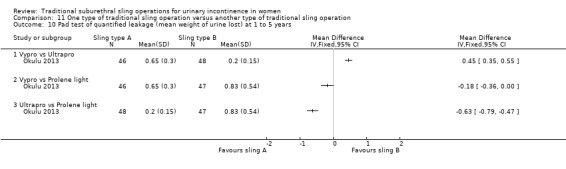
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 10 Pad test of quantified leakage (mean weight of urine lost) at 1 to 5 years.
Clinician's observations
This was not reported.
Surgical outcome measures
Duration of operation
The duration of operation for the traditional long length sling procedure was significantly longer in one trial, which compared long and short lengths of autologous fascia (MD 8 minutes, 95% CI 3 to 13; Analysis 11.7) (Lucas 2000). In another trial comparing three materials, duration of operation was shortest for Prolene (36 minutes), intermediate for anterior vaginal wall patch (42 minutes), and longest when rectus sheath was used as a sling (52 minutes) (Analysis 11.11) (Teleb 2011). However, it is unclear whether these differences in operating time would be enough to be clinically important.
11.11. Analysis.
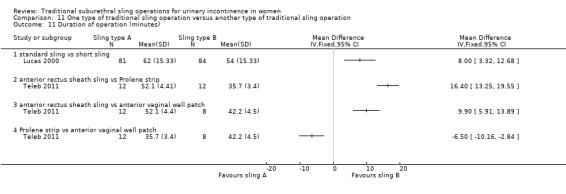
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 11 Duration of operation (minutes).
Length of hospital stay
Length of hospital stay was reported in one trial (Teleb 2011). Hospital stay was longest for women having the anterior rectus sheath sling compared to women with the other two materials (Analysis 11.13).
11.13. Analysis.
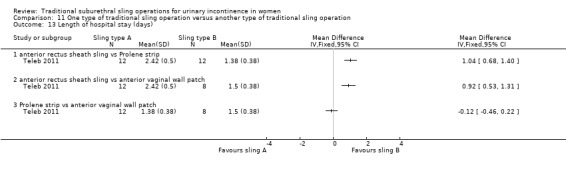
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 13 Length of hospital stay (days).
Time to return to normal activity level
This was not reported.
Blood loss
Blood loss was significantly less with Prolene compared to the other two materials (Analysis 11.12) (Teleb 2011).
11.12. Analysis.
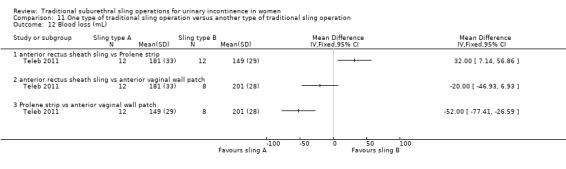
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 12 Blood loss (mL).
Anterior rectus sheath sling versus prolene strip: MD 32.00 mL, 95% CI 7.14 to 56.86; n = 24.
Anterior rectus sheath sling versus anterior vaginal wall patch: ‐20.00 mL, 95% CI ‐46.93 to 6.93; n = 20.
Prolene strip versus anterior vaginal wall patch: MD ‐52.00 mL, 95% CI ‐77.41 to ‐26.59; n = 20.
However, total differences in volumes of blood lost were small, and their clinical importance is uncertain.
Further treatment
This was not reported.
Adverse events
Perioperative surgical complications
The three trials that reported any perioperative complications could not be combined because different materials were compared (Barbalias 1997; Lucas 2000; Viseshsindh 2003). More complications were reported with the use of synthetic non‐absorbable Goretex in one trial (RR 0.05, 95% CI 0.00 to 0.80; Analysis 11.14.2) (Barbalias 1997). In the other trial, evidence was insufficient to show whether there was a difference between two biological slings (RR 1.14, 95% CI 0.78 to 1.66; Analysis 11.14.1; Table 11) (Lucas 2000). There were no perioperative complications in the third trial between the two groups (Viseshsindh 2003).
11.14. Analysis.
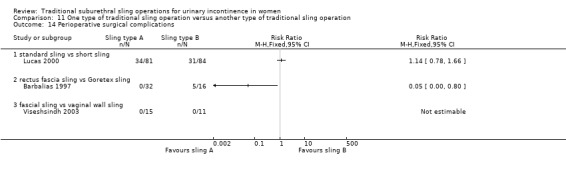
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 14 Perioperative surgical complications.
Bladder perforation
Three trials reported the number of bladder perforations (Guerrero 2008; Lucas 2000; Teleb 2011), showing no evidence of a difference between groups in any comparison (Analysis 11.15).
11.15. Analysis.
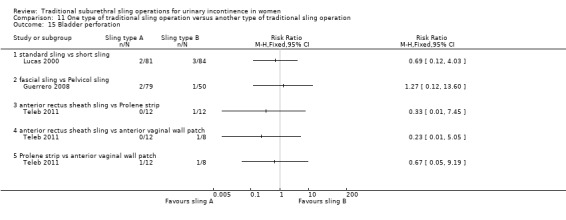
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 15 Bladder perforation.
Urinary tract infection
Two trials reported the number of women with urinary tract infection (Choe 2000; Lucas 2000), providing no evidence of a difference between groups in any comparison (Analysis 11.16).
11.16. Analysis.
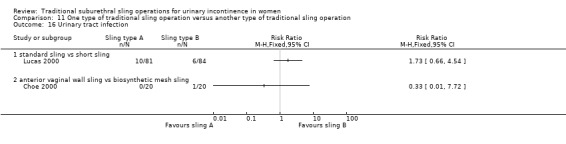
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 16 Urinary tract infection.
Urinary urgency symptoms; urgency urinary incontinence
Three trials reported the number of women with urgency symptoms (Barbalias 1997; Lucas 2000; Okulu 2013), revealing no evidence of a difference between groups in any comparison (Analysis 11.20).
11.20. Analysis.
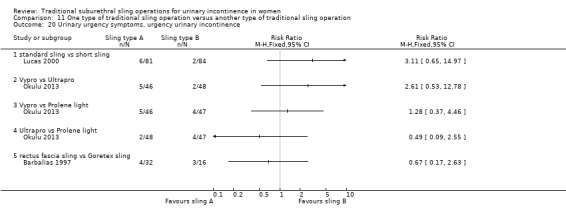
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 20 Urinary urgency symptoms, urgency urinary incontinence.
Detrusor overactivity (urodynamic overactivity)
One trial reported 4 of 33 women in the autologous dermal graft patch group with de novo detrusor overactivity compared with 5 of 20 in the cadaveric fascia lata group (RR 0.48, 95% CI 0.15 to 1.60; n = 53; Analysis 11.21) (Shin 2001).
11.21. Analysis.
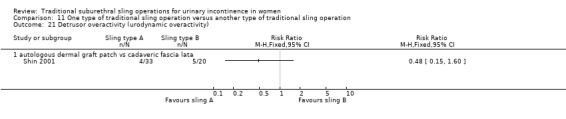
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 21 Detrusor overactivity (urodynamic overactivity).
Voiding dysfunction (with or without urodynamic confirmation)
Six trials reported the number of women with voiding dysfunction (Choe 2000; Guerrero 2008; Lucas 2000; Okulu 2013; Teleb 2011; Viseshsindh 2003), showing no evidence of a difference between groups in any comparison (Analysis 11.19).
11.19. Analysis.
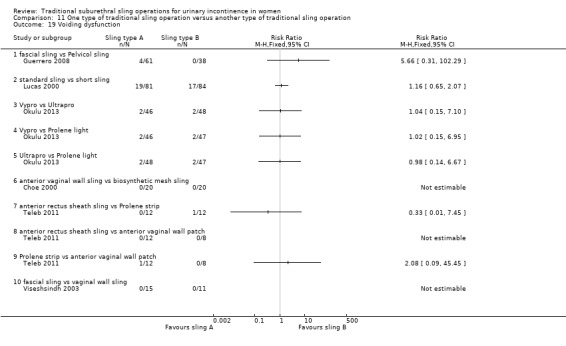
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 19 Voiding dysfunction.
Long‐term adverse effects
One trial reported the number of women with wound pain: 2 of 61 and 0 of 38 in the fascial sling and Pelvicol groups, respectively (RR 3.15, 95% CI 0.16 to 63.80; n = 99; Guerrero 2008). The same trial also reported 2 of 61 and 1 of 38 women requiring release of sling (RR 1.25, 95% CI 0.12 to 13.28; n = 99).
Two women in one trial reported long‐term scar pain after a rectus fascial sling compared to none in the Pelvicol group; there were no graft exposures in either group (Guerrero 2008). In another trial, when participants all received a different type of synthetic mesh, five instances of mesh exposure were reported among 141 women in the three mesh groups (Okulu 2013). One trial of a synthetic versus a biological material reported no mesh exposures (Analysis 11.23; Table 11) (Choe 2000).
11.23. Analysis.
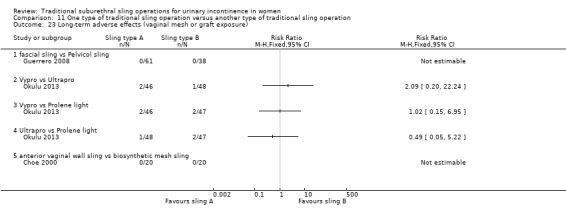
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 23 Long‐term adverse effects (vaginal mesh or graft exposure).
Other adverse effects
One trial reported 1 of 20 women with vaginal bleeding after anterior wall vaginal sling compared with 0 of 20 in the biosynthetic mesh group (RR 3.00, 95% CI 0.13 to 69.52; n = 40) (Choe 2000).
Quality of life
Data were reported in different ways; thus meta‐analysis was not possible (Table 11).
Lucas 2000 showed significant improvement in average scores for the UDI‐6 (reported P = 0.007) and the IIQ‐7 (P = 0.002) when compared with baseline. Scores between groups were similar.
Pacetta 2005 evaluated women using the Incontinence Quality of Life questionnaire (I‐QOL), reporting improvement from 45 at baseline to 97 at one year in the autologous fascia group, and from 39 to 92 in the Fortaperm group.
Okulu 2013 used the International Consultation on Incontinence Questionnaire (ICIQ) Short Form urinary incontinence scale to compare three synthetic meshes. Ultrapro was better than Prolene light, which was better than Vypro, in the short term and in the medium term (Analysis 11.24; Analysis 11.25).
11.24. Analysis.
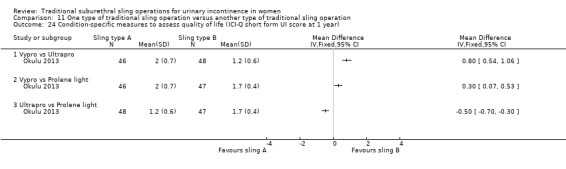
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 24 Condition‐specific measures to assess quality of life (ICI‐Q short form UI score at 1 year).
11.25. Analysis.
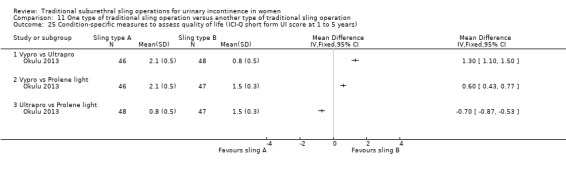
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 25 Condition‐specific measures to assess quality of life (ICI‐Q short form UI score at 1 to 5 years).
Discussion
The main systematic review of effects is discussed below but we sought to supplement this review by identifying economic evaluations that compared traditional suburethral sling operations with any of the other main categories of surgical methods listed in the background section. Identifed economic evaluations have been summarised in a brief economic commentary. A supplementary search in Ovid NHS EED, MEDLINE, and Embase identified two such economic evaluations. Details of the search strategies are given in Appendix 3.
Summary of main results
We included 34 trials involving 3244 women. Traditional slings were compared with 10 other treatments and with each other; but we did not identify any trial comparing suburethral slings with no treatment or sham treatment, conservative management, anterior repair, or laparoscopic retropubic colposuspension. One trial compared traditional slings with bladder neck needle suspension (Table 6), and another trial compared traditional slings with single‐incision slings (Table 10). Both trials were too small to be informative.
Traditional suburethral sling operation versus drugs
One small trial comparing traditional slings with oxybutynin for women with mixed urinary incontinence did not report any of the outcomes used in the 'Summary of findings' tables. However, it is uncertain whether surgery compared with oxybutynin leads to more women being dry (83% vs 0%; odds ratio (OR) 195.89, 95% confidence interval (CI) 9.91 to 3871.03) or having less urgency urinary incontinence (13% vs 43%; risk ratio (RR) 0.29, 95% CI 0.09 to 0.94) (Table 3).
Traditional suburethral sling operation versus injectables
Based on very low‐quality evidence from one small trial, we are uncertain about the impact of surgery versus injectables in terms of the numbers of continent women (100% were dry with a traditional sling vs 71% with the injectable after the first year; OR 11.57, 95% CI 0.56 to 239.74) or the need for repeat surgery for urinary incontinence (RR 0.52, 95% CI 0.05 to 5.36) or the occurrence of perioperative complications (RR 1.57, 95% CI 0.29 to 8.49) (Table 4).
Traditional suburethral sling operation versus open abdominal retropubic colposuspension
Eight trials compared slings with open abdominal retropubic colposuspension. Moderate‐quality evidence shows that traditional suburethral sling probably leads to more continent women in the medium term (one to five years) (69% vs 59% after colposuspension: OR 1.70, 95% CI 1.22 to 2.37). High‐quality evidence indicates that women were less likely to need repeat continence surgery after a traditional sling than after colposuspension (RR 0.15, 95% CI 0.05 to 0.42). We found no evidence of a difference in perioperative complications between the two groups, but the CI was very wide and the quality of evidence was very low (RR 1.24, 95% CI 0.83 to 1.86; Table 7).
Traditional suburethral sling operation versus mid‐urethral sling operation
Fourteen trials addressed the comparison between traditional sling operations and mid‐urethral sling operations. Depending on judgements about what constitutes a clinically important difference between interventions with regard to continence, traditional suburethral slings are probably no better, and may be less effective, than mid‐urethral slings in terms of number of women continent in the medium term (one to five years) (67% vs 74%; OR 0.67, 95% CI 0.44 to 1.02; n = 458; moderate‐quality evidence). One trial reported more continent women with the traditional sling after 10 years (51% vs 32%; OR 2.22, 95% CI 1.07 to 4.61), but this finding needs to be replicated in other trials. Mid‐urethral slings may be associated with fewer perioperative complications (RR 1.74, 95% CI 1.16 to 2.60; low‐quality evidence; Table 9).
One type of traditional sling operation versus another type of traditional sling operation
Nine trials compared one type of traditional sling with another. A number of different materials were used such as porcine dermis, lyophilised dura mater, fascia lata, vaginal wall, autologous dermis, and rectus fascia. Study results could not be pooled due to clinical heterogeneity, as different materials or types of traditional slings were used. Complications were reported by two trials ‐ one comparing non‐absorbable Goretex with a rectus fascia sling, and the second comparing Pelvicol with a rectus fascial sling. The impact was uncertain due to the very low quality of evidence (Table 11).
Overall completeness and applicability of evidence
Historically, traditional suburethral sling procedures were used for women who had recurrent stress incontinence (after a previous failed continence operation). However, the current review includes both women with new and recurrent incontinence, without reporting the results separately. These operations are designed to restore normal urethrovesical junction support by mechanically compressing or kinking the proximal urethra.
Evidence related to the primary outcome ‐ urinary continence ‐ was available in one form or another for most trials to determine the effectiveness of traditional suburethral sling operations for treatment of urinary incontinence. However, study findings were consistent regardless of which method of ascertainment of continence was used (urine leakage using any definition, women's report, clinician's observation, combinations of these, or quantification methods such as pad test weights). More long‐term data are now available, suggesting that traditional slings may be equally as effective or more effective than other currently available surgical treatments (such as colposuspension and mid‐urethral slings). However, most trials did not provide sufficient information to adequately judge risk of bias; therefore most trials had to be judged to be at "unclear risk of bias" due to inadequate reporting.
None of the included trials contained all relevant patient‐reported outcomes. More data on pain after different procedures (both postoperative and long‐term) and time to return to 'normal' daily living following surgery would have been useful. In particular, reporting on medium‐ and long‐term adverse effects and the need for repeat continence surgery in the long term is not available but this information would be essential for informed decision‐making.
This Cochrane Review is limited to randomised controlled trials (RCTs) only. As adverse events were relatively rare and/or may not have been reported, it is not possible to infer accurate information about their frequency or type.
The importance of having a range of surgical options is that a woman can choose the procedure that she is most comfortable with, for example, trading off efficacy for the chance of having fewer adverse effects or a more minimally invasive procedure. Traditional slings appear to be as, if not more, effective than both colposuspension and mid‐urethral slings but without the risks perceived to be associated with synthetic mesh.
This Cochrane Review may not be applicable to clinicians everywhere. High‐income nations have been increasingly using mid‐urethral procedures with synthetic materials as first‐line treatment for stress urinary incontinence for about 20 years but because the safety of these operations has been called into question, this practice may decrease in the future. Use of traditional suburethral operations, which appear to be just as effective, might be reserved for countries where new technology is not available or is too expensive. For women who wish to avoid the possible complications of synthetic materials, biological materials such as rectus fascia (but not porcine dermis) seem as effective as synthetic mid‐urethral slings.
When possible, data were analysed in subgroups according to clinical characteristics of the type of incontinence (urodynamic stress incontinence, stress incontinence symptoms, or mixed urinary incontinence). Study findings were similar regardless of how incontinence was originally diagnosed. Because information was not available on this basis, it was not possible to determine if any type of surgery was more effective for women who had undergone previous failed continence surgery. Further analysis according to clinical characteristics of women, such as primary versus recurrent stress urinary incontinence and presence or absence of prolapse, was not possible due to lack of information. It might also be useful to look at possible differences according to intrinsic urethral sphincter deficiency versus urethral hypermobility (although there is no current clinical support for the use of these terms; Abrams 2006), obesity, ethnicity, vaginal delivery versus C‐section, or experience of the surgeon. These might make the findings of this review more generalisable. However, most trials have not reported these characteristics.
Quality of life, emotional well‐being, and social implications were poorly reported, or they were assessed by a variety of instruments, thus precluding meta‐analysis. These outcomes are of great importance to women and to decision‐makers.
Two searches have been conducted since the last fully incorporated search (9 October 2017 and 23 January 2019). Four studies are awaiting classification: Abou Hashem 2017; Hassan 2018; Kajbafzadeh 2017; Sharifiaghdas 2017. Of these, two are ongoing trials (Hassan 2018; Kajbafzadeh 2017), one is a second but identical publication of an included trial with no useable data (Abou Hashem 2017; Abouhashem 2014, respectively), and one is a 10‐year update of an already included trial (Sharifiaghdas 2017; Sharifiaghdas 2008, respectively).
Quality of the evidence
Quality of evidence plays a crucial role in our confidence in the estimate of effect. Most GRADE‐specific outcomes were judged to be of "low" or "very low" quality. This indicates that when more evidence becomes available, the estimate of effect is likely to be changed, or that any estimate of effect is very uncertain. In this systematic review, we assessed the methodological flaws of the included trials using trial reports. Therefore, our judgement of risk of bias and quality of evidence was influenced by reporting.
Although trial authors stated that their trials were randomised, most reports did not give sufficient detail about the method of sequence generation or concealment of allocation. Ten trials used an adequate randomisation method. Blinding of surgeons or women was generally not possible, but only two trials reported that outcomes were assessed by a nurse who was blinded to allocation. The total number of women enrolled was 3244, but some trials recruited only 10 women per arm. In addition, several types of slings were compared with different interventions, meaning that different materials had to be grouped together for comparison. Thus the numbers in each comparison were small, and the confidence intervals were wide; therefore several outcomes were downgraded due to imprecision.
Study populations varied, including women with and without previous surgery, and one study included only women who were deemed not suitable for another procedure (Hilton 1989). Although most study participants had urodynamic stress incontinence, some trials included women with mixed urinary incontinence. Baseline comparability of groups was not reported in all trials. Several trials assessed different types of sling in comparison with autologous rectus fascia, suggesting that the latter was considered as the 'standard' comparator.
Although eight trials used open abdominal retropubic colposuspension as the comparator, each used a different type of sling, and three followed up on women for only six months. Fourteen trials used a mid‐urethral sling as the comparator as this has arguably become the gold standard procedure for continence surgery in many countries.
In general, most trials reported different outcome measures, often poorly. The principal measure of effectiveness used in most studies was the proportion of women with incontinence following surgery. Few researchers have considered other outcomes, such as activities of daily living and quality of life. Few have addressed general health status, repeat incontinence surgery, later prolapse surgery, or time to return to normal activity level. Satisfaction with and acceptability of the treatment were also seldom addressed but are important factors for choice of management.
Potential biases in the review process
All relevant databases were searched and no language restriction was imposed during the search process, which enabled as many potentially eligible trials as possible to be included. Some reports of trials may not be published; therefore the full extent of the data may not have been captured. To account for any potential bias in the review process, data extraction and risk of bias assessment were performed by at least two independent review authors.
Although most trials reported the outcomes that they mentioned in their methods sections, none reported all outcomes of interest for this review, including, in many cases, the primary outcomes of urinary incontinence and repeat continence surgery (Figure 4).
The review sought to use rigorous methods of synthesis throughout and has sought to identify statistical evidence of differences between interventions. For some comparisons, no statistical evidence of a difference was identified but examination of the confidence intervals produced indicate that clinically important differences may be unlikely. Such conclusions require judgements about the magnitude of the minimum (clinically) important difference. Such judgements might be contested.
Agreements and disagreements with other studies or reviews
No other comparable systematic reviews of RCTs have addressed the specific use of traditional slings for treating women with stress urinary incontinence.
Brief economic commentary
To supplement the main systematic review, we looked for economic evaluations that compared traditional suburethral slings with a variety of surgical interventions for treating women with stress urinary incontinence. Three studies, selected from a search carried out on 10 August 2018, provided a cost analysis (Berman 1997), a cost‐utility analysis (Kilonzo 2004), and another cost‐utility analysis (Kumar 2017).
The comparative cost analysis by Berman 1997 used data from a retrospective observational study carried out in the United States, which compared traditional suburethral retropubic sling procedures with transurethral collagen injections in women with stress urinary incontinence. This study included a total of 14 women across both arms, each of whom had had stress urinary incontinence and had undergone an average of 1.1 procedures between December 1993 and October 1995. The retrospective analysis found that the traditional sling had an average operating room time of 186 minutes and required an average hospital stay of 2.9 days. The total cost per patient was on average $16,229 (in 2019 International Dollars; $10,381 in 1995 USD). The collagen treatment was on average less costly (P < 0.001) with an average cost in 2019 International Dollars of $7810 (or $4996 in 1995 USD). Average procedure time for the collagen injections was 57 minutes, and no time was spent as a hospital inpatient. A high percentage of costs for the traditional sling study arm involved those for the physician (33%) and operating room (36%), and costs for the collagen arm included collagen (40%) and physician fees (22%). Postoperative care for the traditional sling cost $1927 2019 International Dollars ($1,233 1995 USD), which was almost twice the cost of the collagen injection ‐ $980 in 2019 International Dollars ($627 in 1995 USD).
Before the procedure, there was no evidence of a difference in the occurrence of incontinence between groups. However, the average number of pads decreased after the procedure from 4.7 to 1.4 and from 5.2 to 2.3 for traditional sling and collagen injection, respectively (P = 0.049).
Women were followed up for 15 months post surgery, and 71.4% of those in the traditional sling arm were symptom‐free compared with 26.7% in the collagen injection arm (P = 0.05), with 85% from the traditional sling arm having minimal or no incontinence (using one pad or no pads daily).
Despite lower costs associated with the collagen injection, the traditional sling arm showed better overall improvement and had lower reoperation rates. The study author concluded that the traditional sling might be more cost‐effective when compared with collagen injection.
A cost‐utility analysis using a Markov model compared the mid‐urethral sling with open abdominal retropubic colposuspension, laparoscopic colposuspension, the traditional suburethral retropubic sling, and injectables (Kilonzo 2004). This study provides a summary of work presented in the technology assessment review conducted for the UK’s National Institute for Clinical Excellence (NICE) (Cody 2003). Study authors utilised clinical data from a systematic review of RCTs conducted up to mid‐2003 (Lapitan 2003; Moehrer 2002; Ward 2002b), and these results were based on economic modelling for a time horizon of up to 10 years; all costs were originally reported in UK pounds for 2001 and were adjusted to international dollars for 2019.
This study assumed, based upon the findings of Cody 2003, that the traditional sling and open abdominal retropubic colposuspension had equivalent effectiveness. This contrasts with evidence from the current review showing that traditional slings are more effective (Table 7).
The cost for traditional slings was $2756 per woman (2019 International Dollars; £1340 2001 GBP), with operation time of 46 minutes and average hospital stay of 7.2 days. Mid‐urethral slings cost $2176 (2019 International Dollars; £1058 2001 GBP) per woman, with an average hospital stay of 2.9 days and operation time of 30 minutes, but these costs were excluded. Open colposuspension cost $2676 per woman (2019 International Dollars; £1301 2001 GBP), with an operation time of 52 minutes and average hospital stay of 7.1 days, and laparoscopic colposuspension cost $2709 (2019 International Dollars; £1317 2001 GBP), with an operation time of 60 minutes and an average hospital stay of 4.6 days. A formal comparison of the cost‐effectiveness of traditional slings versus any of the other interventions was not performed. However, Kilonzo 2004 estimated that there was an 86% probability that mid‐urethral slings were cost‐effective compared to open colposuspension, if society was willing to pay approximately $62,000 (2019 International Dollars; £30,000 2001 GBP) per quality‐adjusted life‐year (QALY) gained. Given the model assumptions (traditional slings being more costly and as effective as open colposuspension), by implication traditional slings would not in this evaluation be considered cost‐effective compared with mid‐urethral slings or open colposuspension.
A cost‐utility analysis (Markov model) by Kumar 2017 compared the effectiveness of the traditional sling with Burch colposuspension. This study utilised data from published RCTs that included women 60 years of age and older with stress urinary incontinence, which compared the two procedures (Albo 2007; Bai 2005; Culligan 2003; Sand 2000). Follow‐up from these studies varied from three months to 73 months. However, the model extrapolated follow‐up of women for a time horizon of 16 years. The cost perspective was not explicitly stated but appears to be that of the US patient and healthcare provider based on captured costs (procedure costs and costs of caring for the patient with treatment failure for a year). These costs were originally reported in USD for 2015 and were converted to 2019 International Dollars. Literature describing this cost‐utility analysis shows that the cure rate for Burch colposuspension at 3 months, 12 months, 36 months, and 73 months was 90%, 87%, 49%, and 84.6%, respectively, and that for the traditional sling was 100% at 3 months and 73 months, 87.8% at 12 months, and 66% at 36 months. Studies reported that the overall cost of the traditional sling per woman was $8186 (2019 International Dollars; $7619 2015 USD) less than the overall cost of Burch colposuspension. The cost‐utility analysis concluded that the traditional sling was more effective than Burch colposuspension based on the QALY gained. Women in the traditional sling arm (11.18 QALYs) had 0.99 QALYs more compared with those in the Burch colposuspension arm (10.19 QALYs), with an incremental cost per QALY of $8251 (2019 International Dollars; $7696 2015 USD). Kumar 2017 stated that it would be important to have published data from large‐scale trials before a definitive recommendation could be provided.
Eligible economic evaluations were not directly comparable due to differences in methods, time horizons, and settings. We have not sought to determine the potential reasons why results differ between studies, nor have we conducted any critical appraisal. Consequently, we do not attempt to draw any firm or general conclusions regarding the relative costs or efficiency of traditional suburethral retropubic slings for surgical management of stress urinary incontinence compared with current alternatives.
Authors' conclusions
Implications for practice.
Traditional sling procedures appeared to result in less urinary incontinence or need for repeat surgery for incontinence or prolapse and greater satisfaction in comparison to open retropubic colposuspension in the medium and long term. However, the long‐term adverse event profile is still unclear. Traditional slings may be slightly less effective than mid‐urethral slings in the medium term but may be more effective in the long term (based on only one trial). However, they had higher rates of adverse effects. This should be interpreted with some caution, as the quality of evidence in included studies was variable, follow‐up was most often short, and randomised trials have inherent limitations in identifying complication rates.
The data were too scarce to address whether the types of suburethral slings tested were as effective as other sling materials, injectables, drugs, needle suspension, or single‐incision slings. Limited evidence from one small trial suggests that slings made of non‐absorbable synthetic Goretex led to more complications than slings made of biological rectus fascia. However, slings made of porcine dermis (Pelvicol) were less effective than rectus fascia or a mid‐urethral sling in another trial.
The broader effects of suburethral slings could not be established because most trials did not include appropriate outcome measures, such as general health status and time to return to normal activity level, and follow‐up was short in the majority of trials.
Evidence to clarify whether traditional suburethral slings may be better or worse than surgical or conservative management options, other than those reported in this review, is lacking.
Implications for research.
The methods used by trials and their appropriate reporting must be addressed in future research. Some evidence was limited by the poor quality and small numbers of included randomised trials. The CONSORT guidelines should be used to ensure adequate reporting. In the absence of RCTs that compare each method of continence surgery with other types, a network meta‐analysis of all available RCTs would enable interventions to be compared indirectly with each other.
There is a need for additional trials of adequate power and better quality and reporting standards to assess the effectiveness of suburethral slings in comparison with other surgical techniques and different types of slings, and in specific situations, such as among women who have already had previous continence surgery, or those with concomitant prolapse. Long‐term follow‐up is paramount.
Future research on incontinence treatments should incorporate standardised, validated, and simple outcome measures ‐ both woman‐reported and clinician‐observed. Outcomes should be relevant to women who have incontinence and are seeking treatment, taking their preferences into account, and policy makers should commission treatment to allow comparison between treatments. In particular, quality of life and psychological and economic outcomes should be incorporated. Surgical trials related to urinary incontinence should systematically address surgical morbidity outcomes, such as adverse perioperative and postoperative events, length of hospital stay, time to return to normal activities, development of urgency symptoms or detrusor overactivity, and especially the need for repeat surgery or alternative interventions.
To assess the efficacy and safety of these operations in the longer term, it is essential that trialists carry out and report their long‐term follow‐up data for proper evaluation of treatment for incontinence.
What's new
| Date | Event | Description |
|---|---|---|
| 21 January 2020 | New citation required but conclusions have not changed | Updated. Conclusions not changed. |
| 21 January 2020 | New search has been performed | For this update, published in 2020, the following changes were made. 1. The search was updated to February 2017 and 8 trials were newly included (Abouhashem 2014; Al‐Azzawi 2014; Choe 2000; Helmy 2012; Okulu 2013; Sharifiaghdas 2015; Teleb 2011; Zargham 2013). A further search was conducted on 23 January 2019; as a result, several additional reports of studies are awaiting classification. 2. Additional reports for the following trials were identified: Albo 2007; Amaro 2007; Guerrero 2008; Wadie 2005, and extra data were added where appropriate. 3. The methods were substantially updated in line with current Cochrane standards. This includes assessment of risk of bias in included trials and assessment of the quality of the body of evidence via the GRADE approach. 4. The primary outcome was changed from 'Number of women with urinary incontinence' to 'Number of continent (dry) women', and a further outcome, 'Number of women cured', was added. |
History
Protocol first published: Issue 3, 1999 Review first published: Issue 3, 2000
| Date | Event | Description |
|---|---|---|
| 8 December 2010 | New citation required but conclusions have not changed | A total of 13 new studies have been added. |
| 30 July 2010 | New search has been performed | This is the second update of the review of traditional slings. 13 new RCTs have been added (Albo 2007; Amaro 2007; Bai 2005; Basok 2008; Guerrero 2008; Maher 2005; Pacetta 2005; Sharifiaghdas 2008; Silva Filho 2006; Song 2004; Tcherniakovsky 2009; Teixeira 2008; Wadie 2005), and 3 have been updated (Arunkalaivanan 2003; Kondo 2006; Lucas 2000). |
| 13 October 2008 | Amended | Review was converted to new review format. |
| 25 May 2005 | New citation required and conclusions have changed | Substantive amendments were made. The review was divided into 2 separate reviews: 1 on traditional suburethral sling operations (current review, updated) and another on suburethral self‐fixing sling operations (to include the new TVT and SPARC procedures) to be prepared. The trials on TVT vs procedures other than traditional suburethral sling operations (4) were moved to the excluded trials list and will be included in the new review. Five new trials were included. |
| 13 February 2003 | New search has been performed | Minor updates were made; 5 studies were added. |
| 17 May 2001 | New citation required and conclusions have changed | This is the first update. |
Acknowledgements
We are grateful to Adrian Grant, Jonathan Cook, Aldemar Araujo Castro, and several anonymous peer‐referees for assistance and valuable comments on this and previous versions of the review. Sheila Wallace provided support for each version of the review as well as for this update and in the classification and identification of new studies. Fiona Stewart assisted with rewriting the effects of interventions section, conversion of incontinence to continence outcomes, and related changes in 'Summary of findings' tables.
The review was originally conceived and conducted by Carlos CB Bezerra and Homero Bruschini.
An earlier version of this review was completed as part of a project to add brief economic commentaries to Cochrane Incontinence's Reviews on surgery for urinary incontinence in women (Dean 2017). This project was supported by the National Institute for Health Research (NIHR) via the Cochrane Review Incentive Scheme 2016.
Appendices
Appendix 1. Search strategy for effectiveness studies ‐ Cochrane Incontinence Specialised Register
The terms used to search the Cochrane Incontinence Specialised Register are given below: (TOPIC.URINE.INCON*) AND ({DESIGN.CCT*} OR {DESIGN.RCT*}) AND ({INTVENT.SURG.SLIN*} OR {INTVENT.SURG.SUBURETHRAL SLING.} OR {INTVENT.SURG.ABDO.SLING.}) (All searches were of the keyword field of EndNote 2018).
The date of the last fully incorporated search was: 27 February 2017. The date of the last search, which was not fully incorporated into the review, was 23 January 2019.
Appendix 2. Details of extra literature searching performed for older versions of this review
For previous versions of this review (which covered all sling types) extra specific searches were performed by one of the review authors (Carlos Bezerra). These are detailed below.
Systematic searches of electronic bibliographic databases:
PubMed ‐ years searched: January 1966 to January 2000, date searched: 30 January 2000; and
UK National Research Register ‐ 2001, Issue 1, date searched: May 2001.
Search term used: TVT.
Handsearching of conference proceedings: Brazilian Congress of Urology Annual Meeting: 1991 to 2003 inclusive.
Appendix 3. Search strategies for brief economic commentary
We performed additional searches for the brief economic commentary (BEC) in the following databases:
MEDLINE on OvidSP (1 January 1946 to week 5 July 2018) searched on 10 August 2018;
Embase on OvidSP (1 January 1980 to week 32 2018) searched on 10 August 2018; and
NHS Economic Evaluation Database (NHS EED) on OvidSP (1st Quarter 2016) searched on 6 April 2017 (this database is no longer updated by the producer).
We used one search strategy in NHS EED (OvidSP) and two different search strategies on MEDLINE and Embase (OvidSP). Details of the searches run and the search terms used can be found below. The economic evaluation search filters used for MEDLINE and Embase are those developed by and available on the Centre for Reviews and Dissemination web pages.
MEDLINE on OvidSP (1 January 1946 to week 5 July 2018) and Embase on OvidSP (1 January 1980 to week 32 2018) searched on 10 August 2018
We used two different search strategies in MEDLINE and Embase (OvidSP) ‐ these are given below.
