Abstract
Introduction:
Romantic partners are crucial to successful smoking cessation, but the mechanisms by which partners influence cessation is unclear. Research in this area has focused heavily on partner smoking status and support for quitting, but partner influence may not be limited to these two constructs. The current study examines the perceived responsiveness of the partner (i.e., the perception that the partner understands, approves of, and supports the self) as a predictor of smoking cessation in unassisted quitters, independent of smoking-specific support for quitting and more general relationship satisfaction.
Methods:
Data were taken from a sample of smokers (N=62) in relationships with never/former smokers (i.e., members of single-smoker couples) who completed a 21-day ecological momentary assessment study during an unassisted quit attempt. Measures of perceived responsiveness, support for quitting, and relationship satisfaction obtained at baseline were used to predict smoking outcomes over the course of the study.
Results:
Consistent with our predictions, perceived responsiveness emerged as a significant predictor of smoking cessation over and above the effects of support for quitting and relationship satisfaction. Support for quitting only predicted self-reported relapse. Unexpectedly, once perceived responsiveness was considered, greater relationship satisfaction was associated with poorer smoking outcomes.
Conclusions:
The current research suggests that perceived responsiveness is a more effective resource for smoking cessation than support specifically for quitting. These findings extend previous research by demonstrating that perceived responsiveness represents a distinct construct from smoking-specific support or relationship satisfaction, and that it is important for smokers during a quit attempt.
Keywords: perceived partner responsiveness, support for quitting, relationship satisfaction, smoking cessation
INTRODUCTION
Smokers’ romantic partners are crucial to successful smoking cessation. The partner’s mere smoking status is a strong predictor of cessation: smokers are more likely to quit smoking if partnered with a non-smoker than a smoker (Homish & Leonard, 2005; Jackson, Steptoe, & Wardle, 2015) and smokers who quit are more likely to relapse if partnered with a smoker than a non-smoker (Homish & Leonard, 2005; Pollak & Mullen, 1997). The influence of a partner’s smoking status on successful quitting may be due, at least in part, to the partner’s support for and against quitting smoking (Ginsberg, Hall, & Rosinski, 1991; Lüscher, Stadler, & Scholz, 2017; Scholz et al., 2016). However, the perceived responsiveness of the partner (i.e., the perception that the partner understands, approves of, and supports the self; Reis & Clark, 2013; Reis & Shaver, 1988) may have greater predictive utility than the partner’s support for quitting, given that perceived availability of support is often a better predictor of health outcomes than received support (Lakey & Cassady, 1990; Stroebe & Stroebe, 1996). The current paper examines perceived responsiveness as a predictor of smoking outcomes during a quit attempt.
Perceived Responsiveness and Smoking
Previous research suggests that more general social support (i.e., not specific to smoking) is associated with smoking cessation (Holahan et al., 2012; Pollak & Mullen, 1997; Vӓӓanӓnen, Kouvonen, Kivimӓki, Pentti, & Vahtera, 2008). However, only one longitudinal study has examined the association between perceived responsiveness of the partner and smoking cessation. Derrick and colleagues (2013) examined the influence of perceived responsiveness on smoking status and cigarette quantity in a sample of newlywed couples. Among those who initially perceived relatively high responsiveness, both the likelihood of being a smoker and the number of cigarettes smoked decreased over time. This decrease was not apparent for those who initially perceived relatively low responsiveness. This study was notable in that it demonstrated decreases in smoking in a community sample of participants selected for marital status and not desire to quit smoking. Although this is one strength of the study, it is also a possible limitation; perceived responsiveness might not matter for people who are already motivated to quit smoking. Alternatively, assessments of perceived responsiveness might simply tap into support for quitting or relationship satisfaction, constructs known to be associated with smoking cessation. The current study builds on these findings in three important ways.
First, data for the current analyses were taken from a larger parent study that followed smokers (i.e., Quitters) and their partners during a 21-day quit attempt (Derrick et al., 2017; Derrick et al., in press). Single-smoker couples were targeted in the parent study because nonsmoking partners provide more support for quitting (McBride et al., 1998; vanDellen, Boyd, Ranby, MacKillop, & Lipkus, 2016), and Quitters are more likely to quit if their partner is a nonsmoker (Falba & Sindelar, 2007; Homish & Leonard, 2005). It is important to demonstrate that perceived responsiveness predicts smoking outcomes specifically during a quit attempt. Otherwise, we cannot rule out the possibility that people who are motivated to quit smoking are less influenced by perceived responsiveness —because they already have the resources (e.g., self-motivation) needed to quit smoking.
Second, the current study examines whether perceived responsiveness is distinguishable from support for quitting smoking. Greater support for quitting predicts greater likelihood of quitting smoking (Coppotelli & Orleans, 1985; Lüscher et al., 2017; Scholz et al., 2016), but studies examining support for quitting have primarily examined special populations, like pregnant women (McBride et al., 1998; Pollak, Baucom, Peterson, Stanton, & McBride, 2006) or smokers undergoing treatment (Lawhon, Humfleet, Hall, Reus, & Muñoz, 2009; Mermelstein, Lichtenstein, & McIntyre, 1983). In addition, studies that have examined general support or perceived responsiveness have not ruled out the possibility that these perceptions are merely tapping into support for quitting (Derrick et al., 2013; Väänaänen et al., 2008). It is important to compare perceived responsiveness directly with support for quitting to demonstrate that the two constructs differentially impact smoking outcomes, and therefore, represent distinct constructs.
Finally, this study also considers relationship satisfaction, an important predictor of health behaviors (Burman & Margolin, 1992; Derrick & Leonard, 2016; Lewis et al., 2006). Couples who report higher satisfaction are less likely to binge drink or develop future alcohol problems and have better outcomes following treatment for substance dependence (Heinz, Wu, Witkiewitz, Epstein, & Preston, 2009; Leonard & Homish, 2008; Whisman, Uebelacker, & Bruce, 2006). Most important to the current study, people in higher quality relationships smoke less (Fleming, White, & Catalano, 2010). Although overlapping constructs, perceived responsiveness is a more sensitive predictor of relationship functioning than relationship satisfaction; changes in perceived responsiveness predict changes in relationship satisfaction over time, but not vice versa (Derrick et al., 2012). Therefore, perceived responsiveness may also be a more sensitive predictor of smoking cessation than relationship satisfaction. It is important to distinguish between these two constructs when examining smoking outcomes.
