Abstract
Background:
Prescription drug monitoring programs (PDMPs) that collect and distribute information on dispensed controlled substances have been adopted by nearly all US states. We know little about program characteristics that modify PDMP impact on prescription opioid overdose deaths.
Methods:
We measured associations between adoption of any PDMP and changes in fatal prescription opioid overdoses in 2002-2016 across 3,109 counties in 49 states. We then measured changes related to the adoption of “proactive PDMPs”, which report outlying prescribing/dispensing patterns and provide broader access to PDMP data by law enforcement. Comparisons were made within three time intervals that broadly represent the evolution of PDMPs (2002-2004, 2005-2009, 2010-2016). We modeled overdoses using Bayesian space-time models.
Results:
Adoption of electronic PDMP access was associated with 9% lower rates of fatal prescription opioid overdoses after three years (rate ratio [RR]=0.91, 95% credible interval [CI]: 0.88-0.93) with well-supported effects for methadone (RR=0.86, CI: 0.82-0.90) and other synthetic opioids (RR=0.82, CI: 0.77-0.86). Compared to states with no/weak PDMPs, proactive PDMPs were associated with fewer deaths attributed to natural/semi-synthetic opioids (2002-2004: RR=0.72 (0.66-0.78); 2005-2009: RR=0.93 (0.90-0.97); 2010-2016: 0.89 (0.86-0.92)) and methadone (2002-2004: RR=0.77 (0.69-0.85); 2010-2016: RR=0.90 (0.86-0.94)). Unintended effects were observed for synthetic opioids other than methadone (2005-2009: RR=1.29 (1.21-1.38); 2010-2016: RR=1.22 (1.16-1.29)).
Conclusions:
State adoption of PDMPs was associated with fewer prescription opioid deaths overall while proactive PDMPs alone were associated with fewer deaths related to natural/semi-synthetic opioids and methadone, the specific targets of these programs.
Keywords: Prescription Drug Monitoring Programs, opioids, latent class analysis, latent transition analysis, prescribing, opioid overdose
Introduction
Opioid overdoses have more than quadrupled since 1999, from 3.0 deaths per 100,000 in 2000 to 13.3 deaths per 100,000 in 2016.1 This sharp increase coincided with a dramatic increase in the use of prescription opioids to treat chronic pain,2 including a tripling of opioid prescriptions dispensed during the same time period.3 In more recent years, deaths from non-methadone synthetic opioids (primarily illegally manufactured fentanyl and related analogs) have overtaken deaths from the type of opioids prescribed to treat chronic pain (i.e., natural and semi-synthetic opioids).4
Prescription drug monitoring programs (PDMPs), state-level databases which collect information on controlled substance prescriptions have been advanced as tools to reduce prescription opioid-related harm.5,6 Authorized users, including prescribers and law enforcement officials, may access these data as dictated by state law. PDMPs have been hypothesized to reduce prescription opioid-related harm by improving prescribing practices, assisting in the identification of patients who might benefit from targeted health interventions, and detecting patients and prescribers engaged in illegal activities.7 By December 2017, all US states and Washington, D.C. had an operational PDMP or had taken steps to enact a PDMP.8
While many studies have examined the impact of PDMPs on fatal overdoses, their findings are inconsistent: three studies have reported a reduction in prescription opioid-related overdose deaths following PDMP implementation,9-11 one reported a reduction in total opioid overdose deaths,12 one reported a significant increase in total drug overdose rates,13 and two reported no association with prescription opioid-related overdose deaths.14,15 Some studies have investigated the contribution of specific PDMP characteristics on fatal overdose, including mandatory provider review,12,16 mandatory provider review combined with pain clinic laws,17 number of drug schedules monitored,12,18 and data updating at least weekly.12,18 Each of these studies found different PDMP characteristics related to lower fatal overdose rates.12,16-19 and achieved little consensus.
Five factors may contribute to the discrepant findings on the impact of PDMPs on opioid overdose. First, most research treats the presence of a PDMP as a binary variable, without considering that operational characteristics of PDMPs vary greatly across states,7 such that a PDMP implemented in one state may have very different characteristics than that implemented in another. Second, those studies that do examine specific PDMP characteristics have largely ignored the fact that different aspects of PDMPs are often implemented contemporaneously.12,20 Hence, findings related to one PDMP characteristic will be conflated with others to the degree that clusters of PDMP characteristics are adopted at the same time. Third, the characteristics of PDMPs have also changed over time. Thus, equating the effectiveness of PDMPs in 2002 with the effectiveness of PDMPs in 2016 may not be justified, given the substantial changes in PDMP characteristics over this period. Fourth, deaths from opioid overdoses related to natural/semi-synthetic opioids such as diverted oxycodone or hydrocodone may be closely related to prescribing practices, while deaths related to synthetic opioids other than methadone (such as illegally manufactured fentanyl) may not be. And, fifth, prior studies fail to account for within-state heterogeneity in rates of change in PO overdose and in the distribution of key demographic covariates that may affect PO overdose, thus generating the potential for aggregation bias in estimated effects.21
In this study, we addressed these gaps in four ways. First, we built on a prior study, where we had used latent transition analysis to identify those combinations of PDMP characteristics that tend to be adopted together.22 We used the resulting PDMP latent classes to examine the combinations of PDMP characteristics that were associated with the greatest change in prescription opioid overdose fatalities. Second, we assessed these classes across three time periods (1999-2004, 2005-2009, and 2010-2016), and examined how transitions between types of PDMP classes over time contributed to changes in fatal prescription opioid overdose in counties within states in 2002-2016. Third, we examined prescription opioid overdoses overall and by opioid class to better differentiate those deaths involving prescribed opioids that would be tracked by PDMPs (i.e., natural/semi-synthetic opioids and methadone prescribed for pain) from deaths likely involving illegal opioids that would not be tracked by PDMPs (i.e., synthetic opioids other than methadone, which primarily comprised illegally manufactured fentanyl and similar synthetics during the latter period of study, often combined with heroin, cocaine, and other illegal drugs).23 Fourth, we adopted a geospatial approach to examine the impact of state-level PDMPs on county-level fatal overdoses, accounting for within-state variation in the level and rate of growth of fatal prescription opioid overdoses and spatial autocorrelation in overdose deaths across counties and states.
