Supplemental digital content is available in the text.
Key Words: COGNITIVE DECLINE, MULTILEVEL ANALYSIS, SOCIAL CAPITAL, EXERCISE EPIDEMIOLOGY, THE JAPAN GERONTOLOGICAL EVALUATION STUDY COHORT
ABSTRACT
Purpose
Community-level group participation is a structural aspect of social capital that may have a contextual influence on individual health. We investigated the contextual effect of community-level prevalence of sports group participation on the risk of cognitive impairment among older individuals.
Methods
We analyzed prospective cohort data from the Japan Gerontological Evaluation Study, a nationwide survey of 40,308 functionally independent older individuals from 346 communities. Cognitive impairment was assessed by the nationally standardized dementia scale proposed by the Ministry of Health, Labour and Welfare of Japan. Participation in a sports group 1 d per month or more frequently was defined as “participation.” We applied a two-level multilevel survival analysis to calculate hazard ratios (HR) and 95% confidence intervals (CI).
Results
The cumulative incidence of cognitive impairment during the 6-yr follow-up period was 9.8%. The mean proportion of sports group participation was 25.2% (range, 0.0%–56.5%). Higher prevalence of community-level sports group participation was associated with a lower risk of cognitive impairment (HR, 0.92; 95% CI, 0.86–0.99, estimated by 10 percentage points of participation proportion) after adjusting for individual-level sports group participation, sex, age, disease, obesity, social isolation, alcohol, smoking, education, income, depression, daily walking time, population density, and sunlight hours. We found cross-level interaction between individual- and community-level sports group participation (HR, 0.87; 95% CI, 0.76–0.99).
Conclusions
We found a contextual preventive effect of community-level sports group participation on developing cognitive impairment among older individuals. Furthermore, the benefit may favor sports group participants. Therefore, promoting sports groups in a community setting may be effective as a population-based strategy for the prevention of dementia.
Dementia, one of the most important health problems among older populations, threatens an individual’s independence, imposes burden upon caregivers, and increases social care costs (1). The number of individuals with dementia across the world is expected to increase to 66 million by 2030 and to 131 million by 2050 (2).
There is growing interest in modifiable risk factors for the prevention of dementia, as there are no established treatments to date (3). A recent systematic review identified the following modifiable risk factors for dementia: physical inactivity, lower level of education, midlife hypertension, obesity, hearing loss, social isolation, depression, smoking, and diabetes (3). A meta-analysis of 15 prospective cohort studies reported that physical activity had a significant protective effect against cognitive decline, with high levels of exercise being the most protective (4). In particular, participating in a sports group has positive effects of social contact and physical activity upon mental health, leading to enjoyment, enhanced self-esteem, and decreased stress (5–7). Sports group participation may also lower the risk of functional disability as compared with participation in other kinds of social activities such as those associated with the local community, volunteer work, industrial pursuits, and political involvement (8). As the synergistic effects of a lifestyle that is socially, mentally, and physically active may prevent cognitive decline (9), participating in a sports group may be effective to prevent the developing cognitive impairment and the onset of incident dementia. A previous 7-yr follow-up study reported that older individuals who congregated and participated in social activities with mild physical activity had a lower risk of cognitive impairment (10).
Social participation is defined as a “person’s involvement in activities that provide interaction with others in society or the community” and is also an index of social capital (11). Social capital is the “features of social organization, such as trust, norms, and networks, that can improve the efficacy of society by facilitating coordinated actions (12).” It is also described as “resources that are accessed by individuals as a result of their membership of a network or a group” (13) and is an emerging concept in increasingly applied in public health research (14). Social capital can be divided into two levels: 1) Individual level, which refers to resources accessed by the individual through ego-centered networks; and 2) group level, which pertains to the characteristics of the social network (14). Group-, or community-level, sports group participation has been shown to prevent depression, one of the known modifiable risk factors for dementia (15). Thus, older individuals living in communities with higher prevalence of sports group participation were less likely to have depressive symptoms compared with communities with lower prevalence of sports group participation, after adjustment for individual-level participation and other potentially confounding factors (15). However, there is little evidence to support an association between community-level sports group participation and cognitive impairment.
The present study investigated whether older individuals living in communities with higher prevalence of sports group participation have less risk of cognitive impairment compared with those living in communities with lower prevalence of sports group participation, after controlling for individual-level sports group participation. We performed community- and individual-level multilevel analyses to examine the contextual effect of community-level sports group participation on developing cognitive impairment in older individuals.