Overview and Hypotheses
In the current study, we examined the effect of perceived responsiveness on smoking outcomes during a 21-day quit attempt. We directly compared the effects of perceived responsiveness to the effects of support for quitting and relationship satisfaction. Like Derrick et al. (2013), we focused on perceived responsiveness, rather than enacted support, because perceived availability of support is a more consistent predictor of health and well-being than received support (Lakey & Orehek, 2011; Stroebe & Stroebe, 1996). We expected perceived responsiveness to predict smoking outcomes above and beyond support for quitting and relationship satisfaction.
METHOD
Participants
Data were taken from the Daily Experiences with Smoking Cessation (DESC) Study. Couples were recruited primarily through paid Facebook advertising and mass mailing (Derrick et al., 2017). To be eligible, couples had to meet relationship criteria (a different-sex relationship; cohabiting 6+ months or married; one smoker and one never/former smoker), demographic criteria (both partners aged 18–55; comfortable reading/writing English), Quitter smoking criteria (smoked 10+ cigarettes per day for the past 2+ years; no non-cigarette forms of tobacco; motivation to quit of 50+ on a 1–100 scale; not seeing a provider or taking medication to quit smoking), logistical criteria (partners lived together; both could access smart phones during the day), and safety criteria (i.e., no severe intimate partner violence). Additionally, both partners had to agree to participate, and the Quitter had to stop smoking 12 hours prior to the first appointment (verified with an expelled breath carbon monoxide [CO] reading of <10 parts per million [ppm]; West, Hajek, Stead, & Stapleton, 2005). Sixty-four couples attended the initial appointment. One couple did not reschedule after a failed CO reading, and one couple dropped the first day of participation, leaving a final sample of 62 couples. The current analyses focus on data collected from the Quitter.
Procedure
Full details regarding the recruitment process and participation rates are available elsewhere (Derrick et al., in press; Derrick et al., 2017). Briefly, background questionnaires, including motivation to quit, nicotine dependence, support for quitting, and demographics were completed online before the orientation session. At the orientation session, both partners provided CO readings using a Bedfont piCO Smokerlyzer (http://www.bedfont.com/). Quitters who failed the CO reading (>10ppm) rescheduled their orientation session. Those who passed completed additional laboratory tasks and background questionnaires, including perceived responsiveness and relationship satisfaction. Then we provided participants with Android smart phones and training for the ecological momentary assessment (EMA). The use of EMA to assess smoking is valuable in that we can assess participants in near-real-time, thereby reducing the bias introduced by retrospective recall. EMA allows for more precise reporting on smoking outcomes than survey or Timeline Followback methodology (Shiffman, 2009; Shiffman, Stone, & Hufford, 2008).
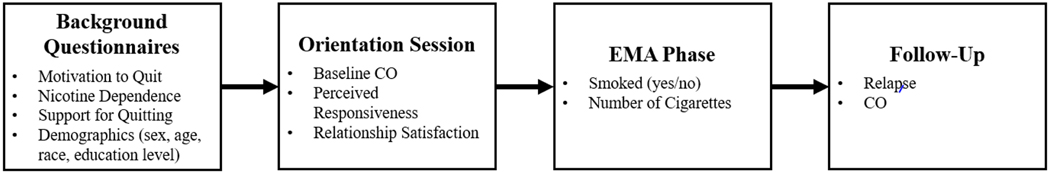
The evening of the orientation session, and for the next 21 days, both partners completed the EMA using a web application. We chose to study smoking outcomes over 21 days because most relapses occur early after a smoker decides to make a quit attempt (22% within two weeks; 19% within one month; Hughes et al., 1992). Each day, both partners completed Evening Reports before bed, Morning Reports as soon as they woke up, and three Random Prompt Reports when signaled. Both partners also completed a Lapse Report anytime the Quitter smoked (or the Partner assumed the Quitter smoked). In each report, both partners were asked about mood, interactions with the partner and other people, and the Quitter’s smoking behavior. Additional details about the content of each report are available in Derrick et al. (in press). After the EMA, couples attended a follow-up session. Quitters reported whether they had relapsed, among other questionnaires, and reports were biochemically verified. They returned the study smart phones and received payment (up to 150 USD per partner) for their participation. Figure 1 provides a visual summary of the various data collected at each assessment point.
Figure 1.
Summary of the relevant data collected at each assessment point.
Measures
Motivation to quit.
Quitters responded to one item, “How motivated are you to quit smoking?” on a scale from 1 (not at all motivated) to 7 (extremely motivated).
Nicotine dependence.
The Fagerström Test for Nicotine Dependence (Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991) measured Quitters’ nicotine dependence on a 6-item scale. Responses were summed (α=. 65) to create the final score.
Support for quitting.
The 20-item expected version of the Partner Interaction Questionnaire (Cohen & Lichtenstein, 1990) was used to assess expectations of support for quitting smoking. Quitters indicated the extent to which their partner would enact positive (α=.94) and negative (α=.85) behaviors on a scale from 1 (strongly disagree) to 7 (strongly agree). The score for positive behaviors was divided by the score for negative behaviors to create a ratio score (Cohen & Lichtenstein, 1990).
Satisfaction.
The Couples Satisfaction Index (Funk & Rogge, 2007) measured Quitters’ relationship satisfaction on a 32-item scale. Responses were averaged (α=. 97) to create the final score.
Perceived responsiveness.
As in other work (e.g., Derrick et al., 2013; Testa et al., in press), the six-item emotional intimacy subscale of the Personal Assessment of Intimacy in Relationships (Schaefer & Olson, 1981) was used to assess perceived responsiveness. The items in this subscale capture perceptions of the partner’s understanding (e.g., “My partner can really understand my hurts and joys”), approval (e.g., “I can state my feelings without him/her getting defensive”), and support (e.g., “My partner listens to me when I need someone to talk to”). Quitters answered on a scale from 1 (strongly disagree) to 7 (strongly agree). Responses were averaged (α=.87) to create the final score.
