Abstract
Background
Helping young people to avoid starting smoking is a widely endorsed public health goal, and schools provide a route to communicate with nearly all young people. School‐based interventions have been delivered for close to 40 years.
Objectives
The primary aim of this review was to determine whether school smoking interventions prevent youth from starting smoking. Our secondary objective was to determine which interventions were most effective. This included evaluating the effects of theoretical approaches; additional booster sessions; programme deliverers; gender effects; and multifocal interventions versus those focused solely on smoking.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), the Cochrane Tobacco Addiction Group's Specialised Register, MEDLINE, EMBASE, PsyclNFO, ERIC, CINAHL, Health Star, and Dissertation Abstracts for terms relating to school‐based smoking cessation programmes. In addition, we screened the bibliographies of articles and ran individual MEDLINE searches for 133 authors who had undertaken randomised controlled trials in this area. The most recent searches were conducted in October 2012.
Selection criteria
We selected randomised controlled trials (RCTs) where students, classes, schools, or school districts were randomised to intervention arm(s) versus a control group, and followed for at least six months. Participants had to be youth (aged 5 to 18). Interventions could be any curricula used in a school setting to deter tobacco use, and outcome measures could be never smoking, frequency of smoking, number of cigarettes smoked, or smoking indices.
Data collection and analysis
Two reviewers independently assessed studies for inclusion, extracted data and assessed risk of bias. Based on the type of outcome, we placed studies into three groups for analysis: Pure Prevention cohorts (Group 1), Change in Smoking Behaviour over time (Group 2) and Point Prevalence of Smoking (Group 3).
Main results
One hundred and thirty‐four studies involving 428,293 participants met the inclusion criteria. Some studies provided data for more than one group.
Pure Prevention cohorts (Group 1) included 49 studies (N = 142,447). Pooled results at follow‐up at one year or less found no overall effect of intervention curricula versus control (odds ratio (OR) 0.94, 95% confidence interval (CI) 0.85 to 1.05). In a subgroup analysis, the combined social competence and social influences curricula (six RCTs) showed a statistically significant effect in preventing the onset of smoking (OR 0.49, 95% CI 0.28 to 0.87; seven arms); whereas significant effects were not detected in programmes involving information only (OR 0.12, 95% CI 0.00 to 14.87; one study), social influences only (OR 1.00, 95% CI 0.88 to 1.13; 25 studies), or multimodal interventions (OR 0.89, 95% CI 0.73 to 1.08; five studies). In contrast, pooled results at longest follow‐up showed an overall significant effect favouring the intervention (OR 0.88, 95% CI 0.82 to 0.96). Subgroup analyses detected significant effects in programmes with social competence curricula (OR 0.52, 95% CI 0.30 to 0.88), and the combined social competence and social influences curricula (OR 0.50, 95% CI 0.28 to 0.87), but not in those programmes with information only, social influence only, and multimodal programmes.
Change in Smoking Behaviour over time (Group 2) included 15 studies (N = 45,555). At one year or less there was a small but statistically significant effect favouring controls (standardised mean difference (SMD) 0.04, 95% CI 0.02 to 0.06). For follow‐up longer than one year there was a statistically nonsignificant effect (SMD 0.02, 95% CI ‐0.00 to 0.02).
Twenty‐five studies reported data on the Point Prevalence of Smoking (Group 3), though heterogeneity in this group was too high for data to be pooled.
We were unable to analyse data for 49 studies (N = 152,544).
Subgroup analyses (Pure Prevention cohorts only) demonstrated that at longest follow‐up for all curricula combined, there was a significant effect favouring adult presenters (OR 0.88, 95% CI 0.81 to 0.96). There were no differences between tobacco‐only and multifocal interventions. For curricula with booster sessions there was a significant effect only for combined social competence and social influences interventions with follow‐up of one year or less (OR 0.50, 95% CI 0.26 to 0.96) and at longest follow‐up (OR 0.51, 95% CI 0.27 to 0.96). Limited data on gender differences suggested no overall effect, although one study found an effect of multimodal intervention at one year for male students. Sensitivity analyses for Pure Prevention cohorts and Change in Smoking Behaviour over time outcomes suggested that neither selection nor attrition bias affected the results.
Authors' conclusions
Pure Prevention cohorts showed a significant effect at longest follow‐up, with an average 12% reduction in starting smoking compared to the control groups. However, no overall effect was detected at one year or less. The combined social competence and social influences interventions showed a significant effect at one year and at longest follow‐up. Studies that deployed a social influences programme showed no overall effect at any time point; multimodal interventions and those with an information‐only approach were similarly ineffective.
Studies reporting Change in Smoking Behaviour over time did not show an overall effect, but at an intervention level there were positive findings for social competence and combined social competence and social influences interventions.
Keywords: Adolescent; Child; Child, Preschool; Humans; Program Evaluation; Smoking Prevention; Health Promotion; Randomized Controlled Trials as Topic; School Health Services; School Health Services/standards; Schools
Plain language summary
Can programmes delivered in school prevent young people from starting to smoke?
Increasing numbers of young people are smoking in developing and poorer countries. Programmes to prevent them starting to smoke have been delivered in schools over the past 40 years. We wanted to find out if they are effective.
We identified 49 randomised controlled trials (over 140,000 school children) of interventions aiming to prevent children who had never smoked from becoming smokers. At longer than one year, there was a significant effect of the interventions in preventing young people from starting smoking. Programmes that used a social competence approach and those that combined a social competence with a social influence approach were found to be more effective than other programmes. However, at one year or less there was no overall effect, except for programmes which taught young people to be socially competent and to resist social influences.
A smaller group of trials reported on the smoking status of all people in the class, whether or not they smoked at the start of the study. In these trials with follow‐up of one year or less there was an overall small but significant effect favouring the controls. This continued after a year; for trials with follow‐up longer than one year, those in the intervention groups smoked more than those in the control groups.
When trials at low risk of bias from randomisation, or from losing participants, were examined separately, the conclusions remained the same. Programmes led by adults may be more effective than those led by young people. There is no evidence that delivering extra sessions makes the intervention more effective.
Background
Children and adolescents in all cultures smoke, with increasing rates in many developing countries. Starting smoking usually leads to the behaviour lasting decades, with great difficulty in quitting. Few studies verify smoking by biochemical tests, and self reported rates probably underestimate true rates. Smoking uptake is associated with existing smoking by family and friends, and with risk‐taking behaviours. Researchers have implemented programmes to counteract these influences. Programmes in schools have evolved over four decades and include those providing information about smoking rates and harms from smoking; teaching children how to be more socially competent to avoid starting smoking; teaching skills to refuse offered tobacco and multimodal programmes with parents, teachers, and the community.
The incidence and prevalence of smoking among children and adolescents
Tobacco use is the main preventable cause of death and disease worldwide, and the five million deaths annually attributable to tobacco use are predicted to increase to eight million annually by 2030 (Warren 2009). Of the US population who were 17 or younger in 1995, it was estimated that five million would die prematurely of tobacco‐related causes, and that 20% of deaths could be avoided if smokers had either never started or had quit (Epstein 2000b).
The World Health Organization (WHO) 'Health behaviour in school‐aged children 1997‐8' survey of 11, 13 and 15 year olds in 29 countries (Europe, Canada and the USA) found that for the 15 year olds in 14 countries more than 20% of females, and in 11 countries more than 20% of males smoked daily (WHO 2000). Surveys of the smoking behaviour of 13 to 15 year olds were then conducted between 1998 and 2008 in all six WHO world regions with 100 initial, 100 second and nine third surveys involving 530,849 students. In 191 of the 209 surveys, more than 90% of the schools participated, and in 190 of 209 surveys, student participation was greater than 80%. The prevalence of both cigarette smoking and other forms of smoking such as water pipes, were both defined as at least monthly (Warren 2009).
For the 100 sites with follow‐up surveys, there were increases in the prevalence of smoking cigarettes at least one day per month at 27 sites and decreases at 10, and for other tobacco products (such as water pipes) at least one day per month there were increases at 33 sites and decreases at 13 (Warren 2009). Therefore, if poorer countries follow the trajectory of the more affluent countries, it is to be expected that 20% to 30% of 13 to 15 year olds may smoke, depending on the culture of the country and the activities of the tobacco companies.
Adolescent smoking remains a risk factor in adulthood. The 1995 US National College Health Risk Behavior Survey found that 70% had ever tried smoking a cigarette, and of these 42% were current smokers and 13% current daily smokers. Females were more likely to smoke than males (Pletcher 2000). Adolescents who begin smoking at younger ages are more likely to become regular smokers and less likely to quit (Tyas 1998). Of concern is the finding that the first use of tobacco after age 18 in the USA increased from 25% to 40% between 2002 and 2009 (SAMHSA 2009).
Villanti 2010 identified five types of smoking behaviour as adolescents become young adults: nonsmokers, early stable smokers, late starters, quitters, and 'light or intermittent smokers'. In adulthood, the early stable and late starter groups had the highest rates of smoking, but the light or intermittent smokers could go either way, and after two years had either temporarily quit or had become heavy smokers.
School‐based interventions
Over the past three decades the school environment has been a particular focus of efforts to influence youth smoking behaviour. The main perceived advantages are that almost all children can be reached through schools, and a focus on education fits naturally with the daily activities of schools. Researchers have used five types of interventions in schools, each based on a different theoretical orientation:
1. Information only curricula
Interventions that provide information to oppose tobacco use (also called normative education) are described by Griffin 2010 as "content and activities to correct inaccurate perceptions regarding the high prevalence of substance use." Griffin describes how many adolescents overestimate smoking prevalence and view smoking as normative behaviour. Normative curricula seek to inform students on actual rates of use and undermine inaccurate beliefs on the social acceptability of smoking. Normative materials are often used by programme deliverers in social resistance programmes. The assumption is that information alone will lead to changes in behaviour (Bangert‐Drowns 1988).
2. Social competence curricula
A group of interventions that aim to help adolescents refuse offers to smoke by improving their general social competence. Griffin 2010 recognises that poor personal and social skills can lead to development of drug use. Therefore, programmes benefit from including social learning processes or life skills such as problem‐solving and decision‐making, cognitive skills for resisting interpersonal or media influences, increased self control and self esteem, coping strategies for stress, and general social and assertive skills. These skills will also have broader applications for the students. The interventions are based on Bandura's social learning theory (Bandura 1977), which hypothesises that children learn drug use by modelling, imitation, and reinforcement, influenced by the child's pro‐drug cognitions, attitudes and skills. Susceptibility is increased by poor personal and social skills and a poor personal self concept (Botvin 2000).
3. Social influence curricula
Interventions that aim to overcome social influences promoting tobacco use by providing skills to adolescents (also called social skills interventions). Griffin 2010 describes these interventions as aiming to increase the "adolescents’ awareness of the various social influences that support substance use." Programmes adopt resistance skills training in which students are taught how to deal with peer pressure, high risk situations, how to effectively refuse attempts to persuade substance use from both direct and indirect sources. The interventions are based on McGuire's persuasive communications theory and Evans's theory of psychological inoculation (McGuire 1968; Evans 1976).
4. Combined social competence and social influences curricula
Methods that draw on both social competence and social influence approaches.
5. Multimodal programmes
These programmes combine curricular approaches with wider initiatives within and beyond the school, including programmes for parents, schools, or communities and initiatives to change school policies about tobacco, or state policies about the taxation, sale, availability and use of tobacco.
Why it is important to do this review
Tobacco education curricula are widely used in US schools, though few of those in use have been rigorously evaluated. The US 2000 National Youth Tobacco Survey national sample of 35,828 6th‐ to12th‐graders in 324 schools found that 70% of the middle schoolers and 50% of the high schoolers said they had received a programme that taught them the short‐term consequences of tobacco use. The percentages for receiving a normative programme were 40% and 18%; for programmes teaching why people smoke 64% and 38%; for programmes teaching refusal skills 51% and 17%; and for multi‐strategy programmes 38% and 17% (Wenter 2002). Wiehe 2005 identified eight programmes that followed participants to age 18 or the 12th grade and found little or no evidence of effectiveness. There is nevertheless continued uncertainty about both the relative and absolute effectiveness of school‐based programmes, and considerable variation in the extent to which they are implemented in other countries.
This review is important because there is no other systematic review of world literature on school‐based smoking prevention programmes without language or date restrictions. This review was first published in 2002. This update has refined how the included studies are categorised to provide analysis based on Pure Prevention cohort studies, Change in Smoking Behaviour over time studies and Point Prevalence of Smoking studies.
Objectives
The primary objective of this review is to assess the effectiveness of school‐based programmes in preventing children and adolescents from starting smoking. A secondary objective is to assess which programme elements, if any, are associated with effectiveness.
We considered one central question:
Are school programmes, categorised by intervention type, more effective than minimal or no intervention in preventing smoking? We considered the hypothesis that they are more effective separately according to the theoretical orientation of the prevention programme:
Information giving
Social competence
Social influence
Combined social influence and social competence
Multimodal programmes
If the review showed the effectiveness of one or more of these types of intervention, we proceeded to the secondary objective, i.e. to examine the direct evidence comparing different types of intervention, categorised by theoretical orientation, including:
Social influences versus information giving
Social influences versus social competence
Combinations of social influences, social competence and information versus single component interventions
Multimodal programmes versus single component interventions
We also aimed to consider the effect by gender and the method of programme delivery, including:
Peer‐led programmes versus those taught by researchers or teachers
Booster sessions after programme completion versus no booster
Tobacco‐focused interventions versus interventions focused on tobacco together with other substances such as alcohol and drugs
Methods
Criteria for considering studies for this review
Types of studies
We included studies in which individual students, classes, schools, or school districts were randomised to receive different programmes or to be the control, and in which baseline tobacco use was measured. We excluded studies if they did not state that allocation of individuals or groups to intervention and control groups was randomised. Random allocation of intervention was either to the individual or to individuals in clusters (in classes, in schools, in classes nested within schools, or in school districts). We assessed whether the studies were analysed using methods appropriate to the level of allocation and the level of measurement of the outcomes. No studies were excluded on the basis of publication status or language of publication.
Types of participants
Children (aged 5 to 12) and adolescents (aged 13 to 18) in school settings. We also included studies in which the participants were 5 to 18 during the intervention phase of the study, but were followed up in a few instances beyond 18.
Types of interventions
We included all school‐based programmes that had as one of their goals preventing tobacco use, irrespective of theoretical intervention. Some programmes aimed simply to provide information about tobacco. Others had more complex goals: teaching generic social skills to reinforce societal norms about individual behaviour; reinforcing the adolescent's self concept; and teaching social skills and specific tobacco refusal skills. Some focused on multiple addictions, and we included any programmes with any drug or alcohol focus provided outcomes for tobacco use were reported. Some focused on 'healthy schools.' We included these provided outcomes for tobacco use were reported. We classified programmes according to their dominant theoretical orientation and then allocated them to one of the five categories described in the Background section or to a sixth category, 'other'. Programmes that solely provided information were placed in the information only category, while recognising that all curricula provided information to participants.
For each study we determined whether the intervention programmes were compared with a control group, and whether the control group received no intervention, or the standard health education curriculum taught in the school, or the tobacco education curriculum in normal use in the school.
There were no restrictions on who delivered the intervention. These could include researchers, classroom teachers, health science teachers, healthcare professionals, undergraduate or graduate students, adolescent peers, or other personnel.
Types of outcome measures
The primary outcome was the effect of the intervention on the smoking status of individuals or cohorts who reported no use of tobacco at baseline. We recorded whether effects of the interventions were found at the conclusion of the programme, and whether such effects were sustained at follow‐up after completion of the programme. We required a minimum follow‐up of six months after the intervention.
We did not require biochemical validation (by saliva thiocyanate or cotinine or expired air carbon monoxide levels) of self reported tobacco use for inclusion, but recorded its use. If saliva samples were collected but not analysed (sometimes described as the 'bogus pipeline' procedure), this was recorded.
One problem in this field is that the studies often use different measures of tobacco use, either recording frequency (monthly, weekly, daily), or the number of cigarettes smoked, or an index constructed from multiple measures. Sometimes the variety of measures is intended to record the fact that young children begin smoking on a monthly basis, but as they get older may proceed to weekly and daily smoking. We excluded studies which did not report any measure of smoking behaviour, studies that did not assess baseline smoking status in the pre‐test survey, and studies that reported only changes in knowledge or attitudes about smoking.
Search methods for identification of studies
We searched the following databases using search strategies similar to those used in MEDLINE for each. Detailed search strategies are displayed in Appendix 1 (MEDLINE) and Appendix 2 (CINAHL):
MEDLINE 1966 ‐ 10/2012
EMBASE 1974 ‐ 10/2012
CINAHL ‐ 10/2012
PsycINFO 1967 ‐ 10/2005
ERIC 1982 ‐ 10/2005
Health Star
Tobacco Control 1992 ‐ 2005
Journal of Smoking Related Disorders 1990 ‐ 2005
Dissertation Abstracts 1960 ‐ [Search strategy = (Tobacco or smoking) and prevent? and (child or adolescent)]
US Department of Health Reviews
Proceedings of the World Conferences on Tobacco and Health
Cochrane Tobacco Addiction Review Group Specialised Register 10/2012
Reference lists of the articles selected in the above sources
Index of Scientific and Technical Proceedings
Conference Papers Index
In addition, we searched MEDLINE from 1966 to October 2012 for 133 individual authors who had published in the field. We also screened the reference lists of the included studies. None of the previous meta‐analyses of the literature (listed in the additional references below) undertook a Cochrane search strategy. The most recent searches were conducted in October 2012.
Data collection and analysis
Selection of studies
Two authors (RET and JM) independently assessed the search results for studies that met the inclusion criteria. Reference lists were checked for further relevant studies. The full text of each study was independently assessed, and the authors contacted for clarification in cases of uncertainty.
Data extraction and management
Two authors (RET and JM) independently extracted data, with disagreements resolved by recourse to co‐author RP. We categorised studies into six groups corresponding to the type of intervention (information; social competence; social influence; combined social competence and social influence; multi‐modal, and other). Information extracted included country of study, intervention focus, description of participants (numbers of participants, classes and schools, age, gender, ethnicity, existing smoking status), description of intervention (duration, nature, deliverer, outcome, follow‐up), quality of delivery, and statistical methods.
Assessment of risk of bias in included studies
Two authors independently assessed five aspects of risk of bias, with adjudication in case of disagreement by a third author. Each potential risk of bias was assessed to be either at low or at unclear risk (if no data were provided which could be judged to assess bias), or at high risk (study design or execution could cause over‐ or underestimation of the intervention effect). We contacted authors to verify any risk of bias information not presented in their publications.
Sequence generation (selection bias)
Allocation concealment (selection bias)
Blinding of outcome assessment (detection bias), which was assessed as unclear unless a specific reference was made to blinding of outcome assessors.
Incomplete outcome data (attrition bias) due to absence of some data for individuals or loss of all data for an individual after a certain time. We examined studies for systematic differences in the rate of loss to follow‐up among different groups. Where there was differential attrition between groups, we considered bias was more likely if there was no sensitivity analysis of the effect of this attrition on outcomes.
Selective reporting (reporting bias) due to authors either (1) not reporting all outcomes as determined by the objectives stated initially in their study protocol, or previous publications about the study or within the current publication, or (2) reporting only a subset of outcomes with significant results.
Data synthesis
We identified three groups of studies:
Pure Prevention cohorts (Group 1): Cohorts in which never‐smokers at baseline were followed and the number remaining never‐smokers at the various follow‐up intervals was ascertained. Where authors did not report these data we either computed them from the published articles or we contacted authors and requested that they compute these data. We obtained absolute numbers or odds ratios from individual randomised trials with the control group as comparator. Where the authors used a denominator which did not include all the participants originally randomised (e.g. a sample which the author described as the 'analysis sample,' which excluded drop‐outs and thus had smaller numbers at follow‐up), we recomputed the data using the numbers originally randomised. We calculated adjusted odds ratios based on the number of never‐smokers at specific time points. Adjustment was made for clustering by school/group based on either reported or estimated intraclass correlation coefficients (ICCs) and cluster sizes to determine design effects for each of the intervention groups. We then used this design effect to determine the effective sample size for each intervention group. We obtained a pooled estimate of the effect using the generalised inverse variance method and a fixed‐effect model. We conducted subanalyses for Group 1 based on gender, peer‐led (or substantially peer‐led) versus adult‐led studies, tobacco as the sole focus of the intervention versus multifocal interventions, and interventions that had subsequent booster sessions versus those with none.
Change in Smoking Behaviour over time (Group 2): Studies where the smoking behaviour was measured as change over time. These studies included those with growth curve analysis. We extracted summary measures for the change in smoking status/use from each study in this group. These were reported either for each study group (mean change or ß‐coefficient of change over time plus their associated standard error by study arm) or as an overall change measure attributed to the intervention (odds ratio (OR) with 95% confidence interval (CI), ß‐coefficients of linear change and associated standard error; one per study comparison). When overall effects were reported as ORs and 95% CI we transformed these into standard mean difference (SMD) by multiplying by √3/∏ = 0.5513 as recommended in the Cochrane Handbook (9.4.6 Combining dichotomous and continuous outcomes).
Point Prevalence of Smoking (Group 3): Studies reporting smoking prevalence at baseline and follow‐ups. Individuals were not followed individually to the follow‐up points, and thus the prevalence rates at baseline and follow‐up are cross‐sectional data. Measures included mean usage (indices and ever‐use), percentage in the past week, past month, lifetime usage, percentage smoker and percentage never‐ or nonsmoker. We calculated a summary measure by comparing the difference in smoking prevalence from baseline to follow‐up between the two arms. We obtained the standard error by estimating the correlation of smoking status from data available from a small selection of Group 1 studies, and using the total number of clusters as a proxy for sample size in each group.
For both Change in Smoking Behaviour over time (Group 2) and Point Prevalence of Smoking (Group 3) studies:
We extracted the most conservative smoking outcome, i.e. the lowest usage of smoking (ever‐smoked, and if not available then monthly smoking).
We contacted all authors (after 1995), asking them to identify a cohort of baseline never‐smokers, which would allow the study to be included in the Pure Prevention cohorts (Group 1)
We obtained a pooled estimate of the effects using the generalised inverse variance method and a standardised mean difference.
If a study provided data that were applicable to more than one group of studies, then the data were accepted for both groups. Data from all three groups were not pooled, but were analysed separately throughout the review.
The three groups (Pure Prevention cohort, Change in Smoking Behaviour over time, Point Prevalence of Smoking) were each analysed as an entire group, and then by the intervention used (information; social competence; social influences; combined social competence and social influences; multimodal; other interventions). Studies in the 'other interventions' group were sufficiently different from each other that, although they were presented within the meta‐analysis for the entire group, it would not be appropriate to combine them as a subgroup by intervention within the Results and Discussion sections.
For all groups, study results were analysed by outcomes of one year or less, and then by longest available follow‐up point. The raw data are tabulated in Appendix 3; Appendix 4; Appendix 5.
Where a study compared more than one intervention arm the control group was split equally between them for both outcome events and sample size. The additional intervention arms within the study were added to the review with a text link to the first.
All RCTs were cluster‐randomised trials (C‐RCTs), except for one trial (Werch 2005), and calculations to allow for the effects of clustering using intraclass correlation coefficients (ICCs) were either made by the study authors or were applied by the review authors.
All studies included in the review were assessed and placed into one of the three analysis groups above (Pure Prevention cohorts, Change in Smoking Behaviour over time, and Point Prevalence of Smoking). Studies were included in the review but excluded from the analysis if, once allocated to one of the three analysis groups, it was established that data were missing from studies, such as no baseline and follow‐up numbers, no control arm data, or the review authors were unable to reconcile the data. In these instances we contacted the study author. If there was no response or data were no longer available for these studies then it was not possible to include the studies in the analysis. In some instances if data were available, but only the total number of schools or classes was known and not the numbers allocated to each arm, then the number of schools or classes was estimated based on the proportion of individuals within the group.
Results are presented as: descriptive text, tables and forest plots (pooled data).
Subgroup analysis and investigation of heterogeneity
We used the I² statistics to assess inconsistency across studies and provide a measure of heterogeneity (Higgins 2003). Thresholds for interpretation of heterogeneity were adopted as outlined in the Cochrane Handbook : 0% to 40% ‐ low, 30% to 60% ‐ moderate, 50% to 90% ‐ possible substantial, 75% to 100% ‐ considerable heterogeneity. Where the heterogeneity was deemed to be considerable we did not pool the results and provided a narrative assessment instead.
We conducted subgroup analyses by theoretical approach in all three groups (Pure Prevention cohorts, Change in Smoking Behaviour over time, and Point Prevalence of Smoking). We completed further subgroup analyses on Pure Prevention cohorts only (Group 1). This group was selected for additional subgroup analyses because these studies followed individual baseline never‐smokers through to follow‐up, and were expected to provide both the clearest indication of intervention effects and to have the lowest heterogeneity between studies. These analyses examined differences by gender, peer‐led versus adult‐led interventions, interventions focusing solely on tobacco versus interventions covering multiple areas, and the effects of adding booster sessions.
Sensitivity analysis
We conducted sensitivity analyses for all groups, to compare the overall study results against those studies with low or unclear risk of bias from attrition. We also viewed only those studies at low risk of bias from sequence generation, to assess whether the quality of randomisation had any impact on the overall results. We did not conduct sensitivity analyses for selective reporting, since all studies were assessed to be at low risk of bias, except for five studies which were rated as being at unclear risk and were not included in any analysis because of lack of data.
Results
Description of studies
Full details of all the trials are given in the Characteristics of included studies, Characteristics of excluded studies, and Characteristics of ongoing studies tables. Each study is identified by the name of the first author and year of publication of the main results paper. Additional references are listed together with this main publication under the study ID.
Included studies
The Characteristics of included studies table provides detail on each of the included studies. Overall, 133 cluster‐randomised controlled trials (C‐RCTs) and one RCT, giving a total of 200 arms and involving 428,293 participants from 25 different countries were included and placed in three groups (Note: ‘arms’ refers to different intervention groups within the RCTs, see Figure 1 and Appendix 6):
1.

Flow chart of retrieval and identification of Group 1, 2 and 3 studies.
Pure Prevention cohorts (Group 1): This group included 56 trials with 184,467 participants. Of these, 49 trials (73 arms) with 142,447 participants from 19 different countries provided analysable data. Twenty‐six were from the USA, four each from the Netherlands and the UK, three each from Canada, Germany and Italy, two each from China and Spain, and one each from Austria, Australia, Belgium, Czech Republic, Denmark, Finland, Greece, Portugal, South Africa, Sweden and Thailand. (N.B. Faggiano 2008 provided the comprehensive write‐up of results for a study set in Austria, Belgium, Germany, Greece, Italy, Spain and Sweden). See Appendix 7 for a list of Group 1 studies by country.
Change in Smoking Behaviour over time (Group 2): Studies which provided change data. This included 16 trials with 57,577 participants, of which 15 trials (27 arms) with 45,555 participants provided analysable data. These studies came from three countries: 12 from the USA, two from India, one from Canada. See Appendix 8 for a list of studies by country.
Point Prevalence of Smoking (Group 3): Studies which provided point prevalence data. This included one RCT and 65 C‐RCTs with 208,518 participants, of which one RCT and 24 C‐RCTs (39 arms) with 110,016 participants from 11 different countries provided usable data. Twelve were from the USA, two each from Australia, the Netherlands and the UK, and one each from France, Germany, India, Mexico, Norway, Romania and Sweden. See Appendix 9 for a list of studies by country. The only three studies (four arms) with intention‐to‐treat analysis are also in this group (McCambridge 2011; Sloboda 2009; Spoth 2002 (LST); Spoth 2002 (LST + SFP)).
Four studies (six arms) provided data to more than one group: Spoth 2001 (ISFP); Spoth 2001 (PDFY) to Pure Prevention cohorts (Group 1) and Change in Smoking Behaviour over time (Group 2), Ringwalt 2009a and Spoth 2002 (LST); Spoth 2002 (LST + SFP) to Pure Prevention cohorts (Group 1) and Point Prevalence of Smoking (Group 3), and Perry 2009 to Change in Smoking Behaviour over time (Group 2) and Point Prevalence of Smoking (Group 3). This is reflected in the total participant numbers and total trial numbers stated being reduced to take account of their multiple contributions.
Forty‐nine studies with 152,544 participants were not analysable for a variety of reasons: (1) the publications did not provide data or only incomplete data on smoking status in the intervention and control groups at either baseline or follow‐ups; (2) Numbers for intervention and control groups were not provided; (3) the data were in an unusable format; (4) the data were judged to be unreliable on closer scrutiny; (5) the authors were not contactable to provide additional data; (6) the authors were not able to provide these missing data.
Some studies focused on tobacco alone, and others on tobacco, alcohol, drugs, violence, cardiac health or policy change. The range of interventions was also heterogeneous. They included information about:
Short‐ and long‐term consequences of smoking;
Prevalence of smoking;
Generic social skills;
Tobacco‐, alcohol‐ and drug‐refusal skills;
Interventions about tobacco included with interventions about risk‐taking, violence and carrying weapons;
School interventions associated also with family and community interventions;
Interventions to change school and state policies about tobacco availability;
Classroom management and reading strategies for teachers;
Culturally sensitive programmes, for example programmes for native North Americans.
The educational techniques were varied, and included lectures, quizzes, skits, collages, puppet plays, debates, role‐plays, making videos, discussions of videotaped role‐plays, films, interactive internet programmes, and meetings with athletes. Some studies compared interventions without a control group, and some included a control group in their comparisons. Some compared different types of presenters (teachers versus peers), and some compared videotaped to lecture presentations.
The presenters were usually the classroom teachers, but also included researchers, health educators, science teachers, undergraduate and graduate students, community members, uniformed police, and same‐age and older peers. The trials identified in this review are also heterogeneous in terms of duration of intervention (one hour to 36 classes spread over three years), and time from completion of intervention to final follow‐up (six months to 12 years).
The outcome measures most frequently chosen by authors were never‐smoking, and lifetime, monthly, weekly or daily smoking. Some studies used Pechacek's (Pechacek 1984) or Botvin's (Botvin 1980; Botvin 1984) composite indices, or constructed their own. Some studies classified students as current nonsmokers (which included never‐smokers, quitters and sometimes experimenters), and this heterogeneous category was the most difficult to assess. The authors were therefore contacted for clarification and/or new data sets. Few studies biochemically confirmed self reports at all stages of the research.
Excluded studies
Two hundred and two studies are excluded from the review. The majority (114) are not randomised controlled trials. Other reasons are that the intervention(s) was not in schools (N = 14), follow‐up was less than six months (N = 27), there were no smoking outcomes (N = 34), there were no baseline data (N = 2), the study was outside the age limits (N = 6), the study goal was smoking cessation only and did not include prevention, or there was no intervention (N = 5). These studies are listed in the Characteristics of excluded studies table, because the title and/or abstract had appeared to be relevance to this review.
Ongoing studies
Six studies are classified as ongoing. In four, some details and data are known from the studies, but are insufficient at this time to confirm inclusion in the review. The remaining two are expected to be included in a future update of the review, but the full results are currently awaiting publication. All six are listed in the Characteristics of ongoing studies table.
Risk of bias in included studies
(See Figure 2)
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies, whether or not they had analysable data. The non‐coloured section of each bar represents different arms of multiple‐arm studies, for which risk of bias is assessed as a single measure for each study.
Selection bias: For the randomised control trials with analysable data, selection bias was assessed at low risk of bias in approximately half of the studies, and at unclear risk in almost all the remaining studies. Within the group of studies without analysable data, 12% were at low risk and 84% at unclear risk. The key area of uncertainty came from authors who mentioned only the word 'randomly', which resulted in a judgement of 'unclear.'
For the trials with analysable data, allocation concealment was assessed as being at unclear risk of bias in almost 95% of the studies. Those with no analysable data were either at unclear or at high risk of bias. This was predominantly because there was no comment in the study about allocation concealment. The Cochrane Handbook notes that:
"Cluster‐randomized trials often randomise all clusters at once, so lack of concealment of an allocation sequence should not usually be an issue. However, because small numbers of clusters are randomised, there is a possibility of chance baseline imbalance between the randomised groups, in terms of either the clusters or the individuals. Although not a form of bias as such, the risk of baseline differences can be reduced by using stratified or pair‐matched randomisation of clusters. Reporting of the baseline comparability of clusters, or statistical adjustment for baseline characteristics, can help reduce concern about the effects of baseline imbalance."
For each C‐RCT we verified, where possible, (1) if all clusters were randomised at the same time, (2) if samples were stratified on variables likely to influence tobacco‐use outcomes, (3) if clusters were pair‐matched, and (4) if there was baseline comparability between the intervention and control groups. Of the C‐RCTs with analysable data, 63% used pair matching and/or stratification.
Blinding: This was assessed as at unclear risk or unstated in almost all studies. Wood 2008, for 146 meta‐analyses involving 1346 trials, found that in trials with subjective outcomes, estimates of effect were exaggerated when there was unclear or inadequate concealment (ratio of odds ratios (ORs) 0.69, 95% confidence interval (CI) 0.59 to 0.82) and lack of blinding (ratio of ORs 0.75, 95% CI 0.61 to 0.93) but not in trials with objective outcomes. The outcomes in the studies in this review are objective smoking outcomes presented subjectively by adolescents. As Adams 2008 has shown, when adolescents' reports are objectively verified biochemically or they are asked to write their name on the questionnaire, their reports of weekly or monthly smoking rates significantly increase.
In this review, in most studies students were promised anonymity as they completed their questionnaires, but would most likely have known which study arm they were in, so that blinding was not feasible. In most studies the interventions were presented by classroom teachers, so that blinding of presenters was not possible. We cannot predict whether these factors would have increased or decreased the reporting of smoking rates.
Attrition bias: Across all study groups and also for those studies without analysable data, the percentage of studies assessed as being at low risk of attrition bias ranged from 40% to 50%, those at unclear risk from 40% to 58%, and those at high risk from 13% to 21%. There is no really satisfactory solution for missing data (Altman 2007). Patients excluded after randomisation are unlikely to be representative of those remaining (Nűesch 2009). The Cochrane Handbook advises mapping any methods for handling missing data closely to the known characteristics of the datasets, and to other datasets in the literature that are likely to have comparable outcomes. Adolescents who smoke may quit and re‐try, but are most likely to increase their frequency over time. There is thus some parallel with studies which tend to have worsening outcomes over time, such as lung cancer. Intention‐to‐treat solutions, such as baseline observation carried forward (BOCF), last observation carried forward (LOCF), and complete case analysis (excluding participants with incomplete outcome data) are therefore inappropriate because they require that the mechanisms governing drop‐out are independent of future unobserved measurements (Molenberghs 2004; Kenward 2009). Such independence is unlikely in this review because those who drop out are known to be more likely to be smokers and to have personal, family, friendship, social and cultural factors that promote smoking. Therefore, we did not replace missing data with our own estimates.
Selective reporting: For the trials with analysable data, the risk of bias from selective reporting was low for all the RCTs in Groups 1, 2 and 3, and for 90% of the studies which provided no analysable data.
Effects of interventions
Studies were classified into three groups according to how authors presented their data: Group 1 (Pure Prevention cohorts), Group 2 (Change in Smoking Behaviour over time), and Group 3 (Point Prevalence of Smoking). We contacted authors in Groups 2 and 3 and invited them to recompute their data to provide datasets of baseline never‐smokers; if they were unable to comply or did not reply we computed such datasets where we could. These results were then further analysed by duration of follow‐up and intervention category.
GROUP 1: PURE PREVENTION COHORT (49 C‐RCTs, 73 arms)
Comparison of all intervention curricula versus control, with duration of follow‐up of one year or less (See Analysis 1.1): When the outcomes for all the trials testing any of the five different intervention curricula were pooled there was no overall effect (odds ratio (OR) 0.94, 95% confidence interval (CI) 0.85 to 1.05; I² = 0%; Analysis 1.1). The I² statistic for subgroup differences across all interventions was 44.1%, but within each intervention category heterogeneity was minimal. One small trial (Howard 1996) which tested an information curriculum found no effect. The combined social competence and social influences curricula (six RCTs/seven arms) showed a statistically significant effect in preventing the onset of smoking (OR 0.49, 95% CI 0.28 to 0.87; P = 0.01; I² = 0%; Analysis 1.1.3). However, for the social influences curricula (16 RCTs/25 arms) (OR 1.00, 95% CI 0.88 to 1.13; I² = 0%; Analysis 1.1.2) and the multimodal curricula (three RCTs/five arms) (OR 0.89, 95% CI 0.73 to 1.08; I² = 50%; Analysis 1.1.4), the results were not significant, with the 95% confidence interval including the line of no effect (= 1). There was no RCT testing a social competence curriculum versus control with a follow‐up duration of less than one year. One study with two arms, Figa‐Talamanca 1989 (F); Figa‐Talamanca 1989 (N.F), was included in the overall effect, but the intervention used did not fit into one of the five main intervention categories.
1.1. Analysis.
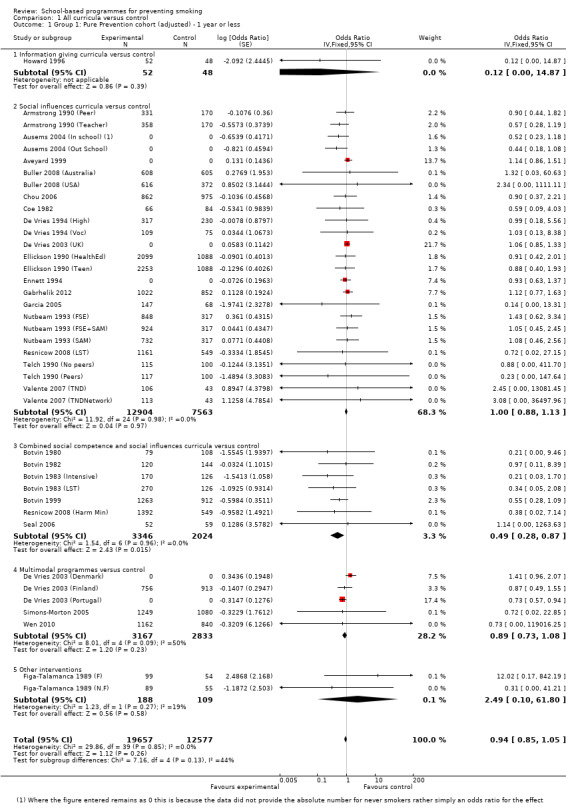
Comparison 1 All curricula versus control, Outcome 1 Group 1: Pure Prevention cohort (adjusted) ‐ 1 year or less.
Sensitivity analyses: Sensitivity analyses restricted to studies at low risk of bias in Group 1 found no differences from the all‐trials versions, apart from the trials of social competence and social influences curricula, which no longer demonstrated a significant effect, i.e. the all‐trials OR was 0.49 (95% CI 0.28 to 0.87), compared with the low risk of bias trial OR of 0.55 (95% CI 0.28 to 1.09; Analysis 2.1.3).
Comparison of all curricula versus control, with longest follow‐up period: [See Analysis 1.2]
1.2. Analysis.

Comparison 1 All curricula versus control, Outcome 2 Group 1: Pure Prevention cohort (adjusted) ‐ longest follow‐up.
When the outcomes for all the trials testing any of the five different intervention curricula were pooled there was a significant effect favouring the intervention (OR 0.88, 95% CI 0.82 to 0.96; P = 0.002; I² = 0%), with a mean risk reduction of 12%. (See Figure 3): Heterogeneity was 0%, except for the multimodal curricula trials (I² = 50%). One C‐RCT testing information curricula detected a nonsignificant effect (OR 0.12, 95% CI 0.00 to 14.87; P not applicable).
3.

Forest plot of comparison: 1 All curricula versus control, outcome: 1.2 Group 1: Pure Prevention cohorts (adjusted) at longest follow‐up.
Social competence curricula (five C‐RCTs/seven arms) versus control showed a statistically significant result in favour of the intervention (OR 0.52, 95 % CI 0.30 to 0.88; P = 0.02; I² = 0%; Analysis 1.2.2), as also did the combined social competence and social influences versus control (eight C‐RCTs/10 arms), (OR 0.50, 95% CI 0.28 to 0.87; P = 0.01; I² = 0%; Analysis 1.2.4).
There were no statistically significant differences for social influences programmes or multimodal curricula.
Four trials (six arms) contributed to the overall results, but not to the individual curricula (Brown 2002; Figa‐Talamanca 1989 (F); Figa‐Talamanca 1989 (N.F); Johnson 2009; Kellam 1998 (GBG); Kellam 1998 (ML)).
Sensitivity analyses:
Sensitivity analyses restricted to trials at low risk of selection bias demonstrated no differences from the all‐trials findings. Ranking by risk of attrition bias made little difference to the findings, apart from a widening of the confidence interval to include the line of no effect, i.e. all‐trials OR 0.88 (95% CI 0.82 to 0.96) versus low risk of bias OR 0.89 (95% CI 0.78 to 1.02).
GROUP 2: CHANGE IN SMOKING BEHAVIOUR OVER TIME (15 C‐RCTs, 27 arms)
Comparison of all curricula versus control, with duration of follow‐up of one year or less: (See Analysis 1.3)
1.3. Analysis.
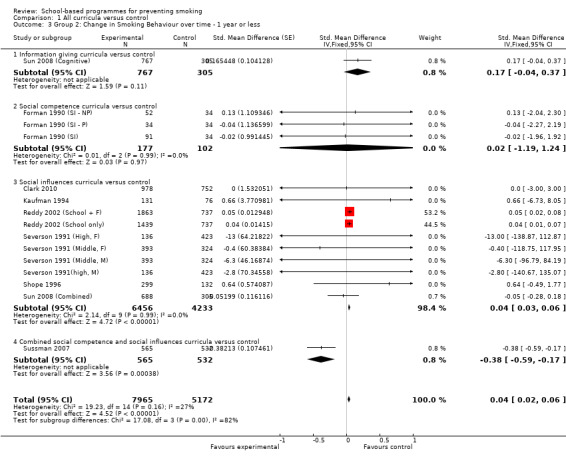
Comparison 1 All curricula versus control, Outcome 3 Group 2: Change in Smoking Behaviour over time ‐ 1 year or less.
The eight studies (15 arms) demonstrated a small statistically significant effect favouring the control group (standardised mean difference (SMD) 0.04, 95 % CI 0.02 to 0.06; P = 0.00001; I² =27%). This is similar to Pure Prevention cohorts (Group 1) combined social competence and social influences curriculum (only one C‐RCT (one arm)) found a significant effect favouring the intervention (SMD ‐0.38, 95%CI ‐0.59 to ‐0.17; P = 0.0004), but unlike Group 1 social influences curricula found a small statistically significant effect favouring the controls (six C‐RCTs/10 arms) (SMD 0.04, 95% CI 0.03 to 0.06; P = 0.00001; I² = 0%). There were no significant effects for information and social competence curricula.
Sensitivity analyses: A sensitivity analysis restricted to trials at low risk of attrition bias demonstrated a nonsignificant effect.
Comparison of all curricula versus control, with longest follow‐up period: (See Analysis 1.4) Fifteen C‐RCTs (27 arms) demonstrated a nonsignificant effect (SMD 0.01, 95% CI ‐0.00 to 0.02; P = 0.18; I² = 57%). Two C‐RCTs (five arms) that tested social competence curricula favoured the intervention (SMD ‐ 0.04, 95% CI ‐0.06 to ‐0.01; P = 0.01; I² = 0%). Ten C‐RCTs (16 arms) testing social influences curricula (SMD 0.05, 95% CI 0.03 to 0.06; P = 0.00001; I² = 0%) favoured the controls. There was no effect for information, combined social competence and social influences or multimodal curricula.
1.4. Analysis.

Comparison 1 All curricula versus control, Outcome 4 Group 2: Change in Smoking Behaviour over time ‐ longest follow‐up.
Sensitivity analyses: Sensitivity analyses restricted to trials at low risk of attrition or selection bias demonstrated no important differences from the all‐trials findings.
GROUP 3: POINT PREVALENCE OF SMOKING (25 C‐RCTs, 39 arms): (See Analysis 1.5, Analysis 1.6)
1.5. Analysis.

Comparison 1 All curricula versus control, Outcome 5 Group 3: Point Prevalence of Smoking ‐ 1 year or less.
1.6. Analysis.

Comparison 1 All curricula versus control, Outcome 6 Group 3: Point Prevalence of Smoking ‐ longest follow‐up.
The heterogeneity in this group of studies (for all interventions and for both follow‐up durations) was extremely high (minimum I² = 99%) and beyond what would be expected by chance alone. We have, therefore, not pooled these trials, but display them for reference
In the 16 studies (21 arms) that provided data at one year or less, eight out of 21 comparisons significantly favoured the controls (Analysis 1.5). This trend continued through longest follow‐up, with 20 of 25 studies (39 arms) significantly favouring the controls (Analysis 1.6).
Sensitivity analyses restricted to trials at low risk of selection bias or at low and unclear risk of attrition bias had no impact on the results.
Subgroup analyses (Pure Prevention cohort, Group 1 only)
Differences by gender (Analysis 3.1, Analysis 3.3): At one year for the limited number of studies which presented data by gender, there was both a significant effect (OR 0.69, 95% CI 0.49 to 0.96; P = 0.04; I² = 30%) for females (seven arms), and for males (six arms) (OR 0.66, 95% CI 0.44 to 0.98; P = 0.04; I² = 30%). The largest effect was found in one study (De Vries 2003 (Finland)) which tested a multimodal curriculum (OR 0.32, 95% CI 0.16 to 0.65; P = 0.002) in males. At longest follow‐up there were no statistically significant differences for females (nine arms) or males (eight arms).
3.1. Analysis.

Comparison 3 Group 1: Gender analysis, Outcome 1 Female ‐ 1 year or less.
3.3. Analysis.

Comparison 3 Group 1: Gender analysis, Outcome 3 Male ‐ 1 year or less.
Peer‐ versus adult‐led interventions: Adult‐led interventions (29 arms) were not shown to be more effective up to one year than controls in any of the programmes, except for combined social competence and social influences curricula (OR 0.46, 95% CI 0.26 to 0.84; P = 0.01; I² = 0%). There was no overall effect for the peer‐led interventions (8 arms) compared to controls, although this only included social influences curricula tested by a single study (Botvin 1982) which offered a combined social competence and social influences curriculum (Analysis 6.1, Analysis 6.3).
6.1. Analysis.

Comparison 6 Group 1: Peer‐led analysis, Outcome 1 Peer‐led ‐ 1 year or less.
6.3. Analysis.

Comparison 6 Group 1: Peer‐led analysis, Outcome 3 Adult‐led ‐ 1 year or less.
In contrast, at longest follow‐up there were significant overall effects for adult‐led interventions (56 arms) compared to the control groups (OR 0.88, 95% CI 0.81 to 0.96; P = 0.002; I² = 17%), and significant effects for two of the four curricula tested: social competence (7 arms) (OR 0.52, 95% CI 0.30 to 0.88; P = 0.02, I² = 0%) and combined social competence and social influences (7 arms) (OR 0.47, 95% CI 0.26 to 0.84; P = 0.01, I² = 0%), but not for social influences or multimodal curricula. For peer‐led programmes (11 arms) compared to controls (Analysis 6.2) there were no statistically significant differences overall, nor for the three curricula tested (social influences, combined social competence and social influences and multimodal).
6.2. Analysis.

Comparison 6 Group 1: Peer‐led analysis, Outcome 2 Peer‐led ‐ longest follow‐up.
Four studies (six arms) which compared peer‐led and adult‐led interventions to controls were not included, either because it was not clear who delivered the programme (Conner 2010 (I); Conner 2010 (SE); Seal 2006) or because it was delivered online (Buller 2008 (Australia); Buller 2008 (USA); Prokhorov 2008).
Interventions focused on tobacco versus interventions covering multiple areas: When the effectiveness of multifocal curricula (i.e. a combined focus on tobacco, drugs and alcohol prevention) was compared to control there was no overall effect at one year or at longest follow‐up. Only one curriculum, social competence (seven arms), showed a significant effect at longest follow‐up (OR 0.52, 95% CI 0.30 to 0.88; P = 0.02; I² = 0%; Analysis 5.2.2).
Curricula focused only on tobacco use prevention (26 arms) compared to controls showed no effect (OR 0.93, 95% CI 0.83 to 1.04) at one year, although there was an effect at longest follow‐up (42 arms) (OR 0.88, 95% CI 0.80 to 0.97; P = 0.01; I² = 20%; Analysis 5.4). None of the the three curricula tested at one year or at longest follow‐up (social influences, combined social competence and social influences, and multi‐modal) found significant differences.
5.4. Analysis.

Comparison 5 Group 1: Tobacco focus, Outcome 4 Tobacco focused ‐ longest follow‐up.
Effect of adding booster sessions: At one year or less there were no significant differences for curricula (36 arms) which did not include booster sessions, compared to controls (OR 0.94, 95% CI 0.85 to 1.05; Analysis 4.1), or at longest follow‐up (66 arms) (OR 0.90, 95% CI 0.83 to 0.97; P = 0.10; I² = 0%; Analysis 4.2).
4.1. Analysis.
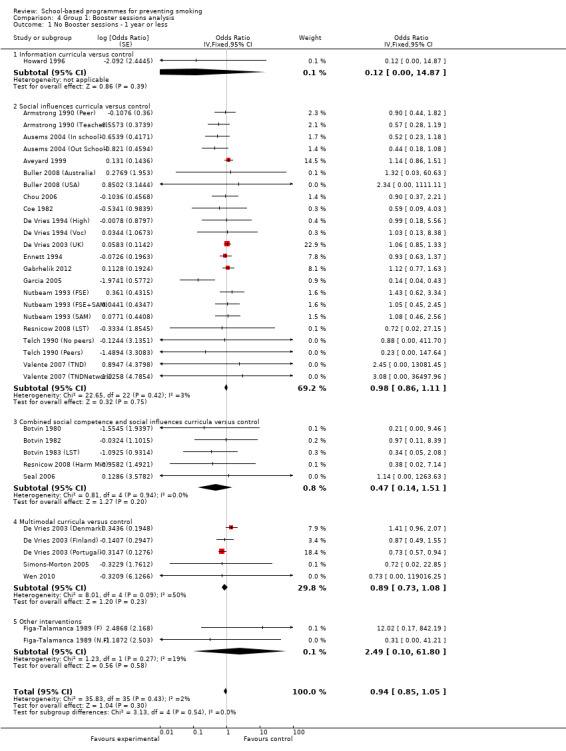
Comparison 4 Group 1: Booster sessions analysis, Outcome 1 No Booster sessions ‐ 1 year or less.
4.2. Analysis.

Comparison 4 Group 1: Booster sessions analysis, Outcome 2 No Booster sessions ‐ longest follow‐up.
For curricula which included booster sessions, there were no significant differences from controls at one year or less (four arms) (OR 0.70, 95% CI 0.40 to 1.07), but at longest follow‐up (seven arms) there was a significant difference (OR 0.73, 95% CI 0.55 to 0.98; Analysis 4.4).
4.4. Analysis.

Comparison 4 Group 1: Booster sessions analysis, Outcome 4 Booster sessions ‐ longest follow‐up.
The combined social competence and social influences curricula (OR 0.50, 95% CI 0.26 to 0.96; P = 0.04; I² = 0%) had a positive effect at one year or less (two arms) and also at longest follow‐up (three arms) (OR 0.51, 95% CI 0.27 to 0.96; P = 0.04; I² = 0%).
Discussion
Summary of Main Results Outcomes are presented for three distinct groups: Pure Prevention cohorts of baseline never‐smokers, studies where authors presented results as Change in Smoking Behaviour over time, and studies where authors presented data as Point Prevalence of Smoking. Only four studies contributed to more than one group.
In the Pure Prevention cohort (Group 1), one might expect the clearest indication of whether smoking interventions prevent smoking, as studies followed the same cohort of never‐smoking individuals from baseline to follow‐ups. This group of cluster‐randomised controlled trials (C‐RCTs) with follow‐up of a year or less demonstrated no overall significant effect, with only the combined social competence and social influences curricula delivering positive results. Pooling the results from all the trials at longest follow‐up favoured the intervention groups (OR 0.88, 95% CI 0.82 to 0.96). This represents a risk reduction of 12% and suggests that interventions were more effective over a longer time period. The only intervention categories within this group that showed a statistically significant result were social competence and combined social competence and social influence curricula. This indicates that the success of the combined social competence and social influence curricula at one year was maintained over a longer period. There were no social competence intervention studies with one year or less of follow‐up for comparison.
Though pooled data suggest a significant effect in favour of the controls on Change in Smoking Behaviour over time (Group 2), the results are not incompatible with those of the Pure Prevention cohort studies (Group 1). Whilst the overall effect marginally favours the controls, there are similarities at intervention programme level to the results from the Pure Prevention cohort studies. This would be expected, since these studies, while measuring a change rate, follow the same groups of participants over time. Higher heterogeneity in this group could be explained by the differences between the participants (never‐smokers, experimenters and quitters) and between outcome measures.
Sensitivity analyses for Pure Prevention cohorts (Group 1) and Change in Smoking Behaviour over time (Group 2) for selection and attrition bias revealed no differences between studies at low risk and those at unclear or high risk.
In the Group 3 studies which present point prevalence smoking data, it was not possible to pool data due to the high level of heterogeneity, though the trends may have favoured the controls. The most likely explanation for the heterogeneity is that the same individuals are not consistently being measured over time, and thus point prevalence data are inadequate to measure the effectiveness of this type of intervention.
Subgroup analyses were only completed for the Pure Prevention cohorts (Group 1) data, and showed that:
Gender: For the few studies that reported results by gender, there were positive significant results for both females and males with one year or less of follow‐up. However, within both groups only one intervention category (multimodal) in one study for males found a positive significant result.
Peer‐led versus adult‐led interventions: There were no significant differences for studies at one year or less for peer‐led compared to adult‐led curricula, except for adult‐led combined social competence and social influences curricula. At longest follow‐up there were significant differences favouring adult‐led curricula, and for adult‐led social competence curricula and adult‐led combined social competence and social influences curricula.
Multifocal versus tobacco‐only interventions: At one year or less there were no differences between multifocal and tobacco‐only programmes. However, at longest follow‐up tobacco‐only curricula had a significant effect, and within multifocal interventions the social competence returned positive findings.
Booster sessions versus no boosters sessions: Major effort has been expended in many studies to provide booster sessions, expecting that they would reinforce the effects of the original programmes. At one year or less the presence or absence of boosters made no difference. Combined social competence and social influences curricula appeared to benefit from booster sessions in the medium and long term. This suggests that curricular orientation may be more important than providing booster sessions.
Overall completeness and applicability of evidence The number of studies which provided no analysable data is large (49 C‐RCTs with 152,544 students), with seven C‐RCTs (42,020 students) from the Pure Prevention cohorts (Group 1), one C‐RCT (12,022 students) from the Change in Smoking Behaviour over time group (Group 2), and 41 C‐RCTs (98,502 students) from the Point Prevalence of Smoking group (Group 3). Twelve per cent of these trials are at low risk and 84% at unclear risk of selection bias, compared with approximately half at low risk and almost all the remaining studies at unclear risk in the trials with usable data. However, the percentages at low and unclear risk were similar for allocation, blinding, attrition and reporting biases. Our inability to include this large number of C‐RCTs and participants therefore excludes data of lower quality with respect to selection bias. A funnel plot (not shown) did not suggest publication bias in Pure Prevention cohorts or Change in Smoking Behaviour analyses.
Population: Of the trials which provided analysable data, 56% were from North America (51% from the USA), 35% from Europe, 5% from Asia, 3% from Australia, and 1% from Africa. There is thus minimal representation from four of the six continents. In the US studies there is wide representation of urban and rural, socioeconomic, and ethnic groups. Few studies reported data separately by gender.
Interventions: We placed no restrictions on the type of intervention that was included, provided it was school‐based. This resulted in a huge variety of interventions, which were analysed in six broad categories. A small number of interventions could not be classified, and although they are included in the overall analysis it was inappropriate to assess them as a separate category.
Social influence curricula were tested more than any other curricula in studies. In the Pure Prevention cohorts group, 63% of intervention arms at one year or less and 67% at longest follow‐up tested social influences interventions. The proportions in the Change in Smoking Behaviour over time group were 67% and 59% respectively. Only in the Change in Smoking Behaviour were social influence curricula found to be significant, and these favoured the controls.
Ideally, the review would have examined the positive effect of social competence or combined social competence and social influences further, by considering studies that made direct comparisons of these intervention types. However, although there were a few studies that explored comparisons between interventions, none of them considered these intervention types.
Outcomes: The trials deployed a wide variety of outcome measures: never‐smoking; lifetime, monthly, weekly or daily smoking; numbers of cigarettes smoked during each of these time intervals; and indices such as Pechacek's (Pechacek 1984) or Botvin's (Botvin 1980; Botvin 1984). Some studies used the term 'current nonsmokers,' but this can include never‐smokers, experimenters and quitters, which can introduce a lack of clarity into any attempt to follow cohorts. The measures used most frequently are never‐smoking; smoking in the past 30 days and current nonsmoking.
Quality of the Evidence The main strength of this review is the large number of included studies (134) and the number of participants (428,293). Although a large number of trials (85) with 275,749 participants provided analysable data, a limitation of this review is that 49 trials (152,544 participants; 37% of the total) were eligible, but did not provide sufficient data in their publications or did not provide the data after study authors were contacted. However, the data we could not include are deemed to be at greater risk of selection bias than the usable information.
For the Pure Prevention cohorts (Group 1) trials, it is worth noting that 49 studies (73 arms) with 142,447 participants were included in the analysis, representing 88% of all potential Pure Prevention cohorts trials.
Key methodological problems: Key problems in some studies are a failure to describe robust methods of randomisation or allocation concealment, high rates of attrition, varying outcome measures for tobacco use, the use of 'current nonsmoker' as an outcome, failure to follow groups of never‐smokers, triers, and quitters separately over time, and failure to report basic data such as the numbers and smoking status in the intervention and control groups at baseline and follow‐ups. Our decision not to pool data from the Point Prevalence of Smoking trials arose from our assessment of point prevalence as an inadequate measure for reporting effects in these types of studies.
Consistency between the Pure Prevention cohorts (Group 1) and Change in Smoking Behaviour over time studies (Group 2) was good, but it was not possible to compare them with the Point Prevalence of Smoking studies (Group 3). Whilst many studies reported inadequately on their randomisation process and on attrition, sensitivity analyses suggest that these potential risks of bias did not have any real effect on the main findings for each group or intervention type.
Potential biases in the review process One strength of this review is that the search was conducted across multiple electronic data bases, and included 'grey' literature, the searching of reference lists of articles, and consultation with experts. There were no limitations of date or language, and translations were obtained for any article as required. It is unlikely that this extensive search would have missed key trials.
Two authors independently reviewed all titles and abstracts and independently entered all data on Cochrane Tobacco Review Group data extraction forms. Extensive correspondence (over 600 emails) was undertaken with all study authors if data on risks of bias, the planning and conduct of the trial, numbers, stratification and pairing of clusters, baseline equivalence of intervention and control arms, and tobacco outcome status were not provided in the publications. Many study authors computed new databases of baseline never‐smokers for the review, or the reviewers computed this data.
Bias could have been introduced due to the high variability of outcome measures, although this has been reduced by dividing the studies into three groups and analysing the data for each group separately. The low heterogeneity in the Pure Prevention cohorts (Group 1) studies supports this approach. Bias may also have been introduced by certain assumptions made by the study authors in data extraction, and subsequent statistical analysis. This is particularly pertinent in the Point Prevalence of Smoking studies (Group 3), where we considered it inappropriate to pool the data.
Agreements and disagreements with other studies or reviews There is no other comprehensive review of interventions in schools for comparison.
Authors' conclusions
Implications for practice.
There was a significant effect for the Pure Prevention cohorts studies which followed participants for more than one year, but not for shorter‐term outcomes: combined social competence and social influences interventions at all time points, and social competence interventions at longest follow‐up prevented smoking uptake compared with controls; social influence interventions did not appear to reduce uptake compared with controls.
Studies at low risk of selection and attrition bias did not deliver better results than the full mix of available trials.
Interventions delivered by adult presenters are more effective in the longer term than peer‐led programmes.
Adding booster sessions in subsequent years do not change outcomes.
Implications for research.
Further studies of social competence and combined social competence and social influences programmes could explore the potential of these interventions.
Further research is required to design and test programmes that will be optimally effective for both genders.
Further research is required to identify factors that can be tailored to the requirements of different ethnic groups.
Studies need to follow up participants for more than one year.
Studies should clearly identify and follow separately students in different stages of their smoking career (never‐smokers, experimenters, quitters, smokers of different frequencies and intensities), as composite change rates and point prevalence scores at baseline and follow‐up make the findings difficult to interpret.
Outcome measures should be standardised at trial design stage.
Studies are needed across all cultural areas of the world.
There is minimal information on the costs of designing and implementing these programmes. Economic evaluation is important, in view of the fact that many interventions have not proven their effectiveness.
What's new
| Date | Event | Description |
|---|---|---|
| 1 May 2013 | Amended | Minor textual edit in the Discussion section, and the Author's conclusion section. Acknowledgement also added. |
History
Protocol first published: Issue 4, 1998 Review first published: Issue 4, 2002
| Date | Event | Description |
|---|---|---|
| 22 March 2013 | New search has been performed | Updated with 51 new studies. Latest search October 2012. |
| 22 March 2013 | New citation required and conclusions have changed | New analysis methods used. New author added. New categories and conclusions |
| 22 June 2011 | Amended | Additional table converted to appendix to correct pdf format |
| 18 April 2008 | Amended | Converted to new review format. |
| 20 April 2006 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
To Dr. Keith Busby for time and advice spent in the initial analysis and data entry of the literature for the first edition; to Tim Lancaster, Lindsay Stead, Kate Cahill and Jamie Hartmann‐Boyce, Cochrane Tobacco Addiction Group, Oxford, for exemplary and detailed help with literature searching, data management, suggestions for analysis, careful and thorough editing, and encouragement. Many thanks also to Steven Sussman, Paul Aveyard and Donald Reid, who read earlier drafts of the manuscript for the first edition and/or this updated version.
In addition, many thanks to the following for their help in clarifying study information or providing further data: Dr M Beets, Dr H Bian, Dr R Brown, Dr D Buller, Dr C Chou, Dr A Connell, Prof M Connor, Dr M Crone, Dr P Ellickson, Prof F Faggiano, Dr R Gabrhelik, Dr K Glanz, Dr J Gordon, Dr K Griffin, Dr B Hansen, Dr D Haynie, Dr C Johnson, Dr H Kimberly, Dr J McCambridge, Dr I Mesters, Dr P Moberg, Dr C Perry, Prof A Prokhorov, Dr C Ringwalt, Dr N Seal, Dr S Shamblen, Ds Z Sloboda, Dr T St Pierre, Dr P Sun, Dr J Unger, Dr T Valente, Dr G Van Breukelen, Dr P Van Lier, Dr X Wen and Dr P Zheng.
Appendices
Appendix 1. MEDLINE search strategy
| 'SMOKING'/ all subheadings or 'SMOKING‐CESSATION'/ all subheadings or SMOK* or TOBACCO or NICOTINE or SMOKING CESSATION PREVENT* or STOP* or QUIT* or ABSTIN* or ABSTAIN* or REDUC* or TOBACCO USE DISORDER OR EX‐SMOKER OR FREEDOM FROM SMOKING OR ANTI‐SMOK* #1 and #2 'HEALTH‐PROMOTION'/ all subheadings explode 'HEALTH‐EDUCATION'/ all subheadings 'ADOLESCENT‐BEHAVIOR'/ all subheadings 'PSYCHOTHERAPY,‐GROUP'/ all subheadings EDUCATION or PREVENT* or PROMOT* or TEACH* or (GROUP near THERAPY) #4 or #5 or #6 or #7 or #8 #3 and #9 'CHILD‐' or 'ADOLESCENCE'/ all subheadings or CHILD or ADOLESCEN* or STUDENT* or SCHOOL* or CLASS* #10 and #11 (CLINICAL‐TRIAL IN PT) OR (randomizED‐CONTROLLED‐TRIAL IN PT) OR (CONTROLLED‐CLINICAL‐TRIAL IN PT) explode 'CLINICAL‐TRIALS'/ all subheadings 'EVALUATION‐STUDIES' 'PROGRAM‐EVALUATION'/ all subheadings 'META‐ANALYSIS' SYSTEMATIC REVIEW RANDOM* #13 or #14 or #15 or #16 or #17 or #18 #12 and #20 |
Appendix 2. CINAHL search strategy
| #14 #9 and (trial* or meta‐analysis or systematic review) #13 review #12 systematic #11 meta‐analysis #10 trial* #9 #2 or #4 or #6 or #8 #8 'Tobacco‐Smokeless' /all topical subheadings / in‐adolescence, in‐infancy‐and‐childhood in DE #7 'Tobacco‐Smokeless' / all topical subheadings / in‐adolescence, in‐infancy‐and‐childhood # 6 'Smoking‐Cessation‐Programs' / all topical subheadings / in‐adolescence, in‐infancy‐and‐childhood in DE #5 'Smoking‐Cessation‐Programs' / all topical subheadings / in‐adolescence, in‐infancy‐and‐childhood #4 'Smoking‐Cessation' / all topical subheadings / in‐adolescence, in‐infancy‐and‐childhood in DE #3 'Smoking‐Cessation' / all topical subheadings / in‐adolescence, in‐infancy‐and‐childhood #2 explode 'Smoking‐' / prevention‐and‐control in‐adolescence, in‐infancy‐and‐childhood in DE #1 explode 'Smoking‐' / prevention‐and‐control in‐adolescence, in‐infancy‐and‐childhood |
Appendix 3. Raw data group 1 studies (included in analysis)
| Study ID | Control arm | OR | Follow‐up | ||||||
| No. lost to never‐smokers | Never‐smokers at baseline | Cluster No. | |||||||
| One year or less follow‐up | |||||||||
| Howard 1996 | I | 0 | 51 | 3 classes | 3 | 47 | 3 classes | 1 yr | |
| Armstrong 1990 (Teacher) | SI | 74 | 358 | 15 | 106 | 339 | 15 | 1 yr | |
| Armstrong 1990 (Peer) | SI | 96 | 331 | 15 | 106 | 339 | 15 | 1 yr | |
| Ausems 2004 (In school) | SI | 9 | 9 baseline/7@1 yr | 0.52 (adj) | 1 yr | ||||
| Ausems 2004 (Out School) | SI | 8 baseline/6@1 yr | 9 baseline/8@1 yr | 0.44 (adj) | 1 yr | ||||
| Aveyard 1999 | SI | 27 | 26 | 1.14 (unadj) | 1 yr | ||||
| Buller 2008 (Australia) | SI | 34 | 608 | 13 | 26 | 605 | 12 | 6 mths | |
| Buller 2008 (USA) | SI | 41 | 616 | 10 | 11 | 372 | 11 | 6 mths | |
| Chou 2006 | SI | 142 | 862 | 7 | 175 | 975 | 7 | 1 yr | |
| Coe 1982 | SI | 8 | 66 | 2 | 16 | 84 | 2 | 1 yr | |
| De Vries 1994 (Voc) | SI | 9 | 109 | 3 | 6 | 75 | 3 | 1 yr | |
| De Vries 1994 (High) | SI | 26 | 317 | 5 | 19 | 230 | 3 | 1 yr | |
| De Vries 2003 (UK) | SI | 22 | 21 | 1.06 (adj) | 1 yr | ||||
| Ellickson 1990 (Teen) | SI | 527 | 2253 | 10 | 561 | 2175 | 10 | 1 yr | |
| Ellickson 1990 (HealthEd) | SI | 506 | 2099 | 10 | 561 | 2175 | 10 | 1 yr | |
| Ennett 1994 | SI | 18 | 18 | 0.93 (adj) | 1 yr | ||||
| Figa‐Talamanca 1989 (F) | SI | 10 | 99 | 8 | 1 | 108 | 8 | 1 yr | |
| Figa‐Talamanca 1989 (N.F) | SI | 0 | 88 | 8 | 1 | 108 | 8 | 1 yr | |
| Gabrhelik 2012 | SI | 160 | 917 | 40 | 125 | 787 | 34 | 1 yr | |
| Garcia 2005 | SI | 7 | 147 | 6 | 18 | 68 | 4 | 1 yr | |
| Nutbeam 1993 (FSE) | SI | 362 | 848 | 10 | 325 | 951 | 10 | 1 yr | |
| Nutbeam 1993 (SAM) | SI | 263 | 732 | 9 | 325 | 951 | 10 | 1 yr | |
| Nutbeam 1993 (FSE+SAM) | SI | 325 | 924 | 10 | 325 | 951 | 10 | 1 yr | |
| Resnicow 2008 (LST) | SI | 182 | 1161 | 12 | 226 | 1097 | 12 | 1 yr | |
| Telch 1990 (Peers) | SI | 4 | 117 | 4 | 27 | 199 | 7 | 6 mths | |
| Telch 1990 (No peers) | SI | 14 | 115 | 4 | 27 | 199 | 7 | 6 mths | |
| Valente 2007 (TND) | SI | 3 | 106 | 22 | 1 | 85 | 28 | 1 yr | |
| Valente 2007 (TNDNetwork) | SI | 4 | 113 | 25 | 1 | 85 | 28 | 1 yr | |
| Botvin 1980 | C | 3 | 79 | 1 | 17 | 108 | 1 | 6mths | |
| Botvin 1982 | C | 26 | 120 | 1 | 32 | 144 | 1 | 1 yr | |
| Botvin 1983 (LST) | C | 31 | 270 | 2 | 70 | 251 | 3 | 1 yr | |
| Botvin 1983 (LST intensive) | C | 13 | 170 | 2 | 70 | 251 | 3 | 1 yr | |
| Botvin 1999 | C | 144 | 1263 | 29 total | 173 | 912 | 29 total | 1 yr | |
| Resnicow 2008 (Harm Min) | C | 126 | 1392 | 12 | 226 | 1097 | 12 | 1 yr | |
| Seal 2006 | C | 0 | 52 | 1 | 1 | 59 | 1 | 6 mths | |
| De Vries 2003 (Denmark) | MM | 30 | 30 | 1.41 | 1 yr | ||||
| De Vries 2003 (Finland) | MM | 185 | 756 | 13 | 248 | 913 | 14 | 1 yr | |
| De Vries 2003 (Portugal) | MM | 14 | 11 | 0.73 | 1 yr | ||||
| Simons‐Morton 2005 | MM | 333 | 1249 | 3 | 361 | 1080 | 4 | 1 yr | |
| Wen 2010 | MM | 92 | 1162 | 2 | 89 | 840 | 2 | 1 yr | |
| Longest Follow‐up (over 1 year) | |||||||||
| Connell 2007 | SC | 95 | 196 | 3 | 100 | 222 | 3 | 11 yrs | |
| Kellam 1998 (GBG) | SC | 92 | 348 | 6 | 299 | 904 | 6 | 8 yrs | |
| Kellam 1998 (ML) | SC | 111 | 352 | 7 | 299 | 904 | 6 | 8 yrs | |
| Spoth 2001 (ISFP) | SC | 46 | 141 | 11 | 71 | 142 | 11 | 4 yrs | |
| Spoth 2001 PDFY) | SC | 50 | 128 | 11 | 71 | 142 | 11 | 4 yrs | |
| Spoth 2002 (LST) | SC | 64 | 462 | 12 | 68 | 408 | 12 | 1.5 yrs | |
| Storr 2002 (CC) | SC | 60 | 230 | 3 | 72 | 219 | 3 | 6 yrs | |
| Storr 2002 (FSP) | SC | 60 | 229 | 3 | 72 | 219 | 3 | 6 yrs | |
| Walter 1986 | SC | 16 | 447 | 8 | 61 | 464 | 7 | 6 yrs | |
| Armstrong 1990 (Teacher) | SI | 116 | 358 | 15 | 70.5 | 169.5 | 7.5 | 2 yrs | |
| Armstrong 1990 (Peer) | SI | 132 | 331 | 15 | 70.5 | 169.5 | 7.5 | 2 yrs | |
| Ausems 2004 (Out school) | SI | 7 baseline/5@18 mths | 8 baseline/7 @18 mths | 0.42 (adj) | 18 mths | ||||
| Aveyard 1999 | SI | 27 | 26 | 1.06 (unadj) | 2 yrs | ||||
| Brown 2002 | SI | 176 | 1313 | 15 | 183 | 1201 | 15 | 2 yrs | |
| Conner 2010 (I) | SI | 65 | 297 | 15 | 104 | 373 | 19 | 2 yrs | |
| Conner 2010 (SE) | SI | 82 | 257 | 13 | 115 | 358 | 18 | 2 yrs | |
| Crone 2011 | SI | 25 | 1311 | 62 | 33 | 1022 | 59 | 19 mths | |
| De Vries 2003 (UK) | SI | 22 | 21 | 0.94 (adj) | 30 mths | ||||
| Denson 1981 | SI | 8 | 256 | 6 | 49 | 272 | 6 | 2 yrs | |
| Elder 1996 | SI | 56 | 40 | 1.01 (adj) | 3 yrs | ||||
| Ellickson 1990 (Teen) | SI | 651 | 2253 | 10 | 338 | 1087.5 | 5 | 15 mths | |
| Ellickson 1990 (HealthEd) | SI | 642 | 2099 | 10 | 338 | 1087.5 | 5 | 15 mths | |
| Ellickson 2003 | SI | 152 | 1765 | 34 | 191 | 1171 | 21 | 18 mths | |
| Ennett 1994 | SI | 18 | 18 | 0.99 (adj) | 2 yrs | ||||
| Faggiano 2008 | SI | 245 | 2939 | 78 | 242 | 2791 | 65 | 18 mths | |
| Gabrhelik 2012 | SI | 262 | 917 | 40 | 235 | 787 | 34 | 2 yrs | |
| Hort 1995 | SI | 50 | 268 | 9 | 84 | 239 | 10 | 2 yrs | |
| Johnson 2009 | SI | 381 | 891 | 10 | 459 | 1116 | 10 | 4 yrs | |
| La Torre 2010 (A) | SI | 22 | 135 | 8 | 23 | 119 | 7 | 2 yrs | |
| La Torre 2010 (C) | SI | 3 | 197 | 11 | 24 | 240 | 13 | 2 yrs | |
| Peterson 2000 | SI | 1466 | 3684 | 20 | 1547 | 3756 | 20 | 12 yrs | |
| Prokhorov 2008 | SI | 2 | 380 | 9 | 8 | 317 | 8 | 18 mths | |
| Resnicow 2008 (LST) | SI | 182 | 1161 | 12 | 162.5 | 548.5 | 6 | 2 yrs | |
| Ringwalt 2009a | SI | 368 | 2335 | 17 | 332 | 2475 | 17 | 3 yrs | |
| Schulze 2006 | SI | 838 | 1205 | 89 | 596 | 872 | 83 | 18 mths | |
| Unger 2004 (FLAVOR) | SI | 194 | 933 | 8 | 115.5 | 538.5 | 4 | 18 mths | |
| Unger 2004 (CHIPS) | SI | 201 | 847 | 8 | 115.5 | 538.5 | 4 | 18 mths | |
| Van Lier 2009 | SI | 52 | 349 | 16 | 51 | 279 | 15 | 4 yrs | |
| Resnicow 2008 (Harm Min) | C | 206 | 1392 | 12 | 162.5 | 548.5 | 6 | 2 yrs | |
| Spoth 2002 (LST + SFP) | C | 48 | 385 | 12 | 34 | 204 | 6 | 1.5 yrs | |
| De Vries 2003 (Denmark) | MM | 30 | 30 | 1.15 (adj) | 30 mths | ||||
| De Vries 2003 (Finland) | MM | 404 | 756 | 13 | 419 | 913 | 14 | 30 mths | |
| De Vries 2003 (Portugal) | MM | 14 | 11 | 0.62 (adj) | 30 mths | ||||
| Piper 2000 (HFL) | MM | 254 | 564 | 7 | 159.5 | 359.5 | 4 | 4 yrs | |
| Piper 2000 (HFL Age) | MM | 385 | 614 | 7 | 159.5 | 359.5 | 4 | 4 yrs | |
| Weichold 2012 (Teacher) | SI & SC | 9 | 45 | 3 | 3.5 | 7.5 | 0.5 | 2 yrs | |
| Weichold 2011 (Peer) | SI & SC | 5 | 9 | 1 | 3.5 | 7.5 | 0.5 | 2 yrs | |
| Wen 2010 | MM | 77 | 571 | 2 | 59 | 449 | 2 | 2 yrs | |
| Clusters are schools unless otherwise stated. |
| (I = information, SI = Social influences, C ‐ Combined social competence and social influences, SC = Social competence, MM = Multi‐modal) |
Appendix 4. Raw data group 2 studies (included in analysis)
| Study ID | Intervention category | Intervention arm | Control arm | OR | Growth rate (SE) | Follow‐up period | ||||
| Baseline smoking measure | Follow‐up smoking measure | Cluster No. | Baseline measure | Follow‐up unit of measure | Cluster No. | |||||
| One year or less follow‐up | ||||||||||
| Sun 2008 (Cognitive) | I | 19.92% cigarette use in the last 30 days 9 (using scale where 0 = none to 7 = 100+) | 6 | 13.29% cigarette use in the last 30 days 9 (using scale where 0 = none to 7 = 100+) | 3 | 1.35 (0.93,195) (adj) | 1yr | |||
| Forman 1990 (SI) | SC | 2.90 (1.49) mean (SD) Freq Cig. Use (1= never to 5 = everyday) | 3.02 (1.48) mean (SD) Freq Cig. Use (1= never to 5 = everyday) | 10 | 2.83 (1.65) mean (SD) Freq Cig. Use (1= never to 5 = everyday) | 2.93 (1.53) mean (SD) Freq Cig. Use (1= never to 5 = everyday) | 3.33 | 1 yr | ||
| Forman 1990 (SI ‐ NP) | SC | 2.84 (1.71) mean (SD) Freq Cig. Use (1= never to 5 = everyday) | 2.81 (1.64) mean (SD) Freq Cig. Use (1= never to 5 = everyday) | 6 | 2.83 (1.65) mean (SD) Freq Cig. Use (1= never to 5 = everyday) | 2.93 (1.53) mean (SD) Freq Cig. Use (1= never to 5 = everyday) | 3.33 | 1 yr | ||
| Forman 1990 (SI ‐ P) | SC | 2.81 (1.44) mean (SD) Freq Cig. Use (1= never to 5 = everyday) | 2.95 (1.47) mean (SD) Freq Cig. Use (1= never to 5 = everyday) | 4 | 2.83 (1.65) mean (SD) Freq Cig. Use (1= never to 5 = everyday) | 2.93 (1.53) mean (SD) Freq Cig. Use (1= never to 5 = everyday) | 3.33 | 1 yr | ||
| Clark 2010 | SI | 1.97 (2.48) mean (SD) Average no. of days smoked in the last 30 days (scale from 0 = 0 to 10 = >38) | 2.31 (2.67) mean (SD) Average no. of days smoked in the last 30 days (scale from 0 = 0 to 10 = >38) | 7 | 2.16 (2.58) mean (SD) Average no. of days smoked in the last 30 days (scale from 0 = 0 to 10 = >38) | 2.5 (2.70) mean (SD) Average no. of days smoked in the last 30 days (scale from 0 = 0 to 10 = >38) | 7 | 1 yr | ||
| Kaufman 1994 | SI | 11.63 (3.98) mean (SD) for cigarette use (scale from 6 ‐ 32, higher = more use). Pretest smoking as covariate. | 2 | 10.99 (2.51) mean (SD) for cigarette use (scale from 6 ‐ 32, higher = more use) Pretest smoking as covariate. | 1 | 6 mths | ||||
| Reddy 2002 (School + F) | SI | 0.034 (0.0219, 0.0525) Mean (CI) ever tried (from SAS PROC Mixed and SAS Glimmix Macro). Based on yes/no to ever use | 0.0366 (0.0264, 0.0504) Mean (CI) ever tried (from SAS PROC Mixed and SAS Glimmix Macro). Based on yes/no to ever use | 10 | 0.0391 (0.251, 0.0605) Mean (CI) ever tried (from SAS PROC Mixed and SAS Glimmix Macro). Based on yes/no to ever use | 0.0937 (0.0728, 0.1198) Mean (CI) ever tried (from SAS PROC Mixed and SAS Glimmix Macro). Based on yes/no to ever use | 5 | 1 yr | ||
| Reddy 2002 (School only) | SI | 0.0416 (000269, 0.0637) Mean (CI) ever tried (from SAS PROC Mixed and SAS Glimmix Macro). Based on yes/no to ever use | 0.0571 (0.0422, 0.0768) Mean (CI) ever tried (from SAS PROC Mixed and SAS Glimmix Macro). Based on yes/no to ever use | 10 | 0.0391 (0.251, 0.0605) Mean (CI) ever tried (from SAS PROC Mixed and SAS Glimmix Macro). Based on yes/no to ever use | 0.0937 (0.0728, 0.1198) Mean (CI) ever tried (from SAS PROC Mixed and SAS Glimmix Macro). Based on yes/no to ever use | 5 | 1 yr | ||
| Severson 1991(high, M) | SI | 9.4 (48.6) mean cigarettes per month (SD) | 24.9 (120.3) mean cigarettes per month (SD) | 13 total for all four arms | 3.2 (26.7) mean cigarettes per month (SD) | 15.9 (83.3 mean cigarettes per month (SD) | 13 total for all four arms | 1 yr | ||
| Severson 1991 (High, F) | SI | 5.7 (35.8) mean cigarettes per month (SD) | 22.7 (97.1) mean cigarettes per month (SD) | 13 total for all four arms | 13.9 (72.6) mean cigarettes per month (SD) | 17.9 (83.4) mean cigarettes per month (SD) | 13 total for all four arms | 1 yr | ||
| Severson 1991 (Middle, M) | SI | 0.7 (5.4) mean cigarettes per month (SD) | 9.1 (47.3) mean cigarettes per month (SD) | 13 total for all four arms | 1.3 (6.9) mean cigarettes per month (SD) | 3.4 (23.1) mean cigarettes per month (SD) | 13 total for all four arms | 1 yr | ||
| Severson 1991 (Middle, F) | SI | 1.9 (18.2) mean cigarettes per month (SD) | 13.6 (59.0) mean cigarettes per month (SD) | 13 total for all four arms | 1.1 (5.7) mean cigarettes per month (SD) | 12.4 (59.0) mean cigarettes per month (SD) | 13 total for all four arms | 1 yr | ||
| Shope 1996 | SI | 0.12 (0.61) mean (SD) cigarette use | 0.27 (0.87) mean (SD) cigarette use |
Estimate 25 classes total | 0.12 (0.51) mean (SD) cigarette use | 0.91 (1.73) mean (SD) cigarette use | Estimate 25 classes total | 1 yr | ||
| Sun 2008 (Combined) | SI | 12.24% cigarette use in the last 30 days 9 (using scale where 0 = none to 7 = 100+) | 6 | 13.29% cigarette use in the last 30 days 9 (using scale where 0 = none to 7 = 100+) | 3 | 0.91 (0.6 ‐ 1.37) (adj) | 1 yr | |||
| Sussman 2007 | C | 30 day smoking prevalence | 6 | 6 | 0.5 (0.34 ‐ 0.73) (adj) | 1 yr | ||||
| Longest Follow‐up (over 1 year) | ||||||||||
| Spoth 2001 (ISFP) | SC | slope growth curve | minus 0.0610 (0.02) | 4 yr | ||||||
| Spoth 2001 (PDFY) | SC | slope growth curve | minus 0.01 (0.02) | 4 yr | ||||||
| Flay 1985 | SI | Measure = never‐smoker, tried once, quitted, experimenter, regular | 11 | 11 | 1.22 (0.83,1.80) | 6 yr | ||||
| Perry 2003 (Dare boys) | SI | 0.28 (0.05) growth rate (mean difference, SEM) | 8 | 0.31 (0.05) growth rate (mean difference, SEM) | 8 | 2.5 yrs | ||||
| Perry 2003 (Dare girls) | SI | 0.25 (0.07) growth rate (mean difference, SEM) | 8 | 0.28 (0.07) growth rate (mean difference, SEM) | 8 | 2.5 yrs | ||||
| Perry 2009 | SI | 0.46 (‐0.19, 1.11) Linear rate of change (CI) | 16 | 1.37 (0.72, 2.02) Linear rate of change (CI) | 16 | 2 yrs | ||||
| St Pierre 2005 (Adult) | SI | 16 | 8 | 0.186 (0.255) logistic coefficent for the interaction of treatment with pre‐post contrast (SE) | 3 yrs | |||||
| St Pierre 2005 (Teen) | SI | 16 | 8 | 0.069 (0.253) logistic coefficent for the interaction of treatment with pre‐post contrast (SE) | 3 yrs | |||||
| Brown 2005 | C | minus 0.153 (0.105) | >1yr | |||||||
| Hecht 2003 | C | slope growth curves. Use model | minus 0.016 (0.011) | 14 mths | ||||||
| Perry 2003 (Dare+ boys) | MM | 0.18 (0.05) growth rate (mean difference, SEM) | 8 | 0.31 (0.05) growth rate (mean difference, SEM) | 8 | 2.5 yrs | ||||
| Perry 2003 (Dare+ girls) | MM | 0.22 (0.07) growth rate (mean difference, SEM) | 8 | 0.28 (0.07) growth rate (mean difference, SEM) | 8 | 2.5 yrs | ||||
| Clusters are schools unless otherwise stated. |
| (I = information, SI = Social influences, C ‐ Combined social competence and social influences, SC = Social competence, MM = Multi‐modal) |
Appendix 5. Raw data group 3 studies (included in analysis)
| Study ID | Intervention category | Intervention arm | Control arm | Follow‐up period | ||||
| Baseline prevalence | Follow‐up prevalence | Cluster No. | Baseline prevalence | Follow‐up prevalence | Cluster No. | |||
| One year or less follow‐up | ||||||||
| Rabinowitz 1974 | I | 27% % smokers, occasional to > pack/day use |
16% % smokers, occasional to > pack/day use |
18 classes in 6 schools total | 25% % smokers, occasional to > pack/day use |
26% % smokers, occasional to > pack/day use |
18 classes in 6 schools total | 6 mths |
| Campbell 2008 | SI | 5% % past week smoking |
12.49% (10.22 ‐ 14.76) % weekly smokers (CI). At least a cigarette in last 7 days |
30 | 7% % past week smoking |
15.13% (12.75 – 17.50) % weekly smokers (CI). At least a cigarette in last 7 days |
29 | 1 yr |
| Dijkstra 1999 (DM + no B) | SI | 13.5% smoker (occasional, weekly & daily) |
21.30% smoker (occasional, weekly & daily) |
8 | 8% smoker (occasional, weekly & daily) |
19.70% smoker (occasional, weekly & daily) |
5 | 1 yr |
| Dijkstra 1999 (DM + B) | SI | 13.5% smoker (occasional, weekly & daily) |
21.20% smoker (occasional, weekly & daily) |
8 | 8% smoker (occasional, weekly & daily) |
19.70% smoker (occasional, weekly & daily) |
5 | 1 yr |
| Dijkstra 1999 (SI + no B) | SI | 7.5% smoker (occasional, weekly & daily) |
19.40% smoker (occasional, weekly & daily) |
8 | 8% smoker (occasional, weekly & daily) |
19.70% smoker (occasional, weekly & daily) |
5 | 1 yr |
| Dijkstra 1999 (SI + B) | SI | 7.5% daily) |
11.2% smoker (occasional, weekly & daily) |
8 | 8% smoker (occasional, weekly & daily) |
19.70% smoker (occasional, weekly & daily) |
5 | 1 yr |
| Elder 1993 | SI | 5.7% past month prevalence of smoking and smokeless tobacco. Any use. |
10.2% past month prevalence of smoking and smokeless tobacco. Any use. |
11 | 6.4% past month prevalence of smoking and smokeless tobacco. Any use. |
11.40% past month prevalence of smoking and smokeless tobacco. Any use. |
11 | 1 yr |
| Gindre 1995 | SI | 1.3% % smokers from Q:Do you smoke? n= 47/3651 |
1.0% % smokers from Q:Do you smoke? n= 37/3651 |
3 groups of secondary schools and linked feeders | 1.5% % smokers from Q:Do you smoke? n= 48/3183 |
2.10% % smokers from Q:Do you smoke? n= 48/3183 |
1 group of secondary schools and linked feeders | 1 yr |
| Hedman 2010 (Lecture) | SI | 4% % smokers based on question Do you smoke y/n |
5% % smokers based on question Do you smoke y/n |
17 dental practices total | 8% % smokers based on question Do you smoke y/n |
7% % smokers based on question Do you smoke y/n |
17 dental practices total | 8 mths |
| Hedman 2010 (Interview) | SI | 4% % smokers based on question Do you smoke y/n |
4% % smokers based on question Do you smoke y/n |
17 dental practices total | 8% % smokers based on question Do you smoke y/n |
7% % smokers based on question Do you smoke y/n |
17 dental practices total | 8 mths |
| Laniado‐Laborín 1993 | SI | 38.3% smoking prevalence in the last 12 months |
8.10% smoking prevalence in the last 12 months |
6 classes from 6 schools total | 23.3% smoking prevalence in the last 12 months |
20.0% smoking prevalence in the last 12 months |
6 classes from 6 schools total | 10 mths |
| Lloyd 1983 | SI | 10.4% smokers, last four weeks | 18.7% smokers, last four weeks |
44 | 9.10% smokers, last four weeks | 15.70% smokers, last four weeks | 44 | 1 yr |
| Lotrean 2010 | SI | 7.5% smoker (at least once per week) |
12.00% smoker (at least once per week) |
10 | 8.0% smoker (at least once per week) |
17.5% smoker (at least once per week) |
10.00% | 6 mths |
| McCambridge 2011 | SI | 32% % smokers (use over last month) |
31% % smokers (use over last month) |
6 | 24% % smokers (use over last month) |
25% % smokers (use over last month) |
6 | 1 yr |
| Noland 1998 | SI | 51.1 (3.3) mean % ever use (mean adjusted for involvement in tobacco production) |
68.7 (1.8) mean % ever use (mean adjusted for involvement in tobacco production) |
10 | 51.4 (2.3) mean % ever use (mean adjusted for involvement in tobacco production) |
68.2 (1.9) mean % ever use (mean adjusted for involvement in tobacco production) |
9 | 1 yr |
| Perry 2009 | SI | 3.9 (2.7 ‐ 5.1) % any tobacco use (CI). SAS and PROC MIXED regression models |
2.2 (1.6 ‐ 2.8) % any tobacco use (CI). SAS and PROC MIXED regression models |
16 | 3.6 (2.4 ‐ 4.8)) % any tobacco use (CI). SAS and PROC MIXED regression models |
2.2 (1.6 ‐ 2.8) % any tobacco use (CI). SAS and PROC MIXED regression models |
16 | 1 yr |
| Ringwalt 2009a | SI | 13.8% lifetime % use yes/no | 23.40% lifetime % use yes/no | 17 | 10.7% lifetime % use yes/no | 18.60% lifetime % use yes/no | 17 | 1 yr |
| Werch 2005 | SI | 0.38 (0.08) mean (SE) 30 day cigarette use (scale from 1‐2 days to 30 days) |
0.36 (0.09) mean (SE) 30 day cigarette use (scale from 1‐2 days to 30 days) |
No clusters | 0.56 (0.08) mean (SE) 30 day cigarette use (scale from 1‐2 days to 30 days) |
0.77 (0.09) mean (SE) 30 day cigarette use (scale from 1‐2 days to 30 days) |
No clusters | 1 yr |
| Botvin 2001 | C | 1.36 (1.05) mean (SE) smoking freq, 1 = never to 9 = > 1 per day |
1.73 (0.04) mean (SE) adjusted for gender, race, % program completed, free lunch, baseline use |
16 | 1.32 (0.97) mean (SE) smoking freq, 1 = never to 9 = > 1 per day |
1.94 (0.05) mean (SE) adjusted for gender, race, % program completed, free lunch, baseline use |
13 | 1 yr |
| Sussman 1995 TND1 CHS C | SI & SC | 56.5% % smokers (any use in last 30 days) |
51.7% % smokers (any use in last 30 days) |
7 | 56.5% % smokers (any use in last 30 days) |
48.6% % smokers (any use in last 30 days) |
3.5 | 1 yr |
| Sussman 1995 TND1 CHS SAC | SI & SC | 60.0% % smokers (any use in last 30 days) |
55.70% % smokers (any use in last 30 days) |
7 | 56.5% % smokers (any use in last 30 days) |
48.6% % smokers (any use in last 30 days) |
3.5 | 1 yr |
| Longest Follow‐up (over 1 year) | ||||||||
| Campbell 2008 | SI | 5% % past week smoking |
18.95% (16.50 ‐ 21.40) % weekly smokers (CI). At least a cigarette in last 7 days |
30 | 7% % past week smoking |
21.74% (19.37 ‐ 4.12) % weekly smokers (CI). At least a cigarette in last 7 days |
29 | 2 yrs |
| Chatrou 1999 | SI | 7.4% % smoker (at least one cigarette per week & experimenters) |
28.40% % smoker (at least one cigarette per week & experimenters) |
13 classes | 11% % smoker (at least one cigarette per week & experimenters) |
34.70% % smoker (at least one cigarette per week & experimenters) |
20 classes | 18 mths |
| Dijkstra 1999 (DM + no B) | SI | 13.5% daily) |
23.90% smoker (occasional, weekly & daily) |
8 | 8% smoker (occasional, weekly & daily) |
21.30% smoker (occasional, weekly & daily) |
5 | 18 mths |
| Dijkstra 1999 (DM + B) | SI | 13.5% daily) |
20.50% smoker (occasional, weekly & daily) |
8 | 8% smoker (occasional, weekly & daily) |
21.30% aily) |
5 | 18 mths |
| Dijkstra 1999 (SI + no B) | SI | 7.5% smoker (occasional, weekly & daily) |
21.20% smoker (occasional, weekly & daily) |
8 | 8% smoker (occasional, weekly & daily) |
21.30% smoker (occasional, weekly & daily) |
5 | 18 mths |
| Dijkstra 1999 (SI + B) | SI | 7.5% smoker (occasional, weekly & daily) |
15.00% smoker (occasional, weekly & daily) |
8 | 8% smoker (occasional, weekly & daily) |
21.30% smoker (occasional, weekly & daily) |
5 | 18 mths |
| Elder 1993 | SI | 5.7% past month prevalence of smoking and smokeless tobacco. Any use. |
14.2% past month prevalence of smoking and smokeless tobacco. Any use. |
11 | 6.4% past month prevalence of smoking and smokeless tobacco. Any use. |
22.50% past month prevalence of smoking and smokeless tobacco. Any use. |
11 | 3 yrs |
| Murray 1992 (MSPP) | SI | 1.78% weekly smoking prevalence |
1.78% weekly smoking prevalence |
18 | 0.73% weekly smoking prevalence |
10.60% weekly smoking prevalence |
23 | 3yrs |
| Murray 1992 (SFG) | SI | 1.85% weekly smoking prevalence |
13% weekly smoking prevalence |
20 | 0.73% weekly smoking prevalence |
10.60% weekly smoking prevalence |
23 | 3yrs |
| Murray 1992 (MDEG) | SI | 1.70% weekly smoking prevalence |
11.60% weekly smoking prevalence |
20 | 0.73% weekly smoking prevalence |
10.60% weekly smoking prevalence |
23 | 3yrs |
| Noland 1998 | SI | 51.1 (3.3) mean % ever use (mean adjusted for involvement in tobacco production) |
72.2 (1.7) mean % ever use (mean adjusted for involvement in tobacco production) |
10 | 51.4 (2.3) mean % ever use (mean adjusted for involvement in tobacco production) |
77.00 (1.8) mean % ever use (mean adjusted for involvement in tobacco production) |
9 | 2 yr |
| Ringwalt 2009a | SI | 13.8% lifetime % use yes/no | 28.90% lifetime % use yes/no | 17 | 10.7% lifetime % use yes/no | 24% lifetime % use yes/no | 17 | 3 yrs |
| Scholz 2000 (G, male) | SI | 95.6% % never‐smokers |
84.40% % never‐smokers |
8 | 93.8% % never‐smokers |
73.60% % never‐smokers |
7 | 2 Yrs |
| Scholz 2000 (G, female) | SI | 94.90% % never‐smokers |
74.90% % never‐smokers |
8 | 93.20% % never‐smokers |
66.90% % never‐smokers |
7 | 2 Yrs |
| Scholz 2000 (R, male) | SI | 91.50% % never‐smokers |
78.30% % never‐smokers |
7 | 85.70% % never‐smokers |
66.30% % never‐smokers |
6 | 2 Yrs |
| Scholz 2000 (R, female) | SI | 89.70% % never‐smokers |
74.80% % never‐smokers |
7 | 90.60% % never‐smokers |
73.40% % never‐smokers |
6 | 2 Yrs |
| Botvin 1990a (Workshop) | C | 1.10 (0.02) mean (SE) current smoking (10 point scale) |
1.46 (0.04) covariate adjusted mean (SE). Adjusted for pre‐test | 18 | 1.10 (0.01) mean (SE) current smoking (10 point scale) |
1.63 (0.03) covariate adjusted mean (SE). Adjusted for pre‐test | 10.5 | 3yrs |
| Botvin 1990a (Video) | C | 1.09 (0.01) mean (SE) current smoking (10 point scale) |
1.50 (0.04) covariate adjusted mean (SE). Adjusted for pre‐test | 17 | 1.10 (0.01) mean (SE) current smoking (10 point scale) |
1.63 (0.03) covariate adjusted mean (SE). Adjusted for pre‐test | 10.5 | 3yrs |
| Jøsendal 1998 (P + T) | C | 6.8% % smoker, any frequency |
31.5% % smoker, any frequency |
25 | 7.20% % smoker, any frequency |
41.70% % smoker, any frequency |
8.33 | 2.5 yrs |
| Jøsendal 1998 (P) | C | 8.4% % smoker, any frequency |
31.70% % smoker, any frequency |
25 | 7.20% % smoker, any frequency |
41.70% % smoker, any frequency |
8.33 | 2.5 yrs |
| Jøsendal 1998 (T) | C | 10.10% % smoker, any frequency |
37.30% % smoker, any frequency |
25 | 7.20% % smoker, any frequency |
41.70% % smoker, any frequency |
8.33 | 2.5 yrs |
| Sloboda 2009 | C | 6.7% % 30 day tobacco use |
28.80% % 30 day tobacco use |
41 | 6.4% % 30 day tobacco use |
19.7% % 30 day tobacco use |
45 | 4 yrs |
| Spoth 2002 (LST + SFP) | C | 0.583 (0.033) adjusted mean for cigarette initiation (SE) |
12 | 0.669 (0.035) adjusted mean for cigarette initiation (SE) |
12 | 5.5 yrs | ||
| Sussman 1995 TND1 CHS C | C | 56.5% % smokers (any use in last 30 days) |
76.40% % smokers (any use in last 30 days) |
7 | 56.5% % smokers (any use in last 30 days) |
68.90% % smokers (any use in last 30 days) |
3.5 | 5 yrs |
| Sussman 1995 TND1 CHS SAC | C | 60.0% % smokers (any use in last 30 days) |
68.30% % smokers (any use in last 30 days) |
7 | 56.5% % smokers (any use in last 30 days) |
68.90% % smokers (any use in last 30 days) |
3.5 | 5 yrs |
| Perry 1996 (cigarettes) | MM | 6.9% (4.9,8.9) mean % cigarette use (CI) more > 1‐2 occasions (occasionally or regularly) |
24.8% (20.2, 29.5) mean % cigarette use (CI) more > 1‐2 occasions (occasionally or regularly) |
10 school districts | 4.7% (2.6,6.7) mean % cigarette use (CI) more > 1‐2 occasions (occasionally or regularly) |
30.7% (26.0, 35.4) mean % cigarette use (CI) more > 1‐2 occasions (occasionally or regularly) |
10 school districts | 2.5 yrs |
| Schofield 2003 | MM | 3.9% % past week smoking |
17.50% % past week smoking |
12 | 4.10% % past week smoking |
20.50% % past week smoking |
10 | 2 yrs |
| Clusters are schools unless otherwise stated. |
| (I = information, SI = Social influences, C ‐ Combined social competence and social influences, SC = Social competence, MM = Multi‐modal) |
Appendix 6. Table to identify Group 1, 2 and 3 studies by analysis group
Appendix 7. Group 1 studies (included in analysis) by country
Note some studies appear more than once because the intervention took place in two or more countries.
Appendix 8. Group 2 studies (included in analysis) by country
Appendix 9. Group 3 studies (included in analysis) by country
| Country |
Number of studies |
Study name |
| Australia | 2 | Lloyd 1983; Schofield 2003; |
| France | 1 | Gindre 1995; |
| Germany | 1 | Scholz 2000 (G, female); Scholz 2000 (G, male); Scholz 2000 (R, female); Scholz 2000 (R, male) |
| India | 1 | Perry 2009 |
| Mexico | 1 | Laniado‐Laborín 1993; |
| Netherlands | 2 | Chatrou 1999; Dijkstra 1999 (DM + B); Dijkstra 1999 (DM + no B); Dijkstra 1999 (SI + B); Dijkstra 1999 (SI + no B); |
| Norway | 1 | Jøsendal 1998 (P); Jøsendal 1998 (P + T); Jøsendal 1998 (T); |
| Romania | 1 | Lotrean 2010; |
| Sweden | 1 | Hedman 2010 (Interview); Hedman 2010 (Lecture) |
| UK | 2 | Campbell 2008; McCambridge 2011; |
| USA | 12 | Botvin 1990a (Video); Botvin 1990a (Workshop); Botvin 2001; Elder 1993; Murray 1992 (MDEG); Murray 1992 (MSPP); Murray 1992 (SFG); Noland 1998; Perry 1996; Rabinowitz 1974; Ringwalt 2009a; Sloboda 2009; Spoth 2002 (LST); Spoth 2002 (LST + SFP); Sussman 1995 TND1 CHS C; Sussman 1995 TND1 CHS SAC; Werch 2005 |
Data and analyses
Comparison 1. All curricula versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Group 1: Pure Prevention cohort (adjusted) ‐ 1 year or less | 40 | 32234 | Odds Ratio (Fixed, 95% CI) | 0.94 [0.85, 1.05] |
| 1.1 Information giving curricula versus control | 1 | 100 | Odds Ratio (Fixed, 95% CI) | 0.12 [0.00, 14.87] |
| 1.2 Social influences curricula versus control | 25 | 20467 | Odds Ratio (Fixed, 95% CI) | 1.00 [0.88, 1.13] |
| 1.3 Combined social competence and social influences curricula versus control | 7 | 5370 | Odds Ratio (Fixed, 95% CI) | 0.49 [0.28, 0.87] |
| 1.4 Multimodal programmes versus control | 5 | 6000 | Odds Ratio (Fixed, 95% CI) | 0.89 [0.73, 1.08] |
| 1.5 Other interventions | 2 | 297 | Odds Ratio (Fixed, 95% CI) | 2.49 [0.10, 61.80] |
| 2 Group 1: Pure Prevention cohort (adjusted) ‐ longest follow‐up | 73 | Odds Ratio (Random, 95% CI) | 0.88 [0.82, 0.96] | |
| 2.1 Information giving curricula versus control | 1 | Odds Ratio (Random, 95% CI) | 0.12 [0.00, 14.87] | |
| 2.2 Social competence curricula versus control | 7 | Odds Ratio (Random, 95% CI) | 0.52 [0.30, 0.88] | |
| 2.3 Social influences curricula versus control | 42 | Odds Ratio (Random, 95% CI) | 0.92 [0.84, 1.01] | |
| 2.4 Combined social competence and social influences versus control | 10 | Odds Ratio (Random, 95% CI) | 0.50 [0.28, 0.87] | |
| 2.5 Multimodal programmes versus control | 7 | Odds Ratio (Random, 95% CI) | 0.95 [0.64, 1.43] | |
| 2.6 Other interventions | 6 | Odds Ratio (Random, 95% CI) | 0.91 [0.50, 1.66] | |
| 3 Group 2: Change in Smoking Behaviour over time ‐ 1 year or less | 15 | 13137 | Std. Mean Difference (Fixed, 95% CI) | 0.04 [0.02, 0.06] |
| 3.1 Information giving curricula versus control | 1 | 1072 | Std. Mean Difference (Fixed, 95% CI) | 0.17 [‐0.04, 0.37] |
| 3.2 Social competence curricula versus control | 3 | 279 | Std. Mean Difference (Fixed, 95% CI) | 0.02 [‐1.19, 1.24] |
| 3.3 Social influences curricula versus control | 10 | 10689 | Std. Mean Difference (Fixed, 95% CI) | 0.04 [0.03, 0.06] |
| 3.4 Combined social competence and social influences curricula versus control | 1 | 1097 | Std. Mean Difference (Fixed, 95% CI) | ‐0.38 [‐0.59, ‐0.17] |
| 4 Group 2: Change in Smoking Behaviour over time ‐ longest follow‐up | 27 | Std. Mean Difference (Fixed, 95% CI) | 0.01 [‐0.00, 0.02] | |
| 4.1 Information giving curricula versus control | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.17 [‐0.04, 0.37] | |
| 4.2 Social competence versus control | 5 | Std. Mean Difference (Fixed, 95% CI) | ‐0.04 [‐0.06, ‐0.01] | |
| 4.3 Social influences curricula versus control | 16 | Std. Mean Difference (Fixed, 95% CI) | 0.05 [0.03, 0.06] | |
| 4.4 Combined social competence and social influences curricula versus control | 3 | Std. Mean Difference (Fixed, 95% CI) | ‐0.02 [‐0.04, 0.00] | |
| 4.5 Multimodal programmes versus control | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.11 [‐0.01, 0.22] | |
| 5 Group 3: Point Prevalence of Smoking ‐ 1 year or less | 21 | Std. Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 5.1 Information giving curricula versus control | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Social influences curricula versus control | 15 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Combined social competence and social influence curricula versus control | 3 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.4 Other interventions | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Group 3: Point Prevalence of Smoking ‐ longest follow‐up | 39 | Odds Ratio (Fixed, 95% CI) | Totals not selected | |
| 6.1 Information giving curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Social competence | 1 | Odds Ratio (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Social influences curricula versus control | 23 | Odds Ratio (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.4 Combined social competence and social influence curricula versus control | 10 | Odds Ratio (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.5 Multimodal curricula versus control | 2 | Odds Ratio (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.6 Other interventions | 2 | Odds Ratio (Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2. Group 1: Sensitivity analyses (adjusted).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Low attrition ‐ 1 year or less | 13 | Odds Ratio (Fixed, 95% CI) | 0.93 [0.75, 1.17] | |
| 1.1 Information curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.12 [0.00, 14.87] | |
| 1.2 Social influences curricula versus control | 10 | Odds Ratio (Fixed, 95% CI) | 1.00 [0.79, 1.27] | |
| 1.3 Combined social competence and social influences curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.55 [0.28, 1.09] | |
| 1.4 Multimodal curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.73 [0.00, 119016.25] | |
| 2 Low attrition ‐ longest follow‐up | 30 | Odds Ratio (Fixed, 95% CI) | 0.89 [0.78, 1.02] | |
| 2.1 Information curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.12 [0.00, 14.87] | |
| 2.2 Social competence curricula versus control | 5 | Odds Ratio (Fixed, 95% CI) | 0.57 [0.32, 1.02] | |
| 2.3 Social influences curricula versus control | 19 | Odds Ratio (Fixed, 95% CI) | 0.94 [0.81, 1.08] | |
| 2.4 Combined social competence and social influences | 3 | Odds Ratio (Fixed, 95% CI) | 0.55 [0.28, 1.09] | |
| 2.5 Multimodal curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 1.03 [0.00, 433.58] | |
| 2.6 Other interventions | 1 | Odds Ratio (Fixed, 95% CI) | 0.86 [0.44, 1.69] | |
| 3 Low & unclear attrition ‐ 1 year or less | 31 | Odds Ratio (Fixed, 95% CI) | 0.92 [0.79, 1.07] | |
| 3.1 Information curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.12 [0.00, 14.87] | |
| 3.2 Social influences curricula versus control | 20 | Odds Ratio (Fixed, 95% CI) | 0.96 [0.82, 1.13] | |
| 3.3 Combined social competence and social influences versus control | 6 | Odds Ratio (Fixed, 95% CI) | 0.50 [0.28, 0.89] | |
| 3.4 Multimodal curricula versus control | 2 | Odds Ratio (Fixed, 95% CI) | 0.72 [0.03, 19.98] | |
| 3.5 Other interventions | 2 | Odds Ratio (Fixed, 95% CI) | 2.49 [0.10, 61.80] | |
| 4 Low & unclear attrition‐ longest follow‐up | 58 | Odds Ratio (Fixed, 95% CI) | 0.90 [0.82, 1.00] | |
| 4.1 Information curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.12 [0.00, 14.87] | |
| 4.2 Social competence curricula versus control | 5 | Odds Ratio (Fixed, 95% CI) | 0.57 [0.32, 1.02] | |
| 4.3 Social influences curricula versus control | 35 | Odds Ratio (Fixed, 95% CI) | 0.94 [0.84, 1.04] | |
| 4.4 Combined social competence and social influences | 8 | Odds Ratio (Fixed, 95% CI) | 0.50 [0.28, 0.89] | |
| 4.5 Multimodal curricula versus control | 4 | Odds Ratio (Fixed, 95% CI) | 1.14 [0.21, 6.37] | |
| 4.6 Other interventions | 5 | Odds Ratio (Fixed, 95% CI) | 0.89 [0.47, 1.69] | |
| 5 Low selection bias ‐ 1 year or less | 16 | Odds Ratio (Fixed, 95% CI) | 0.97 [0.80, 1.17] | |
| 5.1 Social influences curricula versus control | 12 | Odds Ratio (Fixed, 95% CI) | 1.02 [0.84, 1.24] | |
| 5.2 Combined social competence and social influences versus control | 2 | Odds Ratio (Fixed, 95% CI) | 0.55 [0.28, 1.10] | |
| 5.3 Multimodal curricula versus control | 2 | Odds Ratio (Fixed, 95% CI) | 0.72 [0.03, 19.98] | |
| 6 Low selection bias ‐ longest follow‐up | 37 | Odds Ratio (Fixed, 95% CI) | 0.90 [0.80, 1.00] | |
| 6.1 Social competence curricula versus control | 5 | Odds Ratio (Fixed, 95% CI) | 0.57 [0.32, 1.03] | |
| 6.2 Social influences curricula versus control | 24 | Odds Ratio (Fixed, 95% CI) | 0.92 [0.82, 1.03] | |
| 6.3 Combined social competence and social influences versus control | 2 | Odds Ratio (Fixed, 95% CI) | 0.55 [0.28, 1.10] | |
| 6.4 Multimodal curricula versus control | 4 | Odds Ratio (Fixed, 95% CI) | 1.14 [0.21, 6.37] | |
| 6.5 Other interventions | 2 | Odds Ratio (Fixed, 95% CI) | 0.88 [0.47, 1.66] |
2.1. Analysis.

