Abstract
First-degree relatives of women with breast cancer may experience increased worry or perceived risk when faced with reminders of their own cancer risk. Worry and risk reminders may include physical symptoms (e.g., persistent breast pain) and caregiving experiences. Women who engage in pain catastrophizing may be particularly likely to experience increased distress when risk reminders are present. We examined the degree to which persistent breast pain and experience as a cancer caregiver were related to cancer worry and perceived risk in first-degree relatives of women with breast cancer (N = 85) and how catastrophic thoughts about breast pain could impact these relationships. There was a significant interaction between persistent breast pain and pain catastrophizing in predicting cancer worry (p = .03); among women who engaged in pain catastrophizing, cancer worry remained high even in the absence of breast pain. Pain catastrophizing also moderated the relationships between caregiving involvement and cancer worry (p=0.003) and perceived risk (p=0.03). As the degree of caregiving responsibility increased, cancer worry and perceived risk increased for women who engaged in pain catastrophizing; levels of cancer worry and perceived risk remained low and stable for women who did not engage in pain catastrophizing regardless of caregiving experience. The results suggest that first-degree relatives of breast cancer survivors who engage in pain catastrophizing may experience greater cancer worry and perceived risk and may benefit from interventions aimed at reducing catastrophic thoughts about pain.
Keywords: Breast cancer, first-degree relative, breast pain, caregiving, pain catastrophizing
Introduction
Breast cancer is the most commonly diagnosed cancer in women and the second leading cause of women’s cancer-related deaths [1]. An estimated 252,710 new cases and 40,610 deaths due to breast cancer are expected in 2017 in the United States [1]. Diagnostic and treatment advances have resulted in a significant decline in breast cancer mortality, with the death rate dropping 38% since 1989 [1]. Despite improved early detection and overall decreased mortality, many women experience significant psychological distress and worry regarding their risk of breast cancer [2–4]. Women with a first-degree relative with breast cancer are two to four times more likely to develop breast cancer than those without a family history of breast cancer [5–8], and rate their risk of developing breast cancer on measures of risk perception as higher than women with a second- or third-degree relative with breast cancer [9]. These women are at particularly high risk for distress and worry related to their breast cancer risk [10]. Exposure to reminders of their own risk may serve as cues for higher levels of cancer worry or greater perceived risk. Understanding worry and perceived risk is particularly important for first degree relatives of women with breast cancer not only because of the association between worry and perceived risk with increased overall psychological distress, but also because worry and perceived risk can lead to avoidance or delay of regular mammograms and other important breast cancer screening behaviors [11, 12].
While population based figures are currently unknown, estimates suggest as many as 70% of women experience breast pain (i.e., mastalgia) at some point during their adult lives, with 10–30% experiencing pain that is severe [13–15]. Past work has found that women who report breast pain are not at increased risk of being diagnosed with breast cancer, suggesting breast pain is not a feature unique to cancer-prone breast tissue [13]. Despite this, women with a family history of breast cancer who experience breast symptoms, including pain, have been found to experience greater psychological distress when compared with women experiencing symptoms who do not have a family history of breast cancer [16]. One possible explanation for the increased psychological distress is that breast symptoms, like episodes of breast pain, may result in greater cancer worry and perceived risk of breast cancer.
Another possible reminder of cancer risk and trigger for cancer worry is a woman’s experience caring for a close relative with breast cancer. Research consistently shows that familial caregivers of cancer patients may experience psychological distress that can persist long after the termination of their caregiving experience [17–19]. Female, familial caregivers (i.e., daughters), in particular, have been shown to appraise the caregiving experience as more negative and stressful when compared to male caregivers (i.e., sons) [20], and to experience high levels of cancer-specific distress [17, 21].Qualitative data suggest that caring for a first-degree relative with breast cancer may result in increased psychological distress by impacting women’s perceptions of their personal risk of breast cancer; women report feeling increasingly vulnerable to a future cancer diagnosis as a result of their involvement in caregiving and exposure to their relative’s cancer [21]. Female, familial caregivers are confronted with caring for their loved one while also processing that they too may be at increased risk for cancer as a result of their loved one’s diagnosis [21].
First-degree relatives of women with breast cancer who experience persistent breast pain and/or served as a caregiver for a relative with breast cancer may be more likely to engage in pain catastrophizing. Pain catastrophizing is the tendency to maintain exaggerated negative thoughts in response to and in anticipation of pain [30]. Research suggests that pain catastrophizing is associated with increased emotional distress, more intense pain, and avoidance of activities associated with pain and may be indicative of poor adjustment to pain. Pain catastrophizing may impact the pain experience of first degree relatives with persistent breast pain and negatively impact their overall well-being, particularly if pain catastrophizing interferes with adherence to regular cancer screening [31, 33]. In fact, pain catastrophizing has been associated with more severe pain during mammography [32], which can impact future screening behaviors [34].
Further, caregivers often witness their loved one’s pain and distress and report seeing their family member in pain as one of the most stressful and troubling parts of caregiving [22–26]. Caring for a cancer patient with pain may result in added caregiver burden, putting caregivers at increased risk for tension, depression, total mood disturbance, fatigue, and poorer health status [26, 27]. Brain imaging research has shown that when individuals are asked to perceive and assess painful situations experienced by others, cortical areas known to play a significant role in pain processing (i.e., anterior cingulate and anterior insula) are activated [28, 29]. Thus, it is possible that these areas are activated for cancer caregivers witnessing a loved one in pain and prompt anticipation of pain in oneself if one was to encounter a similar situation. Pain catastrophizing has been hypothesized as a marker of pain anticipation and may impact caregivers’ perceptions of cancer risk and worry about a future cancer diagnosis. The present cross-sectional study examined the influence of persistent breast pain and experience as the caregiver for a relative with breast cancer on cancer worry and perceived risk of breast cancer among women with a first-degree relative with breast cancer. The degree to which pain catastrophizing influenced the relationship between reminders of risk (i.e., persistent breast pain, caregiving) and measures of cancer worry and perceived risk was also examined. It was hypothesized that the presence of persistent breast pain and a greater degree of caregiving responsibility would be correlated with increased cancer worry and perceived risk of breast cancer. It was also hypothesized that catastrophic thoughts about breast pain would moderate these relationships such that the magnitude of the relationships would be greater for women reporting higher levels of pain catastrophizing.
