Abstract
Sternal precautions are a universal part of the discharge education for post-sternotomy patients to reduce the risk of sternal complications. However, they are always designed based on physical therapists’ or surgeons’ subjective judgment without any objective evidence. Thus, they could be overly restrictive to hinder the patients’ recovery, physically and psychologically. To fill this gap, this paper proposes a digital biomarker to estimate chest expansion during sit-to-stand transitions based on wearable inertial sensing and data fusion technologies. First, we carried out bench tests to evaluate the reliability of the digital biomarker to represent relative sensor rotation. We also verified effectiveness of this digital biomarker to detect subtle skin extension in proactive chest expansion trials by 11 healthy volunteers. Then, we measured the digital biomarker during sit-to-stand transitions with different strategies and some daily routine activities (walking, sitting, and standing) performed by the healthy volunteers and 22 post-sternotomy patients. The comparison between these measurements evaluated the effectiveness of several known guidelines of sternal precautions for sit-to-stand transitions. The results showed that first, pushing up from a chair by taking support from armrests induced larger chest expansion (p = 0.009) compared with sit-to-stand transition while keeping the arms relaxed; second, crossing the arms or hugging a pillow can help reduce chest expansion (p < 0.05) compared with keeping the arms relaxed during sit-to-stand transitions; third, pushing up while taking support from a frontal support (e.g., table or walker) induced the same level of chest expansion (p > 0.05) as that during sit-to-stand transition while keeping the arms relaxed.
Keywords: Sternal precaution, sit-to-stand transition, chest expansion, digital biomarker, wearable sensor
I. Introduction
Sternal complications after median sternotomy can lead to increased morbidity, decreased quality of life, prolonged hospitalization with increased healthcare costs, and even account for mortality rates of 15% to 40% [1]. Most of the sternal complications occur after patients’ discharge from the hospital [2], so sternal precautions are provided as a universal part of discharge education. Sternal precautions generally represent a series of physical activity restrictions to avoid excessive chest expansion in daily living. For example, for the first week after the surgery, post-sternotomy patients are generally instructed to cross their arms or hug a pillow when performing any sit-to-stand transitions [3]. The patients are not allowed to take support from armrests of the chairs [3]. However, a number of recent studies have shown that current sternal precautions could be overly restrictive to hinder the patients’ recovery and even contribute to functional limitation, emotional stress, and physical inactivity [3], [4]. Additionally, there is considerable diversity in the guidelines on sternal precautions between different healthcare providers, raising both clinicians’ and patients’ doubts about the necessity of performing such restrictions [3].
The limitations of the current sternal precautions are caused by having a lack of any objective measure to evaluate stress on the sternum and the overlying skin. Current guidelines of sternal precautions are designed based on surgeons’ and physical therapists’ subjective consensus without quantitative scientific evidence. The direct measurement of the stress on the sternum of a post-surgery patient would be invasive and would raise ethical concerns [5]. Therefore, a few studies used mechanical modeling methods to estimate the stress on the sternum based on distending pressure (the difference between internal and external pressure) and radius and length of the thoracic cavity [6]–[8]. In recent years, several studies investigated sternal skin deformation to provide new insights into the surrogate evaluation of sternal stress due to chest expansion. These studies used digital camera, ultrasonic Doppler, or electromagnetic tracking technologies [9]–[11]. However, all of these studies were conducted in a laboratory environment involving only healthy volunteers rather than patients, potentially because of the lack of a portable device to conveniently measure subtle skin motion caused by chest expansion.
In this study, we focus on investigating chest expansion during sit-to-stand transitions, since a safe behavior of sit-to-stand transitions is always emphasized in multiple versions of sternal precaution education provided by different healthcare providers [3], [4]. We propose a wearable sensor-based digital biomarker to represent skin deformation related to chest expansion during sit-to-stand transitions. Two flexible sensors are attached to the skin of the left and right pectoralis major below the clavicular, respectively. The maximum yaw rotation angle of one sensor in relation to the other sensor is defined as, the digital biomarker, since the sternal dehiscence mostly occurs in the medial-lateral direction rather than the anterior-posterior or superior-inferior directions [7], and separation of the sternum in the medial-lateral direction does not need to overcome bone-on-bone frictional force [5]. This digital biomarker is extracted from the fusion of triaxial acceleration and triaxial angular velocity signals. A bench test (rotation of two sensors on the table) validates the reliability of the digital biomarker to represent relative rotation between the sensors. We also verified the effectiveness of this digital biomarker to detect skin extension based on observations of proactive chest expansion tests carried out by healthy volunteers. Then, the digital biomarker was measured during sit-to-stand transitions with different strategies (arm relaxed, arm crossed, armrest push-up, or frontal push-up), in addition to few daily routine activities (sitting, standing, and walking), performed by healthy volunteers and/or post-sternotomy patients. Using the measurements from the digital biomarker from these trials, the goal was to examine: 1) whether the sit-to-stand transition with an armrest push-up strategy causes larger chest expansion than that with an arm relaxed strategy (no use of the arms), 2) whether any sternal precaution strategy of using the arms (arm crossed, hugging a pillow, or frontal push-up) during sit-to-stand transition is effective in reducing chest expansion compared to an arm relaxed strategy.
II. Method
A. Definition of the Digital Biomarker
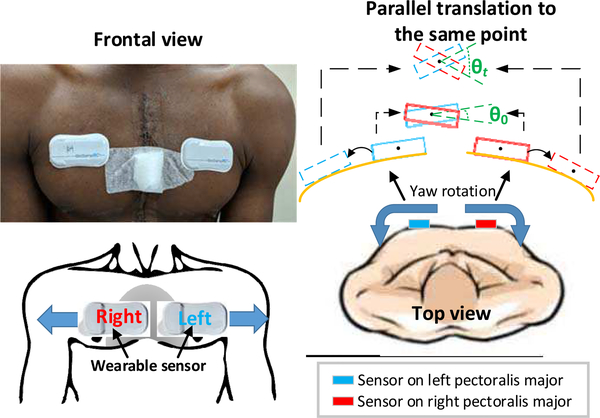
When chest skin deforms due to chest expansion, the two wearable sensors attached to the skins of the left and right pectoralis major will have an opposite rotation in yaw direction (Fig. 1), considering that the thoracic cavity can be approximated to be an elliptic cylinder [6]. Therefore, the yaw rotation of one sensor in relation to the other sensor (θ = θt−θ0 in Fig. 1, where θ0 represents the initial relative orientation between the two sensors in yaw direction at the start of the sit-to-stand transition, and θt represents the relative orientation at time point t during the sit-to-stand transition) can be described as the estimation of skin deformation due to chest expansion. The proposed digital biomarker in this study (Max Expansion Angle, abbr: MEA) is defined as the maximum magnitude of relative yaw rotation angle signal (θ) during the period of the sit-to-stand transition.