Demographics.
Participants completed a measure of demographics that included gender, age, race, and education.
Smoking outcomes.
For number of smoking days, we coded each day in the EMA for smoking by the Quitter reported by either partner (0=no smoking, 1=smoking) and summed these values. Number of cigarettes was computed by summing the Quitter’s reports of how many cigarettes they smoked (from 1 to 10+) across all reports and Winsorizing at the 95th percentile. We calculated first week smoking and final week smoking based on whether the Quitter smoked within the first seven days (West, Hajek, Stead, & Stapleton, 2005) or final seven days (Velicer & Prochaska, 2004) of the EMA phase (0=abstinent, 1=smoked). To assess relapse, the Quitter responded to the question, “Did you relapse during the study?” (0=no, 1=yes). Finally, we used participants’ CO readings at follow-up as a biochemical assessment of recent smoking.
Data Analysis
Data for the count, binomial, and linear outcomes, respectively, were analyzed using a series of negative binomial, logistic, and linear block sequential regressions with robust standard errors. Six participants did not complete background measures, and one participant did not attend the follow-up appointment. We conducted analyses in Stata 14 (StataCorp, 2013) and Mplus 8 (Muthén, 2007) using the runmplus command (Jones, 2013) to capitalize on Mplus’ ability to employ full information maximum likelihood estimation to handle missing data. In the first block of the analyses, we included outcome-specific, smoking-related, and demographic control variables. In the second block, we included support for quitting and relationship satisfaction. In the third block, we entered the variable of primary interest, perceived responsiveness. All continuous predictor variables were centered at the mean prior to analysis (except education, which was centered at 12 years). We confine our in-text discussion to effects involving relationship characteristics.
RESULTS
Descriptive Statistics
Demographic information and descriptive statistics are presented in Table 1. Overall, Quitters reported relatively responsive and satisfying relationships. They expected their partner to provide relatively more positive (M = 4.74, SD = 1.59) than negative (M = 3.78, SD = 1.51) support for quitting, t(55)=3.53, d=0.62,p<.001, with an average expected ratio of three positive behaviors for every two negative behaviors (see Table 1). Bivariate correlations demonstrated that perceived responsiveness was positively and strongly correlated with satisfaction (r=.77, p<.001) but neither variable was associated with support for quitting, r=−.003, p=.981 and r=.09, p=.494, respectively. Most Quitters smoked in the first and final weeks of the EMA. At follow-up, most Quitters reported that they had relapsed, and 60% scored a 10 or higher on their follow-up CO reading.
Table 1.
Demographic information and descriptive statistics for the quitter.
| M (SD) | Range | |
| Demographics | ||
| Age | 35.69 (8.79) | 20–54 |
| Education Level | 13.28 (1.76) | 10–18 |
| Relationship Length | 6.12 (6.83) | 0.83–30.42 |
| % | ||
| Sex | 39 | 0–1 |
| Race | 74 | 0–1 |
| Relationship Status | 41 | 0–1 |
| Work | 34 | 0–1 |
| Children | 54 | 0–1 |
| M (SD) | ||
| Relationship Predictors | ||
| Perceived Responsiveness | 4.90 (1.19) | 1.66–6.67 |
| Satisfaction | 4.99 (0.73) | 2.81–5.97 |
| Support for quitting | 1.47 (0.76) | 0.17–3.63 |
| Smoking Outcomes | ||
| Number of smoking days | 15 (6.96) | 0–22 |
| Number of cigarettes | 47.95 (54.99) | 0–191 |
| % | ||
| First week smoking | 91 | 0–1 |
| Final week smoking | 84 | 0–1 |
| Relapse | 71 | 0–1 |
| M (SD) | ||
| CO | 14.84 (11.43) | 1–52 |
| Control Variables | ||
| Nicotine Dependence | 4.05 | 0–9 |
| Motivation to Quit | 5.45 | 2–17 |
| Number of Complete Days | 20 | 0–22 |
| Baseline CO | 6.60 | 2–17 |
Note. N = 62. Age, education, and relationship length are reported in years. Sex is coded 0 = male, 1 = female. Race is coded 0 = other 1 = white. Relationship status is coded 0 = married, 1 = cohabiting. Work is coded 0 = at least part time, 1 = less than part time. Children is coded 0 = no children, 1 = 1 or more. M = mean; SD = standard deviation.
Number of Smoking Days
Results for negative binomial regressions examining number of smoking days are presented on the left side of Table 2. Neither support for quitting nor relationship satisfaction was significant at entry, but perceived responsiveness emerged as a marginally significant predictor beyond these variables. A one-unit increase in baseline perceived responsiveness was associated with 14% fewer smoking days during the EMA. Unexpectedly, satisfaction was positively associated with the number of smoking days in the final model.
Table 2.
Results of analyses examining EMA smoking data.