Search strategy 1:
1. Economics, Pharmaceutical/ or Economics, Medical/ or Economics/ or Economics, Hospital/ or economics.mp. or Economics, Nursing/ 2. exp "costs and cost analysis"/ 3. "Value of Life"/ 4. exp "fees and charges"/ 5. exp budgets/ 6. budget*.ti,ab. 7. cost*.ti. 8. (economic* or pharmaco?economic*).ti. 9. (price* or pricing*).ti,ab. 10. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab. 11. (financ* or fee or fees).ti,ab. 12. (value adj2 (money or monetary)).ti,ab. 13. ((energy or oxygen) adj cost).ti,ab. 14. (metabolic adj cost).ti,ab. 15. ((energy or oxygen) adj expenditure).ti,ab. 16. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 17. exp Urinary Incontinence/ 18. ((stress* or mix* or urg* or urin*) adj3 incontinen*).tw. 19. Urodynamics/ or Urinary Incontinence, Stress/ or Urinary Incontinence/ or Suburethral Slings/ or mixed incontinence.mp. or Urinary Bladder/ or Urinary Incontinence, Urge/ 20. 17 or 18 or 19 21. anterior vaginal repair*.tw. 22. 16 and 20 and 21 23. anterior colporrhaphy*.tw. 24. 21 or 23 25. 16 and 20 and 23 26. bladder neck needle suspension$.tw. 27. 16 and 20 28. 26 and 27 29. open abdominal retropubic colposuspension*.tw. 30. retropubic colposuspension*.tw. 31. burch colposuspension*.tw. 32. 29 or 30 or 31 33. 27 and 32 34. laparoscopic retropubic colposuspension*.tw. 35. laparoscopic colposuspension*.tw. 36. 34 or 35 37. 27 and 36 38. traditional suburethral retropubic sling procedure$*.tw. 39. traditional sling procedure$*.tw. 40. suburethral retropubic sling procedure$*.tw. 41. retropubic sling procedure$*.tw. 42. traditional suburethral sling*.tw. 43. Suburethral Slings/ or Urinary Incontinence, Stress/ or Urologic Surgical Procedures/ 44. 27 and 43 45. 21 or 23 or 26 or 32 or 36 or 38 or 39 or 40 or 41 or 42 46. suburethral slings/ 47. urological surgical procedures/ 48. 45 or 46 or 47 49. 48 and 27 50. remove duplicates from 49
Search strategy 2:
1. economics.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 2. value of life.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 3. exp "costs and cost analysis"/ 4. exp economics, hospital/ 5. exp economics, medical/ 6. economics, nursing.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 7. economics, pharmaceutical.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 8. exp "fees and charges"/ 9. exp budgets/ 10. budget*.ti,ab. 11. cost*.ti. 12. (economic* or pharmaco?economic*).ti. 13. (price* or pricing*).ti,ab. 14. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab. 15. (financ* or fee or fees).ti,ab. 16. (value adj2 (money or monetary)).ti,ab. 17. or/1‐16 18. economics.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 19. value of life.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 20. exp "costs and cost analysis"/ 21. exp economics, hospital/ 22. exp economics, medical/23. economics, nursing.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 24. economics, pharmaceutical.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 25. exp "fees and charges"/ 26. exp budgets/ 27. budget*.ti,ab. 28. cost*.ti. 29. (economic* or pharmaco?economic*).ti. 30. (price* or pricing*).ti,ab. 31. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab. 32. (financ* or fee or fees).ti,ab. 33. (value adj2 (money or monetary)).ti,ab. 34. 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 35. ((energy or oxygen) adj cost).ti,ab. 36. (metabolic adj cost).ti,ab. 37. ((energy or oxygen) adj expenditure).ti,ab. 38. 34 or 35 or 36 or 37 39. urinary incontinence.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 40. ((stress$ or mix$ or urg$ or urin$) adj3 incontinen$).tw. 41. Urinary incontinence, stress.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 42. stress urinary incontinence*.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 43. 39 or 40 or 41 or 42 44. intervention surgery*.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 45. colporrhaphy.tw. 46. Bologna procedure*.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 47. Kelly‐Kennedy.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 48. Marion Kelly.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 49. Diaphragmplasty.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 50. Vaginal urethrocystopexy.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 51. Cystocele repair.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 52. Kelly plication.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 53. anterior vaginal repair$.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 54. anterior colporrhaphy.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 55. 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 56. 38 and 43 and 55 57. remove duplicates from 56 58. Bladder neck needle suspension$.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 59. 38 and 43 and 58 60. burch colposuspension.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 61. open abdominal retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 62. Paravaginal defect repair.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 63. Marshall‐Marchetti‐Krantz.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 64. abdominal burch.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 65. abdominal colposuspension.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 66. endopelvic Fascia Plication.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 67. 60 or 61 or 62 or 63 or 64 or 65 or 66 68. 38 and 43 69. 67 and 68 70. laparoscopic retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 71. laparoscopic colposuspension.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 72. retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 73. 70 or 71 or 72 74. 68 and 73 75. remove duplicates from 74 76. suburethral sling.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 77. abdominal sling.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 78. traditional sling procedure$*.tw. 79. suburethral sling procedure.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 80. 76 or 77 or 78 or 79 81. 68 and 80 82. remove duplicates from 81 83. mid$urethral sling.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 84. retropubic sling procedure$*.tw. 85. transobturator sling procedure$.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 86. 83 or 84 or 85 87. remove duplicates from 86 88. 68 and 87 89. TVT‐Secur.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 90. mini‐arc.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 91. ajust.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 92. needleless.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 93. solyx.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 94. single$incision sling$.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 95. miniarc.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 96. mini$sling.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 97. Ophira.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 98. Tissue Fixation System.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 99. 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 100. 68 and 99 101. remove duplicates from 100 102. ((urethra$ or periurethra$ or transurethra$) adj3 (agent$ or bulk$ or injection$ or injectable$)).tw. 103. injection therapy.tw. 104. injectable$.tw. 105. (injectable$ adj2 agent$).tw. 106. (bulk$ adj3 agent$).tw. 107. Peri$urethral injection$.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 108. Autologous fat.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 109. Macroplastique.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 110. Calcium hydroxylapatite.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 111. Hyaluronic acid with dextranomer.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 112. Porcine dermal implant.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 113. Ethylene vinyl alcohol copolymer.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 114. Silicon particles.mp. [mp=ti, ab, ot, nm, hw, fx, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, dq] 115. 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114 116. 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114 117. 68 and 115 118. 55 or 58 or 67 or 73 or 80 or 86 or 99 or 115 119. 118 and 38 and 43 120. remove duplicates from 119
NHS EED (Ovid) (1st Quarter 2016)
NHS Economic Evaluation Database (NHS EED) on OvidSP (1st Quarter 2016) searched on 6 April 2017. As this database is no longer updated by the producer, we did not perform further updates of this search as no new records would have been added.
We searched NHS EED using the following search strategy.
1. Urinary incontinence/ 2. Urinary incontinence, stress/ 3. ((stress$ or mix$ or urg$ or urin$) adj3 incontinen$).tw. 4. Colporrhaphy.tw. 5. Colpoperineoplast$.tw. 6. Sling procedure$.tw. 7. Sling$ procedure$.tw. 8. Bladder neck needle suspension$.tw. 9. Anterior vaginal repair$ .tw. 10. Or/1‐9
Data and analyses
Comparison 3. Traditional suburethral sling operation versus drugs.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of continent women within 1 year (any definition) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 urodynamic stress incontinence (only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 stress urinary incontinence (symptoms only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 mixed incontinence | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Urge urinary symptoms, urgency urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 mixed incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
3.1. Analysis.
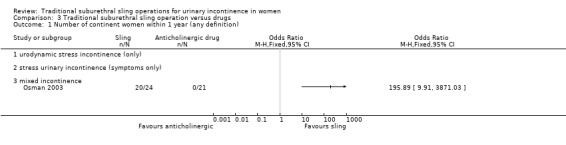
Comparison 3 Traditional suburethral sling operation versus drugs, Outcome 1 Number of continent women within 1 year (any definition).
3.2. Analysis.
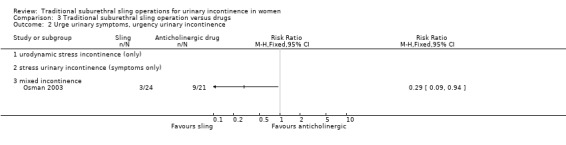
Comparison 3 Traditional suburethral sling operation versus drugs, Outcome 2 Urge urinary symptoms, urgency urinary incontinence.
Comparison 4. Traditional suburethral sling operation versus injectables.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of continent women within 1 year (any definition) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 urodynamic stress incontinence (only) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 stress urinary incontinence (symptoms only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 mixed urinary incontinence | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number of continent women at 1 to 5 years (any definition) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 urodynamic stress incontinence (only) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 stress urinary incontinence (symptoms only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 mixed urinary incontinence | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Repeat surgery for urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Number of women cured after first year (women's observations) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 urodynamic stress incontinence (only) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 stress urinary incontinence (symptoms only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 mixed urinary incontinence | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Number of women satisfied (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Number of women with urinary incontinence within first year (clinician's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Urinary tract infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 De novo detrusor overactivity (urodynamic diagnosis) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Voiding dysfunction | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
4.1. Analysis.
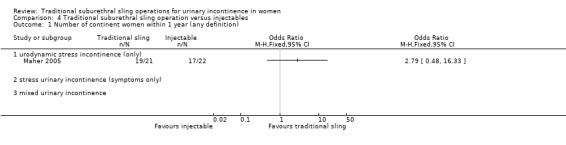
Comparison 4 Traditional suburethral sling operation versus injectables, Outcome 1 Number of continent women within 1 year (any definition).
4.4. Analysis.
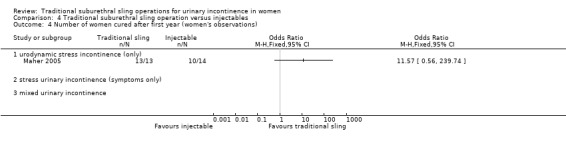
Comparison 4 Traditional suburethral sling operation versus injectables, Outcome 4 Number of women cured after first year (women's observations).
4.5. Analysis.
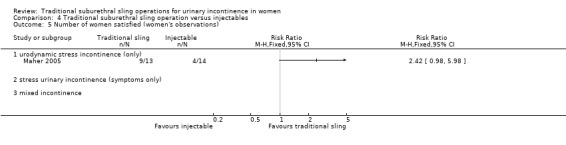
Comparison 4 Traditional suburethral sling operation versus injectables, Outcome 5 Number of women satisfied (women's observations).
4.6. Analysis.
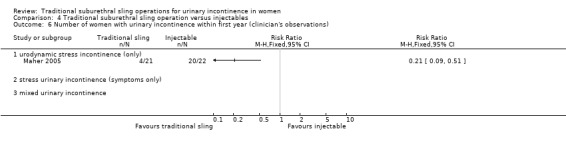
Comparison 4 Traditional suburethral sling operation versus injectables, Outcome 6 Number of women with urinary incontinence within first year (clinician's observations).
4.8. Analysis.
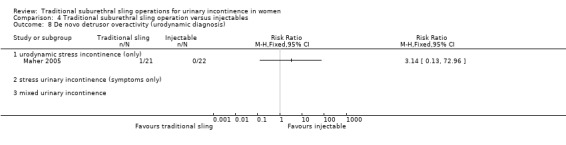
Comparison 4 Traditional suburethral sling operation versus injectables, Outcome 8 De novo detrusor overactivity (urodynamic diagnosis).
4.9. Analysis.
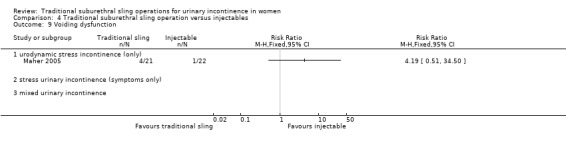
Comparison 4 Traditional suburethral sling operation versus injectables, Outcome 9 Voiding dysfunction.
Comparison 6. Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of continent women within 1 year (any definition) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 urodynamic stress incontinence (only) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 stress urinary incontinence (symptoms only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 mixed incontinence | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number of continent women at 1 to 5 years (any definition) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 urodynamic stress incontinence (only) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 stress urinary incontinence (symptoms only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 mixed incontinence | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 CURE: number of women cured after first year (women's observations) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 urodynamic stress incontinence (only) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 stress urinary incontinence (symptoms only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 mixed incontinence | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Length of hospital stay (hours) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 stress urinary incontinence (symptoms only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 mixed incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Perioperative surgical complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Urinary urgency symptoms, urgency urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Detrusor overactivity (urodynamic diagnosis) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Voiding dysfunction after 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
6.1. Analysis.
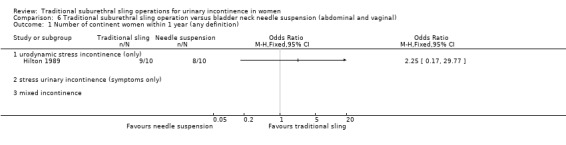
Comparison 6 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 1 Number of continent women within 1 year (any definition).
6.2. Analysis.
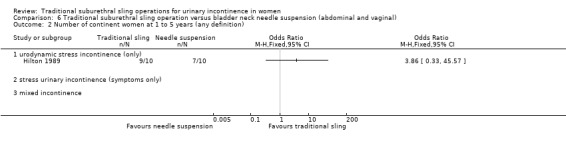
Comparison 6 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 2 Number of continent women at 1 to 5 years (any definition).
6.3. Analysis.
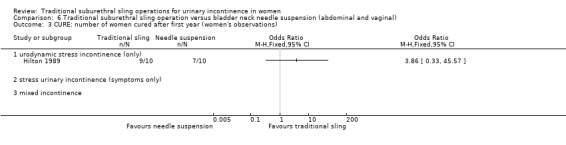
Comparison 6 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 3 CURE: number of women cured after first year (women's observations).
6.4. Analysis.
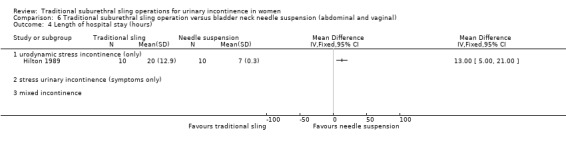
Comparison 6 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 4 Length of hospital stay (hours).
6.5. Analysis.
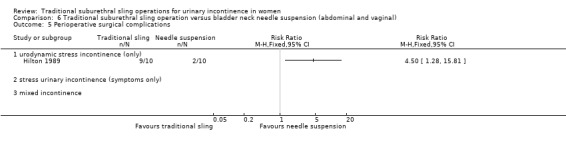
Comparison 6 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 5 Perioperative surgical complications.
6.6. Analysis.
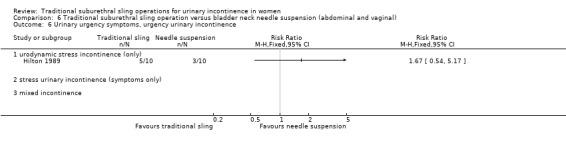
Comparison 6 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 6 Urinary urgency symptoms, urgency urinary incontinence.
6.7. Analysis.
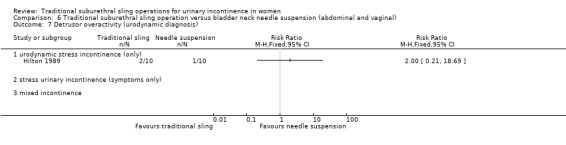
Comparison 6 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 7 Detrusor overactivity (urodynamic diagnosis).
6.8. Analysis.
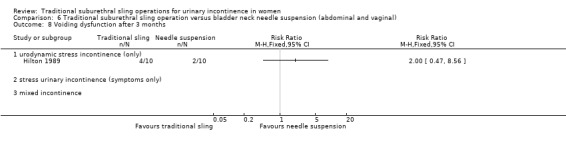
Comparison 6 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 8 Voiding dysfunction after 3 months.
Comparison 7. Traditional suburethral sling operation versus open abdominal retropubic colposuspension.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of continent women within 1 year (any definition) | 4 | 147 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.70 [0.69, 10.55] |
| 1.1 urodynamic stress incontinence (only) | 4 | 147 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.70 [0.69, 10.55] |
| 1.2 stress urinary incontinence (symptoms only) | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 mixed incontinence | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number of continent women at 1 to 5 years (any definition) | 4 | 687 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.70 [1.22, 2.37] |
| 2.1 urodynamic stress incontinence (only) | 3 | 167 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.84 [0.65, 5.24] |
| 2.2 stress urinary incontinence (symptoms only) | 1 | 520 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.69 [1.19, 2.39] |
| 2.3 mixed incontinence | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number of continent women after 5 years (any definition) | 2 | 481 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.55 [1.06, 2.27] |
| 3.1 urodynamic stress incontinence (only) | 1 | 28 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.03, 4.92] |
| 3.2 stress urinary incontinence (symptoms only) | 1 | 453 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.61 [1.09, 2.37] |
| 3.3 mixed incontinence | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Repeat surgery for urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Number of women cured after first year (women's observations) | 3 | 515 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.56 [1.07, 2.28] |
| 5.1 urodynamic stress incontinence (only) | 2 | 62 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.18, 4.89] |
| 5.2 stress urinary incontinence (symptoms only) | 1 | 453 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.61 [1.09, 2.37] |
| 5.3 mixed incontinence | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Number of women satisfied (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Number of women with urinary incontinence within first year (clinician's observations) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Number of women with urinary incontinence at 1 to 5 years (clinician's observations) | 3 | 626 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.59, 1.31] |
| 8.1 urodynamic stress incontinence (only) | 2 | 106 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.16, 1.86] |
| 8.2 stress urinary incontinence (symptoms only) | 1 | 520 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.62, 1.42] |
| 8.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Number of women with urinary incontinence after 5 years (clinician's observations) | 2 | 461 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.80, 1.01] |
| 9.1 urodynamic stress incontinence (only) | 1 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.01, 4.37] |
| 9.2 stress urinary incontinence (symptoms only) | 1 | 433 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.81, 1.02] |
| 9.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Duration of operation (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 stress urinary incontinence (symptoms only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 mixed incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Length of hospital stay (days) | 3 | 137 | Mean Difference (IV, Fixed, 95% CI) | 2.03 [1.47, 2.59] |
| 11.1 urodynamic stress incontinence (only) | 3 | 137 | Mean Difference (IV, Fixed, 95% CI) | 2.03 [1.47, 2.59] |
| 11.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 mixed incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Time to catheter removal (days) | 2 | 108 | Mean Difference (IV, Fixed, 95% CI) | 8.01 [6.84, 9.18] |
| 12.1 urodynamic stress incontinence (only) | 2 | 108 | Mean Difference (IV, Fixed, 95% CI) | 8.01 [6.84, 9.18] |
| 12.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12.3 mixed incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Time to return to normal activity level | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13.3 mixed incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Number of women requiring treatment for pelvic organ prolapse | 3 | 559 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.05, 0.77] |
| 14.1 urodynamic stress incontinence (only) | 2 | 106 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.04, 1.11] |
| 14.2 stress urinary incontinence (symptoms only) | 1 | 453 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.02, 1.74] |
| 14.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Perioperative surgical complications | 4 | 792 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.83, 1.86] |
| 15.1 urodynamic stress incontinence (only) | 3 | 137 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.28, 2.52] |
| 15.2 stress urinary incontinence (symptoms only) | 1 | 655 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.86, 2.04] |
| 15.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Bladder perforation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 16.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Urinary tract infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 17.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Number of women with recurrent UTIs at > 5 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 18.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Urinary urgency symptoms, urgency urinary incontinence | 2 | 525 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.74, 1.64] |
| 19.1 urodynamic stress incontinence (only) | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.54, 7.39] |
| 19.2 stress urinary incontinence (symptoms only) | 1 | 453 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.67, 1.56] |
| 19.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Detrusor overactivity (urodynamic diagnosis) | 4 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [0.52, 3.87] |
| 20.1 urodynamic stress incontinence (only) | 4 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [0.52, 3.87] |
| 20.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Voiding dysfunction after 3 months | 5 | 853 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.08 [3.10, 11.95] |
| 21.1 urodynamic stress incontinence (only) | 4 | 198 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.48 [1.16, 17.36] |
| 21.2 stress urinary incontinence (symptoms only) | 1 | 655 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.63 [3.04, 14.47] |
| 21.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Long‐term voiding dysfunction > 5 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 22.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23 Condition‐specific measures to assess quality of life | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 23.1 Urinary Distress Index (UDI) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.2 Incontinence Impact Questionnaire (IIQ) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
7.22. Analysis.
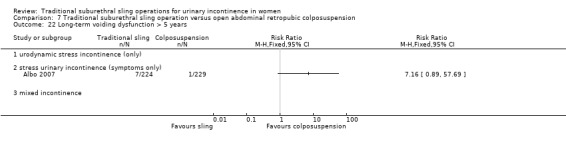
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 22 Long‐term voiding dysfunction > 5 years.
7.23. Analysis.
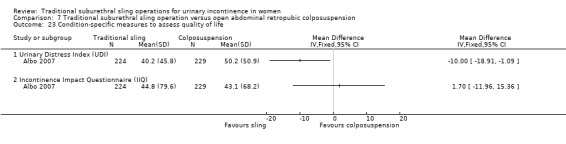
Comparison 7 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 23 Condition‐specific measures to assess quality of life.
Comparison 9. Traditional suburethral sling operation versus mid‐urethral sling or tape.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of continent women within 1 year (any definition) | 11 | 841 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.67, 1.32] |
| 1.1 urodynamic stress incontinence (only) | 5 | 427 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.60, 1.56] |
| 1.2 stress urinary incontinence (symptoms only) | 1 | 53 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.12, 6.79] |
| 1.3 mixed urinary incontinence | 5 | 361 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.55, 1.51] |
| 2 Number of continent women at 1 to 5 years (any definition) | 6 | 458 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.44, 1.02] |
| 2.1 urodynamic stress incontinence (only) | 4 | 364 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.47, 1.25] |
| 2.2 stress urinary incontinence (symptoms only) | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 mixed urinary incontinence | 2 | 94 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.17, 1.04] |
| 3 Number of continent women after 5 years (any definition) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 urodynamic stress incontinence (only) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 stress urinary incontinence (symptoms only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 mixed urinary incontinence | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Repeat surgery for urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Number of women cured after first year (women's observations) | 4 | 337 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.65, 1.72] |
| 5.1 urodynamic stress incontinence (only) | 3 | 293 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.72, 2.03] |
| 5.2 stress urinary incontinence (symptoms only) | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.3 mixed urinary incontinence | 1 | 44 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.10, 1.72] |
| 6 Number of women improved or cured within 1 year (women's observations) | 3 | 425 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.74, 2.39] |
| 6.1 urodynamic stress incontinence (only) | 2 | 286 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.43, 2.64] |
| 6.2 stress urinary incontinence (symptoms only) | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 mixed urinary incontinence | 1 | 139 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.56 [0.72, 3.39] |
| 7 Number of women improved or cured at 1 to 5 years (women's observations) | 2 | 264 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.31, 1.87] |
| 7.1 urodynamic stress incontinence (only) | 2 | 264 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.31, 1.87] |
| 7.2 stress urinary incontinence (symptoms only) | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 mixed urinary incontinence | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Number of women improved or cured after 5 years (women's observations) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 urodynamic stress incontinence (only) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 stress urinary incontinence (symptoms only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 mixed urinary incontinence | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Number of women satisfied (women's observations) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 urodynamic stress incontinence (only) | 2 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.89, 1.33] |
| 9.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.3 mixed urinary incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Pad test of quantified leakage (mean weight of urine lost) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 stress urinary incontinence (symptoms only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 mixed urinary incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Number of women with urinary incontinence within first year (clinician's observations) | 2 | 105 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.45, 3.71] |
| 11.1 urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 mixed urinary incontinence | 2 | 105 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.45, 3.71] |
| 12 Number of women with urinary incontinence at 1 to 5 years (any definition) (clinician's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 12.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.3 mixed urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Duration of operation (minutes) | 7 | 355 | Mean Difference (IV, Fixed, 95% CI) | 57.08 [54.67, 59.49] |
| 13.1 urodynamic stress incontinence (only) | 2 | 61 | Mean Difference (IV, Fixed, 95% CI) | 46.91 [42.31, 51.52] |
| 13.2 stress urinary incontinence (symptoms only) | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | 20.0 [7.08, 32.92] |
| 13.3 mixed urinary incontinence | 4 | 241 | Mean Difference (IV, Fixed, 95% CI) | 62.96 [60.07, 65.86] |
| 14 Length of hospital stay (days) | 4 | 194 | Mean Difference (IV, Fixed, 95% CI) | 0.74 [0.55, 0.93] |
| 14.1 urodynamic stress incontinence (only) | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | 0.65 [0.39, 0.91] |
| 14.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.3 mixed urinary incontinence | 3 | 174 | Mean Difference (IV, Fixed, 95% CI) | 0.83 [0.56, 1.10] |
| 15 Time to catheter removal (days) | 2 | 113 | Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.07, 0.30] |
| 15.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 stress urinary incontinence (symptoms only) | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | 2.3 [0.01, 4.59] |
| 15.3 mixed urinary incontinence | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.09, 0.29] |
| 16 Perioperative surgical complications | 4 | 293 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.74 [1.16, 2.60] |
| 16.1 urodynamic stress incontinence (only) | 2 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.73 [1.01, 2.96] |
| 16.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16.3 mixed urinary incontinence | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.74 [0.94, 3.21] |
| 17 Bladder perforations | 10 | 844 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.34, 1.01] |
| 17.1 urodynamic stress incontinence (only) | 3 | 334 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.19, 2.86] |
| 17.2 stress urinary incontinence (symptoms only) | 1 | 53 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.05, 5.81] |
| 17.3 mixed urinary incontinence | 6 | 457 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.30, 1.03] |
| 18 Urethral injury | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 18.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.3 mixed urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Vaginal bleeding | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 19.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.3 mixed urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Urinary tract infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 20.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.3 mixed urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 Voiding dysfunction | 8 | 629 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.85, 2.12] |
| 21.1 urodynamic stress incontinence (only) | 3 | 325 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.60, 2.46] |
| 21.2 stress urinary incontinence (symptoms only) | 1 | 53 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.61 [0.76, 9.03] |
| 21.3 mixed urinary incontinence | 4 | 251 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.58, 2.40] |
| 22 Urinary urgency symptoms, urgency urinary incontinence | 4 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.58, 3.88] |
| 22.1 urodynamic stress incontinence (only) | 1 | 124 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.01, 8.29] |
| 22.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 22.3 mixed urinary incontinence | 3 | 171 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.81 [0.65, 5.06] |
| 23 De novo detrusor overactivity (urodynamic diagnosis) | 4 | 325 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.61 [1.17, 5.84] |
| 23.1 urodynamic stress incontinence (only) | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 23.2 stress urinary incontinence (symptoms only) | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.13 [0.13, 73.01] |
| 23.3 mixed urinary incontinence | 2 | 219 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.57 [1.12, 5.92] |
| 24 Long‐term adverse effects (release of sling required) | 3 | 326 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.53 [0.87, 7.35] |
| 24.1 urodynamic stress incontinence (only) | 2 | 266 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.68 [0.50, 5.66] |
| 24.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 24.3 mixed urinary incontinence | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 9.6 [0.54, 170.84] |
| 25 Long‐term adverse effects (wound pain at 6 months) | 3 | 257 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.40 [1.94, 21.12] |
| 25.1 urodynamic stress incontinence (only) | 1 | 124 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.16 [0.25, 105.36] |
| 25.2 stress urinary incontinence (symptoms only) | 1 | 53 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.92 [0.90, 17.15] |
| 25.3 mixed urinary incontinence | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 17.0 [1.01, 284.96] |
| 26 Long‐term adverse effects (vaginal mesh or graft exposure) | 5 | 348 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.05, 1.65] |
| 26.1 urodynamic stress incontinence (only) | 2 | 165 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.04, 3.24] |
| 26.2 stress urinary incontinence (symptoms only) | 1 | 53 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 26.3 mixed urinary incontinence | 2 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.97] |
| 27 Condition‐specific measures to assess quality of life: UDI‐6 | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 7.30 [‐2.00, 16.60] |
| 27.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 27.2 stress urinary incontinence (symptoms only) | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 7.30 [‐2.00, 16.60] |
| 27.3 mixed urinary incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Condition‐specific measures to assess quality of life: IIQ‐7 | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐10.17, 11.37] |
| 28.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 28.2 stress urinary incontinence (symptoms only) | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐10.17, 11.37] |
| 28.3 mixed urinary incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
9.4. Analysis.
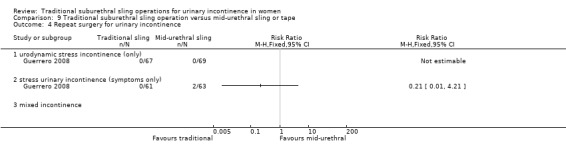
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 4 Repeat surgery for urinary incontinence.
9.18. Analysis.
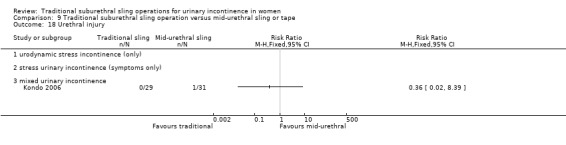
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 18 Urethral injury.
9.21. Analysis.
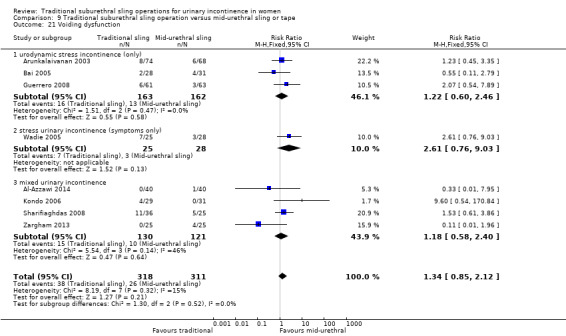
Comparison 9 Traditional suburethral sling operation versus mid‐urethral sling or tape, Outcome 21 Voiding dysfunction.
Comparison 10. Traditional suburethral sling operation versus a single‐incision sling (mini‐sling).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of continent women at 1 to 5 years (any definition) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 urodynamic stress incontinence (only) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 stress urinary incontinence (symptoms only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 mixed incontinence | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number of women cured after first year (women's observations) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 urodynamic stress incontinence (only) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 stress urinary incontinence (symptoms only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 mixed incontinence | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Number of women satisfied (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Number of women with urinary incontinence (clinician's observations) within first year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Bladder perforation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Urinary urgency symptoms, urgency urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Pain with intercourse (dyspareunia) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Long‐term adverse effects (vaginal mesh or graft exposure) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Condition‐specific measures to assess quality of life: IIQ score | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 stress urinary incontinence (symptoms only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 mixed urinary incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
10.1. Analysis.
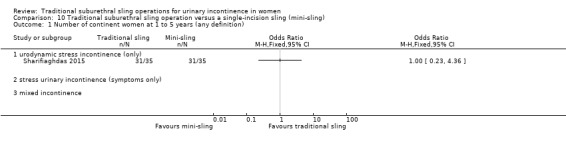
Comparison 10 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 1 Number of continent women at 1 to 5 years (any definition).
10.2. Analysis.
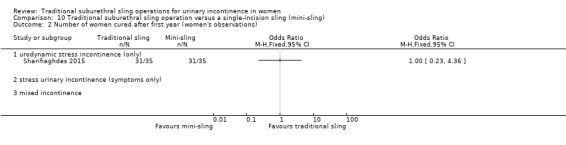
Comparison 10 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 2 Number of women cured after first year (women's observations).
10.3. Analysis.
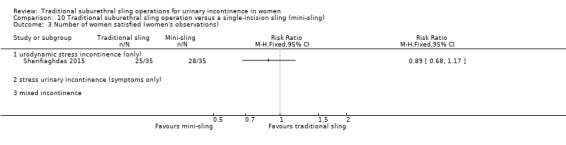
Comparison 10 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 3 Number of women satisfied (women's observations).
10.4. Analysis.
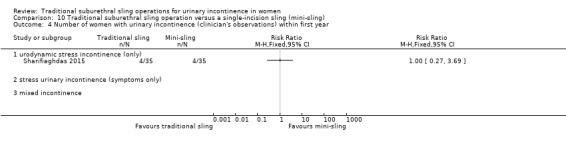
Comparison 10 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 4 Number of women with urinary incontinence (clinician's observations) within first year.
10.5. Analysis.
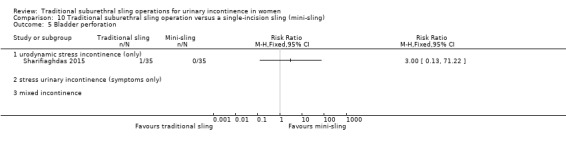
Comparison 10 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 5 Bladder perforation.
10.6. Analysis.
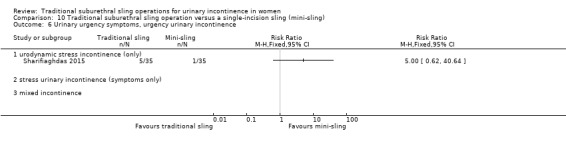
Comparison 10 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 6 Urinary urgency symptoms, urgency urinary incontinence.
10.7. Analysis.
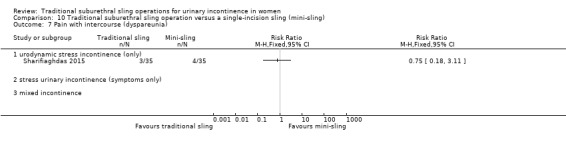
Comparison 10 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 7 Pain with intercourse (dyspareunia).
10.8. Analysis.
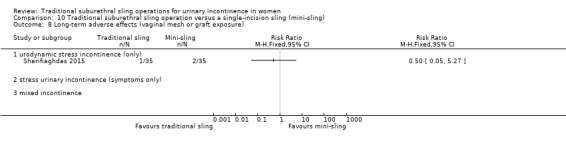
Comparison 10 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 8 Long‐term adverse effects (vaginal mesh or graft exposure).
10.9. Analysis.
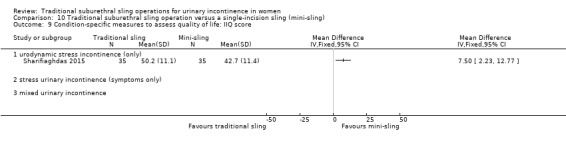
Comparison 10 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 9 Condition‐specific measures to assess quality of life: IIQ score.
