Abstract
BACKGROUND AND PURPOSE:
The Analysis of Recanalization after Endovascular Treatment of Intracranial Aneurysm (ARETA) prospective study aims to determine factors predicting recurrence after endovascular treatment for intracranial aneurysms. In this publication, we review endovascular techniques and present the study population. Characteristics of treated and untreated unruptured aneurysms were analyzed.
MATERIALS AND METHODS:
Sixteen neurointerventional departments prospectively enrolled patients treated for ruptured and unruptured intracranial aneurysms between December 2013 and May 2015. Patient demographics, aneurysm characteristics, and endovascular techniques were recorded.
RESULTS:
A total of 1289 patients with 1761 intracranial aneurysms, 835 (47.4%) ruptured, were enrolled. Of these, 1359 intracranial aneurysms were treated by endovascular means. Ruptured intracranial aneurysms were treated by coiling and balloon-assisted coiling in 97.8% of cases. In unruptured intracranial aneurysms, the rates of flow diversion, flow disruption, and stent-assisted coiling were 11.6%, 6.9%, and 7.8%, respectively. Rupture status and aneurysm location, neck diameter, and sac size significantly influenced the chosen technique. Treated unruptured intracranial aneurysms, compared with untreated counterparts, had larger aneurysm sacs (7.6 ± 4.0 versus 3.4 ± 2.0 mm; P < 0.001) and neck dimensions (4.1 ± 2.2 versus 2.4 ± 1.3 mm; P < 0.001) and more frequently an irregular form (84.6% versus 44.4%; P < 0.001). Also, its location influenced whether an unruptured intracranial aneurysm was treated.
CONCLUSIONS:
Our study provides an overview of current neurointerventional practice in the ARETA cohort. The technique choice was influenced by aneurysm morphology, location, and rupture status. Flow diversion, flow disruption, and stent-assisted coiling were commonly used in unruptured intracranial aneurysms, while most ruptured intracranial aneurysms were treated with coiling and balloon-assisted coiling.
Endovascular embolization is an accepted and, in many cases, the preferred technique for the treatment of ruptured (RIA) and unruptured intracranial aneurysms (UIA). In large prospective multicenter studies, the last patients enrolled were in 2002 in the International Subarachnoid Aneurysm Trial,1 in 2006 in the Analysis of Treatment by Endovascular approach of Nonruptured Aneurysms (ATENA),2 and in 2007 in the Clinical and Anatomical Results in the Treatment of Ruptured Intracranial Aneurysms (CLARITY) trials.3 While the results of these studies are not outdated, it remains unclear whether they continue to reflect current neurointerventional practice, particularly in light of major technical advances that have become available during the past decade, first and foremost the advent of flow diverters4–6 and intrasaccular flow disrupters,7–13 which have broadened the spectrum of aneurysms amenable to reconstructive endovascular treatment. Unfortunately, little is known regarding the use of these devices in common neurointerventional practice. Furthermore, while the “remodeling technique”14 (also known as balloon-assisted coiling [BAC]) and stent-assisted coiling (SAC),15 were already available in the late 1990s and the early 2000s, respectively, it is probable that these techniques are currently more widely applied than a decade ago.
Different factors may influence the neurointerventionist's choice of materials for treatment of an intracranial aneurysm (IA), for example, the aneurysm rupture status, its sac and neck diameter, and location. More important, due to the relative absence of evidence-based guidelines, chosen techniques are guided by personal preferences, resulting in disparate treatment practices. Other factors influencing these practices are regulatory agencies by limiting the reimbursement of novel devices. Publications defining modern treatment strategies are thus rare.16
In this study, we report on the endovascular modalities used to treat RIA and UIA in the Analysis of Recanalization after Endovascular Treatment of Intracranial Aneurysm (ARETA) study, a large prospective, multicenter cohort study. Furthermore, we are seeking to present the demographics of the study population and to gain insight into current practices of neurointerventional aneurysm treatment.
Materials and Methods
The ARETA Study Protocol
ARETA was conceptualized to systematically evaluate factors that affect aneurysm recanalization after endovascular treatment during a follow-up of 12 months. The study was sponsored by the French Ministry of Health in a Programme Hospitalier de Recherche Clinique, No. 12–001–0372, and was registered on www.clinicaltrials.gov (NCT01942512). ARETA received national regulatory authorizations: approval from the Reims Institutional Review Board, the Consultative Committee of Information Processing in Health Care Research Program, and the National Commission for Data Processing and Freedom. The study objective and its protocol with inclusion and exclusion criteria have previously been described.17
Patients were prospectively enrolled in 16 centers in France between December 2013 and May 2015. Consecutive enrollment was not mandatory. The following baseline patient characteristics were reported by the participating study sites: age; sex; current or previous use of cigarettes (including the number of pack-years for current and previous smokers), alcohol, cannabis and other recreational drugs; arterial hypertension (defined as blood pressure >140/90 mm Hg, based on medical history); hypercholesterolemia and hypertriglyceridemia; diabetes mellitus; Ehlers-Danlos syndrome or other connective tissue diseases; polycystic kidney disease; and familial history of IA. Furthermore, centers reported the initial World Federation of Neurosurgical Societies (WFNS) grade for patients with RIA and the preprocedural modified Rankin Scale score (mRS) for patients with UIA.