Materials and Methods
Participants
Women were recruited from the Department of General Internal Medicine (GIM) at Duke University Medical Center (DUMC). Eligible participants 1) were female; 2) were 45 years of age or older, 3) had a family history of breast cancer in at least one first-degree relative, 4) had no personal history of cancer (except basal or squamous cell skin cancer), and 5) were able to speak and read English. The study was performed under an institutional review board-approved protocol and was HIPAA compliant. Overall, 126 women enrolled in the study. Of these, 10 were excluded because they were later found to be ineligible. The present study focused on the degree to which pain catastrophizing influenced the relationship between reminders of risk and measures of cancer worry and perceived risk. Consequently, participants with missing data on the pain catastrophizing variable were excluded. Data on pain catastrophizing was available for 85 of the 116 (73.3%) individuals participating in the study; the remaining 31 participants (26.7%) were excluded due to incomplete data. There were no significant differences between those included and those excluded due to missing data on pain catastrophizing on sociodemographic variables or other variables of interest with the exception of age and persistent breast pain; women who were excluded were older (M=64.9 vs. 60.4) and less likely to have experienced breast pain for 6 months or longer (3% vs. 39%).
Procedures
Study participants provided verbal and written informed consent in a manner that was compliant with the Duke University Health System Institutional Review Board. Contact information was gathered from women who met study criteria and were consented into the study. Women were then mailed a study packet that included self-report assessment tools as well as a postage paid mailing envelope to use when returning the completed assessment. Questionnaires included assessments of socio-demographics (e.g., age, race, partner status), breast pain, caregiving, pain catastrophizing, breast cancer worry, and perceived risk of breast cancer. Women received $10 for completing the assessment.
Measures
All measures were written at an eighth grade reading level and were color coded with clearly marked instructions to assist participants with completion.
Sociodemographic information.
Sociodemographic information collected included age, race, education, and household income.
Breast pain questionnaire.
Persistent breast pain was assessed using an item adapted from the McGill Pain Questionnaire (MPQ) [35] that asked participants about the duration of their breast pain (i.e., “How long have you had breast pain?”). Persistent breast pain was coded as occurring if participants reported having breast pain for more than 6 months and not occurring if they reported having breast pain for 6 months or less. The MPQ has been used in prior research to assess breast pain [13, 36].
Caregiving.
The level of caregiving for a first-degree relative with breast cancer was assessed with an item that asked: “To what degree were you involved in the caregiving of your affected relative?” Participants responded using a 5-point scale (0 = not at all to 4 = a lot).
Pain catastrophizing.
The Pain Catastrophizing Scale (PCS) [37] was used to assess catastrophizing about breast pain. Participants rated how often when having breast pain they had different thoughts and feelings related to helplessness (6 items), magnification (3 items), and rumination (4 items). Each item was rated on a 5-point scale (0 = not at all to 4 = always); items were summed and a total score was used. The PCS has been shown to be a reliable and valid measure in nonclinical samples [38, 39], and we found good internal consistency in this sample (Cronbach’s alpha = .95).
Breast cancer worry.
Cancer worry was assessed using four items from the Cancer Worry Scale (CWS) [40]. Each item (e.g., “how often do you worry about breast cancer?”; “how much do your worries about breast cancer affect your mood?”; “how concerned are you about getting breast cancer?”) used a 0 (not at all) to 6 (very much) response scale. Items were summed and a total score was used. The CWS has been used extensively among first-degree relatives of breast cancer survivors [41, 42], and has been shown to be reliable [10, 42, 43]. In the present sample, this scale demonstrated good internal consistency (Cronbach’s alpha = .85).
Perceived risk of breast cancer.
Perceived risk was measured using 5 items. The items included: “Compared to other women your age what do you believe is the likelihood that you will develop breast cancer in the future?;” “I feel at risk for breast cancer;” “What do you think is your risk for developing breast cancer in the future?;” “The chances that I might develop breast cancer are pretty high;” and “No matter what I do, there’s a good chance of developing breast cancer” [44–46]. Responses to each item were coded using a 0 to 10 response scale with higher scores indicating greater perceived risk. Items were summed to create a total score. This scale had good internal consistency in this sample (Cronbach’s alpha = .81).
Statistical Analyses
Descriptive statistics were computed for all demographic (i.e., age, race, education, income) and study variables. Correlations (Pearson or point-biserial as appropriate) and chi-square analyses were conducted to examine the relationship between participant characteristics, persistent breast pain, degree of caregiving for a first-degree relative with breast cancer, pain catastrophizing, cancer worry, and perceived breast cancer risk as well as the interrelationships between study variables. In all analyses, race was coded as 1 for White and 0 for Non-White. The distribution of pain catastrophizing scores demonstrated a strong positive skew (skew = 4.18) with 54% of women indicating no catastrophizing (i.e., score of zero). As a result, in all analyses, pain catastrophizing was coded as a dichotomous variable, with a score of 0 for no catastrophizing (i.e., score of 0) and 1 for catastrophizing (i.e., score ≥ 1). Significance was set at α < .05.
Multiple linear regression analyses were conducted to examine the relationship between persistent breast pain and caregiving and measures of cancer worry and perceived risk and to test whether pain catastrophizing moderated the effect of persistent breast pain and caregiving on these variables. Separate regression models were conducted with cancer worry and perceived risk as outcomes. Continuous variables were mean centered to aid in the interpretation of results. An empirical selection of control variables was used. Participant demographic characteristics and study variables significantly (p < .05) associated with cancer worry and perceived risk in bivariate analyses were controlled for in subsequent regression analyses. Although participant race was not correlated with outcome variables of interest in this sample, we chose to include it as a control variable based on its demonstrated relationship with our outcomes in past research [47]. Each regression model included demographic variables (e.g., race), persistent breast pain, caregiving, pain catastrophizing, and both, the persistent breast pain x pain catastrophizing and caregiving x pain catastrophizing interaction terms as independent variables. Breast cancer worry and perceived risk were our dependent variables. For significant interaction terms, simple slope analyses were conducted to facilitate interpretation of the interaction [48].