Comparison 11. One type of traditional sling operation versus another type of traditional sling operation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of continent women within 1 year (any definition) | 5 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 fascial sling vs Pelvicol sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 standard sling vs short sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 autologous fascial sling vs Fortaperm sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Vypro vs Ultrapro | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Vypro vs Prolene light | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.6 Ultrapro vs Prolene light | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.7 fascial sling vs vaginal wall sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number of continent women at 1 to 5 years (any definition) | 7 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 fascial sling vs Pelvicol sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 standard sling vs short sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 autologous dermal graft patch vs cadaveric fascia lata | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 rectus fascia sling vs Goretex sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 Vypro vs Ultrapro | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 Vypro vs Prolene light | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.7 Ultrapro vs Prolene light | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.8 anterior vaginal wall sling vs biosynthetic mesh sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.9 anterior rectus sheath sling vs Prolene strip | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.10 anterior rectus sheath sling vs anterior vaginal wall patch | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.11 Prolene strip vs anterior vaginal wall patch | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Number of continent women after 5 years (any definition) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 standard sling vs short sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Repeat surgery for urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Number of women cured after first year (women's observations) | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 fascial sling vs Pelvicol sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 standard sling vs short sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 autologous dermal graft patch vs cadaveric fascia lata | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Number of women improved or cured within first year (women's observations) | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 fascial sling vs Pelvicol sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 autologous fascial sling vs Fortaperm sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 rectus fascia sling vs Goretex sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Number of women improved or cured at 1 to 5 years (women's observations) | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 autologous dermal graft patch vs cadaveric fascia lata | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 rectus fascia sling vs Goretex sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.4 anterior rectus sheath sling vs Prolene strip | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.5 anterior rectus sheath sling vs anterior vaginal wall patch | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.6 Prolene strip vs anterior vaginal wall patch | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Number of women satisfied (women's observations) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Vypro vs Ultrapro | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Vypro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 Ultrapro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.5 anterior vaginal wall sling vs biosynthetic mesh sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Pad test of quantified leakage (mean weight of urine lost) within 1 year | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 standard sling vs short sling | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Vypro vs Ultrapro | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 Vypro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.4 Ultrapro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Pad test of quantified leakage (mean weight of urine lost) at 1 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Vypro vs Ultrapro | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Vypro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Ultrapro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Duration of operation (minutes) | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1 standard sling vs short sling | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 anterior rectus sheath sling vs Prolene strip | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.3 anterior rectus sheath sling vs anterior vaginal wall patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.4 Prolene strip vs anterior vaginal wall patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Blood loss (mL) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 anterior rectus sheath sling vs Prolene strip | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 anterior rectus sheath sling vs anterior vaginal wall patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.3 Prolene strip vs anterior vaginal wall patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Length of hospital stay (days) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13.1 anterior rectus sheath sling vs Prolene strip | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 anterior rectus sheath sling vs anterior vaginal wall patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.3 Prolene strip vs anterior vaginal wall patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Perioperative surgical complications | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 14.1 standard sling vs short sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 rectus fascia sling vs Goretex sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.3 fascial sling vs vaginal wall sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Bladder perforation | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 15.1 standard sling vs short sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.3 anterior rectus sheath sling vs Prolene strip | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.4 anterior rectus sheath sling vs anterior vaginal wall patch | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.5 Prolene strip vs anterior vaginal wall patch | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Urinary tract infection | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 16.1 standard sling vs short sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 anterior vaginal wall sling vs biosynthetic mesh sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Vaginal bleeding | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 17.1 anterior vaginal wall sling vs biosynthetic mesh sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Long‐term adverse effects (wound pain) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 18.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Voiding dysfunction | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 19.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 standard sling vs short sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.3 Vypro vs Ultrapro | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.4 Vypro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.5 Ultrapro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.6 anterior vaginal wall sling vs biosynthetic mesh sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.7 anterior rectus sheath sling vs Prolene strip | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.8 anterior rectus sheath sling vs anterior vaginal wall patch | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.9 Prolene strip vs anterior vaginal wall patch | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.10 fascial sling vs vaginal wall sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Urinary urgency symptoms, urgency urinary incontinence | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 20.1 standard sling vs short sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.2 Vypro vs Ultrapro | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.3 Vypro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.4 Ultrapro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.5 rectus fascia sling vs Goretex sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 Detrusor overactivity (urodynamic overactivity) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 21.1 autologous dermal graft patch vs cadaveric fascia lata | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22 Long‐term adverse effects (release of sling required) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 22.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23 Long‐term adverse effects (vaginal mesh or graft exposure) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 23.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.2 Vypro vs Ultrapro | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.3 Vypro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.4 Ultrapro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.5 anterior vaginal wall sling vs biosynthetic mesh sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24 Condition‐specific measures to assess quality of life (ICI‐Q short form UI score at 1 year) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 24.1 Vypro vs Ultrapro | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.2 Vypro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.3 Ultrapro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 25 Condition‐specific measures to assess quality of life (ICI‐Q short form UI score at 1 to 5 years) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 25.1 Vypro vs Ultrapro | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 25.2 Vypro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 25.3 Ultrapro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
11.17. Analysis.
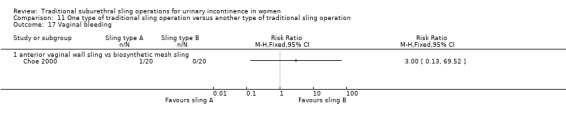
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 17 Vaginal bleeding.
11.18. Analysis.
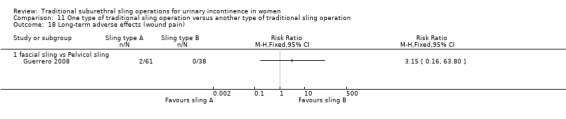
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 18 Long‐term adverse effects (wound pain).
11.22. Analysis.
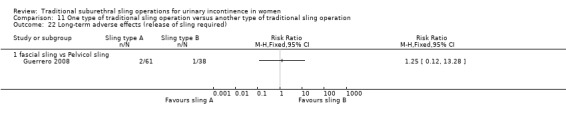
Comparison 11 One type of traditional sling operation versus another type of traditional sling operation, Outcome 22 Long‐term adverse effects (release of sling required).
Comparison 12. Traditional suburethral sling operation versus drugs.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of women with urinary incontinence (worse, unchanged, or improved) within first year (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 mixed incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Urge urinary symptoms, urgency urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 mixed incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
12.1. Analysis.
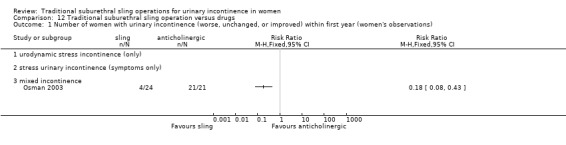
Comparison 12 Traditional suburethral sling operation versus drugs, Outcome 1 Number of women with urinary incontinence (worse, unchanged, or improved) within first year (women's observations).
12.2. Analysis.
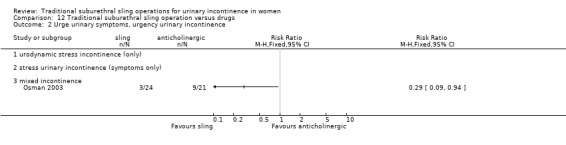
Comparison 12 Traditional suburethral sling operation versus drugs, Outcome 2 Urge urinary symptoms, urgency urinary incontinence.
Comparison 13. Traditional suburethral sling operation versus injectables.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of women with urinary incontinence (worse, unchanged, or improved) within first year (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number of women with urinary incontinence (worse, unchanged, or improved) after first year (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Number of women with urinary incontinence (clinician's observations) within first year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 CURE: number of women cured after first year (women's observations) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 urodynamic stress incontinence (only) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 stress urinary incontinence (symptoms only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 mixed urinary incontinence | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Voiding dysfunction | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 De novo detrusor overactivity (urodynamic diagnosis) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Urinary tract infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Repeat surgery for urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
13.1. Analysis.
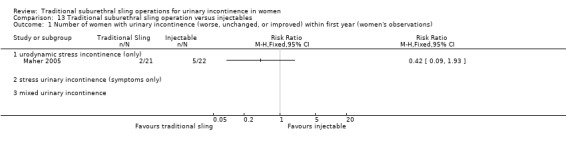
Comparison 13 Traditional suburethral sling operation versus injectables, Outcome 1 Number of women with urinary incontinence (worse, unchanged, or improved) within first year (women's observations).
13.2. Analysis.
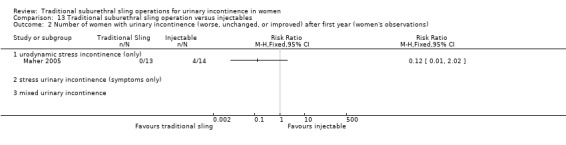
Comparison 13 Traditional suburethral sling operation versus injectables, Outcome 2 Number of women with urinary incontinence (worse, unchanged, or improved) after first year (women's observations).
13.3. Analysis.
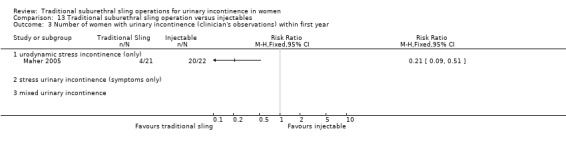
Comparison 13 Traditional suburethral sling operation versus injectables, Outcome 3 Number of women with urinary incontinence (clinician's observations) within first year.
13.4. Analysis.
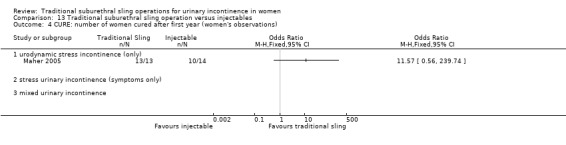
Comparison 13 Traditional suburethral sling operation versus injectables, Outcome 4 CURE: number of women cured after first year (women's observations).
13.5. Analysis.
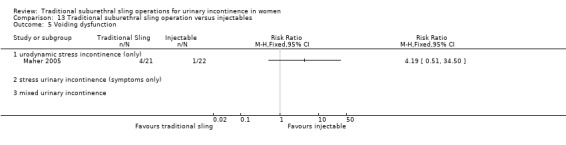
Comparison 13 Traditional suburethral sling operation versus injectables, Outcome 5 Voiding dysfunction.
13.6. Analysis.
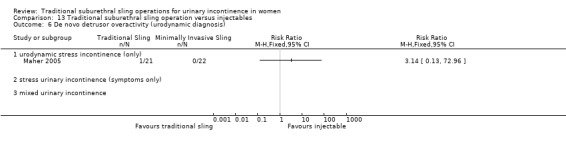
Comparison 13 Traditional suburethral sling operation versus injectables, Outcome 6 De novo detrusor overactivity (urodynamic diagnosis).
13.7. Analysis.
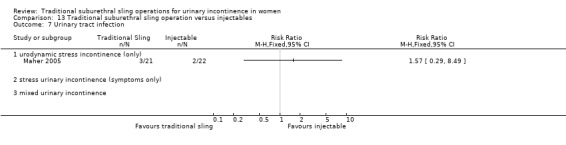
Comparison 13 Traditional suburethral sling operation versus injectables, Outcome 7 Urinary tract infection.
13.8. Analysis.
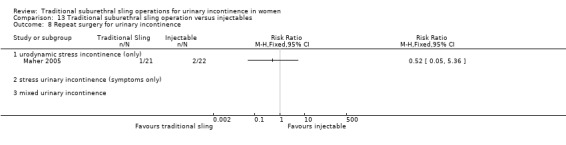
Comparison 13 Traditional suburethral sling operation versus injectables, Outcome 8 Repeat surgery for urinary incontinence.
Comparison 14. Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence (worse, unchanged, or improved) within first year (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number with incontinence (worse, unchanged, or improved) after first year (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 CURE: number of women cured after first year (women's observations) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 urodynamic stress incontinence (only) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 stress urinary incontinence (symptoms only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 mixed incontinence | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Length of hospital stay (hours) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 stress urinary incontinence (symptoms only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 mixed incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Perioperative surgical complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Urge urinary symptoms, urgency urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Voiding dysfunction after 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Detrusor overactivity (urodynamic diagnosis) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
14.1. Analysis.
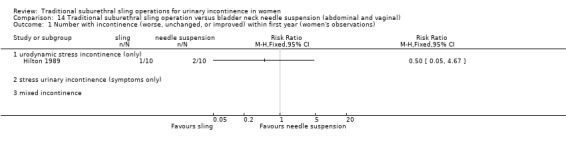
Comparison 14 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 1 Number with incontinence (worse, unchanged, or improved) within first year (women's observations).
14.2. Analysis.
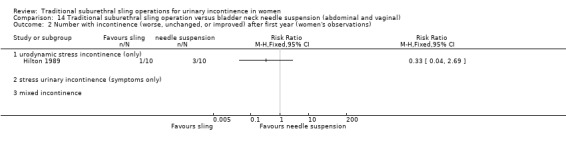
Comparison 14 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 2 Number with incontinence (worse, unchanged, or improved) after first year (women's observations).
14.3. Analysis.
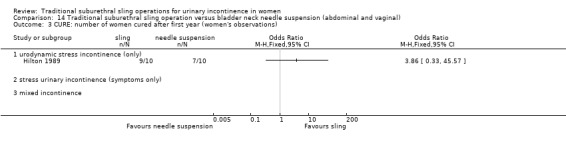
Comparison 14 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 3 CURE: number of women cured after first year (women's observations).
14.4. Analysis.
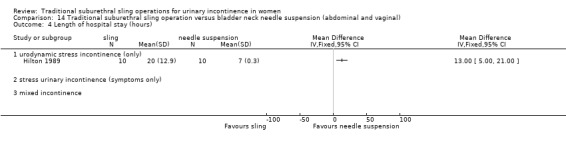
Comparison 14 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 4 Length of hospital stay (hours).
14.5. Analysis.
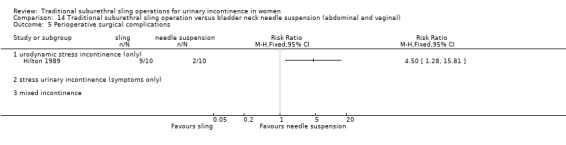
Comparison 14 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 5 Perioperative surgical complications.
14.6. Analysis.
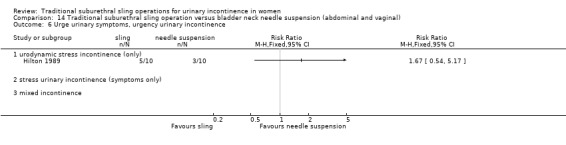
Comparison 14 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 6 Urge urinary symptoms, urgency urinary incontinence.
14.7. Analysis.
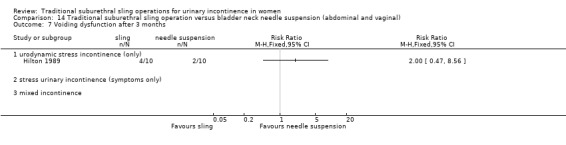
Comparison 14 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 7 Voiding dysfunction after 3 months.
14.8. Analysis.
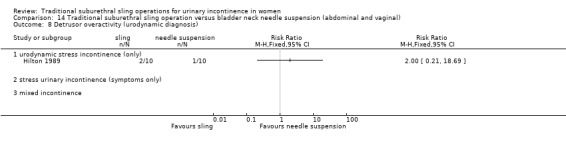
Comparison 14 Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal), Outcome 8 Detrusor overactivity (urodynamic diagnosis).
Comparison 15. Traditional suburethral sling operation versus open abdominal retropubic colposuspension.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of women with urinary incontinence (worse, unchanged, or improved) within first year (women's observations) | 4 | 147 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.11, 1.41] |
| 1.1 urodynamic stress incontinence (only) | 4 | 147 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.11, 1.41] |
| 1.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number not improved (worse or unchanged) within first year (women's observations) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.1 urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number of women with urinary incontinence (worse, unchanged, or improved) at 1 to 5 years (women's observations) | 4 | 687 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.61, 0.89] |
| 3.1 urodynamic stress incontinence (only) | 3 | 167 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.22, 1.49] |
| 3.2 stress urinary incontinence (symptoms only) | 1 | 520 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.62, 0.91] |
| 3.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number not improved (worse or unchanged) at 1 to 5 years (women's observations) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.1 urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Number of women with urinary incontinence (worse, unchanged, or improved) at > 5 years (women's observations) | 2 | 481 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.74, 0.98] |
| 5.1 urodynamic stress incontinence (only) | 1 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.31 [0.24, 22.62] |
| 5.2 stress urinary incontinence (symptoms only) | 1 | 453 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.73, 0.97] |
| 5.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 CURE: number of women cured at > 1 year (women's observations) | 3 | 515 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.56 [1.07, 2.28] |
| 6.1 urodynamic stress incontinence (only) | 2 | 62 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.18, 4.89] |
| 6.2 stress urinary incontinence (symptoms only) | 1 | 453 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.61 [1.09, 2.37] |
| 6.3 mixed incontinence | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number of women not satisfied at > 5 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Incontinent episodes over 24 hours | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.3 mixed incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Number of women with urinary incontinence (clinician's observations) within first year | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.1 urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Number of women with urinary incontinence (clinician's observations) at 1 to 5 years | 2 | 592 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.60, 1.34] |
| 10.1 urodynamic stress incontinence (only) | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.6 [0.15, 2.33] |
| 10.2 stress urinary incontinence (symptoms only) | 1 | 520 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.62, 1.42] |
| 10.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Number of women with urinary incontinence (clinician's observations) at > 5 years | 2 | 461 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.80, 1.01] |
| 11.1 urodynamic stress incontinence (only) | 1 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.01, 4.37] |
| 11.2 stress urinary incontinence (symptoms only) | 1 | 433 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.81, 1.02] |
| 11.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Duration of operation (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 stress urinary incontinence (symptoms only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.3 mixed incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Time to catheter removal (days) | 2 | 108 | Mean Difference (IV, Fixed, 95% CI) | 8.01 [6.84, 9.18] |
| 13.1 urodynamic stress incontinence (only) | 2 | 108 | Mean Difference (IV, Fixed, 95% CI) | 8.01 [6.84, 9.18] |
| 13.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13.3 mixed incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Length of hospital stay (days) | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.1 urodynamic stress incontinence (only) | 3 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 stress urinary incontinence (symptoms only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.3 mixed incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Time to return to normal activity level | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15.3 mixed incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Perioperative surgical complications | 4 | 792 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.83, 1.86] |
| 16.1 urodynamic stress incontinence (only) | 3 | 137 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.28, 2.52] |
| 16.2 stress urinary incontinence (symptoms only) | 1 | 655 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.86, 2.04] |
| 16.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Bladder perforation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 17.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Urinary tract infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 18.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Number of women with recurrent UTIs at > 5 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 19.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Urge urinary symptoms, urgency urinary incontinence | 2 | 525 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.74, 1.64] |
| 20.1 urodynamic stress incontinence (only) | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.54, 7.39] |
| 20.2 stress urinary incontinence (symptoms only) | 1 | 453 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.67, 1.56] |
| 20.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Detrusor overactivity (urodynamic diagnosis) | 4 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [0.52, 3.87] |
| 21.1 urodynamic stress incontinence (only) | 4 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [0.52, 3.87] |
| 21.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Voiding dysfunction after 3 months | 5 | 853 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.08 [3.10, 11.95] |
| 22.1 urodynamic stress incontinence (only) | 4 | 198 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.48 [1.16, 17.36] |
| 22.2 stress urinary incontinence (symptoms only) | 1 | 655 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.63 [3.04, 14.47] |
| 22.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Long‐term voiding dysfunction > 5 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 23.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24 Number of women requiring treatment for pelvic organ prolapse | 3 | 559 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.05, 0.77] |
| 24.1 urodynamic stress incontinence (only) | 2 | 106 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.04, 1.11] |
| 24.2 stress urinary incontinence (symptoms only) | 1 | 453 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.02, 1.74] |
| 24.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Repeat surgery for urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 25.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 25.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 25.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 26 Condition‐specific measures to assess quality of life | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 26.1 Urinary Distress Index (UDI) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 26.2 Incontinence Impact Questionnaire (IIQ) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
15.1. Analysis.
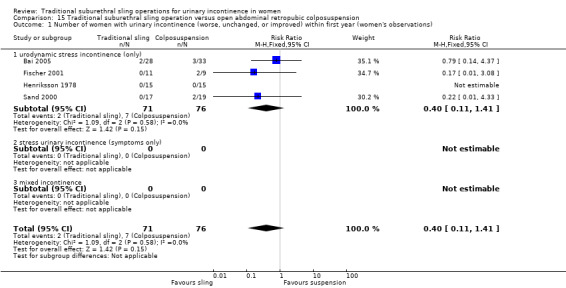
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 1 Number of women with urinary incontinence (worse, unchanged, or improved) within first year (women's observations).
15.3. Analysis.
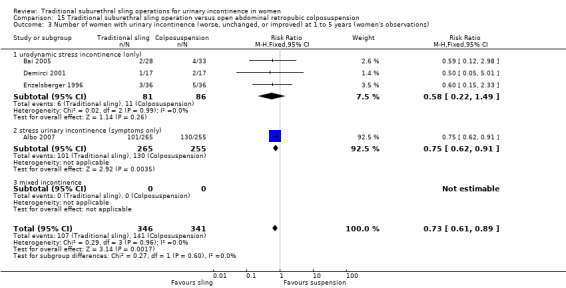
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 3 Number of women with urinary incontinence (worse, unchanged, or improved) at 1 to 5 years (women's observations).
15.5. Analysis.
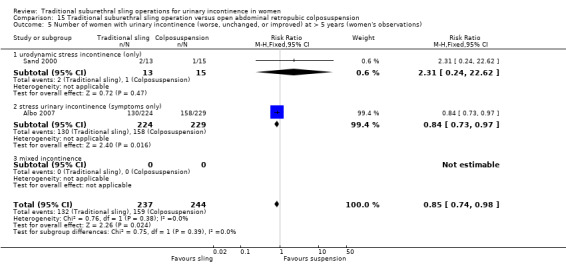
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 5 Number of women with urinary incontinence (worse, unchanged, or improved) at > 5 years (women's observations).
15.6. Analysis.
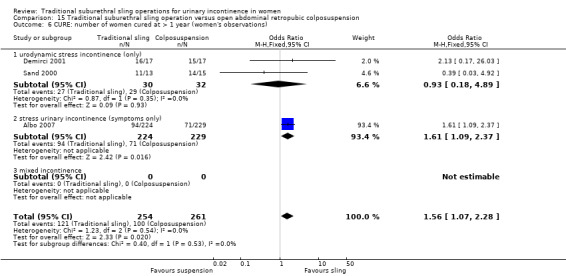
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 6 CURE: number of women cured at > 1 year (women's observations).
15.7. Analysis.
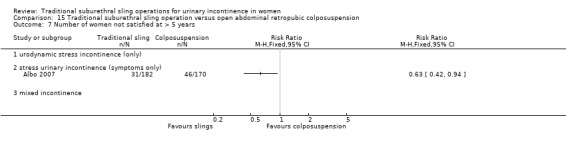
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 7 Number of women not satisfied at > 5 years.
15.10. Analysis.
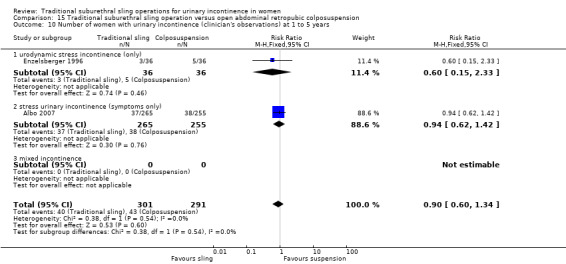
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 10 Number of women with urinary incontinence (clinician's observations) at 1 to 5 years.
15.11. Analysis.
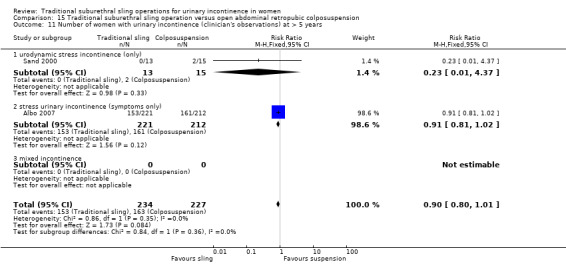
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 11 Number of women with urinary incontinence (clinician's observations) at > 5 years.
15.12. Analysis.
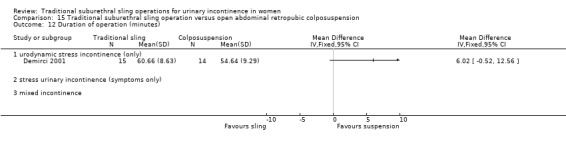
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 12 Duration of operation (minutes).
15.13. Analysis.
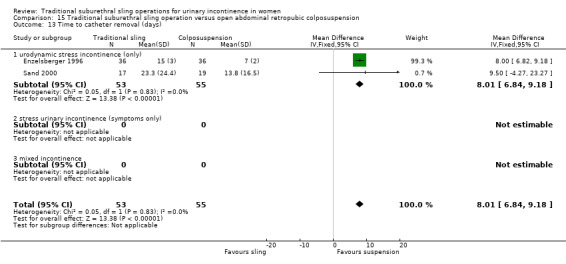
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 13 Time to catheter removal (days).
15.14. Analysis.
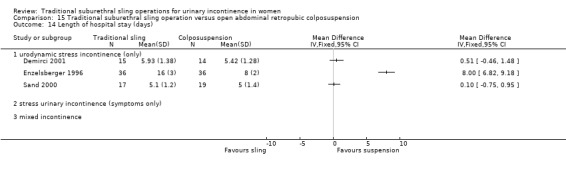
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 14 Length of hospital stay (days).
15.16. Analysis.
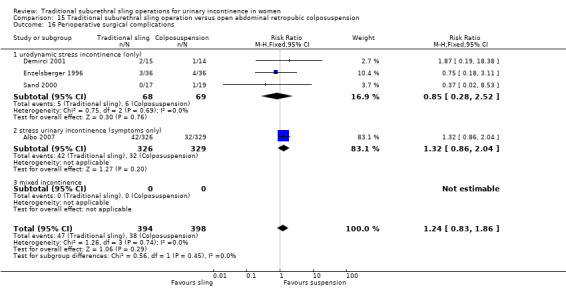
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 16 Perioperative surgical complications.
15.17. Analysis.
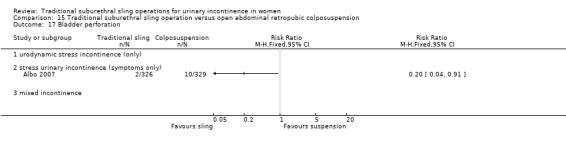
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 17 Bladder perforation.
15.18. Analysis.
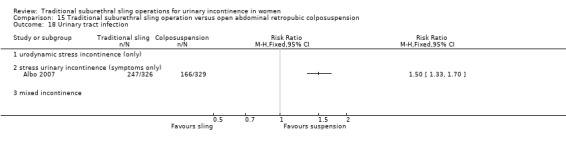
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 18 Urinary tract infection.
15.19. Analysis.
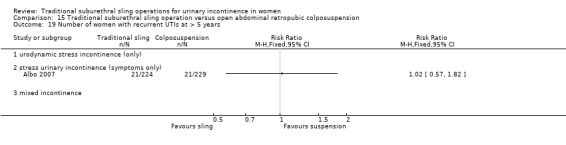
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 19 Number of women with recurrent UTIs at > 5 years.
15.20. Analysis.
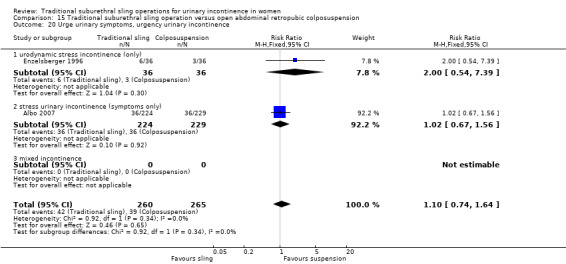
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 20 Urge urinary symptoms, urgency urinary incontinence.
15.21. Analysis.
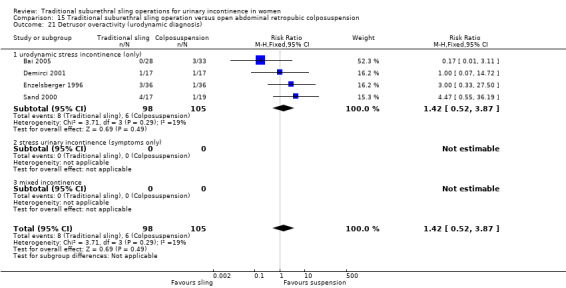
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 21 Detrusor overactivity (urodynamic diagnosis).
15.22. Analysis.
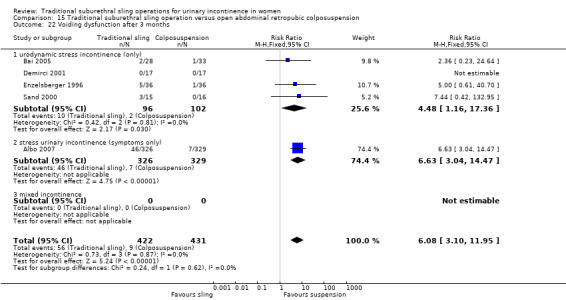
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 22 Voiding dysfunction after 3 months.
15.23. Analysis.
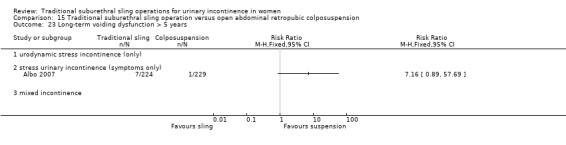
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 23 Long‐term voiding dysfunction > 5 years.
15.24. Analysis.
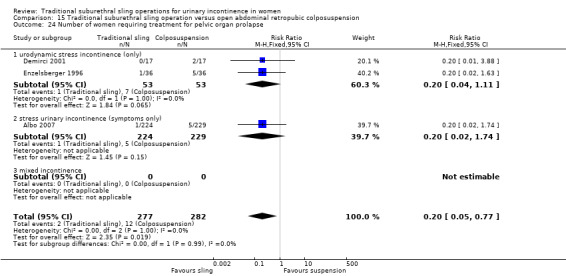
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 24 Number of women requiring treatment for pelvic organ prolapse.
15.25. Analysis.
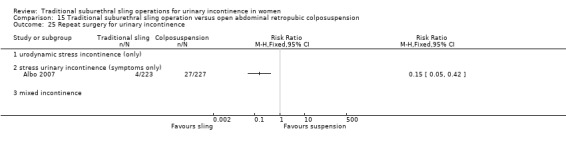
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 25 Repeat surgery for urinary incontinence.
15.26. Analysis.
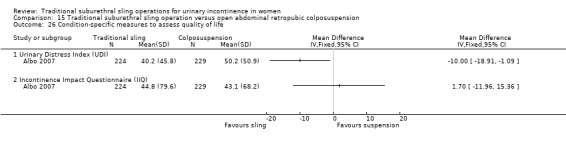
Comparison 15 Traditional suburethral sling operation versus open abdominal retropubic colposuspension, Outcome 26 Condition‐specific measures to assess quality of life.
Comparison 16. Traditional suburethral sling operation versus a mid‐urethral sling or tape.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of women with urinary incontinence (worse, unchanged, or improved) within first year (women's observations) | 11 | 841 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.85, 1.28] |
| 1.1 urodynamic stress incontinence (only) | 5 | 427 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.77, 1.36] |
| 1.2 stress urinary incontinence (symptoms only) | 1 | 53 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.17, 7.37] |
| 1.3 mixed urinary incontinence | 5 | 361 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.78, 1.42] |
| 2 Number not improved (worse or unchanged) within first year (women's observations) | 3 | 425 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.49, 1.29] |
| 2.1 urodynamic stress incontinence (only) | 2 | 286 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.40, 2.21] |
| 2.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 mixed urinary incontinence | 1 | 139 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.40, 1.29] |
| 3 Number of women with urinary incontinence (worse, unchanged, or improved) at 1 to 5 years (women's observations) | 6 | 458 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.98, 1.68] |
| 3.1 urodynamic stress incontinence (only) | 4 | 364 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.87, 1.59] |
| 3.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 mixed urinary incontinence | 2 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.96, 3.31] |
| 4 Number not improved (worse or unchanged) after first year (women's observations) | 2 | 264 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.56, 2.94] |
| 4.1 urodynamic stress incontinence (only) | 2 | 264 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.56, 2.94] |
| 4.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 mixed urinary incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Number of women with urinary incontinence after 5 years (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Number with incontinence not improved after 5 years (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 CURE: number of women cured at > 1 year (women's observations) | 4 | 337 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.65, 1.72] |
| 7.1 urodynamic stress incontinence (only) | 3 | 293 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.72, 2.03] |
| 7.2 stress urinary incontinence (symptoms only) | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 mixed urinary incontinence | 1 | 44 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.10, 1.72] |
| 8 Repeat surgery for urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Number of women not satisfied | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 urodynamic stress incontinence (only) | 2 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.51, 1.32] |
| 9.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.3 mixed urinary incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Pad test of quantified leakage (mean weight of urine loss) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 stress urinary incontinence (symptoms only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 mixed urinary incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Number of women with urinary incontinence (clinician's observations) within first year | 2 | 105 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.45, 3.71] |
| 11.1 urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 mixed urinary incontinence | 2 | 105 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.45, 3.71] |
| 12 Number of women with urinary incontinence (clinician's observations) after first year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 12.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.3 mixed urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Duration of operation (minutes) | 7 | 355 | Mean Difference (IV, Fixed, 95% CI) | 57.08 [54.67, 59.49] |
| 13.1 urodynamic stress incontinence (only) | 2 | 61 | Mean Difference (IV, Fixed, 95% CI) | 46.91 [42.31, 51.52] |
| 13.2 stress urinary incontinence (symptoms only) | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | 20.0 [7.08, 32.92] |
| 13.3 mixed urinary incontinence | 4 | 241 | Mean Difference (IV, Fixed, 95% CI) | 62.96 [60.07, 65.86] |
| 14 Length of hospital stay (days) | 4 | 194 | Mean Difference (IV, Fixed, 95% CI) | 0.74 [0.55, 0.93] |
| 14.1 urodynamic stress incontinence (only) | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | 0.65 [0.39, 0.91] |
| 14.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.3 mixed urinary incontinence | 3 | 174 | Mean Difference (IV, Fixed, 95% CI) | 0.83 [0.56, 1.10] |
| 15 Time to catheter removal (days) | 2 | 113 | Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.07, 0.30] |
| 15.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 stress urinary incontinence (symptoms only) | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | 2.3 [0.01, 4.59] |
| 15.3 mixed urinary incontinence | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.09, 0.29] |
| 16 Perioperative surgical complications | 4 | 293 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.74 [1.16, 2.60] |
| 16.1 urodynamic stress incontinence (only) | 2 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.73 [1.01, 2.96] |
| 16.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16.3 mixed urinary incontinence | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.74 [0.94, 3.21] |
| 17 Bladder perforations | 10 | 844 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.34, 1.01] |
| 17.1 urodynamic stress incontinence (only) | 3 | 334 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.19, 2.86] |
| 17.2 stress urinary incontinence (symptoms only) | 1 | 53 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.05, 5.81] |
| 17.3 mixed urinary incontinence | 6 | 457 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.30, 1.03] |
| 18 Urethral injury | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 18.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.3 mixed urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Vaginal bleeding | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 19.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.3 mixed urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Urinary tract infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 20.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.3 mixed urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 Voiding dysfunction | 8 | 629 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.85, 2.12] |
| 21.1 urodynamic stress incontinence (only) | 3 | 325 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.60, 2.46] |
| 21.2 stress urinary incontinence (symptoms only) | 1 | 53 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.61 [0.76, 9.03] |
| 21.3 mixed urinary incontinence | 4 | 251 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.58, 2.40] |
| 22 De novo detrusor urgency or urge symptoms | 5 | 348 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.62 [0.66, 3.99] |
| 22.1 urodynamic stress incontinence (only) | 1 | 124 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.01, 8.29] |
| 22.2 stress urinary incontinence (symptoms only) | 1 | 53 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.35 [0.14, 78.60] |
| 22.3 mixed urinary incontinence | 3 | 171 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.81 [0.65, 5.06] |
| 23 De novo detrusor overactivity (urodynamic diagnosis) | 4 | 325 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.61 [1.17, 5.84] |
| 23.1 urodynamic stress incontinence (only) | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 23.2 stress urinary incontinence (symptoms only) | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.13 [0.13, 73.01] |
| 23.3 mixed urinary incontinence | 2 | 219 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.57 [1.12, 5.92] |
| 24 Long‐term adverse effects (release of sling required) | 3 | 326 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.53 [0.87, 7.35] |
| 24.1 urodynamic stress incontinence (only) | 2 | 266 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.68 [0.50, 5.66] |
| 24.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 24.3 mixed urinary incontinence | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 9.6 [0.54, 170.84] |
| 25 Long‐term adverse effects (wound pain at 6 months) | 3 | 257 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.40 [1.94, 21.12] |
| 25.1 urodynamic stress incontinence (only) | 1 | 124 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.16 [0.25, 105.36] |
| 25.2 stress urinary incontinence (symptoms only) | 1 | 53 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.92 [0.90, 17.15] |
| 25.3 mixed urinary incontinence | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 17.0 [1.01, 284.96] |
| 26 Long‐term adverse effects (vaginal mesh or graft exposure) | 5 | 348 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.05, 1.65] |
| 26.1 urodynamic stress incontinence (only) | 2 | 165 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.04, 3.24] |
| 26.2 stress urinary incontinence (symptoms only) | 1 | 53 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 26.3 mixed urinary incontinence | 2 | 130 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.97] |
| 27 Condition‐specific measures to assess quality of life: UDI‐6 | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 7.30 [‐2.00, 16.60] |
| 27.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 27.2 stress urinary incontinence (symptoms only) | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 7.30 [‐2.00, 16.60] |
| 27.3 mixed urinary incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Condition‐specific measures to assess quality of life: IIQ‐7 | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐10.17, 11.37] |
| 28.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 28.2 stress urinary incontinence (symptoms only) | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐10.17, 11.37] |
| 28.3 mixed urinary incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
16.1. Analysis.
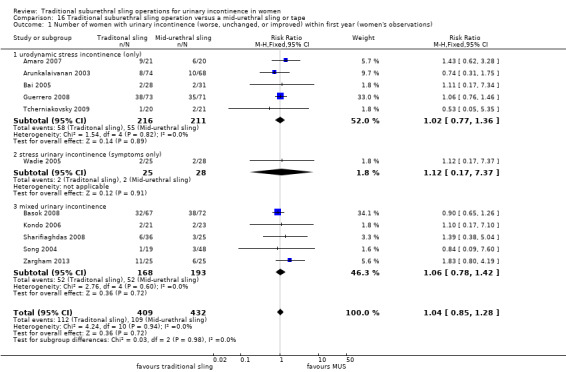
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 1 Number of women with urinary incontinence (worse, unchanged, or improved) within first year (women's observations).
