Abstract
Nationwide firearm-related mortality rates increased in 2015–17 after remaining relatively stable in 1999–2014. Recent increases are reflected across most states and demographics to varying degrees, which suggests a worsening epidemic of firearm mortality that is geographically and demographically broad. In both time periods the fractions of firearm deaths due to suicide and homicide remained consistent.
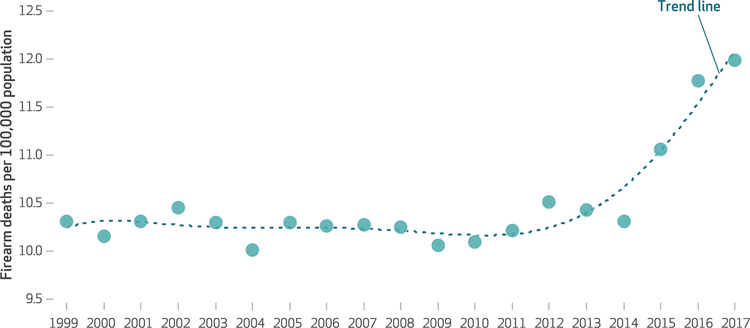
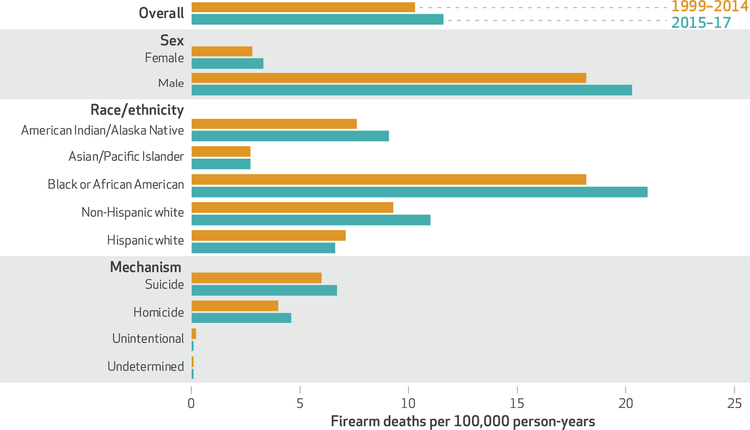
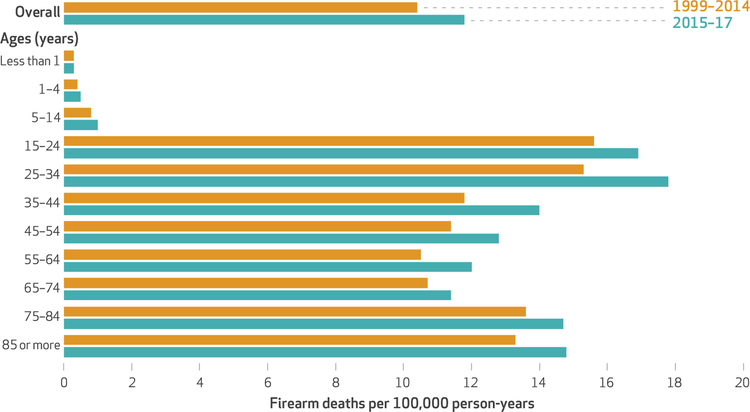
Rates of firearm homicides, suicides, and unintentional deaths in the US are 25.2, 8.0, and 6.2 times higher, respectively, than rates in other developed countries.1 These grave statistics are magnified by the fact that age-adjusted firearm mortality rates in the US, after remaining relatively stable from 1999 to 2014, increased for three consecutive years (exhibit 1). The increases are apparent across most demographics and mechanisms of death (exhibits 2 and 3).
EXHIBIT 1. Age-adjusted rates of firearm mortality per 100,000 population in the US, 1999–2017.
SOURCE Authors’ analysis of data for 1999–2017 from the Wide-ranging Online Data for Epidemiologic Research (WONDER) tool maintained by the Centers for Disease Control and Prevention. NOTE The trend line was superimposed to smooth out the year-to-year fluctuation in the data.
EXHIBIT 2. Age-adjusted rates of firearm mortality per 100,000 person-years in the US in 1999–2014 and 2015–17, by sex, race/ethnicity, and mechanism of death.
