Abstract
Objectives
An understanding of the relationship between individuals’ pregnancy preferences and contraceptive use is essential for appropriate patient-centered counseling and care. We examined the relationship between women’s pregnancy preferences and contraceptive use using a new prospective measure, the Desire to Avoid Pregnancy (DAP) scale.
Study Design
As part of a study examining women’s suspicion and confirmation of new pregnancies, we recruited patients aged 15 – 45 from seven reproductive health and primary health facilities in Arizona, New Jersey, New Mexico, South Carolina, and Texas in 2016–2017. We used multivariable logistic, multinomial logistic, and linear regression models to examine the associations among DAP scores (range: 0 – 4) and contraceptive use outcomes and identify factors associated with discordance between DAP and use of contraception.
Results
Participants with a greater preference to avoid pregnancy had higher odds of contraceptive use (aOR=1.63, 95% CI: 1.31, 2.04) and used contraceptives more consistently (aβ=8.9 percentage points, 95% CI: 5.2, 12.7). Nevertheless, 63% of women with low preference to avoid pregnancy reported using a contraceptive method. Higher preference to avoid pregnancy was not associated with type of contraceptive method used: women with the full range of pregnancy preferences reported using all method types.
Conclusion
When measured using a rigorously developed instrument, pregnancy preferences were associated with contraceptive use and consistency of use. However, our findings challenge assumptions that women with the highest preference against pregnancy use more effective methods and that women who might welcome pregnancy do not use contraception.
Implications
Women’s preferences about pregnancy contribute significantly to their use of contraception. However, health care providers and researchers should consider that contraceptive features besides effectiveness in preventing pregnancy shape contraceptive decision-making and use.
Keywords: pregnancy intention, pregnancy preferences, pregnancy risk, contraceptive use, inconsistency in contraceptive use, United States
Introduction
Determining the contribution of pregnancy “intentions” to contraceptive non-use and unintended pregnancy continues to be one of the more stubborn research challenges in reproductive health [1–3]. Pregnancy intent has been repeatedly found to be associated with fertility and related behavior [4–6]. However, there is little consensus on the strength of the relationship between pregnancy intention and contraceptive behavior and what accounts for discordance, such as contraceptive non-use and inconsistent use among women who report they do not desire pregnancy [7–11].
Research findings are inconsistent. Analyses of the 2002 National Survey of Family Growth (NSFG) found that for women “at risk” for unintended pregnancy – sexually active women aged 15–44 who were not pregnant, not sterilized nor seeking pregnancy – there was no relationship between desire for a baby at any point in the future and contraceptive use [12]. Similarly, analyses of nationally representative data of “at risk” women in the United States aged 18–29 found that neither the importance of avoiding pregnancy nor anticipated feelings if pregnancy were to occur were associated with contraceptive use or method type [3,13]. In contrast, research on a national sample of women aged 18–39, not restricted to “at risk” women, found that only reported importance of avoiding pregnancy was associated with consistent contraceptive use; happiness if pregnancy were to occur was not [14]. Large-scale cohort studies from California, Michigan, and Utah have had mixed results: positive attitudes toward pregnancy were associated with inconsistent contraceptive use [9,11]; strong motivation to avoid pregnancy alone increased the odds of using contraception consistently [10]; and long-acting reversible contraceptive uptake depended on the pregnancy intention measure used [15].
These variations in findings are attributable, in part, to differences in study populations assessed and measures used. Study populations have differed by age and demographics, with some including individuals holding the full ranges of pregnancy intentions, and others restricting to those considered “at risk” of unintended pregnancy or not desiring pregnancy [12,16,17]. Contraceptive outcomes have also varied, with some examining contraceptive use or method type, and others assessing consistency of use, discontinuation, or method switching [3,10,14,18,19]. Studies have operationalized “pregnancy intention” in different ways, including trying to get pregnant, desired number of children, and importance of avoiding pregnancy, and they have utilized diverse measurement approaches (prospective vs. retrospective approaches; categorical or Likert scaled questions) [3,10,11,14,15,18]. Typically, measures have not been 63 formally developed and evaluated nor accounted for the diverse feelings and preferences women may have about a potential pregnancy [20].
In this study, we use a newly developed instrument, the Desire to Avoid Pregnancy scale, to examine the relationship between pregnancy preferences and contraceptive behaviors among reproductive aged women from diverse states [20]. We adopt the term “preferences” instead of “intentions,” in line with the DAP’s theoretic grounding, to acknowledge that individuals often do not have clear intentions, particularly for context-specific outcomes [21]. We assess multiple contraceptive outcomes, including contraceptive use, method type, and consistency of use. We also examine factors associated with discordance between reported pregnancy preferences and contraceptive use. Elucidating how women’s pregnancy preferences affect contraceptive use is critical not only for understanding the underlying factors shaping contraceptive use, but also for guiding appropriate patient-centered contraceptive counseling protocols and clinical care.