16.2. Analysis.
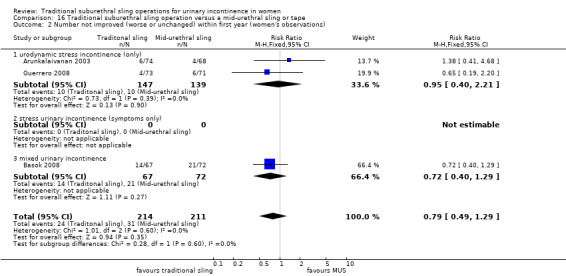
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 2 Number not improved (worse or unchanged) within first year (women's observations).
16.3. Analysis.
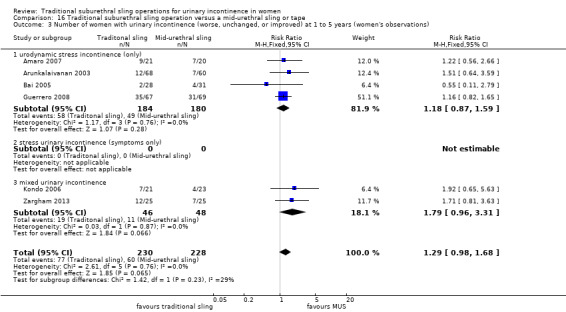
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 3 Number of women with urinary incontinence (worse, unchanged, or improved) at 1 to 5 years (women's observations).
16.4. Analysis.
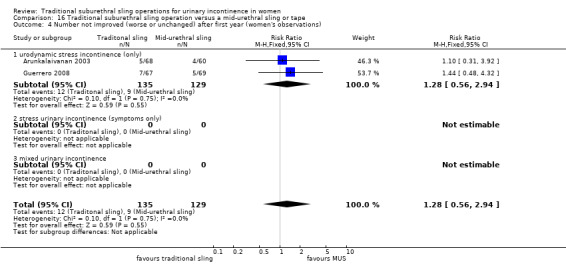
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 4 Number not improved (worse or unchanged) after first year (women's observations).
16.5. Analysis.
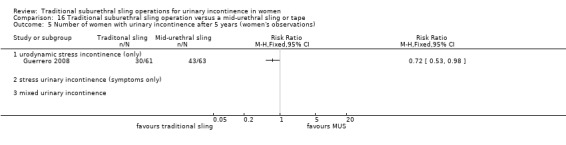
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 5 Number of women with urinary incontinence after 5 years (women's observations).
16.6. Analysis.
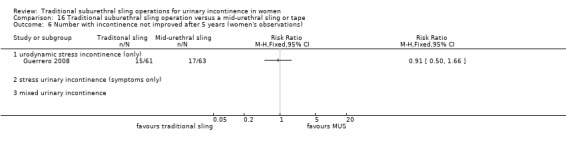
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 6 Number with incontinence not improved after 5 years (women's observations).
16.7. Analysis.
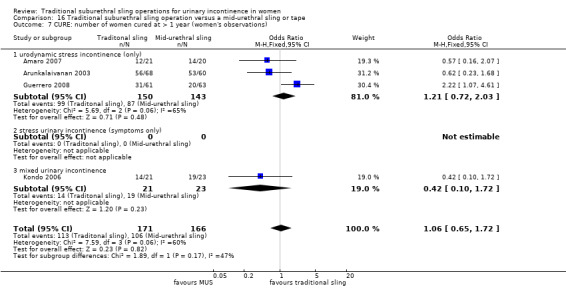
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 7 CURE: number of women cured at > 1 year (women's observations).
16.8. Analysis.
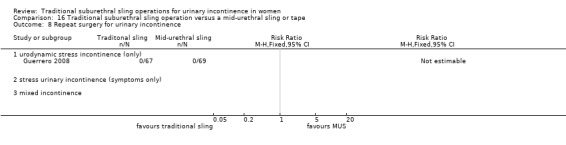
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 8 Repeat surgery for urinary incontinence.
16.9. Analysis.
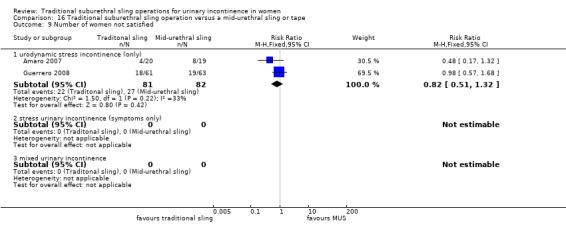
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 9 Number of women not satisfied.
16.10. Analysis.
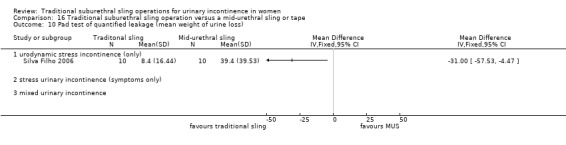
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 10 Pad test of quantified leakage (mean weight of urine loss).
16.11. Analysis.
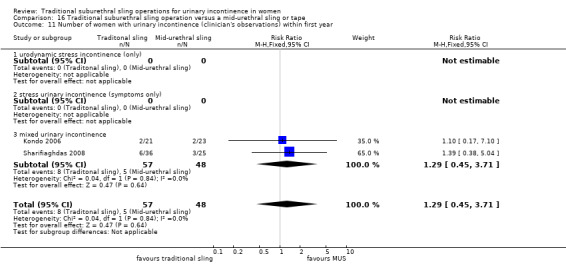
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 11 Number of women with urinary incontinence (clinician's observations) within first year.
16.12. Analysis.
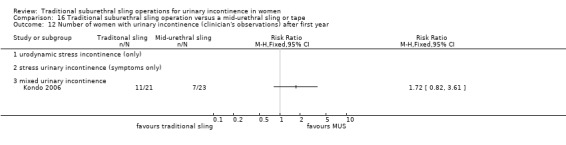
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 12 Number of women with urinary incontinence (clinician's observations) after first year.
16.13. Analysis.
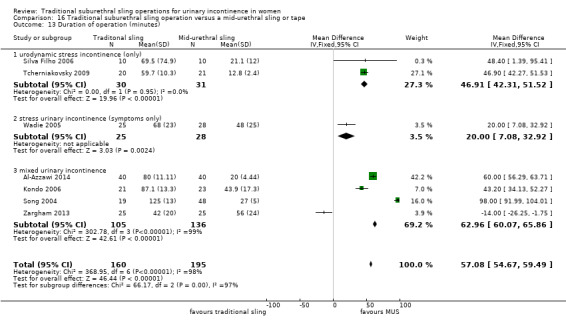
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 13 Duration of operation (minutes).
16.14. Analysis.
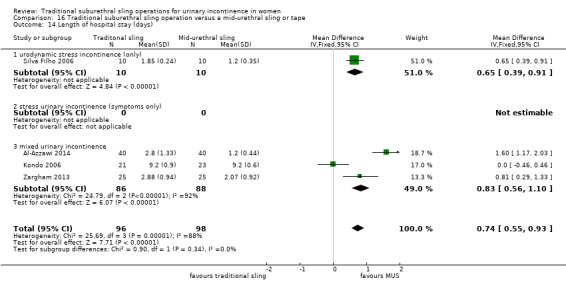
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 14 Length of hospital stay (days).
16.15. Analysis.
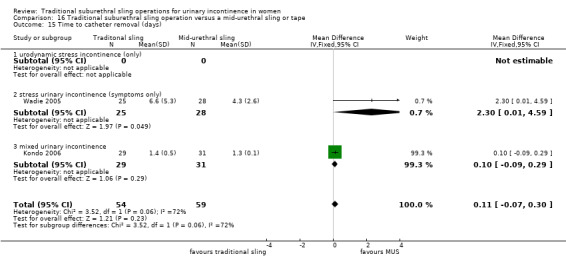
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 15 Time to catheter removal (days).
16.16. Analysis.
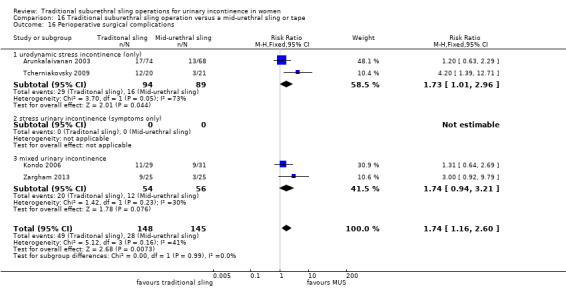
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 16 Perioperative surgical complications.
16.17. Analysis.
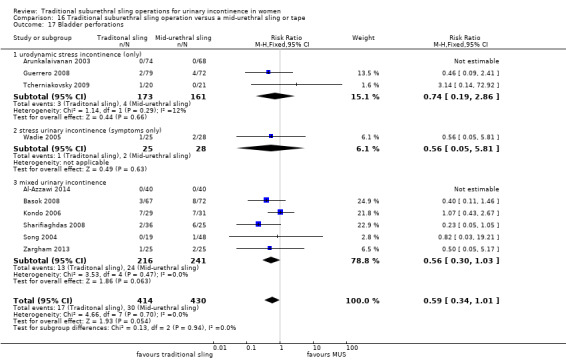
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 17 Bladder perforations.
16.18. Analysis.
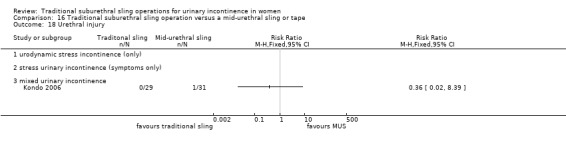
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 18 Urethral injury.
16.19. Analysis.
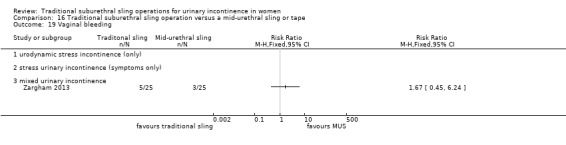
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 19 Vaginal bleeding.
16.20. Analysis.
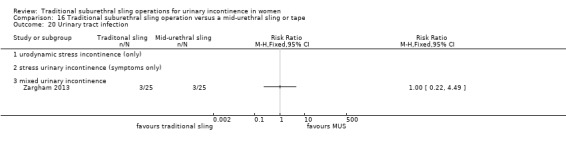
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 20 Urinary tract infection.
16.21. Analysis.
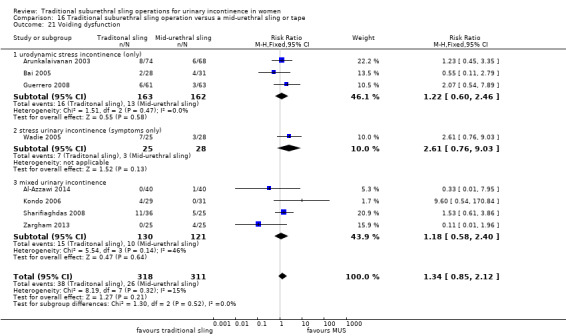
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 21 Voiding dysfunction.
16.22. Analysis.
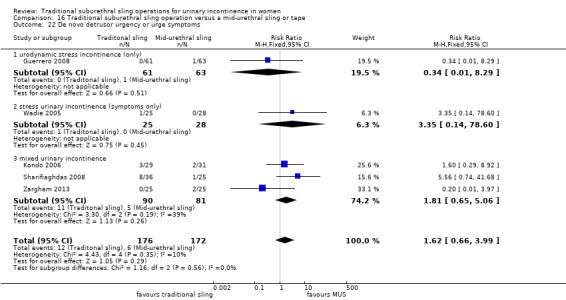
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 22 De novo detrusor urgency or urge symptoms.
16.23. Analysis.
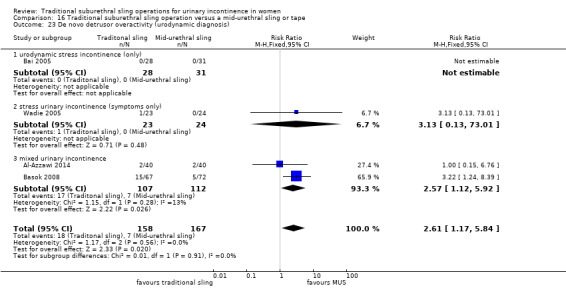
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 23 De novo detrusor overactivity (urodynamic diagnosis).
16.24. Analysis.
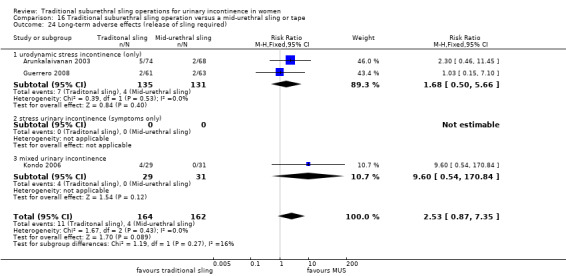
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 24 Long‐term adverse effects (release of sling required).
16.25. Analysis.
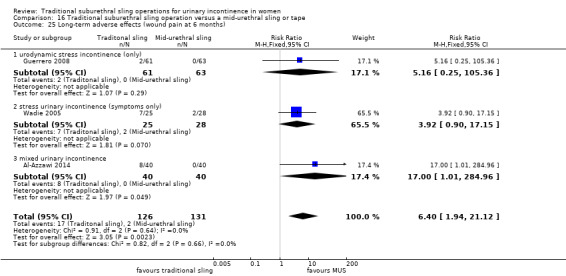
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 25 Long‐term adverse effects (wound pain at 6 months).
16.26. Analysis.
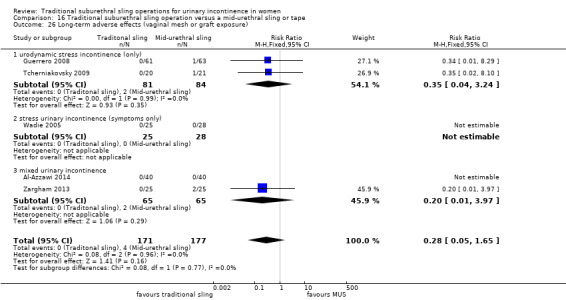
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 26 Long‐term adverse effects (vaginal mesh or graft exposure).
16.27. Analysis.
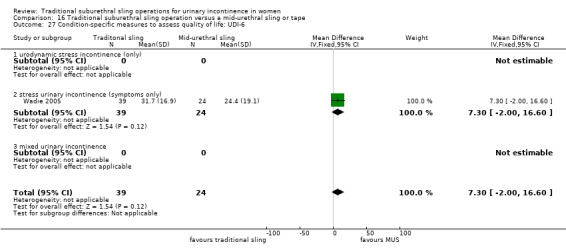
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 27 Condition‐specific measures to assess quality of life: UDI‐6.
16.28. Analysis.
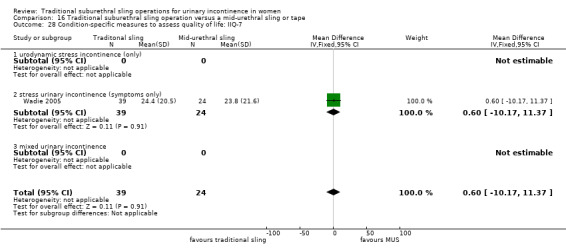
Comparison 16 Traditional suburethral sling operation versus a mid‐urethral sling or tape, Outcome 28 Condition‐specific measures to assess quality of life: IIQ‐7.
Comparison 17. Traditional suburethral sling operation versus a single‐incision sling (mini‐sling).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of women with urinary incontinence in the medium term (1 to 5 years) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number of women not satisfied within first year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Number of women with urinary incontinence (clinician's observations) within first year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 CURE: number of women cured at > 1 year (women's observations) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 urodynamic stress incontinence (only) | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 stress urinary incontinence (symptoms only) | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 mixed incontinence | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Bladder perforation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Urge urinary symptoms, urgency urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Pain with intercourse (dyspareunia) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Long‐term adverse effects (vaginal mesh or graft exposure) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Condition‐specific measures to assess quality of life: IIQ score | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 stress urinary incontinence (symptoms only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 mixed urinary incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
17.1. Analysis.
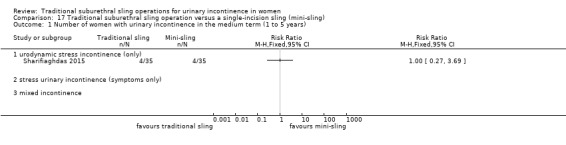
Comparison 17 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 1 Number of women with urinary incontinence in the medium term (1 to 5 years).
17.2. Analysis.
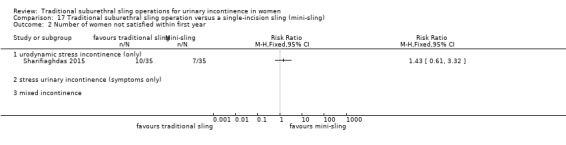
Comparison 17 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 2 Number of women not satisfied within first year.
17.3. Analysis.
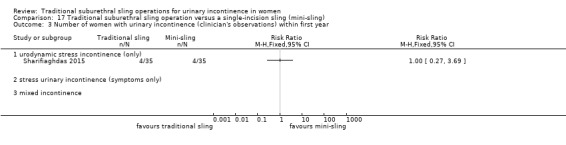
Comparison 17 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 3 Number of women with urinary incontinence (clinician's observations) within first year.
17.4. Analysis.
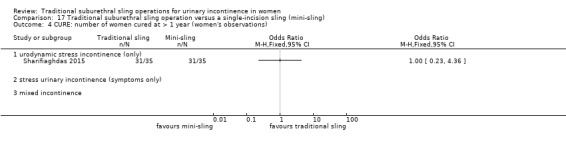
Comparison 17 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 4 CURE: number of women cured at > 1 year (women's observations).
17.5. Analysis.
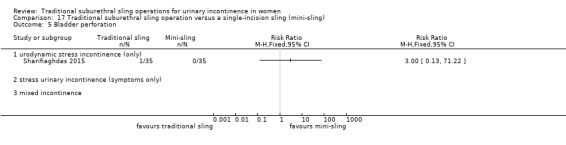
Comparison 17 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 5 Bladder perforation.
17.6. Analysis.
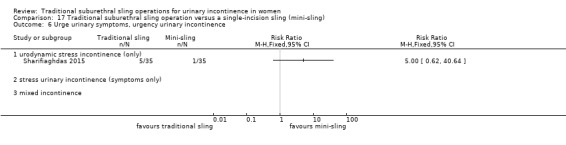
Comparison 17 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 6 Urge urinary symptoms, urgency urinary incontinence.
17.7. Analysis.
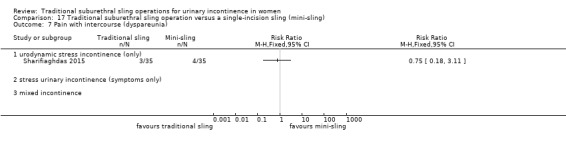
Comparison 17 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 7 Pain with intercourse (dyspareunia).
17.8. Analysis.
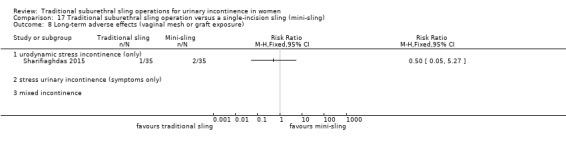
Comparison 17 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 8 Long‐term adverse effects (vaginal mesh or graft exposure).
17.9. Analysis.
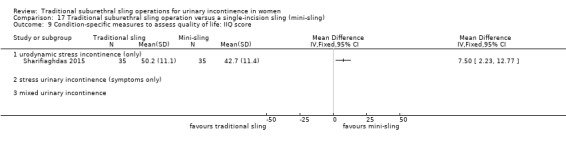
Comparison 17 Traditional suburethral sling operation versus a single‐incision sling (mini‐sling), Outcome 9 Condition‐specific measures to assess quality of life: IIQ score.
Comparison 18. One type of traditional sling operation versus another type of traditional sling operation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of women with urinary incontinence (worse, unchanged, or improved) within first year (women's observations) | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 standard sling vs short sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 autologous fascial sling vs Fortaperm sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Vypro vs Ultrapro | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Vypro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.6 Ultrapro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.7 fascial sling vs vaginal wall sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number not improved (worse or unchanged) within first year (women's observations) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 autologous fascial sling vs Fortaperm sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 rectus fascia sling vs Goretex sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Number of women with urinary incontinence (worse, unchanged, or improved) at 1 to 5 years (women's observations) | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 standard sling vs short sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 autologous dermal graft patch vs cadaveric fascia lata | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 rectus fascia sling vs Goretex sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.5 Vypro vs Ultrapro | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.6 Vypro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.7 Ultrapro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.8 anterior vaginal wall sling vs biosynthetic mesh sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.9 anterior rectus sheath sling vs Prolene strip | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.10 anterior rectus sheath sling vs anterior vaginal wall patch | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.11 Prolene strip vs anterior vaginal wall patch | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Number not improved (worse or unchanged) after first year (women's observations) | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 autologous dermal graft patch vs cadaveric fascia lata | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 rectus fascia sling vs Goretex sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 anterior rectus sheath sling vs Prolene strip | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.5 anterior rectus sheath sling vs anterior vaginal wall patch | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.6 Prolene strip vs anterior vaginal wall patch | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Number of women with urinary incontinence (worse, unchanged, or improved) after 5 years (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 standard sling vs short sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 CURE: number of women with urinary incontinence > 1 year (women's observations) | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 fascial sling vs Pelvicol sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 standard sling vs short sling | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 autologous dermal graft patch vs cadaveric fascia lata | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Number of women not satisfied | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Vypro vs Ultrapro | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 Vypro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.4 Ultrapro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.5 anterior vaginal wall sling vs biosynthetic mesh sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Pad test of quantified leakage (mean weight of urine loss) at 1 year | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 standard sling vs short sling | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Vypro vs Ultrapro | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Vypro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 Ultrapro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Pad test of quantified leakage (mean weight of urine loss) at 1 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 Vypro vs Ultrapro | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Vypro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 Ultrapro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Duration of operation (minutes) | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 standard sling vs short sling | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 anterior rectus sheath sling vs Prolene strip | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 anterior rectus sheath sling vs anterior vaginal wall patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.4 Prolene strip vs anterior vaginal wall patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Blood loss (mL) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1 anterior rectus sheath sling vs Prolene strip | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 anterior rectus sheath sling vs anterior vaginal wall patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.3 Prolene strip vs anterior vaginal wall patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Length of hospital stay (days) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 anterior rectus sheath sling vs Prolene strip | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 anterior rectus sheath sling vs anterior vaginal wall patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.3 Prolene strip vs anterior vaginal wall patch | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Perioperative surgical complications | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 13.1 standard sling vs short sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 rectus fascia sling vs Goretex sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.3 fascial sling vs vaginal wall sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Bladder perforation | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 14.1 standard sling vs short sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.3 anterior rectus sheath sling vs Prolene strip | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.4 anterior rectus sheath sling vs anterior vaginal wall patch | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.5 Prolene strip vs anterior vaginal wall patch | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Urinary tract infection | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 15.1 standard sling vs short sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 anterior vaginal wall sling vs biosynthetic mesh sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Vaginal bleeding | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 16.1 anterior vaginal wall sling vs biosynthetic mesh sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Long‐term adverse effects (wound pain) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 17.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Voiding dysfunction | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 18.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 standard sling vs short sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.3 Vypro vs Ultrapro | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.4 Vypro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.5 Ultrapro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.6 anterior vaginal wall sling vs biosynthetic mesh sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.7 anterior rectus sheath sling vs Prolene strip | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.8 anterior rectus sheath sling vs anterior vaginal wall patch | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.9 Prolene strip vs anterior vaginal wall patch | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.10 fascial sling vs vaginal wall sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Long‐term adverse effects (release of sling required) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 19.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 De novo detrusor urgency or urge symptoms or detrusor overactivity | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 20.1 standard sling vs short sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.2 Vypro vs Ultrapro | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.3 Vypro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.4 Ultrapro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.5 autologous dermal graft patch vs cadaveric fascia lata | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.6 rectus fascia sling vs Goretex sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 Repeat surgery for urinary incontinence at first year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 21.1 Fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22 Long‐term adverse effects (vaginal mesh or graft exposure) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 22.1 fascial sling vs Pelvicol sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22.2 Vypro vs Ultrapro | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22.3 Vypro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22.4 Ultrapro vs Prolene light | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22.5 anterior vaginal wall sling vs biosynthetic mesh sling | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23 Condition‐specific measures to assess quality of life (ICI‐Q short form UI score at 1 year) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 23.1 Vypro vs Ultrapro | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.2 Vypro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.3 Ultrapro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24 Condition‐specific measures to assess quality of life (ICI‐Q short form UI score at 1 to 5 years) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 24.1 Vypro vs Ultrapro | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.2 Vypro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.3 Ultrapro vs Prolene light | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
18.1. Analysis.
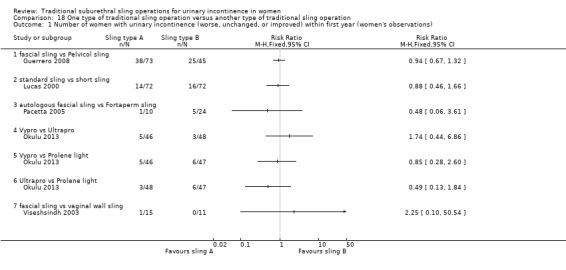
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 1 Number of women with urinary incontinence (worse, unchanged, or improved) within first year (women's observations).
18.2. Analysis.
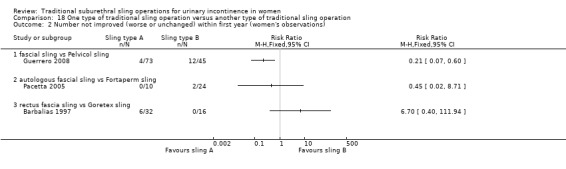
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 2 Number not improved (worse or unchanged) within first year (women's observations).
18.3. Analysis.
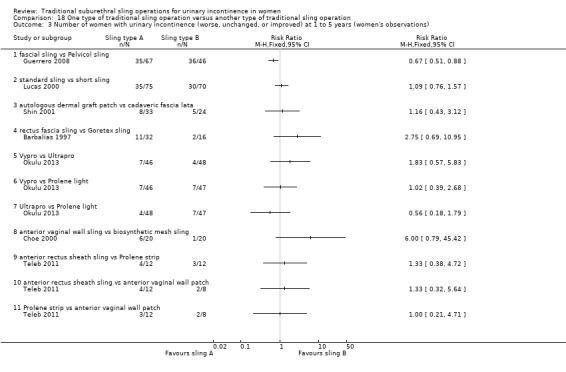
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 3 Number of women with urinary incontinence (worse, unchanged, or improved) at 1 to 5 years (women's observations).
18.4. Analysis.
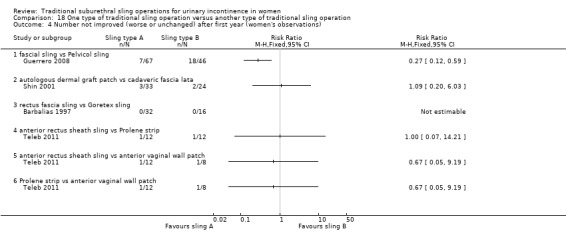
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 4 Number not improved (worse or unchanged) after first year (women's observations).
18.5. Analysis.
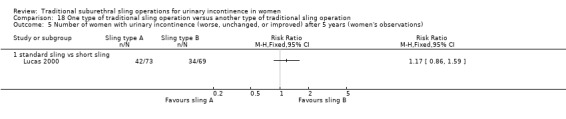
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 5 Number of women with urinary incontinence (worse, unchanged, or improved) after 5 years (women's observations).
18.6. Analysis.
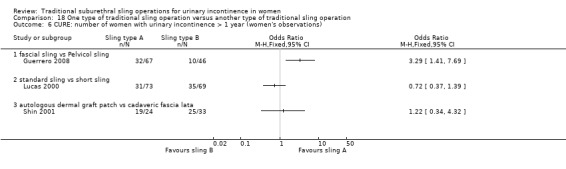
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 6 CURE: number of women with urinary incontinence > 1 year (women's observations).
18.7. Analysis.
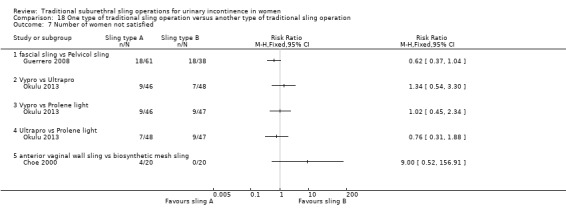
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 7 Number of women not satisfied.
18.8. Analysis.
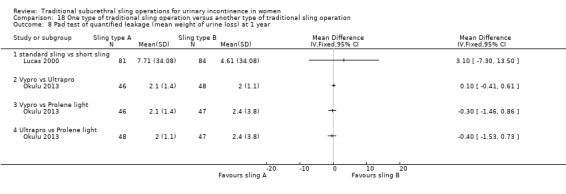
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 8 Pad test of quantified leakage (mean weight of urine loss) at 1 year.
18.9. Analysis.
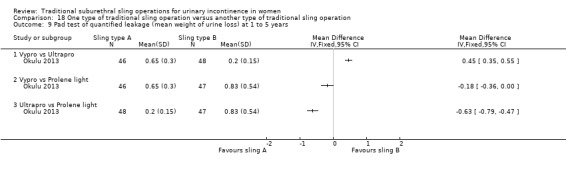
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 9 Pad test of quantified leakage (mean weight of urine loss) at 1 to 5 years.
18.10. Analysis.
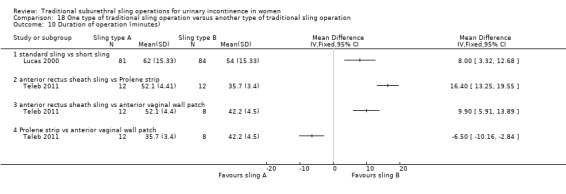
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 10 Duration of operation (minutes).
18.11. Analysis.
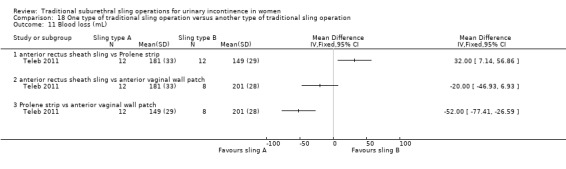
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 11 Blood loss (mL).
18.12. Analysis.
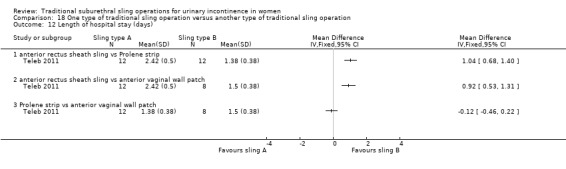
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 12 Length of hospital stay (days).
18.13. Analysis.
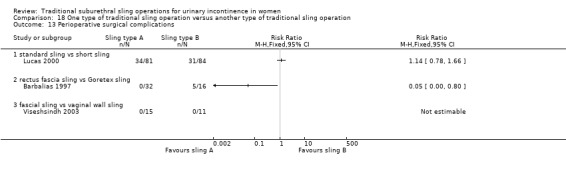
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 13 Perioperative surgical complications.
18.14. Analysis.
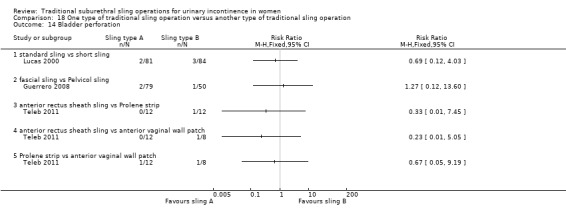
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 14 Bladder perforation.
18.15. Analysis.
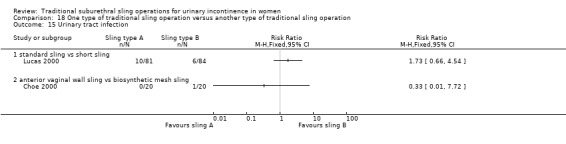
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 15 Urinary tract infection.
18.16. Analysis.
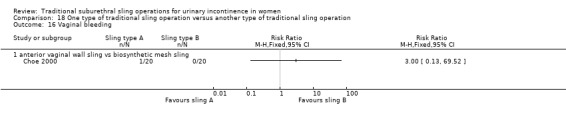
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 16 Vaginal bleeding.
18.17. Analysis.
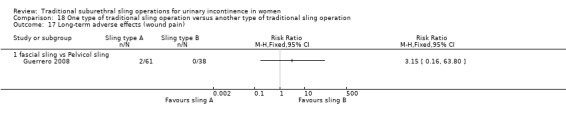
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 17 Long‐term adverse effects (wound pain).
18.18. Analysis.
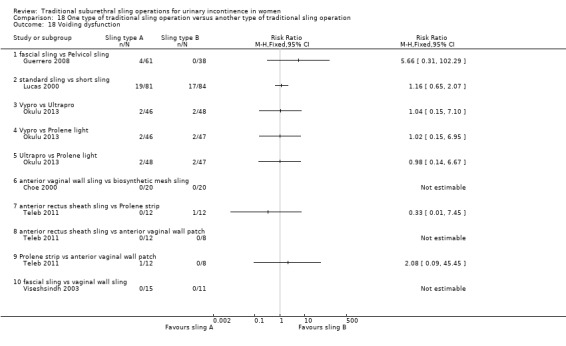
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 18 Voiding dysfunction.
18.19. Analysis.
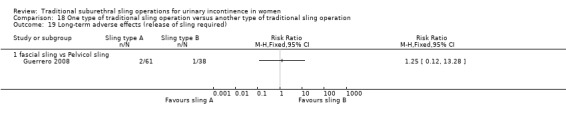
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 19 Long‐term adverse effects (release of sling required).
18.20. Analysis.
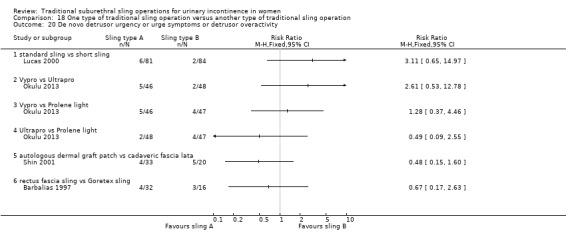
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 20 De novo detrusor urgency or urge symptoms or detrusor overactivity.