Results
Sample Description.
Patient characteristics and descriptive statistics for study variables are provided in Table 1. Women (N = 85) were on average 60.36 (SD = 10.41) years old. Approximately 71% percent self-identified as White (n = 60) and 24% as Black (n = 20). Close to one-fifth had received a high school degree or less and just over a quarter had some college or vocational training. The majority (54%) had earned a college degree, and of these, more than 30% had completed at least some graduate training. With regard to annual household income, approximately 31% earned less than $20,000, 10% earned between $20,000 and $40,000, 10% earned between $40,000 and $60,000, and 49% earned over $60,000.
Table 1.
Participant Characteristics and Descriptive Study Variables (N=85).
| M | SD | % | N | |
|---|---|---|---|---|
| Age | 60.36 | 10.41 | 80 | |
| Race | ||||
| White | 70.6 | 60 | ||
| Black | 23.5 | 20 | ||
| Hispanic | 2.4 | 2 | ||
| Unknown | 3.5 | 3 | ||
| Education | ||||
| Less Than High School | 3.6 | 3 | ||
| High School Graduate | 15.7 | 13 | ||
| Some College | 26.5 | 22 | ||
| College Degree | 20.5 | 17 | ||
| At Least Some Graduate Work | 33.7 | 28 | ||
| Income | ||||
| Less Than $20,000 | 30.7 | 24 | ||
| $20,000 - $40,000 | 10.2 | 8 | ||
| $40,000 - $60,000 | 10.2 | 8 | ||
| Greater Than $60,000 | 48.7 | 38 | ||
| Persistent Breast Pain (%Yes) | 38.8 | 33 | ||
| Caregiving | 1.76 | 1.61 | 82 | |
| Pain Catastrophizing | 3.34 | 7.81 | 85 | |
| Cancer Worry | 5.58 | 3.87 | 83 | |
| Perceived Risk | 28.27 | 9.28 | 82 |
Note: All available data were used
Thirty-nine percent of participants (n = 33) reported persistent breast pain lasting six months or more, and the average degree of involvement in caregiving was 1.76 (SD = 1.61) on a scale from 0 = not at all to 4 = a lot. Approximately half (46%) of the women reported engaging in some amount of pain catastrophizing and 54% reported no pain catastrophizing. Among those reporting catastrophizing, the average pain catastrophizing score was 7.28 (SD=10.26) with a possible range of 1 to 52. The average cancer worry score was 5.58 (SD = 3.87; possible range 0 to 30), and the average perceived risk score was 28.27 (SD = 9.28; possible range 0 to 50).
Correlational Analyses.
Correlations between demographic variables and study variables are provided in Table 2, and assisted in the selection of covariates. Age was significantly associated with perceived risk, with younger women reporting greater perceived risk. Race was associated with persistent breast pain; white women were more likely to have persistent breast pain than non-white women. Education was associated with perceived risk, suggesting that women with more formal education experienced greater perceived risk. Income was negatively associated with cancer worry and positively associated with perceived risk, with women with lower income reporting greater cancer worry but lower perceived risk. There were no significant relationships found between demographic variables and measures of caregiving or pain catastrophizing. Correlations between study variables are also presented in Table 2.
Table 2.
Correlations between study variables.
| Age | Race | Education | Income | Persistent Breast Pain | Caregiving | Pain Catastrophizing | Cancer Worry | Perceived Risk | |
|---|---|---|---|---|---|---|---|---|---|
| Age | - | ||||||||
| Race | .11 | - | |||||||
| Education | −.07 | .33** | - | ||||||
| Income | −.04 | .51** | .60** | - | |||||
| Persistent Breast Pain | −.04 | .30** | .16 | .14 | - | ||||
| Caregiving | −.10 | −.09 | −.18 | −.22 | .02 | - | |||
| Pain Catastrophizing | −.07 | .16 | .10 | −.06 | .33** | .10 | - | ||
| Cancer Worry | −.15 | −.16 | −.03 | −.25* | .14 | .18 | .28* | - | |
| Perceived Risk | −.27* | .22 | .30** | .24* | .16 | .20 | .18 | .49** | - |
Note. Pearson correlation coefficients are reported for associations between continuous measures, point-biserial correlations are reported for associations between continuous and two-level categorical variables, and Pearson contingency coefficients are reported for associations between categorical variables.
Correlation is significant at 0.05 level
Correlation is significant at 0.01 level
Regression Models.
Table 3 displays the results of the multiple linear regression models. Listwise deletion was used. Missing data on predictor and outcome variables resulted in final sample sizes of n=70 and n=69 for the models examining perceived risk and cancer worry as outcome variables, respectively. Participants who were excluded from the analyses due to missing data did not significantly differ from those included in the analyses on sociodemographic and other variables of interest with the exception of persistent breast pain; participants included in the models were more likely to report breast pain lasting 6 months or more. Unstandardized regression coefficients and standard errors are provided; standardized coefficients cannot be interpreted when an interaction term is included in the model [48].
Table 3.
