Abstract
Young adulthood is a major transition period, particularly challenging for those with mental disorders. Though the prevalence of depressive and anxiety disorders is especially high, young adults are less likely to receive mental health treatment than younger and older individuals. Reasons for this mental health treatment gap are multifold and range from individual- to system-level factors that must be taken into consideration when addressing young adult mental health needs. Studies in adults and adolescents have shown that integrated care in primary care settings is an effective model of treatment of mental disorders. After providing an overview of the mental health treatment gap in this developmental period, the argument is made for research focused on integrated care models specifically tailored for young adults that takes into consideration the various needs and challenges that they face and addresses the mental health treatment gap in young adulthood.
Keywords: young adults, mental health care utilization, depression, anxiety, integrated care, collaborative care, health care transition
Introduction
Young adulthood is defined as a developmental period between ages 18 and 25 marked by significant changes and transitions. During this period, young adults continue to explore and form their identity, manage changing interpersonal relationships, increase economical and emotional independence from parents and/or guardians, and navigate complex educational, employment, and healthcare systems.1 Some young adults also have to deal with impairing conditions highly prevalent in the adult years that commonly emerge during young adulthood, such as depressive and certain anxiety disorders.2,3 Despite the frequent occurrence of mood and anxiety disorders, and related comorbidities, young adults are less likely to seek mental health care compared to those in other age groups. The increasing rates of mental disorders combined with low rates of mental health service utilization creates a substantial mental health treatment gap, which makes young adults a particularly vulnerable population with unmet mental health needs. The presence of these disorders can hamper the acquisition of important milestones associated with adulthood, which underscores the importance of receiving appropriate mental health treatment in a timely manner.2,4,5
In its 2015 report entitled “Investing in the Health and Well-Being of Young Adults”, the Institute of Medicine acknowledged that adult studies often lack a specific focus on the 18–25 year old population.6 Currently, data on the prevalence of both mental disorders and mental health care utilization among young adults are scarce. Adult studies usually include young adults, but data specific to this age group is typically subsumed under a general “adult” umbrella that encompasses a wide spectrum of ages ranging from young adults to the elderly. Meanwhile, most child and adolescent studies do not include patients beyond the age of 18. The data that do exist point towards the existence of a mental health treatment gap in young adulthood.
The overall goal of this paper is to lay out the contributors to the mental health treatment gap observed in young adults with mood and anxiety disorders, conditions that are of particular relevance during this critical developmental period, with recommendations of strategies to address this gap. This paper begins with a summary of the existing literature on the prevalence of mood and anxiety disorders, as well as mental health service utilization among young adults, followed by a description of relevant barriers to care that may contribute to the low prevalence of mental health service use among young adults. Finally, an argument is made that integrated care models tailored for this age group could be a potential way to address the many treatment barriers and mental health needs of this vulnerable population.
Depression and Anxiety Disorders among Young Adults: Prevalence and Service Utilization Prevalence of depressive and anxiety disorders
Very few studies with representative samples of adults provide specific information on the prevalence of depression and anxiety disorders in young adults. The most recent US national prevalence rates of past-year depressive disorders in adults have been provided in the 2016 National Survey on Drug Use and Health (NSDUH). In this survey, approximately 10.9% of young adults (18–25) experienced a major depressive episode in the past year, which was greater than adults ages 26–49 (7.4%) and greater than 50 years old (4.8%).7 The most recent information about the 12-month prevalence of any anxiety disorders among young adults comes from the National Comorbidity Survey Replication (2007), which reports a prevalence of 22.3% among those ages 18–29. Prevalence was 22.7% in adults ages 30–44, 20.6% for adults ages 45–59 and 9% for adults 60 and older.8 No updated information has been published since then.
Depressive disorders follow a fairly linear course. The prevalence of depressive disorders is low in childhood and starts increasing around the age of 13, earlier and faster in girls than in boys.9–11 By the age of 17–18, the prevalence of depressive disorders and symptoms levels off and remains relatively stable throughout most of adulthood.3,12 The prevalence of anxiety disorders follows a U-shaped age distribution, with an increase in anxiety disorders during childhood and again during the transition from adolescence to early adulthood, such that by the age of 26 almost 23% of young adults meet criteria for an anxiety disorder, with the most common disorders being generalized anxiety disorder, panic disorder, and agoraphobia.2
Mental health service utilization
Like research on mental disorders, information about mental health service use in the young adult population is often presented within data from older adults, who usually report higher rates of service utilization. The few studies that provide data by age subgroups show that the rate of mental health service utilization is lower among young adults than adolescents and older adults, despite a higher prevalence of psychopathology during young adulthood.13–16 There is also prospective evidence that the percentage of treatment discontinuation during the time of transition to adult services is rather high.13 Specifically, a longitudinal population-based study indicated a significant decline in any service use for psychiatric disorders from 50.9% to 28.9% as adolescents (13–16 years old) transitioned to young adulthood. This occurred despite an observed increase in the prevalence of psychiatric disorders from 8.9% in adolescence to 15.9% in young adulthood.17
Only a handful of epidemiological studies in the US provide specific information on service use for mood and anxiety disorders among young adults.16,18,19 The largest of these studies, The National Epidemiologic Survey of Alcohol and Related Conditions (NESARC), compared professional help seeking across the adult lifespan in a representative sample of adults with mood and anxiety disorders. The survey found lower prevalence of help seeking among young adults ages 20–24 years when compared to older adults from ages 25 to 64. The prevalence of help seeking for young adults was 16% for any anxiety disorder and 28% for any mood disorder; whereas for older age groups the prevalence of help seeking ranged from 19.5% to 22.4% for anxiety disorders and 34% to 42.5% for mood disorders.19 Similarly, data from the Medical Expenditure Panel Survey (MEPS) showed that people ages 18–34 were less likely to receive any treatment for depression when compared to older adults.20
A better understanding of the specific barriers to seeking treatment and of the challenges faced currently when providing treatment for youth and adults in primary care settings is required to strategize about how to best improve access to mental health services among young adults. This information can then help facilitate the development of feasible solutions to these barriers and challenges.
Barriers and Challenges to Mental Health Treatment in Young Adulthood
Historically, young adults have faced a significant challenge with respect to insurance coverage. In 2010, the Affordable Care Act (ACA) expanded insurance coverage for young adults. Specifically, the ACA included provisions that allow for young adults to remain on a parent’s private insurance until age 26, encouraged states to expand Medicaid, and allowed for those aging out of foster care to keep their Medicaid coverage until age 2621–23 These measures led to significant increases in the number of insured young adults. With a little over 64% of young adults insured in the third quarter of 2010, the percentage of insured young adults rose to about 75% just a year later. In 2014, that number was closer to 80% with evidence suggesting that the number of insured young adults would continue to rise.24 Furthermore, beginning in 2014, the ACA required that all new insurance plans cover mental health as an essential health benefit category.25 The combination of these two aspects of the ACA would presumably afford tremendous benefits for young adults with mental health care needs. Yet in reality, the prevalence of mental health care utilization among young adults has not risen as expected. Data from 2012 showed an increase in the use of any mental health treatment among young adults from 30.7% in 2008 to only 32.86% in 2012,26 which suggests that factors that contribute to the treatment gap are complex and that insurance coverage is not the only barrier to young adults obtaining mental health care.