| Number of Smoking Days | Number of Cigarettes | |||||||
|---|---|---|---|---|---|---|---|---|
| Predictor | RR at entry | 95% CI | Final RR | 95% CI | RR at entry | 95% CI | Final RR | 95% CI |
| Intercept | - | - | 14.31*** | [12.26, 16.71] | - | - | 28.85*** | [21.88, 38.03] |
| Block 1 | ||||||||
| Number of complete days | 0.98+ | [0.95, 1.00] | 0.97* | [0.94, 1.00] | 1.07 | [0.99, 1.16] | 1.05 | [0.97, 1.15] |
| Motivation to quit | 0.91+ | [0.81, 1.01] | 0.88* | [0.77, 1.00] | 0.77** | [0.65, 0.91] | 0.76** | [0.62, 0.93] |
| Nicotine dependence | 1.05+ | [1.00, 1.11] | 1.04 | [0.98, 1.10] | 1.18** | [1.07, 1.30] | 1.20** | [1.07, 1.34] |
| Sex | 1.18 | [0.89, 1.56] | 1.15 | [0.85, 1.56] | 1.54+ | [0.94, 2.53] | 1.75+ | [0.95, 3.22] |
| Age | 1.01 | [0.99, 1.02] | 1.01 | [1.00, 1.02] | 1.03* | [1.00, 1.05] | 1.03* | [1.01, 1.06] |
| Race | 0.99 | [0.76, 1.29] | 1.00 | [0.76, 1.32] | 0.80 | [0.46, 1.41] | 0.73 | [0.41, 1.29] |
| Education level | 1.03 | [0.95, 1.11] | 1.01 | [0.93, 1.09] | 1.19** | [1.06, 1.34] | 1.18* | [1.04, 1.35] |
| Block 2 | ||||||||
| Support for quitting | 1.08 | [0.89, 1.32] | 1.07 | [0.88, 1.31] | 0.93 | [0.66, 1.32] | 0.93 | [0.65, 1.32] |
| Relationship satisfaction | 1.13 | [0.95, 1.35] | 1.35* | [1.02, 1.79] | 1.50 | [0.90, 2.52] | 1.66 | [0.70, 3.94] |
| Block 3 | ||||||||
| Perceived responsiveness | - | - | 0.86+ | [0.73, 1.02] | - | - | 0.93 | [0.61, 1.43] |
Note. Data were analyzed using block sequential negative binomial regressions. N = 62. RR = risk ratio; 95% CI = 95% confidence interval.
p < .10
p < .05
p < .01
p <.001
Number of Cigarettes
Results for negative binomial regressions examining number of cigarettes are presented on the right side of Table 2. After controlling for demographic characteristics, none of the relationship predictors were significant.
First Week Smoking1
Results for logistic regressions examining first week smoking are presented on the left side of Table 3. After controlling for demographic characteristics, none of the relationship predictors were significant.
Table 3.
Results analyses examining first and final week smoking.
| First Week Smoking | Final Week Smoking | |||||||
|---|---|---|---|---|---|---|---|---|
| Predictor | OR at entry | 95% CI | Final OR | 95% CI | OR at entry | 95% CI | Final OR | 95% CI |
| Intercept | - | - | 0.05** | [0.01, 0.30] | - | - | 0.11** | [0.30, 0.40] |
| Block 1 | ||||||||
| Motivation to quit | 0.37+ | [0.12, 1.16] | 0.39 | [0.13, 1.21] | 0.63 | [0.24, 1.63] | 0.45 | [0.13, 1.53] |
| Nicotine dependence | 1.02 | [0.66, 1.57] | 0.94 | [0.64, 1.37] | 1.00 | [0.77, 1.30] | 0.91 | [0.67, 1.23] |
| Sex | - | - | - | - | - | - | - | - |
| Age | 0.97 | [0.88, 1.07] | 0.97 | [0.90, 1.05] | 1.02 | [0.93, 1.12] | 1.02 | [0.91, 1.14] |
| Race | 2.65 | [0.34, 20.46] | 3.11 | [0.32, 29.90] | 1.43 | [0.33, 6.24] | 1.62 | [0.34, 7.69] |
| Education level | 1.03 | [0.56, 1.89] | 0.92 | [0.44, 1.92] | 1.03 | [0.69, 1.54] | 0.84 | [0.56, 1.27] |
| Block 2 | ||||||||
| Support for quitting | 1.16 | [0.25, 5.32] | 1.04 | [0.19, 5.57] | 2.29 | [0.49, 10.76] | 2.16 | [0.46, 10.16] |
| Relationship satisfaction | 1.55 | [0.44, 5.42] | 3.40 | [0.32, 35.84] | 1.13 | [0.45, 2.82] | 5.67+ | [0.88, 36.56] |
| Block 3 | ||||||||
| Perceived responsiveness | - | - | 0.47 | [0.12, 1.77] | - | - | 0.26* | [0.08, 0.78] |
Note. Data were analyzed using block sequential logistic regressions. N = 62. Sex was dropped from the analyses for first week smoking because the model would not converge due to problems with multicollinearity. Perceived responsiveness marginally predicts final week smoking when satisfaction is omitted from the model, OR = 0.61, 95% CI = [0.35, 1.06],p = .079. OR = odds ratio; 95% CI = 95% confidence interval.
p < .10
p < .05
p < .01
Final Week Smoking2
Results for logistic regressions examining final week smoking are presented on the right side of Table 3. Neither support for quitting nor relationship satisfaction was significant at entry, but perceived responsiveness emerged as a significant predictor beyond these variables. A one- unit increase in baseline perceived responsiveness was associated with a 74% decrease in the likelihood of smoking during the final week of the EMA. Unexpectedly, greater relationship satisfaction was marginally associated with increased likelihood of smoking in the final model.
Self-Reported Relapse
Results for logistic regressions examining self-reported relapse are presented on the left side of Table 4. Support for quitting emerged as a marginally significant predictor of self-reported relapse at entry and as a significant predictor in the final model. A one-unit increase in baseline support for quitting was associated with a 69% decreased likelihood of self-reporting relapse. Unexpectedly, perceived responsiveness did not emerge as a significant predictor.
Table 4.
Results of analyses examining follow-up assessments.