SOURCE Authors’ analysis of data for 1999–2017 from the Wide-ranging Online Data for Epidemiologic Research (WONDER) tool maintained by the Centers for Disease Control and Prevention.
EXHIBIT 3. Rates of firearm mortality per 100,000 person-years in the US in 1999–2014 and 2015–17, by age.
SOURCE Authors’ analysis of data for 1999–2017 from the Wide-ranging Online Data for Epidemiologic Research (WONDER) tool maintained by the Centers for Disease Control and Prevention. NOTE All rates are crude (that is, not age adjusted).
We used death records from the Wide-ranging Online Data for Epidemiologic Research (WONDER) tool maintained by the Centers for Disease Control and Prevention (CDC)2 to construct state-specific mortality trajectories and determine how mortality increases seen in 2015–17, relative to 1999–2014, are reflected across states and subpopulations. Most subpopulations have seen recent increases in firearm mortality, as shown in online appendix exhibits 1–3,3 with many states showing increases in firearm mortality across nearly all demographics and subcategories. Prior analyses have shown how national trends break down by age, race/ethnicity, and mechanism of death,4 but none have displayed state-level variability in those trends.
Study Data And Methods
Using the CDC WONDER mortality database2 and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10), codes (W32–W34, X72–74, X93–95, Y22–Y24, Y35.0, and U01.4), we extracted firearm-specific mortality rates for each state (in this article, “state” includes the District of Columbia) and each year in the period 1999–2017. Subsequent queries extracted the mechanisms of suicide-specific (codes X72–X74), homicide-specific (X93–X95, Y35.0, and U01.4), and unintentional (W32–W34) firearm deaths. We also obtained overall firearm mortality rates by sex (male or female), race/ethnicity (black or African American, non-Hispanic white, Hispanic white, Asian/Pacific Islander, and American Indian/Alaska Native), and age group (ages less than 1, 1–4, 5–14, and so on up to 75–84 and 85 or more). Hispanic ethnicity was not analyzed among nonwhite races because of high suppression rates (counts below ten are suppressed in all CDC WONDER queries; see the appendix for a discussion of suppression rates).3 All rates (except age-specific rates) were age adjusted using data from the 2000 census. All mortality rates are expressed per 100,000 person-years.
To analyze state- and subpopulation-specific changes in firearm mortality rates in the period 1999–2014 compared to those in 2015–17, we calculated those rates across states and subpopulations in 1999–2014 and 2015–17 and percentage changes between the two time periods. We repeated that analysis for overall firearm mortality, firearm suicide, and firearm homicide.
To more precisely understand within-state trajectories of firearm mortality, we used generalized additive models,5 a regression-based approach to estimating the relationship between variables (in this case, year and age-adjusted mortality rate) without prespecifying the nature of the relationship (for example, linear). In addition, we conducted trend tests for both the full trajectory in 1999–2017 and the trajectory in just 1999–2014, as a rough diagnostic of whether temporal variation was primarily due to more recent shifts. We characterized differences across states in their trajectories in terms of the percentage change in overall fitted age-adjusted firearm mortality rates in 2017, relative to rates in 1999, and in terms of the standard deviation of the year-level estimates from the fitted state-level trajectory. Finally, we broke down state-level mortality trajectories by demographic and sub-type using a slightly modified generalized additive model framework. The methods described in this paragraph are explicated further in the appendix.3
Our analysis had several limitations. First, it was restricted by the suppression of rates in lower-population areas and among smaller subpopulations. Given known geographic differences in rates of different types of firearm-related mortality, such as firearm-related suicide,6 this may have limited the generalizability of our results. However, we were able to characterize risks that affect the greatest numbers of people.
Second, our analysis did not consider nonfatal firearm injuries. This limitation represents an opportunity to highlight the critical need for high-quality data on such injuries.
Third, our subpopulation-specific trend analysis relied on some interpolation to present the most complete picture possible. However, generalized additive models are well suited to smoothly estimating partially observed functions and providing a view that is unobscured by random year-to-year fluctuation.