18.21. Analysis.
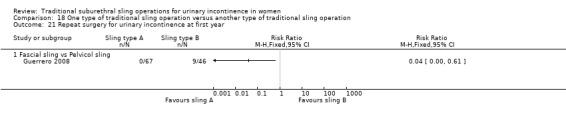
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 21 Repeat surgery for urinary incontinence at first year.
18.22. Analysis.
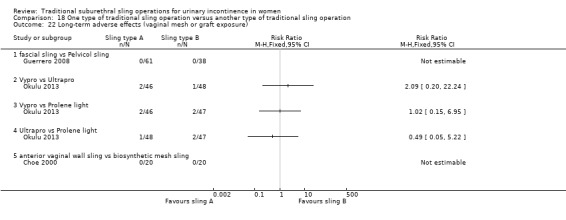
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 22 Long‐term adverse effects (vaginal mesh or graft exposure).
18.23. Analysis.
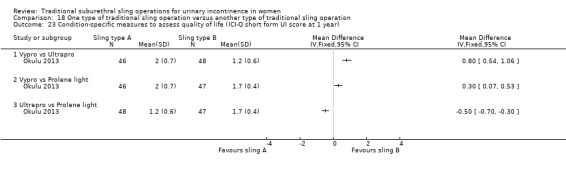
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 23 Condition‐specific measures to assess quality of life (ICI‐Q short form UI score at 1 year).
18.24. Analysis.
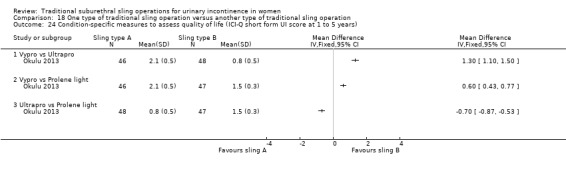
Comparison 18 One type of traditional sling operation versus another type of traditional sling operation, Outcome 24 Condition‐specific measures to assess quality of life (ICI‐Q short form UI score at 1 to 5 years).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abouhashem 2014.
| Methods | Design: RCT | |
| Participants | 56 consecutive women with SUI. Patients followed up for 5 years; 48/56 completed evaluation | |
| Interventions | A: TVT B: rectus sheath sling |
|
| Outcomes | Cure defined as no leakage of urine during stress test and urodynamic testing (clinician‐reported) A: 88.5% B: 84.6% Denominators for individual groups not provided |
|
| Notes | Abstract only; no useable data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Al‐Azzawi 2014.
| Methods | Design: RCT Setting: hospital in Iraq |
|
| Participants | N = 80 Women with main complaint of SUI (mixed group); BMI < 30 kg/m² Exclusion: mild UI (defined as 0 to 1 pad per day; a few drops of urine leaked on stress); cystocoele (anterior prolapse) > grade 1; active vaginal infection or UTI; neurogenic voiding dysfunction; significant postvoid residual urine volume (PVR); other bladder or urethral pathology or fistula Recruitment: December 4 to July 12 Follow‐up: 1 week; 1, 3, 6, and 12 months; yearly thereafter |
|
| Interventions | A (40): autologous rectus fascia sling B (40): transobturator mid‐urethral sling (TOT), synthetic polypropylene tape Cystoscopy at time of surgery to exclude other pathology before surgery and to check for injury after insertion of sling or tape |
|
| Outcomes | Cure of SUI defined as significant dryness as perceived by the patient, no more use of pads, negative stress test, and acceptable voiding stream (combined primary outcome) Cure at 1 week: A: 39/40; B: 38/40 No further data provided for cure at later follow‐up, but trialists state, "there were no significant changes in the continence achieved throughout the follow‐up period" Operation time (mean minutes (SD) N): A: 80 (11.11) 40, B: 20 (4.44) 40 Hospital stay (mean days (SD) N): A: 2.8 (1.33) 40, B: 1.2 (0.44) 40 Adverse effects: Intraoperative visceral injury (bladder perforation): A: 0/40, B: 0/40 Vaginal or urethral erosion: A: 0/40, B: 0/40 De novo detrusor overactivity: A: 2/40, B: 2/40 Other adverse effects: Abdominal wound problems, pain, ooze, haematoma, infection: A: 8, B: 0 Foot drop: A: 1, B: 0 Groin and upper thigh pain: A: 0, B: 5 Voiding difficulty: A: 0, B: 1 Vaginal bleeding: A: 0, B: 1 Late PVR (postvoid residual): A: 3, B: 2 Total other adverse effects: A: 12/40, B: 9/40 All complications described as "marginal, treated conservatively and comparable with other studies" Further treatment required for urinary urgency with anti‐muscarinic drugs: A: 3/40, B: 3/40 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised using random numbers table but with no details on method of generation |
| Allocation concealment (selection bias) | Unclear risk | "were assigned randomly" – too little detail for assessment |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information but full follow‐up of all 80 women assumed |
Albo 2007.
| Methods | Design: RCT by electronic treatment assignment; 2 arms; unblinded. Setting: multi‐centre; tertiary referral centres; USA Follow‐up at 24 months; analysis with intention‐to‐treat SISTER trial |
|
| Participants | N = 655
4 ineligible after randomisation (3 Burch, 1 sling); 1 did not undergo allocated treatment. Only 520 assessed at end of trial (255 Burch, 265 sling) Symptom‐based diagnosis of SUI, confirmed by standard stress test. A few women had DO at baseline as well (A: 16/243, B: 25/239) (MUI), but we have classified the trial as in women with predominant SUI Inclusion: documented pure or predominant symptom of SUI for ≥ 3 months, positive standardised urinary stress test Exclusion: age < 21 years, non‐ambulatory status, pregnancy, current cancer chemotherapy or radiotherapy, systemic disease affecting bladder function, urethral diverticulum, prior augmentation cystoplasty or artificial urethral sphincter, recent pelvic surgery Groups similar in age, ethnic group, marital status, BMI, vaginal deliveries, hormone treatment, smoking, mixed UI, POP, UDS, concomitant surgery |
|
| Interventions | A (326): sling B (329): Burch Burch as modified by Tanagho Sling procedure using autologous rectus fascia at level of the bladder neck and proximal urethra Interventions standardised across centres |
|
| Outcomes | Number with overall success, number with SUI‐specific success, pad test, number of incontinence episodes in a 3‐day voiding diary, POP, adverse events, voiding dysfunction (use of a catheter), postoperative UUI Overall success defined as no self‐reported symptoms of UI, no incontinence on 3‐day diary, negative stress test, no re‐treatment SUI‐specific success defined as no symptoms, negative stress test, and no re‐treatment for SUI (combined outcome) All outcomes reported at 2 years' follow‐up Failure (composite symptoms, self‐report of UI or on diary, or surgical re‐treatment) at 24 months: A: 101/265, B: 130/255 (used as surrogate for subjective UI) Failure (pad test, objective) at 24 months: A: 37/265, B: 38/255 Complications at 24 months: Number of women with any complications: A: 206/326, B: 156/329 Number of women with serious adverse events: A: 42/326, B: 32/329 Number of women with bleeding: A: 8/326, B: 5/329 Number of women with any voiding dysfunction: A: 46/326, B: 7/329 Number of women with voiding dysfunction requiring surgical revision: A: 20/326, B: 0/329 Postoperative cystitis (UTI): A: 247/326, B: 166/329 Bladder perforation: A: 2/326, B: 10/329 5‐year outcomes (Brubaker 2012): Enrolled 482 women: A: 243, B: 239 5‐year FU completed by A: 183, B: 174, but data from more women reported for different outcomes Failure (self‐reported UI) at 5 years: A: 130/224, B: 158/229 (woman‐reported) Composite failure rate (self‐report of UI or on diary, or surgical re‐treatment): A: 153/221, B: 161/212 Surgical re‐treatment for UI: A: 4/223, B: 27/227 Prolapse treatment: A: 1/224, B: 5/229 Not satisfied: A: 31/182, B: 46/170 UDI score (mean (SD) N): A: 40.2 (45.8) 224, B: 50.2 (50.9) 229 IIQ score (mean (SD) N): A: 44.8 (79.6) 224, B: 43.1 (68.2) 229 Adverse events (number): A: 37/224, B: 38/229 Adverse events (number of women): A: 22/224, B: 23/229 Number of women with UTI (included in AE above): A: 21/224, B: 21/229 Urgency urinary incontinence (new or persistent): A: 36/224, B: 36/229 Voiding dysfunction: A: 7/224, B: 1/229 |
|
| Notes | Full text with several other reports in full text and abstract form 5‐year data published in 2012 For some outcomes, denominator assumed to be those who supplied subjective information about continence status |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Use of permuted block randomisation schedule with stratification according to clinical site |
| Allocation concealment (selection bias) | Low risk | Randomisation was performed in the operating room after anaesthesia induction |
| Blinding (performance bias and detection bias) All outcomes | High risk | Patients were aware of study group assignments postoperatively. Independent data and safety monitoring board oversaw progress, interim results, and safety of the study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 135 women were lost to follow‐up at 2 years: 61 from the sling group and 74 from Burch failed to attend clinic. At 5 years, 243 and 239 women were followed up To allow for attrition and missed visits, 655 women had been recruited following power calculation |
Amaro 2007.
| Methods | Design: RCT of autologous fascial sling with TVT; single‐blind Follow‐up assessment carried out at 1, 6, 12, and 36 months |
|
| Participants | Women with involuntary detrusor contractions or pre‐existing bladder outlet obstruction (BOO) during urodynamic study were excluded (USI) | |
| Interventions | A (21): autologous fascial sling B (20): TVT |
|
| Outcomes | Cure rates (defined as complete dryness with no usage of pads (woman‐reported)), operative room time, postoperative analgesia, complications, time of hospital stay, postoperative catheterisation, time to return to normal activities. 60‐minute pad test was used and QoL was evaluated with a validated Portuguese version of King's Health Questionnaire Incontinent at 6 months: A: 9/21, B: 6/20 Incontinent at 12 months: A: 9/21, B: 7/20 Mean operative time (minutes): A: 70, B: 33 Mean dosage of analgesia (milligrams): A: 142, B: 85 Bladder injuries: A: 1, B: 2 Mean hospital stay (hours): A: 24, B: 24 Mean postoperative catheterisation (hours): A: 24, B: 24 Time to return to normal activity (days): A: 30, B: 30 36‐month outcomes: 1 patient died in each group: A: 1/21, B: 1/20 Satisfaction rates at 36 months: dissatisfied: A: 4/20, B: 8/19 QoL on King’s Health Questionnaire at 36 months: Domain of KHQ (median) General health score: A: 50, B: 50 Incontinence impact score: A: 33.34, B: 0 Role limitation score: A: 0, B: 0 Physical limitation score: A: 0, B: 0 Social limitation score: A: 5.56, B: 0 Personal relationship score: A: 0, B: 0 Emotions score: A: 0, B: 0 Sleep score: A: 25, B: 0 Severity perception of UI: A: 16.67, B: 26.57 De novo urgency at 36 months: A: 8/20, B: 8/19 |
|
| Notes | Abstract and poster, 36‐month outcome paper | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation followed a blind raffle where procedures (TVT and sling) were written on small pieces of paper, which were folded and placed into a closed box |
| Allocation concealment (selection bias) | Low risk | The box was opened just before surgery, when the medical team found out which procedure would be performed |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | "Single‐blinded" mentioned in abstract, but no description given |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All outcome data assessed; no women lost to follow‐up |
Arunkalaivanan 2003.
| Methods | Design: RCT; randomisation method unclear. Patient demographics were well reported. Procedures were standardised Follow‐up at 2 to 6 months, 12 months, and 24 months (median 12 months) |
|
| Participants | 142 women with urodynamically proven SUI were recruited. Women with detrusor instability were excluded. Groups were comparable | |
| Interventions | A (74): Pelvicol B (68): TVT |
|
| Outcomes | Outcome measures: cure of incontinence was defined as quality of life (QoL) improvement of 90% and/or patient‐determined continent status as dry (woman‐reported) (subjective, questionnaire‐based; pad used ‐ not weighed), levels of morbidity and impact on quality of life, and symptom severity Failure at 12 months (incontinence): A: 8/74, B: 10/68 Not improved at 12 months: A: 6/74, B: 4/68 Failure at 36 months (incontinence): A: 12/68, B: 7/60 Not improved at 36 months: A: 5/68, B: 4/60 Complications: any complications: A: 17/74, B: 13/68; any voiding dysfunction: A: 8/74, B: 6/68; retention up to 6 weeks A: 6/74, B: 1/68; release of sling required A: 5/74, B: 2/68; bladder perforations: A: 0/74, B: 0/68 |
|
| Notes | Surgery was offered only after conservative therapy had proved unsuccessful | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No patients lost to follow‐up at 12 months. All outcome data assessed. At 36 months, in the Pelvicol arm, 2 patients died and 4 were lost to follow‐up; in the TVT arm, 1 died and 7 were lost to follow‐up. Statistical analysis failed to detect significant differences |
Bai 2005.
| Methods | Design: RCT. Method not described; 3 arms; blinding not mentioned Setting: Ob&Gyne; South Korea Unclear if intention‐to‐treat Follow‐up at 1 year with assessments at 3, 6, and 9 months |
|
| Participants | Urodynamics confirmed; no mixed incontinence Groups comparable as to age, parity, BMI, menopausal status, MUCP, VLPP, functional urethral length, and peak flow rates at baseline Inclusion: USI grades 1 and 2 Exclusion: grade III incontinence, detrusor overactivity, UTI, ISD, POP > grade II |
|
| Interventions | A (28): sling
B (33): Burch
C (31): TVT Sling procedure used a pubovaginal sling with autologous rectus muscle fascia |
|
| Outcomes | Number cured (3, 6, 12 months); complication rate (number with idiopathic detrusor overactivity, hesitancy, urinary retention) Cure defined as absence of subjective complaints of leakage and absence of urinary leakage on stress test Not cured (6 months): A: 2/28, B: 3/33, C: 2/31 Not cured (12 months): A: 2/28, B: 4/33, C: 4/31 De novo detrusor overactivity: A: 0/28, B: 3/33, C: 0/31 Voiding dysfunction: A: 2/28, B: 1/33, C: 4/31 |
|
| Notes | TVT technique according to Ulmsten All procedures performed by 1 surgeon |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
Barbalias 1997.
| Methods | Design: RCT Follow‐up at 6 months and 30 months; all women available at follow‐up Women allocated to 1 of 2 interventions by a computer‐generated random numbers table at a 2:1 ratio |
|
| Participants | 48 consecutive women. Inclusion and exclusion criteria not clearly stated, but some patients with mixed incontinence | |
| Interventions | A (32): rectus fascia sling B (16): Goretex sling operation |
|
| Outcomes | Cure defined as complete freedom from SUI (clinician‐assessed) or improved (persistence or recurrence of SUI, but at lesser intensity) Failure rates at 6 months: A: 6/32, B: 2/16 Failure rates at 30 months: A:11/32, B: 2/16 Complications: B: 2 cases of erosion of sling and 3 other cases of recurrent UTI |
|
| Notes | Pre‐operative characteristics reported but no comparisons between groups made; statistical analysis reported for urodynamic parameters before and after operation. No other statistical comparison between groups reported. Some patients with mixed incontinence, but results not stratified by group or by type of incontinence | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐randomised numbers, assigning 2 successive numbers to the fascial group and the following number to the Goretex group |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
Basok 2008.
| Methods | Design: RCT. Details of randomisation not given; 2 arms Follow‐up: 12 months |
|
| Participants | 139 women randomised. Baseline comparisons made: number of patients, mean age (years), mean daily pad usage, mean parturition, mean BMI, mixed urinary incontinence. No statistical differences Inclusion criteria: stress urinary incontinence due to urethral hypermobility Exclusion criteria: patients with ISD, uterine prolapsed, rectocoele, enterocoele, grade III or IV cystocoele Concomitant urgency urinary incontinence was present in some women; mixed urinary incontinence was present in 49 patients (73%) in the fascia lata sling group and in 44 patients (61%) in the intravaginal slingplasty group |
|
| Interventions | A (67): cadaveric fascia lata B (72): intravaginal slingplasty |
|
| Outcomes | Objective cure rate was evaluated by the pad test, and patient satisfaction rate was assessed by a subjective questionnaire. Cure and improvement were defined as a totally dry patient and 1 pad/d, respectively. Usage of more than 1 pad/d was accepted as surgical failure. The sum of cure and improvement rates was conceded as a total success rate Other outcomes measured were mean operating time, bladder perforation, urinary retention, erosion, sling revision, haematoma, persistent urgency urinary incontinence, defective vaginal wall, de novo detrusor overactivity Total success: A: 79.0%, B: 70.8% Satisfaction at 12 months: A: 82.0%, B: 87.5% Incontinence at 12 months: A: 32/67, B: 38/72 Not improved at 12 months: A: 14/67, B: 21/72 Daily mean pad usage (SD): A: 4.1 (3.5), B: 2.9 (1.7) Operative time: A: 50 minutes, B: 25 minutes Adverse events: de novo detrusor overactivity: A: 15/67, B: 5/72; bladder perforation: A: 3/67, B: 8/72; urinary retention: A: 8/67, B: 8/72; vaginal erosion: A: 0/67, B: 0/72; sling revision: A: 2/67, B: 0/72 |
|
| Notes | Pre‐operative evaluation of all patients included urogynaecological history, previous pelvic surgery, voiding diary, parturition, and daily pad usage Abstract indicated that QoL was significantly improved in the study; full article showed that measurement was carried out by patient satisfaction questionnaire. No comment was made on validity or reliability of this questionnaire |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
Choe 2000.
| Methods | Design: quasi‐RCT. Patients randomised in alternate fashion to mesh or vaginal wall group Mean follow‐up: 22 months (12 to 27 months) |
|
| Participants | 40 women with stress or mixed urinary incontinence and vaginal prolapse underwent implantation of transvaginal sling and vaginal reconstruction from 1997 to 1998 Pre‐operative investigations included urodynamic studies, cystoscopy, cough‐stress test, cotton swab test, and detailed pelvic examination with patients supine and standing Groups were not significantly different with respect to mean age, parity, weight, and pre‐operative pad use, although the biosynthetic mesh group was younger and heavier. Of the entire cohort, 65% of mesh and 86% of vaginal graft groups had undergone previous vaginal operations (P > 0.05) Concomitant prolapse: A: 14/20 (70%), B: 18/20 (90%) |
|
| Interventions | A (20): antimicrobial MycroMesh (1‐mm polytetrafluoroethylene mesh patch impregnated with silver diacetate and chlorhexidine (biosynthetic mesh); average patch size 3.5 × 1.5 cm B (20): autologous vaginal wall sling using a free patch of vaginal skin (biological graft) soaked in antibiotic until ready for use Single transverse suprapubic abdominal incision and polytetrafluoroethylene sutures attached to mesh or graft edges and secured abdominally by tying down across midline anterior to the rectus fascia Concomitant surgery: None: A: 6/20, B: 2/20 Cystocoele repair: A: 6/20, B: 8/20 Cystocoele and rectocoele repair: A: 3/20, B: 6/20 Cystocoele and rectocoele repair + enterocoele or sacrospinous fixation: A: 3/20, B: 2/20 Hysterectomy: A: 2/20, B: 2/20 |
|
| Outcomes | Routine follow‐up with cough‐stress test, cotton swab test, and voiding trial was performed on postoperative day 7 Urine loss during cough‐stress test was defined as persistent (objective) stress incontinence: clinician‐reported Additional follow‐up was done at 1, 3, and every 6 months. At each follow‐up visit, cough‐stress test and cotton swab test were performed at speculum examination to detect recurrent stress incontinence and vaginal wall prolapse Stress incontinence was considered cured if objective loss of urine was not demonstrated and patients did not report involuntary loss of urine during physical activity (combined outcome) Mean time to suprapubic tube removal, days (range): A: 9 (1 to 21); B: 10 (1 to 35) Mean postvoid residual volume, millilitres (range): A: 13 (0 to 60); B: 14 (0 to 50) Mean time to resumption of normal activity in weeks (range): both groups 3.5 weeks (2 to 4 weeks) Postoperative early complications: Blocked suprapubic tube: A: 3/20; B: 0/20 Abdominal wound infection: A: 4/20, B: 2/20 Urinary tract infection: A: 1/20, B: 0/20 Bleeding (intraoperative blood transfusion): A: 0/20, B: 1/20 Vaginitis: A: 1/20, B: 1/20 Transient de novo urgency incontinence resolved after 3 months: A: 1/8, B: 1/7 Late complications: Urethral erosion: A: 0/20, B: 0/20 Voiding dysfunction (‘urethral obstruction’): A: 0/20, B: 0/20 Resolution of pre‐operative urgency incontinence: A: 8/12, B: 7/13 Recurrent stress incontinence: A: 1/20, B: 6/20 Postoperative satisfaction: Dissatisfied (same or worse symptoms): A: 0/20, B: 4/20 (due to recurrent stress incontinence and recurrent prolapse (cystocoele)) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomised in alternate fashion |
| Allocation concealment (selection bias) | High risk | Randomised in alternate fashion |
| Blinding (performance bias and detection bias) All outcomes | High risk | Women in the mesh arm (A) signed a consent form stating that they were receiving a biosynthetic material |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts reported |
Demirci 2001.
| Methods | Design: RCT. No details of allocation method given Follow‐up at 12 months. Not all women available for follow‐up |
|
| Participants | 46 women recruited, 23 in each arm of the study. 34 women available for follow‐up; reasons for loss to follow‐up not reported. Inclusion and exclusion criteria well defined | |
| Interventions | A (23): rectus fascia sling B (23): Burch colposuspension |
|
| Outcomes | Cure defined as dry, symptom‐free (subjective based on history and objective on ultrasonography to assess bladder neck mobility) Failure rate (‘surgical’ – assume objective clinician‐reported at 1 year): A: 0/17, B: 1/17 Dry (symptom‐free patients at 1 year; assume woman‐reported): A: 16/17, B: 15/17 Operating time (mean minutes (SD) N): A: 60.66 (8.63) 15, B: 54.64 (9.29) 14 (women having concomitant hysterectomy excluded) Length of hospital stay (mean days (SD) N): A: 5.93 (1.38) 15, B: 5.42 (1.28) 14 (women having concomitant hysterectomy excluded) UTI: A: 1/15, B: 2/14 Late complications (1‐year follow‐up): A: 1 detrusor instability, 3 suprapubic pain, 1 dyspareunia B: 1 detrusor instability, 2 dyspareunia, 2 genital prolapse (1 cystocoele, 1 enterocoele) |
|
| Notes | Ultrasonography for measurement of bladder neck mobility was tested in both groups pre‐operatively and postoperatively, showing significant improvement but no significant differences between groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 12 women missing and lost to follow‐up; reason not reported. No mention of whether loss had impact on final analysis |
Enzelsberger 1996.
| Methods | Design: RCT. Women allocated to 1 of 2 interventions by open random numbers chart Follow‐up at 32 to 48 months; all women available for follow‐up |
|
| Participants | 72 women recruited, 36 in each arm of the study Inclusion criteria: all patients with GSI (urodynamic and sonographic diagnosis) had a vaginal hysterectomy and at least 1 previous anterior repair; 57 were postmenopausal without hormone replacement therapy Exclusion criteria: urinary tract infection, unstable bladder, voiding difficulty and severe cystocoele and/or rectocoele. Groups were comparable for age, weight, parity, menopausal status, previous surgery, and time of follow‐up |
|
| Interventions | A (36) group II: lyophilised dura mater sling operation B (36) group I: modified Burch colposuspension (2 pairs of sutures instead of 3) |
|
| Outcomes | Cure defined as dry, symptom‐free without objective urine loss during stress with bladder filled to 300 mL or positive urethral closure pressure during stress provocation Failure rate at follow‐up at 32 to 48 months: A: 3/36, B: 5/36 Urodynamic results reported before and at follow‐up: reported longer hospital stay and suprapubic catheter permanence for A. Equal frequency pyrexia and bladder laceration Late complications: Enterocoele or rectocoele: A: 1/36, B: 5/36 Voiding difficulty A: 5/36, B: 1/36; both differences statistically significant Other problems not statistically significant: urgency urinary incontinence (A: 6/36, B: 3/36) Four patients reported in control because of residual urine for B. Equally good results on sonographic investigation at follow‐up |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number chart: even numbers underwent colposuspension; odd numbers underwent sling procedure |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
Fischer 2001.
| Methods | Design: RCT. Details not given Follow‐up at 6 months |
|
| Participants | 22 women with intrinsic sphincter deficiency, 11 in each arm | |
| Interventions | A (11): suburethral sling B (11): Burch retropubic urethropexy |
|
| Outcomes | Subjective cure assessed using comparison between pre‐operative and postoperative Incontinence Impact Questionnaire (IIQ), Urinary Distress Inventory (UDI) (measured) Objective cure by stress test; voiding dysfunction by urodynamic assessment if incontinence seen (clinician‐assessed) Success rate reported as follows: A: 100% (11/11), B: 77.8% (7/9), P = 1 Mean postoperative IIQ and UDI scores not significantly different |
|
| Notes | Abstract only
Aim to evaluate prognostic value of urethral electrodiagnosis Two patients in the Burch group were found to have recurrent UVJ hypermobility or displacement and were not included in the final analysis A high proportion of excluded women were found to have end‐stage urethral neuropathy |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Two patients in the Burch group were found to have recurrent UVJ hypermobility, were considered surgical failures, and were excluded from final analysis. Insufficient information to judge whether appropriately addressed |
Guerrero 2008.
| Methods | Design: RCT (3 arms). Computer‐generated randomisation schedule used for each centre and for each individual surgeon. Remote telephone randomisation undertaken by independent CRU; type of sling faxed on the morning of the operation. Patients were not told which sling they had, although they could not be blinded to Pfannenstiel incision; research nurses collecting data were not told what procedure the women had undergone Setting: 4 centres Follow‐up at 6 months and 1 year; 85% available for follow‐up at 1 year |
|
| Participants | 201 women randomised (mean age 52 years) to Pelvicol‐50, TVT‐72, autologous sling‐79 Inclusion criteria: women requiring primary surgical treatment for urodynamic USI following failed conservative treatment Exclusion criteria: previous surgery for SUI, neurological disease, pelvic organ prolapse > stage 2, detrusor overactivity, or bladder hypocompliance on urodynamic assessment |
|
| Interventions | A (79): autologous fascial sling from rectus (sling‐on‐a‐string) B (50): Pelvicol (randomisation to this arm halted half way through the trial) 12 × 2 cm Pelvicol graft C (72): TVT (Gynecare) Dropout at 12 months: A: 12; B: 4; C: 3; no explanation for differential dropout from group A |
|
| Outcomes | Success and improvement rates described but method of assessment not defined Other outcome measures included operative details, complications, dry/improved rates, quality of life assessment, catheterisation, and re‐operation rates Theatre time, minutes, mean (range): A: 54 (25 to 140); B: 36 (17 to 70); C: 35 (14 to 120) Length postop stay, days, median (range): A: 4 (1 to 22), B: 4 (1 to 12), C: 2 (1 to 10) Incontinent at 6 months: A: 38/73, B: 25/45, C: 35/71 Incontinent at 12 months: A: 35/67, B: 36/46, C: 31/69 Not improved at 6 months: A: 4/73, B: 12/45, C: 6/71 Not improved at 12 months: A: 7/67, B: 18/46, C: 5/69 Re‐operation rate: A: 0/67, B: 9/46, C: 0/69 Self‐catheterisation at 12 months: A: 0/67, B: 0/46, C: 0/69 Adverse effects: Bladder injury: A: 2/79, B: 1/50, C: 4/72 Urethrolysis (release of tape): A: 1/67, B: 0/46, C: 1/69 10‐year follow‐up: 162 women available at 10 years (A: 61, B: 38, C: 63) Incontinence at 10 years: A: 30/61, B: 32/38, C: 43/63 Not improved at 10 years: A: 15/61, B: 16/38, C: 17/63 Satisfaction: A: 43/61, B: 20/38, C: 44/63 Recommend to a friend: A: 46/61, B: 25/38, C: 53/63 Reoperation rate for SUI at 10 years: A: 0/61, B: 5/38, C: 2/63 Other gynaecological surgery: A 7/61, B 4/38, C 5/63 De novo urgency: A: 0/61, B: 0/38, C: 1/63 Self‐catheterisation: A: 4/61, B: 0/38, C: 3/63 Sling release: A: 2/61, B: 1/38, C: 2/63 (long‐term voiding dysfunction at 10 years: A: 6/61, B: 1/38, C: 5/63) Tape/graft exposure: A: 0/61, B: 0/38, C: 1/63 Scar pain: A: 2/61, B: 0/38, C: 0/63 |
|
| Notes | High re‐operation rates (1 in 5) in Pelvicol group (group B), so arm closed. Study closed at 6 years before target number reached. Interim analysis after first 50 patients in each group Although there was no mention of how success rate was assessed in the abstract, on contacting a listed author, we were informed that figures were patient‐reported Interim analysis showed that women randomised to Pelvicol (group B) had significantly poorer outcomes; therefore this arm was dropped and the trial was continued as a 2‐arm RCT Study closed after 6 years due to failure to recruit target numbers and high re‐operation rate |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation schedule used for each centre and for each individual surgeon |
| Allocation concealment (selection bias) | Low risk | Remote telephone randomisation undertaken by the independent CRU; type of sling faxed on the morning of the operation |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Patients were not told which sling they had, although they could not be blinded to Pfannenstiel incision; research nurses collecting data were not told what procedure the women had undergone |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No differential dropout (although group B was stopped early due to poor outcomes) |
Helmy 2012.
| Methods | Design: RCT; randomised prospective study | |
| Participants | 482 women with urinary incontinence Inclusion and exclusion criteria not defined |
|
| Interventions | A: fascial sling B: Burch urethropexy |
|
| Outcomes | Continence rates: defined as no urinary leakage in a 3‐day voiding diary, no self‐reported stress incontinence symptoms, and no stress incontinence surgical treatment (combined outcome) Continence rates: 3 years: A: 30.8%, B: 24.1% Satisfaction rates: 5 years: A: 83%, B: 73% Adverse event rates (follow‐up period not specified): A: 9%, B: 10% Number of women with adverse events: A: 22; B: 23 |
|
| Notes | Abstract only; no useable data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information available |
| Allocation concealment (selection bias) | Unclear risk | No information available |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information available |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information available |
Henriksson 1978.
| Methods | Design: RCT. Details not given Follow‐up at 4 to 6 months |
|
| Participants | 30 women randomised, 15 in each arm of the study, all with genuine stress incontinence. All age groups of patients given but menopausal status not reported Exclusion criteria: cystocoele, uterine prolapse, urgency urinary incontinence, neurogenic bladder, urinary tract infection |
|
| Interventions | A (15): Teflon sling (Zoedler urethroplasty) B (15): MMK urethrocystopexy |
|
| Outcomes | Cure defined as complete freedom from SUI (subjective and objective demonstrations) (combined outcome). All patients in both groups cured. Complications not reported. Main differences observed in stress closing pressure of urethra, which became positive after surgery in both groups | |
| Notes | Groups stated similar, but no comparisons made at baseline. Short follow‐up | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
Hilton 1989.
| Methods | Design: RCT. Women allocated to 1 of 2 interventions by random tables Follow‐up at 2, 3, 12, and 24 months. All women available at follow‐up |
|
| Participants | 20 women recruited, 10 in each arm of the study Inclusion criteria: GSI (urodynamic diagnosis), vaginal narrowing, postsurgical scar, unsuitable for colposuspension Groups comparable for age, parity, and number of previous surgical incontinence procedures. Menopausal status not reported Exclusion criteria: not stated |
|
| Interventions | A (10): porcine dermis sling operation B (10): Stamey bladder neck (needle) suspension |
|
| Outcomes | Cure stated as objective (urodynamic diagnosis, pad test (clinician‐reported)) at 3 months' and as subjective (woman‐reported) at 24 months' follow‐up Failure rates at 3 months: A: 1/10, B: 2/10 Failure rates at 24 months: A: 1/10, B: 3/10 Differences not statistically significant at 3 and 24 months Postoperative complications: A: 9/10, B: 2/10 (operative blood loss, pyrexia, infective complications, suprapubic catheter permanence) Hospital stay: A: 20 (12.9), B: 7 (0.3) Late complications not reported Voiding problems at 3 months: A: 4/10, B:2/10 Detrusor instability: A: 2/10, B: 1/10 Urgency urinary incontinence: A: 5/10, B: 3/10 No difference in frequency of uninhibited detrusor contractions, residual volume, and maximum voiding pressure Peak flow significantly reduced for A, although higher than 15 mL/s |
|
| Notes | Pad test at 12 and 24 months stated but not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers chart |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
Kondo 2006.
| Methods | Design: quasi‐RCT. Randomisation by date of birth method; 2 arms. Odd days assigned to TVT arm, even days to PVS Follow‐up: 3, 12, and 24 months |
|
| Participants | 63 women who complained of SUI were recruited: 3 eventually declined to undergo surgery; therefore a total of 60 women (29 PVS, 31 TVT) with urodynamic stress or mixed incontinence were included Diagnosis was made by a cough‐stress test, a 60‐minute pad‐weighing test, and urodynamic studies |
|
| Interventions | A (29): PVS B (31): TVT |
|
| Outcomes | Primary outcome measure was cure of SUI. Subjective cure was consistent with complete dryness or a few drops of water with strong exercises (assumed to be woman‐reported) Objective cure was defined as complete absence of leakage during cough‐stress test with 250 or 300 mL of water in the bladder (clinician‐reported) Other outcome measures (6‐parameter analysis) were operation time, numbers of analgesics required in a perioperative period, changes in haematocrit, length of a Foley catheter, and length of stay Not cured at 24 months (subjective): A: 7/21, B: 4/23 Not cured at 24 months (objective): A: 11/21, B: 7/23 Operative time, mean minutes (SD) N: A: 87.1 (13.3) 21, B: 43.9 (17.3) 23 Length of hospital stay, mean (SD): A: 9.2 (0.9), B: 9.2 (0.6) days Time to catheter removal, mean (SD): A: 1.4 (0.5), B: 1.3 (0.1) days Complications: All complications: A: 11/29, B: 9/31 Bladder perforation: A: 7/29, B: 7/31 Urethral injury: A: 0/29, B: 1/31 Subcutaneous haematoma: A: 0/29, B: 1/31 Voiding dysfunction: A: 4/29, B: 0/31 Release of sling surgery: A: 4/29, B: 0/31 De novo detrusor urgency: A: 3/29, B: 2/31 |
|
| Notes | Follow‐up at 24 months. Women who underwent concomitant surgery (5 PVS, 8 TVT) and/or had revision surgery were excluded from the 6‐parameter analysis because extra interventions made comparison difficult. Subjects for assessment were reduced to 23 women in the TVT group and 21 in the PVS group Data updated from new publication |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Date of birth method |
| Allocation concealment (selection bias) | High risk | Date of birth |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No mention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Similar loss across groups at follow‐up: 72% remained in sling arm and 74% in Burch arm |
Lucas 2000.
