The authors performed a retrospective analysis of the prospectively maintained Endovascular Treatment of Ischemic Stroke multicentric registry. Data from consecutive patients who benefited from thrombectomy with a first-line Sofia approach between January 2013 and April 2018 were studied. We excluded other first-line approaches (stent retriever or combined aspiration and stent retriever) and extracranial occlusions. During the study period, 296 patients were treated. Mean age and initial NIHSS score were, respectively, 69.5 years and 16. Successful reperfusion, defined by the modified TICI 2b/3, was obtained in 86.1%. Complete reperfusion (modified TICI 3) was obtained in 41.2%. A first-pass effect was achieved in 24.2%. A rescue stent retriever approach was required in 29.7%. The first-line contact aspiration approach appeared safe and efficient with Sofia catheters. These devices achieved very high reperfusion rates with a low requirement for stent retriever rescue therapy, especially for M1 occlusions.
Abstract
BACKGROUND AND PURPOSE:
After publications on the effectiveness of mechanical thrombectomy by stent retrievers in acute ischemic stroke with large-vessel occlusion, alternative endovascular approaches have been proposed using first-line aspiration catheters. Several devices are currently available to perform A Direct Aspiration First Pass Technique. The Sofia catheter aspiration has been widely used by interventionalists, but data are scarce about its efficacy and safety. Our aim was to report our multicenter thrombectomy experience with first-line Sofia catheter aspiration and to identify independent prognostic factors of clinical and procedural outcomes.
MATERIALS AND METHODS:
We performed a retrospective analysis of the prospectively maintained Endovascular Treatment of Ischemic Stroke multicentric registry. Data from consecutive patients who benefited from thrombectomy with a first-line Sofia approach between January 2013 and April 2018 were studied. We excluded other first-line approaches (stent retriever or combined aspiration and stent retriever) and extracranial occlusions. Baseline characteristics, procedural data, and angiographic and clinical outcomes were analyzed.
RESULTS:
During the study period, 296 patients were treated. Mean age and initial NIHSS score were, respectively, 69.5 years and 16. Successful reperfusion, defined by the modified TICI 2b/3, was obtained in 86.1% (n = 255; 95% CI, 81.7%–89.9%). Complete reperfusion (modified TICI 3) was obtained in 41.2% (n = 122; 95% CI, 35.5%–47.1%). A first-pass effect was achieved in 24.2% (n = 71; 95% CI, 19.4%–29.6%). A rescue stent retriever approach was required in 29.7% (n = 88; 95% CI, 24.6%–35.3%). The complication rate was 9.5% (n = 28; 95% CI, 6.4%–13.5%). Forty-three percent (n = 122; 95% CI, 37.1%–48.9%) of patients presented with a favorable 3-month outcome (mRS ≤ 2). Older age, M1-occlusion topography, and intravenous thrombolysis use prior to thrombectomy were independent predictors of the first-pass effect.
CONCLUSIONS:
The first-line contact aspiration approach appeared safe and efficient with Sofia catheters. These devices achieved very high reperfusion rates with a low requirement for stent retriever rescue therapy, especially for M1 occlusions.
After publication of the major trials reporting the efficacy of mechanical thrombectomy for large-vessel occlusion strokes,1 the principal concern is now to optimize recanalization rates. Recent advances in thrombectomy devices progressively enabled major improvement. In addition to stent retrievers, contact aspiration has greatly modified the endovascular approach and is now considered a routine technique. Since the A Direct Aspiration First Pass Technique (ADAPT) was described,2,3 various distal aspiration catheter (DAC) technologies have been developed. ADAPT consists of contact thrombus suction through a large-diameter catheter. This is a seductive first-line approach because it appears effective, safe, fast, and cost-effective.4 With recent publications of the Contact Aspiration Versus Stent Retriever for Successful Revascularization (ASTER) and Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS) trials, ADAPT can now be considered a first-line option in the thrombectomy strategy.5,6 In case of aspiration failure, the endovascular technique can then be converted to a combined aspiration + stent retriever approach.7 These DACs must have specific characteristics such as navigability, torqueability, visibility, kink resistance, and aspiration capacity to obtain higher performance levels.
Sofia (soft torqueable catheter optimized for intracranial access; MicroVention, Tustin, California) is a DAC with a specific hybrid design. Its braid and coil construction combines different softness segments with a distal inner lumen of 0.055–0.070 inches, respectively, in 5F and 6F Plus versions. Despite previous publications,8–11 the safety and efficacy of this DAC in a large population with first-line Sofia use are yet to be reported.
Recanalization is a strong predictor of favorable outcome. Especially, the recently described first-pass effect (FPE), defined as a complete recanalization after 1 pass of mechanical thrombectomy, has been related to substantial improvement in clinical outcome compared with final good recanalization results after numerous passes.12 However, in the North American Solitaire Stent-Retriever Acute Stroke registry study,12 most patients were treated with a first-line stent retriever strategy. Data regarding the FPE under the ADAPT strategy are still undereported to date.
We present here the largest multicentric experience to date of the first-line ADAPT strategy using Sofia 6F Plus or 5F catheters. We aimed to study the clinical and angiographic effectiveness with specific attention to predictive factors of the first-pass effect.