Recorded aneurysm characteristics were aneurysm sac diameter (including trichotomization into <10, 10–25, and >25 mm); neck size (wide-neck being defined as ≥4 mm); aneurysm location (extradural ICA, intradural ICA, including the posterior communicating artery, middle cerebral artery, anterior communicating/anterior cerebral artery, or vertebrobasilar artery; territory branch aneurysms were included in the respective category); aneurysm rupture status (ruptured or unruptured); aneurysm morphology (regular or irregular); and number of IAs (single or multiple).
Treatment modalities were at the discretion of the treating interventional neuroradiologist and categorized into coils, BAC, SAC, flow diversion, intrasaccular flow-disruption, and parent vessel sacrifice. The use of techniques like dual microcatheter coiling, Y-stent placement, or double BAC did not represent an exclusion criterion. Patients treated by these modalities were grouped into the respective categories (for example, double BAC was analyzed as BAC).
Notably, patients with UIAs who did not undergo endovascular treatment of at least 1 aneurysm, including patients who underwent clipping, were not included in the ARETA study.
Data Management and Statistics
Participating centers reported patient, aneurysm, and treatment characteristics on a standardized form. The centers also collected preoperative DSA and immediate postoperative DSA and transferred the results in an anonymized form to Reims University Hospital. Aneurysm characteristics and treatment modalities of all patients were reviewed, checked for accuracy, and, if necessary, revised by 2 neuroradiologists (M.G., S.S.) at the managing site. Data management and statistical analysis were conducted by the Department of Research and Public Health of Reims University Hospital (C.B.). We applied descriptive statistics: Data are presented with mean and SD for quantitative variables and number and percentage for qualitative variables. Comparisons among groups were analyzed using a χ2 or Student t test. No imputation method was used for missing data. Statistical analysis was performed using SAS (Version 9.4; SAS Institute, Cary, North Carolina). A P value < .05 was considered significant.
Results
Population Characteristics
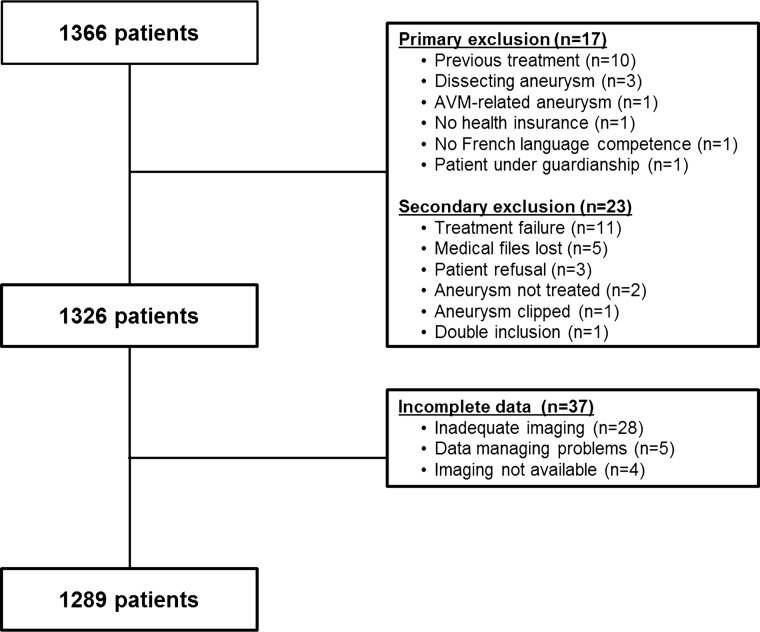
In total, 1289 patients with 1761 IA remained for analysis (Figure). Table 1 details the demographic aspects of the study population. Of 1289 patients, 811 (62.9%) presented with at least 1 RIA. Multiple aneurysms (ie, >1) were detected in 319 patients (24.7%); the maximum number of IAs in a single patient was 8.
FIGURE.
Flow chart of the study population. “Treatment failure” refers to an endovascular treatment attempt that was aborted before a device was implanted.
