Abstract
Many initiatives integrating health and social care have been implemented in order to provide adequate care and support to older people living at home. Further development of existing initiatives requires iterative processes of developing, implementing and evaluating improvements to current practice. This case study provides insight into the process of improving an existing integrated care initiative in the Netherlands. Using a participatory approach, researchers and local stakeholders collaborated to develop and implement activities to further improve collaboration between health and social care professionals. Improvement activities included interprofessional meetings focussing on reflection and mutual learning and workplace visits. Researchers evaluated the improvement process, using data triangulation of multiple qualitative and quantitative data sources. According to participating professionals, the improvement activities improved their communication and collaboration by establishing mutual understanding and trust. Enabling factors included the safe and informal setting in which the meetings took place and the personal relationships they developed during the project. Different organisational cultures and interests and a lack of ownership and accountability among managers hindered the improvement process, whereas issues such as staff shortages, time constraints and privacy regulations made it difficult to implement improvements on a larger scale. Still, the participatory approach encouraged the development of partnerships and shared goals on the level of both managers and professionals. This case study highlights that improving communication between professionals is an important first step in improving integrated care. In addition, it shows that a participatory approach, in which improvements are co‐created and tailored to local priorities and needs, can help in the development of shared goals and trust between stakeholders with different perspectives. However, stakeholders' willingness and ability to participate in such an improvement process is challenged by many factors.
Keywords: case study research, health and social care, integrated care, interprofessional education and service developments, multi‐professional collaborations, participative research
What is known?
Integrated care is perceived as a promising solution to support older people living at home with complex needs.
Although many integrated care initiatives exist, collaboration between health and social care professionals remains challenging.
Integrated care is a complex process that is influenced by factors on multiple levels of the health and social care systems.
What this paper adds?
Good relationships, trust and communication are important prerequisites to interprofessional collaboration.
Participatory methods to improve integrated care allow for the development of partnerships and shared goals on multiple levels of the health and social care systems.
Successful improvement processes require sufficient time, commitment of stakeholders on multiple organisational levels and a process facilitator.
1. INTRODUCTION
Due to demographic changes, health systems face the challenge of providing care and support to an increasing number of older people living in their home environments. As people age, they often encounter multiple health and social care needs. Meeting these needs requires health and social care professionals to collaborate in a proactive and coordinated manner, often called integrated care (de Bruin et al., 2018; World Health Organization, 2008, 2015). Over the last decades, a wide range of integrated care initiatives have been implemented, including, for example, initiatives on multidisciplinary community‐based care (Huss, Stuck, Rubenstein, Egger, & Clough‐Gorr, 2008; Van der Elst et al., 2018) or case management for older people (You, Dunt, Doyle, & Hsueh, 2012). Although evaluations have shown positive effects on outcomes such as healthcare utilisation, well‐being and patient satisfaction, evidence remains inconclusive (de Bruin et al., 2012; Hoogendijk, 2016; Hopman et al., 2016; Huss et al., 2008; Looman, Huijsman, & Fabbricotti, 2018; Martinez‐Gonzalez, Berchtold, Ullman, Busato, & Egger, 2014; Mayo‐Wilson et al., 2014; Ouwens, Wollersheim, Hermens, Hulscher, & Grol, 2005; Stall, Nowaczynski, & Sinha, 2014; Stokes et al., 2015; Stuck, Egger, Hammer, Minder, & Beck, 2002; Van der Elst et al., 2018; You et al., 2012). These inconsistent findings could be due to the heterogeneous nature of integrated care initiatives (Amelung et al., 2017; Busetto, Luijkx, & Vrijhoef, 2017), differences in outcome measures (Hoogendijk, 2016) or because implementation of these initiatives is a complex process (Mayo‐Wilson et al., 2014). Indeed, many enabling and constraining contextual factors regarding the implementation of integrated care initiatives have been identified, such as professionals' skills and motivation, organisational culture, funding or IT‐systems (Busetto, Luijkx, Calciolari, Ortiz, & Vrijhoef, 2018; Cameron, Lart, Bostock, & Coomber, 2014; Mackie & Darvill, 2016).
Because integrated care is complex and the implementation and effectiveness of integrated care initiatives is dependent on the local context within which it is implemented, it has been argued to view integrated care not as an intervention in itself that needs to be proven effective, but rather as a complex overarching strategy to change and innovate service delivery (Amelung et al., 2017). Change strategies, being iterative processes of implementation, evaluation and further refinement, require stakeholder involvement and continuous feedback on process and outcomes in order to learn from past experiences and thus to advance development (van Dongen et al., 2018; Greenhalgh, Robert, Macfarlane, Bate, & Kyriakidou, 2004). Therefore, evaluations of integrated care should not only focus on interventions' outcomes, but also on the process through which such changes happen (Eyre, Farrelly, & Marshall, 2017; Greenhalgh et al., 2004; Manojlovich, Squires, Davies, & Graham, 2015). Participatory research designs, which are characterised by effective partnerships between researchers and local stakeholders and facilitate the development and implementation of locally relevant knowledge, can therefore add a valuable perspective to research on integrated care (Eyre et al., 2017; Glasgow, 2013).
This case study aimed to use a participatory approach as a way to facilitate further improvement of integrated care. The study was part of a larger European research project called SUSTAIN, which investigated integrated care for older people and specifically focused on improving existing integrated care initiatives, rather than developing new ones (de Bruin et al., 2018). Another objective of the project was that improvements to these initiatives should be tailored to the needs of local stakeholders. This particular case study aimed to develop and implement such locally relevant improvements to an existing initiative in the north of the Netherlands. This paper describes this improvement process and the factors influencing it. Insight into these processes and factors provides lessons, which are transferable to other integrated care initiatives.
2. METHODS
2.1. Study design and setting
Following the SUSTAIN project's methodology and timeline (de Bruin et al., 2018), we used a case study design (Yin, 2009) to evaluate the improvement process of an existing integrated care initiative (‘case’) over the course of two and a half years. This case study focused on the West‐Friesland region in the Netherlands. Over the past decade, several services have been implemented within the region with the aim of improving care and support provided to older people living at home with complex needs. These services include (a) a proactive care model implemented among general practitioners (GPs) (Muntinga et al., 2012), (b) comprehensive case‐management for people with dementia and their caregivers (Glimmerveen & Nies, 2015) and (c) so‐called ‘social community teams’, in which municipalities collaborate with home care and social care organisations to deliver instrumental aid and social support. As such, many different organisations are involved in delivering care and support for older people living at home in West‐Friesland, which challenges integrated care.