METHODS
Study Design
Longitudinal cohort data from the Japan Gerontological Evaluation Study (JAGES), an ongoing cohort study with more than 100,000 participants as of 2016 focused on investigating social and behavioral factors related to loss of independence with respect to functional decline, or cognitive impairment, among individuals 65 yr or older (16). Figure 1 outlines the selection process of study participants and those retained for a 6-yr follow-up. The baseline survey was conducted between August 2010 and January 2012 via self-reported questionnaires distributed by mail to 95,827 people 65 yr or older selected from 16 municipalities in seven prefectures within Japan. Enrollment criteria for the baseline survey included physically and cognitively independent individuals who did not receive a needed support and needed long-term care certification under the Japanese long-term care insurance system (17). Next, a random sample was obtained from official residence registers in seven municipalities and from a complete census of older residents residing in the nine smaller municipalities. Among the 62,426 respondents (response rate, 65.1%), ID number, sex, and age were validly collected from 56,687 respondents (valid response rate, 59.2%). To control for the community-level sports group participation variable, we excluded 13,150 respondents whose information regarding extent of sports group participation was unknown, whose area of residence was unknown, or who lived in communities with 30 respondents or less. Excluding these respondents resulted in 43,357 respondents living in 346 areas defined primarily by school district. Further analysis of the original 56,687 valid respondents, yielded 54,539 (96.2%) participants successfully linked to records of developing cognitive impairment during a 6-yr follow-up period. Finally, the analytical sample for the present multilevel survival analyses was comprised of 40,308 participants (19,624 men and 20,684 women). This sample size was derived after excluding survey respondents without information on the community-level variable (the extent of sports group participation), and those respondents inadvertently included later found to have reported limitations in activities of daily living (unable to walk, take a bath, or toilet without assistance) to ensure that the sample was indeed both physically and cognitively independent. The JAGES participants were informed that participation in the study was voluntary and that completing and returning the questionnaire via mail indicated their consent to participate in the study. The Human Subjects Committees of Nihon Fukushi University (no. 10-5) and Chiba University Faculty of Medicine (no. 2493) approved the parent JAGES protocol.
FIGURE 1.
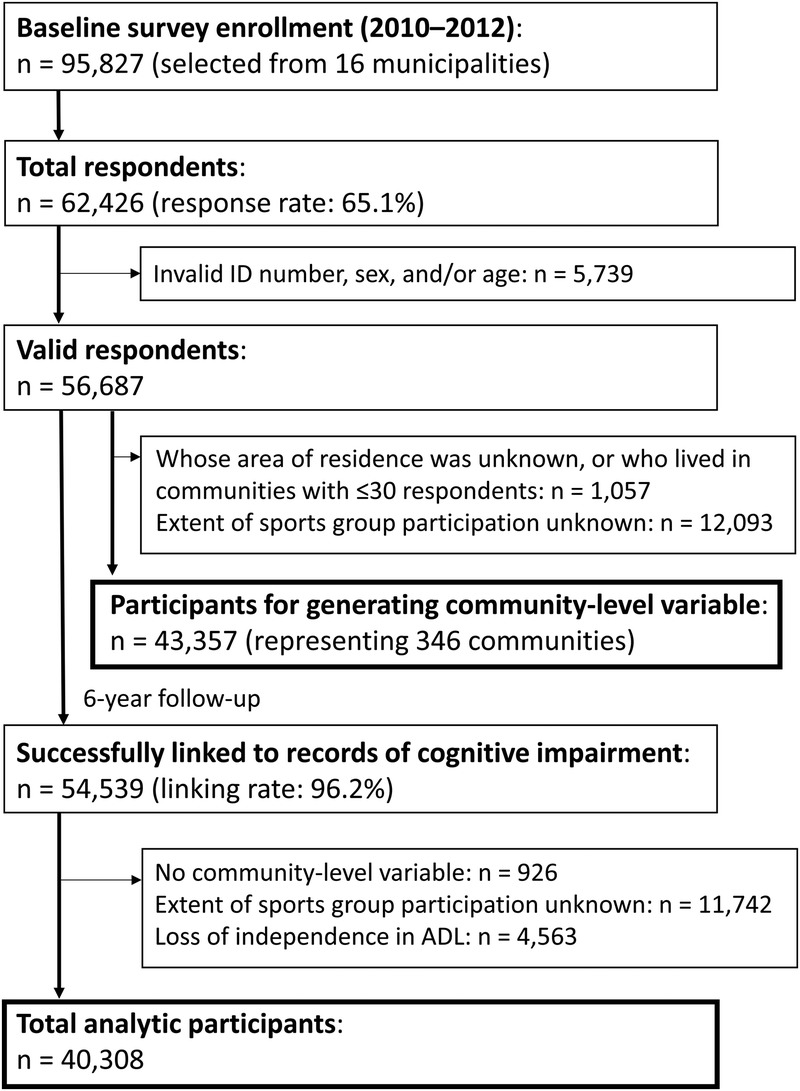
Flow of participants in the cohort study.
