Abstract
Aim and background
Colon and rectum (colorectal) cancer cause substantial mortality and morbidity worldwide. The management and control of a complex disease such as cancer cannot rely on the old strategy of “one disease one medicine” and must make a transition into new-age practices involving predictive, preventive, and personalized medicine (PPPM) at its core. Adoption of PPPM approach to cancer management at the policy level requires quantification of cancer burden at the country level. For this purpose, we examine the burden of colorectal cancer in 185 countries in 2018. Based on results, we discuss the opportunities presented by PPPM and challenges to be encountered while adopting PPPM for the treatment and prevention of colorectal cancer.
Data and methods
Age- and sex-wise estimates of colorectal cancer were procured from the GLOBOCAN 2018. The country- and region-wise burden of colorectal cancer in 185 countries was examined using all-age and age-standardized incidence and mortality estimates. Human development index (HDI) was employed as the indicator of socioeconomic status of a country. Mortality-to-incidence ratio (MIR) was employed as the proxy of 5-year survival rate.
Results
Globally, colorectal cancer claimed an estimated 880,792 lives (males 484,224; females 396,568) with 1.85 million new cases (males 1.03 million; females 823,303) were estimated to be diagnosed in 2018. Globally, the age-standardized incidence rate (ASIR) was 19.7/100,000, whereas age-standardized mortality rate (ASMR) recorded to be 16.3/100,000 in 2018. Age-standardized rates were the highest in developed countries led by Hungary with ASIR of 51.2/100,000 followed by South Korea with ASIR of 44.5/100,000. ASMR followed the patterns of ASIR with the highest ASMR recorded by Hungary (21.5 per 100,000) and Slovakia (20.4 per 100,000). Globally, MIR stood at 0.48, and among the countries recording more than 1000 cases, Nepal registered the highest MIR of 0.83 and the lowest was recorded by South Korea (0.27). The age-standardized rates exhibited nonlinear association with HDI, whereas MIR was negatively associated with HDI.
Conclusion
Colorectal cancer causes a substantial burden worldwide and exhibit a positive association with the socioeconomic status. With the aid of improving screening modalities, preventable nature of the disease (due to dietary and lifestyle risk factors) and improving treatment procedures, the burden of CRC can largely be curtailed. The high burden of CRC in developing countries, therefore, calls for effective prevention strategies, cost-effective screening, and early-stage detection, cost-effective predictive, and personalized treatment regime.
Keywords: Colorectal Cancer, Incidence, Mortality, Predictive preventive personalized medicine, Precision medicine, GLOBOCAN
Introduction
Globally, the burden of communicable diseases has been falling, and mortality and morbidity due to noncommunicable diseases have been rising since the last three decades [1]. The burden of communicable diseases has been proved to be amenable to interventions such as vaccination, public hygiene, and improvement in basic healthcare infrastructure. This, however, is not true for noncommunicable diseases such as cancer which lack an easy solution as a vaccine to treat every kind of neoplasia. Colorectal cancer (CRC) is one of the amenable causes of death and also has been one of the leading cancer groups causing substantial mortality and morbidity worldwide [1, 2]. CRC was previously considered to be a disease of affluence, but as the countries are climbing up the development hierarchy, its burden has risen sharply in developing countries exemplified by surges in countries such as Japan, Singapore and China [3]. Although the CRC burden has been the greatest in developed countries and rising in developing ones, survival rates, which depend crucially upon the stage of diagnosis, are significantly different in countries with different socioeconomic level [4]. The heterogeneous patterns of incidence, mortality, and survival implicate a gap in cancer detection and treatment in countries as per their socioeconomic status.
The majority of colorectal neoplasia are adenocarcinomas originating from epithelial cells of the colorectal mucosa; other rare types include neuroendocrine, squamous cell, adeno-squamous, spindle cell, and undifferentiated carcinomas [5]. Around 80–90% of newly diagnosed cases are sporadic with slow growth from adenomatous polyps to adenoma to adenocarcinoma while the rest (10–20%) is related to familial histories such as familial adenomatous polyposis (FAP) and hereditary nonpolyposis (HNPCC) [6]. The slow march of cancer from polyps to frank carcinoma can be arrested by employing screening methods such as stool-based procedures (e.g., fecal occult blood test and fecal immunochemical test) and structural examinations (e.g., colonoscopy, flexible sigmoidoscopy), thereby resulting in improved survival and low mortality rates [7].
Tackling the burden of a disease as complex as cancer requires new-age strategies such as predictive, preventive, and personalized medicine (PPPM) which is aiming to shift the focus of cancer therapeutics from reactive to a preventive and predictive one to provide individualized treatment paradigms to cancer patients [8–10]. In cancer management, this approach seeks to separate a healthy person from a patient, low-risk individual from the at-risk population, and a low-grade tumor from a high-grade tumor to offer precise and personalized medicine [8]. To devise proper cancer policy and implement PPPM strategies at the patient or provider level, it is pertinent to examine the recent estimates of the burden of cancer-in-question (CRC here) at the macro-level.
In this study, we examined the CRC burden using estimates from GLOBOCAN 2018 which produced country-, age-, and sex-wise estimates of the incidence, mortality, and prevalence of colorectal carcinoma in 185 countries for the year 2018 [11]. The socioeconomic status of a nation was gauged using country-level human development index (HDI)—a summary indicator of income, education, and longevity [12]. Five-year survival rate due to CRC was proxied using mortality-to-incidence ratio (MIR) which has been employed as the proxy of survival rates before [13–16]. An examination of CRC burden is expected to aid policy making and devise appropriate policy interventions to tackle a public health threat that is growing but is also amenable to prevention and early detection.
Data and methods
We procured the estimates of CRC burden from GLOBOCAN 2018, which provided age-, sex-, and country-wise incidence, mortality, and prevalence estimates of 36 neoplasia for 185 countries for the year 2018 [11, 17]. GLOBOCAN 2018 provided incidence and mortality estimates for each cancer group for 21 regions defined by United Nations Population Division (UNPD) in 18 nonoverlapping age groups (0–4, 5–9, 10–14, 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80–84, and > 85 years). The complete GLOBOCAN 2018 estimation framework and calculation of various population health metrics are detailed elsewhere [11, 17]. The full set of GLOBOCAN 2018 results is available in the Global Cancer Observatory (http://gco.iarc.fr [18]). We procured data of CRC encoded as C18-C21 (colon, rectum, and anus) as per International Classification of Diseases tenth revision (ICD-10). In this study, we examine the CRC burden in terms of all-age incidence and mortality along with age-standardized rates expressed in terms of 100,000 person-years. The age-standardized incidence rate (ASIR) of a country was calculated using following formula.
| 1 |
In the above equation, i indexes the country and j indexes the age group. Cij denotes number of cases in jth age group in ith country, Pij denotes population in ith country in jth age group, TPi denotes total population of ith country and wj is the weight of jth age group ascribed by world population reference standard. The age-standardized mortality rate (ASMR) for different countries was calculated similarly by replacing number of cases (Cij) by number of deaths (Dij) in equation 1.
The 5-year survival rate of CRC was proxied using mortality-to-incidence ratio (MIR), which was calculated as the ratio of all-age death counts to all-age incident cases. MIR has been previously employed as a proxy for 5-year survival rate in the case of different neoplasia [13–16]. While we report estimates for all 185 countries, we focus primarily on the heavily burdened countries and regions. In addition to examining the country-wise burden of colorectal carcinoma, we also examined its relationship with a country’s socioeconomic status measured using its human development index (HDI) [12, 19]. HDI, an indicator of human development constructed by United N ations Development Program (UNDP), is a summary index of three indicators: health (life expectancy at birth), education (mean years of schooling and expected number of years of schooling)1, and income (gross national income (GNI) per capita)[12]. Country-specific value for each of the indicators was rescaled by UNDP on 0 to 1 scale with 0 corresponding to the lowest value and 1 to the highest reported value of the variable and the final HDI of a country is calculated as the geometric mean of the three indicators [12] using the following equation:
| 2 |
In the above equation, II is the income index, EI denotes the education index, and HI denotes the health index. As GLOBOCAN estimates were available for the year 2018, and HDI data was available for 2017, we extrapolated the values of HDI for the year 2018 using the country-specific HDI values in the years 2016 and 2017. It was done to make the HDI values consistent with the values of CRC burden in the year 2018. Data analysis was conducted using Python 3.6, MS Excel 2016, and Stata 13.0 statistical software.
Results
Globally, there were an estimated 1.85 million newly diagnosed CRC cases with ASIR estimated to be 19.7 per 100,000 person-years in 2018. Sex-wise, there were 1.03 million incident cases in males and 823,303 cases in females (Table 1). CRC claimed an estimated 880,792 lives in 2018, out of which there were 484,224 males and 396,568 females. The ASMR was estimated to be8.9 per 100,000 person-years in 2018. Region-wise, colorectal cancer burden was the highest in East Asia with 736,573 incident cases (males 426,342 and females 310,231) and 325,128 deaths (males 183,346 and females 141,782). In terms of all-age incidence, North America ranked second with 179,771 cases (93,898 males; 85,873 females) followed by central and eastern Europe with 164,998 (males 84,951 and females 80,047) cases. In terms of deaths, however, central and eastern Europe ranked second after East Asia with 94,545 deaths (males 48,025 and females 46,520). Country-wise, China ranked first with 521,490 cases and 247,563 deaths followed by the USA with 155,098 cases and 54,611 deaths in 2018 (Table 1).
Table 1.