Our study addressed the following questions: (1) what is the relationship between state-level PDMP implementation and county-level fatal prescription opioid overdose counts, overall and by type of opioid class?; (2) what is the relationship between state membership in specific PDMP latent classes and county-level fatal prescription opioid overdose counts, overall and by opioid class? To further explicate the relationship between PDMP latent classes and prescription opioid overdoses, we also examined the relationship between specific PDMP features and prescription opioid overdoses (overall and by opioid class).
METHODS
We used the National Vital Statistics System multiple cause-of-death mortality files to assess opioid-related overdose deaths.24 The International Classification of Disease, Tenth Revision (ICD-10) underlying cause-of-death codes were used to identify drug overdose deaths, including X40-44 (accidental poisoning by and exposure to noxious substances, including analgesics), X60-64 (intentional self-poisoning by and exposure to drugs, including narcotics and psychodysleptics), X85 (assault by drugs, medicaments, and biologic substances), and Y10-14 (events of undetermined intent, including poisoning by and exposure to narcotics and psychodysleptics, not elsewhere classified, undetermined intent). Our analyses were restricted to deaths involving the following ICD-10 multiple cause-of-death codes: natural/semisynthetic opioids (T40.2), methadone (T40.3), and synthetic opioids other than methadone (T40.4). Annual counts of overdose deaths were aggregated across 3,109 counties in 49 US states plus D.C. for the years 2002-2016. We did not include Alaska due to frequent changes in county boundaries during the study period. Overdoses were classified by county of death. The New York University Langone Health Institutional Review Board reviewed and approved the study protocol.
Exposures
We used three approaches to characterize PDMPs in 2002-2016: (1) date when the PDMP provided electronic access to the system; (2) PDMP latent classes;22 and (3) specific PDMP characteristics included in the PDMP latent classes. Dates of electronic PDMP access were obtained from the National Alliance for Model State Drug Laws (NAMSDL) and state PDMP administrators, while features of PDMPs were compiled from the Prescription Drug Abuse Policy System (PDAPS).25
For the PDMP latent transition analysis (LTA),22 we considered PDMP characteristics that have been identified by policy experts as potentially important determinants of prescribing practices and prescription opioid overdose events.6,7 These included: a) state authorization for prescribers to access PDMP data; b) state authorization for law enforcement to access PDMP data; c) state permission or requirement for PDMP to proactively identify suspicious or statistically outlying prescribing, dispensing, or purchasing activity; d) state required timeframe for dispensers to report data to the PDMP; e) state required number of drug schedules to be reported to the PDMP; f) state requirement for prescribers to check the PDMP before prescribing controlled substances; and g) state permission for the PDMP to share data with other state PDMPs. These characteristics were measured on an annual basis; response options are presented in eTable 1 in the online Supplement.
We used LTA26-28 to identify groups of states with similar combinations of PDMP characteristics in three intervals: 1999-2004, 2005-2009, and 2010-2016. These intervals represent different historical periods in the opioid overdose epidemic and the evolution of PDMPs, including: (1) 1999-2004, the “electronic era”, when PDMPs first started to transmit data electronically and prescription opioid overdose rates first started to increase; (2) 2005-2009, the “expansion era”, when increased federal funding for PDMPs became available from the Bureau of Justice Assistance and SAMHSA, among others; and (3) 2010-2016, the “robust PDMP era”, when PDMP capacity expanded, prescription opioid overdose rates stabilized, and heroin (starting in 2010) and fentanyl overdoses (starting in 2013) increased.29-33 Grouping time periods in this way followed a natural characterization of the development of PDMPs and helped to avoid sparseness issues in the LTA response pattern matrix. The methods used to create these classes and the results from this analysis are described elsewhere.22 Results of the LTA are presented in eTable 2 in the online Supplement.
Three classes of PDMPs were identified in each interval. Since the pattern of PDMP characteristics within each class was most comparable in the first two intervals, we used the same labels for classes in 1999-2004 and 2005-2009. The key features of the three latent classes in these two intervals were: (1) the No/Weak PDMP class represented states with either no operational PDMP, especially in the early years, or an operational PDMP with few or no measured characteristics (eTable 2); (2) the Reactive PDMP class represented states with a high probability of having no requirements to proactively report outlying patterns to law enforcement, licensing bodies and prescribers/dispensers, a high probability of providing limited data access for law enforcement, and less frequent reporting requirements for dispensers; (3) the Proactive PDMP class represented states that had a high probability of permitting/requiring proactive reporting of outlying patterns to law enforcement, licensing bodies and prescribers/dispensers, a high probability of providing access to PDMP data to law enforcement without requiring a warrant, subpoena, or active investigation, and a high probability of requiring dispensers to report data to the PDMP on a more frequent basis.
In the last interval (2010-2016), two new features were added to some PDMPs: requiring PDMP access when prescribing and data sharing between states. The Proactive PDMP class remained similar to the Proactive PDMP class in the first two intervals. However, all states except Missouri had by this time enacted a PDMP, so that the No/Weak PDMP class became a Weak PDMP, that represented states with few basic PDMP characteristics. The Reactive PDMP class was no longer relevant and a new Cooperative PDMP class appeared. This class contains states that had a lower probability than Proactive states of permitting/requiring reporting of outlying patterns to PDMP users or providing open access of PDMP data to law enforcement, but had a greater probability of allowing PDMP data to be shared with other states, and reporting more federal drug schedules than states in the Proactive class. Within each interval, states had year-specific probabilities of belonging to a PDMP latent class, and they could transition across classes every year. Class membership probabilities for each state summed to 1; the probability of membership in each latent class, rather than modal assignment, was considered as the exposure of interest.22,34,35
Covariates
Based on prior studies,14,36,37 we accounted for the following county-level demographic characteristics, obtained from annual Geolytics data:38 population density (thousands of people/square mile); age composition (% of the population aged 0-19, 20–44, 45–64, and ≥65 years); racial/ethnic composition (% non-Hispanic White, non-Hispanic Black, Hispanic); % male; and socioeconomic conditions (% of families in poverty, median household income, % unemployed). We also accounted for the overall mortality rate per 1,000 residents in the county. Finally, we accounted for co-occurring state-level policy changes associated with opioid overdose in prior studies, including: medical marijuana legalization,39,40 Good Samaritan laws,41 and naloxone overdose prevention laws.41,42 Annual information on these laws was obtained through PDAPS.25
Analyses
We modeled the county-by-year mortality counts using hierarchical Bayesian space-time Poisson models, with county population included as the offset.43-45 After testing unstructured and structured lag specifications, we chose linear distributed lag 46 specifications to allow a linear progression of policy associations from instantaneous through 3-year-lagged effects. We modeled covariates, including demographic characteristics and the overall mortality rate, as concurrent predictors of overdose deaths.