Finally, the thrust of the analysis focused on the recent increase in mortality in 2015–17. Theoretically, this increase could have arisen from random variation. However, the consistency we found across states and subpopulations makes that possibility less likely.
Study Results
There were 497,627 firearm deaths in 1999–2014 (10.4 per 100,000 person-years), of which 291,623 (58.6 percent) were suicides and 191,531 (38.5 percent) were homicides. There were 114,683 firearm deaths in 2015–17 (11.8 per 100,000 person-years—a 13.8 percent increase from 1999–2014), of which 68,810 (60.0 percent) were suicides and 43,483 (37.9 percent) were homicides (data not shown). Appendix exhibit 3 shows percentage changes in mortality rates in 2015–17, relative to 1999–2014, by subcategory (age, sex, race/ethnicity, and mechanism) for each state.3 When we looked at all of the nonsuppressed rates together, 81.2 percent showed increased mortality in 2015–17 relative to 1999–2014; that percentage differed across states, demographics, and mechanisms. For example, female mortality rates increased in 90.0 percent of states where the rate was not suppressed (only one rate was suppressed). Only California (88.2 percent), New York (87.5 percent, with one rate suppressed), and the District of Columbia (90.0 percent, with seven rates suppressed) saw mortality reductions in a majority of categories. The only demographic that showed majority decreases in mortality were Hispanic whites (55.6 percent, with fifteen rates suppressed); the only mechanism was unintentional firearm deaths (78.3 percent, with twenty-eight rates suppressed). Absolute firearm mortality rates by state, demographic, and mechanism are shown in appendix exhibits 1 and 2, for 1999–2014 and 2015–17, respectively.3
CHANGES IN RATES BY STATE AND DEMOGRAPHIC GROUP
Appendix exhibits 4–9 show firearm homicide and suicide rates—and percentage changes from 1999–2014 to 2015–17—across states and demographics.3 Analogous to the overall firearm mortality results, there were increases across a large majority of unsuppressed rates (homicide, 76.2 percent; suicide, 82.0 percent), though the median change across all unsuppressed rates was larger among homicides (22.7 percent) than among suicides (14.7 percent). Not all states mirrored the national pattern of similar relative increases in both homicide and suicide. For example, Delaware saw an increase from 9.2 firearm deaths per 100,000 person-years in 1999–2014 to 11.6 deaths in 2015–17, but most of that increase was due to the increase in firearm homicides (from 3.9 per 100,000 person-years to 6.0).
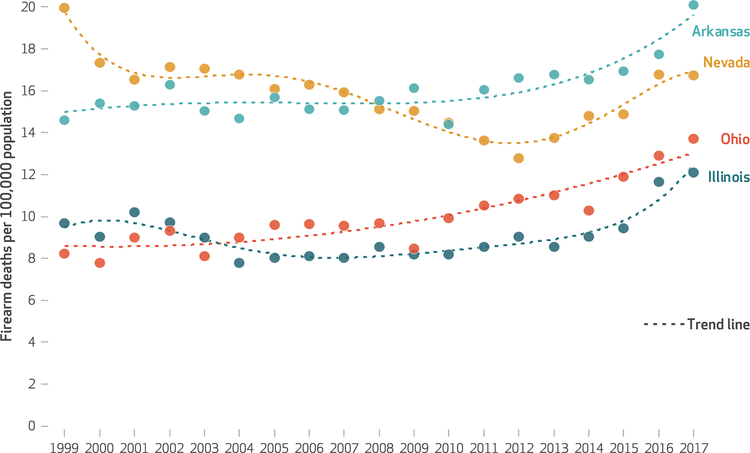
Firearm-related mortality rates in 1999, 2014, and 2017 and scale-less trajectories of overall firearm mortality in 1999–2017 in each state are shown in appendix exhibit 10.3 Only Connecticut, Hawaii, Massachusetts, and Rhode Island did not have time-varying mortality rates. Among the remaining states, a large majority showed one of three growth patterns: linear or nearly linear (twelve), roughly bowl-shaped (seven), or growth mirroring the national trend that began as a plateau but shifted to an increase (twenty-one). Only four states (Arizona, California, Nevada, and New York) and the District of Columbia showed clear evidence of a decrease in the time period 1999–2017. When we restricted our analysis to 1999–2014, twenty states no longer had significant temporal trends. Exhibit 4 shows the trajectories for four states that collectively represent the three common growth patterns—roughly linear increase, plateau followed by increase, roughly bowl-shaped—additionally showing one decreasing trajectory (Nevada).