Table 1:
Demographic characteristics of 1289 patients
| Variables | |
|---|---|
| Female (No.) (%) | 866 (67.2%) |
| Age (mean) | 54.1 ± 12.7 years |
| Single IA (No.) (%) | 970 (75.3%) |
| Multiple IAs (No.) (%) | 319 (24.7%) |
| 2 IAs (No.) (%) | 214 (67.1%) |
| 3 IAs (No.) (%) | 73 (22.9%) |
| 4 IAs (No.) (%) | 23 (7.2%) |
| 5 IAs (No.) (%) | 5 (1.6%) |
| 6 IAs (No.) (%) | 2 (0.6%) |
| 7 IAs (No.) (%) | 1 (0.3%) |
| 8 IAs (No.) (%) | 1 (0.3%) |
| Tobacco (No.) (%)a | 768 (60.4%) |
| Active smoking (No.) (%)b | 559/762 (73.4%) |
| Pack-years (mean)c | 26.0 ± 21.0 |
| Regular alcohol consumption (No.) (%)d | 255 (20.2%) |
| Cannabis use (No.) (%)e | 45 (3.6%) |
| Other recreational drugs (No.) (%)d | 15 (1.2%) |
| Hypertension (No.) (%)f | 462 (36.1%) |
| With treatment (No.) (%)g | 363/449 (80.9%) |
| Normalized blood pressure (No.) (%)h | 304/429 (70.9%) |
| Dyslipidemia (No.) (%)i | 226 (17.8%) |
| Hypercholesterolemia (No.) (%)j | 195/207 (94.2%) |
| Hypertriglyceridemia (No.) (%)k | 47/198 (23.7%) |
| With treatment (No.) (%)l | 151/206 (73.3%) |
| Family history of IA (No.) (%)m | 90 (7.2%) |
| Diabetes mellitus (No.) (%)f | 63 (4.9%) |
| Dietary treatment onlyn | 17/60 (28.3%) |
| Oral antidiabetic treatmento | 40/62 (64.5%) |
| Insulin treatmentp | 9/61 (14.8%) |
| Polycystic kidney disease (No.) (%)q | 17 (1.3%) |
| Connective tissue disease (No.) (%)f | 1 (0.1%) |
The following are missing data: 17 (1.3%).
6 (0.8%).
120 (15.6%).
24 (1.9%).
22 (1.7%).
9 (0.7%).
13 (2.8%).
33 (7.1%).
16 (1.2%).
19 (8.4%).
28 (12.4%).
20 (8.8%).
30 (2.3%).
3 (4.8%).
1 (1.6%).
2 (3.2%).
8 (0.6%).
Among the 811 patients presenting with RIAs, 808 had available data for a World Federation of Neurosurgical Societies score at admission. Distribution of WFNS scores at admission was as follows: I in 390 (48.3%), II in 171 (21.2%), III in 40 (5.0%), IV in 115 (14.2%), and V in 92 (11.4%) patients. Among the 478 patients presenting with UIAs, 467 had available data for pretreatment mRS scores. The distribution of pretreatment mRS was as follows: mRS 0 in 344 (73.7%), mRS 1 in 114 (24.4%), mRS 2 in 5 (1.1%), mRS 3 in 2 (0.4%), and mRS 4 in 2 (0.4%) patients.
Aneurysm Characteristics
Of 1761 observed IAs, 835 (47.4%) were ruptured and 926 (52.6%) were unruptured. Mean aneurysm diameter was 6.1 ± 3.6 mm: 1524 IAs (87.5%) had diameters <10 mm, 214 IAs (12.3%) had diameters between 10 and 25 mm, and 4 IAs (0.2%) had diameters of >25 mm. The mean aneurysm neck diameter was 3.2 ± 1.8 mm. Wide-neck aneurysms with a neck diameter of ≥4 mm accounted for 486 IAs (28.3%). Irregular configurations were observed in 1022 IAs (60.4%). Locations of the IAs are shown in Table 2.
Table 2:
All aneurysms in the study collective and treated aneurysms
| Location | All Aneurysmsa |
Treated Aneurysms |
||
|---|---|---|---|---|
| No. | % | No. | % | |
| ACA/AcomA | 557 | 31.7 | 497 | 36.6 |
| MCA | 458 | 26.0 | 283 | 20.8 |
| Intradural ICA | 530 | 30.1 | 438 | 32.2 |
| Extradural ICA | 88 | 5.0 | 37 | 2.7 |
| Vertebrobasilar | 126 | 7.2 | 104 | 7.6 |
| Total | 1751 | 100 | 1359 | 100 |
Note:—ACA indicates anterior cerebral artery; AcomA, anterior communicating artery.
Two missing data.
Endovascular treatment was performed for 1359 of 1761 aneurysms (77.2%). Among treated aneurysms, 835 (61.4%) were ruptured. More than 1 aneurysm was treated during 1 session in 67 patients (5.2%): 24 of 478 (5.0%) patients with UIAs and 43 of 811 (5.3%) patients with RIAs.
Locations of the treated IAs are shown in Table 2. Treated aneurysms had a mean diameter of 6.8 ± 3.5 mm. Diameters of <10 mm were seen in 1149 IAs (84.5%), 206 IAs (15.2%) had diameters between 10 and 25 mm, and 4 IAs (0.3%) had diameters of >25 mm. The mean neck size was 3.5 ± 1.8 mm. Wide-neck accounted for 434 IAs (31.9%). Irregular shapes were found in 967 treated aneurysms (71.2%).