Colon and rectum cancer burden in 185 countries, 2018
| Incidence | ASIR | Deaths | ASMR | MIR | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Population | T | M | F | T | M | F | T | M | F | T | M | F | T | M | F |
| Australia/New Zealand | 21,217 | 11,444 | 9773 | 36.7 | 41.7 | 32.1 | 7424 | 3893 | 3531 | 11.1 | 12.9 | 9.5 | 0.35 | 0.34 | 0.36 |
| Australia | 17,782 | 9643 | 8139 | 36.9 | 41.9 | 32.4 | 6131 | 3237 | 2894 | 10.9 | 12.8 | 9.2 | 0.34 | 0.34 | 0.36 |
| New Zealand | 3435 | 1801 | 1634 | 35.3 | 40.2 | 30.8 | 1293 | 656 | 637 | 12.1 | 13.4 | 10.9 | 0.38 | 0.36 | 0.39 |
| Caribbean | 10,886 | 5016 | 5870 | 17.9 | 17.9 | 17.8 | 6259 | 2898 | 3361 | 9.6 | 9.9 | 9.3 | 0.57 | 0.58 | 0.57 |
| Bahamas | 115 | 60 | 55 | 22.2 | 26.4 | 19.4 | 50 | 28 | 22 | 9.3 | 12.3 | 7.4 | 0.43 | 0.47 | 0.4 |
| Barbados | 219 | 118 | 101 | 38.9 | 50.3 | 28.8 | 101 | 53 | 48 | 16.6 | 21.4 | 12.4 | 0.46 | 0.45 | 0.48 |
| Cuba | 4238 | 1811 | 2427 | 17.6 | 16.1 | 18.9 | 2811 | 1228 | 1583 | 10.7 | 10.2 | 11.1 | 0.66 | 0.68 | 0.65 |
| Dominican Republic | 1489 | 730 | 759 | 13.4 | 13.9 | 12.9 | 858 | 428 | 430 | 7.4 | 7.9 | 6.9 | 0.58 | 0.59 | 0.57 |
| France, Guadeloupe | 183 | 89 | 94 | 19.8 | 21.2 | 18.5 | 104 | 61 | 43 | 9.4 | 13.1 | 6.4 | 0.57 | 0.69 | 0.46 |
| France, Martinique | 214 | 111 | 103 | 23.9 | 29 | 19.8 | 110 | 56 | 54 | 10.9 | 13.3 | 9 | 0.51 | 0.5 | 0.52 |
| Haiti | 949 | 406 | 543 | 10.8 | 9.9 | 11.7 | 656 | 267 | 389 | 7.5 | 6.7 | 8.3 | 0.69 | 0.66 | 0.72 |
| Jamaica | 953 | 380 | 573 | 24.9 | 21.3 | 28.2 | 467 | 186 | 281 | 11.2 | 9.8 | 12.4 | 0.49 | 0.49 | 0.49 |
| Puerto Rico | 1823 | 979 | 844 | 27.3 | 34.1 | 22.1 | 736 | 414 | 322 | 9.8 | 13.4 | 7.1 | 0.4 | 0.42 | 0.38 |
| Saint Lucia | 36 | 16 | 20 | 14.5 | 13.3 | 16 | 20 | 10 | 10 | 8 | 8.2 | 7.9 | 0.56 | 0.63 | 0.5 |
| Trinidad and Tobago | 381 | 191 | 190 | 19.4 | 21.5 | 17.5 | 188 | 96 | 92 | 9.3 | 10.8 | 8 | 0.49 | 0.5 | 0.48 |
| Central America | 19,520 | 9959 | 9561 | 11 | 12.1 | 10 | 9614 | 4910 | 4704 | 5.3 | 5.9 | 4.7 | 0.49 | 0.49 | 0.49 |
| Belize | 24 | 11 | 13 | 9.7 | 9.2 | 10 | 15 | 7 | 8 | 6.3 | 6.2 | 6.3 | 0.63 | 0.64 | 0.62 |
| Costa Rica | 1128 | 560 | 568 | 16.7 | 17.6 | 15.9 | 617 | 316 | 301 | 8.6 | 9.5 | 7.7 | 0.55 | 0.56 | 0.53 |
| El Salvador | 681 | 267 | 414 | 9 | 8.9 | 9.1 | 367 | 143 | 224 | 4.6 | 4.5 | 4.7 | 0.54 | 0.54 | 0.54 |
| Guatemala | 802 | 368 | 434 | 6.3 | 6.3 | 6.3 | 450 | 206 | 244 | 3.5 | 3.5 | 3.4 | 0.56 | 0.56 | 0.56 |
| Honduras | 573 | 286 | 287 | 8.2 | 9 | 7.6 | 340 | 175 | 165 | 4.5 | 4.9 | 4.1 | 0.59 | 0.61 | 0.57 |
| Mexico | 14,900 | 7795 | 7105 | 11.2 | 12.5 | 10 | 7084 | 3719 | 3365 | 5.2 | 5.9 | 4.6 | 0.48 | 0.48 | 0.47 |
| Nicaragua | 631 | 250 | 381 | 11.3 | 10.2 | 12.2 | 367 | 145 | 222 | 6.5 | 5.9 | 6.9 | 0.58 | 0.58 | 0.58 |
| Panama | 781 | 422 | 359 | 16.2 | 18.5 | 14.1 | 374 | 199 | 175 | 7.4 | 8.4 | 6.5 | 0.48 | 0.47 | 0.49 |
| Central and Eastern Europe | 164,998 | 84,951 | 80,047 | 28.8 | 37.5 | 23.2 | 94,545 | 48,025 | 46,520 | 15.2 | 20.5 | 11.9 | 0.57 | 0.57 | 0.58 |
| Belarus | 5680 | 2802 | 2878 | 31.8 | 41.6 | 26 | 2919 | 1315 | 1604 | 15.1 | 19.2 | 12.8 | 0.51 | 0.47 | 0.56 |
| Bulgaria | 4604 | 2724 | 1880 | 28.5 | 38.3 | 20.7 | 2714 | 1642 | 1072 | 14.9 | 21.3 | 10 | 0.59 | 0.6 | 0.57 |
| Czechia | 7838 | 4538 | 3300 | 32.7 | 42.5 | 24.9 | 3421 | 1974 | 1447 | 12.7 | 17.4 | 9.1 | 0.44 | 0.43 | 0.44 |
| Hungary | 10,809 | 6115 | 4694 | 51.2 | 70.6 | 36.8 | 5076 | 2867 | 2209 | 21.5 | 31.2 | 14.8 | 0.47 | 0.47 | 0.47 |
| Moldova | 2171 | 1241 | 930 | 34.2 | 47.3 | 25.2 | 1202 | 699 | 503 | 18.7 | 26.9 | 13.2 | 0.55 | 0.56 | 0.54 |
| Poland | 24,507 | 14,027 | 10,480 | 30.3 | 41.1 | 22.1 | 14,362 | 8104 | 6258 | 16.1 | 22.6 | 11.4 | 0.59 | 0.58 | 0.6 |
| Romania | 11,076 | 6500 | 4576 | 26.7 | 36.3 | 19.3 | 6319 | 3702 | 2617 | 13.7 | 19.2 | 9.5 | 0.57 | 0.57 | 0.57 |
| Russian Federation | 71,406 | 33,095 | 38,311 | 26.7 | 32.9 | 23.2 | 42,349 | 19,430 | 22,919 | 14.7 | 18.9 | 12.3 | 0.59 | 0.59 | 0.6 |
| Slovakia | 4624 | 2724 | 1900 | 43.8 | 60.7 | 31.2 | 2396 | 1376 | 1020 | 20.4 | 29.5 | 14.4 | 0.52 | 0.51 | 0.54 |
| Ukraine | 22,283 | 11,185 | 11,098 | 25.8 | 33.6 | 21.1 | 13,787 | 6916 | 6871 | 15.1 | 20.3 | 11.9 | 0.62 | 0.62 | 0.62 |
| Eastern Africa | 17,125 | 7933 | 9192 | 7.7 | 7.8 | 7.7 | 12,201 | 5802 | 6399 | 5.7 | 6 | 5.5 | 0.71 | 0.73 | 0.7 |
| Burundi | 418 | 193 | 225 | 8.3 | 7.7 | 8.8 | 357 | 166 | 191 | 7.4 | 7 | 7.6 | 0.85 | 0.86 | 0.85 |
| Comoros | 18 | 8 | 10 | 4.3 | 4.1 | 4.5 | 18 | 8 | 10 | 4.3 | 4.1 | 4.5 | 1 | 1 | 1 |
| Djibouti | 41 | 20 | 21 | 5.6 | 5.8 | 5.5 | 34 | 18 | 16 | 4.9 | 5.4 | 4.4 | 0.83 | 0.9 | 0.76 |
| Eritrea | 189 | 95 | 94 | 6.3 | 7 | 5.8 | 149 | 77 | 72 | 5.2 | 5.9 | 4.7 | 0.79 | 0.81 | 0.77 |
| Ethiopia | 4716 | 2206 | 2510 | 7.5 | 7.8 | 7.4 | 3555 | 1745 | 1810 | 5.8 | 6.3 | 5.5 | 0.75 | 0.79 | 0.72 |
| France, La Réunion | 349 | 186 | 163 | 25.2 | 29.2 | 21.6 | 143 | 72 | 71 | 9.3 | 10.9 | 7.9 | 0.41 | 0.39 | 0.44 |
| Kenya | 2316 | 1134 | 1182 | 9.3 | 10 | 8.7 | 1466 | 738 | 728 | 6 | 6.8 | 5.4 | 0.63 | 0.65 | 0.62 |
| Madagascar | 827 | 366 | 461 | 6.1 | 5.5 | 6.5 | 579 | 258 | 321 | 4.4 | 4.2 | 4.7 | 0.7 | 0.7 | 0.7 |
| Malawi | 354 | 171 | 183 | 3.5 | 3.9 | 3.3 | 239 | 119 | 120 | 2.5 | 2.9 | 2.2 | 0.68 | 0.7 | 0.66 |
| Mauritius | 288 | 156 | 132 | 14.7 | 17.4 | 12.6 | 173 | 92 | 81 | 8.6 | 10.3 | 7.1 | 0.6 | 0.59 | 0.61 |
| Mozambique | 561 | 278 | 283 | 3.3 | 3.7 | 3 | 451 | 224 | 227 | 2.8 | 3.2 | 2.5 | 0.8 | 0.81 | 0.8 |
| Rwanda | 838 | 355 | 483 | 13.4 | 12.6 | 14.1 | 592 | 258 | 334 | 9.8 | 9.7 | 10 | 0.71 | 0.73 | 0.69 |
| Somalia | 599 | 298 | 301 | 8 | 8.4 | 7.6 | 539 | 273 | 266 | 7.4 | 7.9 | 6.9 | 0.9 | 0.92 | 0.88 |
| South Sudan | 509 | 256 | 253 | 7.1 | 7.5 | 6.7 | 420 | 216 | 204 | 6 | 6.6 | 5.5 | 0.83 | 0.84 | 0.81 |
| Tanzania | 2594 | 1004 | 1590 | 9 | 7.4 | 10.4 | 1767 | 704 | 1063 | 6.3 | 5.5 | 7 | 0.68 | 0.7 | 0.67 |
| Uganda | 1345 | 655 | 690 | 8.1 | 8.3 | 7.9 | 961 | 458 | 503 | 6.2 | 6.4 | 5.9 | 0.71 | 0.7 | 0.73 |
| Zambia | 355 | 163 | 192 | 4.6 | 4.9 | 4.4 | 202 | 103 | 99 | 2.8 | 3.2 | 2.4 | 0.57 | 0.63 | 0.52 |
| Zimbabwe | 793 | 382 | 411 | 10.1 | 11.6 | 9.1 | 549 | 269 | 280 | 7.2 | 8.4 | 6.3 | 0.69 | 0.7 | 0.68 |
| Eastern Asia | 736,573 | 426,342 | 310,231 | 26.5 | 32 | 21.3 | 325,128 | 183,346 | 141,782 | 10.9 | 13.3 | 8.7 | 0.44 | 0.43 | 0.46 |
| China | 521,490 | 303,853 | 217,637 | 23.7 | 28.1 | 19.4 | 247,563 | 142,476 | 105,087 | 10.9 | 13.1 | 8.8 | 0.47 | 0.47 | 0.48 |
| Japan | 148,151 | 82,641 | 65,510 | 38.9 | 49.1 | 29.6 | 57,910 | 30,228 | 27,682 | 12 | 15.2 | 9.2 | 0.39 | 0.37 | 0.42 |
| North Korea | 6566 | 3266 | 3300 | 18.8 | 22.7 | 15.8 | 3112 | 1415 | 1697 | 8.5 | 10.4 | 7.3 | 0.47 | 0.43 | 0.51 |
| South Korea | 42,363 | 26,143 | 16,220 | 44.5 | 59.5 | 31.3 | 9762 | 5445 | 4317 | 8.7 | 11.8 | 6.3 | 0.23 | 0.21 | 0.27 |