| Relapse | CO | |||||||
|---|---|---|---|---|---|---|---|---|
| Predictor | OR at entry | 95% CI | Final OR | 95% CI | b at entry | 95% CI | Final b | 95% CI |
| Intercept | - | - | 0.20** | [0.07, 0.63] | - | - | 15.55*** | [12.63, 18.47] |
| Block 1 | ||||||||
| Baseline CO | - | - | - | - | 0.74+ | [−0.04, 1.52] | 0.82* | [0.06, 1.59] |
| Motivation to quit | 0.52* | [0.29, 0.91] | 0.57 | [0.28, 1.16] | −0.98 | [−2.69, 0.73] | −1.44 | [−3.45, 0.57] |
| Nicotine dependence | 1.27+ | [0.96, 1.68] | 1.29 | [0.93, 1.80] | 1.55* | [0.34, 2.77] | 1.06* | [0.02, 2.10] |
| Sex | 0.68 | [0.19, 2.46] | 0.83 | [0.20, 3.45] | 0.82 | [−4.61, 6.26] | 0.52 | [−5.45, 6.49] |
| Age | 1.03 | [0.94, 1.13] | 1.04 | [0.97, 1.13] | 0.24 | [−0.10, 0.58] | 0.27+ | [−0.05, 0.58] |
| Race | 0.76 | [0.13, 4.41] | 0.58 | [0.09, 3.94] | 0.88 | [−4.15, 5.90] | 1.05 | [−4.25, 6.35] |
| Education level | 0.87 | [0.61, 1.22] | 0.88 | [0.59, 1.32] | −0.09 | [−1.43, 1.25] | −0.42 | [−1.70, 0.86] |
| Block 2 | ||||||||
| Support for quitting | 0.30* | [0.11, 0.87] | 0.31* | [0.11, 0.89] | −1.42 | [−5.38, 2.55] | −1.75 | [−5.72, 2.22] |
| Relationship satisfaction | 0.66 | [0.18, 2.50] | 0.63 | [0.09, 4.61] | 1.00 | [−2.74, 4.74] | 5.44* | [0.54, 10.34] |
| Block 3 | ||||||||
| Perceived responsiveness | - | - | 1.06 | [0.38, 2.95] | - | - | −3.70* | [−7.21, −0.19] |
Note. Relapse was analyzed using block sequential logistic regressions and CO was analyzed using block sequential linear regressions. N = 62. OR = odds ratio; b = unstandardized regression coefficient; 95% CI = 95% confidence interval.
p < .10
p < .05
p < .01
p <.001
Expelled Breath CO
Results of linear regressions examining expelled breath CO readings at follow-up are presented on the right side of Table 4. Neither support for quitting nor relationship satisfaction was significant at entry, but perceived responsiveness emerged as a significant predictor beyond these variables. A one-unit increase in baseline perceived responsiveness was associated with a 3.70 ppm decrease in CO at follow-up. Unexpectedly, greater relationship satisfaction was associated with an increase in CO at follow-up.
DISCUSSION
The current study examines the impact of relationship variables on smoking cessation. Whereas previous studies have focused on the impact of support for quitting (Ginsberg et al., 1991; Lüscher et al., 2017; Scholz et al., 2016), the current study moved beyond this narrow scope to examine perceptions of the partner’s willingness and ability to provide support (i.e., perceived responsiveness). Consistent with other studies that have examined the effects of more general support ( Pollak & Mullen, 1997; Väänänen et al., 2008), and building on Derrick et al. (2013), we found that greater perceived responsiveness was associated with better smoking cessation outcomes. Our findings extend this previous literature by demonstrating that perceived responsiveness predicts smoking outcomes above and beyond support for quitting and relationship satisfaction, and among smokers making a quit attempt.
Perceived responsiveness predicted the occurrence and quantity of smoking during the EMA (i.e., near-real-time assessment), as well as CO at follow-up (i.e.,physiological assessment). Support for quitting was only associated with the Quitter’s self-report of relapse. It seems relatively unlikely that our EMA and physiological assessments would be biased by social desirability concerns, faulty memory, or interviewer demand, but our assessment of relapse was retrospective, self-reported, and self-defined (i.e., we did not provide a definition of “relapse” as part of the question wording). Although some Quitters might report relapsing after merely one cigarette, other Quitters might not report relapsing until they were smoking at their previous, pre- quit-attempt levels. Perceived responsiveness may have greater predictive utility for more objective and standardized smoking outcomes, whereas support for quitting may better predict more “subjective” outcomes.
Despite the fact that higher relationship quality is often associated with better substance use outcomes (Derrick & Leonard, 2016), relationship satisfaction in the current study often emerged as a positive predictor of smoking once perceived responsiveness was included in the models.3,4 Perceived responsiveness appears to be acting as a suppressor variable (MacKinnon, 2008). Once levels of perceived responsiveness are taken into account, relationship satisfaction itself is not a protective factor for smoking cessation, and may even be problematic, at least in the absence of high perceived responsiveness. Previous research on substance abuse treatment has found that high relationship satisfaction may lead partners to view substance use as less of a problem, leaving them to offer less support for treatment (McCollum, Nelson, Lewis, & Trepper, 2005). Additionally, the positive effect of relationship satisfaction on smoking could be due to a person’s desire to maintain harmony, or avoid conflict, in their relationship. Relationship satisfaction is associated with forgiveness (e.g., Fincham & Beach, 2007; Fehr, Gelfand, & Nag, 2010). Once perceived responsiveness is taken into account, smokers with higher relationship satisfaction might smoke because they know that their partner will forgive such behavior. Therefore, it is important for researchers to consider multiple aspects of marital quality when considering partner influence on smoking cessation and other health behaviors.
Limitations and Strengths
There are at least three limitations to the current study. First, these data were taken from a study with a relatively small sample size (N=62 couples), so our analyses may have been underpowered. Second, only half of the couples that qualified to participate in the parent study actually participated (Derrick et al., 2017). Smokers were required to stop smoking at least 12 hours prior to their orientation session, so the final sample might have been less nicotine dependent, more highly motivated to quit, or in a different “stage of change” (e.g., the “action” stage vs. the “preparation” stage; Prochaska & Velicer, 1997) than smokers who did not participate. Third, this study examined unaided smoking cessation in different-sex, single-smoker couples. The effect of perceived responsiveness on smoking cessation might be different in a treatment study, where participants have an external source of support, or in dual-smoker couples, where partners might be less supportive of quitting (if not quitting themselves) or in need of support as well (if also quitting). We would not necessarily expect that support dynamics would be different in same-sex couples (Kurdek, 2003, 2004), but we are unable to rule out this possibility in the current study.