Materials and Methods
Study Design and Population
We performed a retrospective analysis of our prospectively maintained, multicentric Endovascular Treatment of Ischemic Stroke (ETIS) data base. ETIS is a prospective registry collecting data from patients benefiting from mechanical thrombectomy in 4 major French comprehensive stroke centers. Local ethics committees approved this study.
Consecutive patients from January 2013 to April 2018, presenting with acute ischemic stroke due to large-vessel occlusion strokes of the anterior or posterior circulation treated by mechanical thrombectomy using first-line ADAPT with a Sofia catheter were analyzed. We excluded patients treated first-line by another DAC, stent retrievers combined with distal aspiration, or stent retrievers alone. Extracranial occlusions were also excluded.
Treatment Protocol
The indication for treatment was left to the discretion of each operator according to local protocol. Intravenous thrombolysis treatment (IVT) was administered in association with mechanical thrombectomy in patients treated within 4.5 hours of stroke onset in the absence of contraindications. Endovascular treatment was performed with the patient under local anesthesia alone, conscious sedation, or general anesthesia depending on the patient's condition and each contributing center's anesthesia protocol.
For all selected cases, the operator's decision was to perform distal aspiration through a Sofia catheter as the first intention. Sofia catheter choice was made according to operator's discretion, local protocols, catheter availability, and occlusion topography to fit with the ADAPT strategy as a first-line treatment option. First, an 8F or 9F guide catheter was placed into the cervical internal carotid artery. Then, a Sofia 6F Plus or 5F was advanced over a microwire to the occlusion site with or without microcatheter support, depending on cervical and intracranial ICA tortuosity. The use of a balloon-guide catheter was left to the interventionist's discretion. A 3-minute aspiration period, using either a dedicated pump or manual depression through a vacuum syringe, was applied before DAC removal. In the case of failure or partial efficacy, this maneuver could be repeated. In case of ADAPT failure or insufficient recanalization, the choice to convert to another endovascular technique (distal aspiration combined with stent retrievers or stent retrievers alone) was left to the operator's discretion. Complementary endovascular treatments, such as cervical or intracranial angioplasty and/or stent placement, were performed depending on stroke etiology and severity and angiographically detected underlying lesions.
Data Collection and Outcome Evaluation
Age, sex, medical history, previous medication, stroke severity using the NIHSS score, stroke etiology, imaging technique, ASPECTS, IVT, and angiographic (arterial occlusion topography, degree of revascularization assessed by the modified TICI [mTICI] score) data were recorded.
Clinical outcome was assessed by the mRS 3 months after stroke. Favorable outcome was defined by an mRS ≤2. Angiographic reperfusion was rated using the mTICI score. Successful revascularization was defined by mTICI ≥2b. Near-complete and excellent reperfusion was defined, respectively, by mTICI of 2c/3 and 3. The FPE was defined as an mTICI 3 after a single aspiration maneuver.
Safety criteria were also recorded, including procedural complications (dissection, embolism in a new territory, and intracranial arterial perforation), intracranial hemorrhage, and mortality. Procedural times were analyzed.
Statistical Analysis
Categoric variables were expressed as frequencies and percentages. Quantitative variables were expressed as means or medians (interquartile range, [IQR]) for non-normal distribution. The normality of distributions was assessed graphically and using the Shapiro-Wilk test.
Associations of baseline characteristics (patient and treatment characteristics) with outcomes (favorable outcome, successful and excellent reperfusion, FPE) were first investigated in center-adjusted analyses using generalized linear mixed models by including center as a random effect. To assess the independent predictors of each outcome, we entered all patient and treatment characteristics with a P < .20 in center-adjusted analyses into a backward-stepwise multivariable generalized linear mixed model using a removal criterion of P > .05. Before developing the multivariable prognostic models, we examined the log-linearity assumption for continuous characteristics using restricted cubic spline functions as well as the absence of collinearity between candidate predictors by calculating the variance inflation factors. To avoid case deletion in analyses due to missing data on baseline characteristics and outcomes, we imputed missing data by multiple imputations using a regression-switching approach (chained equations with m = 10). The imputation procedure was performed under the missing at random assumption using all baseline characteristics and study outcomes with a predictive mean matching method for continuous variables and a multinomial or binary logistic regression model for categoric variables. Estimates obtained in the different imputed datasets were combined using the Rubin rules. Finally, we examined the performance of the final prognostic models in terms of discrimination by calculating the C-statistics in each imputed dataset and by reporting the median and range values.
Statistical testing was performed at the 2-tailed α level of .05. Data were analyzed using the SAS software package, Release 9.4 (SAS Institute, Cary, North Carolina).