EXHIBIT 4. Age-adjusted firearm mortality rate trajectories in four states, 1999–2017.
SOURCE Authors’ analysis of data for 1999–2017 from the Wide-ranging Online Data for Epidemiologic Research (WONDER) tool maintained by the Centers for Disease Control and Prevention. NOTES The trend lines were superimposed to smooth out the year-to-year fluctuation in the data. The states selected for this exhibit were chosen as typical examples of the three most common growth patterms—nearly linear increase (Ohio), a plateau followed by an increase (Arkansas), and a roughly bowl-shaped trajectory (Illinois)—and, in addition, a nonlinear but generally decreasing trajectory (Nevada).
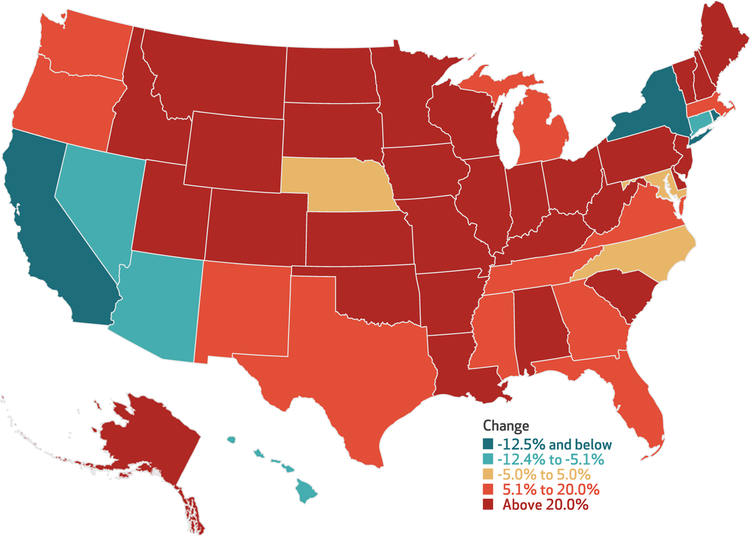
Exhibit 5 shows the percentage changes in the fitted age-adjusted firearm mortality rates for each state in 2017 relative to 1999. Only nine states (including the District of Columbia, which is too small a jurisdiction to appear on the map) had lower fitted firearm mortality rates in 2017 than in 1999, with the District of Columbia (−43.7 percent), New York (−27.7 percent), Rhode Island (−14.8 percent), and California (−14.4 percent) showing the largest decreases. Among the more than half of states shown as having increases above 20 percent, North Dakota (79.9 percent), Missouri (64.1 percent), Ohio (62.5 percent), and New Hampshire (58.2 percent) showed the largest increases.
EXHIBIT 5. Percent changes in fitted firearm mortality rates, by state, from 1999 to 2017.
SOURCE Authors’ analysis of data for 1999–2017 from the Wide-ranging Online Data for Epidemiologic Research (WONDER) tool maintained by the Centers for Disease Control and Prevention. NOTES The changes were calculated with regard to the fitted trends, rather than the observed rates, to characterize the trend as opposed to the values in only 1999 and 2017. The data used to produce the fitted trends were age-adjusted rates.