Measurements
Dependent variable
The Activities of Daily Living Independence Assessment Criteria for Elderly Individuals with Dementia developed by the Ministry of Health, Labour and Welfare of Japan stratifies cognitive decline by utilizing Ranks I, II, III, IV, and M (18,19). Rank I corresponds to a state in which some level of cognitive impairment exists, yet the individual remains able to carry out activities of daily living in both domestic and social spheres independently. Rank II describes symptoms/behaviors and/or communication difficulties that may hinder some daily activities, but independence is maintained with minimal assistance. Rank III patients display occasional communication difficulties and/or symptoms/behaviors hindering daily activities, requiring daily care from a caregiver while maintaining some level of independent living. Rank IV represents difficulties communicating and/or symptoms/behaviors that hinder daily activities and require constant care from a caregiver. Rank M means that the patient displays significant mental health symptoms, problematic behaviors, or severe physical illnesses requiring specialized and constant medical care. This dementia scale was validated by demonstrating its correlation with the Mini Mental State Examination (r = −0.74) (20) and its accordance with the Clinical Dementia Rating (21). We defined Ranks II, III, IV and M as consistent with the developing cognitive impairment for the purposes of this study, as these individuals require either assistance or fulltime care to for activities of daily living (22–24).
Community- and individual-level independent variables
Participants were queried on frequency of sports group participation. Answer choices included: ≥4 d·wk−1, 2 to 3 d·wk−1, 1 d·wk−1, 1 to 3 d per month, a few times per year, or zero. We defined participating 1 d per month or more as “participation in a sports group” (15,25) and aggregated individual-level sports group participation by community as the community-level independent variable. Previous research indicated a strong correlation between the proportion of older individuals with poor self-rated health and/or depressive symptoms living in areas with community-level sports group participation once monthly or more (r = −0.233 and −0.355, respectively) compared with community-level sports group participation once weekly or more (r = −0.210 and −0.314, respectively) (25).
Covariates
Sex and age were collected as basic demographic characteristics. Age groups were categorized as 65 to 69 yr, 70 to 74 yr, 75 to 79 yr, 80 to 84 yr, and ≥85 yr. As community-level covariates, we calculated population density per square kilometer of inhabitable area (≥10,100, 7900–10,099, 3280–7899, or <3280 persons per square kilometer) and annual sunlight hours (≥2090, 2060–2089, 2040–2059, or <2040 h·yr−1) for each community on the basis of data derived from national statistics divided into quartile categories. As individual-level covariates, disease status was collected for those diseases known to increase the risk of dementia (stroke, hypertension, diabetes, and/or hearing loss) (3), with yes/no answer choices. Obesity is also a reported factor for increasing dementia risk (3); thus, body mass index (BMI) was calculated as self-reported weight (kg) divided by height squared (m2), with a BMI ≥30.0 kg·m−2 classified as obese. Social isolation has been defined as social contact with others less than once monthly (3). In the present study, participants were asked about household members living with them and the frequency of meeting with friends/acquaintances. We categorized participants living alone with meetings less than monthly as socially isolated. Drinking status (none, past, or current), smoking status (none, past, or current), and amount of education (≥6 or <6 yr) were categorized by each answer choice. Annual equivalent income was calculated by dividing household income by the square root of the number of household members and categorized into three groups: ≥4,000,000, 2,000,000–3,999,999, or <2,000,000 yen per year. As potential mediators between community-level sports group participation and cognitive impairment, we assessed individual-level depressive symptoms using the 15-item Geriatric Depression Scale (GDS) (26,27) and quantified the amount of daily walking time (<30, 30–59, 60–89, or ≥90 min·d−1). Mild-to-severe depressive symptoms (GDS ≥5) were categorized as “depression,” in accordance with prior research (28,29). The individual-level covariates for which data was not collected due to the lack of participant response were assigned to a “missing” category for that particular question; thus avoiding the exclusion of a participant for failing to answer one or more questions corresponding to individual-level covariates.