Comparison 2 Group 1: Sensitivity analyses (adjusted), Outcome 1 Low attrition ‐ 1 year or less.
2.2. Analysis.

Comparison 2 Group 1: Sensitivity analyses (adjusted), Outcome 2 Low attrition ‐ longest follow‐up.
2.3. Analysis.

Comparison 2 Group 1: Sensitivity analyses (adjusted), Outcome 3 Low & unclear attrition ‐ 1 year or less.
2.4. Analysis.

Comparison 2 Group 1: Sensitivity analyses (adjusted), Outcome 4 Low & unclear attrition‐ longest follow‐up.
2.5. Analysis.

Comparison 2 Group 1: Sensitivity analyses (adjusted), Outcome 5 Low selection bias ‐ 1 year or less.
2.6. Analysis.

Comparison 2 Group 1: Sensitivity analyses (adjusted), Outcome 6 Low selection bias ‐ longest follow‐up.
Comparison 3. Group 1: Gender analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Female ‐ 1 year or less | 7 | Odds Ratio (Fixed, 95% CI) | 0.69 [0.49, 0.96] | |
| 1.1 Social influences curricula versus control | 4 | Odds Ratio (Fixed, 95% CI) | 0.69 [0.41, 1.14] | |
| 1.2 Combined social competence and social influences curricula versus control | 2 | Odds Ratio (Fixed, 95% CI) | 0.55 [0.28, 1.09] | |
| 1.3 Multimodal curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.82 [0.45, 1.47] | |
| 2 Female ‐ longest follow‐up | 9 | Odds Ratio (Fixed, 95% CI) | 0.82 [0.67, 1.00] | |
| 2.1 Social influences curricula versus control | 6 | Odds Ratio (Fixed, 95% CI) | 0.83 [0.66, 1.04] | |
| 2.2 Combined social competence and social influences versus control | 2 | Odds Ratio (Fixed, 95% CI) | 0.55 [0.28, 1.07] | |
| 2.3 Multimodal curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.99 [0.57, 1.73] | |
| 3 Male ‐ 1 year or less | 6 | Odds Ratio (Fixed, 95% CI) | 0.66 [0.44, 0.98] | |
| 3.1 Social influences curricula versus control | 4 | Odds Ratio (Fixed, 95% CI) | 0.92 [0.56, 1.52] | |
| 3.2 Combined social competence and social influences curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 1.15 [0.04, 37.54] | |
| 3.3 Multimodal curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.32 [0.16, 0.65] | |
| 4 Male ‐ longest follow‐up | 8 | Odds Ratio (Fixed, 95% CI) | 0.96 [0.77, 1.20] | |
| 4.1 Social influences curricula verus control | 6 | Odds Ratio (Fixed, 95% CI) | 0.97 [0.76, 1.23] | |
| 4.2 Combined social competence and social influences curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.77 [0.05, 11.85] | |
| 4.3 Multimodal curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.93 [0.54, 1.58] |
3.2. Analysis.

Comparison 3 Group 1: Gender analysis, Outcome 2 Female ‐ longest follow‐up.
3.4. Analysis.

Comparison 3 Group 1: Gender analysis, Outcome 4 Male ‐ longest follow‐up.
Comparison 4. Group 1: Booster sessions analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 No Booster sessions ‐ 1 year or less | 36 | Odds Ratio (Fixed, 95% CI) | 0.94 [0.85, 1.05] | |
| 1.1 Information curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.12 [0.00, 14.87] | |
| 1.2 Social influences curricula versus control | 23 | Odds Ratio (Fixed, 95% CI) | 0.98 [0.86, 1.11] | |
| 1.3 Combined social competence and social influences curricula versus control | 5 | Odds Ratio (Fixed, 95% CI) | 0.47 [0.14, 1.51] | |
| 1.4 Multimodal curricula versus control | 5 | Odds Ratio (Fixed, 95% CI) | 0.89 [0.73, 1.08] | |
| 1.5 Other interventions | 2 | Odds Ratio (Fixed, 95% CI) | 2.49 [0.10, 61.80] | |
| 2 No Booster sessions ‐ longest follow‐up | 66 | Odds Ratio (Fixed, 95% CI) | 0.90 [0.83, 0.97] | |
| 2.1 Information curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.12 [0.00, 14.87] | |
| 2.2 Social competence curricula versus control | 7 | Odds Ratio (Fixed, 95% CI) | 0.52 [0.30, 0.88] | |
| 2.3 Social influences curricula versus control | 38 | Odds Ratio (Fixed, 95% CI) | 0.93 [0.85, 1.02] | |
| 2.4 Combined social competence and social influences curricula versus control | 7 | Odds Ratio (Fixed, 95% CI) | 0.47 [0.15, 1.43] | |
| 2.5 Multimodal curricula versus control | 7 | Odds Ratio (Fixed, 95% CI) | 0.83 [0.69, 1.01] | |
| 2.6 Other interventions | 6 | Odds Ratio (Fixed, 95% CI) | 0.91 [0.50, 1.66] | |
| 3 Boosters sessions ‐ 1 year or less | 4 | Odds Ratio (Fixed, 95% CI) | 0.70 [0.46, 1.07] | |
| 3.1 Social influences curricula versus control | 2 | Odds Ratio (Fixed, 95% CI) | 0.90 [0.51, 1.56] | |
| 3.2 Combined social competence and social influences curricula versus control | 2 | Odds Ratio (Fixed, 95% CI) | 0.50 [0.26, 0.96] | |
| 4 Booster sessions ‐ longest follow‐up | 7 | Odds Ratio (Fixed, 95% CI) | 0.73 [0.55, 0.98] | |
| 4.1 Social influences curricula versus control | 4 | Odds Ratio (Fixed, 95% CI) | 0.81 [0.58, 1.12] | |
| 4.2 Combined social competence and social influences curricula versus control | 3 | Odds Ratio (Fixed, 95% CI) | 0.51 [0.27, 0.96] |
4.3. Analysis.

Comparison 4 Group 1: Booster sessions analysis, Outcome 3 Boosters sessions ‐ 1 year or less.
Comparison 5. Group 1: Tobacco focus.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Multi foci ‐ 1 year or less | 14 | Odds Ratio (Fixed, 95% CI) | 0.92 [0.74, 1.16] | |
| 1.1 Information curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.12 [0.00, 14.87] | |
| 1.2 Social influences curricula versus control | 9 | Odds Ratio (Fixed, 95% CI) | 0.99 [0.78, 1.27] | |
| 1.3 Combined social competence and social influences curricula versus control | 3 | Odds Ratio (Fixed, 95% CI) | 0.54 [0.28, 1.06] | |
| 1.4 Multimodal curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.72 [0.02, 22.85] | |
| 2 Multi foci ‐ longest follow‐up | 29 | Odds Ratio (Fixed, 95% CI) | 0.88 [0.77, 1.01] | |
| 2.1 Information curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.12 [0.00, 14.87] | |
| 2.2 Social competence curricula versus control | 7 | Odds Ratio (Fixed, 95% CI) | 0.52 [0.30, 0.88] | |
| 2.3 Social influences curricula versus control | 14 | Odds Ratio (Fixed, 95% CI) | 0.94 [0.82, 1.09] | |
| 2.4 Combined social competence and social influences curricula versus control | 6 | Odds Ratio (Fixed, 95% CI) | 0.55 [0.29, 1.04] | |
| 2.5 Multimodal curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.82 [0.03, 25.09] | |
| 3 Tobacco focused ‐ 1 year or less | 26 | Odds Ratio (Fixed, 95% CI) | 0.93 [0.83, 1.04] | |
| 3.1 Social influence curricula versus control | 16 | Odds Ratio (Fixed, 95% CI) | 0.97 [0.84, 1.12] | |
| 3.2 Combined social competence and social influences curricula versus control | 4 | Odds Ratio (Fixed, 95% CI) | 0.37 [0.12, 1.13] | |
| 3.3 Multimodal curricula versus control | 4 | Odds Ratio (Fixed, 95% CI) | 0.89 [0.73, 1.08] | |
| 3.4 Other interventions | 2 | Odds Ratio (Fixed, 95% CI) | 2.49 [0.10, 61.80] | |
| 4 Tobacco focused ‐ longest follow‐up | 42 | Odds Ratio (Fixed, 95% CI) | 0.88 [0.80, 0.97] | |
| 4.1 Social influences curricula versus control | 28 | Odds Ratio (Fixed, 95% CI) | 0.91 [0.81, 1.02] | |
| 4.2 Combined social competence and social influences curricula versus control | 4 | Odds Ratio (Fixed, 95% CI) | 0.37 [0.12, 1.13] | |
| 4.3 Multimodal curricula versus control | 4 | Odds Ratio (Fixed, 95% CI) | 0.83 [0.68, 1.00] | |
| 4.4 Other interventions | 6 | Odds Ratio (Fixed, 95% CI) | 0.91 [0.50, 1.66] |
5.1. Analysis.
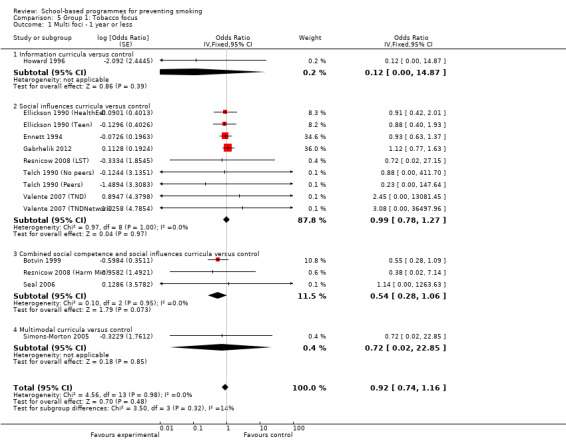
Comparison 5 Group 1: Tobacco focus, Outcome 1 Multi foci ‐ 1 year or less.
5.2. Analysis.

Comparison 5 Group 1: Tobacco focus, Outcome 2 Multi foci ‐ longest follow‐up.
5.3. Analysis.

Comparison 5 Group 1: Tobacco focus, Outcome 3 Tobacco focused ‐ 1 year or less.
Comparison 6. Group 1: Peer‐led analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peer‐led ‐ 1 year or less | 8 | Odds Ratio (Fixed, 95% CI) | 0.91 [0.56, 1.46] | |
| 1.1 Social influences curricula versus control | 7 | Odds Ratio (Fixed, 95% CI) | 0.90 [0.56, 1.47] | |
| 1.2 Combined social competence and social influences curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.97 [0.11, 8.39] | |
| 2 Peer‐led ‐ longest follow‐up | 11 | Odds Ratio (Fixed, 95% CI) | 0.94 [0.61, 1.47] | |
| 2.1 Social influences curricula versus control | 7 | Odds Ratio (Fixed, 95% CI) | 0.93 [0.59, 1.47] | |
| 2.2 Combined social competence and social influences | 2 | Odds Ratio (Fixed, 95% CI) | 0.99 [0.12, 8.00] | |
| 2.3 Multimodal curricula versus control | 2 | Odds Ratio (Fixed, 95% CI) | 1.31 [0.16, 10.73] | |
| 3 Adult‐led ‐ 1 year or less | 29 | Odds Ratio (Fixed, 95% CI) | 0.93 [0.83, 1.03] | |
| 3.1 Information curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.12 [0.00, 14.87] | |
| 3.2 Social influences curricula versus control | 16 | Odds Ratio (Fixed, 95% CI) | 0.98 [0.86, 1.12] | |
| 3.3 Combined social competence and social influences curricula versus control | 5 | Odds Ratio (Fixed, 95% CI) | 0.46 [0.26, 0.84] | |
| 3.4 Multimodal curricula versus control | 5 | Odds Ratio (Fixed, 95% CI) | 0.89 [0.73, 1.08] | |
| 3.5 Other interventions | 2 | Odds Ratio (Fixed, 95% CI) | 2.49 [0.10, 61.80] | |
| 4 Adult‐led ‐ longest follow‐up | 56 | Odds Ratio (Fixed, 95% CI) | 0.88 [0.81, 0.96] | |
| 4.1 Information curricula versus control | 1 | Odds Ratio (Fixed, 95% CI) | 0.12 [0.00, 14.87] | |
| 4.2 Social competence curricula versus control | 7 | Odds Ratio (Fixed, 95% CI) | 0.52 [0.30, 0.88] | |
| 4.3 Social influences curricula versus control | 30 | Odds Ratio (Fixed, 95% CI) | 0.92 [0.84, 1.01] | |
| 4.4 Combined social competence and social influences curricula versus control | 7 | Odds Ratio (Fixed, 95% CI) | 0.47 [0.26, 0.84] | |
| 4.5 Multimodal curricula versus control | 5 | Odds Ratio (Fixed, 95% CI) | 0.83 [0.68, 1.00] | |
| 4.6 Other interventions | 6 | Odds Ratio (Fixed, 95% CI) | 0.91 [0.50, 1.66] |
6.4. Analysis.

Comparison 6 Group 1: Peer‐led analysis, Outcome 4 Adult‐led ‐ longest follow‐up.
Comparison 7. Group 2: Sensitivity analyses.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Low attrition ‐ 1 year or less | 5 | Std. Mean Difference (Fixed, 95% CI) | ‐0.02 [‐3.01, 2.98] | |
| 1.1 Social influences curricula versus control | 5 | Std. Mean Difference (Fixed, 95% CI) | ‐0.02 [‐3.01, 2.98] | |
| 2 Low attrition ‐ > 1 year, longest follow‐up | 15 | Std. Mean Difference (Fixed, 95% CI) | ‐0.02 [‐0.05, 0.00] | |
| 2.1 Social competence curricula versus control | 2 | Std. Mean Difference (Fixed, 95% CI) | ‐0.04 [‐0.06, ‐0.01] | |
| 2.2 Social influences curricula versus control | 10 | Std. Mean Difference (Fixed, 95% CI) | 0.05 [‐0.06, 0.16] | |
| 2.3 Combined social competence and social influences curricula versus control | 1 | Std. Mean Difference (Fixed, 95% CI) | ‐0.15 [‐0.36, 0.05] | |
| 2.4 Multimodal curricula versus control | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.11 [‐0.01, 0.22] | |
| 3 Low & unclear attrition ‐ 1 year or less | 13 | Std. Mean Difference (Fixed, 95% CI) | 0.05 [0.03, 0.06] | |
| 3.1 Information curricula versus control | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.17 [‐0.04, 0.37] | |
| 3.2 Social competence curricula versus control | 3 | Std. Mean Difference (Fixed, 95% CI) | 0.02 [‐1.19, 1.24] | |
| 3.3 Social influences curricula versus control | 9 | Std. Mean Difference (Fixed, 95% CI) | 0.04 [0.03, 0.06] | |
| 3.4 Low & unclear attrition ‐ 1 year or less | 0 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Low & unclear attrition ‐ > 1 year, longest follow‐up | 25 | Std. Mean Difference (Fixed, 95% CI) | 0.01 [‐0.00, 0.02] | |
| 4.1 Information | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.17 [‐0.04, 0.37] | |
| 4.2 Social competence curricula versus control | 5 | Std. Mean Difference (Fixed, 95% CI) | ‐0.04 [‐0.06, ‐0.01] | |
| 4.3 Social influences curricula versus control | 15 | Std. Mean Difference (Fixed, 95% CI) | 0.05 [0.03, 0.06] | |
| 4.4 Combined social competence and social influences curricula versus control | 2 | Std. Mean Difference (Fixed, 95% CI) | ‐0.02 [‐0.04, 0.00] | |
| 4.5 Multimodal curricula versus control | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.11 [‐0.01, 0.22] | |
| 5 Low selection bias ‐ 1 year or less | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.05 [0.03, 0.06] | |
| 5.1 Social influences curricula versus control | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.05 [0.03, 0.06] | |
| 6 Low selection bias ‐ > 1 year, longest follow‐up | 11 | Std. Mean Difference (Fixed, 95% CI) | 0.02 [0.01, 0.04] | |
| 6.1 Social competence curricula versus control | 2 | Std. Mean Difference (Fixed, 95% CI) | ‐0.04 [‐0.06, ‐0.01] | |
| 6.2 Social influences curricula versus control | 7 | Std. Mean Difference (Fixed, 95% CI) | 0.05 [0.03, 0.06] | |
| 6.3 Multimodal curricula versus control | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.11 [‐0.01, 0.22] |
7.1. Analysis.

Comparison 7 Group 2: Sensitivity analyses, Outcome 1 Low attrition ‐ 1 year or less.
7.2. Analysis.

Comparison 7 Group 2: Sensitivity analyses, Outcome 2 Low attrition ‐ > 1 year, longest follow‐up.
7.3. Analysis.

Comparison 7 Group 2: Sensitivity analyses, Outcome 3 Low & unclear attrition ‐ 1 year or less.
7.4. Analysis.

Comparison 7 Group 2: Sensitivity analyses, Outcome 4 Low & unclear attrition ‐ > 1 year, longest follow‐up.
7.5. Analysis.

Comparison 7 Group 2: Sensitivity analyses, Outcome 5 Low selection bias ‐ 1 year or less.
7.6. Analysis.

Comparison 7 Group 2: Sensitivity analyses, Outcome 6 Low selection bias ‐ > 1 year, longest follow‐up.
Comparison 8. Group 3: Sensitivity analyses.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Low attrition ‐ 1 year or less | 14 | Std. Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 1.1 Information curricula versus control | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Social influences curricula versus control | 10 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Combined social competence and social influences curricula versus control | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Other interventions | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Low attrition ‐ > 1 year, longest follow‐up | 20 | Std. Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 2.1 Information | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Social competence | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Social influences curricula versus control | 13 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Combined social competence and social influences curricula versus control | 3 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 Multimodal curricula versus control | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 Other interventions | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Low & unclear attrition ‐ 1 year or less | 17 | Std. Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 3.1 Information curricula versus control | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Social influences curricula versus control | 12 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Combined social competence and social influences curricula versus control | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 Other interventions | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Low & unclear attrition ‐ > 1 year, longest follow‐up | 29 | Std. Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 4.1 Information | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Social competence | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Social influences curricula versus control | 17 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Combined social competence and social influences curricula versus control | 8 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.5 Multimodal curricula versus control | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.6 Other interventions | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Low selection bias ‐ 1 year or less | 9 | Std. Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 5.1 Social influences curricula versus control | 6 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Combined social competence and social influences curricula versus control | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Other interventions | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Low selection bias ‐ > 1 year, longest follow‐up | 19 | Std. Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 6.1 Social influences curricula versus control | 9 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Combined social competence and social influences curricula versus control | 7 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Multimodal curricula versus control | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.4 Other interventions | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.0 [0.0, 0.0] |
8.1. Analysis.
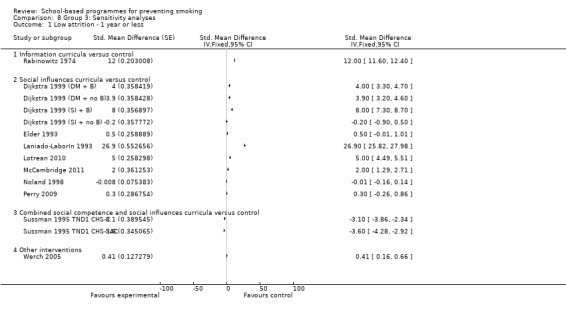
Comparison 8 Group 3: Sensitivity analyses, Outcome 1 Low attrition ‐ 1 year or less.
8.2. Analysis.

Comparison 8 Group 3: Sensitivity analyses, Outcome 2 Low attrition ‐ > 1 year, longest follow‐up.
8.3. Analysis.

Comparison 8 Group 3: Sensitivity analyses, Outcome 3 Low & unclear attrition ‐ 1 year or less.
8.4. Analysis.

Comparison 8 Group 3: Sensitivity analyses, Outcome 4 Low & unclear attrition ‐ > 1 year, longest follow‐up.
8.5. Analysis.

Comparison 8 Group 3: Sensitivity analyses, Outcome 5 Low selection bias ‐ 1 year or less.
8.6. Analysis.