Results
Population and Participating Centers
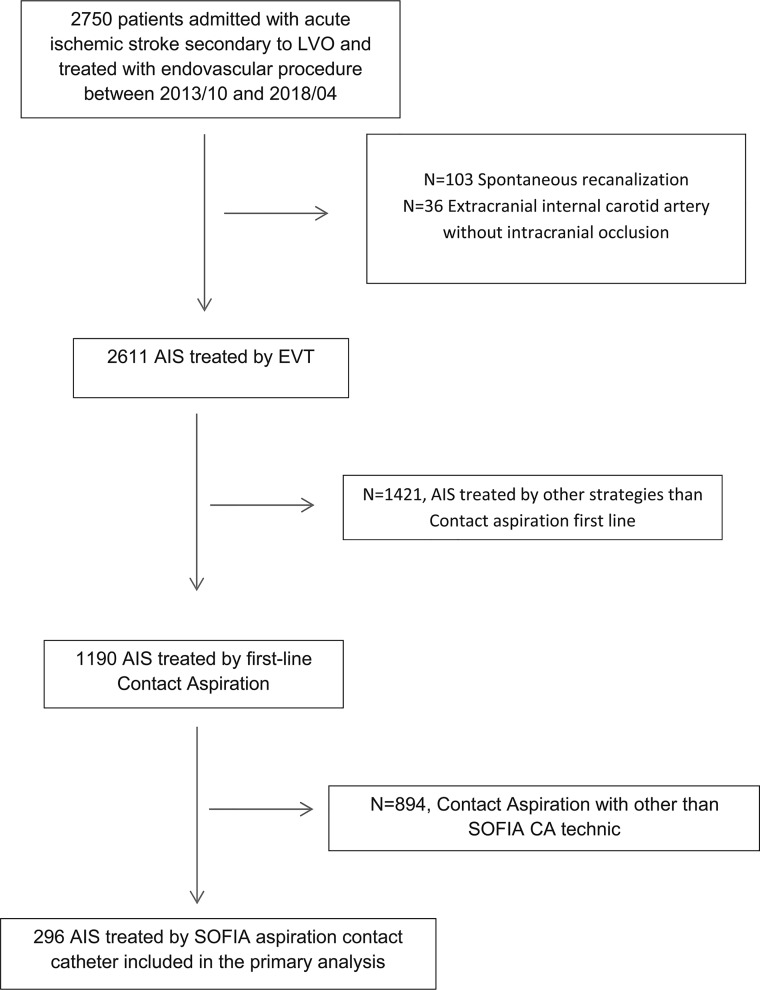
From October 2013 to April 2018, we treated 2750 patients with an arterial large-vessel occlusion by mechanical thrombectomy at 4 comprehensive stroke centers. Of these, 296 (10.8%) who had undergone endovascular treatment with the Sofia aspiration catheter as a first-line approach were included in the present study (center A: 73 patients; B: 103 patients, C: 92 patients, D: 28 patients) (Figure).
FIGURE.
Flowchart of the Sofia-Contact Aspiration, First-Line Technique Registry. AIS indicates acute ischemic stroke; LVO, large vessel occlusion; EVT, endovascular treatment; CA, contact aspiration.
The main patient and treatment characteristics are reported in Table 1. Overall, the mean age was 69.5 ± 13.8 years; 50.7% (n = 150) were men, and the median admission NIHSS score was 16 (IQR, 11–21). Intravenous tPA before endovascular treatment was administered in 48.3% (n = 142) of patients. The median time from symptom onset to arterial puncture was 242 minutes (IQR, 186–324 minutes). Most patients were treated with a 6F Sofia catheter (n = 226, 76.3%), and the remaining 70 (23.7%) were treated with a 5F catheter.
Table 1:
Baseline characteristics (n = 296)a
| Characteristics | No. | Values |
|---|---|---|
| Baseline demographics and medical history | ||
| Age (mean) (yr) | 296 | 69.5 ± 13.8 |
| Men | 296 | 150 (50.7) |
| Hypertension | 288 | 158 (54.9) |
| Diabetes | 285 | 50 (17.4) |
| Dyslipidemia | 284 | 93 (32.7) |
| Current smoking | 272 | 70 (25.7) |
| Previous stroke or TIA | 286 | 43 (15.0) |
| Previous CAD | 285 | 50 (17.5) |
| Antithrombotic medications | 291 | 120 (41.2) |
| Antiplatelet | 291 | 69 (23.7) |
| Anticoagulant | 291 | 34 (11.7) |
| Current stroke event | ||
| Systolic BP (mean) (mm Hg) | 245 | 148 ± 28 |
| Diastolic BP (mean) (mm Hg) | 245 | 82 ± 19 |
| Blood glucose (median) (IQR) (mmol/L) | 229 | 6.4 (5.7–8.0) |
| Admission NIHSS score (median) (IQR) | 290 | 16 (11–21) |
| ASPECTS (median) (IQR) | 278 | 7 (6–9) |
| Prestroke mRS ≥1 | 291 | 64 (22.0) |
| Site of occlusion | ||
| M1 MCA | 296 | 124 (41.9) |
| M2 MCA | 40 (13.5) | |
| T-car | 54 (18.2) | |
| Tandem | 39 (13.2) | |
| Vertebrobasilar | 39 (13.2) | |
| Stroke etiology | ||
| Large-artery atherosclerosis | 295 | 44 (14.9) |
| Cardioembolic | 127 (43.1) | |
| Dissection | 11 (3.7) | |
| Others | 113 (38.3) | |
| Intravenous rtPA | 294 | 142 (48.3) |
| General anesthesia | 291 | 71 (24.4) |
| Procedural times (median) (IQR) (min) | ||
| Onset to imaging | 279 | 113 (84–180) |
| Admission to imaging | 248 | 25 (16–41.5) |
| Imaging to groin puncture | 262 | 107 (69–151) |
| Imaging to recanalization | 279 | 157 (118–205) |
| Onset to puncture | 276 | 242 (186–324) |
| Puncture to recanalization | 287 | 40 (25–65.5) |
| Balloon-guide catheter | 296 | 23 (7.8) |
| Mode of admission | ||
| Mothership | 295 | 121 (41.0) |
| Drip and ship | 174 (59.0) | |
| Sofia catheter | ||
| 5F | 296 | 70 (23.7) |
| 6F | 226 (76.3) |
Note:—BP indicates blood pressure; CAD, coronary artery disease; T-car, occlusion of carotid terminus; Mothership, comprehensive stroke centers with on-site interventional neuroradiologic services; Drip and ship, medical treatment (including intravenous thrombolysis) in a hospital before being transferred to a comprehensive stroke centers for thrombectomy.