Materials and Methods
2.1. Participants and Procedures
In 2016–2017, as part of a study examining how women discover new pregnancies, we recruited participants from seven reproductive health and primary healthcare facilities in Arizona, New Jersey, New Mexico, South Carolina, and Texas. States represented the planned locations of future longitudinal research with the DAP measure. A trained research assistant approached all women in the waiting room, and eligible women (aged 15–45 years, sexually active in the last year, not sterilized, and willing to participate in the anonymous survey) provided verbal informed consent. Ninety-nine percent of women who were screened completed a 30-minute tablet survey on sociodemographic characteristics, relationships, and contraceptive use. Participants who reported that they were not pregnant or did not know whether they were pregnant responded to the pregnancy preferences items. Participants received a $20 gift card for completing the study. The study received approval from the University of California San Francisco Institutional Review Board in July 2015 (IRB #15–16504).
Overall, 810 women enrolled in the study. Among them, 198 reported current pregnancy. Of the remaining 602, 27 were called into their clinical appointment before completing the DAP or were missing more than half of DAP responses for one domain, leaving 575 women with complete DAP scores. Among these, 66 had not had sex with a male within 30 days, leaving 509 women in contraceptive use analyses.
2.2. Measures
The primary outcome was use of any contraceptive method currently or over the last month: long-acting reversible contraception (LARC), including intrauterine devices and the subdermal implant; short-acting reversible contraception (SARC), including oral contraceptive pills, the vaginal ring, transdermal patch, and Depot medroxyprogesterone injection; or male condoms, the only barrier method used by participants. We also examined contraceptive method type used (LARC, SARC, condom, none). We categorized the few participants using more than one method according to the more effective method [22] and the few using withdrawal alone or natural methods as no method. For sensitivity analyses, we also examined a version of the method type variable with separate categories for withdrawal and natural method users and dual method users (using both a LARC or SARC method plus condoms). Finally, we measured consistency of contraceptive use in the prior month by asking respondents to indicate the percentage of acts of sexual intercourse during which contraception was used by selecting a response on a line that ranged from 0 – 100%.
The primary independent variable was pregnancy preferences, measured using the Desire to Avoid Pregnancy (DAP) scale [20]. The DAP scale is the first purposefully developed and evaluated psychometric scale that measures the ranges of women’s preferences regarding a potential future pregnancy. The 14-item scale allows for uncertainty and ambiguity in preferences, captures feelings about both a potential pregnancy (within three months) and child (within a year), and has items covering three domains: desires, emotions, and perceived consequences (Cronbach’s α=0.95). Participants respond to each item on a Likert scale (strongly agree, agree, neither agree nor disagree, disagree, strongly disagree); the scale includes items worded both negatively (a baby would make it harder for me to achieve other things in my life) and positively (thinking about a pregnancy makes me feel excited). Scores are averaged across the items to range from 0 to 4, with 4 indicating higher preference to avoid pregnancy and a lower score indicating greater openness to pregnancy. We also examined quartiles of DAP scores.
Sociodemographic covariables included age (years), self-reported race/ethnicity, parity, relationship status (married/main partner and cohabiting, married/main partner and not cohabiting, not married or having a main partner), education (highest grade completed), receiving public assistance, and state of recruitment. We also included household poverty (below or above 100% Federal Poverty Level [FPL] or missing).
2.3. Analyses
We used bivariable linear regression analysis to assess differences in pregnancy preferences by participant characteristics. Then, we used logistic, multinomial logistic, and linear regression models to examine the associations among pregnancy preferences and any contraceptive use, method type, and consistency of use, respectively, controlling for respondent characteristics. We derived predicted means and percentages from these models. To identify factors associated with discordance between pregnancy preferences and contraceptive use, we used logistic regression models examining contraceptive non-use among women in the highest DAP quartile (DAP Q4; high preference to avoid pregnancy) and contraceptive use among women in the lowest DAP quartile (DAP Q1; low preference to avoid pregnancy). For analyses, we used STATA version 15 (College Station, TX).
3. Results
The 575 participants were on average 27 years old (range: 15–45), and 48% identified as Latina, 27% as black, 16% as white, and 9% as multiracial or other (Table 1). About half were married or had a main partner with whom they lived, and 14% reported no main partner. Thirty-eight percent were nulliparous. Sixty-one percent of participants had completed high school or earned a GED, and 10% had a college degree or more. Forty-three percent of women lived in a household below 100% FPL. Among women who had had sex in the last 30 days, 21% reported not using any contraceptive method, while 17% used LARC, 31% used SARC, and 20% used condoms.
Table 1.