Fig. 1.
Sensors attached to a post-sternotomy patient subject and sensor movements corresponding to chest skin expansion during sit-to-stand transitions.
B. Algorithm
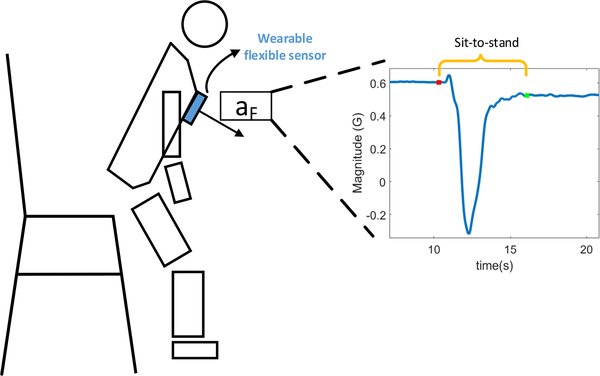
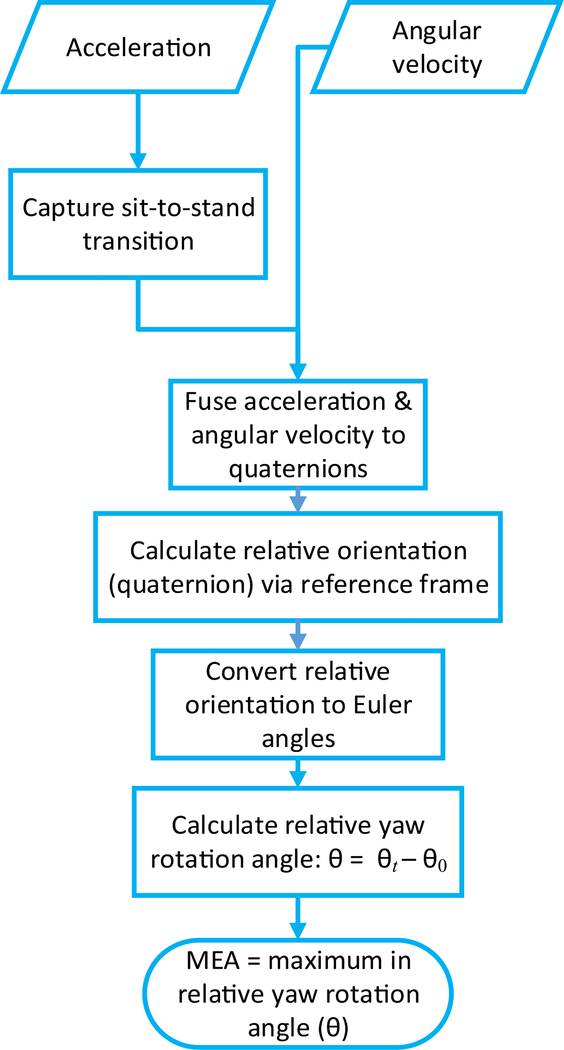
The digital biomarker, MEA, is extracted from triaxial acceleration and triaxial angular velocity signals during the sit-to-stand transition period. The sit-to-stand transition period can be captured based on a negative peak in the frontal acceleration signal of either the sensor on the left or right pectoralis major (aF in Fig. 2) [12]. In the period of a sit-to-stand transition, triaxial acceleration and triaxial angular velocity signals are fused to obtain the orientation of the sensors in terms of quaternions using a gradient descent algorithm developed by Madgwick [13]. At time point t, the relative orientation between the two sensors is computed based on the fact that the orientation obtained from sensor fusion for both sensors are with reference to the same inertial frame [14], and then the relative orientation in quaternion is converted to the Euler angle [15]. In the yaw direction, the difference between relative orientation (Euler angle) at time point t (θt) and the initial relative orientation at the start point of the sit-to-stand transition (θ0) is a sample of relative yaw rotation angle signal (θ). The MEA is the maximum of the relative yaw rotation angle signal for the entire sit-to-stand period. The flowchart of the algorithm is shown in Fig. 3.
Fig. 2.
Detection of a period of sit-to-stand transition based on negative peak in acceleration in the frontal direction.
Fig. 3.
Flow chart of the algorithm to extract max expansion angle (MEA) from acceleration and angular velocity signals during the sit-to-stand transition, where θ, θt, and θ0 refer to the definition of the biomarker (subsection A of section II) and Fig. 1.
When we extracted MEA from proactive chest expansion and daily routine activities, the sit-to-stand transition capture module of the algorithm was not activated. In the data of a proactive chest expansion, MEA was extracted from a signal segment manually centered around the peak of the angular velocity signal. In the data of a daily routine activity, MEA was extracted from a 4-second signal segment centered during the whole period of the activity.
III. Tests
Two flexible wearable sensors (BioStampRC, MC10 Inc., Lexington, MA, USA) were used in a bench test and in trials involving healthy volunteers and post-sternotomy patients. The dimension of each BioStampRC sensor used was 66×34×4.5 mm, and it weighed 7 g. Triaxial accelerometer and triaxial gyroscope housed inside the BioStampRC sensor were configured to continuously collect acceleration and angular velocity signals, respectively, at 125 Hz. The protocol of human trials was approved by the Institutional Review Board of the Baylor College of Medicine (Houston, TX, USA).