Comparison of Treated and Untreated Unruptured Aneurysms
Of 926 UIAs, 524 (56.6%) were treated. Treated UIAs had significantly greater dimensions both of the aneurysm sac (7.6 ± 4.0 versus 3.4 ± 2.0 mm; P < 0.001) and the aneurysm neck (4.1 ± 2.2 versus 2.4 ± 1.3 mm; P < 0.001) than UIAs that were left untreated. Of note, 375 untreated UIAs (97.9%) were significantly smaller than 10 mm versus 413 treated UIAs (78.8%) (P < 0.001), and 311 untreated UIAs (81.2%) were significantly smaller than 5 mm versus 113 treated UIAs (21.6%) (P < 0.001). Treatment rates of UIAs varied among aneurysm locations: Overall, 67.4% of anterior cerebral artery/anterior communicating artery aneurysms (124 of 184), 68.7% of intradural ICA aneurysms (202 of 294), 68.1% of vertebrobasilar aneurysms (47 of 69), 41.4% of extradural ICA aneurysms (36 of 87), and 39.7% of MCA aneurysms (115 of 290) were treated by endovascular means. UIAs of the extradural ICA were significantly less frequently treated than aneurysms in other locations (36 of 87 [41.4%] versus 488 of 837 [58.3%]; P = .002). Likewise, UIAs of the MCA were less frequently treated endovascularly than UIAs in other locations (115 of 290 [39.7%] versus 409 of 634 [64.4%]; P < 0.001). Moreover, UIAs with irregular configurations were significantly more frequently treated than UIAs with regular configurations (303 of 358 [84.6%] versus 221 of 498 [44.4%]; P < 0.001). The 55 irregular untreated UIAs were significantly smaller than their treated counterparts (4.6 ± 2.4 versus 7.0 ± 3.4 mm, P < 0.001).
Endovascular Techniques
Endovascular techniques that were applied are shown in Table 3. UIAs were significantly more frequently treated with intrasaccular flow disruption (36 of 524 [6.9%] versus 5 of 835 [0.6%]; P < 0.001), flow diversion (61 of 524 [11.5%] versus 4 of 835 [0.5%]; P < 0.001), and SAC (41 of 524 [7.8%] versus 8 of 835 [1.0%]; P < 0.001) than RIAs. Altogether, these 3 techniques were used for 26.1% of UIAs. One giant UIA was treated with a detachable balloon for parent vessel occlusion, and 1 RIA was treated by parent vessel occlusion using coils. RIAs were more frequently treated by coiling (461 of 835 [55.2%] versus 189 of 524 [36.1%]; P < 0.001) and BAC (356 of 835 [42.6%] versus 196 of 524 [37.4%]; P = .06) than UIAs, but the difference was not statistically significant for BAC. Of note, 97.8% (817 of 835) of RIAs were treated by coiling or BAC.
Table 3:
Techniques used for embolization of ruptured and unruptured aneurysms
| Treatment Modality | All IAs |
RIAs |
UIAs |
P Value | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Coiling alone | 650 | 47.8 | 461 | 55.2 | 189 | 36.1 | <0.001 |
| Balloon-assisted coiling | 552 | 40.6 | 356 | 42.6 | 196 | 37.4 | .06 |
| Stent-assisted coiling | 49 | 3.6 | 8 | 1.0 | 41 | 7.8 | <0.001 |
| Flow diversiona | 65 | 4.8 | 4 | 0.5 | 61 | 11.6 | <0.001 |
| Flow disruptionb | 41 | 3.0 | 5 | 0.6 | 36 | 6.9 | <0.001 |
| Parent vessel occlusion | 2 | 0.2 | 1 | 0.1 | 1 | 0.2 | .74 |
| Total | 1359 | 100 | 835 | 100 | 524 | 100 | |
Thirty aneurysms were treated in conjunction with coils.
Two aneurysms were treated in conjunction with coils; 3 aneurysms, in conjunction with a remodeling balloon; and 1 aneurysm, with an ancillary stent.
Treatment modalities varied depending on the aneurysm sac dimensions (Table 4). Aneurysms of >10 mm were more frequently treated with flow diverters than aneurysms <10 mm (30 of 210 [13.8%] versus 35 of 1149 [3.1%]; P < 0.001). However, 54.7% (35 of 64) of flow-diverting procedures were performed for treatment of aneurysms of <10 mm. Aneurysms of <10 mm were more frequently treated with standard coiling than aneurysms of >10 mm (569 of 1149 [49.5%] versus 81 of 210 [38.6%]; P = .003). An additional analysis, further dividing small aneurysms (<10 mm) into aneurysms of <5 and ≥5 mm, was conducted and is shown in On-line Table 1. Most important, interclass differences with the fourth size category did not change for most treatment modalities (ie, coiling, BAC, flow diversion, SAC, and parent vessel occlusion) compared with the initial analysis with 3 size categories (<10, 10–25, >25 mm). The only new significant difference was found for flow disruption (P < 0.001), which is explained by the infrequent use of the Woven EndoBridge (WEB aneurysm embolization system; Sequent Medical, Aliso Viejo, California) for aneurysms of <5 mm (2 of 399 [0.5%] versus 39 of 960 [4.1%]; P < 0.001).