Comparison 8 Group 3: Sensitivity analyses, Outcome 6 Low selection bias ‐ > 1 year, longest follow‐up.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abernathy 1992.
| Methods | Country: Canada
Site: All schools in Calgary, Alberta (94 intervention schools, 96 control schools) 'PAL Programme' (Peer Assisted Learning) Focus: Smoking prevention Design: Cluster RCT (Group 1: never smoking prevention cohort, not included in analysis) |
|
| Participants | Baseline: 7508
Age: Grade 6, age 11 ‐ 12 Gender: 49% F Baseline smoking data: Never smoked 67% M 71% F |
|
| Interventions | Category: Social influences vs control Programme deliverer: Teachers and peers (received invitation to in‐service presentations about PAL programme) Intervention: 5 sessions over 3m. Information about the benefits of not smoking (with peer‐led component) Control: No intervention |
|
| Outcomes | Smoking categories: Never smoked/ tried but no longer smoke/currently smoke (main analysis based on baseline never‐smokers) Follow up: From start of programme: 1yr, 2yr, 3yr | |
| Notes | Quality of intervention delivery: A telephone survey found that 5 teachers had not taught the programme; 40 had not taught the entire programme; and 49 had taught the complete programme. Statistical quality: Was a power computation performed? No Was an Intention‐to‐treat analysis performed? No Was a correction for clustering made? No Were appropriate statistical methods used? Analysis by X2 compared proportions smoking in the three groups |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'Schools were classified into quintiles according to median neighbourhood income, and then were randomly assigned to either the test or control groups" Clusters: School Cluster constraint: Stratificaition Baseline comparability: Groups identical at pretest on smoking rates. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Questionnaires were anonymous then linked by a unique number. Unclear if students knew which arm of the study they were in. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 7207 (96%) after 12m; 6884 (92%) after 26m; and 6530 (87%) followed to the 9th grade. "of the students successfully matched across Grades 6, 7 and 8, matches were obtained for 3,567 (82.7%) Grade 9 students". The analysis sample is the 48% of the pretest sample who completed all four questionnaires; no analysis of differential attrition; In the evaluation, intervention classes were divided into those in which teachers reported teaching all lessons, and those where fewer were delivered |
| Selective reporting (reporting bias) | Unclear risk | Reported on primary outcome. But reporting not as expected because of changes during the study caused by incomplete teaching of the programme |
Armstrong 1990 (Peer).
| Methods | Country: Australia Site: 45 primary schools in Nedlands, Western Australia Focus: smoking prevention Design: Cluster RCT (Group 1: never smoking prevention cohort) | |
| Participants | Baseline: (1981) 2366
Age: 7th grade (modal age 12 years) Gender: 49% F Ethnicity: Not stated Baseline smoking data: Smoking prevalence 24 ‐ 37% |
|
| Interventions | Category: Social influences vs control Programme deliverer: Teachers and peers ("all leaders received appropriate previous training") Intervention: (6m duration)
Control: No planned intervention |
|
| Outcomes | Nonsmoking in previous 12m (not smoked a single cigarette, not even a few puffs). Saliva samples collected but not analysed. Follow‐up: 12m, 24m, 7 yrs from end of programme. | |
| Notes | Quality of intervention delivery: No process analysis of delivery of the intervention; the authors state "all leaders received appropriate previous training". Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? The data on schools were erased after 1yr, so that ICCs could not be computed, and the data were not corrected for the effects of clustering [the authors state: "Given the large number of original classes and the subsequent mixing of students that is described above, it is likely that any biases which arose in estimates of their effects or their precision because of the analysis of individuals rather than classes would be small". Were appropriate statistical methods used? Comparison of the proportions of students in the 3 groups who took up smoking was by Pearson's Χ2 (two‐sided); effects of other variables controlled in separate LRs (using EGRET) for boys and girls, and for each year of follow‐up, using only children present at baseline and both follow‐ups. Once the final models were chosen, the parameters were re‐estimated with an added risk model. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Each school was assigned at random to one of three interventional groups: control group (no planned intervention); peer‐led programme; and teacher‐led programme". No comment on method of randomisation. Clusters: Schools Cluster constraint: Stratified by class size and location Baseline comparability: No differences between groups at baseline, smoking prevalence higher for boys than girls |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "At the time of the survey, the children, their teachers and those who conducted the survey did not know the interventional group to which the class was assigned" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Eighty‐two per cent and 64% of students were traced and re‐surveyed in the first and second follow‐up studies respectively". [after 1 and 2 years] "Seven years after the first survey of 2,366 Year 7 students in 1981 68% were traced through public records [Driver's Licences, electoral commissions and registries of births marriages and deaths]; 53 per cent of these responded to a new survey concerning smoking". [i.e. 37% of original sample] No differential attrition by treatment group at 12m follow up. Saliva samples were collected but not analysed. At the 7 yr follow up, non‐response was associated (P < .05) with being male, being in the control group, thinking most adults smoked, and mother and brother smoked. |
| Selective reporting (reporting bias) | Low risk | Abstract states: "How effective are peer‐led programmes in preventing the uptake of smoking by children?" This outcome is fully reported. |
Armstrong 1990 (Teacher).
| Methods | See Armstrong 1990 (Peer) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm in Armstrong 1990 (Peer) | |
Ary 1990.
| Methods | Country: USA
Site: 22 middle/elementary and 15 high schools from 13 Oregon districts 'Project PATH' (Programs to Advance Teen Health) Focus: Tobacco, alcohol and marijuana prevention Design: Cluster RCT (Group1: never smoking prevention cohort, not included in analysis) |
|
| Participants | Baseline: 7837 (6263 completed pretest).
Age: 1943 6th graders (age 11 ‐ 12); 1890 7th graders; 698 8th graders; 1364 9th graders; 205 10th graders; 163 11th graders.
Gender: Not stated. Ethnicity : 89% W, 4.9% B, 2.2% A, 1.8% Latin American, 1.2% H Baseline smoking data: 9.9% weekly smoking. |
|
| Interventions | Category: Social Influences vs control. Programme deliverer: Science or health teachers (received 2 to 3 hrs training). Peer leaders presented some activities in 2 grades. Intervention: 5 classroom sessions in each of grades 6 through 10, typically taught over a one‐week period. "focused most heavily on cigarette smoking and smokeless tobacco use, it was designed to deter the use of marijuana and alcohol". At each grade level (a) awareness of social influences to engage in substance use (b) refusal skills training (c) health facts (d) contracting not to use cigarettes and other substances. Programme different for each grade. Parent message group mailed 3 brochures. Control: Groups typically received 10 classroom sessions of standard tobacco/drug use education. |
|
| Outcomes | Smoking: Pechacek 1984 self reported smoking index to yield an estimate of no. cigarettes smoked in last month (composite of no in last 6m, last month, last week, and last 24 hrs): Dichotomised on >1 cigarette in previous month. Expired air CO tested before survey completion. Follow‐up: 9 ‐ 12m after pretest (Only results for grades 6 ‐ 9 given in Ary 1990) | |
| Notes | Quality of intervention delivery: Surveys of teachers indicated that the control group received 10 sessions of standard tobacco and drug education (with 97% recognizing peer pressures, 97% short‐term effects on the body and brain, 96% long‐term health consequences, 84% decision‐making skills, 72% media pressures, and 67% refusal skills practice), and the experimental schools received a median of 5 sessions of other drug education in addition to PATH. Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? No Were appropriate statistical methods used? ANCOVA |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Schools were randomly assigned either to receive or not receive the intervention. The exception was one middle school assigned to the treatment condition because it had earlier served as a pilot school for program development. ...First, schools were blocked on urban/rural status. Second, schools were matched within blocks on characteristics such as level of tobacco and other drug use, ethnicity, and school size ...". In the 12 intervention schools, parents randomised to receive or not receive parent messages. No method of randomisation. Clusters: Schools. Cluster constraint: Blocked and matched. Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Questionnaire and biochemical data were provided by 7837 elementary‐, middle‐, and high‐school students and by 6263 students (80% of original subjects) at both initial assessment and approximately 1 year (9 ‐ 12 months) later". Attrition: 24.4 % in experimental and 24.6% in control schools; no differential attrition on pretest use by gender, grade, CO level, number of peers who smoked, offers of cigarettes, parental smoking. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Ausems 2004 (Combined).
| Methods | See Ausems 2004 (In school) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 3rd intervention arm (combined in and out of school) within Ausems 2004 (In school) | |
Ausems 2004 (In school).
| Methods | Country: Netherlands Site: 8 local health departments were approached, 6 participated and 36 vocational schools participated. Focus: Smoking prevention Design: Cluster RCT (Group 1: never smoking prevention cohort, only arms 1 and 2 vs control included in the analysis)) | |
| Participants | Baseline: Intervention 1 (in‐school) = 525; Intervention 2 (out of school) = 513; Intervention 3 (combined in/out) = 829; control = 509. Age: Average 13 yrs Gender: 48% Male Smoking status at baseline: 59.7% ever smoked; 19.5% current smokers. | |
| Interventions | Category : Social influences (intervention 1/in school) vs social influences (intervention 2/out of school) vs control Programme deliverer: Teachers Intervention:
Control: No statement. |
|
| Outcomes | Self reported never smoked even one puff; not in past month; smoked in past month. Follow‐up: 1yr, 18m. |
|
| Notes | Quality of intervention delivery: Process analysis for students was 15‐item questionnaire; and for teachers a 5‐item implementation questionnaire. Only 58% of schools returned the teacher process questionnaire; and only 65% of out‐of‐school students received and read the letters. Statistical quality: Was a power computation performed? Power computation to demonstrate an effect size with an OR = 2, with power = 80%, α 2‐tailed = 0.05, with 25 students per school, and between‐school variance = 0.30, implying an ICC = 0.08, required 36 schools, and sample size achieved. Was an intention‐to‐treat analysis performed? Yes. Missing data: replaced by previous observation; drop‐outs were treated as smokers. Was a correction for clustering made? Yes, using multilevel modelling Were appropriate statistical methods used? Multilevel regression modelling using MIXREG for continuous and MIXOR for dichotomous outcomes. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Nineteen schools that already participated in the in‐school program were randomly assigned to the in‐school or to the combined in‐school and out‐of‐school condition. The remaining 17 schools were randomly assigned to the out‐of‐school condition or to the control group". [i.e. randomisation of schools did not give all schools an equal chance of being assigned to the three groups]. No method of randomisation stated. Clusters: Schools Cluster constraint: Not stated Baseline comparability: Students in out‐of‐school condition older than control (OR 1.27, 95%CI 1.03 to 1.57) |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Numbers at 12m: Intervention 1 = 434 (83%); numbers at 18m: Intervention 2 = 265 (52%); Intervention 3 = 625 (75%);control = 317 (61%) "Attrition at student level was 17.3% at post‐test 1, 25.4% at post‐test 2, and 24.6% at post‐test 3". Attrition at post‐test 3 less likely if: living with both parents (OR = 0.53, 95%CI 0.37 to 0.77); with 2 Dutch parents (OR = 0.63, 95%CI 0.47 to 0.84), less 'diffusely' surrounded by smokers (OR = 0.87; 95% CI 0.84 to 0.90). |
| Selective reporting (reporting bias) | Low risk | Original goals of study met |
Ausems 2004 (Out School).
| Methods | See Ausems 2004 (In school) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (out‐of‐school) within Ausems 2004 (In school) | |
Aveyard 1999.
| Methods | Country: UK Site: 53 West Midlands secondary schools. Focus: Smoking prevention. Design: Cluster RCT (Group 1: never smoking prevention cohort) | |
| Participants | Baseline: (1997) 8352, 90% of potential participants.
Age: Year 9, 13 ‐ 14 yrs Gender: 50% Male Ethnicity: 86% W, 5% Indian subcontinent, 4% Afro‐Caribbean. |
|
| Interventions | Category: Social influences vs control Programme deliverer: Teachers (received 2 day training course) Intervention: 6 hrs over 3 terms. 1 class lesson and 1 computer session per term for three terms based on Prochaska's transtheoretical model/ stages of change. Students used individual computers to answer questions about their smoking, and an expert system gave feedback on how their temptations compared to those of others in same stage, and their changes from previous sessions. The questionnaires were interspersed with video clips of young people talking about their thoughts about smoking that were relevant to the stage of change of the student concerned. Class lessons developed understanding of stages of change, and pros and cons of smoking at different stages. Students could be in one of nine stages (precontemplation to cessation maintenance) and were given advice appropriate to their stage, e.g., those in the acquisition preparation stage were told: "To be more like others who were thinking about trying it [smoking] but have chosen to stay smoke free, think more about the cons of smoking." Teachers delivered a one‐hr classroom 'transtheoretical model' intervention "how the pros and cons of smoking would vary in different stages, and lessons got young people to use these concepts" Control: Normal health education on tobacco. Teachers provided with lesson plans and handouts but were not required to use them, and received no training. |
|
| Outcomes | Self reported behaviour: Ex‐smoker/smoker/tried/never. Primary outcome was smoking one or more cigarettes a week. Questionnaires were confidential. Follow‐up: 12m after start of intervention. | |
| Notes | Quality of intervention delivery: 79% of baseline non‐regular smokers and 69% of baseline regular smokers received all three computer lessons; 70‐80% of sessions lasted long enough to read all the material; though baseline smokers were less likely to attend, and smokers were less likely to spend long enough to receive the individualised messages. Data on attendance and the students' reactions to the classroom lessons were not collected by the researchers. Half the teachers returned data, with a mean score of 4/5 for delivery of the lesson, and pupils' understanding and enjoyment. The researchers reported that: "All teachers reported that all intervention lessons were delivered, but we have no record of which individuals received the class‐based intervention. … Teachers were reluctant to return their questionnaires, despite prompting". Statistical quality: Was a power computation performed? Sample size of 8500 was calculated to achieve 90% power to detect a 4% difference in smoking with 5% Type I error (the ICC for smoking was calculated from a lifestyle survey as 0.008) Was an intention‐to‐treat analysis performed? Yes Was a correction for clustering made? Yes Were appropriate statistical methods used? Multilevel modelling to allow for clustering; sensitivity analysis for handling of losses to follow‐up; analyses performed by adjusting for baseline smoking status and other variables. Odds ratios used from Table 5 (Aveyard 2001) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Schools sampled with probability proportional to size of year 9 enrolment; 89 schools approached,53 agreed to participate. Randomised in 5 strata based on year 9 size. "We randomly allocated schools, not individuals, to receive the intervention or be controls. We ensured that the arms were balanced by ordering schools into five groups based on numbers of students in year 9. We allocated each school a number between 1 and N (the maximum number in the group). A computer program generated n/2 random numbers between 1 and n, and these schools were allocated to intervention". Clusters: Schools Cluster constraint: 5 strata based on year 9 size. Baseline comparability: Equivalent. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | One school dropped out after randomisation leaving 52. 8352 13‐ and 14 yr olds enrolled; 7413 (90%) at year 1 and 6782 (82%) at year 2 follow‐ups. "For regular weekly smoking, the assumptions about those lost to follow‐up are as follows. We assumed that all those lost to follow‐up were smokers, those lost were not smokers, those lost had the same smoking status as at baseline (with unknown baseline smoking status counted as smokers), and those lost had the same smoking status as at baseline (with unknown baseline smoking status counted as nonsmokers). We then confined the analysis to all those who were followed up and all those and for whom smoking status could be calculated and all those followed up and who gave no inconsistent data on smoking status. Only the data for all those with known smoking status at follow‐up are presented in this report … In all these analyses there should be no reason why loss to follow‐up or unreliable data would be associated with the TTM or control group…". |
| Selective reporting (reporting bias) | Low risk | All study objectives met |
Biglan 1987b.
| Methods | Country: USA Site: 3 high schools and 6 middle schools in Eugene, Oregon. Focus: Smoking prevention (focus on effects of attrition) Design: Cluster RCT (excluded from analysis) | |
| Participants | Baseline: 1730 (873 7th; 588 9th; 262 10th graders)
Age: 7th (age 12 ‐ 13), 9th and 10th graders.
Gender: 49% F Ethnicity: "almost all white". Baseline smoking data: No data on baseline smoking rates |
|
| Interventions | Category: Social influences vs control Programme deliverer: Regular science or health teachers. Intervention: 3 consecutive days with a 4th session 2 weeks later. Social‐reinforcement short‐ and long‐term consequences of smoking; public commitment; teaching of refusal skills (film; practised role‐playing refusal skills; skits; teachers praised skills; class voted on best refusal). Control: No intervention. |
|
| Outcomes | Self reported smoking (Pechacek 1984 index) = a weighted average of the number of cigarettes smoked last week and the reported number smoked yesterday. Also categorised into 4 baseline groups: never‐smoked/triers/experimenters (1 ‐ 6 in previous week)/ regular. Expired air CO content. Refusal skills assessed for a sample (Hops 1986) Follow‐up: 6m and 1yr | |
| Notes | Quality of intervention delivery: No process analysis of delivery of the intervention. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? X2 of proportions smoking in the two groups; ANCOVA of pretest smoking status, treatment condition, grade and gender (smoking rates log transformed to control skew). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 9 schools from 2 school districts [no further statement on school selection]. "Within each school, the classes of teachers who had agreed to participate were randomly assigned either to the intervention or to a no‐program condition". No method of randomisation stated. Cluster: Classes. Cluster constraint: Not stated. Baseline comparability: No baseline difference between groups. Differences in baseline characteristics of drop‐outs: more likely to have been baseline smokers and have multiple risk factors for smoking. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Attrition rates were substantial at both 6 months (21.6%) and 1 year (31.8%)". Significant differences (P = 0.00) between those remaining and those missing both at 6 and 12m on cigarettes/week and for all family members and best friend smoking, but no differential attrition |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Biglan 2000.
| Methods | Country: USA Site: 8 Oregon communities Focus: Tobacco, alcohol, marijuana, and antisocial behaviours. Design: Community‐ and school‐based RCT (excluded from analysis). | |
| Participants | Baseline: 4438
Age: 6th grade (11‐12)
Gender: 52% M Ethnicity: 85% W, 7% H, 6% N‐A, 1% A‐A, 1% A, < 1% Other. Baseline smoking data: Smoking prevalence index for school‐based only intervention 8%, community intervention 10.5% (no actual numbers of nonsmokers/smokers, just index) |
|
| Interventions | Category: Social Influences vs social influences + multimodal. Programme deliverer: Teachers and community adults. Intervention 1: Schools Only PATH programme (Effects of smoking; refusal skills for smoking, drugs, antisocial behaviour; video assisted instruction in refusal skills; public commitment not to smoke; peer‐led education and skill practice; 35 sessions Grades 6 ‐ 9). Intervention 2: School PATH + Community Programme (4 modules: media advocacy, youth anti‐tobacco activities, family communication, and ACCESS module programmes to stores to reduce selling tobacco to minors). Control: No group. |
|
| Outcomes | Smoking defined as (1) level of smoking (never to pack+/day); (2) number of cigarettes (past month, week and day, with responses scaled to form Pechacek 1984 smoking index [monthly x 4.3 + weekly + daily/7] to form an index of the number of cigarettes smoked weekly), (3) net CO score (expired air minus classroom CO level). Similar measures were derived for smokeless tobacco. Follow‐up: Annually up to 5 yrs. |
|
| Notes | Quality of intervention delivery: Information was collected on adolescents' exposure to information about smoking cessation; awareness of efforts to reduce illegal tobacco sales to minors; and media activities; however, no process analysis for the school intervention component. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? No. Was a correction for clustering made? No. Were appropriate statistical methods used? Generalized estimating equations and MANOVA; individual students were nested within communities, and community means were the unit of analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "It was a randomised controlled study in which small Oregon communities were assigned to one of two conditions." "Pairs of communities were matched on community socioeconomic status and population. One member of each pair was assigned at random (via the flip of a coin) to receive a school based tobacco and other substance use prevention programme (school based only (SBO) condition) in grades 6 through to 12. The other member received a community intervention in addition to the school based programme (CP condition)". Clusters: Communities Cluster constraint: Pair‐matched on community socioeconomic status and population. Baseline comparability: There were no differences at baseline between community pairs in size, per capita income, median household income, % below poverty level, % minority students, or % high school graduates. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Baseline = 4438; after 1 yr = 4515; after 2 yrs = 4395; after 4 yrs = 4708; after 5 yrs = 4165 [there is no explanation of the fluctuating numbers of over time, with more students after 1 yr compared to baseline and more students after 4 than 3 yrs; this is presumably due to in‐migration of students exceeding out‐migration]. Attrition was low at 6%; 13.5% of students were not assessed across all 5 yrs of the study; no assessment of differential attrition. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Botvin 1980.
| Methods | Country: USA Site: 2 suburban New York City schools. Focus: Smoking prevention. Design: Cluster RCT (Group 1: never smoking prevention cohort) | |
| Participants | Baseline: 281
Age: 8th (age 13 ‐ 14), 9th and 10th graders.
Gender: Not stated Ethnicity: "predominantly white". Baseline smoking data: 70% nonsmokers. |
|
| Interventions | Category: Social influences and social competence vs control. Programme deliverer: Outside specialists. Intervention: 10 lessons over 12 weeks. Social influences and psychosocial skills; group discussion, modelling, behaviour rehearsal, and the application of special skills training to life situations, including the decision to smoke; homework; self improvement project. Control: No intervention. |
|
| Outcomes | Smoking: Self reported smoking (last month, and last week). Pretest smokers excluded from analysis. Follow‐up: 6m from pretest. | |
| Notes | Quality of intervention delivery: No process analysis of delivery of the intervention. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? Yes, Χ², 2‐way ANOVA |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After randomly assigning the two schools to an experimental (n = 121) and control (n = 160) condition...". Clusters: Schools. Cluster constraint: Not applicable as only 2 schools. Baseline comparability: "Both schools had approximately the same baseline smoking rates" (School A = 31%, School B = 29%). |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Unfortunately, follow‐up data (post‐test 2) were collected on only about 77% of the post‐test 1 sample (80% for the experimental group and 74% for the control group.". ["The first post‐test occurred at the completion of the smoking prevention program (12 weeks after the pretest), and the second post‐test occurred approximately three months later ..."] differential attrition from baseline. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Botvin 1982.
| Methods | Country: USA Site: 2 suburban New York City schools (all 7th grade classes) Focus: Smoking prevention Design: Cluster RCT (Group 1: never smoking prevention cohort) | |
| Participants | Baseline: 426
Age: 7th graders (age 12 ‐ 12). Gender: Not stated Ethnicity: W (school A 93%; school B 90%); B (2%,4%); A (3%,3%); H (2%,3%) Baseline smoking data: 74% of 374 analysable sample. |
|
| Interventions | Category: Social influences and social competence vs control. Programme deliverer: Peers (recruited from neighbouring high school, received 4 hr training workshop. Supervised by a teacher and project staff) Intervention: 12 1hr sessions over 12 weeks. Physiological effects; teenage smoking rates; LST smoking prevention programme skills (self image, self improvement, decision making, independent thinking, advertising techniques, coping with anxiety, communication skills, social skills, assertiveness); homework; a self improvement project. Control: No programme. Note: See Botvin 1980 for similar programme delivered by outside specialists and Botvin 1983 for delivery by classroom teachers. |
|
| Outcomes | Smoking: Self reported smoking (last month, and last week). Pretest smokers excluded from analysis. Saliva samples collected, 25% subsample analysed for thiocyanate. Follow‐up: 1 yr after post‐test. | |
| Notes | Quality of intervention delivery: No process analysis of delivery of the intervention. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? X². |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Schools were randomly assigned to experimental and control conditions". Only two schools were randomised. Method of randomisation not stated. Clusters: Schools. Cluster constraint: Not applicable as only 2 schools. Baseline comparability: Not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Complete pretest and post‐test data were obtained on 357 students. Of these, 264 (74%) were classified as nonsmokers at the time of the pretest. This group represents the nonsmoking cohort that was the focus of attention over the course of the intervention and follow‐up phases of the study". 426 baseline, 357 at 3m post‐test; no data on total numbers at 1 yr follow‐up; There were 264 nonsmokers at pretest, and of these 210 were reported present at 1 yr. Complete pre‐ and post‐test data on 84%, of whom 74% were nonsmokers at the pretest. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Botvin 1983 (Intensive).
| Methods | See Botvin 1983 (LST) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (LST intensive) within Botvin 1983 (LST) | |
Botvin 1983 (LST).
| Methods | Country: USA Site: 7 schools in suburban New York (2 schools to intervention 1, 2 schools to intervention 2, 3 to control). Focus: Smoking prevention Design: Cluster RCT (Group 1: never smoking prevention cohort) | |
| Participants | Baseline: 902.
Age: 7th grade (age 12 ‐13). Gender: Not stated. Ethnicity: 91% W. Baseline smoking data: The numbers at pretest giving their smoking status ranged from 891 to 911 of whom nonsmokers were 92%. |
|
| Interventions | Category: Social influences and social competence vs control. Programme deliverer: Classroom teachers (received one‐day workshop training). Intervention: LST: immediate physiologic effects of smoking, self image, self improvement, decision making, advertising techniques, coping with anxiety, communication skills, social skills, assertiveness, techniques for resisting peer pressure to smoke. Direct comparison of long or short delivery format
Control: Standard smoking education mandated by NY State. |
|
| Outcomes | Self report of smoking (monthly recall; weekly recall; daily recall). Saliva samples collected but not analysed. Follow‐up: 1 yr from pre‐test. |
|
| Notes | Quality of intervention delivery: Process analysis performed but not reported. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? X², ANCOVA. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The seven schools in the study were randomly assigned to the following conditions: (1) LST Smoking Prevention Program, ...(2) LST Smoking Prevention Program, utilizing an intensive mini course ... and (3) control". Clusters: Schools. Cluster constraint: Not stated. Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The number at the 1yr follow‐up ranged from 605 to 633 (67%); no attrition analysis. The largest number of participants at the pretest recorded in Table III was 876, and after one yr in Table V was 633 (72%). |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Botvin 1990a (Video).
| Methods | See Botvin 1990a (Workshop) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from the second intervention within Botvin 1990a (Workshop) | |
Botvin 1990a (Workshop).
| Methods | Country: USA Site: 56 schools in 3 regions of New York state. Focus: Substance abuse prevention. Design: Cluster RCT (Group 3: point prevalence). | |
| Participants | Baseline: (1985) 5954.
Age: 7th graders (age 12 ‐ 13).
Gender: 48% F Ethnicity: 91% W, 2% B, 2% H, 1% N‐A. Baseline smoking data: Smoking based on 10 point scale. Intervention 1: mean (SE) = 1.10 (0.02), intervention 2: mean (SE) = 1.09 (0.01), control: mean (SE) = 1.10 (0.01). |
|
| Interventions | Category: Social influences and social competence vs control. Programme deliverer: Teachers. Intervention: 12 lessons over 15 class periods for 8 weeks in grade 7, 10 booster sessions in grade 8 and 5 in grade 9. LST (cognitive‐behavioural skills for building self esteem; resisting advertising pressure; managing anxiety; communicating effectively; developing personal relationships; asserting one's rights; developing specific skills to resist social influences to smoke, drink or use drugs).
Control: No intervention. |
|
| Outcomes | Smoking: 10 point scale: 1 (never) ‐ 10 (more than a pack a day). Breath samples were collected, but not analysed. Follow‐up: 3 yrs (9th grade, end of programme) and 5 ‐ 6 yrs (12th grade) from baseline. | |
| Notes | Quality of intervention delivery: Average 68% implementation (ranging from 27% ‐ 97%), with only 75% of the students in the prevention conditions exposed to 60% or more of the prevention programmes. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? No. Was a correction for clustering made? No. Were appropriate statistical methods used? Appropriate analysis with GLM; MANOVA, and ANOVA; students who received at least 60% of the programme were included in the analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | " ... schools were divided into tertiles consisting of schools with either high, medium or low cigarette smoking prevalence rates. From within groups of schools with similar levels of cigarette smoking, schools were randomly assigned within each of the geographic areas: (1) prevention program with a formal 1‐day training workshop and implementation feedback ...(2) prevention program with training provided by videotape ...and (3) a "treatment as usual" control group". Clusters: Schools. Cluster constraint: tertiles based on cigarette smoking prevalence rates, followed by geographical area. Baseline comparability: Botvin 1995: "No significant pretest differences were found ...". |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 5,954 7th graders participated in the pretest in the Fall of 1985‐86, 4,466 (75%) provided data at the end of the 9th grade, and 3597 (60%) in 1991 Pretest smokers more likely to be lost but no differential attrition across conditions |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Botvin 1990b.
| Methods | Country: USA Site: 10 suburban New York junior high schools (2 to each of 4 intervention groups, 2 to control). Focus: Substance abuse prevention. Design: Cluster RCT (excluded from analysis). | |
| Participants | Baseline: 1311.
Age: 7th grade (age 12 ‐13).
Gender: 51% F (at 1yr follow‐up).
Ethnicity: 80% W, 13% B, 2% H, 2% A, 4% Other. Baseline smoking data: No data.. |
|
| Interventions | Category: Social influences and social competence vs. control. Programme deliverer: Teachers and peers (received a 4 hr training workshop conducted by project staff). Intervention: All groups using LST approach. In 7th grade all experimental groups received a 20‐session multicomponent substance abuse prevention curriculum focusing on social, psychological, cognitive, and attitudinal factors ‐ facilitation of basic life skills and improvement of personal competence (teaching social resistance skills). In 8th grade selected groups received 10 booster sessions which were directed toward the consequences of smoking, decision making, resistance to advertising, anxiety coping skills, communication skills, social skills, assertiveness, and problem solving.
Control: No intervention. |
|
| Outcomes | Smoking: monthly, weekly, and daily smoking dichotomous measures, and an index of smoking frequency (5‐point scale: never to everyday). Results presented as adjusted response proportions. Follow‐up: 1 yr. |
|
| Notes | Quality of intervention delivery: The field staff noted the low degree of fidelity of implementation by many teachers. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No stated. Were appropriate statistical methods used? Attrition tested by ANOVA, treatment and control conditions compared using GLM ("One‐year follow‐up response frequencies were compared for each of the five conditions, with pretest response frequencies being used for covariates"). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The 10 schools participating in the study had previously been randomly assigned to the following conditions during the first year of the study ...". No method of randomisation stated. Clusters: Schools. Cluster constraint: Not stated. Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Of the original sample of 1311 7th graders, 1185 (90%) were available for the initial post‐test and 998 (76%) were available for the one‐year follow‐up". No differential attrition between smokers and non‐smokers. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Botvin 1999.
| Methods | Country: USA Site: 29 New York junior high schools. Focus: Reduction in tobacco and motivation to use substances by providing knowledge and skills to resist tobacco, alcohol and drugs. Design: Cluster RCT (Group 1: never smoking prevention cohort). | |
| Participants | Baseline: 2690
Age: 7th grade (11 ‐ 12).
Gender: 100% F Ethnicity: 60% A‐A, 23% H, 7% A, 3% W, 2% N‐A, 5% biracial or other. Baseline smoking data: 19% lifetime prevalence, 4% 30‐day prevalence; nonsmokers: intervention N = 1005, control N = 726. |
|
| Interventions | Category: Social Influences and social competence vs control. Programme deliverer: Teachers (received one‐day training workshop) Intervention: 15 session LST Programme, with cognitive‐behavioural skills to enhance assertiveness, resist advertising pressures, manage anxiety, communicate effectively, develop strong interpersonal relationships, and problem‐specific skills related to drug use influences, including assertiveness skills for use in situations in which students experience pressure from peers to smoke, drink or use drugs. The programme was modified for minority group use by changing the examples and the situations used for the behavioural exercises. They received 10 boosters the following year. Control: Received 10 sessions of an information‐only drug programme + 3 boosters the following year. |
|
| Outcomes | Smoking was defined as a 9‐point index from 1 (never) to 9 (more than 1 a day), and CO samples were collected at pre‐ and post‐test. Follow‐up: During grade 8 (approximately 1 yr). |
|
| Notes | Quality of intervention delivery: Project staff randomly monitored how much of the material was implemented by the teachers, and assigned an implementation score (material covered in full by 55%), which was used as a covariate in the ANCOVA. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Not stated. Were appropriate statistical methods used? X² and GLM ANCOVA were used to compare the experimental and control groups. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Each of 29 participating junior high schools was randomly assigned to either receive the psychosocial prevention program or to serve as controls". E‐mail from Dr Botvin 29 January 2012: randomisation by computer. Clusters: Schools. Cluster constraint: Not stated. Baseline comparability: At baseline the intervention group differed from the control in higher % black (P < 0.001), higher % receiving free lunches (P < .0.001), lower grades (P < 0.02). |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2,690 at baseline in 7th grade, 2209 (82%) in 8th grade; smokers had higher attrition rates (P < 0.0001), but there was no differential attrition across groups. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Botvin 2001.
| Methods | Country: USA Site: 29 inner city middle schools, New York. Focus: Universal drug prevention. Design: Cluster RCT (Group 3: point prevalence). | |
| Participants | Baseline: Botvin 2001: 5222: 3621 intervention, 1477 control (Griffin 2003: 758 identified as at high risk of using drugs from Botvin 2001 study; 426 intervention; 332 control).
Age: Middle school students.
Gender: 53% F Ethnicity: 61% A‐A, 22% H, 6% A, 6% W, 5% mixed or Other. Baseline smoking data: Smoking: Intervention 1.36, Control 1.32 [? per week ? per month ? per year ?] |
|
| Interventions | Category: Social Influences and social competence vs control. Programme deliverer: Teachers. Intervention: LST taught drug resistance skills, norms against substance abuse, development of personal and social skills, improved self esteem, managing anxiety, communicating effectively, developing personal relationships, asserting one's rights, and resistance to advertising; main programme of 15 lessons in 7th grade, 10 boosters in 8th grade. Control: Substance abuse curriculum normally provided in NY schools. |
|
| Outcomes | Frequency of smoking from 1 (never) to 9 (more than once a day); quantity of smoking from 1 (none) to 8 ( > 2 packs a day); CO samples at pretest. Follow‐up: 3m (end of 8th grade),1 yr after first post‐test. |
|
| Notes | Quality of intervention delivery: Staff randomly monitored protocol adherence in classrooms (8 teachers monitored 167 times); average number of programme points covered = 48% (SD = 19.8), (compared to 68% in the Botvin 1990 implementation of the LST programme). Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Yes. Were appropriate statistical methods used? X², GLM ANOVA; and generalized estimated equations independent (PROC GENMOD in SAS); regression analyses. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Prior to randomisation, schools were surveyed and divided into high, medium, or low smoking prevalence. From within these groups, each of the 29 participating schools were randomised to either receive the intervention (16 schools) or be in the control group (13 schools)". Email from K Griffin 24 Jan. 2012: randomisation "was done by computer". Clusters: Schools. Cluster constraint: Grouped according to smoking prevalence. Baseline equivalence: No statistical differences on any substance use variables, but more Blacks in experimental (68%) than control (54%) group (P < 0.001), more Hispanic students in control (31%) than experimental (19%) (P < 0.001) and more students receiving free lunch in experimental (68%) than control (58)%) (P < 0.001) so all 3 included as covariates in regression analyses. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 5222 7th graders, of whom 3621 (69%) received intervention ‐ 2144 completed pretest, intervention and provided data at the one‐yr follow‐up. "Significant differences were found in attrition rate according to pretest substance use, with smokers (F[1,5218] = 23.2, P < 0.0001), drinkers (F[1,5218] = 12.0, P < 0.0005), and those who use marijuana (F[1,5218] = 42.3, P < 0.0001), having higher attrition rates that that [sic] of non users". |
| Selective reporting (reporting bias) | Low risk | No selective publication |
Brown 2002.
| Methods | Country: Canada Site: 6 school boards in SW Ontario; 30/35 schools participated. Focus: Tobacco prevention. Design: Cluster RCT (Group 1: never smoking prevention cohort). | |
| Participants | Baseline: 2776 (out of 3028 students).
Age: Grade 8 (age 13 ‐ 14).
Gender: 50% F Ethnicity: Not stated Baseline smoking data: Smoking at end of Grade 8: intervention group 16%; control 18%. |
|
| Interventions | Category: Other interventions vs control. This intervention did not align with the main five categories; the programme intervenes by creating school anti‐smoking activities. Programme deliverer: Teachers and students. Intervention: A teacher in each school facilitated students and staff to participate in as many activities as possible inconsistent with smoking, build commitment to nonsmoking, and strengthen nonsmoking as a school norm. Co‐interventions not ascertained. Control: "usual care", not described further. |
|
| Outcomes | Outcomes:
Follow‐up: Grade 10 (approximately 2 yrs). |
|
| Notes | Quality of intervention delivery: Adequate activities occurred: 3.8 intervention activities in Grade 9 and 3.5 in Grade 10. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Yes. Was a correction for clustering made? Yes. Were appropriate statistical methods used? Analysis of paired clusters using a variance term appropriate to the randomisation of schools. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The 30 schools were matched within school board (by size, number of elementary school cohort students projected to attend, and proportion of cohort students from the elementary school control condition), and then randomised within pairs to intervention or control conditions". Email from E Brown 18 Jan 2012: "one school from each matched pair was assigned to intervention condition via coin flip". Clusters: Schools Cluster constraint: Pair‐matched. Baseline comparability: No significant baseline differences in Grade 8 baseline smoking status, social models risk score or elementary school risk of smoking; but intervention schools included marginally higher proportion of children who had been in an elementary intervention group in Cameron 1999 study (P < 0.10). |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Collectors blinded to assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2776 at baseline in grade 8. "Data were provided by 2,643 students (95.2% of those who consented) at the end of Grade 10, with no differential attrition across conditions, and no difference between dropouts and the retained sample in gender ratio, Grade 8 smoking status, elementary study condition, or Grade 8 social models risk score". |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Brown 2005.
| Methods | Country: USA Sites: 10 elementary schools, north of Seattle (10/25 selected). 'Raising Healthy Children Project'. Focus: Reducing students’ likelihood to use alcohol, marijuana or cigarettes and altering the frequency at which students use alcohol, marijuana or cigarettes. Design: Cluster RCT (Group 2: change rates). |
|
| Participants | Baseline: Year 1 = 938 (1230 eligible), Year 2 = additional 102 from new intake (131 eligible); Age: Grades 1and 2; mean age 7.7 yrs. Gender: 54% M Ethnicity: 82% European American, 7% Asian/Pacific Islander, 4% A‐A, 4% H, 3% N‐A. Baseline smoking data: No data until Grade 7. |
|
| Interventions | Category: Social influences and social competence vs control (school and family). Programme deliverer: Study co‐ordinator, staff, student peers. Intervention: One intervention with 4 strategies to deter substance use:
Control: No intervention stated. |
|
| Outcomes | Annual cigarette use: previous month and year; self reported; cigarette 6 point scale: 0 (no use) to 5 (more than 40 cigarettes a day). Follow‐up: Intervention from recruitment until grade 10. Data collection from grade 6 ‐ 10 (ages 11 ‐ 16). Grades 6 ‐ 9 complete group and 1:1 surveys during school hrs (those not in school completed by visit, mail or phone); Grades 9 ‐ 10 complete 1:1 interviews recorded directly on to computer. |
|
| Notes | Quality of intervention delivery: Over 94% of eligible teachers and staff in intervention schools attended the workshops with mean attendance of 5.7 sessions. 27% of intervention students attended study clubs. 40% of intervention students attended school retreats or workshops. 51% attended summer camps. 51% of intervention families attended at least one workshop (3 per year available). 35% of intervention families received individual contact. 77% of intervention families received at least one booster workshop. All intervention students and their families received at least one intervention component with overall mean of 28.3 contacts received by students and 12.6 by their families. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Yes. Was a correction for clustering made? No. Were appropriate statistical methods used? Multiple regression latent growth models, with intervention status and background factors as covariates. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Of the 25 elementary schools in the district, the 10 schools that ranked the highest in an aggregate measures of risk (e.g., low income status, low standardized achievement test scores, high absenteeism, high mobility) were selected into the study. Schools were matched on these risk factors, and one school from each matched pair was assigned randomly to either an intervention (n = 5) or control (n = 5) condition". Exclusion of students who did not remain in the school for the first year of the intervention. No method of randomisation. Clusters: Schools Cluster constraint: Ranked and pair‐matched. Baseline comparability: Missing outcome data for N = 81; more female 9.8% than male (6.0%), P < 0.05 and logistic regression showed no difference in missing data between intervention and control. No comment on imbalances in smoking or smoking‐related factors. Email from E Brown 19 December 2011 "baseline for the Raising Healthy Children Project was when students were in Grades 1 and 2; therefore, technically we did have baseline equivalency (no smokers that young). However, to your point, analyses of these and other data indicated that students in intervention schools did not differ significantly between intervention and control schools on variables considered to be related to antisocial behaviours". |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "To maintain confidentiality, students' parents, teachers, and other school personnel were not present and did not participate in any student data‐collection activities. All students were informed that their responses would not be shared with their parents or other school personnel". [we interpreted this as assuring confidentiality, but did not constitute blinding of participants or researchers to intervention status] |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Final pretest sample = 959 (92%) "77 excluded from analysis as missing substance use data for grades 6 ‐ 10, and 4 excluded as questionable validity of data". Retention rates in grade 6 ‐ 10 were all greater than 88%. No differential attrition between groups |
| Selective reporting (reporting bias) | Low risk | Two outcomes reported as stated. |
Buller 2008 (Australia).
| Methods | Country: 1) Australia 2) America. Sites: 1) 25 secondary schools in Victoria and New South Wales (13 intervention, 12 control). 2) 21 middle schools in Colorado and New Mexico (10 intervention, 11 control). 'Consider This' Focus: Reduce 30‐day smoking prevalence. Design: Cluster RCT, internet‐based intervention (Group 1: never smoking prevention cohort). |
|
| Participants |
Australia: Baseline: 2077 Age: Grades 7,8,9 (11 ‐ 14 yrs old). Gender: 48.3% M Ethnicity: Australian/European ancestry = 73.4%. Non‐European ancestry = 17%. Mixed ancestry = 7.4%. Baseline smoking data: 58.4% never smoked. America: Baseline: 1233 Age: Mostly years 6 and 7 (11 ‐ 13 yrs old). Gender: 48% M Ethnicity: W 55.8%; H 23.9%; A‐A 3.4%; N‐A 1.6%. A 3.9%. Native Hawaiian = 0.6%. Other 7.2% Baseline smoking data: 80.1% never smoked. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: On‐line web‐based programme. Intervention: 73 online activities organised into 6 modules (Introduction, Media Literacy, Relationships, Mind and Body, Decision Making, and Resistance strategies). Programme aim to convince those who had not smoked not to start and persuade those who had already tried smoking to stop. Programme progression controlled by teachers. After pretest teachers ran 'Consider This' in computer lab classes, each session lasted 45 ‐ 60 minutes (first half of school year). Control: Standard health education. |
|
| Outcomes | Primary outcome: 30‐day smoking prevalence (number of days in the past month in which they smoked at least a whole cigarette). All students asked if they had ever smoked, even a puff. Those who had not were classified as nonsmokers and given a value of zero for the 30‐day prevalence. Remaining students classified as:
Secondary outcome: Completion of Pierce et al’s 3 susceptibility items and question on future likelihood of smoking. Follow‐up: For both trials at end of school yr. |
|
| Notes | Quality of intervention delivery: IT difficulties meant variation in time between testing and post‐test, loss of schools in the American trial, breaking of some matched pairs. In new Mexico the trial was delayed by one year. Australia: Children completed 43.2 out of 73 activities (59%) Only 26% of students completed at least 90% of activities. America: Children completed 46.6 out of 73 activities (64%). Only 24.8% of students completed at least 90% of activities. 83.1% of children completed module 1. Matching of schools failed because of teachers and IT problems. Statistical quality: Was a power computation performed? Yes, but not stated. Was an intention‐to‐treat analysis performed? No. Was a correction for clustering made? Yes by linear mixed models. Were appropriate statistical methods used? Descriptive statistics of participant characteristics. Linear mixed models. Bivariate linear mixed models to examine associations between outcome measures and potential covariates. Multivariate analysis to focus on significant predictors from the bivariate model. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Schools approached directly or via districts Schools paired on location, size, proportion of female, minority, and Hispanic students, and proportion of students who received free or reduced‐fee meals as an indicator of socioeconomic status of the catchment areas (American trial only). One school in each pair was assigned at random to the intervention group. Email from D Buller 19 December 2011 "Our project statistician used a computer program to randomise them after matching". Clusters: Schools. Cluster constraint: Paired matching based on number of factors. Baseline comparability: One Australian school enrolled without a match. Control group in US study had more children (78.3%) than experimental (83.2%) who had never smoked, but nonsmokers. (P = 0.92) "No significant differences in individual drop‐outs based on treatment group". |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk |
Australia: Analysable sample = 1510 (intervention =754). Only 73% of original sample completed both pretest and post‐test. Large drop out: 207 due to classes withdrawing because of IT issues. Remainder largely due to timing of post‐test as number of students doing activities outside school. No significant differences in drop‐outs based on treatment group, gender, race/ethnicity or home language. America: Analysable sample = 1004 (intervention = 640). 82% of the original sample completed both pretest and post‐test. Half of drop out due to IT, remainder mostly absent. No differential attrition between groups. |
| Selective reporting (reporting bias) | Low risk | All outcomes clearly expressed. |
Buller 2008 (USA).
| Methods | See Buller 2008 (Australia) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from the second American study within Buller 2008 (Australia) | |
Bush 1989.
| Methods | Country: USA
Sites: 9 schools, Washington, D.C. 'Know Your Body' Programme. Focus: Prevent cigarette smoking, and improve fitness and nutrition; involved parents and community physicians. Design: Cluster RCT (excluded from analysis). |
|
| Participants | Baseline: 1234 eligible students (1983), 892 (72%) screened and completed questionnaires
Age: 4 ‐ 6th grade (average age at baseline 10.5 yrs). Gender: 54% F Ethnicity: Not stated. Baseline smoking data: % nonsmokers: intervention 97.9%, control 96.3% but no separate data for intervention and control; serum thiocyanate measure: intervention 40.8; control 25.8 mu/L. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Teachers (received four 3 hr training sessions) Intervention: Two 45 min sessions per week throughout grades 4 to 6 through grades 7 to 9. 'Know Your Body' programme, (values clarification, goal setting, modelling, rehearsal, feedback of screening results, and reinforcement). The PRECEDE programme was used to target predisposing, enabling and reinforcing factors for the success of the school‐based programme, and also recognized the importance of teachers and parents. Half the students received their screening results to enter on their Health Passport, and half did not (the results were sent to their parents). All family physicians and paediatricians in the area were sent letters describing the programme and informing them that parents might bring them their child's Health Passport with screening results. A quarterly newsletter, The Pacesetter, was taken home by the students after class discussion. Staff presented the programme at Parent Teacher Association meetings (Similar programme to the 2 other 'Know Your Body' studies (Walter 1985; Walter 1986)). Control: The students did not receive the 'Know Your Body' programme, and only the parents received the screening results for their children. |
|
| Outcomes | % nonsmokers (data only provided for baseline). Measure of smoking at baseline and 2 yr follow‐up: serum thiocyanate (cut off point is > 100 mu/L) "used as an indication of possible smoking...". Follow‐up: 3 yrs. |
|
| Notes | Quality of intervention delivery: Adherence to curriculum and the quality of teaching were monitored. No process analysis of delivery of the intervention. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? Mean differences; LR was used to adjust for gender, age, SES, and baseline risk factors. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The schools were ranked according to the percentage of students eligible for Title 1 (federal school lunch program), and the rank order was divided into tertiles. Three schools were then randomly selected from each of these socioeconomic levels'. Method of randomisation not stated. Clusters: Schools Cluster constraint: Schools ranked and divided into tertiles. Baseline comparability: Nonparticipants at baseline did not differ from participants in health knowledge, attitudes and psychosocial attributes. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Of 1,234 subjects eligible at baseline, 1,041 (84.4 per cent) participated in the baseline examination of risk factors; 892 (73.3 per cent) also completed questionnaires. Of baseline participants, 432 (41.4 per cent) were available for re‐screening after two years of intervention, forming the cohort". At two years similar across groups. Significantly more males, lower SES, and older students in control group. Females were more likely to be available at the 2 yr follow‐up (P < 0.05). Serum thiocyanate in the baseline cohort was 34.2 umol/L and 33.3 in those lost to the 1 yr follow‐up (P < 0.41). High attrition due to transfers to other schools. |
| Selective reporting (reporting bias) | Unclear risk | No statement |
Byrne 2005.
| Methods | Country: Australia Sites: Canberra high schools (intervention), high and secondary schools in Canberra and Adelaide (control). Focus: Smoking rates of participants Design: Cluster RCT (Group 1: never smoking prevention cohort, not included in analysis). |
|
| Participants | Baseline: 2719 (intervention), 6410 (control). Age: 11 ‐ 17 years (grades 7‐10). Gender: 48% M (intervention), 52% M (control). Ethnicity: Not stated. Baseline smoking data: Rates of smoking over previous 12m at outset. Health programme = 9.7%, fitness programme = 9.5%, social skills = 12.5%, control = 14.4%. |
|
| Interventions | Category: Social Influences vs information. Programme deliverer: Usual class teachers (all trained by research group) Intervention: 3 programmes aimed at knowledge acquisition and behaviour change. Each programme based on four class sessions which had a distinctive active learning approach:
Control: Non‐randomised, from a separate, older study. No stated intervention. |
|
| Outcomes | Smoking behaviour. Self reported Follow‐up: Immediately after intervention (intervention), end of one yr study (intervention and control). |
|
| Notes | Quality of intervention delivery: No comment on quality of delivered material, or how many of the sessions were completed, or how many sessions participants attended. Statistical quality: Was a power computation performed? "the design had sufficient statistical power to provide an adequate test of the effectiveness of interventions" (but no power computations presented). Was an intention‐to‐treat analysis performed? No. Was a correction for clustering made? No. Were appropriate statistical methods used? Χ² appropriate for categorical data. No correction for multiple comparisons. Analysis only on participants who completed all three data collection points in intervention group. Control group only two collections points – intake and 12m. Control group data from previous study and only limited. Can only analyse between interventions, not vs control. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Schools were selected to reflect socioeconomic diversity across the city". Classes within selected schools randomised to one of three intervention programmes. No method of randomisation stated. No controls within selected schools. Control group from previous study. Clusters: Schools Cluster constraint: Not stated. Baseline comparability: No significant differences in smoking rates at baseline between groups. Classes did not differ on gender and had representations in classes from all age groups in the school (intervention). |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | As classes were within the same school there was no mention of how the study dealt with interclass discussion and comparison of interventions. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Intervention group: 86.2% of the original group had completed data immediately after intervention (n = 2344). At end of one yr 62.3% completed follow up (n = 1694). No differential attrition analysis. Control group: 65.5% of the original cohort completed the 12m follow‐up (n = 4198). No explanation of low levels of response at 12m. |
| Selective reporting (reporting bias) | Low risk | Only goal was reporting smoking outcomes. |
Cameron 1999.
| Methods | Country: Canada Site: 100 elementary schools in 7 boards. Focus: Smoking prevention Design: Cluster RCT (excluded from analysis). | |
| Participants | Baseline: 4971 eligible students, 4466 provided baseline data.
Age: 6th grade (age 11 ‐ 12). Gender: Not stated Ethnicity: Not stated Baseline smoking data: Smoking rate 18.6% for cohort followed. |
|
| Interventions | Category: Social influences vs control [nurse workshop vs nurse self prep vs teacher workshop vs teacher self prep]. Programme deliverer: Public Health Nurses regularly involved in school programming, or teachers. Intervention: Direct comparison of different programme providers and training methods. All taught same social influences curriculum, developed at University of Waterloo. See Flay 1985, Santi 1992, Santi 1994. All sessions 40 mins, taught over consecutive weeks; 6 lessons in grade 6 (information on the social consequences and short‐term physiological consequences of tobacco use; peer, parent and media influences on tobacco use; modelling and building resistance skills); 3 lessons in grade 7 (review of Grade 6 programme, develop social norms supporting nonsmoking, build awareness of the hazards of second‐hand smoke, and develop self efficacy for assertive behaviour around the issue of second‐hand smoke), 6 lessons in grade 8 (similar content). All providers given a manual, audiovisual aids, student workbook, peer leader manual and host teacher manual for each grade unit and a 1hr orientation session. Self preparation: Materials listed above and videotape demonstrating interactive learning. Workshops: 1 day before each grade and ½‐day after 2 lessons in grade 6
Control: No intervention. |
|
| Outcomes | Smoking categories: Never/tried once/quit/experimental (< 1 a week)/regular (weekly). Prespecified breath samples collected but not analysed. Social models risk score calculated from friends, older siblings, parents who smoked. Follow‐up: 3 yrs (end of grade 8). | |
| Notes | Quality of intervention delivery: Detailed analysis of provider training, but no process analysis of programme delivery. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Not stated. Were appropriate statistical methods used? LR. Pearson goodness of fit used to allow for between school variation. Some analyses for smokers/nonsmokers separately. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Schools within boards were ranked by risk score and classed (on the basis of tertiles) as either high, medium, or low risk. Then schools within each board and risk level were assigned randomly to 1 of the 5 experimental conditions. In the case of the board that provided only 10 schools, schools were ranked by risk score and defined as either high or low risk based on a median split". Method of randomisation is not stated. Clusters: Schools Cluster constraint: Ranked by risk and divided into high, medium and low tertiles. Baseline comparability: No significant differences smoking, gender, high social models of risk. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "A total of 4466 students ‐ 80.2% of those eligible [4971] and 89.8% of those with consent, provided data in grade 6. Of these students, 3972 (88.9%) were successfully tracked and provided data at the end of grade 8". "Measures taken in grade 6 were used as predictor variables in a logistic regression model to compare students who were successfully followed up with those who were not. No significant differences were seen between those who were retained and those lost by conditions or school risk score. However, differences by sex (P < 0.05), board (P < 0.001), social models risk score in grade 6 (P < 0.001) , and smoking status in grade 6 (P < 0.001) were significant. Boys, students who had high social models risk scores, and students who were smoking in grade 6 were less likely to be retained. Grade 8 smoking rates in this study are therefore likely to be underestimated because (in the retained cohort) students who had high social models risk scores and students who were smoking in grade 6 were more likely to be smoking in grade 8. However, the internal validity of the study apparently was not compromised by attrition because there was no evidence of differential patterns of attrition across treatment conditions". [we were influenced by the final sentence to assign low risk of bias]; |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Campbell 2008.
| Methods | Country: UK
Site: 59 schools in west of England & Wales (29 to control, 30 to intervention). A Stop Smoking In Schools Trial (ASSIST). Focus: Spread and sustain nonsmoking as normal behaviour, prevent smoking uptake. Design: Cluster RCT (Group 3 : point prevalence). |
|
| Participants | Baseline: 5562 control, 5481 intervention (potentially eligible students); 5372 control, 5358 intervention (baseline data collection). Age: School year 8 (12 ‐ 13 yrs old). Gender: 51% M Ethnicity: Not stated Baseline smoking data: Weekly smoker control: 7%, intervention: 5% (analysable samples); never smoked: intervention = 53.8%; all students = 52.2%; tried once = 22.2%, all students = 20.9%; occasional ( < 1 a week) intervention 4.1%, all students 5.3% (baseline sample of 5358). |
|
| Interventions | Category: Other interventions vs control. This intervention did not align with the main five categories; the programme intervenes by promoting conversations with peers when they are smoking. Programme deliverer: Peer supporters (received 2 day out‐of‐school, plus 4 follow‐up training sessions from external trainers). Intervention: 10 week intervention period. Peer nominated year 8 students "use informal contacts with peers in their school year group to encourage them not to smoke". Control: "Usual smoking education and policies for tobacco control". |
|
| Outcomes | Prevalence of smoking in the past week in the year group of the school (defined as students smoking a cigarette in the previous 7 days).
Self report (some saliva samples taken to assess misreporting, not to correct self reported data) at baseline, 1 yr follow‐up and 12 intervention and 12 control schools at 2 yr follow‐up. Follow‐up: Immediately post intervention, 1 and 2 yr follow‐up. |
|
| Notes | Quality of intervention delivery: "835 (16%) of 5358 students completed the training and agreed to work as peer supporters, achieving the prespecified target of 15% of the year group". "fidelity of intervention delivery was high. Each stage of the intervention was delivered in every intervention school, the desired peer supporter recruitment levels were reached and attrition was low". "Peer supporter attendance at follow‐up meetings did not fall below 86%, and 82% of peer supporters handed in a diary". 66.9% of peer supporters attended all four follow‐up meetings. Statistical quality: Was a power computation performed? Yes. "planned study (33 schools per group) was powered to detect either a 7.5% or 8.5% difference dependent on loss to follow‐up (10% or 15% respectively). Only 59 of 66 schools agreed to randomisation, but the average size of the year group was much larger than was anticipated". Was an intention‐to‐treat analysis performed? Yes Was a correction for clustering made? Yes Were appropriate statistical methods used? Multilevel modelling. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Positive responses were received from 113 schools. 66 schools were selected from these 113 by random sampling with stratification by country, type of school including independent or state, mixed‐sex or single‐sex, English‐speaking or Welsh‐speaking; size of school; and level of entitlement to free school meals". 59 signed up schools "used stratified‐block randomisation, with strata defined by the same criteria as for the random selection procedure. One investigator (RC) determined the sequence in which schools were to be allocated using a randomly ordered list of schools for each stratum". Clusters: Schools Cluster constraint: Stratification Baseline comparability: "more students in control schools reported smoking every week than did those in intervention schools’ (7% vs. 5%) (no significance stated), and at 1 yr follow‐up 5% and 4%. |
| Allocation concealment (selection bias) | Low risk | "To conceal allocation, another investigator (LM) was at a different location and was unaware of which school was the next to be randomised. LM used a random number generator to establish the group allocation of the next school, which he communicated to RC by telephone". |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Two schools withdrew due to changes in decision by management – "replaced by two from the same strata in the list of 113 interested schools, and were then randomly allocated to treatment as a block of two". Two schools closed in follow‐up period – ‘of the 123 students registered at these two schools, 117 transferred to other schools within the trial and were therefore not lost to follow‐up". Intervention: Baseline: 5358 eligibles, 5187 participated (97%), 5087 (95%) analysed. At 2 yr follow‐up 5293 eligibles, 4984 (94%) participated (97%), 4966 (94%) analysed. Control: Baseline: 5372 eligibles, 4821 participated (91%), 4753 (89%) analysed. At 2 yr follow‐up 5284 eligibles, 4763 (90%) participated (97%), 4700 (89%) analysed "At every data collection point, more than 90% of eligible students provided self‐reported data for smoking". No differential attrition analysis |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Chatrou 1999.
| Methods | Country: Netherlands Site: 48 classes in 4 Brabant schools (13 to intervention, 15 to active control, 20 to control). Focus: Prevention of smoking onset Design: Cluster RCT (Group 3: point prevalence). | |
| Participants | Baseline: 949 Age: 12 ‐ 14 yr olds. Gender: Not stated Ethnicity: Not stated Baseline smoking data: 832 (88.6%) nonsmoker; 107 (11.4%) smokers (including 67 experimental and 40 regular smokers). |
|
| Interventions | Category: Social influences vs control. [social Influences and information vs control, social influences vs control] Programme deliverer: Adults trained by the researchers Intervention:
Control: No intervention "standard information about smoking if it was included by chance in their regular curriculum". |
|
| Outcomes | Nonsmoking = none in past month; smoking = regular (at least 1 cigarette a week) or experimental ( < 1 cigarette a week) in past month. Follow‐up: 18m. |
|
| Notes | Results only used from intervention 1 and control in analysis. Quality of intervention delivery: No process analysis. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No "Although classes were the units of assignment, individuals were taken as the units of analysis. The reason for this was that the classes changed greatly during the entire study‐period of one and a half years, whereas the individuals who were studied remained the same". Were appropriate statistical methods used? Individual was unit of analysis; X²; LR to predict smoking; no ICC. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "...classes were randomly assigned to treatment conditions, and all students within the same class were given the same treatment. ...The classes within a school were randomly selected in order to avoid the problems that arise when the social context of a given school moderates treatment impact". Method of randomisation not described. Clusters: Classes Cluster constraint: Not stated. Baseline comparability: At baseline treatment group had more nonsmokers (93%) than control (89%) or active control (85%; P < 0.01); fewer intending to smoke (P < 0.01), fewer friends who smoked (P < 0.01), and the treatment groups had more males (47%) than the control (38%; P < 0.02). The active control group had more students with a lower level of education. "The groups also differed with respect to gender, age and school type". |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 949 at baseline; at 18m follow‐up N = 845 (89%), because 94 "had no valid score on the smoking variable". |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Chou 2006.
| Methods | Country: China
Site: 4 classes from each of 14 middle schools in Wuhan urban districts (7 to intervention and 7 to control). Wuhan Smoking Prevention Trial (WSPT). Focus: Prevention of smoking initiation. Design: Cluster RCT (Group 1: never smoking prevention cohort). |
|
| Participants | Baseline: 2661
Age: 12.5 yrs (average).
Gender: 52.3% M Ethnicity: Not stated Baseline smoking data: Ever smoked intervention = 34.9%, control = 27.1% (P = 0.001); females: intervention 20.5%, control 16.3%; males: intervention 49.2%, control, 37.3% (P = 0.001); Past 30 day: female 3%, male 16%; age 11 5%; age 12 8%; age 13 11%, age 14 11%; age 15 11%. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: US‐trained health educators from the Wuhan Centre for Disease Control and Prevention. Intervention: Modified version of Project SMART (changes to accommodate Chinese culture). 13 consecutive 45‐minute classroom lessons with one lesson each week. Public commitment in front of their classmates not to smoke and discuss consequences of smoking. Emphasis on avoidance of household exposure to tobacco smoke. Control: "normal activities". |
|
| Outcomes | Self reported. Ever smoking and recent past (past month) smoking: ‘Have you ever tried cigarette smoking, even a few puffs? (0 = no, 1 = yes) and think about the last 30 days. On how many of those days did you smoke cigarettes? (0 = 0 days, 1 = 1‐30 days)’. Established smoking = ≥ 100 in lifetime. Bogus pipeline (Vitalograph). Follow‐up: Post‐test 1 yr after baseline. |
|
| Notes | Quality of intervention delivery: Not stated. Statistical quality: Was a power computation performed? Not stated. Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Yes Were appropriate statistical methods used? X² tests, multilevel logistic regression models. Additional attrition analysis carried out assuming that all boys not observed in the follow‐up became recent smokers still showed "a trend of secondary prevention for boys; however, the effect was no longer statistically significant". |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A middle school was randomly selected from each of the 7 urban districts win Wuhan. Another middle school with similar school size, teacher/student ratio, and academic rating in the same district was selected later. One school from each matched pair was randomly assigned to the program group. Four 7th grade classrooms from each school were randomly selected to participate in the evaluation of WSPT". Email from author "Randomization was done with a random number generator in SAS". Clusters: Schools Cluster constraint: Pair‐matched. Baseline comparability: "Smoking was significantly more prevalent in the program than in the control group at baseline’ [Ever smoked: intervention = 34.9%, control = 27.1% (P = 0.001); females: intervention 20.5%, control 16.3%; males: intervention 49.2%, control, 37.3% (P = 0.001)] |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Response rate at baseline was 97%". "The attrition rates were 7.8% among the sample at baseline. The program group has a higher attrition rate than the control group". Not significant. ‘’Difference in attrition between program and control groups was significant among males" (P = 0.05 level) "and not significant among females". "Attrition rates varied directly with smoking behaviour". (Baseline ever smoker P = 0.05 level, baseline recent smoker P = 0.01 level). Attrition rate for baseline sample: 7.8% (Programme 9.6%, Control 6.0%, P = 0.01). Attrition for males 10.3% (Programme 13.1%, Control 7.5%, P = 0.01); Not significant among females. Attrition for baseline nonsmokers: 6.6% (Programme 8.0%, Control 5.4%, P = 0.05); males 9.0% (Programme 11.5%, Control 7.1%, P = 0.05). Nonsignificant for control vs programme for females. Attrition for baseline ever‐smokers: 10.4% (Programme 12.5%, Control 7.7%, P = 0.05); males: 11.9% (Programme 14.6%, Control 8.4%, P = 0.05) nonsignificant for females; Attrition for baseline past month smokers: 13.7% (Programme 17.7%, Control 8.1%, P = 0.01) (males 13.8% (Programme 19.1%, Control 6.1%), P = 0.01), nonsignificant for females. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported as planned. |
Clark 2010.
| Methods | Country: USA
Site: 14 alternative high schools in Washington State (7 to intervention, 7 to control). Project ‘SUCCESS’ (Schools using coordinated community efforts to strengthen students) Focus: Substance use prevention (alcohol, marijuana, illegal drugs, tobacco). Design: Cluster RCT (Group 2: change rates). |
|
| Participants | Baseline: 2871 consented, of whom 2467 returned parental consent forms and 2249 elected to participate; 1730 at baseline (Intervention 752, control 978) with 30‐day substance use data and of these 52% reported past 30 day use.
Age: Average 16.64 control, 16.79 intervention
Gender: 51% F (control); 48% F (intervention) Ethnicity: 78% W, 7% A‐A, 12% H (control); 74% W, 5% A‐A, 19% H (intervention) Baseline smoking data: 30‐day cigarette use: Intervention 1.97, Control 2.16. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Masters‐level professional counsellors based in schools for 1 yr (received 3 days training). Intervention: Project SUCCESS: 1) Prevention Education Series (4 topics in 6 ‐ 8 weekly sessions: being an adolescent, alcohol, tobacco and other drugs, family pressures and problems, skills for coping); 2) Individual and group counselling; 3) Communication with parents; 4) Referrals to community agencies (all students are screened "to assess their own and their family's use of alcohol and other drugs and their need for professional treatment or other services."). "Project SUCCEESS counsellors engage in outreach to parents, students and the community by participating in task forces and attending related school and community events". Control: No statement if received intervention. |
|
| Outcomes | Self report. Past 30‐day cigarette use (from 0 to 38 or more) Follow‐up: Initial post‐test and 1 yr later. |
|
| Notes | Quality of intervention delivery: "89% provided all three waves of survey data, and 97% provided two waves". Counsellors recorded students’ exposure weekly to programme activities (68.5% attended a Prevention Education session and 49.6% attended at least four), screening (181 = 24% attended any session) and if recommendation was made, number of individual counselling sessions (36% attended one), number of referrals to outside agencies, contacts with parents and teachers, number of group counselling sessions attended (17% attended any). Statistical quality: Was a power computation performed? Yes for 80% power, 2‐tailed α = 0.05, mean ICC = 0.04, needed 136 students/school; "our study may have been underpowered". Was an intention‐to‐treat analysis performed? Yes. Was a correction for clustering made? Yes. Were appropriate statistical methods used? Multilevel hierarchical modelling, missing covariate data replaced with Expectation Maximization algorithm. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Subcontracted recruitment to educational service districts in Washington state. "Two successive cohorts of alternative high schools were randomly assigned to an intervention or control group…". 100‐200 students in 9th to 12th grades, focus on youth with behaviour problems including delinquency. Excluded students who attended night school (Project ACCESS not offered at night), and Running Start students who attended community colleges. No method of randomisation stated. Clusters: Schools Cluster constraint: Not stated. Baseline comparability: "tendency for control schools to be larger and more suburban (vs. urban) than the intervention schools". "no evidence to suggest significant differences between the intervention and control groups on 30‐day substance use". |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Pretest survey 1742, post‐test at end of academic year 1650 (1603 reported in Table 2), post‐test 1 yr later 1582 in text (1535 reported in Table 2); no differential attrition by group. "there were no differences between the intervention and control groups at baseline on past 30‐day substance use among those lost to attrition". |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Clarke 1986.
| Methods | Country: USA Site: 10 schools in Vermont (2 to each of 3 interventions, 4 to control). Focus: smoking prevention. Design: Cluster RCT (excluded from analysis). | |
| Participants | Baseline: (1980) 1321
Age: 7th grade (age 12 ‐13). Gender: Numbers not stated, but analysis by gender given. Ethnicity: Not stated. Baseline smoking data: Prevalence of daily smoking ranged from 1 ‐ 13% across treatment groups. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Peers (9th graders selected by school administrators, 1 day training), professional health experts, usual health teachers. Intervention: Direct comparison of programme deliverer. Social influences programme: sources of pressure to smoke, with videotapes, role playing, question periods, and resistance strategies.
Control: No intervention. |
|
| Outcomes | Self report of smoking last month, last week, or yesterday. Saliva samples for thiocyanate testing. The authors state only: "saliva thiosalinatic tests were included in the evaluation procedure, though not with reliable results". Follow‐up: 1 yr and 18m after intervention. | |
| Notes | Quality of intervention delivery: No process analysis. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? ANCOVA for trends over time. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Schools were randomised into various treatment modalities after school administrators agreed to participate. The design scheme involved assigning two schools to each of three treatment interventions and four schools to a control setting". Method of randomisation not stated. Cluster: Schools Cluster constraint: Not stated. Baseline comparability: No statement. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Students were assured of anonymity both to protect confidentiality of responses and to enhance truthful reporting" [we interpret this assurance of confidentiality as providing blinding for neither participants nor researchers]. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Nonresponse ranged from 1% to 5% within study schools at each of the four observations; most loss was due to routine absenteeism rather than refusal". The numbers remaining at 12m are not stated; differential attrition from baseline characteristics not stated. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Clayton 1996.
| Methods | Country: USA
Site: 31 schools in Lexington, Kentucky (23 to intervention, 2 to control) Project DARE (Drug Abuse Resistance Education). Focus: Drug abuse prevention Design: Cluster RCT (excluded from analysis). |
|
| Participants | Baseline: 2071 (93% of all 6th graders in community).
Age: 11 ‐ 12 yrs
Gender: 49% F
Ethnicity: 75% W; 22% A‐A. Baseline smoking data: 28% had tried tobacco. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Uniformed police officers. Intervention: 1 hr a week x 17 weeks. DARE curriculum: information about drugs and their effects, peer pressure resistance skills, awareness of media influences; decision‐making skills; accurate perceptions of levels of drug usage, enhancement of self esteem, taking responsibility. Control: Usual drug education curricula, which varied by school. |
|
| Outcomes | Smoking: No of cigarettes in past year. Follow‐up: yearly for 5 yrs, 10 yrs (age 20). | |
| Notes | Quality of intervention delivery: No process analysis; and usual drug education varied across the control schools. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Not stated. Were appropriate statistical methods used? 3‐stage mixed‐effects regression modelling. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | " ...23 of Lexington's 31 elementary schools were randomly assigned to receive the treatment (i.e. the DARE curriculum). Eight schools were randomly selected as comparisons. (While a balanced design would have been preferable, the school system would only allow 8 comparison schools. The primary reason for the number of schools in each condition was the number of officers (four) who had been trained to deliver DARE". Method of randomisation not stated. Clusters: Schools Cluster constraint: Not stated. Baseline comparability: Past yr cigarette smoking: Treatment = 1.36, Control = 1.31. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Confidentiality was emphasized verbally by trained data collectors who were independent of the school system. Confidentiality was dramatized by having the students tear off the first page of the questionnaire which contained identifying material. This material was then placed by the data collector in a separate envelope in front of the class" [we assess this assurance of confidentiality as blinding neither participants nor researchers]. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "The rate of attrition in the total sample between pretest and the fifth follow‐up was approximately 45%". "The only significant difference between those who remained in the study and dropouts with regard to gender occurred in the 9th grade (X2 = 5.86; df = 1; P<.05)....The only significant difference for race/ethnicity (i.e., white, African American, other) occurred in the 8th grade (X2 = 9,.22; df = 2; P <.01)...". "...those students who dropped out of the study at all follow‐up periods, with the exception of the posttest, are significantly more likely than those who remained in the study to have used cigarettes and marijuana at pretest". "In sum, the attrition analyses conducted on the total sample suggest that attrition does not seriously threaten the internal validity of this study, but does place some limits on the generalisability of the findings. Regarding internal validity, differential attrition by condition was not substantial and, with only two exceptions, drug users were not found to be more likely to drop out of either condition". |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Coe 1982.
| Methods | Country: USA Site: 2 classes in 2 public schools in St Louis Metropolitan area. Focus: Smoking prevention. Design: Cluster RCT (Group 1: never smoking prevention cohort). | |
| Participants | Baseline: 226
Age: 7 ‐ 8th grade (School A: experimental group had a median age of 13 yrs and control group had median age of 14 years; school B: both groups had a median age of 12 years). Ethnicity: School A = 88% B; school B = 89% W. Baseline smoking data: School A: experimental group had 56% never‐smoked and 44% never‐smokers in the control group; school B: 54% never‐smokers in the experimental group and 60% in the control group. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: 1st yr medical students (received 4 hrs training) led groups of 15 ‐ 20 students. Intervention: 8 sessions. Group sizes 15 ‐ 20 students. Social influences (peer pressure to smoke, advertising, role plays, and promoting group support for nonsmoking). In one school positive reinforcement offered to the class with greatest reduction in smoking behaviour. Control: No intervention. |
|
| Outcomes | Never smoked/experimenting (had not smoked within the last 30 days)/smoker (had smoked at least 1 cigarette in past 30 days). Saliva samples were collected but results not presented. Follow‐up: 12m. | |
| Notes | Quality of intervention delivery: No process analysis. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? Comparison of % remaining nonsmokers and becoming smokers. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The study was conducted in two public middle schools in the Saint Louis Metropolitan area with seventh or eight grade students. One class in each school was randomly assigned to the experimental condition and one to the control condition". No method of randomisation stated. Clusters: Classes Cluster constraint: Not stated. Baseline comparability: School A in its experimental group had a significantly higher percentage of both never‐smokers and smokers, and in its control group more experimenters; School B in its experimental group had a higher percentage of never‐smokers and in its control group a higher percentage of smokers. One school was 89% white and the other 88% black |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Intervention: Baseline = 102, 1 yr follow‐up = 66 (65%); Control: Baseline = 124, yr 1 follow‐up = 84 (68%). No attrition analysis. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Cohen 1989.
| Methods | Country: USA Site: Williamsport Consolidated School District. Focus: Tobacco, nutrition and blood pressure. Design: Cluster RCT (excluded from analysis). | |
| Participants | Baseline: 1051 households: 273 5th, 272 6th, 255 7th, and 251 8th graders
Age: 5 ‐ 13 yrs.
Gender: No data Ethnicity: No data Baseline smoking data: Child ever smoke = 18%. |
|
| Interventions | Category: Social influences vs control [control = health curriculum]. Programme deliverer: Older peers (received received 4 days of training) and teachers. Intervention: Students in 5th grade received the nutrition programme (5 schools). Students in 6th grade received the blood pressure programme (5 schools). Students in 7th grade received the smoking prevention programme (3 schools). In each grade the intervention programme was 4 sessions taught by the older peer leaders, with a focus on (a) parents as role models; (b) homework completed by the child and parents; (c) risk factor information mailed to the parents. Parents were viewed as enablers of health behaviour change. The smoking curriculum was adapted from Project CLASP (review tobacco advertisements to counter media pressure; practise resisting peer pressure; public commitment to nonsmoking; homework where child interviewed a parent about smoking). Control: Health curricula taught by teachers and received neither group discussion nor homework. |
|
| Outcomes | Ever smoking; baseline (grade 6) 18%; grade 7 35%; grade 8 48%. Follow‐up: grade 6 to grade 8. |
|
| Notes | Quality of intervention delivery: No process analysis. Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No Were appropriate statistical methods used? Pearson correlations for parents' and students' responses; phi coefficients for dichotomous smoking responses; and repeated measures ANOVA for curricula evaluation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "... students were then randomly assigned as individuals to either the older peer‐led or teacher‐led group". Method of randomisation not stated Clusters: Groups Cluster constraint: Not stated. Baseline comparability: No significant differences. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Baseline = 328; no statement on number at 1 yr follow‐up, but number for ANOVA is stated as 322 (98%). No attrition analysis. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Connell 2007.
| Methods | Country: USA
Site: 3 urban middle schools in northwest USA. 'Adolescents Transitions Program' Focus: Tobacco, alcohol, marijuana rates, lifetime substance abuse diagnoses. Design: Cluster RCT. A family‐focused randomised encouragement trial, family‐centred intervention. Students allocated to a family resource centre (FRC) (Group 1: never smoking prevention cohort). |
|
| Participants | Baseline: 998 (over 2 cohorts).
Age: 6th grade (age 11).
Gender: 47.3% F Ethnicity: 42.3% W, 29.1% A‐A, 6.8% H, 5.2% Asian Americans, 16.4% other. Baseline smoking data: 0.50 (previous month tobacco use, on scale 0 = never, 6 ≥ 20 times). |
|
| Interventions | Category: Social competence vs control. Programme deliverer: FRC parent consultants (2 Masters‐level therapists, one BSc). Intervention: Intervention participants randomised to a Family Resource Center (FRC) for 2 yrs. All participants received 6 SHAPe sessions in school (school success; health decisions; building positive peer groups; cycle of respect; coping with stress and anger; solving problems peacefully) [adapted from 16 session LST]. Optional additional ‘selected intervention’ for families of high risk youths (teacher‐determined): 3 session Family Check‐Up (FCU) (interview, assessment, feedback) [modelled on Drinkers’ Check‐Up], resulting in collaborative decision to receive behaviorally oriented parent group intervention, or individually based family therapy, or multisystemic family therapy. 115 families (23%) elected to receive Family Check‐Up Control: No stated intervention. "We did not deliver any intervention components to any control participants". |
|
| Outcomes | Self reported. Previous month tobacco use, on scale 0 = never, 6 ≥ 20 times; and at age 18 ‐ 19 Composite International Diagnostic Interview (WHO, 1997) for lifetime diagnosis of nicotine dependence or withdrawal Follow‐up: Spring semester of 6th ‐ 11th grades (age 11 ‐17). |
|
| Notes | Quality of intervention delivery: No statement on how many students attended SHAPe 6 session in school programme. No process analysis; families more likely to engage in FCU therapy if biological father not present, youth reports of elevated family conflict and deviant peer affiliation, and teacher reports of elevated risk behaviour at school (all P < 0.05). Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Yes. Was a correction for clustering made? No, not required as students individually randomised. Were appropriate statistical methods used? Descriptive statistics and correlations between variables. Mplus 4.1 Complier Average Causal Effect model to "identify a subset of the randomised control group that resembles those who do actively engage in a voluntary intervention.. This group of control families should provide the most accurate picture of how youths receiving the FCU would have developed without intervention". Never‐smoking prevention cohort data provided for analysis, but only for cohort 1 (cohort 2 still ongoing). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Students were randomly assigned…". "Youths were randomly assigned at the individual level to either control or intervention classrooms….schools agreed to randomisation of students to a family resource center (FRC)". E‐mail from Dr. Connell 29.01.2012: randomisation with random number generator Clusters: None Cluster constraint: None Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 998 agreed to participate, 498 allocated to control (99 lost to follow‐up by age 18 ‐ 19), 500 to intervention (106 lost to follow‐up by age 18 ‐ 19). No statement on how many students attended SHAPe 6‐session in school programme; 23% of families elected family therapy; no differential attrition analysis; however intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
Conner 2010 (I).
| Methods | Country: UK
Site: 20 schools (65 classes) in a Local Education Authority in northern England. Focus: Smoking rates (self reported and measured by CO), attitudes to smoking. Design: Cluster RCT (Group 1: never smoking prevention cohort). |
|
| Participants | Baseline: 1551
Age: 11 ‐ 12 yrs.
Gender: 792 M, 759 F. Ethnicity: Not stated Baseline smoking data: Self reported smoking at baseline: control 1 = 3.6%, control 2 = 3.5%, intervention 1 (Implementation intention) = 5.7%, intervention 2 (self efficacy) = 3.0%. Coding: not smoked last term = 0; smoked last term = 1. |
|
| Interventions | Category: Social influences vs control (acknowledgement active control). [tobacco refusal intention skills + tobacco information vs intervention 2 (self efficacy in tobacco refusal + tobacco information) + control groups (tobacco information + schoolwork completion implementation skills)]. Programme deliverer: Not stated; research assistant assessed carbon monoxide levels on subsample. Intervention:
Control:
"Participants in all conditions read information against smoking and committed to not smoking (i.e. an active control)". |
|
| Outcomes | Smoking rate: never, or smoked once, or used to smoke sometimes = 0; sometimes now = 1 (differs from baseline measure); random sample of 305 for CO testing. Follow‐up: 48m. |
|
| Notes | Quality of intervention delivery: No process statement. "On average participants were present on 6.2 of the 8 testing occasions … Those in control Condition 1 (M = 6.53, SD = 1.55) were present on significantly more testing occasions than those in the other 3 conditions (M = 6.09, SD = 1.85), F (1, 1336) = 7.76, P < 0.01. However, number of times participants were present did not influence measures of smoking at 48 months". Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Yes. ITT calculated as last response carried forward. Due to high attrition, > 64% of the data in all arms of the study is imputed data. Was a correction for clustering made? Yes. Were appropriate statistical methods used? In analysis, Controls 1 and 2 were amalgamated with Intervention 2 (efficacy group) as no differences. Х² to compare smoking rates between groups; Multilevel modelling with HLM6 for multivariate analyses; logistic multilevel modelling (Bernoulli model) for outcome variables at 48m. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Classes of adolescents (aged 11 ‐ 12 yrs) were randomly allocated…". No method of randomisation stated. Clusters: Classes Cluster constraint: None stated. Baseline comparability: Intervention 1 (implementation condition) more friends smoking (P < 0.001). Intervention 1 baseline self report smoking 5.7% compared to all other groups at 3%. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The objective measure of smoking was conducted by a research assistant blind to condition". |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Analysable sample = 1338. Excluded 213 pretest participants; author correspondence "The excluded 213 were missing because one or more of the baseline measures were missing ‐ we could work out which variables were missing if that were important. You are correct that it is unclear whether participants were excluded before or after randomisation. Indeed as it was classes that were randomised then in effect participants were excluded after randomisation when it became clear that they had missing data on the time 1 baseline measures". High levels of loss to follow‐up over the 48m (control 1 = 64%, control 2 = 69%, intervention 2 = 74%, intervention 1 = 77%). Author correspondence: "The drop outs at each of the time points is attributable to participants not being present on the day of testing. As we note in the paper the ITT analyses we perform for the self‐report measure assume no change in smoking status since the last time the participant was present for testing and provided data". N at 24m = 998 (75% of 1338) and at 48m = 397 (30%) so main attrition was between 24 and 48m. "To examine the effects of dropout we compared our final sample (N = 1,338) for the self‐reported smoking measure to those lost to follow‐up (N = 213) on the baseline measures. Chi‐square tests indicated no significant differences on sex, attitudes, friends smoking, or family smoking, X² s(1) < 2.12, ps > .15 (two‐tailed). This confirmed that our final sample for the self‐reported smoking analyses was not biased in relation to the initial sample. Similarly, in relation to our final sample for the objective measure of smoking, we compared our final sample (N = 305) to those lost to follow‐up (N = 1,246) on the baseline measures. Chi‐square tests indicated no significant differences on sex or attitudes, χ² s(1) < 3.10, PS > 0.08 (two‐tailed). However, those who completed the smoking objective measures had fewer smoking friends, χ² (1) = 8.88, P < 0.01 and fewer family members who smoked at baseline χ² (1) = 8.71, P < 0.01." No differences at 48m follow‐up comparing Intervention 1 to Intervention 2 + Control 1 and 2 on gender, attitudes to smoking or family smoking. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Conner 2010 (SE).
| Methods | See Conner 2010 (I) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (SE) within Conner 2010 (I) | |
Crone 2003.
| Methods | Country: Netherlands Site: 26 schools that provided lower secondary education. Focus: Smoking prevention. Design: All 54 community health services (except 3 already involved in another project) were invited to participate; 14 services provided the names of 48 schools and 18 agreed; 4 community services approached the researchers directly and recruited 8 schools. Cluster RCT (Group 1: never smoking prevention cohort, not included in analysis). | |
| Participants | Baseline: 2562 (1444 intervention; 1118 control group) in 154 classes.
Age: Average 13 yrs Gender: Intervention: 49.5% M, control: 60.9% M. Ethnicity: No data Baseline smoking data: From short‐term follow‐up: nonsmokers in intervention = 519, in control = 328; from longer term follow‐up: nonsmokers in intervention 352, in control 249. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Teachers ("Stivoro and the researchers trained the intervention schools in the use of the intervention and the procedure of the study activities"). Intervention: 3 lessons on knowledge, attitudes and social influences, class agreement not to smoke, class competition (for entry class had to have < 10% smokers after 5m); 2 optional video lessons. Control: Intervention and control schools continued to use usual anti‐smoking programmes. |
|
| Outcomes | Self reported smoking: Experimenting; weekly; daily. Follow‐up: Approximately 7m and 19m after baseline measurement. |
|
| Notes | Quality of intervention delivery: Stivoro and Trimbos Institute "supported the schools in all activities concerning the intervention ... and looked at adherence to the protocol in the intervention", but no data on adherence were provided. Statistical quality: Was a power computation performed? A power calculation indicated that 1400 students were needed in both the intervention and control groups to find a difference in the increase in smoking of 5% with power of 80% and α of 0.05 and ICC of 0.075. Was an intention‐to‐treat analysis performed? Yes Was a correction for clustering made? Yes, multilevel analysis. Were appropriate statistical methods used? multilevel techniques. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by toss of a coin by an independent person. Clusters: Schools Cluster constraint: Schools were stratified on size and their use of a frequently used national drug programme. Baseline comparability: Significantly more boys in intervention group at baseline. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | At 1 yr Intervention = 537, Control = 414 (63% attrition after 12m, and 3 schools dropped out). Nonresponse higher among smokers, especially in control group. Drop‐outs were examined in an ITT analysis under 3 assumptions (started smoking; stopped smoking; or did not change behaviour) with persistent lack of effect on the long‐term outcome. |
| Selective reporting (reporting bias) | Unclear risk | No statement |
Crone 2011.
| Methods | Country: Netherlands
Site: 151 classes in 121 elementary schools in five community health centre regions (intervention = 78 classes in 62 schools, control 73 classes in 59 schools). Focus: Prevention of smoking onset in adolescence. Design: Cluster RCT (Group 1: never smoking prevention cohort). |
|
| Participants | Baseline: 3173 baseline survey.
Age: 10 – 12 yrs