| Mongolia | 146 | 67 | 79 | 6.2 | 6.5 | 6 | 88 | 42 | 46 | 3.8 | 4 | 3.6 | 0.6 | 0.63 | 0.58 |
| Melanesia | 906 | 557 | 349 | 12.8 | 17.8 | 9 | 561 | 372 | 189 | 8.1 | 12.3 | 4.9 | 0.62 | 0.67 | 0.54 |
| Fiji | 86 | 43 | 43 | 10.1 | 11.3 | 9.3 | 50 | 27 | 23 | 6.2 | 7.9 | 5.2 | 0.58 | 0.63 | 0.53 |
| France, New Caledonia | 101 | 59 | 42 | 25.8 | 31.7 | 20.5 | 34 | 23 | 11 | 9 | 13 | 5.6 | 0.34 | 0.39 | 0.26 |
| Papua New Guinea | 684 | 439 | 245 | 13 | 19.3 | 8.4 | 447 | 307 | 140 | 8.7 | 14 | 4.8 | 0.65 | 0.7 | 0.57 |
| Solomon Islands | 25 | 12 | 13 | 7 | 7.3 | 6.6 | 21 | 11 | 10 | 5.9 | 6.7 | 5.1 | 0.84 | 0.92 | 0.77 |
| Vanuatu | 10 | 4 | 6 | 5.1 | 4.3 | 5.9 | 9 | 4 | 5 | 4.6 | 4.3 | 5 | 0.9 | 1 | 0.83 |
| Micronesia | 96 | 55 | 41 | 17.4 | 20.9 | 13.9 | 51 | 31 | 20 | 9.5 | 12.5 | 6.8 | 0.53 | 0.56 | 0.49 |
| Guam | 38 | 21 | 17 | 17.2 | 20.1 | 14.6 | 20 | 12 | 8 | 9.1 | 11.6 | 7.1 | 0.53 | 0.57 | 0.47 |
| Middle Africa | 6010 | 2895 | 3115 | 7.5 | 7.8 | 7.3 | 4562 | 2232 | 2330 | 5.9 | 6.3 | 5.6 | 0.76 | 0.77 | 0.75 |
| Angola | 733 | 374 | 359 | 5.3 | 6 | 4.8 | 480 | 254 | 226 | 3.6 | 4.3 | 3.1 | 0.65 | 0.68 | 0.63 |
| Cameroon | 871 | 450 | 421 | 6.9 | 7.7 | 6.3 | 609 | 322 | 287 | 5 | 5.8 | 4.4 | 0.7 | 0.72 | 0.68 |
| Central African Republic | 151 | 78 | 73 | 5.8 | 6.5 | 5.2 | 139 | 73 | 66 | 5.4 | 6.3 | 4.8 | 0.92 | 0.94 | 0.9 |
| Chad | 413 | 214 | 199 | 5.9 | 6.6 | 5.3 | 325 | 169 | 156 | 5 | 5.6 | 4.5 | 0.79 | 0.79 | 0.78 |
| Congo | 152 | 81 | 71 | 5 | 5.7 | 4.5 | 102 | 56 | 46 | 3.5 | 4.1 | 3 | 0.67 | 0.69 | 0.65 |
| Democratic Republic of Congo | 3568 | 1627 | 1941 | 9.1 | 9 | 9.2 | 2831 | 1314 | 1517 | 7.4 | 7.5 | 7.3 | 0.79 | 0.81 | 0.78 |
| Equatorial Guinea | 40 | 24 | 16 | 5.8 | 6.4 | 5.2 | 30 | 18 | 12 | 5 | 5.8 | 4.2 | 0.75 | 0.75 | 0.75 |
| Gabon | 82 | 47 | 35 | 5.5 | 6.3 | 4.9 | 46 | 26 | 20 | 3.3 | 3.8 | 3 | 0.56 | 0.55 | 0.57 |
| Sao Tome and Principe | 5 | 3 | 2 | 6.6 | 9.5 | 4.4 | 3 | 2 | 1 | 4.1 | 6.6 | 2.2 | 0.6 | 0.67 | 0.5 |
| North America | 179,771 | 93,898 | 85,873 | 26.2 | 29.5 | 23.2 | 64,121 | 33,752 | 30,369 | 8.4 | 9.9 | 7.1 | 0.36 | 0.36 | 0.35 |
| Canada | 24,617 | 13,039 | 11,578 | 31.5 | 35.2 | 28 | 9494 | 5086 | 4408 | 10.1 | 12.2 | 8.2 | 0.39 | 0.39 | 0.38 |
| USA | 155,098 | 80,829 | 74,269 | 25.6 | 28.8 | 22.6 | 54,611 | 28,658 | 25,953 | 8.2 | 9.6 | 6.9 | 0.35 | 0.35 | 0.35 |
| Northern Africa | 18,810 | 9696 | 9114 | 9.2 | 10 | 8.6 | 10,902 | 5801 | 5101 | 5.4 | 6.1 | 4.7 | 0.58 | 0.6 | 0.56 |
| Algeria | 5537 | 2910 | 2627 | 13.9 | 14.8 | 13 | 3027 | 1684 | 1343 | 7.5 | 8.5 | 6.6 | 0.55 | 0.58 | 0.51 |
| Egypt | 5393 | 2661 | 2732 | 6.5 | 6.6 | 6.3 | 3041 | 1487 | 1554 | 3.7 | 3.8 | 3.5 | 0.56 | 0.56 | 0.57 |
| Libya | 675 | 309 | 366 | 12.6 | 13 | 12.5 | 404 | 192 | 212 | 8 | 8.5 | 7.6 | 0.6 | 0.62 | 0.58 |
| Morocco | 4118 | 2205 | 1913 | 10.9 | 12.2 | 9.8 | 2462 | 1381 | 1081 | 6.5 | 7.7 | 5.4 | 0.6 | 0.63 | 0.57 |
| Sudan | 1398 | 746 | 652 | 5.4 | 6.2 | 4.7 | 1004 | 555 | 449 | 3.9 | 4.7 | 3.3 | 0.72 | 0.74 | 0.69 |
| Tunisia | 1657 | 848 | 809 | 11.9 | 13 | 11 | 950 | 493 | 457 | 6.6 | 7.5 | 5.9 | 0.57 | 0.58 | 0.56 |
| Northern Europe | 75,900 | 41,255 | 34,645 | 32.1 | 37.5 | 27.3 | 32,659 | 17,367 | 15,292 | 11.2 | 13.5 | 9.3 | 0.43 | 0.42 | 0.44 |
| Denmark | 5585 | 2966 | 2619 | 41 | 45.9 | 36.6 | 1934 | 1003 | 931 | 12 | 13.7 | 10.5 | 0.35 | 0.34 | 0.36 |
| Estonia | 942 | 416 | 526 | 29.2 | 34.8 | 25.9 | 482 | 234 | 248 | 12.5 | 17.8 | 9.5 | 0.51 | 0.56 | 0.47 |
| Finland | 3440 | 1826 | 1614 | 24.6 | 28.7 | 21.2 | 1393 | 755 | 638 | 8.6 | 10.8 | 6.8 | 0.4 | 0.41 | 0.4 |
| Iceland | 168 | 92 | 76 | 26.2 | 30.5 | 22 | 82 | 46 | 36 | 10.9 | 13.4 | 8.6 | 0.49 | 0.5 | 0.47 |
| Ireland | 2968 | 1752 | 1216 | 34 | 42.4 | 26.4 | 1207 | 686 | 521 | 12.2 | 15.2 | 9.7 | 0.41 | 0.39 | 0.43 |
| Latvia | 1550 | 735 | 815 | 33 | 42.6 | 27.7 | 706 | 321 | 385 | 12.8 | 17.3 | 10.4 | 0.46 | 0.44 | 0.47 |
| Lithuania | 1831 | 898 | 933 | 27.2 | 35.6 | 22.1 | 996 | 535 | 461 | 12.8 | 19.6 | 8.9 | 0.54 | 0.6 | 0.49 |
| Norway | 4887 | 2530 | 2357 | 42.9 | 46.9 | 39.3 | 1750 | 915 | 835 | 13.2 | 15.3 | 11.3 | 0.36 | 0.36 | 0.35 |
| Sweden | 6421 | 3370 | 3051 | 26.9 | 29.7 | 24.3 | 3062 | 1637 | 1425 | 10.6 | 12.4 | 9 | 0.48 | 0.49 | 0.47 |
| UK | 47,892 | 26,551 | 21,341 | 32.1 | 37.8 | 27 | 20,957 | 11,186 | 9771 | 11.1 | 13.3 | 9.3 | 0.44 | 0.42 | 0.46 |
| Polynesia | 113 | 67 | 46 | 16.2 | 20 | 12.4 | 30 | 23 | 7 | 4.4 | 7.4 | 2.1 | 0.27 | 0.34 | 0.15 |
| French Polynesia | 47 | 27 | 20 | 13.9 | 15.9 | 11.6 | 11 | 9 | 2 | 3.4 | 5.6 | 1.2 | 0.23 | 0.33 | 0.1 |
| Samoa | 37 | 24 | 13 | 22.6 | 30.6 | 14.8 | 13 | 8 | 5 | 7.8 | 10.9 | 6.3 | 0.35 | 0.33 | 0.38 |
| South America | 97,600 | 48,061 | 49,539 | 18.6 | 20.6 | 17.1 | 48,793 | 24,563 | 24,230 | 8.9 | 10.3 | 7.8 | 0.5 | 0.51 | 0.49 |
| Argentina | 15,692 | 8527 | 7165 | 25 | 31.5 | 20.2 | 8721 | 4751 | 3970 | 12.6 | 16.6 | 9.8 | 0.56 | 0.56 | 0.55 |
| Bolivia | 605 | 311 | 294 | 6.1 | 6.7 | 5.6 | 371 | 194 | 177 | 3.7 | 4.1 | 3.2 | 0.61 | 0.62 | 0.6 |
| Brazil | 51,783 | 24,737 | 27,046 | 19.6 | 21.1 | 18.6 | 24,482 | 12,031 | 12,451 | 9 | 10.1 | 8.1 | 0.47 | 0.49 | 0.46 |
| Chile | 5914 | 3002 | 2912 | 20.7 | 23.9 | 18.2 | 3144 | 1556 | 1588 | 10.2 | 11.9 | 8.9 | 0.53 | 0.52 | 0.55 |
| Colombia | 9140 | 4396 | 4744 | 15.8 | 16.9 | 15 | 4489 | 2203 | 2286 | 7.6 | 8.4 | 6.9 | 0.49 | 0.5 | 0.48 |
| Ecuador | 2025 | 902 | 1123 | 11.3 | 10.8 | 11.7 | 1100 | 507 | 593 | 5.8 | 5.9 | 5.8 | 0.54 | 0.56 | 0.53 |
| French Guyana | 54 | 32 | 22 | 21.7 | 26.8 | 17 | 14 | 8 | 6 | 5.8 | 7.3 | 4.3 | 0.26 | 0.25 | 0.27 |
| Guyana | 36 | 15 | 21 | 5 | 4.4 | 5.4 | 27 | 12 | 15 | 3.8 | 3.5 | 3.9 | 0.75 | 0.8 | 0.71 |
| Paraguay | 895 | 466 | 429 | 13.9 | 15 | 12.7 | 552 | 284 | 268 | 8.3 | 9 | 7.5 | 0.62 | 0.61 | 0.62 |
| Peru | 4610 | 2255 | 2355 | 13.3 | 14.2 | 12.4 | 2367 | 1220 | 1147 | 6.5 | 7.5 | 5.7 | 0.51 | 0.54 | 0.49 |
| Suriname | 94 | 51 | 43 | 15.4 | 18.8 | 12.7 | 70 | 38 | 32 | 11.3 | 14.1 | 8.9 | 0.74 | 0.75 | 0.74 |
| Uruguay | 2273 | 1152 | 1121 | 35 | 43.8 | 28.3 | 1093 | 555 | 538 | 15 | 19.3 | 12.1 | 0.48 | 0.48 | 0.48 |
| Venezuela | 4479 | 2215 | 2264 | 13.6 | 14.8 | 12.6 | 2363 | 1204 | 1159 | 7.1 | 8.1 | 6.2 | 0.53 | 0.54 | 0.51 |
| South-Eastern Asia | 95,223 | 53,542 | 41,681 | 14.3 | 17.6 | 11.6 | 52,475 | 29,384 | 23,091 | 7.9 | 9.9 | 6.3 | 0.55 | 0.55 | 0.55 |
| Brunei | 140 | 84 | 56 | 35 | 43.4 | 27.4 | 50 | 32 | 18 | 13.9 | 18.5 | 9.8 | 0.36 | 0.38 | 0.32 |
| Cambodia | 1314 | 637 | 677 | 11.1 | 13 | 9.9 | 859 | 414 | 445 | 7.5 | 8.8 | 6.7 | 0.65 | 0.65 | 0.66 |
| Indonesia | 30,017 | 19,113 | 10,904 | 12.1 | 16.2 | 8.4 | 16,386 | 10,279 | 6107 | 6.9 | 9.3 | 4.8 | 0.55 | 0.54 | 0.56 |
| Lao PDR | 652 | 326 | 326 | 13.9 | 14.9 | 13.1 | 394 | 197 | 197 | 8.6 | 9.4 | 8 | 0.6 | 0.6 | 0.6 |