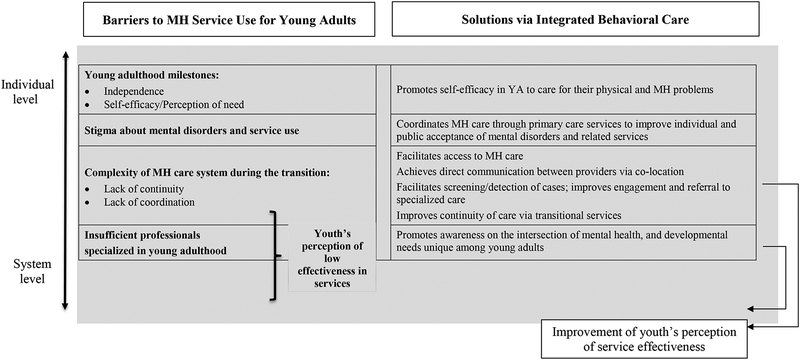
A few studies have examined barriers to mental health treatment in young adult populations.27–31 There are several barriers highlighted below that are especially relevant for the developmental period of young adulthood and have direct implications for the implementation of mental health services in the US. The barriers range from individual to system level ones (Figure 1), including: 1) changes in perception of mental health need and self-efficacy at the time of transition, 2) stigma about mental health disorders and treatment, 3) the complexity of the mental health care system during the transition period, and 4) the dearth of professionals who are trained in developmentally appropriate approaches to treat young adults. Identifying and understanding these barriers can help guide research and design interventions to improve service use and treatment for young adults with depressive and anxiety disorders.
Figure 1.
Barriers to mental health service use among young adults and targeted solutions via integrated behavioral care model
Changes in perception of need for mental health treatment and self-efficacy at the time of transition to young adulthood. Young adults may have a lower perceived need for mental health treatment. In one study assessing perception of need for and engagement in mental health treatment among a young adult sample, over 50% of those in the study reported no need for treatment despite meeting criteria for serious psychological distress.32 This may relate to the developmentally natural desire for increased independence and self-sufficiency. It is possible that one way young adults seek to achieve this desire is by attempting to manage symptoms on their own in the service of feeling more self-efficacious. In addition, many minors may have been previously forced to engage in treatment by parental figures so that once they reach the age of majority, they may choose not to continue in treatment.31
Stigma about mental health disorders and treatment. Young adults face issues related to stigma of mental disorders during a period of identity formation and the development of more stable relationships and career paths. Using data from the Behavioral Risk Factor Surveillance System, a study on patient health behaviors and health care access, Kobau and Zack (2013) assessed the level of stigma among patients across several U.S. states.33 The authors found that young adults were consistently less likely than older adult groups to strongly believe that patients with mental illness could live normal lives, receive sympathy and care from others, or benefit from psychiatric treatment. These negative attitudes towards mental health disorders may impact the desire to seek treatment as a way of maintaining a more positive self-concept.34,35 It is possible that at a time of identity consolidation, young adults may view a label such as “depression” as representing a negative self-perception.36 Furthermore, though young adults may be shifting away from older adults and peers for decision-making, they may still be concerned about how obtaining treatment may impact the perceptions that others have of them.31 For example, many young adults may be concerned about how having a mental health disorder in their record may impact admission in higher education or securing a first job.
- Complexity of the mental health care system during transition. The task of navigating the complex mental health system during the transition from pediatric to adult services can be quite difficult for young adults.
- Lack of continuity between pediatric and adult services. The point at which adolescent patients “age out” of specialized mental health systems can vary; in some systems, youth services end at age 18 and in others they end at age 22, with growing pressure to keep patients even older but, in most systems, services are clearly terminated at some point. The abrupt end of services is sometimes referred to as a “transition cliff”.37 Moreover, many services available for children and adolescents no longer exist for adults. For example, many adolescents have accessed mental health services through school-based programs, but after high school these resources are often no longer available to them unless they attend college. Even in college, the amount of treatment available at the counseling center may not be sufficient as visits are often limited. For those who do not go to college, options are more limited and/or difficult to access. Unfortunately, resources to aid young adults in this transition do not exist in many states. In a 2006 survey of transition services provided by state child mental health systems in 42 states, researchers found that existing transition services were woefully inadequate and rarely provided.38 The 2016–2017 National Survey on Child Health surveyed families of children ages 12–17 and revealed that only 15.4% of adolescents with special mental health care needs (including emotional, behavioral, or developmental issues) received services to assist with the transition to adult care services.39
- Lack of care coordination between adolescent and adult services. The lack of coordination between adult health care providers and community agencies providing care to adolescents can make it quite difficult for young adults to transition between services and access the mental health resources that they need.37,40 It also makes it difficult for the new providers to fully assess the needs of these patients. This can most greatly impact young adults who are members of high-risk populations that are typically in greater need of public services, such as justice-involved youth, youth in foster care, racial/ethnic minorities, or those with developmental disabilities.41,42
Lack of professionals trained in developmental approaches. The young adult population has only recently been recognized as one with unique challenges and treatment needs, thus relevant training and specialty care programs are still scarce. As a result, accessing mental health professionals who specialize in addressing the challenges faced during young adulthood (e.g. identify formation, increased number of adult responsibilities, etc.) can be exceedingly difficult. Furthermore, this challenge exists in the context of a baseline dearth of mental health professionals in the United States, and is magnified in rural as well as other underserved (e.g., lower socioeconomic resource) areas where even fewer mental health professionals may be available.37
The Opportunity and Challenge of Providing Mental Health Care for Young Adults in Primary Care Settings
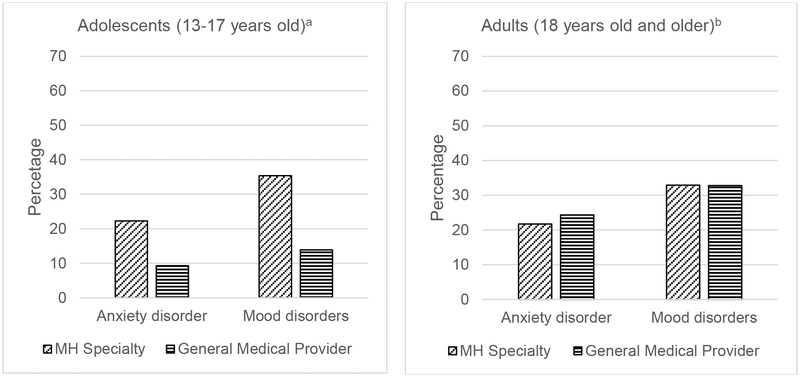
The primary care system is a setting where barriers preventing young adults from connecting to mental health services could be overcome. Pediatricians and primary care physicians are the front line of care and are in more frequent contact with young adults than mental health providers. According to US national data, adolescents receive treatment for mood and anxiety disorders mostly from specialized mental health providers (e.g. psychiatrists, psychologists, social workers, or counselors). Adults, on the other hand, are treated by primary care or general practitioners (Figure 2).43,44 A more recent study using the 2012–2013 Medical Expenditure Panel Surveys revealed that most adult patients receiving treatment for depression were treated by general medical professionals exclusively (73.3%) and far less were treated by psychiatrists (23.6%) or other mental health specialists (12.6%).20
Figure 2. Twelve-month mental health (MH) use for mood and anxiety disorders among adolescents and adults.