Gender: 53% F Ethnicity: 92% industrialised. Baseline smoking data: : From grade 6 follow‐up: nonsmokers in intervention = 1311, in control = 1022; from grade7 follow‐up: nonsmokers in intervention 787, in control 611. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Teachers (received training from community health centre). Intervention: 6 lessons of 1 hr each. Lessons 1 ‐ 3 in 5th grade: information, attitude to smoking and expressing intention not to smoke. (projects, discussions, parent meetings). Lessons 4 ‐ 6 in 6th grade: factors influencing smoking, skills to express opinion, social pressure, strengthen intention not to smoke (discussion, videos, role‐playing, nonsmoking certificate, campaign materials). Control: Usual treatment. |
|
| Outcomes | Self report. Smoking categorised as 1) non‐current smoker: never smoked, only smoked once; and quitters 2) current smokers: experimenters with smoking or smokers weekly or monthly. Before and after the lessons in 5th, after lessons in 6th grade, 1 yr after lessons in 6th grade. |
|
| Notes | Quality of intervention delivery: "47% of students in the intervention group received all activities in the 5th grade and 31% received all activities in 6th grade. The activity less often provided was planning how to react to social pressure towards smoking". Statistical quality: Was a power computation performed? Yes; 1400 students needed in both intervention and control groups for difference of 5% in smoking increase, power 80%, α = 0.05, ICC = 0.075. Was an intention‐to‐treat analysis performed? Yes in addition to complete case analysis. "ITT analyses were conducted to assess potential bias due to selective nonresponse. Effect sizes were calculated for the significant intervention effects on behavioural determinants at the last measurement …Stratified analyses were conducted to assess whether the effects differed for gender, educational level, or socio‐economic status". "To assess the potential effect of selective drop out, we conducted an “intention‐to‐treat” analysis on the basis of the assumption that drop outs did not change their smoking since their last measurement, last observation carried forward. This did not change the effect (OR=0.67, 95% confidence interval (95% CI)=0.47–0.97)". Was a correction for clustering made? Yes. Were appropriate statistical methods used? Multilevel techniques for clustering, linear and logistic regression. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "we ranked the schools by community health centre region. Within each region, the schools were randomly assigned to either the intervention or the control group. This was done by asking an independent person to toss a coin". Clusters: Schools Cluster constraint: Ranked Baseline comparability: "The intervention group more often had a Christian religion [p<.01], more often had parents with a higher education level [p<.05], and more often attended a higher level secondary school [p<.001] than the control group. There were no significant differences between the two groups in baseline behavioural determinants of smoking". "At baseline smoking was more often allowed and lessons on smoking were less often provided in the intervention schools". |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Post‐test 1 Intervention: 3%, control: 5% attrition from baseline. Post‐test 2 Intervention:16%, control: 18% attrition from baseline. Post‐test 3 Intervention: 23%, control: 24% attrition from baseline. Post‐test 4 Intervention: 42%, control: 43% attrition from baseline. "The non‐response rate did not differ between intervention and control group". "students who dropped out were more likely to be male, to have parents who were immigrants from a non‐industrialised country, to not know the work situation of their parents, to have another religion than being a Christian, and to be older. They also had a lower intention to refrain from smoking and they more often had a mother who smoked" (no significance stated). |
| Selective reporting (reporting bias) | Low risk | Outcomes reported as intended |
De Vries 1994 (High).
| Methods | See De Vries 1994 (Voc) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from the 8 high schools within De Vries 1994 (Voc) | |
De Vries 1994 (Voc).
| Methods | Country: Netherlands Site: 6 vocational and 8 high schools, Maastricht. Focus: Smoking prevention Design: Cluster RCT (Group 1: never smoking prevention cohort). | |
| Participants | Baseline: (1986) approximately 1784 (inferred from attrition rate); Intervention = 343 vocational students and 585 high school students; Control = 217 vocational and 384 high school students.
Age: 2nd grade of secondary school.
Gender: Not stated. Ethnicity: No data Baseline smoking data: Nonsmokers total population: intervention N = 426 (48.4%), control N = 304 (50.7%); nonsmokers at vocational schools: intervention N = 113 (64.6%), control N = 83 (56.6%); nonsmokers at high schools: intervention N = 313 (42.5%), control N = 221 (48.4%). |
|
| Interventions | Category: Social influences vs control [school type (vocational vs high school)]. Programme deliverer: Peer leaders and teachers (received training and manuals). Intervention: 5 x 45 min lessons: 1) Introduction, reasons for smoking; 2) Short‐term effects of smoking; 3) Pressure from peers "dealt with resisting peer pressure, which was also modelled on video. Refusal skills were practiced in role‐plays"; 4) Adults and advertising; 5) Alternatives; and decision making. Students formed their own groups and chose their own peer leaders. Teachers co‐ordinated the lessons and assisted the peer leaders. Control: Not stated. |
|
| Outcomes | Self reported smoking: (1) Never smoked (not even one puff), (2) initial smoker, tried up to 5 times, (3) quitter (4) occasional smoker, but not every week, (5) weekly regular smoker: smokes at least 1 cigarette a week, (6) daily regular smoker, smokes at least 1 cigarette a day. Weekly and daily regular smokers were combined into a 'regular smokers' category. Questionnaires were confidential. Saliva was collected and CO levels correlated with smoking (r = 0.79 to 0.85). Follow‐up: 1 yr from pretest. |
|
| Notes | Quality of intervention delivery: No process analysis. 'Students, peer leaders and teachers had their own manuals, summarizing the activities and providing instructions' Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? Not stated Were appropriate statistical methods used? Linear regression for quantitative effect measures and for binary effect measures; multi‐level analyses using VARCL. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The first author provided additional information that a table of random numbers was used for school assignment. Clusters: Schools Cluster constraint: Not stated Baseline comparability: Baseline 'regular smokers' : experimental 8.3%, control 7.4%; (vocational schools 16.2% and 15.1%; high schools 4.2 and 3.1%). No other data on baseline comparability. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "The respondents were informed that the results would be treated confidentially by the research team and that neither volunteers nor teachers had access to the data". [we assessed this as meaning that neither researchers nor participants were blinded as to intervention]. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | At 1 yr attrition was 14.3% and did not differ between the experimental and control groups. More pretest smokers (27%) dropped out than nonsmokers (13%; P < 0.001), but no differential attrition between groups. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
De Vries 2003 (Denmark).
| Methods | See De Vries 2003 (Finland) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the European Smoking Prevention Framework Approach in Denmark within De Vries 2003 (Finland) | |
De Vries 2003 (Finland).
| Methods | Countries: Denmark, Finland, Portugal, UK. [in Netherlands schools were matched but not randomised; in Spain, Barcelona and Madrid regions not randomly assigned: non‐RCTs so data excluded from this review].
Site: Schools 'European Smoking Prevention Framework Approach' (EFSA). Focus: Smoking prevention Design: In Finland, schools randomised; in Denmnark 2 regions randomly assigned, in Portugal 2 regions randomly assigned, in UK 2 health authority regions randomised. Cluster RCTs (Group 1: never smoking prevention cohort) |
|
| Participants | Baseline: 23,531, of whom 23,125 (98%) completed baseline questionnaires. Age: Average 13.3 yrs Gender: 50% F Ethnicity: Varied according to study. Majority Eupopean. Baseline smoking data: 19034 nonsmokers. | |
| Interventions | Category: Social Influences vs control (UK); multimodal [social influences + parent + community intervention] vs control (Finland, Denmark); multimodal [social influences + community] vs control (Portugal). Programme deliverer: Teachers in school. Intervention:
Control: 'Usual care' which differed between countries (not further described). |
|
| Outcomes | Self reported never‐smoker; nonsmoking deciders [had quit experimenting]; triers; experimenters [not smoking weekly]; regular [at least once a week]; and quitters [had quit after having smoked at least once a week]. Follow‐up: 2 yrs, 30m. |
|
| Notes | Quality of intervention delivery: Intervention schools implemented on average 3 ‐ 4 lessons and the control schools 1 ‐ 2; large variations in teacher training; projects understaffed in all countries; wide variations in content of intervention between countries. Statistical quality: Was a power computation performed? Yes, power calculation assumed drop‐out rate of 30% except 20% in Finland, with power = 0.095 and significance = 0.001, and differences in probability of success = 10%, resulted in recommended sample size of 2 x 1200 in countries with smoking incidence < 30% and 2 x 1500 in countries > 30% [with higher expected drop out]; target sizes amply achieved. Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Yes. Final models run with multilevel analysis. Were appropriate statistical methods used? Logistic regression to compare drop‐outs to non‐drop‐outs and compare smoking rates; exposure to lessons by t‐tests; final models run with multilevel analysis. Final models run with multilevel analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | In Finland, schools randomised; in Denmark 2 regions randomly assigned, in Portugal 2 regions randomly assigned, in UK 2 health authority regions randomised. No statement about method. Not randomised in Spain and Netherlands ("Because a Dutch substance abuse programme had been widely disseminated, it was impossible to randomly assign schools. Consequently, schools were assigned according to their own preference..."). Clusters: Schools Cluster constraint: Not stated. Baseline comparability: Groups not significantly different at baseline. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | De Vries 2006: Baseline = 19,034 nonsmokers; at 2 years = 10,751 nonsmokers; at 30m = 9282 (48.8% of 19,034); no significant differences in attrition between groups. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
De Vries 2003 (Portugal).
| Methods | See De Vries 2003 (Finland) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the European Smoking Prevention Framework Approach in Portugal within De Vries 2003 (Finland) | |
De Vries 2003 (UK).
| Methods | See De Vries 2003 (Finland) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the European Smoking Prevention Framework Approach in the UK within De Vries 2003 (Finland) | |
Denson 1981.
| Methods | Country: Canada Site: 12 elementary schools in Saskatoon. Focus: smoking prevention Design: Cluster RCT (Group 1: never smoking prevention cohort). | |
| Participants | Baseline: (1976) 604
Age: Grades 7,8 and 9 (12 ‐14 yrs).
Gender: Not stated Ethnicity: Not stated Baseline smoking data: In experimental schools 14% were regular smokers, in control schools 10%. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Researcher. Intervention: 3 lectures with films (drugs and the nervous system; choosing to smoke; advertising) over 2 school yrs. Particular emphasis on addictive nature of smoking. Control: No intervention. |
|
| Outcomes | Weekly smoking (≥ 1 cigarette a week). Follow‐up: End of grade 8. | |
| Notes | Quality of intervention delivery: Schools received between 1 and 4 lectures ("In the class which graduated in 1978, one school heard lectures A, D and B in grade 6 and lecture C at the beginning of grade 7. The other five schools received lectures A and B at the beginning of grade 7. All six schools heard lecture C at the beginning of grade 8, so that in one school it was given twice.") No process analysis. Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No Were appropriate statistical methods used? Experimental and control cohorts followed from beginning of Grade 7 to end of Grade 8. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'We chose six pairs of elementary schools, matching the members of each pair for size of enrolment and socio‐economic characteristics. By random selection from each pair we formed experimental and control groups" Method of randomisation was not stated. Clusters: Schools Cluster constraint: Pair‐matched. Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The intervention began in 1976, but only the class which graduated in 1978 received the complete programme, and that is the group analysed. 604 at baseline, 88% followed up at 1 yr. No differential attrition analysis. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Dijkstra 1999 (DM + B).
| Methods | See Dijkstra 1999 (SI + no B) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from intervention arm 2 for participants that received the booster sessions within Dijkstra 1999 (SI + no B) | |
Dijkstra 1999 (DM + no B).
| Methods | See Dijkstra 1999 (SI + no B) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from intervention arm 2 for participants that received no booster sessions within Dijkstra 1999 (SI + no B) | |
Dijkstra 1999 (SI + B).
| Methods | See Dijkstra 1999 (SI + no B) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from intervention arm 1 for participants that received the booster sessions within Dijkstra 1999 (SI + no B) | |
Dijkstra 1999 (SI + no B).
| Methods | Country: Netherlands Site: 20 of 62 health districts were approached, 15 agreed to participate, and health educators invited school boards to participate; 52 schools participated (51 classes to intervention 1(SI), 64 classes to intervention 2 (DM), 67 classes to control). Focus: Tobacco Design: Cluster RCT (Group 3: point prevalence). | |
| Participants | Baseline: Intervention 1 group N = 1221; Intervention 2 group N = 1381; Control group N = 1458. Age: Grade 8 and 9 Gender: "Boys and girls were almost equally represented" Ethnicity: No data Baseline smoking data: Smokers (combined the occasional, weekly and daily smokers = smokers): Decision‐making Group 13.5%; Decision‐making + Social Influences Group 7.5%; Control 8.0%. |
|
| Interventions | Category: Social influences vs control Programme deliverer: Teachers and peers. Intervention:
Control: No statement. |
|
| Outcomes | Self report as (1) never, not even 1 puff, (2) initial smoker, tried up to 5 times, (3) initial smoker, tried up to 5 times, not a smoker now, (4) occasional smoker, not every week, (5) weekly smoker, at least 1 a week, (6) daily smoker, at least 1 a day (combined as occasional, weekly and daily smokers = smokers; never and initial smokers = nonsmokers). Follow‐up: 16m follow‐up from main intervention. |
|
| Notes | Quality of intervention delivery: Minimal risk: 91% of teachers used the manuals; 90% used the video, 84% used activities, 87% worked with peer leaders, 91% used group activities, 78% gave out summaries to students, 75% asked students to write their name on a nonsmoking poster, and 81% handed out quit brochures. Of the students in the SI+DM condition, 73% read 1 magazine, 58% 2 and 42% 3. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Yes, missing data substituted by last recorded smoking status. Was a correction for clustering made? Not stated, but used multilevel analyses. Were appropriate statistical methods used? Multilevel analyses using VARCL and VARCL with model reduction by SPSS showed < 5% residual variance was due to between‐class and between‐school effects, and no differences between VARCL and SPSS analyses. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Fifty‐two schools from 15 district health centres were randomly assigned by the university research team to the
SI program (51 classes), the DM program (64 classes) or the control group (67 classes)". "Within the treatment condition, half of the schools were randomly assigned to the condition receiving three boosters, while the other half did not receive any boosters". Method of randomisation was not stated. Clusters: Schools Cluster constraint: Not stated Baseline comparability: Not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | At T3: DM (N = 460); DM+boosters (N = 351); Social Influences (N = 575); SI+boosters (N = 526); Control (N = 1192). 1722 at 16m (36% attrition), with students in the control compared with those in the experimental social influences decision‐making group less likely to drop out (OR 1.57; 95% CI 1.36 to 1.82), and students in the social influences programme less likely to drop out than those in the control group (OR 0.61; 95% CI 0.51 to 0.72), but the authors comment "In sum, the attitude analyses showed that at T2, T3 as well as T4 there were no significant interactions between pre‐test smoking and treatment conditions with respect to attrition". |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Eisen 2003.
| Methods | Country: USA
Site: 34 middle schools in four metropolitan school district areas; Los Angeles, Washington‐Baltimore, Detroit, Wayne County (17 schools to intervention and 17 to control). 'Lion’s Quest Skills for Adolescence' (SFA) Focus: Prevention or delaying the onset of student tobacco, alcohol, and illegal substance use. Design: Cluster RCT (excluded from analysis). |
|
| Participants | Baseline: 7426 (consent obtained, 71% of eligible population).
Age: 11 yrs (mean). Grade 6.
Gender: 51.7% F Ethnicity: Asian‐American 7.1%, N‐A 1.4%, A‐A 17.6%, H 33.9%, W 25.7%, Combination 6.9%, Other 6.3%, missing 1.0%. Baseline smoking data: Smoked cigarettes in the last 30 days = 3.5%, no cigarettes in the last 30 days = 93.4% (missing 3.2%). |
|
| Interventions | Category: Social competence vs control. Programme deliverer: Teachers (received 3 day workshop). Intervention: Multicomponent life skills education programme: utilising social influence and social cognitive approaches to teach cognitive‐behavioural skills. 1‐yr intervention in 7th grade. 40 (35 ‐ 45 min) sessions: three sessions on the challenges involved in entering the teen years, four on building self confidence and communication skills, five on managing emotions in positive ways, eight on improving peer relationships. 8 key sessions. Zero approach to all substance use. Teacher manuals and student workbooks. Control: Usual drug education programming (ranging from simple school assemblies to DARE exposure). |
|
| Outcomes | "five to seven‐point ordinal response categories (e.g. ‘never’ or ‘none’ to ‘ more than 100 cigarettes [more than 5 packs]). These ordinal indicators of lifetime and recent substance use then were recorded to 0 = no/1 = yes response categories" Follow‐up: Surveyed annually from 6th to Spring 2000 (8th grade). |
|
| Notes | Quality of intervention delivery: Not stated Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Yes. Was a correction for clustering made? Yes. Were appropriate statistical methods used? Nested cohort design. Mixed‐model regression procedures. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Two stage cluster sampling: "4 of the 10 largest metropolitan areas ranked by population size were selected at random2. 'Within each of the public districts that had at least four middle schools in the 1996‐1997 school year….met the following criteria: (1) contained grades 6‐8 or 7‐9; (2) had an enrolment of at least 200 students by the end of the eighth or ninth grade; and (3) were not using SFA at that time". "pair‐matched within each district on sixth‐grade prevalence of any recent use (previous 30 days) of tobacco, alcohol, or one of several illicit drug from the intervention survey data and on parent consent rates, then randomised to study conditions from within pairs". No method of randomisation stated. Clusters: Schools Cluster constraint: Pair‐matching Baseline comparability: "17 SFA and the 17 control schools were equivalent with respect to self‐reported drug use and tobacco prior to the seventh‐grade SFA intervention program". |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 7th grade survey – 84% of consented baseline sample 8th grade survey – 77% of consented baseline sample, 87% of those that completed the 7th grade survey. "no differential attrition evident". |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Elder 1993.
| Methods | Country: USA
Site: 22 junior high schools in San Diego County, CA (11 to intervention, 11 to control). 'SHOUT' Students Helping Others Understand Tobacco. Focus: Tobacco use prevention. Design: Cluster RCT (Group 3: point prevalence). |
|
| Participants | Baseline: 3655. Cohort of 2668, 73% of initial sample, 1174 in Experimental, 1494 in Control.
Age: mean 12 yrs (range 11 ‐ 16). Gender: "near equal proportions of M and F" Ethnicity: overall ‐ 57% W/non‐H, 24% H, 19% Other. Baseline smoking data: Smoking rates: beginning 7th grade Intervention 5% control 5.6%. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: undergraduates (received 15 hrs of training including videotaped role plays). Intervention: 7th grade: Fall: (6 lessons, 1 a week) videos of health consequences of tobacco use, celebrity endorsements of non‐use, psychosocial consequences, refusal skills, decision‐making, skits; Spring: (4 lessons, 1 a month) review of refusal methods, discussion of tobacco addiction/cessation, public declarations of non‐use and skits; 8th grade (8 lessons, 1 a month): demonstration/rehearsal of refusal skills, writing campaigns against tobacco use, community action projects, discussion groups and debates. 9th grade (booster intervention) ‐ 5 newsletters containing tobacco control events, legislation, research and tobacco industry's power, cessation tips, 2 newsletters mailed to SHOUT participants' parents and phone calls (2 per semester) following Pawtucket Heart Health Programme protocol oriented toward newsletter material, refusal skills training and cessation support (79.9% call completion rate). Control: No interventions. |
|
| Outcomes | Smoking: Any tobacco use (cigarettes and smokeless) in past month and past week. Self report surveys under 'bogus pipeline' conditions. Follow up: End of 7th, end of 8th, end of 9th grades. | |
| Notes | Elder 1993a and 1993b discrepant on number of sessions/year. See also Eckhardt 1997 which provided further intervention to the cohort. Quality of intervention delivery: No process analysis, but the 100 undergraduate volunteers were closely supervised, received academic credit, 15 hrs of training included videotaped role plays, and "attrition was rare". "Training included how to teach effectively and how to implement SHOUT lessons. The leader's role plays were videotaped and reviewed. Proficiency was evaluated by staff, and feedback was given during training and later in the field". Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Not stated. Were appropriate statistical methods used? LR and logit model ORs. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "An initial sample of 22 schools with 3655 participants was identified in fall 1988. This sample was matched by tobacco use prevalence (in past week) and school size, and randomly assigned to either a control or an intervention condition". Clusters: Schools Cluster constraint: Schools matched by tobacco prevalence use and school size. Baseline comparability: Ethnicity showed significant group differences (P < 0.001). |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Pretest: 3655. Cohort of 2668 (73% of initial sample). No differential attrition. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Elder 1996.
| Methods | Country: USA
Sites: 96 schools in Texas, California, Louisiana and Minnesota (10 schools at each site randomised to control, 7 to school‐based intervention, 7 to school and family). 'CATCH' study (The Child and Adolescent Trial for Cardiovascular Health). Focus: cardiovascular health promotion. Design: Cluster RCT (Group 1: never smoking prevention cohort). |
|
| Participants | Baseline: N at end of 5th grade: 7827, of whom 6527 gave complete information.
Age: 5th graders (age 10 ‐ 11). Gender: 51% F. Ethnicity: 71% W, 16% H; 14% A‐A. Baseline smoking data: Intervention 3845 of whom 181 ever‐smoked; Control 2682, of whom 134 ever smoked. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Teachers Intervention: 4 x 50 min sessions. CATCH used social learning theory and organizational change to intervene in school environments, class room curricula, family interventions and school smoking policies to change smoking status and cardiovascular health. CATCH intervention began in 3rd grade cohort but smoking prevention curriculum not introduced until 5th grade.
Control: No intervention. |
|
| Outcomes | % of schools with smoke‐free policies. Smoking prevalence Follow‐up: 3 yrs. | |
| Notes | Quality of intervention delivery: Of the children who began in a school which offered the school + family intervention, 47% attended such a school for the entire 3 yrs. The process analysis for the FACTS tobacco curriculum showed that 87% of teachers participated in the classroom sessions; checklists were returned for 96% of classroom sessions; 96% completed the entire lesson; and 87% were implemented without modification. For the Family Intervention for tobacco 97% of session‐specific activities were completed; 78% of adults participated in the home activities; and 48% of home team activity cards were returned; one third of schools held assemblies about tobacco; 40% participated in 'Great American Smokeout' activities; and 25% sponsored anti‐tobacco or anti‐drug clubs. Statistical quality: Was a power computation performed? No (study not designed to find a difference in smoking prevalence). Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Not stated. Were appropriate statistical methods used? Analysis was by multiple LR (including a school random effect), but school effects were not stated. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Ten schools at each site were randomly assigned to the control condition and 7 schools each to a school‐based intervention (food service, physical education, classroom curricula) or the school‐based plus family intervention program". Clusters: School Cluster constraint: Not stated. Baseline comparability: No report of differential characteristics at baseline. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 100% of 3rd grade teachers and 67% of students attended Family Fun Nights; 100% of schools remained in the dietary assessment process; no attrition analysis. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Ellickson 1990 (HealthEd).
| Methods | Country: USA
Site: 30 schools from 8 districts, California and Oregon (10 schools to each: intervention 1, intervention 2 and control). Project 'ALERT' Focus: Smoking, alcohol and marijuana prevention. Design: Cluster RCT (Group 1: never smoking prevention cohort). |
|
| Participants | Baseline: 6527 (14% baseline nonresponse due to parental refusals or absence).
Age: 7th grade (age 13 ‐ 14 yrs). Gender: 52% M Ethnicity: W 67%, H 10%, B 10%, A 8%, N‐A/mixed 5%. Baseline smoking data: At baseline 95% of students with cotinine scores that identified them as recent tobacco users (N = 603) reported cigarette use in the past month. |
|
| Interventions | Category: Social influences vs social influences vs control [Social influences delivered by teachers vs teachers + peers vs control]. Programme deliverer: Community adults (received conventional Project ALERT training), teens (school selected, 1‐day training by researchers, state co‐operative extension educators, and adult programme leaders). Intervention: 8 lessons (1 a week) in 7th grade and 3 booster sessions in 8th grade; based on social influence model with self efficacy model of behaviour change: develop reasons not to use drugs; identify pressures to use them; counter pro‐drug measures; learn how to say no to internal and external pressures; understand that most people do not use drugs; and to recognize the benefits of resistance. Participatory curriculum, with question‐and‐answer sessions, small group exercises, role modelling, and repeated skills practices.
Control: 6 schools no intervention, 4 schools continued traditional drug education programmes. |
|
| Outcomes | Analysis based on 3 risk levels for future smoking at baseline (Non‐user: never / Experimenters: tried but < 3 times in yr before baseline and not in month prior to baseline / Users: 3 times in past year and any use in prior month to baseline). Saliva cotinine levels obtained and analysed. Follow‐up: 15m and age 23. | |
| Notes | Quality of intervention delivery: In a process analysis 17 monitors observed 950 of the 2300 lessons and found that every scheduled class was delivered, and in 92% of the observed classes all lesson activities were covered. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Not stated (individual level and school level analyses performed). Were appropriate statistical methods used? LR, student level analyses to assess curriculum's effectiveness according to risk level (non‐user, experimenters, users), common covariates used included district, dummy variables for Black/Asian ethnicity and a composite variable (peer/family use and attitudes, personal beliefs and background variables; individual level analyses were used as they produced more conservative results than school level analyses. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The method of sample blocking is stated, but method of randomisation not stated ("The 30 schools were randomly assigned to one of three experimental conditions"). Email from author 19 Jan 2012: "we can't find original (25 year‐old) documentation describing the randomisation method, but both the statistician for Study 1 and I have the same recollection, i.e. that we used a random numbers table". Clusters: Schools Cluster constraint: Sample blocking by district and restricted assignment to minimise imbalance in school test scores, language spoken at home, ethnic and income of catchment areas. Baseline comparability: Groups were equivalent at baseline. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 yrs (9th grade) approximately 72% of baseline; Analysis sample = 59% (N = 3852) had data for first 4 points. 53‐57% attrition between grade 7 and 12 (18% lost as moved, 25% failed to take the 10th or 11th grade survey). Students lost from the analysis significantly more likely to have baseline characteristics (low grades, family disruption, early drug use) linked with later drug use. At 24 months; "We found no evidence that either attrition rates or which students were lost from the analysis varied across experimental conditions". At 6 years: "We found no evidence that treatment affected either the frequency of sample loss or the characteristics of those who were lost". At 10‐yr follow‐up, N = 3,056 (60% of baseline). |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Ellickson 1990 (Teen).
| Methods | See Ellickson 1990 (HealthEd) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (led by peer teen leaders) within Ellickson 1990 (HealthEd) | |
Ellickson 2003.
| Methods | Country: USA
Site: 55 South Dakota middle schools (high schools and their associated middle school feeders). Project 'ALERT' Focus: Drug, alcohol and tobacco prevention. Design: Cluster RCT (Group 1: never smoking prevention cohort). |
|
| Participants | Baseline: 5412 enrolled, of whom 4669 (86.6%) completed the baseline survey (2810 Revised project ALERT, 1879 Control).
Age: 7th graders.
Gender: 50% F Baseline smoking data: ⅓ had tried cigarettes. |
|
| Interventions | Category: Social Infuences vs social influences vs control. Programme deliverer: Teachers (received 1‐day training workshops, manuals and videotaped lessons). Intervention:
Control: Other prevention curricula (not described). |
|
| Outcomes | 1. Self reported ever, past month and weekly smoking.
2. Saliva samples collected, and analysed for a random sample of 654 (only 3 (0.5%) of the 560 who reported not smoking in the prior month or 2 days had saliva cotinine concentrations > 10 ng/ml; 1.7% gave inconsistent responses at baseline; 1.5% at follow‐up, and 6.5% across waves). Follow‐up: 8 to 10th grade. |
|
| Notes | Quality of intervention delivery: "Teacher reports for 1446 lessons indicated that they covered all or some of each activity in 88% of the 7th‐grade lessons and 93% of the 8th‐grade lessons. However, 1 or more activities were rushed in 40% of the 7th‐Grade lessons and 31% of the 8th‐grade lessons...Overall just 9% of the lessons were interrupted by external events such as fire drills, school announcements or shortened class periods". Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Yes Was a correction for clustering made? Yes Were appropriate statistical methods used? Generalized estimating equation to account for ICCs, with adjustment for multiple covariates, including school geographic location and community size; missing data imputed using Bayesian model. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Fifty‐five South Dakota middle schools were randomly assigned to program or control conditions". "Schools were organized into three strata by community size and type (city, town, rural community). Blocks of school clusters consisted of 3 clusters from the same stratum located in the same geographic region of the state. Within each block, 1 school cluster was randomly assigned to each experimental conditon. Across blocks, we restricted the allowable assignments to those that reduced the imbalance among experimental conditions based on district enrolment, an index of school academic performance and socioeconomic status, and the existence of a drug prevention program in the district". Clusters: Schools Cluster constraint: Stratified by community size and type. Strata divided according to geographical region and then placed in blocks of three. Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Baseline enrolled 5412, of whom 4669 (86.6%) completed the baseline survey; and 18m after baseline 4276 followed up in 8th grade. Analysis sample = 4276 (2553 revised Project ALERT, 1723 control). No differential attrition across groups, "attriters tended to be students at greater risk for substance use". |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Ennett 1994.
| Methods | Country: USA
Site: 36 elementary schools, Illinois. Project 'DARE' Focus: Drug abuse prevention. Design: Cluster RCT (Group 1: never smoking prevention cohort). |
|
| Participants | Baseline: 1803
Age: 33% 5th and 67% 6th grade (age 10 ‐ 11 years).
Gender: 49% F
Ethnicity: 54% W, 22% A‐A, 9% H. Baseline smoking data: 20% had smoked cigarettes. "only adolescents who reported no lifetime use at Wave 1 are included in analyses indicating initiation at Waves 2, 3 or 4". |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Uniformed police officers. Intervention: 1 hr a week x 17 weeks. DARE curriculum: see Clayton 1996. Control: Unspecified, but likely to have included some drug‐education programme. |
|
| Outcomes | Smoking: Initiation (for those reporting no use at baseline); Increased use (for those reporting past 30 day use); quitting (for those reporting current use). Follow‐up: Post‐test, 1 yr (6th or 7th grade) and 2 yrs. Participants were tracked to their middle schools. | |
| Notes | Quality of intervention delivery: No process analysis; and usual drug education varied across the control schools. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Nested cohort to adjust for unit of analysis. Were appropriate statistical methods used? For continuous measures analysis used least squares regression and expressed results as regression coefficients; for categorical data used LR with results expressed as ORs. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "..a convenience sample of 18 pairs of elementary schools in northern and central Illinois that were stratified by metropolitan status (i.e., urban, suburban and rural). Within strata, school pairs were matched closely by ethnic composition, number of students with limited English proficiency, and the percentage of students from low income families. ...Six pairs of schools serving urban and suburban areas were randomly assigned either to receive DARE in the spring of 1990 or to the control condition. The remaining six pairs of schools in rural areas were assigned to DARE or control conditions using a nonrandom procedure because of the travel time and scheduling requirements for DARE officers ...". Method of randomisation not stated. Clusters: Schools Cluster constraint: Stratified by metropolitan status. Within strata pair‐matching of schools based on ethnic composition, English proficiency, and percentage from low income families. Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Extensive procedures were instituted to demonstrate assurances of confidentiality to students". [we assess this as meaning neither students nor researchers were blinded]. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was 12% (defined as students dropping out by the end of 2nd yr) and 26% (defined as students missing at 1 or more of 4 data collection points). More urban students and those with more positive attitudes towards drugs dropped out, but there was no differential attrition across conditions. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Faggiano 2008.
| Methods | Country: Austria, Belgium, Germany, Greece, Italy, Spain, Sweden.
Site: 170 schools EU‐Dap school prevention program called ‘Unplugged’. Focus: Delay onset of cigarettes, episodes of drunkenness and cannabis use. Design: Cluster RCT (Group 1: never smoking prevention cohort). |
|
| Participants | Baseline: 7079 (from 143 schools).
Age: 12 – 14 yr olds (27.2% = 12 yrs, 34.9% = 13 yrs, 37.9% = 14 yrs).
Gender: 52% M Ethnicity: Not stated. Baseline smoking data:
Nonsmoker past 30 day smoking (first analysable sample, N = 6370): control = 68.9% (N = 1719/3059 [total number of students answering the question]), pooled intervention = 75.2% (N = 2052/3098[total number of students answering the question]). |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Classroom teachers (received 2½ ‐ 3 day training course). Intervention: 12 1‐hr sessions to be delivered weekly. 3 formats:
Control: "usual curriculum". |
|
| Outcomes | Self report. Own lifetime, past year, current use and past 30 days use of cigarettes. Past 30 day use: 1) any cigarette smoking; 2) frequent cigarette smoking (6 ≥ cigarettes); 3) daily smoking (20 ≥ cigarettes). Follow‐up: At least 3m post‐intervention (approximately 6m, though discrepancy in the text) and 18m post‐intervention. |
|
| Notes | Quality of intervention delivery: "56% of the enrolled classes implemented all the units in the curriculum, while 66% received at least 10 units and 77% of classes were taught at least 50% of it. Less than 5% of classes failed to implement any part of the curriculum. On average, each unit was taught to 78% of the target population. This level of program implementation is comparable to that of other curricula administered in a European setting". "degree of implementation of the peer program was low in all centres. Very few classes conducted all seven of the planned meetings (8%), while 71% did not conduct any meeting at all". "degree of implementation of the parents programme was high…however, the average attendance was very low at 12 parents per seminar". Statistical quality: Was a power computation performed? Yes. Was an intention‐to‐treat analysis performed? Both complete case and ITT analysis completed (last observation carried forward). Was a correction for clustering made? Yes. Were appropriate statistical methods used? Students unit of analysis. Chi². Multilevel modelling (centre, class and students). Sensitivity analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "a complete list of schools in each centre’s catchment area was obtained, and stratified into three socio‐economic strata". Inclusion criteria: at least two classes at correct age level, mainstream education system, consent to participate, not currently undertaking any intervention, able to implement in the following school year. Email from author 25 January 2012: "the randomisation was performed centrally (to ensure the allocation concealment) using a computer software". Clusters: Schools Cluster constraint: Stratification. Baseline comparability: "baseline imbalance in the prevalence of substance use between intervention and control condition, with the control group showing consistently higher prevalence". "prevalence appeared to be due to the inclusion among the controls of a single large school…..unusually high prevalence of substance use….excluding this school, the baseline prevalence was very similar between arms…..no other school characteristic in either centre or stratification level could be linked to difference in prevalence of substance use". |
| Allocation concealment (selection bias) | Low risk | "randomisation of the schools arms was carried out centrally (Turin, Italy) ... using computer software". |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "27 schools (15.9%, 23.5% in intervention arms and 4.4% in controls) dropped out following the assignment to a study arm" (3 control, 24 intervention) "since all of the intervention schools that dropped out from the study did so during, of just after the teachers’ training course, the most likely explanation is that there was an initial underestimations of the intervention commitment among some teachers"; the drop out "was comparable in all centres, and similar across the three levels of area social stratification". "After baseline two schools dropped out, one from the control arm and one from the intervention arm corresponding to 119 students". 590 student surveys could not be matched to pretests. 90% of the original 7079 did the post‐test and could be matched to pretest (first analysable sample = 6370). "5 schools refused to continue during the 18 month follow‐up, two from the intervention arm and three from the control arm. Reasons…lack of time….disapproving questions about inhalants…mistrust of confidentiality". "Across all centres 81.3% of the records generated by the students at baseline could be linked to those generated at second post‐test" (second analysable sample = 5541). "students who could not be linked at the 18 month follow‐up showed significantly higher baseline prevalence of past 30‐day substance use compared to those retained in the analysis". |
| Selective reporting (reporting bias) | Low risk | Outcomes reported as intended. |
Figa‐Talamanca 1989 (F).
| Methods | Country: Italy Site: 4 schools; one professional or technical school in each of Perugia, Cagliari, Pavia and Genova. Focus: Smoking prevention and cessation. Design: Cluster RCT (Group 1: never smoking prevention cohort). | |
| Participants | Baseline: 562
Age: 15 ‐ 17 yrs. Gender: 47% F Ethnicity: Not stated. Baseline smoking data: Never smoked 51.7%; ex‐smoker 14.8%, occasionally 14.3%, everyday 19.1%. |
|
| Interventions | Category: Other interventions vs control. This intervention did not align with the main five categories; the programme intervenes by promoting discussions of motivations for smoking. Programme deliverer: Health education specialist. Intervention: 3 sessions over 3 days. Creating awareness of smoking as a cultural, economic, social and health problem; information on physiology of respiratory and cardiovascular systems, motivation for smoking, role of media:
Control: No intervention. |
|
| Outcomes | Smoking: Everyday (1 ‐ 4 cigarettes a day; 5 ‐ 9; 10 ‐ 19; 20+)/ occasionally/ex‐smoker/never smoked. In intervention classes students coded and analysed the baseline questionnaire themselves. Follow‐up: 12m. | |
| Notes | Quality of intervention delivery: No process analysis. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? Comparison of % smoking in the experimental and control schools. No statistical analysis for tobacco outcomes other than percentages. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Health Education Specialist selected a school in each of the 4 cities willing to participate. "In each school, six classes were selected (ages 15 ‐ 17) and randomly assigned to one of three experimental groups A, B and C". Method of randomisation was not stated. Clusters: Classes Cluster constraint: Not stated. Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was 7%; no adjustment for attrition. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Figa‐Talamanca 1989 (N.F).
| Methods | See Figa‐Talamanca 1989 (F) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (no forum) within Figa‐Talamanca 1989 (F) | |
Flay 1985.
| Methods | Country: Canada
Site: 22 schools in 2 counties of Ontario. 'The Waterloo Smoking Prevention Programme'. Focus: Smoking prevention. Design: Cluster RCT (Group 2: change rates). |
|
| Participants | Baseline: 654 (94% of target population).
Age: 6th grade (age 11 ‐ 12 yrs). Gender: Not stated. Ethnicity: Not stated. Baseline smoking data: 42% never‐smokers. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Not stated Intervention: 6 x 1hr weekly sessions in Grade 6 on information and attitudes to smoking; family, peer and media influences on smoking; decision‐making and commitment. 2 maintenance sessions in grade 6, 2 booster sessions in 7th grade and 1 in 8th. "The activities were designed to start the development of future attitude and behavior changes and the acquisition of social skills. The information was elicited from the children rather than provided for them.... The second ... component of the program focused on social influences to smoke (family, peer, media) and the development of skills to resist such pressures. Again, ideas were elicited form the children and repetition achieved by the use of multiple modalities. Specific coping skills, such as saying "No thank you, I don't smoke" were taught, role played and practiced". Control: Usual health education. |
|
| Outcomes | Self reported smoking; never/tried once/quit/experimenter/regular. Regular smokers divided into ≤ 3 a week; and > 3 a week. Saliva for thiocyanate levels. Follow‐up: 18m (end of grade 7), 5 yrs (grade 11), 6 yrs (grade 12). | |
| Notes | Quality of intervention delivery: No statement about numbers present at intervention and boosters other than absenteeism analysis; no process analysis. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Not stated. Were appropriate statistical methods used? Analysis was both for the individual and the school, X². |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "On average, unmatched schools were not different in size, geographic location, or SES from those that were matched and subsequently included in the study. Assignment to treatment or control conditions from the matched groups was random except in three cases in Oxford County, where an administrator thought that principals might not cooperate as fully if their schools were assigned to the control condition". Method of randomisation not stated. Clusters: Schools. Cluster constraint: Schools matched on size, rural/urban location and SES. Baseline comparability: Mean age of controls higher (P < 0.001). |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 4.3% per year; absenteeism was 5.2%. Baseline N = 654, analysis sample at 2‐yr follow‐up = 498 (76%) present at all tests. No between‐group differences. At the 6‐yr follow up 90% of students were traced and data obtained from 80% of these; 17% of drop‐outs were experimenting with smoking compared to 12% of the sample (OR 1.84; 95%CI 1.04 to 3.28), and students 9 ‐ 11 at pretest more likely to be retained compared to 12‐yr olds at pretest (OR 2.53; 95%CI 1.45 to 4.39). |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Flay 1995.
| Methods | Country: USA
Site: 340 classes in 6 school districts with 35 Los Angeles and 12 San Diego schools. 'Television, School and Family project' (TVSFP). Focus: Tobacco Design: Cluster RCT (excluded from analysis). |
|
| Participants | Baseline: 7352 (6695 (91%) indicated gender, race and smoking status). Age: beginning of 7th grade (approximately 12 yrs). Gender: 49% M Ethnicity: 35% H, 33% W, 14% A‐A, 17% Other. Baseline smoking data: never‐smokers: intervention N = 112, control N = 81. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Trained health educators. Intervention: (a) correction of misperceptions about tobacco usage; (b) awareness of peer influences to smoke; (c) development of peer resistance skills; (d) awareness of family influences to use tobacco; (e) development of media influences resistance skills; (f) social and physiological effects of smoking; (g) development of decision‐making skills. Control: No intervention. |
|
| Outcomes | Self reported smoking for the past week (test‐retest stability 0.26 between waves B and C, and 0.31 between waves C and D); ever‐use in lifetime (test‐retest stability 0.71 between waves B and C, and 0.72 between waves C and D). Follow‐up: End of grade 7, 1 yr post‐intervention, 2 yrs post‐intervention. |
|
| Notes | Quality of intervention delivery: Numerical results of process analysis not stated; "Instructors completed delivery process questionnaires daily, weekly and immediately post program. Classroom teacher observers were surveyed weekly. The school staff was interviewed during the week immediately following the class session". Parents signed when student‐parent homework was complete; the authors commented "Fidelity of implementation was assured through curriculum delivery by trained health educators [but] Unfortunately the television programming was poorly executed and there was significant variability in the integrity of classroom program delivery". Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Yes. Were appropriate statistical methods used? Results were adjusted for clustering using ML3 multilevel analysis programme for unbalanced data that uses iterative generalized least‐squares estimation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Within each of two counties (Los Angeles and San Diego) we assigned entire schools to conditions (22) using a randomised multi‐attribute blocking approach developed by Graham et al". Method of randomisation not stated. Clusters: Schools. Cluster constraint: Multi‐attribute blocking. Baseline comparability: No differences at pretest in smoking rates across conditions. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 53% attrition at 2 yrs, with higher attrition among African‐Americans, and students with lower school grades, but there was no differential attrition across groups. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Focarile 1994.
| Methods | Country: Italy Site: Health District of Rozzano, Milan (53 classes). Focus: Smoking prevention Design: Cluster RCT (excluded from analysis). | |
| Participants | Baseline: 1268 registered students; 1057 (83%) were registered in the randomised classes and 1057 were randomised (508 intervention, 549 control);
Age: 12 ‐ 13 yrs. Gender: 50% F Ethnicity: Not stated. Baseline smoking data: No data. |
|
| Interventions | Category: Social Influences vs Information. Programme deliverer: Volunteer teachers. Intervention: 6 lessons over 3m. Social influences, resistance skills training, based on Waterloo Smoking Prevention Program. Control: Programme of information on cardiovascular risks (including the risk of smoking). |
|
| Outcomes | Never‐smoking; 1 cigarette a month; 1 cigarette a week; > 1 cigarette a week; < 7 cigarettes a week; > 1 cigarette a day. Follow‐up: 18m. At 36m only pupils in classes which completed the programme were followed up. Some were sent postal questionnaires and some contacted by telephone. | |
| Notes | Quality of intervention delivery: The analysis at 36m is limited to the classes which delivered ⅔ of the material, and was limited by the resources available for telephone follow‐up; no process analysis. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Yes. Were appropriate statistical methods used? Results were adjusted for clustering with LR and binomial LR. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Nel Settembre del 1987 53 classi seconde medie del Distretto Scolastico corrispondente sono state suddivise in quattro strati, in funzione dell'abitudine al fumo dell'insegnante (= fumatore si/no) disponibilie a realizzare l'intervento ed al rischio sociale (= basso/alto) della classe per l'abitudine al fumo. Sone state quindi assegnate, con procedura randomizzata, basata su una tavola di numeri casuali...". Randomly allocated using table of random numbers. Clusters: Classes Cluster constraint: Stratified by baseline smoking and risk factors. Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Students with a high risk of smoking had a lower response rate; attrition at 36m was 60%. Follow‐up at 36m: 420 (222 intervention, 198 control). |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Forman 1990 (SI ‐ NP).
| Methods | See Forman 1990 (SI) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from intervention 2 where no parent attended in Forman 1990 (SI) | |
Forman 1990 (SI ‐ P).
| Methods | See Forman 1990 (SI) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from intervention 2 where the parent attended in Forman 1990 (SI) | |
Forman 1990 (SI).
| Methods | Country: USA
Site: All 30 secondary schools in south‐eastern metropolitan area. Focus: To evaluate the effectiveness of personal and social coping skills training, with generalization programming in the social environment of the school and home, in preventing substance use in high risk adolescents Design: Cluster RCT (Group 2: change rates). |
|
| Participants | Baseline: 327
Age: 14.72 yrs.
Gender: Not stated. Ethnicity: W 74%, B 24%, Other 1%. Baseline smoking data: never smoked: school intervention 26%, school and parent intervention 32%, control 27%; used to smoke but quit: school intervention 14%, School and parent intervention 20%, control 18%. |
|
| Interventions | Category: Social competence vs control [social competence and information vs competence control] Programme deliverer: Project Personnel (Master’s degree in a human service discipline and experience working with youth). Intervention:
Control: Students attended a structured group that provided attention and focused on self awareness and building a cohesive support group. Students receive the same training schedule as the school intervention. Content adapted from a state school‐based substance abuse programme. |
|
| Outcomes |
Results for intervention 2 were split between where parent did attend (SI ‐ P) and where parent did not attend (SI ‐ NP). Follow‐up: Pre and post‐test plus 1 yr. |
|
| Notes | Quality of intervention delivery: All sessions recorded and coded by independent raters to establish intended implementation of the interventions. Intercoder agreement > 90%. "Among the coping skills training groups, half of the sessions covered at least 80% of the planned activities as designed. The average completion rate of intervention activities across all coping skills sessions was 74%. Nearly two thirds of the students completed 9 or 10 of the intervention sessions, and 91.9% completed at least 7 sessions. 44% of the students in the School Plus Parent intervention condition had at least one parent participate in the parent training group sessions. Of the parents who came to the first meeting 66.1% attended all five sessions. 74% of the parents attended at least 4 meetings". Saliva samples collected with a bogus pipeline procedure to enhance the validity of self report results. Statistical quality: Was a power computation performed? Not stated. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Analysis both on individual and cluster basis. Only individual analysis reported as results similar. Were appropriate statistical methods used? Mean plus SD table; repeated measures multivariate analysis; multiple ANOVA. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Schools "were matched into groups of three on the basis of secondary level (middle vs high school), racial composition, percentage of students receiving free lunch, and school size so that each matched cluster contained schools that were most similar to each other with regard to these characteristics. Within each cluster, schools were randomly assigned to three treatment conditions". Method of randomisation not stated. Participants within a school selected by staff referral based on observations of high risk characteristics (two or more of: no. of disciplinary incidents, low grades, unexcused absences, drug or alcohol abuse by family member, low self esteem, social withdrawal, experimental substance use). Clusters: School groups. Cluster constraint: Matched groups of three based on secondary school level, racial composition, percentage of students receiving free lunch, and school size. Baseline comparability: never‐smokers: school intervention group 26%, school + parent intervention 32%, control 27%; race (White) School 83%; School + parent 71%, Control 68% (no significances stated). |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Analysis sample = 279 completed the pre‐ and post‐treatment assessment sessions (85.3%). Non‐completing students: 41.7% no longer attended the school, 50% withdrew voluntarily, 8.3% withdrawn due to disruptive behaviour. 201 (72%) completed a booster intervention and follow‐up assessment. Non‐completing students: More than 90% no longer attended the school, 5.1% refused to participate. No differential attrition analysis. |
| Selective reporting (reporting bias) | Low risk | Purpose of study clearly stated and all expected outcomes provided. |
Gabrhelik 2012.
| Methods | Country: Czech Republic
Site: 74 schools in 3 regions (40 intervention, 34 control). Focus: Alcohol, tobacco, inhalants, illegal drugs. 'Unplugged' Design: Cluster RCT (Group 1: never smoking prevention cohort). |
|
| Participants | Baseline: 1874 (1022 experimental, 852 control).
Age: 11 yrs (mean)
Gender: 49.5% F Ethnicity: Czech, others not stated. Baseline smoking data: never‐smokers: intervention = 917/1022 (7 missing), control = 787/852 (1 missing). |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Teachers (received 2½ hrs of technical training and 12 hrs of theoretical and direct practical training). Intervention: (12 lessons x 45 mins over 1 school yr): Czech translation of “Unplugged” used in EU‐Dap intervention (Figganio 2008). 4 units knowledge and attitudes, 4 units interpersonal skills, 4 units intrapersonal skills. Changes include "a new lesson order, changed graphics in student workbook, shortened lessons for easier implementation, and added innovative ‘ice‐breaker’ activities in the teacher’s handbook". Van der Kreeft (2009) states that in the 4 units of interpersonal skills students practised refusal skills, assertiveness, and analysed coping strategies. Gabrhelik implemented only the classroom intervention from the EU‐Dap intervention described by Faggiano (2008) and not the Classroom curricula with side activities involving peers or involving parents. Control: ‘Minimal Prevention Program ‘ targeting alcohol, tobacco and other drugs, and other risk behaviours (mandatory in Czech Republic). |
|
| Outcomes | Smoked cigarettes last 30 days, smoked ≥ 6 cigarettes last 30 days; smoked ≥ 20 cigarettes last 30 days. Follow‐up: baseline = Wave 1, Sept 2007; Wave 2 June 2008; Wave 3 Sept 2008; Wave 4 June 2009; Wave 5 Sept 2009; Wave 6 Sept 2010. |
|
| Notes | Quality of intervention delivery: Teacher’s Handbook describes each unit, core activities, tips, conclusions. Monthly meetings with Regional Co‐ordinators "to monitor intervention fidelity". "Progress on the delivery of the Unplugged curriculum in the experimental arm was continuously tracked via Internet‐based questionnaires that were submitted by teachers after the completion of each lesson". "All 12 lessons …were delivered in all classes". Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? No; but 125 at baseline, 122 at 2‐yr follow‐up. Was a correction for clustering made? Yes (GEE) Were appropriate statistical methods used? Chi² for differences between intervention and control groups. GEE. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by computer (statistical software). Email from author 5/11/12. Clusters: Schools Cluster constraint: Three regions in the Czech Republic. “Stratified random sampling was used to obtain a representative sample.” [not further described]. 5 schools withdrew from control arm before baseline and were not replaced. Baseline comparability: No differences in gender, age, family income level, substance use (after applying Bonferroni correction for number of tests). Ethnicity was not assessed. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Baseline (experimental 1022, control 852); 24m (914,839); N of schools (E40, C34) at both baseline and 24m; 1 control arm school deleted as high levels of missing data at baseline. "…program effects were examined using Last Observation Carried Forward and Best‐Case, Worst‐Case scenario. The results did not change. Chi‐square and t‐tests were performed on demographic variables to assess the effect of missing data. All of the results were insignificant. Thus, it was concluded that missing data were completely at random". |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Garcia 2005.
| Methods | Country: Spain
Site: 9 classes, Murcia. Project ‘ALERT’ implemented model called ‘Extension and School Enhancing Life Skills’ (EXSELS). Focus: Tobacco use, attitudes to use. Design: Cluster RCT (Group 1: never smoking prevention cohort). |
|
| Participants | Baseline: Intervention 159, control 73; baseline questionnaire: Intervention 147, control 68.
Age: 12.7 years (mean).
Gender: 47% F, 2.7% no response. Ethnicity: Not stated. Baseline smoking data: Experimenters (a few times): Intervention: 59.8%, Control 47.1%; Weekly: Intervention 4.7%, Control 4.4%; Daily Intervention 10.9%, Control 9.0%. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Teachers Intervention: 8 x 1‐hr sessions: 1) Written exercises on medium and long‐term effects of tobacco (received also by control group); 2) audiovisuals on short‐term effects and also components causing these effects; 3) critical commentary and group discussion on text in Catalan by an adolescent smoker and reasons why started smoking, then individual and group discussion; 4) computations in maths class of loss of respiratory capacity, class discussions; 5) situations where experienced pressures from friends to smoke, practised refusal skills; 6) discussed text that described a family celebration during which children were invited to smoke; 7) tobacco companies’ need for new markets among youth and women, and publicity strategies; 8) rights of nonsmokers for clean air and not to be pressured by smokers to smoke. Control: Usual school district 1‐hr annual lecture on effects of tobacco on health. |
|
| Outcomes | Never smoking vs ever (monthly, weekly, daily). Follow‐up: 7 ‐ 9m after intervention. |
|
| Notes | Quality of intervention delivery: Median attendance 97.3%. Statistical quality: Was a power computation performed? Not stated. Was an intention‐to‐treat analysis performed? No. Was a correction for clustering made? No. All classes in the same school ‐ potential contamination. Were appropriate statistical methods used? Comparison of proportions for independent groups. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Classes randomised, sequence computer‐generated. Clusters: 9 classes. Cluster constraint: None. Baseline comparability: Experimenters (a few times): Intervention: 59.8%, Control 47.1%; weekly: Intervention 4.7%, Control 4.4%; daily Intervention 10.9%, Control 9.0% (all n.s); for 16 attitude and knowledge items, only difference is for “most adults smoke”. Intervention 73.9%, Control 49.2% (P < 0.001). |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Baseline Questionnaire: Intervention 147, control 68; 7m follow‐up: Intervention 128 (87%); Control 49 (72%); no analysis of differential attrition. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Gatta 1991.
| Methods | Country: Italy Site: 163 schools in Milan (55 schools to intervention; 52 schools where half the classes were randomised to intervention, 56 schools to control). Focus: Smoking prevention. Design: Cluster RCT (excluded from analysis). | |
| Participants | Baseline: 16,074
Age: 9 ‐10 yrs (4th year primary school).
Gender: Not possible to determine from data in Table 1. Ethnicity: Not stated. Baseline smoking data: Smoking: 8.4% (1.4% daily; 2.4% at least once a week; 4.2% < once a week; 0.4% did not report smoking frequency). |
|
| Interventions | Category: Information vs control. Programme deliverer: Teachers. Intervention: 1 day of lessons; harmful effects of tobacco taught by slides, comic strips and posters; poster of a famous nonsmoking sports person and comic books on adolescent smoking given to each student. Control: No intervention. |
|
| Outcomes | Definition of smoking: nonsmoking (< 1 cigarette a week); at least 1 cigarette a week, and at least 1 cigarette a day. Anonymous self administered questionnaires. Follow‐up: 4 yrs | |
| Notes | Quality of intervention delivery: "Teachers were encouraged to develop these lesson topics in subsequent weeks". No process analysis. Statistical quality: Was a power computation performed? Yes, power computation performed post‐hoc power, and showed that the study had only 67% power to detect the prespecified outcome. Was an intention‐to‐treat analysis performed? No. Was a correction for clustering made? No. Were appropriate statistical methods used?. The unit of allocation was the school and the unit of analysis the individual. X². |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "In 1982 out of all 185 Milan state schools, 163 accepted the intervention program and were randomised in three groups...". "After the anatomizations, two more schools in the second group (110 children) refused the educational intervention". Method of randomisation not described. Clusters: Schools Cluster constraint: Not stated Baseline comparability: No statistically significant differences on age, gender, place of birth and family smoking habits. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | At the 4 yr follow‐up attrition was 36%; no attrition analysis was stated. "Out of a target population of 16,074 children, 548 belonged to the schools refusing data collection and 1139 were absent on the day of data collection. A total of 3946 children were excluded because the questionnaire showed that they did not belong to the randomised population and 124 since it was not possible to categorize them in the three randomised groups. Consequently, 10,317 questionnaires were analysed" (64%). |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Gersick 1988.
| Methods | Country: USA Site: 32 classrooms in 20 schools from public school systems in 2 New England towns. Focus: Substance abuse prevention. Design: Cluster RCT (excluded from analysis). | |
| Participants | Baseline: Not stated, 1372 at post‐test.
Age: 6th grade (2 cohorts, 1980‐81 and 1981‐82).
Gender: 49% F Ethnicity: "dominant ethnic group in both towns is third or later generation Italian and mixed European", 9.2% B or non‐W, 3.5% did not indicate race. Baseline smoking data: Not available. |
|
| Interventions | Category: Social competence + social influences vs control. Programme deliverer: Project staff. Intervention: 40 mins a week for 12 weeks. Social cognitive skills; effective decision‐making (assessing situations realistically, brainstorming alternatives, using a balance sheet to identify negative and positive consequences, evaluating risk); role flexibility (peer influence and conflict resolution, decisions about drugs, alcohol and cigarettes); enhancing support (basic concepts of social networks, family and non‐family support systems). Control: No intervention. |
|
| Outcomes | Student Drug Use Survey (self report of 10 drugs including tobacco, with 7‐point scale (1. never; 2. once or twice; 3. < once a month; 4. once or twice a month; 5. once a week; 6. 2 or 3 times a week; 7. almost every day). Follow‐up: 1 yr, 2 yrs. | |
| Notes | Quality of intervention delivery: No process analysis. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Not stated. Were appropriate statistical methods used? Analysis was both at the individual and classroom means levels.by t‐tests and X². |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A posttest only, control group design was utilized. This design was selected to minimize test exposure effects and thereby increase the validity of the evaluation. The random assignment of classrooms to Program and Control conditions is used to control for selection, history and maturation". Method of randomisation not stated. Clusters: Classrooms Cluster constraint: Grouped into 2 clusters by SES and ethnicity. Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | % of grade cohort participating: 1 yr ‐ 73% for 1st cohort, 90% for 2nd; 2 yr ‐ 79%, 1360 baseline (680 programme, 680 control), df= 1073 in MANOVA for tobacco after 2 yrs reported on page 107. "... baseline mean substance use among dropouts at eight grade follow up was significantly higher than baseline mean use among stayers ... for tobacco ...(p<.006)". No significant differences in absentee rate for intervention and controls. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Gilchrist 1986.
| Methods | Country: USA Site: Middle schools, Seattle, Washington. Focus: Smoking prevention. Design: Cluster RCT (excluded from analysis). | |
| Participants | Baseline: 741
Age: 5th and 6th grade (average 11.4 yrs). Gender: 49% F Ethnicity: Most were white. Baseline smoking data: 69% nonsmokers. |
|
| Interventions | Category: Social competence + social influences vs control. Programme deliverer: 'Leaders', female/male co‐leader team conducted all sessions in self control and placebo groups (received 30 hrs training). Intervention:
Control: Measurement only. |
|
| Outcomes | Main outcome: Self reported smoking of 1 or more cigarettes during past week, not grouped by baseline status. Smoking: never, experimental (tried at least once but had never smoked weekly), regular smokers (1 or more cigarettes a week). Saliva collected but not analysed. Follow‐up: 15m from pretest. | |
| Notes | Quality of intervention delivery: No process analysis. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? ANOVA. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "...subjects were randomly assigned by school to experimental, placebo and control conditions". N of schools not reported. Method of randomisation not stated. Clusters: Schools Cluster constraint: Not stated. Baseline comparability: Equivalence of groups at baseline not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Baseline = 741; Follow‐up at 15m (701) 94%, no differential attrition across conditions. Higher attrition amongst baseline smokers at 15m. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Gindre 1995.
| Methods | Country: France Site: 4 secondary schools and the primary schools linked to them in Lyon. Focus: Health, especially tobacco addiction. Design: Cluster RCT (Group 3: point prevalence). | |
| Participants | Baseline: CM2 year group: intervention: 3651; control: 3183 (numbers for SES Special education (5th form) not stated as this publication reported results only for CM2 students). Age: CM2 (10 ‐ 11 yrs), 5th form (12 ‐ 13 yrs). Gender: 49.5% F Ethnicity: W 81.4%, A‐A 5.4%, N‐A 2.2%, H 1.3%, Asian‐American 1.1%, Other 8.5%. Baseline smoking data: Smokers: intervention = 1.3%, Control = 1.5% per day? week? month? |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Teachers, educational staff, health professionals. (received 3 ‐ 6 days training per yr). Intervention: 10 interventions a yr in class to encourage reflection on behaviour and health, particularly on tobacco addiction, through dialogues with teachers, health professionals and students (not further described). Control: No statement. |
|
| Outcomes | One question: 'Do you smoke?' Follow‐up: End of school year (approx 9m). |
|
| Notes | Quality of intervention delivery: 75% of teachers responded to the process questionnaire (90% judged the programme was easily integrated into the curriculum; 91% the collaboration between health professionals and teachers was good; 94% felt it had a positive impact in class; and 86% were motivated to continue in subsequent years; but there was no statement of a protocol and no measurement of adherence to a protocol). Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? No statement of method of analysis (probabilities are reported). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A random sample of four groups of secondary schools and the primary schools linked to them by virtue of their location were randomly allocated to the following groups: A. intervention in CM2 and 5th form pupils; B: Iintervention in CM2 only; C: intervention in 5th form only; D: both CM2 and 5th form were non‐intervention controls". Method of randomisation not stated. Clusters: Schools Cluster constraint: Not stated. Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Only one question on smoking status. Baseline = 3651 CM2, 3183 control. Response rate was over 85%. No numbers stated at 18m. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Glanz 2007.
| Methods | Country: USA
Site: 20 middle schools, Hawaii. Project 'SPLASH' (Smoking Prevention Launch Among Students in Hawaii). Focus: 30‐day smoking/smoking prevention. Design: Cluster RCT (Group 1: never smoking prevention cohort, not included in analysis). |
|
| Participants | Baseline: 3617
Age: 12 yrs (grade 7)
Gender: 52% F Ethnicity: 27% Native Hawaiian; 21% Filipino; 19% W, 14% Japanese, 13% Other Asian/Mixed and Pacific Islander;7% Other. Baseline smoking data: 25.7% ever smokers; 8.1% past 30 days; TNT 24% baseline, SPLASH 26%. |
|
| Interventions | Category: Social influences vs social influences Programme deliverer: Teachers and SPLASH drama artists. Intervention: SPLASH: (a) 7th grade: 3 computer lessons on tobacco control, drama education residency (1 week); (b) 8th grade: 2 computer lesson on tobacco advertising (including Virtual Day during which students can post messages on Internet); 4 youth advocacy lessons (including 2‐day mock state legislative hearing by drama artists). Control: TNT: (a) 7th grade ; 8 lessons; (b) 8th grade: 5 lessons (effective communication, assertiveness training, tobacco advertising) "typical of effective social influence‐based tobacco education programs". |
|
| Outcomes | Ever smoked (Y/N); smoked past 30 days (Y/N); 947 provided saliva samples for cotinine measurement (of whom 8% reported smoking past day, but < 2% had > 10 mg/ml cotinine). Follow‐up: End 8th grade (18m). |
|
| Notes | Quality of intervention delivery: Teacher surveys and interviews, classroom observation, analysis of homeworks and drama and student surveys; "most teachers in both the TNT and SPLASH schools implemented the majority of the lessons". Statistical quality: Was a power computation performed? Yes. Was an intention‐to‐treat analysis performed? No. Was a correction for clustering made? Yes. Were appropriate statistical methods used? SUDAAN for multiple correlated measurements; LR used DESIGN modelled similarly to GEE. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was at the level of the school. We used a combined stratified/matched pair randomisation procedure. Schools were stratified by rural/urban location and blocked on school size (large, medium, small) and baseline smoking rate (low, medium, high), using data from a 1998 state survey. One school per pair was then randomly selected and assigned to the intervention arm, with the other school going to the control arm. Three schools agreed to serve as pilot sites for the interventions". Email from Dr Glanz 2 February 2012: "Once two schools were in the matched pairs, we determined treatment or control group status of the first school ‐ in alphabetical order by name ‐ by selecting a paper from an envelope (Intervention/Control). Half the papers were marked Intervention and half were marked Control. This was the equivalent of a coin toss but assured equal numbers in both groups (which a coin toss might not). Clusters: Schools Cluster constraint: Blocked by schools size and rural/urban. Baseline equivalence: No significant differences 'ever tried smoking' or 'current smoking past 30 days' between Intervention groups. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition greater among TNT participants, ever smokers and past 30 day smokers; in SPLASH significantly more ever smokers who did not complete study; 71.4% SPLASH and 72.2% TNT teachers reported high implementation. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Gordon 2008.
| Methods | Country: USA Sites:40 middle schools (Intervention N = 20, Control = 20) Focus: Smoking prevalence and smoking susceptibility Design: Two‐condition Cluster RCT (two cohorts due to resource restrictions if all schools completed the trial at the same time) (excluded from analysis) |
|
| Participants | Baseline: 6276 Age: 6th grade (age 11) Gender: 50% Male Ethnicity: W 68%, H 11%, N‐A 6%, A‐A 2%, Asian 2%, Pacific Islander 1% Baseline smoking data: Non‐smokers; intervention groups N = 2833, control N = 2574 |
|
| Interventions | Category: Information vs control; Social influences vs control. Programme deliverer: Research team provided material. Issued by research team and schools. Intervention: Two components :
Control: No intervention (Not stated whether control schools received any form of state programme) |
|
| Outcomes | Indices of smoking prevalence for males and females. Based on number of days smoked in the past month and number of cigarettes per day in past month. Use of smokeless tobacco for males in the prior month. Email from Dr Gordon (30 January 2012) "never‐smokers here includes students who reported 'I have never smoked'". Follow‐up: Change in tobacco use prevalence from 6th to 8th grade (2 years). |
|
| Notes | Quality of intervention delivery: one control school received intervention material in error so switched to intervention group. Statistical quality: Was a power computation performed? Reference to but not stated: "While it would have been ideal to cross FC and YAT in a 2 x 2 design in schools, there was insufficient statistical power to do so...". Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Yes, ICCS computed from mixed‐model ANCOVA. Were appropriate statistical methods used? Changes to intervention between two cohorts gave different results between the two groups. Nested time x condition analysis. Mixed model analysis of covariance (ANCOVA). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Study marketed to schools across 70 school districts around Oregon. Schools selected with the highest smoking prevalence. Method of randomisation not stated. Clusters: Schools Cluster constraint: Email from Dr Gordon (30 January 2012): "We rank‐ordered schools on tobacco prevalence and size. We first approached only schools with a tobacco prevalence at or above the median, then accepted schools with lower prevalence. Schools were ranked on size within prevalence". Baseline comparability: Not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All schools completed the trial. Analysable sample (both pre‐test and follow‐up prevalence data) N = 3575 (60%). No reasons for loss of students stated. Follow‐up post‐test survey completed on Grade 8 students regardless of whether took the original pre‐test survey. "No attrition‐by‐condition", but "students without post‐test information reported higher levels of prevalence (at pre‐test) than students with post‐test data" ‐ no explanation for this result except unsubstantiated comment that "students with greater mobility may be more susceptible to cigarettes". |
| Selective reporting (reporting bias) | Unclear risk | No statement |
Hamilton 2005.
| Methods | Country: Australia
Site: 30 high schools in Perth (intervention = 14; control = 16) 'Smoking Cessation for Youth project' (SCYP) Focus: Reduce transition to regular smoking, tobacco harm minimisation Design: Cluster RCT (Group 1: never‐smoking prevention cohort, not included in the analysis) Two data sets: Hamilton 2005 all students, Hamilton 2007 nonsmokers (lifetime abstinence from smoking at baseline). |
|
| Participants | Baseline: 4636 Hamilton 2005: 4383 (ages outside 10 ‐ 16 removed), intervention = 1937; control = 2446. Hamilton 2007: 2078 never‐smokers Age: Hamilton 2005 and 2007: Avg 13.6. Gender: Hamilton 2005: 50.5% F; Hamilton 2007: 48.2% F. Ethnicity: Not stated. Baseline smoking data: Hamilton 2005 (4383): never‐smokers: intervention 50.2%, comparison 45.9% (P < .01); smoked past 30 days: intervention 19.4%, comparison 22.0% (P < 0.05); regular: intervention 7.5%, comparison 10.2% (P < 0.01); Hamilton 2007 (2078): never‐smokers: intervention 46.5%, comparison 53.5%; no significance stated. |
|
| Interventions | Category: Social influences vs social influences. Programme deliverer: Teachers (received 6 hrs training plus brief follow‐up training by phone); nurses (received 3 hrs training). Intervention: 4 components: (1) Harm minimisation (“Keep Left” ), 8 x 1 hr lessons (four hrs each year): (a) prevention/refusal to assist nonsmokers; (b) cessation for current smokers (c) reduction of use (d) assistance to provide peer support for reduction/cessation; (e) reducing environmental smoke exposure. (2) School nurses used motivational interviewing to assist quitting; (3) parent newsletter; (4) letter to accompany letters from school to inform parents child had been smoking. Control: Usual social influence and skills activities to avoid smoking (7 hrs); state‐wide training for teachers. |
|
| Outcomes | Regular = (≥ 4 days during previous week); past 30 days = any smoking in past 30 days; self report. Follow‐up: Hamilton 2005 and 2007, post‐tests 1 and 2, in years one and two immediately after intervention, post‐test 3 at the end of year 10 (2 years after baseline). |
|
| Notes | Quality of intervention delivery: Hamilton 2005: intervention students reported receiving average 4.2 of 8 hrs classroom instruction (comparison students average 3 hrs of 7); intervention students: 34.7% reported receiving up to ⅓ of programme; 30.7% ⅓ to ⅔, and 34.6% > ⅔. Hamilton 2007 for baseline never‐smokers: intervention students reported receiving average 4.5 of 8 hrs classroom instruction (comparison students average 6.7 hrs of 7). Statistical quality: was a power computation performed? Yes; for intermediate estimated ICC of 0.01, α = 0.05, power = 80%, assuming standard intervention would reduce frequent smoking to 15% and harm minimisation intervention to 10%, requires 3360 students (120 in each of 14 schools). Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Yes Were appropriate statistical methods used? Yes; Multilevel modelling; all analyses adjusted for family smoking, SES, gender. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Thirty (58%) of the eligible 52 government highs schools in the Perth metropolitan area agreed to participate and were assigned randomly to intervention and comparison". No method of randomisation Clusters: Schools Cluster constraint: schools stratified on SES and number of enrolled grade 9 students. Baseline comparability: never‐smokers: intervention 50.2%, comparison 45.9%, P < 0.01); smoked past 30 days: intervention 19.4%, comparison 22.0%, P < 0.05); regular smoker (7.5% vs 10.2% P < 0.01); comparison group more below Australian SES average (50% vs. 47%, P < 0.05; fewer of their mothers completed grade 12 (45% vs 49%, P < 0.01). Multilevel analysis controlled for differences in gender, family smoking, SES, school, student. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1 school dropped out after randomisation. Hamilton 2005: "Attrition was similar for both groups from baseline to post‐test 3 (45.5% among intervention students vs 45.6% among comparison students)"; "Some evidence exists that attrition may have been differential with comparison students lost to follow‐up more likely… to smoke regularly (13.8% vs 10.7%).". Significance not stated. Hamilton 2007: "selective attrition occurred…to family smoking status. The students lost to follow‐up were more likely at baseline to report another family member smoked (42.9% vs 34.7% among the cohort). There were no other differences…Among the baseline never‐smokers, retention was similar in both groups at … post‐test 3 (58.9% and 60.7%)". "Attrition is a limitation of this study….approximately 40% of students were lost to follow‐up". |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Hanewinkel 1994.
| Methods | Country: Germany Site: 2 Realschulen, 3 Hauptschulen and 1 Gymnasium in Schleswig‐Holstein. Focus: Tobacco Design: Cluster RCT (excluded from the analysis) | |
| Participants | Baseline: 1985, eligibles 1299, baseline 650. Age: average 13.8 yrs Gender: 339/650 M Ethnicity: not stated Baseline smoking data ‐ smokers: intervention = 70, control = 58; nonsmokers: intervention = 419, control = 119. |
|
| Interventions | Category: Social competence + social influences vs control. Programme deliverer: not stated. Intervention ‐ 10 sessions covering: confronting socially uncertain situations; learning to differentiate facial expressions and feelings; understanding gestures; making demands, recognizing others' demands; accepting and working with criticism; getting through difficult situations, self confidence in relations with others; coping with failure; fate and self responsibility. Tobacco resistance training was discussed in sessions 4 and 6. There were also homework, relaxation exercises and the use of comics, story books, and role‐plays (there were separate stop‐smoking programmes for students and parents who smoked). Control: group on a 'waiting list' and later received the intervention (personal communication). |
|
| Outcomes | Smoking in last 7 days Follow‐up: 6m, 1 yr, 16m. |
|
| Notes | Quality of intervention delivery: no process analysis. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? X². |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The study was evaluated with a waiting‐list‐control‐group design. "...handelt es sich um ein Warte‐listen‐Kontrollgruppen‐Design...Während die Studie an 4 Schulen lief ("Experimentalgruppe 1"), dienten 2 weiteren Schulen als Kontrollgruppe." 1 Gymnasium did not participate in the intervention phase for organisational reasons; experimental group 1 (2 Hauptschulen) differed in student composition from the control group (1 Hauptschule, 2 Realschulen, 1 Gymnasium). Method of randomisation not stated. Clusters: Schools Cluster constraint: Not stated Baseline comparability: No analysis of equivalence at baseline |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 1985 baseline. 1 gymnasium withdrew for organisational reasons, leaving 1299 potential. Intervention groups 1 and 2: 650 completed the baseline questionnaire (May/June 1992), 650 at 6 months (January 1993), 658 at one year August 1993). Wait list control group: 177 baseline, 183 (January 1993) 36% attrition at 6m if combine intervention and wait list control groups; no differential attrition analysis. 50% attrition at 16m |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Hansen 1988a.
| Methods | Country: USA
Site: 8 Junior high schools, Los Angeles (2 schools to intervention 1, 2 schools to intervention 2, 4 schools to control). Project 'SMART' Focus: Substance abuse prevention Design: Cluster RCT (excluded from analysis) |
|
| Participants | Baseline: 2863 Age: 7th grade (12 ‐ 13 yrs) Gender: 49% F Ethnicity: 38% H, 30% B, 22% W Baseline smoking data: Not stated |
|
| Interventions | Category: Social influences vs social competence vs control. Programme deliverer: staff health educators and regular classroom teachers with peer opinion leader involvement. Intervention: 12 sessions over 1 term
Control: No intervention (36 classrooms). |
|
| Outcomes | Smoking: Smoking index, with aggregated classroom means. Dichotomised on +/‐ 30 day use. Separate analysis for baseline non‐users, with onset to various levels of use. Saliva samples collected but not analysed. Follow‐up: initial post‐test 1 yr after pre‐test (grade 8), 2nd post‐test at 2 yrs. | |
| Notes | Quality of intervention delivery: No process analysis. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? Aggregate classroom scores used (85 classes). Indices of use by ANOVA and ANCOVA using pre‐test scores as covariates. Dichotomous 30‐day use by Fisher's exact test. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Of 63 junior high school complexes in the Los Angeles Unified School District available for assignment, 44 were randomly assigned to intervention and control conditions using a multi‐attribute approach...". Method of randomisation not stated. Clusters: Schools Cluster Constraint: No matching or stratification. Baseline comparability: Control and social group subjects differed on baseline smoking within the past 30 days in Data set 1 ‐ 2 (P < 0.005). |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Baseline 2863; attrition 37% from baseline to first post‐test, and 32% from pre‐test to final post‐test. Attrition of smokers compared to nonsmokers at the 1 yr follow‐up (P < 0.0001); and more attrition from the social influences and control groups (60%) than the affective social condition group (37%; P < 0.0001). |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Hansen 1991.
| Methods | Country: USA
Site: 12 Junior high schools in LA and Orange County, CA. Adolescent Alcohol Prevention trial (AAPT). Focus: Preventing onset of alcohol abuse, marijuana and tobacco use; primary outcome was alcohol use. Design: Cluster RCT (excluded from analysis). |
|
| Participants | Baseline: (1987) 3011
Age: 7th graders Gender: 48 ‐ 55% F. Ethnicity (range by intervention group): Asian 9% ‐ 26% (significant differences); B 1 ‐ 3%; H 11 ‐ 43% (significant differences); W 33 ‐ 52%. Baseline smoking data: smoking public schools = 4%, private schools = 4%. |
|
| Interventions | Category: information vs social influences vs information/perceptions vs social influences. Programme deliverer: project staff (received 2 wks intensive training) Intervention:
Control: No control (author considers intervention 1 a placebo comparison) |
|
| Outcomes | Smoking index, and never/ever smoking/ 30 day smoking. Follow up: 8th grade, 1 yr from baseline. | |
| Notes | Part of Adolescent Alcohol Prevention Trial (AAPT); Rohrbach 1993 discusses techniques of implementing the AAPT in Los Angeles, but without any data on student smoking. Quality of intervention delivery: Process analysis showed high fidelity in the delivery (average 6 on a 7‐point scale for 8 aspects of programme implementation were achieved) of the interventions; but 3 of the independent variables (skill, resistance knowledge and acceptability) were judged by programme specialists to have been affected by programme integrity. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? Yes. Were appropriate statistical methods used? The unit of allocation was the school, and the unit of analysis in the 1991 paper was class. General linear model analysis of covariance approach was used with classroom means for each composite index and for each dichotomous item. In the 1998 re‐analysis, a combination of multilevel analysis (ML3 programme) and ordinary least‐squares analysis for the post‐test at 2 yrs were used for: (i) the 2370 individuals, (ii) the 120 classes, and (iii) the 12 schools. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No statement on how schools were selected. "Schools were stratified by size, test scores and ethnic composition and then randomly assigned to receive one of four intervention programs". Method of randomisation not stated. Clusters: Schools Cluster constraint: Stratification by size, test scores and ethnic composition. Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Pre‐test (1987) = 3011; Follow‐up at 1 year: 20% attrition with differential attrition in the resistance training group (P < 0.01), but the authors comment: "Since main effects of Resistance Training did not even approach significance, the interpretation of findings is not threatened". |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Hecht 2003.
| Methods | Country: USA
Site: 35 middle schools in Phoenix, Arizona (25 intervention, 10 control) 'Keepin’ it REAL'. Focus: Prevention and reduction of alcohol, drugs, marijuana and tobacco. Design: Cluster RCT (Group 2: change rates). |
|
| Participants | Baseline: Warren 2006: 4734 at pre‐test (Fall 1998) "completed at least some portion of the questionnaire" and/or 14m post‐test (Spring 2000); Hecht 2003: 3318 Mexican or Mexican‐Americans, 1141 other Latino, 1040 non‐Hispanic whites; 527 A‐A (total = 6035); Hecht 2006 (The Drug resistance strategies intervention…Health Communication 2006): 6298 7th graders who responded to at least 1 of 4 questionnaires. Age: 7th graders average 12.53 years (at Wave 1, baseline). Gender: 47% F (Warren 2006). Ethnicity: 55% Latin American, Mexican or Chicano, 17% Other Latino (Puerto Rican, Cuban), 19% W, 9% A‐A. Baseline smoking data: No. of cigarettes past 30 days: control mean = 1.36705, intervention group (0 ‐ 3 videos seen) mean = 1.42515, intervention group (4 ‐ 5 videos seen) mean = 1.32071; no. of days smoked in past 30 days: control mean = 1.25954, intervention group (0 ‐ 3 videos seen) mean = 1.33055, intervention group (4 ‐ 5 videos seen) mean = 1.24393. |
|
| Interventions | Category: Social influences and social competence vs control [social influences and social competence vs "local, regularly administered ATOD programming"]. Programme deliverer: Regular classroom teachers (training prior to teaching curriculum). Intervention: 10 lessons, Drug Resistance Skills kiR (Keepin' it Real) curriculum; 4 resistance skills with videos (3 versions: Mexican/Mexican‐American, European‐American/African‐American, Multicultural) followed by guided discussion (Refuse, Explain, Avoid, Leave [ REAL]), + TV Public Service Annnouncements (PSA) + neighbourhood billboards + in‐school booster sessions. Control: "local, regularly administered ATOD programming" "Close proximity of both treatment and control schools meant that students in all conditions received exposure to the media campaign". |
|
| Outcomes | Cigarette past 30 days (1 = 0 to 8 = > 2 packs); no. of days smoked past 30 days (1 = 0 to 6 = 16 ‐ 30) Follow‐up: Three follow‐up assessments with final one after 14m. |
|
| Notes | Quality of intervention delivery: "Approximately 54% (1,789) of the intervention students reported that they had seen four to five of the five classroom videotapes. The remaining intervention students (1,546) reported that they saw zero to three of the videotapes". "62% (2,081) of the intervention students and 44% (2,081) of all students reported that they had seen one or more of the televised PSAs". Observation of 37/49 teachers rated appropriate = 5.8 (on scale 1 = inappropriate to 7 = appropriate). Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Unclear. Authors state used multiple imputation NORM software control for imputed data; no data presented. Was a correction for clustering made? Yes, Stata complex survey sample routines for clustering. Were appropriate statistical methods used? Authors state used multiple imputation NORM software control for imputed data and Stata complex survey sample routines for clustering; but no data presented; ANCOVA. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "25 schools randomly assigned to one of the three intervention conditions and 10 schools to the control condition." Clusters: Schools Cluster constraint: Block randomisation to assign each school to one of four conditions (Mexican American, Black/White, Multicultural, Control). Baseline comparability: Students who had seen 4 ‐ 5 videos were more likely to be female than the group that had seen 0 ‐ 3 videos and did not differ significantly from the control group. The 0 ‐ 3 video group and the 4 ‐ 5 video group "appeared homogenous with respect to students’ self‐reported racial/ethnic backgrounds". The two groups who had seen a PSA at least once or those who had not seen a PSA were equally likely to be male or female and were homogenous in respect to ethnic/racial background. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "Intervention students comprised 70% (3335) of the 4734 middle school students who completed a baseline and/or follow‐up assessment". There is no differential attrition analysis; 14m follow‐up = 3148 (50%). "Approximately 54% (1789) of the intervention students reported that they had seen four to five of the five classroom videotapes. The remaining intervention students (1546) reported that they saw zero to three of the videotapes.... 62% (2081) of the intervention students and 44% (2081) of all students reported that they had seen one or more of the televised PSAs". Missing data: NORM software used to produce 10 multiply‐imputed datasets and fitted regression models to address ICC, SEs and P values from randomisation by cases. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Hecht 2008.
| Methods | Country: USA
Site: 23 middle schools in Phoenix, Arizona (13 intervention, 10 control). "Students in six additional schools participated in a third condition of the study, in which they received a new version of the kiR which focused on acculturation issues". Focus: Prevention and reduction of alcohol, drugs, marijuana and tobacco. Design: Cluster RCT (excluded from analysis). |
|
| Participants | Baseline: Baseline = Wave 1: Hecht 2008: 1566 students (768 intervention, 798 control); Elek 2010: 1984.
Age: 10.4 average (range 7 ‐ 15) at Wave 1, baseline.
Gender: 49.1% F (Table), 49.7% F (text). Ethnicity: 75% Latin American, Mexican or Other Latino, 4.9% W, 9.1% B, 2.6% N‐A, 0.4% Asian American, 7.8% not stated. Baseline smoking data: Not stated. |
|
| Interventions | Category: Social influences and social competence vs social influences [Project ALERT or local programmes]. Programme deliverer: Regular classroom teachers (training prior to teaching curriculum). Intervention: kiR‐Plus Adapted from 7th grade Keep it REAL (kiR) for 5th graders: 12 lessons, Drug Resistance Skills kiR curriculum; 4 resistance skills with videos followed by guided discussion (Refuse, Explain, Avoid, Leave [ REAL]). Elek 2010 notes that half of the classes in each grade level received kiR‐Plus and half received kiR‐Acculturation Enhanced (AE) . Control: Students in 7 control schools participated in Project ALERT in 5th or 6th grade; some control schools used Gonzo’s 20 Ground Rules (Communities in Schools in Arizona, 2007); some used Red Ribbon Week (National Family Partnership, 2005). |
|
| Outcomes | Lifetime prevalence/tried ('even if it was only once or only a little'); Cigarettes past 30 days (0 = 0, 1 = any) Follow‐up: Post‐intervention, post‐booster sessions. |
|
| Notes | Quality of intervention delivery: "Lesson observation by the study personnel indicated that the teachers in the multicultural condition implemented the kiR intervention with both high quality (organization, preparation, student participation, student enjoyment, etc.) and fidelity (of instruction, video presentation, student practice, and homework). Teachers implementing the kiR intervention self‐reported presentation of all program lessons and activities". Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not, but authors state used multiple imputation NORM software for missing data. Was a correction for clustering made? Yes, Stata complex survey sample routines to account for ICCs in classes. Were appropriate statistical methods used? Stata survey programme for %s, means and SEs and complex survey sample routines to account for ICCs in classes; multiple imputation NORM software control for imputed data; linear mixed effects regression. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "10 schools were randomly assigned to the intervention conditions, 13 schools to the control condition". No method of randomisation. Clusters: Schools Cluster constraint: Not stated. Baseline comparability: No differences on lifetime substance use at baseline, no use in past month, or characteristics correlated with substance use. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Baseline to wave 3 = 28% Missing data: NORM software used to produce 10 multiply‐imputed datasets for missing data. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Hedman 2010 (Interview).
| Methods | Country: Sweden.
Site: 17 dental clinics in Uppsala county. Focus: Prevention of oral disease, influence attitude toward tobacco. Design: Cluster RCT (Group 3: point prevalence). |
|
| Participants | Baseline: All children born 1989 and 1992 in Uppsala county who were assessed by a dental hygienist or clinician during 2003 ‐ 4 as high risk (N = 382).
Age: 12 ‐ 15 yrs.
Gender: 49.5% F (control), 48.4% F (lecture), 56.3% F (Interview). Ethnicity: Not stated (except 10% immigrant background). Baseline smoking data: "Smoke": Lecture 4%; Interview 4%, control 8%; "Use snuff": Lecture 6%; Interview 4%, control 5%. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Dental hygienist or nurse who presented school lecture (8 hrs training) and conducted interviews (2‐day course) Intervention:
Control: No intervention |
|
| Outcomes | "Participants who smoke"; "Participants who use snuff". Follow‐up: 8 ‐ 10m. |
|
| Notes | Quality of intervention delivery: "All of the students in the class participated in the lecture…". Statistical quality: Was a power computation performed? Yes (no details). Was an intention‐to‐treat analysis performed? No. Was a correction for clustering made? No. Were appropriate statistical methods used? Yes, Differences over time within groups by McNemar’s test; between groups by Χ². |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by "drawing lots". Clusters: 17 dental clinics. Cluster constraint: Clinics matched on no. of subjects and urban/rural distribution, and geographical area (to ensure attended the same schools). Baseline comparability: no statistical difference on smoking, sex, age, country of birth. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Baseline: Lecture N = 120; Interview N = 142, control = 120; Loss was after randomisation and before intervention: "After the clinics had been divided into three groups, it was decided by drawing lots which group of clinics should perform lectures (91 patients), conduct motivational interviews (103 patients) or be in the control group (107 patients)". "The dropout rate….was 33%. The reasons for refusing to take part are not known". No analysis Pre‐test and follow‐up 8 ‐ 10m: Lecture N = 91; Interview N = 103, control = 107. No attrition. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Hedman 2010 (Lecture).
| Methods | See Hedman 2010 (interview) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from intervention 2 within Hedman 2010 (interview) | |
Hirschmann 1989.
| Methods | Country: USA.
Site: 1 public middle school in Milwaukee, Wisconsin (Non‐random selection of school chosen for representative distribution of gender and race; random assignment of classrooms (7 experimental, 6 control). Focus: Smoking prevention. Design: Cluster RCT (excluded from analysis). |
|
| Participants | Baseline: 315
Age: 16% 6th grade, 41% 7th grade, 43% 8th grade.
Gender: 51% F. Ethnicity: Not reported. Baseline smoking data: Baseline never‐smokers 124; 1 try (initiation) 59; 2+ tries (experimentation) 83; smoked past month (continued experimentation) 55; past week (regular smoking) 35. |
|