| Malaysia | 6137 | 3342 | 2795 | 19.9 | 22 | 17.9 | 3414 | 1863 | 1551 | 11.2 | 12.5 | 9.9 | 0.56 | 0.56 | 0.55 |
| Myanmar | 4751 | 2600 | 2151 | 9.1 | 11.1 | 7.6 | 2960 | 1606 | 1354 | 5.8 | 7.1 | 4.8 | 0.62 | 0.62 | 0.63 |
| Philippines | 15,680 | 8791 | 6889 | 18.9 | 23.5 | 15.2 | 8821 | 4841 | 3980 | 11 | 13.9 | 8.9 | 0.56 | 0.55 | 0.58 |
| Singapore | 4202 | 1994 | 2208 | 36.8 | 38.9 | 34 | 1980 | 1050 | 930 | 17.3 | 20.2 | 14.6 | 0.47 | 0.53 | 0.42 |
| Thailand | 17,534 | 9015 | 8519 | 15.5 | 17.6 | 13.9 | 9462 | 4963 | 4499 | 8.4 | 9.7 | 7.4 | 0.54 | 0.55 | 0.53 |
| Timor-Leste | 63 | 33 | 30 | 8.9 | 9.7 | 8.1 | 45 | 23 | 22 | 6.5 | 7.1 | 5.9 | 0.71 | 0.7 | 0.73 |
| Viet Nam | 14,733 | 7607 | 7126 | 13.4 | 16 | 11.6 | 8104 | 4116 | 3988 | 7 | 8.7 | 5.9 | 0.55 | 0.54 | 0.56 |
| Southern Africa | 7167 | 3637 | 3530 | 13.4 | 16.8 | 11.2 | 3801 | 1979 | 1822 | 7.1 | 9.5 | 5.7 | 0.53 | 0.54 | 0.52 |
| Botswana | 53 | 35 | 18 | 2.9 | 4.9 | 1.6 | 28 | 20 | 8 | 1.7 | 3.2 | 0.8 | 0.53 | 0.57 | 0.44 |
| Eswatini | 30 | 16 | 14 | 3.6 | 4.6 | 2.9 | 18 | 11 | 7 | 2.4 | 3.5 | 1.7 | 0.6 | 0.69 | 0.5 |
| Lesotho | 47 | 27 | 20 | 3.1 | 4.4 | 2.4 | 35 | 21 | 14 | 2.5 | 3.6 | 1.8 | 0.74 | 0.78 | 0.7 |
| Namibia | 100 | 51 | 49 | 6.3 | 7.3 | 5.5 | 56 | 29 | 27 | 3.6 | 4.3 | 3.1 | 0.56 | 0.57 | 0.55 |
| South Africa | 6937 | 3508 | 3429 | 14.4 | 18.1 | 12 | 3664 | 1898 | 1766 | 7.6 | 10.2 | 6.1 | 0.53 | 0.54 | 0.52 |
| South-Central Asia | 88,033 | 53,534 | 34,499 | 4.9 | 6.1 | 3.8 | 63,401 | 39,852 | 23,549 | 3.6 | 4.6 | 2.6 | 0.72 | 0.74 | 0.68 |
| Afghanistan | 805 | 487 | 318 | 4 | 4.7 | 3.4 | 709 | 436 | 273 | 3.7 | 4.2 | 3 | 0.88 | 0.9 | 0.86 |
| Bangladesh | 5549 | 3164 | 2385 | 3.8 | 4.3 | 3.3 | 4469 | 2605 | 1864 | 3 | 3.5 | 2.6 | 0.81 | 0.82 | 0.78 |
| Bhutan | 30 | 23 | 7 | 4.2 | 6 | 2.1 | 24 | 19 | 5 | 3.7 | 5.5 | 1.6 | 0.8 | 0.83 | 0.71 |
| India | 56,751 | 36,687 | 20,064 | 4.4 | 5.8 | 3.1 | 43,090 | 28,591 | 14,499 | 3.4 | 4.6 | 2.2 | 0.76 | 0.78 | 0.72 |
| Iran | 9864 | 5630 | 4234 | 12.9 | 14.6 | 11.1 | 4153 | 2395 | 1758 | 5.6 | 6.3 | 4.8 | 0.42 | 0.43 | 0.42 |
| Kazakhstan | 3049 | 1392 | 1657 | 15.4 | 17.7 | 14.1 | 2108 | 1023 | 1085 | 10.5 | 13.3 | 8.9 | 0.69 | 0.73 | 0.65 |
| Kyrgyzstan | 352 | 174 | 178 | 7.3 | 8.1 | 6.5 | 274 | 136 | 138 | 5.7 | 6.4 | 5 | 0.78 | 0.78 | 0.78 |
| Maldives | 41 | 30 | 11 | 11.9 | 15.9 | 7.2 | 20 | 17 | 3 | 6.3 | 10.5 | 1.8 | 0.49 | 0.57 | 0.27 |
| Nepal | 1432 | 514 | 918 | 5.8 | 4.4 | 7 | 1191 | 449 | 742 | 4.8 | 3.9 | 5.7 | 0.83 | 0.87 | 0.81 |
| Pakistan | 6475 | 3587 | 2888 | 4.2 | 4.5 | 3.8 | 5003 | 2822 | 2181 | 3.3 | 3.7 | 3 | 0.77 | 0.79 | 0.76 |
| Sri Lanka | 1441 | 734 | 707 | 5.2 | 5.8 | 4.7 | 968 | 518 | 450 | 3.4 | 4 | 2.9 | 0.67 | 0.71 | 0.64 |
| Tajikistan | 263 | 165 | 98 | 4 | 4.9 | 3.1 | 207 | 131 | 76 | 3.1 | 4 | 2.4 | 0.79 | 0.79 | 0.78 |
| Turkmenistan | 278 | 134 | 144 | 6 | 6.7 | 5.6 | 168 | 87 | 81 | 3.7 | 4.2 | 3.2 | 0.6 | 0.65 | 0.56 |
| Uzbekistan | 1703 | 813 | 890 | 6.3 | 6.5 | 6 | 1017 | 623 | 394 | 3.8 | 5.1 | 2.7 | 0.6 | 0.77 | 0.44 |
| Southern Europe | 119,949 | 69,446 | 50,503 | 31.6 | 40.4 | 24.1 | 53,975 | 30,991 | 22,984 | 11.5 | 15.4 | 8.4 | 0.45 | 0.45 | 0.46 |
| Albania | 402 | 225 | 177 | 8.4 | 9.6 | 7.2 | 198 | 115 | 83 | 3.7 | 4.5 | 3 | 0.49 | 0.51 | 0.47 |
| Bosnia and Herzegovina | 1818 | 1046 | 772 | 26.1 | 33 | 20.4 | 1081 | 628 | 453 | 13.3 | 18.2 | 9.4 | 0.59 | 0.6 | 0.59 |
| Croatia | 3387 | 1951 | 1436 | 34.1 | 45.9 | 24.9 | 2187 | 1288 | 899 | 18.9 | 27.4 | 12.7 | 0.65 | 0.66 | 0.63 |
| Greece | 7319 | 4158 | 3161 | 26.2 | 32.3 | 21.1 | 3430 | 1985 | 1445 | 9.7 | 12.7 | 7.3 | 0.47 | 0.48 | 0.46 |
| Italy | 49,327 | 26,930 | 22,397 | 29.9 | 36 | 24.8 | 21,172 | 11,491 | 9681 | 10.2 | 12.8 | 8 | 0.43 | 0.43 | 0.43 |
| Macedonia FYR | 996 | 517 | 479 | 28.4 | 30.9 | 26.3 | 472 | 248 | 224 | 12.5 | 14.2 | 11.1 | 0.47 | 0.48 | 0.47 |
| Malta | 302 | 180 | 122 | 29.1 | 36 | 23.2 | 121 | 70 | 51 | 10.6 | 13.2 | 8.6 | 0.4 | 0.39 | 0.42 |
| Montenegro | 210 | 115 | 95 | 18.6 | 22.7 | 14.9 | 115 | 62 | 53 | 9.2 | 11.2 | 7.5 | 0.55 | 0.54 | 0.56 |
| Portugal | 10,270 | 6104 | 4166 | 40 | 54 | 28.7 | 4261 | 2497 | 1764 | 13.5 | 18.7 | 9.6 | 0.41 | 0.41 | 0.42 |
| Serbia | 6149 | 3775 | 2374 | 36.7 | 49 | 26.4 | 3232 | 1966 | 1266 | 16.8 | 23.3 | 11.6 | 0.53 | 0.52 | 0.53 |
| Slovenia | 1987 | 1301 | 686 | 41.1 | 58.9 | 25.5 | 740 | 423 | 317 | 12.5 | 17.1 | 8.9 | 0.37 | 0.33 | 0.46 |
| Spain | 37,172 | 22,744 | 14,428 | 33.4 | 45.2 | 23.3 | 16,683 | 10,038 | 6645 | 12 | 16.8 | 8 | 0.45 | 0.44 | 0.46 |
| Western Africa | 12,734 | 6489 | 6245 | 6.4 | 6.8 | 6.1 | 8568 | 4440 | 4128 | 4.5 | 4.9 | 4.2 | 0.67 | 0.68 | 0.66 |
| Benin | 433 | 274 | 159 | 6.8 | 9.5 | 4.6 | 299 | 190 | 109 | 4.8 | 6.8 | 3.2 | 0.69 | 0.69 | 0.69 |
| Burkina Faso | 583 | 243 | 340 | 6.3 | 5.5 | 6.7 | 463 | 194 | 269 | 5.3 | 4.8 | 5.6 | 0.79 | 0.8 | 0.79 |
| Cabo Verde | 30 | 9 | 21 | 6.4 | 7.3 | 6.3 | 21 | 6 | 15 | 4.2 | 4.2 | 4.3 | 0.7 | 0.67 | 0.71 |
| Côte d’Ivoire | 737 | 333 | 404 | 5.8 | 4.9 | 6.9 | 552 | 259 | 293 | 4.5 | 3.9 | 5.2 | 0.75 | 0.78 | 0.73 |
| Gambia | 11 | 9 | 2 | 1.1 | 1.7 | 0.48 | 9 | 7 | 2 | 0.98 | 1.5 | 0.48 | 0.82 | 0.78 | 1 |
| Ghana | 1228 | 658 | 570 | 7.8 | 9.6 | 6.6 | 824 | 467 | 357 | 5.5 | 7.1 | 4.2 | 0.67 | 0.71 | 0.63 |
| Guinea | 145 | 77 | 68 | 2 | 2.1 | 1.8 | 118 | 65 | 53 | 1.7 | 1.9 | 1.5 | 0.81 | 0.84 | 0.78 |
| Guinea-Bissau | 61 | 30 | 31 | 6.1 | 7.1 | 5.5 | 53 | 28 | 25 | 5.6 | 6.9 | 4.7 | 0.87 | 0.93 | 0.81 |
| Liberia | 102 | 43 | 59 | 3.9 | 3.4 | 4.3 | 84 | 37 | 47 | 3.4 | 3 | 3.6 | 0.82 | 0.86 | 0.8 |
| Mali | 917 | 385 | 532 | 10.5 | 9 | 11.7 | 686 | 290 | 396 | 8.3 | 7.3 | 9.1 | 0.75 | 0.75 | 0.74 |
| Mauritania | 159 | 70 | 89 | 6.1 | 5.2 | 6.7 | 111 | 48 | 63 | 4.5 | 3.8 | 4.9 | 0.7 | 0.69 | 0.71 |
| Niger | 583 | 305 | 278 | 5.3 | 5.5 | 5 | 522 | 284 | 238 | 4.9 | 5.3 | 4.5 | 0.9 | 0.93 | 0.86 |
| Nigeria | 6692 | 3568 | 3124 | 6.2 | 6.8 | 5.6 | 4059 | 2202 | 1857 | 4 | 4.5 | 3.5 | 0.61 | 0.62 | 0.59 |
| Senegal | 529 | 226 | 303 | 6.5 | 6.3 | 6.6 | 372 | 165 | 207 | 4.8 | 4.9 | 4.7 | 0.7 | 0.73 | 0.68 |
| Sierra Leone | 216 | 103 | 113 | 5.5 | 5 | 5.9 | 173 | 83 | 90 | 4.7 | 4.3 | 5 | 0.8 | 0.81 | 0.8 |
| Togo | 303 | 153 | 150 | 7.2 | 7.2 | 7.1 | 219 | 113 | 106 | 5.5 | 5.6 | 5.3 | 0.72 | 0.74 | 0.71 |
| Western Asia | 38,067 | 21,490 | 16,577 | 16.3 | 19.4 | 13.6 | 20,418 | 11,240 | 9178 | 8.7 | 10.4 | 7.3 | 0.54 | 0.52 | 0.55 |
| Armenia | 990 | 367 | 623 | 19.9 | 18.4 | 20.8 | 640 | 252 | 388 | 12.4 | 12.6 | 12.1 | 0.65 | 0.69 | 0.62 |
| Azerbaijan | 1114 | 668 | 446 | 10.2 | 13.8 | 7.4 | 774 | 482 | 292 | 7.1 | 10.2 | 4.8 | 0.69 | 0.72 | 0.65 |
| Bahrain | 120 | 72 | 48 | 12.6 | 14.2 | 11.2 | 70 | 40 | 30 | 8.1 | 8.9 | 7.6 | 0.58 | 0.56 | 0.63 |
| Cyprus | 511 | 338 | 173 | 24.2 | 34.4 | 15.3 | 242 | 154 | 88 | 10.2 | 14.6 | 6.5 | 0.47 | 0.46 | 0.51 |