| Methods | Design: RCT. Women allocated to each arm by a central telephone randomisation system. Not blinded ‐ operation obvious to all medical and nursing personnel Setting: 3 hospitals Follow‐up at 3, 6, and 12 months |
|
| Participants | 165 women randomly assigned to 2 groups. Baseline demographics and symptoms were similar: age, height, weight, symptom years, previous surgery, number and type of concurrent problems between groups Inclusion criteria: patients older than 18 years; urodynamically proven SUI Exclusion criteria: evidence of neurological disease; urodynamic evidence of detrusor instability and hypocompliance |
|
| Interventions | A (81): standard sling insertion (long) B (84): sling on a string (short) |
|
| Outcomes | Primary outcome was to compare QoL scores in both groups over time. Success rate was measured by recurrence of stress leakage as reported on patient questionnaire (woman‐reported) Secondary outcomes were measured by patient quality of life, clinical indicators (such as immediate postoperative complications, time to first void, pad tests), administrative indicators, pain scores, and patient satisfaction Patient satisfaction at 12 months: A: 57/73, B: 62/82 Stress leakage at 12 months: A: 14/72, B: 16/72 Stress leakage at 3 years: A: 35/75, B: 30/70 Stress leakage at 6 years: A: 42/73, B: 34/69 De novo urgency: A: 6/81, B: 2/84 Pad test volumes (mL): A: 7.71, B: 4.61, P = 0.56 Mean operative time, minutes (range): A: 62 (38 to 135), B: 54 (25 to 140), P = 0.001 (P used to calculate SD: 15.33 in each group) Mean blood loss (mL): A: 274 (50 to 800), B: 230 (50 to 700), P = 0.07 Length of stay (days): A: 6.48, B: 6.73 Voiding dysfunction 12 months: A: 19/81, B: 17/84 Re‐admission within 3 months: A: 19/79, B: 9/83 Surgery to release sling: A: 1/81, B: 4/84 Further continence surgery: A: 2/56, B: 5/69 Pain at 3 months: A: 52/78, B: 42/82 Adverse effects: Perioperative surgical complications: A: 34/81, B: 31/84 Bladder perforation: A: 2/81, B: 3/84 UTI: A: 10/81, B: 6/84 |
|
| Notes | Detailed outcome measures at 3, 6, and 12 months were provided. Both groups showed improvement in quality of life with no significant statistical differences between allocated operations 46 patients had previously undergone 1 or more forms of incontinence surgery Data were updated from new publication |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation schedule |
| Allocation concealment (selection bias) | Low risk | Remote telephone randomisation |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not blinded; operation performed obvious to all medical and nursing personnel involved in the assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Ouctome data analysed according to randomised group, per protocol, and best possible. Twenty‐one women lost to follow‐up by 12 months, 23 lost by 3 years. Similar losses from each arm unlikely to affect the final analysis. Actual numbers with outcomes reported |
Maher 2005.
| Methods | Design: RCT of pubovaginal sling vs Macroplastique Intention‐to‐treat analysis performed Follow‐up: 6 months, 1 year |
|
| Participants | 45 women randomised. 1 from each arm lost to follow‐up by 1 year Inclusion criteria: women with USI and ISD diagnosed by MUCP ≤ 20 cm H₂O who failed to respond to conservative treatment Exclusion criteria: required prolapse surgery, had undergone a sling procedure, were unsuitable for general anaesthesia Baseline comparison included age (years), BMI (kg/m²), menopause status, parity, previous surgery (abdominal hysterectomy, vaginal hysterectomy/repair, retropubic continence surgery, needle suspension) |
|
| Interventions | A (22): pubovaginal sling B (23): transurethral Macroplastique |
|
| Outcomes | Subjective success: no or occasional (less than once a week) stress incontinence (woman‐reported) Objective success: no leakage due to SUI on repeat urodynamic study (clinician‐reported) Other outcome measures included voiding dysfunction, patient satisfaction, operating time, blood loss, inpatient days, duration of catheterisation, time to resume normal activities Incontinent within 1 year: A: 2/21, B: 5/22, P = 0.41 Incontinent after 1 year: A: 0/13, B: 4/14, P = 0.1 Incontinent within 1 year (objective): A: 4/21, B: 20/22, P ≤ 0.0001 Patient satisfaction (self‐reported at 6 months): A: 7/21, B: 13/22, P = 0.41 Patient satisfaction (self‐reported at 5 years): A: 9/13, B: 4/14, P = 0.057 Operative time, minutes (range): A: 60 (25 to 105), B: 22 (10 to 41), P ≤ 0.0001 Length of hospital stay, days (range): A: 4 (3 to 81), B: 1 (1 to 2), P ≤ 0.0001 Time to normal activity, weeks (range): A: 4 (0 to 42), B: 28 (0 to 35), P ≤ 0.0001 Time to catheter removal, days (range): A: 5 (2 to 42), B: 1 (0 to 7), P ≤ 0.0001 Further continence surgery: A: 1/21, B: 2/22 Complications: UTI: A: 3/21, B: 2/22 De novo detrusor overactivity: A: 1/21, B: 0/22 Voiding dysfunction: A: 4/21, B: 1/22 |
|
| Notes | Tertiary referral centres Macroplastique (uroplasty, Minneapolis, Minnesota, USA) is a vulcanised silicone microimplant (polydiamethylsiloxane) suspended in a povidone gel designed to provide urethral bulking for treatment of SUI |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Computer randomisation software; no description given |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Ouctome data analysed according to randomised group. One woman in each group failed to return or complete any review. Actual numbers with outcomes reported |
Okulu 2013.
| Methods | Design: RCT: randomised prospective study | |
| Participants | 144 women Inclusion criteria: incontinence, clinical and/or urodynamic diagnosis of SUI, positive stress test Exclusion criteria: urodynamic MUI, detrusor overactivity, > 200 mL postvoid residual urine, contraindication to anaesthesia, pelvic organ prolapse, pregnancy, neurogenic bladder, bladder outlet obstruction, urinary fistula, active UTI, vaginal infection Some women had failed previous continence surgery, hysterectomy; some were post menopause |
|
| Interventions | A (48): broad‐based double‐forced sling using Vypro mesh (semi‐absorbable multi‐filament) B (48): broad‐based double‐forced sling using Ultrapro mesh (synthetic combined mesh, non‐absorbable with absorbable coating, monofilament) C (48): broad‐based double‐forced sling with Prolene light mesh (non‐absorbable, monofilament) Meshes fixed with 2 polypropylene sutures to fascia of the rectus muscle |
|
| Outcomes |
Cure defined as no pad use (measured): 6 months: A: 40/46, B: 44/48, C: 41/47 12 months: A: 41/46, B: 45/48, C: 41/47 48 months: A: 39/46, B: 44/48, C: 40/47 Incontinence rate: A: 6/46 ICIQ‐SF score (higher is worse), mean (SD) N: At 6 months: A: 3.1 (0.9) 46, B: 2.1 (0.8) 48, C: 2.7 (0.8) 47 At 12 months: A: 2 (0.7) 46, B: 1.2 (0.6) 48, C: 1.7 (0.4) 47 At 48 months: A: 2.1 (0.5) 46, B: 0.8 (0.5) 48, C: 1.5 (0.3) 47 24‐hour pad test (grams), mean (SD) N: 6 months: A: 4.2 (6.4) 46, B: 2.7 (6.2) 48, C: 3.03 (5.8) 47 12 months: A: 2.1 (1.4) 46, B: 2 (1.1) 48, C: 2.4 (3.8) 47 48 months: A: 2.3 (1.1) 46, B: 1.3 (0.8) 48, C: 2.4 (1.1) 47 Number of pads used mean (SD) N: At 6 months: A: 0.93 (0.5) 46, B: 0.83 (0.5) 48, C: 1.1 (0.8) 47 At 12 months: A: 0.62 (0.4) 46, B: 0.33 (0.2) 48, C: 0.94 (0.6) 47 At 48 months: A: 0.65 (0.3) 46, B: 0.2 (0.15) 48, C: 0.83 (0.54) 47 Voiding or storage symptoms: A: 9/46; B: 4/48; C: 7/47 Dissatisfaction rate: A: 9/46; B: 7/48; C: 9/47 Complications at 48 months: Vaginal erosion: A: 2/46, B: 1/48, C: 2/47 Urethral erosion: A: 1/46, B: 0/48, C: 1/47 Suture granuloma: A: 3/46, B: 1/48, C: 3/47 Urine retention: A: 2/46, B: 2/48, C: 2/47 De novo urgency: A: 5/46, B: 2/48, C: 4/47 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ‘randomly allocated into three groups by centralised computerised system (1:1:1)’ |
| Allocation concealment (selection bias) | Low risk | ‘randomly allocated into three groups by centralised computerised system (1:1:1)’ |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No differential dropout; dropout rate is low |
Osman 2003.
| Methods | Design: RCT (block randomisation technique). Selection criteria well reported Follow‐up reported at 6 months |
|
| Participants | 75 women with mixed incontinence symptoms and a negative cystometrogram for motor detrusor overactivity. All had proven stress urinary incontinence. No details on demographic data were reported 21 patients (anticholinergic) and 24 (sling) were available for follow‐up |
|
| Interventions | A (50): surgery (Ai (24) Burch colposuspension, Aii (26) rectus fascia sling) B (25): anticholinergic treatment |
|
| Outcomes | Patients were evaluated by SEAPI score (subjective and objective) and underwent urodynamic examination before and after treatment (combined outcome) Cure for urge symptoms: Aii: 88%, B: 57% Cure for SUI: Aii: 83%, B: 0 |
|
| Notes | Study was designed to investigate anticholinergic therapy in comparison with surgery. Patients allocated to surgery had a sling procedure if Valsalva leak point pressure was < 90 cm H₂O. We extracted only data on sling in comparison with anticholinergics | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of 75 women randomised, 68 evaluated after 6 months. Four in anticholinergic arm and 3 in surgical arm lost. Insufficient information to determine whether appropriately addressed or not |
Pacetta 2005.
| Methods | Design: RCT. Abstract. Randomisation 2:1. Two arms Follow‐up: 1 year |
|
| Participants | 34 women randomised. No mention of baseline comparison Inclusion criteria: women 30 to 77 years old with SUI due to hypermobility or ISD underwent surgical correction |
|
| Interventions | A (10): autologous fascia B (24): Fortaperm |
|
| Outcomes | Subjective patient evaluations included QoL questionnaire, incontinence diary, pain, and global outcome assessments (measured) Objective outcome assessment was urine loss with a provocative pad test (clinician‐reported) Biopsies were taken at 1 year from FP implant sites adjacent to urethra for histology Objective incontinence within first year: A: 1/10, B: 5/24 Not improved within first year (subjective): A: 0/10, B: 2/24 |
|
| Notes | Fortaperm is absorbable biomaterial composed of laminated sheets of purified porcine collagen matrix | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
Sand 2000.
| Methods | Design: RCT by random numbers table Follow‐up at 3 months and at 72.6 months (mean) |
|
| Participants | 36 women with genuine stress incontinence and maximum urethral closure pressure ≤ 20 cm H₂O. Groups comparable in terms of age, parity, and urodynamic variables, except for detrusor instability (> Burch vs sling) and residual volume (> Burch vs sling) | |
| Interventions | A (17): PTFE sling operation B (19): modified (overcorrection) Burch colposuspension |
|
| Outcomes | Cure defined as objective (urodynamic: clinician‐reported separately) and subjective (history: woman‐reported) Number of continent women (short‐term): A: 17/17, B: 17/19 Objective cure (long‐term): A: 100%, 13/13, B: 86%, 13/15 Subjective cure (long‐term): A: 84%, 11/13, B: 93%, 14/15 There were no statistically significant differences in outcome measures |
|
| Notes | First publication (2000) reported short‐term follow‐up and was considered the primary reference. Last publication (2003) reported long‐term results | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Similar losses in both groups at long‐term assessment |
Sharifiaghdas 2008.
| Methods | Design: RCT of tension‐free vaginal tape with autologous rectus fascia sling. Randomisation by sealed opaque envelopes Follow‐up: 1, 3, 6, and 12 months |
|
| Participants | 100 women randomised into 2 groups. However, only 61 followed up to 1 year. 16 lost due to distance and expense of travel ‐ 12 were age‐related and 11 occurred because of dissatisfaction with surgical result (6 sling, 5 TVT) Inclusion criteria: history of USI, 1‐hour pad test (> 2 grams of leakage), objective positive cough (effort or exertion), induced stress test, normal cystourethroscopy and urodynamic confirmation of SI, urethral hypermobility, competent bladder neck Exclusion criteria: history of more than 3 episodes of UTI in past 2 years, other gynaecological problems such as high‐grade uterine prolapse, high‐grade rectocoele and enterocoele, cystocoele ≥ grade 2, abnormal filling phase of urodynamic study, low flow rates (< 15 mL/s), residual urine of more than 100 mL, trabeculated bladder mucosa on cystourethroscopy, history of major pelvic trauma, fracture that might negatively affect urethral function Women with mixed incontinence symptoms were included provided urodynamics showed normal capacity, normal compliance, and stable bladder The 2 groups had similar characteristics with respect to age, parity, hysterectomy, previous incontinence surgery, sensory urgency incontinence, pre‐operative IIQ score |
|
| Interventions | A (52): pubovaginal sling B (48): TVT |
|
| Outcomes | Objective cure defined as negative cough‐induced stress test with full bladder (at least 250 mL filled) in the lithotomy and standing positions (clinician‐reported) and a 1‐hour pad test ≤ 2 grams (measured) Subjective cure defined by mean IIQ score in each group Also assessed were type of anaesthesia, operative time, estimated blood loss, bladder penetration, and satisfaction with procedure Incontinent within 1 year (stress test): A: 6/36, B: 3/25, P = 0.9 Incontinent within 1 year (1‐hour pad test): A: 10/36, B: 6/25, P = 0.83 Patient satisfaction at 12 months: A: 20/36, B: 15/25 Operative time (minutes): A: 80 (50 to 180), B: 45 (30 to 70), P = 0.01 Length of hospital stay (days): A: 5 (3 to 7), B: 2 (1 to 5), P = 0.001 Time to catheter removal, days (range): A: 4.6 (3 to 6), B: 1.3 (1 to 5), P = 0.001 Complications: De novo urgency symptoms: A: 8/36, B: 1/25 Voiding dysfunction: A: 11/36, B: 5/25 Bladder perforation: A: 2/36, B: 6/25, P = 0.05 Bleeding (> 250 mL): A: 1/36, B: 1/25, P = 1.00 Suprapubic incisional hernia after 8 months: A: 1/36, B: 1/25 |
|
| Notes | Procedures were performed by single surgeon All patients were pre‐operatively evaluated by physical examination, plain abdominal X‐ray, urinary tract ultrasound, cystourethroscopy, and urodynamic study Physical examination assessed degree of prolapse and basal lab tests (FBC, renal and liver function tests, serum electrolytes, urine analysis, culture) Assumption was made that t‐test was used for operative time, catheterisation, and hospital stay 10‐year follow‐up was published (Sharifiaghdas 2017), but data were not added to the review |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Sealed opaque envelopes; no mention of numbering |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All outcomes assessed in randomised groups. 39 patients lost to follow‐up. Similar losses in each group |
Sharifiaghdas 2015.
| Methods | Design: RCT Setting: Shahid Labbafinejad Medical Centre, Iran Follow‐up: mean 13.8 months (SD 4.4), range 12 to 20 Follow‐up at hospital visits at 1 week; 1, 3, 6, and 12 months after surgery |
|
| Participants | 72 women with main complaint of SUI unresponsive to conservative treatment, urethral hypermobility, positive cough‐stress test; urodynamics in all women and DO excluded ‐ therefore classes and USI Exclusion criteria: persistent UTI, active UTI at surgery, urogynaecological malignancy, cystocoele (prolapse) ≥ grade 3, neurogenic bladder, abnormal filling or voiding, detrusor overactivity, low flow rate, residual urine > 100 mL, abnormal cystourethroscopy findings |
|
| Interventions | A (35): autologous rectus fascia pubovaginal sling B (35): mini‐sling (Ophira) |
|
| Outcomes | Cure defined as woman report of some degree of SUI at 1 year after surgery Cure: A: 31/35, B: 31/35 Number of women satisfied: A: 25/35, B: 28/35 Number of women with UI: A: 4/35, B: 4/35 Objective UI (positive cough‐stress test): A: 4/35, B: 4/35 IIQ score, mean (SD) N: A: 50.2 (11.1) 35, B: 42.7 (11.4) 35 Adverse effects: Surgery for tape exposure: A: 0/35, B: 2/35 Adverse effects (dyspareunia, bladder perforation, urethral erosion, vaginal erosion/wound haematoma and/or infection: A: 21.6%, B: 2.9% (all treated conservatively with antibiotics, local care, or dressings) Haematoma and/or infection: A: 8/35, B: 1/35 Dyspareunia: A: 3/35, B: 4/35 Bladder perforation: A: 1/35, B: 0/35 Vaginal erosion: A: 1/35, B: 2/35 Urgency incontinence: A: 5/35, B: 1/35 Obstructive voiding symptoms: A: 6/35, B: 1/35 (1 woman required urethral dilatation, but group is unknown) UTI: A: 0, B: 0 |
|
| Notes | Groups were comparable at baseline, although sling group was younger | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned by envelope sealed cards |
| Allocation concealment (selection bias) | Low risk | Randomly assigned by envelope sealed cards |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up reported |
Shin 2001.
| Methods | Design: RCT stated. Details not given in abstract of the trial Follow‐up after first year reported |
|
| Participants | 57 women with various types of SUI. Patient characteristics not reported | |
| Interventions | A (33): autologous dermal graft patch B (24): cadaveric fascia lata |
|
| Outcomes | Outcome measures reported were success rate (dry/improved) (method unspecified: assumed woman‐reported), de novo detrusor instability Success rate (dry or improved): A: 30/33 (91.6%), B: 22/24 (93.2%) Dry: A: 25/33, B: 19/24 Improved (only): A: 5/33, B: 3/27 De novo detrusor instability: A: 4/33, B: 5/20 Voiding delay in first 30 days: A: 0/33, B: 1/24 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data (based on abstract) |
Silva Filho 2006.
| Methods | Design: RCT of SAFYRE TOT with autologous pubovaginal sling. Randomisation method unclear Follow‐up: 6 months |
|
| Participants | 20 women (average age 52.5 ± 11.8 years) with both USI and SUI but without detrusor overactivity The 2 groups had similar characteristics with respect to age, parity, BMI, menopausal status, presence of pelvic floor defects, and mean Valsalva leak point pressure in pre‐operative UDS |
|
| Interventions | A (10): pubovaginal sling B (10): SAFYRE TOT |
|
| Outcomes | Cure rates and intraoperative and postoperative morbidity. Women were declared objectively cured when they had a postoperative pad test ≤ 8 grams All patients were pre‐operatively evaluated by history, physical examination, quality of life questionnaire (King's Health Questionnaire), 24‐hour pad weight test, 2‐day voiding diary, and multi‐channel urodynamic study that included uroflowmetry, postvoid residual volume measured by urethral catheter, and cystometrogram. Objective quantification of the severity of incontinence was done by mean stress leaking point pressure in the urodynamic study. Pre‐operative measurements included type of anaesthesia, duration of surgery, intraoperative complications, occurrence of combined procedures, and hospital stay At 6‐month follow‐up, aforementioned measurements were carried out excluding UDS Postoperative pad test, mean (SD): A: 8.4 (16.44), B: 39.4 (39.53) grams, P = 0.01 Operative time, mean (SD): A: 69.5 (23.7), B: 21.1 (3.8) minutes, P < 0.001 Length of hospital stay, mean (SD): A: 44.4 (5.8), B: 28.8 (8.4) hours, P < 0.001 |
|
| Notes | SAFYRE consists of a monofilament polypropylene mesh between 2 silicone columns made of multiple cone‐shaped soft tissue anchors. The 2 columns are fixed to the obturator muscle. Pubovaginal sling uses rectus fascia | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
Song 2004.
| Methods | Design: RCT of TVT compared with autologous fascia lata pubovaginal sling Setting: single centre |
|
| Participants | 67 women with SUI were randomised. Basline comparisons of age, menopausal status, parity, SUI, mixed incontinence, and intrinsic sphincter dysfunction were made Inclusion criteria: type II to IV SUI, mixed SUI, intrinsic sphincter dysfunction, failed previous operations Mixed incontinence was included in this study |
|
| Interventions | A (19): autologous fascia lata pubovaginal sling B (48): TVT |
|
| Outcomes | Cure rates and operative morbidity Damage to bladder, urinary retention, difficulty voiding Incontinent at 3 months: A: 1/19, B: 3/48 Not improved at 3 months A: 0/19, B: 0/48 Operative time (SD): A: 125 (13), B: 27 (5) minutes Mean length of hospital stay: A: 7.2, B: 1.8 days Mean time to catheter removal: A: 5.3, B: 1 days Complications: Voiding dysfunction: A: 3/19, B: 3/48 Urinary retention: A: 2/19, B: 0/48 Bladder injury: A: 0/19, B: 2/48 Detrusor overactivity: A: 1/19, B: 3/48 |
|
| Notes | Follow‐up on average was between 20 and 37 months. Cure rates were assessed at 3 months Full text was translated from Chinese |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Divided into 2 groups randomly (no details given, but numbers in groups unequal) |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
Tcherniakovsky 2009.
| Methods | Design: RCT Follow‐up at 12 months |
|
| Participants | 41 women randomly distributed into 2 groups. Patients had similar baseline characteristics (age, BMI, parity, vaginal births, postmenopausal conditions, hormone replacement therapy, previous SUI surgery, genital prolapse, previous surgery/previous hysterectomy, disease duration) Inclusion criteria: USI, confirmed through medical history, physical exam, and urodynamic investigation |
|
| Interventions | A (20): retropubic sling (aponeurotic sling) B (21): SAFYRE TOT (synthetic transobturator) |
|
| Outcomes | Cure was defined as the reported absence of SUI and no urinary loss during effort manoeuvres (combined outcome) during 12‐month follow‐up re‐evaluation Failure at 12 months: A: 1/20, B: 2/21 Operative time, mean (SD): A: 59.7 (10.3), B: 12.8 (2.4) minutes Time to catheter removal: A: 2, B: 1 day Complications: All complications: A: 12/20, B: 3/21 UTI: A: 2/20 B: 0/21 Bladder perforation: A: 1/20, B: 0/21 Urinary retention: A: 2/21, B: 3/20 Vaginal mesh erosion (isolated): A: 0/20, B: 1/21 |
|
| Notes | Physical exam specifically evaluated urinary loss through Valsalva maneuver and presence of other concurrent dystopia of pelvic floor (anterior, posterior, and apical), using POP‐Q classification VLPP standardised in this study at 200 mL of vesical repletion Urodynamic study performed on every patient included |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Patients "randomly distributed". No details provided |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
Teixeira 2008.
| Methods | Design: RCT. Details not given in abstract Follow‐up: 24 hours and 90 days |
|
| Participants | 42 patients were randomised (porcine collagen 21, polypropylene tapes 21) Inclusion criteria: stress urinary incontinence |
|
| Interventions | A (21): porcine collagen B (21): polypropylene tapes |
|
| Outcomes | No outcome measure relevant to this review C‐reactive protein and white blood count measured previous day and at 24 hours after surgery Biopsy at 90 days post operation for local inflammatory markers (polymorphonuclear cells, mononuclear cells, giant cells, and neovascularisation) and collagen reaction (collagen amount, composition, and organisation) |
|
| Notes | Trial assessing systemic and local inflammatory responses with different sling materials | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Unclear risk | "blindly randomised" ‐ no details provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 2 patients with missing outcome data. No details provided on whether losses were similar in both groups or within a single arm of the trial |
Teleb 2011.
| Methods | Design: prospective randomised study All operations were performed by the same surgical team |
|
| Participants | 32 women with main complaint of SUI established by history, examination, and urodynamic evaluation Exclusion criteria: neurological disease, overactive bladder, other causes and forms of incontinence (overflow or pure urge), recurrent SUI (after anti‐incontinence procedure), any form of prolapse requiring surgery (only cases with grade 1 asymptomatic cysto‐urethrocoele included) |
|
| Interventions | Transvaginal tension‐free mid‐urethral slings were used under the mid‐urethra via a retropubic route A (12): anterior rectus sheath sling harvested via 7‐cm Pfannenstiel incision and with 0 Prolene suture placed at each end to be pulled up B (12): 7 × 1.5‐cm tailored Prolene strip with 0 Prolene sutures placed at each end to be used as a sling C (8): rectangular anterior vaginal wall patch 5 × 1.5 cm harvested and placed under mid‐urethra with Prolene sutures in the same manner |
|
| Outcomes | Cured defined as no leakage reported by patient or noticed at examination (at ˜ 18 months): A: 8/12, B: 9/12, C: 6/8 Improved defined as leakage occurring only with severe exertion unlike before surgery (at 3 months): A: 3/12, B: 2/12, C: 1/8 Failure: A: 1/12, B: 1/12, C: 1/8 Operative blood loss, mean (SD; range): A: 181.2 (33.1; 130 to 230), B: 149.2 (28.8; 100 to 200), C: 200.8 (28.1; 160 to 360) Duration minutes, mean (SD; range): A 52.1 (4.4; 45 to 60), B 35.7 (3.4; 30 to 40), C 42.2 (4.5; 35 to 50) Hospital stay (hours), mean (SD; range): A: 58 (12.3; 48 to 72), B: 33 (9; 24 to 48), C 36 (9.1; 24 to 48) Adverse outcome: bladder perforation: A: 0/12, B:1/12, C: 1/8 Urinary retention: managed by urethral dilators: A: 0/12, B: 1/12, C: 0/8 |
|
| Notes | Mean follow‐up was 18, 18.5, and 18 months in Groups A, B, and C. 11 patients completed 36 months of follow‐up (A: 4, B: 4, C: 3) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No differential dropout was reported at 18 months. Only 11/32 patients completed 36 months of follow‐up. No outcome data were provided at 36 months |
Viseshsindh 2003.
| Methods | Design: RCT. Method not clarified Only short‐term follow‐up reported |
|
| Participants | 26 women with stress urinary incontinence | |
| Interventions | A (15): fascial sling B (11): vaginal wall sling |
|
| Outcomes |
Measures of outcomes included SEAPI‐QMN questionnaire, presence of SUI at postoperative period, urinary symptoms and hospital stay at 3 months (median follow‐up 7 months): SEAPI scores: decreased from 6.1 to 0.9 for B, from 6.3 to 0.8 for A Persistent SUI: A: 1/15, B: 0/11 Urgency incontinence: A: 2/15, B: 1/11 Serious postoperative complications: A: 0/15, B: 0/11 Permanent urinary retention (voiding disorder): A: 0/15, B: 0/11 |
|
| Notes | All procedures performed by the same surgeon | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
Wadie 2005.
| Methods | Design: RCT. Randomisation by closed envelope delivered to surgeon by a third party. Procedures performed by 1 surgeon Follow‐up: 6 months |
|
| Participants | 63 women (mean age 47.8 years) with SUI were randomised; all had similar background characteristics (age, BMI, parity, grade of associated cystocoele) Inclusion criteria: age > 21 years, predominant symptom of SUI, willing to give informed consent, life expectancy > 1 year, normal upper urinary tract, normal manual dexterity Exclusion criteria: pelvic or vaginal surgery within 6 months, urgency urinary incontinence as predominant symptom, > grade 2 cystocoele, associated urethral pathology (e.g. diverticulum), associated bladder pathology (e.g. fistula, culture‐proven, active UTI) 12 lost to follow‐up; no information about which group |
|
| Interventions | A (25): autologous fascial sling (harvested from rectus sheath) B (28): TVT Concomitant surgery: grade 2 or 3 cystocoele or rectocoele (27) Median follow‐up: 54 (± 21.9) (range 24 to 102 months) |
|
| Outcomes | Cure defined as complete dryness with no usage of pad and negative cough‐stress test Not cured at 6 months: A: 2/25, B: 2/28 Operative time, mean (SD) N: A: 68 (23) 25, B: 48 (25) 28 minutes Time to catheter removal, mean (SD) N: A: 6.6 (5.3) 25, B: 4.3 (2.6) 28 days Complications: Bladder perforation: A: 1/25, B: 2/28 De novo detrusor overactivity at 6 months: A: 1/23, B: 0/24 Stitch sinus at 1 week: A: 0/25, B: 1/28 Vaginal erosion: A: 0/25, B: 0/28 Wound pain at 6 months: A: 7/25, B: 2/28 Voiding dysfunction: A: 7/25, B: 3/28 2‐year results: NB: denominators reported at 2 years were different from those reported at 6 months Quality of life/condition‐specific score: UDI‐6, mean (SD) N: A: 31.7 (16.9) 39; B: 24.4 (19.1) 24 (higher is worse) IIQ‐7, mean (SD) N: A: 24.4 (20.5) 39; B: 23.8 (21.6) 24 (higher is worse) Female sexual function Index (FSFI): no reference to score cited; SD not given Data on pain, satisfaction, lubrication, desire, arousal, and orgasm also provided but not used due to uncertainty about the instrument |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Low risk | Closed opaque envelopes held by a non‐involved third party who revealed the allocation after patient was anaesthetised just before start of surgery |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcomes collected by nurse blinded to treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Differential dropout at 2 years |
Zargham 2013.
| Methods | Design: quasi‐randomised clinical trial Setting: Isfahan University of Medical Sciences, Iran Follow‐up: 3 days and 18 days; 1, 6, 12, and 18 months |
|
| Participants | Inclusion criteria: 56 women with severe SUI or mixed urinary incontinence with predominant stress component and anterior vaginal wall prolapse (grade 1 to 3 prolapse based on half‐way classification system) Severity of SUI was diagnosed by ICIQ‐SF or a positive 1‐hour pad test (> 10 grams urine loss with a full bladder) Exclusion criteria: active urinary tract infection; urolithiasis; neurogenic bladder; urogenital malignancy; high‐grade rectocoele, enterocoele, or cystocoele; > POP stage 3 28 women (56%) had previous surgery: vaginal POP A: 12, B: 16; incontinence surgery A: 18, B: 21 Age, mean, years: A: 54.1, B: 55.9 |
|
| Interventions | A (26): anterior colporrhaphy (Kelly placation) and sling placement with a strip of anterior vaginal wall tied over rectus fascia and placed tension‐free under the mid‐urethra B (30): TVT (craniocaudal, top‐to‐bottom, SPARC) with transvaginal tension‐free self‐fixing sling for mesh correction of anterior vaginal wall prolapse with a T‐sling mesh kit (Herniamesh Company Polypropylene, Italy). Monofilament non‐woven polypropylene with central portion of mesh absorbable ‐ used for both SUI and cystocoele repair |
|
| Outcomes | Objective assessment via 48‐hour frequency volume chart, 48‐hour pad test, and standardised stress test Surgery was considered successful when there was no postoperative SUI (patient was dry and stress test was negative) and postoperative cystocoele was less than grade 2 Objective and subjective cure rates were evaluated between 3 and 18 days, and 1, 6, 12, and 18 months after surgery (data extracted from graphs) Cure at 18 months (from abstract): A: 54%, B: 72% Subjective cure (graph 1): 12 months: A: 14/25, B: 19/25 18 months: A: 13/25, B: 18/25 Objective cure (graph 1): 12 months: A: 13/25, B: 20/25 18 months: A: 13/25, B: 20/25 Mean duration of operation, minutes (SD): A: 42 (20), B: 56 (24) Mean duration of hospital stay, days (SD): A: 2.88 (0.94), B: 2.07 (0.92) Any complications (from abstract): A: 9/25, B: 3/25 Short‐term complications: Vaginal bleeding: A: 5/25, B: 3/25 Haematoma: A: 0/25, B: 2/25 Bladder injury: A: 1/25, B: 2/25 Long‐term complications (> 1 month): Cystitis: A: 3/25, B: 3/25 Vaginal erosion: A: 0/25, B: 2/25 De novo urgency: A: 0/25, B: 2/25 Recurrence of SUI: A: 8/25, B: 1/25 Chronic urinary retention: A: 0/25, B: 4/25 |
|
| Notes | Denominators in the table are different from those in the text | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | File number (assumed to be alternation by record number) |
| Allocation concealment (selection bias) | Unclear risk | Randomised into 2 groups |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 1 patient reported as lost to follow‐up, but data reported for 25 in each group (actual loss of 4 and 5) |
BMI: body mass index. ISD: intrinsic sphincter dysfunction. MMK: Marshall‐Marchetti‐Krantz. PVR: postvoid residual. RCT: randomised controlled trial. SUI: stress urinary incontinence. UDS: urodynamics. USI: urodynamic stress incontinence.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Amat 2007 | RCT. One mid‐urethral sling vs another |
| Atherton 2000 | Not an RCT: non‐randomised |
| Aurunkalaivanan 2001 | We are not sure about the population studied; it could be the same population as Barrington 2003 and Arunkalaivanan 2003 (included in the review). We have written to study authors to clarify this point |
| Barrington 2003 | We are not sure about the population studied; it could be the same population as Arunkalaivanan 2001 and Arunkalaivanan 2003 (included in the review). We have written to study authors to clarify this point |
| Brandt 2009 | Not an RCT: prospective longitudinal study |
| Bruschini 2005 | Not an RCT: no comparator group |
| Choe 2001 | All participants were randomised to undergo or not undergo pre‐operative urodynamic evaluation. They then had implantation of sub‐urethral Mycromesh sling. Therefore this study analyses the impact on effectiveness of a sling if the diagnosis of SUI is made with or without urodynamic evaluation |
| Chong 2003 | All participants had a TVT operation and were randomised to division/no division of tape |
| Corcos 2001 | Participants were randomised to surgery or collagen injection, but those in the surgery arm were selected to sling by patient option. Three types of operations could be chosen in the surgery group: Burch, sling, or bladder neck suspension. Results were reported in terms of collagen vs surgery |
| Darai 2007 | RCT; comparators not of interest One mid‐urethral sling vs another |
| Debodinance 1993 | Not all participants had stress incontinence. Debodinance 2000 is a 10‐year follow‐up of the first published study. This is a comparative study between Bologna (a sling made of strips of vaginal wall) and Ingelman‐Sundberg procedures (anterior colporrhaphy with pubococcygeum muscle) |
| Debodinance 1994 | Not clear how participants were allocated. Paper in French; needs translation |
| Gamble 2010 | RCT in women with low‐pressure urethra but of TVT vs TOT (TOT described as 'bladder neck sling') |
| Giri 2004 | We are not sure about the population studied; it could be the same population as Giri 2006, which has been excluded as it was a non‐randomised study. We have made attempts to contact study authors |
| Giri 2006 | Not an RCT; non‐randomised |
| Goldberg 2001 | Prolapse surgery rather than incontinence surgery |
| Halaska 2001 | Study comparing transvaginal tape vs colposuspension |
| Han 2001 | Study comparing transvaginal tape vs colposuspension |
| Hung 2001 | Not clear how patients were allocated; we have written to study authors |
| Ishenko 1999 | Randomisation process and groups unclear ('randomised by age'). Excluded as attempts to contact study authors were unsuccessful and insufficient information was given in the abstract Interventions: vaginal hysterectomy, modified Pereyra procedure, anterior and posterior repair vs vaginal hysterectomy, sling procedure with Mersilene mesh, anterior and posterior repair |
| Kocjancic 2008 | Study comparing transvaginal tape procedures; will be included in a separate review on self‐fixing slings |
| Kuo 2001 | Comparison between rectus fascia and polypropylene mesh |
| Kwon 2002 | Not all patients had stress incontinence; all patients were treated for prolapse, but 1 group received concomitant transvaginal sling (processed fascia lata), 1 group received an alternate surgery for SUI, and the last group did not have SUI and received only treatment for prolapse |
| Lemieux 1991 | Interventions were for clamping vs non‐clamping of catheters post anti‐incontinence surgery |
| Liapis 2002 | Study comparing transvaginal tape vs colposuspension |
| Lim 2005 | Study comparing mid‐urethral sling procedures |
| Meschia 2001 | Surgery for prolapse rather than incontinence |
| Naumann 2006 | This study is comparing tape procedures |
| O'Sullivan 2000 | Patients randomised to colposuspension or transvaginal tape. Reported outcome measures (collagen metabolism) not included in this review |
| Obrink 1978 | Not clear how patients were allocated. Request sent to study author October 2001 but no reply received |
| Oremus 2010 | RCT of injectables vs 3 types of surgery; not reported separately |
| Palomba 2008 | RCT of 3 different materials to carry out TOT; http://clinicaltrials.gov/show/NCT00744198 |
| Schostak 2001 | Unclear how patients were allocated. Bone anchoring used |
| Seo 2007 | One mid‐urethral sling vs another |
| Trezza 2001 | Occult incontinence treated at the same time as prolapse repair performed |
| Wang 1999 | Randomised to different types of anaesthetic |
| Ward 2002a | Study comparing transvaginal tape vs colposuspension |
| Yoo 2007 | This study is comparing tape procedures |
RCT: randomised controlled trial. SUI: stress urinary incontinence. TOT: transobturator tape. TVT: tension‐free vaginal tape.