Sociodemographic Characteristics and Contraceptive Use among Participants (N=575)
| Key Variables | N | % |
|---|---|---|
| Age (Range: 15 – 45) | ||
| Mean years (SD) | 27.2 | (7.4) |
| Age Group | ||
| 15 – 24 | 239 | 41.4 |
| 25 – 45 | 336 | 58.6 |
| Race/Ethnicity (N=572) | ||
| Latina | 273 | 47.7 |
| Non-Latina Black | 155 | 27.1 |
| Non-Latina White | 92 | 16.1 |
| Multiracial/other | 52 | 9.1 |
| Relationship Status (N=570) | ||
| Main Partner & Cohabiting | 285 | 50.0 |
| Main Partner & Not Cohabiting | 203 | 35.6 |
| No Main Partner | 82 | 14.4 |
| Parity (N=542) | ||
| 0 | 206 | 38.0 |
| 1 | 116 | 21.4 |
| 2 | 106 | 19.6 |
| 3+ | 114 | 21.0 |
| Education (N=556) | ||
| Less than high school | 83 | 14.9 |
| High school or GED | 341 | 61.3 |
| Some Community College/Tech | 75 | 13.5 |
| College Degree or More | 57 | 10.3 |
| Receives Public Assistance (N=573) | 258 | 45.0 |
| Poverty (N=572) | ||
| Above 100% FPL | 238 | 41.7 |
| Below 100% FPL | 245 | 42.8 |
| Missing | 89 | 15.6 |
| State of Recruitment (N=573) | ||
| Texas | 309 | 53.9 |
| New Mexico/Arizona | 88 | 15.4 |
| South Carolina | 116 | 20.2 |
| New Jersey | 60 | 10.5 |
| Contraceptive Use | ||
| Any Contraceptive Method | 388 | 76.2 |
| Long-acting reversible | 97 | 16.9 |
| Short-acting hormonal | 175 | 30.5 |
| Male condom | 116 | 20.1 |
| No Method | 121 | 21.0 |
| No sex with male in last 30 days | 66 | 11.5 |
| Consistency of Contraceptive Use (N=505) | ||
| Mean percent of sex acts in last 30 days (SD) | 65.9 | (43.6) |
Note: Consistency of contraceptive use is the percentage of acts of sexual intercourse in the last 30 days in which contraception was used among participants who had sex with a male in the last 30 days.
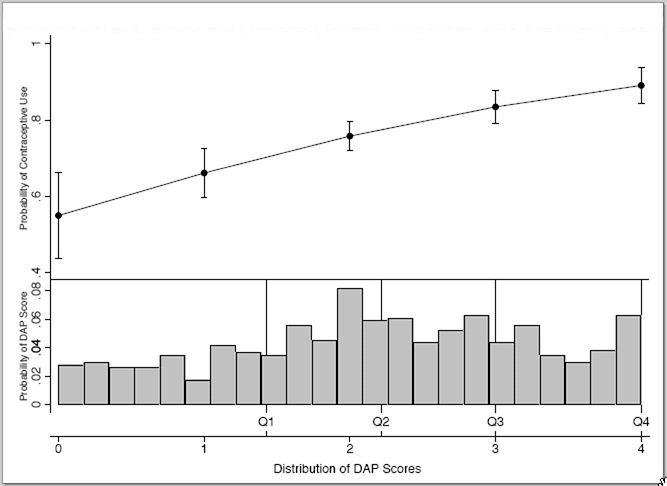
Participants’ DAP scores covered the full range from 0 – 4, with a mean of 2.2 (SD=1.1) (Figure 1). The distribution was slightly left skewed, with the lowest quartile of scores ranging 0 – 1.43 and the highest ranging from 3.01 – 4.00. Compared to participants cohabiting with a main partner (mean DAP: 1.86), those with a main partner but not cohabiting (mean: 2.50; β=0.64, 95% CI: 0.45, 0.82) and those with no main partner (mean: 2.54; β=0.67, 95% CI: 0.43, 0.92) had higher DAP scores (high preference to avoid pregnancy) (Table 2). Women living below 100% FPL had lower DAP scores compared to those living above 100% FPL (means: 2.02 vs. 2.31; β=−0.28, 95% CI: −0.47, −0.10).
Fig. 1.
Distribution of DAP Scores and Predicted Probability of Contraceptive Use by DAP Score.
Table 2.
