Abstract
Precis:
Chinese Glaucoma Study Consortium (CGSC) as the first nationwide glaucoma registry in China, we describe its design, rationale, the geographic distribution of the hospitals, and baseline patient characteristics.
Aim:
As a leading cause of blindness in China, glaucoma affects 2% to 4% of adults over the age of 40 and will become increasingly prevalent as the population ages. At the national level, there are few reports on the current medical practice for glaucoma patients. CGSC will be considered as the first nationwide glaucoma registry in China. Here we describe its design, rationale, the geographic distribution of the hospitals, and baseline patient characteristics.
Methods:
From December 21, 2015 to September 9, 2018, CGSC recruited patients with the diagnoses of primary angle-closure suspect, primary angle-closure, primary angle-closure glaucoma, acute primary angle closure, primary open-angle glaucoma (POAG), pigmentary glaucoma (PG), and pseudoexfoliative glaucoma (PXG) from 111 hospitals covering 67 cities from 22 provinces, 4 municipalities, and 5 autonomous regions in mainland China. Clinical data were collected using an Electronic Data Capture System designed by Tongren hospital and Gauss informed Ltd. Blood samples were collected from every patient for further genetic analysis.
Results:
Medical records of 10,892 patients were collected, of which 5762 patients have complete information. The average age of those with complete information (n=5762) was 62.05±11.26 years old, and 35.25% were males. Primary angle-closure disease, including primary angle-closure suspect/primary angle-closure/primary angle-closure glaucoma/acute primary angle closure, was predominant (4588, 79.63%), and the distribution for others is as follows: POAG (1116, 19.37%), PXG (41, 0.71%) and PG (17, 0.30%). A total of 16,684 blood samples were collected, of which 9917 (82.68%) were primary angle-closure disease, 1987 (16.57%) were POAG, 69 (0.58%) were PXG, 22 (0.18%) were PG, and 4689 were normal controls.
Conclusions:
The CGSC is the first national-level glaucoma registry study in China. Clinical data and blood samples will provide the opportunity to study the epidemiology of glaucoma in Chinese hospitals, to evaluate the level of medical diagnosis and treatment of glaucoma in China, and to identify the susceptibility loci for glaucoma.
Key Words: glaucoma, China, epidemiology, protocol
Glaucoma is the leading cause of irreversible blindness worldwide, affecting between 60.6 and 79.6 million people from 2010 to 2020.1 The number of glaucoma patients worldwide is projected to increase to 111.8 million by 2040.2,3 The age-standardized prevalence rates of glaucoma have increased over the past 20 years,1 reaching 2.6% in rural China.4
Although some information regarding glaucoma epidemiology had been collected from different hospitals in China,5–8 these studies were mostly regional therefore the number of subjects was limited. As China is a nation with a large population of over 1.3 billion, the treatment choice for glaucoma can be diverse due to different geographical locations and economic conditions. The economic development in eastern China is rapid with rich medical resources benefiting a concentrated population distribution in the area. Meanwhile, the western region lags are sparsely populated with poor medical resources.
Drugs, laser, or surgical therapies are sometimes inadequate in controlling the progression of the disease. Furthermore, it is meaningful to evaluate current glaucoma therapies throughout the whole country. While genetic factors are known to be associated with glaucoma occurrence, the pathogenesis is still poorly understood. The current study attempts to clarify the genetic mechanisms behind glaucoma and identify genetic biomarkers for glaucoma in China. The study is also trying to clarify the genetic mechanism of glaucoma and to identify the genetic biomarkers for glaucoma in China.
In this report, we look at The Chinese Glaucoma Study Consortium (CGSC), rationale, design, geographic coverage, baseline patient characteristics, uniqueness, and limitations. The consortium is built to further develop glaucoma genetic research, construct research platform to carry out high-quality multicenter clinical research, improve clinical research capacity, and promote new technology and new projects throughout China.
METHODS
The CGSC is a nationwide registry study for adult glaucoma patients in hospitals, which started in 2015. The CGSC was designed to acquire hospital epidemiological information, explore the glaucoma pathogenesis, improve glaucoma therapy, and guide the treatment and prevention in China. The purpose of the CGSC was to establish a platform for a clinical study to evaluate the diagnosis and treatment level of glaucoma in China, to explore the glaucoma pathogenesis, and to find the genetic biomarkers for glaucoma. The current study will contribute to genetic testing for early diagnosis and prediction of glaucoma and guide further treatment in the early phase and prevention.