Statistical Analyses
The multilevel analysis framework assumes that an individual health outcome is partly dependent upon the community in which an individual lives. Multilevel models estimate the variation in outcome between community areas (random effects) and the effects of community-level variables while adjusting for individual- and community-level characteristics (fixed effects). We used multilevel survival analysis to calculate the hazard ratio (HR) and the 95% confidence interval (CI) for the developing cognitive impairment during the follow-up period. The HR of community-level sports group participation was estimated as a 10 percentage point change in aggregated sports group participation. Five multivariate models of analysis were used. Community- and individual-level sports group participation and cross-level interaction terms were included in the crude model. The next four models included the following: 1) Crude model + age and sex; 2) Model 1 + community-level covariates; 3) Model 2 + all individual-level covariates except depression and daily walking time; and, 4) Model 3 + depression and daily walking time, assuming potential mediators. To attenuate the possibility of reverse causality, we performed sensitivity analyses excluding participants whose follow-up periods were less than 1, 2, and 3 yr. Analyses were performed using STATA/MP 14.2 (Stata Corp., College Station, TX).
RESULTS
The 40,308 participants in this study contributed 213,906 person-years with a maximum follow-up duration of 2328 d and a mean follow-up duration of 1937 d. The total sample included 3940 (9.8%) individuals who comprised new development of cognitive impairment. The incidence per 1000 person-years was found to be 18.4 people. Table 1 outlines the descriptive data and cumulative incidence of cognitive impairment. The proportion of sports group participation was calculated for each community and the mean (SD) and the range were 25.2% (8.4%) and 0.0% to 56.5%, respectively. Supplemental Table 1 (see Table, Supplemental Digital Content 1, Comparison of individual-level variables between sports group participants and nonparticipant, http://links.lww.com/MSS/B638) shows the demographic characteristics of sports group participants and nonparticipants. The latter were older and in poorer physical, psychological, and social conditions than sports group participants.
TABLE 1.
Descriptive statistics of individual- and community-level variables and cumulative incidence of cognitive impairment.
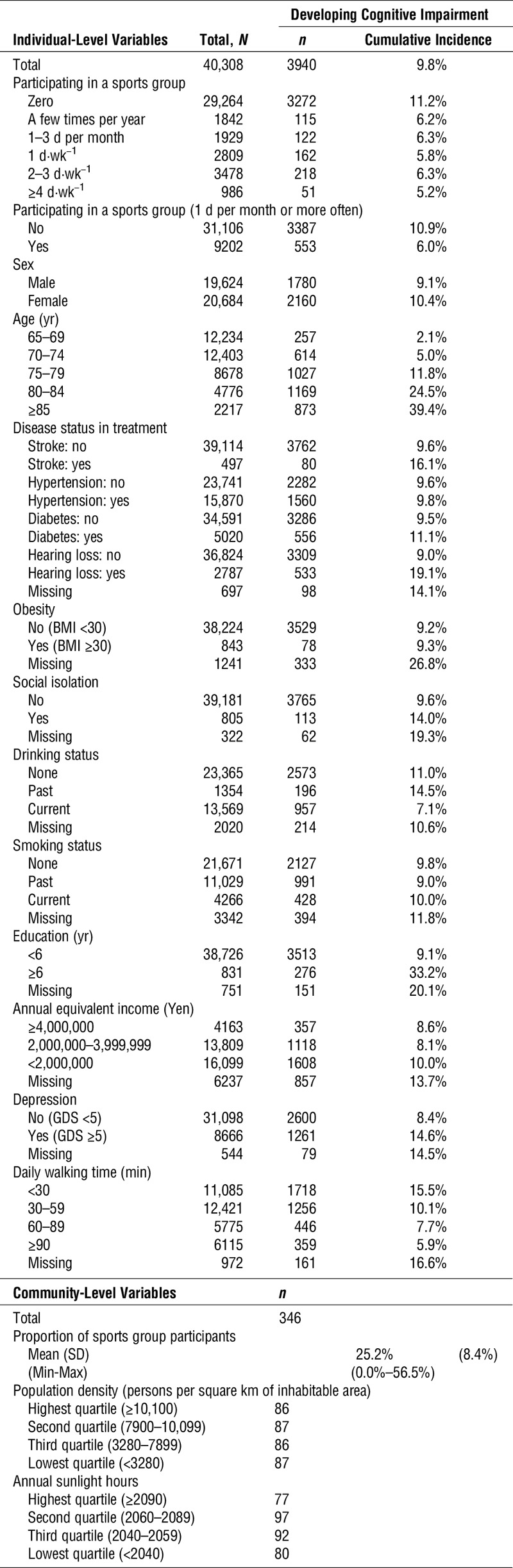
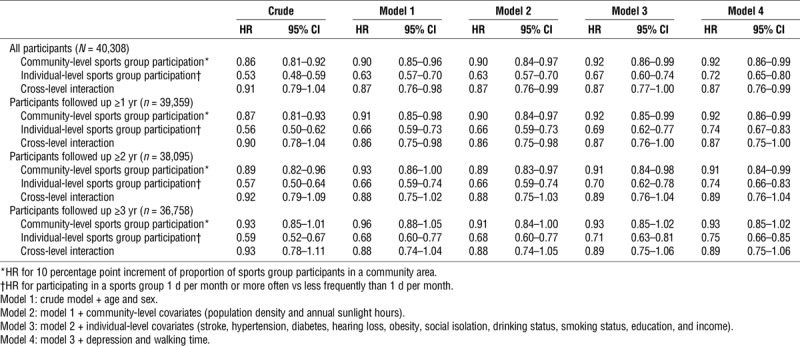
Table 2 and Supplemental Table 2 (see Table, Supplemental Digital Content 2, All point estimates of HR and 95% CI estimated from multilevel survival analyses for incident dementia, http://links.lww.com/MSS/B639) show the results of the multilevel survival analyses. According to the analysis for all participants, regardless of models including covariates, community-level higher prevalence of sports group participation demonstrated a statistically significant relationship with lower risk of cognitive impairment (HR, 0.92; 95% CI, 0.86–0.99 in the fully adjusted model), estimated by 10 percentage