| Interventions | Category: Social influences vs information. Programme deliverer: Teachers, actors. Intervention: 3x 45‐min sessions, "each of which began with a 10 to 15‐minute slide‐tape show ...with four male and four female students and a physician moderator discussing smoking. At least one student was programmed to fit each of the three roles involved in the pathways to regular smoking: the self‐defining risk‐takers, the affect‐regulator, and the student submissive to social pressure". After each slide‐tape show there was a 30‐min discussion. "The first discussion reviewed why aversive symptoms may or may not occur with the first cigarette ...The second discussion covered the concept of adaptation to symptoms ... the illusion that cigarettes are not damaging ... The third discussion reviewed the process of becoming addicted. In all three sessions, the leader spent a few minutes describing specific inducements to smoking (e.g. peer pressure) and asked students to generate strategies to resist. Students role‐played ways of refusing or delaying a cigarette while avoiding social rejection and not hurting someone's feelings. Students were reinforced for their participation and intentions to apply the skills". Control: 3 films on 3 days (Who's in charge here?; The tobacco problem: what do you think?; and First cigarette); wrote down what they liked and disliked about each, and ideas for improvement. Film content focused on immediate and long‐term health effects of smoking. |
|
| Outcomes | Self reported smoking (0 tries; 1 try; 2+ tries; smoked in past month; smoked in past week). Follow‐up: 6 and 18m. | |
| Notes | Quality of intervention delivery: 49 (15%) students failed to attend at least 2 sessions, with 20% in the control group and 12% in the experimental group missing 2 or more sessions, and nonattenders more likely to smoke (P < 0.05). Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? Correlation, X², ANCOVA. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Participation in the experimental or control conditions was determined by random assignment of classrooms...". Method of randomisation was not stated. Clusters: Classrooms. Cluster constraint: Not stated. Baseline comparability: No differences in characteristics between groups at baseline. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Baseline 315; 49 differential drop‐out between groups (Experimental: 11.6%, Control: 20.5%, P < 0.01); absentees at follow‐up were more likely to have smoked in the past week; 266 (84%) included in analysis at 15m. Follow‐up = 84%. Students who had not attended at least 2 programme sessions were excluded. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Hort 1995.
| Methods | Country: Germany Site: 19 secondary schools in Dusseldorf (intervention 9 schools, control 10 schools). Focus: Reduce current and new onset smoking. Design: Cluster RCT (Group 1: never smoking prevention cohort). | |
| Participants | Baseline: 878, 93% of eligible population.
Age: 13 yrs. Gender: 38% F. Ethnicity: Not stated. Baseline smoking data: Nonsmokers: intervention N = 268, control N = 239, smokers: intervention N = 83, control N = 40. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Teachers, physicians. Intervention: Yr 1: 6 wk period. Classroom teachers (2 hrs) explained lung and heart function, and how advertisers encouraged children to smoke (1 hr). Investigators (physicians) discussed (2 hrs) body function, protective mechanisms of the airways, heart attack, cancer. Students in groups simulated how cilia in an airway remove particles. Non‐smoking students conducted role‐plays (2 hrs) on refusing a cigarette without feeling uncomfortable. Excerpts videotaped and used in 2nd half of session. Competition for an advertisement against smoking. Yr 2: (15 hrs) physicians discussed lung function and smoker's cough. Role‐plays. Students introduced to top nonsmoking sports personalities, who discussed their sport and training system and conducted Q&A sessions. Posters of these personalities were displayed and students could attach their own photo to them and receive a copy of the poster. Control: Talk by a physician on a topic of their choice: most wanted to hear about alcohol, but they were permitted to chose tobacco and its consequences. Experimental intervention for smokers (35 students in 4 schools); 11 x 1 hr sessions: Each cigarette smoked was recorded; stories suitable for the age group were told to provide relaxation. |
|
| Outcomes | Never‐smoker (never or only 1 cigarette); Nonsmoker (never‐smoker, or had not smoked for more than 6m); Smokers (precise number of cigarettes smoked to date, or stopped smoking less than ½ yr ago): weak smoker = 2 ‐ 10 cigarettes to date; moderate smoker = 11 ‐ 100 cigarettes to date; strong smoker = 100 cigarettes to date; daily smoker = at least 1 cigarette per day). Anonymous questionnaire with matching for cohort. Follow‐up: 24m | |
| Notes | Quality of intervention delivery: No process analysis. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? X² for comparison of %s, McNemar test for comparison of changes in samples, and t‐tests for comparison of means. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A prospective controlled study." ["Die Interventionsprogramm wurde in 9 annähernd gleichmãβig über die ganze Stadt verteilten Schulen durchgeführt, die anderen 10 dienten als Kontrolle. Mit der Matched‐pairs‐Technik wurde eine ausgewogene Verteilung der Schulen unter Berücksichtigung ihrer Gröβe und der unterschiedlichen sozialen Verhältnisse in den verschiedenen Stadtteilen angestrebt.' [no use of the word randomisation, only 'prospective controlled study' and 'matched pairs"]. Method of randomisation not stated. Clusters: Schools. Cluster constraint: Matched on student enrolments and social composition of catchment areas. Baseline comparability: Baseline smokers ("from the weakest to the strongest" were grouped together) M; Control 13.9%, Experimental 26.1%; F: Control 15.0%, Experimental 20.3%. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Baseline = 878; follow‐up after 2 yrs = 630; differential attrition from baseline in intervention and control classes; 20.2% attrition at 24m with no differential attrition analysis performed. Differential attrition from baseline: 0.4% refusals in the intervention classes, 5.7% in the controls. Refusals plus missing students comprised 7% at the first questionnaire, and 9.5% at 2 yr follow‐up. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Howard 1996.
| Methods | Country: USA Site: Private school, location not identified, but study team based in Spokane, WA. Focus: Cardiovascular risk reduction programme. Design: Cluster RCT (Group 1: never‐smoking prevention cohort). | |
| Participants | Baseline: 98
Age: 9 ‐ 12 yrs (av 10.4) 4th ‐ 6th grade.
Gender: 46% F. Ethnicity: No data Baseline smoking data: "No children (0%) reported any past or current smoking behaviour". |
|
| Interventions | Category: Information vs control. Programme deliverer: Teachers Intervention: 5 x 40‐min sessions. Cardiovascular risk reduction programme on physiology of the heart, smoking, hypertension, diet and physical activity and how to reduce those risks based on the American Heart Association Getting to know your heart and Future Fit materials. Control: No intervention relevant to smoking and cardiovascular health. |
|
| Outcomes | Current or experimental smoking. Follow‐up: 1 yr. | |
| Notes | Quality of intervention delivery: No process analysis. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? ANCOVA. Within text method stated as "quasi experimental", but description of method sufficient to warrant inclusion. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A stratified random sampling technique was used to assign one of two classes within fourth through sixth grades to the experimental group (EG). The other class within each grade was then assigned to the control group (CG)". "A pretest‐posttest, control group design was used in the quasi‐experimental, longitudinal study". Clusters: Classes Cluster constraint: Stratified random sampling. Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Baseline = 98; no child smoked at baseline; For children whose knowledge of a heart‐healthy diet was assessed at 1 yr 97 were present, so appears to be no attrition. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Johnson 2009.
| Methods | Country: USA
Site: 20 high schools in 6 Louisiana parishes (10 to intervention, 10 to control). Acadiana Coalition of Teens against Tobacco (ACTT). Focus: Difference in 30‐day cigarette‐smoking prevalence. Design: Cluster RCT (Group 1: never‐smoking prevention cohort). |
|
| Participants | Baseline: 5156 enrolled, 4808 responded to survey, 4763 (final sample, 40 removed due to missing answers).
Age: 9th grade (mean age 15.4 yrs).
Gender: 51% F. Ethnicity: 61% W, 32.8% A‐A, a little over 1% H, Asians, N‐A, 1.9% Other. Baseline smoking data: 30‐day smoking prevalence control = 26.1%, intervention = 23% (nonsignificant difference); ever smoked at baseline = 2738/4728 (57.9%). Email from Dr Johnson 31 January 2012 confirmed no‐smokers ("ever" smoked):intervention N = 891, control N = 1116. |
|
| Interventions | Category: Other interventions vs control. This intervention did not align with the main 5 categories; the programme intervenes by creating school anti‐smoking activities. Programme deliverer: Teachers (40 ‐ 45‐min ACTT workshop in 1st yr, booster 10 ‐ 15‐min workshops after 1st yr, final year teacher newsletter) Intervention: Use school environmental opportunities to deliver the intervention (began 1 yr after baseline for 2½ years), three components:
Control: No statement. However "at the time of the study, four of the five participating school districts has ‘ restricted’ smoking policy i.e. adults could smoke in designated places on campus". |
|
| Outcomes | Self reported 30‐day prevalence: "had smoked in the past 30 days, how often in the past 30 days they had smoked, and how many cigarettes they had smoked in the past 30 days. A non‐zero answer to the last two questions categorised the respondent as a smoker". Salvia cotinine samples at baseline only from students with active parental consent. Follow‐up: 10th & 11th grade tobacco use with full post‐test at 12th grade. |
|
| Notes | Quality of intervention delivery: No statement. Statistical quality: Was a power computation performed? Yes. Was an intention‐to‐treat analysis performed? No. Was a correction for clustering made? No. Were appropriate statistical methods used? Fisher’s exact test, t‐tests, mixed models (ANOVA). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | E‐mail from Dr Johnson 31/01/2012: "Relative to randomisation, we stratified by parish (county), and randomised (by computer process) the schools within the parish (county). The school was the unit or randomisation and therefore the unit of analysis". Clusters: Schools Cluster constraint: Stratification. Baseline comparability: "At baseline (9th grade), there were no significant differences in the prevalence of tobacco use". "No gender differences were observed for having ever smoked". |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Baseline N = 4763. Numbers at baseline varies in Table 4: 4459 according to ethnic status, 4454 according to gender status. At 12th grade 2643 according to ethnic status, 2639 according to gender status. No statement on attrition (approximately 40%) or attrition analysis. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported as stated. |
Jøsendal 1998 (P + T).
| Methods | Country: Norway.
Site: Nationwide sample of 4441 students in 195 classes in 100 schools 'BE Smokefree programme'. Focus: Smoking prevention. Design: Cluster RCT (Group 3: point prevalence). |
|
| Participants | Baseline: 4441 students, of whom 4215 provided written consent.
Age: Born 1981, grade 7 (approximately 13 yrs)
Gender: 47.3% M. Ethnicity: Not stated. Baseline smoking data: Nonsmokers 91.9% (F 92.3%, M 91.6%). |
|
| Interventions | Category: Social competence + social influences vs control. Programme deliverer: Teachers (received 2 days training, received detailed programme manuals). Intervention: The 8‐session programme focused on personal freedom, freedom to choose, freedom from addiction, making one's own decisions, tobacco‐resistance skills, and the short‐term consequences of smoking. Teachers filled in a questionnaire after each lesson to evaluate programme fidelity. Students brought 2 brochures home; teachers involved parents in discussions "at appropriate occasions", and students and parents signed nonsmoking contracts.
Control: Unclear whether the control group received any intervention. |
|
| Outcomes | Daily, weekly, < weekly smoking, and non‐smoking. Follow‐up: 6m, 18m, 2½ yrs (10th grade). |
|
| Notes | Quality of intervention delivery: Process analysis conducted but results not stated; also, the programme was varied and no process analysis of the variations as time progressed: "During Grade 8, teachers and students indicated to the program administrators that the main messages and educational approaches that had been chosen when planning the intervention had been sufficiently emphasized" and "Grade 9 students developed, carried out, and evaluated their own campaign to promote a smoke‐free lifestyle among Grade 7 students at their own school". Statistical quality: Was a power computation performed? Power computation: power 80% α = 0.05 required N = 757 in each group, and sample sizes achieved. Was an intention‐to‐treat analysis performed? No. Was a correction for clustering made? No adjustment for clustering in Josendal 1998; multilevel modelling allowed for clustering for 3‐yr follow‐up (Josendal 2005). Were appropriate statistical methods used? Pearson X² for differences across groups; McNemar's test for significance of changes and multiple LR for changes in smoking rates. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Schools were chosen as sampling units and as units for allocation to groups. Schools were drawn from a list containing all Norwegian schools in order of ascending zip‐code. Control schools were first selected (every nth school, starting with a randomly selected number between 1 and n), then the first three following schools with a similar number of students (± 10%) on the school list were chosen". Clusters: Schools Cluster constraints: Not stated. Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Baseline = 4441 after 4 yrs attrition, 11.2% in intervention and 5.8% in control; more smokers left comparison than model intervention group. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Jøsendal 1998 (P).
| Methods | See Josendal 1998 (P + T) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from second intervention within Josendal 1998 (P + T) | |
Jøsendal 1998 (T).
| Methods | See Josendal 1998 (P + T) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from third intervention within Josendal 1998 (P + T) | |
Kaufman 1994.
| Methods | Country: USA Site: 3 Chicago public high schools. Focus: Tobacco Design: Cluster RCT (Group 2: change rates). | |
| Participants | Baseline: 276 (Pre‐test information available on 131 (75%) in experimental and 76 (75%) in control schools).
Age: 6th and 7 graders (11 ‐ 13 yrs)
Gender: 52% F. Ethnicity: 99.5% B. Baseline smoking data: 12.29 (SD = 1.91) modified Botvin scale. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Community adults (received conventional Project ALERT training), teens (school selected, 1‐day training by researchers, state co‐operative extension educators, and adult programme leaders) Intervention:
Control: No other intervention. |
|
| Outcomes | Modified form of Botvin’s cigarette usage scales (range 6 to 32). Follow‐up: 6m. |
|
| Notes | Quality of intervention delivery: No statement if children completed the interactive exercises with parents related to the 5‐week campaign in the Chigago Defender, or that parents listened to the 8 radio programmes on WGCI to help them communicate with their children, or that children listened to and participated in the Smoking Prevention Rap Contest, or that children participated in the poster contest. The School Board had sent all schools the American Lung Association's curriculum; and 65% of the experimental and 31% of the control group reported reading part of the Defender curriculum;to design a billboard poster. Also: "After completion of the follow‐up data collection the research team learned that the sixth graders in the C school had been exposed to the DARE program during the year preceding this intervention. This participation may have resulted in the significant pre‐point differences between the P and C groups". Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? No. Were appropriate statistical methods used? ANOVA. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Students were randomly assigned by school to be in either the Program group(P), which included schools plus media, or the Comparison group (C), which included just the media programs". Method of randomisation not stated. Clusters: Schools. Cluster constraint: Not stated, although schools were specifically chosen as they were in black neighbourhoods. Baseline comparability: At pre‐test the intervention groups smoked more than the control (P < 0.02). |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Programme group: baseline = 175, pre‐test = 131, post‐test = 98, 6m follow‐up = 89 (68% of pre‐test). Comparison group: baseline = 101, pre‐test = 76, post‐test = 67, 6m follow‐up = 57 (75% of pre‐test). "There were no significant pre‐point differences in race, age, gender, or SES between those students who completed the entire pre‐test versus those who did not. Thus the students who participated in the study are considered representative of the original sample." [however, no comments about differential attrition at the 6m follow‐up]. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Kellam 1998 (GBG).
| Methods | Country: USA.
Site: 19 elementary schools in Baltimore. 'Good Behaviour Game'. Focus: Smoking prevention by changing behaviour predicting later smoking uptake. Design: Cluster RCT (Group 1: never‐smoking prevention cohort). |
|
| Participants | Baseline: 2311 (analysis limited to 1604 nonsmokers at baseline (Cohort 1 = 818 entered 1st grade in 1985, Cohort 2 = 786 entered 1st grade in 1986) .
Age: 5 ‐ 6 yrs.
Gender: 49.6% F Ethnicity: Greek and Italian 14%, White 16%, A‐A 70%. Baseline smoking data: Tobacco users: N = 502 (for group which entered 1st grade in 1985 = 275, for group which entered 1st grade in 1986 = 227); Tobacco nonusers = 1102 (for group which entered 1st grade in 1985 = 543, for group which entered 1st grade in 1986 = 559). |
|
| Interventions | Category: Other interventions vs control. This intervention did not align with the main 5 categories; the programme intervenes by rewarding good behaviour in the classroom. Programme deliverer: Teachers. Intervention: 2 yrs (1st and 2nd grades). Compared 2 programmes designed to reduce future tobacco usage by addressing risk factors for uptake:
Control: "customary school programs" / reading skills intervention. |
|
| Outcomes | Definition of smoking: "tobacco user", 'tobacco nonuser'. Assessed at individual interview. Follow‐up: From age 8 to 14. | |
| Notes | Quality of intervention delivery: No process analysis. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Yes, three different statistical methods were performed. Was a correction for clustering made? "To accommodate clustering of students within initial elementary schools, this analysis involved presorting of students into strata defined by school attended in first grade". Were appropriate statistical methods used? Yes. "We used standard life table and survival analysis methods to compare risk of initiating tobacco use for 2 interventions and all internal and external control classrooms. Kaplan‐Meier survival curves for each group were compared via log‐rank statistics as an aid to interpretation. Adjusted estimates for the relative risk of tobacco smoking were also obtained via conditional forms of Cox proportional hazards modelling; EGRET was used in calculating estimates". |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Five urban area were defined with socioeconomic levels ranging from very poor to middle class. In each area, 3 to 4 public elementary schools with similar racial/ethnic profiles were selected. Within each area, the Good Behavior game was randomly assigned to 1 school and Mastery Learning to another; 1 or 2 schools were controls". Method of randomisation not stated. Clusters: Schools Cluster constraint: Schools with geographical area stratified according to socioeconomic levels. Baseline comparability: "There were no significant differences between the intervention groups on baseline characteristics of teacher ratings of aggressive, disruptive behavior, fall‐of‐first ‐grade achievement, or free or reduced‐price school lunch when we took into account school as a random factor". |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "When attrition occurred it was unrelated to intervention status". Attrition 31%; Kellam 2008 reported on students who were re‐interviewed at age 19‐21; For Cohort 1, Table 6 lists 278 males and Table 7 348 females (total N = 626, (i.e. 77% of Cohort 1 in Grade 1 in 1985). The analysis offers 3 different intention‐to‐treat analyses, but these data are for a smaller sample size than baseline. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Kellam 1998 (ML).
| Methods | See Kellam 1998 (GBG) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (ML) within Kellam 1998 (GBG) | |
La Torre 2010 (A).
| Methods | Country: Italy
Site: Adolescent trial: 15 classes in Classical and Scientific Liceo of Cassino; Children’s trial: 24 classes, in Pontecorvo and Capodirise. Focus: Tobacco prevention. Design: Cluster RCT (Group 1: never‐smoking prevention cohort). |
|
| Participants | Baseline: Children’s trial: Intervention 242, Control 292; adolescent trial: Intervention 162, Control 146.
Age: Children’s trial 11 yrs; adolescent 14.36.
Gender: Children’s trial intervention: 48.5% F, control: 50% F; adolescent trial intervention: 52.5%, control: 52.1%. Ethnicity: Not stated. Baseline smoking data: Children’s trial: never‐smokers: Intervention 81.7%, Control: 82.2%; adolescent trial: never‐smokers: Intervention 83.1%, Control 81.5%. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Teachers (participated in tobacco prevention course). Intervention: Health facts, effects of smoking, mechanisms of initiating smoking, refusal skills (peer‐led discussions, skills practice). Control: Not stated. |
|
| Outcomes | "Have you ever smoked a cigarette?" indicating the status of current or ex‐smoker. Follow‐up: 2 yrs. |
|
| Notes | Quality of intervention delivery: Questionnaire on interest in issues covered (95%), comprehensiveness of intervention (97%), availability of staff to answer questions (99%), and usefulness of intervention (91%). Statistical quality: Was a power computation performed? Yes, 778 required for α = 0.1, power = 80%, expected smoking frequency = 30%, "estimated OR of smoking equal to 0.70 for students participating in the intervention group". Was an intention‐to‐treat analysis performed? No. Was a correction for clustering made? Yes. Were appropriate statistical methods used? Х² for differences between groups, multiple logistic regression for influence of sociodemographic factors, GEEs for clustering. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "We randomised 24 elementary classes and 15 high school classes to both intervention or control groups". Email from author "using a randomisation list generated by the Random Number Generator command in SPSS". Clusters: Schools. Cluster constraint: None. Baseline comparability: Yes: Children’s trial: never‐smokers: Intervention 81.7%, Control 82.2%; Adolescent trial: never‐smokers: Intervention 83.1%, Control 81.5%. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 yrs: Children’s trial: Intervention 239 (98.8%), Control 292 (100%); adolescent trial: Intervention 160 (98.8%), Control 144 (98.6%). |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
La Torre 2010 (C).
| Methods | See La Torre 2010 (A) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 'Childrens' trial' within La Torre 2010 (A) | |
Laniado‐Laborín 1993.
| Methods | Country: Mexico Site: 6 elementary schools, Tijuana. Design: Cluster RCT (Group 3: point prevalence). | |
| Participants | Baseline: 168 Age: average 12 yrs Gender: 46% M Ethnicity: No data Baseline smoking data: 63% never‐smokers. |
|
| Interventions | Category: Social influences vs control. Programme deliverer: Medical student. Intervention: 4 sessions. Groups of 6 ‐ 8 discussed noxious aspects of smoking; advertising strategies of the tobacco companies; influences of family and friends; and resisting offers to smoke. Control: No statement. |
|
| Outcomes | Smoking: past year/past week/past 24 hrs. Saliva samples collected and tested for nicotine/cotinine. Follow‐up: 10m. | |
| Notes | Quality of intervention delivery: No process analysis. Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? All 168 subjects completed the study. Was a correction for clustering made? No. Were appropriate statistical methods used? t‐tests for independent means; Z test for proportions, multiple regression for variables to predict smoking. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After a baseline survey students were randomly assigned to an intervention and a control group". Method of randomisation not stated. Clusters: Schools/groups. Cluster constraint: Pairs matched on baseline smoking prevalence. Baseline comparability: Difference in % of never‐smokers at baseline in the experimental (58.5%) and control (68.9%) groups, and minimal smoking (26.6% and 13.5%), but was not significant. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Did not state intention‐to‐treat, but all 168 subjects completed the study. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Lloyd 1983.
| Methods | Country: Australia Site: 88 primary schools in NSW. Focus: Smoking prevention. Design: Cluster RCT (Group 3: point prevalence). | |
| Participants | Baseline: 6299. Age: Yrs 5 and 6 (10 ‐ 12 yrs). Gender: 49% F (1657 boys were surveyed in yr 5 and 1572 in yr 6, 1574 girls in yr 5 and 1496 in yr 6). Ethnicity: Not stated. Baseline smoking data: Boys yr 5 (intervention 9.4%, control 10.3%), boys yr 6 (intervention 17.2%, control 14.3%); girls yr 5 (intervention 4.7%, control 5.5%), girls yr 6 (intervention 10.7%, control 6.2%). | |
| Interventions | Category: Social influences vs control. Programme deliverer: Teachers Intervention: 6 wk, 90‐mins a wk. 'Smoking or Health' programme of the Teaching Resources Centre of the NSW Department of Education: (1) Respiration process; (2 ‐ 3) physiological effects of smoking, 'Puffing Poll', creative dance; (4) advertising; (5) resisting peer pressure; (6) decision‐making, value clarification (7 ‐ 9) revision. Control: No intervention. |
|
| Outcomes | Never‐smoker; or smoked in the past 4 wks. Participants were assured of confidentiality and surveys were identified by numbers and not names. Follow‐up: 12m. | |
| Notes | Quality of intervention delivery: Teachers received 1 day of training. 80% replied to a questionnaire which asked if they had used the programme (no actual process analysis of fidelity of protocol delivery). The control group received no intervention, and 72% of those teachers replied to a questionnaire which asked if they had used any anti‐smoking interventions. More children took up smoking in the group where teachers scored lowest on the implementation scale. "...there were initial differences in their smoking behavior, attitudes and knowledge which confounded the effects of the quality of the programme implementation..Initially, those teachers who scored highest on this implementation scale had children who smoked slightly, but not significantly, more than other children in the treatment group. These children also disapproved less of tobacco smoking and cigarette advertising and knew less about the effects of smoking on health.On the other hand, the teachers judged poorest on this scale had children who smoked less, disapproved more of smoking and were more knowledgeable about the health consequences of smoking. The initial attitude and knowledge scores were significantly different between various categories of programme implementation". Statistical quality: Was a power computation performed? Yes, to detect differences of 5% smoking levels (two‐tailed test) and 80% power required 720 children per group; power computation achieved desired sample sizes. Was an intention‐to‐treat analysis performed? Not stated. Was a correction for clustering made? N.o Were appropriate statistical methods used? X² and multiple regression. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "...we selected 88 feeder primary schools for the 20 state and Catholic secondary schools in the Hunter region. ... the feeder primary schools for each secondary school were matched on the number of children in Years 5 and 6, and on the proportion of parents in unskilled occupations. One of each matched pair was then randomly allocated to receive the smoking prevention education, while the other remained a control school". Method of randomisation not stated. Clusters: Schools Cluster constraint: Pair‐matched on basis of year numbers and proportion of parents in unskilled occupations. Baseline comparability: Smoking rates at baseline were similar across groups, except that they were higher for the 6th grade females in the experimental group (P < 0.002). |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 49% attrition; no attrition analysis. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Longshore 2006.
| Methods | Country: USA.
Site: 45 South Dakota high schools and their feeder middle schools (16 to ALERT groups, 14 to ALERT Plus groups and 15 to control groups). Project ALERT and ALERT Plus Focus: Tobacco, alcohol and drug use prevention. [National Youth Anti‐Drug Media Campaign launched at the same time as trial entered grade 9 year, this campaign focused on illegal drug use prevention especially marijuana use]. Design: Cluster RCT. (one trial with two data sets; first including all adolescents (Longshore 2006), and second including at‐risk adolescents where at‐risk is defined as youth who had already used tobacco or marijuana before delivery of the curriculum in grade 7 (Longshore 2007)) (excluded from analysis). |
|
| Participants | Baseline: 4689 completed baseline survey; Longshore 2006: analytic sample of 4015 (85.6% of baseline); Longshore 2007: 1772 at‐risk students in baseline sample.
Age: 7th through 10th grade (12 ‐ 15 yrs).
Gender: 49.4% F (Longshore 2006); 44% F (Longshore 2007). Ethnicity: Longshore 2006: 11.7% non‐W ("mostly American Indian"); Longshore 2007: 19.6% non‐W ("mostly American Indian"). Baseline smoking data: Longshore 2006 analytic sample 4015: Past month tobacco: 9.4%. Longshore 2007 for high risk sample: baseline 1772: past month tobacco 33%, weekly tobacco 17.4%; 99% had tried tobacco. |
|
| Interventions | Category: Social influences vs social influences vs control [parental part is small so did not assess as multi‐modal]. Programme deliverer: Not stated. Intervention:
National Youth Anti‐Drug Media Campaign (focus on drug use, especially marijuana, no focus on tobacco) coincidentally nationally implemented nationally during grade 9 of ALERT Plus and had 3 foci: resistance self efficacy, anti‐drug norms, negative consequences of use. Control: "other prevention curricula already in place at their schools". Longshore 2006: N = 1613; Longshore 2007: N = 556. |
|
| Outcomes | Weekly use (= 3 ≥ days in past month); "saliva specimen that could be tested to detect drug use". Follow‐up: Intervention7th grade; follow‐up 9th grade survey administered 30m after baseline and delivery of 9th grade boosters in ALERT Plus schools. |
|
| Notes | Quality of intervention delivery: Adolescents asked how often had seen anti‐drug ads "in recent months" on TV, radio, newspapers, magazines, billboards, movie theatres or video rentals with 6 possible responses (not at all, < 1 a month, 1 ‐ 3 times a month, 1 ‐ 3 times a week, 1 ‐ 3 times a day; daily or almost daily, > 1 a day), and authors chose as outcome: at least 1 ‐ 3 times a week in any media; In ALERT Plus schools, 28 teachers delivered 9th grade programme and "teacher reports for 357 lessons indicated they covered all or some of each activity in 93% of the lessons and all of each activity except the wrap‐up in 80% of lessons. One or more of the activities was rushed in one third of the lessons. ...Overall, only 8% of lessons were interrupted by external events…". Statistical quality: Was a power computation performed? No. Was an intention‐to‐treat analysis performed? Yes. Was a correction for clustering made? Yes. Were appropriate statistical methods used? Backwards stepwise deletion to select covariates that predicted exposure to Campaign among a subsample; LR models, GEEs; missing data imputed using NORM. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Longshore 2006 and 2007: "45 school clusters, i.e., high schools and their associated middle‐school feeder(s), were randomly assigned to two treatment conditions or a control condition". Longshore 2007: "After we completed randomisation, two districts (each with one high school) recanted their decision to participate in the study. Schools in a similar region of the state and with a similar ethnic composition replaced the schools that dropped out". No method of randomisation stated. Clusters: School clusters. Cluster constraint: Longshore 2006 and 2007; "To enhance pretreatment equivalence across conditions, we used blocking by geographic region and community size and restricted assignment when randomising schools to conditions". Baseline comparability: No statement. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Longshore 2006: 4015 (85.67% of baseline 4689); "Adolescents who missed the 9th grade survey were more likely to be non‐White and male; to have low grades (C or below); to live with a single parent or step‐parent; to have reported use of alcohol, tobacco or marijuana at baseline; and to have elevated risk factors at baseline (e.g., offers to use drugs and intentions to use drugs)". Multiple imputation technique for missing data using NORM. Longshore 2007: "Of the 1,772 at‐risk students in the baseline sample, 389 (22%) were not surveyed in the ninth grade, leaving an analytic sample of 1,383 at risk students … Most (85.6%) of the 389 lost students had moved or were chronically absent and could not be tracked by phone or mail follow‐up. Overall, students lost at ninth grade were more likely to be male, be non‐White, have low grades, have parents with low educational attainment, live with a single parent or stepparent, and have used tobacco or marijuana as recently as the past month at baseline or report weekly use of these substances. However, when weighted to account for differential loss at follow‐up, the analytic sample was nearly identical to the original baseline sample of at‐risk students…Attrition rates were very similar for the control and Alert Only conditions (24.5% and 23.4%, respectively) and slightly lower for ALERT Plus (20.2%)". "self‐reported tobacco use was highly consistent with cotinine levels in a random sample of 654 saliva specimens". [assessed as UNCLEAR as no assessment of differential attrition of tobacco users across groups]. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Lotrean 2010.
| Methods | Country: Romania
Site: 20 schools (10 intervention, 10 control) in Cluj‐Napoca (25 schools approached). Focus: Smoking prevention. Design: Cluster RCT (Group 3: point prevalence). |
|
| Participants | Baseline: 1071 (523 intervention, 548 control).
Age: 13.7 yrs (mean).
Gender: 50.9% F intervention, 51.5% F control. Ethnicity: Not stated. Baseline smoking data: Weekly smoking: intervention 7.5%, control 8%. |
|
| Interventions | Category: Social influences vs. control. Programme deliverer: Peers (1 hr training); assistance by teachers (1 hr training); manuals. Intervention: 5 weekly lessons of 45 mins. Social influences and tobacco refusal skills; Each lesson included introduction of theme on video, peer‐led activities in small groups, continuation of lesson in group on video, peer‐led activities in small groups, sometimes home activities. Control: No statement. |
|
| Outcomes | Self report. Nonsmokers (never having smoked, experimented with smoking but had quit; experimenting with smoking, but not smoking weekly and those who had quit); or regular smokers (at least once a week). [E‐mail from Dr. Lotrean 9 Dec 2011 says nonsmoker data in article includes quitters, experimenters]. Follow‐up: 6m. |
|
| Notes | Quality of intervention delivery: Students evaluated programme overall, lessons on videos, watching videos, home activities, activities during lessons, manual, working in groups, having a peer leader, assistance by peer leader, assistance by teacher. 523 students completed process evaluation (on scale ‐2 to +2): Programme 1.10; watching videos 1.36; lessons on video 1.15; manual 1.23; activities during lessons 1.24; home activities 1.03; working in groups 1.39; having a peer leader 1.33; assistance by peer leader 1.29; assistance by teacher 1.35. Statistical quality: Was a power computation performed? Yes. For α = 0.05 and power of 95%, drop‐out rate 15% required 2 x 483 nonsmokers. Was an intention‐to‐treat analysis performed? No. Was a correction for clustering made? Yes. Were appropriate statistical methods used? LR to compare participants and drop‐outs; Х² and independent sample t‐tests to compare treatment conditions; multilevel analyses. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "randomly assigned 10 schools to the experimental and 10 to the control condition. All names of the schools were put into a box and an independent person picked out names one by one until 10 schools were out of the box. These fist 10 names were assigned to the first group and the remainder of the schools were assigned to the second group. Then, by tossing a coin, the two groups were randomly assigned to the experimental or control group". Clusters: Classes and schools. Cluster constraint: None. Baseline comparability: "No significant differences were found between the experimental and control groups with respect to the prevalence of health‐risk behaviours". |
| Allocation concealment (selection bias) | Unclear risk | Not possible to judge whether the person tossing the coin was independent or aware of the school groups. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Drop‐out rates similar (P > 0.05) in both conditions: 11% intervention, 9.8% control; no significant differences for gender, health risk behaviours (truant monthly, monthly alcohol, spending time frequently in bars/discos), bad school achievement, spending > 15 EUR per month); weekly smoking experimental 7.5%, control 8.0%. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
MacPherson 1980.
| Methods | Country: USA. Site: 8 school superintendencies in Vermont Focus: Prevention of smoking by past and current cigarette smokers. Design: RCT (excluded from analysis) | |
| Participants | Baseline: 1750 students in 85 classrooms (82% of eligible).
Age: Not stated.
Gender: Not stated Ethnicity: No data Baseline smoking data: Current smokers: (Mobile unit 1.2%; Traditional group 2.6%, Combination 5.4%, Control 3.3%) |
|
| Interventions | Category: Information vs. control Programme deliverer: Teachers, researchers, lung educators Intervention:
Control: No statement |
|
| Outcomes | Definition of smoking: 'Current cigarette smokers'; 'Past cigarette smokers' Follow‐up: 6m. | |
| Notes | Quality of intervention delivery: No process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? No Were appropriate statistical methods used? The unit of allocation was the superintendencies and the unit of analysis was the individual; 'Significance' reported but no level or statistical measure stated. SPSS |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'A representative sample of 8 of the 56 school superintendencies from the state of Vermont was selected to participate in the study. These 8 were chosen to be similar with respect to attendance rates, school nurse density, district wealth, expenditures per student, population, experience of the educational staff and physical facilities. Each study superintendency served five or six rural communities with each community usually having a single elementary school ...unexpected circumstances did not permit two to participate ... school superintendencies were randomised into each curricular modality using a table of random numbers' Clusters:schools (unit of analysis individuals) Cluster constraint: schools preselected for similarity Baseline comparability: Not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 21% attrition; no attrition analysis Number at follow up: Completed questionnaires were obtained from 1750 students in 85 classrooms at baseline (82%), and 1683 (79%) 6m later, including 345 (86%) from the group which only received the post‐test. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
McCambridge 2011.
| Methods | Country: UK
Site: 12 London Further Education Colleges (of 21 approached) Focus: Prevent substance use (cigarettes, alcohol, cannabis) in non‐users, reduce risks among users Design: Cluster RCT (Group 3: point prevalence) |
|
| Participants | Baseline: 416 (206 intervention, 210 control)
Age: 17.5 years
Gender: 55% intervention; 52% control Ethnicity: Intervention: 27% W, 46% B, 17% Asian, 10% mixed/other; Control: 24% W, 48% B, 19% Asian, 9% mixed/other Baseline smoking data: Smoking: intervention: 27% W, 46% B, 17% Asian, 10% mixed/other; control: 24% W, 48% B, 19% Asian, 9% mixed/other. Non smokers: intervention N = 140 (68%), control N = 159 (76%) |
|
| Interventions | Category: social influences vs. control Programme deliverer: 2 researchers, 6 college‐based practitioners (received workshop based training) Intervention: 1 hr ‐ 'motivational Interviewing' (perceptions of risk, problem recognition, concerns, consideration of change, activity of practitioner in directing attention to resolution of ambivalence) "Motivational interviewing is a highly individualised intervention. Its aim is to help the participant explore their own behavior. Particular emphasis is given to perceptions of risk and problem recognition, concerns, and consideration of change, and also to the activity of the practitioner in directing attention towards the resolution of ambivalence... participants were encouraged to think through and discuss a series of hypothetical situations in which they might find it difficult to refuse offers of drugs they had not previously used. We also explored the reason for not using specific substances, and how initiation of use might affect future plans." Control: Authors designed 'Drug Awareness' bases on usual practice as described by college‐based practitioners (quiz, discussion, leaflets). |
|
| Outcomes | Prevalence; For smokers: 30‐day; number per day. Follow‐up: 3 and 12 months. |
|
| Notes | Quality of intervention delivery: 31/150 Motivational Interviewing sessions audio‐recorded ‐ "There were differences in outcome apparent between the three practitioner groupings." Statistical quality: Was a power computation performed? Yes, computed 420 subjects needed for effect size = 0.40, assuming within‐cluster variance = 0.9, ICC = 0.01, 2/3 users α = 0.05, power = 80% Was an intention‐to‐treat analysis performed? Yes (last observation carried forward) Was a correction for clustering made? Yes using Huber/White Sandwich estimator of variance Were appropriate statistical methods used? Logistic regression, multiple regressions |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised randomisation by Clinical Trials Unit Clusters: Classes Cluster constraint: "stratified by college so equivalent numbers from any one college allocated to each study condition". Baseline comparability: Equivalent on gender, language, race, substance use "randomisation successfully created baseline equivalence between groups". |
| Allocation concealment (selection bias) | Low risk | "..decisions were communicated by telephone to researchers after recruitment and baseline data collection on an individual college basis to preserve allocation concealment." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Baseline: 206 Motivational Interviewing, 210 Drug Awareness; 12 months: 169 Intervention (82%), 179 (85%) Drug Awareness. No differential attrition. "Older study participants were more likely to be lost to follow‐up at both intervals…..as were males at both intervals…mixed race or other at 3 months compared to white, black, Asian…..those who ever sold drugs…cigarette smokers at 3 months (19% [22/117] smokers, 8% [23/299] non‐smokers, x2 [1] = 10.76, p = 0.001)… and cannabis smokers." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Murray 1984a.
| Methods | Country: USA
Site: 8 junior high schools in Minneapolis (study 1 & study 2) 'Minnesota Smoking Prevention program' Focus: smoking prevention Design: cluster RCT (Group 1: never smoking prevention cohort, not included in analysis) |
|
| Participants | Baseline: Study 1: 3184 7th graders (94% of enrolled 7th graders); Study 2: 3846 (two additional schools, non equivalent control)
Age: 12 Gender 50% F Ethnicity: "nearly all white" Baseline smoking data: 49‐62% were non smokers |
|
| Interventions | Category: social influences (adult vs peer‐led) Programme deliverer: teachers, peers Intervention: 5 sessions over 6 m
Control: "Two additional schools, not randomised, provided a non‐equivalent control group for the second study." |
|
| Outcomes | Smoking Index (Pechacek) of average cigarettes/week. Separate analyses for baseline never‐smokers and those with scores 0‐1, with categories of ever, weekly and daily smoking incidence. Index used as a continuous measure for smoking intensity. Saliva test for thiocyanate at pre‐ and post‐test and 1yr follow up. Outcome assessed for baseline nonsmokers and experimental smokers. Follow up: Post‐test, 1yr (1981), 2yr (1982), 3yr (1983), 5yr (1985), 6yr (1985/6) | |
| Notes | Quality of intervention delivery: no process analysis; however, all interventions were led or facilitated by programme staff. Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? No, statistical modelling to allow for allocation by school. Were appropriate statistical methods used? For study 2 only the experimental groups could be compared, as the non‐equivalent control groups were selected in the 2nd year of the study; large sample size, but small number of clusters; LR for dichotomous smoking incidence and prevalence dependent variables, ANOVA for intensity of smoking. Adjustments made for baseline differences. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "During the 1979 ‐ 80 school year, the entire seventh grade population in each of eight suburban Twin Cities junior high schools participated...The eight schools were ranked based on the baseline prevalence of weekly smoking. They were randomly assigned to the four treatment conditions from the upper and lower halves of the weekly smoking distribution...Two additional schools, not randomised, provided a non‐equivalent control group for the second study." (Twin Cities = Minneapolis and St. Paul, Minnesota). Method of randomisation not stated Clusters: Schools Cluster constraint: Schools ranked according to baseline prevalence of weekly smoking, split into top and bottom half. Baseine comparability: Not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No differential attrition: "In both Study I and Study II, significantly more baseline ever‐smokers were lost to follow‐up than were baseline never‐smokers (8.9% vs. 5.9%); however, this greater loss of baseline ever‐smokers was small and, more important, was equivalent across the study conditions." Study I at baseline = 3181, after 6 years = 2879 (90.5%); Study II (began one year later) at baseline = 3943 (included two non‐randomised control groups) and after 5 years = 3557 (90%) |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Murray 1992 (MDEG).
| Methods | See Murray 1992 (MSPP) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from the third intervention arm within Murray 1992 (MSPP) | |
Murray 1992 (MSPP).
| Methods | Country: USA
Site: 48 sampling units in Minnesota (from 112 invitees) 'Minnesota Smoking Prevention Program' (MSPP) and 'Smoke‐Free Generation program' (SFG) Focus: compare 3 social influences anti‐tobacco programmes with the existing curriculum Design: cluster RCT (Group 3: point prevalence) |
|
| Participants | Baseline: 8992 eligible; 8271 (92%) participated (7180 enrolled in 7th grade) Age: 6th grade (11‐12 years) Gender: 50% M Ethnicity: not stated Baseline smoking data: smoking prevalence: MSPP = 1.4%, SFG = 1.3%, Minnesota guidelines = 1.8%, control = 0.6% |
|
| Interventions | Category: social influences vs. control Programme deliverer: teachers (received a 2 hr instructional videotape) Intervention:
Control: Existing curricula |
|
| Outcomes | Smoking defined as an Index of weekly smoking (number of cigarettes/week), and expired CO was measured Follow‐up: 9th grade |
|
| Notes | Quality of intervention delivery: For the process analysis 1 researcher observed 90% of the health teachers in the 81 schools once, and the MSPP had higher compliance than the 2 other programmes, with the control having the lowest compliance; differences in teacher compliance with programme implementation between groups. Statistical quality: Was a power computation performed? The power analysis hypothesized that the most effective intervention would result in a 50% reduction in the incidence of weekly smoking, (4.5% vs 9% in the existing curriculum group), and the other curricula would have intermediate effectiveness. Estimated sample sizes achieved. Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? Not stated Were appropriate statistical methods used? Within‐school ICCs were estimated = 0.02, and the variance reduction expected from covariance adjustments (25%), 2‐tailed tests, Type I error rate = 5%, and power = 80%, that usable data be required from 90 students from each of 12 sampling units to detect treatment effects using hierarchical ANOVA |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "One of the goals of the Two State Comparison Study was to employ samples that represented the entire ninth grade enrolments in Minnesota and Wisconsin... As a result we developed a sampling plan that gave each ninth grade student in those states a roughly equal chance of selection. Instead of sampling schools per se, since they vary widely in size, we defined a range for the size of an artificial sampling unit such that: (1) the largest unit would be no more than twice the size of the smallest unit and (b) the average expected unit size would be 14% larger than the required unit size obtained from the power analysis... From the 468 Minnesota and 441 Wisconin public schools that included ninth graders in 1985‐1986, 694 Minnesota and 781 Wisconsin sampling units were created. These units were listed in random order for each state and invited in sequence to participate in the Two State Comparison study. When a unit declined participation, the next unit on the list for the same state was invited." Although the actual method of randomisation was not stated, bias is unlikely Clusters: sampling units Cluster Constraint: not stated Baseline comparability: not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 13% attrition in 2nd yr and those lost to follow‐up had more family members and friends who smoked, but there was no differential attrition across groups; students reported exposure to 2 ‐ 3 traditional anti‐smoking programmes, but there were no differences between groups during the study. Those lost to follow up were more likely to report smoking by their father (P < 0.0005), mother (P < 0.0001), older siblings (P < 0.0024) and best friend (P < 0.0012). |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Murray 1992 (SFG).
| Methods | See Murray 1992 (MSPP) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from the second intervention arm within Murray 1992 (MSPP) | |
Noland 1998.
| Methods | Country: USA. Site: 19 schools in Kentucky. Focus: Tobacco use prevention in a high tobacco production area. Design: Cluster RCT (Group 3: point prevalence) | |
| Participants | Baseline: 3588 Age: average 12.4 yrs. Gender: 51% F Ethnicity: 92% W; 6% B; 2% O Baseline smoking data: mean percentage ever use (adjusted): intervention = 51.1 (3.3), control = 51.4 (2.3) |
|
| Interventions | Category: social influences vs. control Programme deliverer: project staff educators & peers Intervention: 9 sessions over 2yrs. Social influences programme consisted of 6 X 45 ‐ 50 min sessions in the 7th grade (skills training in learning to recognize types of peer pressure, refusal skills, and assertiveness, recognizing and countering advertising appeals, student pledges, the negative social and immediate physical consequences of using tobacco; peer leaders were trained); and 3 similar sessions in the 8th grade. Control: Usual health education |
|
| Outcomes | Smoking: Ever, 30‐day, 7‐day, and 24‐hr smoking. Expired air was collected and CO content was analysed, but not reported. Follow‐up: 2yrs from baseline | |
| Notes | Quality of intervention delivery: No process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Yes Were appropriate statistical methods used? "The school was used as the unit of analysis in evaluating program effectiveness. For baseline scores, mean responses were computed for each school, and a 2‐sample t test based on these means was used to compare groups... A mixed‐model analysis of variance was used to compare means between the groups after adjustment for the covariates: tobacco involvement and baseline scores... Pearson correlations between carbon monoxide readings and self‐report of tobacco use were calculated with the student as the unit of analysis." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The sample included 19 schools in 14 counties. The counties involved produce an average of 7.7 million lb (3.5 million kg) of tobacco annually... In the fall of 19792, all seventh graders in the 19 study schools were surveyed. As a means of making groups more comparable, schools were then ranked by baseline tobacco usage to form 10 blocks of 2 schools each ...The experimental treatment and control conditions were randomly assigned to a single school within each block." Clusters: Schools Cluster constraint: Ranked by baseline tobacco usage to form 10 pairs Baseline comparability: Groups were similar at baseline on smoking status. There was no differential attrition from baseline between groups. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | At 24 months 14.4% attrition; no differential attrition. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Norman 2008.
| Methods | Country: Canada
Site: 14 secondary schools in Toronto (81 classes) 'Smoking Zine' through 'TeenNet' Focus: Smoking prevention and cessation Design: Cluster RCT (although individuals randomly assigned to treatment vs. control group by computer, students were in classes and participated in class activities), (excluded from analysis) |
|
| Participants | Baseline: Eligibles 2210; 1402 randomly assigned (548 grade 9, 418 grade 10, 436 grade 11)
Age: Grades 9 to 11 (age 11 – 17)
Gender: 46% F Ethnicity: East Asian 16% (220), Eastern European 16% (220), Central Asian 12% (172), 17 % (235) omitted their ethnicity, remainder not stated. Baseline smoking data: Not stated for groups, but "211 (15%) assessed as smokers at baseline" for total sample. |
|
| Interventions | Category: Other interventions vs. control This intervention did not align with the main five categories; the programme intervenes by assessing readiness to change smoke intentions and encouraging change using a website. Programme deliverer: Motivational interviewing led by graduate level counsellors or public health nurses (received 2 days "intensive training") Intervention: 4 components:
First three components delivered in 60‐minute session, emails monthly post intervention for 6 m Control: Evaluated 3 web sites on climate change, wrote journals and participated in small group discussions, generic monthly e‐mails to evaluate online information |
|
| Outcomes | Smoker (> 2 cigs past month and > 100 in lifetime); self‐report (initially CO measurement served as a bogus pipeline) Follow‐up: post intervention, 3 m and 6 m |
|
| Notes | Quality of intervention delivery: Apart from server problems in 3 schools on 1 day "No serious implementation issues.". Investigators or team leader monitored implementation during class session and 15.48/17 recommended discussion points were covered in smoker and 16.01/17 in non‐smoker groups; expired CO monitoring (served as 'bogus pipeline') suspended during SARS epidemic Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Yes Were appropriate statistical methods used? Path analysis using MPlus; multilevel logistic regression to assess multi‐level model; because distribution of outcome scores differed between groups, tobacco scores dichotomised |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly assigned to each group by computer at the individual level with an algorithm using the PHP programming language…" Clusters: Schools, classes, individuals Cluster constraint: "Eighty–one classes were sampled from fourteen secondary schools in the Greater Toronto area using a purposeful, stratified, and modified snowball sampling approach that included an initial strategic selection of schools to balance differences in school size, neighbourhood (location) and unique characteristics (e.g. single‐sex schools and special education programs) to reflect the diversity of the community and population. Schools that were interested in our study referred us to other schools they believed fit our criteria …" Baseline comparability: More smokers Eastern European or Mediterranean (p < 0.001); no statement if groups differed on smoking status (Table 4 incorporates post‐test, 3 and 6 m follow‐up data and does not state separate results for baseline. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 87% at 6 m; multilevel regression to estimate missing data; 5% of e‐mail addresses for follow up e‐mails were invalid; no assessment if differential attrition between groups |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Nutbeam 1993 (FSE).
| Methods | Country: U.K. Study site: 39 secondary schools in 4 different educational authorities in Wales and England (10 schools (controls), 10 schools (FSE), 9 schools (SAM), and 10 schools (both projects in sequence FSE/SAM)) Focus: Smoking prevention and changes in attitudes, knowledge, and values toward smoking; evaluating effectiveness of 2 school‐based smoking education programmes Design: Cluster RCT (Group 1: never smoking prevention cohort) | |
| Participants | Baseline: 5078 students were eligible, with 4562 (89.8%) completing the pretest Age: 11 ‐ 12 yrs Gender: 2188 F and 2347 M Ethnicity: Not stated Baseline smoking data: non‐smokers: control = 951, intervention 1 (FSE) = 848, intervention 2 (SAM) = 732, intervention 3 (FSE + SAM) = 924 |
|
| Interventions | Category: Social influences vs. social influences vs. control Programme deliverer: Classroom teachers (received 1‐day training) Intervention: 3 m
Control: No formal interventions |
|
| Outcomes | Self‐reported smoking (never; tried once or twice; < 1 cig/week; 1‐6 cigs/week; > 6 cigs/week). Saliva for thiocyanate levels collected but not processed or analysed; 5 scales assessing health knowledge, self‐esteem, health values, external and internal locus of control Follow‐up: immediate post‐test following programmes and 1yr after |
|
| Notes | Quality of intervention delivery: "… the organisation and management of the projects were at the discretion of the teachers, who recorded their lessons in a book." Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made?Yes Were appropriate statistical methods used? "Mixed model analysis of variance was used to test for the effects of intervention. School was fitted as a random effect nested within groups.The two projects were fitted as fixed effects... The maximum likelihood method was used to fit the models... Chi‐squared was used to test for overall differences in proportions ..." (and adjusted for clustering). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Cluster randomised controlled trial." ‐ e‐mail from Dr. Nutbeam says method was by using cards from a hat. "The schools were not a strict random sample since in two of the areas schools were approached because of their past commitment to health education. In the other two authorities the schools were selected randomly from school lists. The schools were matched by size and catchment area and assigned to one of four groups..." Clusters: schools Cluster constraint: schools matched by size and catchment area Baseline comparability: 83% never‐smokers in the FSE/SAM and 74% in the SAM group (P = 0.02); difference in rates of non‐smokers (P = 0.03), non‐significant after adjusted for potential confounders |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 4538 before teaching (1988), 3930 immediately after teaching (1989), 3786 at one year follow up (1990) (83.4%). "Pupils were significantly less likely to have participated in the follow up studies if at baseline they had reported being smokers or having previously smoked or tried cigarettes, if their father or mother was a smoker, or if their father was unemployed or a manual worker."; no differential attrition analysis. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Nutbeam 1993 (FSE+SAM).
| Methods | See Nutbeam 1993 (FSE) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 3rd intervention arm (FSE+SAM) within Nutbeam 1993 (FSE) | |
Nutbeam 1993 (SAM).
| Methods | See Nutbeam 1993 (FSE) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm within Nutbeam 1983 (FSE) | |
O'Donnell 1995.
| Methods | Country: USA
Site: Seattle 'Seattle Social Development Project' Focus: School failure, drug abuse, delinquency Design: RCT (excluded from analysis) |
|
| Participants | Baseline: 424
Age: 5th grade (10 ‐ 11 years) Gender: 48% F Ethnicity: 49% European American, 22% African American, 19% Asian‐American, 6% Native American, 4% Other Baseline smoking data: not stated |
|
| Interventions | Category: social competence vs. control Programme deliverer: teachers Intervention:
Control: teachers did not receive training in instructional skills; teachers were observed to document their teaching practices during four classes on different days |
|
| Outcomes | Smoked cigarettes (not further defined) Follow‐up: 1.5 years from baseline |
|
| Notes | Quality of intervention delivery: Teachers observed and given feedback every 3 weeks; control teachers observed over 4 periods to document their teaching practices; no numerical presentation of process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? Non‐randomly assigned groups not separated from randomly assigned; students randomly assigned as individuals or to classes not separately analysed; statistical method not stated; apparently by differences of means; students in intervention or control groups enrolled in 5th or 6th grade for < 1 semester were excluded from the analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | In 1981, 2 schools assigned to either intervention or control and then students in the remaining 6 schools randomly assigned; then from 1981 ‐ 1984 newly entering students were randomly assigned to intervention or control classrooms; and in 1985 study expanded to include all 18 Seattle elementary schools. Method of randomisation not stated Clusters: not clear, schools, individuals and subsequently classes Cluster constraint: not stated Baseline comparability: not stated |
| Allocation concealment (selection bias) | High risk | Inadequate |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 40% attrition; no differential attrition Baseline 1985 when entered 5th grade: results are reported only for 177 low income students (42%) from the 424 students in 5th grade; Completion of 6th grade in 1987: 106 (60%) of the low income group completed 6th grade surveys. |
| Selective reporting (reporting bias) | Unclear risk | No statement |
Perry 1996.
| Methods | Country: USA
Site: Rural communities in 6 NE Minnesota counties (24 school districts merged into 20 districts) Project 'Northland' Focus: diminishing alcohol use; tobacco and marijuana use also measured but no specific intervention Design: cluster RCT (Group 3: point prevalence) |
|
| Participants | Baseline beginning of 6th grade: 2351 Age: 6th grade (11 ‐ 12 years) Gender: no data Ethnicity: no data Baseline smoking data: non‐smokers = 61% |
|
| Interventions | Category: multimodal vs. control Programme deliverer: teachers, peers, parents Intervention: Project Northland had 4 components: parent involvement/education; behavioural curricula; peer participation; community task force activities. Each grade had a unique theme: 6th grade (Slick Tracy Home team programme); 7th grade (Amazing Alternatives! programme); and 8th grade (Power Lines). (40% of students had taken part in Project DARE, 2% taken part in Project Quest sponsored by the Lion's Club) Control: usual alcohol and other drug education programmes (90% of students had taken part in Project DARE, 21% taken part in Project Quest sponsored by the Lion's Club) |
|
| Outcomes | Cigarette and smokeless tobacco use defined as > 2 or 3 uses in lifetime, and then defined as occasionally but not regularly; regularly in the past; or regularly now. Follow‐up: 2.5 years from baseline |
|
| Notes | Quality of intervention delivery: all schools implemented the curricula; peer leaders organised 60 alcohol‐free activities in 16 of 20 intervention schools during the year; and half of the students participated in peer out‐of‐school non‐alcohol activities; of the 66 adult volunteers recruited, 33 remained active in the programme throughout the year. "School district intra‐lass correlations ranged from 0.002 (past week alcohol use, spring 1994) to 0.03 (past year alcohol use, spring 1993), with a median value of 0.15. (Other intra‐class correlations available from the authors)." Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? No Were appropriate statistical methods used? Mixed model regression and ANOVA to adjust for ICCs |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Project Northland, conducted in northeast Minnesota, involves mostly rural, lower‐middle‐class to middle‐class communities... This area of Minnesota rates at the top in terms of alcohol‐related problems in the state. There are seven Amerian Indian reservations in the area. The 24 school districts were recruited systematically; 4 smaller school districts were combined with nearby districts (to ensure an adequate sample size in each unit to be randomised), and these 20 combined districts were blocked by size (small, medium, lage, very large), and randomised to an intervention condition (N = 10) or a reference condition (N = 10)." E‐mail from Dr. Perry (28 Dec. 2011): "We assigned the districts numbers and used a random numbers table to assign the 20 districts to education or delayed control groups." Clusters: school districts Cluster constraints: 24 school districts combined into 20 then blocked by size and randomised Baseline comparability: more cigarette smoking (P < 0.05) at baseline in Intervention compared to reference districts, no significant difference for smokeless tobacco; more students in intervention districts reported alcohol use at baseline; fewer White and more American Indian students in intervention districts. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 19 % attrition by end of 8th grade (no differential attrition). |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Perry 2003 (Dare boys).
| Methods | Country: USA
Site: 24 middle and junior high schools in Minneapolis and St. Paul, Minnesota (8 schools to DARE, 8 to DARE. and DARE Plus, and 8 to control with delayed delivery of DARE) 'DARE & DARE Plus' Focus: tobacco, alcohol and marijuana use and violent behaviour Design: cluster RCT (Group 2: change rates) |
|
| Participants | Baseline 6726 7th graders in 1999 ‐ 2000 or 8th grade in 2000 ‐ 2001; of these 6237 (82.7%) completed the baseline questionnaire (2226 DARE; 2221 DARE Plus; 1790 control)
Age: middle and junior high school
Gender: 48.4% F Ethnicity: 67.3% White Baseline smoking data: shown in growth curve analysis |
|
| Interventions | Category: social influences vs. multimodal vs. control Programme deliverer: police officer instructors (received instruction in the elementary school DARE curriculum and had taught DARE for at least 2 semesters; those who taught DARE Plus received an additional 2 hrs instruction on interactive teaching methods). Intervention:
Control: no intervention |
|
| Outcomes | Current use of tobacco on a scale from 1 to 10 Follow up: after 18m at the end of 8th grade. E‐mail from Dr. Perry 28 Dec. 2011: "average length of follow‐up following the school‐based component was 5 months to final follow‐up". |
|
| Notes | Quality of intervention delivery: no process data for DARE; for 1461 in DARE PLus, Youth Action Teams conducted 420 meetings and planned and executed 310 activities; 411 mini‐proposals funded; authors state "high participation rates" and "extraordinary support on the part of the school districts and police departments", but no further details or references Statistical quality: Was a power computation performed? Yes. Power computation for 80% power and alpha = 0.05 and ICC = 0.008, the design could detect a 43% reduction in behaviours with a population prevalence of 10% and a 24% reduction in behaviours with a prevalence of 30%; schools were surveyed and those with at least 200 in the 7th grade were "targeted for sufficient statistical power". Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Yes. 3‐level linear random coefficients model testing for differences in growth curves over time and account for clustering. Were appropriate statistical methods used? 3‐level linear random coefficients model testing for differences in growth curves over time and account for clustering. Data on extracurricular activities analysed with mixed model linear regression. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...24 middle and junior high schools in Minnesota that were matched on socioeconomic measures, drug use and size and randomly assigned to 1 of 3 conditions." E‐mail from Dr. Perry 28 Dec. 2011: "we formed 8 triples of schools (N = 24), so that schools within a triplet were matched on socio‐demographic data. We used random numbers to assign schools within triplets to one of three conditions." Clusters: schools Cluster constraint: matched on socioeconomic measures, drug use and size Baseline comparability: no differences at baseline |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 16 % attrition No differential attrition "The main outcomes of the study were analysed using growth curve analyses. This analytic method permits retention of subjects who do not have complete data." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Perry 2003 (Dare girls).
| Methods | See Perry 2003 (Dare boys) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from the female participants in the Dare intervention arm within Perry 2003 (Dare boys) | |
Perry 2003 (Dare+ boys).
| Methods | See Perry 2003 (Dare boys) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from the male participants in the Dare plus intervention arm within Perry 2003 (Dare boys) | |
Perry 2003 (Dare+ girls).
| Methods | See Perry 2003 (Dare boys) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from the female participants in the Dare plus intervention arm within Perry 2003 (Dare boys) | |
Perry 2009.
| Methods | Country: India
Site: 16 schools in Delhi and 16 in Chennai (8 private and 8 state within each 16 schools) Focus: prevention of use of cigarettes, bidis and chewing tobacco 'Mobilising Youth for Tobacco Related Initiatives (MYTRI)' Design: cluster RCT (Group 2: change rates / Group 3: point prevalence) |
|
| Participants | Baseline: 12484 (Stigler 2011 states: "All students enrolled in participating schools in the 6th and 8th grades in 2004 (i.e. N = 12,484), 7th and 8th grades in 2005 (i.e. N = 12,075), and 8th and 10th grades in 2006 (i.e. N = 12,752) were eligible and invited to complete each survey... The study focuses on the 14,085 students who completed one or more of the three surveys : 6,365 (45.3% ) completed three surveys, 3,780 (26.9%) completed two surveys, and 3,918(27.9%) completed one survey.")
Age: 6th and 8th grade (average age 11 and 12.8 respectively)
Gender: 48.4% F Ethnicity: not stated Baseline smoking data: past 30 days ‐ intervention: cigarettes 0.43, bidis 1.25, or chewed tobacco 0.97, or any tobacco 3.42; control: smoking cigarettes 0.00, bidis 0.00, or chewed tobacco 0.14, or any tobacco 1.38 |
|
| Interventions | Category: social influences vs. control Programme deliverer: teachers and peer leaders (training and manuals) Intervention: four components ‐ (1) 7 peer‐led classes for 6th and 8th graders; 6 additional classes for 7th and 9th graders; (2) 6 posters; (3) 6 postcards sent parents; (4) peer leadership activism. Aim of intervention to to influence environmental factors (social norms, role models, social support and opportunities) and intrapersonal factors (knowledge, values, meanings, beliefs, skills) that predict tobacco use. Classroom supplies and handbook for each student. Control: Delayed intervention |
|
| Outcomes | Self reported past 30 days cigarette, bidi and smoking tobacco; if yes to any = current user Follow‐up: after one year of intervention and two years, at conclusion, of intervention |
|
| Notes | Quality of intervention delivery: 88% of all curriculum activities completed in 1st year and 93% in 2nd; all posters hung; 76% of postcards sent (58.7% of signed postcode stubs returned); 678 students trained to be peer leaders in first year, and 761 in second; 53 teachers trained 1st year and 133 in second; 3569 students (67% of intervention cohort) attended an interschool activity in 1st year and 4652 (81%) in 2nd. Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated, although ‘growth curve analysis methods allowed estimates of tobacco use trajectories over time among students who did not complete the final survey’ Was a correction for clustering made? Yes, not stated, but used multilevel model. Were appropriate statistical methods used? Yes, mixed effects regression; for repeated measures (growth curve analysis), mediation analysis (comparison of changes in mediators and outcomes). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Schools were stratified by city, matched by school type and gender, and randomly assigned to intervention groups and delayed‐intervention groups..." From author correspondence ‐ "We then used random numbers to assign schools within pairs to treatment condition." Clusters: schools Cluster constraint: stratified and matched Baseline comparability: no baseline differences in cigarette and chewing tobacco, but intervention > control for bidis (P < 0.05); no baseline differences in intention to use tobacco or any psychological variable related to tobacco use. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "In 2004, all 32 schools participated in the survey; in 2005 and 2006, 2 schools did not participate as a result of conflicting academic schedules… An additional 3 schools would not allow 10th graders to participate in 2006 because of upcoming national exams. All students enrolled in the participating schools in the 6th and 8th grades in 2004 (N = 12484), in the 7th and 9th grades in 2005 (N = 12075), and in the 8th and 10th grades in 2006 (N = 12752) were eligible… Response rates were 94.1% in 2004 (N = 11748), 94.7% in 2005 (N = 12821) and 84% in 2006 (N = 10625). < 1% provided inconsistent replies and were excluded; no between group differences in missing data about tobacco use." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Peterson 2000.
| Methods | Country: USA
Site: 40 school districts in Washington state (20 intervention, 20 control) 'Hutchinson Smoking Prevention Project' (HSPP) Focus: tobacco Design: cluster RCT (Group 1: never smoking prevention cohort) |
|
| Participants | Baseline: 8388 (4177 intervention, 4211 in control) Age: 3rd grade (7 ‐ 9 years) Gender: 49.2% F Ethnicity: 89.8% Caucasian, 2.9% Hispanic, 2.0% native, 1.6% Asian, 0.7% African, 3.0% mixed and other Baseline smoking data: collected in grade 5 'Not tried cigarettes': intervention = 88.2%, control = 89.2%; 'Not tried smokeless tobacco': intervention = 93.6%, control = 94.9% |
|
| Interventions | Category: social influences vs. control Programme deliverer: teachers Intervention: students received 65 sessions consisting of: (1) skills to identify marketing and peer influences to smoke; (2) skills to resist marketing and other influences; (3) information to correct erroneous perceptions about smoking; (4) motivation to be smoke‐free, and distinguishing between what the adolescent wants to do and is able to do; (5) promoting self‐confidence in the ability to refuse influences and pressure to smoke; (6) enlisting positive family influences. Control: schools continued usual health curricula |
|
| Outcomes | Self reported smoking in Grade 12 and Gr 12 + 2; saliva cotinine measured on a 12.6% random sample of Grade 12, and no differential bias in reporting between experimental and control groups. Follow‐up: 10 years, 12 years |
|
| Notes | Quality of intervention delivery: all teachers participated in the training; > 99% implemented the interventions; and teachers effectively communicated the key concepts in 80% of the lessons observed Statistical quality: Was a power computation performed? Yes, based on number of districts, number of students, actual attrition, prevalence of daily smoking at Grade 12 + 2yrs; programme exposure estimated at 0.745 due to out migration, ICCs of 0.01, and 2‐sided alpha = 0.05, which was estimated to provide power to detect a 30% nominal relative reduction in daily smoking prevalence at the endpoint 2 yrs after high school. Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? No Were appropriate statistical methods used? Analysis by randomisation‐based permutation inference, which requires no distributional or modelling assumptions, and accommodates ICCs. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Schools selected with < 35% attrition from Grades 3 to 7, 50‐250 students/grade level, and within 200 miles of study HQ, matched on high school smoking, size and location. School districts were assigned randomly to one of two conditions: "The randomisation was witnessed by two non‐study FHCRC scientists... a computerized coin flip for each randomly ordered pair". Clusters: school districts Cluster constraint: pair matching Baseline comparability: "A comparison of the distribution of the baseline variables between experimental and control conditions shows that the randomised assignment of of the school districts generally provided good balance in the important variables between the two conditions." |
| Allocation concealment (selection bias) | Low risk | "... that was performed openly and witnessed, recorded, and signed by to two non‐HSPP scientists." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Major effort was invested in explaining the purpose of the RCT and maintaining the long‐term collaboration of the school districts, parents and students and there were 7,865 (94%) at follow‐up two years after Grade 12. At Grade 12 + 2 yrs follow up 48 developmentally unable to participate, unable to locate 241, 181 no reply, 8 declined, yielding 7864 (93.8%). |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Piper 2000 (HFL Age).
| Methods | See Piper 2000 (HFL) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm within Piper 2000 (HFL) | |
Piper 2000 (HFL).
| Methods | Country: USA
Site: Suburbs, small towns and rural areas in Wisconsin 'Healthy for Life Project' (HFL) Design: Cluster RCT (Group 1: never smoking prevention cohort) |
|
| Participants | Baseline: 2483
Age: 6th grade (68% 14yrs, 29% 15yrs)
Gender: 52% F Ethnicity: % white: intervention 1 (HFL) N = 758 (92%), intervention 2 (HFL age appropriate) N = 827 (94%), control N = 898 (94%) Baseline smoking data: past month cigarette use: intevention 1 = 4%, intervention 2 = 5%, control = 5% |
|
| Interventions | Category: Multimodal vs. multimodal vs. control Programme deliverer: community adults (received conventional Project ALERT training), teens (school selected, 1‐day training by researchers, state cooperative extension educators, and adult program leaders) Intervention: the curriculum used 8 strategies: social inoculation; peer leaders; parent interviews; health advocacy; short‐term effects; advertising and media; public commitments; peer norms. Included peer, family and community components
Control: "usual programming, often included prevention oriented curricula such as Quest, Choices, Here's Looking at You, 2000 or locally developed curricula." |
|
| Outcomes | Annual self reported smoking status; saliva samples collected but not analysed Follow‐up: Grade 9 |
|
| Notes | Quality of intervention delivery: "extensive qualitative data indicate positive reception of the program by the participating students", and that: "implementation fidelity was not a problem " but provided no documentation. The authors also commented that the teaching techniques were not commonly used by teachers and would have needed additional resources to sustain them Statistical quality: Was a power computation performed? Power computation calculation was that 6 schools per condition were needed with average enrolment of 200 students per school to detect a 20% reduction in tobacco use; achieved needed sample size of schools. Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? Parametric ANCOVA , with school level differences in substance abuse and health risk behaviours as covariates; hierarchical linear modelling with the HLM/3L programme; hierarchical multilevel regression models; and school level models controlled for multiple levels. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The original design proposed a stratified random assignment of schools to one of the three conditions. However, in recruiting schools for the project, it became apparent that most interested schools could not accommodate the fully randomised design, largely due to scheduling constraints which dictated choice of either the Intensive or Age Appropriate versions. Possible assignment to the control condition was seldom problematic... A two‐step procedure was implemented which allowed schools to select either the Intensive or Age Appropriate condition, with the understanding that random assignment to the control condition or the selected treatment condition would occur... Schools selecting each condition were separately stratified in groups of three into high, medium and low levels of substance use (among the existing student bodies ‐ cohorts older than the HFL students). The schools were then randomly assigned from these strata..." Email from Dr Moberg 20 February 2012 ‐ "numbers out of a bowl" Clusters: schools Cluster constraint: stratified in groups of three into high, medium and low levels of substance use. Baseline comparability: the groups were equivalent at baseline. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1,981 students provided data in both 6th and 9th grade (80%), and 68% in both 6th and 10th grade (because were unable to schedule in school surveys of two Intensive and one control school). No attrition analysis |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Prokhorov 2008.
| Methods | Country: US
Site: 16 inner city schools in Houston (intervention = 8, control = 8) ‘A Smoking Prevention Interactive Experience’ (ASPIRE) Focus: Smoking initiation prevention Design: Cluster RCT (Group 1: never smoking prevention cohort) |
|
| Participants | Baseline: 1935 informed consent, 1608 baseline survey (783 Intervention, 825 Control) then 34 excluded as no baseline smoking data = 1574 (monnix 2011: never‐smokers = 1095)
Age: Average 15.7 years
Gender: 58.8% F Ethnicity: Hispanic 50.6%, African American 39.5%, Caucasian 5.9%, other 4.1% Baseline smoking data: Of 1574: 907 never (e‐mail from Dr. Prokhorov 13 Dec 2011: 484 intervention; 423 control), 667 ever (of whom 500 experimenter, 111 current, 56 former) |
|
| Interventions | Category: social influences vs. control (actually social influences vs. information control) Programme deliverer: computer Intervention: ASPIRE: students viewed CD‐Roms. 5 weekly sessions and 2 boosters (each 30 minute duration), featured eight educational ‘tracks’ over 5 hrs of videos, animations and interactive quizzes to help make decisions about smoking "The program helps students choose a tobacco‐free lifestyle... a nonsmoker entering in acquisition‐preparation can move through educational tracks tailored to prevent the acquisition of smoking and can reach stable acquisition‐pre contemplation, where the participant is rewarded for not contemplating adoption of smoking." "At the commencement of each session, students completed a series of questions designed to determine their smoking status and stage of smoking acquisition or cessation. They were then provided with a series of activities that were tailored to stage of intention and designed to promote movement through the stages toward smoking cessation (for smokers) or reduced likelihood of initiation (for nonsmokers). ASPIRE was founded on the Social Cognitive Theory (Bandura, 1977) and the Transtheoretical Model of Change (Prochaska, Redding & Ivers, 1997)." "The curriculum modules... aim to engage cognitive processes that facilitate the student's progression into the next stage of change (for preventing or stopping smoking)...". "Students who do not progress out of a stage after one session receive new messages designed for the same stage during the subsequent session; these messages continue to encourage movement toward more advanced stages of prevention or cessation." Control: Standard care (National Cancer Institute’s “Clearing the Air” self help booklet). |
|
| Outcomes | Self‐report: Non smokers ("never smoked even part of a cigarette"); former smokers ("used to smoke regularly but quit in last 12 months" or "quit more than 12 months ago"); experimenters ("only smoked part of a cigarette", "smoked only a few times"); current smokers (pack/week, 1 pack/week, > pack/week, pack/day, > pack/day). Follow‐up: 18 months |
|
| Notes | Quality of intervention delivery: no statement "ASPIRE project staff monitored the program fidelity" Statistical quality: Was a power computation performed? Yes. For α = 0.01, 125 students per school in 16 schools were required. Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Not explicitly stated, but used generalized linear mixed model regression. Were appropriate statistical methods used? Comparison of baseline variables with 2 sample t‐tests for continuous and Chi‐square for categorical variables; generalized linear mixed model regression. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "specifically targeted schools that were ethnically diverse and located in socioeconomically challenged neighbourhoods " "16 participating schools were randomly assigned to ASPIRE (eight schools) or the standard care comparison (eight schools) " E‐mail from Dr. Prokhorov 4 January 2012: "The schools were first pair‐matched on the size and ethnic background of students. Then, computer‐generated random numbers were used to assign the schools to either intervention or standard care condition." Clusters: schools Cluster constraint: air matching Baseline comparability: more Hispanics at baseline in intervention (58.9%) than control 41.6%, p < .01), no statement about smoking status at baseline (sample included 111 baseline smokers); no differences gender, academic performance, number of suspensions/detentions, depression, n close friends who smoked, n household members who smoked. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Baseline 1574, 18 months 1160 (26% attrition); no differences between groups on age, gender, ethnicity or determinants of smoking. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Rabinowitz 1974.
| Methods | Country: USA Site: 5 schools in Niagara County, N.Y. (36 classes from 1 urban and 4 rural) Focus: to increase anti‐smoking health knowledge, attitudes and behaviours, to assess the effects of an anti‐smoking programme. Design: cluster RCT (Group 3; point prevalence) | |
| Participants | Baseline: 758
Age: grades 7 ‐ 9 (age 12 ‐ 14 years)
Gender: not stated Ethnicity: no data Baseline smoking data: non‐smokers: intervention N = 303 (73%), control N = 277 (75%) |
|
| Interventions | Category: information vs. control Programme deliverer: teachers (training not stated) Intervention: teachers taught anti‐smoking health knowledge, attitudes and behaviours in a programme developed by the authors in conjunction with teachers' committees. Number of sessions not stated (N = 381). Control: No statement (N = 347). |
|
| Outcomes | Definition of smoking: (1) 'Occasional'; (2) < 3/day; (3) 3 ‐ 5/day; (4) 5 ‐ 10/day; (5) 10 ‐ 20/day; (6) > pack/day; data reported are self‐report as a 'smoker' Follow‐up: 6 m | |
| Notes | Quality of intervention delivery: Number of sessions not stated; no process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? Yes Were appropriate statistical methods used? ANOVA, "... the basic design was a 6 x 3 x 2 x 2 analysis of covariance model with an n number of observations per cell. The principal factors were Schools (N = 6), Classes (N = 3), Treatments (N = 2), and Sequence (N = 2). The Class factor was random and collapsed under Schools. Treatments, Schools, and Sequence were treated as fixed factors."; ICCs were not computed. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Pupils were members of 36 randomly selected classes in grades seven through nine, chosen from five participating urban (1) and rural (4) school districts. The classes were randomly assigned to experimental and control status ..."; no statement of the method of randomisation. Clusters: classes Cluster constraint: not stated Baseline comparability: not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 5% attrition after 6 months; no attrition analysis Baseline 758. At 1yr follow‐up 728 (96%) (however, adding the post‐test cells within Table VI totals to 748) |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Reddy 2002 (School + F).
| Methods | See Reddy 2002 (School only) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from the second intervention arm within Reddy 2002 (school only) | |
Reddy 2002 (School only).
| Methods | Country: India;
Site: New Delhi 'Health‐Related Information and Dissemination Among Youth Project' (HRIDAY) Focus: alcohol and tobacco prevention; Design: cluster RCT (Group 2: change rates) |
|
| Participants | Baseline: 5752 students, 5043 (88%) provided consent, 4776 (83%) participated in the baseline survey Age: 11.9 years Gender: 50.5% M Ethnicity: not stated Baseline smoking data: "ever tried cigarette or bidi": intervention 1 (school) mean = 0.0416 (95%CI 0.0265 ‐ 0.0637); intervention 2 (school + family) mean = 0.0340 (0.0219 ‐ 0.0525); control mean = 0.0391 (0.0251 ‐ 0.0605) |
|
| Interventions | Category: social influences vs. social influences vs. control Programme deliverer: teachers, student peers (1‐day training by researchers) Intervention:
Control: usual intervention curriculum |
|
| Outcomes | One question: "Have you ever tried a cigarette/bidi?" Follow‐up: 1 year |
|
| Notes | Quality of intervention delivery: No process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Yes Were appropriate statistical methods used? " 'Individual students' survey data could not be matched from pretest to posttest, due to problems with student code numbers. However, the populations of the schools were fairly stable during the study period, ensuring that the data collected represented students who took part in the entire study."; analysis was by mixed effects regression with the school specified as the nested effect (E‐mail from Dr. Cheryl Perry says data adjusted for clustering). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The 30 schools in the study were representative of all schools in the urban area of New Delhi and were randomly selected from a sampling frame of all New Delhi schools (Government vs Private, same sex vs. coed)." Randomization by coin toss (e‐mail from Dr. Cheryl Perry) Clusters: schools Cluster constraint: blocked on type (private, government) and gender (males only, females only, and co‐educational). Baseline comparability: groups were equivalent at baseline. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Present after 1yr: 4452 (77%) no attrition analysis; no linkage of pre‐ and post student responses. (e‐mail from Dr. Cheryl Perry states there was adjustment for clustering, but insufficient funding for process evaluation and assessment of attrition). |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Resnicow 2008 (Harm Min).
| Methods | See Resnicow 2008 (LST) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (Harm Min) within Resnicow 2008 (LST) | |
Resnicow 2008 (LST).
| Methods | Country: South Africa
Site: 36 public schools in KwaZulu‐Natal and Western cape ‘Life Skills Training’ (LST) & ‘Keep Left’ (Harm minimisation) Focus: Prevention and reduction of tobacco and drug use Design: Cluster RCT (Group 1: never smoking prevention cohort) |
|
| Participants | Baseline: 5266 completed baseline survey
Age: 14.0 cohort (dropouts 14.7)
Gender: 49.5% F cohort; dropouts 41.9% Ethnicity: Cohort: Black 59.7%, "Coloured" 26.4%, White 9.9%; dropouts: Black 48.6%, "Coloured" 39.2%, White 5.2% dropouts Baseline smoking data: 30 days cigarette use = control 18%; HM group 17%; LST group 20 % |
|
| Interventions | Category: Social influences & social competence vs. social influences vs. control Programme deliverer: Life orientation teachers, who teach the mandatory LO health education course in schools (received 3 day course for each of LST and HM courses) Intervention: (both interventions culturally adapted by focus groups)
Control: usual tobacco and substance education |
|
| Outcomes | Lifetime, past month; frequent use (> 20 days/month): re‐coded as 0 = non‐use, 1 = use Follow‐up: 18 months (post‐test at the end of grade 8 and at the end of grade 9) |
|
| Notes | Cohort members defined as those with baseline and at least one post‐test data Quality of intervention delivery: each teacher visited at least 4 times over 2 years, and implementation rated on classroom management, how well questions were answered, overall implementation of the lesson, extent to which specific lesson objectives was taught. Feedback given. 10 student workbooks collected from each teacher. "If more than half of the activities in a lesson where completed in at least five of the workbooks audited, the lesson was considered taught by that teacher that year... students receiving at last 50% of the planned 16 sessions over 2 years were classified as "high exposure"". "Overall, for LST and HM, 85% and 93%, respectively, of students received at least 75% of the planned lessons." Statistical quality: Was a power computation performed? Yes; "powered to detect a 6% to 7% difference in 30‐day smoking at posttest between either the HM or LST groups and the control group... which we did not attain." Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Yes Were appropriate statistical methods used? Mixed effects ANOVA, using PROC MIXED and SAS GLIMMIX |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Schools were then randomly selected within each ethnicity, size and SES strata."; SES status by poverty index scores. Schools with > 100 students and within 50 km of project offices included No method of randomisation Clusters: Schools Cluster constraint: Stratified by ethnicity, size and socioeconomic status Baseline comparability: No differences on demographics or substance use |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropouts = 582 (control 167; HM 227; LS 188) compared to cohort = 4684 (control 1404; HM 1751; LS 1529); "Dropouts between intervention groups do not differ for any of the variables." "Dropouts were significantly more likely to have been baseline substance users." 30 day cigarette use (%): total dropouts = 37.5% compared to cohort =15.2%; control group dropouts = 36.1% compared to cohort = 16.2%; HM dropouts = 41.2% compared to cohort = 14.2%, LST dropouts = 34.2% compared to cohort 15.3%. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Ringwalt 2009a.
| Methods | Country: US
Site: 34 schools in 21 school districts located in California, Idaho, Indiana, Kansas, New Jersey, New Mexico, North Carolina, Texas, Virginia, and Washington; (8059 schools from all US schools approached who met selection criteria; all schools in the US that did not use an evidence‐based substance use curriculum, at least 100 students per grade and committed to participation of all grade 6 students were eligible) Project ‘ALERT’ Focus: substance use prevention ‐ cigarettes, alcohol, marijuana, inhalants Design: Cluster RCT (Group 1: never smoking prevention cohort / Group 3: point prevalence) |
|
| Participants | Baseline: Cohort 1 (2004/5) 1483 randomised (of whom 343 received intervention, 378 control); cohort 2 (2005/6) 6855 randomised (of whom 2474 received intervention, 2667 control) Age: Grade 6 (age 11) Gender: 52.4% F (intervention); 52.1% F (control) Ethnicity: White 53.3%, African American 18.4%, Hispanic 24.6% (intervention); White 49.1%, African American 14.2%, Hispanic 27.8% (control) Baseline smoking data: 30 day use: 3.1% (intervention), 2.2% (control), P = 0.34; lifetime use: 13.8% (intervention), 10.7% (control), P = 0.34 |
|
| Interventions | Category: social influences vs. control Programme deliverer: teachers (received Project ALERT training programme) Intervention: Project ALERT‐ skills to resist inducement from peers to use substances, support attitudes and beliefs that mitigate substance use; 11 x 45 minute lessons in first and 3 boosters second year; guided class discussions, role playing, videos Control: no intervention All schools allowed to administer non‐evidence based substance use curricula |
|
| Outcomes | Lifetime cigarette use (no/yes); past 30 days: 0, 1‐2, 3‐5, 6‐19, 20 or more days, dichotomised to none or at least 1 day Follow‐up: 30 days after last booster session, plus a second 1 year later |
|
| Notes | Quality of intervention delivery: videos of 633/641 (98.8%) lessons, attendance logs for all lessons (which also confirmed that the 8 classes without video recordings were actually taught); "... overall 2074/2129 (97% ) lessons actually taught." Statistical quality: Was a power computation performed? Yes. 17 schools per condition required with 80% power and α = 0.05 (2 tailed) to detect 50% difference for substance outcomes, with 40% attrition. Was an intention‐to‐treat analysis performed? Yes Was a correction for clustering made? Yes Were appropriate statistical methods used? Hierarchical nonlinear model; no cohort effect so cohorts combined for analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Assignments were made of a flow basis as soon as a district’s schools entered the study. Single schools from different districts were paired and randomly assigned to a condition." 3 schools from first cohort intervention group did not include the majority of 6th graders and did not provide census, so dropped, so then used the most comparable school in control group. 2 remaining control group schools re‐enrolled in 2005/6. "Assignment was implemented through the use of computer generated random numbers". Clusters: schools from different districts paired and randomised Cluster constraint: blocked by school district, paired Baseline comparability: "At baseline, students in the intervention condition were slightly to moderately more likely to report use for each of the 8 measures examined than were students in the control condition..." (no significant differences for tobacco measures). |
| Allocation concealment (selection bias) | Unclear risk | "...each survey was identified only by a unique code number that had been previously assigned by the research team, which maintained exclusive possession of the link to their names.", (which states that allocation was not concealed, it does not state that the researchers were or were not aware of allocation at the time of intervention or data analysis). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Data collectors collected forms in each school; each student had unique code number. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "There was no evidence to suggest differential inconsistency [in responses] as a function of intervention group." Dropouts more likely to be white (P = 0.03); attrition 21% both intervention and control groups. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Rohrbach 2010a.
| Methods | Country: US
Site: 65 high schools in 14 school districts across northeast, south, central, and west of US (59 regular high schools, 6 alternative continuation high schools; 43 in two intervention arms, 21 control) ‘Project Towards No Drug Abuse’ (TND) Focus: substance use and violence related behaviour Design: cluster RCT (excluded from analysis) |
|
| Participants | Baseline: 4351 eligibles; 3751 consented; 3346 randomised and pretest survey (94.8% enrolled in regular high schools) 4 cohorts from 2004‐2007
Age: 14.8 years (mean), range 13 ‐ 18/20 (discrepancy between articles over upper age)
Gender: 53.4% F Ethnicity: White 41.1%, Hispanic 28.7%, African American 15.8%, Asian 3.3%, mixed 7.3%, other 3.8% Baseline smoking data: Last 30 days ‐ TND Implementation Support 11.9; TND Regular 16.8; Control 11.3; (P = 0.053) |
|
| Interventions | Category: Social influences & social competence vs. social influences vs control Programme deliverer: Teachers (1 days training); implementation support group (2 on site coaching sessions from trainer, and web support) Intervention:
Control: Standard 45 minute anti‐smoking curriculum, textbook with 3 pages about smoking, and brief celebration of WHO Day of No Smoking. |
|
| Outcomes | 30 day cigarettes: 0, 1‐10, 11‐30, 31‐50, 51‐70, 71‐90, 91‐100, > 100 times ("for data analysis, we created dichotomous variables where the outcome was defined as ‘true’ if a specific substance was used one or more times in the past 30 days".) Follow‐up: 1 year |
|
| Notes | Quality of intervention delivery: assessed by classroom observation. Observation was on a 7 point scale for process, quality and perceived student acceptance. "For 11 of the 54 teachers, observation was possible during only one classroom period; thus, analyses of implementation fidelity data are based on a total of 97 observations." Students rated their teacher’s delivery skills higher in TND Support (6.18/7 vs. TND Regular (5.91; P < 0l.05) and had higher programme acceptance (2.34/4 vs. 2.21/4 (P < 005) Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Yes, generalized mixed‐linear model. Were appropriate statistical methods used? generalized mixed‐linear model, two‐level random coefficients modelling. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "... schools…from school districts… recruited as convenience sample." School districts had to have at least 3 regular or alternative high schools. "Within each school district, participating schools were randomly assigned to one of three condition... Prior to assignment, schools were blocked by enrolment size, student ethnicity, and the percentage of students receiving free or reduced price lunch. Specifically, each group of three schools was aligned using a linear composite factor scores across a drug‐use inflate‐suppress continuum." No method of randomisation stated. Clusters: schools Cluster constraint: blocked into groups of three. Baseline comparability: no differences between groups for age, ethnicity, substance use past 30 days, only difference propensity for attrition score for TND Implementation = 0.81, TND Regular = 0.72, Control = 0.78 (P = 0.004). |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Retention TND Implementation support 79.4%, TND Regular 70.6%, Control 76.9%; "The analyses showed statistically significant incomparability between the lost to follow‐up and retained subjects with regard to all the variables. Retained subjects were younger, less likely to be enrolled in an alternative continuation school, more likely to be living with both parents, and had parents with a higher level of education. In addition the retained sample contained more whites, and had a lower prevalence of substance use for cigarette use, for alcohol, for marijuana use and for hard drug use... attrition did not occur differentially across experimental conditions by substance use status (in a model where condition, substance use, and the interaction term between condition and substance use were used to predict attrition status at the one‐year follow‐up, all P’s > 0.50 for the interaction terms between condition and substance use status)." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Scheier 2001.