Despite these limitations, the current study also had four noteworthy strengths. First, it extended the results of Derrick et al. (2013), which focused on newlywed couples where one or both partners were smokers at any point during the study, to single-smoker couples engaged in an unassisted quit attempt. Therefore, we were able to demonstrate that perceived responsiveness influences smoking cessation even in those who already have effective resources (e.g., self-motivation). Second, this study is the first empirical work to demonstrate that perceived responsiveness is an important resource for quitting above and beyond behavior-specific support for quitting. Third, most of our smoking outcomes were obtained from EMA reports. The ability of EMA to assess participants in near-real-time is a great strength when assessing smoking outcomes. These reports are less biased by retrospective recall, thereby improving the accuracy of reporting cigarette quantity and other smoking behaviors (Shiffman, Stone, & Hufford, 2008; Shiffman, 2009). Finally, we also biochemically verified reports of relapse, which allows for an unbiased assessment of smoking in the final days of the study.
Conclusions
Past relationship-oriented interventions targeting smoking cessation have attempted to manipulate partner support for quitting, with little success (May & West, 2000; Park, Tudiver, Schultz, & Campbell, 2004; Westmaas et al., 2010). The results from the current study suggest that interventions might attempt to enhance perceptions of perceived responsiveness. Perceived responsiveness arises through the experience of actual, objective events demonstrating (or failing to demonstrate) caring (Collins & Feeney, 2000; Debrot, Cook, Perrez, & Horn, 2012) but also through motivated perceptions biased by people’s own needs, goals, and wishes (Lakey & Cassady, 1990; Lemay, Clark, & Feeney, 2007). If these findings were replicated, relationship-oriented smoking cessation programs might direct efforts at minimizing smokers’ negatively biased perceptions of their partner in combination with, or even instead of, targeting the partner’s actual behavior.
HIGHLIGHTS.
Romantic partners influence smoking cessation in important ways (e.g., support).
This paper examines the impact of perceived responsiveness on smoking cessation.
Perceived responsiveness predicted cessation beyond support or satisfaction.
Findings may be relevant for partner-oriented interventions for smoking cessation.
ACKNOWLEDGEMENTS
We thank Rebecca K. Eliseo-Arras, Courtney Hanny, Yan Yan Sze, Kathryn Solecki, and a team of undergraduate research assistants for their assistance in conducting this research.
FUNDING
Research reported in this publication was supported by the National Institute on Drug Abuse (NIDA) of the National Institutes of Health under award number R21DA034068. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
DECLARATION OF INTERESTS
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
We also conducted analyses examining smoking in the first 24 hours and three days. Results were comparable to those for first week smoking.
We also conducted analyses examining smoking in the final three days and 24 hours. Results were similar but the effect for perceived responsiveness failed to reach statistical significance.
Given the high correlation between satisfaction and perceived responsiveness in the current study (r=.77), readers might question what remains after the variance due to satisfaction is partialed from the equations. We believe that partialing out satisfaction takes away the variance attributable to one’s own feelings toward the partner, leaving behind beliefs about the partner’s feelings toward the self (see Derrick et al., 2012; Murray et al., 2000).
One potential explanation is that satisfaction and perceived responsiveness might be so highly correlated as to be collinear, and thus the unexpected results for satisfaction might be a statistical artifact. Indeed, inspection of our primary results (Tables 2–4) reveals unexpectedly wide confidence intervals (and inflated standard errors) for two satisfaction results (see Table 3). However, the 95% confidence intervals for perceived responsiveness appeared normal, and the effect of perceived responsiveness on smoking outcomes was marginally significant when satisfaction was omitted from the model (see note to Table 3). Furthermore, the confidence intervals for some of the demographic variables were unexpectedly wide. Therefore, the culprit for multicollinearity appears to be a demographic covariate, and not perceived responsiveness.
REFERENCES
- Burman B, & Margolin G (1992). Analysis of the association between marital relationships and health problems: An interactional perspective. Psychological Bulletin, 112(1), 39–63. 10.1037/0033-2909.112.L39 [DOI] [PubMed] [Google Scholar]
- Cohen S, & Lichtenstein E (1990). Perceived stress, quitting smoking, and smoking relapse. Health Psychology, 9(4), 466–478. 10.1037/0278-6133.9A466 [DOI] [PubMed] [Google Scholar]
- Collins NL, & Feeney BC (2000). A safe haven: An attachment theory perspective on support seeking and caregiving in intimate relationships. Journal of Personality and Social Psychology, 75(6), 1053–1073. 10.1037/0022-3514.78.6.1053 [DOI] [PubMed] [Google Scholar]
- Coppotelli HC, & Orleans CT (1985). Partner support and other determinants of smoking cessation maintenance among women. Journal of Consulting and Clinical Psychology, 53(4), 455–460. 10.1037/0022-006X.53A455 [DOI] [PubMed] [Google Scholar]
- Debrot A, Cook WL, Perrez M, & Horn AB (2012). Deeds matter: Daily enacted responsiveness and intimacy in couples’ daily lives. Journal of Family Psychology, 26(4), 617–627. 10.1037/a0028666 [DOI] [PubMed] [Google Scholar]