From November 2015 to April 2018, we used a participatory approach to facilitate the development and implementation of improvements to the way of working in West‐Friesland, in order to achieve better integrated care. This improvement process was guided by the Evidence Integration Triangle (EIT) (Glasgow, Green, Taylor, & Stange, 2012), and consisted of three interacting core elements: the participatory process, improvement activities and practical measures for evaluation (see Figure 1). The participatory process was characterised by collaboration between researchers and stakeholders to ensure the improvement process was tailored to local priorities and context. This participatory process resulted in improvement activities that were implemented to improve current practice, and practical measures were used to evaluate the improvement process. This evaluation focused both on impact of the improvement activities and on the participatory process itself, to gain an understanding of how and why these activities brought about change. The next sections will further elaborate on the practical application of these three core elements.
Figure 1.
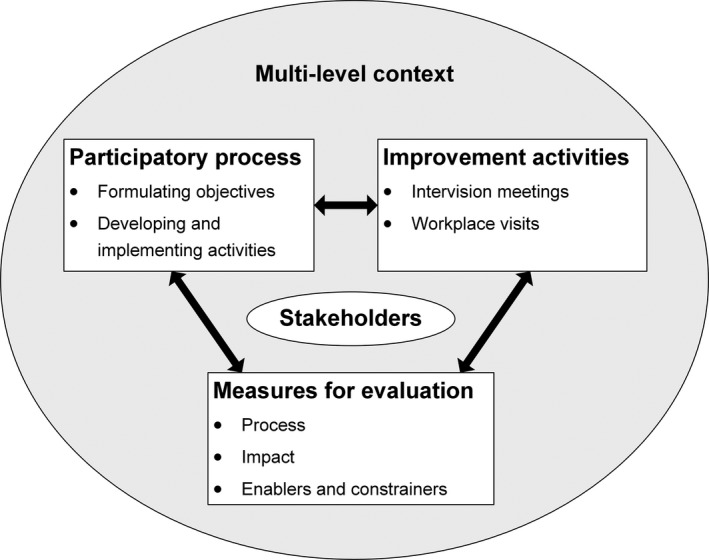
The improvement process guided by the Evidence Integration Triangle. This figure was adapted from Glasgow et al. (2012)
2.2. Participatory process and stakeholders
Several steps were taken to ensure the desired participatory approach was maintained during development and implementation of the improvement activities. First, members of the research team formed coalitions of stakeholders on multiple levels of health and social care in West‐Friesland. Table 1 shows the stakeholders on managerial level, from now on ‘steering group’, and operational level, from now on ‘professionals’, that participated in the improvement process. Professionals were employed by the same organisations that participated in the steering group. Additionally, one of the research team members (MB) was a former coordinator of elderly care in this region. Already known to and trusted by the steering group and professionals, she did not represent any specific organisation and could thus act as a neutral convenor between individual professionals, and between management and operational levels.
Table 1.
Stakeholders participating in the improvement process
| Steering group (managerial level) | Professionals (operational level) |
|---|---|
|
Manager of home care organisation 1 Manager of home care organisation 2 |
Home care nurse 1 Home care nurse 2 Home care nurse 3 |
| Manager of organisation providing integrated community care to people with dementia |
Case manager for people with dementia 1 Case manager for people with dementia 2 |
| Manager of social care organisation | Social worker |
| Policy officer from municipality | Municipality support consultant |
| General Practitioner |
Geriatric practice nurse 1 Geriatric practice nurse 2 Geriatric practice nurse 3 |
| Representative from regional advocacy organisation for older people |
The research team organised and facilitated regular steering group meetings, during which the research team and the steering group collaborated to identify potential areas for improvement, define shared objectives and develop improvement activities. Improvement activities were verified during an additional meeting with professionals in order to ensure improvements were tailored to their needs as well. The research team was responsible for data collection (see below under ‘Measures and data collection’) to evaluate process and impact and provide the steering group with feedback on this.
2.3. Improvement activities
Steering group members identified two main areas for improvement and formulated the following objectives:
It appeared to be difficult for professionals to truly put the needs and wishes of older people at the centre of their activities. The steering group aspired to enhance professionals' awareness regarding their own professional habits, and how these affect the person‐centredness of their way of working.
Available services were still very fragmented across different domains of health and social care. The steering group aspired to align communication and collaboration between professionals and increase their understanding of one another's roles and responsibilities.
Two improvement activities were developed and implemented among the professionals. The first comprised of regular ‘intervision meetings’. These are meetings in which peer supervision and methodical discussions help participants to reflect on their personal and professional development (Bellersen & Kohlmann, 2016). These meetings aimed to stimulate reflection on their professional habits in relation to the older people they cared for. Meetings were held once every two months during evening hours in an informal setting and included dinner. The meetings were organised by the principal researcher (ML) during which MB, who had experience with intervision methods, facilitated the process. The second improvement activity consisted of workplace visits, whereby professionals visited and shadowed each other during relevant parts of the day, in order to increase their understanding of one another's roles, responsibilities and expertise. The research team encouraged these visits during the intervision meetings, but the responsibility for organising these visits lay with the professionals.
2.4. Measures and data collection
Using a mixed‐methods approach, this case study used a combination of qualitative and quantitative data sources to collect data among steering group members and professionals participating in the improvement activities (see Table 2). Quantitative data sources included timesheets, which professionals used to record time spent on the improvement activities, and the Team Climate Inventory (TCI) (Kivimaki & Elovainio, 1999). The TCI assesses team climate and functioning on a scale from one to five, and includes subscales addressing team vision, participative safety, task orientation and support for innovation. Qualitative data sources included interviews with steering group members and a group interview with professionals. Interviews addressed participants' experiences with the implementation and perceived impact of the improvement activities, as well as enabling and constraining factors. In addition, we collected process data through minutes of meetings and researchers' field notes.
Table 2.