| Methods | Country: USA Site: NE USA Focus: Alcohol, cigarettes and tobacco Design: Cluster RCT (excluded from analysis) | |
| Participants | Baseline: 3288 Age: 7th grade (12 ‐ 13 years) Gender: 48% F Ethnicity: 91% white Baseline smoking data: No data at baseline. |
|
| Interventions | Category: Social Influences and social competence vs. control Programme deliverer: teachers Intervention: 15 session Life Skills Training (LST) programme with normative education (drug‐specific cognitions, including the short‐ and long‐term consequences of substance use; knowledge about the levels of drug use among adults and adolescents; information about smokers' rights and the declining social acceptability of smoking; media pressures to smoke, drink or use drugs; techniques used by cigarette and alcoholic beverage advertisers; and techniques to resist pressure to smoke, drink or use drugs); social skills (improving interpersonal skills; effective communication; initiating social interactions; conversational skills; complimenting; skills relating to boy/girl relationships; verbal and non verbal assertiveness skills); and social and personal competence (self management; critical thinking; responsible decision‐making; coping with anxiety by cognitive and behavioural self‐control strategies) in the fall of the 7th grade + 10 booster sessions in the 8th grade + 5 booster sessions in the 9th grade.
Control: no training or prevention curriculum |
|
| Outcomes | Self reported answers to one question: 'How much do you generally smoke now?' rated from 1 (never) to 7 (> pack/day). Follow‐up: 1, 2, 3 years |
|
| Notes | Quality of intervention delivery: no process analysis. "Teachers were given primary responsibility for implementing the prevention curriculum." Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? Latent variable structural equation modelling (SEM); confirmatory factor analysis (CFA). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After blocking on pretest levels of cigarette use, schools were assigned randomly to one of three conditions..." Method of randomisation not stated Clusters: schools Cluster constraint: blocking on pretest cigarette use Baseline equivalence: not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Researchers used identification numbers lithocoded on each survey to link information across time... No teachers or school personnel were present during the testing procedure." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | After 1 year = 2,724 (8th grade) 2 years = 2,468 (9th grade) and 3 years = 2,228 (10 th grade) 32% attrition at 10th grade. More attrition for smokers (P < 0.001), users of alcohol (P < 0.001) and marijuana (P < 0.001), and males ( P < 0.001). Attrition analysis showed no differential attrition across conditions. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
Schinke 1984.
| Methods | Country: USA Site: Washington state Focus: Smoking prevention Design: Cluster RCT (excluded from analysis) | |
| Participants | Baseline: 234 Age: 6th graders (11 ‐ 12 years) Gender: No data Ethnicity: No data Baseline smoking data: No data |
|
| Interventions | Category: Social influences vs. information vs. control Programme deliverer: pairs of graduate students (received training in skills‐building and attitude modification) Intervention:
Control: No statement of whether the control group received an intervention |
|
| Outcomes | Smoking: Cigarette use, not further specified. Percentage change from pre‐test to post‐test; Saliva thiocyanate assessed. Follow‐up: 12 months |
|
| Notes | Quality of intervention delivery: No process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? No statistical analysis for tobacco outcomes was presented other than: "Biochemical data on thiocyanate levels in samples of subjects' saliva did not differ by condition at any measurement period." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were pre‐tested, then by classroom randomly divided into three conditions..." Method of randomisation not stated Clusters: Class Cluster constraint: Not stated Baseline comparability: No statement of equivalence at baseline. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No assessment of attrition. N = 234, numbers recorded with F scores are 229 or 230, implying 2% attrition. No analysis of differential attrition. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Schinke 1985a.
| Methods | Country USA Setting: 9 elementary schools, Washington State (3 to each intervention and control) Focus: Smoking prevention Design: Cluster RCT (excluded from analysis) | |
| Participants | Baseline: 689
Age: 6th grade, mean 11.76 years
Gender: 53% F Ethnicity: No data Baseline smoking data: past week smoking ‐ control 3.8%, information3.6%, skills 4%. |
|
| Interventions | Category: Social influences vs. information vs. control Programme deliverer: Graduate social workers (received 40 hrs training prior to randomisation to intervention) Intervention:
Control: measurements only |
|
| Outcomes | Primary outcome was smoking in past week. Saliva thiocyanate measured. Follow up: post‐test, 6m,12m and 24m. | |
| Notes | Quality of intervention delivery: "Observational data gathered by two research assistants showed close agreement between written protocols and delivery of both interventions. Observed rates of subject participation were similar for skills and information conditions."; no numerical data from process analysis. Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? No significance levels presented; school as unit of analysis, Scheffe contrasts on % smoking in past week at each time. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "In a nested design, three schools were randomly assigned to each of three conditions..." Method of randomisation not stated Clusters: schools Cluster constraint: not stated Baseline comparability: no differences between schools at pre‐test. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was 6% in skills, 9% in information and 8% in control group; no differential attrition. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Schinke 1985b.
| Methods | Country: USA Setting: 3 elementary schools, Washington state Focus: smoking prevention Design: cluster RCT (excluded from analysis) | |
| Participants | Baseline: 193 (97% of eligible students at pretest)
Age: 6th grade (11‐12 years)
Gender: no data Ethnicity: no data Baseline smoking data: no data |
|
| Interventions | Category: social influences vs. information vs. control Programme deliverer: graduate assistants Intervention:
Control: pre‐ and post‐tests only |
|
| Outcomes | Main outcome was weekly smoking. Saliva samples analysed for thiocyanate. Follow up: post‐test, 6m, 1yr, 2yrs | |
| Notes | Quality of intervention delivery: "Observational data from the two research assistants showed agreements between written protocols and the in vivo delivery of both interventions. Research assistants' recordings of subject participation indicated uniformly high rates and no differences between Skills and Attention‐placebo intervention conditions."; no numerical data on process analysis. Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? Yes. Comparison of baseline equivalence by one way ANOVA, and outcome measures by MANOVA. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were pre‐tested and were randomly divided by school into skills, attention‐placebo and control..." No statement of method of randomisation. Clusters: schools Cluster constraint: not applicable Baseline comparability: no differences between the groups at baseline |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition at 24m = 5.6% for the skills‐building, 7.1% for the attention‐placebo, and 7.7% for the control group; no differential attrition. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Schinke 1985c.
| Methods | Country: USA Setting: 4 elementary schools, Washington state Focus: smoking and smokeless tobacco prevention Design: cluster RCT (excluded from analysis) | |
| Participants | Baseline: 331
Age: 6th grade (11 ‐ 12 years) Gender: no data Ethnicity: no data Baseline smoking data: no data |
|
| Interventions | Category: social influences vs. information vs. control Programme deliverer: 4 pairs of graduate social workers leaders (received 40 hrs training prior to randomisation to intervention) Intervention: direct comparison of skills training and information ‐
Control:
|
|
| Outcomes | Main outcome was ever‐smoking, reported as change in % between test points. Follow up: post‐test, 6m,12m and 15m | |
| Notes | Quality of intervention delivery: no process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? X2, analysis by dependent t‐tests. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "By school, subjects were randomly divided into four groups..." Method of randomisation not stated Clusters: schools Cluster constraint: not stated Baseline comparability: groups similar at baseline in age and gender and parental smoking, but student smoking rates were not compared. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | N = 331. "Subject attrition was non significantly different by condition, across measurements."; no statement of final N at 15 months. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Schinke 1986a.
| Methods | Country: USA Setting: 12 elementary schools, Washington state Focus: smoking and smokeless tobacco prevention Design: cluster RCT (excluded from analysis) | |
| Participants | Baseline: 1281
Age: 5th and 6th graders (age 10‐12) Gender: no data Ethnicity: no data Baseline smoking data: 4% smoked |
|
| Interventions | Category: social influences vs. information vs. control Programme deliverer: film peers, guest speakers, (teachers?) Intervention:
Control: not stated if control received an intervention |
|
| Outcomes | Primary outcome was smoking or smokeless tobacco use in previous 7 days. 25% of saliva samples were tested for thiocyanate, and levels in µgrams/ml correlated 0.37 with reported tobacco use (P < 0.001). Follow up: post‐test, 6m,12m and 24m. | |
| Notes | Quality of intervention delivery: intervention groups showed "no difference among conditions for pupil attention, involvement and participation."; no numerical data presented for process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? Duncan multiple‐range comparisons |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Pupils were presented and randomly divided by school into skills, discussion and control conditions..." Method of randomisation not stated Clusters: schools Cluster constraint: not stated Baseline comparability: groups similar at baseline |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 10.8% attrition; no differential attrition among groups |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Schinke 1986b.
| Methods | Country: USA Setting: 2 elementary schools, Washington state Focus: smoking prevention Design: cluster RCT (excluded from analysis) | |
| Participants | Baseline: 65
Age: 6th grade (age 11 ‐ 12 years)
Gender: 54% F Ethnicity: no data Baseline smoking data: control and intervention both 1.5 cigarettes/week |
|
| Interventions | Category: Social influences vs. information Programme deliverer: pairs of graduate assistants Intervention: 8 x 50 min weekly sessions. Both groups observed the same films, discussions and testimonials; then tobacco refusal skills learned by problem solving, self instruction and communication skills vs. tobacco refusal skills learned by quizzes, games and debates.
Control: not stated |
|
| Outcomes | Weekly smoking. Saliva samples analysed for thiocyanate. Follow up: post‐test, 6m, 12m, 24m | |
| Notes | Quality of intervention delivery: no process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? Only 1 school per condition, very small numbers (N = 65); analysis by t tests of means. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were pre‐tested then randomly divided into health education and skills conditions." Method of randomisation not stated Clusters: school Cluster constraint: not stated Baseline comparability: not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No attrition stated No attrition analysis |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Schinke 1986c.
| Methods | Country: USA Site: 3 schools Focus: tobacco prevention Design: cluster RCT (excluded from analysis) | |
| Participants | Baseline: 214 Age: 5th and 6th graders (10 ‐ 12 years) Gender: no data Ethnicity: no data Baseline smoking data: no data |
|
| Interventions | Category: Social influences vs. information vs. control Programme deliverer: social workers Intervention: 8 x 50 min sessions. Both groups observed the same information about smoking from films and testimonials from peers. Then tobacco refusal skills learned by problem solving, self instruction and communication skills vs. tobacco refusal skills learned by quizzes, games, debates and media analyses.
Control: No intervention, pre‐ and post test only |
|
| Outcomes | Smoking behaviour. Saliva thiocyanate used for biochemical validation Follow‐up: |
|
| Notes | Quality of intervention delivery: No process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? ANOVA |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After being pre tested, the subjects were randomly divided by school into three conditions..." Method of randomisation not stated Clusters: schools Cluster constraint: not stated Baseline comparability: no differences in smoking rates at baseline among the groups |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No statement of attrition. However, N = 214, N's reported with F statistics at follow up = 196 (92%), no differential attrition |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Schinke 1988.
| Methods | Country: USA. Site: 2 Indian reservations in western Washington state Focus: prevention of smoking, alcohol and drug use; assess the effects of a 10 session prevention programme. Design: cluster RCT (excluded from analysis) | |
| Participants | Baseline: 137
Age: 11.8yrs Gender: 54% F Ethnicity: all Native Americans Baseline smoking data: no data |
|
| Interventions | Category: social influences vs. control Programme deliverer: Native American counsellors Intervention: 10 sessions; programme to learn bicultural competence skills taught by Native American counsellors. Communication, coping and discrimination skills, modelled, coached and praised turning down substance offers from peers without offence, taught self instruction and relaxation to help refuse offers of substances, rewarded refusals, anticipated temptations, predicted high‐risk situations, built networks with friends and family, homework supporting each others' refusals. Control: No programme |
|
| Outcomes | Definition of smoking: Self reported smoking in previous 14 days Follow up: 6m | |
| Notes | Quality of intervention delivery: no process analysis Statistical quality: Was a power computation performed? No (n only 137) Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? Comparisons at baseline by by ANOVA, for intervention effects over time MANOVA, "When univariate ANOVAS showed significant condition differences, posttest and follow‐up data were analysed by Tukey‐Kramer procedures for paired comparisons...". |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After pre‐testing, subjects were randomly divided by reservation site into prevention and control conditions." Method of randomisation not stated Clusters: reservations Cluster constraint: not stated Baseline comparability: experimental and control groups were similar at baseline. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition 8% at 6m with no differential attrition between groups |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Schinke 2000.
| Methods | Country: USA Setting: 27 schools from 10 reservations in N. and S Dakota, Idaho, Montana, and Oklahoma Focus: tobacco, alcohol, and marijuana Design: cluster RCT (excluded from analysis) | |
| Participants | Baseline: 1,396 Age: 3rd. to 5th. graders (8 ‐ 10 years) Gender: no data Ethnicity: all Native American Baseline smoking data: not stated |
|
| Interventions | Category: social influences vs. multi modal vs. control; [substance refusal skills (instruction, modelling and rehearsal) vs. substance refusal skills (instruction, modelling and rehearsal) + involving community in substance abuse prevention vs. no intervention control] Programme deliverer: community adults (received conventional Project ALERT training), teens (school selected, 1‐day training by researchers, state cooperative extension educators, and adult program leaders) Intervention: tobacco, alcohol, and marijuana intervention (15 sessions + 12 boosters) designed to help them resist pressures within the Native American community and the wider society to use substances. Within the context of Native American culture they learned problem‐solving, personal coping, and interpersonal communication skills for preventing substance abuse, which were explained by group leaders, then demonstrated by older peers, and practised by the students. Every session incorporated Native American values, legends and stories and holistic concepts of health, and also drew on cultural materials specific to individual communities to take account of the wide variations among Plains Indians. Community members were mobilised to support the youths' activities. Control: no intervention |
|
| Outcomes | Smoking was defined as 7 or more cigarettes or uses of snuff/chewing tobacco in the week prior to each measurement. Saliva cotinine was collected at each test, and the correlation with self reported smoking and smokeless tobacco use was r = 0.53. Follow‐up: 3.5 years |
|
| Notes | Quality of intervention delivery: no process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? One‐way ANOVA's, with individuals as the unit. Significant omnibus F‐ratios from the ANOVA's were then tested with Scheffe' post‐hoc multiple comparison tests. Covariates were not included in post‐baseline analyses. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After completing pretest measurements, 1,396 third‐ through fifth‐grade Native American students from 27 elementary schools in five states were divided randomly into two intervention and one control arms..." Method of randomisation not described Cluster: schools Cluster constraint: not stated Baseline comparability: groups equal at baseline including substance use abuse |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 14% attrition; no differential attrition |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Schofield 2003.
| Methods | Country: Australia
Site: 24 public secondary schools in the Hunter Valley Region of NSW, of which 22 participated (12 intervention and 10 control) 'Health promoting Schools programme' Focus: tobacco prevention Design: cluster RCT (Group 3; point prevalence) |
|
| Participants | Baseline: 4841 (intervention 2573; control 2268)
Age: Yr 7 ‐ 8 students (12 ‐ 14 years)
Gender: 55% F Ethnicity: both parents Australian 1361, one Australian 204, other 287 Baseline smoking data: non‐smoker 1678, smoked last month 148, smoked last week: intervention 3.9%, control 4.1% |
|
| Interventions | Category: multimodal vs. control Programme deliverer: schools liaison officer Intervention: tobacco information, health promotion, encouragement of peers, parents and teacher as non‐smoking role models, drama, posters vs. offer of help to other schools to develop health promotion projects Intervention: Health Promoting Schools intervention, with schools encouraged to adopt health promoting strategies to address health risk behaviours; information leaflets; school newsletters for parents; letters to tobacco retailers; development of policies for smoke‐free schools; encouragement of non‐smoking parents, peers, and teachers as role models; peer influence programmes; and incentive programmes Control: on request schools were offered help for other health promotion projects; and smoking‐specific support at the completion of the research project; not stated if received other interventions |
|
| Outcomes | Self‐reported smoking: never; just a few puffs; < 10 cigarettes in life; >10 cigarettes in life; number of cigarettes in past 7 days Follow‐up: Year 9 ‐ 10 (age 14 ‐ 16 years) |
|
| Notes | Quality of intervention delivery: 100% of schools ensured curriculum covered effects of smoking; 100% distributed the smoking pamphlet to parents; 83% implemented a school no‐smoking policy; 83% distributed letters to tobacco retailers; 83% had discussion groups or conducted surveys with parents; 58% followed up with action after the discussion groups or survey; and 33% trained leaders to deal with smoking issues. Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? Yes Were appropriate statistical methods used? "For the test of intervention effect, we had planned to use a cluster‐based multilevel analytic method. However, preliminary analysis of variability between and across schools revealed that the cluster effect of schools was relatively small, and the effect of schools in predicting smoking rates was not statistically significant... Logistic regression was used to estimate the independent effects of explanatory variables after adjustment for all other factors..." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The design was a randomised controlled trial with 24 secondary schools randomly selected from a population of 31 schools in the Hunter and Taree school districts of NSW, and then randomly allocated to control and intervention groups prior to recruitment." Method of randomisation not stated Clusters: schools Cluster constraint: not stated Baseline comparability: no statement |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition after 2yrs: 1852 (38%) 48% of drop‐outs were from the intervention and 52% from control group (P < 0.05); 18% of those lost to follow‐up had smoked in the last week compared to 8% of those remaining in the study); no analysis of differential attrition of smokers from intervention and control groups; |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Scholz 2000 (G, female).
| Methods | See Scholz 2000 (G, male) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from the female participants in the Gymnasien within Scholz 2000 (G, male) | |
Scholz 2000 (G, male).
| Methods | Country: Germany
Site: 15 Gymnasien (59 classes) and 13 Realschulen (25 classes) in 3 towns (Hanau, Darmstadt, Offenbach) in Hesse.
Focus: on tobacco, but the screening questionnaire also asked about alcohol and drug consumption Design: cluster RCT (Group 3: point prevalence) |
|
| Participants | Baseline: 1956 (98.3% of possible); 1080 experimental, 876 control Age: 13 yr olds Gender: 757 M, 841 F (at follow‐up) Ethnicity: not stated Baseline smoking data: never‐smokers ‐ intervention Gymnasien male = 95.60%, female = 94.90%; intervention Realschulen male = 91.50%, female = 89.70%; control Gymnasien male = 93.80%, female = 93.20%; control Realschulen male = 85.70%, female = 90.60% |
|
| Interventions | Category: social influences vs. control Programme deliverer: physicians Intervention: 8 x 60 min lessons delivered by non‐smoking physicians ‐ (1,2) function of the heart, circulation and lungs; (3) action of the pulse and blood pressure; (4) motivations for smoking and non‐smoking, prevalence rates, consequences; (5,6) role plays about conflicts between smokers and nonsmokers, developed by participants; (7) cigarette advertising; (8) quiz with small prizes Control: received "no particular instruction" |
|
| Outcomes | Smoking defined as at least 1/week; at least 1 in the last 24 hrs Follow‐up: 2 years |
|
| Notes | Quality of intervention delivery: no process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? Analysis by chi‐square |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Nach der Befragung wurde die Hälfte der Klassen jeder Schule randomisiert der Interventionsgruppe bzw. der Kontrollgruppe zugeordnet. Bei ungerader Klassenzahl einer Schule wurden mehr Klassen in die Interventionsgruppe als in der Kontrollgruppe randomisiert." Half of the classes in each school were randomised to experimental and control groups, with more allocated to the experimental group due to inexact enumeration of classes. Method of randomisation not stated Clusters: half classes Cluster constraint: not stated Baseline comparability: not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The students for whom code numbers were lost by the schools could not be tested, and the analysis is limited to the 1598 for whom there were code numbers both at pretest and 2 yrs later (81.7%). |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Scholz 2000 (R, female).
| Methods | See Scholz 2000 (G, male) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from the female participants in the Realschulen within Scholz 2000 (G, male) | |
Scholz 2000 (R, male).
| Methods | See Scholz 2000 (G, male) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from the male participants in the Realschulen within Scholz 2000 (G, male) | |
Schulze 2006.
| Methods | Country: Germany
Site: 172 classes in 68 schools; Heidelberg Children’s Panel Study (1998 and 2000), all 7th grades in Heidelberg, and random sample of schools from Mannheim and Rheine‐Neckar county, (89 intervention classes, 83 control classes) ‘Smoke‐Free Class competition’, known as ‘Be smart – don't start’ in Germany Focus: prevention of starting smoking Design: cluster RCT (Group 1: never smoking prevention cohort) |
|
| Participants | Baseline: baseline information on 4043, (N = 1704; 948 intervention, 756 control)
Age: 7th grade
Gender: Intervention: 470 M, 510 F; control: 386 M, 486 F Ethnicity: not stated Baseline smoking data: not stated |
|
| Interventions | Category: social influences vs. control (social influences + competition vs. control) Programme deliverer: regular teachers (invited to information session and sent brochures) Intervention: 'Smoke‐Free Class Competition' ('Be smart – don't start'). 1. Classes decided to be non‐smoking for 6 months, monitor smoking, and if 90% remain non‐smokers can participate in competition for attractive prizes 2. Weekly curricula integrated into existing classes (duration not stated), about health effects of smoking, how to quit, how to deal with peer pressure, tobacco industry strategies Control: no intervention |
|
| Outcomes | Self reported. Never, ex‐smoker, current. "For the sake of consistency, ex‐smokers at baseline who declared themselves to be never‐smokers at follow up (control N = 16, ; intervention N = 40) were assessed as ex‐smokers…" Follow‐up: 18 months |
|
| Notes | Quality of intervention delivery: no statement Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? No Were appropriate statistical methods used? Yes; logistic regression, mobility tables |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "... all classes of the 7th grade in Heidelberg, as well as a random sample of schools of Mannheim and the Rhine‐Neckar County, which were stratified by school type and number of classes… sample of 172 classes of the 7th grade from 68 schools."; "After the first measurement, the 172 classes were stratified by school type and regional similarities (size of the school and rural or urban region). Matched pairs of schools were formed and randomly assigned collectively to one of two groups in order to prevent interaction effects. No school had classes in intervention and control group at the same time... However, 3 classes of one school assigned to the control group were unwilling to forego the intervention: thus in 89 classes (with 2163 pupils), the above‐specified intervention was performed…" No method of randomisation stated Clusters: classes, schools Cluster constraint: stratification and pair matching; matched on school size and urban/rural Baseline comparability: intervention never‐smoker 62.1%, control 52.1%, P < 0.05 |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "So after the follow‐up questioning of 3924 pupils in October 2000, about 46% of the 4043 pupils of the baseline sample from October 1998 could be identified by in both measurements... [pupils were identified by a 6 digit code]... 948 pupils of the intervention and 756 pupils of the control were examined... There are no substantial changes in the gender, age and smoking distributions due to the attrition in intervention and control group… As a result of the lower average age of the intervention group, 4.5% fewer pupils of the intervention group had already started smoking at the time of the baseline measurement."; "From baseline to the follow‐up measurement, we have an overall attrition rate of 54%... but there are no systematic differences between the intervention and the control groups concerning losses at follow‐up, nor regarding the rate of attrition." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Seal 2006.
| Methods | Country: Thailand
Site: 2 high schools in Bangkok Focus: tobacco and drug prevention Design: cluster RCT (Group 1: never smoking prevention cohort) |
|
| Participants | Baseline: 170 (85 control, 85 intervention)
Age: 15.5 years (mean)
Gender: 11% F Ethnicity: Thai Baseline smoking data: never‐smokers ‐ intervention 63%, control 71% |
|
| Interventions | Category: social influences & social competence vs. control Programme deliverer: not stated Intervention: Life Skills Training ‐ effects of drugs and tobacco, self‐awareness skills, decision making and problem‐solving skills, stress and coping skills (10 classes, 60 minutes each), using instruction, demonstration, feedback, role‐playing, presentations, games, videotapes, life skills booklet Control: tobacco and drug curriculum normally provided |
|
| Outcomes | Smoking: never, once per week, more than once per week Follow‐up: 6 months after intervention |
|
| Notes | Quality of intervention delivery: not stated Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? No Were appropriate statistical methods used? ANOVA, Chi‐square |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The program was implemented in two randomly selected high schools in Bangkok." "...assigned randomly to either control or intervention." Email from author: "I randomly selected the schools to intervention and control by asking my research assistant to blindly pick up a ball with a name of a school out. First pick was a school to receive intervention." Clusters: 2 high schools Cluster constraint: none stated Baseline comparability: "... the results revealed no significant differences between the control and the intervention groups at pretest." |
| Allocation concealment (selection bias) | Low risk | Email from author: "I randomly selected the schools to intervention and control by asking my research assistant to blindly pick up a ball with a name of a school out. First pick was a school to receive intervention." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No statement |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Severson 1991 (High, F).
| Methods | See Severson 1991 (High, M) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from female participants in the high schools within Severson 1991 (High, M) | |
Severson 1991 (Middle, F).
| Methods | See Severson 1991 (High, M) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from female participants in the middle schools within Severson 1991 (High, M) | |
Severson 1991 (Middle, M).
| Methods | See Severson 1991 (High, M) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from male participants in the middle schools within Severson 1991 (High, M) | |
Severson 1991(high, M).
| Methods | Country: USA
Site: 22 schools (13 middle, 9 high) in Lane County, Oregon Project 'PATH' (Programs to Achieve Teen health) Focus: smokeless tobacco (ST) and cigarette prevention/cessation Design: cluster RCT (Group 2: change rates) |
|
| Participants | Baseline: 2552 (1434 middle school, 1118 high school), 4.7% parental refusal, 2% of students chose not to complete questionnaire
Age: not stated
Gender: approximately 50/50
Ethnicity: not reported Baseline smoking data: ≥ 1 cigarette past month: middle school (males 10.5%, females 13.5%), high school (males 14.8%, females 20.3%) |
|
| Interventions | Category: social influences vs. control Programme deliverer: regular science or health teachers; 5/7 sessions included activities led by peer leaders (teachers received 2 ‐ 3 hrs training; peer leaders received 2 half‐days of training) Intervention: 7 sessions over 2 ‐ 3weeks; social‐influences model; overt and covert pressures to use tobacco; refusal skills training; public commitment not to smoke; 7 videos standardized instruction and maintained students' interest. Parents were sent 3 brochure messages. See Biglan studies for similar programme. Control: no intervention ‐ usual curricula |
|
| Outcomes | Expired air and saliva samples; smoker defined as a student with an expired air CO > 10 ppm; self report of no smoking but expired air CO > 20 ppm reclassified as a smoker. Due to cost, saliva samples were not analysed. Self report of daily, weekly, monthly and 6‐monthly smoking. Index based on weighted average of use in last day, week and month computed. Follow‐up: 12 m | |
| Notes | Quality of intervention delivery: no process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? X2 ANOVA, ANCOVA, LR, with students as unit of analysis. "Treatment outcome was assessed using individual subjects as the unit of analysis. We attempted to tabulate and analyse classroom means, but due to the small number of classrooms and students within a classroom, as well as the impact of attrition, the resulting means were very unstable... The intra‐class correlation for ST use was r = 0.028 and for 0.03 for cigarette smoking.", (although ICCs were computed, they were not used to correct for the effects of clustering). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A drug‐use composite was formed which combined the Z‐scores for the four substances with double weighting for the tobacco use items. The seven rural school districts were then blocked into three high drug use school districts and three low drug use school districts based on this composite measure, and randomly assigned to treatment condition within blocks. There were only two urban school districts. In one district, the high school was assigned to the treatment condition. The two high schools in the other district were randomly assigned to treatment and control conditions. The two middle schools which fed into each urban high school were randomly assigned to treatment and control conditions." Method of randomisation not stated Cluster: schools Cluster constraint: rural schools placed in 2 blocks according to drug use composite Baseline comparability: not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 31% attrition; attrition analyses revealed no significant differences between groups, but fewer high school than middle school students were available at follow up. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Shope 1996.
| Methods | Country: USA
Site: 179 classes in 6 school districts in Michigan Focus: alcohol, tobacco, marijuana, cocaine Design: cluster RCT (Group 2: change rates) |
|
| Participants | Baseline: 4730, of whom 1,911 participated in the intervention or control for 2 years, and Shope 1996 reported on 442 (308 intervention, 134 control) Age: 6th and 7th grade students Gender: equal distribution in experimental and control groups at baseline Ethnicity: not assessed at the request of school boards; rural boards were predominantly White, and urban boards predominantly Black Baseline smoking data cigarettes (N = 257) Grade 6 (mean = 0.09; SD = 0.50; prevalence 5.7%); Grade 12 (N = 257), (mean = 1.16; SD = 1.88; prevalence 35%) Smokeless tobacco: Grade 6 (mean = 0.02; SD = 0.14; prevalence 2.4%); Grade 12 (mean = 0.34; SD = 1.10; prevalence 11.6%); |
|
| Interventions | Category: Social influences vs. control Programme deliverer: teachers Intervention: 30 lesson cigarettes, smokeless tobacco, alcohol, marijuana, and cocaine intervention, with a focus on tobacco in the 5th grade, alcohol in the 6th grade, and on tobacco, alcohol, marijuana and cocaine in the 8th Control: no programme |
|
| Outcomes | Smoking and smokeless tobacco use measured "... by a single item on current frequency of use..." Follow‐up: Baseline 6th grade, follow‐up 12th grade, based on 262 students who completed all four questionnaires (reported in Shope, 1998) |
|
| Notes | Quality of intervention delivery: teachers received 1 day of instruction, and copies of the curricula; process analysis showed that 84% of teachers documented their teaching, and they reported having taught 92% of the 5th grade and 100% of the other grades' curricula. However, (i) some teachers delivered less than 50% of the programme; (ii) classes that received less than 50% of the intervention programme were included in the control group; (iii) the oldest cohort (which received only the 8th grade programme, and for which no programme was available in the 9th grade) were classified as programme students); (iv) whereas "the three younger cohorts who, by virtue of their assignment to classroom teachers received only one year of curriculum were omitted from analyses." Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? Analysis by repeated measures ANOVA |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Random assignment to equal‐size experimental and control groups was sought but not achieved in every district, therefore control students will be referred to as comparison students." Method of randomisation not stated Clusters: classes Cluster constraint: not stated Baseline comparability: not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 4370 pre‐tested, 4222 at 2 month posttest, 4116 at one year posttest, 3112 (71%) tested on all three occasions; 262 who completed the full 2 year intervention, 257 analysed who completed all 4 questionnaires including 12th grade. Attrition analyses were conducted only for the 6 ‐ 7th grade cohort, and excluded 703 students who received only 1yr of the programme: these analyses found no differences at pretest between the longitudinal and attrition students on use of cigarettes, but attrition students reported higher smokeless tobacco use. "Students in the three younger cohorts who, by virtue of their assignments to classroom teachers, received only one year of curriculum were omitted from analyses." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Simons‐Morton 2005.
| Methods | Country: US
Site: 7 middle schools in 1 Maryland school district (3 treatment, 4 comparison) 'Going Places' Program Focus: increase social skills, prevent smoking, drinking and antisocial behaviours Design: cluster RCT (Group 1: never smoking prevention cohort) |
|
| Participants | Baseline: two 6th grade cohorts: 2969 eligibles, 2651 (87.8% provided consent) students in special education excluded; final analysable sample: 1320
Age: Grade 6 (age 11)
Gender: 750 F, 570 M (analysable sample) Ethnicity: 72% (939) White, 18% (273) Black, 10% (108) other eligible at T1 assessment Baseline smoking data: treatment 0.15; control 0.23 (for analysable sample) |
|
| Interventions | Category: multimodal vs. control Programme deliverer: teachers (received "substantial training and support from a master teacher...") Intervention: foci are to increase academic engagement, commitment to school, alter perceptions, attitudes and expectations about substance use and reduce antisocial behaviours. Three components:
Control: No stated intervention |
|
| Outcomes | Never; 12 month user; recent user (past 30 days); frequent user (≥ 3 times in past 30 days); smoking stage with range 0 to 4 is used in outcomes Table 1 Follow‐up: final 40 month survey beginning of 9th grade at T5 (40 months after baseline T1 assessment) |
|
| Notes | Quality of intervention delivery: "Teachers reported completing 95% of the lessons [sic] sixth grade and 84% in the seventh grade. During scheduled observations, teachers completed all core lessons. Teacher ratings of the percentage of students fully participating in the lessons, including staying on task, were 90% in the sixth grade and 88% in the seventh grade. On average 77% of sixth grade students and 65% of seventh grade students indicated usually or always paying attention to the Going Places classes… with 54% reporting they used the skills from the program at school and 41% indicating they used program skills outside school' 'Of 45 parents interviewed, 40 indicated they or their spouse viewed the whole video and parenting booklet, of which 80% reported liking these manuals." Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? No. "Using one‐Way ANOVA we found that mean smoking stage was not significantly different among schools. Therefore, school was not included in the final analyses." Were appropriate statistical methods used? Latent growth curve analysis; ANCOVA to compare baseline and follow up outcomes; growth mixture modelling to evaluate treatment effects for each latent class within treatment groups. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "7 middle schools in 1 Maryland school district were …randomised..." E‐mail from Dr. Denise Haynie 16 December 2011: "The study employs a randomised, quasi‐experimental design in which the seven Charles County, MD middle schools were match on size and students' racial composition and randomised, three to the special intervention condition and four to the minimal‐intervention condition. Notably, it is a small number on which to randomise. We did the intervention as part of the core curriculum, in language arts classes and it was unlikely to be feasible to randomise within the schools. Given it was an efficacy study, we decided to take advantage of being in those classes with good attendance to which every child was enrolled over other strategies that may have enhanced the effectiveness of the randomisation." Emai from Dr Haynie 1 February 2012: "...the assignments were computer generated." Clusters: schools Cluster constraint: not stated Baseline comparability: e‐mail from Dr. Denise Haynie 16 December 2011: "...two groups were not equivalent, in that the control group more likely to smoke and the treatment group more likely to be non‐white." |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "When consent was again obtained upon entry into high school in the ninth grade, 59 parents refused consent and 242 students failed to return completed forms, leaving a sample of 2350… Of these, 119 became ineligible during the study by failing a grade or being newly classified as special education, leaving as a sample of 2231, of whom 32 moved out of the school district and 715 were absent and missed an assessment, leaving a final sample of 1484. An additional 164 study participants were not included in the final analyses because they did not provide data on smoking on all five surveys... Compared with the final sample, study participants lost to follow up were significantly more likely to be black, live in a single parent family, and to have reported smoking, drinking, and antisocial behaviour. Attrition by treatment group did not vary by sex, one or two parent family, drinking or antisocial behaviour, but was greater among Blacks in the intervention than the comparison group."; (there is no statement regarding differential attrition between groups according to smoking status). "... loss to follow up of high‐risk youth was not different between treatment conditions, avoiding the most serious threat to validity posed by these losses." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Sloboda 2009.
| Methods | Country: US
Site: 83 school clusters from 6 metropolitan areas including Detroit, Houston, Los Angeles, Newark, New Orleans and St Louis ( 41 intervention, 42 control) ‘Adolescent Substance Abuse Prevention Study’ (ASAPS) implementing ‘Take Charge of Your Life’ program (TCYL) Focus: prevention and reduction of tobacco, alcohol, marijuana / substance use at grade 11 Design: cluster RCT collecting longitudinal data over 5 years (Group 3: point prevalence) |
|
| Participants | Baseline: 19529 consented, 17320 (10028 treatment, 7292 control) completed baseline survey
Age: intervention: 12.4 years (mean); control: 12.5 (mean) Gender: intervention: 44.5% M; control: 43.7% M Ethnicity: intervention: White 32.8%, Black 12.6%, Latino/Hispanic 27.8%, Asian 4.2%, American Indian 8.3%, Other 11.8%; Control: White 39.4%, Black 15.4%, Latino/Hispanic 17.9%, Asian 4.7%, American Indian 8.3%, Other 12.9% Baseline smoking data: 30 day: 672/10,028 (6.7%) |
|
| Interventions | Category: social influences & social competence vs. control Programme deliverer: trained D.A.R.E. police officers (six 3 days training for each of 7th and three 3‐day for the 9th grade lessons, role plays) Intervention: Take Charge of Your Life (TCYL) ‐ personal, social, legal risks and consequences of tobacco, alcohol, illicit drugs, normative beliefs, communication, decision‐making, assertiveness, refusal skills, interactive tasks for students to "make sense of their experiences...", role playing; 10 lessons in 7th grade (9 on tobacco), 7 in 9th grade (3 on tobacco). Control: no statement |
|
| Outcomes | Past 30 days, past 12 months: scored 0 to 6 (2 packs/day), "As students' responses across surveys were heavily skewed, with most subjects reporting no use, substance use variables were converted into dichotomous variables coded 0 for no use and 1 for any use." Follow‐up: tests at baseline, annually until the 11th grade and 2 years post intervention; total 5 years from baseline. |
|
| Notes | Quality of intervention delivery: "Fidelity of implementation of TCYL was examined using independent observations, student assessments, and officer‐instructor assessments... the officers taught every lesson and implemented the curricula as designed with an average content coverage (i.e. activities within each lesson) score of 74% and used the appropriate instructional strategy on average, 55.5% of the time." Statistical quality: Was a power computation performed? Yes. To detect 8% difference in marijuana use in 11th grade, with 300 students/cluster/3 loss to follow up, ICC 0.05, required 40 school clusters for power = 0.80 and P = 0.05. "Although the actual loss to follow‐up through 11th grade was higher than the initial power calculations (45.7% compared to 33 1/3%), intra‐cluster correlations were much lower than expected,… this study is adequately powered." Was an intention‐to‐treat analysis performed? No, not explicitly stated, note that analysis has been done on imputed data. Both original and imputed data shown and the result for 30 day smoking is significant in both. Was a correction for clustering made? Yes Were appropriate statistical methods used? Yes. Multilevel logistic model. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "School clusters... were randomly assigned to either the treatment or control conditions." "To achieve diversity of study participants, the study consisted of school clusters within school districts in and around Detroit, Houston, Los Angeles, Newark (NJ), New Orleans, and St. Louis. A stress index representing poverty based on the percentage of students eligible for free lunch programs and the percentage of minority students attending schools within the districts was calculated... Two strata of high and low stress districts were created… Cities were randomly assigned to represent either low or high stress and then one inner city school district in the appropriate stress condition was randomly selected… school clusters within a 50‐mile radius of the inner city school cluster were randomly selected and recruited." Email from author 12 Jan, 2012 confirmed randomisation by computer generated selection. Clusters: "School clusters consisting of a high school and its feeder middle schools..." Cluster constraint: stratification Baseline comparability: equivalent on demographics and substance use "... the only significant difference noted was for region, with Detroit having a greater number of control students." |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 10434 completed 11th grade survey (of baseline 17320) Intervention: 5756/10028 (57%) Control: 4678/7292 (64%) 80/83 school districts retained in 11th grade (2 schools destroyed in Hurricane Katrina); "... because of the No Child Left behind Act of 2001, many inner city students transferred from the study high school to schools outside the study." "The treatment and control samples at the 11th grade were more likely to be white with a loss of Blacks and Latinos. Also there were fewer alcohol users in the control group by the 11th grade and fewer treatment students in Los Angeles and New Orleans. Because of the nested nature of our data, in order to describe attrition at the time of the 11th grade survey, we utilized a design adjusted logistic regression… attritors were more likely to be older at baseline, female, non‐white, users of alcohol, marijuana and tobacco, and from Los Angeles and Detroit."; (no significance levels stated). "To address the problem of missing data, we used a multiple imputation approach under a model that assumes values are missing at random... Multiple imputations were carried out using the NORM program with separate imputations for the treatment and control conditions…" "We employed multiple imputation techniques to estimate missing data… readers should interpret the results presented in this paper with some caution." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Smith 2004.
| Methods | Country: US
Site: 9 rural schools, central Pennsylvania ‘ADAPT’ (Adoption of Drug Abuse Prevention Training) Focus: Smoking (cigarettes and smokeless tobacco), drinking, binge drinking, inhalant use Design: cluster RCT (excluded from analysis) |
|
| Participants | Baseline: 732 with active parent and student consent (LST 234, I‐LST 297, control 201)
Age: 7th grade (age 12)
Gender: 45.6% F Ethnicity: White 96.6% Baseline smoking data: not available |
|
| Interventions | Category: social influences & social competence vs. control ( (1)social influences & social competence vs. (2) social influences & social competence integrated into regular lessons vs. (3) control) Programme deliverer: Teachers (LST trained by LST trainers, I‐LST by ADAPT LST trainers) Intervention:
Control: "...no special preventive programs being offered in these schools..." |
|
| Outcomes | Self‐report; 1 (never), 2 (a few times, but not in past year, 3 (a few times/year), 4 (once/month), 5 (a few time/month), 6 (once/wk), 7 (few times/week), 8 (once/day), 9 ( > once/day); "categories 1 and 2 were combined due to the inconsistent responses." Follow‐up: Year‐end post‐tests for 3 years |
|
| Notes | Quality of intervention delivery: teacher self rating forms; and at least one lesson videotaped or observed; Smith 2004 says: 81% of topics covered in LST, 84% in I‐LST; in all schools 93% average attendance; Vicary 2006 says: "LST average 90% of lessons delivered; I‐LST 48 lessons delivered/school, covering 95% of LST topics..." (Vicary covers off this difference in that % quoted by Smith are student participation, the % by Vicary quoted here are lesson delivery). Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? No, because ICCs 'negligible' Were appropriate statistical methods used? For 9 schools, multilevel analysis not appropriate (requires ≥ 10 groups). As ICCs "negligible", used fixed effects covariance regression model. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "... school district selection criteria for the study focused on two main characteristics: low socioeconomic status... relatively small size, as indicated by a school district enrolment of less than 1000, and only one middle school per district. After selecting very similar districts based on these characteristics, these schools were then randomly assigned to one of three conditions." No method of randomisation stated. Clusters: schools Cluster constraint: matched at school district level Baseline comparability: "some pre‐test differences across the three groups in free lunch eligibility, substance use, and the incidence of problem behaviours; as a result, these variables were controlled in the analyses.", (no statistical significances stated). |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 578 (78.9%) of students completed all four tests. "No differential attrition across conditions.", missing variables replaced at random using NORM programme; 17 students gave inconsistent replies; no change in results if these students excluded. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Spoth 2001 (ISFP).
| Methods | Country: USA
Site: 33 rural schools in 19 contiguous counties in a Midwestern US state [Iowa] 'Iowa Strengthening Families Program' (ISFP) and 'Preparing for the Drug Free Years Program' (PDFY) Focus: tobacco, alcohol, marijuana prevention Design: cluster RCT (Group 1: never smoking prevention cohort / Group 2: change rates) |
|
| Participants | Baseline: 1309 eligible families, of whom 667 (51%) completed the pretest;
Age: 6th graders, age 11
Gender: 55% F Ethnicity: no data Baseline smoking data (Wave 1): log‐transformed index of tobacco use: control (n = 129) 0.05 (SD 0.21), PDFY (n = 122) 0.13 (SD 0.34), ISFP (n = 122) 0.08 (SD 0.28) |
|
| Interventions | Category: social competence vs. social competence vs. control Programme deliverer: project staff Intervention:
Control: 4 mailed booklets (physical and emotional changes in adolescence; and parent‐child relationships). |
|
| Outcomes | (1) Ever smoked, (2) ever used chewing tobacco, (3) cigarettes per day, (4) no. of times chewed tobacco in the past month. All 4 measures dichotomised Yes = 1/No = 0, then summed from 0 to 4, then log transformed. Follow‐up: age 18 |
|
| Notes | Quality of intervention delivery: (a) for the PDFY programme a process analysis showed that all teams covered all key concepts, and 69% of the detailed tasks in the group leaders' manual were completed. Of the attending families, 93% attended at least 4/5 sessions. The leaders covered all of the key concepts, and of the activities in the group leader's manual, 87% were covered in the family sessions, 83% in the parent sessions, and 89% in the youth sessions; (b) for the ISFP intervention, 94% of attending families were represented by 1 family member in 5 or more sessions, and observation of ISFP teams showed that all key programme concepts were covered; 373 families (56%) completed all 5 data assessments across 4yrs Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? Yes Were appropriate statistical methods used? The groups were equivalent at baseline and multilevel analyses with logistic growth curve techniques controlled for the effects of clustering; multilevel mixed model ANCOVA; dichotomous outcomes by z tests |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Schools were blocked on the proportion of students who resided in lower income households and on school size. Within blocks, each school was randomly assigned to one of the three experimental conditions... Random assignment was computer‐generated by a data‐analyst..." Clusters: schools Cluster constraint: blocked on the proportion of students who resided in lower income households and on school size Baseline comparability: no differences (Spoth 2001, Guyll 2004) |
| Allocation concealment (selection bias) | Low risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1,309 eligible families recruited, and 667 (51%) completed pretest. Although only 447 (67%) remained at 4 years, there was no differential attrition across groups; a multiple imputation Monte Carlo software programme (NORM) showed that attrition did not affect the findings; there was also no differential attrition after 6 years (Spoth 2004) |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Spoth 2001 (PDFY).
| Methods | See Spoth 2001 (ISFP) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (PDFY) within Spoth 2001 (ISFP) | |
Spoth 2002 (LST + SFP).
| Methods | Country: USA
Site: 36 randomly selected schools in 22 contiguous counties with the same selection criteria as Spoth 2001 'SFP 10' Programme Focus: tobacco, alcohol and marijuana prevention Design: cluster RCT (Group 1: never smoking prevention cohort / Group 3: point prevalence) |
|
| Participants | Baseline: 1677 (LST 622; LST + SFP 543; control 489) Age: 7th graders Gender: LST 45.3% F; LST + SPP 46.5% F; control 48.3% F Ethnicity: Caucasian ‐ LST Group 95.3%, LST + SFP 10‐14 group 96.5%, control 96.8% Baseline smoking data: Ever smoked ‐ LST Group 25.2%, LST + SFP 10‐14 group 26.9%, control 17.0% |
|
| Interventions | Category: social competence vs. combined social influences, and social competence vs. control Programme deliverer: teachers, project staff Intervention: one intervention group received LST, another both LST + SFP
Control: no statement |
|
| Outcomes | Self reported: never smoking, lifetime use Follow‐up: 5.5 years |
|
| Notes | Quality of intervention delivery: adherence to the SFP programme was 92%, and to the LST programme 85%. Of the students who participated, the % attending 50% or more of the lessons were 100% for the LST programme; 100% for the LST booster; 90% for the SFP programme; and 89% for the SFP booster Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Yes Was a correction for clustering made? Yes Were appropriate statistical methods used? Allocation was at the school level and multilevel analysis controlled for the effects of clustering; multilevel ANCOVA analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A randomised block design guided the assignment of the 36 schools to the three experimental conditions." Method of randomisation not stated. Cluster: schools Cluster constraint: "Criteria for selection of the initial pool of schools were: 20% or more of households in the school district within 185% of the federal poverty level; community size (school district enrolment under 1,200, and all middle school grades (6‐8) taught at one location... After we matched the schools and randomly assigned them to conditions..." (Spoth 2002); "... experimental assignment, which was guided by a randomised block design. Based on school‐level risk measures calculated from data collected through a prospective telephone survey of randomly selected parents of eligible children, the schools were split into 12 matched sets of three." (Spoth 2008). Baseline comparability: groups equivalent at baseline on smoking |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Spoth 2002 (used "listwide deletion of missing data"): totals: baseline 1664, postest 1563, 1 yr follow‐up in 8th grade 1372 (LST pretest 621, postest 583, 1 yr follow‐up up 503) (LST+SFP: pretest 549, posttest 517, 1 yr follow‐up 453) (Control: pretest 494, postest 463, 1 yr follow‐up 416); Trudeau 2003 ‐ same data. Spoth 2008: (used multiple imputation for missing data, so N's larger than for Spoth 2002): totals: baseline 1677, postest 1690, 1 yr follow‐up 1633; 12 th grade follow‐up 1237) (LST pretest 622, postest 618, 1 yr follow‐up up 583, 12th grade 428)(LST+SFP: pretest 543, posttest 554, 1 yr follow‐up 539, 12 th grade follow‐up 450), (control: pretest 489, postest 496, 1 yr follow‐up 488, 2th grade follow‐up 347), ("undetermined" pretest 23, 8th grade 23, 12th grade 12). No differential drop out between groups Expired air samples were collected but not analysed |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Spoth 2002 (LST).
| Methods | See Spoth 2002 (LST + SFP) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (LST) within Spoth 2002 (LST + SFP) | |
Spoth 2007.
| Methods | Country: US
Site: 28 school districts in Iowa and Pennsylvania rural towns and small cities PROSPER Project (PROmoting School‐community‐university Partnerships to Enhance Resilience) Focus: prevention of alcohol, cigarettes, marijuana, amphetamines, ecstasy, inhalant use Design: cluster RCT (Group 2: change rates, not included in the analysis) |
|
| Participants | Baseline: 2 cohorts; Pretest: intervention 14 schools districts (6091 students); Control: 14 schools districts (5931 students)
Age: 6th graders and families (age 11)
Gender: 51% F Ethnicity: White 85%, Hispanic/Latino 5%; African Americans 3% Baseline smoking data: Cohort I Intervention group: ever smoked N = 66, regular smoking N = 14; cohort I control group: ever smoked N = 43, regular smoked N = 8; cohort II intervention group: ever smoked N = 88, regular smoking N = 14; cohort II control group: ever smoked N = 67, regular smoking N = 20 |
|
| Interventions | Category: Social influences & social competence vs. control Programme deliverer: Facilitators (received 2 day training) Intervention: two components ‐
Control: usual programming provided by school districts |
|
| Outcomes | Never, new user, past month, past year and lifetime cigarettes Follow‐up: 18 months |
|
| Notes | Quality of intervention delivery: Year 1 ‐ Each team of facilitators observed 2‐3 times; coverage of activities in manual: average 92% in family sessions, 88% in parent sessions, 91% in youth sessions; Year 2 ‐ Implementation adherence rates: Life Skills Training 89%; Project Alert 89%, All Stars 91% Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Yes Was a correction for clustering made? Not stated, but use multilevel modelling. Were appropriate statistical methods used? Yes. Multilevel modelling, multilevel ANCOVA comparisons of substance initiation by group. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | School districts selected on enrolment (1300‐5200 students), and at least 15% eligible free or reduced price lunch. "Communities were blocked on school district size and geographic location, and then they were randomly assigned to the partnership intervention and 'normal programming' comparison conditions." "During the first year, two communities withdrew from the study and were replaced." No method of randomisation Clusters: individuals and communities Cluster constraint: blocked on school district size and geographical location Baseline comparability: equivalent on biological parents present, gender, age, grades, school absence, ethnicity, free lunch, 14 outcome measures. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | At pretest: (Intervention 6091; Control 5931); completed 7th grade: (Intervention 5500, Control 5281); no differential attrition across conditions; 1064 families (2650 family members) attended at least one session of SFP 10‐14 in 142 groups, in 14 intervention schools (17% of eligible families); 90% attended at least 4 sessions; 63% attended at least 6 sessions. "On average, 88% of all eligible students completed assessments at each data collection point..." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
St Pierre 2005 (Adult).
| Methods | Country: US
Site: 8 Pennsylvania middle schools Project ‘ALERT’ implemented model called ‘Extension and School Enhancing Life Skills’ (EXSELS) Focus: alcohol, cigarette, marijuana use Design: cluster RCT (Group 2: change rates) |
|
| Participants | Baseline: 1649 (2 consecutive cohorts)
Age: 7th grade (11‐12)
Gender: 49.5% F Ethnicity: Caucasian 81.4%, African American 5.4%, Native American 2.2%, Hispanic 1.3%, Asian American 1.1%, other 8.5% Baseline smoking data: not stated, though shown in graph |
|
| Interventions | Category: social influences vs. control (social influences adult led & information vs. social influences adult led, teenage assisted & information vs. control) Programme deliverer: community adults (received conventional Project ALERT training), teens (school selected, 1‐day training by researchers, state cooperative extension educators, and adult program leaders) Intervention:
Control: No statement |
|
| Outcomes | Last month: 0, 1 ‐ 2, 3 ‐ 5, 6 ‐ 19, 20 or more days. Last year; 1 or 2, 3 ‐ 10, 11 ‐ 20, more than 20 times. Lifetime: never, ever Follow‐up: e‐mail from Dr. St. Pierre, 3 January 2012: "There were five waves of testing for each cohort (i.e. baseline pretest before program implementation in 7th grade, followed by posttests after the 7th‐grade curriculum, and before and after the 8th grade curriculum. The follow‐up posttest was given approximately 12 months after program delivery when students were in the 9th grade.". |
|
| Notes | Quality of intervention delivery: "Analysis of observation reports... from all of the 90 classrooms and 654 lessons taught indicated that 98% of program activities were covered in the 7th ‐ and 8th ‐ grade Project ALERT classes." "Observer ratings of eight items (participation in small‐group activities, student interest, class control, elicitation of responses, correct use of feedback, respect for students, conveying purpose of lesson, and lesson preparation) on a scale of 1 ‐ 7 (poor to high quality) for each lesson were averaged… Project ALERT was implemented with high quality both years, as reflected by mean ratings across schools ranging from 5.8 to 6.8 for 7th ‐ grade lessons, and from 4.8 to 6.7 for 8th ‐ grade lessons. In addition, student ratings on reaction forms after each program year indicated high quality implementation. Mean ratings (scales 1 ‐ 5, low to high) for regard for program leaders were 4.0 in 7th grade and 3.8 in 8th. Mean scores for perceived effect of program on students was 3.7 in 7th and 3.3 in 8th." Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Yes. "These ANOVAs took into account the nesting of students within schools, treating classrooms as a random effect..." Were appropriate statistical methods used? ANOVA to compare equivalence of intervention and control groups, Multilevel regression modelling, growth curve analysis, 3 level hierarchal linear model. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Each of the eight schools randomly assigned two 7th ‐ grade classrooms to each of three conditions." E‐mail from Dr St. Pierre, 3 January 2012: "Classrooms at each school were randomly assigned by coin tosses..." Clusters: classes Cluster constraint: no statement Baseline comparability: "... site specific analyses revealed that most of the Cohort 2 differences resulted from two sites, which were therefore removed from further analyses. After eliminating these sites, only three nominally significant differences remained, no more than would be expected by chance. Furthermore, no consistent patterns of differences among conditions emerged for either cohort. In sum, there was satisfactory evidence of equivalence among the treatment and control conditions at the pre‐test." |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 88% completed 4/5 and 72.5% 5/5 waves of questionnaires; "... attrition was comparable across the three conditions, with students in the control condition completing a mean of 4.51 waves, students in the adult‐led condition, 4.43 waves, and students in the teen‐assisted condition, 4.54 waves..." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
St Pierre 2005 (Teen).
| Methods | See St Pierre 2005 (Adult) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from the second intervention arm within St Pierre 2005 (Adult) | |
Storr 2002 (CC).
| Methods | Country: USA Site: 9 public primary schools in Baltimore Focus: classroom management Design: cluster RCT (Group 1: never smoking prevention cohort) | |
| Participants | Baseline: 678
Age: 5.3 ‐ 7.7 years (av 5.7)
Gender: 47% F Ethnicity: 86% African Americans, 14% European heritage Baseline smoking data: As age 6, assumed no smoking |
|
| Interventions | Category: social competence vs. social competence vs. control (classroom management vs. teachers communicating with parents vs. usual contact control) Programme deliverer: teachers Intervention:
Control: usual curriculum and parent‐teacher communications |
|
| Outcomes | Self reported time to initiation of smoking Follow‐up: At age 12, "... 6 years after end of intervention year..." |
|
| Notes | Quality of intervention delivery: implementation scores for the CC intervention averaged 60% (range 30% to 78%), and parents in the FSP intervention attended an average of 4/7 sessions; teachers received 60 hrs of training and attended monthly meetings to discuss intervention issues and receive support; fidelity to the interventions was assessed at the monthly meetings and during observation of 3 classroom sessions during the year; the FSP group teachers were asked to document all contacts with parents; and parents reported on the interventions and the skill of the presenters; teachers rated the child's adaptation to school on a 6‐point scale and family and household characteristics were assessed in a 60‐min interview with parents. Statistical quality: Was a power computation performed? The power computation assessed that 150 children per group would be needed; with an av 30% cumulative risk of initiating smoking; between‐group relative risk of initiating smoking = 1.75; and alpha 0.05, 2‐tailed for 80% power. Was an intention‐to‐treat analysis performed? Yes Was a correction for clustering made? No Were appropriate statistical methods used? Yes. Analysis was by general estimating equations with a multivariate response profile approach; Cox regression models to estimate risk of starting smoking. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Within each school, children and teachers were randomly assigned to one of two intervention or control classrooms."; (an e‐mail from Dr. Ialongo states that an SAS programme generated the class lists and randomly assigned students; that children and teachers were randomly assigned to 1st grade within each of the 9 participating schools; and that there was balancing for gender and kindergarten teacher ratings of aggressive disruptive behaviour and academic readiness). Clusters: classrooms Cluster constraints: "A randomised block design was employed, with each of the nine schools serving as a blocking factor..." Baseline comparability: Children in control group somewhat less likely to be male, and African American, more likely to be from 2 parent households, teacher ratings of problem behaviour higher in CC group; these differences were statistically adjusted in the analyses. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Storr 2002 (Figure 1): Of the 678 pupils who entered Grade 1, 549 at 6 year (7th grade) follow‐up (189 CC, 192 FS, 168 control); Furr‐Holden 2004 reported ‐ "At follow‐up, 5, 6, 7 years after randomisation (sixth through eighth grades), approximately 84% (566/678) of the sample was available.". No differential attrition among groups across baseline characteristics or smoking status. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Storr 2002 (FSP).
| Methods | See Storr 2002 (CC) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (FSP) within Storr 2002 (CC) | |
Sun 2008 (Cognitive).
| Methods | Country: USA
Site: 18 high schools in Southern California (2 intervention arms: each with 6 schools: 3 regular high schools (RHS) and 3 alternative (CHS/continuation) high schools with 8 classes from each school; 6 schools in the control arm with 4 classes each). 'Project Towards No Drug Abuse' (TND‐4) Focus: substance use prevention Design: cluster RCT (Group 2: change rates) |
|
| Participants | Baseline: 3908 enrolled students, 2734 Baseline survey (70%) Age: 15.3 years (mean) Gender: 52.1% M Ethnicity: 18.2 % white, 62.1% Hispanic, 8.4% Asian, 8.1% African American, 3.2% other Baseine smoking data: percentage usage of cigarettes in the last 30 days ‐ cognitive only = 19.92%, combined = 12.24%, control = 13.29; number of times used past 30 days ‐ cognitive only = 0.62; Combined = 0.25; control = 0.28 |
|
| Interventions | Category: social Influences vs. information vs. control (Social influences + Correction of Cognitive Misperceptions vs. Correction of Cognitive Misperceptions vs. Usual) Programme deliverer: health teachers (received 1 ½ day training session) Intervention: Over a 4 week period. Intervention based on previous TND trial (Sussman 1995)
Control: Usual prevention activities provided directly by school |
|
| Outcomes | Self report. 1. 30 day use of cigarettes (dichotomous outcome 0 = none, 1+ = yes) 2. Frequency (no of times used; 0 = 0; 1 = 1 ‐ 10; 2 = 11 ‐ 30; 3 = 31 ‐ 50; 4 = 51 ‐ 70; 5 = 71 ‐ 90; 6 = 91 ‐ 100; 7 = 100+ times) Follow‐up: 1 year | |
| Notes | Quality of intervention delivery: no statement Statistical quality: Was a power computation performed? Not stated Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Yes Were appropriate statistical methods used? Generalised mixed‐linear model, chi square, t‐test |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "...schools were blocked by estimates of drug use prevalence... ethnic composition of the school, student enrolment, standardised achievement test scores..., school type and size... The nine RHS‐CHS pairs were aligned using a linear composite of actor scores across a drug use inflate‐suppress continuum and randomly assigned to the three conditions." No method of randomisation stated Clusters: schools Cluster constraint: block, inflate‐suppress continuum Baseline comparability: % cigarette use in the last 30 days – difference across interventions and control is non‐significant, P = 0.92 |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "2064 (75.5% of those for whom had pre‐test survey) also completed the 1 year follow‐up post‐test (P value at the 0.05 level)... Compared to lost‐to‐follow‐up sample, the retained sample was slightly younger (15.7 vs. 15.9 years of age), less likely to smoke cigarettes (21.9% vs. 26.4%), less likely to be male (52.9% vs. 61%), less likely to be African American (7.2% vs. 10.4%) and more likely to be Latino (65.7% vs. 61.9%), and more likely to live with both parents (59.4% vs. 49.3%)... the retention rate... did not differ across program conditions."; no differential attrition analysis. |
| Selective reporting (reporting bias) | Low risk | Outcomes as intended |
Sun 2008 (Combined).
| Methods | See Sun 2008 (Cognitive) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (combined) within Sun 2008 (Cognitive) | |
Sussman 1993.
| Methods | Country: USA
Site: 48 junior high schools in California 'Project Towards No Tobacco Use' (TNT) Focus: tobacco use prevention Design: cluster RCT (excluded from analysis) |
|
| Participants | Baseline: 6716
Age: 7th graders (12‐13yr olds) Gender: 50% F Ethnicity: 60% W, 27% H, 7% B, 6% Asian or other Baseine smoking data: no baseline data, only immediate post‐test and 1 year follow‐up |
|
| Interventions | Category: social influences vs. social competence vs. information vs. all combined vs. control Programme deliverer: community adults (received conventional Project ALERT training), teens (school selected, 1‐day training by researchers, state cooperative extension educators, and adult program leaders) Intervention: 10 lessons in 7th grade academic year
Control: 'usual care' standard health education programme |
|
| Outcomes | Trial cigarette use; weekly cigarette use; trial smokeless tobacco use; weekly smokeless tobacco use. Saliva or breath sample collected before each questionnaire administration, but not analysed Follow‐up: 24m | |
| Notes | Quality of intervention delivery: "Adherence did not vary by condition; the curricula were implemented at all program schools. Exposure to the curriculum did not vary by condition; all activities were completed in each curriculum... Student attendance, as indicated on attendance records, averaged 90% across conditions, equivalent to the average attendance in the regular classroom situation... Students' reports of homework return averaged about 85% across conditions, and was 10% higher than actual homework returns averaged across conditions, as recorded by the health educator." Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? Two methods of data collection were used: for cohort 1 all 7th grade students at 20 of the schools were surveyed and followed as individuals; in cohort 2 students from the remaining 28 schools were surveyed as repeated cross‐sectional partial samples of approximately 3 classes per school; ANCOVA with school as the unit of analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Forty‐eight junior high schools from 27 southern California school districts were recruited and randomly assigned to participate in one of five conditions..." Method of randomisation not stated Clusters: schools Cluster constraint: blocks defined by region (urban, rural), school type (middle school with 6th‐8th grades, junior high with 7th‐8th grades), and a composite based on school size, SES, language, income, academic status, ethnicity, population, age, tobacco use Baseline comparability: not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 7219 9th graders of which 65% (4365) had attended a Project TNT school 2yrs before; there were more students at 2 year follow up (7,219) than at baseline (6,716) due to students joining the study (in the analysis turnover of approximately 7% per year was added to the model to adjust for this difference), and attrition from baseline was not estimated. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Sussman 1995 TND1 CHS C.
| Methods | Country: USA
Site: 29 school districts in a 5‐county region of southern California (each district contained 1 Continuation High School (CHS) for students unable to remain in regular high schools for reasons including drug abuse). Project 'Towards No Drug Abuse' (TND) Focus: alcohol, tobacco and drugs Design: cluster RCT Study TND‐1 (CHS): 21 schools continuation schools to assess the impact of TND Study TND‐I (RHS): trial in 26 classes in 3 regular high schools (RHS) to assess whether the TND programme could be used in regular high schools Study TND‐II (CHS): 18 continuation high schools, to compare the relative effectiveness of the TND programme as delivered by health educators or by self instruction (Group 3: point prevalence). |
|
| Participants | Baseline: TND‐1 (CHS): 2001 out of a potential 2863; TND‐II CHS trial at baseline: 715 students in 18 continuation high schools; TND‐1 RHS trial at baseline: 679 students in 26 classes in 3 regular high schools.
Age: 16.8 years
Gender: 44.6% F Ethnicity: 31.6% White, 49.5% Hispanic, 9% African American; 9% other Baseline smoking data: In Continuation high schools in the past month 57% used cigarettes, 64% alcohol, 55% marijuana, 21% stimulants, and 13% hallucinogens. Percentages for comprehensive high schools from overlapping school districts were 24%, 36%, 22%, 2% and 2% respectively. |
|
| Interventions | Category: social influences & social competence vs. control Programme deliverer: 9 project staff health educators (trained by the project manager). In the 21 TND‐1 (CHS) schools in the schools + school‐as‐community group, a volunteer staff member taught the school‐as‐community component. Intervention: 9 session health motivation, social skills and decision making curriculum about alcohol, marijuana, cocaine, and hallucinogen use. First 3 sessions motivated youth to listen to subsequent health programming and provided them with effective listening skills (listening, stereotyping, drug use myths, and denial sessions); 2nd set of 3 sessions instructed students in chemical dependency issues and alternative coping strategies (stages of chemical dependency, a talk show on the consequences of drug abuse, and stress coping sessions); 3rd set of 3 sessions encouraged making non‐drug‐use choices (self control skills, taking a moderate perspective, decision‐making, and commitment sessions). After the first year three more sessions were added: a session on the confusion between the effects and causes of marijuana use and consequences on use; a session on tobacco cessation and coping with withdrawal; and a session on coping with feelings of anger that could lead to substance abuse or violence. TND‐1 (CHS) had two interventions:
Control: received 'standard care' |
|
| Outcomes | Past 30 days smoking: measured on 11 point scale (from 0 to 9 = 1 to 100+ times/month), and measured expired air CO Follow‐up: 5 years |
|
| Notes | Quality of intervention delivery: health educators delivered the programme and received 2.5 hrs training for each session. At 1 year the process analysis showed that students attended 2/3 of the drug abuse sessions, with good adherence by educators to planned lesson delivery (99 ‐ 100% in 10/20 lessons); all scores on class control appropriateness of the material were 5 or higher on a 1 to 7 scale. Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? Yes Were appropriate statistical methods used? Corrections for estimated ICCs pretest 0.08, then between 0.013 and 0.019. If these correlations had not been included, the true standard errors would have been underestimated and the P values overestimated by 75 ‐ 77% for the cluster (school) sizes. Analysis by ANCOVA. Results only available for TND‐1 (CHS) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A total of 29 school districts from a five‐county region of southern California were recruited for participation in a procedure approximating random selection. Each of these cooperating districts contained 1 continuation high school. Twenty‐one continuation high schools were selected from that pool for participation in the present study... Selected schools were blocked by estimates of drug use prevalence (based on preliminary student and staff interviews at each school), ethnic composition of the school and community, student enrolment, and standardized achievement scores (based on public data) and were randomly assigned by block to one of three experimental conditions..." Method of randomisation not stated Clusters: schools Cluster constraint: blocked by estimates of drug use prevalence (based on preliminary student and staff interviews at each school), ethnic composition of the school and community, student enrolment, and standardized achievement scores (based on public data). Baseline comparability: no significant differences in drug use and 6 demographic variables when pretest sample compared to sample re‐surveyed after 2 years |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | TND‐II (CHS) trial: 2863 students in 21 schools were contacted (75% of those enrolled). Pretest data obtained from 2001 (70%). There were no significant differences on 31 items of drug use and psychosocial correlates between the pretest sample and those measured at both pretest and 1yr. Access to 2863 students (75% of those on enrolment lists); Pretest data on 70% (N = 2001) of these; 1 year follow up on 54% (N = 1074). No significant differences on 31 items of drug use and psychosocial correlates between those measured at pretest and 1 year; at 2 years no significant differences in attrition rates across programmes. Sun 2006 provides 4 ‐ 5 year follow‐up: states eligibles = 1867; baseline = 1578, with follow up data at 1 year for 68% (N = 1074), years 2 or 3 for 66% (N = 1047), and at years 4 or 5 for 46% (N = 725 ); at 4 ‐ 5 years no significant differences in attrition rates across programmes. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Sussman 1995 TND1 CHS SAC.
| Methods | See Sussman 1995 TND1 CHS C | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the data from the school plus school as community component in the TND‐1 CHS trial within Sussman 1995 TND1 CHS C | |
Sussman 2007.
| Methods | Country: USA
Site: 12 alternative (continuation) high schools in Southern California (6 to intervention, 6 to control); 8 classes from each school Project Ex‐4 Focus: Smoking cessation among smokers and smoking prevention for non‐smokers Design: Cluster RCT (Group 2: change rates) |
|
| Participants | Baseline: 2020 (total enrolment in all classes), 1367 consented, 1097 baseline survey (532 in control, 565 in intervention)
Age: 16.5 years (mean)
Gender: 62.7% M Ethnicity: 16.4% White, 70.9% Hispanic, 3.5% Asian, 5.1% African American, and 4.1% other Baseline smoking data: 33% weekly smokers, 42% monthly smokers |
|
| Interventions | Category: Social influences & social competence vs. control (mostly social influences plus a bit of social competence) Programme deliverer: project staff Intervention: adapted from the Project EX program (cessation program), 8 sessions over a 6 week period: four sessions in two weeks to strengthen resolve against tobacco; four sessions once per week in the next month to focus on intentions not to use tobacco. Sessions include how smokers and non‐smokers feel, increased stress levels, guest speakers, industry marketing tactics, healthy lifestyle, commitments to remain tobacco free, nicotine addiction with consequences, relaxation techniques. Control: standard care (only activities already provided directly by school) |
|
| Outcomes | Last 7 days and last 30 days smoked. Responses could be a number from 0 to 100+: no = non‐smoker, yes = > 0% Follow‐up: three post‐tests (immediate, 6 month, 1 year) |
|
| Notes | "Continuation high schools students report almost twice the amount of last 30‐day use of cigarettes as regular high schools..."; project EX‐4 has not been attempted in regular schools. Quality of intervention delivery: students were asked after the program to (1) rate each session from 1 = terrible to 10 = excellent; (2) rate each session using 9 adjectives e.g. 'interesting, informative, well‐organised, enthusiastic, well‐informed', and rate from 1 = 'not at all' to 10 = 'extremely' (3) did program help them quit using 8 options from 'quit tobacco use completely' to "... strengthen your commitment to stay tobacco free..." (4) how much they liked or disliked 7 major curriculum components: 'Talk show: family and friends confront smokers about their habit'; 'Talk show: cigarettes may be stressing you out'; 'Healthy breathing'; 'Game: is smoking on the menu?'; 'Talk show: quitting smoking: I’ve been there and it does get better'; 'Yoga'; 'Meditation' (5) 16 program knowledge items. Only data for knowledge items were reported: control: 53.5% pretest; 51.2% posttest (p = 0.06); intervention groups: 51.2%, 57.4%, (P < 0.0001) Statistical quality: Was a power computation performed? Not stated Was an intention‐to‐treat analysis performed? No (except with immediate post‐test data which revealed a similar result to the compete case analysis at that point) Was a correction for clustering made? Yes Were appropriate statistical methods used? Multi‐level random coefficients models, chi square, t‐tests |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "... blocked prior to assignment by school size, ethnicity, composition, average social economic status, and % of students in classes with English as second language. Specifically, six pairs of schools were aligned using a linear composite of factor scores across a tobacco use inflate suppress continuum and randomly assigned to the two conditions." No method of randomisation Clusters: schools Cluster constraint: blocks, inflate suppress continuum Baseline comparability: not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Immediate post‐test control = 391, intervention = 487 (20% attrition) 6 month post‐test control = 426, intervention = 439 (21% attrition) 12 month post‐test control = 335, intervention = 375 (35% attrition) "... at the six survey on age, ethnicity, gender, living situation, parents’ education level, and cigarette smoking prevalence. Compared with the 'lost' sample, the 'retained' sample was slightly younger, contained more Hispanic (74% vs. 60%, P < 0.0001) and less white (14% vs. 25%, P = 0.0001) subjects, more females subjects (39% vs. 30%, P < 0.01), more students that lived with both parents (55% vs. 39%. P < 0.0001), a lower educational level among students’ parents (2.9 vs. 3.3, P < 0.0001), and a lower prevalence on the smoking outcome variables (e.g. 25% daily smoking vs. 41%, P < 0.0001). Some of these statistically significant differences were found at the one‐year follow‐up as well; that is, fewer whites and more Latinos, more students who lived with both parents, lower levels of parental education, and a lower prevalence of cigarette smoking students in the retained sample relative to those lost to follow‐up." |
| Selective reporting (reporting bias) | Low risk | Outcomes reported as intended |
Telch 1990 (No peers).
| Methods | See Telch 1990 (Peers) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (No peers) within Telch 1990 (Peers) | |
Telch 1990 (Peers).
| Methods | Country: USA Site: 2 junior high schools in southern California (15 social studies classes in 1 school divided between 2 interventions and control) Focus: smoking prevention (other drug use also assessed) Design: cluster RCT (Group 1: never smoking prevention cohort) | |
| Participants | Baseline: 540 in randomised classes, 234 in control school
Age: 7th grade (12 yrs)
Gender: 47% F Ethnicity: 24% W, 17% B, 19% H, 24% A, 16% O Baseline smoking data: approx 80% baseline never users in school 1 |
|
| Interventions | Category: social influences vs. control (social influences with videotapes and teachers and without peer‐leaders), an additional control group is non‐random Programme deliverer: teachers, same‐age peers elected (received 1hr training) Intervention: 5 sessions over 3 weeks
Control: (Not random) in another school; survey only, no intervention |
|
| Outcomes | Self reported smoking, nonsmoker; experimental ( < 1/week); regular (once/week or more). Individual students were tracked using coded questionnaires. Results presented both as pre and post prevalences, and as onset rates for baseline non‐users. Expired CO (analysed but not reported) and saliva ('bogus pipeline'); alcohol and marijuana use. Follow‐up: 5 session Intervention 7th grade; pretest Oct 1984, post‐test May 1985 | |
| Notes | Quality of intervention delivery: No process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? Analysis by chi‐square |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Initial selection of schools not reported "Seventh grade students (N = 540)... were randomly assigned by classroom to... (a) videotape social pressure resistance training with peer leader involvement; (b) videotape social pressure resistance training alone, or (c) survey‐only..." Method of randomisation not stated The control group in the 2nd school was non‐random. Clusters: classes Cluster constraint: not stated Baseline comparability: no significant differences |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Table 1 totals to 572 at posttest, but randomisation statement says 540 were randomised. Complete pretest‐post‐test data from 81% in school 1; 58% from school 2 No attrition analysis. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Unger 2004 (CHIPS).
| Methods | See Unger 2004 (FLAVOR) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (CHIPS) within Unger 2004 (FLAVOR) | |
Unger 2004 (FLAVOR).
| Methods | Country: USA
Site: 16 middle schools in southern California Multiculturally adapted Project 'Fun Learning About Vitality, Origins and Respect' (FLAVOR) compared to Choosing Healthy Influences for a Positive Sel (CHIPS) Focus: smoking prevention; multicultural curriculum vs same curriculum without multicultural content Design: cluster RCT (Group 1: never smoking prevention cohort) |
|
| Participants | Baseline: 2775 invited; of whom 2131 (77%) provided parental consent and of these 1978 (92%) completed the 6th grade survey (1,455 never‐smokers, 316 smokers); Johnson (2005) gives data for 24 schools (including 8 wait‐list control schools): 3157 completed baseline survey. Age: 6th grade (11.3 years) Gender: 54% F Ethnicity: (FLAVOR: 57.6% Hispanic, 24.1% Asian American, 1.6% African American, 6.2% White, 10.5% Other); (CHIPS: 61.2% Hispanic, 21.6% Asian American, 1.0% African American, 6.1% White, 10.3% Other); (Control: 59.2% Hispanic, 23.2% Asian American, 0.5% African American, 7.8% White, 9.4% Other) Baseline smoking data: never‐smokers, N = 2219 |
|
| Interventions | Category: social influences vs. social influences vs control (social influences (multicultural) + state of California tobacco education vs. social influences (role plays, games, art projects) + state of California) tobacco education. Programme deliverer: health educator Intervention:
Control: wait‐list Co‐interventions: all schools in California are legally obliged to provide tobacco education in grades 4 ‐ 8 |
|
| Outcomes | Lifetime smoking: even a few puffs; past month (smoked on at least one day); analysis of past month smoking Follow‐up: 18 months (email form Dr Unger 24 February 2012) |
|
| Notes | Quality of intervention delivery: no statement Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Yes Were appropriate statistical methods used? Pre‐intervention equivalence of groups assessed by X2 and ANOVA; LR assessed differential attrition; multilevel LR with school as a random effect assessed outcomes. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Clusters of public schools were identified and grouped together based on similar ethnic composition and geographic location (within the same school district if possible). Schools within each cluster were randomly selected... Because the Catholic schools were geographically diverse, assignments were done using a principal components analytic method previously found to be valid in assigning generally dissimilar schools to conditions. The method controlled for potential confounding variables by generating a composite score based on those variables. Subsequent groups of schools with the highest and most similar composite scores were then clustered and assigned randomly to conditions." Email from Dr Unger 24 February 2012: "A computerized random number generator in SAS was used to allocate schools to conditions..." Clusters: schools Cluster constraint: grouped according to similar ethnic composition and geographic location; principal components analytic method Baseline comparability: student or parent born outside US (FLAVOR 72%; CHIPS 79.3%; Control 75.5%; P < 0.001); median household income > US$40,000 (FLAVOR 34.2%; CHIPS 28.2%; Control 22.6%, P < 0.001); lifetime smoking prevalence (FLAVOR 11.1; CHIPS 10.4%; Control 7.3%, P < 0001) |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Completion of forms was anonymous, but not clear students knew to which group they were assigned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Follow up 1yr later: of those who completed the 6th grade survey, 1571 (80%) completed 7th grade survey; follow‐up 2yrs later: 2412 (76.4%) completed the 8th grade survey; 23.6% attrition between 6th and 8th grade; no differential attrition between groups. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Valente 2007 (TND).
| Methods | Country: US
Site: 14 high schools provided 75 classes (22 TND regular, 25 TND Networked, 28 Control) from 7 school districts in California (8 out of 25 districts invited agreed to participate, 1 acted as pilot district) 'Project Towards No Drug Abuse' (TND) Focus: substance abuse prevention in high risk adolescents Design: cluster RCT (Group 1: never smoking prevention cohort) |
|
| Participants | Baseline: 938
Age: 16.3 years (mean)
Gender: 38% F Ethnicity: 72% Hispanic/Latino, 6% African‐American, 11% White, 11% other Baseline smoking data: (N = 855): TND 2.48, TND Network 2.36, Control 2.14, total 2.34 |
|
| Interventions | Category: Social influences (random peers) vs. social influences (peer networks) Programme deliverer: Peers (trained by health educators) Intervention: Delivered over 3‐4 weeks, and provided to 47 classes over a 9 month period
Control: "prevention as usual..." |
|
| Outcomes | Monthly tobacco use: 1 = none, 2 = 2 ‐ 10 times/month, 3 = 11 ‐ 20 times/month… 11 = 91+ times/month Follow‐up: 1 year |
|
| Notes | Quality of intervention delivery: no statement Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Yes. Multilevel regression analysis ‐ "All regression analyses controlled for within classroom clustering by specifying school as the clustering variable..." Were appropriate statistical methods used? Appropriate; lagged regression model, multi level model. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "... classrooms that could be assigned randomly to one of three conditions..."; E‐mail from Dr. Valente, 3 January 2012: "Method of randomisation was systematic so that schools were ordered on school ID number and classes within schools on class ID number (typically period) and then assigned 1, 2, 3 (control, TND, TND Network)." Clusters: no statement school and class Cluster constraint: no statement Baseline comparability: no differences between group on age, grade, mother’s education, ethnicity, networks |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Baseline surveys = 938, 1 year follow‐up = 594, complete data at 1 year = 541; then 53 who did not state substance abuse removed from baseline survey to yield new baseline = 885. "There were no differences on any variables between those retained in the study and those lost to follow up."; age = 16.2 at 1 year follow‐up (Table 1) implying older students dropped out. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Valente 2007 (TNDNetwork).
| Methods | See Valente 2007 (TND) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (TNDNetwork) within Valente 2007 (TND) | |
Van Lier 2009.
| Methods | Country: Netherlands
Site: 13 elementary schools in Rotterdam and Amsterdam (31 classes – 16 intervention and 15 to control) 'Good Behaviour Game' (GBG) Focus: reduction in disruptive classroom behaviour to reduce tobacco and alcohol initiation Design: cluster RCT (Group 1: never smoking prevention cohort) |
|
| Participants | Baseline: 744 eligible, 666 consented
Age: 6.9 years
Gender: 52% M Ethnicity:69% Dutch descent, 10% Turkish, 9% Moroccan, 5% Surinam/Dutch Antillean, 7% Other ethnic groups Baseline smoking data: % of children in both intervention and control groups having smoked less than one cigarette per week or more at age 10 = 5.7%. % of children having used tobacco at age 10 (baseline) = intervention 4%, control 8%. never‐smokers: intervention N = 253 (96%), control N = 197 (93%) |
|
| Interventions | Category: social influences vs. control Programme deliverer: teachers (received 3 afternoons of training each year) Intervention: Good Behavior Game: teachers and students choose positively formulated class rules, teachers assign children to teams based on behavioural observations of rule breaking behaviour; children encouraged to manage own and team‐mates' behaviours. Introduction stage (10 minutes, 3 x/week), then 'Expansion' stage (expansion of time and behaviours), then 'Generalization' stage (rules always apply). Control: no intervention |
|
| Outcomes | Cigarette use: 0 (did not smoke at given age ) to 7 (> 20 cigarettes/day); self reported. "Probably because of our young sample, in those who reported smoking, the majority reported smoking less than one cigarette per week. We focused of use versus nonuse, (0 = no tobacco use at given age, 1 = tobacco use; defined as ‘smoking one cigarette or less a week’ to ‘smoked more than 20 cigarettes per day’)." Follow‐up: 4 years (follow up age 10 to 13) |
|
| Notes | Quality of intervention delivery: external school advisors checked fidelity: 9/13 schools implemented programme completely, 3 implemented Introduction and Expansion stage, one Introduction stage only; over 2 years. GBG played average 116 times, for total of 136 hrs; and in 5 classes in which teacher did not move on to expansion stage, GBG played 63 times, and in remaining 13 classes in which programme was implemented completely, average number of sessions 139; teachers of control classes were monitored for not implementing GBG. "Among all the activities, 'the nicotine toxicity experiment' had the highest rate of participation (88.5%), followed by 'a letter to parents' (73.6%), 'agreement of building families free of smoking' (69.8%), 'health education through experiments' (68.6%), 'health education through multimedia' (65.7%) and 'signature on the 18th World Day of No Smoking' (65.6%)..." Statistical quality: Was a power computation performed? Yes Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Yes Were appropriate statistical methods used? Multilevel growth model, logistic growth model |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "... classes were randomly assigned... " Email from Dr Van Lier 1 February 2012 "... a computerized randomisation procedure was used..." Cluster: classes Cluster constraint: not stated Baseline comparability: not stated other than "... 51% of children were male, which did not differ for ethnic groups..." Van Lier 2004. Email from Dr Van Lier 1 February 2012: "No differences between intervention and control group children were found with respect to gender or SES (low SES; defined as parents being unemployed or holding an elementary job), current parental smoking or smoking during pregnancy." |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Children told answers confidential, teachers not present, but not clear if children knew which group they were in. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 21% attrition (525 of 666 baseline); no differential attrition "Assessments of substance use from age 10 to 13 were available for 525 children (79% of initial sample). However, because of our focus on the prevention of early substance use, we decided that data had to be available from the age 10 year assessment onward; this was the case for 477 children... Loss to follow‐up was neither related to intervention condition, nor the child’s gender, but related to being of low SES (P < 0.01)." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Vaughan 2007.
| Methods | Country: USA
Site: 2 schools, one middle & one high Focus: substance use prevention Design: RCT (excluded from analysis) |
|
| Participants | Baseline: 364
Age: intervention: 12.9; control: 13.0 (mean)
Gender: intervention: 51.1% M; control: 53.6% M Ethnicity: not stated Baseline smoking data: not stated |
|
| Interventions | Category: multimodal vs. control Programme deliverer: Project Success Counsellor (school based) Intervention: five components: 1) 8 session substance prevention program with small groups 2) school‐wide activities to increase awareness and encourage compliance 3) individual and group counselling 4) parent programs 5) referral (additional help within the community) Control: exposed to school wide activities |
|
| Outcomes | Ever use of cigarettes Follow‐up: 1 & 2 years |
|
| Notes | Quality of intervention delivery: "total of 22 prevention series were implemented... reaching 191 students... analysis of checklist showed that counsellors covered 100% of the learning objectives for each of the four topics..." Statistical quality: Was a power computation performed? Not stated Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? Not applicable Were appropriate statistical methods used? Linear mixed model |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "... a within‐school randomised design was employed, in which students with even‐numbered birthdays received the intervention whereas students with odd numbered birthdays did not... in addition there were two schools without Project SUCCESS that were included for a school comparison group.", (i.e. non‐randomly assigned). Clusters: individuals Cluster constraint: none stated Baseline comparability: not stated |
| Allocation concealment (selection bias) | High risk | "The within‐school design of the study interfered with program implementation and caused contamination between treatment and control conditions." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition 17% over 2 years. "... serious limitation in the study was the differential attrition that occurred between these two groups... more males and respondents involved with substances dropped out over the course of study. This occurred primarily among control group participants and made it more difficult to find significant differences between treatment and control group participants in terms of substance usage, as well as, in the risk and protective factors." |
| Selective reporting (reporting bias) | Low risk | Outcomes as planned |
Villalbí 1993.
| Methods | Country: Spain Site: 23 schools in Barcelona Focus: prevent tobacco, alcohol and drug use Design: cluster RCT (excluded from analysis) | |
| Participants | Baseline: target population: 2205; anonymous questionnaires completed by 2,033 students present in winter 1990
Age: 12‐14
Gender: not stated Ethnicity: not stated Baseline smoking data: the experimental group had slightly more one‐time smokers (P < 0.05), regular smokers (P < 0.01) and those who had purchased tobacco (P < 0.01) than the control. |
|
| Interventions | Category: social competence vs. control Programme deliverer: not stated Intervention: 8 sessions; information on addictions; group pressures; mechanisms of advertising; personal experience; external pressures to use ATOD; the diffusion of addictive activities in society; difficulties in breaking addictions; confronting anticipated situations; personal expression of attitudes; information for parents Control: no statement |
|