Table 4:
Treatment modality with regard to aneurysm sac diameter
| Treatment Modality | All IAs |
<10 mm |
10–25 mm |
>25 mm |
P Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | ||
| Coiling alone | 650 | 47.8 | 569 | 49.5 | 81 | 39.3 | 0 | 0 | .003 |
| Balloon-assisted coiling | 552 | 40.6 | 472 | 41.1 | 80 | 38.8 | 0 | 0 | .24 |
| Stent-assisted coiling | 49 | 3.6 | 37 | 3.2 | 12 | 5.8 | 0 | 0 | .20 |
| Flow diversion | 65 | 4.8 | 35 | 3.1 | 27 | 13.1 | 3 | 75.0 | <0.001 |
| Flow disruption | 41 | 3.0 | 35 | 3.1 | 6 | 2.9 | 0 | 0 | .93 |
| Parent vessel occlusion | 2 | 0.2 | 1 | 0.1 | 0 | 0 | 1 | 25.0 | .006 |
| Total | 1359 | 100 | 1149 | 100 | 206 | 100 | 4 | 100 | |
Treatment modalities also varied depending on the aneurysm neck diameter (Table 5). Stent-assisted coiling, intrasaccular flow disrupters, and flow diverters were significantly more frequently deployed in wide-neck aneurysms (32 of 434 [7.4%] versus 17 of 925 [1.8%]; P < 0.001; 36 of 434 [8.3%] versus 5 of 925 [0.5%]; P < 0.001; and 48 of 434 [11.1%] versus 17 of 925 [1.8%]; P < 0.001, respectively) than in narrow-neck IAs. Simple coiling was significantly more frequently used in narrow-neck IAs (511 of 925 [55.2%] versus 139 of 434 [32.0%]; P < 0.001). Most interesting, BAC was not used more frequently in wide-neck than in narrow-neck aneurysms (177 of 434 wide-neck [40.8%] versus 375 of 925 narrow-neck IAs [40.6%]; P = .93).
Table 5:
Treatment modality with regard to aneurysm neck diameter
| Treatment Modality | All IAs |
<4 mm |
≥4 mm |
P Value | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Coiling alone | 650 | 47.8 | 511 | 55.2 | 139 | 32.0 | <0.001 |
| Balloon-assisted coiling | 552 | 40.6 | 375 | 40.5 | 177 | 40.8 | .93 |
| Stent-assisted coiling | 49 | 3.6 | 17 | 1.8 | 32 | 7.4 | <0.001 |
| Flow diversion | 65 | 4.8 | 17 | 1.8 | 48 | 11.1 | <0.001 |
| Flow disruption | 41 | 3.0 | 5 | 0.5 | 36 | 8.3 | <0.001 |
| Parent vessel occlusion | 2 | 0.2 | 0 | 0 | 2 | 0.5 | .10 |
| Total | 1359 | 100 | 925 | 100 | 434 | 100 | |
Aneurysm location affected the chosen treatment technique, as shown in On-line Table 2. Notably, BAC was performed more often for aneurysms of the intradural segment of the ICA than in other aneurysm locations (204 of 438 [46.6%] versus 348 of 921 [37.8%]; P = .002). Conversely, flow diverters were deployed more often in aneurysms of the intra- and extradural ICA than in other aneurysm locations (41 of 438 [9.4%] versus 24 of 921 [2.6%]; P < 0.001; and 15 of 37 [40.5%] versus 50 of 1322 [3.8%]; P < 0.001, respectively). Also, SAC was used more often for extradural ICA aneurysms (6 of 37 [16.2%] versus 43 of 1322 [3.2%]; P = .002). Furthermore, these extradural ICA aneurysms were less frequently treated by standard coiling than IAs in other locations (7 of 37 [18.9%] versus 643 of 1322 [48.6%]; P < 0.001). Intra-aneurysmal flow disruption was used more often in MCA and vertebrobasilar aneurysms than in other aneurysm locations (19 of 283 [6.7%] versus 22 of 1076 [2.0%]; P < 0.001; and 7 of 104 [6.7%] versus 34 of 1255 [2.7%]; P = .03, respectively).
Discussion
Relevance of Flow Diversion, Intrasaccular Flow Disruption, and Stent-Assisted Coiling
In ARETA, 11.6% of UIAs were treated by flow diversion, representing a significant proportion in this cohort. The US FDA approved the use of flow diverters for patients with unruptured large or giant wide-neck intracranial aneurysms in the ICA from the petrous to the superior hypophyseal segments.18 The ARETA results are in line with current recommendations because flow diverters were used for wide-neck large and giant aneurysms at a proportionally higher rate than for small and narrow-neck aneurysms. Flow diverters were also used more frequently in aneurysms of the intradural (9.4%) and extradural (40.5%) ICA. However, the extension of treatment indications to ruptured, small, narrow-neck, or distal bifurcation aneurysms is increasingly reported by some groups.19 Of note, in the present study, 53.8% of flow diverters were used in aneurysms of <10 mm, and 26.2% of aneurysms treated with a flow diverter had a neck diameter of <4 mm. A limited number of flow-diverting stents were also used for the treatment of MCA and anterior communicating artery aneurysms, a treatment concept that is currently under discussion.20,21 These numbers thus reflect a flexible application of current recommendations for the use of flow diversion if judged necessary by the interventionist. Because an endoluminal implant is left in place, dual antiplatelet therapy is usually necessary and the aneurysm is at least temporarily left circulating (if no coils are added during the procedure). Flow diverters were thus very rarely used in RIAs (4 of 835 ruptured aneurysms [0.5%]); however, these results may be biased by the exclusion of dissecting, fusiform, and blisterlike aneurysms, where flow diversion is sometimes the only treatment option when parent vessel sacrifice is not possible.22,23
Intrasaccular flow disruption by the WEB device was used to treat 3.0% of patients. This device was introduced in 2011, primarily for treatment of complex wide-neck bifurcation aneurysms of the MCA and basilar artery in particular.7–13 If we grouped these aneurysms, 6.7% of both MCA and basilar artery aneurysms were treated by this technique; 87.8% of WEB devices were used in wide-neck aneurysms with neck diameters of ≥4 mm. In ARETA, intrasaccular flow disruption was often used in UIAs (6.9% were treated by the WEB) and only in 0.6% of RIAs. This may be because a wide range of WEB devices suitable for various aneurysm configurations were not permanently available in all departments; furthermore, the learning curve in WEB application might be a limiting factor as well as a possible reluctance to use this novel device in a ruptured aneurysm. Whereas the current literature indicates that it may be safe and effective to treat RIAs with flow disrupters24—particularly because postinterventional antiplatelet therapy is not imperative—large prospective controlled data are not available and are subject to the CLinical Assessment of WEB Device in Ruptured aneurYSms (CLARYS) study, which recently completed recruitment (NCT02687607: www.clinicaltrials.gov).