| West Bank and Gaza Strip | 501 | 262 | 239 | 19.1 | 21.1 | 17.3 | 303 | 159 | 144 | 11.9 | 13.3 | 10.7 | 0.6 | 0.61 | 0.6 |
| Georgia | 645 | 331 | 314 | 8.7 | 11.1 | 7.1 | 427 | 226 | 201 | 5.7 | 7.5 | 4.4 | 0.66 | 0.68 | 0.64 |
| Iraq | 1391 | 763 | 628 | 6.1 | 7.2 | 5.2 | 813 | 446 | 367 | 3.7 | 4.4 | 3.1 | 0.58 | 0.58 | 0.58 |
| Israel | 2519 | 1336 | 1183 | 20.1 | 22.8 | 18 | 1390 | 717 | 673 | 9.3 | 11 | 7.9 | 0.55 | 0.54 | 0.57 |
| Jordan | 1105 | 460 | 645 | 17 | 14.8 | 19.2 | 589 | 257 | 332 | 9.3 | 8.5 | 10 | 0.53 | 0.56 | 0.51 |
| Kuwait | 352 | 195 | 157 | 13.2 | 12.9 | 14 | 178 | 97 | 81 | 7.5 | 7.4 | 7.9 | 0.51 | 0.5 | 0.52 |
| Lebanon | 1463 | 775 | 688 | 20 | 20.8 | 19.2 | 851 | 451 | 400 | 10.9 | 11.7 | 10.3 | 0.58 | 0.58 | 0.58 |
| Oman | 368 | 262 | 106 | 11 | 11.7 | 9.6 | 195 | 137 | 58 | 6.4 | 6.8 | 5.6 | 0.53 | 0.52 | 0.55 |
| Qatar | 142 | 100 | 42 | 13 | 13.5 | 13.8 | 79 | 54 | 25 | 8.7 | 9 | 9.5 | 0.56 | 0.54 | 0.6 |
| Saudi Arabia | 3564 | 2405 | 1159 | 13.1 | 14.9 | 10.6 | 1603 | 1077 | 526 | 6.3 | 7.3 | 5 | 0.45 | 0.45 | 0.45 |
| Syrian Arab Republic | 1890 | 870 | 1020 | 14.4 | 14.3 | 14.5 | 1248 | 583 | 665 | 9.5 | 9.7 | 9.4 | 0.66 | 0.67 | 0.65 |
| Turkey | 20,031 | 11,548 | 8483 | 21 | 27.4 | 16 | 10,033 | 5571 | 4462 | 10.2 | 13.1 | 7.9 | 0.5 | 0.48 | 0.53 |
| United Arab Emirates | 662 | 437 | 225 | 14.1 | 14.8 | 13.5 | 314 | 207 | 107 | 7.4 | 7.7 | 7.3 | 0.47 | 0.47 | 0.48 |
| Yemen | 1210 | 639 | 571 | 8.6 | 9.5 | 7.8 | 911 | 484 | 427 | 6.7 | 7.5 | 6 | 0.75 | 0.76 | 0.75 |
| Western Europe | 138,820 | 75,948 | 62,872 | 28.8 | 34.5 | 23.7 | 61,304 | 33,323 | 27,981 | 10.3 | 13.1 | 8 | 0.44 | 0.44 | 0.45 |
| Austria | 4421 | 2531 | 1890 | 20.7 | 26.3 | 16.1 | 2276 | 1318 | 958 | 8.9 | 12 | 6.2 | 0.51 | 0.52 | 0.51 |
| Belgium | 9346 | 5266 | 4080 | 35.3 | 43.8 | 28 | 3224 | 1669 | 1555 | 9.7 | 11.9 | 7.8 | 0.34 | 0.32 | 0.38 |
| France | 47,025 | 25,813 | 21,212 | 30.4 | 36.9 | 24.8 | 19,962 | 10,821 | 9141 | 10.2 | 13.1 | 7.9 | 0.42 | 0.42 | 0.43 |
| Germany | 58,047 | 31,026 | 27,021 | 26.2 | 31 | 22.1 | 27,334 | 14,931 | 12,403 | 10.1 | 13 | 7.7 | 0.47 | 0.48 | 0.46 |
| Luxembourg | 323 | 170 | 153 | 28.1 | 31.4 | 25.3 | 134 | 72 | 62 | 10.1 | 12.3 | 8.1 | 0.41 | 0.42 | 0.41 |
| Netherlands | 14,921 | 8513 | 6408 | 37.8 | 45.3 | 31.1 | 6442 | 3443 | 2999 | 13.8 | 16.5 | 11.5 | 0.43 | 0.4 | 0.47 |
| Switzerland | 4681 | 2598 | 2083 | 24 | 28.4 | 20.2 | 1909 | 1054 | 855 | 8.1 | 10.1 | 6.4 | 0.41 | 0.41 | 0.41 |
| World | 1,849,518 | 1,026,215 | 823,303 | 19.7 | 23.6 | 16.3 | 880,792 | 484,224 | 396,568 | 8.9 | 10.8 | 7.2 | 0.48 | 0.47 | 0.48 |
| t Test (male vs female) | 2.20** (0.014) | 10.27*** (0.000) | 2.14** (0.016) | 12.29*** (0.000) | 5.00*** (0.000) | ||||||||||
T: Total, both sexes, all age-groups; F: Females, all age-groups; M: Males, all age-groups; ASIR: age-standardized incidence rate per 100,000 person-years; ASMR: age-standardized mortality rate per 100,000 person-years; MIR: Mortality-to-incidence ratio. Data Source: GLOBOCAN 2018 (IARC). T-test in the last column tests for the hypothesis of M (male mean) – F (female mean) = 0 against the one-sided alternate hypothesis M-F < 0; **/*** denotes statistical significance at 5%/1% respectively
Age-standardized rates were the highest in developed regions led by Australia/New Zealand region with ASIR of 36.7/100,000 followed by northern Europe with ASIR of 32.1/100,000. ASIR was the lowest in south-central Asia at 4.9 per 100,000 person-years in 2018. ASMR was again the highest in central and eastern Europe (15.2/100,000) followed by southern Europe (11.5/100,000) with south-central Asia registering the lowest ASMR of 3.6/100,000 in 2018. Top-3 countries with highest ASIR were Hungary (51.2/100,000), South Korea (44.5 per 100,000) and Slovakia (43.8 per 100,000) in 2018 (Table 1; Fig. 1a). The estimated ASMR was again the highest in developed countries led by Hungary (21.5/100,000) and Slovakia (20.4 per 100,000) (Table 1; Fig. 1b). Among the countries with more than 1000 incident cases in 2018, ASIR varied 13-fold from Bangladesh with ASIR of 3.8/100,000 to 51.2/100,000 recorded by Hungary. ASMR varied 7-fold in these countries (> 1000 cases) ranging from Bangladesh with ASMR of 3.0/100,000 to Hungary which recorded ASMR of 21.5/100,000 in 2018.
Fig. 1.
Geographical distribution of colorectal cancer burden in both sexes in 2017. a ASIR. b ASMR. ASIR age-standardized incidence rate per 100,000 person-years, ASMR age-standardized mortality rate per 100,000 person-years. Data source: GLOBOCAN 2018 (IARC)
Sex-wise, we noted that CRC had more proclivity towards males than females with males recording ASIR of 23.8/100,000 as against female ASIR of 21.8/100,000. The male-female difference in ASIR was the greatest in European regions, e.g., Southern Europe, male ASIR 40.4/100,000 and female ASIR 24.1/100,000. Globally, the ASMR was again higher in males (10.8/100,000) than females (7.2/100,000). The male-female difference in ASMR was the highest in European regions, e.g., central and eastern Europe, male ASMR 20.5/100,000 and female ASMR 11.9/100,000. The pattern of male dominance in terms of CRC burden was preserved across other world regions with few of the heavily burdened countries recording male age-standardized rates approximately twice as that of female age-standardized rates; for instance, Poland has an estimated male ASMR of 22.6/100,000 and female ASMR of 11.4/100,000 (Table 1). The t test of mean difference between male and females across countries was again found to be significant across all the metrics (bottom row of Table 1).
Across the age groups, the CRC incidence exhibited bell-shaped distribution; deaths due to CRC, however, increased monotonically with age (Fig. 2). The male dominance in terms of CRC burden was again preserved across different age groups with each of them except the oldest (85 plus) registering higher incidence as well as the death counts in males than in females (Fig. 2).
Fig. 2.
Age-group and gender-wise burden of colon and rectum cancer in 2018. a Incidence. b Deaths. Data source: GLOBOCAN 2018 (IARC)
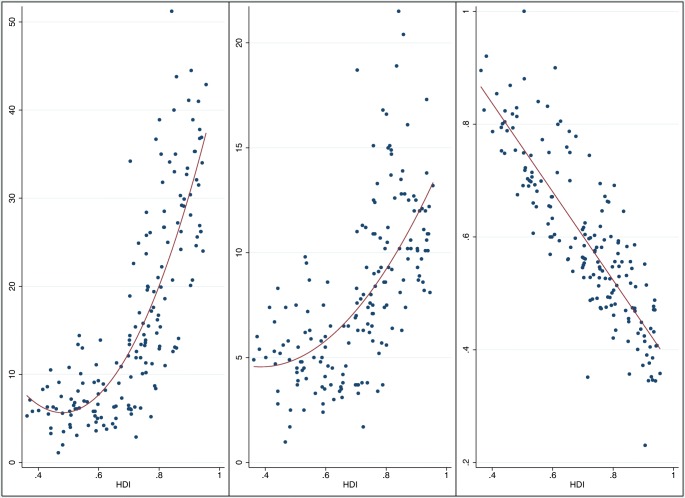
To examine the statistical relationship between CRC and HDI, we regressed ASIR and ASMR on HDI in linear form as well as by including the quadratic term (Table 2). The model including only the linear term of HDI could explain 58.7% variation in ASIR, whereas it explained 38.6% variation in ASMR. The inclusion of quadratic term resulted in a better fit of the model with regression involving both linear and quadratic term explaining 66.8% and 40.9% variation in ASIR and ASMR, respectively. CRC was generally higher in developed countries with a sharp upsurge in the positive relationship at HDI around 0.5 and 0.37 with the nonlinearity not as sharp in case of ASMR as it was in the case of ASIR (Table 2, Fig. 3).