Desire to Avoid Pregnancy (DAP) Scores by Participant Characteristics and Bivariable Linear Regression Models for DAP Scores
| DAP Score |
Bivariable Models |
|||
|---|---|---|---|---|
| Mean | SD | β | 95% CI | |
| Age (years) (N=575) | – | – | −0.02 | [−0.03, −0.01] |
| Race/Ethnicity (N=572) | ||||
| Latina | 2.16 | 1.03 | Ref. | |
| Non-Latina Black | 2.18 | 1.03 | 0.01 | [−0.20, 0.22] |
| Non-Latina White | 2.29 | 1.20 | 0.13 | [−0.12, 0.38] |
| Multiracial/other | 2.20 | 1.05 | 0.03 | [−0.28, 0.35] |
| Relationship Status (N=570) | ||||
| Main Partner & Cohabiting | 1.86 | 1.03 | Ref. | |
| Main Partner & Not Cohabiting | 2.50 | 1.01 | 0.64 | [0.45, 0.82] |
| No Main Partner | 2.54 | 0.93 | 0.67 | [0.43, 0.92] |
| Parity (N=542) | ||||
| Nulliparous | 2.28 | 1.12 | Ref. | |
| Parous | 2.09 | 1.00 | −0.19 | [−0.37, −0.01] |
| Education (N=556) | ||||
| Less than high school | 2.29 | 1.01 | Ref. | |
| High school or GED | 2.11 | 1.05 | −0.18 | [−0.43, 0.08] |
| Some Community College/Tech | 2.22 | 1.13 | −0.07 | [−0.40, 0.26] |
| College Degree or More | 2.39 | 1.12 | 0.10 | [−0.26, 0.46] |
| Poverty (N=572) | ||||
| Above 100% FPL | 2.31 | 1.10 | Ref. | |
| Below 100% FPL | 2.02 | 1.04 | −0.28 | [−0.47, −0.10] |
| Missing | 2.36 | 0.94 | 0.06 | [−0.20, 0.32] |
| Receives Public Assistance (N=573) | ||||
| No | 2.16 | 1.06 | Ref. | |
| Yes | 2.21 | 1.06 | −0.05 | [−0.23, 0.12] |
| State (N=573) | ||||
| Texas | 2.23 | 1.04 | Ref. | |
| New Mexico/Arizona | 2.02 | 1.18 | −0.20 | [−0.45, 0.05] |
| South Carolina | 2.19 | 1.05 | −0.04 | [−0.26, 0.19] |
| New Jersey | 2.25 | 0.98 | 0.03 | [−0.26, 0.32] |
Desire to avoid pregnancy was strongly associated with use of contraception. The mean DAP score among women not using contraception was 1.75 (SD=1.13) compared to 2.30 (SD=1.03) for women using any method. The odds of contraceptive use increased 64% for each increasing point on the DAP scale (OR=1.64; 95% CI: 1.35–2.00) (Table 3, Figure 1). This relationship was unchanged in the multivariable model (adjusted OR [aOR]=1.63; 95% CI: 1.31–2.04). Results were also unchanged when withdrawal and natural family planning users (n=30) were included as contraceptive users (mean DAP: 1.64 (SD=1.10) for no method vs. 2.29 (SD=1.04) for using contraception (aOR=1.70; 95% CI: 1.33–2.19).
Table 3.
Logistic Regression Models for Any Contraceptive Use among All Sexually Active Women (N = 509)
| Bivariable Model |
Multivariable Model |
|||
|---|---|---|---|---|
| OR | 95% CI | aOR | 95% CI | |
| DAP Score | 1.64 | [1.35, 2.00] | 1.63 | [1.31, 2.04] |
| Age (years) | - | - - | 1.01 | [0.97, 1.05] |
| Race/Ethnicity | ||||
| Latina | - | - - | Ref. | |
| Non-Latina Black | - | - - | 0.59 | [0.26, 1.33] |
| Non-Latina White | - | - - | 0.54 | [0.28, 1.04] |
| Multiracial/other | - | - - | 0.32 | [0.14, 0.69] |
| Relationship Status | ||||
| Main Partner & Cohabiting | - | - - | Ref. | |
| Main Partner & Not Cohabiting | - | - - | 1.40 | [0.80, 2.36] |
| No Main Partner | - | - - | 0.83 | [0.39, 1.78] |
| Nulliparous | - | - - | 1.28 | [0.80, 2.35] |
| Education | ||||
| Less than high school | - | - - | Ref. | |
| High school or GED | - | - - | 0.55 | [0.27, 1.18] |
| Some Community College/Tech | - | - - | 0.80 | [0.33, 2.21] |
| College Degree or More | - | - - | 0.71 | [0.26, 2.08] |
| Poverty | ||||
| Above 100% FPL | - | - - | Ref. | |
| Below 100% FPL | - | - - | 1.29 | [0.78, 2.19] |
| Missing | - | - - | 1.06 | [0.51, 2.23] |
| Receives Public Assistance | - | - - | 1.19 | [0.71, 2.01] |
| State | ||||
| Texas | - | - - | Ref. | |
| New Mexico/Arizona | - | - - | 1.01 | [0.51, 2.00] |
| South Carolina | - | - - | 1.42 | [0.63, 3.20] |
| New Jersey | - | - - | 1.81 | [0.71 4.59] |
Notes: aOR = adjusted Odds Ratio
Among women in the lowest DAP quartile (Q1), the predicted percentage of those using contraception was 63%; this percentage increased with increasing desire to avoid pregnancy: 75% for the second (Q2), 81% for the third (Q3), and 87% for the highest DAP quartile (Q4). For method type, higher DAP score was associated with increased odds of using LARC (aOR=1.73; 95% CI: 1.30, 2.30), SARC (aOR=1.68; 95% CI: 1.30, 2.16), and condoms (aOR=1.55, 95% CI: 1.18, 2.04), vs. no method (Table 4). However, there were no differences in DAP scores among the method types (mean DAP: 2.25 (SD=1.07) for LARC; 2.32 (SD=1.01) for SARC; 2.34 (SD=1.05) for condoms), and women with a broad range of DAP scores (from 0–4) used each method type. When considering the 41 dual method users as a separate group, results were similar (mean DAP: 2.56 (SD=0.93) for dual; 2.20 (SD=1.06) for LARC; 2.27 (SD=1.02) for SARC; 2.35 (SD=1.05) for condoms). Among all sexually active women, a greater desire to avoid pregnancy was also associated with more consistent contraceptive use (adjusted β [aβ]=8.9 percentage points, 95% CI: 5.2, 12.7) (Table 5). However, DAP scores were not significantly associated with contraceptive consistency among SARC and condom users only (aβ =2.2, 95% CI: −1.6, 6.1).