aMental health (MH) specialty: visit to a psychiatrist or psychologist in a setting such as a mental health clinic, community mental health center, drug or alcohol abuse clinic, or emergency room or admission to a psychiatric hospital or other facility. General medical setting: service provided by a general practitioner, family physician, pediatrician, or any other physician (Data from the National Comorbidity Survey-Adolescent, NCS-A).43
bMental health (MH) specialty: psychologists or other non-psychiatrist mental health professionals in any setting, social worker or counselor in a mental health specialty setting, or use of a mental health hotline. General medical provider: primary care physician, other general physician, nurse, and any other health professional not previously mentioned (Data from the National Comorbidity Survey Replication, NCS-R).44
Challenges that young adults may encounter in primary care settings include issues around detection of mental disorders and the quality of the mental health treatment provided. Primary care patients with depressive disorders often go unidentified, with up to 50% of depressed adults 18 and older not being recognized by primary care physicians.45 Furthermore, one study found that patients between 18 and 35 years old were less likely to be identified as depressed in the primary care setting compared to patients older than 35.46 There is evidence to suggest a similar situation for anxiety disorders. In a meta-analysis including studies with adult samples, primary care providers identified patients with anxiety disorders with a sensitivity of 30.5% when unassisted by rating scales as compared to a sensitivity of 63.6% when assisted.47
Even when patients do receive a diagnosis, some do not initiate treatment or the treatment received in the primary care setting may fail to adequately target the symptoms. Kroenke and colleagues (2007) found that in a sample of adults (ages 18–85), 41% of patients with at least one anxiety disorder (generalized anxiety disorder, panic disorder, social anxiety disorder, or post-traumatic stress disorder) reported receiving no treatment for their anxiety.48 Another study looking at the quality of care for depressive and anxiety disorders among adults (ages 18–85) found that 80.5% of patients who only reported primary care visits received inappropriate or no care during a 1-year period as opposed to 11.4% among patients who reported receiving care from mental health specialists. Younger (ages 18–29 years) and older (60 and older) adults in the study were less likely to receive appropriate care than for any other age group.49
In sum, the tendency of young adults to seek mental health treatment in primary care settings, coupled with the complex barriers to accessing specialized care, and the challenges of providing mental health care in primary care settings suggest that a closer look at the provision of adequate mental health treatment within primary care settings is warranted through the integrated care lens.
Proposed Solution: Integrated Behavioral Health Care for Young Adults
Integrated care is defined as the coordination of care between general and mental health care providers.50 The term ‘integrated care’ currently encompasses a spectrum of models, varying primarily in the nature of the relationship between the mental health provider and the primary care provider.51 This relationship ranges from coordinated care with minimal to basic collaboration between specialties, to co-located care, to full integration where members of both specialties work together as part of an interdisciplinary team to treat patients.52 Studies of integrated care models have occurred in a wide variety of populations and clinical settings, amassing a strong evidence base.
While studies of integrated care in primary care settings initially focused on patients with depression and little co-morbidity, they have since expanded to include other mental health diagnoses and co-morbidities, such as anxiety disorders.53–55 These studies have demonstrated that the integration of mental health resources into primary care settings can improve outcomes among patients with mental health needs. Three reviews focused on integrated care models in adult populations have shown significant improvement in several areas, including depressive and anxiety symptoms, patient satisfaction with care, adherence to treatment, treatment response, and quality of life/functional status for patients being treated for depression in primary care settings.56–58 There have also been studies demonstrating efficacy in pediatric and adolescent populations, showing a decrease in depressive symptoms, improvement in quality of life, greater satisfaction with health care, and higher prevalence of mental health service use.59,60 A 2017 review of studies focused on older adolescents and/or young adults conducted by Richardson and colleagues revealed that only two United States studies and one Australian study meeting the authors’ inclusion criteria included young adults in their samples. None of the studies focused solely on young adults and all of the studies focused on depression alone.61
A brief summary of key studies evaluating the efficacy of integrated care models for depression and anxiety disorders in primary care is provided in Table 1. This table is not meant to be exhaustive or cover all relevant research. Rather, it shows examples of studies investigating different integrated care models delivered to adolescent and adult populations while highlighting the gap of research on integrated care models specifically tailored for the young adult population. As displayed in the table, information collected from young adults is often merged with information collected from older adults.
Table 1.
Examples of studies of integrated care in primary care for adolescents and adults
| Author (year) | Collaborative Care Model | Age Range | Main Outcome | Brief Intervention Description | Comparison Condition | Results on Main Outcome (effect size) |
|---|---|---|---|---|---|---|
| Clarke et al. (2005)89 | Collaborative Stepped Care (CSS) | 12–18 | Depression | CSS [Brief CBT] | CAU | 12 month: No significant differences (effect size 0.17). |
| Richardson et al. (2014)60 | Reaching Out to Adolescents in Distress (ROAD) Study (adapted from IMPACT) | 13–17 | Depression | Collaborative Care Intervention (CCI) [Psychoeducation plus brief CBT, medication or both] | CAU | CCI: Significant improvement at 12-month follow up (effect size of 0.194). |
| Asarnow et al. (2005)59
Asarnow et al. (2009)62 |
Youth Partners in Care (YPIC) | 13–21 | Depression | Quality Improvement Intervention (QII) [Collaborative decision making about depression care management (CBT, medication, both)] | CAU | QII: Significant improvement at 6-month follow up. 18 month: No significant differences. |
| Van Voorhees, et al. (2008)63
Van Voorhees et. al. (2009)64 Hoek et al. (2011)65 |
Competent Adulthood Transition with CBT and Interpersonal Training (CATCH-IT) | 14–21 | Subthreshold depression | PCP brief motivational interview (MI) + CATCH-IT Internet program | PCP brief advice (BA) + CATCH-IT Internet program | 4–8 weeks: No significant differences. 12 weeks: MI group reported significant decrease in depressive episodes and hopelessness. 6 months: No significant differences (effect size 1.12 (MI) vs. 0.63 (BA)). |
| Reid et. al. (2011)66
Reid et. al. (2013)67 |
Mobile Tracking Young People’s Experiences (mobiletype) - phone app | 14–24 | Anxiety, Depression | Mobiletype: Selfmonitoring mood, stress, substance use, sleep, exercise, and diet with phone app. | Attention control | 6 weeks and 6 months: No significant difference in depression or anxiety symptoms. |
| Hobbs, et. al. (2017)68 | ThisWayUp iCBT (internet-delivered CBT) | 18 – 60+ | Anxiety, Depression | ThisWayUp iCBT: Six online sessions of iCBT. | None | For 18–29 year-old group: Significant reduction in anxiety and depressive symptoms. |
| Oosterbann et al. (2013)53 | Collaborative Stepped Care (CSS) | 18 or older | Anxiety, Depression | CSC [Step 1: self-help training and medication; Step 2: CBT plus medication] | CAU | CSC: Significant improvement at the 4-month follow up. 8 month and 12 month: No longer significant differences (effect size = 0.80). |
| Miranda et al. (2003)90 | Partners in Care (PIC) | 18 or older | Depression | Quality Improvement Intervention (QII) [CBT or medication] | CAU | QII: Significant improvement at 6- and 12-month follow ups for Latinos and African-American compared to CAU. |
| Rollman et al. (2005)54 | Coordinated Anxiety Learning and Management (CALM) (adapted from IMPACT) | 18–64 | Anxiety | CALM: Telephone-based care management intervention | Notification of anxiety disorder alone | CALM: Significant improvement at 12-month follow up (effect size of 0.330.38). |
| Roy-Byrne et al. (2010)55 | Coordinated Anxiety Learning and Management (CALM) (adapted from IMPACT) | 18–75 | Anxiety | CALM [CBT or medication or both] | CAU | CALM: Significant improvement at 6-, 12- and 18-month follow ups (effect sizes: −0.30, −0.31, −0.18). |
| Unutzer et al. (2002)91 | Improving Mood-Promoting Acess to Collaborative Treatment (IMPACT) | 60 and older | Depression | IMPACT [antidepresants or brief psychotherapy] | CAU | IMPACT: Significant improvement at 12-month follow up. |
Note: The psychological interventions are conducted by trained (Master’s of PhD level) clinicians or care managers.