A. Bench Test
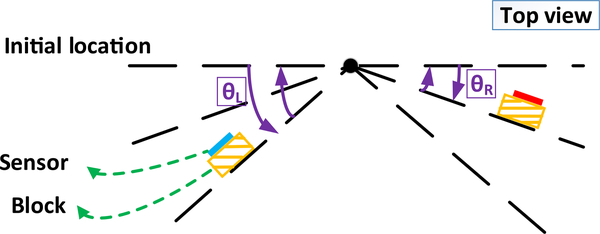
In the bench test, two wearable sensors were attached to vertical planes of the two blocks kept on the table, and the sensors were rotated about a vertical axis, along with the blocks, to simulate yaw rotation of one sensor in relation to the other sensor during chest expansion. The rotations about the other axes, or linear movements along any of the axes were not tested, considering that the digital biomarker is solely derived from relative yaw rotation between the two sensors. In each rotation test, the two blocks were placed along a straight line initially. Then, the two blocks with the sensors were rotated in the opposite direction following scale marks on the paper: the left one was rotated by a predefined angle (θL in Fig. 4) in the anticlockwise direction (top view), and the right one was rotated by a predefined angle (θR in Fig. 4) in the clockwise direction (top view). After the rotation, the two blocks remained static for five seconds at their respective new locations. Finally, the two blocks were rotated back to the initial location. Theoretically, the MEA extracted from the sensor signals should approximate the relative rotation angle (RRA = θL + θR) according to the paper scale. The RRA was set between 5° and 40° with 5 degrees as the minimal scale. Each rotation test with a specific RRA was repeated three times to control errors caused by human factors.
Fig. 4.
Sensor and block movements in bench tests and the corresponding expansion angle signal.
B. Trial Involving Healthy Volunteers
Healthy volunteers were recruited from the staffs and students at the Baylor College of Medicine. The tasks included proactive chest expansion, three types of sit-to-stand transitions (arm relaxed, armrest push up, and arm crossed), and daily routine activities (sitting, standing, and walking). The task of proactive chest expansion was used to qualitatively verify whether chest expansion causes a positive magnitude of MEA. The tasks of daily routine activities were used to determine the non-risky MEA level in daily living. Each task was conducted only once and lasted for about 30 seconds. At the start of each task, the volunteer was asked to remain still for about 10 seconds, and the acceleration and angular velocity signals collected during this period were used as a baseline to remove the offset of sensor signals. Then, the volunteer was instructed to conduct a specific task. If the task was proactive chest expansion or sit-to-stand transition, the volunteer would be asked to remain still after he/she finished the action. On the other hand, if the task was one of the daily routine activities, the volunteer would be asked to remain in that activity for the remaining time of that task.
In the proactive chest expansion, the volunteer was asked to first lift his/her arms to the chest level and then do chest expansion once as much as possible, at their preferred speed. In the sit-to-stand transition with an arm relaxed strategy, the volunteer was asked to stand up without any support from the upper extremities. In the sit-to-stand transition with an armrest push-up strategy, the volunteer was asked to stand up using his/her upper extremities to take support from the armrests of the chair. In the sit-to-stand transition with an arm crossed strategy, the volunteer was asked first to cross his/her arms and then stand up.
C. Trial Involving Post-Sternotomy Patients
Post-sternotomy patients participated in our trial during their follow-up visit (typically, three to four weeks after the surgery) at Harris Health Ben Taub Hospital (Houston, TX, USA). These patients were asked to perform the same tasks as the healthy volunteers, except the proactive chest expansion and sit-to-stand transition with an armrest push-up strategy. It is because that these two actions may induce excessive chest expansion and are always prohibited in known sternal precaution guidelines [3]. Especially, a chair without arms was used in the tasks of sit-to-stand transitions for patients to avoid the case that the patient subconsciously adopted the armrest push-up strategy.
Additionally, a subset of post-sternotomy patients performed two new strategies during sit-to-stand transitions: while hugging a pillow, and frontal push-up. In the sit-to-stand transition while hugging a pillow, the patient was asked to hug a pillow first and then stand up. In the sit-to-stand transition with a frontal push-up strategy, the patient was asked to stand up using his/her upper extremities to take support from a hard surface in front of his/her body (a bed in the clinic room with a height of 81.3 cm). We tested different strategies used during sit-to-stand transitions to find the most effective way to reduce chest expansion during sit-to-stand transitions. Table I shows all tasks in the trials involving healthy volunteers and post-sternotomy patients.
TABLE I.
The Tasks of Human Trials
| Seq. | Tasks | Healthy | Patient |
|---|---|---|---|
| 0 | Proactive chest expansion | ✓ | × |
| 1 | Sit-to-stand, arm relaxed | ✓ | ✓ |
| 2 | Sit-to-stand, armrest push-up | ✓ | × |
| 3 | Sit-to-stand, arm crossed | ✓ | ✓ |
| 4 | Sit-to-stand, hug pillow | × | ✓ |
| 5 | Sit-to-stand, frontal push-up | × | ✓ |
| 6 | Walk | ✓ | ✓ |
| 7 | Sit | ✓ | ✓ |
| 8 | Stand | ✓ | ✓ |
Symbol ‘✓’ represents the cohort of participants performs the corresponding task. Symbol ‘×’ represents the cohort of participants does NOT performs the corresponding task.
D. Statistical Analyses
Statistical analyses were performed using IBM SPSS Statistics version 24 (IBM, Armonk, NY, USA). For all statistical analyses, p < 0.05 was considered statistically significant.
For the dataset of the bench test, absolute and relative agreements between the MEA and the RRA were tested using intraclass correlation coefficients (ICC2,1) and using Pearson’s correlation coefficients (r), respectively. The cutoff of ICC2,1 is that values below 0.50 indicate poor reliability, values between 0.50 and 0.75 indicate moderate reliability, values between 0.75 and 0.90 indicate good reliability, and values above 0.90 indicate excellent reliability [16]. The cutoff of r is that values below 0.35 indicate weak correlation, values between 0.35 and 0.67 indicate moderate correlation and values between 0.68 and 1.0 indicate strong correlation [17].
For the dataset of the trials involving healthy volunteers, paired sample t-tests were used to compare the MEA of the sit-to-stand transition with an arm relaxed strategy to the ones of the sit-to-stand transition with armrest push-up and arm crossed strategies, as well as the daily routine activities.
For the dataset of the trials involving post-sternotomy patients, paired sample t-tests were used to compare MEA of the sit-to-stand transition with an arm relaxed strategy to the ones of the sit-to-stand transition with an arm crossed strategy, as well as the daily routine activities.
Specially, for the dataset of the subset of post-sternotomy patients who performed three different arm-involved sternal precaution strategies during sit-to-stand transitions, repeated measures ANOVA was used to analyze the difference between MEA measurements of sit-to-stand transitions with strategies of arm crossed, hugging a pillow, and frontal push-up. Then, paired sample t-tests were used to compare the MEA of the sit-to-stand transition with an arm relaxed strategy to the ones of arm-involved sit-to-stand transitions.