- Derrick JL, Eliseo-Arras RK, Haddad S, Britton M, & Hanny C (in press). Feasibility of Using Ecological Momentary Assessment to Study Unaided Smoking Cessation in Couples. Nicotine & Tobacco Research; 10.1093/ntr/ntx240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derrick JL, Eliseo-Arras RK, Hanny C, Britton M, & Haddad S (2017). Comparison of internet and mailing methods to recruit couples into research on unaided smoking cessation. Addictive Behaviors, 75, 12–16. https://doi.org/10.1016ZJ.ADDBEH.2017.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derrick JL, & Leonard KE (2016). Substance Use in Committed Relationships. (Sher KJ, Ed.) (Vol. 1). Oxford University Press; 10.1093/oxfordhb/9780199381678.013.012 [DOI] [Google Scholar]
- Derrick JL, Leonard KE, & Homish GG (2012). Dependence regulation in newlywed couples: A prospective examination. Personal Relationships, 19(4), 644–662. 10.1111/j.1475-6811.2011.01384.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derrick JL, Leonard KE, & Homish GG (2013). Perceived Partner Responsiveness Predicts Decreases in Smoking During the First Nine Years of Marriage. Nicotine & Tobacco Research, 15(9), 1528–1536. 10.1093/ntr/ntt011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falba TA, & Sindelar JL (2007). Spousal Concordance in Health Behavior Change. Health Services Research, 43(1p1), 96–116. 10.1111/j.1475-6773.2007.00754.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehr R, Gelfand MJ, & Nag M (2010). The road to forgiveness: a meta-analytic synthesis of its situational and dispositional correlates. Psychological Bulletin, 136(5), 894–914. 10.1037/a0019993 [DOI] [PubMed] [Google Scholar]
- Fincham F, & Beach SR (2007). Forgiveness and marital quality: Precursor or consequence in well-established relationships?. The Journal of Positive Psychology, 2(4), 260–268. 10.1080/17439760701552360 [DOI] [Google Scholar]
- Fleming CB, White HR, & Catalano RF (2010). Romantic Relationships and Substance Use in Early Adulthood. Journal of Health and Social Behavior, 51(2), 153–67. 10.1177/0022146510368930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk JL, & Rogge RD (2007). Testing the ruler with item response theory: Increasing precision of measurement for relationship satisfaction with the Couples Satisfaction Index. Journal of Family Psychology, 21(4), 572–583. 10.1037/0893-3200.2L4.572 [DOI] [PubMed] [Google Scholar]
- Ginsberg D, Hall SM, & Rosinski M (1991). Partner interaction and smoking cessation: A pilot study. Addictive Behaviors, 16(5), 195–202. 10.1016/0306-4603(91)90012-7 [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, & Fagerstrom K-O (1991). The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Addiction, 86(9), 1119–1127. 10.1111/j.1360-0443.1991.tb01879.x [DOI] [PubMed] [Google Scholar]
- Heinz AJ, Wu J, Witkiewitz K, Epstein DH, & Preston KL (2009). Marriage and relationship closeness as predictors of cocaine and heroin use. Addictive Behaviors, 34(3), 258–263. https://doi.org/10.1016ZJ.ADDBEH.2008.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holahan CJ, North RJ, Holahan CK, Hayes RB, Powers DA, & Ockene JK (2012). Social influences on smoking in middle-aged and older women. Psychology of Addictive Behaviors, 26(3), 519–526. 10.1037/a0025843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homish GG, & Leonard KE (2005). Spousal influence on smoking behaviors in a US community sample of newly married couples. Social Science & Medicine, 61(12), 2557–2567. 10.1016/J.SOCSCIMED.2005.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Gulliver SB, Fenwick JW, Valliere WA, Cruser K, Pepper S, & …Flynn BS. (1992). Smoking cessation among self-quitters. Health Psychology, 11(5), 331–334. 10.1037/0278-6133.1L5.331 [DOI] [PubMed] [Google Scholar]
- Jackson SE, Steptoe A, & Wardle J (2015). The Influence of Partner’s Behavior on Health Behavior Change. JAMA Internal Medicine, 175(3), 385 10.1001/jamainternmed.2014.7554 [DOI] [PubMed] [Google Scholar]
- Jones R (2013). RUNMPLUS: Stata module to run Mplus from Stata . Statistical Software Components. Retrieved from https://ideas.repec.org/c/boc/bocode/s457154.html [Google Scholar]
- Kurdek LA (2003). Differences between Gay and Lesbian Cohabiting Couples. Journal of Social and Personal Relationships, 20(4), 411–436. 10.1177/02654075030204001 [DOI] [Google Scholar]
- Kurdek LA (2004). Are Gay and Lesbian cohabiting couples really different from heterosexual married couples? Journal of Marriage and Family, 66(4), 880–900. 10.1111/j.0022-2445.2004.00060.x [DOI] [Google Scholar]
- Lakey B, & Cassady PB (1990). Cognitive processes in perceived social support. Journal of Personality and Social Psychology, 59(2), 337–343. 10.1037/0022-3514.59.2.337 [DOI] [Google Scholar]
- Lakey B, & Orehek E (2011). Relational regulation theory: A new approach to explain the link between perceived social support and mental health. Psychological Review, 118(3), 482–495. 10.1037/a0023477 [DOI] [PubMed] [Google Scholar]
- Lawhon D, Humfleet GL, Hall SM, Reus VI, & Muñoz RF (2009). Longitudinal analysis of abstinence-specific social support and smoking cessation. Health Psychology, 28(4), 465–472. 10.1037/a0015206 [DOI] [PubMed] [Google Scholar]
- Lemay EP, Clark MS, & Feeney BC (2007). Projection of responsiveness to needs and the construction of satisfying communal relationships. Journal of Personality and Social Psychology, 92(5), 834–853. 10.1037/0022-3514.92.5.834 [DOI] [PubMed] [Google Scholar]
- Leonard KE, & Homish GG (2008). Predictors of heavy drinking and drinking problems over the first 4 years of marriage. Psychology of Addictive Behaviors, 22(1), 25–35. 10.1037/0893-164X.22.L25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, McBride CM, Pollak KI, Puleo E, Butterfield RM, & Emmons KM (2006). Understanding health behavior change among couples: An interdependence and communal coping approach. Social Science & Medicine, 62(6), 1369–1380. 10.1016/LS0CSCIMED.2005.08.006 [DOI] [PubMed] [Google Scholar]
- Luscher J, Stadler G, & Scholz U (2017). A Daily Diary Study of Joint Quit Attempts by Dual-Smoker Couples: The Role of Received and Provided Social Support. Nicotine & Tobacco Research, 20(1), 100–107. 10.1093/ntr/ntx079 [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. (2008). Introduction to Statistical Mediation Analysis. New York: Lawrence Erlbaum Associates; 10.4324/9780203809556 [DOI] [Google Scholar]