Multiple regression analysis
| B | SE | t | P | sr2 | |
|---|---|---|---|---|---|
| Cancer Worry (Total R2 = .365) | |||||
| Age | −.01 | .05 | −.23 | .82 | .000529 |
| Race | −1.00 | 1.34 | −.74 | .46 | .005776 |
| Education | .53 | .36 | 1.49 | .14 | .02 |
| Income | −.29 | .21 | −1.36 | .18 | .02 |
| Persistent Breast Pain | 1.79 | 1.42 | 1.26 | .21 | .02 |
| Caregiving | −.27 | .39 | −.70 | .49 | .005184 |
| Pain Catastrophizing | 4.35 | 1.27 | 3.43 | .001 | .12 |
| Persistent Breast Pain x Pain Catastrophizing | −4.33 | 1.92 | −2.26 | .03 | .05 |
| Caregiving x Pain Catastrophizing | 1.78 | .58 | 3.04 | .003 | .10 |
| Perceived Risk (Total R2 = .294) | |||||
| Age | −.12 | .10 | −1.16 | .25 | .02 |
| Race | −.42 | 2.85 | −.15 | .88 | .000256 |
| Education | 1.84 | .82 | 2.25 | .03 | .06 |
| Income | .59 | .49 | 1.20 | .23 | .02 |
| Persistent Breast Pain | .13 | 3.30 | .04 | .97 | .000016 |
| Caregiving | −.27 | .91 | −.30 | .77 | .001024 |
| Pain Catastrophizing | 3.01 | 2.93 | 1.03 | .31 | .01 |
| Persistent Breast Pain x Pain Catastrophizing | −.55 | 4.39 | −.12 | .90 | .000196 |
| Caregiving x Pain Catastrophizing | 3.09 | 1.36 | 2.28 | .03 | .06 |
Predictors of Cancer Worry.
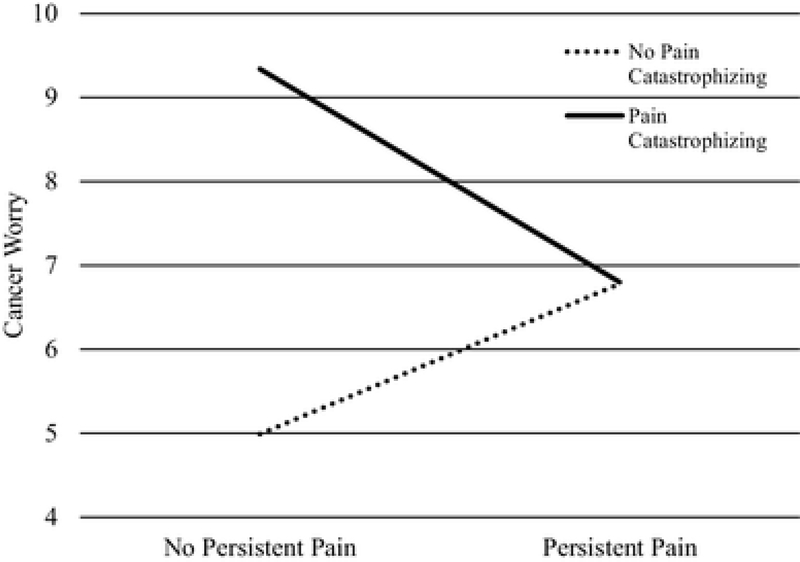
The overall model for cancer worry was significant [total R2 = .37, F (9, 60) = 3.83, p = .001]. The relationship between persistent breast pain and cancer worry was moderated by pain catastrophizing (B = −4.33, SE = 1.92, t = −2.26, p = .03). Figure 1 shows the relationship between persistent breast pain and cancer worry for those who did and did not report pain catastrophizing. Simple slopes were not significant. There was no relationship between persistent breast pain and cancer worry for women who catastrophized about pain (slope: B = −2.54, SE = 1.42, t = 1.78, p = .08) or women who did not catastrophize about pain (slope: B = 1.79, SE = 1.42, t = 1.26, p = .21). However, the intercepts for women who did and did not catastrophize significantly differed, with women who catastrophized experiencing greater cancer worry regardless of whether they experienced persistent breast pain.
Fig. 1.
Cancer worry: persistent breast pain × pain catastrophizing. The line graph illustrates the relationship between persistent breast pain and cancer worry by pain catastrophizing. Lines represent estimated cancer worry scores based on simple slopes analyses
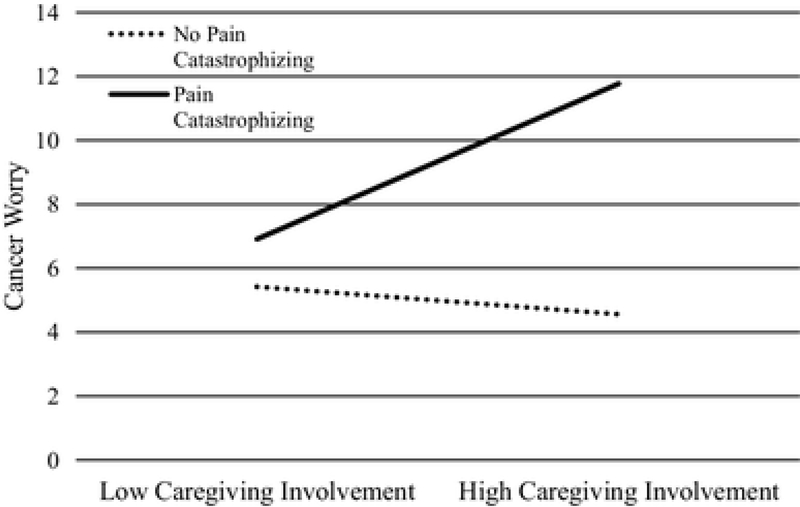
Pain catastrophizing also moderated the relationship between caregiving and cancer worry (B = 1.78, SE = .58, t = 3.04, p = .003). Figure 2 shows the relationship between caregiving and cancer worry for those who did and did not engage in pain catastrophizing. Among women who catastrophized about pain, cancer worry significantly increased as the degree of caregiving increased (slope: B = 1.51, SE = .41, t = 3.66, p < .001). For those who did not engage in pain catastrophizing, cancer worry remained low for those engaging in both low and high levels of caregiving (slope: B = −.27, SE = .39, t = −.070, p = .49).
Fig. 2.
Cancer worry: caregiving involvement × pain catastrophizing. The line graph illustrates the relationship between caregiving involvement and cancer worry by pain catastrophizing. Lines represent estimated cancer worry scores based on simple slopes analyses
Predictors of Perceived Risk.