Additionally, independent sample t tests were used to compare MEA between the groups of healthy volunteers and post-sternotomy patients for sit-to-stand transitions with the same strategies and the same daily routine activities.
IV. Results
A. Demographic Data
Healthy volunteers’ and post-sternotomy patients’ demographic information (number, sex, age, height, weight, and body mass index-BMI) is shown in Table II.
TABLE II.
Demographic Information for Healthy Volunteers and Post-Sternotomy Patients
| Healthy volunteers | Post-sternotomy patients |
||
|---|---|---|---|
| Total | Subset | ||
| Number | 11 | 22 | 10 |
| Female, N (%) | 4 (36.4) | 7 (31.8) | 3 (30) |
| Age, years | 30.2 ± 7.9 | 56.4 ± 12.4 | 56.0 ± 14.1 |
| Height, cm | 166.3 ± 6.8 | 164.9 ± 11.0 | 160.5 ± 8.9 |
| Weight, kg | 68.7 ± 13.3 | 75.8 ± 17.9 | 72.9 ± 15.0 |
| BMI, kg/m2 | 24.7 ± 3.6 | 27.7 ± 4.6 | 28.3 ± 5.3 |
The values in the rows of ‘Age’, ‘Height’, and ‘Weight’ are presented as means ± standard deviations. The values in the column “Total” are demographic information of all post-sternotomy patients, while the values in the column “Subset” are demographic information of the patients who conducted two additional sit-to-stand transitions (hugging a pillow and using a frontal push-up strategy).
B. Agreement of RRA and MEA
Table III shows predefined settings of RAA and the corresponding means of MEA measurements in the bench test. The intraclass correlation coefficient between MEA and RRA (ICC2,1 = 0.998, p < 0.001) indicates excellent reliability with statistical significance. Pearson’s correlation coefficient between MEA and RRA (r = 0.998, p < 0.001) indicates a strong correlation with statistical significance.
TABLE III.
The ΘL, ΘR, RAA, and MEA in Bench Tests
| Seq. | ΘL (°) | ΘR (°) | RRA (°) | MEA (°) |
|---|---|---|---|---|
| 1 | 5 | 0 | 5 | 5.2 |
| 2 | 5 | 5 | 10 | 10.8 |
| 3 | 10 | 5 | 15 | 14.9 |
| 4 | 10 | 10 | 20 | 21.2 |
| 5 | 15 | 10 | 25 | 25.0 |
| 6 | 15 | 15 | 30 | 30.3 |
| 7 | 20 | 15 | 35 | 36.2 |
| 8 | 20 | 20 | 40 | 41.5 |
Each value in the column of ‘MEA’ are the mean of the three repeated MEA measurements for each specific RAA.
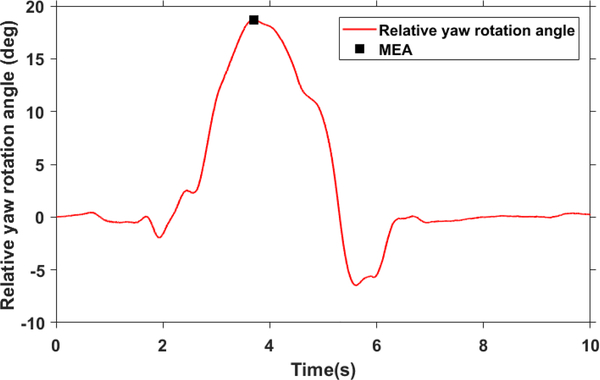
C. MEA of Proactive Chest Expansion
Fig. 5 shows an example signal of relative yaw rotation angle during a proactive chest expansion performed by a healthy volunteer. The mean and standard error of the mean (SEM) of MEA measurements across all eleven healthy volunteers’ proactive chest expansion was 14.9°± 1.5°.
Fig. 5.
Relative yaw rotation angle and its maximum magnitude (MEA) in an example proactive chest expansion by a healthy volunteer.
D. MEA of Sit-to-Stand Transitions and Daily Routine Activities
Table IV shows MEA measurements during sit-to-stand transitions with different strategies, and daily routine activities conducted by healthy volunteers and post-sternotomy patients.
TABLE IV.
The MEA Measured in Sit-to-Stand Transitions and Daily Routine Activities by Healthy Volunteers and Post-Sternotomy Patients
| MEA (°) | ||||
|---|---|---|---|---|
| healthy | patients | p | ||
| Sit-to-stand transitions | Arm relaxed | 5.5 ± 1.1 | 9.0 ± 1.5 | 0.044 |
| Armrest push-up | 8.6 ± 1.6 | N/A | ||
| Arm crossed | 2.2 ± 0.5 | 4.3 ± 1.3 | 0.069 | |
| Daily routine activities | Walking | 2.3 ± 0.3 | 3.3 ± 1.0 | 0.025 |
| Sitting | 0.4 ± 0.1 | 0.6 ± 0.2 | 0.060 | |
| Standing | 0.2 ± 0.1 | 1.3 ± 0.4 | 0.016 | |
Each MEA value in this table is presented as mean ± SEM. ‘N/A’ represents no information presented, since post-sternotomy patients did not perform sit-to-stand transition with an armrest push-up strategy considering safety issues.