Values are expressed as No. (percentage) unless otherwise indicated.
Effectiveness and Safety Outcomes
The main safety and effectiveness outcomes are summarized in Table 2. Thrombectomy was effective in 86.1% (n = 255; 95% CI, 81.7%–89.9%) of patients (successful reperfusion, mTICI 2b–3) with a median number of passes of 2 (IQR, 1–3) and a median time of 40 minutes (IQR, 24–65 minutes) from groin puncture. Excellent reperfusion (mTICI 3) was achieved in 41.2% of patients (n = 122; 95% CI, 35.5%–47.1%). The first-pass effect was achieved in 24.2% (n = 71, 95% CI, 19.4–29.6%). Rescue therapy was required in 29.7% (n = 88; 95% CI, 24.6%–35.3%).
Table 2:
Efficacy and safety outcomes in the overall population and population without rescue therapy (n = 296)a
| Outcomes | Overall |
Patients without Rescue Therapy |
||
|---|---|---|---|---|
| Values | 95% CI | Values | 95% CI | |
| Efficacy outcomes | ||||
| Successful reperfusion (mTICI 2b/3) | 255/296 (86.1) | 81.7–89.9 | 191/208 (91.8) | 87.2–95.2 |
| Near-complete reperfusion (mTICI 2c/3) | 157/296 (53.0) | 47.4–58.7 | 128/208 (61.5) | 54.6–68.2 |
| Excellent reperfusion (mTICI 3) | 122/296 (41.2) | 35.5–47.1 | 104/208 (50.0) | 43.0–57.0 |
| FPE (mTICI 3 after first pass) | 71/293 (24.2) | 19.4–29.6 | 71/208 (34.1) | 27.7–41.0 |
| Early neurologic improvementb | 133/258 (51.6) | 45.4–57.7 | 109/184 (59.2) | 51.8–66.4 |
| Favorable outcome | 122/284 (43.0) | 37.1–48.9 | 100/198 (50.5) | 43.3–57.7 |
| Groin puncture-to-recanalization time (median) (IQR) | 40 (24–65)c | 30.0 (21.0–50.0)d | ||
| No. of passes >2 | 117/293 (39.9) | 34.3–45.8 | 46/208 (22.1) | 16.7–28.4 |
| Rescue therapy | 88/296 (29.7) | 24.6–35.3 | ||
| Safety outcomes | ||||
| Procedural complications | 28/294 (9.5) | 6.4–13.5 | 19/208 (9.1) | 5.6–13.9 |
| Any ICH | 115/258 (44.6) | 38.4–50.9 | 79/177 (44.6) | 37.2–52.3 |
| PH | 31/258 (12.0) | 8.3–16.6 | 22/177 (12.4) | 8.0–18.2 |
| sICH | 16/258 (6.2) | 3.5–9.8 | 10/177 (5.6) | 2.7–10.1 |
| All-cause death (90-day) | 65/284 (22.9) | 18.1–28.2 | 40/198 (20.2) | 14.8–26.5 |
Note:—ICH indicates intracranial hemorrhage; sICH, symptomatic intracranial hemorrhage.
Values expressed as No./total No. (%) unless otherwise indicated.
Early neurologic improvement is defined as NIHSS score 0–1 at 24 hours or a decrease of ≥4 points in the NIHSS score at 24 hours. Favorable outcome is defined as a 90-day mRS ≤ 2.
Twenty-six missing data.
Fourteen missing data.
Procedural complications occurred in 9.5% (n = 28; 95% CI, 6.4%–13.5%) of patients. These included 14 (4.7%) new-territory embolisms, 4 (1.4%) vessel perforations, 4 (1.4%) extracranial carotid dissections, and 6 (2.0%) vasospasms. Intracranial hemorrhage within 24 hours occurred in 44.6% (n = 115; 95% CI, 38.4%–50.9%). Among these, there were 31 (12.0%) parenchymal hematomas (PH-1 and PH-2) and 16 (6.2%) symptomatic intracranial hemorrhages. At 90 days, 43% of patients (n = 122; 95% CI, 37.1%–48.9%) were functionally independent (mRS 0–2) and 22.9% had died (n = 65; 95% CI, 18.1%–28.2%) (See the On-line Figure for the overall distribution of 90-day mRS). Results according to anterior or posterior occlusion topography are presented in On-line Tables 1 and 2.