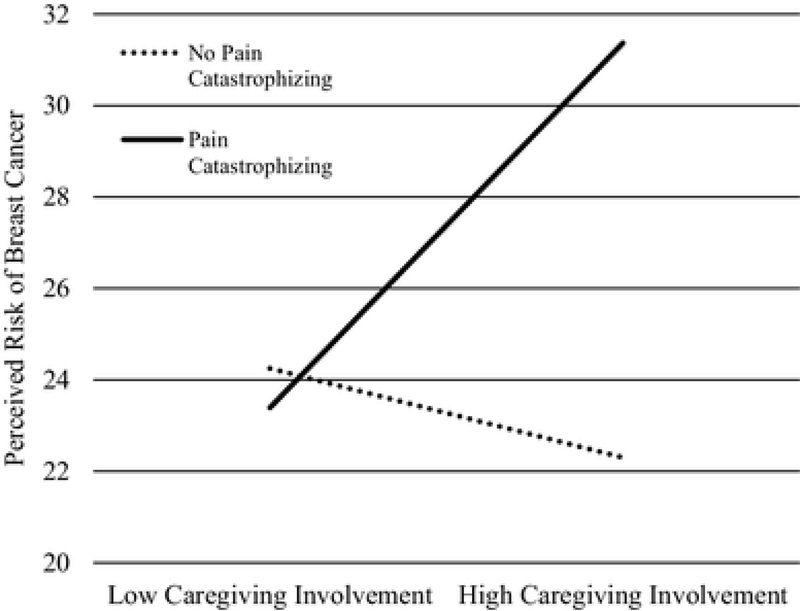
The overall model for perceived breast cancer risk was significant [total R2 = .29, F (9, 59) = 2.73, p = .01]. Pain catastrophizing did not moderate the relationship between persistent breast pain and perceived risk, but there was a significant interaction between pain catastrophizing and caregiving involvement (B = 3.09, SE = 1.36, t = 2.28, p = .03). Figure 3 shows the relationship between caregiving involvement and perceived risk for those who did and did not engage in pain catastrophizing. For those who engaged in pain catastrophizing, perceived risk was low among those with low levels of caregiving involvement, but perceived risk increased as the degree of caregiving involvement increased (slope: B = 2.82, SE = .97, t = 2.89, p = .005). Among women who did not engage in pain catastrophizing, perceived risk was similar at both low and high degrees of caregiving involvement (slope: B = −.27, SE = .91, t = −.30, p = .77).
Fig. 3.
Perceived risk of breast cancer: caregiving involvement × pain catastrophizing. The line graph illustrates the relationship between caregiving involvement and perceived risk of breast cancer by pain catastrophizing. Lines represent estimated perceived risk scores based on simple slopes analyses
Discussion
In a cross-sectional sample of first-degree relatives of women with breast cancer, we examined the relationship of persistent breast pain and caregiving involvement with cancer worry and perceived breast cancer risk. We also examined whether these relationships were moderated by pain catastrophizing. Overall, we found pain catastrophizing to moderate the relationships between persistent breast pain and cancer worry, caregiving involvement and cancer worry, and caregiving involvement and perceived risk of breast cancer. First, women with a first-degree relative with breast cancer who engaged in pain catastrophizing had higher levels of cancer worry compared to women who did not engage in pain catastrophizing. However, this relationship was not dependent on women’s reports of persistent breast pain.
Second, the interaction between pain catastrophizing and caregiving involvement in predicting cancer worry was significant. Women reporting low levels of caregiving responsibility for a first-degree relative with breast cancer experienced relatively low levels of cancer worry regardless of whether they engaged in pain catastrophizing. At high levels of caregiving, women who engaged in pain catastrophizing reported much higher levels of cancer worry compared to their counterparts who did not engage in pain catastrophizing. So while caregiving and cancer worry by themselves were not related, among those participants who engaged in pain catastrophizing, higher levels of caregiving were related to higher levels of cancer worry.
Finally, our data suggest that pain catastrophizing moderated the relationship between caregiving and perceived risk. This relationship was similar to the relationship between caregiving and cancer worry such that at low levels of caregiving, women who did and did not engage in pain catastrophizing reported relatively low levels of perceived risk. However, at high levels of caregiving, women who catastrophized about pain reported higher levels of perceived risk compared to their counterparts who did not engage in pain catastrophizing.
These findings are the first to demonstrate that in women with a first-degree relative with breast cancer, pain catastrophizing is important in understanding women’s cancer worry and perceived risk of breast cancer. Women who engaged in pain catastrophizing experienced higher levels of worry, even in the absence of persistent breast pain. Many women experience persistent breast pain and even more experience breast pain from time to time [13, 49]. While breast pain can be related to injury or disease (e.g., leukemia), there is evidence to suggest that breast pain is rarely a presenting symptom of breast cancer [49]. In a study of 5,463 women, 1,532 reported experiencing breast pain, or roughly every one out of three women; however, the results also indicated that those who reported breast pain were actually less likely to be diagnosed with breast cancer [13]. Given that breast pain is common and one of the most frequent concerns of women presenting to specialty breast clinics [49], educating first-degree relatives about pain is important. Providing information about medical resources and training in pain control skills might decrease pain catastrophizing, and ultimately, lower women’s levels of cancer worry and perceived risk.
Interestingly, we found that caregiving was not associated with cancer worry and perceived risk of breast cancer in correlational analyses. However, when examining pain catastrophizing as a moderator, we found that women who were caregivers and engaged in pain catastrophizing were much more likely to experience increased worry and perceived risk. One explanation is that women who were caregivers may have witnessed their loved one’s distress and pain [50]. As a result, when experiencing their own breast pain, these women may have more readily activated pain processing cortical regions (i.e., anterior cingulate and anterior insula). Evidence from the pain literature suggests that simply witnessing a loved one in pain activates the same areas as if physically experiencing the pain oneself [28, 29].