CBT: cognitive-behavioral therapy; CAU: care as usual
One of the three studies identified in the Richardson review, which included studies involving adolescents as well as young adults, is the Youth Partner in Care (YPIC) Study (Table 1). The YPIC Study included a US sample of patients aged 13 to 21 and evaluated a quality improvement intervention aimed at promoting access to evidence-based depression treatment in primary care settings for patients with either depressive disorders or sub-syndromal depressive symptoms compared to usual care.59 As part of the intervention, primary care physicians were given training on depression evaluation and management, on-site leader teams helped implement the intervention, care managers who were trained in cognitive behavioral therapy were available to support the primary care physician, and patients and their clinicians were able to choose the treatment modality (CBT, medication, or both). At 6-month follow up, patients in the intervention arm had significantly lower scores of severe depression, reported higher prevalence of mental health treatment, improvement in quality of life, and greater satisfaction with care than those in the usual care arm. At 18-month follow up, there was no statistically significant difference between the two groups.62
Another study is the Competent Adulthood Transition with CBT and Interpersonal Training (CATCH-IT) study. This study tested an internet-based program that comprised 14 modules developed to assist with depression prevention in adolescents. Patients aged 14 to 21 with sub-syndromal depression were recruited for the study. The internet modules were based on behavioral activation and cognitive behavioral therapy with goal of teaching adolescents to reduce behaviors that contribute to depression and increase behaviors that increase resilience. The study compared motivational interviewing (MI) plus CATCH-IT to brief advice plus CATCH-IT.63 Brief advice consisted of a 1–2 min interview in which the physician recommends completion of the CATCH-IT program and follow up in 4–6 weeks. Those in the MI arm completed a 5–15 min interview during which the physician helped the patient identify personal reasons for completing CATCH-IT and received three phone calls from a social worker. At 12 weeks, both groups showed a decrease in depressed mood, but the MI group also had lower cumulative prevalence of depressive episodes and lower prevelance of hopelessness. Reductions in depression were sustained at 6 months in both groups, but the MI group continued to show fewer depressive episodes and lower prevelance of hopelessness.64,65
The third study assessed the Mobile Tracking Young People’s Experiences (mobiletype) application, a mobile phone assessment and management tool that monitored several items, including the user’s mood, stress, coping strategies, daily activities, eating habits, sleep, exercise, and substance use.66,67 Patients aged 14 to 24 who had a mild or more severe mental health problem were included in the study. The intervention group engaged in self-monitoring with the mobile type app and their data was uploaded to a website that the user’s physician could access. The comparison group (also referred to as the “attention control” group) monitored themselves with a less extensive version of the mobiletype app which did not assess the user’s mood, stress, coping strategies, or substance use. Both groups also received usual care. The intervention was associated with improved physician assessment, diagnosis, and treatment decision making. However, there were no significant differences in reported depression or anxiety symptoms at the 6-week and 6-month assessments.
The only study with adult patients that included separate analyses for young adults (ages 18 to 29) was conducted by Hobbs and colleagues. This open trial tested the use of ThisWayUp internet-delivered CBT (iCBT) in clinical care for anxiety in adults.68 ThisWayUp iCBT was prescribed by a treating provider (e.g. general practitioner, psychiatrist, psychologist, or other health professional), though 67% of participants were prescribed the intervention by a general practitioner. The intervention consisted of six online treatment sessions after which participants were encouraged to complete homework. Treatment was completed over a 12-week course and providers were encouraged to reach out to the participates after the first two lessons to provide support. The 18–29 year-old group showed significant decrease in both anxiety and depressive symptoms from pre- to post-treatment. However, one limitation of the study was the absence of a control group.
Although findings on the long-term efficacy are mixed, some models are promising and suggest that these types of interventions could be helpful for young adults.
How Would Behavioral Health Integrated Care Help Young Adults with Mental Health Needs?
Given the characteristics of young adults and the specific barriers that they face when accessing care, there are several ways in which the integration of mental health care in primary care settings could lead to substantial improvements in mental health care access and treatment. Specifically, integrated care has the potential to successfully address the four barriers that prevent young adults from obtaining mental health services (Figure 1), as described below.
Changes in perception of need for mental health treatment and self-efficacy at the time of transition to young adulthood. Resources common to integrated care settings, such as the team-based approach and the presence of care managers, can be immensely valuable for improving the likelihood of engagement in mental health care for youth and building youth’s feelings of self-efficacy as the scaffolding provided by parents may begin to wane. The support of a treatment team may also aid in helping a young adult better understand his or her need for mental health treatment. Indeed, several integrated care studies in primary care with adolescents and adults have shown a significant increase in treatment adherence and treatment satisfaction among patients assigned to the integrated care intervention group.59,69,70
Stigma about mental disorders during a period of identity formation. There is evidence suggesting that integration of mental health treatment in primary care can lead to stigma reduction among youth seeking mental health care. In the Partners in Care (YPIC) Study, adolescents in the intervention group who had received extra therapy were less likely to have concerns about others learning about their mental health history.71 In another study, the Primary Care Research in Substance Abuse and Mental Health for the Elderly (PRISM-E) study, 93% of the surveyed primary care providers believed that integration of care led to less stigma among patients.72 While these conclusions are drawn based on observations of adolescent and adult patients, the potential for and benefits related to stigma reduction among young adults is significant, such that it could not only increase rates of help seeking in this population, but also to help the young adult to develop a healthy and positive identity. Furthermore, the co-location of behavioral and medical health services in primary care settings has the potential to reduce public stigma (i.e., prejudice and stereotypes placed by society on the mentally ill), which may lead young adults to actively seek treatment while maintaining a positive self-concept, a key achievement at times of great identity change.