Chinese Glaucoma Genome-Wide Association Study (GWAS) Study: Genotyping
Systematic quality controlling was performed on the raw genotyping data before correlation analysis. The population outliers and stratification were evaluated using a principle-component analysis-based method. Genotyping was performed using an Affymetrix single nucleotide polymorphisms (SNP) 6.0 array and data analyzed using the Genotype Calling Algorithm Genome Studio software. We analyzed the total SNPs and <100 were selected for the first-stage validation. The SNPs that were significantly associated with primary angle-closure glaucoma (PACG) risk in the first-stage validation were further genotyped in samples during the second-stage validation. The genotyping analyses for the 2 validation sample sets were performed by the TaqMan Open Array platform and TaqMan assays.9
Site Selection
There are 3 grades of public hospitals in China: grade I is defined as community hospitals, grade II is defined as hospitals which serve several communities, and grade III is defined as central hospitals for a city or a district and teaching hospitals.10 Grade III hospitals are further classified into class A, B, and C, with class IIIA, regarded as the hospitals with top technology and leading level of medical care. Grade III hospitals mostly are polyclinic, ophthalmology clinics only are mostly private hospitals or grade I to II in China. The CGSC steering committee selected 111 sites after evaluating the research capability and clinical level of the hospitals in China, including 104 grade III (IIIA94, IIIB1, IIIC9), 4 grade II, 1 grade I and 2 private eye hospitals. The CGSC steering committee tried to geographically cover all 22 provinces, 4 municipalities and 5 autonomous regions in mainland China.
All selected hospitals had more glaucoma patients, surgeries, research resources and glaucoma expertise than the other hospitals in the local area. Most of the expertise from the selected hospitals are familiar with each other with regards to domestic glaucoma conferences or they had previous research cooperation with the steering committee. Table 1 encompasses the list of selected hospitals with the grades classification. Figure 1 illustrates the map of the 67 cities comprising the selected sites.
TABLE 1.
Selected Hospital Classification Levels in Chinese Glaucoma Study Consortium (n=111)
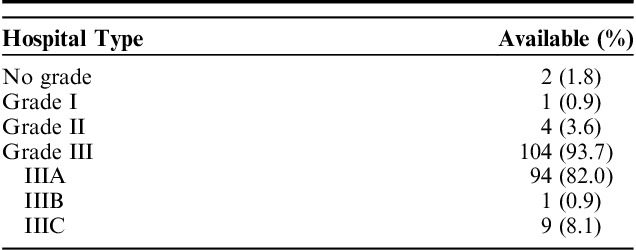
FIGURE 1.

The 67 cities of the selected hospitals in Chinese Glaucoma Study Consortium. Is the illustration of the 67 cities of the 111 selected hospitals in Chinese Glaucoma Study Consortium in which Chinese patients’ blood samples were from the CGSC blood bank. The data collected by CGSC will be analyzed in order to provide a reference for future clinical practice of glaucoma and the application of evidence-based medicine for glaucoma treatment in China. Hospital-based surveys and prospective clinical studies focused on glaucoma are being performed in the hospitals of CGSC. CGSC indicates Chinese Glaucoma Study Consortium.
The CGSC was approved by the Ethics Committee of Beijing Tongren Hospital, Capital Medical University, 2015.
Patients Enrollment
The recruited new and return patients for the registry between December 21, 2015 and September 9, 2018 met the following inclusion criteria:
Over 18 years of age.
Clinical diagnosis of primary angle-closure suspect (PACS), primary angle-closure (PAC), PACG, acute primary angle closure (APAC), primary open-angle glaucoma (POAG), pigmentary glaucoma (PG), and pseudoexfoliative glaucoma (PXG), any patient with these diagnosis in 1 eye or both eyes.
The ability of patient or legally authorized representative (primarily spouse, parents, adult children, otherwise indicated) to provide informed consent.