Table 2.
Association between human development and indicators of CRC burden
| ASIR as dependent Variable | ASMR as dependent Variable | MIR as dependent Variable | ||||
|---|---|---|---|---|---|---|
| HDI | 56.9*** (3.4) | − 134.8*** (22.9) | 16.1*** (1.3) | − 20.8* (11.0) | − 0.7839*** (0.0324) | − 0.6718** (0.2833) |
| HDI SQ | 140.5*** (17.5) | 27.0*** (8.1) | − 0.0821 (0.2108) | |||
| Intercept | − 24.0*** (2.3) | 38.0*** (7.1) | − 3.4*** (0.9) | 8.6*** (3.5) | 1.1504*** (0.0239) | 1.1142*** (0.0900) |
| R2 | 0.5869 | 0.6691 | 0.3850 | 0.4101 | 0.7240 | 0.7242 |
| Turning Point | 0.4797 | 0.3852 | ||||
Data source: MIR was calculated directly as the ratio of all-age death numbers and no. of all-age incident cases which were procured from GLOBOCAN 2018 (IARC) and HDI estimates from UNDP. Robust standard errors are presented inside parenthesis
ASMR age-standardized mortality rate per 100,000 person-years, both sexes, ASIR age-standardized incidence rate per 100,000 person-years, both sexes, MIR mortality-to-incidence ratio, HDI country-wise human development index
*, **, *** represent statistical significance at 10, 5, and 1% level of significance. Turning point is calculated as
Fig. 3.
Nonlinear relationship between human development and age-standardized rates. a ASIR vs HDI. b ASMR vs HDI. c MIR vs HDI. ASMR age-standardized mortality rate per 100,000 person-years, both sexes, ASIR age-standardized incidence rate per 100,000 person-years, both sexes, MIR mortality-to-incidence ratio, HDI human development index. Data source: MIR was calculated directly as the ratio of all-age death numbers and no. of all-age incident cases, both of which were procured from GLOBOCAN 2018 (IARC) and HDI estimates were obtained from UNDP
MIR, a proxy indicator of 5-year survival rate, exhibited negative gradient with HDI (Fig. 3c). The global MIR of CRC stood at 0.48 with 140 countries recording MIR above the global MIR. Among the regions, the highest MIR (or the lowest survival rates) was recorded by African regions (middle Africa 0.76 and eastern Africa 0.71). The MIR was also high in south-central Asia at 0.71. Although ASIR was one of the highest in Australia/New Zealand region, its MIR was one of the lowest at 0.35. Among the countries with incidence greater than 1000 in 2018, MIR exhibited a 3.6-fold variation ranging from 0.23 in South Korea to 0.83 in Nepal. Unlike ASIR and ASMR, the pattern of association of MIR with HDI was found to be strictly linear and downward sloping rather than quadratic (Fig. 3c; Table 2). HDI could explain 72.6% of the variation in MIR (Table 2) with the inclusion of quadratic term does not significantly improve the fit of the model, which is again apparent from Fig. 3c.
Globally, 1 in 24 persons (1 in 19 men and 1 in 29 women) had the risk of developing CRC during their lifetime (before the age 85) whereas the risk of dying from CRC were 1 in 37 in males and 1 in 57 in females (Table 3; Table 4 of Appendix). There was wide geographical variations between the risk of developing and dying from CRC during lifetime i.e. before the age 85 (Table 3; Table 4 of Appendix). While the odds of CRC incidence were the greatest in Australia/New Zealand region with 1 in 13 persons (males 1 in 11; females: 1 in 15) were expected to develop CRC during their lifetime, the odds of CRC death, however, were the greatest in central and eastern Europe (both sexes 1 in 28; males 1 in 20; females 1 in 36). Country-wise, odds of developing CRC were the greatest in developed countries led by Hungary with odds of CRC incidence 1 in 10 (males 1 in 7; females 1 in 13). In females, the highest odds of CRC incidence and death were estimated in Singapore (incidence 1 in 11; death 1 in 27). Fifty-three countries had more than 5% risk of CRC incidence during a person’s lifetime, whereas 7 countries recorded greater than 10% risk of developing CRC. As per the development status, the CRC risk was the highest in developed countries and lowest in lesser developed and populous countries in Asia and Africa. India, for instance, had one of the lowest risks (incidence 1 in 120; death 1 in 149) of CRC incidence and mortality.
Table 3.
Region-wise probability of incidence and death due to colorectal cancer
| Incidence | Deaths | |||||
|---|---|---|---|---|---|---|
| Population | Both | Male | Female | Both | Male | Female |
| Australia and New Zealand | 7.83 (1 in 13) | 8.98 (1 in 11) | 6.75 (1 in 15) | 2.77 (1 in 36) | 3.16 (1 in 32) | 2.4 (1 in 42) |
| Caribbean | 3.97 (1 in 25) | 4.01 (1 in 25) | 3.94 (1 in 25) | 2.37 (1 in 42) | 2.45 (1 in 41) | 2.29 (1 in 44) |
| Central America | 2.17 (1 in 46) | 2.38 (1 in 42) | 1.98 (1 in 51) | 1.17 (1 in 85) | 1.3 (1 in 77) | 1.06 (1 in 94) |
| Central and Eastern Europe | 5.9 (1 in 17) | 7.92 (1 in 13) | 4.7 (1 in 21) | 3.56 (1 in 28) | 4.93 (1 in 20) | 2.78 (1 in 36) |
| Eastern Africa | 1.49 (1 in 67) | 1.54 (1 in 65) | 1.45 (1 in 69) | 1.19 (1 in 84) | 1.28 (1 in 78) | 1.12 (1 in 89) |
| Eastern Asia | 5.67 (1 in 18) | 6.86 (1 in 15) | 4.58 (1 in 22) | 2.83 (1 in 35) | 3.44 (1 in 29) | 2.28 (1 in 44) |
| Melanesia | 2.82 (1 in 35) | 4.23 (1 in 24) | 1.75 (1 in 57) | 1.85 (1 in 54) | 3.02 (1 in 33) | 0.97 (1 in 103) |
| Micronesia | 3.63 (1 in 28) | 4.1 (1 in 24) | 3.13 (1 in 32) | 1.81 (1 in 55) | 2.69 (1 in 37) | 1.09 (1 in 92) |
| Middle Africa | 1.72 (1 in 58) | 1.84 (1 in 54) | 1.63 (1 in 61) | 1.47 (1 in 68) | 1.61 (1 in 62) | 1.37 (1 in 73) |
| North America | 5.18 (1 in 19) | 5.88 (1 in 17) | 4.57 (1 in 22) | 1.88 (1 in 53) | 2.21 (1 in 45) | 1.59 (1 in 63) |
| Northern Africa | 1.68 (1 in 60) | 1.9 (1 in 53) | 1.51 (1 in 66) | 1.14 (1 in 88) | 1.35 (1 in 74) | 0.97 (1 in 103) |
| Northern Europe | 6.89 (1 in 15) | 8.23 (1 in 12) | 5.74 (1 in 17) | 2.9 (1 in 34) | 3.55 (1 in 28) | 2.37 (1 in 42) |
| Polynesia | 3.48 (1 in 29) | 4.53 (1 in 22) | 2.55 (1 in 39) | 0.77 (1 in 130) | 1.35 (1 in 74) | 0.26 (1 in 385) |
| South America | 3.91 (1 in 26) | 4.42 (1 in 23) | 3.51 (1 in 28) | 2.14 (1 in 47) | 2.53 (1 in 40) | 1.84 (1 in 54) |
| South-Central Asia | 0.93 (1 in 108) | 1.2 (1 in 83) | 0.68 (1 in 147) | 0.72 (1 in 139) | 0.95 (1 in 105) | 0.5 (1 in 200) |
| South-Eastern Asia | 2.92 (1 in 34) | 3.65 (1 in 27) | 2.35 (1 in 43) | 1.84 (1 in 54) | 2.36 (1 in 42) | 1.46 (1 in 68) |
| Southern Africa | 2.89 (1 in 35) | 3.78 (1 in 26) | 2.37 (1 in 42) | 1.72 (1 in 58) | 2.37 (1 in 42) | 1.35 (1 in 74) |
| Southern Europe | 6.64 (1 in 15) | 8.66 (1 in 12) | 4.95 (1 in 20) | 2.89 (1 in 35) | 3.92 (1 in 26) | 2.06 (1 in 49) |
| Western Africa | 1.15 (1 in 87) | 1.24 (1 in 81) | 1.07 (1 in 93) | 0.9 (1 in 111) | 0.99 (1 in 101) | 0.82 (1 in 122) |
| Western Asia | 3.38 (1 in 30) | 4.15 (1 in 24) | 2.75 (1 in 36) | 2.05 (1 in 49) | 2.5 (1 in 40) | 1.69 (1 in 59) |
| Western Europe | 6.12 (1 in 16) | 7.48 (1 in 13) | 4.94 (1 in 20) | 2.6 (1 in 38) | 3.32 (1 in 30) | 1.99 (1 in 50) |
Data source: cumulative risk of developing and dying from cancer (before age 85) were procured from GLOBOCAN 2018 and the odds were calculated using the CRC risk. Odds of developing and dying from CRC are presented inside parenthesis
Table 4.