The analytic approach addressed potential biases that could arise from mis-specifications of unit and time effects (the primary concerns addressed by standard difference-in-difference methods) by including state-level fixed effects (dummy variables included for each state except the reference) and county-level random intercepts and trends. Thus, growth mixtures between counties within states that arose over the course of study and could bias estimates of intervention effects were explicitly modeled. Acknowledging that difference-in-difference methods are not applicable to Poisson distributed outcomes, this approach provides substantial control for potential biases that could arise when examining heterogeneous policy effects across counties within states and avoids other biases that arise in difference-in-difference analyses due to over- and under-differencing.47 By incorporating a conditional autoregressive spatial random effect, we account for the lack of independence in spatially contiguous geographic areas, and minimize biases due to small area effects.48 Finally, by using linear distributed lags, our models separately estimated concurrent (yet temporally ambiguous) policy impacts, as well as impact over the subsequent three years, where it was possible to establish a clear temporal order between the policy and overdose.49 All analyses were performed using R-INLA.50,51
We fit three types of models, in each case accounting for demographic characteristics, overall mortality rates, and co-occurring marijuana, overdose Good Samaritan and naloxone laws. First, we examined the association between the proportion of each year with electronic PDMP implementation and the rate of prescription opioid overdose, including the concurrent impact within the year of PDMP implementation, and over the subsequent 3 years.49 Second, we examined the association between the probability of PDMP latent class membership in each year and interval and the rate of prescription opioid overdose. Third, given the increase in fentanyl-related overdose deaths since 2013, and the potential for prescription opioid overdoses in the latter period to represent a mix of prescription opioids and illegally manufactured synthetics such as fentanyl, we examined the association between PDMP electronic access, PDMP latent class membership, and types of opioid overdose deaths: natural/semi-synthetic opioids, synthetic opioids other than methadone, and methadone.
Secondary analysis
To explicate the relationships between PDMP electronic access and opioid overdose deaths, and to inform our understanding of impacts of specific PDMP characteristics within latent classes, we estimated the relationship between individual PDMP characteristics and opioid overdoses, overall and by class. These models jointly estimated the relationship between all features and overdose counts, adjusting for covariates described above. Results are presented as log relative rates.
Sensitivity analyses
We conducted two sensitivity analyses. First, we replicated our analyses excluding states that had a greater than 5% absolute difference in reported versus imputed opioid overdose rates based on a prior study that imputed county-level rates when no specific drug was identified (i.e., Alabama, Indiana, Louisiana, and Pennsylvania).52 This analysis addressed two sources of bias that could arise when relying on ICD-10 coded death certificate data: specific drugs involved in overdose are not always identified on death certificates, and drug-specific overdose rates may be variously underestimated or overestimated between states.52 Second, we estimated the relationship between PDMP electronic access and PDMP latent classes, and opioid overdose mortality, accounting for the potentially confounding role of other prescription opioid laws, notably adoption of any pain management clinic laws, and adoption of a 7-day or less prescribing limit. Information on these laws was obtained from PDAPS.25
RESULTS
The top portion of Table 1 presents the overall assessment of relationships between state PDMP electronic access and relative rates of opioid overdose fatalities for the initial year in which the electronic PDMP became operational and for the subsequent 3 years. The observed associations indicate that electronic PDMP access was associated with a 2% increase in opioid overdose deaths in the initial year (RR=1.02; 95% CI: 1.00-1.04), then related to lower overdose fatalities over the subsequent 3 years (a 9% decrease by year 3, RR=0.91, 95% CI: 0.88-0.93). Both effects were specific to methadone (RR=0.86, CI: 0.82-0.90) and synthetic opioids other than methadone (RR=0.82, CI: 0.77-0.86) with no well-supported effects for natural/semi-synthetic opioids, the key target of PDMP programs (RR=1.01, 95% CI: 0.98-1.04 initial year; RR=1.01, 95% CI: 0.97-1.04 year 3).
Table 1.
Relationships of initial access to PDMPs (top) and latent class membership probabilities (bottom) to county-level rates of opioid overdose deaths overall and for specific opioid classes, 1999-2016, United Statesa,b
| All opioids | Natural/semi- synthetic opioids |
Methadone | Synthetic opioids other than methadone |
|||||
|---|---|---|---|---|---|---|---|---|
| Median RR |
95% CI | Median RR |
95% CI | Median RR |
95% CI | Median RR |
95% CI | |
| Access to electronic PDMP | ||||||||
| Initial year of access | 1.02 | 1.00, 1.04 | 1.01 | 0.98, 1.04 | 1.04 | 1.00, 1.08 | 1.10 | 1.05, 1.15 |
| Year 1 post-access | 0.98 | 0.96, 1.00 | 1.01 | 0.98, 1.03 | 0.98 | 0.94, 1.01 | 0.99 | 0.96, 1.04 |
| Year 2 post-access | 0.94 | 0.92, 0.96 | 1.01 | 0.98, 1.03 | 0.92 | 0.88, 0.95 | 0.90 | 0.86, 0.94 |
| Year 3 post-access | 0.91 | 0.88, 0.93 | 1.01 | 0.97, 1.04 | 0.86 | 0.82, 0.90 | 0.82 | 0.77, 0.86 |
| PDMP latent classes | ||||||||
| Interval 1: 1999-2004 | ||||||||
| Reactive vs. No/Weak | 0.97 | 0.94, 1.00 | 0.94 | 0.90, 0.98 | 0.89 | 0.84, 0.94 | 1.11 | 1.03, 1.19 |
| Proactive vs. No/Weak | 0.86 | 0.80, 0.91 | 0.72 | 0.66, 0.78 | 0.77 | 0.69, 0.85 | 0.98 | 0.85, 1.13 |
| Proactive vs. Reactive | 0.88 | 0.83, 0.94 | 0.77 | 0.71, 0.83 | 0.86 | 0.78, 0.96 | 0.89 | 0.76, 1.04 |
| Interval 2: 2005-2009 | ||||||||
| Reactive vs. No/Weak | 1.10 | 1.08, 1.13 | 1.01 | 0.99, 1.04 | 1.09 | 1.05, 1.12 | 1.37 | 1.31, 1.43 |
| Proactive vs. No/Weak | 1.03 | 1.00, 1.06 | 0.93 | 0.90, 0.97 | 1.02 | 0.97, 1.07 | 1.29 | 1.21, 1.38 |
| Proactive vs. Reactive | 0.93 | 0.91, 0.96 | 0.92 | 0.89, 0.96 | 0.94 | 0.89, 0.99 | 0.95 | 0.89, 1.01 |
| Interval 3: 2010-2016 | ||||||||
| Cooperative vs. Weak | 0.95 | 0.92, 0.97 | 0.98 | 0.95, 1.01 | 0.85 | 0.81, 0.89 | 0.96 | 0.92, 1.02 |
| Proactive vs. Weak | 0.99 | 0.97, 1.01 | 0.89 | 0.86, 0.92 | 0.90 | 0.86, 0.94 | 1.22 | 1.16, 1.29 |
| Proactive vs. Cooperative | 1.05 | 1.02, 1.08 | 0.91 | 0.88, 0.95 | 1.06 | 1.00, 1.12 | 1.27 | 1.20, 1.35 |
Results based on models that adjust for annual county-level age, race/ethnic, sex, and socioeconomic composition, population density, and the overall mortality rate; annual state-level medical marijuana laws, Good Samaritan laws, and naloxone overdose prevention laws; calendar year; state-level fixed effects; county unit and trend random effects.