Elevated levels of cancer worry and perceived risk may play a particularly important role in the physical and psychological well-being of women with a family history of breast cancer. These women often overestimate their risk of developing breast cancer [51] and report elevated levels cancer worry and perceived risk. Raveis and Pretter’s [21] study identified shock, denial, panic, fear, distress, and sadness as emotional responses of daughters to their mothers’ diagnosis of breast cancer. As it pertains to cancer worry, these daughters recalled being extremely overwhelmed and traumatized to the degree that they felt very drained, were unable to function, and were affected in their ability to relate to other people. Not only do elevated levels of cancer worry and perceived risk have the capability of affecting these women’s daily lives, but also their breast health and surveillance behaviors (e.g., regular mammograms).
Of particular concern may be women who tend to engage in pain catastrophizing. The findings of the current study may help to identify a particular subset of women who have a first-degree relative with breast cancer for whom pain catastrophizing leads to high levels of distress (i.e., worry, risk perception) and could potentially impact their adherence to breast cancer surveillance behaviors. Research has consistently found high levels of cancer worry to be a barrier to mammography use for women with a family history of breast cancer especially when worry leads to additional distress [3, 52–54]. It is possible that providing psychosocial interventions designed to decrease pain catastrophizing to first-degree relatives of breast cancer survivors may not only decrease distress, cancer worry, and risk perceptions but also increase adherence to surveillance behaviors such as receiving regular and timely mammograms.
Interventions have been developed to help participants better manage pain and have been shown to be efficacious in decreasing pain catastrophizing [55–57]. For example, based on a cognitive-behavioral model, pain coping skills training provides participants with strategies (e.g., cognitive restructuring, relaxation training) to help them better cope with pain by changing their thoughts, feelings and behaviors [56, 58]. Several randomized controlled trials of pain coping skills training protocols have found these interventions to be associated with reductions in pain catastrophizing [59, 60]. However, these interventions have typically been tested among chronic illness populations (e.g., cancer, osteoarthritis). To our knowledge, formal pain coping skills training protocols have not been provided to and tested among first degree relatives of breast cancer survivors with breast pain. Future research should examine the efficacy of pain coping skills training in reducing pain catastrophizing for this population.
Despite the strengths of the present study, there are several limitations that warrant attention. First, this study was limited to first-degree, female relatives of breast cancer survivors. Thus, the results of this study may not generalize to first-degree relatives of cancer survivors with other forms of cancer or to males. Additionally, the relatively small sample size, the exclusion of participants due to missing data, and the fact that the sample was primarily Caucasian, highly educated, and had a high income limits our ability to generalize these results to the larger population of first-degree relatives of breast cancer survivors. Studies with a larger and more diverse (e.g., race, education, income) sample are necessary to confirm the results of the present study.
Second, we present the results of a cross-sectional study. Thus, we cannot determine the direction of the relationships between persistent breast pain and caregiving with cancer worry and perceived risk, and we cannot be certain as to how these relationships and the effect of catastrophic thoughts on these relationships may change over time. A longitudinal study examining these variables is warranted. Finally, it is possible that the relationship between cancer worry and pain catastrophizing could be an indicator of a more generalized tendency to engage in catastrophizing about anxiety-provoking situations. While some studies have found catastrophizing to be highly correlated with trait anxiety, others suggest that catastrophizing may be associated with poor outcomes even after controlling for trait anxiety [30]. Future studies would benefit from exploring the relationship between pain catastrophizing and trait anxiety among first-degree relatives of women with breast cancer.
In summary, this study examined the relationship between persistent breast pain and the amount of caregiving and cancer worry and perceived breast cancer risk in first-degree relatives of women with breast cancer. This study also examined how this relationship is impacted by pain catastrophizing. For cancer worry, pain catastrophizing moderated the effect of persistent breast pain and caregiving on cancer worry. For perceived risk, only pain catastrophizing’s effect on the relationship between caregiving and perceived risk was significant.
Acknowledgements:
This work was supported by a grant from the National Institutes of Health (T32 MH019109).
Footnotes
Ethical Standards
All human studies have been approved by the Duke University Health System Institutional Review Board and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons gave their informed consent prior to their inclusion in the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Contributor Information
Colette A. Whitney, Duke University Medical Center, 2200 W. Main Street, Suite 340, Durham, North Carolina, 27705
Caroline S. Dorfman, Duke University Medical Center, 2200 W. Main Street, Suite 340, Durham, North Carolina, 27705.
Rebecca A. Shelby, Duke University Medical Center, 2200 W. Main Street, Suite 340, Durham, North Carolina, 27705.
Francis J. Keefe, Duke University Medical Center, 2200 W. Main Street, Suite 340, Durham, North Carolina, 27705.
Vicky Gandhi, Duke University Medical Center, 2200 W. Main Street, Suite 340, Durham, North Carolina, 27705.