Among patients treated with the ADAPT approach alone without the need for rescue therapy, successful reperfusion was obtained in 91.8% (n = 191; 95% CI, 87.2%–95.2%); 50.5% (n = 100; 95% CI, 43.3%–57.7%) had a 90-day favorable outcome. In this subgroup of patients, the mortality rate was 20.2% (n = 40; 95% CI, 14.8%–26.5%) and the procedural complication rate was 9.1% (n = 19; 95% CI, 5.6%–13.9%). These results are presented in Table 2.
Predictors of 90-Day Favorable Outcome
Center-adjusted analyses of predictors of favorable outcome are detailed in On-line Table 3. In backward stepwise multivariable regression analysis, age, admission NIHSS score, hypertension, time intervals between onset to imaging and imaging to groin puncture, prestroke mRS≥1, general anesthesia, and non-M1 MCA occlusion were associated with a decrease in the favorable outcome rate, whereas intravenous thrombolysis was associated with an increase (Table 3). This prognosis model had good discrimination (median C-statistic, 0.827; range, 0.816–0.838 across imputed datasets).
Table 3:
Independent predictors of favorable outcome; successful, excellent reperfusion; and first-pass effecta
| OR (95%CI) | P Valueb | |
|---|---|---|
| Favorable outcome | ||
| Age | 0.72 (0.58–0.91)b | .005 |
| Admission NIHSS score | 0.86 (0.81–0.91)c | <.001 |
| Prestroke mRS ≥1 | 0.37 (0.17–0.78) | .009 |
| Intravenous rtPA | 2.61 (1.42–4.78) | .002 |
| Site of occlusion | .026 | |
| M1 MCA | 1.00 (ref) | |
| M2 MCA | 0.81 (0.31–2.09) | .66 |
| T-car | 0.65 (0.30–1.41) | .27 |
| Tandem | 0.49 (0.21–1.14) | .098 |
| Vertebrobasilar | 0.15 (0.05–0.49) | .002 |
| General anesthesia | 0.36 (0.17–0.76) | .008 |
| Procedural time (min) | ||
| Onset to imaging | 0.87 (0.77–0.97)d | .017 |
| Imaging to groin puncture | 0.67 (0.52–0.90)d | .007 |
| Successful reperfusion | ||
| Current smoking | 0.36 (0.18–0.72) | .004 |
| ASPECTS | 1.25 (1.08–1.45)c | .003 |
| Excellent reperfusion | ||
| Age | 1.26 (1.04–1.54) | .018 |
| Antiplatelet drugs | 2.31 (1.24–4.32) | .009 |
| Blood glucose (mmol/L) | 0.87 (0.77–0.97) | .012 |
| Site of occlusion | <.001 | |
| M1 MCA | 1.00 (ref) | |
| M2 MCA | 0.86 (0.35–2.14) | .75 |
| T-car | 0.38 (0.18–0.79) | .010 |
| Tandem | 0.38 (0.16–0.91) | .030 |
| Vertebrobasilar | 2.55 (1.11–5.85) | .027 |
| Sofia catheter | ||
| >5F | 0.38 (0.17–0.83) | .015 |
| >6F | 1.00 (ref) | |
| First-pass effect | ||
| Age | 1.48 (1.16–1.90) | .002 |
| Site of occlusion | <.001 | |
| M1 MCA | 1.00 (ref) | |
| M2 MCA | 0.75 (0.32–1.75) | |
| T-car | 0.11 (0.03–0.38) | |
| Tandem | 0.13 (0.03–0.60) | |
| Vertebrobasilar | 2.46 (1.07–5.75) | |
| Intravenous rtPA | 2.01 (1.09–3.71) | .024 |
Note:—ref indicates reference; T-Car, occlusion of carotid terminus.
Factors included in multivariate analysis of favorable outcome: age, hta, previous stroke or TIA, systolic BP, admission NIHSS score and ASPECTS, prestroke mRS ≥1, intravenous rtPA, general anesthesia, delay in imaging-to-groin puncture, site of occlusion, and the Sofia catheter. Factors included in multivariate model of successful reperfusion: age, current smoking, admission ASPECTS, site of occlusion, intravenous rtPA, etiology, delay in onset to imaging. Factors included in multivariate analysis of excellent reperfusion: age, sex, current smoking, antiplatelet use, glycemia, admission ASPECTS, site of occlusion, intravenous rtPA, and the Sofia catheter. Factors included in multivariate analysis of first-pass effect: age, current smoking, previous stroke or TIA, antiplatelet use, glycemia, admission NIHSS score and ASPECTS, prestroke mRS ≥1, site of occlusion. and intravenous rtPA.
Per 10-year increase.
Per 1-point increase.
Per 1-hour increase.
Predictors of Successful and Complete Reperfusion
Center-adjusted analyses of predictors of successful and excellent reperfusion outcome are detailed in On-line Tables 4 and 5. A higher ASPECTS (OR per 1-point increase, 1.25; 95% CI, 1.08–1.45) and no current smoking (OR, 0.36; 95% CI, 0.18–0.72) were independently associated with successful reperfusion in backward stepwise multivariate regression analysis (Table 3). This prognosis model had good discrimination (median C-statistic, 0.681; range, 0.672–0.688 across imputed datasets).
For excellent reperfusion, we identified 5 independent predictors: older age, previous antiplatelet medications, lower blood glucose, site of occlusion (with a greater rate of excellent reperfusion for MCA M1 and vertebrobasilar occlusions), and Sofia 6F catheters (Table 3). This prognosis model also had good discrimination (median C-statistic, 0.735; range, 0.725–0.741 across imputed datasets).