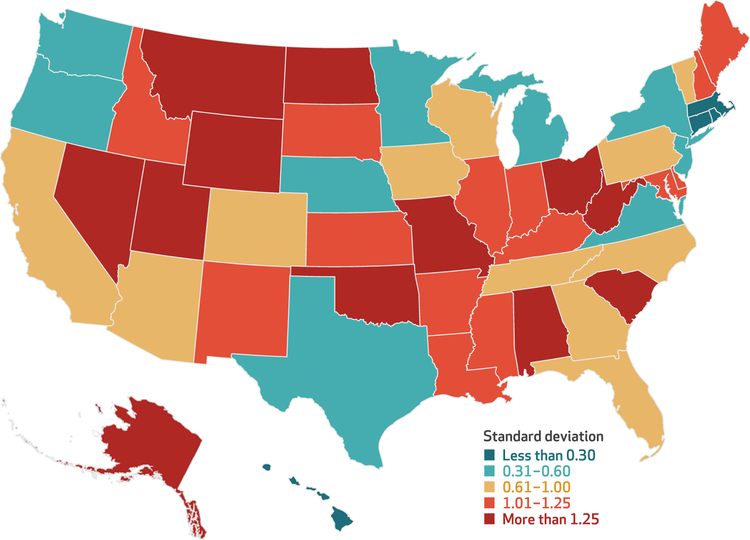
Exhibit 6 shows the standard deviation of the year-level estimates from the estimated (fitted) state-level firearm mortality trajectory. Small values indicate little year-to-year variability in the trend (for example, a trend that is nearly constant over time), while large values indicate more year-to-year variability in the trajectory. There was substantial spatial variation in the level of temporal variability, with Missouri (the state with the greatest standard deviation, 2.53), showing more than fifteen times the variation of Connecticut (the state with the smallest standard deviation, 0.16).
EXHIBIT 6. Between-year variation in firearm mortality, by state, 1999–2017.
SOURCE Authors’ analysis of data for 1999–2017 from the Wide-ranging Online Data for Epidemiologic Research (WONDER) tool maintained by the Centers for Disease Control and Prevention. NOTES The measure of variation was the standard deviation of the values for each year that made up the fitted trend. Small values indicate a nearly constant trajectory (for example, a completely constant trajectory would produce a standard deviation of zero), and larger values indicate a more variable trajectory. The data used to produce the fitted trends were age-adjusted rates.
SUBPOPULATION TRAJECTORIES WITHIN EACH STATE
Appendix exhibit 11 shows a state-by-state breakdown of firearm mortality trends within subpopulations based on age, sex, race/ethnicity, and mechanism (suicide or homicide), expressed as relative changes from baseline (1999).3 Several states showed relative uniformity in temporal changes across subpopulations. For example, the overall decreasing trend in California seen during the latter half of the period 1999–2017 was observed in nearly every subpopulation. Similarly, the nonlinear patterns in states such as Nevada and Illinois were relatively consistent across subpopulations. Other states showed heterogeneity across subpopulations in the temporal trend: For example, while the overall firearm mortality rate increased in Pennsylvania, among African Americans it was roughly constant, and among Hispanic whites it decreased.
Discussion
More than 610,000 people died from firearms in the US in the period 1999–2017, and temporal patterns in firearm death rates varied across states, subpopulations, and mechanisms of firearm mortality (suicide or homicide). Subpopulation trends departed from the overall state trend in some cases (for example, Pennsylvania), but not in others (such as California). One common feature was that twenty-one states showed evidence of mirroring the national trend of a marked increase in mortality in 2015–17. This increase was reflected to varying degrees across demographics and mechanisms of death. These facts suggest a worsening epidemic of firearm mortality that is geographically and demographically broad.
Some states (for example, California and New York) and subpopulations (such as Hispanic whites) appeared to be more insulated against national increases in firearm mortality, while other states (for example, Missouri and Ohio) and subpopulations (such as females and non-Hispanic whites) were more affected. Strategies focusing on those subpopulations may be an important part of reversing the current trend. Analogously, geographically specific prevention strategies should be aligned with cause-specific strategies. For example, suicide remains the most common mechanism of firearm mortality in most states, and the availability of a firearm dramatically increases the lethality of a suicide attempt.7 Jurisdictions with higher rates of mental health disorders that facilitate suicidal ideation (for example, substance use disorder),8 those with subpopulations at higher risk for suicide attempt (such as the elderly and males),9 and those in rural areas (where suicide risk is higher)6 might consider suicide-specific prevention strategies.
Policy-based interventions can have different effects on different subpopulations. For example, women have an elevated risk for firearm mortality related to domestic violence.10 This suggests that the use of extreme risk protection orders would primarily affect firearm mortality among females, which has risen in most states. However, these orders are relatively new, and their effectiveness at preventing firearm mortality related to domestic violence is unknown. Yet there is evidence that firearm restrictions for domestic violence offenders or people convicted of violent misdemeanors correspond to reductions in domestic violence homicide.11 Similarly, there are policies that have child-specific effects. Laws preventing child access correspond to lower rates of firearm suicide12 and unintentional firearm death13 among children. Policy proposals should consider state-specific firearm mortality epidemiology, including both the demographic subgroups most affected and the predominant mechanisms of death.