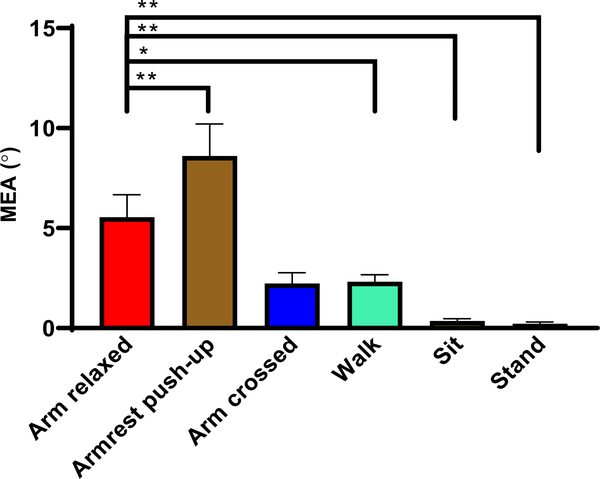
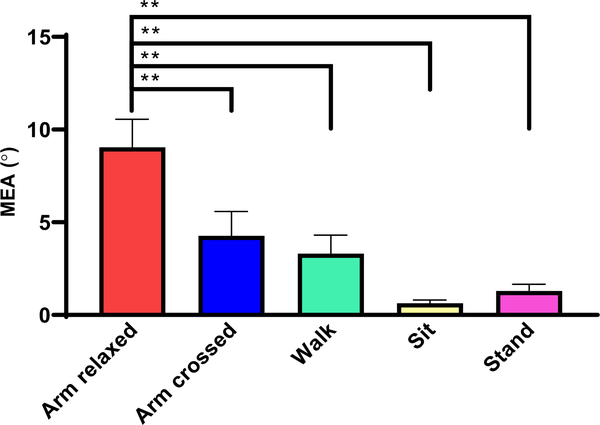
The results of paired sample t-test comparisons between the sit-to-stand transition with an arm relaxed strategy and the sit-to-stand transition with armrest push-up and/or arm crossed strategies as well as the daily routine activities are shown in Fig. 6 and Fig. 7, respectively for healthy volunteers and post-sternotomy patients. We observed that the MEA of the sit-to-stand transition with an arm relaxed strategy was significantly larger than the ones of the daily routine activities (walking, sitting, and standing), for both healthy volunteers and patients. Furthermore, in the dataset of healthy volunteers, the sit-to-stand transition with an armrest push-up strategy induced significantly larger MEA than the sit-to-stand transition with an arm relaxed strategy (p = 0.009). For post-sternotomy patients, the arm crossed strategy during sit-to-stand transitions significantly reduced MEA (p = 0.008) compared with the arm relaxed strategy. Similarly, for healthy volunteers, a reduction in the MEA was also observed in the sit-to-stand transition with an arm crossed strategy compared to the sit-to-stand transition with an arm relaxed strategy. However, it failed to reach statistical significance (p = 0.054), possibly due to the limited sample size.
Fig. 6.
The MEA (mean and SEM) of different sit-to-stand transitions and daily routine activities performed by healthy volunteers. Symbol ‘*’ represents statistical significance with p < 0.05 for difference between two tasks, and symbol ‘**’ represents statistical significance with p < 0.01 for difference between two tasks.
Fig. 7.
The MEA (mean and SEM) of sit-to-stand transitions and daily routine activities performed by all post-sternotomy patients. Symbol ‘**’ represents statistical significance with p < 0.01 for difference between two tasks.
As Table IV showed, we also observed that there were significant differences (p < 0.05) between the groups of healthy volunteers and post-sternotomy patients in the arm-relaxed sit-to-stand transition, walking and standing tasks.
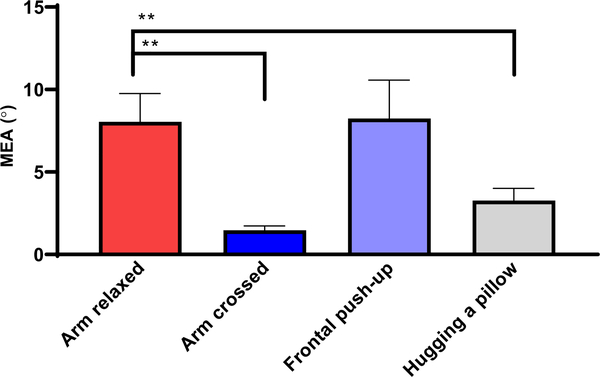
E. Comparisons of MEA Between Different Strategies for Sit-to-Stand Transitions in Post-Sternotomy Patients
In the trials performed by the subset of post-sternotomy patients, the means and SEMs of MEA measurements from sit-to-stand transitions with four different strategies of arm relaxed, arm crossed, frontal push-up, and hugging a pillow were 8.0°± 1.7°, 1.5°± 0.3°, 8.2° ± 2.3°, and 3.3°± 0.7°, respectively (Fig. 8). Repeated measures ANOVA analysis showed that there was a significant difference (p = 0.020) for MEA between sit-to-stand transitions with these strategies. Compared with the reference (the sit-to-stand transition with an arm relaxed strategy), the strategies of arm crossed and hugging a pillow were effective to reduce MEA significantly (p < 0.05), while the strategy of using front support was not (p = 0.946). The largest reduction in MEA (mean ± SEM: −6.5°± 1.7°) was observed in the sit-to-stand transition with an arm crossed strategy.
Fig. 8.
The MEA (mean and SEM) of different sit-to-stand transitions performed by a subset of post-sternotomy patients. Symbol ‘**’ represents statistical significance with p < 0.01 for difference between two tasks.
V. Discussions
To our knowledge, this is the first study to investigate chest expansion during sit-to-stand transitions using flexible wearable sensors. We propose a digital biomarker based on inertial sensing and data fusion technologies to objectively estimate chest expansion during sit-to-stand transitions with different strategies (such as armrest push-up, arm relaxed, arm crossed, frontal push-up, and hugging a pillow), as well as other daily routine activities (such as walking, sitting, and standing). The results of the bench test validated the reliability of the proposed digital biomarker to represent relative yaw rotation between the sensors. The proactive chest expansion test verified the effectiveness of the digital biomarker to detect subtle skin extension due to chest expansion. The measurements of this digital biomarker collected in the trials of healthy and patient participants determined the effective strategy (i.e., arm crossed and hugging a pillow) to reduce chest expansion during sit-to-stand transitions, compared with the arm relaxed strategy (the reference strategy with no use of the arms). Additionally, we also found that some strategy (e.g., frontal push-up) was ineffective to reduce chest expansion, and even some strategy (i.e., armrest push-up) induced larger chest expansion which should be discouraged for post-sternotomy patients. Our study provides critical evidence for surgeons and physical therapists to improve sternal precaution guidelines regarding what can be an adequate way to perform sit-to-stand transition after patients’ discharge from the hospital.