Data sources, data collection moments and quantity of data collected per source
| Data source | Objective | Collection | Quantity |
|---|---|---|---|
| Team Climate Inventory (TCI) (Kivimaki & Elovainio, 1999) | Measures changes in team coherence among steering group members and professionals | At start and end of implementation |
Baseline: n = 11 respondents Follow‐up: n = 10 respondents |
| Interviews with steering group members | Provides perceptions and experiences of steering group members with regard to process, outcomes and contextual factors | At end of implementation | n = 4 participants |
| Group interview with professionals | Provides perceptions and experiences of professionals with regard to process, outcomes and contextual factors | At end of implementation | 1 interview with n = 4 participants |
| Timesheets | Provides information on amount of time spent on intervention by professionals | Halfway and at end of implementation | n = 7 respondents |
| Minutes of steering group meetings | Provides information on processes, discussions and decisions during steering group meetings | During development and implementation | n = 4 meetings |
| Minutes of intervision meetings | Provides information on processes, discussions and decisions during intervision meetings | During implementation | n = 6 meetings |
| Field notes | Researchers notes on the process and progress of the improvement process | During development and implementation | Notes from a 30‐month period |
Recruitment of participants took place during meetings, via email or through telephone. Of the seven steering group members who were approached, five completed a questionnaire and four participated in an interview. Of the 10 professionals who were approached, eight completed a questionnaire (either at baseline, follow‐up or both). Furthermore, eight professionals completed a timesheet and four participated in the group interview. Data for the questionnaires and time sheets were collected by mail or during meetings. Interviews with steering group members were conducted over telephone, whereas professionals were interviewed during a group interview.
The principal researcher took minutes of all steering group and intervision meetings, recording attendance, topics discussed and decisions made. Minutes were shared with participants to ensure they properly reflected the meetings. Field notes were recorded by the principal researcher throughout the improvement process. These notes included records of telephone calls, emails or one‐on‐one meetings with stakeholders, decisions made by the research team outside the steering group or intervision meetings and information about other relevant events in the region.
2.5. Data analyses
This case study used a triangulation approach in order to validate findings using multiple sources and types of data (Giacomini & Cook, 2000). Data were analysed in three steps:
Each data source was analysed individually. Qualitative data were analysed according to the framework analysis method (Gale, Heath, Cameron, Rashid, & Redwood, 2013) using predefined code‐structures. The code‐structure for the interview transcripts was derived from the interview's topic list, whereas the code structure for both meeting and field notes were based on predefined themes identified in literature. Two researchers (ML and LL) independently coded the data, crosschecked each other's codes and discussed differences to reach consensus. Software for qualitative data analysis (MAXQDA 2018.0.5) was used to aid in the analysis by sorting data according to codes and themes. For quantitative data, different analytical approaches were used. Hours spent on the intervention were summed up to calculate a total score. Outcomes of the TCI were analysed with SPSS 24.0.0.1 by calculating and comparing mean scores.
Findings from each individual data source were reduced to a series of thematic statements (for qualitative data) and summaries (for quantitative data).
These thematic statements and summaries were amalgamated and subjected to a process of pattern‐matching across the data, in order to find patterns, themes and evidence that explained what worked when improving integrated care and which enabling and constraining factors influenced this process.
2.6. Ethics
The Medical Research Ethics Committee of the VU University Medical Centre in Amsterdam concluded that the Medical Research Involving Human Subjects Act (WMO) does not apply to this study (reference number 2016.507). Study participation was voluntarily and data collection took part upon informed consent.
3. FINDINGS
Findings are presented in four sub‐sections, that describe (a) the implementation and impact of the improvement activities, (b) the experiences with the participatory process, and the factors that (c) enabled and (d) constrained the improvement process undertaken in this case study. Where appropriate, we will refer to some illustrative quotes supporting our findings. Table 3 provides these quotes.
Table 3.
Quotes from (group)interviews to illustrate findings
| Quote # | Participant | Extract |
|---|---|---|
| 1 | Geriatric practice nurse 1 | ‘It's that you feel comfortable to ask someone, because you know it's something that is probably part of their job. Otherwise, you wonder sometimes about whom to go to. Now you know a little bit of what everyone is doing. And you know each other, so it's not so bad if you ask the wrong question to the wrong person sometimes. Because then the other one will just tell you, no, you should go to him or her with that question. That is that feeling of safety and trust that you have’. |
| 2 | Municipality support consultant | ‘Definitely the collaboration with the others involved in my working area. Or OUR working area, I should say. Just that you know where to find each other’. |
| 3 | Manager of home care organisation 2 | ‘What I would have preferred to get out of the project was for us to formulate together what we actually expect from the [proactive primary care model previously implemented in the region] and how we would approach that in the community together, because then we would have had something that we could all make agreements on […] and then we would collectively commit to a model that would help us to get those older people at home in the picture. I think that would be more valuable overall compared to what we did now […]’ |
| 4 | Manager of home care organisation 1 | ‘…[M]ost of all you see the divide between the doctors and the nurses versus social care and the municipality. Those really are two different worlds, and they have to grow towards each other. That's what I think was the beauty of this project’. |
| 5 | Manager of dementia care organisation | ‘How I see it, from what I know, is that at least at the level of the people who are in charge, so the managers and the administrators, that these people have come to find each other better and better. Of course, there were other things going on in the region that supported this […]. But meeting each other for [this project] did definitely supported that, especially in terms of vision’. |
| 6 | Manager of home care organisation 2 | ‘I think that […] we've been searching for a long time for what it was that we would work on with each other, specifically. As I've experienced it, there would be nuances or we would suddenly be doing something different, or someone else would join the steering group which meant we were repeating a lot. Or people didn't come to the meetings or I didn't come myself. All in all, for me it never became specific enough’. |
3.1. Implementation of the improvement activities
Six intervision meetings were held during a 12‐month period. Although 10 professionals were invited to participate, five of them dropped out throughout the course of the meetings due to lack of time and high caseload. The remaining five participants, being a practice nurse, a case‐manager, a home care nurse, a social worker and a municipality support consultant, attended meetings regularly. Professionals indicated to have spent a total of 102.5 hr on the project, most of which were allocated to attending intervision meetings. Some time was also spent on workplace visits. Three out of the five regular attendants to the meetings performed at least one workplace visit.
Initially, the intervision meetings aimed to target the steering group's first improvement objective regarding the person‐centredness of professionals' way of working. Meeting notes showed that responsiveness among professionals to address this aspect of their way of working was low, as they gave precedence to the need to explore and reflect on their relations to each other. After two meetings, the facilitators chose to adapt the meeting content, making it more flexible to address questions arising from the professionals. This meant that the focus of the intervision meetings shifted towards collaboration and communication between professionals. As such, the steering group's first improvement objective was not addressed as initially intended.