The definition of Glaucoma was in accordance with the International Society of Geographical and Epidemiologic Ophthalmology criteria11 and Consensus on diagnosis and treatment of primary glaucoma in China,12 as detailed below:
POAG is defined as open-angle, with either glaucomatous optic neuropathy (GON) or the visual field loss, with or without raised intraocular pressure (IOP) 11.
PACS is defined as 2 or more quadrants of iridotrabecular contact (ITC), normal IOP, no PAS, and no evidence of GON 11.
PAC is defined as ITC resulting in PAS and, or raised IOP. No evidence of GON 11.
PACG is defined as ITC resulting in GON, PAS, and raised IOP may be absent at the time of initial examination 11.
APAC is defined as when iris quickly and completely contacts the entire trabecular meshwork, leading to sudden symptomatic elevation of IOP,13 pressure-induced corneal edema, a mid-dilated pupil, vascular congestion, eye pain, and/or headache.14
PG is defined as reduction of trabecular outflow owing to melanin granules, raised IOP resulting in GON. The background condition is pigmentary syndrome 15.
PXG is defined as pseudoexfoliative material and pigment granules accumulate in the trabecular meshwork causing decreased aqueous humor outflow and significantly elevated IOP resulting in GON.15
If there are different diagnosis in both eyes, the patient would be considered as for the more severe diagnosis. For example, if 1 eye is PACG, the other eye is PAC, we considered the patient as PACG patient. If 1 eye is APAC, the other eye is PACS, then we considered the patient as APAC patient. If 1 eye is PXG, the other eye is POAG, then we considered the patient as PXG patient.
If there is combined-mechanism glaucoma or the diagnosis is hard to make, the information of the patient will be sent to Beijing Tongren Hospital, the steering committee will help the doctors to make the diagnosis. We count the patients as the first diagnosis of glaucoma.
Other types of glaucoma such as post-traumatic glaucoma, neovascular glaucoma, inflammatory glaucoma, were not included in the CGSC, because the study was more focused on the genetic research of glaucoma.
The study will collect 10,000 primary angle-closure disease (PACD) patients, 10,000 POAG patients, and 10,000 normal controls for the end of the enrollment.
Outcome Assessments
Patients who did not meet the inclusion criteria were excluded from the research (ie, missing diagnosis, such as other secondary glaucoma, post-traumatic glaucoma, neovascular glaucoma, inflammatory glaucoma, etc.), patients under 18 years of age or refuse to sign the informed consent).
Collection and Management of the Data and Blood Samples
A clinical data collection protocol and case report form were designed by the CGSC steering committee. Electronic Data Capture (EDC) designed by experts from Tongren Hospital and Gauss Informed Ltd was used for data collection.
The information collected included demographics, contact information, medical and surgical history, medication use, diagnosis, disease management. Patient examination was performed and included visual acuity, IOP, slit-lamp examination, fundus photograph, gonioscopy, ultrasound biomicroscopy, anatomical parameters including axial length, anterior chamber depth, lens thickness, and central corneal thickness and visual field. Pupil dilation was only performed in POAG/PXG/PG patients. There are standard operating procedures of information collection, examination, blood collection. The data collection was performed by trained research coordinators from the outpatient and inpatient medical records. The examinations were conducted by experienced doctors, trained nurses, and optometrists.
All data elements were automatically checked for completeness and proper examination results by EDC. Each investigator had his own account and password to login on the EDC system. EDC also provided functions to mark the queries, summarize and finalize the report, and remind investigators and research team of the site to correct mistakes. Doctors from Tongren Hospital, check the clinical information and diagnosis and treatment in the EDC system. They give queries to the doctors of the site, to make sure the data accuracy (examination, diagnosis, and treatment, etc.).
Research coordinators were trained before and during the trial kick-off meeting. During the trial, training meetings were held every year since December 2015. Trained research coordinators timely visited each site to review the medical records to identify and monitor the patients’ data collection and blood sample collection.
Beijing Clinical Service Center, an independent research organization, was responsible for checking the whole progress and visiting each site to ensure the accuracy, completeness of the data, and the correct procedure throughout the study period.
All the aggregate data was collected and analyzed by an expert statistician from Tongren Center for research purposes.
The blood samples were collected from the peripheral vein of each patient by trained nurses and transferred to Tongren Hospital for genetic analysis by a cold chain logistics company, named JINYU, equipped with real-time temperature monitoring.