Abbreviations: PDMP: prescription drug monitoring program; RR: relative rate
The bottom portion of Table 1 also presents the association between the probability of membership in each PDMP latent class and opioid overdoses during each of the three study intervals. For these analyses, the first PDMP interval is examined from 2002 to 2004 (rather than 1999 to 2004), as the outcome (overdose deaths) is measured starting in 2002. These results are not assessed using distributed lags since the lags would cut across study intervals. In the first interval (2002-2004), states in the Reactive PDMP class had 3% lower opioid overdose fatality rates than the states with a No/Weak PDMP (RR=0.97; 95% CI: 0.94-1.00), while states with a Proactive PDMP had 14% lower opioid overdose fatality rates than the states with No/Weak PDMPs (RR=0.86; 95% CI: 0.80-0.91). States with Proactive PDMPs also had lower opioid overdose fatality rates than states with Reactive PDMPs (RR = 0.88; 95% CI: 0.83-0.94). In the second interval (2005-2009), states with Reactive PDMPs had 10% higher opioid overdose fatality rates than states with No/Weak PDMPs (RR=1.10; 95% CI: 1.08-1.13), while opioid overdose rates in states with Proactive PDMPs were no different from those in states with No/Weak PDMPs, but 7% lower than in states with Reactive PDMPs (RR=0.93; 95% CI: 0.91-0.96). Finally, in the third interval (2010-2016), states with Cooperative PDMPs had 5% lower fatal opioid overdose rates than states with Weak PDMPs (RR=0.95; 95% CI: 0.92-0.97), but states with Proactive PDMPs showed no difference in opioid overdose rates compared to states with Weak PDMPs. States with Proactive PDMPs had 5% higher fatal overdose rates than states with Cooperative PDMPs (RR=1.05; 95% CI: 1.02-1.08).
Drug-specific analyses revealed three different patterns of findings. First, the Proactive class was consistently associated with the lowest rates of overdose from natural/semi-synthetic opioids (the type of opioid most likely to be reported to PDMPs) across all three intervals for both the Proactive vs. No/Weak (2002-2004: RR=0.72 (0.66-0.78); 2005-2009: RR=0.93 (0.90-0.97); 2010-2016: 0.89 (0.86-0.92)) and the Proactive vs. Reactive or Cooperative comparisons (2002-2004: RR=0.77; 95% CI: 0.71-0.83; 2005-2009: RR=0.92; 95% CI: 0.89-0.96; 2010-2016: RR=0.91; 95% CI: 0.88-0.95). Second, the Proactive class was associated with the lower rates of fatal methadone overdoses in the first period (Proactive vs. No/Weak: 2002-2004: RR=0.77; 95% CI: 0.69-0.85), was no different from the No/Weak class in the second period, and was associated with lower rates of overdose from methadone in the third period (2010-2016: RR=0.90; 95% CI: 0.86-0.94). Third, in contrast, the Proactive class was associated with higher rates of overdose from non-methadone synthetic opioids in the second and third periods (Proactive vs. No/Weak: 2005-2009: RR=1.29; 95% CI: 1.21-1.38; 2010-2016: RR=1.22; 95% CI: 1.16-1.29).
In the third period, the Cooperative class was associated with the lowest rates of fatal overdose from methadone (RR=0.85; 95% CI: 0.81-0.89) and non-methadone synthetic opioids (RR=0.96; 95% CI: 0.92-1.02).