| Outcomes | Definition of smoking: accepted a cigarette; smoked once; bought tobacco; regular smoker (weekly or daily)
Post‐test by 1,904 at end of 1989/90 school year, analytic sample 1,723 Follow up: After completing intervention 6 months? |
|
| Notes | Quality of intervention delivery: No process analysis Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? Analysis by chi‐square |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Las 25 escuelas que aceptaron participar fueron asignadas de manera aleatoria al grupo de intervención o al grupo control, estratificando la asignación según tipo y tamaño de la escuela." 25 schools agreed to participate, were stratified by school type, and were randomly assigned to experimental and control groups; 2 schools withdrew before the study commenced Method of randomisation not described Clusters: schools Cluster constraint: stratified by school type Baseline comparability: there was a higher proportion of smokers in the experimental group. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 2033 at baseline, 1904 at second follow up, 1795 (86.5%) present at completion of study, 1723 responses at conclusion of the study; 15% attrition. No attrition analysis |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Walter 1985.
| Methods | Country: USA
Site: 22 elementary schools in The Bronx, New York (14 schools to intervention, 8 schools to control) 'Know Your Body' Studies Focus: Prevent cigarette smoking and improve fitness and nutrition Design: Cluster RCT (excluded from analysis) |
|
| Participants | Baseline: 2283 eligible subjects (risk factors measured in 1563 (68.5%))
Age: 4th grade (9 ‐ 10 years) Gender: 51.5% M Ethnicity: 25% W, 49% B, 23% H, 3% Asian or Pacific Baseline smoking data: Current cigarette smokers = 1.3% |
|
| Interventions | Category: social influences vs. control Programme deliverer: teachers (received 1.5 days training) Intervention: 'Know Your Body' programme addressed nutrition, physical fitness and smoking components with 5 teaching techniques (modelling of desired behaviours, behavioural rehearsal, goal specification, feedback of results, and reinforcement for favourable behavioural change) vs. received health screening. "The curriculum... uses the techniques of modeling, rehearsal, goal specification, feedback of results, and reinforcement to effect voluntary favorable behavior change... The cigarette smoking prevention component... was based on previous research identifying three major factors believed to influence adolescents' decisions regarding smoking; namely, health beliefs, psychological influences, and social influences. The health beliefs section featured biofeedback experiments demonstrating the immediate effects of smoking... In the psychological influences section, students explored the the effects of self‐image, values, stress, and anxiety on smoking‐related decisions. Skills training in this section included alternative stress management techniques, such as progressive muscle relaxation and mental imagery. The social influences section focused on parental modeling, peer pressure, and media influences in relation to initiation of cigarette smoking. Training in decision‐making, communication, and assertiveness skills was emphasized." Duration: 2 hrs/w over school yr, from 4th ‐ 8th grade Control: received the results of their health screens and explanatory information (authors note that this may constitute a minor treatment effect) |
|
| Outcomes | Serum thiocyanate at first follow‐up, saliva cotinine subsequent, (blind analysis of double samples correlated r = 0.97). Follow‐up: 1yr (from start of programme), 5yrs (Walter 1988) | |
| Notes | Quality of intervention delivery: teacher adherence to programme monitored; results of the process analysis not stated Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? Difference in risk‐factor change; analysis by linear regression |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Pairs of districts were matched demographically before random assignment... 4 schools randomly assigned to the intervention condition, eight schools to the control condition..." Method of randomisation not stated Clusters: schools Cluster constraint: pair matched by demographics Baseline comparability: no differences at baseline |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1115 (71.3%) at 1yr due to high mobility from inner schools and high absenteeism; 29% attrition. Follow‐up data were computed for individuals No differential attrition at 12m, except for serum thiocyanate (37.6 µmol/L for those examined at the 12 m vs. 35.0 µmol/L (P < 0.036) for subjects lost to follow‐up). |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Walter 1986.
| Methods | Country: USA
Site: 22 schools in 6 districts (data reported for 15 schools in 4 districts), Westchester County NY 'Know Your Body' studies Focus: smoking prevention, improving nutrition and fitness Design: cluster RCT (Group 1: never smoking prevention cohort) |
|
| Participants | Baseline: 1822 eligible subjects, of whom baseline risk factors measured in 1525 (84%) Age: 4th grade (9 yrs) Gender: 47% F Ethnicity: 84% W, 9.5% B, 2% H, 4% Asian or Pacific Baseline smoking data: serum thiocyanate (micromoles/L): intervention 35.7, control 35.3 |
|
| Interventions | Category: social competence vs. control Programme deliverer: teachers Intervention: information and skills training about tobacco, diet and exercise. 'Know Your Body' programme to prevent smoking, and improve nutrition and fitness. See Walter 1985. 2 class periods/w during the school year, 4th to 9th grade. Control: received the results of their health screens and explanatory information |
|
| Outcomes | Definition of smoking: serum thiocyanate at baseline and 1yr (cut off for smoking ≥100 µmol/L). At subsequent follow ups saliva cotinine (cut off = any detectable levels) Follow‐up: 1 yr from baseline, 5 years, 6 years, later results for 15 schools in 4 districts | |
| Notes | Quality of intervention delivery: researchers monitored teachers' proficiency in delivering the curriculum, but the results were not stated Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? Not stated Was a correction for clustering made? No Were appropriate statistical methods used? Analysis by linear regression |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "At baseline in The Bronx, all 22 eligible elementary schools agreed to participate, and the schools subsequently were randomly assigned to either the intervention (1590 students in 14 schools) or the non‐intervention (693 students in 8 schools) treatment group... At baseline in Westchester... Pairs of districts were matched demographically before random assignment..." Method of randomisation not stated Clusters: schools in districts Cluster constraint: pair matched districts based on demographics Baseline comparability: no differences in health knowledge and behaviours at baseline among the groups |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | N at 12m follow‐up: 1215; 20% attrition (for the 12 months results based on 22 schools); No explanation as to why data only reported for 15 schools in 4 districts at 5 and 6 years; 5yrs (Walter 1988, analytic sample = 733), 6yrs (Walter 1989, analytic sample 593). Serum thiocyanate concentrations did not differ between those present at baseline; and between those present at baseline and lost to follow up. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Weichold 2011 (Peer).
| Methods | See Weichold 2011 (Teacher) | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | This represents the 2nd intervention arm (Peer) within Weichold 2011 (Teacher) | |
Weichold 2012 (Teacher).
| Methods | Country: Germany
Site: 5 Classes in a one Gymnasium in town of 24,000 in Thűringen, E. Germany (3 classes teacher‐led intervention, 1 class peer‐led intervention, 1 class control) Focus: alcohol and tobacco prevention 'Life Skills Program' Design: cluster RCT (Group 2: changes rates) |
|
| Participants | Baseline: 105
Age: 10.74 years (mean)
Gender: 44% F Ethnicity: German, others not stated Baseline smoking data: prevalence smoking (ever use) teacher‐led intervention group 0.29 mean (0.45 SD), peer‐led intervention group 0.45 mean (0.61 SD), control group 0.35 mean (0.57 SD) |
|
| Interventions | Category: social competence and social influences vs. control Programme deliverer: teachers; 4 peers delivered programme to one 5th grade classroom Intervention: (Grade 5: ten 90‐minute and five 45‐minute sessions (in one week); Grade 6 & 7 booster: project day (total three 90‐minute and four 45‐minute project sessions) IPSY (Information + Psychosocial Competence = Protection): generic, intra‐ and interpersonal Life Skills (e.g. communication skills, coping with anxiety and stress, problem solving) with the training of skills related to substance use (e.g. refusal skills). Knowledge concerning alcohol and cigarette use (e.g. actual prevalence rates, short‐term consequences of substance use, advertising strategies), information on the adequate structuring of leisure time, sessions on school issues (e.g. attitudes towards school); interactive teaching methods (role‐play, group discussions).
Control: produced a student newspaper (same time commitment). |
|
| Outcomes | Self reports of 1. ever used cigarettes, 2. frequency of smoking previous month (0 = never to 4 = daily) Follow‐up: 2 years |
|
| Notes | Quality of intervention delivery: teachers reported they taught the full content of the programme manual in > 90% of the sessions, peer facilitators reported whole content according to IPSY manual for 80% of those sessions. Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No; but 125 at baseline, 122 at 2 year follow‐up. Was a correction for clustering made? No Were appropriate statistical methods used? 2‐way ANOVAS with group and time |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No method of randomisation stated other than 'classroom‐wise randomisation' Clusters: classes Cluster constraint: not stated Baseline comparability: equivalent on gender, SES, smoking and drinking behaviour of family and friends, adolescent smoking and drinking and resistance skills. "Students in the control group were more likely to come from the town compared to the students of the other two conditions." |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 125 at baseline, 122 at 2 year follow‐up |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Wen 2010.
| Methods | Country: China
Site: 4 junior high schools in Huangpu district in eastern suburb of Guangzhou (18 schools screened for eligibility, only 12 met the criteria (>100 students for each 7th and 8th grade, > 80% students remaining in the same school until 9th grade; four agreed to participate) Focus: prevention of smoking initiation, reduction of current smoking Design: cluster RCT (Group 1: never smoking prevention cohort) |
|
| Participants | Baseline: 2343 (2 cohorts: cohort I N = 1169, cohort II N = 1174)
Age: 13.4 years (mean)
Gender: 45.9% F, 52.1% M, 2% not stated Ethnicity: not stated Baseline smoking data: cohort I intervention group: ever smoked N = 66, regular smoking N = 14; cohort I control group: ever smoked N = 43, regular smoked n = 8; cohort II intervention group: ever smoked N = 88, regular smoking N = 14; cohort II control group: ever smoked N = 67, regular smoking N = 20 |
|
| Interventions | Category: multimodal vs. control Programme deliverer: school nurses and health education teachers (after attending 8 hr training workshop) Intervention: (staggered over 1 1/2 year period), 3 components:
Control: standard 45 minute anti‐smoking curriculum, textbook with 3 pages about smoking, and brief celebration of WHO Day of No Smoking. |
|
| Outcomes | Never smoked vs. ever (1 or 2 puffs or at least 1 cigarette/week for 3 months). Self reported Follow‐up: stated 2 years, but from end of last intervention stage only 6 months |
|
| Notes | Quality of intervention delivery: 20 intervention activities, 5636 anti smoking pamphlets and textbooks, posted 151 posters, collected 123 samples of essays and posters, and received 950 signed family no‐smoking contracts. "Among all the activities, the 'nicotine toxicity experiment' had the highest rate of participation (88.5%), followed by 'a letter to parents' (73.6%), 'agreement of building families free of smoking' (69.8%), 'health education through experiments'(68.6%), 'health education through multimedia' (65.7%) and 'signature on the 18th World Day of No Smoking' (65.6%)." Statistical quality: Was a power computation performed? Yes. "Assuming Type I error α = 0.05 and the power level 1 – β = 0.8, about 300 students per group (intervention or control) were required for each cohort to detect a small effect size of 0.23 which was equivalent to 9% in the prevalence of ever smoking (25% control vs. 16 % intervention) or a difference of 6% in the prevalence of regular smoking (10% control vs. 4% intervention) at 1‐year follow‐up." For the post hoc power calculation: "With Type I error of 0.05 and the power level of 0.8, the randomisation of intervention at school level would require six or four schools per group with ever smoking or regular smoking as the outcome, respectively, to detect the hypothesized differences in the a priori calculation of sample size." Was an ITT analysis performed? Data presented on a complete case analysis. Authors stated ITT completed but no data was presented. Was a correction for clustering made? Yes Were appropriate statistical methods used? Chi square for baseline characteristics; Cohen’s d for effect sizes, mixed effects regression model. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "... within each pair, one school was randomly assigned as the control group and the other as the intervention group. The randomisation was performed using a random number generation method by a statistician who was uninvolved in this study and also blinded to school names." Clusters: school Cluster constraint: matched on public/private status Baseline comparability: no substantial differences in age and gender, or baseline smoking prevalence in cohort I. Cohort II had a higher baseline prevalence of smoking (5.6 vs. 2.2%, P = 0.006). The class size in the intervention group was larger than the control group. |
| Allocation concealment (selection bias) | Low risk | See above |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "... only students, neither research assistants nor school administrators, were blind to intervention allocation." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Cohort I: of 650 in Intervention group, 88.6% completed 1 year and 83.2% 2 year follow‐up; for 519 in control group, 70.7% and 61.3% Cohort II: for 689 in intervention group 90.9% completed 1 year follow up and for 485 in control 73.6%. "There were no apparent differences (P > 0.05) in gender or age between full and retained samples in follow‐ups, except for the Cohort II control group in which males were more likely (P = 0.042) to drop out than females. Students reporting ever smoking and regular smoking at baseline were more likely (P < 0.05) than non‐smokers to drop out in 1 year follow‐up." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Werch 2005.
| Methods | Country: US
Site: 1 Suburban High School near Florida 'Project SPORT' Focus: Fitness assessment and consultation, and messages against alcohol use to increase activity and decrease substance use. Design: RCT (Group 3: point prevalence) |
|
| Participants | Baseline: 604
Age: 15.24 years
Gender: 56% F Ethnicity: Caucasian 51%, 21.5% African‐American, 27.5% other Baseline smoking data: mean smoking frequency in past 30 days Intervention group = 0.38, Control = 0.56 |
|
| Interventions | Category: other interventions vs. control This intervention did not align with the main five categories; the programme intervenes by linking sports with substance non‐use. Programme deliverer: nurses, certified health education specialists (received 2 days training in demonstrations, role playing and feedback) Intervention: 7 items health and fitness screen, one‐on‐one SPORT fitness consultation, take home fitness prescription, one‐page flyer was mailed out to participants after 1 week Control 1: standard 45 minute anti‐smoking curriculum, textbook with 3 pages about smoking, and brief celebration of WHO Day of No Smoking Control 2: commercially prepared generic alcohol prevention and health promotion print materials |
|
| Outcomes | 30 day (1 = 1 ‐ 2 days, 2 = 3 ‐ 5 days, 3 = 6 ‐ 9 days, 4 = 10 ‐ 19 days, 5 = 20 ‐ 29 days, 6 = all 30 days), self reported Follow‐up: 3 months & 1year |
|
| Notes | Quality of intervention delivery: random sample of N = 15 audio taped one‐on‐one consultations rated 3.93/4 for completeness, 3.73/4 for altering tone of voice, 3.40/4 for accuracy of following protocol, and 3.40/4 for student’s responsiveness to the lesson. Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No Was a correction for clustering made? No Were appropriate statistical methods used? Descriptive, ANCOVA, MANCOVA |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A randomised controlled trial was conducted, with participating students randomly assigned within grade levels (9th and 11th grades) by computer to either the intervention or control group." Clusters: individual students Cluster constraint: not applicable Baseline comparability: "No differences were found on any of the socio‐demographic measure between groups with one exception. A greater proportion of control adolescents (42.7%) reported a family alcohol or drug problem, than intervention adolescents (34.9%), x2 = 3.89, 1 df, p = 0.05. No differences were found between groups on any of the alcohol and drug consumption or exercise habit measures (p’s>0.05)..." |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | At 1 year, 514 (85%), no differential attrition between groups |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
Zheng 2005.
| Methods | Country: China
Site: 2 communities in the south of the Xu‐Hui district. Focus: smoking prevention Design: cluster RCT (excluded from analysis) |
|
| Participants | Baseline: 546 (234 intervention, 314 control); 542 returned valid questionnaires
Age: 9.6 years (average)
Gender: not stated Ethnicity: not stated Baseline smoking data: proportion of children who have attempted smoking: 41 (18%) in intervention and 40 (12.7%) in control; however Table 3. "Changes in smoking attempts between the intervention and control groups within the last year..."; baseline ‐ 7.8 intervention, 3.8 control. |
|
| Interventions | Category: multimodal vs. control (school component = information and social influences) Programme deliverer: teachers Intervention: 1) 22 lessons on: dangers of active and passive smoking, how to reject smoking, how to prevent becoming a victim of passive smoking; (2)smoke‐free policy in school; (3) training to educate teachers about 'smoking control'; (4) posters, comic strip competitions; (5) letters to parents to become smoke‐free role models, and campaign by students to involve parents in signing smoking cessation pacts; (6) smoking control activities in community during summer holidays. Control: no statement |
|
| Outcomes | Smoking attempters: "... those who have tried smoking, including those who have smoked an entire cigarette or just one or two breaths."; passive smokers: "non‐smokers who on average inhaled cigarette smoke passively for 15 minutes or more, one day or more a week." Follow‐up: 1 & 1 ½ years post baseline |
|
| Notes | Quality of intervention delivery: No statement Statistical quality: Was a power computation performed? No Was an intention‐to‐treat analysis performed? No, but 542 baseline, 539 at 1 ½ years Was a correction for clustering made? No Were appropriate statistical methods used? Chi2, t‐tests, logistic regression |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Chang‐Qiao district was randomly allocated as the intervention group, while the Mei‐Long district was randomly allocated as the control group..." Email from Dr Zheng, 4 April 2012 ‐ randomisation by "coin to decide the group" Clusters: schools Cluster constraint: "Two schools were randomly drawn from the two communities. The schools were required to be fundamentally similar in terms of the background of the students, the teaching staff available, the size of the school, the standards of the teaching, etc." Baseline Equivalence: no difference in smoking attempts, age, gender, but parents in control group better educated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | At 1 year post‐test 545; at 1 ½ year post‐test 539 |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
av = average (mean) ATOD = alcohol, tobacco and other drugs 'bogus pipeline' = biochemical verification samples collected but not tested CI = confidence interval cig = cigarette CO = carbon monoxide DARE = Drug Abuse Resistance Education Ethnicity: W = white; B = black; H = hispanic; A = Asian; A‐A = African‐American; N‐A = Native American; O = other F = female GEE = generalized estimating equation Gender: M = Male; F = female GLM = General Linear Model hr = hour ICC = Intraclass correlation coefficient ITT = intention‐to‐treat LR = logistic regression LST = Life Skills Training m = month M = male N, n or No. = number NNT = number needed to treat n.s. ‐ not statistically significant OR = odds ratio ppm = parts per million SD = standard deviation SES = socio‐economic status sig diff = significant differencen ST = smokeless tobacco µmol/L = micromole per litre w = week yr = year
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aarø 1983 | Not an RCT. "The schools had been divided into four groups in advance, and the package was presented in four different versions." |
| Abernathy 1994 | Programme aimed at tobacco vendors and changing city by‐laws. |
| Andrews 1984 | Not an RCT |
| Arciti 1986 | Not an RCT |
| Arora 2011 | Not an RCT |
| Aslan 2007 | Not an RCT |
| Ausems 2002 | Follow‐up less than 6 months |
| Aßhauer 1999 | Quasi‐experimental pre‐post design |
| Banerjee 2007 | No smoking outcomes, only behavioural intentions |
| Barrueco 1998 | Not an RCT |
| Beaglehole 1978 | Not an RCT |
| Becker 1992 | Not an RCT |
| Beets 2009 | No assessment of baseline smoking status |
| Benni 2011 | Not an RCT |
| Bergamaschi 2000 | Not an RCT. "Participation in the previous middle school campaign depended solely on the assent of teachers to the proposal of the work group; no other selection or randomization was made." |
| Berman 2011 | Not an RCT |
| Bier 2011a | No smoking outcomes |
| Biglan 1987a | Not an RCT. "In one school district (one middle school, two junior highs, and three high schools), whole schools were assigned to conditions. For the remaining schools, classes of teachers who had agreed to teach the experimental curriculum within each school were randomly assigned to intervention or control conditions.". It is not possible to separate outcomes for the randomly assigned classes. |
| Bloor 2000 | No statement on randomization; 3 month follow‐up |
| Botvin 1989a | RCT; but only 3.5 month follow‐up |
| Botvin 1989b | RCT; but only 4 month follow‐up |
| Botvin 1992 | RCT; but only pre‐test and post‐test measurements |
| Botvin 1997 | Controlled trial, only 3 month follow‐up |
| Botvin 2000 | Data collected only on illicit drugs, not on smoking behaviour |
| Botvin 2003 | RCT; but only post‐test at 3 months |
| Bowen 1991 | Not an RCT. |
| Buhler 2008 | No smoking/tobacco outcomes |
| Burke 1987 | Not an RCT, and no smoking‐related data reported |
| Burke 1992 | Not an RCT; and no smoking related data |
| Calafat 1995 | Programme description; no data on smoking behaviour reported |
| Caldwell 2009 | Not an RCT; < 6 month follow up |
| Calleja 2010 | Follow‐up < 6 months |
| Calman 1985 | Pretest, post‐test study with no follow‐up |
| Charlton 1986 | Controlled trial, not randomized, only 4 month follow‐up |
| Chen 2006 | Not an RCT |
| Connell 1985 | School Health Education Evaluation project: 20,000 children in Grades 4 ‐ 7 in 20 U.S. States, but does not report if the study was randomized; and reports "self‐reported health practices", but within this category tobacco use is not identified. |
| Cote 2006 | Not an RCT |
| Cruz 2009 | Not an RCT |
| Danhua 2005 | Follow‐up < 6 months |
| Davis 1995 | Quasi‐experimental; pretest, 13 week intervention, then post‐test conducted only 3 weeks after the intervention |
| De Jong 1987 | Not an RCT; post‐test only |
| Del Greco 1986 | Not an RCT |
| Dielman 1985 | Not an RCT |
| Donato 1994 | No mention of randomization; "The other 632 students not involved in the programme formed the control group." |
| Dupont 1984 | Only drug use knowledge and attitudes reported, no smoking‐related data, also < 30 participants |
| Elder 1989 | RCT; at baseline intervention 215, control 229, 214 no intervention lottery; at post‐test April 1989 215 intervention, 286 control, 25i lottery, no explanation why control and lottery numbers larger at post‐test; not able to establish non smoking prevalence at baseline (author no longer had data) |
| Emam Hadi 2008 | No smoking/tobacco outcomes |
| Epstein 2000a | Longitudinal survey; no intervention |
| Errecart 1991 | Not an RCT; no smoker/nonsmoker N's, no information on time/duration of intervention or follow‐up |
| Evans 1978 | RCT; but only 10 week follow‐up |
| Evans 1981 | Not an RCT; "junior high schools were assigned to three experimental and four control groups." |
| Flay 1987 | Not an RCT; quasi‐experimental design: "... we selected one or more potential control schools comparable in size, ethnic composition and socioeconomic status."; included in Cochrane review of 'Mass media interventions for preventing smoking in young people' |
| Flay 2004 | No smoking outcomes |
| Flynn 1992 | Not an RCT; 2 pairs of US Standard Metropolitan Statistical Areas not randomized to treatments; included in Cochrane review 'Mass media interventions for preventing smoking in young people' |
| Frydman 1985 | Not an RCT |
| Gilchrist 1987 | Not school intervention |
| Gillies 1984 | Not an RCT |
| Gingiss 2006 | Not an RCT; no smoking prevention intervention or outcomes |
| Gislason 1995 | Not an RCT |
| Gohlke 1989 | Not an RCT |
| Gomez 2009 | Not an RCT |
| Gomez Fraguela 2003 | Not an RCT |
| Gordon 1997 | RCT; but school and community based; 6 month follow‐up, but community interventions introduced throughout that period. |
| Gritz 1992 | 18 ‐ 60 year old females; 18 year olds not separately analysed |
| Guilamo‐Ramos 2010 | 'Towards no Tobacco Use' programme, but intervention is a parent‐based add on. |
| Hamm 1994 | Does not report if the 1320 7th grade students in Omaha, Nebraska, were randomised to the 4 experimental and 3 control groups. At the 12 month follow‐up, more smokers quit in the experimental than the control groups (chi squared 4.70, one‐tailed test, no P value reported), but there were no differences in nonsmokers staying nonsmokers. |
| Hanewinkel 1996 | Not an RCT; quasi‐experimental pre‐test post‐test |
| Hanewinkel 2003 | Not an RCT |
| Hanewinkel 2004 | Not an RCT |
| Hansen 1982 | No statement of randomisation; only 9 week follow‐up |
| Hansen 1988b | On page 96 the authors state that the study has a 'quasi‐experimental design' with schools referred to as being 'assigned', and 'rather than being pure copntrols, they are more appropriately viewed as standard treatment comparison schools'. However, on p. 111 the authors use the words 'random assignment'. |
| Hansen 1996 | Not an RCT; "The study involved the entire eighth grade of the school... All students had received D.A.R.E. in the fifth grade. Four of the eight classes participated in the seventh grade D.A.R.E. booster program... and became a comparison group."; 4 months' follow‐up |
| Hansen 1997 | Not an RCT; students tracked over time by school number only, with low tracking rates between grades. |
| Harmon 1993 | Quasi‐experimental design |
| Harrell 1996 | RCT; but only 8 week follow‐up; smoking rates low at baseline, and no change was reported. |
| Harrell 1998 | RCT; no data reported on smoking behaviour, only on predictors of smoking. |
| Hawkins 2009 | Community based intervention, only recruitment was through schools |
| Hecht 1993 | Not RCT; follow‐up 1 month |
| Hiemstra 2009 | Whilst randomisation is by school, the intervention does not take place in the schools |
| Higgs 2000 | Not an RCT |
| Hinz 2007 | Not an RCT |
| Hodder 2011 | Not an RCT |
| Homel 1981 | Controlled trial, not randomised |
| Hovell 1996 | Not school‐based |
| Hruba 2012 | Not an RCT |
| Hrubá 2007 | Not an RCT |
| Hurd 1980 | Controlled trial, not randomised |
| Ishaq 2004 | Cessation only |
| Jason 1982 | RCT, secondary prevention, no intervention for baseline nonsmokers |
| Johnson 1986 | Controlled trial, not randomised |
| Katz 1989 | RCT; only pre‐ and post‐test |
| Kersch 1998 | Not an RCT; the experimental groups were carefully 'made parallel' on demographic and pedagogical variables, and then compared to a corresponding control population. |
| Killen 1988 | RCT, but only 4 months' follow‐up. |
| Killen 1989 | RCT; but only 2 months' follow‐up |
| Kim 1982 | Not an RCT |
| Kim 1993 | Not an RCT: "6 schools served as the experimental group while two randomly selected schools served as a control group." |
| Knutsen 1991 | RCT; family intervention, but no school intervention |
| Kolpin 2008 | No smoking outcomes |
| Kovach 2010 | No smoking/tobacco outcomes |
| Kröger 2000 | Not an RCT |
| Kupersmidt 2010 | No smoking outcomes |
| Kupersmidt 2012 | No smoking outcomes |
| Lammers 1984 | Quasi‐experimental non‐equivalent pre‐test post‐test design |
| Ledwith 1985 | Controlled trial, not randomised |
| Lee 2007 | Not an RCT |
| Lillington 1984 | Those younger than 18 excluded |
| Litrownik 2000 | Pretest, 8 week intervention, then immediate post‐test |
| Lopez Gonalez 1998 | Not an RCT; no tobacco outcomes (See Ausems 2009 for Dutch arm of the Octopus study) |
| Luepker 1983 | Not an RCT |
| Lwegaba 2005 | Not an RCT |
| MacKinnon 1991 | Not an RCT (the Kansas City part of the Midwestern Prevention Project was not randomised) |
| Malcon 2011 | Follow‐up < 6 months |
| McAlister 1980 | Controlled trial, not randomised |
| McFall 1993 | Participants > 18 years |
| Metz 2006 | Follow‐up < 6 months |
| Moberg 1990 | Not an RCT; control groups not randomised |
| Morehouse 2000 | No smoking outcomes |
| Moskowitz 1984 | Not an RCT: non‐equivalent control group; no smoking‐related data (frequencies or %) reported |
| Murray 1982 | Not an RCT |
| Murray 1984b | Not an RCT |
| Newman 1991 | RCT; no data on children's smoking; data on teachers' acceptance of the 'Smoking and Me' programme. |
| Nichols 2006 | No intervention to prevent starting smoking. No smoking/tobacco outcomes |
| Nilsson 2006 | Not an RCT |
| Nishioka 2005 | Not an RCT |
| Ofstad 2007 | Intervention in hospitals, not schools |
| Olsen 1980 | Not an RCT |
| Parcel 1995 | Not an RCT: the adoption of the Smart Choices intervention programme was made by the school administrators |
| Patrick 2009 | No intervention to prevent starting smoking |
| Pederson 1981a | RCT; but no data on smoking behaviour reported |
| Pederson 1981b | Not an RCT, no Ns reported for smoker/nonsmoker groups, no follow‐up |
| Pederson 1987 | Not an RCT |
| Pentz 1989 | Not an RCT; the MidWestern Prevention Project was a community intervention with a school component. In the Kansas City study schools were not randomly assigned. However, in the Indianapolis study the schools were randomized. Chou 1998 reports effects for baseline substance users only. |
| Perry 1980 | Not an RCT |
| Perry 1990 | Not an RCT |
| Perry 1992 | Minnesota Heart Health Program was quasi‐experimental, and communities were assigned to intervention or control. |
| Perry 1999 | No data on smoking behaviour; only attitudes and intentions |
| Pertusa 2011 | Not a RCT |
| Pfau 1994 | No smoking‐related data reported, only attitudes to smoking |
| Philips 1990 | Study of the intentions of 3 ‐ 6 year olds to protect themselves from adult smoking, with only a 6 week follow‐up; no data on smoking behaviour. |
| Pilgrim 1998 | Not an RCT; no school intervention |
| Piper 1971 | Not an RCT; "we allocated two thirds of them [schools] to the study and one third to the control group." |
| Pomrehn 1995 | Not an RCT: partial cross‐sectional study, with no control group |
| Price 1992 | No data on smoking behaviour; no control group, post‐test or follow‐up |
| Price 1998 | Controlled trial, not randomised; reports no data on smoking behaviour; only knowledge, attitudes and smoking intentions. |
| Primack 2009 | No smoking outcomes |
| Prinz 2000 | No further publications; no results |
| Prokhorov 1994 | Controlled trial, non random. Schools were randomly selected for intervention, but control schools were in a different district. |
| Reimers 1990 | Not an RCT |
| Renaud 2003 | Not an RCT |
| Ringwalt 1991 | RCT; but only pre‐test post‐test design |
| Ringwalt 2009b | Follow‐up not > six months |
| Robinson 1999 | RCT; but no data on smoking behaviour |
| Rohrbach 1993 | No data on smoking behaviour |
| Rohrbach 2010b | Only considering reasons for adopting the TND programme |
| Roncarolo 2008 | Not an RCT |
| Sarvela 1987 | Controlled trial, not randomised |
| Schaps 1986 | No baseline or follow‐up smoking data provided |
| Schinke 1982 | Considered not to be randomised in a meaningful way (two small clusters of 14 each in same school) |
| Schinke 1983 | RCT; only pre‐ and post‐test |
| Schinke 1994 | RCT; but pre‐test post‐test only |
| Schinke 1996 | RCT; but community intervention |
| Schinke 2004 | Students recruited from community agencies not schools |
| Schinke 2005 | No smoking outcomes |
| Scholz 1985 | Not an RCT |
| Secker‐Walker 1997 | Not an RCT |
| Secker‐Walker 1998 | Females < 18 not analysed separately from adults |
| Seid 1994 | RCT; but control group schools were selected from a separate list; only 5 months' follow‐up; 70% attrition at 5 months |
| Shaffer 1983 | Only a 3 month follow‐up. |
| Skinner 1985 | Not an RCT |
| Sorensen 2012 | Not an RCT |
| Spitzzeri 1979 | RCT; only 3 months' follow‐up |
| Steenkamp 1990 | 15 ‐18 year olds not analysed separately from 19 ‐ 64 year olds |
| Stone 1978 | Controlled trial, not randomised; no assessment of smoking behaviour |
| Sussman 2001b | Includes only smokers, without control or comparison group |
| Svoen 1999 | Not an RCT; non‐randomised selection of control group |
| Szymborski 1999 | No data on smoking behaviour; is a description of an anti‐smoking programme for schools |
| Telch 1982 | Not an RCT |
| Tell 1984 | Not an RCT |
| Tessier 2008 | Not an RCT |
| Thompson 2010 | Participants > 18 years |
| Tudor‐Smith 1998 | Quasi‐experimental design |
| Turner 1993 | No data on tobacco use, only on refusals of offers of tobacco immediately after 3 experimental stimuli |
| Van Dyke 2002 | Not an RCT |
| Vartiainen 1998 | Not an RCT |
| Wagner 2006 | No smoking outcomes |
| Wahlgren 1997 | Trial in orthodonists' offices |
| Walsh 2003 | Not smoking, only 'spit tobacco' |
| Webster 2002 | Not an RCT |
| Wenzel 2007 | Not an RCT |
| Werch 1991 | Pre‐test post‐test design |
| Werch 2008 | Follow up less than 6 months |
| Wiist 1991 | Not an RCT |
| Williamson 1981 | Controlled trial, not randomised; no assessment of smoking behaviour |
| Worden 1988 | Not an RCT |
| Worden 1996 | Mass‐media intervention |
| Wu 2003 | RCT; no school component |
| Young 1996 | RCT; but pre‐test post‐test design; and no data on smoking behaviour |
| Zavela 2004 | Not an RCT |
| Zheng 2006 | Not an RCT |
| Zoller 1986 | RCT; but pre‐test, post‐test design with post‐test only 2 weeks after the intervention |
| Zollinger 2003 | Not an RCT |
| Öhrig 2001 | No school intervention, no tobacco outcomes comparing intervention against control |
N = number
Characteristics of ongoing studies [ordered by study ID]
Andrews 2011.
| Trial name or title | 'Click City: tobacco' |
| Methods | Country: USA
Site: 47 elementary schools in Western Oregon (24 intervention schools, 23 control schools) Focus: substance use prevention Design: cluster‐RCT |
| Participants | Baseline: 2322
Age: 5th and 6th graders (age 10 and 11 yrs)
Gender: 50% F Ethnicity: W 78.3%, H 11.1%, A‐A 3.3%, N‐A 3.1%, Asian 4.1% Baseline smoking data: 5% tried smoking |
| Interventions | Category: social influences Programme deliverer: intranet, facilitated by teachers Intervention: 8 sessions in grade 5 (21 activities and 17 components), 2 booster sessions in grade 6 (5 components). Programme covers normative social images, short‐ and long‐term consequences, addiction, lack of control, cravings, difficulty in quitting and finally a commitment. Accompanied by a guide for teachers and newsletter for parents with information and tips. Control: usual school curriculum |
| Outcomes | Smoking status Follow‐up: postintervention and 1 yr after intervention (7th grade) |
| Starting date | 2008 |
| Contact information | Dr Judy Andrews, Oregon Research Institute, 1715 Franklin Blvd, Eugene, OR 97403 judy@ori.org |
| Notes | June 2012: currently undertaking write up for long‐term results |
Bier 2011b.
| Trial name or title | |
| Methods | Country: USA
Site: high risk area middle schools 'Youth Empowerment In Action! Tobacco Education, Advocacy, and Media (YEA!TEAM) Program' Focus: reduce student susceptibility to tobacco initiation Design: not clear |
| Participants | No details |
| Interventions | Category: not clear Programme deliverer: teachers (2‐day courses and ongoing meetings through the year) Intervention: 8 ‐ 16 hrs of lessons; cross‐disciplinary academic curriculum. Teaches how to identify and process tobacco media messages; understand political, social and economic implications; engage in community outreach activities and how to be advocate for tobacco control. Also seeks to develop number of cognitive skills. Control: no information |
| Outcomes | No details |
| Starting date | Between 2006 and 2009 |
| Contact information | Centre for Character & Citzenship, University of Missouri‐St Louis, USA ccc@umsl.edu |
| Notes | Study adherence: more than 90% |
Cremers 2012.
| Trial name or title | |
| Methods | Country: Netherlands
Site: 175 primary schools 'Fun without smokes' Focus: smoking prevention Design: cluster‐RCT Dutch Trial Register NTR3116 |
| Participants | Age: age 10 to 13 yrs |
| Interventions | Category: social competence vs. control Programme deliverer: web Intervention: web‐based intervention; plus personalised letters. Information on website about non‐smoking, short movies about consequences of smoking, games and questions and answers.
Control: no information |
| Outcomes | Self report; 'ever smoking'; plus assessment of smoking frequency. Follow‐up: 1 yr, 2 yrs |
| Starting date | October 2011 |
| Contact information | p.cremers@maastrichtuniversity.nl |
| Notes | Randomisation by computer‐determined sequence Was a power computation performed? Yes. "We used the OD (Optimal Design) method of Raudenbush with a two sided significance level of 0.05, a target power of 0.80 and an ICC of 0.04 (based on the study of Ausems et al.) to calculate the sample size." Statistical analysis: Multilevel logistic regression analyses Full details of study yet to be released; randomisation and questionnaires in school; but intervention described as 'out of school'. Clarification will be needed to determine inclusion within future review updates. |
Evers 2012.
| Trial name or title | |
| Methods | Country: USA
Site: 22 middle and junior high schools Focus: cessation and prevention of alcohol, tobacco, marijuana and other drug use Design: cluster‐RCT |
| Participants | Age: grades 6 to 9
Gender: 47.4% F Ethnicity: W 76.3%, H 11.8%, A‐A 10.4% Baseline smoking data: 26.2% tried tobacco |
| Interventions | Not stated for prevention |
| Outcomes | Smoking status Follow‐up: postintervention and 1 yr after intervention (7th grade) |
| Starting date | Not stated |
| Contact information | Dr Kerry Evers, Pro‐Change Behavior Systems Inc Kevers@prochange.com |
| Notes | Current publication only considers cessation. Awaiting further publication of prevention data. |
Kirshnan‐Sarin 2012.
| Trial name or title | |
| Methods | Country: USA
Site: High schools Focus: smoking prevention Design: cluster‐RCT |
| Participants | Baseline: 1651 Age: 13 yrs and older |
| Interventions | Category: unclear Intervention: incentive‐based intervention; participants pledge to remain smoke‐free. Control: not stated |
| Outcomes | Changes in tobacco us rates |
| Starting date | 7 January 2010 |
| Contact information | suchitra.krishnan‐sarin@yale.edu |
| Notes | Final data collection date: May 2011 Limited information on study design and intervention details |
O'Leary‐Barrett 2011.
| Trial name or title | |
| Methods | Country: UK (London)
Site: 20 secondary schools Focus: drinking and illicit drug use prevention (not clear whether smoking prevention is included) |
| Participants | Enrollment 3190 Age: 13 ‐ 16 yr‐olds |
| Interventions | Delivery by educational professionals Personality‐targeted interventions (cognitive behavioural) |
| Outcomes | Follow‐up: 6‐month intervals for 2 yrs |
| Starting date | May 2007 |
| Contact information | Dr. Patricia Conrod, Institute of Psychiatry, King's College London patricia.conrod@kcl.ac.uk |
| Notes | Completion date: March 2010 |
Differences between protocol and review
No subgroup analyses were completed for age or longer versus shorter durations of programme: Intervention programmes that developed interventions for specific age groups were not analysed because of the difficulties of categorising studies within predefined age thresholds. This analysis would have been conducted within the Pure Prevention cohorts (Group 1) which had no heterogeneity. Programme intensity was also difficult to define: high number of short sessions compared to few long sessions and then how to categorise the variety of intervention programme designs consistently within these categories.
Addition of Risk of Bias tables in this review update: During the review process it became clear that several trials did not fit the five intervention categories used in the first and second editions of this review. The Amendment to the Protocol adds a sixth category 'Other Interventions'. Six different subtypes of interventions were noted as appropriate to this group: 1. Creating school anti‐smoking activities (Brown 2002; Johnson 2009); 2. Conversations with peers when they are smoking (Campbell 2008); 3. Discussion of motivations for smoking, role of mass media, comparison of students’ respiratory indices with spirometers (Figa‐Talamanca 1989 (F)); 4. Good Behaviour rewarded in classroom, compared to Reading Skills Intervention (Kellam 1998 (GBG); 5. Sports consultations linking sports with substance non‐use (Werch 2005); 6. Assessing readiness to change smoking intentions and encouraging change using a web site (Norman 2008).
Contributions of authors
RT conceived the review and wrote the first edition (2002), with Dr. Keith Busby as a co‐author. For the first update, RP became co‐author. RT and RP both extracted data. RT wrote the updated review, and RP provided statistical support and meta‐analyses. For the current review JM became a co‐author and both RT and JM extracted data; RP continued to provide statistical support and meta‐analyses, RT and JM wrote the text.
Sources of support
Internal sources
No sources of support supplied
External sources
National Institute for Health Research (NIHR), UK.
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Abernathy 1992 {published data only}
- Abernathy TJ, Bertrand LD. Preventing cigarette smoking among children: Results of a four‐year evaluation of the PAL program. Canadian Journal of Public Health 1992;83:226‐9. [MEDLINE: ] [PubMed] [Google Scholar]
- Bertrand L, Abernathy TJ. Predicting smoking among adolescents using cross‐sectional and longitudinal approaches. Journal of School Health 1993;63:100‐5. [DOI] [PubMed] [Google Scholar]
Armstrong 1990 (Peer) {published data only}
- Armstrong BK, Klerk NH, Shean RE, Dunn DA, Dolin PJ. Influence of education and advertising on the uptake of smoking by children. Medical Journal of Australia 1990;152:117‐24. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Fisher DA, Armstrong BK, Klerk NH. A randomised‐controlled trial of education for prevention of smoking in 12 year old children. Proceedings of the 5th World Conference on Smoking and Health, Winnipeg, Canada 1983. Ottawa: Canadian Council on Smoking and Health, 1985. [Google Scholar]
- Shean RE, Klerk NH, Armstrong BK, Walker NR. Seven‐year follow‐up a smoking‐prevention program for children. Australian Journal of Public Health 1994;18:205‐8. [DOI] [PubMed] [Google Scholar]
Armstrong 1990 (Teacher) {published data only}
Ary 1990 {published data only}
- Ary DV, Biglan A, Glasgow R, Zoref L, Black C, Ochs L, et al. The efficacy of social‐influence prevention programs versus "standard care": Are new initiatives needed?. Journal of Behavioral Medicine 1990;13(3):281‐96. [DOI] [PubMed] [Google Scholar]
Ausems 2004 (Combined) {published data only}
Ausems 2004 (In school) {published data only}
- Ausems M, Mesters I, Breukelen G, Vries H. Effects of in‐school and tailored out‐of‐school smoking prevention among Dutch vocational school students. Health Education Research 2004;19(1):51‐63. [DOI] [PubMed] [Google Scholar]
Ausems 2004 (Out School) {published data only}
Aveyard 1999 {published data only}
- Aveyard P, Cheng KK, Almond J, Sherratt E, Lancashire R, Lawrence T, et al. Cluster randomised controlled trial of expert system based on the transtheoretical (''stages of change'') model for smoking prevention and cessation in schools. BMJ 1999;319:948‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aveyard P, Markham WA, Almond J, Lancashire E, Cheng KK. The risk of smoking in relation to engagement with a school‐based smoking intervention. Social Science & Medicine 2003;56:869‐82. [DOI] [PubMed] [Google Scholar]
- Aveyard P, Sherratt E, Almond J, Lawrence T, Lancashire R, Griffin C, Cheng KK. The change‐in‐stage and updated smoking status results from a cluster‐randomised trial of smoking prevention and cessation using the transtheoretical model among British adolescents. Preventive Medicine 2001;33:313‐324. [DOI] [PubMed] [Google Scholar]
Biglan 1987b {published data only}
- Biglan A, Severson H, Ary D, Faller C, Gallison C, Thompson R, et al. Do smoking prevention programs really work? Attrition and the internal and external validity of an evaluation of a refusal skills training program. Journal of Behavioral Medicine 1987;10:159‐71. [DOI] [PubMed] [Google Scholar]
- Hops H, Weissman W, Biglan A, Thompson R, Faller C, Severson HH. A taped situation test of cigarette refusal skills among adolescents. Behavioral Assessment 1986;8:145‐54. [Google Scholar]
Biglan 2000 {published data only}
- Biglan A, Ary DV, Smolkowski K, Duncan T, Black C. A randomised controlled trial of a community intervention to prevent adolescent tobacco use.. Tobacco Control 2000;9:24‐32. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biglan A, Ary DV, Yudelson H, Duncan TE, Hood D, James L, et al. Experimental evaluation of a modular approach to mobilizing anti tobacco influences of peers and parents. American Journal of Community Psychology 1996;24(3):311‐39. [DOI] [PubMed] [Google Scholar]
Botvin 1980 {published data only}
- Botvin GJ, Eng A. A comprehensive school‐based smoking prevention program. Journal of School Health 1980;50:209‐13. [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Eng A, Williams C. Preventing the onset of cigarette smoking through life skills training. Prev Med 1980;9:135‐43. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Botvin 1982 {published data only}
- Botvin GJ, Eng A. The efficacy of a multi component approach to the prevention of cigarette smoking. Preventive Medicine 1982;11:199‐211. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Botvin 1983 (Intensive) {published data only}
Botvin 1983 (LST) {published data only}
- Botvin GJ, Renick NL, Baker E. The effects of scheduling format and booster sessions on a broad‐spectrum psychosocial approach to smoking prevention. Journal of Behavioral Medicine 1983;6:359‐79. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Botvin 1990a (Video) {published data only}
Botvin 1990a (Workshop) {published data only}
- Botvin GJ, Baker E, Dusenbury L, Botvin EM, Diaz T. Long‐term follow‐up results of a randomised drug abuse prevention trial in a white middle‐class population. JAMA 1995;273:1106‐12. [PubMed] [Google Scholar]
- Botvin GJ, Baker E, Dusenbury L, Tortu S, Botvin EM. Preventing adolescent drug abuse through a multimodal cognitive‐behavioral approach: Results of a 3‐year study. Journal of Consulting and Clinical Psychology 1990;58(4):437‐46. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Tortu S, Baker E, Dusenbury L. Preventing adolescent cigarette smoking: Resistance skills training and development of life skills. Special Services in the Schools 1990;6:37‐61. [Google Scholar]
- Nichols TR, Graber JA, Brooks‐Gunn J, Botvin GJ. Ways to say no: refusal skill strategies among urban adolescents. American Journal of Health Behavior 2006;30(3):227‐36. [DOI] [PubMed] [Google Scholar]
- Scheier LM, Botvin GJ, Griffin KW. Preventive intervention effects on developmental progression in drug use: Structural equation modeling using longitudinal data. Prevention Science 2001;2(2):91‐112. [DOI] [PubMed] [Google Scholar]
Botvin 1990b {published data only}
- Botvin GJ, Baker E, Filazzola AD, Botvin EM. A cognitive‐behavioral approach to substance abuse prevention: One‐year follow‐up. Addictive Behaviors 1990;15:47‐63. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Baker E, Renick NL, Filazzola AD, Botvin EM. A cognitive‐behavioral approach to substance‐abuse prevention. Addictive Behaviors 1984;9:137‐47. [DOI] [PubMed] [Google Scholar]
- Donaldson SI, Graham JW, Piccinin AM, Hansen WB. Resistance‐skills training and onset of alcohol use: Evidence of beneficial and potentially harmful effects in public schools and private Catholic schools. Health Psychology 1995;14(4):291‐300. [DOI] [PubMed] [Google Scholar]
Botvin 1999 {published data only}
- Botvin GJ, Griffin KW, Diaz T, Miller N, Ifill‐Williams M. Smoking initiation and escalation in early adolescent girls: one‐year follow‐up of a school‐based prevention intervention for minority youth. Journal of the American Medical Women's Association 1999;54:139‐43, 152. [PubMed] [Google Scholar]
Botvin 2001 {published data only}
- Botvin GJ, Griffin KW, Diaz T, Ifill‐Wiliams M. Drug abuse prevention among minority adolescents: Posttest and one‐year follow‐up of a school‐based preventive intervention. Prevention Science 2001;2(1):1‐13. [DOI] [PubMed] [Google Scholar]
- Griffin KW, Botvin GJ, Nichols TR, Doyle MM. Effectiveness of a universal drug abuse prevention approach for youth at high risk for substance use initiation. Preventive Medicine 2003;36(1):1‐7. [DOI] [PubMed] [Google Scholar]
Brown 2002 {published data only}
- Brown KS, Cameron R, Madill C, Payne ME, Filsinger S, Manske SR, Best JA. Outcome evaluation of a high school smoking reduction intervention based on extracurricular activities. Preventive Medicine 2002;35(5):506‐10. [DOI] [PubMed] [Google Scholar]
Brown 2005 {published data only}
- Brown EC, Catalano RF, Fleming CB, Haggerty KP, Abbott RD. Adolescent substance use outcomes in the Raising Healthy Children Project: A two‐part latent growth curve analysis. Journal of Consulting and Clinical Psychology 2005;73(4):699‐710. [DOI] [PubMed] [Google Scholar]
Buller 2008 (Australia) {published data only}
- Buller DB, Borland R, Woodall WG, Hall JR, Hines JM, Burris‐Woodall P, et al. Randomized trials on consider this, a tailored, internet‐delivered smoking prevention program for adolescents. Health Education & Behavior 2008;35(2):260‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Buller 2008 (USA) {published data only}
Bush 1989 {published data only}
- Bush PJ, Zuckerman AE, Theiss PK, Taggart VS, Horowitz C, Sheridan MJ, et al. Cardiovascular risk factor prevention in black schoolchildren: Two‐year results of the "Know Your Body" Program. American Journal of Epidemiology 1989;129:466‐82. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Byrne 2005 {published data only}
- Byrne DG, Mazanov J. Prevention of adolescent smoking: a prospective test of three models of intervention. Journal of Substance Use 2005;10(6):363‐74. [Google Scholar]
Cameron 1999 {published data only}
- Cameron R, Brown KS, Best JA, Pelkman CL, Madill CL, Manske SR, et al. Effectiveness of a social influences smoking prevention program as a function of provider type, training method, and school risk. American Journal of Public Health 1999;89:1827‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santi SM, Best JA, Payne ME, Brown KS, Cameron R. A comparison between instructional experience and performance of teachers and nurses delivering a smoking prevention program. Canadian Journal of Public Health 1992;83:433‐6. [PubMed] [Google Scholar]
- Santi SM, Cargo M, Brown KS, Best JA, Cameron R. Dispositional risk factors for smoking‐stage transitions: A social influences program as an effect modifier. Addictive Behaviors 1994;19(3):269‐85. [DOI] [PubMed] [Google Scholar]
- Sashegyi AI, Brown KS, Farrell PJ. Application of a generalized random effects regression model for cluster‐correlated longitudinal data to a school‐based smoking prevention trial. American Journal of Epidemiology 2000;152(12):1192‐200. [DOI] [PubMed] [Google Scholar]
Campbell 2008 {published data only}
- Audrey S, Cordall K, Moore L, Cohen D, Campbell R. The development and implementation of a peer‐led intervention to prevent smoking among secondary school students using their established social networks. Health Education Journal 2004;63:266‐84. [Google Scholar]
- Audrey S, Holliday J, Campbell R. Commitment and compatibility: Teachers' perspectives on the implementation of an effective school‐based, peer‐led smoking intervention. Health Education Journal 2008;67(2):74‐90. [Google Scholar]
- Campbell R, Starkey F, Holliday J, Audrey S, Bloor M, Parry‐Langdon N, et al. An informal school‐based peer‐led intervention for smoking prevention in adolescence (ASSIST): a cluster randomised trial.[see comment]. Lancet 2008;371(9624):1595‐602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holliday J, Audrey S, Moore L, Parry‐Langdon N, Campbell R. High fidelity? How should we consider variations in the delivery of school‐based health promotion interventions?. Health Education Journal 2009;68:44‐62. [Google Scholar]
- Hollingworth W, Cohen D, Hawkins J, Hughes RA, Moore LAR, Holliday JC, et al. Reducing smoking in adolescents: Cost‐effectiveness results from the cluster randomized ASSIST (A Stop Smoking In Schools Trial). Nicotine & Tobacco Research 2012;14(2):161‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mermelstein R. Moving tobacco prevention outside the classroom. Lancet 2008;371(9624):1556‐7. [DOI] [PubMed] [Google Scholar]
- Starkey F, Audrey S, Holliday J, Moore L, Campbell R. Identifying influential young people to undertake effective peer‐led health promotion: the example of A Stop Smoking In Schools Trial (ASSIST). Health Education Research 2009;24(6):977‐88. [DOI] [PubMed] [Google Scholar]
- Starkey F, Holliday J, Audrey S, Campbell R. Identifying influential young people for peer education: the case study of a stop smoking in schools trial, England and Wales, 2001‐2005. European Journal of Public Health 2005;15:72‐3. [Google Scholar]
- Starkey F, Moore L, Campbell R, Sidaway M, Bloor M. Correction: rationale, design and conduct of a comprehensive evaluation of a school‐based peer‐led anti‐smoking intervention in the UK: the ASSIST cluster randomised trial. BMC Public Health 2007;7:301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starkey F, Moore L, Campbell R, Sidaway M, Bloor M. Rationale, design and conduct of a comprehensive evaluation of a school‐based peer‐led anti‐smoking intervention in the UK: the ASSIST cluster randomised trial [ISRCTN55572965]. BMC Public Health 2005;5(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varun N. A novel approach to preventing adolescent smoking in schools. Thorax 2008;63(10):882. [Google Scholar]
Chatrou 1999 {published data only}
- Chatrou M, Maes S, Dusseldorp E, Seegers G. Effects of the Brabant smoking prevention programme: A replication of the Wisconsin programme. Psychology and Health 1999;14:159‐78. [Google Scholar]
- Leventhal H, Fleming R, Glynn K. A cognitive‐development approach to smoking intervention. In: Maes S, Spielberger CD, Defares PB, Sarason IG editor(s). Topics in health psychology. New York: John Wiley, 1988:79‐105. [Google Scholar]
Chou 2006 {published data only}
- Chen X, Li Y, Unger JB, Gong J, Johnson CA, Gun Q. Hazard of smoking initiation among adolescents in Wuhan, China. Preventive Medicine 2001;32:437‐45. [DOI] [PubMed] [Google Scholar]
- Chou CP, Li Y, Unger JB, Xia J, Sun P, Guo Q, et al. A randomised intervention of smoking for adolescents in urban Wuhan, China [see comment]. Preventive Medicine 2006;42(4):280‐5. [DOI] [PubMed] [Google Scholar]
- Sakuma KK, Sun P, Unger J, Johnson CA. Evaluating depressive symptom Interactions on adolescent smoking prevention program mediators: A mediated moderation analysis. Nicotine & Tobacco Research 2010;12(11):1099‐107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun P, Unger JB, Guo Q, Gong J, Ma H, Palmer PH, et al. Comorbidity between depression and smoking moderates the effect of a smoking prevention program among boys in China. Nicotine & Tobacco Research 2007;9(Suppl. 4):599‐609. [DOI] [PubMed] [Google Scholar]
- Unger J, Yan L, Chen X, Jiang X, Azen S, Qian G, et al. Adolescent smoking in Wuhan, China: Baseline data from the Wuhan Smoking Prevention Trial. American Journal of Preventive Medicine 2001;21(3):162‐9. [DOI] [PubMed] [Google Scholar]
Clark 2010 {published data only}
- Clark HK, Ringwalt CL, Hanley S, Shamblen SR, Flewelling RL, Hano MC. Project SUCCESS' effects on the substance use of alternative high school students. Addictive Behaviors 2010;35:209‐17. [DOI] [PubMed] [Google Scholar]
- Clark HK, Ringwalt CL, Shamblen SR, Hanley SM. Project success' effects on substance use‐related attitudes and behaviours: a randomised controlled trial in alternative high schools. Journal of Drug Education 2011;41(1):17‐44. [DOI] [PubMed] [Google Scholar]
Clarke 1986 {published data only}
- Clarke JH, MacPherson B, Holmes DR, Jones R. Reducing adolescent smoking: A comparison of peer‐led, teacher‐led, and expert interventions. Journal of School Health 1986;56(3):102‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Clayton 1996 {published data only}
- Bennett GT. An Exploration of Patterns of Drug Use and of the Effectiveness of a Substance Abuse Prevention Program According to Adolescents' Level of Academic Achievement. University of Kentucky Ph.D. Dissertation DAI‐A 55/10; April 1995:3091.
- Clayton RR, Cattarello AM, Johnstone BM. The effectiveness of Drug Abuse Resistance Education (Project DARE): 5‐year follow‐up results. Preventive Medicine 1996;25:307‐18. [DOI] [PubMed] [Google Scholar]
- Cleckler PEJ. An Evaluation of an Educational Substance Abuse Prevention Program. EDD Dissertation University of Georgia. University of Georgia. DA‐A 52/06 p. 1956, 1991. [Google Scholar]
- Lynam DR, Milich R, Zimmerman R, Novak SP, Logan TK, Martin C, et al. Project DARE: no effects at 10‐year follow‐up. Journal of Consulting and Clinical Psychology 1999;67:590‐3. [DOI] [PubMed] [Google Scholar]
- Wysong E, Wright DW. A decade of DARE: efficacy, politics and drug education. Sociological Focus 1995;28(3):283‐311. [Google Scholar]
Coe 1982 {published data only}
- Coe RM, Crouse E, Cohen JD, Fisher Jr EB. Patterns of change in adolescent smoking behavior and results of a one year follow‐up of a smoking prevention program. Journal of School Health 1982;August:348‐53. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Cohen 1989 {published data only}
- Cohen RY, Felix MR, Brownell KD. The role of parents and older peers in school‐based cardiovascular prevention programs: implications for program development. Health Education Quarterly 1989;16:245‐53. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Connell 2007 {published data only}
- Connell AM. Employing compiler average causal effect analytic methods to examine effects of randomised encouragement trials. American Journal of Drug & Alcohol Abuse 2009;35(4):253‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell AM, Dishion TJ, Yasui M, Kavanagh K. An adaptive approach to family intervention: linking engagement in family centred intervention to reductions in adolescent problem behavior. Journal of Consulting and Clinical Psychology 2007;75(4):568‐79. [DOI] [PubMed] [Google Scholar]
Conner 2010 (I) {published data only}
- Connor M, Higgins AR. Long‐term effects of implementation intentions on prevention of smoking uptake among adolescents: a cluster randomised controlled trial. Health Psychology 2010;29(5):529‐38. [DOI] [PubMed] [Google Scholar]
Conner 2010 (SE) {published data only}
Crone 2003 {published data only}
- Crone MR, Reijneveld SA, Willemsen MC, Leerdam FJ, Spruijt RD, Sing RA. Prevention of smoking in adolescents with lower education: a school based intervention study. Journal of Epidemiology and Community Health 2003;57(9):675‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Crone 2011 {published data only}
- Crone MR, Spruijt R, Dijkstra NS, Willemsen MC, Paulussen TG. Does a smoking prevention program in elementary schools prepare children for secondary school?. Preventive Medicine 2011;52(1):53‐9. [DOI] [PubMed] [Google Scholar]
Denson 1981 {published and unpublished data}
- Denson R, Stretch S. Prevention of smoking in elementary schools. Canadian Journal of Public Health 1981;72:259‐63. [PubMed] [Google Scholar]
De Vries 1994 (High) {published data only}
De Vries 1994 (Voc) {published data only}
- Vries H, Backbier E, Dijkstra M, Breukelen G, Parcel G, Kok G. A Dutch social influence smoking prevention approach for vocational school students. Health Education Research 1994;9:365‐74. [Google Scholar]
- Vries H, Dijkstra M, Kok G. A Dutch Smoking Prevention Project: An overview. Hygie 1992;11:14‐8. [PubMed] [Google Scholar]
- Vries H, Weijts W, Dijkstra M, Kok G. The utilization of qualitative and quantitative data for health education program planning, implementation, and evaluation: A spiral approach. Health Education Quarterly 1992;19:101‐15. [DOI] [PubMed] [Google Scholar]
De Vries 2003 (Denmark) {published data only}
De Vries 2003 (Finland) {published data only}
- Ariza C, Nebot M, Tomas Z, Gimenez E, Valmayor S, Tarilonte V, et al. Longitudinal effects of the European smoking prevention framework approach (ESFA) project in Spanish adolescents. European Journal of Public Health 2008;18(5):491‐7. [DOI] [PubMed] [Google Scholar]
- Vries H, Dijk F, Wetsels J, Mudde A, Kremers S, Ariza C, et al. The European Smoking Prevention Framework Approach (ESFA): effects after 24 and 30 months. Health Education Research 2006;21(1):116‐32. [DOI] [PubMed] [Google Scholar]
- Vries H, Mudde A, Kremers S, Wetzels J, Uiters E, Ariza C, et al. The European Smoking Prevention Framework Approach (ESFA): short‐term effects. Health Education Research 2003;18(6):649‐63. [DOI] [PubMed] [Google Scholar]
- Vries H, Mudde A, Leijs I, Charlton A, Vartiainen E, Buijs G, et al. The European Smoking Prevention Framework Approach (EFSA): an example of integral prevention. Health Education Research 2003;18(5):611‐26. [DOI] [PubMed] [Google Scholar]
- Haukkala A, Vartianen E, Vries H. Progression of oral snuff use among Finnish 13‐16 year old students and its relation to smoking behavior. Addiction 2006;101(4):581‐9. [DOI] [PubMed] [Google Scholar]
- Mercken L, Candel M, Willems P, Vries H. Social influence and selection effects in the context of smoking behavior. Changes during early and mid adolescence. Health Psychology 2009;28(1):73‐82. [DOI] [PubMed] [Google Scholar]
- Vartianen E, Pennanen M, Haukkala A, Dijk F, Lehtovuori R, Vries H. The effects of a three‐year smoking prevention programme in secondary schools in Helsinki. European Journal of Public Health 2007;17(3):249‐56. [DOI] [PubMed] [Google Scholar]
De Vries 2003 (Portugal) {published data only}
De Vries 2003 (UK) {published data only}
Dijkstra 1999 (DM + B) {published data only}
Dijkstra 1999 (DM + no B) {published data only}
Dijkstra 1999 (SI + B) {published data only}
Dijkstra 1999 (SI + no B) {published data only}
- Dijkstra M, Mesters I, Devries H, Breukelen G, Parcel GS. Effectiveness of a social influence approach and boosters to smoking prevention. Health Education Research 1999;14:791‐802. [DOI] [PubMed] [Google Scholar]
Eisen 2003 {published data only}
- Eisen M. Intermediate outcomes from a life skills education program with a media literacy component. In: Crano WD, Burgoon M editor(s). Mass Media and Drug Prevention. Lawrence Erlbaum Associates Inc., 2002:187‐212. [Google Scholar]
- Eisen M, Zellman GL, Massett HA, Murray DM. Evaluating the Lions‐Quest "Skills for Adolescence" drug education program: First‐year behavior outcomes. Addictive Behaviors 2002;27:619‐32. [DOI] [PubMed] [Google Scholar]
- Eisen M, Zellman GL, Murray DM. Evaluating the Lions‐Quest "Skills for Adolescence" drug education program: Second‐year behavior outcomes. Addictive Behaviors 2003;28:883‐97. [DOI] [PubMed] [Google Scholar]
- Sprunger B, Pellaux D. Skills for adolescence: experience with the International Lions‐Quest program. Crisis: Journal of Crisis Intervention & Suicide 1989;10(1):88‐104. [PubMed] [Google Scholar]
Elder 1993 {published data only}
- Eckhardt L, Woodruff SI, Elder JP. Relative effectiveness of continued, lapsed, and delayed smoking prevention intervention in senior high school students. American Journal of Health Promotion 1997;11:418‐21. [DOI] [PubMed] [Google Scholar]
- Elder JP, Sallis JF, Woodruff SI, Wildey MR. Tobacco‐refusal skills and tobacco use among high‐risk adolescents. Journal of Behavioral Medicine 1993;16:629‐41. [DOI] [PubMed] [Google Scholar]
- Elder JP, Wildey M, Moor C, Sallis Jr JF, Eckhardt L, et al. The long‐term prevention of tobacco use among junior high school students: Classroom and telephone interventions. American Journal of Public Health 1993;83:1239‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder JP, Woodruff SI, Eckhardt L. Participation in a telephone‐based tobacco use prevention program for adolescents. American Journal of Health Promotion 1994;9(2):92‐5. [DOI] [PubMed] [Google Scholar]
- Elder JP, Woodruff SI, Sallis JF, Moor C, Edwards C, Wildey MB. Effects of health facilitator performance and attendance at training sessions on the acquisition of tobacco refusal skills among multi‐ethnic, high‐risk adolescents. Health Education Research 1994;9(2):225‐33. [DOI] [PubMed] [Google Scholar]
- Young RL, Elder JP, Green MS, Moor C, Wildey MB. Tobacco use prevention and health facilitator effectiveness. Journal of Sch Health 1988;58(9):370‐3. [DOI] [PubMed] [Google Scholar]
Elder 1996 {published data only}
- Edmundson E, Parcel GS, Perry CL, Feldman HA, Smyth M, Johnson CC, et al. The effects of the child and adolescent trial for cardiovascular health intervention on psychosocial determinants of cardiovascular disease risk behavior among third‐grade students. American Journal of Health Promotion 1996;10(3):217‐25. [DOI] [PubMed] [Google Scholar]
- Elder JP, McGraw SA, Stone EJ, Reed DB, Harsha DW, Greene T, et al. CATCH: Process evaluation of environmental factors and programs. Health Education Quarterly 1994;Supplement 2:S107‐S127. [DOI] [PubMed] [Google Scholar]
- Elder JP, Perry CL, Stone EJ, Johnson CC, Yang M, Edmundson EW, et al. Tobacco use measurement, prediction and intervention in elementary schools in four states: The CATCH Study. Preventive Medicine 1996;25:486‐94. [DOI] [PubMed] [Google Scholar]
- Johnson CC, Li D, Galati T, Pedersen S, Smth M, Parcel GS. Maintenance of the Classroom Health Education Curricula: Results from the CATCH‐ON study. Health Education & Behavior 2003;30(4):476‐88. [DOI] [PubMed] [Google Scholar]
- Johnson CC, Li D, Perry CL, Elder JP, Feldman HA, Kelder SH, et al. Fifth through eighth grade longitudinal predictors of tobacco use among a racially diverse cohort CATCH. Journal of School Health 2002;72(2):58‐64. [DOI] [PubMed] [Google Scholar]
- Johnson CC, Osganian SK, Budman SB, Lytle LA, Barrera EP, Bonura SR, et al. CATCH: Family process evaluation in a multicenter trial. Health Education Quarterly 1994;Supplement 2:S91‐S106. [DOI] [PubMed] [Google Scholar]
- Nader PR, Sellers DE, Johnson CC, Perry CL, Stone EJ, Cook KC, et al. The effect of adult participation in a school‐based family intervention to improve children's diet and physical activity: The Child and Adolescent Trial for Cardiovascular Health. Preventive Medicine 1996;25:455‐64. [DOI] [PubMed] [Google Scholar]
- Perry CL, Sellers DE, Johnson C, Pedersen S, Bachman KJ, Parcel GS, et al. The Child and Adolescent Trial for Cardiovascular Health (CATCH): Intervention, implementation, and feasibility for elementary schools in the United States.. Health Education & Behavior 1997;24(6):716‐35. [DOI] [PubMed] [Google Scholar]
- Perry CL, Stone EJ, Parcel GS, Ellison RC, Nader PR, Webber LS, et al. School‐based cardiovascular health promotion: The Child and Adolescent Trial for Cardiovascular Health (CATCH). Journal of School Health 1990;60(3):406‐13. [DOI] [PubMed] [Google Scholar]
- Stone EJ, Osganian SK, McKinlay SM, Wu MC, Webber LS, Luepker RV, et al. Operational design and quality control in the CATCH multicenter trial. Preventive Medicine 1996;25:384‐99. [DOI] [PubMed] [Google Scholar]
Ellickson 1990 (HealthEd) {published data only}
- Bell RM, Ellickson PL, Harrison ER. Do drug prevention effects persist into high school? How Project ALERT did with ninth graders. Preventive Medicine 1993;22:463‐83. [DOI] [PubMed] [Google Scholar]
- Ellickson PL, Bell RM. Drug prevention in Junior High: A multi‐site longitudinal test. Science 1990 16 March;247:1299‐1305. [DOI] [PubMed] [Google Scholar]
- Ellickson PL, Bell RM, Harrison ER. Changing adolescent propensities to use drugs: results from Project ALERT. Health Education Quarterly 1993;20:227‐42. [DOI] [PubMed] [Google Scholar]
- Ellickson PL, Bell RM, McGuigan K. Preventing adolescent drug use: long‐term results of a Junior High program. American Journal of Public Health 1993;83(6):856‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orlando M, Tucker JS, Ellickson PL, Klein DJ. Developmental trajectories of cigarette smoking and their correlates from early adolescence to young adulthood. Journal of Consulting and Clincial Psychology 2004;72(3):400‐10. [DOI] [PubMed] [Google Scholar]
- Tucker JS, Ellickson PL, Klein DJ. Predictors of the transition to regular smoking during adolescence and young adulthood. Journal of Adolescent Health 2003;32:314‐24. [DOI] [PubMed] [Google Scholar]
- Tucker JS, Martinez JF, Ellickson PL, Edelen MO. Temporal Associations of cigarette smoking with social influences, academic performance, and delinquency: a four‐wave longitudinal study from ages 13 to 23. Psychology of addictive Behaviors 2008;22(1):1‐11. [DOI] [PubMed] [Google Scholar]
Ellickson 1990 (Teen) {published data only}
Ellickson 2003 {published data only}
- Ellickson PL, McCaffrey DF, Ghosh Dastidar B, Longshore DL. New inroads in preventing adolescent drug use: results from a large‐scale trial of Project ALERT in middle schools. American Journal of Public Health 2003;93(11):1830‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh‐Dastidar B, Longshore DL, Ellickson PL, McCaffrey DF. Modifying pro‐drug risk factors in adolescents: results from Project ALERT. Health Education & Behavior 2004;31:318‐34. [DOI] [PubMed] [Google Scholar]
- Orlando M, Ellickson PL, McCaffrey DF, Longshore DL. Mediation analysis of a school‐based drug prevention program: effects of Project ALERT. Prevention Science 2005;6(1):35‐46. [DOI] [PubMed] [Google Scholar]
Ennett 1994 {published data only}
- Ennett ST, Rosenbaum DP, Flewelling RL, Bieler GS, Ringwalt CL, Bailey SL. Long‐term evaluation of Drug Abuse Resistance Education. Addictive Behaviors 1994;19:113‐25. [DOI] [PubMed] [Google Scholar]
- Ennett ST, Tobler NS, Ringwalt CL, Flewelling RL. How effective is Drug Abuse Resistance Education? A meta‐analysis of Project DARE outcome evaluations. American Journal of Public Health 1994;84(9):1394‐1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum DP, Flewelling RL, Bailey SL, Ringwalt CL, Wilkinson DL. Cops in the classroom: A longitudinal evaluation of Drug Abuse Resistance Education (DARE). Journal of Research in Crime and Delinquency 1994;31(1):3‐31. [Google Scholar]
Faggiano 2008 {published data only}
- Faggiano F, Galanti MR, Bohrn K, Burkhart G, Vigna‐Taglianti F, Cuomo L, et al. The effectiveness of a school‐based substance abuse prevention program: EU‐Dap cluster randomised controlled trial. Preventive Medicine 2008;47(5):537‐43. [DOI] [PubMed] [Google Scholar]
- Faggiano F, Richardson C, Bohrn K, Galanti MR, EU‐Dap Study Group. A cluster randomised controlled trial of school‐based prevention of tobacco, alcohol and drug use: the EU‐Dap design and study population. Preventive Medicine 2007;44(2):170‐3. [DOI] [PubMed] [Google Scholar]
- Faggiano F, Vigna‐Taglianti F, Burkhart G, Bohrn K, Cuomo L, Gregori D, et al. The effectiveness of a school‐based substance abuse prevention program: 18‐month follow‐up of the EU‐Dap cluster randomised controlled trial. Drug & Alcohol Dependence 2010;108(1‐2):56‐64. [DOI] [PubMed] [Google Scholar]
- Kreeft P, Wiborg G, Galanti MR, Siliquini R, Bohrn K, Scatigna M, et al. ‘Unplugged’: a new European school programme against substance abuse. Drugs: Education, Prevention and Policy 2009;16(2):167‐81. [Google Scholar]
- Vigna‐Taglianti F, Vadrucci S, Faggiano F, Burkhart G, Siliquini R, Galanti MR. Is universal prevention against youths' substance misuse really universal? Gender‐specific effects in the EU‐Dap school‐based prevention trial. Journal of Epidemiology and Community Health 2009;63(9):722‐8. [DOI] [PubMed] [Google Scholar]
Figa‐Talamanca 1989 (F) {published data only}
- Figa‐Talamanca I, Modolo M. Evaluation of an anti‐smoking educational programme among adolescents in Italy. Hygie 1989;8(3):24‐8. [PubMed] [Google Scholar]
Figa‐Talamanca 1989 (N.F) {published data only}
Flay 1985 {published data only (unpublished sought but not used)}
- Best JA, Flay BR, Brown JS. Smoking prevention in the Schools: Program Dissemination. Ontario Ministry of Health Report No. CHS‐R26 1983.
- Flay BR, Koepke D, Thomson SJ, Santi S, Best JA, Brown KS. Six‐year follow‐up of the first Waterloo school smoking prevention trial. American Journal of Public Health 1989;79(10):1371‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flay BR, Ryan CB, Best JA, Brown KS, Kersell MW, d'Avernas JR, et al. Are social‐psychological smoking programs effective? The Waterloo study. Journal of Behavioral Medicine 1985;8(1):37‐59. [DOI] [PubMed] [Google Scholar]
Flay 1995 {published data only}
- Brannon BR, Dent CW, Flay BR, Smith G, Sussman S, Pentz MA, et al. The Television, School and Family Project. V. The impact of curriculum delivery. Preventive Medicine 1989;18:492‐502. [DOI] [PubMed] [Google Scholar]
- Flay BR, Brannon BR, Johnson CA, Hanson WB, Ulene AL, Whitney‐Saltiel DA, et al. The Television, School, and Family Smoking Prevention and Cessation Project. I. Theoretical basis and program development. Preventive Medicine 1988;17:585‐607. [DOI] [PubMed] [Google Scholar]
- Flay BR, Hu FB, Richardson J. Psychosocial predictors of different stages of cigarette smoking among high school students. Preventive Medicine 1998;27 (5 Pt 3):A18‐A19. [DOI] [PubMed] [Google Scholar]
- Flay BR, Miller TQ, Hedeker D, Siddiqui O, Britton CF, Brannon BR, et al. The Television, School, and Family Smoking Prevention and Cessation Project. VIII student outcomes and mediating variables. Preventive Medicine 1995;24:29‐40. [DOI] [PubMed] [Google Scholar]
- Sussman S, Dent CW, Brannon BR, Glowacz KJ, Gleason LR, Ullery S, et al. The Television, School and Family Smoking Prevention and Cessation Project. IV. controlling for program expectancies across experimental and control conditions. Addictive Behaviors 1989;14:601‐10. [DOI] [PubMed] [Google Scholar]
- Sussman S, Flay BR, Sobel JL, Rauch JM, Hansen WB, Johnson CA. Viewing and evaluation of a televised drug education program by students previously or concurrently exposed to school‐based substance abuse prevention programming. Health Education Research 1987;2(4):373‐83. [Google Scholar]
Focarile 1994 {published data only}
- Focarile F, Scaffino L. Results of a randomised controlled trial on preventing the smoking habit in adolescents [Risultati di uno studio controllato randomizzato sulla prevenzione dell'abitudine al fumo degli adolescenti]. Epidemiologia e Prevenzione 1994;18:157‐63. [PubMed] [Google Scholar]
- Focarile FA, Scaffino L, Nardi A, Vaccari R. Protocol and feasibility of a randomized controlled study on preventing the smoking habit in adolescents [Protocollo e fattibilita di uno studio controllato randomizzato sulla prevenzione dell'abitudine al fumo negli adolescenti]. Epidemiologia e Prevenzione 1989;11:41‐6. [PubMed] [Google Scholar]
Forman 1990 (SI) {published data only}
- Forman SG, Linney JA, Brondino MJ. Effects of coping skills training on adolescents at risk for substance use. Psychology of Addictive Behavior 1990;4(2):67‐76. [Google Scholar]
Forman 1990 (SI ‐ NP) {published data only}
- Forman SG, Linney JA, Brondino MJ. Effects of coping skills training on adolescents at risk for substance use. Psychology of Addictive Behavior 1990;4(2):67‐76. [Google Scholar]
Forman 1990 (SI ‐ P) {published data only}
- Forman SG, Linney JA, Brondino MJ. Effects of coping skills training on adolescents at risk for substance use. Psychology of Addictive Behavior 1990;4(2):67‐76. [Google Scholar]
Gabrhelik 2012 {published data only}
- Gabrhelik R, Duncan A, Lee MH, Stastna L, Furr‐Holden CDM, Miovsky M. Sex specific trajectories in cigarette smoking behaviours among students participating in the Unplugged school‐based randomised control trial for substance use prevention. Addictive Behaviors 2012;37(10):1145‐50. [DOI] [PubMed] [Google Scholar]
- Gabrhelik R, Duncan A, Miovsky M, Furr‐Holden CDM, Stastna L, Jurystova L. “Unplugged”: A school‐based randomised control trial to prevent and reduce adolescent substance use in the Czech Republic. Drug and Alcohol Dependence 2012;124:79‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Garcia 2005 {published data only}
- García P, Fernández A, Sánchez JM, Carrillo A, Alcaraz J, Abad E. Randomized controlled trial of a health prevention program against smoking in a population of secondary school students. Revista de Calidad Asistencial 2005;20(1):4‐13. [Google Scholar]
Gatta 1991 {published data only}
- Gatta G, Malvezzi I, Sant M, Micheli A, Panico S, Ravasi G, et al. Randomized trial of primary school education against smoking. Tumori 1991;77:367‐71. [PubMed] [Google Scholar]
Gersick 1988 {unpublished data only}
- Gersick KE, Grady K, Snow DL. Social‐cognitive skill development with sixth graders and its initial impact on substance use. Journal of Drug Education 1988;18(1):55‐70. [DOI] [PubMed] [Google Scholar]
- Snow DL, Tebes JK, Arthur MW, Tapasak RC. Two‐year follow‐up of a social‐cognitive intervention to prevent substance use. Journal of Drug Education 1992;22:101‐14. [DOI] [PubMed] [Google Scholar]
- Snow DL, Tebes JK, Ayers TS. Impact of two social‐cognitive interventions to prevent adolescent substance use: test of an amenability to treatment model. Journal of Drug Education 1997;27(1):1‐17. [DOI] [PubMed] [Google Scholar]
Gilchrist 1986 {published data only}
- Gilchrist LD, Schinke SP, Bobo JK, Snow WH. Self‐control skills for preventing smoking. Addictive Behaviors 1986;11:169‐74. [DOI] [PubMed] [Google Scholar]
Gindre 1995 {published data only}
- Gindre C, Conard J, Ducos‐Mieral C, Champetier de Ribes G. Departmental programme for the early prevention of tobacco addiction among school children. In: Slama K editor(s). Tobacco and Health. Proceedings of the 9th World Conference on Tobacco and Health 1994. New York: Plenum Press, 1995. [Google Scholar]
Glanz 2007 {published data only}
- Glanz K, Lunde KB, Leakey T, Maddock J, Koga K, Yamauchi J, et al. Activating multi‐ethnic youth for smoking prevention: Design, baseline findings, and implementation of project SPLASH. Journal of Cancer Education 2007;22(1):56‐61. [DOI] [PubMed] [Google Scholar]
- Glanz K, Maskarinec G, Carlin L. Ethnicity, sense of coherence, and tobacco use among adolescents. Annals of Behavioral Medicine 2005;29(3):192‐9. [DOI] [PubMed] [Google Scholar]
- Glanz K, Mau M, Steffen M, Maskarinec G, Arriola KR. Tobacco use among Native Hawaiian middle School students: its prevalence, correlates and implications. Ethnicity and Health 2007;12(3):1‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leakey T, Lunde K, Koga K, Glanz K. Written parental consent and incentives in a youth smoking prevention trial: A case study from Project SPLASH. American Journal of Evaluation 2004;25(4):509‐23. [Google Scholar]
- Sy A, Glanz K. Factors influencing teachers' implementation of an innovative tobacco prevention curriculum for multiethnic youth: Project SPLASH. Journal of School Health 2008;78(5):264‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gordon 2008 {published data only}
- Gordon J, Biglan A, Smolkowski K. The impact on tobacco use of branded youth anti‐tobacco activities and family communications about tobacco. Prevention Science 2008;9(2):73‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hamilton 2005 {published data only}
- Hamilton G, Cross D, Resnicow K, Hall M. A school‐based harm minimization smoking intervention trial: outcome results. Addiction 2005;100(5):689‐700. [DOI] [PubMed] [Google Scholar]
- Hamilton G, Cross D, Resnicow K, Shaw T. Does harm minimisation lead to greater experimentation? Results from a school smoking intervention trial. Drug & Alcohol Review 2007;26:605‐13. [DOI] [PubMed] [Google Scholar]
Hanewinkel 1994 {published data only}
- Hanewinkel R, Ferstl R, Burow F. Conception and evaluation of a behavioural non‐smoking intervention in schools [Konzeption und Evaluation einer verhaltensorientierten Nichtraucherförderung an Schulen]. Verhaltenstherapie 1994;4:104‐10. [Google Scholar]
Hansen 1988a {published data only}
- Graham JW, Johnson CA, Hansen WB, Flay BR, Gee M. Drug use prevention programs, gender and ethnicity: evaluation of three seventh‐grade Project SMART cohorts. Preventive Medicine 1990;19:305‐13. [DOI] [PubMed] [Google Scholar]
- Hansen WB, Johnson CA, Flay BR, Graham JW, Sobel J. Affective and social influences approaches to the prevention of multiple substance abuse among seventh grade students: Results from Project SMART. Preventive Medicine 1988;17:135‐54. [DOI] [PubMed] [Google Scholar]
- Unger JB, Johnson CA, Stoddard JL, Nezami E, Chou CP. Indentification of the adolescents at risk for smoking initiation: validation of a measure of susceptibility. Addictive Behaviors 1997;22(1):81‐91. [DOI] [PubMed] [Google Scholar]
Hansen 1991 {published data only}
- Donaldson SI, Graham JW, Hansen WB. Testing the generalisability of intervening mechanism theories: understanding the effects of adolescent drug use prevention interventions. Journal of Behavioral Medicine 1994;17(2):195‐216. [DOI] [PubMed] [Google Scholar]
- Donaldson SI, Graham JW, Piccinin AM, Hansen WB. Resistance‐skills training and onset of alcohol use: evidence for beneficial and potentially harmful effects in public schools and in private Catholic schools. Health Psychology 1995;14(4):291‐300. [DOI] [PubMed] [Google Scholar]
- Donaldson SI, Thomas CW, Graham JW, Au JG, Hansen WB. Verifying drug abuse prevention program effects using reciprocal best friend reports. Journal of Behavioral Medicine 2000;23(6):585‐601. [DOI] [PubMed] [Google Scholar]
- Hansen WB, Graham JW. Preventing alcohol, marijuana and cigarette use among adolescents: Peer Pressure Resistance Training versus Establishing Conservative Norms. Preventive Medicine 1991;20:414‐30. [DOI] [PubMed] [Google Scholar]
- Hansen WB, Graham JW, Wolkenstein BH, Rohrbach LA. Program integrity as a moderator of prevention program effectiveness: results for fifth‐grade students in the Adolescent Alcohol Prevention Trial. Journal of Studies on Alcohol 1991;53(5):568‐79. [DOI] [PubMed] [Google Scholar]
- Palmer RF, Graham JW, White EL, Hansen WB. Applying multilevel analytic strategies in adolescent substance use prevention research. Preventive Medicine 1998;27:328‐36. [DOI] [PubMed] [Google Scholar]
- Rohrbach LA, Graham JW, Hansen WB. Diffusion of a school‐based substance abuse prevention program: predictors of program implementation. Preventive Medicine 1993;22:237‐60. [DOI] [PubMed] [Google Scholar]
- Taylor BJ, Graham JW, Cumsille P, Hansen WB. Modeling prevention program effects on growth in substance use: analysis of five years of data from the Adolescent Alcohol Prevention Trial. Prevention Science 2000;1(4):183‐97. [DOI] [PubMed] [Google Scholar]
Hecht 2003 {published data only}
- Hecht ML, Graham JW, Elek E. The drug resistance strategies intervention: program effects on substance use. Health Communication 2006;20(3):267‐76. [DOI] [PubMed] [Google Scholar]
- Hecht ML, Krieger JLR. The principle of cultural grounding in school‐based substance abuse prevention. Journal of Language and Social Psychology 2006;25(3):301‐19. [Google Scholar]
- Hecht ML, Marsiglia FF, Elek E, Wagstaff DA, Kulis S, Dustman P, et al. Culturally grounded substance use prevention: an evaluation of the keepin' it REAL curriculum. Prevention Science 2003;4(4):233‐48. [DOI] [PubMed] [Google Scholar]
- Warren JR, Hecht ML, Wagstaff DA, Elek E, Ndiaye K, Dustman P, et al. Communicating prevention: The effects of the keepin' it REAL classroom videotapes and televised PSAs on middle‐school students substance use.. Journal of Applied Communication Research 2006;34(2):209‐27. [Google Scholar]
Hecht 2008 {published data only}
- Elek E, Wagstaff DA, Hecht ML. Effects of the 5th and 7th grade enhanced versions of the keepin' it real substance use prevention curriculum. Journal of Drug Education 2010;40(1):61‐79. [DOI] [PubMed] [Google Scholar]
- Hecht ML, Elek E, Wagstaff DA, Kam JA, Marsiglia FF, Dustman P, et al. Immediate and short‐term effects of the 5th grade version of the keepin' it REAL substance use prevention intervention. Journal of Drug Education 2008;38(3):225‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hedman 2010 (Interview) {published data only}
- Hedman E, Riis U, Gabre P. The impact of behavioural interventions on young people's attitudes toward tobacco use. Oral Health & Preventive Dentistry 2010;8(1):23‐32. [PubMed] [Google Scholar]
Hedman 2010 (Lecture) {published data only}
Hirschmann 1989 {published data only}
- Hirschman RS, Leventhal H. Preventing smoking behavior in school children: an initial test of a cognitive‐development program. Journal of Applied Social Psychology 1989;19(7):559‐83. [Google Scholar]
Hort 1995 {published data only}
- Hort W, Hort H, Willers R. Intervention study against cigarette smoking in Duesseldorf high school pupils [Interventionsstudie gegen das Zigarettenrauchen von Düsseldorfer Hauptschülern 1992‐94]. Zeitschrift Kardiologie 1995;84:700‐11. [PubMed] [Google Scholar]
Howard 1996 {published data only}
- Howard JK, Bindler RM, Synoground G, Gemert FC. A cardiovascular risk reduction program for the classroom. Journal of School Nursing 1996;12:4‐11. [DOI] [PubMed] [Google Scholar]
Johnson 2009 {published data only}
- Johnson CC, Myers L, Webber LS, Boris NW. Profiles of the adolescent smoker:models of tobacco use among 9th grade high school students Acadiana Coalition of Teens against Tobacco (ACTT). Preventive Medicine 2004;39:551‐8. [DOI] [PubMed] [Google Scholar]
- Johnson CC, Myers L, Webber LS, Boris NW, He H, Brewer D. A school‐based environmental intervention to reduce smoking among high school students: The Acadiana Coalition of Teens against Tobacco (ACTT). International Journal of Environmental Research and Public Health 2009;6(4):1298‐316. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jøsendal 1998 (P) {published data only}
Jøsendal 1998 (P + T) {published data only}
- Josendal O, Aaro E. Be Smokefree ‐ evaluation of a programme for Smokefree schools [Vaer roykFRI ‐ evaluering av et tiltak for roykfrie skoler]. Tidsskr Nor Laegeforen 2002;122(4):403‐7. [PubMed] [Google Scholar]
- Josendal O, Aaro LE, Bergh I. Effects of a school‐based smoking prevention program among subgroups of adolescents. Health Education Research 1998;13:215‐24. [DOI] [PubMed] [Google Scholar]
- Josendal O, Aaro LE, Torsheim T, Rasbash J. Evaluation of the school‐based smoking prevention program "BE smokeFree". Scandinavian Journal of Psychology 2005;46:189‐99. [DOI] [PubMed] [Google Scholar]
Jøsendal 1998 (T) {published data only}
Kaufman 1994 {published data only}
- Kaufman JS, Jason LA, Sawlski LM, Halpert JA. A comprehensive multi‐media program to prevent smoking among black students. Journal of Drug Education 1994;24:95‐108. [DOI] [PubMed] [Google Scholar]
Kellam 1998 (GBG) {published data only}
- Kellam SG, Anthony JC. Targeting early antecedents to prevent tobacco smoking: findings from an epidemiologically based randomised field trial. American Journal of Public Health 1998;88:1490‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellam SG, Brown CH, Poduska JM, Ialongo NS, Wang W, Toyinbo P, et al. Effects of a universal classroom behavior management program in first and second grades on young adult behavioral, psychiatric, and social outcomes. Drug and Alcohol Dependence 2008;95(Supplement 1):S5‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellam SG, Mackenzie AC, Brown CH, Poduska JM, Wang W, Petras H, et al. The good behavior game and the future of prevention and treatment. Addicion Science & Clincial Practice 2011;6(1):73‐84. [PMC free article] [PubMed] [Google Scholar]
- Petras H, Kellam SG, Brown CH, Muthen BO, Ialongo NS, Poduska JM. Developmental epidemiological courses leading to antisocial personality disorder and violent and criminal behavior: Effects by young adulthood of a universal preventive intervention in first‐ and second‐ grade classrooms. Drug & Alcohol Dependence 2008;95(Supplement 1):S45‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poduska JM, Kellam SG, Wang W, Brown CH, Ialong NS, Toyinbo P. Impact of the Good Behavior Game, a universal classroom‐based behavior intervention, on young adult service use for problems with emotions, behavior, or drugs or alcohol. Drug and Alcohol Dependence 2008;95(Supplement 1):S29‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox H, Kellam SG, Brown CH, Poduska JM, Ialongo NS, Wang W, et al. The impact of two universal randomised first‐ and second‐grade classroom interventions on young adult suicide ideation and attempts. Drug & Alcohol Dependence 2008;95(Supplement 1):S60‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kellam 1998 (ML) {published data only}
Laniado‐Laborín 1993 {published data only}
- Laniado‐Laborín R, Molgaard CA, Elder JP. Effectiveness of a tobacco prevention programme in Mexican students [Efectividad de un programa de prevención de tabaquismo en escolares mexicanos]. Salud Publica de Mexico 1993;35(4):403‐8. [PubMed] [Google Scholar]
La Torre 2010 (A) {published data only}
- Torre G, Chiaradia G, Monte L, Moretti C, Mannocci A, Capitanio D, et al. A randomised controlled trial of a school‐based intervention to prevent tobacco use among children and adolescents in Italy. Journal of Public Health 2010;18(6):533‐42. [Google Scholar]
La Torre 2010 (C) {published data only}
Lloyd 1983 {published data only}
- Alexander HM, Callcott R, Dobson AJ, Hardes GR, Lloyd DM, O'Connell DL, et al. Cigarette smoking and drug use in schoolchildren: IV‐‐factors associated with changes in smoking behaviour. International Journal of Epidemiology 1983;12:59‐66. [DOI] [PubMed] [Google Scholar]
- Hardes GR, Alexander HM, Dobson AJ, Lloyd DM, O'Connell DL, Purcell I, et al. Cigarette smoking and drug use in schoolchildren in the Hunter Region, New South Wales. I. Tobacco, alcohol and analgesic use in 10 to 12 year and primary school children. Medical Journal of Australia 1981;1:579‐81. [PubMed] [Google Scholar]
- LLoyd DM, Alexander HM, Callcott R, Dobson AJ, Hardes GR, O'Connell DL, et al. Cigarette smoking and drug use in schoolchildren: III ‐ Evaluation of a smoking prevention education programme. International Journal of Epidemiology 1983;12:51‐8. [DOI] [PubMed] [Google Scholar]
Longshore 2006 {published data only}
- Longshore D, Ellickson PL, McCaffrey DF, Clair PA. School‐based drug prevention among at‐risk adolescents: effects of ALERT plus. Health Education & Behavior 2007;34(4):651‐68. [DOI] [PubMed] [Google Scholar]
- Longshore D, Ghosh‐Dastidar B, Ellickson PL. National youth anti‐drug media campaign and school‐based drug prevention: Evidence for a synergistic effect in ALERT plus. Addictive Behaviors 2006;31(3):496‐508. [DOI] [PubMed] [Google Scholar]
Lotrean 2010 {published data only}
- Lotrean LM, Dijk F, Mesters I, Ionut C, Vries H. Evaluation of a peer‐led smoking prevention programme for Romanian adolescents. Health Education Research 2010;25(5):803‐14. [DOI] [PubMed] [Google Scholar]
MacPherson 1980 {published data only}
- MacPherson BV, Ashikaga T, Dickstein MS, Jones RP Jr. Evaluation of a respiratory health education program. Journal of School Health 1980;50:564‐7. [DOI] [PubMed] [Google Scholar]
McCambridge 2011 {published data only}
- McCambridge J, Hunt C, Jenkins RJ, Strang J. Cluster randomised trial of the effectiveness of Motivational Interviewing for universal prevention. Drug and Alcohol Dependence 2011;114(2‐3):117‐84. [DOI] [PubMed] [Google Scholar]
Murray 1984a {published data only}
- Arkin RM, Roemhild HF, Johnson CA, Luepker RV, Murray DM. The Minnesota Smoking Prevention Program: A seventh‐grade health curriculum supplement. Journal of School Health 1981;51:611‐6. [DOI] [PubMed] [Google Scholar]
- Murray DM, Davis‐Hearn M, Goldman AI, Pirie P, Luepker RV. Four‐ and five‐year follow‐up results from seventh grade smoking prevention strategies. Journal of Behavioral Medicine 1988;11:395‐405. [DOI] [PubMed] [Google Scholar]
- Murray DM, Luepker RV, Johnson CA, Mittelmark MB. The prevention of cigarette smoking in children: A comparison of four strategies. Journal of Applied Social Pschology 1984;14:274‐88. [Google Scholar]
- Murray DM, Pirie P, Luepker RV, Pallonen U. Five‐ and six‐year follow‐up results from four seventh‐grade smoking prevention strategies. Journal of Behavioral Medicine 1989;12(2):207‐18. [DOI] [PubMed] [Google Scholar]
- Murray DM, Richards PS, Luepker RV, Johnson CA. The prevention of cigarette smoking in children: Two‐ and three‐year follow‐up comparisons of four prevention strategies. Journal of Behavioral Medicine 1987;10:595‐611. [DOI] [PubMed] [Google Scholar]
Murray 1992 (MDEG) {published data only}
Murray 1992 (MSPP) {published data only}
- Murray DM, Perry CL, Griffin G, Harty KC, Jacobs DR Jr, Schmid L, et al. Results from a statewide approach to adolescent tobacco use prevention. Preventive Medicine 1992;21:449‐72. [DOI] [PubMed] [Google Scholar]
- Perry CL, Murray DM, Griffin G. Evaluating the statewide dissemination of smoking prevention curricula: factors in teacher compliance. Journal of School Health 1990;60(10):501‐4. [DOI] [PubMed] [Google Scholar]
Murray 1992 (SFG) {published data only}
Noland 1998 {published data only}
- Noland MP, Kryscio RJ, Riggs RS, Linville LH, Ford VY, Tucker TC. The effectiveness of a tobacco prevention program with adolescents living in a tobacco‐producing region. American Journal of Public Health 1998;88:1862‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Norman 2008 {published data only}
- Norman CD, Maley O, Li X, Skinner HA. Using the internet to assist smoking prevention and cessation in schools: A randomised, controlled trial. Health Psychology 2008;27(6):799‐810. [DOI] [PubMed] [Google Scholar]
- Norman CD, Skinner HA. Engaging youth in e‐health promotion: lessons learned from a decade of TeenNet research. Adolescent Medicine 2007;18(2):357‐69. [PubMed] [Google Scholar]
- Skinner H, Maley O, Norman C. Website intervention for youth smoking prevention: findings from school‐based randomised controlled trial. Society for Research on Nicotine and Tobacco 11th Annual Meeting, 20‐23 March 2005; Prague, Czech Republic. 2005.
Nutbeam 1993 (FSE) {published data only}
- Newman R, Nutbeam D. Teachers' views of the family smoking education project. Health Education Journal 1989;48:9‐13. [Google Scholar]
- Nutbeam D, Macaskill P, Smith C, Simpson JM, Catford J. Evaluation of two school smoking education programmes under normal classroom conditions. BMJ 9 January 1993;Vol 306:102‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nutbeam 1993 (FSE+SAM) {published data only}
Nutbeam 1993 (SAM) {published data only}
O'Donnell 1995 {published data only}
- O'Donnell J, Hawkins JD, Catalano RF, Abbott RD, Day LE. Preventing school failure, drug use, and delinquency among low‐income children: Long‐term intervention in elementary schools. American Journal of Orthopsychiatry 1995;65(1):87‐100. [DOI] [PubMed] [Google Scholar]
Perry 1996 {published data only}
- Komro KA, Perry CL, Veblen‐Mortensen S, Williams CL. Peer participation in project Northland: a community‐wide alcohol use prevention project. Journal of School Health 1994;64(8):318‐22. [DOI] [PubMed] [Google Scholar]
- Perry CL, Williams CL, Forster JL, Wolfson M, Wagenaar AC, Finnegan JR, et al. Background, conceptualisation and design of a community‐wide research program on adolescent alcohol use: Project Niorthland. Health Education Research 1993;8(1):125‐36. [DOI] [PubMed] [Google Scholar]
- Perry CL, Williams CL, Veblen Mortenson S, Toomey TL, Komro KA, Anstine PS, et al. Project Northland: outcomes of a community wide alcohol use prevention program during early adolescence [see comments]. American Journal of Public Health 1996;86(7):956‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Perry 2003 (Dare+ boys) {published data only}
Perry 2003 (Dare+ girls) {published data only}
Perry 2003 (Dare boys) {published data only}
- Eischens A, Komro KA, Perry CL, Bosma LM, Farbakhsh K. The association of extracurricular activity participation with substance use among youth in the DARE Plus Project. American Journal of Health Education 2004;35(2):68‐75. [Google Scholar]
- Perry CL, Komro KA, Veblen‐Mortenson S, Bosma LM, Farbakhsh K, Munson KA, et al. A randomised controlled trial of the middle and junior high school D.A.R.E. and D.A.R.E. Plus programs. Archives of Pediatric and Adolescent Medicine 2003;157:178‐84. [DOI] [PubMed] [Google Scholar]
- Perry CL, Komro KA. Veblen‐Mortensen S, Bosma L, Munson K, Stigler M, et al. The Minnesota DARE PLUS project: Creating community partnerships to prevent drug use and violence. Journal of School Health 2000;70(3):84‐8. [DOI] [PubMed] [Google Scholar]
Perry 2003 (Dare girls) {published data only}
Perry 2009 {published data only}
- Arora M, Gupta VK, Nazar GP, Stigler MH, Perry CL, Reddy KS. Impact of tobacco advertisements on tobacco use among urban adolescents in India: results from a longitudinal study. Tobacco Control 2012;21:318‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora M, Reddy KS, Stigler MH, Perry CL. Associations between tobacco marketing and use among urban youth in India. American Journal of Health Behavior 2008;32(3):283‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babar AA, Stigler MH, Perry CL, Arora M, Shrivastav R, Reddy KS. Tobacco‐use psychosocial risk profiles of girls and boys in urban India: implications for gender‐specific tobacco intervention development. Nicotine & Tobacco Research 2010;12(1):29‐36. [DOI] [PubMed] [Google Scholar]
- Bate SL, Stigler MH, Thompson MS, Arora M, Perry CL, Reddy KS, et al. Psychosocial mediators of a school‐based tobacco prevention program in India: results from the first year of project MYTRI. Prevention Science 2009;10(2):116‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goenka S, Tewari A, Arora M, Stigler MH, Perry CL, Arnold JP, et al. Process evaluation of a tobacco prevention program in Indian schools‐‐methods, results and lessons learnt. Health Education Research 2010;25(6):917‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra A, Arora M, Stigler MH, Komro KA, Lytle LA, Reddy KS, et al. Indian youth speak about tobacco: results of focus group discussions with school students. Health Education & Behavior 2005;32(3):363‐79. [DOI] [PubMed] [Google Scholar]
- Perry CL, Stigler MH, Arora M, Reddy KS. Preventing tobacco use among young people in India: Project MYTRI. American Journal of Public Health 2009;99(5):899‐906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry CL, Stigler MH, Arora M, Reddy KS. Prevention in translation: tobacco use prevention in India. Health Promotion Practice 2008;9(4):378‐86. [DOI] [PubMed] [Google Scholar]
- Stigler MH, Perry CL, Arora M, Reddy KS. Why are urban Indian 6th graders using more tobacco than 8th graders? Findings from Project MYTRI. Tobacco Control 2006;15 Suppl 1:54‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stigler MH, Perry CL, Arora M, Shrivastav R, Mathur C, Reddy KS. Intermediate outcomes from project MYTRI: Mobilizing youth for tobacco‐related initiatives in India. Cancer Epidemiology, Biomarkers & Prevention 2007;16(6):1050‐6. [DOI] [PubMed] [Google Scholar]
- Stigler MH, Perry CL, Smolenski D, Arora M, Reddy KS. A mediation analysis of a tobacco prevention program for adolescents in India: how did project MYTRI work?. Health Education & Behavior 2011;38(3):231‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peterson 2000 {published data only}
- Kealey KA, Peterson AV Jr, Gaul MA, Dinh KT. Teacher training as a behavior change process: principles and results from a longitudinal study. Health Education & Behavior 2000;27:64‐81. [DOI] [PubMed] [Google Scholar]
- Mann SL, Peterson AV Jr, Marek PM, Kealey KA. The Hutchinson Smoking Prevention Project trial: design and baseline characteristics. Preventive Medicine 2000;30:485‐95. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Peterson AV Jr, Kealey KA, Mann SL, Marek PM, Sarason IG. Hutchinson Smoking Prevention Project: long‐term randomised trial in school‐based tobacco use prevention‐results on smoking. Journal of the National Cancer Institute 2000;92:1979‐91. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Peterson AV Jr, Mann SL, Kealey KA, Marek PM. Experimental design and methods for school‐based randomised trials: Experience from the Hutchinson Smoking Prevention Project (HSSP). Controlled Clinical Trials 2000;21:144‐65. [DOI] [PubMed] [Google Scholar]
Piper 2000 (HFL) {published data only}
- Moberg DP, Piper DL, Wu J, Serlin RC. When total randomisation is impossible: Nested randomised assignment. Evaluation Review 1993;17(3):271‐91. [Google Scholar]
- Piper DL, Moberg DP, King MJ. The healthy for life project: Behavioral outcomes. Journal of Primary Prevention 2000;21:47‐73. [Google Scholar]
Piper 2000 (HFL Age) {published data only}
Prokhorov 2008 {published data only}
- Minnix JA, Blalock JA, Marani S, Prokhorov AV, Cinciripini PM. Self‐efficacy mediates the effect of depression on smoking susceptibility in adolescents. Nicotine & Tobacco Research 2011;13(8):699‐705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prokhorov AV, Kelder SH, Shegog R, Conroy JL, Murray N, Peters R, et al. Project ASPIRE: an interactive, multimedia smoking prevention and cessation curriculum for culturally diverse high school students. Substance Use & Misuse 2010;45(6):983‐1006. [DOI] [PubMed] [Google Scholar]
- Prokhorov AV, Kelder SH, Shegog R, Murray N, Peters R, Jr, Agurcia‐Parker C, et al. Impact of A Smoking Prevention Interactive Experience (ASPIRE), an interactive, multimedia smoking prevention and cessation curriculum for culturally diverse high‐school students. Nicotine & Tobacco Research 2008;10(9):1477‐85. [DOI] [PubMed] [Google Scholar]
Rabinowitz 1974 {published data only}
- Rabinowitz HS, Zimmerli WH. Effects of a health education program on junior high school students' knowledge, attitudes and behavior concerning tobacco use. Journal of School Health 1974;64:324‐30. [DOI] [PubMed] [Google Scholar]
Reddy 2002 (School + F) {published data only}
Reddy 2002 (School only) {published data only}
- Reddy KS, Arora M, Perry CL, Nair B, Kohli A, Lytle LA, et al. Tobacco and alcohol use outcomes of a school‐based intervention in New Delhi. American Journal of Health Behavior 2002;26(3):173‐81. [DOI] [PubMed] [Google Scholar]