In the ARETA study, SAC was used in 3.6% of all aneurysms. The use of dedicated self-expanding endoluminal devices for SAC was first reported in 200215 and is now a standard technique. SAC was primarily designed for the treatment of unruptured wide-neck aneurysms, and in ARETA, it was used in 7.8% of these aneurysms: Wide-neck aneurysms accounted for 65.3% of SAC procedures. Stents usually necessitate a dual-antiplatelet regimen and are associated with a higher complication rate in RIAs compared with UIAs.25 Conversely, only 8 patients (1%) with RIAs were treated with stent assistance; moreover, it is not clear in how many of these patients SAC was used as a rescue treatment.
Overall, our study confirms that in patients presenting with a ruptured saccular aneurysm, flow diversion, flow disruption, and SAC currently play a minor role, given that 97.8% of RIAs were amenable to treatment with simple coiling or BAC in our study.
Balloon-Assisted Coiling
BAC, also known as a remodeling technique, was used in 40.6% of aneurysms in the present series (42.6% of RIAs and 37.4% of UIAs). Since its initial description by Moret et al14 in 1997, BAC has emerged as a standard treatment option. Apart from the ability to treat wide-neck aneurysms and offer improved immediate and follow-up anatomic results,26 it has 2 additional potential advantages over simple coiling, with a similar safety profile26: 1) The microcatheter is stabilized during embolization, making it easier to maintain access; and 2) in case of aneurysm perforation during coiling, the balloon can be inflated while detaching several coils to immediately protect and seal the rupture site. These potential advantages are also reflected by the fact that BAC was not more frequently used for the treatment of wide-neck than narrow-neck aneurysms in the present study. Aneurysm location influenced the frequency of BAC: Notably, it was used more often for aneurysms of the intradural ICA (ie, posterior communicating artery and paraophthalmic aneurysms).
In CLARITY, BAC was used in 20.5% of cases (versus 40.6% in the present cohort); our study confirms the wider application of BAC in cases of RIAs. The rationale behind this development is likely linked to the increased risk of perforation in RIAs.3,27 While the rates of BAC between ARETA and ATENA for UIAs are comparable (37.3% in ATENA versus 37.4% in the present series), we observed a decline in simple coiling approaches (54.5% in ATENA versus 36.1% in ARETA).2 Flow diversion, flow disruption, and SAC were used in 26.2% of UIAs in the present series, whereas neither flow diversion nor intrasaccular flow disruption was available during the recruitment period of ATENA; 7.8% of patients were treated by SAC in that study. Our results indicate that treatment modalities of UIAs are currently shifting toward more complex and novel approaches, away from the simple coiling technique.
Comparison of Treated and Untreated Unruptured Aneurysms
The rupture risk of UIAs depends on aneurysm size, location, and shape and is generally low, especially in small aneurysms.28,29 Preventive treatment is generally justified if the benefit of treatment outweighs the anticipated treatment risks. Therefore, it is not surprising that untreated UIAs in ARETA were smaller than treated counterparts and presented less frequently with an irregular form. Furthermore, extradural ICA aneurysms, in which subarachnoid hemorrhage is usually not a concern, were less frequently treated than UIAs of the anterior cerebral artery/anterior communicating artery, the intradural ICA segment (which included the posterior communicating artery in this study), and the vertebrobasilar territory. Also, unruptured MCA aneurysms were less frequently treated than UIAs in other locations, which may be because they are less likely to rupture.28
Limitations of the Study
Our study has limitations. Because patients who underwent clipping were not included in the study, a selection bias may exist, in particular with MCA aneurysms in which clipping is still widely used. However, endovascular treatment is currently the treatment of choice for RIAs and UIAs in many institutions. Another limitation is that consecutive enrollment of all patients treated in 1 center was not mandatory for the participation in the study. Because the study inclusion period ended in 2015, modifications of the current practice with an even broader implementation of novel techniques are probable, particularly intrasaccular flow disruption. The low percentage of novel techniques could also be partly explained by regulatory mechanisms because during the study period, there was no reimbursement for intrasaccular flow disrupters or intravascular flow diverters and limited reimbursement for conventional microstents by the French Health Insurance (whereas the devices are, in case of nonreimbursement, paid for by the hospital itself). Moreover, there is certainly a variance of technical approaches among the participating centers. Another limitation is that only the aneurysm rupture status was assessed at inclusion into the ARETA cohort and compressive symptoms were not evaluated. Our observations of the characteristics of treated and untreated UIAs must be viewed with caution because this study did not focus on the natural course of UIAs and there was no prospective observation of rupture risk. Finally, this article does not present clinical or anatomic outcome data, which will be the subject of future publications.