Secondary analysis
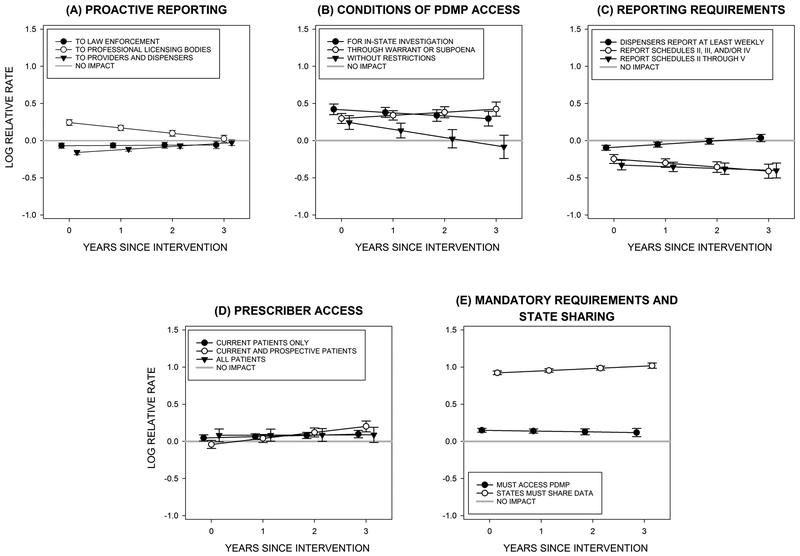
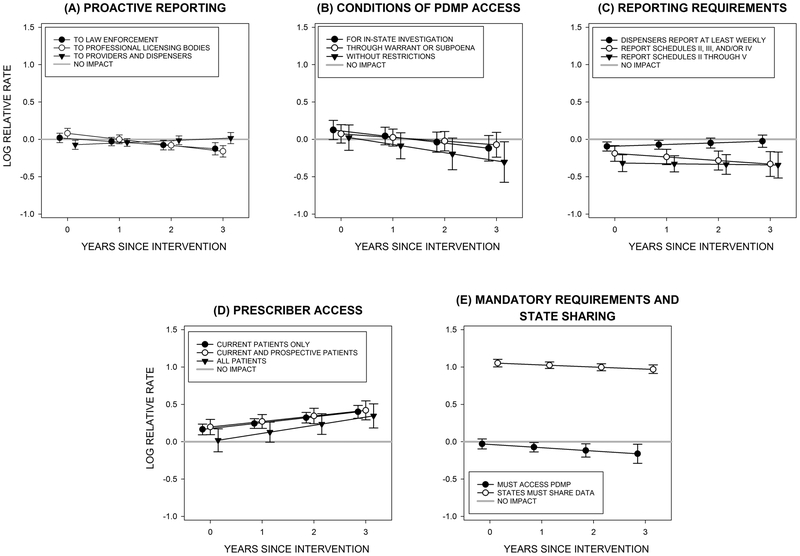
Initial and subsequent 3-year associations of specific PDMP characteristics with rates of opioid deaths, overall and by classes, are summarized in Figures 1-4. Specific characteristics were heterogeneously related to opioid overdose deaths and showed inconsistencies with respect to findings observed for the latent classes. Taking proactive reporting as a key example, proactive reporting to providers/dispensers was associated with lower log rates of overdose deaths from all POs (Figure 1), and in particular, natural/semi-synthetic opioids (Figure 2). Proactive reporting to law enforcement was also associated with lower rates of overdose deaths, but not those for natural/semi-synthetic opioids. Proactive reporting to professional licensed bodies was related to greater overdose deaths and specifically deaths related to natural/semi-synthetic opioids. Among important well-supported effects that were also heavily weighted indicators of proactive programs (eTable 2), reports on the broadest schedule of drugs (i.e., II through V) was related to substantial reductions across years among all overdose deaths (Figure 1), but not among overdose specifically related to natural/semi-synthetic opioids (Figure 2).
Figure 1:
Relationships between Prescription Drug Monitoring Program (PDMP) features and county-level log relative rates of overdose deaths from all opioids, 2002-2016, United Statesa
aResults based on models that adjust for annual county-level age, race/ethnicity, sex, and socioeconomic composition, population density, and overall mortality rate; annual state-level medical marijuana laws, Good Samaritan laws, and naloxone overdose prevention laws; calendar year; state-level fixed effects; county unit and trend random effects.
Figure 4:
Relationships between Prescription Drug Monitoring Program (PDMP) features and county-level log relative rates of overdose deaths from methadone, 2002-2016, United Statesa
aResults based on models that adjust for annual county-level age, race/ethnicity, sex, and socioeconomic composition, population density, and overall mortality rate; annual state-level medical marijuana laws, Good Samaritan laws, and naloxone overdose prevention laws; calendar year; state-level fixed effects; county unit and trend random effects.
Figure 2:
Relationships between Prescription Drug Monitoring Program (PDMP) features and county-level log relative rates of overdose death from natural/semi-synthetic opioids, 2002-2016, United Statesa
aResults based on models that adjust for annual county-level age, race/ethnicity, sex, and socioeconomic composition, population density, and overall mortality rate; annual state-level medical marijuana laws, Good Samaritan laws, and naloxone overdose prevention laws; calendar year; state-level fixed effects; county unit and trend random effects.
Sensitivity analyses
As shown in eTable 3 in the online supplement, the results presented in Table 1 remained mostly unchanged when we removed four states with high levels of underreporting of specific drugs (eTable 3, left columns 2-5), although in the last time interval, the Cooperative PDMP became associated with lower rates of synthetic opioid overdoses (Cooperative vs. No/Weak: 2010-2016: RR=0.82; 95% CI=0.77- 0.87).
As shown in eTable 4 in the online supplement, accounting for the state-level enactment of pain management clinic laws and prescribing limits had no substantive impacts on parameter estimates for the relationship between PDMP electronic access, or PDMP latent classes, and opioid overdose deaths.
DISCUSSION
The results of this study showed that a simple binary measure of access to prescribing information through PDMPs was broadly associated with lower rates of opioid overdose deaths over time. However, the magnitude and direction of changes in these deaths following implementation differed by opioid class, with no apparent change in overdoses involving natural/semi-synthetic opioids, and decreases in overdoses involving methadone and synthetic opioids. These observations suggest that the many different versions of PDMPs that occurred across states over the 15 years of this study were associated with no change in overdoses involving opioids that were the target of PDMPs. In contrast, they were associated with reductions in overdoses among classes of opioids that were not the target of PDMPs. From this perspective, PDMPs could be considered program failures.
Such a perspective is contradicted by more detailed analyses of PDMP characteristics. The results of LTA analyses from related work22 demonstrated that many characteristics of PDMPs were implemented in concert but differed in content over time and, importantly, could be statistically formed into natural classes that emerged as these programs developed. The LTAs enabled classifications of states into those with No or Weak PDMPs, Proactive PDMPs, Reactive PDMPs, or Cooperative PDMPs over three time intervals. In all cases, those states with a greater probability of appearing in the Proactive PDMP class were also those states where rates of opioid overdose deaths from natural/semi-synthetic opioids were lowest. Importantly, the Proactive PDMP class had greater impacts than those related to the Reactive or Cooperative PDMP classes and the Reactive or Cooperative PDMP classes had greater impacts than the No or Weak PDMP class. From this perspective, PDMPs could be considered program successes.