Questionnaires
The National Eye Institute Visual Functioning Questionnaire-25 (NEI VFQ-25), and Hospital Anxiety and Depression Scale (HADS) were used for both glaucoma patients and cataract patients as controls in the CGSC. The VFQ-25 is a reliable and valid 25-item version of the 51-item National Eye Institute Visual Function Questionnaire (NEI-VFQ).16,17 The self-administered questionnaire with 25 items exploring 12 dimensions can assess health-related quality of life in any vision decreased eye disease.18 The HADS is a 14-item scales with a valid and reliable self-rating scale that measures anxiety and depression in both hospital and community settings. HADS gives clinically meaningful results as a psychological screening tool and can assess the symptom severity of anxiety disorders and depression in patients with illness and the general population.19 Scores and grades are assigned for these questionnaires. Scores of 8 or above are “anxiety or depression” and scores of 11 or higher are “moderate to severe anxiety and depression” (normal 0 to 7, mild 8 to 10, moderate 11 to 14, severe 15 to 21). Both questionnaires were used because they were widely used in a number of quality of life studies of ocular diseases.
Statistical Analysis
Frequency and percentages were used for statistical description of categorical variables including sex, ethnicity and glaucoma subtypes. Mean values and SD were used to make a statistical description for age, which was normally distributed. For other continuous variables and ordinal variables, the median values and interquartile range were used.
RESULTS
Between December 21, 2015 and September 9, 2018, the medical records of a total of 10,892 patients were collected. Of these, 5762 (52.9%) had complete information. However, patient recruitment has not been completed yet and therefore the medical information and blood sample collection are still ongoing.
The baseline characteristics of patients are summarized in Table 2. Sex distribution indicated that of all patients 64.75% were females, while 35.25% were male. The mean age at enrollment was 62.05±11.26 years. In Table 2 are also listed the patient diagnosis, as follows: PACD was predominant (4588, 79.63%), including PACS (160, 3.49%)/PAC (246, 5.36%)/PACG (1903, 33.03%)/APAC (2279, 39.55%), and the others were POAG (1116, 19.37%), PXG (41, 0.71%) and PG (17, 0.30%).
TABLE 2.
Patients’ Demographic, Characteristics, and Glaucoma Subtypes
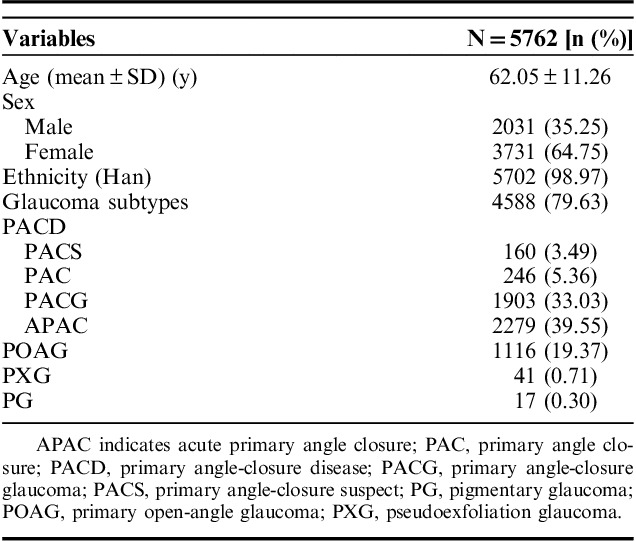
A total of 16,684 blood samples were collected, of these, 9917 (82.68%) were PACD, 1987 (16.57%) were POAG, 69 (0.58%) were EG, 22 (0.18%) were PG, and 4689 were normal control.
The CGSC has established the biggest glaucoma clinical information databank and blood bank.
DISCUSSION
The CGSC has enrolled patients since December 21, 2015 and the enrollment is still ongoing. During this study, the baseline characteristics of the participating hospitals and patients were reported. The CGSC has become a database of glaucoma patients from 111 hospitals covering all parts of mainland China. This study provides an opportunity to assess the level of glaucoma diagnosis and treatment across the country at different regional and economic levels. The economic development of the eastern China region is rapid, with a concentrated population and rich medical resources,20 therefore more hospitals were selected from this part of the nation. Meanwhile, the economic development of the western region lags behind, the population is scarce and the medical resources are also relatively inadequate, hence the hospitals from western China are rare in the CGSC registry.