The test scenarios between healthy and patient participants were not identical. For example, for the patient population, we didn’t include the sit-to-stand transition with an armrest push-up strategy, since it could be harmful to post-sternotomy patients. On the other hand, some strategies such as hugging a pillow or frontal push-up were not tested in healthy subjects. This was because the main purpose of the tests in healthy subjects was to demonstrate the effectiveness of the proposed digital biomarker to detect skin deformation due to chest expansion rather than examine the most effective strategy to reduce chest expansion. We believe the lack of inclusion of these scenarios for healthy subjects will not affect our conclusion about the effective strategy to reduce chest expansion during sit-to-stand transitions among the patients undergoing median sternotomy. In addition, it is not guaranteed that a strategy that may be effective to reduce chest expansion in healthy subjects remained effective in post-sternotomy patients, because the post-sternotomy patients may poorly execute those strategies during sit-to-stand transitions due to the pain induced by surgical incision.
From Table IV, Fig. 6 and Fig. 7, we can see that the sit-to-stand transition with an arm relaxed strategy (i.e., without any support from the arms) induces larger chest expansion than the other daily routine activities (walking, sitting, and standing). Additionally, the patient group had larger chest expansion than the healthy group in arm relaxed sit-to-stand transitions with statistical significance (Table IV). These observations suggest that performing sit-to-stand transitions always involve notable chest expansion, especially for post-sternotomy patients with possibly frailer lower extremities and larger BMI compared to healthy volunteers. It highlights the significance of our study to find the appropriate way for post-sternotomy patients to perform sit-to-stand transitions during their post-surgery rehabilitation periods.
Based on the dataset of healthy volunteers (Fig. 6), the sit-to-stand transition with an armrest push-up strategy (pushing up from a chair) induced larger chest expansion than the sit-to-stand transition with an arm relaxed strategy (no use of the arms). Therefore, this result supports the original experience-based judgment from surgeons or physical therapists that post-sternotomy patients should not be allowed to push up from sitting to standing in their first several weeks after discharge from the hospital [18]. Irion et al. also reported a similar result that pushing up from a chair led to larger sternal skin stress than the sit-to-stand transition without using the arms, and the result was derived from Doppler acceleration measurements of skin overlying the sternum [10].
Although crossing the arms in a “self-hugging” posture or hugging a pillow has already been widely accepted as a sternal precaution strategy for sitting up and coughing or sneezing [4], [19], [20], there was no quantitative evidence to support that such restriction of the upper body can take the stress off the sternal suture line to the best of our knowledge. The presented results in Fig. 7 supports that crossing the arms during sit-to-stand transitions is indeed effective to reduce chest expansion compared to the sit-to-stand transition with an arm relaxed strategy for post-sternotomy patients. As a result, the chest expansion during the sit-to-stand transition with an arm crossed strategy was at the same level as that during walking, which can be treated to be non-risky to sternal stability. When comparing different strategies used in the sit-to-stand transition (Fig. 8), hugging a pillow was also found to be another effective way to reduce chest expansion compared with the arm relaxed strategy. However, adding a pillow to assist self-hugging posture cannot provide further reduction of chest expansion compared with the arm crossed strategy. The lowest chest expansion was still observed in the sit-to-stand transition with an arm crossed strategy.
Compared with the relatively conservative strategies (crossing the arms and hugging a pillow), the use of upper extremities while keeping the shoulder in a neutral position is allowed for the patients whose risk of sternal complication becomes low via the progress of recovery (usually two weeks after the surgery) [3]. The frontal push-up strategy tested in our study follows this moderate guideline. Our results showed that there was no significant difference in chest expansion between the sit-to-stand transitions with arm relaxed and with frontal push-up strategies (Fig. 8). Therefore, this strategy cannot provide sufficient benefits to reduce chest expansion like crossing the arms or hugging a pillow, and it should not be recommended to the patient with a high risk of sternal complication during the early postoperative period. However, from another perspective, the frontal push-up strategy outperforms the “dangerous” armrest push-up strategy (with larger chest expansion than the arm relaxed strategy as seen in the dataset of healthy adults), and hence may be recommended to the patients whose risk of sternal complication becomes low but lower extremities’ muscle force is still insufficient to perform sit-to-stand transitions independently without involving the upper extremities.
Some previous studies used piezoelectric or piezoresistive strain sensors [21], [22] or knitted conductive textiles [23], [24] to measure chest expansion for monitoring respiration rate. These studies reported the estimation of respiration rate rather than measurements of chest expansion. Thus, it is not possible to draw direct comparisons with our results about the quantity of chest expansion. These technologies (strain sensors or knitted conductive textiles) were excluded from being used in our study, since almost all of those devices were still in the development phase and only tested in a lab environment on healthy volunteers. In contrast, our study was conducted in a hospital environment involving post-sternotomy patient population with high standards for reliability and safety. The fixed appliance and wired communication of these devices could have potentially created significant difficulties in our data collection process, such as restrictions of body movements when performing sit-to-stand transitions or walking. By contrast, the flexible wearable sensors used in our study have a small form factor and can wirelessly upload the data to cloud. Additionally, they can be easily attached to or taken off from the body. As a result, all measurements could be conveniently collected during the patients’ follow-up visits in the hospital setting, avoiding their concern for additional trip to participate in the trial. Another limitation specifically for knitted conductive textiles embedded in a garment is that the garment needs to be customized to fit for each participant’s body shape, ensuring the accuracy of measurements for chest expansion. Taking on or off such tight garment is difficult for frail patients and may potentially increase the risk of sternal complications due to excess extended movements of the shoulder during this action.
Table V shows several studies investigating chest expansion during sit-to-stand transitions for sternal precaution. Irion et al. [10] and Balachandran et al. [25] used an ultrasound technique to study the motion of skin and sternal edge caused by chest expansion, respectively. Ge et al. measured sternal skin strain using a digital camera [9] and an electromagnetic tracking system [11], and chest expansion was reflected by an increase of distance between the skins overlying sternoclavicular. Interestingly, the results in the studies by Ge et al. showed that pushing up from a chair caused chest compression. This conclusion is opposite to our findings and Irion’s and Balachandran’s reports [10], [25], as well as the known clinical consensus about sternal precaution. There were three main limitations to the studies by Ge et. al [9], [11]. First, the reported mean skin strain was only 2.5% (SD = 5.8%). Without statistical verification, their near-zero measurement could be just noise. Second, the strain was measured from the skin overlying the sternoclavicular joints. However, the arms are connected to the entire sternum through the sternocostal part of pectoralis major muscle, and partial separation of the sternum usually happens at the lower third of sternum [26]. Therefore, the skin strain overlying the sternoclavicular joints cannot reflect the chest expansion of the entire sternal area. In contrast, in our study, two wearable sensors were attached to the pectoralis major below the clavicular, and the locations of the sensors were closer to the high-risk area of sternal dehiscence than the area studied by Ge et al. Third, the subjects in the study by Ge et al. were all young healthy volunteers, while our study involved both healthy volunteers and post-sternotomy patients (target population).