As we suggested in the introduction, the contrast here is likely due to the many different ways in which PDMPs developed and differed over time; PDMPs initiated in the early years of study had different characteristics than those initiated later, and all programs acquired additional characteristics over time. Under these circumstances, access to information on prescribing practices would mean something very different for those programs initiating in the first, second, and third intervals of study, while across all intervals LTA classes would remain meaningfully stable; for example, Proactive PDMPs would remain more Proactive than Reactive, Cooperative, or No or Weak PDMPs. These observations suggest that, since the meaning of simple measures of PDMP access shift over time, they cannot meaningfully be used to measure PDMP success. An ancillary consequence is that the meanings of the individual features of these programs also shift as the bundles of PDMP characteristics used in any PDMP change over time (i.e., the statistical relationship of any characteristic to the outcome shifts as new characteristics are added or removed from the program, Figure 1-4).
With these thoughts in mind, our findings provide empirical support for the proposed designation of unsolicited reporting of PDMP data to prescribers, dispensers and law enforcement—components of the “Proactive” class—as PDMP “best practices.”31 Overdoses from those opioids most likely to be monitored by the PDMP (i.e., natural/semi-synthetic opioids) were consistently lower in states with Proactive PDMPs. Although the specifics vary between states, unsolicited reports to medical professionals are typically triggered when a patient receives prescriptions for the same drug type from multiple prescribers and pharmacies in a relatively short time period, is prescribed a high daily dose of opioids, or is simultaneously prescribed opioids and benzodiazepines.53 Sending such reports can increase the ability of PDMPs to improve clinical practice by reducing overlapping prescriptions to these patients and identifying patients in need of substance use disorder treatment. Our findings are consistent with research that has found a reduction in risky prescribing practices after receipt of unsolicited reports from the PDMP.54,55
However, proactive PDMPs were associated with higher rates of overdose from synthetic opioids other than methadone. The last period of study (2010-2016) coincided with a shift in the profile of the opioid overdose epidemic, so that illegally produced synthetic opioids such as fentanyl and related analogs broadly contaminated the illegal opioid supply and became the leading type of opioid involved in overdose deaths.23 While most studies have not examined the impact of PDMPs on prescribing or overdoses associated with specific types of prescription opioids, one study in Florida did find that implementation of a PDMP in that state combined with pain clinic regulations was associated with reduced rates of diversion from natural/semi-synthetic opioids such as morphine and oxycodone, but not with reduced rates of diversion of synthetics such as fentanyl.56 Our findings may reflect unintended consequences of more proactive PDMPs. In states with more proactive PDMPs, and in the absence of an effective system to refer patients with substance use disorders to treatment, patients identified through the PDMP proactive reports as having a history of inappropriate prescribing may have been tapered off opioids without any attention to their opioid use disorder. This may have increased substitution of prescription opioids with products from the illegal market, including heroin and drugs contaminated with potent synthetics, such as fentanyl.57-59 Future work will investigate the impact of PDMP latent classes on heroin overdoses.
Our study found potentially promising effects of Cooperative PDMPs, that is, programs characterized by interstate data sharing and reporting on more drug schedules, were associated with lower rates of methadone overdoses in the first and third periods, and lower rates of overdoses involving non-methadone synthetic opioids in the third period. PDMPs which allow for greater interaction with other states have the potential to reduce drug diversion, which commonly involves illegal synthetic opioids, across neighboring states. Interpreting PDMP impacts on methadone overdose fatalities is difficult because many methadone-related deaths involve methadone prescribed for substance use disorder, which is not reported to PDMPs.
Several limitations are noted. First, we rely on ICD-10 coding of death certificate data, which may not reliably identify the drugs involved in fatal overdoses and may lead to an underestimation or misclassification of fatal opioid overdose rates52. However, our findings were robust to sensitivity analyses conducted to address this concern. Second, some of the PDMP features hypothesized to have the greatest impact on prescribing practices and overdose risk, including mandated access, were only implemented in the third study interval (2010-2016), limiting our ability to examine how they contributed to overdose fatalities over the long term. Third, our study is not able to examine the causal mechanisms through which specific PDMP features influence the risk of prescription opioid overdose. Future studies should examine the extent to which rates of PDMP usage and changes in prescribing practices and in drug diversion may mediate the impact of PDMP characteristics on prescription opioid overdose. Fourth, this study focused on the impact of PDMPs on fatal opioid overdoses. Future studies should consider the impact of PDMPs on the spectrum of opioid-related harm, from opioid misuse, to disorder, to nonfatal overdoses, including potential effects on overdose from illegal opioids. Fifth, increased news coverage and heightened awareness of the opioid overdose epidemic may have influenced prescribing practices above and beyond the PDMPs, as there is a greater understanding of the harms of opioids. To the extent this coincided with state enactment of more comprehensive PDMPs, this may explain some of the reported findings attributed to PDMPs. At a broader level, PDMP laws likely cluster with other opioid-related policies. Future studies should go beyond examining PDMP laws, to examine the range of opioid policies and laws that, as a cluster, affect opioid prescribing and opioid overdose risk.
State adoption of PDMPs was associated with fewer opioid deaths overall while proactive PDMPs were associated with fewer deaths related to natural/semi-synthetic opioids and methadone, the specific targets of these programs. Important components of successful PDMPs seem to include providing PDMPs with the resources to proactively identify and notify users about outlying prescribing, dispensing, and use patterns, and providing broader access of PDMP data to law enforcement. Measurement of specific PDMP components is essential to the identification of PDMP effects.
Supplementary Material
Figure 3:
Relationships between Prescription Drug Monitoring Program (PDMP) features and the county-level log relative rates of overdose death from non-methadone synthetic opioids, 2002-2016, United Statesa
aResults based on models that adjust for annual county-level age, race/ethnicity, sex, and socioeconomic composition, population density, and overall mortality rate; annual state-level medical marijuana laws, Good Samaritan laws, and naloxone overdose prevention laws; calendar year; state-level fixed effects; county unit and trend random effects.
Acknowledgments:
We thank Dr. Andrew Crawford, Ms. Julia Schleimer, and Ms. Veronica Pear for their assistance compiling policy and fatal overdose data.
Funding: The results reported herein correspond to specific aims of grant R01DA039962 to investigator Magdalena Cerdá, where R01DA039962 is a project number, Magdalena Cerdá is the Principal Investigator, and the National Institute on Drug Abuse is the funding agency. This work was also supported by grant number T32DA031099 from the National Institute on Drug Abuse, where David S. Fink is the recipient.