References
- 1.Siegel RL, Miller KD, and Jemal A, Cancer statistics, 2017. CA: A Cancer Journal for Clinicians, 2017. 67(1): p. 7–30. [DOI] [PubMed] [Google Scholar]
- 2.Loescher LJ, Cancer worry in women with hereditary risk factors for breast cancer. Oncol Nurs Forum, 2003. 30(5): p. 767–72. [DOI] [PubMed] [Google Scholar]
- 3.Lerman C, Kash K, and Stefanek M, Younger women at increased risk for breast cancer: perceived risk, psychological well-being, and surveillance behavior. J Natl Cancer Inst Monogr, 1994(16): p. 171–6. [PubMed] [Google Scholar]
- 4.Gibbons A. and Groarke A, Can risk and illness perceptions predict breast cancer worry in healthy women? J Health Psychol, 2016. 21(9): p. 2052–62. [DOI] [PubMed] [Google Scholar]
- 5.Pharoah PD, et al. , Family history and the risk of breast cancer: a systematic review and meta-analysis. Int J Cancer, 1997. 71(5): p. 800–9. [DOI] [PubMed] [Google Scholar]
- 6.Nelson HD, et al. , Risk factors for breast cancer for women aged 40 to 49 years: a systematic review and meta-analysis. Ann Intern Med, 2012. 156(9): p. 635–48. PCMID: PMC3561467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McPherson K, Steel CM, and Dixon JM, ABC of breast diseases. Breast cancer-epidemiology, risk factors, and genetics. BMJ, 2000. 321(7261): p. 624–8. PCMID: PMC1118507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barlow WE, et al. , Prospective breast cancer risk prediction model for women undergoing screening mammography. J Natl Cancer Inst, 2006. 98(17): p. 1204–14. [DOI] [PubMed] [Google Scholar]
- 9.Tracy KA, et al. , The impact of family history of breast cancer and cancer death on women’s mammography practices and beliefs. Genet Med, 2008. 10(8): p. 621–5. [DOI] [PubMed] [Google Scholar]
- 10.McCaul KD, et al. , A descriptive study of breast cancer worry. J Behav Med, 1998. 21(6): p. 565–79. [DOI] [PubMed] [Google Scholar]
- 11.Hyman RB, et al. , Health Belief Model variables as predictors of screening mammography utilization. J Behav Med, 1994. 17(4): p. 391–406. [DOI] [PubMed] [Google Scholar]
- 12.Kim C, et al. , Quality of preventive clinical services among caregivers in the health and retirement study. J Gen Intern Med, 2004. 19(8): p. 875–8. PCMID: Pmc1492495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khan SA and Apkarian AV, Mastalgia and breast cancer: a protective association? Cancer Detect Prev, 2002. 26(3): p. 192–6. [DOI] [PubMed] [Google Scholar]
- 14.Kataria K, et al. , A systematic review of current understanding and management of mastalgia. Indian J Surg, 2014. 76(3): p. 217–22. PCMID: PMC4141056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ader DN, et al. , Cyclical mastalgia: prevalence and associated health and behavioral factors. J Psychosom Obstet Gynaecol, 2001. 22(2): p. 71–6. [DOI] [PubMed] [Google Scholar]
- 16.Gilbar O, Coping With Threat: Implications for Women With a Family History of Breast Cancer. Psychosomatics, 1998. 39(4): p. 329–339. [DOI] [PubMed] [Google Scholar]
- 17.Erblich J, Bovbjerg DH, and Valdimarsdottir HB, Looking forward and back: Distress among women at familial risk for breast cancer. Annals of Behavioral Medicine, 2000. 22(1): p. 53–59. [DOI] [PubMed] [Google Scholar]
- 18.Romito F, et al. , Informal caregiving for cancer patients. Cancer, 2013. 119 Suppl 11: p. 2160–9. PCMID: PMC3816360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Braun M, et al. , Hidden Morbidity in Cancer: Spouse Caregivers. Journal of Clinical Oncology, 2007. 25(30): p. 4829–4834. [DOI] [PubMed] [Google Scholar]
- 20.Kim Y, Baker F, and Spillers RL, Cancer Caregivers’ Quality of Life: Effects of Gender, Relationship, and Appraisal. Journal of Pain and Symptom Management. 34(3): p. 294–304. [DOI] [PubMed] [Google Scholar]
- 21.Raveis VH and Pretter S, Existential plight of adult daughters following their mother’s breast cancer diagnosis. Psycho-Oncology, 2005. 14(1): p. 49–60. [DOI] [PubMed] [Google Scholar]
- 22.Butler LD, et al. , Psychological distress and pain significantly increase before death in metastatic breast cancer patients. Psychosom Med, 2003. 65(3): p. 416–26. [DOI] [PubMed] [Google Scholar]
- 23.Perreault A, Fothergill-Bourbonnais F, and Fiset V, The experience of family members caring for a dying loved one. International Journal of Palliative Nursing, 2004. 10(3): p. 133–143. [DOI] [PubMed] [Google Scholar]
- 24.Ferrell B, Pain Observed: The Experience of Pain from the Family Caregiver’s Perspective. Clinics in Geriatric Medicine, 2001. 17(3): p. 595–609. [DOI] [PubMed] [Google Scholar]
- 25.Meeker MA, Finnell D, and Othman AK, Family Caregivers and Cancer Pain Management: A Review. Journal of Family Nursing, 2011. 17(1): p. 29–60. [DOI] [PubMed] [Google Scholar]
- 26.Miaskowski C, et al. , Differences in mood states, health status, and caregiver strain between family caregivers of oncology outpatients with and without cancer-related pain. J Pain Symptom Manage, 1997. 13(3): p. 138–47. [DOI] [PubMed] [Google Scholar]
- 27.Ovayolu O, et al. , Pain in cancer patients: pain assessment by patients and family caregivers and problems experienced by caregivers. Support Care Cancer, 2015. 23(7): p. 1857–64. [DOI] [PubMed] [Google Scholar]
- 28.Botvinick M, et al. , Viewing facial expressions of pain engages cortical areas involved in the direct experience of pain. Neuroimage, 2005. 25(1): p. 312–9. [DOI] [PubMed] [Google Scholar]
- 29.Jackson PL, Meltzoff AN, and Decety J, How do we perceive the pain of others? A window into the neural processes involved in empathy. Neuroimage, 2005. 24(3): p. 771–9. [DOI] [PubMed] [Google Scholar]
- 30.Sullivan MJ, et al. , Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain, 2001. 17(1): p. 52–64. [DOI] [PubMed] [Google Scholar]
- 31.Sullivan MJ, et al. , An experimental investigation of the relation between catastrophizing and activity intolerance. Pain, 2002. 100(1–2): p. 47–53. [DOI] [PubMed] [Google Scholar]