TABLE V.
The Studies on Chest Expansion in Sit-to-Stand Transitions
| Author | Participants (N) | Method | Measure | Results |
|---|---|---|---|---|
| Ge [9] | Healthy (30) | Digital camera | Skin deformation | Compression (2.5%) for pushing up from a chair |
| Irion [10] | Healthy (22) | Ultrasonic doppler | Skin acceleration | Extension (256* and 302*) for cautious sit-to-stand and pushing up from a chair respectively |
| Ge [11] | Healthy (30) | Electromagnetic tracking system | Skin deformation | Compression (1.1%) for pushing up from a chair |
| Balachandran [25] | Patient (75) | Ultrasound | Motion of sternal edge | Extension (0.08 to 0.10 cm) for sit-to-stand |
Doppler shift, unitless
In our study, we measured the relative yaw orientation change of the two wearable sensors (the proposed digital biomarker, MEA) to estimate chest expansion. Theoretically, we can also determine chest expansion during sit-to-stand transitions based on the change of the linear distance between the two wearable sensors. However, it is not accurate to estimate displacement via double integration of acceleration samples collected by wearable inertial sensors, since the drift derived from acceleration signals is accumulated in the integration process [27], and the growing drift finally distorts the tiny measurement of skin displacement due to chest expansion.
One limitation of our study is the lack of validation on the accuracy of the presented digital biomarker when the wearable sensors are attached to the human body. Alternatively, the bench test was conducted to validate the reliability of the digital biomarker to represent the yaw rotation of one sensor in relation to the other sensor. Then the measurements collected in healthy volunteers’ proactive chest expansion test qualitatively verified the effectiveness of this digital biomarker to detect skin extension caused by chest expansion. In the future, the accuracy of the digital biomarker will be examined quantitatively using a camera-based motion capture system, and the camera can track the motion of wearable sensors along with the skin in real-time during sit-to-stand transitions.
Another limitation of our study is that the proposed digital biomarker on chest expansion is linked with skin deformation rather than stress on the sternum. The distraction force is the main cause of sternal dehiscence [5], which is an acute or chronic complication during the rehabilitation of post-sternotomy patients. Until now, no study supports the association between skin strain and mechanical separation force on the sternum. However, our findings based on this digital biomarker are still meaningful to compare different sit-to-stand transitions due to the following reasons: 1) The excessive skin strain overlying the sternum is also a risk factor of skin breakage and wound infection in the early postoperative period (within ten days after the surgery) [4]. 2) Based on an understanding of anatomy and biomechanical analysis [11], the skin strain can be treated as a surrogate proof to judge whether the direction of the stress is compressive or distractive, and also determine which upper body movements induce larger force on the sternum than the others.
VI. Conclusions
This paper proposes a wearable sensor-based digital biomarker to assess chest expansion during sit-to-stand transitions. Based on the measurements of this digital biomarker during sit-to-stand transitions with different strategies, the findings of this study objectively examined several known sternal precaution guidelines about sit-to-stand transitions. First, pushing up from a chair induces larger chest expansion compared with the other strategies of sit-to-stand transitions. Second, crossing the arms or hugging a pillow can help reduce chest expansion during sit-to-stand transitions. Third, the sit-to-stand transition in a frontal push-up strategy induces the same level of chest expansion as that with the arm relaxed strategy. In future, this digital biomarker will be tested in other activity scenarios which sternal precaution guidelines cover, such as lifting heavy objects or getting out of bed. In this way, an objective and personalized sternal precaution plan can be provided to the patients, minimizing the risk of sternal complications while promoting physical activities to facilitate recovery. Furthermore, the wearable flexible sensors with the algorithm to extract this digital biomarker can be developed to be a tele-monitoring system to alert post-sternotomy patients from “dangerous” activities of daily living.
Acknowledgment
The authors would like to acknowledge Ms. Ana Enriquez, Ms. Jana Bishop, Mr. Manuel Gardea, and Mr. Hector Elizondo who contributed to the IRB approval process, and data collection. The authors also would like to give special thanks to Ms. Qianzi Zhang for her support on statistical analyses, and Mr. Patrick Pecson for proofreading the article. The study is supported in part by a grant from the National Institute of Health (No: 1R41-AG061951 01).
Contributor Information
Changhong Wang, iCAMP (Interdisciplinary Consortium on Advanced Motion Performance), Michael E. DeBakey Department of Surgery, Baylor College of Medicine, Houston, TX 77030, US.
Rahul Goel, Department of Neuroscience, Baylor College of Medicine, Houston, Texas 77030, US.
Maria Noun, iCAMP (Interdisciplinary Consortium on Advanced Motion Performance), Michael E. DeBakey Department of Surgery, Baylor College of Medicine, Houston, TX 77030, US.
Ravi K. Ghanta, Michael E. DeBakey Department of Surgery, Baylor College of Medicine, Houston, TX 77030, US
Bijan Najafi, iCAMP (Interdisciplinary Consortium on Advanced Motion Performance), Michael E. DeBakey Department of Surgery, Baylor College of Medicine, Houston, TX 77030, US.