- May S, & West R (2000). Do social support interventions ("buddy systems") aid smoking cessation? A review. Tobacco Control, 9(4), 415–422. 10.1136/TC.9A415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride CM, Curry SJ, Grothaus LC, Nelson JC, Lando H, & Pirie PL (1998). Partner smoking status and pregnant smoker’s perceptions of support for and likelihood of smoking cessation. Health Psychology, 17(1), 63–69. 10.1037/0278-6133.17.1.63 [DOI] [PubMed] [Google Scholar]
- McCollum EE, Nelson TS, Lewis RA, & Trepper TS (2005). Partner Relationship Quality and Drug Use as Predictors of Women’s Substance Abuse Treatment Outcome. The American Journal of Drug and Alcohol Abuse, 31(1), 111–127. 10.1081/ADA-47906 [DOI] [PubMed] [Google Scholar]
- Mermelstein R, Lichtenstein E, & McIntyre K (1983). Partner support and relapse in smoking-cessation programs. Journal of Consulting and Clinical Psychology, 51(3), 465–466. 10.1037/0022-006X.5L3.465 [DOI] [PubMed] [Google Scholar]
- Muthen LK (2007). Mplus: Statistical Analysis with Latent Variables (Version 4.21) [Computer software. Retrieved from http://citeseerx.ist.psu.edu/viewdoc/summary?doi=10.1.1.310.2841
- Murray SL, Holmes JG, & Griffin DW (2000). Self-esteem and the quest for felt security: How perceived regard regulates attachment processes. Journal of Personality and Social Psychology, 78, 478–498. doi: 10.1037/0022-3514.78.3.478 [DOI] [PubMed] [Google Scholar]
- Park E-W, Tudiver F, Schultz JK, & Campbell T (2004). Does enhancing partner support and interaction improve smoking cessation? A meta-analysis. Annals of Family Medicine, 2(2), 170–174. 10.1370/AFM.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollak KI, Baucom DH, Peterson BL, Stanton S, & McBride CM (2006). Rated helpfulness and partner-reported smoking cessation support across the pregnancy-postpartum continuum. Health Psychology, 25(6), 762–770. 10.1037/0278-6133.25.6.762 [DOI] [PubMed] [Google Scholar]
- Pollak KI, & Mullen PD (1997). An exploration of the effects of partner smoking, type of social support, and stress on postpartum smoking in married women who stopped smoking during pregnancy. Psychology of Addictive Behaviors, 11(3), 182–189. 10.1037/0893-164X.11.3.182 [DOI] [Google Scholar]
- Prochaska JO, & Velicer WF (1997). The Transtheoretical Model of Health Behavior Change. American Journal of Health Promotion, 12(1), 38–48. 10.4278/0890-1171-12.L38 [DOI] [PubMed] [Google Scholar]
- Reis HT, & Shaver PR (1988). Intimacy as an interpersonal process In Duck S, Hay DF, Hobfoll SE, Ickes W, & Montgomery BM (Eds.), Handbook of Personal Relationships: Theory, Research and Interventions. (pp. 367–389). Oxford England: John Wiley & Sons. [Google Scholar]
- Reis HT, & Clark MS (2013). Responsiveness In Simpson JA & Campbell L (Eds.), The Oxford Handbook of Close Relationships (pp. 400–423). New York: Oxford University Press. [Google Scholar]
- Schaefer MT, & Olson DH (1981). Assessing Intimacy: The Pair Inventory. Journal of Marital and Family Therapy, 7(1), 47–60. https://doi.org/10.1111Xj.1752-0606.1981.tb01351.x [Google Scholar]
- Scholz U, Stadler G, Ochsner S, Rackow P, Hornung R, & Knoll N (2016). Examining the relationship between daily changes in support and smoking around a self-set quit date. Health Psychology, 35(5), 514–517. 10.1037/hea0000286 [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, & Hufford MR (2008). Ecological Momentary Assessment. Annual Review of Clinical Psychology, 4(1), 1–32. 10.1146/annurev.clinpsy.3.022806.091415 [DOI] [PubMed] [Google Scholar]
- Shiffman S (2009). How many cigarettes did you smoke? Asssessing cigarette consumption by global report, time-line follow-back, and ecological momentary assessment. Health Psychology, 28(5) 519–526. 10.1037/a0015197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. (2013). Stata Statistical Software. College Station, TX: StataCorp LP. [Google Scholar]
- Stroebe W, & Stroebe M (1996). The social psychology of social support In Social psychology: Handbook of basic principles. (pp. 597–621). New York, NY, US: Guilford Press. [Google Scholar]
- Testa M, Wang W, Derrick JL, & Leonard KE (in press). Marijuana use by intimate partners: Does discrepant use impair relationship functioning? Psychology of Addictive Behaviors. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Väänänen A, Kouvonen A, Kivimäki M, Pentti J, & Vahtera J (2008). Social Support, Network Heterogeneity, and Smoking Behavior in Women: The 10-Town Study. American Journal of Health Promotion, 22(4), 246–255. 10.4278/0701094RL1 [DOI] [PubMed] [Google Scholar]
- vanDellen MR, Boyd SM, Ranby KW, MacKillop J, & Lipkus IM (2016). Willingness to provide support for a quit attempt: A study of partners of smokers. Journal of Health Psychology, 21(9), 1840–1849. 10.1177/1359105314567209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velicer WF, & Prochaska JO (2004). A comparison of four self-report smoking cessation outcome measures. Addictive Behaviors, 29, 51–60. 10.1016/S0306-4603(03)00084-4. [DOI] [PubMed] [Google Scholar]
- Wagner J, Burg M, & Sirois B (2004). Social support and the transtheoretical model: Relationship of social support to smoking cessation stage, decisional balance, process use, and temptation. Addictive Behaviors, 29(5), 1039–1043. 10.1016/J.ADDBEH.2004.02.058 [DOI] [PubMed] [Google Scholar]
- West R, Hajek P, Stead L, & Stapleton J (2005). Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction, 100(3), 299–303. 10.1111/j.1360-0443.2004.00995.x [DOI] [PubMed] [Google Scholar]
- Westmaas JL, Bontemps-Jones J, & Bauer JE (2010). Social support in smoking cessation: Reconciling theory and evidence. Nicotine & Tobacco Research, 12(7), 695–707. 10.1093/ntr/ntq077 [DOI] [PubMed] [Google Scholar]
- Whisman MA, Uebelacker LA, & Bruce ML (2006). Longitudinal association between marital dissatisfaction and alcohol use disorders in a community sample. Journal of Family Psychology, 20(1), 164–167. 10.1037/0893-3200.20.1.164 [DOI] [PubMed] [Google Scholar]