-
Complexity of the mental health care system during transition. Integrated care in primary care may also help mitigate the challenges of navigating an ever-changing health and healthcare landscape, as well as improve the communication between professionals, with basic physical and mental health care needs being addressed in a single location.
The integrated care model could be adapted to include a greater emphasis on referrals from primary care to specialized adult services for young adults who may benefit from or need ongoing specialized mental health care. This includes close monitoring of patients who are currently being treated for anxiety or depression or who are at high risk for recurrence of anxiety or depressive symptoms to identify those who are at highest risk of falling out of care during the time of transition. Schraeder and Reid (2017) proposed criteria that could be used to identify youth who may require transition to adult specialized mental health services.73 These criteria are based on the patient’s risk trajectory, level of illness severity, presence of comorbidity, level of interpersonal functioning and familial support present. While the authors focus primarily on the transition to adult specialized mental health services, they do acknowledge that the involvement of primary care would be important. The identification and monitoring of those who are likely to need ongoing care through adult mental health services could allow for more targeted efforts to facilitate this transition from primary care. The American Academy of Pediatrics recently published updated recommendations about the incorporation of transition planning and services for adolescents and young adults, emphasizing care coordination and a team based approach.74 Care coordinators, if part of integrated primary care clinics, could be trained to identify the needs of these patients and aide in coordination of ongoing services within the current clinic or assistance with transition to and follow up in the specialized adult mental health care system. The presence of a care coordinator in a pediatric practice has been found to increase the likelihood of transition planning, particularly if the role is specifically designated for transition planning.75 The incorporation of this element of young adult care coordination is particularly important for those who are being seen in pediatric clinics rather than family medicine clinics because patients treated in pediatric clinics “age out” whereas those in family medicine clinics may likely be able to continue in treatment given that family practitioners see patients across the life span. Further research in transition services for young adults is needed. In a recently published systematic review of interventions for pediatric to adult heath care transitions, many studies showed statistically significant positive outcomes in various areas, including adherence to care, improvements in self-care, improvements in satisfaction with care, decreases in barriers to care, and improvements in appropriate health care utilization. However, the authors also note that many of the studies reviewed suffered from various limitations. Furthermore, none of the reviewed studies focused on young adults with mental health conditions.76
Lack of professionals trained in developmental approaches. Members of the clinical team providing medical and behavioral health care for young adults could be trained in engagement strategies and issues relevant to young adulthood. For example, given that the assertion of independence is a significant goal during this period, it may be important to work together with young adult patients on their aim of independence and self-efficacy by highlighting the ways in which treatment can facilitate achievement of this goal.
Integrated care may also address some of the specific challenges of providing mental health care in primary care settings. An integrated care model can empower primary care physicians to be more mindful of the mental health disorders occurring during young adulthood and, therefore, increase the likelihood that patients are screened and treated for common psychiatric disorders. Working together with teams specializing in young adulthood may also translate to increased awareness among primary care providers of young adults’ mental and developmental needs. In addition, studies on integrated care models have demonstrated that it can help ensure that patients receive adequate mental health care, even if patients are not seen directly by a psychiatrist.53,77
Barriers to integrating mental health in primary care certainly also exist. The current structure of the primary care system may not in its current state allow for proper integration of behavioral health. For example, with many clinics operating with 15 min appointments, primary care physicians are often working under time constraints which may make it difficult to adequately assess for and treat mental disorders in general practice and properly consider developmental issues relevant to young adults. In a cross-sectional survey of non-retired members of the American Academy of Pediatrics, 77% of respondents reported lack of time to treat as a major barrier to addressing mental health problems in practice. Sixty-five percent reported a lack of training in treatment of child mental disorders.78 Lack of time has also been cited as a major barrier among adult providers.79 We expect time constraints to be as or even more challenging in the care of young adults, given the several developmental transitions and changes described above.
In sum, integrated care stands to address barriers and challenges of engaging in mental health treatment and to improve youth’s perception of service’s effectiveness. Elements such as provider education, team coordination, care management, and provision of adequate mental health interventions in primary care can help increase access.80 To the authors’ knowledge, there are no effectiveness studies about integrated mental health focused on the young adult population (Table 1). As mentioned earlier, none of the currently published studies have included young adults in sufficient numbers to draw conclusions specific to this developmental group, highlighting the need for research within this population. Research studies are needed to assess the full potential of integrated care models to address the mental health needs of young adults.
Future Opportunities and Challenges
Opportunities.
Government agencies have begun to fully recognize the benefits of integrated care. In November 2016, the Centers for Medicare and Medicaid Services (CMS) announced changes to the Medicare physician fee schedule that would revise payment for care coordination and chronic disease management provided in primary care. In addition, it pays for services using a psychiatric collaborative care model. The CMS proposed to provide reimbursement for other integrated care models as well. These changes went into effect in the beginning of 2017.59 While not likely to directly impact most young adults initially, this decision addresses some of the structural challenges of providing mental health care in primary care and paves the way for revisions to fee schedules from other payers including Medicaid and private insurers that do cover more significant numbers of young adults. Therefore, it is possible that any models tailored for young adults could also capitalize on reimbursements for care coordination.
Most studies that have evaluated integrated care and also included young adults in the study sample tend to focus on depression alone, though anxiety is also a prevalent disorder in this population. More research is needed to evaluate the utility of these interventions for anxiety alone or comorbid with depression in this age group.
Challenges.
Financing and resource allocation will be key for integrated care models for young adults to succeed. The primary care system is not often equipped to identify mental health needs or to provide mental health care, considering its current structure. The system is often characterized by lack of training and a fee structure that does not include resources (time, personnel, and reimbursement) for screening or treatment of mental health problems.81–83 In addition, given the number of young adults who were able to acquire insurance through the Affordable Care Act, this population could be particularly vulnerable to any policy changes made that could re-introduce the lack of insurance coverage as a major barrier to mental health care for this population.
The ideal setting for implementation of these models is not yet clear. It is easily conceivable that an integrated care model with transition services might be best implemented in a pediatric setting, as professionals already treating children may more easily understand the developmental challenges of young adulthood. However, clarification on this issue will likely require studies that examine the benefits of implementation in a pediatric setting versus and an adult setting.
There also remain confidentiality issues that may complicate the decision to access mental health care if young adults are on their parent’s insurance. Slive and Cramer (2012) outline issues around confidentiality for young adults in the age of health care reform, specifically noting the billing practices such as the practice of sending policyholders (e.g., parents) an explanation of benefits (EOB), which can often reveal private medical information to parents, even if this information was not disclosed by the provider.84 While the data on perceptions of confidentiality and its impact on treatment seeking are more robust in the adolescent literature, there are reasons to be concerned about this issue among young adults as well.85–87 For example, approximately three years after Massachusetts instituted its health care reform, Besset and colleagues (2015) conducted focus groups among young adults on barriers to contraceptive access.88 Young adults expressed apprehension about confidentiality after the coverage expansion that allowed them to remain on their parents’ insurance due to concerns about insurance disclosures of certain types of care to parents. This concern made them hesitant to pursue oral contraception. If young adults are worried about their confidentiality being maintained, they may be more likely to disengage from mental health treatment or not engage at all.