Table 4.
Multivariable Multinomial Logit Model of DAP and Contraceptive Method Use (N = 509)
| LARC vs. None |
SARC vs. None |
Condoms vs. None |
||||
|---|---|---|---|---|---|---|
| aRR | 95% CI | aRR | 95% CI | aRR | 95% CI | |
| DAP Score | 1.73 | [1.30, 2.30] | 1.68 | [1.30, 2.16] | 1.55 | [1.18, 2.04] |
Notes: aRR = adjusted Risk Ratios; No significant differences between method types
Table 5.
Multivariable Linear Regression Models for Consistency of Contraceptive Use
| All Sexually Active Women (N = 509) | Women Using SARC or Condoms (N = 291) | |||
|---|---|---|---|---|
| aβ | 95% CI | aβ | 95% CI | |
| DAP Score | 8.9 | [5.2, 8.9] | 2.2 | [−1.6 6.1] |
| Age (years) | −0.1 | [−0.7, −0.1] | −0.1 | [−0.7, 0.6] |
| Race/Ethnicity | ||||
| Latina | Ref. | Ref. | Ref. | |
| Non-Latina Black | −12.2 | [−26.0, −12.2] | −5.9 | [−18.9, 7.2] |
| Non-Latina White | −8.2 | [−19.8, −8.2] | 2.4 | [−9.9, 14.6] |
| Multiracial/other | −19.6 | [−34.4, −19.6] | −4.4 | [−20.3, 11.5] |
| Relationship Status | ||||
| Main Partner & Cohabiting | Ref. | Ref. | ||
| Main Partner & Not Cohabiting | 3.4 | [−5.8, 12.7] | −1.2 | [−9.9, 7.5] |
| No Main Partner | −7.8 | [−21.2, 5.6] | −7.8 | [−20.6 4.9] |
| Nulliparous | 13.3 | [2.8, 23.8] | 10.8 | [0.7, 20.8] |
| Education | ||||
| Less than high school | Ref. | Ref. | ||
| High school or GED | −2.7 | [−13.7, 8.3] | 3.7 | [−6.2, 13.7] |
| Some Community College/Tech | 4.0 | [−10.9, 18.8] | 7.9 | [−5.5, 21.3] |
| College Degree or More | 6.8 | [−9.7, 23.2] | 13.5 | [−2.1, 29.1] |
| Poverty | ||||
| Above 100% FPL | Ref. | Ref. | ||
| Below 100% FPL | 0.7 | [−8.6, 10.1] | −5.5 | [−14.6, 3.7] |
| Missing | 4.7 | [−8.3, 17.7] | 4.4 | [−7.9, 16.7] |
| Receives Public Assistance | 0.3 | [−9.2, 9.80] | 0.5 | [−8.5, 9.5] |
| State of Residence | ||||
| Texas | Ref. | Ref. | ||
| New Mexico/Arizona | 4.6 | [−7.8, 17.0] | 9.0 | [−3.9, 21.9] |
| South Carolina | 6.4 | [−8.0, 20.8] | 5.2 | [−8.8, 19.1] |
| New Jersey | 9.4 | [−5.8, 24.7] | 6.2 | [−7.8, 20.2] |
Notes: aβ = adjusted β; Consistency of contraceptive use = the percentage of acts of sexual intercourse in the last 30 days in which contraception was used, as reported by the participant.
Despite the strong association between pregnancy preferences and contraceptive use, a predicted 63% of women in the lowest DAP quartile, Q1, nevertheless reported using a contraceptive method, and a predicted 13% of women in the highest DAP quartile, Q4, reported not using a method. Among those in Q1, women living in poverty had higher odds of using contraception (aOR=2.56 vs. not living in poverty, 95% CI: 1.02, 6.41), as did nulliparous women (aOR=3.09 vs. parous women, 95% CI: 1.13, 8.46) (Table 6). For those in Q4, participant characteristics were not significantly associated with contraceptive non-use.
Table 6.