Resnicow 2008 (Harm Min) {published data only}
Resnicow 2008 (LST) {published data only}
- Resnicow K, Reddy SP, James S, Gabebodeen OR, Kambaran NS, Langner HG, et al. Comparison of two school‐based smoking prevention programs among South African high school students: results of a randomised trial. Annals of Behavioral Medicine 2008;36(3):231‐43. [DOI] [PubMed] [Google Scholar]
- Resnicow K, Zhang N, Vaughan RD, Reddy SP, James S, Murray DM. When intra‐class correlation coefficients go awry: A case study from a school‐based smoking prevention study in South Africa. American Journal of Public Health 2010;100(9):1714‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ringwalt 2009a {published data only}
- Clark HK, Ringwalt CL, Hanley S, Shamblen SR. Project ALERT's effects on adolescents' prodrug beliefs: a replication and extension study. Health Education & Behavior 2010;37(3):357‐76. [DOI] [PubMed] [Google Scholar]
- Clark HK, Ringwalt CL, Shamblen SR, Hanley SM, Flewelling RL. Are substance use prevention programs more effective in schools making adequate yearly progress? A study of Project ALERT. Journal of Drug Education 2011;41(3):271‐88. [DOI] [PubMed] [Google Scholar]
- Clark HK, Ringwalt Cl, Shamblen SR. Predicting adolescent substance use: The effects of depressed mood and positive expectancies. Addictive Behaviors 2011;36(5):488‐93. [DOI] [PubMed] [Google Scholar]
- Ringwalt CL, Clark HK, Hanley S, Shamblen SR, Flewelling RL. Project ALERT: a cluster randomized trial. Archives of Pediatrics & Adolescent Medicine 2009;163(7):625‐32. [DOI] [PubMed] [Google Scholar]
- Ringwalt CL, Kovach Clark H, Hanley S, Shamblen SR, Flewelling RL. The effects of Project ALERT one year past curriculum Completion. Prevention Science 2010;11:172‐84. [DOI] [PubMed] [Google Scholar]
Rohrbach 2010a {published data only}
- Rohrbach LA, Gunning M, Sun P, Sussman S. The Project Towards No Drug Abuse (TND) Dissemination Trial: Implementation fidelity and immediate outcomes. Prevention Science 2010;11:77‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohrbach LA, Sun P, Sussman S. One‐year follow‐up evaluation of the Project Towards No Drug Abuse (TND) Dissemination Trial. Preventive Medicine 2010;51:313‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Scheier 2001 {published data only}
- Scheier LM, Botvin GJ, Griffin KW. Preventive intervention effects on developmental progression in drug use: structural equation modelling analyses using longitudinal data. Prevention Science 2001;2(2):91‐112. [DOI] [PubMed] [Google Scholar]
Schinke 1984 {published data only}
- Schinke SP, Gilchrist LD. Preventing cigarette smoking with youth. Journal of Primary Prevention 1984;5:48‐56. [DOI] [PubMed] [Google Scholar]
Schinke 1985a {published data only}
- Schinke SP, Gilchrist LD, Snow WH. Skills intervention to prevent cigarette smoking among adolescents. American Journal of Public Health 1985;75:665‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schinke 1985b {published data only}
- Schincke SP, Gilchrist LD. Preventing substance abuse with children and adolescents. Journal of Consulting and Clinical Psychology 1985;53:596‐602. [DOI] [PubMed] [Google Scholar]
Schinke 1985c {published data only}
- Schinke SP, Gilchrist LD, Snow WH, Schilling RF II. Skills‐building methods to prevent smoking by adolescents. Journal of Adolescent Health Care 1985;6:439‐44. [DOI] [PubMed] [Google Scholar]
Schinke 1986a {published data only}
- Schinke SP, Bebel MY, Orlandi MA, Botvin GJ. Prevention strategies for vulnerable pupils. School social work practices to prevent substance abuse. Urban Education 1988;22(4):510‐9. [Google Scholar]
- Schinke SP, Gilchrist LD, Schilling RF II, Senechal VA. Smoking and smokeless tobacco use among adolescents: trends and intervention results. Public Health Reports 1986;101:373‐8. [PMC free article] [PubMed] [Google Scholar]
Schinke 1986b {published data only}
- Schinke SP, Gilchrist LD, Schilling RF II, Snow WH, Bobo JK. Skills methods to prevent smoking. Health Education Quarterly 1986;13:23‐7. [DOI] [PubMed] [Google Scholar]
Schinke 1986c {published data only}
- Schinke SP, Gilchrist LD. Preventing tobacco use among young people. Health and Social Work 1986;11:59‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schinke 1988 {published data only}
- Schinke SP, Botvin GJ, Trimble JE, Orlandi MA, Gilchrist LD, Locklear VS. Preventing substance abuse among American‐Indian adolescents: A bicultural competence skills approach. Journal of Counseling Psychology 1988;35:87‐90. [PMC free article] [PubMed] [Google Scholar]
Schinke 2000 {published data only}
- Moncher M, Schinke S. Group intervention to prevent tobacco use among Native American youth. Research on Social Work Practice 1994;4(2):160‐71. [Google Scholar]
- Schinke SP, Tepavac L, Cole KC. Preventing substance use among native American youth: Three‐year results. Addictive Behaviors 2000;25:387‐97. [DOI] [PubMed] [Google Scholar]
Schofield 2003 {published data only}
- Lynagh M, Knight J, Schofield MJ, Paras L. Lessons learned from the Hunter Region Health Promoting Schools project in New South Wales, Australia. Journal of School Health 1999;9(6):227‐32. [DOI] [PubMed] [Google Scholar]
- Schofield MJ, Lynagh M, Mishra G. Evaluation of a Health Promoting Schools program to reduce smoking in Australian secondary schools. Health Education Research 2003;18(6):678‐92. [DOI] [PubMed] [Google Scholar]
Scholz 2000 (G, female) {published data only}
Scholz 2000 (G, male) {published data only}
- Scholz M, Kaltenbach M. Promoting non‐smoking behavior in 13‐year‐old students in primary schools and high schools. A prospective, randomised intervention study with 1,956 students [Förderung des Nichtraucherverhaltens bei 13‐jährigen Schülerinnen und Schülern von Realschule und Gymnasium. Eine prospektive, randomisierte Interventionsstudie bei 1956 Schülern]. Gesundheitswesen 2000;62(2):78‐85. [DOI] [PubMed] [Google Scholar]
Scholz 2000 (R, female) {published data only}
Scholz 2000 (R, male) {published data only}
Schulze 2006 {published data only}
- Schulze A, Mons U, Edler L, Potschke‐Langer M. Lack of sustainable prevention effect of the "Smoke‐Free Class Comptetition" on German pupils. Preventive Medicine 2006;42(1):33‐9. [DOI] [PubMed] [Google Scholar]
Seal 2006 {published data only}
- Seal N. Preventing tobacco and drug use among Thai high school students through life skills training. Nursing & Health Sciences 2006;8(3):164‐8. [DOI] [PubMed] [Google Scholar]
Severson 1991 (High, F) {published data only}
Severson 1991(high, M) {published data only}
- Severson HH, Glasgow R, Wirt R, Brozovsky P, Zoref L, et al. Preventing the use of smokeless tobacco and cigarettes by teens: results of a classroom intervention. Health Education Research 1991;6(1):109‐20. [Google Scholar]
Severson 1991 (Middle, F) {published data only}
Severson 1991 (Middle, M) {published data only}
Shope 1996 {published data only}
- Shope JT, Copeland LA, Kamp ME, Lang SW. Twelfth grade follow‐up of the effectiveness of a middle school‐ based substance abuse prevention program. Journal of Drug Education 1998;28:185‐97. [DOI] [PubMed] [Google Scholar]
- Shope JT, Copeland LA, Marcoux BC, Kamp ME. Effectiveness of a school‐based substance abuse prevention program. Journal of Drug Education 1996;26:323‐37. [DOI] [PubMed] [Google Scholar]
Simons‐Morton 2005 {published data only}
- Simons MB, Chen RS. Over time relationships between early adolescent and peer substance use. Addictive Behaviors 2006;31:1211‐23. [DOI] [PubMed] [Google Scholar]
- Simons‐Morton B, Haynie D, Saylor K, Crump AD, Chen R. Impact analysis and mediation of outcomes: the Going Places program. Health Education & Behavior 2005;32(2):227‐41. [DOI] [PubMed] [Google Scholar]
- Simons‐Morton B, Haynie D, Saylor K, Crump AD, Chen R. The effects of the Going Places Program on early adolescent substance use and antisocial behavior. Prevention Science 2005;6(3):187‐97. [DOI] [PubMed] [Google Scholar]
Sloboda 2009 {published data only}
- Sloboda Z, Stephens RC, Stephens PC, Grey SF, Teasdale B, Hawthorne RD, et al. The Adolescent Substance Abuse Prevention Study: A randomised field trial of a universal substance abuse prevention program.[see comment]. Drug and Alcohol Dependence 2009;102(1‐3):1‐10. [DOI] [PubMed] [Google Scholar]
- Stephens PC, Sloboda Z, Grey S, Stephens R, Hammond A, Hawthorne R, et al. Is the receptivity of substance abuse prevention programming affected by students' perceptions of the instructor. Health Education & Behavior 2009;36(4):724‐45. [DOI] [PubMed] [Google Scholar]
- Teasdale B, Stephens PC, Sloboda Z, Grey SF, Stephens RC. The influence of program mediators on eleventh grade outcomes for seventh grade substance users and nonusers. Drug and Alcohol Dependence 2009;102:11‐8. [DOI] [PubMed] [Google Scholar]
Smith 2004 {published data only}
- Smith EA, Swisher JD, Vicary JR, Bechtel LJ, Minner D, Henry KL, et al. Evaluation of Life Skills Training and Infused‐Life Skills Training in a rural setting: Outcomes at two years. Journal of Alcohol and Drug Education 2004;48:51‐70. [Google Scholar]
- Swisher JD, Smith EA, Vicary JR, Bechtel LJ, Hopkins AM. A cost‐effectiveness comparison of two approaches to life skills training. Journal of Alcohol and Drug Education 2004;48:71‐87. [Google Scholar]
- Vicary JR, Smith EA, Swisher JD, Bechtel LJ, Elek E, Henry KL, et al. Results of a 3‐year study of two methods of delivery of life skills training. Health Education & Behavior 2006;33:325‐39. [DOI] [PubMed] [Google Scholar]
Spoth 2001 (ISFP) {published data only}
- Guyll M, Spoth RL, Wickrama KAS, Russell D. Family‐focused preventive interventions: Evaluating parental risk moderation of substance use trajectories. Journal of Family Psychology 2004;18(2):293‐301. [DOI] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Shin C, Azevedo K. Brief family intervention effects on adolescent substance initiation: School‐level growth curve analyses 6 years following baseline. Journal of Consulting and Clinical Psychology 2004;72(3):535‐42. [DOI] [PubMed] [Google Scholar]
- Spoth R, Reyes ML, Redmond C, Shin C. Assessing a public health approach to delay onset and progression of adolescent substance use: Latent transition and log‐linear analyses of longitudinal family preventive intervention outcomes. Journal of Consulting and Clinical Psychology 1999;67(5):619‐30. [DOI] [PubMed] [Google Scholar]
- Spoth R, Trudeau L, Guyll M, Shin C, Redmond C. Universal intervention effects on substance use among young adults by delayed adolescent substance initiation. Journal of Consulting and Clincial Psychology 2009;77(4):620‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth RL, Redmond C, Shin C. Randomized trial of brief family interventions for general populations: adolescent substance use outcomes 4 years following baseline. Journal of Consulting and Clinical Psychology 2001;69(4):627‐42. [DOI] [PubMed] [Google Scholar]
- Trudeau L, Spoth R, Randall K, Azevedo K. Longitudinal effects of a universal family‐focused intervention on growth patterns of adolescent internalising symptoms and polysubstance use: Gender comparisons. Journal of Youth Adolescence 2007;36:725‐40. [Google Scholar]
Spoth 2001 (PDFY) {published data only}
Spoth 2002 (LST) {published data only}
Spoth 2002 (LST + SFP) {published data only}
- Spoth R, Randall GK, Shin C, Redmond C. Randomised study of combined universal family and school preventive interventions: patterns of long‐term effects on initiation, regular use, and weekly drunkness. Psychology of Addictive Behaviours 2005;19(4):372‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth RL, Randall GK, Trudeau L, Shin C, Redmond C. Substance use outcomes 5½ years past baseline for partnership‐based, family‐school preventive interventions. Drug and Alcohol Dependence 2008;96(1‐2):57‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth RL, Redmond C, Trudeau L, Shin C. Longitudinal substance initiation outcomes for a universal preventive intervention combining family and school programs. Psychology of Addictive Behaviors 2002;16(2):129‐34. [PubMed] [Google Scholar]
- Trudeau L, Spoth R, Lillehoj C, Redmond C, Wickrama KAS. Effects of a preventive intervention on adolescent substance use initiation, expectancies, and refusal intentions. Prevention Science 2003;4(2):109‐22. [DOI] [PubMed] [Google Scholar]
Spoth 2007 {published data only}
- Greenberg MT, Feinberg ME, Meyer‐Chilenski S, Spoth R, Redmond, C. Community and team member factors that influence the early phase functioning of community prevention teams: the PROSPER Project. Journal of Primary Prevention 2007;28:485‐504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redmond C, Spoth R, Shin C, Schainker LM, Greenberg MT, Feinberg ME. Long‐term protective factor outcomes of evidence‐based interventions implemented by community teams through a community‐university partnership. Journal of Primary Prevention 2009;30:513‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Clair S, Greenberg MT, Redmond C, Shin C. Toward dissemination of evidence‐based family interventions: Maintenance of community‐based partnership recruitment results and associated factors. Journal of Family Psychology 2007;21(2):137‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Greenberg MT, Bierman K, Redmond C. PROSPER Community‐university partnership model for public education systems: capacity‐building for evidence‐based, competence‐building prevention. Prevention Science 2004;5(1):31‐9. [DOI] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Clair S, Shin C, Greenberg M, Feinberg M. Preventing substance misuse through community‐university partnerships: Randomized controlled trial outcomes 4½ years past baseline. American Journal of Preventive Medicine 2011;40(4):440‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Shin C, Greenberg M, Clair S, Feinberg M. Substance‐use outcomes at 18 months past baseline. The PROSPER community‐university partnership trial. American Journal of Preventive Medicine 2007;32(5):395‐402. [DOI] [PMC free article] [PubMed] [Google Scholar]
Storr 2002 (CC) {published data only}
- Furr‐Holden CD, Ialongo NS, Anthony JC, Petras H, Kellam SG. Developmentally inspired drug prevention: middle school outcomes in a school‐based randomised prevention trial. Drug and Alcohol Dependence 2004;73:149‐58. [DOI] [PubMed] [Google Scholar]
- Ialongo NS, Werthamer L, Kellam SG, Brown CH, Wang S, Lin Y. Proximal impact of two first‐grade preventive interventions on the early risk behaviours for later substance abuse, depression, and antisocial behavior. American Journal of Community Psychology 1999;27(5):599‐641. [DOI] [PubMed] [Google Scholar]
- Lambert SF, Brown TL, Phillips CM, Ialongo NS. The relationship between perceptions of neighbourhood characteristics and substance use among urban African American adolescents. Amerian Journal of Community Psychology 2004;34(3/4):205‐18. [DOI] [PubMed] [Google Scholar]
- Ramchand R, Ialong NS, Chilcoat HD. The effect of working for pay on adolescent tobacco use. American Journal of Public Health 2007;97(11):2056‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramchand R, Ialongo NS, Chilcoat HD. Sex differences in the linkage between adolescent work experience and alcohol, tobacco, and marijuana use in an urban environment. 67th Annual Scientific Meeting of the College on Problems of Drug Dependence. 2005.
- Storr CL, Ialongo NS, Kellam SG, Anthony JC. A randomised controlled trial of two primary school intervention strategies to prevent early onset tobacco smoking. Drug and Alcohol Dependence 2002;66(1):51‐60. [DOI] [PubMed] [Google Scholar]
- Wang Y, Browne DC, Petras H, Stuart EA, Wagner FA, Lambert SF, et al. Depressed mood and the effect of two universal first grade preventive interventions on survival to the first tobacco cigarette smoked among urban youth. Drug and Alcohol Dependence 2009;100(3):194‐203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Ialongo N, Wagner FA, Lambert SF, Storr CL, Browne DC. Gender differences in the efficacy of intervention trials on preventing tobacco smoking among children and adolescents. 68th Annual Scientific Meeting of the College on Problems of Drug Dependence. 2006.
- Wang Y, Storr CL, Green KM, Zhu S, Stuart EA, Lynne‐Landsman SD, et al. The effect of two elementary school‐based preventions on being offered tobacco and the transition to smoking. Drug and Alcohol Dependence 2012;120:202‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Storr 2002 (FSP) {published data only}
St Pierre 2005 (Adult) {published data only}
- Pierre TL, Osgood DW, Mincemoyer CC, Kaltreider DL, Kauh TJ. Results of an independent evaluation of Project ALERT delivered in schools by cooperative extension. Pevention Science 2005;6(4):305‐17. [DOI] [PubMed] [Google Scholar]
- Pierre TL, Osgood DW, Siennick SE, Kauh TJ, Burden FF. Project ALERT with outside leaders: What leader characteristics are important for success?. Prevention Science 2007;8:51‐64. [DOI] [PubMed] [Google Scholar]
St Pierre 2005 (Teen) {published data only}
Sun 2008 (Cognitive) {published data only}
- Sun P, Sussman S, Dent CW, Rohrbach LA. One‐year follow‐up evaluation of Project Towards No Drug Abuse (TND‐4). Preventive Medicine 2008;47(4):438‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sun 2008 (Combined) {published data only}
Sussman 1993 {published data only}
- Burton D, Chakravorty B, Weeks K, Flay BR, Dent C, Stacy A, et al. Outcome of a tobacco use cessation randomised trial with high‐school students. Substance Use & Misuse 2009;44(7):965‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dent CW, Sussman S, Stacy AW, Craig S, Burton D, Flay BR. Two‐year behavior outcomes of Project Towards No Tobacco Use. Journal of Consulting and Clinical Psychology 1995;63:676‐7. [DOI] [PubMed] [Google Scholar]
- Sussman S, Dent CW, Stacy AW, Hodgson CS, Burton D, Flay BR. Project Towards No Tobacco Use: implementation, process and post‐test knowledge evaluation. Health Education Research 1993;8:109‐23. [DOI] [PubMed] [Google Scholar]
- Sussman S, Dent CW, Stacy AW, Sun P, Craig S, Simon TR, et al. Project Towards No Tobacco Use: 1‐year behavior outcomes. American Journal of Public Health 1993;83:1245‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner GE, Burciaga C, Sussman S, Kleinselski E, Craig S, Dent CW, et al. Which lesson components mediate refusal assertion skill improvement in school‐based adolescent tobacco use prevention. International Journal of the Addictions 1993;28(8):749‐66. [DOI] [PubMed] [Google Scholar]
Sussman 1995 TND1 CHS C {published data only}
- Dent CW, Galaif ER, Sussman S, Stacy AW. Use of the "Theme Study" as means of curriculum development in continuation high schools. Journal of Drug Education 1996;26(4):377‐93. [DOI] [PubMed] [Google Scholar]
- Dent CW, Sussman S, Hennesy M, Galaif ER, Stacy AW, Moss MA, et al. Implementation and process evaluation of a school‐based drug abuse prevention program Project Towards No Drug Abuse. Journal of Drug Education 1998;28(4):361‐75. [DOI] [PubMed] [Google Scholar]
- Simon TR, Sussman S, Dahlberg LL, Dent CW. Influence of a substance abuse prevention curriculum on violence‐related behavior. American Journal of Health Behavior 2002;26(2):103‐10. [DOI] [PubMed] [Google Scholar]
- Sun P, Unger JB, Sussman S. A new measure of smoking initiation and progression among adolescents. American Journal of Health Behavior 2005;29(1):3‐11. [DOI] [PubMed] [Google Scholar]
- Sun W, Skara S, Sun P, Dent CW, Sussman S. Project Towards No Drug Abuse: Long‐Term substance use outcomes evaluation. Preventive Medicine 2006;42:188‐192. [DOI] [PubMed] [Google Scholar]
- Sussman S. Development of a school‐based drug abuse prevention curriculum for high risk youths. Journal of Psychoactive Drugs 1996;28(2):169‐82. [DOI] [PubMed] [Google Scholar]
- Sussman S, Craig S, Simon TR, Galaif ER. School‐as‐community activity selection at continuation high schools. Substance Use & Misuse 1997;32(2):113‐31. [DOI] [PubMed] [Google Scholar]
- Sussman S, Dent CW. Project Towards No Drug Abuse. In: Hansen WB, Giles SM, Fearnow‐Kenney editor(s). Increasing Drug Prevention Effectiveness: Readings for Educators. Clemmons N.C.: Tanglewood Research, 1999:1‐10. [Google Scholar]
- Sussman S, Dent CW, Caig S, Ritt‐Olsen A, McCuller WJ. Development and immediate impact of a self‐instruction curriculum for an adolescent indicated drug abuse prevention trial. Journal of Drug Education 2002;32(2):121‐37. [DOI] [PubMed] [Google Scholar]
- Sussman S, Dent CW, Simon TR, Stacy AW, Galaif ER, Moss AM, et al. Immediate impact of social influence‐oriented substance abuse prevention curricula in traditional and continuation high schools. Drugs & Society 1995;8(3/4):65‐81 (Simultaneous publication in: Prevention Practice in Substance Abuse. CG Leukefeld & RR Clayton (eds). The Haworth Press Inc. 1995, pp. 65‐81). [Google Scholar]
- Sussman S, Dent CW, Stacy AW. Project Towards No Drug Abuse: A review of the findings and future directions. American Journal of Health Behavior 2002;26(5):354‐65. [DOI] [PubMed] [Google Scholar]
- Sussman S, Dent CW, Stacy AW, Craig S. One‐year outcomes of Project Towards No Drug Abuse. Preventive Medicine 1998;27:632‐42. [DOI] [PubMed] [Google Scholar]
- Sussman S, Galaif ER, Newman R, Hennesy M, Pentz MA, Dent CW, et al. Implementation and process evaluation of a student "School‐as‐Community" group. Evaluation Review 1997;21(1):94‐123. [DOI] [PubMed] [Google Scholar]
- Sussman S, Simon TR, Dent CW, Stacy AW, Galaif ER, Moss AM, et al. Immediate impact of thirty‐two drug use prevention activities among students at continuation high schools. Substance Use & Misuse 1997;32(3):265‐81. [DOI] [PubMed] [Google Scholar]
- Sussman S, Stacy AW, Dent CW, Simon TR, Galaif ER, Moss MA, et al. Continuation high schools: Youth at risk for drug abuse. Journal of Drug Education 1995;25(3):191‐209. [DOI] [PubMed] [Google Scholar]
- Sussman S, Sun P, McCuller WJ, Dent CW. Project Towards No Drug Abuse: two‐year outcomes of a trial that compares health educator delivery to self‐instruction. Preventive Medicine 2003;37:155‐62. [DOI] [PubMed] [Google Scholar]
- Sussman S, Yang D, Baezconde‐Garbanati L, Dent CW. Drug abuse prevention program development: Results among Latino and non‐Latino white adolescents. Evaluation & the Health Professions 2003;26:355‐79. [DOI] [PubMed] [Google Scholar]
Sussman 1995 TND1 CHS SAC {published data only}
Sussman 2007 {published data only}
- Sun P, Miyano J, Rohrbach LA, Dent CW, Sussman S. Short‐term effects of Project EX‐4: A classroom‐based prevention and cessation intervention program. Addictive Behaviors 2007;32:342‐350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S, Miyano J, Rohrbach LA, Dent CW, Sun P. Corrigendum to 'Six‐month and 1‐year effects of Project EX‐4, a classroom‐based smoking prevention and cessation intervention program. Addictive Behaviors 2010;35(8):803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S, Miyano J, Rohrbach LA, Dent CW, Sun P. Six‐month and one‐year effects of Project EX‐4: A classroom‐based smoking prevention and cessation intervention program. Addictive Behaviors 2007;32:3005‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Telch 1990 (No peers) {published data only}
Telch 1990 (Peers) {published data only}
- Telch MJ, Miller LM, Killen JD, Cooke S, Maccoby N. Social influences approach to smoking prevention: The effects of videotape delivery with and without same‐age peer leader participation. Addictive Behaviors 1990;15:21‐8. [DOI] [PubMed] [Google Scholar]
Unger 2004 (CHIPS) {published data only}
Unger 2004 (FLAVOR) {published data only}
- Johnson CA, Cen S, Gallaher P, Palmer PH, Xiao L, Ritt‐Olson A, et al. Why smoking prevention programs sometimes fail. Does effectiveness depend on sociocultural context and individual characteristics?. Cancer Epidemiology, Biomarkers & Prevention 2007;16(6):1043‐9. [DOI] [PubMed] [Google Scholar]
- Johnson CA, Unger JB, Ritt‐Olson A, Palmer PH, Cen SY, Gallaher P, et al. Smoking prevention for ethnically diverse adolescents; 2‐year outcomes of a multicultural, school‐based smoking prevention curriculum in Southern California. Preventive Medicine 2005;40:842‐52. [DOI] [PubMed] [Google Scholar]
- Unger JB, Chou CP, Palmer PH, Ritt‐Olson A, Gallaher P, Cen S, et al. Project FLAVOR: 1‐year outcomes of a multicultural, school‐based smoking prevention curriculum for adolescents. American Journal of Public Health 2004;94(2):263‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unger JB, Gallaher P, Palmer PH, Baezconde‐Garbanati L, Trinidad DR, Cen S, et al. No news is bad news: Characteristics of adolescents who provide neither parental consent nor refusal for participation in school‐based survey research. Evaluation Review 2004;28(1):52‐63. [DOI] [PubMed] [Google Scholar]
- Valente TW, Hoffman BR, Ritt‐Olson A, Lichtman K, Johnson CA. Effects of a social‐network method for group assignment strategies on peer‐led tobacco prevention programs in schools. American Journal of Public Health 2003;93:1837‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valente TW, Unger JB, Ritt‐Olson A, Cen SY, Anderson JC. The interaction of curriculum type and implementation method on 1‐year smoking outcomes in a school‐based prevention program. Health Education Research 2006;21(3):315‐24. [DOI] [PubMed] [Google Scholar]
- Weiss JW, Mouttapa M, Cen S, Johnson CA, Unger J. Longitudinal effects of hostility, depression, and bullying on adolescent smoking initiation. Journal of Adolescent Health 2011;48(6):591‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Valente 2007 (TND) {published data only}
- Valente TW, Ritt‐Olson A, Stacy A, Unger JB, Okamoto J, Sussman S. Peer acceleration: Effects of a social network tailored substance abuse prevention program among high‐risk adolescents. Addiction 2007;102(11):1804‐15. [DOI] [PubMed] [Google Scholar]
Valente 2007 (TNDNetwork) {published data only}
Van Lier 2009 {published data only}
- Huizink AC, Lier PA, Crijnen AA. Attention deficit hyperactivity disorder symptoms mediate early‐onset smoking. European Addiction Research 2009;15(1):1‐9. [DOI] [PubMed] [Google Scholar]
- Lier P, Huizink A, Crijnen A. Impact of a preventive intervention targeting childhood disruptive behavior problems on tobacco and alcohol initiation from age 10 to 13 years. Drug and Alcohol Dependence 2009;100(3):228‐33. [DOI] [PubMed] [Google Scholar]
- Lier PA, Huizink A, Vuijk P. The role of friends' disruptive behavior in the development of children's tobacco experimentation: results from a preventive intervention study. Journal of Abnormal Child Psychology 2011;39:45‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lier PAC, Muthen BO, Sar RM, Crijnen AAM. Preventing disruptive behaviour in elementary schoolchildren: impact of a universal classroom‐based intervention. Journal of Consulting and Clincial Psychology 2004;72(3):467‐78. [DOI] [PubMed] [Google Scholar]
Vaughan 2007 {unpublished data only}
Villalbí 1993 {published data only}
- Villalbí JR, Aubà J, Garcia González A. Results of a school addictive substances abuse prevention program: the Barcelona PASE pilot project [Resultados de un programa escolar de prevención del abuso de sustancia adictivas: proyecto piloto PASE de Barcelona]. Gaceta Sanitaria 1993;7:70‐7. [PubMed] [Google Scholar]
- Villalbí JR, Aubà J, García‐González A. Evaluation of a project of primary prevention of smoking: the Barcelona PASE project [Evaluacion de un proyecto de prevencion primaria del tabaquismo: el proyecto piloto PASE de Barcelona]. Revista de Sanidad E Higiene Publica (Madrid) 1992;66:143‐8. [PubMed] [Google Scholar]
Walter 1985 {published data only}
- Walter HJ. Primary prevention of chronic disease among children: The school‐based "Know Your Body" intervention trials. Health Education Quarterly 1989;16(2):201‐4. [DOI] [PubMed] [Google Scholar]
- Walter HJ, Hofman A, Connelly PA, Barrett LT, Kost KL. Primary prevention of chronic disease in childhood: Changes in risk factors after one year of intervention. American Journal of Epidemiology 1985;122:772‐81. [DOI] [PubMed] [Google Scholar]
- Walter HJ, Hofman A, Vaughan RD, Wynder EL. Modification of risk factors for coronary heart disease. Five‐year results of a school‐based intervention trial. New England Journal of Medicine 1988;318(17):1093‐100. [DOI] [PubMed] [Google Scholar]
- Walter HJ, Wynder EL. The development, implementation, evaluation, and future directions of a chronic disease prevention program for children: The "Know Your Body" studies.. Preventive Medicine 1989;18:59‐71. [DOI] [PubMed] [Google Scholar]
Walter 1986 {published data only}
- Walter HJ. Primary prevention of chronic disease among children: The school‐based "Know Your Body" intervention trials. Health Education Quarterly 1989;16(2):201‐4. [DOI] [PubMed] [Google Scholar]
- Walter HJ, Hofman A, Barrett LT, Connelly PA, Kost KL, Walk EH, et al. Primary prevention of cardiovascular disease among children: three year results of a randomised intervention trial. In: Hetzel BS, Berenson GS editor(s). Cardiovascular risk factors in childhood: Epidemiology and prevention. Amsterdam: Elsevier North Holland Biomed, 1987:161‐81. [Google Scholar]
- Walter HJ, Hofman A, Connelly PA, Barrett LT, Kost KL. Coronary heart disease prevention in childhood: One‐year results of a randomised intervention study. American Journal of Preventive Medicine 1986;2:239‐49. [PubMed] [Google Scholar]
- Walter HJ, Hofman A, Vaughan RD, Wynder EL. Modification of risk factors for coronary heart disease. Five‐year results of a school‐based intervention trial. New England Journal of Medicine 1988;318(17):1093‐100. [DOI] [PubMed] [Google Scholar]
- Walter HJ, Vaughan RD, Wynder EL. Primary prevention of cancer among children: Changes in cigarette smoking and diet after six years of intervention. Journal of National Cancer Institute 1989;81:995‐9. [DOI] [PubMed] [Google Scholar]
- Walter HJ, Wynder EL. The development, implementation, evaluation, and future directions of a chronic disease prevention program for children: The "Know Your Body" studies.. Preventive Medicine 1989;18:59‐71. [DOI] [PubMed] [Google Scholar]
Weichold 2011 (Peer) {published data only}
Weichold 2012 (Teacher) {published data only}
- Weichold K, Silbereisen RK. Peers and teachers as facilitators of the Life Skills Program IPSY ‐ Results from a pilot study. Sucht 2012;58:247‐58. [Google Scholar]
Wen 2010 {published data only}
- Wen X, Chen W, Gans KM, Colby SM, Lu C, Liang C, et al. Two‐year effects of a school‐based prevention programme on adolescent cigarette smoking in Guangzhou, China: a cluster randomised trial. International Journal of Epidemiology 2010;39(3):860‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen XZ, Chen WQ, Lu CY, Liang CH, Zhang CX, Han K, et al. Process evaluation on a health promotion model regarding smoking prevention among Chinese secondary school students. Zhonghua Liu Xing Bing Xue Za Zhi 2007;28(3):224‐8. [PubMed] [Google Scholar]
Werch 2005 {published data only}
- Werch C, Moore MJ, Diclemente CC, Bledsoe R, Jobli E. A multi health behavior intervention integrating physical activity and substance use prevention for adolescents. Prevention Science 2005;6(3):213‐26. [DOI] [PubMed] [Google Scholar]
Zheng 2005 {published data only}
- Zheng PP, Fu YY, Yang SY, Cui HW, Guo FX, Ye TT, et al. Smoking prevention and control among elementary school students in Xuhui district, Shanghai. Zhonghua liuxingbingxue zazhi 2005;26(10):782‐5. [PubMed] [Google Scholar]
References to studies excluded from this review
Aarø 1983 {published data only}
- Aarø LE, Bruland E, Hauknes A, Løchsen PM. Smoking among Norwegian schoolchildren 1975‐1980. III. The effect of anti‐smoking campaigns. Scandinavian Journal of Psychology 1983;24:277‐83. [DOI] [PubMed] [Google Scholar]
- Aarø LE, Hauknes A, Berglund EL. Smoking among Norwegian schoolchildren 1975‐1980. II. The influence of the social environment. Scandinavian Journal of Psychology 1981;22:291‐309. [DOI] [PubMed] [Google Scholar]
Abernathy 1994 {published data only}
- Abernathy TJ. Compliance for Kids: A community‐based tobacco prevention project. Canadian Journal of Public Health 1994;March‐April:82‐4. [PubMed] [Google Scholar]
Andrews 1984 {published data only}
- Andrews RL, Hearne JT. Effects of Primary Grades Health Curriculum Project on student and parent smoking attitudes and behavior. Journal of School Health 1984;54:18‐20. [DOI] [PubMed] [Google Scholar]
Arciti 1986 {published data only}
- Arciti C, Santi L. An Italian program of information and education on cancer prevention and the hazards of smoking: A 3‐year report. Cancer Detection and Prevention 1986;9:421‐7. [PubMed] [Google Scholar]
Arora 2011 {published data only}
- Arora M, Stigler MH, Reddy KS. Effectiveness of health promotion in preventing tobacco use among adolescents in India: research evidence informs the National Tobacco Control Programme in India. Global Health Promotion 2011;18(1):9‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aslan 2007 {published data only}
- Aslan D, Sahin A. Adolescent peers and anti‐smoking activities. Promotion et Education 2007;14(1):36‐40. [PubMed] [Google Scholar]
Aßhauer 1999 {published data only}
- Aßhauer M, Hanewinkel R. Life skills training and drug prevention in the primary school: Development, implementation and evaluation of primary prevention [Lebenskompetenzfðrderung und Suchtprophylaxe in der Grundschule: Entwicklung, Implementation und Evaluation primär ‐präventiver Unterrichtseinheiten]. Zeitschrift für Gesundheitspsychologie 1999;7(4):158‐71. [Google Scholar]
Ausems 2002 {published data only}
- Ausems M, Mesters I, Breukelen G, Vries H. Do Dutch 11‐12 years old who never smoke, smoke experimentally or smoke regularly have different demographic backgrounds and perceptions of smoking?. European Journal of Public Health 2003;13(2):160‐7. [DOI] [PubMed] [Google Scholar]
- Ausems M, Mesters I, Breukelen G, Vries H. Short‐term effects of a randomised computer‐based out‐of‐school smoking prevention trial aimed at elementary school children. Preventive Medicine 2002;34:581‐9. [DOI] [PubMed] [Google Scholar]
- Ausems M, Mesters I, Breukelen G, Vries H. Smoking among Dutch elementary schoolchildren: gender‐specific predictors. Health Education Research 2009;24(5):818‐29. [DOI] [PubMed] [Google Scholar]
Banerjee 2007 {published data only}
- Banerjee SC, Greene K. Antismoking initiatives: effects of analysis versus production media literacy interventions on smoking‐related attitude, norm, and behavioral intention. Health Communication 2007;22(1):37‐48. [DOI] [PubMed] [Google Scholar]
Barrueco 1998 {published data only}
- Barrueco M, Vicente M, Garavís JL, García J, Blanco A, Rodríguez MC. Smoking prevention in the school: results of a 3‐year program [Prevención del tabaquismo en la escuela: resultados de un programa realizado durante 3 años]. Archivos de Bronconeumologia 1998;34(7):323‐8. [DOI] [PubMed] [Google Scholar]
Beaglehole 1978 {published data only}
- Beaglehole R, Brough D, Harding W. A controlled smoking intervention programme in secondary schools. New Zealand Medical Journal 1978;87:278‐80. [PubMed] [Google Scholar]
Becker 1992 {published data only}
- Becker HK, Agopian MW, Yeh S. Impact evaluation of Drug Abuse Resistance Education (DARE). Journal of Drug Education 1992;22:283‐91. [DOI] [PubMed] [Google Scholar]
Beets 2009 {published data only}
- Beets MW, Flay BR, Vuchinich S, Snyder FJ, Acock A, Li K, et al. Use of a social and character development program to prevent substance use, violent behaviours, and sexual activity among elementary‐school students in Hawaii. American Journal of Public Health 2009;99(8):1438‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Benni 2011 {published data only}
- Benni E, Sacco S, Roncarolo F, Bonfanti M, Tenconi MT. Evaluation of the efficacy of a school‐based program to prevent tobacco smoking among adolescents in Lombardy (Italy) [Valutazione dell'efficacia del programma ' Liberi di decidere' per la prevenzione del tabagismo nella Scuola Secondaria di secondo grado]. Igieni e Sanità Pubblica 2011;67(6):683‐95. [PubMed] [Google Scholar]
Bergamaschi 2000 {published data only}
- Bergamaschi A, Gambi A, Gentilini F, Monti C, Stampi S, Zanetti F. Tobacco smoking among high school students in Romagna (Italy) and evaluation of a prevention campaign. Substance Use & Misuse 2000;35(9):1277‐95. [DOI] [PubMed] [Google Scholar]
Berman 2011 {published data only}
- Berman B, Guthmann A, Crespi CM, Liu W. Development and testing of an anti tobacco school‐based curriculum for deaf and hard of hearing youth. American Annals of the Deaf 2011;155(5):592‐604. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bier 2011a {published data only}
- Bier MC, Schmidt SJ, Shields D. School‐based smoking prevention with media literacy: a pilot study. Journal of Media Literacy Education 2011;2(3):185‐98. [Google Scholar]
Biglan 1987a {published data only}
- Biglan A, Glasgow RE, Ary DV, Thompson R, Severson H, Lichtenstein E, et al. How generalisable are the effects of smoking prevention programs? Refusal skills training and parent messages in a teacher‐administered program. Journal of Behavioral Medicine 1987;10:613‐28. [DOI] [PubMed] [Google Scholar]
Bloor 2000 {published data only}
- Bloor M, Frankland J, Langdon NP, Robinson M, Allerston S, Catherine A, et al. A controlled evaluation of an intensive, peer‐Ied, schools‐based anti‐smoking programme. Health Education JoumaI 1999;58:17‐24. [Google Scholar]
Botvin 1989a {published data only}
- Botvin GJ, Dusenbury L, Baker E, James‐Ortiz S, Kerner J. A skills training approach to smoking prevention among Hispanic youth. Journal of Behavioral Medicine 1989;12(3):279‐96. [DOI] [PubMed] [Google Scholar]
Botvin 1989b {published data only}
- Botvin GJ, Batson HW, Witts‐Vitale S, Bess V, Baker E, Dusenbery L. A psychosocial approach to smoking prevention for urban black youth. Public Health Reports 1989;184(6):573‐82. [PMC free article] [PubMed] [Google Scholar]
Botvin 1992 {published data only}
- Botvin GJ, Dusenbury L, Baker E, James‐Ortiz S, Botvin EM. Smoking prevention among urban minority youth: Assessing effects on outcome and mediating variables. Health Psychology 1992;11(5):290‐9. [DOI] [PubMed] [Google Scholar]
Botvin 1997 {published data only}
- Botvin GJ, Epstein JA, Baker E, Diaz T, Ifill‐Williams M. School‐based drug abuse prevention with inner‐city minority youth. Journal of Child & Adolescent Substance Abuse 1997;6:5‐19. [Google Scholar]
Botvin 2000 {published data only}
- Botvin GJ, Griffin KW, Diaz T, Scheier LM, Williams C, Epstein JA. Preventing illicit drug use in adolescents: Long‐term follow‐up data from a randomised control trial of a school population. Addictive Behaviors 2000;25:769‐74. [DOI] [PubMed] [Google Scholar]
Botvin 2003 {published data only}
- Botvin GJ, Griffin KW, Paul E, Macaulay AP. Preventing tobacco and alcohol use among elementary school students through LIfe Skills Training. Journal of Child & Adolescent Substance Abuse 2003;12(4):1‐17. [Google Scholar]
Bowen 1991 {published data only}
- Bowen DJ, Dahl K, Mann SL, Peterson AV. Descriptions of early triers. Addictive Behaviors 1991;16:95‐101. [DOI] [PubMed] [Google Scholar]
Buhler 2008 {published data only}
- Buhler A, Schroder E, Silbereisen RK. The role of life skills promotion in substance abuse prevention: a mediation analysis. Health Education Research 2008;23(4):621‐32. [DOI] [PubMed] [Google Scholar]
Burke 1987 {published data only}
- Burke JA, Naughton MJ, Becker SL, Arbogast R, Louer RM, Krohn MD. The short‐term effects of competition and rewards in an adolescent smoking prevention program. Health Education Quarterly 1987;14(2):141‐52. [DOI] [PubMed] [Google Scholar]
Burke 1992 {published data only}
- Burke JA, Salazar A, Daughety V, Becker SL. Activating interpersonal influence in the prevention of adolescent tobacco use: An evaluation of Iowa's Program Against Smoking. Health Communication 1992;4(1):1‐17. [Google Scholar]
Calafat 1995 {published data only}
- Calafat A, Amengual M, Guimerans C, Rodriguez Martos A, Ruiz R. Decide yourself: Ten years of a school prevention program ['Tu decides': 10 años de un programa de prevención escolar]. Adicciones 1995;7:509‐26. [Google Scholar]
Caldwell 2009 {published data only}
- Caldwell LL, Bradley S, Coffman D. A person‐centred approach to individualizing a school‐based universal preventive intervention. American Journal of Drug and Alcohol Abuse 2009;35(4):214‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Calleja 2010 {published data only}
- Calleja N, Pick S, Reidi L, Gonzalez‐Forteza C. Smoking prevention programs for girls. Salud Mental 2010;33(5):419‐27. [Google Scholar]
Calman 1985 {published data only}
- Calman ALH, Carmichael S, Deans HG, Calman KC. Development of a primary school health education programme with special emphasis on the prevention of cigarette smoking. Health Education Journal 1985;44:65‐8. [Google Scholar]
Charlton 1986 {published data only}
- Charlton A. Evaluation of a family‐linked smoking programme in primary schools. Health Education Journal 1986;45(3):140‐4. [Google Scholar]
Chen 2006 {published data only}
- Chen X, Fang X, Li X, Stanton B, Lin D. Stay away from tobacco: a pilot trial of a school‐based adolescent smoking prevention program in Beijing, China. Nicotine & Tobacco Research 2006;8(2):227‐37. [DOI] [PubMed] [Google Scholar]
Connell 1985 {published data only}
- Connell DB, Turner RR, Mason EF. Summary of findings of the School Health Education Evaluation: Health Promotion Effectiveness, Implementation, and Costs. Journal of School Health 1985;55(8):316‐21. [DOI] [PubMed] [Google Scholar]
Cote 2006 {published data only}
- Cote F, Godin G, Gagne C. Efficiency of an evidence‐based intervention to promote and reinforce tobacco abstinence among elementary schoolchildren in a school transition period. Health Education & Behavior 2006;33(6):747‐59. [DOI] [PubMed] [Google Scholar]
Cruz 2009 {published data only}
- Cruz GG, Ferrero MB, Coca IA, Maderuelo JA, Garcia MT. Program for the prevention of smoking in secondary school students. Archivos de Broncomeumologia 2009;45(1):16‐23. [DOI] [PubMed] [Google Scholar]
Danhua 2005 {published data only}
- Danhua L, Xiaoyi F. Effects of different leaders on preventing adolescents' smoking behavior. Psychological Science (China) 2005;28(3):702‐5. [Google Scholar]
Davis 1995 {published data only}
- Davis SM, Lambert LC, Gomez Y, Skipper B. Southwest cardiovascular curriculum project: study findings for American Indian elementary students. Journal of Health Education 1995;26 Suppl:S72‐S81. [Google Scholar]
De Jong 1987 {published data only}
- Jong W. A short‐term evaluation of Project DARE (Drug Abuse Resistance Education): Preliminary indications of effectiveness. Journal of Drug Education 1987;17(4):279‐94. [DOI] [PubMed] [Google Scholar]
Del Greco 1986 {published data only}
- Greco L, Breitbach L, Rumer S, McCarthy RH, Suissa S. Four‐year results of a youth smoking prevention program using assertiveness training. Adolescence 1986;21(83):631‐40. [PubMed] [Google Scholar]
Dielman 1985 {published data only}
- Dielman TE, Lorenger AT, Leech SL, Lyons AL, Klos DM, Horvath WJ. Fifteen‐month follow‐up results of an elementary school based smoking prevention project. Resisting pressures to smoke. Hygie 1985;4:28‐35. [PubMed] [Google Scholar]
Donato 1994 {published data only}
- Donato F, Monarca S, Savaresi AS, Coppini C, Olivetti A, Zanardini A, et al. Health education and smoking: a controlled study of an intervention carried out among the junior high school students in a local health screening unit [Educazione e fumo: studio controllato dell'efficaci di un intervento svolto tra studenti di scuola media inferiore dio una USSl]. Annale Igiene 1994;6:729‐39. [PubMed] [Google Scholar]
Dupont 1984 {published data only}
- Dupont PJ, Jason LA. Assertiveness training in a preventive drug education program. Journal of Drug Education 1984;14:369‐78. [DOI] [PubMed] [Google Scholar]
Elder 1989 {published data only}
- Elder JP, Atkins C, Moor C, Edwards CC, Golbeck A, Hovell MF, et al. Prevention of tobacco use among adolescents in public schools in San Diego County, U.S. A.. Sozial und Praeventivmedizin 1989;34:24‐9. [DOI] [PubMed] [Google Scholar]
Emam Hadi 2008 {published data only}
- Emam Hadi MA, Jalilvand M, Hadian M, Heydari G. Efficacy of different methods in decreasing the students' tendency towards smoking. Tanaffos 2008;7(3):53‐8. [Google Scholar]
Epstein 2000a {published data only}
- Epstein JA, Griffin KW, Botvin GJ. Competence skills help deter smoking among inner city adolescents. Tobacco Control 2000;9:33‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Errecart 1991 {published data only}
- Errecart MT, Walberg HJ, Ross JG, Gold RS, Fiedler JL, Kolbe LJ. Effectiveness of teenage health teaching modules. Journal of School Health 1991;61:26‐30. [DOI] [PubMed] [Google Scholar]
- Gold RS, Parcel GS, Walberg HJ, Luepker RV, Portnoy B, Stone EJ. Summary and conclusions of the THTM evaluation: The expert work group perspective. Journal of School Health 1991;61:39‐42. [Google Scholar]
- Ross JG, Gold RS, Lavin AT, Errecart MT, Nelson GD. Design of the Teenage Health Teaching Modules: Evaluation. Journal of School Health 1991;61(1):21‐5. [DOI] [PubMed] [Google Scholar]
Evans 1978 {published data only}
- Evans RI, Rozelle RM, Maxwell SE, Raines BE, Dill CA, Guthrie TJ. Social modelling films to deter smoking in adolescents: Results of a three‐year field investigation. Journal of Applied Psychology 1981;66(4):399‐414. [Google Scholar]
- Evans RI, Rozelle RM, Mittelmark MB, Hansen WB, Bane AL, Havis J. Deterring the onset of smoking in children: Knowledge of immediate physiological effects and coping with peer pressure, media pressure, and parent modelling. Journal of Applied Social Psychology 1978;8:126‐35. [Google Scholar]
Evans 1981 {published data only}
- Evans RI, Rozelle RM, Maxwell SE, Raines BE, Dill CA, Guthrie TJ, et al. Social modelling films to deter smoking in adolescents: Results of a three‐year field investigation. Journal of Applied Psychology 1981;66(4):399‐414. [Google Scholar]
Flay 1987 {published data only}
- Flay BR, Hansen WB, Johnson CA, Collins LM, Dent CW, Dwyer KM, et al. Implementaton effectiveness of a social influences smoking prevention program using schools and television. Health Education Research 1987;2(4):385‐400. [Google Scholar]
Flay 2004 {published data only}
- Flay BR, Graumich S, Segawa E, Burns JL, Holliday MY. Effects of 2 prevention programs on high‐risk behaviours among African American youth. Archives of Pediatrics & Adolescent Medicine 2004;158:377‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu LC, Flay BR. Evaluating mediation in longitudinal multivariate data: Mediation effects for the Aban Aya Youth Project Drug Prevention Program. Prevention Science 2009;10:197‐207. [DOI] [PubMed] [Google Scholar]
Flynn 1992 {published data only}
- Flynn BS, et al. Cigarette smoking prevention effects of mass media and school interventions targeted to gender and age groups. Journal of Health Education 1995;26(2):s45‐51. [Google Scholar]
- Flynn BS, Worden JK, Secker‐Walker RH, Badger GJ, Geller BM, Costanza MC. Prevention of cigarette smoking through mass media intervention and school programs. American Journal of Public Health 1992;82:827‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn BS, Worden JK, Secker‐Walker RH, Pirie PL, Badger GJ, Carpenter JH. Long‐term responses of higher and lower risk youth to smoking prevention interviews. Preventive Medicine 1997;26:389‐94. [DOI] [PubMed] [Google Scholar]
- Flynn BS, Worden JK, Secker‐Walker RH, Pirie PL, Badger GJ, Carpenter JH, et al. Mass media and school interventions for cigarette smoking prevention: Effects 2 years after completion. American Journal of Public Health 1994;84:1148‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Frydman 1985 {published data only}
- Frydman M. Application and evaluation of antitobacco programs in schools [Mise au point, application et évaluation de programmes anti‐tabac en milieu scolaire]. Psychotropes 1985;2(2):83‐90. [Google Scholar]
Gilchrist 1987 {published data only}
- Gilchrist LD, Schinke SP, Trimble JE, Cvetkovich GT. Skills enhancement to prevent substance abuse among American‐Indian adolescents. International Journal of Addictions 1987;22:869‐79. [DOI] [PubMed] [Google Scholar]
Gillies 1984 {published data only}
- Gillies PA, Wilcox B. Reducing the risk of smoking amongst the young. Public Health 1984;98:49‐54. [DOI] [PubMed] [Google Scholar]
Gingiss 2006 {published data only}
- Gingiss P, Boerm M, Roberts‐Gray C. Follow‐up comparisons of intervention and comparison schools in a state tobacco prevention and control initiative. Journal of School Health 2006;76(3):98‐103. [DOI] [PubMed] [Google Scholar]
Gislason 1995 {published data only}
- Gislason T, Yngvadottir A, Benediktsdottir B. Alcohol consumption, smoking and drug abuse among Icelandic teenagers: A study into the effectiveness of the 'Skills for Adolescence' programme. Drugs: Education, Prevention and Policy 1995;2(3):243‐58. [Google Scholar]
Gohlke 1989 {published data only}
- Gohlke H, Gohlke‐Bärwolf C, Peters K, Schmitt M, Katzenstein M, Gaida C, et al. Prevention of cigarette smoking at school: A prospective controlled study [Prävention des Zigarettenrauchens in der Schule: Eine prospektive kontrollierte Studie.]. Deutsche Medizinische Wochenschrift 1989;114. Jahrgang Nr. 46:1780‐4. [DOI] [PubMed] [Google Scholar]
Gomez 2009 {published data only}
- Gomez CG, Barrueco FM, Aparicio CI, Maderuelo JA, Torrecilla GM. Program for the prevention of smoking in secondary school students. Archivos de Bronconeumologia 2009;45(1):16‐23. [DOI] [PubMed] [Google Scholar]
Gomez Fraguela 2003 {published data only}
- Gomez Fraguela JA, Luengo Martin A, Romero Trinanes E. Drug‐abuse prevention in the school: Four‐year follow‐up of a programme. Psychology in Spain 2003;7(1):29‐38. [Google Scholar]
Gordon 1997 {published data only}
- Gordon I, Whitear B, Guthrie D. Stopping them starting: evaluation of a community‐based project to discourage teenage smoking in Cardiff. Health Education Journal 1997;56:42‐50. [Google Scholar]
Gritz 1992 {published data only}
- Gritz ER, Berman BA, Bastani R, Wu M. A randomised trial of a self‐help smoking cessation intervention in a non volunteer female population: Testing the limits of the public health model. Health Psychology 1992;11(5):280‐9. [DOI] [PubMed] [Google Scholar]
Guilamo‐Ramos 2010 {published data only}
- Guilamo‐Ramos V, Jaccard J, Dittus P, Gonzalez B, Bouris A, Banspach S. The linking lives health education program: a randomised clinical trial of a parent‐based tobacco use prevention program for African American and Latino youths. American Journal of Public Health 2010;100(9):1641‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hamm 1994 {published data only}
- Hamm NH. Outcomes of the Minnesota smoking prevention program. Psychological Reports 1994;75:880‐2. [DOI] [PubMed] [Google Scholar]
Hanewinkel 1996 {published data only}
- Hanewinel R, Asshauer M. Effects of a smoking prevention programme in primary schools. In: Tudor‐Smith C editor(s). Working together for better health: tackling tobacco. Cardiff: Health promotion Wales, 1999:179‐91. [Google Scholar]
- Hanewinkel R. The "Smokefree School:" Study of primary‐ and secondary‐preventive interventions for parents, teachers and schoolchildren [Die "Rauchfreie Schule": Studie zu primär‐ und secundärpräventiven Interventionen für Eltern, Lehrer und Schüler]. Forum Sucht Band 14 Landschaftsverband Wesfalen‐Lippe Koordinationstelle für Drogenfragen. Schloß Eringerfeld, 19./20 November 1996.
Hanewinkel 2003 {published data only}
- Hanewinkel R, Wiborg G. Primary and secondary prevention of smoking in adolescence: Effects of the "Be Smart ‐ Don't Start" campaign [Primär‐ und Sekundärprävention des Rauchens im Jugendalter: Effekte der Kampagne "Be Smart ‐ Don't Start."]. Gesundheitswesen 2002;64:492‐8. [DOI] [PubMed] [Google Scholar]
- Hanewinkel R, Wiborg G. Promotion of nonsmoking in the school: Results of a prospective controlled intervention study [Förderung des Nichtrauchens in der Schule: Ergebnisse einer prospektiven kontrollierten Interventionsstudie]. Sucht 2003;49(6):333‐41. [Google Scholar]
- Wiborg G, Hanewinkel R. Effectiveness of the "Smoke‐Free Class Competition" in delaying the onset of smoking in adolescence. Preventive Medicine 2002;35:241‐249. [DOI] [PubMed] [Google Scholar]
- Wiborg G, Hanewinkel R, Kliche K‐O. Prevention of starting smoking through the campaign "Be Smart ‐ Don't Start": an analysis by type of school [Verhütung des Einstiegs in das Rauchen durch die Kampagne "Be Smart ‐ Don't Start ": eine Analyse nach Schularten]. Deutsche Medizinische Wochenschrift 2002;127:430‐6. [DOI] [PubMed] [Google Scholar]
- Wiborg, G, Hanewinkel R. Conception and process evaluation of a school non‐smoking competition [Konzeption und Prozessevaluation eines schulischen Nichtraucherwettbewerbs]. Sucht 2001;47(1):S25‐S32. [Google Scholar]
Hanewinkel 2004 {published data only}
- Hanewinkel R, Aßhauer M. Fifteen‐month follow‐up results of a school‐based life‐skills approach to smoking prevention. Health Education Research 2004;19(2):125‐37. [DOI] [PubMed] [Google Scholar]
Hansen 1982 {published data only}
- Hansen WB, Evans RI. Feedback versus information concerning carbon monoxide as an early intervention strategy in adolescent smoking. Adolescence 1982;17(65):90‐8. [PubMed] [Google Scholar]
Hansen 1988b {published data only}
- Hansen WB, Malotte CK, Fielding JE. Evaluation of a tobacco and alcohol abuse prevention curriculum for adolescents. Health Education Quarterly 1988;15(1):93‐114. [DOI] [PubMed] [Google Scholar]
- Hansen WB, Malotte CK, Fielding JE. Tobacco and alcohol prevention: Preliminary results of a four‐year study. Adolescent Psychiatry 1987;14:556‐75. [PubMed] [Google Scholar]
Hansen 1996 {published data only}
- Hansen WB. Pilot test results comparing All Stars program with seventh grade D.A.R.E.: Program integrity and mediating variable analysis. Substance Use & Misuse 1996;31(10):1359‐77. [DOI] [PubMed] [Google Scholar]
Hansen 1997 {published data only}
- Hansen WB, McNeal RB Jr. How D.A.R.E. works: An examination of program effects on mediating variables. Health Education & Behavior 1997;24(2):165‐76. [DOI] [PubMed] [Google Scholar]
Harmon 1993 {published data only}
- Harmon MA. Reducing the risk of drug involvement among early adolescents: An evaluation of Drug Abuse Resistance Education (DARE). Evaluation Review 1993;17(2):221‐39. [Google Scholar]
Harrell 1996 {published data only}
- Harrell JS, McMurray RG, Bangdiwala SI, Frauman AC, Gansky SA, Bradley CB. Effects of a school‐based intervention to reduce cardiovascular disease risk factors in elementary school children: The Cardiovascular Health in Children (CHIC) Study. Journal of Pediatrics 1996;128:797‐805. [DOI] [PubMed] [Google Scholar]
Harrell 1998 {published data only}
- Harrell JS, Bangdiwala SI, Deng S, Webb JP, Bradley CB. Smoking initiation in youth: The roles of gender, race, socioeconomics, and developmental status. Journal of Adolescent Health 1998;23:271‐9. [DOI] [PubMed] [Google Scholar]
Hawkins 2009 {published data only}
- Hawkins JD, Oesterle S, Brown EC, Arthur MW, Abbott RD, Fagan AA, et al. Resutls of a type 2 transitional research trial to prevent adolescent drug use and delinquency: a test of Communities that Care. Archives of Pediatrics & Adolescent Medicine 2009;163(9):789‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuklinski MR, Briney JS, Hawkins JD, Catalano RF. Cost‐benefit analysis of communities that care outcomes at eighth grade. Prevention Science 2012;13(2):150‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hecht 1993 {published data only}
- Hecht ML, Corman SR, Miller‐Rassulo M. An evaluation of the Drug Resistance Project: A comparison of film versus live performance media. Health Communication 1993;5:75‐88. [Google Scholar]
Hiemstra 2009 {published data only}
- Hiemstra M, Ringlever L, Otten R, Jackson C, Schayck OC, Engels RC. Efficacy of smoking prevention program 'smoke‐free kids': study protocol of a randomised controlled trial. BMC Public Health 2009;9:477. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgs 2000 {published data only}
- Higgs PE, Harbin RE, Edwards D, Higgs PC. Evaluation of a self‐directed smoking prevention and cessation program. Pediatric Nursing 2000;26(2):150‐5. [PubMed] [Google Scholar]
Hinz 2007 {published data only}
- Hinz A. A school‐based smoking prevention programme: results from a gender‐specific intervention for smokers and nonsmokers [Schulische Nikotinprävention. Ergebnisse einer raucherstatus‐ und geschlectergerechten Intervention]. Sucht: Zeitschrift fur Wissenschaft und Praxis 2007;53(1):42‐51. [Google Scholar]
Hodder 2011 {published data only}
- Hodder RK, Daly J, Freund M, Bowman J, Hazell T, Wiggers J. A school‐based resilience intervention to decrease tobacco, alcohol and marijuana use in high school students. BMC Public Health 2011;11:722. [DOI] [PMC free article] [PubMed] [Google Scholar]
Homel 1981 {published data only}
- Homel PJ, Daniels P, Reid TR, Lawson JS. Results of an experimental school‐based health development programme in Australia. International Journal of Health Education 1981;24:263‐70. [PubMed] [Google Scholar]
Hovell 1996 {published data only}
- Hovell MF, Slymen DJ, Jones JA, Hofstetter CR, Burkham‐Kreitner S, Conway TL, et al. An adolescent tobacco‐use prevention trial in orthodontic offices. American Journal of Public Health 1996;86(12):1760‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hrubá 2007 {published data only}
- Hrubá D, Zachovalová V, Matějová H, Daňková I. "Our Class Does Not Smoke"; The Czech version of the "Smoke‐Free Class Competition" Programme. Central European Journal of Public Health 2007;15(4):163‐166. [DOI] [PubMed] [Google Scholar]
Hruba 2012 {published data only}
- Hrubá D, Zaloudiková I. What limits the effectiveness of school‐based anti‐smoking programmes?. Central European Journal of Public Health 2012;20(1):18‐23. [DOI] [PubMed] [Google Scholar]
Hurd 1980 {published data only}
- Hurd PD, Johnson CA, Pechacek T, Bast LP, Jacobs DR, Luepker RV. Prevention of cigarette smoking in seventh grade students. Journal of Behavioral Medicine 1980;3:15‐28. [DOI] [PubMed] [Google Scholar]
- Luepker RV, Johnson CA, Murray DM, Pechacek T. Prevention of cigarette smoking: Three‐year follow‐up of an educational program for youth. Journal of Behavioral Medicine 1983;6:53‐62. [DOI] [PubMed] [Google Scholar]
Ishaq 2004 {published data only}
- Ishaq M, Khan SMI. The successful outcome of the role of the mass media & school program in the prevention of smoking amongst adolescent high school boys. Chest: Abstracts of original investigations. 2004:867.
Jason 1982 {published data only}
- Jason LA, Mollica M, Ferrone L. Evaluating an early secondary smoking prevention intervention. Preventive Medicine 1982;11:96‐102. [DOI] [PubMed] [Google Scholar]
Johnson 1986 {published data only}
- Johnson CA, Hansen WB, Collins LM, Graham JW. High school smoking prevention: Results of a three‐year longitudinal study. Journal of Behavioral Medicine 1986;9(5):439‐52. [DOI] [PubMed] [Google Scholar]
Katz 1989 {published data only}
- Katz RC, Robisch CM. Acquisition of smoking refusal skills in Junior High students. Addictive Behaviors 1989;14:201‐4. [DOI] [PubMed] [Google Scholar]
Kersch 1998 {published data only}
- Kersch B. Tobacco‐distance ‐ An evaluation criterion of drug prevention measures in schools with 13 to 16 year old students. Results of a longitudinal study in Leipzig, Germany ["Tabakdistanz" ‐ein Evaluationskriterium unterrichtlicher Suchtpraeventionsmaßnahmen bei 13‐ bis 16 jaehrigen Schuelerinnen und Schuelern. Ergebnisse einer Leipziger Laengschnittstudie]. Sucht 1998;44(1):15‐24. [Google Scholar]
Killen 1988 {published data only}
- Killen JD, Telch MJ, Robinson TN, Maccoby N, Taylor B, Farquhar JW. Cardiovascular disease risk reduction for tenth graders. A multiple‐factor school‐based approach. JAMA 1988;260(12):1728‐33. [PubMed] [Google Scholar]
Killen 1989 {published data only}
- Killen JD, Robinson TN, Telch MJ, Saylor KE, Maron DJ, Rich T, et al. The Stanford Adolescent Heart Health Program. Healh Education Quarterly 1989;16(2):263‐83. [DOI] [PubMed] [Google Scholar]
Kim 1982 {published data only}
- Kim S. Feeder Area Approach: An impact evaluation of a prevention program on student drug abuse. The International Journal of the Addictions 1982;17(2):305‐13. [DOI] [PubMed] [Google Scholar]
Kim 1993 {published data only}
- Kim S, McLeod JH, Shantzis C. An outcome evaluation of Here's Looking at You 2000. Journal of Drug Education 1993;23(1):67‐81. [DOI] [PubMed] [Google Scholar]
Knutsen 1991 {published data only}
- Knutsen SF, Knutsen R. The Tromso Survey: The Family Intervention Study ‐ the effect of intervention on some coronary risk factors and dietary habits, a 6‐year follow‐up. Preventive Medicine 1991;20:197‐212. [DOI] [PubMed] [Google Scholar]
Kolpin 2008 {published data only}
- Kolpin TG. Alcohol tobacco and other drugs prevention program for third grade students. Dissertation Abstracts International Section A: Humanities and Social Sciences 2008;69(4‐A):2008, pp‐A. [Google Scholar]
Kovach 2010 {published data only}
- Kovach, Clark H, Ringwalt CL, Hanley S, Shamblen SR. Project ALERT's effects on adolescents' prodrug beliefs: a replication and extension study. Health Education & Behavior 2010;37(3):357‐76. [DOI] [PubMed] [Google Scholar]
Kröger 2000 {published data only}
- Kröger C, Reese A. Substance abuse prevention in schools through life skills training‐results of a four year intervention study [Schulische Suchtprävention nach dem Lebenskompetenzkonzept‐ Ergebnisse einer vierjährigen Jnterventionsstudie]. Sucht 46;3:209‐17. [Google Scholar]
Kupersmidt 2010 {published data only}
- Kupersmidt JB, Scull TM, Austin EW. Media literacy education for elementary school substance use prevention: study of media detective. Pediatrics 2010;126(3):525‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kupersmidt 2012 {published data only}
- Kupersmidt JB, Scull TM, Benson JW. Improving media message interpretation processing skills to promote healthy decision making about substance use: The effects of the middle school media ready curriculum. Journal of Health Communication: International Perspectives 2012;17:546‐63. [DOI] [PubMed] [Google Scholar]
Lammers 1984 {published data only}
- Lammers JW, Kreuter MW, Smith BC. The effects of the SHCP on selected aspects of decision‐making among fifth graders. Health Education 1984;March/April:14‐17. [PubMed] [Google Scholar]
Ledwith 1985 {published data only}
- Ledwith F, Osman L. The evaluation of a secondary school smoking education intervention. Health Education Journal 1985;44(3):131‐5. [Google Scholar]
Lee 2007 {published data only}
- Lee PH, Wu DM, Lai HR, Chu NF. The impacts of a school‐wide no smoking strategy and classroom‐based smoking prevention curriculum on the smoking behavior of junior high school students. Addictive Behaviors 2007;32(10):2099‐107. [DOI] [PubMed] [Google Scholar]
Lillington 1984 {published data only}
- Lillington L, Royce J, Novak D, Ruvalcaba M, Chlebowski R. Evaluation of a smoking cessation program for pregnancy minority women. Cancer Practice 1995;3(3):157‐63. [PubMed] [Google Scholar]
Litrownik 2000 {published data only}
- Litrownik AJ, Elder JP, Campbell NR, Ayala GX, Slymen DJ, Parra‐Medina D, et al. Evaluation of a tobacco and alcohol use prevention program for Hispanic migrant adolescents: promoting the protective factor of parent‐child communication. Preventive Medicine 2000;31:124‐33. [DOI] [PubMed] [Google Scholar]
Lopez Gonalez 1998 {published data only}
- Lopez González ML, Comas Fuentes A, Herrero Puente P, Pereiro Gallo S, Fernández Carral M, Thomas H, et al. Intervención educativa escolar para prevenir el tabaquismo: evaluación del proceso. Rev Esp Salud Pública 1998;72:303‐318. [PubMed] [Google Scholar]
Luepker 1983 {published data only}
- Luepker RV, Johnson CA, Murray DM, Pechacek TF. Prevention of cigarette smoking: Three‐year follow‐up of an education program for youth. Journal of Behavioral Medicine 1983;6(1):53‐62. [DOI] [PubMed] [Google Scholar]
Lwegaba 2005 {published data only}
- Lwegaba A. Field trial to test and evaluate primary tobacco prevention methods in clusters of elementary schools in Barbados. West Indian Medical Journal 2005;54(5):283‐91. [DOI] [PubMed] [Google Scholar]
MacKinnon 1991 {published data only}
- MacKinnon DP, Johnson CA, Pentz MA, Dwyer JH, Hansen WB, Flay BR, et al. Mediating mechanisms in a school‐based drug prevention program: First‐year effects of the Midwestern Prevention Project. Health Psychology 1991;10(3):164‐72. [DOI] [PubMed] [Google Scholar]
Malcon 2011 {published data only}
- Malcon MC, Menezes AMB, Assuncao MCF, Neutzling MB, Challa P. Effectiveness of an educational intervention on smoking among school adolescents. Revista Brasileira de Epidemiologia 2011;14(1):63‐72. [Google Scholar]
- Malcon MC, Menezes AMB, Assuncao MCF, Neutzling MB, Hallal PC. Agreement between self‐reported smoking and cotinine concentration in adolescents: A validation study in Brazil. Journal of Adolescent Health 2008;43:226‐30. [DOI] [PubMed] [Google Scholar]
McAlister 1980 {published data only}
- McAlister A, Perry C, Killen J, Slinkard LA, Maccoby N. Pilot study of smoking, alcohol and drug abuse prevention. American Journal of Public Health 1980;70(7):719‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telch M, Killen JD, McAlister AL, Perry CL, Maccoby N. Long term follow‐up of a pilot project on smoking prevention with adolescents. Journal of Behavioral Medicine 1982;5:1‐8. [DOI] [PubMed] [Google Scholar]
McFall 1993 {published data only}
- McFall SL, Michener A, Rubin D, Flay BR, Mermelstein RJ, Burton D, et al. The effects of maintenance newsletters in a smoking cessation intervention. Addictive Behaviors 1993;18:151‐8. [DOI] [PubMed] [Google Scholar]
Metz 2006 {published data only}
- Metz AE, Fuemmeler BF, Brown RT. Implementation and assessment of an empirically validated intervention program to prevent tobacco use among African‐American middle‐school youth. Journal of Clinical Psychology in Medical Settings 2006;13(3):229‐38. [Google Scholar]
Moberg 1990 {published data only}
- Moberg DP, Piper DL. An outcome evaluation of Project Model Health: A middle school health promotion program. Health Education Quarterly 1990;17(1):37‐51. [DOI] [PubMed] [Google Scholar]
Morehouse 2000 {unpublished data only}
- Morehouse ER, Tobler NS. Third year cohort results and summary of Project SUCCESS over the three years. Project SUCCESS Final Report (obtained from the authors) 2000.
Moskowitz 1984 {published data only}
- Moskowitz JM, Malvin JH, Schaeffer GA, Schaps E. An experimental evaluation of a drug education course. Journal of Drug Education 1984;14:9‐22. [DOI] [PubMed] [Google Scholar]
- Moskowitz JM, Malvin JH, Schaeffer GA, Schaps E. Evaluation of a junior high school primary prevention program. Addictive Behaviors 1983;8:393‐401. [DOI] [PubMed] [Google Scholar]
- Moskowitz JM, Schaps E, Schaeffer GA, Malvin JH. Evaluation of a substance abuse prevention program for junior high students. International Journal of the Addictions 1984;19:419‐30. [DOI] [PubMed] [Google Scholar]
Murray 1982 {published data only}
- Murray M, Swan AV, Clarke G. Long term effect of a school based anti‐smoking programme. Journal of Epidemiology and Community Health 1984;38:247‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray M, Swan AV, Enock C, Johnson MRD, Banks MH, Reid DJ. The effectiveness of the Health Education Council's "My Body" Schools Health Education Project. Health Education Journal 1982;41:126‐32. [Google Scholar]
Murray 1984b {published data only}
- Murray M, Rona RJ, Morris RW, Tait N. The smoking and dietary behaviour of Lambeth schoolchildren. I. The effectiveness of an anti‐smoking and nutrition education programme for children. Public Health 1984;98:163‐72. [DOI] [PubMed] [Google Scholar]
Newman 1991 {published data only}
- Newman R, Smith C, Nutbeam D. Teachers' views of the 'Smoking and Me' Project. Health Education Journal 1991;50(3):107‐10. [Google Scholar]
Nichols 2006 {published data only}
- Nichols TR, Graber JA, Brooks‐Gunn J, Botvin GJ. Ways to say no: refusal skill strategies among urban adolescents. American Journal of Health Behavior 2006;30(3):227‐36. [DOI] [PubMed] [Google Scholar]
Nilsson 2006 {published data only}
- Nilsson M, Stenlund H, Bergstrom E, Weinehall L, Janlert U. It takes two: reducing adolescent smoking uptake through sustainable adolescent‐adult partnership. Journal of Adolescent Health 2006;39(6):880‐6. [DOI] [PubMed] [Google Scholar]
Nishioka 2005 {published data only}
- Nishioka N, Kawabata T, Minagawa K, Nakamura M, Ohshima A, Mochizuki Y. Three‐year follow‐up on the effects of a smoking prevention program for elementary school children with a quasi‐experimental design in Japan. Japanese Journal of Public Health 2005;52(11):971‐8. [PubMed] [Google Scholar]
- Nishioka N, Kawabata T, Minagawa KH, Nakamura M, Oshima A, Mochizuki Y. The short‐term effect of a smoking prevention program for the upper graders of elementary schools‐‐the results of intervention study for two years with quasi‐experimental design. [Japanese]. Nippon Koshu Eisei Zasshi 1996;43(6):434‐45. [PubMed] [Google Scholar]
Ofstad 2007 {published data only}
- Ofstad EH, Knudsen K, Skaare C, Svendsrud I, Tveit EJ, Gallefoss F, et al. A randomised controlled intervention study to prevent secondary school students from taking up smoking. American Thoracic Society International Conference, San Francisco, USA. May 18 ‐ 23 2007.
Öhrig 2001 {published data only}
- Öhrig E, Geiß HC, Haas G‐M, Schwandt P. The Prevention Education Program (PEP) Nuremberg: design and baseline data of a family‐oriented intervention study. International Journal of Obesity 2001;25(Suppl 1):589‐92. [DOI] [PubMed] [Google Scholar]
Olsen 1980 {published data only}
- Olsen LK, Redican KJ, Krus PH. The School Health Curriculum Project: A review of research studies. Health Education 1980;11(1):16‐21. [PubMed] [Google Scholar]
Parcel 1995 {published data only}
- Brink AG, Basen‐Engquist KM, O'Hara‐Tompkins NM, Parcel GS, Gottlieb NH, Lovato CY. Diffusion of an effective tobacco prevention program. Part 1: evaluation of the dissemination phase. Health Education Research 1995;10(3):283‐95. [DOI] [PubMed] [Google Scholar]
- Parcel GS, O'Hara‐Tompkins N, Harrist RB, Basen‐Engquist KM, McCormick LK, Gottlieb NH, et al. Diffusion of an effective tobacco prevention program. Part II: evaluation of the adoption phase. Health Education Research 1996;10(3):297‐307. [DOI] [PubMed] [Google Scholar]
Patrick 2009 {published data only}
- Patrick ME, Collins LM, Smith E, Caldwell L, Flisher A, Wegner L. A prospective longitudinal model of substance use onset among South African adolescents. Substance Use & Misuse 2009;44(5):647‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pederson 1981a {published data only}
- Pederson LL, Baskerville JC, Lefcoe NM. Change in smoking status among school‐aged youth: Impact of a smoking‐awareness curriculum, attitudes, knowledge and environmental factors. American Journal of Public Health 1981;71(12):1401‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pederson 1981b {published data only}
- Pederson LL, Stennett RG, Lefcoe NM. The effects of a smoking education program on the behavior, knowledge and attitudes of children in grades 4 and 6. Journal of Drug Education 1981;11:141‐9. [Google Scholar]
Pederson 1987 {published data only}
- Pederson LL, Lefcoe NM. Short‐ and long‐term prediction of self‐reported cigarette smoking in a cohort of later adolescents: report of an 8‐year follow‐up of public school students. Preventive Medicine 1987;16(3):432‐47. [DOI] [PubMed] [Google Scholar]
Pentz 1989 {published data only}
- Chou CP, Montgomery S, Pentz MA, Rohrbach LA, Johnson CA, Flay BR, et al. Effects of a community‐based prevention program on decreasing drug use in high‐risk adolescents. American Journal of Public Health 1998;88:944‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan L, Chou CP, Andreeva VA, Pentz MA. Trajectories of peer social influences as long‐term predictors of drug use from early through late adolescence. Journal of Youth & Adolescence 2009;38(3):454‐65. [DOI] [PubMed] [Google Scholar]
- Johnson CA, Pentz MA, Weber MD, Dwyer JH, Baer N, MacKinnon DP, et al. Relative effectiveness of comprehensive community programming for drug abuse prevention with high‐risk and low‐risk adolescents. Journal of Consulting and Clinical Psychology 1990;58:447‐56. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Johnson CA, Pentz MA, Dwyer JH, Hansen WB, Flay BR, et al. Mediating mechanisms in a school‐based drug prevention program: First‐effects of the Midwestern Prevention Project. Health Psychology 1991;10:164‐72. [DOI] [PubMed] [Google Scholar]
- Pentz MA, Dwyer JH, MacKinnon DP, Flay BR, Hansen WB, Wang EY, et al. A multi‐community trial for primary prevention of adolescent drug abuse. Effects on drug use prevalence. American Journal of Public Health 1989;261:3259‐66. [PubMed] [Google Scholar]
- Pentz MA, MacKinnon DP, Dwyer JH, Wang EYI, Hansen WB, Flay BR, et al. Longitudinal effects of the Midwestern Prevention Project on regular and experimental smoking in adolescents. Preventive Medicine 1989;18:304‐21. [DOI] [PubMed] [Google Scholar]
- Pentz MA, MacKinnon DP, Flay BR, Hansen WB, Johnson CA, Dwyer JH. Primary prevention of chronic diseases in adolescence: Effects of the Midwester prevention project on tobacco use. American Journal of Epidemiology 1989;130(4):713‐24. [DOI] [PubMed] [Google Scholar]
- Rohrbach LA, Hodgson CS, Broder BI, Montgomery SB, Flay B, Hansen WB, et al. Parental participation in drug abuse prevention: Results from the Midwestern Prevention Project. Journal of Research on Adolescence 1994;4(2):295‐317. [Google Scholar]
Perry 1980 {published data only}
- Perry C, Killen J, Telch M, Slinkard LA, Danaher BG. Modifying smoking behavior of teenagers: A school‐based intervention. American Journal of Public Health 1980;70:722‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry CL, Killen J, Slinkard LA. Peer teaching and smoking prevention among junior high students. Adolescence 1980;15(58):277‐81. [PubMed] [Google Scholar]
- Perry CL, Maccoby N, McAlister AL. Adolescent smoking prevention: A third year follow‐up. World Smoking and Health 1980;50:40‐5. [Google Scholar]
Perry 1990 {published data only}
- Perry CL, Pirie P, Holder W, Halper A, Dudovitz B. Parent involvement in cigarette smoking prevention: Two pilot evaluations of the "Unpuffables Program". Journal of School Health 1990;60(9):443‐7. [DOI] [PubMed] [Google Scholar]
Perry 1992 {published data only}
- Blackburn H, Luepker RV, Kline FG, et al. The Minnesota Heart Health Program: a research and demonstration project in cardiovascular disease prevention. In: Matarazzo JD, Weiss SM, Herd JA, et al. editor(s). Behavioral Health: A Handbook of Health Enhancement and Disease Prevention. New York: Wiley, 1984:1171‐8. [Google Scholar]
- Jacobs DR Jr, Lueker RV, Mittelmark MB, Folsom AR, Pirie PL, Mascioli SR, et al. Community‐wide prevention strategies: evaluation design of the Minnesota Heart Health Program. Journal of Chronic Diseases 1986;39:775‐88. [DOI] [PubMed] [Google Scholar]
- Klepp KI, Halper I, Perry CL. The efficacy of peer leaders in drug abuse prevention. Journal of School Health 1986;56:407‐11. [DOI] [PubMed] [Google Scholar]
- Perry CL, Griffin G, Murray DM. Assessing needs for youth health promotion. Preventive Medicine 1985;14:379‐93. [DOI] [PubMed] [Google Scholar]
- Perry CL, Jessor R. The concept of health promotion and the prevention of adolescent drug abuse. Health Education Quarterly 1985;12:169‐84. [DOI] [PubMed] [Google Scholar]
- Perry CL, Kelder SH, Klepp KI. Community‐wide cardiovascular disease prevention in young people: long‐term outcomes of the Class of 1989 Study. European Journal of Public Health 1994;4:188‐94. [Google Scholar]
- Perry CL, Kelder SH, Murray DM, Klepp KI. Community‐wide smoking prevention: Long‐term outcomes of the Minnesota Heart Health Program and the Class of 1989 Study. American Journal of Public Health 1992;82(9):1210‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry CL, Klepp KI, Siler C. Community‐wide strategies for cardiovascular health: the Minnesota Heart Health Program youth program. Health Education Research 1989;4:87‐101. [Google Scholar]
Perry 1999 {published data only}
- Perry CL, Komro KA, Dudovitz B, Veblen‐Mortensen S, Jeddeloh R, Koele R, et al. An evaluation of a theatre production to encourage non‐smoking among elementary age children: 2 Smart 2 Smoke. Tobacco Control 1999;8:169‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pertusa 2011 {published data only}
- Pertusa M, Rodriguez JA, Sanchez JP. Effectiveness of two smoking prevention programs according to type of applicator [Efi cacia diferencial de dos programas de prevención escolarsobre el consumo de tabaco, según el tipo de aplicador]. Psicothema 2011;23(4):537‐43. [PubMed] [Google Scholar]
Pfau 1994 {published data only}
- Pfau M, Bockern S. The persistence of inoculation in conferring resistance to smoking initiation among adolescents. The second year. Human Communication Research 1994;20:413‐30. [Google Scholar]
Philips 1990 {published data only}
- Philips BU, Longoria JM, Parcel GS, Ebeling EW. Expectations of preschool children to protect themselves from cigarette smoke: Results of a smoking prevention program for preschool children. Journal of Cancer Education 1990;5(1):27‐31. [DOI] [PubMed] [Google Scholar]
Pilgrim 1998 {published data only}
- Pilgrim C, Abbey A, Hendrickson P, Lorenz S. Implementation and impact of a family‐based substance abuse prevention program in rural communities. Journal of Primary Prevention 1998;18(3):341‐61. [Google Scholar]
Piper 1971 {published data only}
- Piper GW, Jones JA, Matthews VL. The Saskatoon Smoking Study ‐ Results of the first year. Canadian Journal of Public Health September/0ctober 1971;62:432‐40. [PubMed] [Google Scholar]
- Piper GW, Jones JA, Matthews VL. The Saskatoon Smoking Study ‐ Results of the second year. Canadian Journal of Public Health March/April 1974;62:127‐9. [PubMed] [Google Scholar]
Pomrehn 1995 {published data only}
- Pomrehn PR, Jones MP, Ferguson KJ, Becker SL. Tobacco use initiation in middle school children in three Iowa communities: Results of the Iowa Program Against Smoking (I‐PAS). Journal of Health Education 1995;26:92‐100. [Google Scholar]
Price 1992 {published data only}
- Price JH, Telljohann SK, Roberts SM, Smit D. Effects of incentives in an inner city junior high school smoking prevention program. Journal of Health Education 1992;23:388‐96. [Google Scholar]
Price 1998 {published data only}
- Price JH, Beach P, Everett S, Telljohann SK, Lewis L. Evaluation of a three‐year urban elementary school tobacco prevention program. Journal of School Health 1998;68:26‐31. [DOI] [PubMed] [Google Scholar]
Primack 2009 {published data only}
- Primack BA, Fine D, Yang CK, Wickett D, Zickmund S. Adolescents' impressions of anti‐smoking media literacy education: qualitative results from a randomised controlled trial. Health Education Research 2009;24(4):608‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Prinz 2000 {published data only}
- Dumas JE. Lynch AM. Laughlin JE. Phillips Smith E. Prinz RJ. Promoting intervention fidelity. Conceptual issues, methods, and preliminary results from the EARLY ALLIANCE prevention trial. American Journal of Preventive Medicine. 2001;20(1 Suppl):38‐47. [DOI] [PubMed] [Google Scholar]
- Prinz RJ, Dumas JE, Smith EP, Laughlin JE. The EARLY ALLIANCE prevention trial. A dual design to test reduction of risk for conduct problems, substance abuse, and school failure in childhood. Controlled Clinical Trials 2000;21(3):286‐302. [DOI] [PubMed] [Google Scholar]
- Prinz RJ, Smith EP, Dumas JE, Laughlin JE, Barron R. Recruitment and retention of participants involving family‐based interventions. Am J Prev Med 2001;20(1 Suppl):31‐37. [DOI] [PubMed] [Google Scholar]
Prokhorov 1994 {published data only}
- Prokhorov AV, Alexandrov AA. Prevention of adolescent smoking in Russia: General situation and results from a Moscow randomized trial. European Journal of Public Health 1994;4:169‐74. [Google Scholar]
Reimers 1990 {published data only}
- Reimers TM, Pomrehn PR, Becker SL, Lauer RM. Risk factors for adolescent cigarette smoking. The Muscatine Study. American Journal of Diseases of Children 1990;144:1265‐72. [DOI] [PubMed] [Google Scholar]
Renaud 2003 {published and unpublished data}
- Renaud L, O'Loughlin J, Dery V. The St‐Louis du Parc Heart Health Project: a critical analysis of the reverse effects on smoking. Tobacco Control 2003;12:302‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ringwalt 1991 {published data only}
- Ringwalt C, Ennett ST, Holt KD. An outcome evaluation of project DARE (Drug Abuse Resistance Education). Health Education Research 1991;6:327‐37. [Google Scholar]
Ringwalt 2009b {published data only}
- Giles S, Jackson‐Newsom J, Pankratz MM, Hansen WB, Ringwalt CL, Dusenbury L. Measuring quality of delivery in a substance use prevention program. Journal of Primary Prevention 2008;29:489‐501. [DOI] [PubMed] [Google Scholar]
- Ringwalt CL, Pankratz MM, Gottfredson NC, Jackson‐Newsom J, Dusenbury L, Giles D, et al. The effects of students' curriculum engagement, attitudes toward their teachers, and perception of their teachers' skills on school‐based prevention curriculum outcomes. Journal of Drug Education 2009;39(3):223‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ringwalt CL, Pankratz MM, Hansen WB, Dusenbury L, Jackson‐Newsom J, Giles SM, et al. The potential of coaching as a strategy to improve the effectiveness of school‐based substance use prevention curricula. Health Education & Behavior 2009;36(4):696‐710. [DOI] [PubMed] [Google Scholar]
Robinson 1999 {published data only}
- Robinson LA, Klesges RC, Levy MC, Zbikowski SM. Preventing cigarette use in a bi‐ethnic population: Results of the Memphis Smoking Prevention Program. Cognitive and Behavioral Practice 1999;6:136‐43. [Google Scholar]
Rohrbach 1993 {published data only}
- Rohrbach LA, Graham JW, Hansen WB. Diffusion of a school‐based substance abuse prevention program: Predictors of program implementation. Preventive Medicine 1993;22:237‐60. [DOI] [PubMed] [Google Scholar]
Rohrbach 2010b {published data only}
- Rohrbach LA, Gunning M, Grana R, Gunning G, Sussman S. Dissemination of Project Towards No Drug Abuse (TND): Findings from a survey of program adopters. Substance & Misuse 2010;45:2551‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roncarolo 2008 {published data only}
- Roncarolo F, Ramella FC, Rizzo M, Vlacos E, Bonfanti M, Tenconi MT. Effectiveness of the project "I don't smoke, and you?" against smoking in a secondary school in Italy. Igiene e Sanità Pubblica 2008;64(6):773‐86. [PubMed] [Google Scholar]
Sarvela 1987 {published data only}
- Sarvela PD, McClendon EJ. An impact evaluation of a rural youth drug education program. Journal of Drug Education 1987;17(3):213‐31. [DOI] [PubMed] [Google Scholar]
Schaps 1986 {published data only}
- Shaps E, Moskowitz JM, Malvin JH, Schaeffer GA. Evaluation of seven school‐based prevention programs: A final report on the Napa Project. International Journal of the Addictions 1986;21(9/10):1081‐112. [DOI] [PubMed] [Google Scholar]
Schinke 1982 {published data only}
- Schinke SP, Blythe BJ. Cognitive‐behavioral prevention of children's smoking. Child Behavior Therapy 1982;3:25‐42. [Google Scholar]
Schinke 1983 {published data only}
- Schinke SP, Gilchrist LD. Primary prevention of tobacco smoking. Journal of School Health 1983;53(7):416‐9. [DOI] [PubMed] [Google Scholar]
Schinke 1994 {published data only}
- Schinke SP, Moncher MS, Singer BR. Native American youths and cancer risk reduction: Effects of software intervention. Journal of Adolescent Health 1994;15:105‐10. [DOI] [PubMed] [Google Scholar]
Schinke 1996 {published data only}
- Schinke SP, Singer B, Cole K, Contento IR. Reducing cancer risk among Native American adolescents. Preventive Medicine 1996;25:146‐55. [DOI] [PubMed] [Google Scholar]
Schinke 2004 {published data only}
- Schinke SR, Schwinn TM, Noia JD, Cole KC. Reducing the effects of alcohol use among urban youth: Three‐year effects of a computer‐based intervention with and without parental involvement. Journal of Studies in Alcohol 2004;65:443‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schinke 2005 {published data only}
- Schinke S, Schwinn T. Gender‐specific computer‐based intervention for preventing drug abuse among girls. American Journal of Drug and Alcohol Abuse 2005;31(4):609‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Scholz 1985 {published data only}
- Scholz H. Experience of anti smoking training for pupils [Erfahrungen aus einem Nichtrauchertraining mit Schülern]. Prävention 1985 8 Jahrgang;2(1):57‐9. [Google Scholar]
Secker‐Walker 1997 {published data only}
- Secker‐Walker RH, Worden K, Holland RR, Flynn BS, Detsky SS. A mass media programme to prevent smoking among adolescents: costs and cost effectiveness. Tobacco Control 1997;6:207‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Secker‐Walker 1998 {published data only}
- Secker‐Walker RH, Solomon LJ, Flynn BS, Skelly JM, Mead PB. Reducing smoking during pregnancy and postpartum: Physician's advice supported by individual counselling. Preventive Medicine 1988;27:422‐30. [DOI] [PubMed] [Google Scholar]
Seid 1994 {published data only}
- Seid M. The prevention of tobacco use: The S.T.E.P. program. Peer Facilitator Quarterly 1994;12(2):23‐9. [Google Scholar]
Shaffer 1983 {published data only}
- Shaffer H, Beck JC, Boothroyd P. The primary prevention of smoking onset: An inoculation approach. Journal of Psychoactive Drugs 1983;15(3):177‐84. [DOI] [PubMed] [Google Scholar]
Skinner 1985 {published data only}
- Skinner WF, Massey JL, Krohn MD, Lauer RM. Social influences and constraints on the initiation and cessation of adolescent tobacco use. Journal of Behavioral Medicine 1985;8(4):353‐76. [DOI] [PubMed] [Google Scholar]
Sorensen 2012 {published data only}
- Sorensen G, Gupta PC, Nagler E, Viswanath K. Promoting life skills and preventing tobacco use among low‐income Mumbai youth: effects of Salaam Bombay Foundation intervention. PLOS ONE 2012;7(4):e34982. [DOI] [PMC free article] [PubMed] [Google Scholar]
Spitzzeri 1979 {published data only}
- Spitzzeri A, Jason LA. Prevention and treatment of smoking in school age children. Journal of Drug Education 1979;9(4):315‐25. [Google Scholar]
Steenkamp 1990 {published data only}
- Steenkamp HJ, Jooste PL, Jordaan PCJ, Swanepoel ASP, Rossouw JE. Changes in smoking during a community‐based cardiovascular disease intervention programme. South African Journal of Medicine 1990;79:250‐3. [PubMed] [Google Scholar]
Stone 1978 {published data only}
- Stone EJ. The effects of fifth grade health education curriculum model on perceived vulnerability and smoking attitudes. Journal of School Health 1978;48:667‐71. [DOI] [PubMed] [Google Scholar]
Sussman 2001b {published data only}
- Lichtman K, Dent CW, Colwell B, Smith DW, Sussman S. Case Study ‐ Project EX component study. In: Sussman S editor(s). Handbook of program development for health behaviour research and practice. Sage, 2000:348‐60. [Google Scholar]
- Sussman S, Dent CW, Lichtman KL. Project EX: Outcomes of a teen smoking cessation program. Addictive Behaviors 2001;26:425‐38. [DOI] [PubMed] [Google Scholar]
Svoen 1999 {published data only}
- Svoen N, Schei E. Adolescent smoking prevention ‐ primary health care in cooperation with local schools: A controlled intervention study. Scandinavian Journal of Primary Health Care 1999;17:54‐8. [DOI] [PubMed] [Google Scholar]
Szymborski 1999 {published data only}
- Szymborski J, Kowalczyk T, Sito A. Anti‐smoking educational programmes for children and young people at different educational levels [Edukacyjne programy antytytoniowe dla Dzieci i Mlodziezy na róznych poziomach nauczania]. Medycyna Wieku Rozwojowego 1999;4:471‐84. [PubMed] [Google Scholar]
Telch 1982 {published data only}
- Telch MJ, Killen JD, McAlister AL, Perry CL, Maccoby N. Long‐term follow‐up of a pilot project on smoking prevention with adolescents. Journal of Behavioral Medicine 1982;5(1):1‐8. [DOI] [PubMed] [Google Scholar]
Tell 1984 {published data only}
- Klepp KI, Tell GS, Vellar OD. Ten‐year follow‐up of the Oslo Youth Study Smoking Prevention Program. Preventive Medicine 1993;22:453‐62. [DOI] [PubMed] [Google Scholar]
- Klepp KI, Øygard L, Tell GS, Vellar OD. Twelve‐year follow‐up of a school‐based health education programme: The Oslo Youth Study. European Journal of Public Health 1994;4:195‐200. [Google Scholar]
- Tell GS, Klepp KI, Vellar OD, McAlister A. Preventing the onset of cigarette smoking in Norwegian adolescents: The Oslo Youth Study. Preventive Medicine 1984;13:256‐75. [DOI] [PubMed] [Google Scholar]
- Øygard L, Klepp KI, Tell GS, Vellar OD. Parental and peer influences on smoking among young adults: ten‐year follow‐up of the Oslo youth study participants. Addiction 1995;90:561‐9. [DOI] [PubMed] [Google Scholar]
Tessier 2008 {published data only}
- Tessier SF, Bissette E, Bantegnie D, Lebeau C. Evaluation of a tobacco prevention program in secondary schools of the Ile‐de‐France region. Alcoologie et Addictologie 2008;30(2):173‐80. [Google Scholar]
Thompson 2010 {published data only}
- Thompson B, McLerran D, Livaudais JC, Coronado GD. A group‐randomised tobacco trial among 30 Pacific Northwest colleges: results from the Campus Health Action on Tobacco study. Nicotine & Tobacco Research 2010;12(6):635‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tudor‐Smith 1998 {published data only}
- Tudor‐Smith C, Nutbeam D, Moore L, Catford J. Effects of the Heartbeat Wales programme for over five years on behavioural risks for cardiovasacular disease: quasi‐experimental comparison of results from Wales and a matched reference area. BMJ March 14 1998;316(7134):818‐822 (Comments BMJ September 26 1998;317(7162):886; and BMJ 26 September 1998;317(7162):887). [DOI] [PMC free article] [PubMed] [Google Scholar]
Turner 1993 {published data only}
- Turner GE, Burciaga C, Sussman S, Klein‐Selski E, Craig S, Dent CW, et al. Which lesson components mediate refusal assertion skill improvement in school‐based adolescent tobacco use prevention?. International Journal of the Addictions 1993;28:749‐66. [DOI] [PubMed] [Google Scholar]
Van Dyke 2002 {published data only}
- Dyke EM, Riesenberg LA. Effectiveness of a school‐based intervention at changing preadolescents' tobacco use and attitudes. Journal of School Health 2002;72(6):221‐5. [DOI] [PubMed] [Google Scholar]
Vartiainen 1998 {published data only}
- Vartiainen E, Fallonen U, McAlister AL, Puska P. Eight‐year follow‐up results of an adolescent smoking prevention project: The North Karelia Youth Project. American Journal of Public Health 1990;80(1):78‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vartiainen E, Paavola M, McAlister A, Puska P. Fifteen‐year follow‐up of smoking prevention effects in the North Karelia Youth Project. American Journal of Public Health 1998;88(1):81‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vartiainen E, Pallonen U, McAlister A, Koskela K, Puska P. Four‐year follow‐up results of the smoking prevention program in the North Karelia Youth project. Preventive Medicine 1986;15:692‐8. [DOI] [PubMed] [Google Scholar]
- Vartiainen E, Puska P, Tossavainen K, Viri L, Niskanen E, Moisio S. Prevention of non‐communicable diseases: Risk factors in youth. The North Karelia Youth Project (1984‐88). Health Promotion 1989;1(3):269‐83. [Google Scholar]
- Vartiainen E, Tossavainen K, Viri L, Niskanen E, Puska P. The North Karelia Youth Project. Annals of the New York Academy of Sciences 1991;23:332‐49. [DOI] [PubMed] [Google Scholar]
- Vartianinen E, Pallonen U, McAlister A, Koskela K, Puska P. Effect of two years of educational intervention on adolescent smoking (The North Karelia Youth Project). Bulletin of the World Health Organisation 1983;61(3):529‐32. [PMC free article] [PubMed] [Google Scholar]
Wagner 2006 {published data only}
- Wagner EF, MacGowan MJ. School‐based group treatment for adolescent substance abuse. In: HA Liddle, CL Rowe editor(s). Adolescent substance abuse: research and clinical advances. New York: Cambridge University Press, 2006:333‐56. [Google Scholar]
Wahlgren 1997 {published data only}
- Wahlgren OR, Hovell MF, Slymen OJ, Conway TL, Hofstetter CR, Jones JA. Predictors of tobacco use initiation in adolescents: a two‐year prospective study and theoretical discussion. Tobacco Control 1997;6:95‐103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Walsh 2003 {published data only}
- Walsh MM, Hilton JF, Ellison JA, Gee L, Chesney MA, Tomar SL, et al. Spit (smokeless) tobacco intervention for high school athletes. Results after 1 year. Addictive Behaviors 2003;28(6):1095‐113. [DOI] [PubMed] [Google Scholar]
Webster 2002 {published data only}
- Webster RA, Hunter M, Keats JA. Evaluating the effects of a peer support programme on adolescents' knowledge, attitudes and use of alcohol and tobacco. Drug and Alcohol Review 2002;21:7‐16. [DOI] [PubMed] [Google Scholar]
Wenzel 2007 {published data only}
- Buhler A, Schroder E, Silbereisen RK. The role of life skills promotion in substance abuse prevention: a mediation analysis. Health Education Research 2008;23(4):621‐32. [DOI] [PubMed] [Google Scholar]
- Wenzel V, Weichold K, Silbereisen RK. School‐type‐specific effectiveness of a life‐skills programme to influence tobacco use of students in college‐bound and professional‐level schools. Sucht 2007;53:335‐46. [Google Scholar]
- Wenzel V, Weichold K, Silbereisen RK. The life skills program IPSY: positive influences on school bonding and prevention of substance misuse. Journal of Adolescence 2009;32(6):1391‐401. [DOI] [PubMed] [Google Scholar]
Werch 1991 {published data only}
- Werch CE, Young M, Clark M, Garrett C, Hooks S, Kersten C. Effects of a take‐home drug prevention program on drug‐related communication and beliefs of parents and children. Journal of School Health 1991;61(8):346‐50. [DOI] [PubMed] [Google Scholar]
Werch 2008 {published data only}
- Werch CE, Bian H, Moore MJ, Ames SC, DiClemente CC, Thombs D, et al. Brief multiple behavior health interventions for older adolescents. American Journal of Health Promotion 2008;23(2):92‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wiist 1991 {published data only}
- Wiist WH, Snider G. Peer education in friendship cliques: prevention of adolescent smoking. Health Education Research 1991;6(1):101‐8. [DOI] [PubMed] [Google Scholar]
Williamson 1981 {published data only}
- Williamson JA, Campbell LP. Evaluating the effectiveness of an anti‐smoking program. Journal of School Health 1981;51:146‐7. [DOI] [PubMed] [Google Scholar]
Worden 1988 {published data only}
- Worden JK, Flynn BS, Geller BM, Chen M, Shelton LG, Secker‐Walker RH, et al. Development of a smoking prevention mass media program using diagnostic and formative research. Preventive Medicine 1988;17:531‐58. [DOI] [PubMed] [Google Scholar]
Worden 1996 {published data only}
- Worden JK, Flynn BS, Solomon LJ, Secker‐Walker RH, Badger GJ, Carpenter JH. Preventing smoking among adolescent girls using mass media. Health Education Quarterly 1996;23(4):453‐66. [DOI] [PubMed] [Google Scholar]
Wu 2003 {published data only}
- Santon B, Cole M, Galbraith J, Li X, Pendleton S, Cottrell L, et al. Randomized trial of a parental intervention. Parents can make a difference in long‐term adolescent behaviours, perceptions, and knowledge. Archives of Pediatric and Adolescent Medicine 2004;158:947‐55. [DOI] [PubMed] [Google Scholar]
- Wu Y, Stanton BF, Galbraith J, Kaljee L, Cottrell L, Li X, et al. Sustaining and broadening intervention impact: A longitudinal randomised trial of 3 adolescent risk reduction approaches. Pediatrics 2003;111(1):e32‐e38. [DOI] [PubMed] [Google Scholar]
Young 1996 {published data only}
- Young M, Kersten C, Werch C. Evaluation of a parent child drug education program. Journal of Drug Education 1996;26(1):57‐68. [DOI] [PubMed] [Google Scholar]
Zavela 2004 {published data only}
- Zavela KJ, Battistich V, Dean BJ, Flores R, Barton R, Delaney RJ. Say Yes First: A longitudinal, school‐based alcohol and drug prevention project for rural youth and families. Journal of Early Adolescence 1997;17:67‐96. [Google Scholar]
- Zavela KJ, Battistich V, Gosselink CA, Dean BJ. Say Yes First: Follow up of a five‐year rural drug prevention program. Journal of Drug Education 2004;34(1):73‐88. [DOI] [PubMed] [Google Scholar]
Zheng 2006 {published data only}
- Zheng PP, Cui HW, Fu YY, Yang SY. Smoking prevention and control among students of middle schools in Shanghai. Wei sheng yan jiu [Journal of Hygiene Research] 2006;35(3):331‐5. [PubMed] [Google Scholar]
Zoller 1986 {published data only}
- Zoller U, Maymon T. Attitude modification in health education through an interventive, anti smoking program incorporated within traditional science curriculum. Journal of Research in Science Education 1989;26:385‐99. [Google Scholar]
- Zoller U, Maymon T. Effectiveness evaluation of smoking, drug, and alcohol education courses via actual relevant behavior (The smoking education curriculum MSACS as an illustrative case study). Journal of Drug Education 1986;16:1‐12. [DOI] [PubMed] [Google Scholar]
Zollinger 2003 {published data only}
- Zollinger TW, Saywell RM Jr, Muegge CM, Woodridge JS, Cummings SF, Caine VA. Impact of the Life Skills Training curriculum on middle school students tobacco use in Marion County, Indiana, 1997‐2000. Journal of School Health 2003;73(9):338‐46. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Andrews 2011 {published data only}
- Andrews JA, Gordon JS, Hampson SE, Christiansen SM, Gunn B, Slovic P, et al. Short‐term efficacy of Click City: Tobacco: changing etiological mechanisms related to the onset of tobacco use. Prevention Science 2011;12(1):89‐102. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bier 2011b {published data only}
- Bier MC, Zwarun L, Fehrmann Warren V. Getting universal primary tobacco use prevention into priority area schools: a media literacy approach. Health Promotion Prcatice 2011;12:152S‐8S. [DOI] [PubMed] [Google Scholar]
Cremers 2012 {published data only}
- Cremers HP, Mercken L, Oenema A, Vries H. A web‐based computer‐tailored smoking prevention programme for primary school children: intervention design and study protocol. BMC Public Health 2012;12:277. [DOI] [PMC free article] [PubMed] [Google Scholar]
Evers 2012 {published data only}
- Evers KE, Paiva AL, Johnson JL, Cummins CO, Prochaska JO, Prochaska JM, et al. Results of a transtheoretical model‐based alcohol, tobacco and other drug intervention in middle schools. Addictive Behaviors 2012;37:1009‐18. [DOI] [PubMed] [Google Scholar]
Kirshnan‐Sarin 2012 {published data only}
- Krishnan‐Sarin S. Incentive‐based intervention for smoking cessation and prevention in high schools. Clinical Trials NCT01173835 2012.
O'Leary‐Barrett 2011 {published data only}
- O'Leary‐Barrett M, Topper L, MacKie CJ, Castellanos‐Ryan N, Al‐Khudhairy N, Conrod PJ. The adventure RCT: Effective delivery of personality‐targeted interventions for substance misuse by educational professionals. Clinicaltrials.gov NCT00776685 2010.
Additional references
Adams 2008
- Adams J, Parkinson L, Sanson‐Fisher RW, Walsh RA. Enhancing self‐report of adolescent smoking: The effects of bogus pipeline and anonymity. Addictive Behaviors 2008;33:1291–1296. [DOI] [PubMed] [Google Scholar]
Altman 2007
- Altman DG, Bland JM. Statistics Notes. Missing data. BMJ 2007;334:424 doi:10.1136/bmj.38977.682025.2C. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bandura 1977
- Bandura A. Social Learning Theory. Englewood Cliffs, N.J.: Prentice Hall, 1977. [Google Scholar]
Bangert‐Drowns 1988
- Bangert‐Drowns RL. The effects of school‐based substance abuse education. A meta‐analysis. Journal of Drug Education 1988;18:243‐64. [DOI] [PubMed] [Google Scholar]
Botvin 1984
- Botvin GJ, Baker E, Renick NL, Filazzola AD, Botvin EM. A cognitive‐behavioral approach to substance‐abuse prevention. Addictive Behaviors 1984;9:137‐47. [DOI] [PubMed] [Google Scholar]
Cochrane Handbook
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011].. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Epstein 2000b
- Epstein JA, Griffin KW, Botvin GJ. A model of smoking among inner‐city adolescents: The role of personal competence and perceived social benefits of smoking. Preventive Medicine 2000;31:107‐14. [DOI] [PubMed] [Google Scholar]
Evans 1976
- Evans RI. Smoking in children: Developing a social psychological strategy of deterrence. Preventive Medicine 1976;5:122‐7. [DOI] [PubMed] [Google Scholar]
Griffin 2010
- Griffin KW, Botvin GJ. Evidence‐based interventions for preventing substance use disorders in adolescents. Child and Adolescent Psychiatric Cinics of North America 2010;19(3):505‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;7414:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kenward 2009
- Kenward MG, Molenberghs G. Last Observation Carried Forward: A Crystal Ball?. Journal of Biopharmaceutical Statistics 2009;19(5):872‐88. [DOI: 10.1080/10543400903105406] [DOI] [PubMed] [Google Scholar]
McGuire 1968
- McGuire WJ. The nature of attitudes and attitude change. In: Lindzey G, Aronson E editor(s). Handbook of Social Psychology. Reading, MA: Addison‐Wesley, 1968:136‐314. [Google Scholar]
Molenberghs 2004
- Molenberghs G, Thijs H, Jansen I, Beunckens C, Kenward MG, Mallinckrodt C, et al. Analyzing incomplete longitudinal clinical trial data. Biostatistics 2004;5(3):445–64. [DOI: 10.1093/biostatistics/kxh001] [DOI] [PubMed] [Google Scholar]
Nűesch 2009
- Nűesch E, Trelle S, Reichenbach S, Rutjes AWS, Bűrgi L, Scherer M, et al. The effects of excluding patients from the analysis in randomised controlled trials: meta‐epidemiological study. BMJ 2009;339:b3244. [DOI: 10.1136/bmj.b3244] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pechacek 1984
- Pechacek TF, Murray DM, Luepker RV, Mittelmark MB, Johnson CA, Schultz JM. Measurement of adolescent smoking behavior: Rationale and methods. Journal of Behavioral Medicine 1984;7:123‐40. [DOI] [PubMed] [Google Scholar]
Pletcher 2000
- Pletcher JR, Schwarz DF. Current concepts in adolescent smoking. Current Opinion in Pediatrics 2000;12:444‐9. [DOI] [PubMed] [Google Scholar]
SAMHSA 2009
- Substance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings. Office of Applied Studies, SAMHSA, U.S. Department of Health and Human Services 2010, issue NSDUH Series H–38A, HHS Publication No.SMA 10–4856 Findings.
Tyas 1998
- Tyas SL, Pederson LL. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tobacco Control 1998;7:409‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Villanti 2010
- Villanti AC, McKay HS, Abrams DB, Holtgrave DR, Bowie JV. Smoking‐cessation interventions for U.S. young adults. A systematic review. American Journal of Preventive Medicine 2010;39(6):564‐74. [DOI] [PubMed] [Google Scholar]
Warren 2009
- Warren CW, Lea V, Lee J, Jones NR, Asma S, McKenna M. Change in tobacco use among 13−15 year olds between 1999 and 2008: findings from the Global Youth Tobacco Survey. Global Health Promotion 2009;16:38. [DOI: 10.1177/1757975909342192] [DOI] [PubMed] [Google Scholar]
Wenter 2002
- Wenter DL, Blackwell S, Davis KS, Farrelly MC. Using multiple strategies in tobacco use prevention. Legacy first look report 8 [http://www.americanlegacy.org/content/PDF/FLR8.pdf]. Washington, DC: American Legacy Foundation, February 2002. [Google Scholar]
WHO 2000
- Currie C, Hurrelmann K, Settertobulte W, Smith R, Todd J. Health and health behaviour among young people. Health behaviour in school‐aged children: a WHO cross‐national study. International report. WHO Regional Office for Europe 2000; Vol. www.ruhbc.ed.ac.uk/hbsc/download/hbsc.pdf [accessed 30th April 2004].
Wiehe 2005
- Wiehe SE, Garrison MM, Christakis DA, Ebel BE, Rivara FP. A systematic review of school‐based prevention trials with long‐term follow‐up. Adolescent Health 2005;36:162‐9. [DOI] [PubMed] [Google Scholar]
Wood 2008
- Wood L, Egger M, Gluud LL, Schulz KF, Juni P, Altman DG, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta‐epidemiological study. BMJ 2008, March 15;336(7644):601‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Thomas 2002
- Thomas R. School‐based programmes for preventing smoking. Cochrane Database of Systematic Reviews 2002, Issue 4. [DOI: 10.1002/14651858.CD001293] [DOI] [PubMed] [Google Scholar]
Thomas 2006
- Thomas RE, Perera R. school‐based programmes for preventing smoking. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD001293.pub2] [DOI] [PubMed] [Google Scholar]