It was observed that reports of POAG were much more common than PACG worldwide in many western-based studies, as PACG is considered a fairly rare disease in white populations.1 The prevalence of PACG was observed to be much higher in the Asian population (0.12% to 2.5%) compared with western white population (rare—0.6%) and African descent (0.5%).21 In a population-based study, the overall pooled prevalence of POAG and PACG were 0.7%, and 1.4% in China, respectively.22 However, in the hospital-based study, PACG was more predominant, the percentage of PACG varying between 45.40% 5 and 51.69% 6 because PACG patients are more likely to come to the hospital for eye pain 8. With a smaller corneal diameter, smaller anterior chamber depth and more anteriorly placed lens, PACD is much easier to diagnose than POAG 5. From the CGSC data, PACD is also in majority at 79.63%, notably more than POAG (19.37%), the POAG-to-PACD ratio being 4.11:1.
Female sex is recognized as a major predisposing factor for the development of PACG23,24 in the CGSA database as 64.75% of patients were female and the sex ratio (female/male) was 1.89. Furthermore, advancing age is one of the most consistent risk factors for glaucoma, irrespective of being POAG, PACG or secondary glaucoma.25,26 In the CGSC study, the average age was 62.05±11.26 years.
The CGSC is a special study because it collected information about history anatomy, biometry and different treatment strategies for glaucoma patients. The information collected will play an important role in understanding the medical treatment situation, geographical distribution and local level of diagnosis, and the treatment of glaucoma patients in China. The consortium is built to construct a research platform to carry out high-quality multicenter clinical research, improve clinical research capacity and promote new technology and new projects throughout China. The blood samples collected will be used in following GWAS and other genetic studies. We already collected 16,684 blood samples to establish a blood bank of glaucoma in China.
Some limitations were also noted in the CGSC study. Although the participating hospitals covered all parts of mainland China, the steering committee selected through agencies such as the China Glaucoma Association by convenience. As a result, these participating hospitals have more glaucoma patients, research resources and glaucoma specialists. Therefore, it may be difficult to represent the level of glaucoma diagnosis and treatment in primary hospitals, especially in remote areas.
Despite these limitations, CGSC was designed to be the first registry study for glaucoma patients in China. In 2016, 5 new loci associated with PACG were found in the multicenter international collaborative GWAS research27 in which blood samples of Chinese patients were from the CGSC blood bank.
The data collected by CGSC will be analyzed in order to provide reference for future clinical practice of glaucoma and the application of evidence-based medicine for glaucoma treatment in China. Hospital-based surveys and prospective clinical studies focused on glaucoma are being performed in the hospitals of CGSC.
ACKNOWLEDGMENTS
The authors are on behalf of the investigators for The Chinese Glaucoma Study Consortium investigators and thank them for their cooperation and hard work.
Footnotes
Supported by the Natural Science Foundation of China (grant number: 81570837).
Disclosure: The authors declare no conflict of interest.