- 32.Asghari A. and Nicholas MK, Pain during mammography: the role of coping strategies. Pain, 2004. 108(1): p. 170–179. [DOI] [PubMed] [Google Scholar]
- 33.Shelby RA, et al. , Prospective study of factors predicting adherence to surveillance mammography in women treated for breast cancer. J Clin Oncol, 2012. 30(8): p. 813–9. PCMID: Pmc3295570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Whelehan P, et al. , The effect of mammography pain on repeat participation in breast cancer screening: A systematic review. The Breast, 2013. 22(4): p. 389–394. [DOI] [PubMed] [Google Scholar]
- 35.Melzack R, The McGill Pain Questionnaire: major properties and scoring methods. Pain, 1975. 1(3): p. 277–99. [DOI] [PubMed] [Google Scholar]
- 36.Ferreira VT, et al. , Characterization of chronic pain in breast cancer survivors using the McGill Pain Questionnaire. J Bodyw Mov Ther, 2015. 19(4): p. 651–5. [DOI] [PubMed] [Google Scholar]
- 37.Sullivan MJL, Bishop S, and Pivik J, The Pain Catastrophizing Scale: development and validation. Psychological Assessment, 1995. 7: p. 524–532. [Google Scholar]
- 38.Osman A, et al. , Factor Structure, Reliability, and Validity of the Pain Catastrophizing Scale. Journal of Behavioral Medicine, 1997. 20(6): p. 589–605. [DOI] [PubMed] [Google Scholar]
- 39.Sullivan MJL, Bishop SR, and Pivik J, The Pain Catastrophizing Scale: Development and validation. Psychological Assessment, 1995. 7(4): p. 524–532. [Google Scholar]
- 40.Lerman C, et al. , Psychological side effects of breast cancer screening. Health Psychol, 1991. 10(4): p. 259–67. [DOI] [PubMed] [Google Scholar]
- 41.Quillin JM, et al. , Genetic risk, perceived risk, and cancer worry in daughters of breast cancer patients. J Genet Couns, 2011. 20(2): p. 157–64. PCMID: PMC4870590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mellon S, et al. , Risk perception and cancer worries in families at increased risk of familial breast/ovarian cancer. Psychooncology, 2008. 17(8): p. 756–66. PCMID: PMC3947579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brain K, et al. , A randomized trial of specialist genetic assessment: psychological impact on women at different levels of familial breast cancer risk. Br J Cancer, 2002. 86(2): p. 233–8. PCMID: PMC2375197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weinstein ND and Klein WM, Resistance of personal risk perceptions to debiasing interventions. Health Psychology, 1995. 14(2): p. 132–140. [DOI] [PubMed] [Google Scholar]
- 45.Weinstein ND, et al. , Risk perceptions: Assessment and relationship to influenza vaccination. Health Psychology, 2007. 26(2): p. 146–151. [DOI] [PubMed] [Google Scholar]
- 46.Somers TJ, et al. , Cancer genetics service interest in women with a limited family history of breast cancer. J Genet Couns, 2009. 18(4): p. 339–49. [DOI] [PubMed] [Google Scholar]
- 47.Orom H, et al. , Perceived risk for breast cancer and its relationship to mammography in Blacks, Hispanics, and Whites. J Behav Med, 2013. 36(5): p. 466–76. PCMID: Pmc3565065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aiken LS, West SG, and Reno RR, Multiple regression : testing and interpreting interactions. 1991, Newbury Park, CA: Sage Publications. [Google Scholar]
- 49.Smith RL, Pruthi S, and Fitzpatrick LA, Evaluation and Management of Breast Pain. Mayo Clinic Proceedings. 79(3): p. 353–372. [DOI] [PubMed] [Google Scholar]
- 50.Hashemi-Ghasemabadi M, et al. , Living under a cloud of threat: the experience of Iranian female caregivers with a first-degree relative with breast cancer. Psycho-Oncology, 2017. 26(5): p. 625–631. [DOI] [PubMed] [Google Scholar]
- 51.Unic I, et al. , A review on family history of breast cancer: screening and counseling proposals for women with familial (non-hereditary) breast cancer. Patient Educ Couns, 1997. 32(1–2): p. 117–27. [DOI] [PubMed] [Google Scholar]
- 52.Lerman C. and Schwartz M, Adherence and psychological adjustment among women at high risk for breast cancer. Breast Cancer Res Treat, 1993. 28(2): p. 145–55. [DOI] [PubMed] [Google Scholar]
- 53.Kash KM, et al. , Psychological distress and surveillance behaviors of women with a family history of breast cancer. J Natl Cancer Inst, 1992. 84(1): p. 24–30. [DOI] [PubMed] [Google Scholar]
- 54.Audrain-McGovern J, Hughes C, and Patterson F, Effecting behavior change: awareness of family history. Am J Prev Med, 2003. 24(2): p. 183–9. [DOI] [PubMed] [Google Scholar]
- 55.Riddle DL, et al. , Pain coping skills training for patients with elevated pain catastrophizing who are scheduled for knee arthroplasty: a quasi-experimental study. Arch Phys Med Rehabil, 2011. 92(6): p. 859–65. PCMID: PMC3104058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Syrjala KL, et al. , Psychological and Behavioral Approaches to Cancer Pain Management. Journal of Clinical Oncology, 2014. 32(16): p. 1703–1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Quartana PJ, Campbell CM, and Edwards RR, Pain catastrophizing: a critical review. Expert Rev Neurother, 2009. 9(5): p. 745–58. PCMID: PMC2696024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Keefe FJ, Dunsmore J, and Burnett R, Behavioral and cognitive-behavioral approaches to chronic pain: recent advances and future directions. J Consult Clin Psychol, 1992. 60(4): p. 528–36. [DOI] [PubMed] [Google Scholar]
- 59.Bennell KL, et al. , Effectiveness of an Internet-Delivered Exercise and Pain-Coping Skills Training Intervention for Persons With Chronic Knee Pain: A Randomized Trial. Ann Intern Med, 2017. 166(7): p. 453–462. [DOI] [PubMed] [Google Scholar]
- 60.Somers TJ, et al. , Pain coping skills training and lifestyle behavioral weight management in patients with knee osteoarthritis: a randomized controlled study. Pain, 2012. 153(6): p. 1199–209. PCMID: PMC3358356. [DOI] [PMC free article] [PubMed] [Google Scholar]