points of participation proportion. Individual-level sports group participation also showed a significant relationship with low likelihood of developing cognitive impairment (HR, 0.72; 95% CI, 0.65–0.80 in the fully adjusted model). We found statistically significant cross-level interaction terms (HR, 0.87; 95% CI, 0.76–0.99 in the fully adjusted model). According to sensitivity analyses, the point estimates of HR showed minimal change and similar results when excluding participants whose follow-up period was less than 1, 2, and 3 yr.
TABLE 2.
Results of multilevel survival analyses for developing cognitive impairment and its sensitivity analyses (participants nested in 346 community areas).
DISCUSSION
As far as we are aware, this is the first study to find the contextual effects of community-level prevalence of sports group participation and developing cognitive impairment among older individuals. A 10 percentage point increase in community-level sports group participation was associated with an 8% reduction in the risk of cognitive impairment after adjusting for individual-level sports group participation and covariates. The results of this study suggest that promoting sports groups in a community may be effective for the prevention of dementia for both sports group participants and nonparticipants.
It is important to note that the lack of a significant association between community-level social participation and cognitive function was reported previously (30). In that cross-sectional study, multilevel analysis was used to determine the relationship between community-level social participation (the mean number of social participation items among older individuals tabulated at the elementary school ward units) and cognitive function (30). However, the following limitations were reported in power: limited samples at both the individual- and community-levels (n = 180, selected from 11 areas within a single Japanese prefecture) with only small differences found in community-level social participation among public school areas (30). Thus, we aimed to overcome such deficits to find a statistically significant relationship between community-level sports group participation and cognitive impairment. Our study design utilized 6-yr follow-up data from a large-scale sample of older individuals residing in 346 areas nationwide, representing a large variance in community-level sports group participation. The results of the present study were in accordance with the findings of another previous cross-sectional study that reported a contextual preventive relationship between community-level sports group participation and depressive symptoms in older individuals (15). Because depression and physical activity in older age are modifiable risk factors for dementia (3), we hypothesized that depressive symptoms and walking time were also potential mediators between community-level sports group participation and cognitive impairment. However, little change was noted in the effect of community-level sports group participation by adding depression and daily walking time into the statistical model, which suggested the presence of other pathways reducing dementia risk.