Predictors of First-Pass Effect (mTICI 3 after 1 Pass)
Center-adjusted analyses of predictors of FPE are detailed in On-line Table 6. We identified 3 independent predictors: older age, site of occlusion (with a greater rate of excellent reperfusion after 1 pass for MCA M1 and verterbobasilar occlusions), and intravenous thrombolysis (Table 3). This prognosis model also showed good discrimination (median C-statistic, 0.795; range, 0.793–0.795 across imputed datasets).
Discussion
Our study demonstrated a very high efficacy of first-line contact aspiration using the Sofia catheter with 86.1% successful reperfusion (mTICI 2b, 2c/3) and 43% favorable clinical outcome (mRS <3). The FPE rate was high (24.2%). Factors associated with higher recanalization rates were, notably, M1 and vertebrobasilar occlusions and the use of a 6F catheter.
Clinical Outcomes
As previously described,1,13 outcome was significantly negatively influenced by age, stroke severity assessed by admission NIHSS score, prestroke mRS ≥1, general anesthesia, ICA terminus and tandem occlusions, and late treatment timeframe. Most interesting, IVT in combination with mechanical thrombectomy is associated with favorable outcome. These predictive factors have already been previously demonstrated with the use of either stent retrievers or the ADAPT technique.
The influence of general anesthesia on clinical outcomes is currently under debate.14 In our study, general anesthesia was not the first-line option for thrombectomy procedures among most participating centers. This anesthesia regimen was proposed for selected severe cases, thus likely explaining the association between general anesthesia and poorer outcomes in our work.
Despite several studies demonstrating the association between IVT and favorable outcome in cases of stroke treated with thrombectomy,15 IVT influence is still discussed. Future randomized trials will probably bring answers.
Angiographic Outcome
We present here the largest population treated with first-line ADAPT using Sofia catheters. Our final rate of favorable mTICI (≥2b) appears similar to those previously published because authors noted favorable recanalization rates between 86.9% and 94.1% with the Sofia catheter.8–11 Gory et al16 reported 89% of mTICI 2b/3 in a meta-analysis of the overall literature dealing with ADAPT using various kinds of DACs. In comparison, reperfusion rates among ADAPT major trails were 92% and 85.4%, respectively, in the COMPASS and ASTER trials. Our results are consistent with these values.
Considering all types of mechanical thrombectomy approaches, these rates are among the best reported. For example, considering stent retrievers for most cases, the Highly Effective Reperfusion Evaluated in Multiple Endovascular Stroke (HERMES) trial meta-analysis revealed 71% successful reperfusion (mTICI 2b/3).1 Among the stent retriever subgroups of both the COMPASS and ASTER trials, final successful recanalization rates were, respectively, 89% and 83.1%. Of course, the maximalist strategy combining contact aspiration and stent retriever is currently presented as a promising technique. Previous studies reported a rate of 72.4% with the Aspiration-Retriever Technique for Stroke (ARTS) approach.17 New approaches such as Proximal Balloon Occlusion Together with Direct Thrombus Aspiration during Stent Retriever Thrombectomy (PROTECTPlus)18 and Stent Retriever Assisted Vacuum-Locked Extraction (SAVE) techniques19 seem to achieve very high revascularization levels. However, these findings can be balanced with the advantages of ADAPT as a first-line approach: ease of use, high effectiveness, and cost-effectiveness.
High-quality revascularization (mTICI 2c/3) is now considered a strong prognostic factor.20 We found that Sofia distal aspiration alone could achieve mTICI 2c/3 and mTICI 3 results in 53% and 41.2%. These rates are—as other indicators previously reported here—close to recently published data.5,21
In our study, rescue therapy using a stent retriever was required in 29.7%. This was a low rate, enhancing the high-efficacy level of aspiration first-pass alone in our experience. In the comparable current literature, rescue therapy after the ADAPT technique was needed in 31%–40%.6,16,22–24 Lower rescue therapy rates have been published with stent retrievers.25 However, this has to be questioned because the stent retriever approaches are often already associated with an intermediate catheter able to perform combined aspiration and thus can be seen as a maximalist strategy. Nevertheless, the probable need of a complementary rescue technique seems low.
Most interesting, we also emphasized a higher excellent reperfusion rate (mTICI 3) with a Sofia 6F than Sofia 5F. This strongly suggested a need for the largest diameter DAC possible to reach higher rates of reperfusion. This confirms previously published data.24,26,27
Our complication rate is low and in accordance with earlier reports. Moreover, the complication rate included benign events such as vasospasm. In the ASTER trial,6 the first-line contact aspiration group had a 16.2% complication rate, and the first-line stent retriever ASTER group had a 15.9% complication rate (nonsignificant difference). Blanc et al22 also reported a 13.3% rate.