Implications for Behavioral Health
Young adulthood is a highly vulnerable developmental period, as individuals tend to present with the precarious combination of an increase in mental health needs – particularly with the spike in anxiety and depressive disorders - and a decrease in mental health service utilization, likely due to several individual- and system-level barriers. It is imperative that efforts focus on removing barriers to mental health care in young adulthood. Based on research with older and younger populations, integrating mental health care into primary care could be a very successful strategy. Integrated care in primary care settings is a well-established, evidence-based model of care for mental illness in adults (with growing support for adolescents) that stands to greatly mitigate the numerous challenges young adults face in accessing and engaging in care. Integrated care models tailored for young adults have the potential of improving detection and the quality of care provided in primary care settings, as well as of addressing the young adults’ individual- and system-level barriers for accessing care. Adapting existing integrated care models for young adults can help reduce stigma, support positive identity formation, and mitigate the challenges associated with navigation of the adult healthcare system. The success of this model will certainly require developing behavioral health models that are viable within the existing and evolving primary care system. This may require changes and adaptations in current behavioral health as well as primary care practice to properly respond to the needs of young adults in primary care. Such integrated care models could incorporate interventions and guidelines to facilitate transition to adult specialized mental health services when illness severity warrants an increase in service intensity thereby addressing a myriad of clinical presentations.
Conflict of Interest Statement:
Laura Mufson, PhD receives book royalties from Guilford Publications, Inc. and Oxford University Press. She is a recipient of grants from NIMH, SAMHSA, and NARSAD, and honoraria for academic grand rounds. She does not have any consultancies.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
The remaining authors have no conflicts of interest to declare.
REFERENCES
- 1.Arnett J Emerging adulthood: A theory of development from the late teens through the twenties. The American Psychologist. 2000;55(5):469–480. [PubMed] [Google Scholar]
- 2.Copeland W, Angold A, Shanahan L, et al. Longitudinal patterns of anxiety from childhood to adulthood: The great smoky mountains study. Journal of the American Academy of Child and Adolescent Psychiatry. 2014;53(1):21–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hankin B Adolescent depression: Description, causes, and interventions. Epilepsy and Behavior. 2006;8(1):102–114. [DOI] [PubMed] [Google Scholar]
- 4.Scott J, Scott EM, Hermens DF, et al. Functional impairment in adolescents and young adults with emerging mood disorders. The British Journal of Psychiatry. 2014;205(5):362–368. [DOI] [PubMed] [Google Scholar]
- 5.Swan AJ, Kendall PC. Fear and missing out: Youth anxiety and functional outcomes. Clinical Psychology: Science and Practice. 2016;23(4):417–435. [Google Scholar]
- 6.Investing in the health and well-being of young adults. Institute of Medicine and National Research Council;2015. [Google Scholar]
- 7.Substance Abuse and Mental Health Services Administration. Behavioral health trends in the united states: Results from the 2016 national survey on drug use and health. In: Center for Behavioral Health Statistics and Quality; 2017. [Google Scholar]
- 8.National comorbidity survey (ncs). In. Harvard Medical School: Harvard Medical School; 2007. [Google Scholar]
- 9.Lewinsohn P, Rohde P, Seeley J, et al. Gender differences in suicide attempts from adolescence to young adulthood. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(4):427–434. [DOI] [PubMed] [Google Scholar]
- 10.Salk R, Petersen J, Abramson L, et al. The contemporary face of gender differences and similarities in depression throughout adolescence: Development and chronicity. Journal of Affective Disorders. 2016;205:28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kessler R, Avenevoli S, Merikangas K. Mood disorders in children and adolescents: An epidemiologic perspective. Biological Psychiatry. 2001;49(12):1002–1014. [DOI] [PubMed] [Google Scholar]
- 12.Yaroslavsky I, Pettit J, Lewinsohn P, et al. Heterogeneous trajectories of depressive symptoms: Adolescent predictors and adult outcomes. Journal of Affective Disorders. 2013;148(0):391–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pottick KJ, Bilder S, Vander Stoep A, et al. Us patterns of mental health service utilization for transition-age youth and young adults. Journal of Behavioral Health Services and Research. 2008;35:373–389. [DOI] [PubMed] [Google Scholar]
- 14.Walker ER, Cummings JR, Hockenberry JM, et al. Insurance status, use of mental health services, and unmet need for mental health care in the united states. Psychiatric Services. 2015;66(6):578–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kessler R, Demler OD, Frank RG, et al. Prevalence and treatment of mental disorders, 1990 to 2003. New England Journal of Medicine. 2005;352(24):2515–2523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Druss BG, Hoff RA, Rosenheck RA. Underuse of antidepressants in major depression: Prevalence and correlates in a national sample of young adults. The Journal of Clinical Psychiatry. 2000;61(3):234–237. [PubMed] [Google Scholar]
- 17.Copeland W, Shanahan L, Davis M, et al. Increase in untreated cases of psychiatric disorders during the transition to adulthood. Psychiatric Services. 2015;66(4):397–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kessler R, Walters E. Epidemiology of dsm-iii-r major depression and minor depression among adolescents and young adults in the national comorbidity survey. Depression and Anxiety. 1998;7(1):3–14. [DOI] [PubMed] [Google Scholar]
- 19.Mackenzie CS, Reynolds K, Cairney J, et al. Disorder-specific mental health service use for mood and anxiety disorders: Associations with age, sex, and psychiatric comorbidity. Depression and Anxiety. 2012;29(3):234–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Olfson M, Blanco C, Marcus SC. Treatment of adult depression in the united states. Journal of the American Medical Association Internal Medicine. 2016;176(10):1482–1491. [DOI] [PubMed] [Google Scholar]
- 21.Patient protection and affordable care act. In: U.S.C., ed. 111–148 2010. [Google Scholar]
- 22.Kenney G, Zuckerman S, Dubay L, et al. Opting in to the medicaid expansion under the aca : Who are the uninsured adults who could gain health insurance coverage ? : Urban Institute;2012. [Google Scholar]
- 23.Rudowitz R, Artiga S, Arguello R. Children’s health coverage: Medicaid, chip and the aca. The Henry J Kaiser Family Foundation;2014. [Google Scholar]
- 24.McMorrow S, Kenney GM, Long SK, et al. Uninsurance among young adults continues to decline, particularly in medicaid expansion states. Health Affairs. 2015;34(4):616–620. [DOI] [PubMed] [Google Scholar]
- 25.Beronio K, Po R, Skopec L, et al. Affordable care act expands mental health and substance use disorder benefits and federal parity protections for 62 million americans. In: U.S. Department of Health & Human Services, ed. Washington, DC: 2013. [Google Scholar]
- 26.Saloner B, Le Cook B. An aca provision increased treatment for young adults with possible mental illnesses relative to comparison group. Health Affairs. 2014;33(8):1425–1434. [DOI] [PubMed] [Google Scholar]