Conclusions
Our study presents the demographics of the patient collective of the ARETA study and provides a representative overview of current endovascular treatment strategies for RIAs and UIAs. The technique choice was influenced by the rupture status of the aneurysm, sac size, neck diameter, and location. While the evolving techniques of flow diversion, intrasaccular flow disruption, and stent-assisted coiling were deployed in a significant proportion of UIAs, most RIAs were treated with simple coiling and balloon-assisted coiling. When we compared the present study collective with previously published series, shifting treatment regimens toward more advanced techniques—away from simple coiling—was observed. Moreover, we observed an influence of size, location, and form on the decision of whether to treat UIAs.
ABBREVIATIONS:
- BAC
balloon-assisted coiling
- IA
intracranial aneurysm
- RIA
ruptured intracranial aneurysm
- SAC
stent-assisted coiling
- UIA
unruptured intracranial aneurysm
- WFNS
World Federation of Neurosurgical Societies
Footnotes
Disclosures: Laurent Pierot—UNRELATED: Consultancy: Balt, Cerenovus, MicroVention, Penumbra, Vesalio. Philip White—RELATED: Fees for Participation in Review Activities such as Data Monitoring Boards, Statistical Analysis, End Point Committees, and the Like: University of Reims*; UNRELATED: Consultancy: MicroVention, Stryker; Grants/Grants Pending: MicroVention,* Laurent Spelle—UNRELATED: Consultancy: Stryker, Balt, MicroVention, Medtronic; Stock/Stock Options: Sensome. Coralie Barbe—RELATED: Grant: French Ministry of Health, Comments: Programme Hospitalier de Recherche Clinique.* *Money paid to the institution.
Study group (to be listed as collaborators) is presented in the On-line Appendix.
The ARETA study was sponsored by the French Ministry of Health in a Programme Hospitalier de Recherche Clinique (PHRC), No. 12-001-0372.
References
- 1. Molyneux A, Kerr R, Stratton I. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 2002;360:1267–74 10.1016/S0140-6736(02)11314-6 [DOI] [PubMed] [Google Scholar]
- 2. Pierot L, Spelle L, Vitry F. Immediate clinical outcome of patients harboring unruptured intracranial aneurysms treated by endovascular approach: results of the ATENA study. Stroke 2008;39:2497–504 10.1161/STROKEAHA.107.512756 [DOI] [PubMed] [Google Scholar]
- 3. Pierot L, Cognard C, Ricolfi F, et al. . Immediate anatomic results after the endovascular treatment of ruptured intracranial aneurysms: analysis in the CLARITY series. AJNR Am J Neuroradiol 2010;31:907–11 10.3174/ajnr.A1954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kallmes DF, Brinjikji W, Boccardi E, et al. . Aneurysm Study of Pipeline in an Observational Registry (ASPIRe). Interv Neurol 2016;5:89–99 10.1159/000446503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kallmes DF, Hanel R, Lopes D, et al. . International retrospective study of the Pipeline Embolization Device: a multicenter aneurysm treatment study. AJNR Am J Neuroradiol 2015;36:108–15 10.3174/ajnr.A4111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Becske T, Kallmes DF, Saatci I, et al. . Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology 2013;267:858–68 10.1148/radiol.13120099 [DOI] [PubMed] [Google Scholar]
- 7. Pierot L, Spelle L, Molyneux A, et al. . Clinical and anatomical follow-up in patients with aneurysms treated with the WEB device: 1-year follow-up report in the cumulated population of 2 prospective, multicenter series (WEBCAST and French Observatory). Neurosurgery 2016;78:133–41 10.1227/NEU.0000000000001106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pierot L, Klisch J, Cognard C, et al. . Endovascular WEB flow disruption in middle cerebral artery aneurysms: preliminary feasibility, clinical, and anatomical results in a multicenter study. Neurosurgery 2013;73:27–34; discussion 34–35 10.1227/01.neu.0000429860.04276.c1 [DOI] [PubMed] [Google Scholar]