Regarding the second improvement objective, interviews with professionals and steering group members revealed that they thought the project had resulted in improved alignment between health and social care professionals. Steering group members indicated they experienced better working relationships and more trust on management level. Professionals explained that the intervision meetings allowed for professional development. According to them, both these meetings and the workplace visits increased their awareness of one another's roles, responsibilities and expertise. Professionals also felt the intervision meetings resulted in more understanding and trust, making it easier for them to collaborate (see Table 3, quote 1 and 2). TCI scores seemed to confirm these patterns found in the qualitative data (see Table 4). Although the number of respondents is small, overall scores improved during the implementation period, from a mean score of 3.3 (SD 0.84) at baseline to 3.6 (SD 0.62) at follow‐up.
Table 4.
Mean scores on the Team Climate Inventory
| Baseline (mean; SD) | Follow‐up (mean; SD) | |||||
|---|---|---|---|---|---|---|
| Total (n = 10) | SG (n = 4) | Profs (n = 6) | Total (n = 10) | SG (n = 4) | Profs (n = 6) | |
| Total TCI score | 3.3 (0.84) | 3.1 (0.56) | 3.3 (1.03) | 3.6 (0.62) | 3.8 (0.22) | 3.4 (0.76) |
| Vision | 3.6 (0.95) | 3.8 (0.80) | 3.5 (1.10) | 3.7 (0.68) | 4.0 (0.35) | 3.5 (0.78) |
| Participative safety | 3.1 (0.98) | 2.8 (0.94) | 3.4 (1.01) | 3.7 (0.94) | 4.1 (0.29) | 3.5 (1.11) |
| Task orientation | 2.9 (1.12) | 2.6 (0.74) | 3.1 (1.34) | 3.3 (0.39) | 3.2 (0.19) | 3.3 (0.47) |
| Support for innovation | 3.3 (0.75) | 3.3 (0.32) | 3.3(0.98) | 3.4 (0.68) | 3.4 (0.19) | 3.3 (0.84) |
This table presents data on team climate collected among steering group members and professionals at the start and end of implementation of the improvement project. A more detailed table providing scores per participant may be found in Appendix S1.
Abbreviations: Profs, professionals; SD, standard deviation; SG, steering group members; TCI, Team Climate Inventory.
3.2. Participatory process
In the interviews, professionals indicated they valued the opportunity to participate in the improvement process. They felt their feedback throughout the process was taken seriously, the improvement activities were tailored to their needs and they were satisfied about the impact of the activities on their way of working. Steering group members had more ambivalent views. While some perceived the implemented improvement activities to be meaningful, albeit on a small scale, others felt they could have gotten more out of the improvement process. Minutes of steering group meetings and research notes reflected that the steering group's initial ideas were more ambitious, both in terms of scope (i.e. health and social care working with one shared model for care) and scale (i.e. improvements implemented throughout the entire region). However, the research team's efforts to convert the steering group's ideas and ambitions into concrete and tangible improvement activities resulted in a more pragmatic and small‐scale approach. The additional refinement of the activities during their implementation implied another step further from the steering groups' initial ambition, causing some steering group members to indicate that the project had lost focus on these aspects and that they had not always felt involved in these decisions (see Table 3, quote 3).
3.3. Factors that enabled the improvement process
Several factors were identified that enabled the improvement process in West‐Friesland (see Table 5). For readability purposes, we sorted factors into different themes on the micro, meso and macro levels of the health and social care system. In reality, these factors were often interrelated. On the micro level, professionals indicated in interviews that the research team who organised and facilitated the intervision meetings had been important to the process. According to professionals, the research team motivated them and took action upon their feedback, ensuring that they felt respected and that the meetings had been valuable to them. Furthermore, professionals explained that the research team created a safe environment for them to discuss their experiences and issues. The informal setting of the meetings contributed to this and encouraged the development of personal relationships and trust, which was a recurring theme in the data. Both steering group members and professionals indicated that collaboration begins with trust and understanding (see Table 3, quote 4). Other factors that enabled implementation of the improvement activities included the motivation and commitment and the multidisciplinary background of professionals participating in intervision meetings and workplace visits. Professionals also experienced a sense of mutual gain from participating, as they felt their attendance was not only valuable to themselves, but to the other participants as well.
Table 5.
Factors enabling and constraining the improvement process in West‐Friesland
| Enabling factors | Constraining factors | |
|---|---|---|
| Micro (operational) level |
Facilitation of intervision meetings Informal setting Safe environment Broad composition of professionals participating in meetings Commitment of participating professionals Personal relationships and trust among professionals from different organisations |
Discrepancy between goal of intervision meetings and needs of participating professionals Lack of continuity in intervision meeting attendance Lack of time due to staff shortages and high case load |
| Meso (managerial) level |
Process facilitation and management Broad composition of steering group Commitment on managerial level of participating organisations Personal relationships and trust among managers from different organisations Shared sense of urgency |
Lack of continuity in steering group meeting attendance Lack of ownership and accountability among steering group members Conflicting organisational cultures and interests |
| Macro (regional and national) level |
Regional policy to improve collaboration Complementary collaborative initiatives in the region |
Limiting privacy regulations Lack of shared IT‐system Separate payment systems Lack of shared accountability |
The enabling and constraining factors presented in this table were identified based on interviews, meeting notes and field notes.
On meso level, the commitment and support of participating managers enabled professionals to invest time in the improvement activities. Furthermore, interviews with steering group members revealed that their meetings had helped them to develop shared vision regarding the core objectives of care and support for older people. Factors on the macro‐level, such as regional policies and collaborative initiatives across organisations, also facilitated this process (see Table 3, quote 5). Moreover, steering group members valued the presence of a representative of the regional advocacy organisation for older people. According to them, this representative's perspective helped to create a shared sense of urgency, and this binding factor was important in the development of trust and understanding on managerial level. These patterns in the qualitative data were also observed in the TCI scores (Table 4), which showed that improved total scores were largely due to improvements in participative safety on steering group member level. Additionally, steering group members indicated that the research team's role as process facilitators and managers had been important to the progress of the improvement process.