Country-wise probability of incidence and death due to colorectal cancer
| Incidence | Deaths | |||||
|---|---|---|---|---|---|---|
| Country | Both | Male | Female | Both | Male | Female |
| Afghanistan | 0.68 (1 in 147) | 0.77 (1 in 130) | 0.59 (1 in 169) | 0.62 (1 in 161) | 0.69 (1 in 145) | 0.55 (1 in 182) |
| Albania | 1.49 (1 in 67) | 1.73 (1 in 58) | 1.27 (1 in 79) | 0.84 (1 in 119) | 1.02 (1 in 98) | 0.66 (1 in 152) |
| Algeria | 2.6 (1 in 38) | 2.93 (1 in 34) | 2.29 (1 in 44) | 1.64 (1 in 61) | 1.97 (1 in 51) | 1.35 (1 in 74) |
| Angola | 1.04 (1 in 96) | 1.22 (1 in 82) | 0.9 (1 in 111) | 0.79 (1 in 127) | 0.96 (1 in 104) | 0.66 (1 in 152) |
| Argentina | 5.11 (1 in 20) | 6.69 (1 in 15) | 3.98 (1 in 25) | 3 (1 in 33) | 4.09 (1 in 24) | 2.25 (1 in 44) |
| Armenia | 4.81 (1 in 21) | 4.42 (1 in 23) | 5.06 (1 in 20) | 3.19 (1 in 31) | 3.21 (1 in 31) | 3.16 (1 in 32) |
| Australia | 7.77 (1 in 13) | 8.95 (1 in 11) | 6.67 (1 in 15) | 2.7 (1 in 37) | 3.09 (1 in 32) | 2.33 (1 in 43) |
| Austria | 4.56 (1 in 22) | 5.91 (1 in 17) | 3.44 (1 in 29) | 2.29 (1 in 44) | 3.16 (1 in 32) | 1.6 (1 in 63) |
| Azerbaijan | 2.01 (1 in 50) | 2.85 (1 in 35) | 1.41 (1 in 71) | 1.54 (1 in 65) | 2.31 (1 in 43) | 1 (1 in 100) |
| Bahamas | 4.59 (1 in 22) | 5.6 (1 in 18) | 3.75 (1 in 27) | 2.2 (1 in 45) | 2.91 (1 in 34) | 1.68 (1 in 60) |
| Bahrain | 2.41 (1 in 41) | 3.12 (1 in 32) | 1.73 (1 in 58) | 1.72 (1 in 58) | 2.28 (1 in 44) | 1.26 (1 in 79) |
| Bangladesh | 0.68 (1 in 147) | 0.76 (1 in 132) | 0.61 (1 in 164) | 0.58 (1 in 172) | 0.66 (1 in 152) | 0.49 (1 in 204) |
| Barbados | 8.25 (1 in 12) | 9.65 (1 in 10) | 7 (1 in 14) | 3.99 (1 in 25) | 4.87 (1 in 21) | 3.28 (1 in 30) |
| Belarus | 6.4 (1 in 16) | 8.77 (1 in 11) | 5.17 (1 in 19) | 3.48 (1 in 29) | 4.57 (1 in 22) | 2.95 (1 in 34) |
| Belgium | 7.53 (1 in 13) | 9.47 (1 in 11) | 5.9 (1 in 17) | 2.51 (1 in 40) | 3.15 (1 in 32) | 1.99 (1 in 50) |
| Belize | 1.52 (1 in 66) | 1.48 (1 in 68) | 1.54 (1 in 65) | 1.16 (1 in 86) | 1.08 (1 in 93) | 1.22 (1 in 82) |
| Benin | 0.91 (1 in 110) | 1.42 (1 in 70) | 0.52 (1 in 192) | 0.68 (1 in 147) | 1.07 (1 in 93) | 0.37 (1 in 270) |
| Bhutan | 0.68 (1 in 147) | 0.78 (1 in 128) | 0.57 (1 in 175) | 0.65 (1 in 154) | 0.74 (1 in 135) | 0.53 (1 in 189) |
| Bolivia | 1.16 (1 in 86) | 1.29 (1 in 78) | 1.03 (1 in 97) | 0.75 (1 in 133) | 0.87 (1 in 115) | 0.65 (1 in 154) |
| Bosnia and Herzegovina | 5.19 (1 in 19) | 6.61 (1 in 15) | 4.07 (1 in 25) | 3.19 (1 in 31) | 4.34 (1 in 23) | 2.33 (1 in 43) |
| Botswana | 0.53 (1 in 189) | 0.93 (1 in 108) | 0.27 (1 in 370) | 0.4 (1 in 250) | 0.73 (1 in 137) | 0.2 (1 in 500) |
| Brazil | 4 (1 in 25) | 4.42 (1 in 23) | 3.68 (1 in 27) | 2.09 (1 in 48) | 2.43 (1 in 41) | 1.85 (1 in 54) |
| Brunei | 6.97 (1 in 14) | 8.72 (1 in 11) | 5.44 (1 in 18) | 3.03 (1 in 33) | 4.15 (1 in 24) | 2.07 (1 in 48) |
| Bulgaria | 5.67 (1 in 18) | 7.82 (1 in 13) | 4.1 (1 in 24) | 3.47 (1 in 29) | 5.05 (1 in 20) | 2.36 (1 in 42) |
| Burkina Faso | 1.21 (1 in 83) | 1.05 (1 in 95) | 1.32 (1 in 76) | 1.11 (1 in 90) | 0.98 (1 in 102) | 1.18 (1 in 85) |
| Burundi | 1.93 (1 in 52) | 1.67 (1 in 60) | 2.14 (1 in 47) | 1.81 (1 in 55) | 1.61 (1 in 62) | 1.97 (1 in 51) |
| Cabo Verde | 1.97 (1 in 51) | 2.65 (1 in 38) | 1.64 (1 in 61) | 1.26 (1 in 79) | 1.76 (1 in 57) | 0.99 (1 in 101) |
| Cambodia | 2.39 (1 in 42) | 2.8 (1 in 36) | 2.12 (1 in 47) | 1.85 (1 in 54) | 2.16 (1 in 46) | 1.65 (1 in 61) |
| Cameroon | 1.53 (1 in 65) | 1.75 (1 in 57) | 1.35 (1 in 74) | 1.24 (1 in 81) | 1.46 (1 in 68) | 1.06 (1 in 94) |
| Canada | 6.49 (1 in 15) | 7.4 (1 in 14) | 5.68 (1 in 18) | 2.55 (1 in 39) | 3.1 (1 in 32) | 2.06 (1 in 49) |
| Central African Republic | 1.19 (1 in 84) | 1.43 (1 in 70) | 1.01 (1 in 99) | 1.16 (1 in 86) | 1.41 (1 in 71) | 0.98 (1 in 102) |
| Chad | 1.07 (1 in 93) | 1.23 (1 in 81) | 0.93 (1 in 108) | 0.97 (1 in 103) | 1.11 (1 in 90) | 0.85 (1 in 118) |
| Chile | 4.65 (1 in 22) | 5.45 (1 in 18) | 4.03 (1 in 25) | 2.62 (1 in 38) | 3.11 (1 in 32) | 2.25 (1 in 44) |
| China | 5.05 (1 in 20) | 5.99 (1 in 17) | 4.16 (1 in 24) | 2.86 (1 in 35) | 3.42 (1 in 29) | 2.34 (1 in 43) |
| Colombia | 3.45 (1 in 29) | 3.68 (1 in 27) | 3.27 (1 in 31) | 1.89 (1 in 53) | 2.09 (1 in 48) | 1.74 (1 in 57) |
| Comoros | 1.01 (1 in 99) | 0.83 (1 in 120) | 1.14 (1 in 88) | 1.01 (1 in 99) | 0.83 (1 in 120) | 1.14 (1 in 88) |
| Congo, Democratic Republic of | 2.21 (1 in 45) | 2.26 (1 in 44) | 2.19 (1 in 46) | 1.95 (1 in 51) | 2.05 (1 in 49) | 1.88 (1 in 53) |
| Congo, Republic of | 1.14 (1 in 88) | 1.35 (1 in 74) | 0.97 (1 in 103) | 0.9 (1 in 111) | 1.08 (1 in 93) | 0.75 (1 in 133) |
| Costa Rica | 3.61 (1 in 28) | 3.83 (1 in 26) | 3.42 (1 in 29) | 2.09 (1 in 48) | 2.32 (1 in 43) | 1.88 (1 in 53) |
| Côte d’Ivoire | 1.11 (1 in 90) | 0.91 (1 in 110) | 1.35 (1 in 74) | 0.95 (1 in 105) | 0.79 (1 in 127) | 1.13 (1 in 88) |
| Croatia | 7.19 (1 in 14) | 9.91 (1 in 10) | 5.22 (1 in 19) | 4.71 (1 in 21) | 7 (1 in 14) | 3.14 (1 in 32) |
| Cuba | 4.12 (1 in 24) | 3.74 (1 in 27) | 4.45 (1 in 22) | 2.76 (1 in 36) | 2.66 (1 in 38) | 2.85 (1 in 35) |
| Cyprus | 5.39 (1 in 19) | 7.81 (1 in 13) | 3.28 (1 in 30) | 2.62 (1 in 38) | 3.81 (1 in 26) | 1.62 (1 in 62) |
| Czechia | 6.96 (1 in 14) | 9.31 (1 in 11) | 5.19 (1 in 19) | 3.17 (1 in 32) | 4.4 (1 in 23) | 2.26 (1 in 44) |
| Denmark | 8.99 (1 in 11) | 10.29 (1 in 10) | 7.85 (1 in 13) | 3.18 (1 in 31) | 3.71 (1 in 27) | 2.74 (1 in 36) |
| Djibouti | 0.81 (1 in 123) | 1 (1 in 100) | 0.65 (1 in 154) | 0.75 (1 in 133) | 0.97 (1 in 103) | 0.56 (1 in 179) |
| Dominican Republic | 2.66 (1 in 38) | 2.62 (1 in 38) | 2.68 (1 in 37) | 1.64 (1 in 61) | 1.66 (1 in 60) | 1.62 (1 in 62) |
| Ecuador | 2.53 (1 in 40) | 2.37 (1 in 42) | 2.66 (1 in 38) | 1.45 (1 in 69) | 1.44 (1 in 69) | 1.46 (1 in 68) |
| Egypt | 1.16 (1 in 86) | 1.15 (1 in 87) | 1.16 (1 in 86) | 0.78 (1 in 128) | 0.78 (1 in 128) | 0.77 (1 in 130) |
| El Salvador | 1.91 (1 in 52) | 1.71 (1 in 58) | 2.07 (1 in 48) | 1.08 (1 in 93) | 0.96 (1 in 104) | 1.16 (1 in 86) |
| Equatorial Guinea | 0.98 (1 in 102) | 1.19 (1 in 84) | 0.79 (1 in 127) | 0.92 (1 in 109) | 1.15 (1 in 87) | 0.71 (1 in 141) |
| Eritrea | 1.03 (1 in 97) | 1.25 (1 in 80) | 0.85 (1 in 118) | 0.91 (1 in 110) | 1.13 (1 in 88) | 0.73 (1 in 137) |
| Estonia | 6.64 (1 in 15) | 8.18 (1 in 12) | 5.8 (1 in 17) | 3.36 (1 in 30) | 4.87 (1 in 21) | 2.55 (1 in 39) |
| Eswatini | 0.59 (1 in 169) | 0.77 (1 in 130) | 0.49 (1 in 204) | 0.46 (1 in 217) | 0.67 (1 in 149) | 0.34 (1 in 294) |
| Ethiopia | 1.16 (1 in 86) | 1.35 (1 in 74) | 1.01 (1 in 99) | 0.97 (1 in 103) | 1.19 (1 in 84) | 0.79 (1 in 127) |
| Fiji | 1.87 (1 in 53) | 2.02 (1 in 50) | 1.77 (1 in 56) | 1.2 (1 in 83) | 1.5 (1 in 67) | 0.99 (1 in 101) |
| Finland | 5.38 (1 in 19) | 6.45 (1 in 16) | 4.5 (1 in 22) | 2.18 (1 in 46) | 2.79 (1 in 36) | 1.69 (1 in 59) |
| France | 6.39 (1 in 16) | 7.92 (1 in 13) | 5.08 (1 in 20) | 2.55 (1 in 39) | 3.31 (1 in 30) | 1.91 (1 in 52) |
| France, Guadeloupe | 3.92 (1 in 26) | 4.59 (1 in 22) | 3.4 (1 in 29) | 2.32 (1 in 43) | 3.53 (1 in 28) | 1.39 (1 in 72) |
| France, La Réunion | 5.3 (1 in 19) | 6.31 (1 in 16) | 4.45 (1 in 22) | 2.4 (1 in 42) | 2.95 (1 in 34) | 1.94 (1 in 52) |