Characteristics of studies awaiting assessment [ordered by study ID]
Abou Hashem 2017.
| Methods | Please see Abouhashem 2014 |
| Participants | Please see Abouhashem 2014 |
| Interventions | Please see Abouhashem 2014 |
| Outcomes | Please see Abouhashem 2014 |
| Notes | Please note: this appears to be exactly the same abstract as the only report (a conference abstract) of the already included Abouhashem 2014. This study report was identified by the search conducted 23 January 2019, which has not been fully incorporated into this review |
Hassan 2018.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Ongoing trial. This study report was identified by the search conducted 23 January 2019, which has not been fully incorporated into this review |
Kajbafzadeh 2017.
| Methods | RCT. Single‐blind trial. 'Randomly (computer‐based) categorized into two groups' |
| Participants | 40 women aged 30 to 50 with proven pure type 3 SUI (USI) |
| Interventions | Acellular skin graft using tension‐free vaginal tape (TVT) vs placement of synthetic mesh |
| Outcomes | Mean number of postsurgical problems and improvement in SUI |
| Notes | Ongoing trial Start date: 08.12.2016 to 01.06.2018 Contact information: kajbafzd@sina.tums.ac.ir This study report was identified by the search conducted 23 January 2019, which has not been fully incorporated into this review |
Sharifiaghdas 2017.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | This is a report at 10 years of the already included Sharifiaghdas 2008 study. This study report was identified by the search conducted 23 January 2019, which has not been fully incorporated into this review |
RCT: randomised controlled trial. SUI: stress urinary incontinence. TVT: tension‐free vaginal tape. USI: urodynamic stress incontinence.
Characteristics of ongoing studies [ordered by study ID]
Hilton 2000.
| Trial name or title | A prospective randomised comparative trial of a tension‐free vaginal tape (TVT) and fascial sling procedure for 'secondary' genuine stress incontinence |
| Methods | |
| Participants | 146 planned recruitment |
| Interventions | TVT vs fascial sling |
| Outcomes | No information |
| Starting date | |
| Contact information | |
| Notes |
Zhu 2014.
| Trial name or title | A multi‐center, randomized, controlled clinical trial of the safety and efficacy of Regen sling treatment for female patients with stress urinary incontinence |
| Methods | Multi‐centre, randomised, single‐blind, positive parallel controlled, non‐inferiority validation clinical trial: 'allocate random number to the patients in chronological order (random number allocation method: small to large' |
| Participants | Female patients with stress urinary incontinence |
| Interventions | Regen sling (high‐biocompatibility polyvinylidene fluoride (PVDF)) vs transobturator sling TVT‐O™ (Gynecare™, USA) |
| Outcomes | Anti‐urinary incontinence effect; sexual life situation; vaginal tape erosion; improvement in patients' symptoms |
| Starting date | December 2014 to December 2015 |
| Contact information | tianquan@medprin.com; Professor Zhu Lan |
| Notes |
Differences between protocol and review
For this update, published in 2020, the following changes were made.
New comparison was added: traditional suburethral sling operation versus a single‐incision sling (mini‐sling). The mini‐sling is a new procedure for surgical treatment of women with SUI, which differs significantly from the mid‐urethral sling technique and is considered to be less invasive.
Two new subgroup analyses were specified: primary versus recurrent SUI, and presence or absence of prolapse. These factors might be expected to affect the outcome and choice of surgery. We wished to explore whether different interventions had differential effects among women with these different clinical characteristics.
Outcome measures were re‐defined: primary outcomes were re‐defined as numbers of continent (dry) women using any definition of urinary incontinence and the need for repeat continence surgery. An additional outcome of 'cure' as reported by women was added.
We adopted the GRADE method for assessing the quality of evidence for those outcomes included in the 'Summary of findings' tables.
A brief economic commentary was added.
Contributions of authors
LS and CG updated the protocol and conducted the update of the review including screening, data abstraction, and updating of results and discussion. MO analysed and interpreted the results, assessed the quality of evidence (with LS), wrote the first draft of the abstract and plain language summary, and critically revised other sections of the review. HR updated a previous version of the review and contributed to this update by screening abstracts and commenting on the results, with assistance provided by JDC. PA conducted the brief economic commentary. All review authors contributed to writing the review.
Sources of support
Internal sources
No sources of support supplied
External sources
-
The National Institute for Health Research (NIHR), UK.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure, Cochrane Programme Grant, or Cochrane Incentive funding to Cochrane Incontinence. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS, or the Department of Health. The NIHR is the single largest funder of Cochrane Incontinence.
Declarations of interest
LS: none known. HR: none known. MIO: none known. JDC: none known. PA: none known. CG: none known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Abouhashem 2014 {published data only}
- Abouhashem S, Mostafa M, Elbrombely W. Five‐years follow‐up of tension‐free vaginal tape (TVT) versus rectus sheath sling for surgical treatment of female stress urinary incontinence (Abstract number MP33‐14). Journal of Urology 2014;191(4 Suppl):e343. [sr‐incont62142] [Google Scholar]
Al‐Azzawi 2014 {published data only}
- Al‐Azzawi IS. The first Iraqi experience with the rectus fascia sling and transobturator tape for female stress incontinence: a randomised trial. Arab Journal of Urology Print 2014;12(3):204‐8. [DOI: 10.1016/j.aju.2014.04.004; sr‐incont68245] [DOI] [PMC free article] [PubMed] [Google Scholar]
Albo 2007 {published data only}
- Albo M, Wruck L, Baker J, Brubaker L, Chai T, Dandreo KJ, et al. The relationships among measures of incontinence severity in women undergoing surgery for stress urinary incontinence. Journal of Urology 2007;177(5):1810‐4. [sr‐incont23120] [DOI] [PubMed] [Google Scholar]
- Albo ME, Richter HE, Brubaker L, Norton P, Kraus SR, Zimmern PE, et al. Burch colposuspension versus fascial sling to reduce urinary stress incontinence.[see comment]. New England Journal of Medicine 2007;356(21):2143‐55. [sr‐incont23077] [DOI] [PubMed] [Google Scholar]
- Brubaker L. Five year continence rates, satisfaction and adverse events of Burch urethropexy and fascial sling surgery for urinary incontinence (Abstract). European Urology Supplements 2012;11(1):e172. [sr‐incont62253] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brubaker L, Chiang S, Zyczynski H, Norton P, Kalinoski DL, Stoddard A, et al. The impact of stress incontinence surgery on female sexual function. American Journal of Obstetrics and Gynecology. 2009;200(5):562.e1‐7. [sr‐incont31130] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brubaker L, Litman HJ, Kim HY, Zimmern P, Dyer K, Kusek JW, et al. Missing data frequency and correlates in two randomized surgical trials for urinary incontinence in women. International Urogynecology Journal 2015;26(8):1155‐9. [sr‐incont68159] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brubaker L, Richter HE, Norton PA, Albo M, Zyczynski HM, Chai TC, et al. 5‐year continence rates, satisfaction and adverse events of Burch urethropexy and fascial sling surgery for urinary incontinence. Journal of Urology 2012;187(4):1324‐30. [sr‐incont44723] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brubaker L, Rickey L, Xu Y, Markland A, Lemack G, Ghetti C, et al. Symptoms of combined prolapse and urinary incontinence in large surgical cohorts. Obstetrics and Gynecology 2010;115(2 Pt 1):310‐6. [sr‐incont39373] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brubaker L, Stoddard A, Richter H, Zimmern P, Moalli P, Kraus SR, et al. Mixed incontinence: comparing definitions in women having stress incontinence surgery. Neurourology and Urodynamics 2009;28(4):268‐73. [31415] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgio KL, Brubaker L, Richter HE, Wai CY, Litman HJ, France DB, et al. Patient satisfaction with stress incontinence surgery. Neurourology and Urodynamics 2010;29(8):1403‐9. [sr‐incont40322] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chai T, Albo M, Richter H, Norton P, Dandreo K, Kenton K, et al. Adverse events from a randomized trial for the surgical treatment of stress urinary incontinence (Abstract number 512). Proceedings of the 37th Annual Meeting of the International Continence Soceity (ICS), 2007 Aug 20‐24, Rotterdam, Netherlands. 2007. [sr‐incont23535]
- Chai TC, Albo ME, Richter HE, Norton PA, Dandreo KJ, Kenton K, et al. Complications in women undergoing Burch colposuspension versus autologous rectus fascial sling for stress urinary incontinence. Journal of Urology 2009;181(5):2192‐7. [sr‐incont31150] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diokno AC, Richter HE, Kenton K, Norton P, Albo M, Kraus S, et al. Risk factors associated with failure of surgical treatment for stress urinary incontinence at 24 months follow‐up (Abstract number 115). Neurourology and Urodynamics 2007;26(5):745. [sr‐incont23533] [Google Scholar]
- FitzGerald MP, Burgio KL, Borello‐France DF, Menefee SA, Schaffer J, Kraus S, et al. Pelvic‐floor strength in women with incontinence as assessed by the brink scale. Physical Therapy 2007;87(10):1316‐24. [sr‐incont23825] [DOI] [PubMed] [Google Scholar]
- Kenton K, Tennstedt S, Litman H, Zimmern P, Getti C, Kusek JW, et al. Improvement in quality of life in women at two years after undergoing the Burch colposuspension or fascial sling procedure (Abstract number 206). Proceedings of the 38th Annual Meeting of the International Continence Society (ICS), 2008 Oct 20‐24, Cairo, Egypt. 2008. [sr‐incont31863]
- Kirby AC, Nager CW, Litman HJ, FitzGerald MP, Kraus S, Norton P, et al. Preoperative voiding detrusor pressures and stress incontinence surgery outcomes (Abstract number 38). Neurourology and Urodynamics 2010;29(6):860‐2. [sr‐incont40122] [Google Scholar]
- Kirby AC, Nager CW, Litman HJ, FitzGerald MP, Kraus S, Norton P, et al. Preoperative voiding detrusor pressures do not predict stress incontinence surgery outcomes. International Urogynecology Journal 2011;22(6):657‐63. [sr‐incont41732] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby AC, Nager CW, Litman HJ, FitzGerlad MP, Kraus S, Norton P, et al. Perineal surface electromyography to measure urethral and pelvic floor activity does not typically demonstrate expected relaxation during normal voiding (Abstract number: Short Oral 10). Journal of Pelvic Medicine and Surgery 2010;16(5 Suppl 2):S80‐1. [sr‐incont63670] [Google Scholar]
- Kraus SR, Lemack GE, Sirls LT, Chai TC, Brubaker L, Albo M, et al. Urodynamic changes associated with successful stress urinary incontinence surgery: is a little tension a good thing?. Urology 2011;78(6):1257‐62. [sr‐incont42989] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraus SR, Markland A, Chai TC, Stoddard A, FitzGerald MP, Leng W, et al. Race and ethnicity do not contribute to differences in preoperative urinary incontinence severity or symptom bother in women who undergo stress incontinence surgery. American Journal of Obstetrics and Gynecology. 2007;197(1):92‐6. [sr‐incont23802] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemack G, Krauss S, Litman H, FitzGerald M, Chai T, Nager C, et al. Preoperative urodynamic testing does not predict postoperative voiding dysfunction among women undergoing surgery for SUI: results from a prospective randomized trial comparing Burch versus pubovaginal sling (Abstract number 7, poster). Neurourology and Urodynamics 2008;27(2):123. [sr‐incont26919] [Google Scholar]
- Lemack G, Litman H, Nager C, Brubaker L, Lowder J, Norton P, et al. Pre‐operative clinical, demographic and urodynamic measures associated with failure to demonstrate urodynamic stress incontinence in women enrolled in two randomized clinical trials of surgery for stress urinary incontinence (Abstract number: Podium #10). Neurourology and Urodynamics 2012;31(2):215. [sr‐incont62279] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemack GE, Krauss S, Litman H, FitzGerald MP, Chai T, Nager C, et al. Normal preoperative urodynamic testing does not predict voiding dysfunction after Burch colposuspension versus pubovaginal sling. Journal of Urology 2008;180(5):2076‐80. [sr‐incont27705] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemack GE, Litman HJ, Nager C, Brubaker L, Lowder J, Norton P, et al. Preoperative clinical, demographic, and urodynamic measures associated with failure to demonstrate urodynamic stress incontinence in women enrolled in two randomized clinical trials of surgery for stress urinary incontinence. International Urogynecology Journal 2013;24(2):269‐74. [sr‐incont47045] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemack GE, Xu Y, Brubaker L, Nager C, Chai T, Moalli P, et al. Clinical and demographic factors associated with Valsalva leak point pressure among women undergoing Burch bladder neck suspension or autologous rectus fascial sling procedures. Neurourology and Urodynamics 2007;26(3):392‐6. [sr‐incont23233] [DOI] [PubMed] [Google Scholar]
- Mallett VT, Brubaker L, Stoddard AM, Borello‐France D, Tennstedt S, Hall L, et al. The expectations of patients who undergo surgery for stress incontinence. American Journal of Obstetrics and Gynecology 2008;198(3):308.e1‐6. [sr‐incont27182] [DOI] [PubMed] [Google Scholar]
- Markland AD, Kraus SR, Richter HE, Nager CW, Kenton K, Kerr L, et al. Prevalence and risk factors of fecal incontinence in women undergoing stress incontinence surgery. American Journal of Obstetrics and Gynecology 2007;197(6):662‐7. [sr‐incont26334] [DOI] [PubMed] [Google Scholar]
- Nager C, Chai T, FitzGerald M, Lemack G, Kraus S, Sirls L, et al. Valsalva leak point pressure and detrusor overactivity do not predict, but urodynamic stress incontinence does predict continence outcomes after Burch or pubovaginal sling procedures (Abstract number 85). Neurourology and Urodynamics 2007;26(5):709‐11. [sr‐incont23532] [Google Scholar]
- Nager C, Kraus S, Zyczynski H, Chai T, Lloyd K, FitzGerald M, et al. Urodynamic measures do not predict stress continence outcomes after surgery for stress urinary incontinence in women (Abstract number 7 Oral). Journal of Pelvic Medicine & Surgery 2007;13(5):230‐3. [NCT00064662; sr‐incont34198] [Google Scholar]
- Nager CW, Albo ME, FitzGerald MP, McDermott S, Wruck L, Kraus S, et al. Reference urodynamic values for stress incontinent women. Neurourology and Urodynamics 2007;26(3):333‐40. [NCT00064662; sr‐incont23232] [DOI] [PubMed] [Google Scholar]
- Nager CW, Albo ME, FitzGerald MP, McDermott SM, Kraus S, Richter HE, et al. Process for development of multicenter urodynamic studies. Urology 2007;69(1):63‐7; discussion 67‐8. [sr‐incont23195] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nager CW, FitzGerald M, Kraus SR, Chai TC, Zyczynski H, Sirls L, et al. Urodynamic measures do not predict stress continence outcomes after surgery for stress urinary incontinence in selected women. Journal of Urology 2008;179(4):1470‐4. [sr‐incont27210] [DOI] [PubMed] [Google Scholar]
- Nygaard I, Brubaker L, Chai TC, Markland AD, Menefee SA, Sirls L, et al. Risk factors for urinary tract infection following incontinence surgery. International Urogynecology Journal 2011;22(10):1255‐65. [sr‐incont42698] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter H, Goode P, Brubaker L, Zyczynski H, Stoddard A, Dandreo K, et al. Two‐year outcomes after surgery for stress urinary incontinence in older versus younger women (Abstract number 95). Neurourology and Urodynamics 2008;27(7):682‐3. [sr‐incont31854] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter HE, Brubaker L, Stoddard AM, Xu Y, Zyczynski HM, Norton P, et al. Patient related factors associated with long‐term urinary continence after Burch colposuspension and pubovaginal fascial sling surgeries. Journal of Urology 2012;188(2):485‐9. [sr‐incont45162] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter HE, Burgio KL, Brubaker L, Moalli PA, Markland AD, Mallet V, et al. Factors associated with incontinence frequency in a surgical cohort of stress incontinent women. American Journal of Obstetrics and Gynecology. 2005;193(6):2088‐93. [sr‐incont21231] [DOI] [PubMed] [Google Scholar]
- Richter HE, Diokno A, Kenton K, Norton P, Albo M, Kraus S, et al. Predictors of treatment failure 24 months after surgery for stress urinary incontinence. Journal of Urology 2008;179(3):1024‐30. [sr‐incont27213] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter HE, Diokno AC, Kenton K, Norton P, Albo M, Kraus S, et al. Predictors of treatment failure 24 months after surgery for stress urinary incontinence (Abstract number 5 Oral). Journal of Pelvic Medicine and Surgery 2007;13(5):227‐8. [sr‐incont34197] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter HE, Goode PS, Brubaker L, Zyczynski H, Stoddard AM, Dandreo KJ, et al. Two‐year outcomes after surgery for stress urinary incontinence in older compared with younger women. Obstetrics and Gynecology 2008;112(3):621‐9. [sr‐incont29193] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter HE, Kenton K, Huang L, Nygaard I, Kraus S, Whitcomb E, et al. The impact of obesity on urinary incontinence symptoms, severity, urodynamic characteristics and quality of life. Journal of Urology 2010;183(2):622‐8. [sr‐incont49290] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rickey LM, Huang L, Rahn DD, Hsu Y, Litman HJ, Mueller ER. Risk factors for urgency incontinence in women undergoing stress urinary incontinence surgery. Advances in Urology 2013;2013:567375. [sr‐incont50474] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steers WD, NCT00064662. Comparison of surgical procedures to reduce urinary stress incontinence (SISTEr) [Randomized clinical trial of the Burch modified Tanagho and autologous fascia sling procedures for women with predominantly stress urinary incontinence]. clinicaltrials.gov/show/NCT00064662 (first received 11 July 2003). [NCT00064662; sr‐incont49815]
- Subak LL, Brubaker L, Chai TC, Creasman JM, Diokno AC, Goode PS, et al. High costs of urinary incontinence among women electing surgery to treat stress incontinence. Obstetrics and Gynecology 2008;111(4):899‐907. [sr‐incont27122] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subak LL, Goode PS, Brubaker L, Kusek JW, Schembri M, Lukacz ES, et al. Urinary incontinence management costs are reduced following Burch or sling surgery for stress incontinence. American Journal of Obstetrics and Gynecology 2014;211(2):171‐7. [sr‐incont62600] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tennstedt S, Borello‐France D, FitzGerlad MP, Goode P, Kraus S, Kusek J, et al. Identification of factors related to health‐related quality of life in women with stress urinary incontinence that may improve with surgical treatment (Abstract number 321). Proceedings of the International Continence Society (ICS), 35th Annual Meeting, 2005 Aug 28‐Sep 2, Montreal, Canada. 2005. [sr‐incont21098]
- Tennstedt S, Urinary Incontinence Treatment Network. Design of the Stress Incontinence Surgical Treatment Efficacy trial (SISTEr). Urology 2005;66(6):1213‐7. [sr‐incont21530] [DOI] [PubMed] [Google Scholar]
- Tennstedt SL, FitzGerald MP, Nager CW, Xu Y, Zimmern P, Kraus S, et al. Quality of life in women with stress urinary incontinence. International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(5):543‐9. [sr‐incont30914] [DOI] [PubMed] [Google Scholar]
- Tennstedt SL, Litman HJ, Zimmern P, Ghetti C, Kusek JW, Nager CW, et al. Quality of life after surgery for stress incontinence. International Urogynecology Journal. 2008;19(12):1631‐8. [sr‐incont31221] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh LP, Zimmern PE, Pope N, Shariat SF, Urinary Inc. Comparison of the Q‐tip test and voiding cystourethrogram to assess urethral hypermobility among women enrolled in a randomized clinical trial of surgery for stress urinary incontinence.[see comment]. Journal of Urology 2006;176(2):646‐9, discussion 650. [sr‐incont22387] [DOI] [PubMed] [Google Scholar]
- Zimmern P, Nager CW, Albo M, FitzGerald MP, McDermott S, Urinary Incontinence Treatment Network. Interrater reliability of filling cystometrogram interpretation in a multicenter study. Journal of Urology 2006;175(6):2174‐7. [sr‐incont22424] [DOI] [PubMed] [Google Scholar]
- Zimmern P, Tennstedt S, Dickinson T, Dandreo K. Lessons learned from a patient burden survey following a large randomized controlled trial for the surgical management of stress urinary incontinence in women (Abstract number 152). Neurourology and Urodynamics 2009;28(7):770‐1. [20805; sr‐incont39356] [Google Scholar]
- Zimmern P, Urinary Incontinence Treatment Network (UITN). Design of the SISTEr (Stress Incontinence Surgical Treatment Efficacy Trial) study: a randomized surgical trial comparing Burch colposuspension and the autologous rectus fascia sling. A clinical trial of the NIH/NIDDK urinary incontinence treatment network (UITN) (Abstract number 81). Progres en Urologie 2004;14(3 Suppl 3):26. [sr‐incont19780] [Google Scholar]
- Zimmern PE, Dandreo KJ, Sirls L, Howell A, Hall L, Gruss J, et al. Lessons from a patient experience survey in a randomized surgical trial of treatment of stress urinary incontinence in women. International Urogynecology Journal 2011;22(10):1273‐8. [sr‐incont42697] [DOI] [PMC free article] [PubMed] [Google Scholar]
Amaro 2007 {published data only}
- Amaro JL, Yamamoto H, Kawano PR, Barros G, Gameiro MO, Agostinho AD. Clinical and quality‐of‐life outcomes after autologous fascial sling and tension‐free vaginal tape: a prospective randomized trial. International Brazilian Journal of Urology 2009;35(1):60‐6; discussion 66‐7. [sr‐incont31437] [DOI] [PubMed] [Google Scholar]
- Amaro JL, Yamamoto HA, Kawano PR, Fugita O, Gameiro MOO, Barros G, et al. A prospective randomized trial of autologous fascial sling (AFS) versus tension‐free vaginal tape (TVT) for treatment of stress urinary incontinence (SUI) (Poster abstract number 1460). Journal of Urology 2007;177(4 Suppl 4):482. [sr‐incont23764] [Google Scholar]
- NCT00565838, Amaro JL. Quality‐of‐life outcomes after autologous fascial sling and TVT: a prospective randomized trial [Clinical and quality‐of‐life outcomes after autologous fascial sling and tension‐free vaginal tape: a prospective randomized trial]. clinicaltrials.gov/show/NCT00565838 (first received 30 November 2007). [NCT00565838; sr‐incont59990] [DOI] [PubMed]
Arunkalaivanan 2003 {published data only}
- Abdel‐Fattah M, Arunkalaivanan AS, Barrington JW. Pelvicol (trademark) implant v TVT (trademark): an update (Abstract). Proceedings of the 27th Annual Meeting of the International Urogynecological Association, 2002 Aug 21‐24, Prague, Czech Republic. 2002. [sr‐incont22144]
- Abdel‐Fattah M, Barrington JW, Arunkalaivanan AS. Pelvicol pubovaginal sling versus tension‐free vaginal tape for treatment of urodynamic stress incontinence: a prospective randomized three‐year follow‐up study. European Urology 2004;46(5):629‐35. [sr‐incont19434] [DOI] [PubMed] [Google Scholar]
- Arunkalaivan AS, Barrington JW. Randomized trial of porcine dermal sling (Pelvicol TM implant) vs. tension‐free vaginal tape (TVT) in the surgical treatment of stress incontinence: a questionnaire‐based study. International Urogynecology Journal 2003;14:17‐23. [sr‐incont16033] [DOI] [PubMed] [Google Scholar]
- Arunkalaivanan AS, Barrington JW. Comparison of porcine pubovaginal sling (Pelvicol) vs tension free vaginal tape (TVT) in the surgical management of stress incontinence (Abstract). International Urogynecology Journal 2001;12(Suppl 3):S21. [sr‐incont16333] [DOI] [PubMed] [Google Scholar]
Bai 2005 {published data only}
- Bai SW, Sohn WH, Chung DJ, Park JH, Kim SK. Comparison of the efficacy of Burch colposuspension, pubovaginal sling, and tension‐free vaginal tape for stress urinary incontinence. International Journal of Gynaecology and Obstetrics 2005;91(3):246‐51. [sr‐incont21260] [DOI] [PubMed] [Google Scholar]
Barbalias 1997 {published data only}
- Barbalias G, Liatsikos E, Barbalias D. Use of slings made of indigenous and allogenic material (Goretex) in type III urinary incontinence and comparison between them. European Urology 1997;31(4):394‐400. [sr‐incont5560] [DOI] [PubMed] [Google Scholar]
Basok 2008 {published data only}
- Basok EK, Yildirim A, Atsu N, Basaran A, Tokuc R. Cadaveric fascia lata versus intravaginal slingplasty for the pubovaginal sling: surgical outcome, overall success and patient satisfaction rates. Urologia Internationalis 2008;80(1):46‐51. [sr‐incont26435] [DOI] [PubMed] [Google Scholar]
Choe 2000 {published data only}
- Choe JM. The use of synthetic materials in pubovaginal sling. Advances in Experimental Medicine and Biology 2003;539(Pt A):481‐92. [DOI: 10.1007/978-1-4419-8889-8_33; sr‐incont19205; PUBMED: 15088924] [DOI] [PubMed] [Google Scholar]
- Choe JM, Ogan K, Battino BS. Antimicrobial mesh versus vaginal wall sling: a comparative outcomes analysis [see comments]. Journal of Urology 2000;163(6):1829‐34. [sr‐incont11144] [PubMed] [Google Scholar]
Demirci 2001 {published data only}
- Demirci F, Yucel O. Comparison of free rectus fascial sling and Burch colposuspension procedures in type I and type II genuine stress incontinence (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction 2000;11(Suppl 1):S48. [sr‐incont13419] [Google Scholar]
- Demirci F, Yucel O. Comparison of pubovaginal sling and Burch colposuspension procedures in type I/II genuine stress incontinence. Archives of Gynecology and Obstetrics 2001;265(4):190‐4. [sr‐incont13079] [DOI] [PubMed] [Google Scholar]
Enzelsberger 1996 {published data only}
- Enzelsberger H, Helmer H, Schatten C. Comparison of Burch and lyodura sling procedures for repair of unsuccessful incontinence surgery. Obstetrics and Gynecology 1996;88(2):251‐6. [sr‐incont2759] [DOI] [PubMed] [Google Scholar]
- Enzelsberger H, Kurz C, Seifert M, Raimann H, Schatten C. Surgical treatment of recurrent stress incontinence: Burch versus lyodura sling operation ‐ a prospective study [Zur operativen Behandlung der RezidivstreBinkontinenz: Burch versus Lyoduraschlingeoperation ‐ eine prospektive studie]. Geburtshilfe und Frauenheilkunde 1993;53(7):467‐71. [sr‐incont100] [DOI] [PubMed] [Google Scholar]
Fischer 2001 {published data only}
- Fischer JR, Hale DS, McClellan E, Benson JT. The use of urethral electrodiagnosis to select the method of surgery in women with intrinsic sphincter deficiency (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction 2001;12(Suppl 1):S33. [sr‐incont12008] [Google Scholar]
Guerrero 2008 {published data only}
- Guerrero K, Whareham K, Watkins A, Ismail S, Lucas M, Emery S. A randomised control trial comparing TVT, Pelvicol and autologous fascial slings for the management of stress urinary incontinence in women (Abstract number 1). Neurourology and Urodynamics 2008;27(7):571. [sr‐incont31847] [Google Scholar]
- Guerrero KL, Emery SJ, Wareham K, Ismail S, Watkins A, Lucas MG. A randomised controlled trial comparing TVT, Pelvicol and autologous fascial slings for the treatment of stress urinary incontinence in women. BJOG 2010;117(12):1493‐502. [sr‐incont40338] [DOI] [PubMed] [Google Scholar]
- Khan Z, Nambiar A, Emery S, Lucas M. Long term follow‐up of a multicentre randomised controlled trial comparing TVT, Pelvicol (tm) and autologous fascial slings for the treatment of stress urinary incontinence in women (Abstract number 637). Neurourology and Urodynamics 2014;33(6):937‐8. [NCT01057550; sr‐incont64340] [Google Scholar]
- Khan ZA, Nambiar A, Morley R, Chapple CR, Emery SJ, Lucas MG. Long‐term follow‐up of a multicentre randomised controlled trial comparing tension‐free vaginal tape, xenograft and autologous fascial slings for the treatment of stress urinary incontinence in women. BJU International 2015;115(6):968‐77. [sr‐incont68156] [DOI] [PubMed] [Google Scholar]
- Lucas M. Sling operation for stress urinary incontinence: randomized trial of three operative procedures. UK National Research Register 2001. [sr‐incont16379]
- Lucas M, Emery S, Alan W, Kathy W. Failure of porcine xenograft sling in a randomised controlled trial of three sling materials in surgery for stress incontinence (Abstract). Proceedings of the International Continence Society (34th Annual Meeting) and the International UroGynecological Association, 2004 Aug 23‐27, Paris. 2004:Abstract number 309. [sr‐incont19056]
- NCT01057550, Lucas MG, Guerrero K. Randomised controlled trial comparing tension‐free vaginal tape (TVT), Pelvicol & autologous slings for stress urinary incontinence (SUI) [A randomised controlled trial comparing TVT, Pelvicol and autologous fascial slings for the treatment of stress urinary incontinence in women]. clinicaltrials.gov/show/NCT01057550 (first received 27 January 2010). [NCT01057550; sr‐incont59998]
- Nambiar AK, Khan ZA, Morley R, Chapple CR, Emery SJ, Lucas MG. Long term follow‐up of a multicentre randomised controlled trial comparing TVT, Pelvicol (TM) and autologous fascial slings for the treatment of stress urinary incontinence in women (Abstract number P67). BJU International 2014;113(Suppl S5):50‐1. [sr‐incont64349] [DOI] [PubMed] [Google Scholar]
Helmy 2012 {published data only}
- Helmy H, El‐Gamal S. Three‐year continence rates, satisfaction and adverse events of Burch urethropexy and fascial sling surgery for urinary incontinence (Abstract number 589). Proceedings of the 42nd Annual Meeting of the International Continence (ICS), 2012 Oct 15 to 19, Beijing, China. 2012. [sr‐incont45471]
Henriksson 1978 {published data only}
- Henriksson L, Asmussen M, Löfgren O, Ulmsten U. A urodynamic comparison between abdominal urethrocystopexy and vaginal sling plasty in female stress incontinence. Urologia Internationalis 1978;33:111‐6. [sr‐incont5152] [Google Scholar]
- Henriksson L, Ulmsten U. A urodynamic evaluation of the effects of abdominal urethrocystopexy and vaginal sling urethroplasty in women with stress incontinence. American Journal of Obstetrics and Gynecology 1978;131(1):77‐82. [sr‐incont2670] [DOI] [PubMed] [Google Scholar]
Hilton 1989 {published data only}
- Hilton P. A clinical and urodynamic study comparing the Stamey bladder neck suspension and suburethral sling procedures in the treatment of genuine stress incontinence. British Journal of Obstetrics and Gynaecology 1989;96(2):213‐20. [sr‐incont453] [DOI] [PubMed] [Google Scholar]
Kondo 2006 {published data only}
- Kondo A, Isobe Y, Kimura K, Kamihira O, Matsuura O. A randomized control trial of tension‐free vaginal tape vs pubovaginal sling: cure rates and QOL improvement (Abstract number 629). Proceedings of the International Continence Society (ICS), 35th Annual Meeting, 2005 Aug 28‐Sep 2, Montreal, Canada. 2005. [sr‐incont21077]
- Kondo A, Isobe Y, Kimura K, Kamihira O, Matsuura O, Gotoh M, et al. Efficacy, safety and hospital costs of tension‐free vaginal tape and pubovaginal sling in the surgical treatment of stress incontinence. Journal of Obstetrics and Gynaecology Research 2006;32(6):539‐44. [sr‐incont22233] [DOI] [PubMed] [Google Scholar]
- Kondo A, Kimura K, Isobe Y, Kamihira O, Matsuura O. A randomised control trial of tension‐free vaginal tape in comparison with pubovaginal sling in the treatment of stress incontinence (Abstract). Neurourology and Urodynamics 2003;22(5):485‐7. [sr‐incont17109] [Google Scholar]
Lucas 2000 {published data only}
- Guerrero K, Watkins A, Emery S, Wareham K, Stephenson T, Logan V, et al. A randomised controlled trial comparing two autologous fascial sling techniques for the treatment of stress urinary incontinence in women: short, medium and long‐term follow‐up. International Urogynecology Journal 2007;18(11):1263‐70. [sr‐incont23957] [DOI] [PubMed] [Google Scholar]
- Lucas M, Emery S, Stephenson T, Wareham K, Cheung I. A randomised study to assess and compare the clinical effectiveness of two surgical techniques for the treatment of stress urinary incontinence in women. Spotlight (Newsletter of The Wales Office of Research) 2000. [sr‐incont12901]
- Lucas M, Emery S, Stephenson T, Wareham K, Cheung I, Russell I, et al. A randomised study to assess and compare the clinical effectiveness of two surgical techniques for the treatment of stress urinary incontinence in women. Report No. RC080. Cardiff, Wales, UK: The Wales Office of Research & Development for Health & Social Care, 2000. [sr‐incont8995] [Google Scholar]
Maher 2005 {published data only}
- Maher CF, Dwyer PL, Carey MP, Cornish A, Schluter PJ. Pubovaginal sling or transurethral Macroplastique for genuine stress incontinence and intrinsic sphincter deficiency: a prospective randomised trial (Abstract). International Urogynecology Journal 2001;12(Suppl 3):S9. [sr‐incont14360] [DOI] [PubMed] [Google Scholar]
- Maher CF, O'Reilly BA, Dwyer PL, Carey MP, Cornish A, Schluter P. Pubovaginal sling versus transurethral Macroplastique for stress urinary incontinence and intrinsic sphincter deficiency: a prospective randomised controlled trial. BJOG 2005;112(6):797‐801. [sr‐incont20579] [DOI] [PubMed] [Google Scholar]
Okulu 2013 {published data only}
- Okulu E, Aldemir M, Onen E, Kayigil O. Use of three types of synthetic mesh materials in sling surgery: a prospective randomized clinical trial evaluating effectiveness and complications (Abstract number S136). European Urology Supplements 2012;11(4):166. [sr‐incont62135] [DOI] [PubMed] [Google Scholar]
- Okulu E, Kayigil O, Aldemir M, Onen E. The use of three types of synthetic mesh materials in the surgery for stress incontinence: the clinical results (Abstract number 765). International Urogynecology Journal and Pelvic Floor Dysfunction 2011;22(2 Suppl):S1024‐5. [sr‐incont62216] [Google Scholar]
- Okulu E, Kayigil O, Aldemir M, Onen E. Use of three types of synthetic mesh material in sling surgery: a prospective randomized clinical trial evaluating effectiveness and complications. Scandinavian Journal of Urology 2013;47(3):217‐24. [sr‐incont48505] [DOI] [PubMed] [Google Scholar]
- Okulu E, NCT01348334. Synthetic mesh materials in sling surgery [Use of three types of synthetic mesh materials in sling surgery: a prospective randomized clinical trial evaluating effectiveness and complications]. clinicaltrials.gov/show/NCT01348334 (first received 5 May 2011). [NCT01348334; sr‐incont42756]
Osman 2003 {published data only}
- Osman T. Stress incontinence surgery for patients presenting with mixed incontinence and a normal cystometrogram. BJU International 2003;92:964‐8. [sr‐incont16660] [DOI] [PubMed] [Google Scholar]
Pacetta 2005 {published data only}
- Pacetta AM, Carramao SS, Limoge DC, Mendes V, Date A, Sousa E, et al. Stress urinary incontinence: a prospective randomized study comparing FortaPerm to autologous fascia (Abstract number 109). International Urogynecology Journal 2005;16(Suppl 2):S58. [sr‐incont29163] [Google Scholar]
Sand 2000 {published data only}
- Culligan PJ, Goldberg RP, Sand PK. A randomized controlled trial comparing a modified Burch procedure and a suburethral sling: long‐term follow‐up. International Urogynecology Journal 2003;14(4):229‐33. [sr‐incont16706] [DOI] [PubMed] [Google Scholar]
- Culligan PJ, Winkler HA, Blackhurst DW, Sand PK. A prospective randomized study of modified Burch retro pubic urethropexy and suburethral sling for genuine stress incontinence and low pressure urethra (Abstract). Proceedings of the International Continence Society (ICS), 28th Annual Meeting, 1998 Sept 14‐17, Jerusalem, Israel. 1998:133. [sr‐incont5689]
- Goldberg RP, Sand PK, Koduri S, Culligan PJ. A prospective randomized study comparing modified Burch retropubic urethropexy and suburethral sling: long term follow‐up [abstract]. International Urogynaecology Journal 2001;12(Suppl 1):S6. [sr‐incont12004] [Google Scholar]
- Sand PK, Winkler H, Blackhurst DW, Culligan PJ. A prospective randomized study comparing modified Burch retropubic urethropexy and suburethral sling for treatment of genuine stress incontinence with low‐pressure urethra. American Journal of Obstetrics and Gynecology 2000;182(1 Pt 1):30‐4. [sr‐incont9013] [DOI] [PubMed] [Google Scholar]
Sharifiaghdas 2008 {published data only}
- Sharifiaghdas F, Mortazavi N. Tension‐free vaginal tape and autologous rectus fascia pubovaginal sling for the treatment of urinary stress incontinence: a medium‐term follow‐up. Medical Principles and Practice 2008;17(3):209‐14. [31878; sr‐incont27098] [DOI] [PubMed] [Google Scholar]
Sharifiaghdas 2015 {published data only}
- Sharifiaghdas F, Nasiri M, Mirzaei M, Narouie B. Mini sling (Ophira) versus pubovaginal sling for treatment of stress urinary incontinence: a medium‐term follow‐up. Prague Medical Report 2015;116(3):210‐8. [DOI: 10.14712/23362936.2015.60; sr‐incont69267] [DOI] [PubMed] [Google Scholar]
Shin 2001 {published data only}
- Shin MS, Kim JH, Koh JS, Jung JH. Comparison of the results of sling procedure using autologous dermal graft patch and cadaveric fascia lata as a sling material for stress urinary incontinence (Abstract). Proceedings of the International Continence Society (ICS), 31st Annual Meeting, 2001 Sept 18‐21, Seoul, Korea. 2001:Abstract number 313. [sr‐incont14477]
Silva Filho 2006 {published data only}
- Silva‐Filho AL, Candido EB, Noronha A, Triginelli SA. Comparative study of autologous pubovaginal sling and synthetic transobturator (TOT) SAFYRE sling in the treatment of stress urinary incontinence. Archives of Gynecology and Obstetrics 2006;273(5):288‐92. [sr‐incont21600] [DOI] [PubMed] [Google Scholar]
Song 2004 {published data only}
- Song YF, Huang HJ, Xu B, Hao L. Comparative study of tension‐free vaginal tape and fascia lata for stress urinary incontinence [Chinese]. Chung‐Hua Fu Chan Ko Tsa Chih [Chinese Journal of Obstetrics and Gynecology] 2004;39(10):658‐61. [sr‐incont20768] [PubMed] [Google Scholar]
Tcherniakovsky 2009 {published data only}
- Tcherniakovsky M, Fernandes CE, Bezerra CA, Roy CA, Wroclawski ER. Comparative results of two techniques to treat stress urinary incontinence: synthetic transobturator and aponeurotic slings. International Urogynecology Journal 2009;20(8):961‐6. [sr‐incont32120] [DOI] [PubMed] [Google Scholar]
Teixeira 2008 {published data only}
- Teixeira M, Pinto AR, Montalvao M, Candoso B. Systemic and local inflammatory response in collagen vs. polypropylene tapes for stress urinary incontinence: is there any difference? (Abstract number 527). Proceedings of the 38th Annual Meeting of the International Continence Society (ICS), 2008 Oct 20‐24, Cairo, Egypt. 2008. [sr‐incont31878]
Teleb 2011 {published data only}
- Teleb M, Salem EA, Naguib M, Kamel M, Hasan U, Elfayoumi AR, et al. Evaluation of transvaginal slings using different materials in the management of female stress urinary incontinence. Arab Journal of Urology 2011;9(4):283‐7. [sr‐incont59731] [DOI] [PMC free article] [PubMed] [Google Scholar]
Viseshsindh 2003 {published data only}
- Viseshsindh W, Kochakarn W, Waikakul W, Roongruangsilp U. A randomized controlled trial of pubovaginal sling versus vaginal wall sling for stress urinary incontinence. Journal of the Medical Association of Thailand 2003;86(4):308‐15. [sr‐incont15733] [PubMed] [Google Scholar]
Wadie 2005 {published data only}
- Wadie B, Henawy A. Does urethral pressure measurement correlate to the outcome of incontinence surgery? (Abstract number 546). Proceedings of the 37th Annual Meeting of the ICS, 2007 Aug 20‐24, Rotterdam, The Netherlands. 2007. [sr‐incont26689]
- Wadie BS, Edwan A, Nabeeh A. Autologous fascial sling verus polypropylene tape at short term follow up, a prospective randomized study (Abstract number 636). Proceedings of the International Continence Society (ICS), 35th Annual Meeting, 2005 Aug 28‐Sep 2, Montreal, Canada. 2005. [sr‐incont21100]
- Wadie BS, Edwan A, Nabeeh AM. Autologous fascial sling vs polypropylene tape at short‐term followup: a prospective randomized study. Journal of Urology 2005;174(3):990‐3. [sr‐incont20796] [DOI] [PubMed] [Google Scholar]
- Wadie BS, Hefnawy AS. Urethral pressure measurement in stress incontinence: does it help?. International Urology and Nephrology 2009;41(3):491‐5. [sr‐incont32131] [DOI] [PubMed] [Google Scholar]
- Wadie BS, Mansour A, El‐Hefnawy AS, Nabeeh A, Khair AA. Minimum 2‐year follow‐up of mid‐urethral slings, effect on quality of life, incontinence impact and sexual function. International Urogynecology Journal 2010;21(12):1485‐90. [sr‐incont41437] [DOI] [PubMed] [Google Scholar]
Zargham 2013 {published data only}
- Zargham M, Alizadeh F, Tadayyon F, Khorrami M‐H, Nouri‐Mahdavi K, Gharaati MR, et al. Concomitant surgical correction of severe stress urinary incontinence and anterior vaginal wall prolapse by anterior vaginal wall wrap: 18 months outcomes. Journal of Research in Medical Sciences 2013;18(7):588‐93. [sr‐incont59874] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Amat 2007 {published data only}
- Amat LL, Franco EM, Saavedra AH, Martinez AV. Needleless (R): A new technique for correction of urinary incontinence. Randomized controlled trial compared with TVT‐O (R). Preliminary results (Abstract number 225). International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(Suppl 1):S128. [27329] [Google Scholar]
Atherton 2000 {published data only}
- Atherton MJ, Stanton SL. TVT and colposuspension: comparisons and contrasts of possible mechanisms (Abstract). Neurourology and Urodynamics 2000;19(4):396‐8. [Google Scholar]
Aurunkalaivanan 2001 {published data only}
- Arunkalaivanan AS, Barrington JW. Comparison of porcine pubovaginal sling (Pelvicol) vs tension free vaginal tape (TVT) in the surgical management of stress incontinence (Abstract). International Urogynecology Journal 2001;12(Suppl 3):S21. [DOI] [PubMed] [Google Scholar]
Barrington 2003 {published data only}
- Barrington JW. Pelvicol implant vs TVT ‐ a randomised prospective study. Proceedings of the BARD Satellite Symposium to the International Continence Society Annual Meeting, 7 Oct. 2003; Vol. 8.