3.4. Factors that constrained the improvement process
Factors that constrained the improvement process were also distinguished into different themes on micro, meso and macro level (See Table 5). On the micro level, professionals indicated in interviews that the goals and timeline of the improvement activities had not been clear to them during the first two intervision meetings, which was related to the discrepancy between the initial meeting goals and professionals' own goals and needs. In addition, meeting and field notes indicate that continuity in attendance of the intervision meetings fluctuated especially during the first intervision meetings. The group interview revealed that this lack of continuity was perceived as disruptive by the regular attendees, as it hindered the development of personal relationships, trust and participative safety. Furthermore, professionals indicated that due to staff shortages and high caseloads, it was difficult to invest enough time in the intervention.
On the meso level, the composition of the steering group also changed throughout the process. Meeting and field notes showed that attendance during steering group meetings fluctuated due to time constraints and job changes. Some members felt that at times, this resulted in less constructive meetings due to repetition or lack of understanding of the topics discussed (see Table 3, quote 6). Additionally, the research team observed little ownership for the improvement process among the steering group. Steering group members also indicated in interviews that they never felt accountable for the process and at times had been unclear about the progress of the improvement process and their tasks and responsibilities in it. Furthermore, steering group members indicated that the different organisations involved often have different cultures and incompatible interests, which made it difficult to come to tangible agreements.
On the macro‐level, several other constraining factors emerged from the data. Recurring themes in the interviews and meeting notes included the fragmentation between the health and social care systems, for example regarding financing, privacy regulations, a lack of a shared IT‐system and a lack of shared accountability across the collaborative partners. According to steering group members, these factors impeded collaboration agreements and made it difficult to implement improvement activities on a larger scale. Professionals mainly mentioned fragmented financing and privacy regulations as issues that made their day‐to‐day work difficult, although at the same time they indicated that they often found ways to work around these issues.
4. DISCUSSION
This case study described the experiences with an improvement process of an existing integrated care initiative in the Netherlands. The implemented improvement activities enhanced communication, trust and understanding between health and social care professionals, and were considered valuable by the participants. In addition, our study revealed the challenges related to such a process. Different organisational cultures and interests and lack of ownership and accountability among managers hindered the improvement process, whereas issues such as staff shortages, time constraints and privacy regulations made it difficult to implement improvements on a larger scale. Still, the participatory approach encouraged the development of shared goals, vision and sense of urgency both on the managerial and operational levels. Overall, many factors were identified that influenced the improvement process. Some of these were related to the content of the improvement activities, whereas others were related to the actual improvement process or to the methodological approach to this process. Although these factors operated on different levels of the health and social care system, they were often interrelated.
The intended content of the improvement activities contained elements to improve both person‐centredness of care delivery as well as collaboration between different stakeholders in health and social care. Ultimately, however, the implemented improvement activities mainly targeted collaboration, as the initial aim of improving person‐centredness of care delivery appeared to be unfeasible. Previous studies suggest that communication, understanding and trust are important prerequisites for interprofessional collaboration (Borgermans et al., 2017; Mulvale, Embrett, & Razavi, 2016; Xyrichis & Lowton, 2008), and are part of a transformational process that needs to be established before one can change actual care delivery processes (Manojlovich et al., 2015). This could explain why activities targeting person‐centredness were not in line with professionals' needs at the time of the improvement process; these activities targeted the care delivery process, whereas the prerequisites for interprofessional collaboration still needed to be established.
To achieve and improve prerequisites such as communication, understanding and trust, active investment in teambuilding and professional development is necessary (Mager & Lange, 2014; McEwan, Ruissen, Eys, Zumbo, & Beauchamp, 2017)—after all, as we observed in our study, unknown makes unloved. This and other studies have shown that dedicating time to engage in shared reflection and mutual learning is a useful approach to establish this (Jones & Jones, 2011; Kassianos et al., 2015). Furthermore, having a facilitator to guide this group process has been shown to ensure a safe environment (Sorensen, Stenberg, & Garnweidner‐Holme, 2018). Policy makers and professionals aiming to improve collaboration in integrated care are therefore recommended to invest time and resources in activities targeting collaborative skills and interpersonal dynamics, in order to establish well‐functioning teams.
The experiences described in this case study confirm that improving an existing way of working is a complex and nonlinear process. Although existing models for change and improvement acknowledge the iterative and cyclical nature of these activities (van Dongen et al., 2018; Glasgow, 2013; Taylor et al., 2014), this study highlights that even the process within one iteration of goal setting, implementing, evaluating and refining is not straightforward. Several lessons for a successful improvement process can be learned from this case study. First, there should be time and space allocated to all steps of the improvement cycle, including the process of developing mutual trust and setting shared goals (Rycroft‐Malone et al., 2016). This case study showed that developing partnerships and shared goals is especially difficult and time‐consuming when the improvement process involves multiple organisations with different cultures and ambitions. Second, it is important to have an initiator or facilitator who functions as driving force and connector. In this case, the research team had this role, and other studies have shown similar positive experiences with such ‘champions’ who facilitate boundary spanning and help create team vision and a sense of urgency (Greenhalgh et al., 2004; Mulvale et al., 2016; Rycroft‐Malone et al., 2016). However, the potential of such a facilitator is also dependent on their credibility, authority and a supportive environment (Rycroft‐Malone et al., 2018). Finally, developing and implementing tangible improvements to integrated care requires commitment from stakeholders on multiple levels, since sustainable improvements need adjustments on the operational, managerial and administrative levels of the health and social care systems (Borgermans et al., 2017; Mulvale et al., 2016). Our study showed that, as the improvement activities narrowed and became more pragmatic, professionals became more committed to the improvement process while the steering group members' commitment and engagement decreased. This discrepancy suggests that multiple improvement cycles with more rapid evaluation and learning mechanisms may be needed to incentivise continued commitment on multiple levels (Rycroft‐Malone et al., 2016).
Some observations regarding the use of participatory methods to improve and evaluate integrated care practice can also be made based on this case study. In line with the EIT and other models (Glasgow et al., 2012; Horowitz, Robinson, & Seifer, 2009; Jull, Giles, & Graham, 2017), the needs and priorities of local stakeholders were the starting point of the improvement process. This approach facilitated the establishment of partnerships between researchers and stakeholders, but also between stakeholders themselves, and it stimulated stakeholders to challenge their established mind‐set and views (Eyre et al., 2017; Martin Fortin & Moira, 2016). Theoretically, another key aspect of participatory research is that researchers and local stakeholders share decision‐making, ownership and accountability for the process (Blevins, Farmer, Edlund, Sullivan, & Kirchner, 2010; Horowitz et al., 2009; Jull et al., 2017; Viswanathan et al., 2004). Unfortunately, this extent of participation was not achieved in this case. In fact, the research team functioned as initiators and driving force of the project and, unable to transfer ownership to local stakeholders, their role remained prominent until the end.