Conclusion
The firearm mortality rate in the US increased by nearly 14 percent in 2015–17, relative to 1999–2014, and the temporal trends in firearm mortality varied by subpopulation and across regions. The epidemiology of firearm violence is complex and varies based on the mechanism of death, demographic group under study, and regionally specific culture, making a one-size-fits-all solution inappropriate.
Supplementary Material
Acknowledgments
The work of Jason Goldstick, April Zeoli, and Rebecca Cunningham was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grant No. R24HD087149 to the Firearm Safety Among Children and Teens Consortium; principal investigator: Rebecca Cunningham). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Jason E. Goldstick, Department of Emergency Medicine, University of Michigan Medical School, in Ann Arbor
April Zeoli, School of Criminal Justice, Michigan State University, in East Lansing.
Christina Mair, Department of Behavioral and Community Health Sciences, University of Pittsburgh Graduate School of Public Health, in Pennsylvania.
Rebecca M. Cunningham, Department of Emergency Medicine, University of Michigan Medical School, and a professor in the Department of Health Behavior and Health Education, University of Michigan School of Public Health
NOTES
- 1.Grinshteyn E, Hemenway D. Violent death rates: the US compared with other high-income OECD countries, 2010. Am J Med 2016;129(3): 266–73. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. CDC WONDER: multiple cause of death data [Internet]. Atlanta (GA): CDC; [last reviewed 2018 Dec 6; cited 2019 Jul 24]. Available from: https://wonder.cdc.gov/mcd.html [Google Scholar]
- 3. To access the appendix, click on the Details tab of the article online.
- 4.Wintemute GJ. The epidemiology of firearm violence in the twenty-first century United States. Annu Rev Public Health. 2015;36:5–19. [DOI] [PubMed] [Google Scholar]
- 5.Wood SN. Generalized additive models: an introduction with R 2nd ed. Boca Raton (FL): CRC; 2017. [Google Scholar]
- 6.Congdon P The spatial pattern of suicide in the US in relation to deprivation, fragmentation, and rurality. Urban Stud 2011;48(10): 2101–22. [DOI] [PubMed] [Google Scholar]
- 7.Spicer RS, Miller TR. Suicide acts in 8 states: incidence and case fatality rates by demographics and method. Am J Public Health. 2000;90(12): 1885–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Substance Abuse and Mental Health Services Administration. Behavioral health, United States, 2012 [Internet]. Rockville (MD): SAMHSA; 2013. [cited 2019 Jul 24]. (HHS Publication No. [SMA] 13–4797). Available from: https://www.samhsa.gov/data/sites/default/files/2012-BHUS.pdf [PubMed] [Google Scholar]
- 9.Bertolote JM, Fleischmann A. A global perspective in the epidemiology of suicide. Suicidologi [serial on the Internet]. 2002. [cited 2019 Aug 2]. Available for download from: https://www.journals.uio.no/index.php/suicidologi/article/view/2330
- 10.Fox JA, Fridel EE. Gender differences in patterns and trends in U.S. homicide, 1976–2015. Violence Gend 2017;4(2):37–43. [Google Scholar]
- 11.Zeoli AM, McCourt A, Buggs S, Frattaroli S, Lilley D, Webster DW. Analysis of the strength of legal firearms restrictions for perpetrators of domestic violence and their association with intimate partner homicide. Am J Epidemiol 2018; 187(7):1449–55. [DOI] [PubMed] [Google Scholar]
- 12.Webster DW, Vernick JS, Zeoli AM, Manganello JA. Association between youth-focused firearm laws and youth suicides. JAMA 2004;292(5): 594–601. [DOI] [PubMed] [Google Scholar]
- 13.Webster DW, Starnes M. Reexamining the association between child access prevention gun laws and unintentional shooting deaths of children. Pediatrics. 2000;106(6): 1466–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.