- 9. Pierot L, Moret J, Turjman F, et al. . WEB treatment of intracranial aneurysms: clinical and anatomic results in the French Observatory. AJNR Am J Neuroradiol 2016;37:655–59 10.3174/ajnr.A4578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pierot L, Moret J, Turjman F, et al. . WEB treatment of intracranial aneurysms: feasibility, complications, and 1-month safety results with the WEB DL and WEB SL/SLS in the French Observatory. AJNR Am J Neuroradiol 2015;36:922–27 10.3174/ajnr.A4230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pierot L, Gubucz I, Buhk JH, et al. . Safety and efficacy of aneurysm treatment with the WEB: results of the WEBCAST 2 study. AJNR Am J Neuroradiol 2017;38:1151–55 10.3174/ajnr.A5178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Asnafi S, Rouchaud A, Pierot L, et al. . Efficacy and safety of the Woven EndoBridge (WEB) device for the treatment of intracranial aneurysms: a systematic review and meta-analysis. AJNR Am J Neuroradiol 2016;37:2287–92 10.3174/ajnr.A4900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fiorella D, Molyneux A, Coon A, et al. . Demographic, procedural and 30-day safety results from the WEB Intra-saccular Therapy Study (WEB-IT). J Neurointerv Surg 2017;9:1191–96 10.1136/neurintsurg-2016-012841 [DOI] [PubMed] [Google Scholar]
- 14. Moret J, Cognard C, Weill A, et al. . Reconstruction technic in the treatment of wide-neck intracranial aneurysms: long-term angiographic and clinical results—apropos of 56 cases [in French]. J Neuroradiol 1997;24:30–44 [PubMed] [Google Scholar]
- 15. Henkes H, Bose A, Felber S, et al. . Endovascular coil occlusion of intracranial aneurysms assisted by a novel self-expandable nitinol microstent (Neuroform). Interv Neuroradiol 2002;8:107–19 10.1177/159101990200800202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fargen KM, Soriano-Baron HE, Rushing JT, et al. . A survey of intracranial aneurysm treatment practices among United States physicians. J Neurointerv Surg 2018;10:44–49 10.1136/neurintsurg-2016-012808 [DOI] [PubMed] [Google Scholar]
- 17. Benaissa A, Barbe C, Pierot L. Analysis of recanalization after endovascular treatment of intracranial aneurysm (ARETA trial): presentation of a prospective multicenter study. J Neuroradiol 2015;42:80–85 10.1016/j.neurad.2014.04.003 [DOI] [PubMed] [Google Scholar]
- 18. U.S. Food and Drug Administration. Premarket Approval (PMA) of the Pipeline Embolization Device. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=P100018. Accessed August 15, 2018.
- 19. Patel PD, Chalouhi N, Atallah E, et al. . Off-label uses of the Pipeline Embolization Device: a review of the literature. Neurosurg Focus 2017;42:E4 10.3171/2017.3.FOCUS1742 [DOI] [PubMed] [Google Scholar]
- 20. Gawlitza M, Januel AC, Tall P, et al. . Flow diversion treatment of complex bifurcation aneurysms beyond the circle of Willis: a single-center series with special emphasis on covered cortical branches and perforating arteries. J Neurointerv Surg 2016;8:481–87 10.1136/neurintsurg-2015-011682 [DOI] [PubMed] [Google Scholar]
- 21. Pistocchi S, Blanc R, Bartolini B, et al. . Flow diverters at and beyond the level of the circle of Willis for the treatment of intracranial aneurysms. Stroke 2012;43:1032–38 10.1161/STROKEAHA.111.636019 [DOI] [PubMed] [Google Scholar]
- 22. Fischer S, Perez MA, Kurre W, et al. . Pipeline embolization device for the treatment of intra- and extracranial fusiform and dissecting aneurysms: initial experience and long-term follow-up. Neurosurgery 2014;75:364–74; discussion 374 10.1227/NEU.0000000000000431 [DOI] [PubMed] [Google Scholar]
- 23. Lozupone E, Piano M, Valvassori L, et al. . Flow diverter devices in ruptured intracranial aneurysms: a single-center experience. J Neurosurg 2018;128:1037–43 10.3171/2016.11.JNS161937 [DOI] [PubMed] [Google Scholar]
- 24. van Rooij SB, van Rooij WJ, Peluso JP, et al. . WEB treatment of ruptured intracranial aneurysms: a single-center cohort of 100 patients. AJNR Am J Neuroradiol 2017;38:2282–87 10.3174/ajnr.A5371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bechan RS, Sprengers ME, Majoie CB, et al. . Stent-assisted coil embolization of intracranial aneurysms: complications in acutely ruptured versus unruptured aneurysms. AJNR Am J Neuroradiol 2016;37:502–07 10.3174/ajnr.A4542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pierot L, Cognard C, Spelle L, et al. . Safety and efficacy of balloon remodeling technique during endovascular treatment of intracranial aneurysms: critical review of the literature. AJNR Am J Neuroradiol 2012;33:12–15 10.3174/ajnr.A2403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cloft HJ, Kallmes DF. Cerebral aneurysm perforations complicating therapy with Guglielmi detachable coils: a meta-analysis. AJNR Am J Neuroradiol 2002;23:1706–09 [PMC free article] [PubMed] [Google Scholar]
- 28. Morita A, Kirino T, Hashi K, et al. ; UCAS Japan Investigators. The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med 2012;366:2474–82 10.1056/NEJMoa1113260 [DOI] [PubMed] [Google Scholar]
- 29. Wiebers DO. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 2003;362:103–10 10.1016/S0140-6736(03)13860-3 [DOI] [PubMed] [Google Scholar]