Several explanations could be provided for these experienced difficulties regarding ownership. First, stakeholders' level of participation was influenced by the reality of day‐to‐day practice. Contextual factors such as financing problems, new privacy regulations and staffing shortages meant that stakeholders were not completely willing or able to commit to the improvement project at that time. Second, the research team experienced tension between tailoring the improvement process to stakeholders' needs and priorities and complying with the requirements set by the larger European project it was part of (de Bruin et al., 2018). For instance, as the stakeholders' initial ambitions were not compatible with the scale and timeline of the European project, several pragmatic decisions were made for which stakeholders may not have felt ownership. Future research should consider this tension between the flexibility needed for participatory approaches and the rigour and structure associated with traditional research projects. Expectation management towards stakeholders regarding the timeline and scale of future projects may additionally help to improve commitment (Allen et al., 2017; Horowitz et al., 2009; Viswanathan et al., 2004).
4.1. Methodological considerations
Data were collected among participating stakeholders. As this number was limited, our study sample was small. Staff changes and drop out of professionals during the project further affected the study sample size. However, data triangulation revealed similar patterns across different sources and types of data. Therefore, although results from each individual data source should be treated with caution, the overall picture provided by this case study approach is robust. Furthermore, the process‐oriented and multimethod approach provided detailed insights into the complexity of improving integrated care (Greenhalgh et al., 2004). Still, this case study only provides insight into experiences and outcomes at the level of service providers. Given the short implementation period, it was not feasible or functional to assess effects at the level of older people receiving care and support. The question of whether and how improvements to integrated care affect the experiences of service recipients might be addressed in future research.
5. CONCLUSION
On the basis of this study, we conclude that the participatory method is a promising approach to improve integrated care practice. However, achieving true participatory research in the reality of day‐to‐day practice is difficult, as many factors can influence stakeholders' willingness and ability to commit to this participatory role. In addition, researchers need to find a balance between the flexibility needed for participatory research and the structured context in which such research projects are usually embedded. Nevertheless, the participatory approach allows for the development of partnerships and shared goals on multiple levels of organisations. Since improving integrated care starts with improving interprofessional collaboration, establishing relationships, trust and communication between stakeholders are important prerequisites that should not be overlooked. Rather, they are the necessary foundation based on which further improvements to integrated care may be developed.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
AUTHORS' CONTRIBUTIONS
As members of the SUSTAIN consortium, SdB, CB, GN, AS and ML were involved in the development of the SUSTAIN methodology. ML, MB and CB facilitated the case study presented in this paper. ML collected the data, ML, LL and AS analysed the data and all authors together interpreted the data. ML drafted the manuscript and MB, LL, AS, GN, CB and SdB critically revised the manuscript. All authors approved of the final manuscript.
Supporting information
ACKNOWLEDGEMENTS
This paper was published on behalf of the SUSTAIN consortium: Borja Arrue, Eliva Atieno Ambugo, Caroline Baan, Jenny Billings, Simone de Bruin, Michele Calabro, Nuri Cayuelas Mateu, Sandra Degelsegger, Mireia Espallargues Carreras, Erica Gadsby, Nick Goodwin, Terje Hagen, Christina Häusler, Viktoria Hoel, Henrik Hoffmann, Usman Khan, Julie MacInnes, Federica Margheri, Jenna McArthur, Maggie Langins, Manon Lette, Lina Masana, Mirella Minkman, Giel Nijpels, Konrad Obermann, Gerli Paat‐Ahi, Jillian Reynolds, Mari Rull, Georg Ruppe, Monique Spierenburg, Annerieke Stoop, Lian Stouthard, Nhu Tram, Gerald Wistow and Nick Zonneveld. In addition, the authors are grateful to the steering group members and professionals who participated in this study.
Lette M, Boorsma M, Lemmens L, et al. Unknown makes unloved—A case study on improving integrated health and social care in the Netherlands using a participatory approach. Health Soc Care Community. 2020;28:670–680. 10.1111/hsc.12901
Funding information
This study is part of the SUSTAIN project which is funded under Horizon 2020—the Framework Programme for Research and Innovation (2014‐2020) from the European Commission under grant agreement No. 634144. The content of this paper reflects only the authors' views. The European Union is not liable for any use that may be made of the information contained herein.
REFERENCES
- Allen, J. D. , Towne, S. D. Jr , Maxwell, A. E. , DiMartino, L. , Leyva, B. , Bowen, D. J. , … Weiner, B. J. (2017). Meausures of organizational characteristics associated with adoption and/or implementation of innovations: A systematic review. BMC Health Serv Res, 17(1), 591 10.1186/s12913-017-2459-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amelung, V. , Stein, V. , Goodwin, N. , Balicer, R. , Nolte, E. , & Suter, E. (2017). Handbook integrated care. Cham, Switzerland: Springer International Publishing. [Google Scholar]
- Bellersen, M. , & Kohlmann, I. (2016). Intervision: Dialogue methods in action learning. Alphen a/d Rijn, The Netherlands: Vakmedianet. [Google Scholar]