Multivariable Logistic Regression Models for Any Contraceptive Use for Participants in the Lowest Quartile of DAP Scores; N = 138
| aOR | 95% CI | |
|---|---|---|
| Age (years) | 1.00 | [0.94, 1.08] |
| Race/Ethnicity | ||
| Latina | Ref. | |
| Non-Latina Black | 0.26 | [0.05, 1.39] |
| Non-Latina White | 0.68 | [0.20, 2.28] |
| Multiracial/other | 0.05 | [0.01, 0.45] |
| Relationship Status | ||
| Main Partner & Cohabiting | Ref. | |
| Main Partner & Not Cohabiting | 2.40 | [0.83, 6.97] |
| No Main Partner | 0.68 | [0.12, 3.95] |
| Nulliparous | 3.09 | [1.13, 8.46] |
| Education | ||
| Less than high school | Ref. | |
| High school or GED | 0.67 | [0.16, 2.75] |
| Some Community College/Tech | 0.99 | [0.16, 6.31] |
| College Degree or More | 0.57 | [0.09, 3.65] |
| Poverty | ||
| Above 100% FPL | Ref. | |
| Below 100% FPL | 2.56 | [1.02, 6.41] |
| Missing | 4.18 | [0.79, 22.01] |
| State of Residence | ||
| Texas | Ref. | |
| New Mexico/Arizona | 1.12 | [0.32, 3.93] |
| South Carolina | 3.94 | [0.62, 24.90] |
| New Jersey | 6.09 | [0.77, 48.08] |
Notes: aOR = adjusted Odds Ratio; Low DAP Score includes first quartile of DAP Scores and any contraceptive use includes long-acting reversible contraception, short-acting reversible contraception, and condoms.
4. Discussion
In this investigation of pregnancy preferences and contraceptive use, Desire to Avoid Pregnancy score was the factor most strongly associated with both contraceptive use and consistency of use. Pregnancy preferences, however, were not associated with the types of contraceptive methods women used. Interesting discordance between pregnancy preferences and contraceptive use emerged, with 63% of women with the lowest DAP scores nonetheless using contraception. Nulliparous women and those living in poverty were more likely to report contraceptive use while having a low DAP score, demonstrating openness to pregnancy.
Researchers have posited that women who are strongly motivated to prevent pregnancy might use more effective methods, while those more open to the possibility of pregnancy might be satisfied relying on less effective methods [13,19]. Indeed, among 1,000 privately insured women not intending pregnancy, feeling that preventing pregnancy was very important was associated with LARC or SARC use, but not condom use [19], findings also reflected in NSFG data [23]. Our results are consistent with these two studies in terms of finding LARC and SARC users had comparable pregnancy preferences, but they run counter to prior studies for condom users, who, in our study, had similar preferences to avoid pregnancy as those using more effective methods. Our finding of no differences in contraceptive method types used by DAP score – and the broad range of DAP scores among women using each method type – support work indicating that a variety of features, other than effectiveness at preventing pregnancy, drive women’s selection of a contraceptive method [24,25]. Even for women with strong preferences to avoid pregnancy, overemphasizing effectiveness in contraceptive counseling may not lead to contraceptive uptake and satisfaction if other contraceptive features are not addressed [26].
Significant research has documented discrepancies between stated pregnancy intentions and contraceptive behavior, focusing on women who do not intend pregnancy yet are not using contraception or are doing so inconsistently [7,8,10,27]. In this study, a more surprising discordance emerged: while about 13% of women with a high preference to avoid pregnancy reported no use of contraception, nearly two-thirds of those with low preference to avoid pregnancy nevertheless used contraception. This apparent discordance is likely related to the many individual, interpersonal, and contextual factors that contribute to contraceptive decision-making and use [28]. First, women use contraception for reasons other than pregnancy prevention, including other medical reasons and sexually transmitted disease prevention [29]. Second, women may use contraception when they might prefer not to because they feel pressured to by partners, family or providers, or they are unable to have a long-acting device removed [3,30,31]. Nulliparous women and those living in poverty were most likely to use contraception while not preferring to avoid pregnancy, suggesting that such factors might apply more to these women. Notably, the DAP scale is designed to measure how respondents feel about potential pregnancy in the next three months and childbearing within a year; it does not address preferences beyond that timeframe [20]. Some women may want to delay pregnancy but would be open to a pregnancy sooner. Nonetheless, our finding of discordance may help explain prior research that births occurring after contraceptive failure are reported as wanted births [32].
Our finding that over half of women with low DAP scores used contraception points to a potential limitation of guiding contraceptive counseling by pregnancy preferences alone. The Centers for Disease Control and the American College of Obstetricians and Gynecologists endorse universal pregnancy intention screening to identify patients in need of contraceptive care [33,34]. Strategies including One Key Question®, whereby contraceptive and preconception counseling is guided by asking “Would you like to become pregnant in the next year?” are being increasingly implemented in health systems [35]. Reliance on this strategy alone may miss patients who would like to use contraception. To better meet patient needs, contraceptive counseling should allow women to express a range of feelings about pregnancy across different 236 domains of pregnancy preferences and consider each woman’s interest in obtaining contraceptive information [36].