Footnotes
Conflict of interest: None
Access to code and data: The computer code used to conduct analyses for this paper, as well as all the policy and county-level demographic data is available from the study authors upon request. The mortality data has been obtained through a restricted data use agreement with the National Center for Health Statistics, and is therefore not available for public dissemination.
REFERENCES
- 1.Rudd RA, Seth P, David F, Scholl L. Increases in Drug and Opioid-Involved Overdose Deaths - United States, 2010-2015. MMWR Morb Mortal Wkly Rep 2016;65(5051):1445–1452. [DOI] [PubMed] [Google Scholar]
- 2.Kolodny A, Courtwright DT, Hwang CS, Kreiner P, Eadie JL, Clark TW, Alexander GC. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health 2015;36:559–74. [DOI] [PubMed] [Google Scholar]
- 3.CDC. Opioid Prescribing: Where you live matters CDC Vital Signs. Atlanta, GA: Centers for Disease Control and Prevention, 2017. [Google Scholar]
- 4.Seth P, Scholl L, Rudd RA, Bacon S. Overdose Deaths Involving Opioids, Cocaine, and Psychostimulants - United States, 2015-2016. MMWR Morb Mortal Wkly Rep 2018;67(12):349–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain-United States, 2016. Jama-Journal of the American Medical Association 2016;315(15):1624–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pew Charitable Trusts. Prescription Drug Monitoring Programs: Evidence-based practices to optimize prescriber use. 2016.
- 7.Davis CS, Pierce M, Dasgupta N. Evolution and convergence of state laws governing controlled substance prescription monitoring programs, 1998-2011. Am J Public Health 2014;104(8):1389–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.NAMSDL. Compilation of State Prescription Monitoring Program Maps. Santa Fe, NM: National Alliance for Model State Drug Laws, 2014. [Google Scholar]
- 9.Kilby AA. Opioids for the masses: Welfare tradeoffs in the regulation of narcotic pain medications. Cambridge, MA: Massachusetts Institute of Technology, 2015. [Google Scholar]
- 10.Pardo B Do more robust prescription drug monitoring programs reduce prescription opioid overdose? Addiction 2016. [DOI] [PubMed] [Google Scholar]
- 11.Delcher C, Wagenaar AC, Goldberger BA, Cook RL, Maldonado-Molina MM. Abrupt decline in oxycodone-caused mortality after implementation of Florida’s Prescription Drug Monitoring Program. Drug Alcohol Depend 2015;150:63–8. [DOI] [PubMed] [Google Scholar]
- 12.Patrick SW, Fry CE, Jones TF, Buntin MB. Implementation Of Prescription Drug Monitoring Programs Associated With Reductions In Opioid-Related Death Rates. Health Aff (Millwood) 2016;35(7):1324–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li G, Brady JE, Lang BH, Giglio J, Wunsch H, DiMaggio C. Prescription drug monitoring and drug overdose mortality. Injury epidemiology 2014;1(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paulozzi LJ, Kilbourne EM, Desai HA. Prescription drug monitoring programs and death rates from drug overdose. Pain Med 2011;12(5):747–54. [DOI] [PubMed] [Google Scholar]
- 15.Nam YH, Shea DG, Shi Y, Moran JR. State prescription drug monitoring programs and fatal drug overdoses. Am J Manag Care 2017;23(5):297–303. [PubMed] [Google Scholar]
- 16.Phillips E, Gazmararian J. Implications of prescription drug monitoring and medical cannabis legislation on opioid overdose mortality. J Opioid Manag 2017;13(4):229–239. [DOI] [PubMed] [Google Scholar]
- 17.Dowell D, Zhang K, Noonan RK, Hockenberry JM. Mandatory Provider Review And Pain Clinic Laws Reduce The Amounts Of Opioids Prescribed And Overdose Death Rates. Health Aff (Millwood) 2016;35(10):1876–1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim M The impact of prescription drug monitoring programs on opioid-related poisoning deaths. Vol. Doctor of Philosophy. Baltimore, Maryland: Johns Hopkins University, 2013. [Google Scholar]
- 19.Fink DS, Schleimer JP, Sarvet A, Grover KK, Delcher C, Castillo-Carniglia A, Kim JH, Rivera-Aguirre AE, Henry SG, Martins SS, Cerda M. Association Between Prescription Drug Monitoring Programs and Nonfatal and Fatal Drug Overdoses: A Systematic Review. Ann Intern Med 2018;168(11):783–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pauly NJ, Slavova S, Delcher C, Freeman PR, Talbert J. Features of prescription drug monitoring programs associated with reduced rates of prescription opioid-related poisonings. Drug Alcohol Depend 2018;184:26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clark W, Avery K. The Effects of Data Aggregation in Statistical Analysis. Geographical Analysis 1976;8(4):428–438. [Google Scholar]
- 22.Smith N, Martins SS, Kim J, Rivera-Aguirre A, Fink DS, Castillo-Carniglia A, Henry SG, Mooney SJ, Marshall BDL, Davis C, Cerda M. A typology of prescription drug monitoring programs: A latent transition analysis of the evolution of programs from 1999 to 2016. Addiction 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seth P, Rudd RA, Noonan RK, Haegerich TM. Quantifying the Epidemic of Prescription Opioid Overdose Deaths. Am J Public Health 2018;108(4):500–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Center for Health Statistics. Mortality—all county, micro-data and compressed, 2002-2016, for 49 states and DC, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. 2017.
- 25.PDAPS. Prescription Drug Abuse Policy System. Available from: http://pdaps.org/, 2017.