- Blevins, D. , Farmer, M. S. , Edlund, C. , Sullivan, G. , & Kirchner, J. E. J. I. S. (2010). Collaborative research between clinicians and researchers: A multiple case study of implementation. Implementation Science, 5(1), 76 10.1186/1748-5908-5-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgermans, L. , Marchal, Y. , Busetto, L. , Kalseth, J. , Kasteng, F. , Suija, K. , … Devroey, D. (2017). How to improve integrated care for people with chronic conditions: Key findings from EU FP‐7 Project INTEGRATE and beyond. International Journal of Integrated Care, 17(4), 7, 10.5334/ijic.3096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busetto, L. , Luijkx, K. , Calciolari, S. , Ortiz, L. G. G. , & Vrijhoef, H. J. M. (2018). Barriers and facilitators to workforce changes in integrated care. International Journal of Integrated Care, 18(2), 17, 10.5334/ijic.3587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busetto, L. , Luijkx, K. , & Vrijhoef, H. J. M. (2017). Advancing integrated care and its evaluation by means of a universal typology. International Journal of Care Coordination, 20(1–2), 41–44. 10.1177/2053434517705732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron, A. , Lart, R. , Bostock, L. , & Coomber, C. (2014). Factors that promote and hinder joint and integrated working between health and social care services: A review of research literature. Health and Social Care in the Community, 22(3), 225–233. 10.1111/hsc.12057 [DOI] [PubMed] [Google Scholar]
- de Bruin, S. R. , Stoop, A. , Billings, J. , Leichsenring, K. , Ruppe, G. , Tram, N. , … Baan, C. A. (2018). The SUSTAIN Project: A European study on improving integrated care for older people living at home. International Journal of Integrated Care, 18(1), 6 10.5334/ijic.3090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bruin, S. R. , Versnel, N. , Lemmens, L. C. , Molema, C. C. , Schellevis, F. G. , Nijpels, G. , & Baan, C. A. (2012). Comprehensive care programs for patients with multiple chronic conditions: A systematic literature review. Health Policy, 107(2–3), 108–145. 10.1016/j.healthpol.2012.06.006 [DOI] [PubMed] [Google Scholar]
- Eyre, L. , Farrelly, M. , & Marshall, M. (2017). What can a participatory approach to evaluation contribute to the field of integrated care? BMJ Quality & Safety, 26(7), 588–594. 10.1136/bmjqs-2016-005777 [DOI] [PubMed] [Google Scholar]
- Fortin, M. , Couture, M. , Bouhali, T. , Leclerc, E. , & Stewart, M. (2016). It takes two to tango: Researchers and decision‐makers collaborating to implement practice changes for patients with multimorbidity. Healthcare Quarterly, 19(2), 55–59. 10.12927/hcq.2016.24700 [DOI] [PubMed] [Google Scholar]
- Gale, N. K. , Heath, G. , Cameron, E. , Rashid, S. , & Redwood, S. (2013). Using the framework method for the analysis of qualitative data in multi‐disciplinary health research. BMC Medical Research Methodology, 13, 117 10.1186/1471-2288-13-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacomini, M. K. , & Cook, D. J. (2000). Users' guides to the medical literature: XXIII. Qualitative research in health care a. are the results of the study valid? JAMA, 284(3), 357–362. 10.1001/jama.284.3.357 [DOI] [PubMed] [Google Scholar]
- Glasgow, R. E. (2013). What does it mean to be pragmatic? Pragmatic methods, measures, and models to facilitate research translation. Health Education & Behavior, 40(3), 257–265. 10.1177/1090198113486805 [DOI] [PubMed] [Google Scholar]
- Glasgow, R. E. , Green, L. W. , Taylor, M. V. , & Stange, K. C. (2012). An Evidence Integration Triangle for aligning science with policy and practice. American Journal of Preventive Medicine, 42(6), 646–654. 10.1016/j.amepre.2012.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glimmerveen, L. , & Nies, H. (2015). Integrated community‐based dementia care: The Geriant model. International Journal of Integrated Care, 15, e020 10.5334/ijic.2248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh, T. , Robert, G. , Macfarlane, F. , Bate, P. , & Kyriakidou, O. (2004). Diffusion of innovations in service organizations: Systematic review and recommendations. Milbank Quarterly, 82(4), 581–629. 10.1111/j.0887-378X.2004.00325.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoogendijk, E. O. (2016). How effective is integrated care for community‐dwelling frail older people? The case of the Netherlands. Age and Ageing, 45(5), 585–588. 10.1093/ageing/afw081 [DOI] [PubMed] [Google Scholar]
- Hopman, P. , de Bruin, S. R. , Forjaz, M. J. , Rodriguez‐Blazquez, C. , Tonnara, G. , Lemmens, L. C. , … Rijken, M. (2016). Effectiveness of comprehensive care programs for patients with multiple chronic conditions or frailty: A systematic literature review. Health Policy, 120(7), 818–832. 10.1016/j.healthpol.2016.04.002 [DOI] [PubMed] [Google Scholar]
- Horowitz, C. R. , Robinson, M. , & Seifer, S. (2009). Community‐based participatory research from the margin to the mainstream. Circulation, 119(19), 2633–2642. 10.1161/CIRCULATIONAHA.107.729863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huss, A. , Stuck, A. E. , Rubenstein, L. Z. , Egger, M. , & Clough‐Gorr, K. M. (2008). Multidimensional preventive home visit programs for community‐dwelling older adults: A systematic review and meta‐analysis of randomized controlled trials. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 63(3), 298–307. [DOI] [PubMed] [Google Scholar]
- Jones, A. , & Jones, D. (2011). Improving teamwork, trust and safety: An ethnographic study of an interprofessional initiative. Journal of Interprofessional Care, 25(3), 175–181. 10.3109/13561820.2010.520248 [DOI] [PubMed] [Google Scholar]
- Jull, J. , Giles, A. , & Graham, I. D. (2017). Community‐based participatory research and integrated knowledge translation: Advancing the co‐creation of knowledge. Implementation Science, 12(1), 150 10.1186/s13012-017-0696-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassianos, A. P. , Ignatowicz, A. , Greenfield, G. , Majeed, A. , Car, J. , & Pappas, Y. (2015). "Partners rather than just providers…": A qualitative study on health care professionals' views on implementation of multidisciplinary group meetings in the North West London Integrated Care Pilot. International Journal of Integrated Care, 15, e032 10.5334/ijic.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivimaki, M. , & Elovainio, M. (1999). A short version of the Team Climate Inventory: Development and psychometric properties. Journal of Occupational and Organizational Psychology, 72(2), 241–246. 10.1348/096317999166644 [DOI] [Google Scholar]
- Looman, W. M. , Huijsman, R. , & Fabbricotti, I. N. (2018). The (cost‐)effectiveness of preventive, integrated care for community‐dwelling frail older people: A systematic review. Health and Social Care in the Community, 27(1), 1–30. 10.1111/hsc.12571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackie, S. , & Darvill, A. (2016). Factors enabling implementation of integrated health and social care: A systematic review. British Journal of Community Nursing, 21(2), 82–87. 10.12968/bjcn.2016.21.2.82 [DOI] [PubMed] [Google Scholar]
- Mager, D. R. , & Lange, J. (2014). Teambuilding across healthcare professions: The ELDER project. Applied Nursing Research, 27(2), 141–143. 10.1016/j.apnr.2013.06.006 [DOI] [PubMed] [Google Scholar]