Another possible intermediate factor is the enhancement of social support. A systematic review and meta-analysis of longitudinal cohort studies found that although infrequent social contact and loneliness were associated significantly with incident dementia, social support may provide a buffer against stress and thereby protect against dementia (9). Including social support exchange with friends or acquaintances in the community into our statistical models, however, showed that social support did not have a consistent association with cognitive impairment; effect on the relationship between community-level sports group participation and cognitive impairment was negligible (data not shown).
We hypothesized three pathways (social contagion, informal social control, and collective efficacy) to explain the contextual effect of group-level social capital upon individual-level health outcomes (13). Social contagion refers to the notion that behaviors spread more quickly throughout a close social network (13). Behavioral modifications that spread via the social network may ultimately promote healthy lifestyle changes, such as smoking cessation (31). Informal social control is the ability of individuals in a community to maintain social order; for instance, one might step in and intervene when witnessing deviant behaviors in an effort to mediate undesirable outcomes (13). The social contagion and informal social controls relevant to this study extend to older individuals who may be encouraged by sports group participants to acquire more physical activity through either individual- or group-based sporting activities. Finally, collective efficacy is the group-level analogue of the concept of self-efficacy and refers to the ability of the collective group to mobilize in an effort to undertake collective action (13,32). Facilities, industries, systems, and/or bylaws for health promotion may develop to reflect the opinions and actions of communities with many sports groups and sports group participants. Group-level mechanisms of widespread sports group participation may result in positive spillover effects for the community at large (15).
A statistically significant cross-level interaction was observed in the present study, suggesting that sports group participants living in communities with higher prevalence of sports group participation may be less likely to develop cognitive impairment compared with those living in community areas with a lower prevalence of sports group participation. One of the possible benefits of group participation is the opportunity for acquiring a leadership role within the group. According to a previous 10-yr follow-up study (23), older individuals, 65 to 74 yr, who participated in any organization (e.g., sports group, hobby group, or religious group) and held a leadership position within the organization had a 20% lower risk of cognitive impairment compared with members not participating in a leadership role. It is assumed that communities with many sports group participants naturally also have many sports groups within the community. Accordingly, each group requires individuals in leadership positions to be responsible for management of the group. Therefore, older participants living in areas with many active sports groups might also have many opportunities to participate in key leadership roles.
One of the greatest strengths of this study is its large-scale sample of older individuals spread nationwide through 16 different municipalities. Another strength is the availability of extensive longitudinal data, with a high follow-up rate for the 6-yr period. This study also includes several limitations. First, cognitive impairment was assessed using the nationally standardized dementia scale, rather than by a clinical diagnosis of dementia. This limitation may introduce some degree of misclassification of dementia for study participants. Therefore, it cannot be ruled out that older individuals who were diagnosed with dementia at baseline may have been included in the present study. Yet, scale criteria were validated in accordance with the Mini Mental State Examination (20) and with the Clinical Dementia Rating (21), yielding credibility to this research tool. Second, selection bias may have affected results due to the relatively low valid response rate (59.2%). According to our previous study, both the response rate and the percentage of sports group participation were significantly lower for older versus younger individuals (33). Consequently, participants in this study might have a relatively low risk of dementia, as those with significant dementia may have failed to respond to the survey altogether; as such, the relationship between sports group participation and cognitive impairment may have been underestimated according to unmeasurable characteristics between respondents and those who failed to respond to the survey. Third, although the participants’ daily walking time was determined, their levels of physical activity/inactivity were not evaluated using a valid index. In addition, the frequency, intensity, and type of sports and exercises that older individuals engaged in were not assessed. Emerging evidence shows that physical inactivity accounts for about 3.8% of cases of dementia worldwide (34). Therefore, studies are needed to determine how frequency, intensity, and type of sports activity at the community-level affect cognitive impairment. Nevertheless, we believe that utilization of the criteria “at least 1 d per month” to define sports group participation is both a feasible and acceptable frequency of measurement.
CONCLUSIONS
Older individuals living in communities with higher prevalence of sports group participation among their age demographic are less likely to develop cognitive impairment compared with those living in areas with lower prevalence of sports group participation, after adjustment for individual-level sports group participation and other covariates. The results of this study suggest a contextual preventive relationship between community-level sports group participation and developing cognitive impairment in the older individuals, a benefit that may favor sports group participants.