REFERENCES
- 1.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tham YC, Li X, Wong TY, et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–2090. [DOI] [PubMed] [Google Scholar]
- 3.Wang B, Congdon N, Bourne R. Burden of vision loss associated with eye disease in China 1990-2020: findings from the Global Burden of Disease Study 2015. Br J Ophthalmol. 2018;102:220–224. [DOI] [PubMed] [Google Scholar]
- 4.Pan CW, Zhao CH, Yu MB, et al. Prevalence, types, and awareness of glaucoma in a multi-ethnic population in rural China: the Yunnan Minority Eye Study. Ophthalmic Physiol Opt. 2016;36:664–670. [DOI] [PubMed] [Google Scholar]
- 5.Yang Z, Fu JL, Li YL, et al. Epidemiology and clinical characteristics of patients with glaucoma: an analysis of hospital data between 2003 and 2012. Indian J Ophthalmol. 2015;63:825–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zheng YY, Zhang YQ, Sun XH. Epidemiologic characteristics of 10 years hospitalized patients with glaucoma at Shanghai eye and ear, nose, and throat hospital. Medicine (Baltimore). 2016;95:e4254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lü ZP, Chen XM. Proportion and its changes in hospitalized patients with glaucoma in West China Hospital. Int J Ophthalmol. 2011;11:1953–1956. [Google Scholar]
- 8.Zhang YL, Wang CY, Peng AM. The characteristics of proportion in hospitalized patient with glaucoma. Chin J Pract Ophthalmol. 2011;29:284–286. [Google Scholar]
- 9.Hu Z, Li Z, Yu J, et al. Association analysis identifies new risk loci for non-obstructive azoospermia in Chinese men. Nat Commun. 2014;5:3857. [DOI] [PubMed] [Google Scholar]
- 10.Minister of Health. Acts for Hospital Classification. China: Minister of Health; 1989. [Google Scholar]
- 11.Foster PJ, Buhrmann R, Quigley HA, et al. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86:238–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glaucoma Section, Ophthalmology Branch, Chinese Medical Association. Consensus on diagnosis and treatment of primary glaucoma in China. Chin J Ophthalmol. 2014;50:382–383. [Google Scholar]
- 13.Sun X, Dai Y, Chen Y, et al. Primary angle-closure glaucoma: what we know and what we don’t know. Prog Retin Eye Res. 2017;57:26–45. [DOI] [PubMed] [Google Scholar]
- 14.Prum BE, Herndon LW, Moroi SE, et al. Primary angle closure preferred practice pattern(®) guidelines. Ophthalmology. 2016;123:P1–P40. [DOI] [PubMed] [Google Scholar]
- 15.European Glaucoma Society. Terminology and guidelines for glaucoma (OL). 2014. Available at: www.eugs.org. [DOI] [PubMed]
- 16.Mangione CM, Berry S, Spritzer K, et al. Identifying the content area for the 51-item National Eye Institute Visual Function Questionnaire: results from focus groups with visually impaired persons. Arch Ophthalmol. 1998;116:227–233. [DOI] [PubMed] [Google Scholar]
- 17.Mangione CM, Lee PP, Pitts J, et al. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ). NEI-VFQ Field Test Investigators. Arch Ophthalmol. 1998;116:1496–1504. [DOI] [PubMed] [Google Scholar]
- 18.Reynaud C, Rousseau A, Kaswin G, et al. Persistent impairment of quality of life in patients with herpes simplex keratitis. Ophthalmology. 2017;124:160–169. [DOI] [PubMed] [Google Scholar]
- 19.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. [DOI] [PubMed] [Google Scholar]
- 20.Zhang J, Shia B, Yi H, et al. Illness and medical and other expenditures: observations from western and eastern China. BMC Health Serv Res. 2015;15:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cho HK, Kee C. Population-based glaucoma prevalence studies in Asians. Surv Ophthalmol. 2014;59:434–447. [DOI] [PubMed] [Google Scholar]
- 22.Cheng JW, Cheng SW, Ma XY, et al. The prevalence of primary glaucoma in mainland China: a systematic review and meta-analysis. J Glaucoma. 2013;22:301–306. [DOI] [PubMed] [Google Scholar]
- 23.Yamamoto T, Iwase A, Araie M, et al. The Tajimi Study report 2: prevalence of primary angle closure and secondary glaucoma in a Japanese population. Ophthalmology. 2005;112:1661–1669. [DOI] [PubMed] [Google Scholar]
- 24.He M, Foster PJ, Ge J, et al. Prevalence and clinical characteristics of glaucoma in adult Chinese: a population-based study in Liwan District, Guangzhou. Invest Ophthalmol Vis Sci. 2006;47:2782–2788. [DOI] [PubMed] [Google Scholar]
- 25.Vijaya L, George R, Asokan R, et al. Prevalence and causes of low vision and blindness in an urban population: the Chennai Glaucoma Study. Indian J Ophthalmol. 2014;62:477–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wong TY, Foster PJ, Seah SK, et al. Rates of hospital admissions for primary angle-closure glaucoma among Chinese, Malays, and Indians in Singapore. Br J Ophthalmol. 2000;84:990–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khor CC, Do T, Wang N, et al. Genome-wide association analyses identify five new susceptibility loci for primary angle-closure glaucoma. Nat Genet. 2016;48:556–562. [DOI] [PubMed] [Google Scholar]