- Manojlovich, M. , Squires, J. E. , Davies, B. , & Graham, I. D. (2015). Hiding in plain sight: Communication theory in implementation science. Implementation Science, 10, 58 10.1186/s13012-015-0244-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez‐Gonzalez, N. A. , Berchtold, P. , Ullman, K. , Busato, A. , & Egger, M. (2014). Integrated care programmes for adults with chronic conditions: A meta‐review. International Journal for Quality in Health Care, 26(5), 561–570. 10.1093/intqhc/mzu071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayo‐Wilson, E. , Grant, S. , Burton, J. , Parsons, A. , Underhill, K. , & Montgomery, P. (2014). Preventive home visits for mortality, morbidity, and institutionalization in older adults: A systematic review and meta‐analysis. PLoS ONE, 9(3), e89257 10.1371/journal.pone.0089257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwan, D. , Ruissen, G. R. , Eys, M. A. , Zumbo, B. D. , & Beauchamp, M. R. (2017). The effectiveness of teamwork training on teamwork behaviors and team performance: A systematic review and meta‐analysis of controlled interventions. PLoS ONE, 12(1), e0169604 10.1371/journal.pone.0169604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulvale, G. , Embrett, M. , & Razavi, S. D. (2016). 'Gearing Up' to improve interprofessional collaboration in primary care: A systematic review and conceptual framework. BMC Family Practice, 17, 83 10.1186/s12875-016-0492-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muntinga, M. E. , Hoogendijk, E. O. , van Leeuwen, K. M. , van Hout, H. P. J. , Twisk, J. W. R. , van der Horst, H. E. , … Jansen, A. P. D. (2012). Implementing the chronic care model for frail older adults in the Netherlands: Study protocol of ACT (frail older adults: Care in transition). BMC Geriatrics, 12, 19 10.1186/1471-2318-12-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouwens, M. , Wollersheim, H. , Hermens, R. , Hulscher, M. , & Grol, R. (2005). Integrated care programmes for chronically ill patients: A review of systematic reviews. International Journal for Quality in Health Care, 17(2), 141–146. 10.1093/intqhc/mzi016 [DOI] [PubMed] [Google Scholar]
- Rycroft‐Malone, J. O. , Burton, C. R. , Wilkinson, J. , Harvey, G. , McCormack, B. , Baker, R. , … Williams, L. (2016). Collective action for implementation: a realist evaluation of organisational collaboration in healthcare. Implementation Science, 11(1), 17 10.1186/s13012-016-0380-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rycroft‐Malone, J. O. , Seers, K. , Eldh, A. C. , Cox, K. , Crichton, N. , Harvey, G. , … Wallin, L. (2018). A realist process evaluation within the Facilitating Implementation of Research Evidence (FIRE) cluster randomised controlled international trial: an exemplar. Implementation Science, 13(1), 138 10.1186/s13012-018-0811-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen, M. , Stenberg, U. , & Garnweidner‐Holme, L. (2018). A scoping review of facilitators of multi‐professional collaboration in primary care. International Journal of Integrated Care, 18(3), 13 10.5334/ijic.3959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall, N. , Nowaczynski, M. , & Sinha, S. K. (2014). Systematic review of outcomes from home‐based primary care programs for homebound older adults. Journal of the American Geriatrics Society, 62(12), 2243–2251. 10.1111/jgs.13088 [DOI] [PubMed] [Google Scholar]
- Stokes, J. , Panagioti, M. , Alam, R. , Checkland, K. , Cheraghi‐Sohi, S. , & Bower, P. (2015). Effectiveness of case management for 'At Risk' patients in primary care: A systematic review and meta‐analysis. PLoS ONE, 10(7), e0132340 10.1371/journal.pone.0132340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuck, A. E. , Egger, M. , Hammer, A. , Minder, C. E. , & Beck, J. C. (2002). Home visits to prevent nursing home admission and functional decline in elderly people: Systematic review and meta‐regression analysis. JAMA, 287(8), 1022–1028. 10.1001/jama.287.8.1022 [DOI] [PubMed] [Google Scholar]
- Taylor, M. J. , McNicholas, C. , Nicolay, C. , Darzi, A. , Bell, D. , & Reed, J. E. (2014). Systematic review of the application of the plan‐do‐study‐act method to improve quality in healthcare. BMJ Quality & Safety, 23(4), 290–298. 10.1136/bmjqs-2013-001862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Elst, M. , Schoenmakers, B. , Duppen, D. , Lambotte, D. , Fret, B. , Vaes, B. , & … D‐SCOPE Consortium . (2018). Interventions for frail community‐dwelling older adults have no significant effect on adverse outcomes: a systematic review and meta‐analysis. BMC Geriatrics, 18(1), 249 10.1186/s12877-018-0936-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dongen, J. J. J. , van Bokhoven, M. A. , Goossens, W. N. M. , Daniëls, R. , van der Weijden, T. , & Beurskens, A. (2018). Development of a customizable programme for improving interprofessional team meetings: An action research approach. International Journal of Integrated Care, 18(1), 8–8. 10.5334/ijic.3076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viswanathan, M. , Ammerman, A. , Eng, E. , Gartlehner, G. , Lohr, K. N. , Griffith, D. , … Whitener, L. (2004). Community‐based participatory research: Assessing the evidence. (Evidence Reports/Technology Assessments, No. 99.). Rockville, MD: Agency for Healthcare Research and Quality; Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK37279/ [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2008). Caring for people with chronic conditions. A health system perspective. Maidenhead, UK: Open University Press - McGraw-Hill Education; Retrieved from http://www.euro.who.int/__data/assets/pdf_file/0006/96468/E91878.pdf [Google Scholar]
- World Health Organization (2015). World report on ageing and health. Geneva, Switzerland: World Health Organization; Retrieved from https://www.who.int/ageing/publications/world-report-2015/en/ [Google Scholar]
- Xyrichis, A. , & Lowton, K. (2008). What fosters or prevents interprofessional teamworking in primary and community care? A literature review. International Journal of Nursing Studies, 45(1), 140–153. 10.1016/j.ijnurstu.2007.01.015 [DOI] [PubMed] [Google Scholar]
- Yin, R. K. (2009). Case study research: Design and methods (4th edn). Los Angeles, CA: SAGE Publications Inc. [Google Scholar]
- You, E. C. , Dunt, D. , Doyle, C. , & Hsueh, A. (2012). Effects of case management in community aged care on client and carer outcomes: A systematic review of randomized trials and comparative observational studies. BMC Health Services Research, 12(1), 395 10.1186/1472-6963-12-395 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