This research has limitations. The study was cross-sectional and assessed contraceptive use over the prior 30 days; it is possible that participants’ pregnancy preferences changed after the time of contraceptive use. Future longitudinal research should examine the relationship between pregnancy preferences and subsequent contraceptive use. The study also relied on participant-reported estimates of consistency of contraceptive use, which may not be uniformly applicable across method types. In addition, restrictions on access to contraceptives could have modified the pregnancy preferences-contraceptive use relationships; however, restricted access is less likely at play because participants were recruited from healthcare settings that provided contraceptive care. Still, results may not be generalizable to women who do not have access to health care. The study also did not account for partners’ preferences, which may modify the relationship between women’s preferences and contraceptive use [3,31]. Strengths of the study include the use of a rigorously developed and evaluated measure of pregnancy preferences in a racially/ethnically and geographically diverse sample.
Women’s multifaceted preferences about pregnancy contribute significantly to their willingness to use contraception. However, women may use contraception despite being open to a possible pregnancy. Healthcare providers and researchers should not assume that pregnancy preferences are the sole motivation for contraceptive use. More likely, the particular circumstances of women’s lives simultaneously shape women’s pregnancy preferences and whether they use contraceptives in accordance with those preferences.
Acknowledgements
We are very grateful to the contributions of Heather Gould and Rana Barar for project direction and Brenly Rowland, Clara Finley Baba, and Jasmine Powell for data collection and study administration. We thank the seven recruitment sites in Arizona, New Jersey, New Mexico, South Carolina, and Texas.
Funding: This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Office of Research on Women’s Health, Building Interdisciplinary Research Careers in Women’s Health grant #2K12 HD052163 and funding from an anonymous private foundation.
Footnotes
Conflict of Interest: The authors report no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J of Med. 2016;374:843–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Mosher W, Jones J, Abma J. Nonuse of contraception among women at risk of unintended pregnancy in the United States. Contraception. 2015;92:170–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Higgins JA, Popkin RA, Santelli JS. Pregnancy ambivalence and contraceptive use among young adults in the United States. Perspectives on sexual and reproductive health. 2012;44:236–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Morgan SP, Rackin H. The Correspondence Between Fertility Intentions and Behavior in the United States. Popul Dev Rev. 2010;36:91–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Bachrach CA, Morgan SP. A cognitive–social model of fertility intentions. Popul Dev Rev. 2013;39:459–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Schoen R, Astone NM, Kim YJ, Nathanson CA, Fields JM. Do fertility intentions affect fertility behavior? J Marriage Fam. 1999:790–9. [Google Scholar]
- [7].Trussell J, Vaughan B, Stanford J. Are all contraceptive failures unintended pregnancies? Evidence from the 1995 National Survey of Family Growth. Fam Plann Perspect. 1999;31:246–60. [PubMed] [Google Scholar]
- [8].Kaye K, Suellentrop K, Sloup C. The fog zone: How misperceptions, magical thinking, and ambivalence put young adults at risk for unplanned pregnancy. The National Campaign to Prevent Teen and Unplanned Pregnancy; Washington, D.C: 2009. [Google Scholar]
- [9].Rocca CH, Hubbard AE, Johnson-Hanks J, Padian NS, Minnis AM. Predictive ability and stability of adolescents’ pregnancy intentions in a predominantly Latino community. Stud Fam Plann. 2010;41:179–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Moreau C, Hall K, Trussell J, Barber J. Effect of prospectively measured pregnancy intentions on the consistency of contraceptive use among young women in Michigan. Hum Reprod. 2013;28:642–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Raine TR, Foster-Rosales A, Upadhyay UD, et al. One-year contraceptive continuation and pregnancy in adolescent girls and women initiating hormonal contraceptives. Obstet Gynecol. 2011;117:363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Wu J, Meldrum S, Dozier A, Stanwood N, Fiscella K. Contraceptive nonuse among US women at risk for unplanned pregnancy. Contraception. 2008;78:284–9. [DOI] [PubMed] [Google Scholar]
- [13].Rocca CH, Harper CC. Do racial and ethnic differences in contraceptive attitudes and knowledge explain disparities in method use? Perspect Sex Reprod Health. 2012;44:150–8. [DOI] [PubMed] [Google Scholar]