References
- [1].Adams J, Lotshaw A, Exum E, Campbell M, Spranger CB, Beveridge J, et al. , “An alternative approach to prescribing sternal precautions after median sternotomy,“Keep Your Move in the Tube”,” in Baylor University Medical Center Proceedings, 2016, pp. 97–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Swanson LB and LaPier TK, “Upper Extremity Forces Generated During Activities of Daily Living: Implications for Patients Following Sternotomy,” Journal of Acute Care Physical Therapy, vol. 5, pp. 70–76, 2014. [Google Scholar]
- [3].Cahalin LP, LaPier TK, and Shaw DK, “Sternal precautions: is it time for change? Precautions versus restrictions–a review of literature and recommendations for revision,” Cardiopulmonary physical therapy journal, vol. 22, p. 5, 2011. [PMC free article] [PubMed] [Google Scholar]
- [4].Brocki BC, Thorup CB, and Andreasen JJ, “Precautions related to midline sternotomy in cardiac surgery: a review of mechanical stress factors leading to sternal complications,” European Journal of Cardiovascular Nursing, vol. 9, pp. 77–84, 2010. [DOI] [PubMed] [Google Scholar]
- [5].McGregor WE, Trumble DR, and Magovern JA, “Mechanical analysis of midline sternotomy wound closure,” The Journal of Thoracic and Cardiovascular Surgery, vol. 117, pp. 1144–1150, 1999. [DOI] [PubMed] [Google Scholar]
- [6].Adams J, Schmid J, Parker RD, Coast JR, Cheng D, Killian AD, et al. , “Comparison of force exerted on the sternum during a sneeze versus during low-, moderate-, and high-intensity bench press resistance exercise with and without the valsalva maneuver in healthy volunteers,” The American journal of cardiology, vol. 113, pp. 1045–1048, 2014. [DOI] [PubMed] [Google Scholar]
- [7].Casha AR, Manché A, Gatt R, Duca E, Gauci M, Schembri-Wismayer P, et al. , “Mechanism of sternotomy dehiscence,” Interactive cardiovascular and thoracic surgery, vol. 19, pp. 617–621, 2014. [DOI] [PubMed] [Google Scholar]
- [8].Parker R, Adams J, Ogola G, McBrayer D, Hubbard J, McCullough T, et al. , “Current activity guidelines for CABG patients are too restrictive: comparison of the forces exerted on the median sternotomy during a cough vs. lifting activities combined with valsalva maneuver,” The Thoracic and cardiovascular surgeon, vol. 56, pp. 190–194, 2008. [DOI] [PubMed] [Google Scholar]
- [9].Ge W, Hians B, and Sfara A, “Noncontact Measurement of the Deformation of Sternal Skin During Shoulder Movements and Upper Extremity Activities Restricted by Sternal Precautions,” Physical therapy, vol. 98, pp. 911–917, 2018. [DOI] [PubMed] [Google Scholar]
- [10].Irion GL, Gamble J, Harmon C, Jones E, and Vaccarella A, “Effects of upper extremity movements on sternal skin stress,” Journal of Acute Care Physical Therapy, vol. 4, pp. 34–40, 2013. [Google Scholar]
- [11].Ge W, Sfara A, and Hians B, “Skin deformation during shoulder movements and upper extremity activities,” Clinical Biomechanics, vol. 47, pp. 1–6, 2017. [DOI] [PubMed] [Google Scholar]
- [12].Najafi B, Armstrong DG, and Mohler J, “Novel wearable technology for assessing spontaneous daily physical activity and risk of falling in older adults with diabetes,” ed: SAGE Publications Sage CA: Los Angeles, CA, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Madgwick S, “An efficient orientation filter for inertial and inertial/magnetic sensor arrays,” Report x-io and University of Bristol (UK), vol. 25, pp. 113–118, 2010. [Google Scholar]
- [14].Lebel K, Hamel M, Duval C, Nguyen H, and Boissy P, “Camera pose estimation to improve accuracy and reliability of joint angles assessed with attitude and heading reference systems,” Gait & posture, vol. 59, pp. 199–205, 2018. [DOI] [PubMed] [Google Scholar]
- [15].Diebel J, “Representing attitude: Euler angles, unit quaternions, and rotation vectors,” Matrix, vol. 58, pp. 1–35, 2006. [Google Scholar]
- [16].Koo TK and Li MY, “A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research,” Journal of chiropractic medicine, vol. 15, pp. 155–163, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Taylor R, “Interpretation of the Correlation Coefficient: A Basic Review,” Journal of Diagnostic Medical Sonography, vol. 6, pp. 35–39, 1990/01/01 1990. [Google Scholar]
- [18].Westerdahl E and Möller M, “Physiotherapy-supervised mobilization and exercise following cardiac surgery: a national questionnaire survey in Sweden,” Journal of cardiothoracic surgery, vol. 5, p. 67, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Tuttle K, Mincer AB, and Thompson AW, “Medial sternotomies: a systematic review and evidence-based guidelines for postoperative sternal precautions,” Journal of Acute Care Physical Therapy, vol. 1, pp. 36–37, 2010. [Google Scholar]
- [20].Robicsek F, Fokin A, Cook J, and Bhatia D, “Sternal instability after midline sternotomy,” The Thoracic and cardiovascular surgeon, vol. 48, pp. 1–8, 2000. [DOI] [PubMed] [Google Scholar]
- [21].Liu H, Guo S, Zheng K, Guo X, Kuramoto-Ahuja T, Sato T, et al. , “Reliability and validity of measuring respiration movement using a wearable strain sensor in healthy subjects,” Journal of physical therapy science, vol. 29, pp. 1543–1547, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hughes J and Iida F, “Multi-Functional Soft Strain Sensors for Wearable Physiological Monitoring,” Sensors, vol. 18, p. 3822, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Agcayazi T, Yokus MA, Gordon M, Ghosh T, and Bozkurt A, “A stitched textile-based capacitive respiration sensor,” in 2017 IEEE SENSORS, 2017, pp. 1–3.29780437 [Google Scholar]
- [24].Kundu SK, Kumagai S, and Sasaki M, “A wearable capacitive sensor for monitoring human respiratory rate,” Japanese Journal of Applied Physics, vol. 52, p. 04CL05, 2013. [Google Scholar]
- [25].Balachandran S, Denehy L, Lee A, Royse C, Royse A, and El-Ansary D, “Motion at the Sternal Edges During Upper Limb and Trunk Tasks In-Vivo as Measured by Real-Time Ultrasound Following Cardiac Surgery: A Three-Month Prospective, Observational Study,” Heart, Lung and Circulation, vol. 28, pp. 1283–1291, 2019/08/01/2019. [DOI] [PubMed] [Google Scholar]
- [26].El-Ansary D, Waddington G, and Adams R, “Control of separation in sternal instability by supportive devices: a comparison of an adjustable fastening brace, compression garment, and sports tape,” Archives of physical medicine and rehabilitation, vol. 89, pp. 1775–1781, 2008. [DOI] [PubMed] [Google Scholar]
- [27].Boore DM, “Analog-to-digital conversion as a source of drifts in displacements derived from digital recordings of ground acceleration,” Bulletin of the Seismological Society of America, vol. 93, pp. 2017–2024, 2003. [Google Scholar]