Supplementary Material
Acknowledgments
The authors would like to thank the study participants and the JAGES team for data collection. This study was supported by a grant of the Strategic Research Foundation Grant-aided Project for Private Universities from the Ministry of Education, Culture, Sport, Science, and Technology, Japan (MEXT), 2009–2013, for the Center for Well-being and Society, Nihon Fukushi University; a Health Labour Sciences Research Grant, Comprehensive Research on Aging and Health [grants H22-Choju-Shitei-008, H24-Junkankitou-Ippan-007, H24-Chikyukibo-Ippan-009, H24-Choju-Wakate-009, H25-Kenki-Wakate-015, H25-Irryo-Shitei-003 (Fukkou), H26-Choju-Ippan-006, H28-Chouju-Ippan-02] from the Japanese Ministry of Health, Labour and Welfare; JSPS KAKENHI [grants 22330172, 22390400, 23243070, 23590786, 23790710, 24390469, 24530698, 24653150, 24683018, 25253052, 25870573, 25870881, 22390400, 15K18174, 15KT0007, 15H01972, 16K16595, 17K15822] from the Japan Society for the Promotion of Science; a grant from the National Center for Geriatrics and Gerontology [grants 24-17, 24-23]; the Research and Development Grants for Longevity Science from AMED; a grant from the Japan Foundation for Aging and Health; and also World Health Organization Centre for Health Development (WHO Kobe Centre) [grant WHO APW 2017/713981]. The funding sources had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors declare that the results of the present study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation, and do not constitute endorsement by ACSM.
Conflict of Interest: None of the authors have a conflict of interest in relation to this manuscript.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.acsm-msse.org).
REFERENCES
- 1.Prince MJ, Wu F, Guo Y, et al. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385(9967):549–62. [DOI] [PubMed] [Google Scholar]
- 2.Alzheimer’s Disease International. World Alzheimer Report 2015: The Global Impact of Dementia. London, UK; 2015. [Google Scholar]
- 3.Livingston G, Sommerlad A, Orgeta V, et al. Dementia prevention, intervention, and care. Lancet. 2017;390(10113):2673–734. [DOI] [PubMed] [Google Scholar]
- 4.Sofi F, Valecchi D, Bacci D, et al. Physical activity and risk of cognitive decline: a meta-analysis of prospective studies. J Intern Med. 2011;269(1):107–17. [DOI] [PubMed] [Google Scholar]
- 5.Eime RM, Young JA, Harvey JT, Charity MJ, Payne WR. A systematic review of the psychological and social benefits of participation in sport for adults: informing development of a conceptual model of health through sport. Int J Behav Nutr Phys Act. 2013;10:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanamori S, Takamiya T, Inoue S. Group exercise for adults and elderly: determinants of participation in group exercise and its associations with health outcome. J Phys Fitness Sports Med. 2015;4(4):315–20. [Google Scholar]
- 7.Tsuji T, Sasaki Y, Matsuyama Y, et al. Reducing depressive symptoms after the Great East Japan Earthquake in older survivors through group exercise participation and regular walking: a prospective observational study. BMJ Open. 2017;7(3):e013706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kanamori S, Kai Y, Aida J, et al. Social participation and the prevention of functional disability in older Japanese: the JAGES cohort study. PLoS One. 2014;9(6):e99638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuiper JS, Zuidersma M, Oude Voshaar RC, et al. Social relationships and risk of dementia: a systematic review and meta-analysis of longitudinal cohort studies. Ageing Res Rev. 2015;22:39–57. [DOI] [PubMed] [Google Scholar]
- 10.Hikichi H, Kondo K, Takeda T, Kawachi I. Social interaction and cognitive decline: results of a 7-year community intervention. Alzheimers Dement (N Y). 2016;3(1):23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levasseur M, Richard L, Gauvin L, Raymond E. Inventory and analysis of definitions of social participation found in the aging literature: proposed taxonomy of social activities. Soc Sci Med. 2010;71(12):2141–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Putnam RD. Making Democracy Work: Civic Traditions in Modern Italy. Princeton, NJ: Princeton University Press; 1993. 167 p. [Google Scholar]
- 13.Kawachi I, Berkman LF. Social Capital, Social Cohesion, and Health. In: Berkman LF, Kawachi I, Glymour MM, editors. Social Epidemiology Second Edition New York, NY: Oxford University Press; 2014. pp. 290–319. [Google Scholar]
- 14.Murayama H, Fujiwara Y, Kawachi I. Social capital and health: a review of prospective multilevel studies. J Epidemiol. 2012;22(3):179–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsuji T, Miyaguni Y, Kanamori S, Hanazato M, Kondo K. Community-level sports group participation and older individuals’ depressive symptoms. Med Sci Sports Exerc. 2018;50(6):1199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kondo K. Progress in aging epidemiology in Japan: the JAGES project. J Epidemiol. 2016;26(7):331–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsutsui T, Muramatsu N. Care-needs certification in the long-term care insurance system of Japan. J Am Geriatr Soc. 2005;53(3):522–7. [DOI] [PubMed] [Google Scholar]
- 18.Ministry of Health, Labour and Welfare. The Degree of Autonomy in the Daily Lives of Elderly Individuals with Dementia Scale [Internet]. 2010. [cited 2018 Oct 3] Available from: http://www.mhlw.go.jp/topics/2013/02/dl/tp0215-11-11d.pdf. [in Japanese].