- 27.Biddle L, Donovan J, Sharp D, et al. Explaining non-help-seeking amongst young adults with mental distress: A dynamic interpretive model of illness behaviour. Sociology of Health and Illness. 2007;29(7):983–1002. [DOI] [PubMed] [Google Scholar]
- 28.Fox JC, Blank M, Rovnyak VG, et al. Barriers to help seeking for mental disorders in a rural impoverished population. Community Mental Health Journal. 2001;37(5):421–436. [DOI] [PubMed] [Google Scholar]
- 29.Rickwood DJ, Deane FP, Wilson CJ. When and how do young people seek professional help for mental health problems? The Medical Journal of Australia. 2007;187(7suppl):S35–S39. [DOI] [PubMed] [Google Scholar]
- 30.Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. British Medical Journal. 2010;10:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Munson MR, Jacaard J, Smalling SE, et al. Static, dynamic, integrated, and contextualized: A framework for understanding mental health service utilization among young adults. Social Science and Medicine. 2012;75:1441–1449. [DOI] [PubMed] [Google Scholar]
- 32.Narendorf S, Palmer A. Perception of need and receipt of mental health treatment: A three-group comparison of young adults with psychological distress. Psychiatric Services. 2016;67(8):924–927. [DOI] [PubMed] [Google Scholar]
- 33.Kobau R, Zack MM. Attitudes toward mental illness in adults by mental illness–related factors and chronic disease status: 2007 and 2009 behavioral risk factor surveillance system. American Journal of Public Health. 2013;103(11):2078–2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van Voorhees BW, Fogel J, Houston TK, et al. Attitudes and illness factors associated with low perceived need for depression treatment among young adults. Social Psychiatry and Psychiatric Epidemiology. 2006;41(9):746–754. [DOI] [PubMed] [Google Scholar]
- 35.Van Voorhees BW, Fogel J, Houston TK, et al. Beliefs and attitudes associated with the intention to not accept the diagnosis of depression among young adults. Annals of Family Medicine. 2005;3(1):38–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Laursen B, Collins AW, eds. Relationship pathways: From adolescence to young adulthood. Los Angeles: SAGE Publications, Inc; 2012. [Google Scholar]
- 37.Roy S Successful transition models for youth with mental health needs: A guide for workforce professionals. In: National Collaborative on Workforce and Disability for Youth, ed 2009:1–5. [Google Scholar]
- 38.Davis M, Geller JL, Hunt B. No within-state availability of transition-to-adulthood services for youths with serious mental health conditions. Psychiatric Services. 2006;57(11):1594–1599. [DOI] [PubMed] [Google Scholar]
- 39.Child and Adolescent Health Measurement Initiative. 2016–2017 national survey of children’s health (nsch) data query. Data Resource Center for Child and Adolescent Health supported by Cooperative Agreement U59MC27866 from the U.S. Department of Health and Human Services, Health Resources and Services Administration’s Maternal and Child Health Bureau (HRSA MCHB). www.childhealthdata.org. Accessed 11/4/18.
- 40.Davis M, Sondheimer DL. State child mental health efforts to support youth in transition to adulthood. Journal of Behavioral Health Services and Research. 2005;32(1):27–42. [DOI] [PubMed] [Google Scholar]
- 41.MacLeod KB, Brownlie E. Mental health and transitions from adolescence to emerging adulthood: Developmental and diversity considerations. Canadian Journal of Community Mental Health. 2014;33(1):77–86. [Google Scholar]
- 42.Merikangas K, He J-p, Burstein ME, et al. Service utilization for lifetime mental disorders in u.S. Adolescents: Results of the national comorbidity survey-adolescent supplement (ncs-a). Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50(1):32–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Costello EJ, He J-p, Sampson NA, et al. Services for adolescents with psychiatric disorders: 12-month data from the national comorbidity survey-adolescent. Psychiatric Services. 2014;65(3):359–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the united states: Results from the national comorbidity survey replication. Journal of the American Medical Association Psychiatry. 2005;62(6):629–640. [DOI] [PubMed] [Google Scholar]
- 45.Simon G, VonKorff M. Recognition, management, and outcomes of depression in primary care. Archives of Family Medicine. 1995;4(2):99–105. [DOI] [PubMed] [Google Scholar]
- 46.Borowsky SJ, Rubenstein LV, Meredith LS, et al. Who is at risk of nondetection of mental health problems in primary care? Journal of General Internal Medicine. 2000;15(6):381–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Olariu E, Forero CG, Castro-Rodriguez JI, et al. Detection of anxiety disorders in primary care: A meta-analysis of assisted and unassisted diagnoses. Depression and Anxiety. 2015;32(7):471–484. [DOI] [PubMed] [Google Scholar]
- 48.Kroenke K, Spitzer RL, Williams JBW, et al. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine. 2007;146(5):317–325. [DOI] [PubMed] [Google Scholar]
- 49.Young AS, Klap R, Sherbourne CD, et al. The quality of care for depressive and anxiety disorders in the united states. Archives of General Psychiatry. 2001;58(1):55–61. [DOI] [PubMed] [Google Scholar]
- 50.What is integrated care? SAMHA-HRSA Center for Integrated Health Solutions; https://www.integration.samhsa.gov/about-us/what-is-integrated-care. Accessed February 8, 2018. [Google Scholar]
- 51.Wulsin LR, Söllner W, Pincus HA. Models of integrated care. Medical Clinics of North America. 2006;90(4):647–677. [DOI] [PubMed] [Google Scholar]
- 52.Heath B, Wise RP, Reynolds K. A review and proposed standard framework for levels of integrated healthcare. Washington, DC: SAMHSA-HRSA Center for Integrated Health Solutions; March 2013. [Google Scholar]
- 53.Oosterbaan DB, Verbraak MJPM, Terluin B, et al. Collaborative stepped care v. Care as usual for common mental disorders: 8-month, cluster randomised controlled trial. British Journal of Psychiatry. 2013;203(2):132–139. [DOI] [PubMed] [Google Scholar]
- 54.Rollman BL, Belnap BH, Mazumdar S, et al. Randomized trial to improve the quality of treatment for panic and generalized anxiety disorders in primary care. Archives of General Psychiatry. 2005;62(12):1332–1341. [DOI] [PubMed] [Google Scholar]
- 55.Roy-byrne P, Craske MG, Sullivan G, et al. Delivery of evidence-based treatment for multiple anxiety disorders in primary care: A randomized controlled trial. Journal of American Medical Association. 2010;303(19):1921–1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gilbody S, Bower P, Fletcher J, et al. Collaborative care for depression: A cumulative meta-analysis and review of longer-term outcomes. Archives of Internal Medicine. 2006;166(21):2314–2321. [DOI] [PubMed] [Google Scholar]
- 57.Thota A, Sipe TA, Byard GJ, et al. Collaborative care to improve the management of depressive disorders: A community guide systematic review and meta-analysis. American Journal of Preventive Medicine. 2012;42(5):525–538. [DOI] [PubMed] [Google Scholar]
- 58.Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database of Systematic Reviews. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Asarnow JR, Jaycox LH, Duan N, et al. Effectiveness of a quality improvement intervention for adolescent depression in primary care clinics: A randomized controlled trial. Journal of the American Medical Association. 2005;293(3):311–319. [DOI] [PubMed] [Google Scholar]
- 60.Richardson LP, Ludman E, McCauley E, et al. Collaborative care for adolescents with depression in primary care: A randomized clinical trial. Journal of American Medical Association. 2014;312(8):809–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Richardson L, McCarty C, Radovic A, et al. Research in the integration of behavioral health for adolescents and young adults in primary care settings: A systematic review. Journal of Adolescent Health. 2017;60(3):261–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Asarnow JR, Jaycox LH, Tang L, et al. Long-term benefits of short-term quality improvement interventions for depressed youths in primary care. American Journal of Psychiatry. 2009;166(9):1002–1010. [DOI] [PubMed] [Google Scholar]