First-Pass Effect
The FPE has recently been described as a strong prognostic factor of favorable outcome. Zaidat et al12 reported an FPE rate of 25.1% using stent retrievers exclusively. We report here an FPE rate of 24.2%. M1 and vertebrobasilar occlusions were significant predictors of FPE. These topographies appear to particularly fit with the first-line ADAPT strategy using the Sofia catheter. Predictors of FPE were also older age and intravenous thrombolysis. Zaidat et al found that older age was also associated with the FPE but only in univariate analysis. Most interesting, we found that IVT was 1 remarkable factor associated with a higher prevalence of FPE. This has not been described to date, to our knowledge. In our study, the use of a balloon-guide catheter was not significantly associated with FPE, but this could be explained by the rare use of balloon-guide catheters in our population.
Recent publications reported very high rates of FPE.18,19 Once again, considering our results and literature data, the ADAPT approach, especially with large-bore catheters, has to be considered a reliable front-line technique. In particular, M1 and basilar occlusions are very favorable targets, as demonstrated here.
Limitations
One limitation of this study is its retrospective nature, which also limits the possibility of harmonizing endovascular procedures among different operators. This can constitute a bias in perioperative data analysis. Nevertheless, this point makes our results very likely to be representative of daily practice in different thrombectomy centers. The absence of core lab analysis might also constitute a limitation. Other potential limitations include differences in study-entry criteria and patient characteristics among the centers that may be a source of bias.
Conclusions
The Sofia catheter is an efficient thrombectomy tool, with a good efficacy and safety profile. We demonstrated very high reperfusion rates (mTICI 2b/3 and FPE) with a first-line thrombectomy strategy using Sofia catheters. Further trials comparing different catheters may be useful to appreciate the efficacy and safety differences between these devices.
ABBREVIATIONS:
- ADAPT
A Direct Aspiration First Pass Technique
- DAC
distal aspiration catheter
- ETIS
Endovascular Treatment of Ischemic Stroke
- FPE
first-pass effect
- IQR
interquartile range
- IVT
intravenous thrombolysis
- mTICI
modified TICI
- PH
parenchymal hematoma
Footnotes
Disclosures: Bertrand Lapergue—UNRELATED: Consultancy: Stryker; Grants/Grants Pending: research grant from MicroVention for supporting the ETIS Network, research grant for the ASTER 2 trial from Stryker, MicroVention, Penumbra*; Payment for Lectures Including Service on Speakers Bureaus: Bristol-Myers Squibb, Servier, Boehringer Ingelheim. Xavier Barreau—RELATED: Grant: Bordeaux University Hospital Neuroradiology Unit.* *Money paid to the institution.
Financial support was provided by MicroVention (Tustin, California).
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
REFERENCES
- 1. Goyal M, Menon BK, Van Zwam WH, et al. ; HERMES collaborators. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016;387:1723–31 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- 2. Turk AS, Spiotta A, Frei D, et al. . Initial clinical experience with the ADAPT technique: a direct aspiration first pass technique for stroke thrombectomy. J Neurointerv Surg 2014;6:231–37 10.1136/neurintsurg-2013-010713 [DOI] [PubMed] [Google Scholar]
- 3. Turk AS, Frei D, Fiorella D, et al. . ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg 2014;6:260–64 10.1136/neurintsurg-2014-011125 [DOI] [PubMed] [Google Scholar]
- 4. Stapleton CJ, Leslie-Mazwi TM, Torok CM, et al. . A direct aspiration first-pass technique vs stentriever thrombectomy in emergent large vessel intracranial occlusions. J Neurosurg 2018;128:567–74 10.3171/2016.11.JNS161563 [DOI] [PubMed] [Google Scholar]
- 5. Turk AS 3rd, Siddiqui A, Fifi JT, et al. . Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet 2019;393:998–1008 10.1016/S0140-6736(19)30297-1 [DOI] [PubMed] [Google Scholar]
- 6. Lapergue B, Blanc R, Gory B, et al. ; ASTER Trial Investigators. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER randomized clinical trial. JAMA 2017;318:443–52 10.1001/jama.2017.9644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Humphries W, Hoit D, Doss VT, et al. . Distal aspiration with retrievable stent assisted thrombectomy for the treatment of acute ischemic stroke. J Neurointerv Surg 2015;7:90–94 10.1136/neurintsurg-2013-010986 [DOI] [PubMed] [Google Scholar]
- 8. Stampfl S, Kabbasch C, Muller M, et al. . Initial experience with a new distal intermediate and aspiration catheter in the treatment of acute ischemic stroke: clinical safety and efficacy. J Neurointerv Surg 2016;8:714–18 10.1136/neurintsurg-2015-011801 [DOI] [PubMed] [Google Scholar]
- 9. Möhlenbruch MA, Kabbasch C, Kowoll A, et al. . Multicenter experience with the new SOFIA Plus catheter as a primary local aspiration catheter for acute stroke thrombectomy. J Neurointerv Surg 2017;9:1223–27 10.1136/neurintsurg-2016-012812 [DOI] [PubMed] [Google Scholar]