- 19.Hikichi H, Aida J, Kondo K, et al. Increased risk of dementia in the aftermath of the 2011 Great East Japan Earthquake and Tsunami. Proc Natl Acad Sci U S A. 2016;113(45):E6911–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hisano S. The relationship between Revised Hasegawa Dementia Scale (HDS-R), Mini-Mental State Examination (MMSE) and Bed-fast Scale, dementia scale. Jpn J Geriatr Psychiatry. 2009;20(8):883–91. [Google Scholar]
- 21.Meguro K, Tanaka N, Kasai M, et al. Prevalence of dementia and dementing diseases in the old-old population in Japan: the Kurihara Project. Implications for Long-Term Care Insurance data. Psychogeriatrics. 2012;12(4):226–34. [DOI] [PubMed] [Google Scholar]
- 22.Saito T, Murata C, Saito M, Takeda T, Kondo K. Influence of social relationship domains and their combinations on incident dementia: a prospective cohort study. J Epidemiol Community Health. 2018;72(1):7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nemoto Y, Saito T, Kanamori S, et al. An additive effect of leading role in the organization between social participation and dementia onset among Japanese older adults: the AGES cohort study. BMC Geriatr. 2017;17(1):297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tomata Y, Sugiyama K, Kaiho Y, et al. Green tea consumption and the risk of incident dementia in elderly Japanese: the Ohsaki Cohort 2006 Study. Am J Geriatr Psychiatry. 2016;24(10):881–9. [DOI] [PubMed] [Google Scholar]
- 25.Saito M, Kondo N, Aida J, et al. Development of an instrument for community-level health related social capital among Japanese older people: the JAGES Project. J Epidemiol. 2017;27(5):221–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. 5(1–2):165–73. [Google Scholar]
- 27.Wada T, Ishine M, Kita T, Fujisawa M, Matsubayashi K. Depression screening of elderly community-dwelling Japanese. J Am Geriatr Soc. 2003;51(9):1328–9. [DOI] [PubMed] [Google Scholar]
- 28.Schreiner AS, Hayakawa H, Morimoto T, Kakuma T. Screening for late life depression: cut-off scores for the Geriatric Depression Scale and the Cornell Scale for Depression in Dementia among Japanese subjects. Int J Geriatr Psychiatry. 2003;18(6):498–505. [DOI] [PubMed] [Google Scholar]
- 29.Nyunt MS, Fones C, Niti M, Ng TP. Criterion-based validity and reliability of the Geriatric Depression Screening Scale (GDS-15) in a large validation sample of community-living Asian older adults. Aging Ment Health. 2009;13(3):376–82. [DOI] [PubMed] [Google Scholar]
- 30.Sakamoto A, Ukawa S, Okada E, et al. The association between social participation and cognitive function in community-dwelling older populations: Japan Gerontological Evaluation Study at Taisetsu community Hokkaido. Int J Geriatr Psychiatry. 2017;32(10):1131–40. [DOI] [PubMed] [Google Scholar]
- 31.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358(21):2249–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–24. [DOI] [PubMed] [Google Scholar]
- 33.Kondo K. Exploring “Inequalities in Health”: A Large-Scale Social Epidemiological Survey for Care Prevention in Japan. Igaku-Shoin Ltd.: Tokyo, Japan; 2007. P.87, 124. [In Japanese]. [Google Scholar]
- 34.Sallis JF, Bull F, Guthold R, et al. Progress in physical activity over the Olympic quadrennium. Lancet. 2016;388(10051):1325–36. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