- [14].Jones RK. Change and consistency in US women’s pregnancy attitudes and associations with contraceptive use. Contraception. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Geist C, Aiken AR, Sanders JN, et al. Beyond intent: exploring the association of contraceptive choice with questions about Pregnancy Attitudes, Timing and How important is pregnancy prevention (PATH) questions. Contraception. 2019;99:22–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Upson K, Reed SD, Prager SW, Schiff MA. Factors associated with contraceptive nonuse among US women ages 35–44 years at risk of unwanted pregnancy. Contraception. 2010;81:427–34. [DOI] [PubMed] [Google Scholar]
- [17].Masinter LM, Feinglass J, Simon MA. Pregnancy intention and use of contraception among Hispanic women in the United States: data from the National Survey of Family Growth, 2006–2010. J Womens Health. 2013;22:862–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Yoo SH, Guzzo KB, Hayford SR. Understanding the complexity of ambivalence toward pregnancy: does it predict inconsistent use of contraception? Biodemogr Soc Biol. 2014;60:49–66. [DOI] [PubMed] [Google Scholar]
- [19].Weisman CS, Lehman EB, Legro RS, Velott DL, Chuang CH. How do pregnancy intentions affect contraceptive choices when cost is not a factor? A study of privately insured women. Contraception. 2015;92:501–7. [DOI] [PubMed] [Google Scholar]
- [20].Rocca CH, Ralph LJ, Wilson M, Gould H, Foster DG. Psychometric Evaluation of an Instrument to Measure Prospective Pregnancy Preferences: The Desire to Avoid Pregnancy Scale. Medical Care. 2019;57:152–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ní Bhrolcháin M, Beaujouan É. How real are reproductive goals? Uncertainty and the construction of fertility preferences. 2015. [Google Scholar]
- [22].Daniels K, Daugherty J, Jones J, Mosher W. Current Contraceptive Use and VAriation by Selected Characteristics Among Women Aged 15–44: United States, 2011–2013 In: National Center for Health Statistics, editor. National Health Statistics Reports. Atlanta, GA: Center for Disease Control and Prevention; 2015. [PubMed] [Google Scholar]
- [23].Frost JJ, Darroch JE. Factors associated with contraceptive choice and inconsistent method use, United States, 2004. Perspect Sex Reprod Health. 2008;40:94–104. [DOI] [PubMed] [Google Scholar]
- [24].Jackson AV, Karasek D, Dehlendorf C, Foster DG. Racial and ethnic differences in women’s preferences for features of contraceptive methods. Contraception. 2016;93:406–11. [DOI] [PubMed] [Google Scholar]
- [25].Marshall C, Kandahari N, Raine-Bennett T. Exploring young women’s decisional needs for contraceptive method choice: a qualitative study. Contraception. 2018;97:243–8. [DOI] [PubMed] [Google Scholar]
- [26].Lessard LN, Karasek D, Ma S, et al. Contraceptive features preferred by women at high risk of unintended pregnancy. Perspect Sex Reprod Health. 2012;44:194–200. [DOI] [PubMed] [Google Scholar]
- [27].Rocca CH, Doherty I, Padian NS, Hubbard AE, Minnis AM. Pregnancy intentions and teenage pregnancy among Latinas: a mediation analysis. Perspect Sex Reprod Health. 2010;42:186–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Dehlendorf C, Rodriguez MI, Levy K, Borrero S, Steinauer J. Disparities in family planning. Am J Obstet Gynecol. 2010;202:214–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Marshall C, Guendelman S, Mauldon J, Nuru-Jeter A. Young Women’s Contraceptive Decision Making: Do Preferences for Contraceptive Attributes Align with Method Choice? Perspect Sex Reprod Health. 2016;48:119–27. [DOI] [PubMed] [Google Scholar]
- [30].Dehlendorf C, Park SY, Emeremni CA, Comer D, Vincett K, Borrero S. Racial/ethnic disparities in contraceptive use: variation by age and women’s reproductive experiences. Am J Obstet Gynecol. 2014;210:526.e1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Aiken AR, Potter JE. Are Latina women ambivalent about pregnancies they are trying to prevent? Evidence from the Border Contraceptive Access Study. Perspectives on sexual and reproductive health. 2013;45:196–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Curtis S, Evens E, Sambisa W. Contraceptive discontinuation and unintended pregnancy: an imperfect relationship. Int Perspect Sex Reprod Health. 2011;37:58–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Johnson K, Posner SF, Biermann J, et al. Recommendations to Improve Preconception Health and Health Care—United States: Report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. 2006;55:1–CE-4. [PubMed] [Google Scholar]
- [34].American College of Obstetricians and Gynecologists, Committee on Health Care for Underserved Women. Committee Opinion No. 654: Reproductive Life Planning to Reduce Unintended Pregnancy. Obstet Gynecol. 2016;127:e66. [DOI] [PubMed] [Google Scholar]
- [35].Bellanca HK, Hunter MS. ONE KEY QUESTION(R): Preventive reproductive health is part of high quality primary care. Contraception. 2013;88:3–6. [DOI] [PubMed] [Google Scholar]
- [36].Callegari LS, Aiken AR, Dehlendorf C, Cason P, Borrero S. Addressing potential pitfalls of reproductive life planning with patient-centered counseling. Am J Obstet Gynecol. 2017;216:129–34. [DOI] [PubMed] [Google Scholar]