- 10. Wong JY, Do HM, Telischak NA, et al. . Initial experience with SOFIA as an intermediate catheter in mechanical thrombectomy for acute ischemic stroke. J Neurointerv Surg 2017;9:1103–06 10.1136/neurintsurg-2016-012750 [DOI] [PubMed] [Google Scholar]
- 11. Shallwani H, Shakir HJ, Rangel-Castilla L, et al. . Safety and efficacy of the Sofia (6F) PLUS distal access reperfusion catheter in the endovascular treatment of acute ischemic stroke. Clin Neurosurg 2018;82:312–21 10.1093/neuros/nyx169 [DOI] [PubMed] [Google Scholar]
- 12. Zaidat OO, Castonguay AC, Linfante I, et al. . First pass effect: a new measure for stroke thrombectomy devices. Stroke 2018;49:660–66 10.1161/STROKEAHA.117.020315 [DOI] [PubMed] [Google Scholar]
- 13. Hungerford JP, Hyer M, Turk AS, et al. . Impact of ASPECT scores and infarct distribution on outcomes among patients undergoing thrombectomy for acute ischemic stroke with the ADAPT technique. J Neurointerv Surg 2017;9:823–29 10.1136/neurintsurg-2016-012528 [DOI] [PubMed] [Google Scholar]
- 14. Sørensen LH, Speiser L, Karabegovic S, et al. . Safety and quality of endovascular therapy under general anesthesia and conscious sedation are comparable: results from the GOLIATH trial. J Neurointerv Surg 2019. March 29. [Epub ahead of print] 10.1136/neurintsurg-2019-014712 [DOI] [PubMed] [Google Scholar]
- 15. Gariel F, Lapergue B, Bourcier R, et al. ; ASTER Trial Investigators. Mechanical thrombectomy outcomes with or without intravenous thrombolysis. Stroke 2018;49:2383–90 10.1161/STROKEAHA.118.021500 [DOI] [PubMed] [Google Scholar]
- 16. Gory B, Armoiry X, Sivan-Hoffmann R, et al. . A direct aspiration first pass technique for acute stroke therapy: a systematic review and meta-analysis. Eur J Neurol 2018;25:284–92 10.1111/ene.13490 [DOI] [PubMed] [Google Scholar]
- 17. Malisch TW, Zaidat OO, Castonguay C. Clinical and angiographic outcomes with the combined local aspiration and retriever in the North American Solitaire Stent-Retriever Acute Stroke (NASA) Registry. Interv Neurol 2018;7:26–35 10.1159/000480353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Maegerlein C, Berndt M, Mönch S, et al. . Further development of combined techniques using stent retrievers, aspiration catheters and BGC: the PROTECTPLUS technique. Clin Neuroradiol 2018. November 9. [Epub ahead of print] 10.1007/s00062-018-0742-9 [DOI] [PubMed] [Google Scholar]
- 19. Maus V, Henkel S, Riabikin A, et al. . The SAVE technique: large-scale experience for treatment of intracranial large vessel occlusions. Clin Neuroradiol 2018. July 19. [Epub ahead of print] 10.1007/s00062-018-0702-4 [DOI] [PubMed] [Google Scholar]
- 20. Dargazanli C, Fahed R, Blanc R, et al. . Modified Thrombolysis in Cerebral Infarction 2c/Thrombolysis in Cerebral Infarction 3 reperfusion should be the aim of mechanical thrombectomy: insights from the ASTER trial (Contact Aspiration Versus Stent Retriever for Successful Revascularization). Stroke 2018;49:1189–96 10.1161/STROKEAHA.118.020700 [DOI] [PubMed] [Google Scholar]
- 21. Kaschner MG, Rubbert C, Caspers J, et al. . A retrospective single-center case series of direct aspiration thrombectomy as first-line approach in ischemic stroke and review of the literature. J Stroke Cerebrovasc Dis 2019;28:640–48 10.1016/j.jstrokecerebrovasdis.2018.11.004 [DOI] [PubMed] [Google Scholar]
- 22. Blanc R, Redjem H, Ciccio G, et al. . Predictors of the aspiration component success of A Direct Aspiration First Pass Technique (ADAPT) for the endovascular treatment of stroke reperfusion strategy in anterior circulation acute stroke. Stroke 2017;48:1588–93 10.1161/STROKEAHA.116.016149 [DOI] [PubMed] [Google Scholar]
- 23. Schramm P, Navia P, Papa R, et al. . ADAPT technique with ACE68 and ACE64 reperfusion catheters in ischemic stroke treatment: results from the PROMISE study. J Neurointerv Surg 2019;11:226–31 10.1136/neurintsurg-2018-014122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Alawieh A, Chatterjee AR, Vargas J, et al. . Lessons learned over more than 500 stroke thrombectomies using ADAPT with increasing aspiration catheter size. Neurosurgery 2018. November 10. [Epub ahead of print] 10.1093/neuros/nyy444 [DOI] [PubMed] [Google Scholar]
- 25. Tsang CO, Cheung IH, Lau KK, et al. . Outcomes of stent retriever versus aspiration-first thrombectomy in ischemic stroke: a systematic review and meta-analysis. AJNR Am J Neuroradiol 2018;39:2070–76 10.3174/ajnr.A5825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nikoubashman O, Nikoubashman A, Büsen M, et al. . Necessary catheter diameters for mechanical thrombectomy with ADAPT. AJNR Am J Neuroradiol 2017;38:2277–81 10.3174/ajnr.A5401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Delgado Almandoz JE, Kayan Y, Wallace AN, et al. . Larger ACE 68 aspiration catheter increases first-pass efficacy of ADAPT technique. J Neurointerv Surg 2019;11:141–46 10.1136/neurintsurg-2018-013957 [DOI] [PubMed] [Google Scholar]