- 26.Duncan TE, Duncan SC, Alpert A, Hops H, Stoolmiller M, Muthen B. Latent variable modeling of longitudinal and multilevel substance use data. Multivariate Behavioral Research 1997;32(3):275–318. [DOI] [PubMed] [Google Scholar]
- 27.Muthen B, Muthen LK. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism-Clinical and Experimental Research 2000;24(6):882–891. [PubMed] [Google Scholar]
- 28.Muthen B Latent variable analysis: Growth mixture modeling and related techniques for longitudinal data In: Kaplan D, ed. Handbook of quantitative methodology for the social sciences. Newbury Park, CA: Sage, 2004;345–368. [Google Scholar]
- 29.Hedegaard H, Warner M, Minino A. Drug Overdose Deaths in the United States, 1999-2015. NCHS Data Brief No. 273, 2017. [PubMed] [Google Scholar]
- 30.Gugelmann H, Perrone J, Nelson L. Windmills and pill mills: can PDMPs tilt the prescription drug epidemic? J Med Toxicol 2012;8(4):378–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Clark T, Eadie JL, Kreiner P, Strickler G. Prescription Drug Monitoring Programs: An Assessment of the Evidence for Best Practices. Heller School for Social Policy and Management, Brandeis University: The Pew Charitable Trusts, 2012. [Google Scholar]
- 32.Rudd R, Aleshire N, Zibbell J, Gladden M. Increases in Drug and Opioid Overdose Deaths -- United States, 2000-2014. MMWR 2016;64(50):1378–82. [DOI] [PubMed] [Google Scholar]
- 33.Ciccarone D The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. International Journal of Drug Policy 2019; 10.1016/j.drugpo.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chung H, Lanza ST, Loken E. Latent transition analysis: Inference and estimation. Statistics in Medicine 2008;27(11):1834–1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bakk Z, Oberski D, Vermunt J. Relating latent class assignments to external variables: Standard errors for correct inference. Political Analysis 2014;22:520–540. [Google Scholar]
- 36.Cerda M, Gaidus A, Keyes KM, Ponicki W, Martins S, Galea S, Gruenewald P. Prescription opioid poisoning across urban and rural areas: identifying vulnerable groups and geographic areas. Addiction 2017;112(1):103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bohnert AS, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, Blow FC. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA 2011;305(13):1315–21. [DOI] [PubMed] [Google Scholar]
- 38.Geolytics Estimates Premium. Geolytics, Inc. In: Geolytics Estimates Premium, ed. East Brunswick, NJ, 2011. [Google Scholar]
- 39.Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA Intern Med 2014;174(10):1668–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shi Y Medical marijuana policies and hospitalizations related to marijuana and opioid pain reliever. Drug Alcohol Depend 2017;173:144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rees DI, Sabia J, Argys L, Latshaw J, Dave D. With a Little Help from My Friends: The Effects of Naloxone Access and Good Samaritan Laws on Opioid-Related Deaths. NBER Working Paper No. 23171, 2017. [Google Scholar]
- 42.McClellan C, Lambdin BH, Ali MM, Mutter R, Davis CS, Wheeler E, Pemberton M, Kral AH. Opioid-overdose laws association with opioid use and overdose mortality. Addict Behav 2018. [DOI] [PubMed] [Google Scholar]
- 43.Besag J, York J, Mollie A. Bayesian image restoration, with two applications to spatial statistcs (with discussion). Annals of the Institute of Statistical Mathematics 1991;43:1–59. [Google Scholar]
- 44.Bernardinelli L, Clayton D, Pascutto C, Montomoli C, Ghislandi M, Songini M. Bayesian analysis of space-time variation in disease risk. Stat Med 1995;14(21-22):2433–43. [DOI] [PubMed] [Google Scholar]
- 45.Carlin B, Louis T. Bayes and Empirical Bayes Methods for Data Analysis, 2nd ed New York: Chapman & Hall, 2000. [Google Scholar]
- 46.Almon S The distributed lag between capital appropriations and net expenditures. Econometrica 1965;33:178–196. [Google Scholar]
- 47.Gibbons C, Suárez Serrato J, Urbancic M. Broken or fixed effects? Vol. Working Paper 20342. Cambridge, MA: National Bureau of Economic Research, 2018. [Google Scholar]
- 48.Waller L, Gotway C. Applied Spatial Statistics for Public Health Data. Wiley Series in Probability and Statistics Wiley Publishers, 2004. [Google Scholar]
- 49.Greene W Econometric Analysis, 7th edition New York, NY: Prentice-Hall, 2012. [Google Scholar]
- 50.Rue H, Martino S, Chopin N. Approximate Bayesian inference for latent Gaussian models using integrated nested Laplace approximations (with discussion). Journal of the Statistical Society, Series B 2009;71(2):319–392. [Google Scholar]
- 51.Blangiardo M, Cameletti M. Spatial and Spatial-Temporal Bayesian Models with R-INLA. Chichester, UK: Wiley, 2015. [Google Scholar]
- 52.Ruhm CJ. Geographic Variation in Opioid and Heroin Involved Drug Poisoning Mortality Rates. Am J Prev Med 2017;53(6):745–753. [DOI] [PubMed] [Google Scholar]
- 53.PDMP Center of Excellence. Guidance on PDMP Best Practices: Options for Unsolicited Reporting. Waltham, MA: Heller School, Brandeis University, 2016;http://www.pdmpassist.org/pdf/PDMP_admin/Update%20to%20%20Guidance%20on%20Unsolicited%20Reporting%20final.pdf. [Google Scholar]
- 54.Young LD, Kreiner PW, Panas L. Unsolicited Reporting to Prescribers of Opioid Analgesics by a State Prescription Drug Monitoring Program: An Observational Study with Matched Comparison Group. Pain Med 2017. [DOI] [PubMed] [Google Scholar]
- 55.McDonald DC, Carlson KE, Jalbert SK. An Experimental Test of the Effectivess of Unsolicited Reporting by a Prescription Drug Monitoring Program in Reducing Inappropriate Acquisition of Opioids. Pain Med 2018. [DOI] [PubMed] [Google Scholar]
- 56.Surratt HL, O’Grady C, Kurtz SP, Stivers Y, Cicero TJ, Dart RC, Chen M. Reductions in prescription opioid diversion following recent legislative interventions in Florida. Pharmacoepidemiol Drug Saf 2014;23(3):314–20. [DOI] [PubMed] [Google Scholar]
- 57.Meinhofer A. Prescription Drug Monitoring Programs: The Role of Asymmetric Information on Drug Availability and Abuse. Journal of Health Economics 2017. (early access):1–48. [Google Scholar]
- 58.Delcher C, Wang Y, Wagenaar AC, Goldberger BA, Cook RL, Maldonado-Molina MM. Prescription and Illicit Opioid Deaths and the Prescription Drug Monitoring Program in Florida. Am J Public Health 2016;106(6):e10–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yuanhong Lai A, Smith KC, Vernick JS, Davis CS, Caleb Alexander G, Rutkow L. Perceived Unintended Consequences of Prescription Drug Monitoring Programs. Substance Use & Misuse 2019;54(2):345–349. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.