- 63.Van Voorhees BW, Vanderplough-Booth K, Fogel J, et al. Integrative internet-based depression prevention for adolescents: A randomized clinical trial in primary care for vulnerability and protective factors. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2008;17(4):184–196. [PMC free article] [PubMed] [Google Scholar]
- 64.Van Voorhees BW, Fogel J, Reinecke M, et al. Randomized clinical trial of an internet-based depression prevention program for adolescents (project catch-it) in primary care: 12 week outcomes. Journal of Developmental and Behavioral Pediatrics. 2009;30(1):23–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hoek W, Marko M, Fogel J, et al. Randomized controlled trial of primary care physician motivational interviewing versus brief advice to engage adolescents with an internet-based depression prevention intervention: 6-month outcomes and predictors of improvement. Translational Research. 2011;158(6):315–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Reid S, Kauer S, Hearps S, et al. A mobile phone application for the assessment and management of youth mental health problems in primary care: A randomised controlled trial. BMC Family Practice. 2011;12(131). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Reid S, Kauer S, Hearps S, et al. A mobile phone application for the assessment and managemenr of youth mental health problems in primary care: Health service outcomes from a randomised controlled trial of mobiletype. BMC Family Practice. 2013;14(84). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hobbs M, Mahoney A, Andrews G. Integrating icbt for generalized anxiety disorder into routine clinical care: Treatment effects across the adult lifespan. Journal of Anxiety Disorders. 2017;51:47–54. [DOI] [PubMed] [Google Scholar]
- 69.Rost K, Nutting P, Smith J, et al. Improving depression outcomes in community primary care practice: A randomized trial of the quest intervention. Journal of General Internal Medicine. 2001;16(3):143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sirey JA, Bruce ML, Kales HC. Improving antidepressant adherence and depression outcomes in primary care: The treatment initiation and participation program. American Journal of Geriatric Psychiatry. 2010;18(6):554–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Klap R, Tang L, Schell T, et al. How quality improvement interventions for depression affect stigma concerns over time: A nine-year follow-up study. Psychiatric Services. 2009;60(2):258–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gallo JJ, Zubritsky C, Maxwell J, et al. Primary care clinicians evaluate integrated and referral models of behavioral health care for older adults: Results from a multisite effectiveness trial (prism-e). Annals of Family Medicine. 2004;2(4):305–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schraeder KE, Reid GJ. Who should transition? Defining a target population of youth with depression and anxiety that will require adult mental health care. The Journal of Behavioral Health Services and Research. 2017;44(2):316–330. [DOI] [PubMed] [Google Scholar]
- 74.White PH, Cooley WC, Transitions Clinical Report Authoring Group, et al. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2018;142(5). [DOI] [PubMed] [Google Scholar]
- 75.Sharma N, O’hare K, O’connor KG, et al. Care coordination and comprehensive electronic health records are associated with increased transition planning activities. Academic Pediatrics. 2017;18(1):111–118. [DOI] [PubMed] [Google Scholar]
- 76.Gabriel P, McManus M, Rogers K, et al. Outcome evidence for structured pediatric to adult health care transition interventions: A systematic review. The Journal of Pediatrics. 2017;188:263–269. [DOI] [PubMed] [Google Scholar]
- 77.Chaney EF, Rubenstein LV, Chuan-Fen L, et al. Implementing collaborative care for depression treatment in primary care: A cluster randomized evaluation of a quality improvement practice redesign. Implementation Science. 2011;6:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Horwitz S, Kelleher K, Stein R, et al. Barriers to the identification and management of psychosocial issues in children and maternal depression. Pediatrics. 2007;119(1):e208–218. [DOI] [PubMed] [Google Scholar]
- 79.Hutton C, Gunn J. Do longer consultations improve the management of psychological problems in general practice? A systematic review. BMC Health Services Research. 2007;7(71). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wells KB, Sherbourne C, Schoenbaum M, et al. Impact of disseminating quality improvement programs for depression in managed primary care: A randomized controlled trial. Journal of American Medical Association. 2000;283(2):212–220. [DOI] [PubMed] [Google Scholar]
- 81.Monson SP, Sheldon CJ, Ivey LC, et al. Working toward financial sustainability of integrated behavioral health services in a public health care system. Families, Systems, & Health. 2012;30(2):181–186. [DOI] [PubMed] [Google Scholar]
- 82.Grazier KL, Klinkman MS. The economics of integrated depression care: The university of michigan study. Administration and Policy in Mental Health and Mental Health Services Research. 2006;33(1):16–20. [DOI] [PubMed] [Google Scholar]
- 83.Wallace NT, Cohen DJ, Gunn R, et al. Start-up and ongoing practice expenses of behavioral health and primary care integration interventions in the advancing care together (act) program. Journal of the American Board of Family Medicine. 2015;28(S86-S97). [DOI] [PubMed] [Google Scholar]
- 84.Slive L, Cramer R. Health reform and the preservation of confidential health care for young adults. Journal of Law, Medicine & Ethics. 2012;40(2):383–390. [DOI] [PubMed] [Google Scholar]
- 85.Ford CA, Best D, Miller WC. Confidentiality and adolescents’ willingness to consent to sexually transmitted disease testing. Archives of Pediatric and Adolescent Medicine. 2001;155(9):1072–1073. [PubMed] [Google Scholar]
- 86.Ford CA, Millstein SG, Halpern-Felsher BL, et al. Influence of physician confidentiality assurances on adolescents’ willingness to disclose information and seek future health care: A randomized controlled trial. Journal of the American Medical Association. 1997;278(12):1029–1034. [PubMed] [Google Scholar]
- 87.Lehrer J, Pantell R, Tebb K, et al. Forgone health care among u.S. Adolescents: Associations between risk characteristics and confidentiality concern. Journal of Adolescent Health. 2007;40(3):218–226. [DOI] [PubMed] [Google Scholar]
- 88.Bessett D, Prager J, Havard J, et al. Barriers to contraceptive access after health care reform : Experiences of young adults in massachusetts. Women’s Health Issues. 2015;25(2):91–96. [DOI] [PubMed] [Google Scholar]
- 89.Clarke G, Debar L, Lynch F, et al. A randomized effectiveness trial of brief cognitive-behavioral therapy for depressed adolescents receiving antidepressant medication. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44(9):888–898. [PubMed] [Google Scholar]
- 90.Miranda J, Duan N, Sherbourne C, et al. Improving care for minorities: Can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized, controlled trial. Health Services Research. 2003;38(2):613–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Unützer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: A randomized controlled trial. Journal of the American Medical Association. 2002;288(22):2836–2845. [DOI] [PubMed] [Google Scholar]