Brandt 2009 {published data only}
- Brandt FT, Lorenzato F, Albuquerque CDC, Machado AS, Poca AC, Viana RA. Tension‐free vaginal tape versus lata fascia sling: the importance of transvulvar ultrasound in the assessment of relevant anatomical parameters in treatment of women with stress urinary incontinence. Indian Journal of Urology 2009;25(1):62‐7. [sr‐incont42535] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bruschini 2005 {published data only}
- Bruschini H, Nunes R, Truzzi JC, Simonetti R, Cury J, Ortiz V, et al. Low cost polypropylene sling procedure for correction of stress urinary incontinence: a possible solution for developing countries? (Abstract number 360). Proceedings of the International Continence Society (ICS), 35th Annual Meeting, 2005 Aug 28‐Sep 2, Montreal, Canada. 2005. [21055]
Choe 2001 {published data only}
- Choe JM. Sling surgery performed with and without preoperative urodynamics: a comparative outcomes analysis. Proceedings of the International Continence Society (ICS), 31st Annual Meeting, 2001 Sept 18‐21, Seoul, Korea. 2001:Abstract number 175.
Chong 2003 {published data only}
- Chong C, Bane A, Corstiaans A. Intraoperative division of tensionless vaginal tape (TVT) ‐ prospective randomized trial (Abstract). Singapore Journal of Obstetrics and Gynaecology 2003;34(Suppl 1):55. [Google Scholar]
Corcos 2001 {published data only}
- Corcos J, Collet JP, Shapiro S, Herschorn S, Radomski SB, Schick E, et al. Multicenter randomized clinical trial comparing surgery and collagen injections for treatment of female stress urinary incontinence. Urology 2005;65(5):898‐904. [20346] [DOI] [PubMed] [Google Scholar]
- Corcos J, Collet JP, Shappiro S, Schick E, Macramallah E, Tessier J, et al. Surgery vs collagen for the treatment of female stress urinary incontinence (SUI): results of a multicentric randomized trial (Abstract). Journal of Urology 2001;165(5 Suppl):198. [Google Scholar]
Darai 2007 {published data only}
- Darai E, Frobert JL, Grisard‐Anaf M, Lienhart J, Fernandez H, Dubernard G, et al. Functional results after the suburethral sling procedure for urinary stress incontinence: a prospective randomized multicentre study comparing the retropubic and transobturator routes. European Urology 2007;51(3):795‐802. [22550] [DOI] [PubMed] [Google Scholar]
- David‐Montefiore E, Frobert JL, Grisard‐Anaf M, Liehart J, Fernandez H, Dubernard G, et al. Functional results after suburethral sling procedure for urinary stress incontinence at 1 year: a French prospective randomised multicentre study comparing the retropubic and transobturator routes (Abstract number 063). International Urogynecology Journal 2006;17(Suppl 2):S95. [Google Scholar]
- David‐Montefiore E, Frobert JL, Grisard‐Anaf M, Lienhart J, Bonnet K, Poncelet C, et al. Peri‐operative complications and pain after the suburethral sling procedure for urinary stress incontinence: a French prospective randomised multicentre study comparing the retropubic and transobturator routes. European Urology 2006;49(1):133‐8. [21623] [DOI] [PubMed] [Google Scholar]
Debodinance 1993 {published data only}
- Debodinance P. Comparison of the Bologna and Ingelman‐Sundberg procedures for stress incontinence associated with genital prolapse: ten‐year follow‐up of a prospective randomized study [French]. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction 2000;29(2):148‐53. [PubMed] [Google Scholar]
- Debodinance P, Querleu D. Comparison of the Bologna and Ingelman‐Sundber procedures for stress incontinence associated with genital prolapse: prospective randomized study. European Journal of Obstetrics, Gynecology, and Reproductive Biology 1993;52(1):35‐40. [DOI] [PubMed] [Google Scholar]
Debodinance 1994 {published data only}
- Debodinance P, Bievre P, Parmentier D, Dubrulle R, Querleu D, Crepin G. The "hazards" of using a Gore‐Tex sling in the treatment of stress urinary incontinence [French]. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction 1994;23(6):665‐70. [3127] [PubMed] [Google Scholar]
Gamble 2010 {published data only}
- Gamble T, Du H, Roger G, Nguyen A, Vu M, Gafni‐Kane A, et al. TVT versus bladder neck sling in the treatment of low pressure urethra (Abstract number 243). Neurourology and Urodynamics 2010;29(6):1154‐5. [sr‐incont40162] [Google Scholar]
Giri 2004 {published data only}
- Giri SK, Hickey JP, Macdonald J, Narasimahulu G, Cashman E, Drumm J, et al. Prospective, randomised trial of xenograft versus rectus fascia pubovaginal sling in the treatment of stress urinary incontinence [abstract number 13]. Irish Journal of Medical Science 2004;173(1 Suppl 1):18. [29716] [Google Scholar]
Giri 2006 {published data only}
- Giri SK, Hickey JP, Sil D, Mabadeje O, Shaikh FM, Narasimhulu G, et al. The long‐term results of pubovaginal sling surgery using acellular cross‐linked porcine dermis in the treatment of urodynamic stress incontinence. Journal of Urology 2006;175(5):1788‐92; discussion 1793. [22459] [DOI] [PubMed] [Google Scholar]
- Giri SK, Sil D, Drumm J, Mabadeje O, Narasimahulu G, Flood HD. Is acellular porcine dermis material durable for pubovaginal sling surgery? (Abstract number 349). Proceedings of the International Continence Society (ICS), 35th Annual Meeting, 2005 Aug 28‐Sep 2, Montreal, Canada. 2005. [21068]
Goldberg 2001 {published data only}
- Goldberg RP, Koduri S, Lobel RW, Culligan PJ, Tomezsko JE, Winkler HA, et al. Long‐term effects of three different anti‐incontinence procedures on the posterior compartment (Abstract). Proceedings of the International Continence Society (ICS), 31st Annual Meeting, 2001 Sept 18‐21, Seoul, Korea. 2001:Abstract number 243.
Halaska 2001 {published data only}
- Halaska M, Kolbl H, Petri E, Danes L, Voigt R, Otcenasek M, et al. Preliminary results of a prospective randomized study comparing Burch colposuspension and tension‐free vaginal tape ‐ urodynamic and sexuological aspects. Neurourology and Urodynamics 2001;20(4):421‐2. [Google Scholar]
Han 2001 {published data only}
- Han WHC. Burch colposuspension or tension‐free vaginal tape for female stress urinary incontinence?. International Urogynecology Journal and Pelvic Floor Dysfunction 2001;12(Suppl 3):S23. [DOI] [PubMed] [Google Scholar]
Hung 2001 {published data only}
- Hung MJ. Tension free vaginal tape versus traditional polypropylene pubovaginal sling for the treatment of stress urinary incontinence (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction 2001;12(Suppl 3):253. [Google Scholar]
Ishenko 1999 {published data only}
- Ishenko AI, Slobodenyuk AI, Chushkov YV. Modified pereyra and sling procedures in combined surgical treatment in patients with uterine prolapse and stress urinary incontinence ‐ randomized study. European Journal of Obstetrics, Gynecology, and Reproductive Biology 1999;86(Suppl):S15. [Google Scholar]
Kocjancic 2008 {published data only}
- Kocjancic E, Constantini E, Crivellaro S, Tosco L, Grossetti B, Frea B, et al. Mixed incontinence: the best solution for a difficult task (Abstract number 485). Proceedings of the 38th Annual Meeting of the International Continence Society (ICS), 2008 Oct 20‐24, Cairo, Egypt. 2008.
- Kocjancic E, Constantini E, Giannantoni A, Crivellaro S, Mearini L, Frea B, et al. Tension free vaginal tape (TVT) and trans obturator suburethral tape (TOT): a prospective randomized study (Poster abstract number 1462). Proceedings of the American Urological Association (AUA), Annual Meeting, 2007 May 19‐24, Anaheim, CA. 2007. [23765]
Kuo 2001 {published data only}
- Kuo HC. Comparison of video urodynamic results after the pubovaginal sling procedure using rectus fascia and polypropylene mesh for stress urinary incontinence. Journal of Urology 2001;165(1):163‐8. [DOI] [PubMed] [Google Scholar]
Kwon 2002 {published data only}
- Kwon C, Goldberg R, Sanjay G, Sumana K, Krotz S, Sand P. Protective effect of transvaginal slings on recurrent anterior vaginal wall prolapse after pelvic reconstructive surgery (abstract). Neurourology and Urodynamics 2002;21(4):321‐2. [Google Scholar]
Lemieux 1991 {published data only}
- Lemieux MC, Kung R, Drutz HP. Suprapubic clamping routine after anti‐incontinence surgery: a randomized prospective study comparing continuous vs intermittent clamping (Abstract). Proceedings of the American Urogynecology Society, 12th Annual Meeting, 1991 Oct 23‐26, California, USA. 1991.
Liapis 2002 {published data only}
- Liapis A, Bakas P, Creatsas G. Burch colposuspension and tension‐free vaginal tape in the management of stress urinary incontinence in women. European Urology 2002;41(4):469‐73. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Liapis A, Bakas P, Creatsas G. Comparison of open retropubic colposuspension with tension‐free vaginal tape for the treatment of genuine stress incontinence in women (Abstract). Neurourology and Urodynamics 2000;19(4):385‐6. [Google Scholar]
Lim 2005 {published data only}
- Lim YN, Muller R, Corstiaans A, Dietz HP, Barry C, Rane A. Suburethral slingplasty evaluation study in North Queensland, Australia: the SUSPEND trial. Australian & New Zealand Journal of Obstetrics & Gynaecology 2005;45(1):52‐9. [DOI] [PubMed] [Google Scholar]
Meschia 2001 {published data only}
- Meschia M, Spennacchio M, Amicarelli F, Pifarotti P, Cavoretto P, Stoppelli S. A randomized prospective comparison of TVT and endopelvic fascia plication in the treatment of occult stress urinary incontinence in patients with genital prolapse: preliminary data (Abstract). Neurourology and Urodynamics 2001;20(4):423‐4. [Google Scholar]
Naumann 2006 {published data only}
- Naumann G, Lobodasch K, Bettin S, Meyer P, Koelbl H. Tension free vaginal tape (TVTtm) vs less invasive free tape (LIFTtm) ‐ a randomized multicentric study of suburethral sling surgery (Abstract number 481). Proceedings of the International Continence Society (ICS), 36th Annual Meeting, 2006 Nov 27‐Dec 1, Christchurch, New Zealand. 2006.
O'Sullivan 2000 {published data only}
- O'Sullivan S, Avery N, Bailey A, Keane D. The effect of surgery on the collagen metabolism of paraurethral tissue in women with genuine stress incontinence. International Urogynaecology Journal. 11 2000; Vol. 11, issue Suppl 1:S5. [11903]
Obrink 1978 {published data only}
- Obrink A, Bunne G. The margin to incontinence after three types of operation for stress incontinence. Scandinavian Journal of Urology and Nephrology 1978;12(3):209‐14. [DOI] [PubMed] [Google Scholar]
Oremus 2010 {published data only}
- Oremus M, Tarride JE. An economic evaluation of surgery versus collagen injection for the treatment of female stress urinary incontinence. Canadian Journal of Urology 2010;17(2):5087‐93. [sr‐incont39605] [PubMed] [Google Scholar]
Palomba 2008 {published data only}
- Palomba S, Zullo F, NCT00744198. Autologous versus synthetic versus biological sling for trans‐obturator correction of urinary stress incontinence [A comparison in terms of efficacy and safety among three different materials for trans‐obturator correction of urinary stress incontinence: autologous, synthetic and biological sling]. clinicaltrials.gov/show/NCT00744198 (first received 29 August 2008). [NCT00744198; sr‐incont49349]
Schostak 2001 {published data only}
- Schostak M, Gottfried HW, Heicappell R, Muller M, Sauter T, Steiner U, et al. Minimally invasive bone anchoring for female stress incontinence: a treatment with moderate results (Abstract). European Urology 2001;39(Suppl 5):3. [Google Scholar]
Seo 2007 {published data only}
- Seo JH, Lee JW, Kim DY, Lee YG, Seo YJ, Kwon TG, et al. Treatment of obstructive voiding dysfunction after transobturator sling surgery: results of multicenter study (Abstract number 287). Proceedings of the 37th Annual Meeting of the International Continence Society (ICS), 2007 Aug 20‐24, Rotterdam, The Netherlands. 2007. [23762]
Trezza 2001 {published data only}
- Trezza G, Rotondi M, Palmisano B, Iervolino P. Uterovaginal prolapse and occult urinary incontinence: a prospective randomized study on the necessity to associate reconstructive surgery and antiincontinence procedure. Urogynaecologia International Journal 2001;15(1 Suppl):152‐4. [Google Scholar]
Wang 1999 {published data only}
- Wang AC. Local anesthesia is superior to epidural blockade in tension‐free vaginal tape installation. International Urogynecology Journal and Pelvic Floor Dysfunction. 10 1999; Vol. 10, issue Suppl 1:S13.
Ward 2002a {published data only}
- Abrams P, Martin K, Bulmer P, Donovan J, Hilton P. Responsiveness of the Bristol female lower urinary tract symptoms questionnaire (BFLUTS‐Q) to surgical intervention in a randomised controlled trial. Proceedings of the International Continence Society (ICS), 30th Annual Meeting, 2000 Aug 28‐31, Tampere, Finland. 2000:A173.
- Sculpher MJ, Ward KL, Hilton P, on behalf of the UK & Ireland TVT Trial Group. A comparison of the hospital costs of tension free vaginal tape (TVT) and colposuspension. Neurourology and Urodynamics. 19 2000; Vol. 19, issue 4:333‐4.
- Ward K, Hilton P, on behalf of the UK & Ireland TVT Trial Group. A randomised trial of colposuspension and tension‐free vaginal tape (TVT) for primary genuine stress incontinence ‐ 2 yr follow‐up (Abstract). International Urogynaecological Association, Pelvic Floor Dysfunction. 12 2001; Vol. 12, issue Suppl 3:S7.
- Ward K, Hilton P, on behalf of the United Kingdom and Ireland Tension‐free Vaginal Tape Trial Group. Prospective multicentre randomised trial of tension‐free vaginal tape and colposuspension as primary treatment for stress incontinence. British Medical Journal 2002;325(7355):67‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward KL, Hilton P, Browning J. A randomized trial of colposuspension and tension‐free vaginal tape (TVT) for primary genuine stress incontinence (Abstract number 7A). Neurourology and Urodynamics 2000;19(4):386‐8. [Google Scholar]
- Ward KL, Hilton P, Browning J. Urodynamic variables in a randomised comparison of colposuspension and tension‐free vaginal tape (TVT) for primary GSI (Abstract number 7B). Neurourology and Urodynamics 2000;19(4):388‐9. [Google Scholar]
Yoo 2007 {published data only}
- Yoo ES, Jung HC, Shin HS, Seo JH, Seo YJ. Comparison of the two different approaches for the treatment of female stress urinary incontinence (Abstract number 282). Proceedings of the 37th Annual Meeting of the International Continence Society (ICS), 2007 Aug 20‐24, Rotterdam, The Netherlands. 2007.
References to studies awaiting assessment
Abou Hashem 2017 {published data only}
- Abou Hashem S, Mohamed Mostafa M, Elbrombely W. Five‐years follow‐up of tension‐free vaginal tape (TVT) versus rectus sheath sling for surgical treatment of female stress urinary incontinence: a comparative study (Abstract number 863). European Urology Supplements 2017;16(3):e1503. [sr‐incont78114] [Google Scholar]
Hassan 2018 {published data only}
- Hassan SM, NCT03473041. Autologous rectus sheath fascia versus midurethral transobturator tension free vaginal [Surgeon tailored hybrid autologus rectus sheath fascia versus midurethral transobturator tension free vaginal tape for treatment of stress urinary incontinence]. clinicaltrials.gov/show/NCT03473041 (first received 21 March 2018). [NCT03473041; sr‐incont77874]
Kajbafzadeh 2017 {published data only}
- Kajbafzadeh A, Mohseni M, IRCT201611278554N3. Use of acellular sling graft for stress urinary incontinence [Investigating effectiveness of using tissue engineered skin instead of mesh in pubovaginal tape procedure in stress urinary incontinence]. en.irct.ir/trial/9046 (first received 28 May 2017). [IRCT201611278554N3; sr‐incont76181]
Sharifiaghdas 2017 {published data only}
- Sharifiaghdas F, Mirzaei M, Daneshpajooh A, Narouie B. Long‐term results of tension‐free vaginal tape and pubovaginal sling in the treatment of stress urinary incontinence in female patients. Clinical and Experimental Obstetrics & Gynecology 2017;44(1):44‐7. [sr‐incont75581] [PubMed] [Google Scholar]
References to ongoing studies
Hilton 2000 {unpublished data only}
- Hilton P. A prospective randomised comparative trial of a tension‐free vaginal tape (TVT) and fascial sling procedure for "secondary" genuine stress incontinence. UK National Research Register 2002. [sr‐incont16383]
Zhu 2014 {published data only}
- NCT02106299, Zhu L, Tian Q. Safety and efficacy study of Regen sling to treatment SUI [A multi‐center, randomized, controlled clinical trial of the safety and efficacy of Regen sling treatment for female patients with stress urinary incontinence]. clinicaltrials.gov/show/NCT02106299 (first received 8 April 2014). [NCT02106299; sr‐incont61984]
Additional references
Abrams 2006
- Abrams P, Artibani W, Cardozo L, Dmochowski R, Kerrebroeck P, Sand P. Reviewing the ICS 2002 terminology report: the ongoing debate. Neurourology and Urodynamics 2006;25(3):293. [sr‐incont22055] [DOI] [PubMed] [Google Scholar]
Agarwal 2017
- Agarwal BK, Agarwal N. Urinary incontinence: prevalence, risk factors, impact on quality of life and treatment seeking behaviour among middle aged women. International Surgery Journal 2017;4(6):1953‐8. [Google Scholar]
Amaral 2015
- Amaral MO, Coutinho EC, Nelas PA, Chaves CM, Duarte JC. Risk factors associated with urinary incontinence in Portugal and the quality of life of affected women. International Journal of Gynecology and Obstetrics 2015;131(1):82‐6. [DOI] [PubMed] [Google Scholar]
Berman 1997
- Berman CJ, Kreder KJ. Comparative cost analysis of collagen injection and fascia lata sling cystourethropexy for the treatment of type III incontinence in women. Journal of Urology 1997;157(1):122‐4. [PubMed] [Google Scholar]
Blaivas 1988
- Blaivas JG, Olsson CA. Stress incontinence: classification and surgical approach. Journal of Urology 1988;139(4):727‐31. [DOI] [PubMed] [Google Scholar]
Cody 2003
- Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al. Systematic review of the clinical effectiveness and cost‐effectiveness of tension‐free vaginal tape for treatment of urinary stress incontinence. Health Technology Assessment 2003;7(21):iii, 1‐189. [DOI] [PubMed] [Google Scholar]
Culligan 2003
- Culligan PJ, Goldberg RP, Sand PK. A randomized controlled trial comparing a modified Burch procedure and a suburethral sling: long‐term follow‐up. International Urogynecology Journal 2003;14(4):229‐33. [DOI] [PubMed] [Google Scholar]
Dean 2017
- Dean N, Ellis G, Herbison GP, Wilson D, Mashayekhi A. Laparoscopic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. [DOI: 10.1002/14651858.CD002239.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Debodinance 2000
- Debodinance P. Comparison of the Bologna and Ingelman‐Sundberg procedures for stress incontinence associated with genital prolapse: ten‐year follow‐up of a prospective randomized study [French]. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction 2000;29(2):148‐53. [PubMed] [Google Scholar]
EndNote 2018 [Computer program]
- Clarivate Analytics. EndNote. Version X8.2. Philadelphia (PA): Clarivate Analytics, 2018.
Ford 2017
- Ford AA, Rogerson L, Cody JD, Aluko P, Ogah J. Mid‐urethral sling operations for stress urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. [DOI: 10.1002/14651858.CD006375.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Glazener 2017a
- Glazener CMA, Cooper K, Mashayekhi A. Anterior vaginal repair for urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. [DOI: 10.1002/14651858.CD001755.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Glazener 2017b
- Glazener CMA, Cooper K, Mashayekhi A. Bladder neck needle suspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. [DOI: 10.1002/14651858.CD003636.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2011a
- Guyatt GH, Oxman AD, Schunemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. Journal of Clinical Epidemiology 2011;64(4):380‐2. [DOI] [PubMed] [Google Scholar]
Guyatt 2011b
- Guyatt GH, Oxman AD, Sultan S, Glasziou P, Akl EA, Alonso‐Coello P, et al. GRADE guidelines: 9. Rating up the quality of evidence. Journal of Clinical Epidemiology 2011;64(12):1311‐6. [DOI] [PubMed] [Google Scholar]
Guyatt 2013a
- Guyatt GH, Thorlund K, Oxman AD, Walter SD, Patrick D, Furukawa TA, et al. GRADE guidelines: 13. Preparing Summary of Findings tables and evidence profiles ‐ continuous outcomes. Journal of Clinical Epidemiology 2013;66(2):173‐83. [DOI] [PubMed] [Google Scholar]
Guyatt 2013b
- Guyatt GH, Oxman AD, Santesso N, Helfand M, Vist G, Kunz R, et al. GRADE guidelines: 12. Preparing Summary of Findings tables ‐ binary outcomes. Journal of Clinical Epidemiology 2013;66(2):158‐72. [DOI] [PubMed] [Google Scholar]
Haylen 2010
- Haylen BT, Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. International Urogynecology Journal and Pelvic Floor Dysfunction 2010;21(1):5‐26. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org. Available from: www.cochrane‐handbook.org: The Cochrane Collaboration.
Jackson 1996
- Jackson S, Donovan J, Brookes S, Eckford S, Swithinbank L, Abrams P. The Bristol Female Lower Urinary Tract Symptoms questionnaire: development and psychometric testing. British Journal of Urology 1996;77(6):805‐12. [DOI] [PubMed] [Google Scholar]
Kilonzo 2004
- Kilonzo M, Vale L, Stearns S, Grant A, Cody J, Glazener C, et al. Cost effectiveness of tension‐free vaginal tape for the surgical management of female stress incontinence. International Journal of Technology Assessment in Health Care 2004;20(4):455‐63. [DOI] [PubMed] [Google Scholar]
Kirchin 2017
- Kirchin V, Page T, Keegan PE, Atiemo K, Cody JD, McClinton S, et al. Urethral injection therapy for urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. [DOI: 10.1002/14651858.CD003881.pub4] [DOI] [PubMed] [Google Scholar]
Kumar 2017
- Kumar S, Ghildayal N, Ghildayal N. Markov chain decision model for urinary incontinence procedures. International Journal of Health Care Quality Assurance 2017;30(2):187‐202. [sr‐incont74304] [DOI] [PubMed] [Google Scholar]
Lapitan 2003
- Lapitan MC, Cody JD. Open retropubic colposuspension for urinary stress incontinence in women. Cochrane Database of Systematic Reviews 2003, Issue 1. [DOI: 10.1002/14651858.CD002912] [DOI] [Google Scholar]
Lapitan 2017
- Lapitan MCM, Cody JD, Mashayekhi A. Open retropubic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. [DOI: 10.1002/14651858.CD002912.pub7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lasserre 2009
- Lasserre A, Pelat C, Gueroult V, Hanslik T, Chartier‐Kastler E, Blanchon T, et al. Urinary incontinence in French women: prevalence, risk factors, and impact on quality of life. European Urology 2009;56(1):177‐83. [DOI] [PubMed] [Google Scholar]
McGuire 1993
- McGuire EJ, Fitzpatrick CC, Wan J, Bloom D, Sanvordenker J, Ritchey M, et al. Clinical assessment of urethral sphincter function. Journal of Urology 1993;150(5 Pt 1):1452‐4. [DOI] [PubMed] [Google Scholar]
McGuire 2004
- McGuire EJ. Pathophysiology of stress urinary incontinence. Reviews in Urology 2004;6 Suppl 5:S11‐7. [PMC free article] [PubMed] [Google Scholar]
Moehrer 2002
- Moehrer B, Ellis G, Carey M, Wilson PD. Laparoscopic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2002, Issue 2. [DOI: 10.1002/14651858.CD002239] [DOI] [PubMed] [Google Scholar]
Nambiar 2017
- Nambiar A, Cody JD, Jeffery ST, Aluko P. Single‐incision sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. [DOI: 10.1002/14651858.CD008709.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
NICE 2013
- National Collaborating Centre for Women's and Children's Health, NHS National Institute for Health and Clinical Excellence (NICE). Urinary incontinence: the management of urinary incontinence in women. NICE Clinical Guideline (CG171). London, UK: Royal College of Obstetricians and Gynaecologists; 2013. Available at guidance.nice.org.uk/CG171/NICEGuidance/pdf/English (accessed 22 June 2015).
O'Donnell 1994
- O'Donnell P. Goals of therapy and mechanisms of urethral incontinence. In: McGuire EJ, Kursh ED editor(s). Female Urology. 1st Edition. Philadelphia (PA): JB Lippincott Company, 1994:175‐201. [Google Scholar]
Shemilt 2010
- Shemilt I, Thomas J, Morciano M. A web‐based tool for adjusting costs to a specific target currency and price year. Evidence and Policy 2010;6(1):51‐9. [Google Scholar]
Shemilt 2019
- Shemilt I, Aluko P, Graybill E, Craig D, Henderson C, Drummond M, et al. on behalf of the Campbell and Cochrane Economics Methods Group. Chapter 20. Economic evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Smith 2002
- Smith ARB, Daneshgari F, Dmochowski R, Ghoniem G, Jarvis GJ, Nitti V, et al. Surgical treatment of incontinence in women. Incontinence. 2nd International Consultation on Incontinence. Plymouth, UK: Health Publication Ltd, 2002. [Google Scholar]
Subak 2014
- Subak LL, Goode PS, Brubaker L, Kusek JW, Schembri M, Lukacz ES. Urinary incontinence management costs are reduced following Burch or sling surgery for stress incontinence. American Journal of Obstetrics & Gynecology 2014;211(2):171.e171‐7. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Villoro 2016
- Villoro R, Merino M, Hidalgo‐Vega A, Jimenez M, Martinez L, Aracil J. Women with urinary incontinence in Spain: health‐related quality of life and the use of healthcare resources. Maturitas 2016;94:52‐7. [DOI: ] [DOI] [PubMed] [Google Scholar]
Ward 2002b
- Ward K, Hilton P, on behalf of the UK & Ireland TVT Trial Group. Prospective multicentre randomised trial of tension‐free vaginal tape and open colposuspension as primary treatment for stress incontinence. BMJ 2002;325:67‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ware 1993
- Ware JE, Snow KK, Kosinski M, Gandek B. SF‐36 Health Survey Manual and Interpretation Guide. Boston (MA): The Health Institute, New England Medical Centre, 1993. [Google Scholar]
References to other published versions of this review
Bezerra 1999
- Bezerra CA, Bruschini H. Sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 1999, Issue 3. [DOI: 10.1002/14651858.CD001754] [DOI] [Google Scholar]
Bezerra 2000
- Bezerra CA, Bruschini H. Suburethral sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2000, Issue 3. [DOI: 10.1002/14651858.CD001754] [DOI] [PubMed] [Google Scholar]
Bezerra 2001
- Bezerra CA, Bruschini H, Cody DJ. Suburethral sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2001, Issue 3. [DOI: 10.1002/14651858.CD001754] [DOI] [PubMed] [Google Scholar]
Bezerra 2005
- Bezerra CCB, Bruschini H, Cody JD. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD001754.pub2] [DOI] [PubMed] [Google Scholar]
Rehman 2011
- Rehman H, Bezerra CCB, Bruschini H, Cody JD. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2011, Issue 1. [DOI: 10.1002/14651858.CD001754.pub3] [DOI] [PubMed] [Google Scholar]
Rehman 2017
- Rehman H, Bezerra CA, Bruschini H, Cody JD, Aluko P. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 7. [DOI: 10.1002/14651858.CD001754.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]