| France, Martinique | 4.93 (1 in 20) | 5.82 (1 in 17) | 4.2 (1 in 24) | 2.29 (1 in 44) | 2.92 (1 in 34) | 1.8 (1 in 56) |
| France, New Caledonia | 5.36 (1 in 19) | 6.51 (1 in 15) | 4.28 (1 in 23) | 1.64 (1 in 61) | 2.06 (1 in 49) | 1.24 (1 in 81) |
| French Guyana | 3.8 (1 in 26) | 4 (1 in 25) | 3.45 (1 in 29) | 0.84 (1 in 119) | 1.37 (1 in 73) | 0.39 (1 in 256) |
| French Polynesia | 3.24 (1 in 31) | 4.04 (1 in 25) | 2.47 (1 in 40) | 0.72 (1 in 139) | 1.29 (1 in 78) | 0.17 (1 in 588) |
| Gabon | 0.75 (1 in 133) | 0.94 (1 in 106) | 0.6 (1 in 167) | 0.5 (1 in 200) | 0.64 (1 in 156) | 0.41 (1 in 244) |
| Gaza Strip and West Bank | 4.01 (1 in 25) | 4.65 (1 in 22) | 3.47 (1 in 29) | 2.81 (1 in 36) | 3.27 (1 in 31) | 2.43 (1 in 41) |
| Georgia | 1.85 (1 in 54) | 2.42 (1 in 41) | 1.49 (1 in 67) | 1.26 (1 in 79) | 1.71 (1 in 58) | 0.98 (1 in 102) |
| Germany | 5.62 (1 in 18) | 6.74 (1 in 15) | 4.65 (1 in 22) | 2.56 (1 in 39) | 3.27 (1 in 31) | 1.96 (1 in 51) |
| Ghana | 2.03 (1 in 49) | 2.69 (1 in 37) | 1.54 (1 in 65) | 1.56 (1 in 64) | 2.17 (1 in 46) | 1.1 (1 in 91) |
| Greece | 5.57 (1 in 18) | 7.11 (1 in 14) | 4.31 (1 in 23) | 2.48 (1 in 40) | 3.33 (1 in 30) | 1.8 (1 in 56) |
| Guam | 3.59 (1 in 28) | 3.96 (1 in 25) | 3.21 (1 in 31) | 1.76 (1 in 57) | 2.51 (1 in 40) | 1.16 (1 in 86) |
| Guatemala | 1.28 (1 in 78) | 1.27 (1 in 79) | 1.29 (1 in 78) | 0.8 (1 in 125) | 0.8 (1 in 125) | 0.79 (1 in 127) |
| Guinea | 0.31 (1 in 323) | 0.33 (1 in 303) | 0.29 (1 in 345) | 0.28 (1 in 357) | 0.3 (1 in 333) | 0.26 (1 in 385) |
| Guinea-Bissau | 1.29 (1 in 78) | 1.53 (1 in 65) | 1.11 (1 in 90) | 1.23 (1 in 81) | 1.52 (1 in 66) | 1.01 (1 in 99) |
| Guyana | 1.85 (1 in 54) | 1.54 (1 in 65) | 2.08 (1 in 48) | 1.53 (1 in 65) | 1.42 (1 in 70) | 1.61 (1 in 62) |
| Haiti | 2.93 (1 in 34) | 3.29 (1 in 30) | 2.7 (1 in 37) | 2.07 (1 in 48) | 2.06 (1 in 49) | 2.1 (1 in 48) |
| Honduras | 1.73 (1 in 58) | 2.09 (1 in 48) | 1.45 (1 in 69) | 0.86 (1 in 116) | 0.93 (1 in 108) | 0.81 (1 in 123) |
| Hungary | 10.09 (1 in 10) | 14.02 (1 in 7) | 7.43 (1 in 13) | 5.01 (1 in 20) | 7.37 (1 in 14) | 3.53 (1 in 28) |
| Iceland | 5.98 (1 in 17) | 6.84 (1 in 15) | 5.15 (1 in 19) | 2.78 (1 in 36) | 3.44 (1 in 29) | 2.17 (1 in 46) |
| India | 0.83 (1 in 120) | 1.16 (1 in 86) | 0.53 (1 in 189) | 0.67 (1 in 149) | 0.96 (1 in 104) | 0.41 (1 in 244) |
| Indonesia | 2.33 (1 in 43) | 3.19 (1 in 31) | 1.62 (1 in 62) | 1.58 (1 in 63) | 2.16 (1 in 46) | 1.11 (1 in 90) |
| Iran, Islamic Republic of | 2.6 (1 in 38) | 2.99 (1 in 33) | 2.18 (1 in 46) | 1.37 (1 in 73) | 1.52 (1 in 66) | 1.19 (1 in 84) |
| Iraq | 1.11 (1 in 90) | 1.31 (1 in 76) | 0.95 (1 in 105) | 0.74 (1 in 135) | 0.88 (1 in 114) | 0.63 (1 in 159) |
| Ireland | 7.55 (1 in 13) | 9.5 (1 in 11) | 5.77 (1 in 17) | 3.21 (1 in 31) | 3.95 (1 in 25) | 2.56 (1 in 39) |
| Israel | 4.32 (1 in 23) | 5.3 (1 in 19) | 3.54 (1 in 28) | 2.4 (1 in 42) | 2.89 (1 in 35) | 2.01 (1 in 50) |
| Italy | 6.45 (1 in 16) | 7.95 (1 in 13) | 5.18 (1 in 19) | 2.61 (1 in 38) | 3.36 (1 in 30) | 2 (1 in 50) |
| Jamaica | 5.14 (1 in 19) | 4.4 (1 in 23) | 5.78 (1 in 17) | 2.63 (1 in 38) | 2.28 (1 in 44) | 2.93 (1 in 34) |
| Japan | 8.09 (1 in 12) | 10.27 (1 in 10) | 6.17 (1 in 16) | 2.92 (1 in 34) | 3.72 (1 in 27) | 2.24 (1 in 45) |
| Jordan | 3.34 (1 in 30) | 3.14 (1 in 32) | 3.54 (1 in 28) | 2.04 (1 in 49) | 2.01 (1 in 50) | 2.08 (1 in 48) |
| Kazakhstan | 3.14 (1 in 32) | 3.81 (1 in 26) | 2.79 (1 in 36) | 2.4 (1 in 42) | 3.17 (1 in 32) | 1.99 (1 in 50) |
| Kenya | 1.68 (1 in 60) | 1.95 (1 in 51) | 1.47 (1 in 68) | 1.21 (1 in 83) | 1.48 (1 in 68) | 0.99 (1 in 101) |
| Korea, Democratic Republic of | 3.88 (1 in 26) | 4.7 (1 in 21) | 3.37 (1 in 30) | 2.17 (1 in 46) | 2.62 (1 in 38) | 1.91 (1 in 52) |
| Korea, Republic of | 8.38 (1 in 12) | 11.25 (1 in 9) | 5.97 (1 in 17) | 2.23 (1 in 45) | 3.06 (1 in 33) | 1.61 (1 in 62) |
| Kuwait | 2.98 (1 in 34) | 3.05 (1 in 33) | 2.94 (1 in 34) | 1.91 (1 in 52) | 1.98 (1 in 51) | 1.86 (1 in 54) |
| Kyrgyzstan | 1.58 (1 in 63) | 1.61 (1 in 62) | 1.52 (1 in 66) | 1.31 (1 in 76) | 1.41 (1 in 71) | 1.22 (1 in 82) |
| Lao People’s Democratic Republic | 2.72 (1 in 37) | 2.99 (1 in 33) | 2.51 (1 in 40) | 1.97 (1 in 51) | 2.23 (1 in 45) | 1.78 (1 in 56) |
| Latvia | 7.21 (1 in 14) | 9.81 (1 in 10) | 5.87 (1 in 17) | 3.31 (1 in 30) | 4.64 (1 in 22) | 2.65 (1 in 38) |
| Lebanon | 4.13 (1 in 24) | 4.41 (1 in 23) | 3.9 (1 in 26) | 2.58 (1 in 39) | 2.83 (1 in 35) | 2.37 (1 in 42) |
| Lesotho | 0.54 (1 in 185) | 0.81 (1 in 123) | 0.39 (1 in 256) | 0.46 (1 in 217) | 0.72 (1 in 139) | 0.32 (1 in 313) |
| Liberia | 0.73 (1 in 137) | 0.63 (1 in 159) | 0.82 (1 in 122) | 0.68 (1 in 147) | 0.6 (1 in 167) | 0.74 (1 in 135) |
| Libya | 2.21 (1 in 45) | 2.49 (1 in 40) | 1.99 (1 in 50) | 1.58 (1 in 63) | 1.85 (1 in 54) | 1.37 (1 in 73) |
| Lithuania | 5.77 (1 in 17) | 7.93 (1 in 13) | 4.57 (1 in 22) | 3.2 (1 in 31) | 5.04 (1 in 20) | 2.2 (1 in 45) |
| Luxembourg | 6.21 (1 in 16) | 7.43 (1 in 13) | 5.21 (1 in 19) | 2.67 (1 in 37) | 3.42 (1 in 29) | 2.05 (1 in 49) |
| Madagascar | 1.35 (1 in 74) | 1.19 (1 in 84) | 1.47 (1 in 68) | 1.07 (1 in 93) | 0.98 (1 in 102) | 1.15 (1 in 87) |
| Malawi | 0.53 (1 in 189) | 0.64 (1 in 156) | 0.47 (1 in 213) | 0.43 (1 in 233) | 0.54 (1 in 185) | 0.35 (1 in 286) |
| Malaysia | 4.3 (1 in 23) | 4.78 (1 in 21) | 3.86 (1 in 26) | 2.87 (1 in 35) | 3.25 (1 in 31) | 2.51 (1 in 40) |
| Maldives | 2.28 (1 in 44) | 2.94 (1 in 34) | 1.55 (1 in 65) | 1.57 (1 in 64) | 2.4 (1 in 42) | 0.67 (1 in 149) |
| Mali | 2.07 (1 in 48) | 1.75 (1 in 57) | 2.33 (1 in 43) | 1.78 (1 in 56) | 1.56 (1 in 64) | 1.96 (1 in 51) |
| Malta | 6.63 (1 in 15) | 8.56 (1 in 12) | 4.99 (1 in 20) | 2.81 (1 in 36) | 3.62 (1 in 28) | 2.16 (1 in 46) |
| Mauritania | 1.27 (1 in 79) | 1.03 (1 in 97) | 1.44 (1 in 69) | 1.03 (1 in 97) | 0.86 (1 in 116) | 1.15 (1 in 87) |
| Mauritius | 3.08 (1 in 32) | 3.8 (1 in 26) | 2.55 (1 in 39) | 2.04 (1 in 49) | 2.47 (1 in 40) | 1.71 (1 in 58) |
| Mexico | 2.16 (1 in 46) | 2.41 (1 in 41) | 1.93 (1 in 52) | 1.14 (1 in 88) | 1.3 (1 in 77) | 1 (1 in 100) |
| Mongolia | 1.29 (1 in 78) | 1.36 (1 in 74) | 1.25 (1 in 80) | 0.72 (1 in 139) | 0.83 (1 in 120) | 0.65 (1 in 154) |
| Montenegro | 3.55 (1 in 28) | 4.13 (1 in 24) | 3.05 (1 in 33) | 2.17 (1 in 46) | 2.63 (1 in 38) | 1.83 (1 in 55) |
| Morocco | 1.92 (1 in 52) | 2.26 (1 in 44) | 1.63 (1 in 61) | 1.33 (1 in 75) | 1.67 (1 in 60) | 1.05 (1 in 95) |
| Mozambique | 0.61 (1 in 164) | 0.66 (1 in 152) | 0.58 (1 in 172) | 0.54 (1 in 185) | 0.59 (1 in 169) | 0.5 (1 in 200) |
| Myanmar | 1.73 (1 in 58) | 2.13 (1 in 47) | 1.43 (1 in 70) | 1.28 (1 in 78) | 1.58 (1 in 63) | 1.06 (1 in 94) |
| Namibia | 1.25 (1 in 80) | 1.48 (1 in 68) | 1.09 (1 in 92) | 0.8 (1 in 125) | 1.04 (1 in 96) | 0.64 (1 in 156) |
| Nepal | 1.32 (1 in 76) | 1.09 (1 in 92) | 1.53 (1 in 65) | 1.15 (1 in 87) | 0.99 (1 in 101) | 1.3 (1 in 77) |
| New Zealand | 8.14 (1 in 12) | 9.13 (1 in 11) | 7.23 (1 in 14) | 3.12 (1 in 32) | 3.51 (1 in 28) | 2.77 (1 in 36) |
| Nicaragua | 2.28 (1 in 44) | 1.99 (1 in 50) | 2.51 (1 in 40) | 1.47 (1 in 68) | 1.29 (1 in 78) | 1.6 (1 in 63) |
| Niger | 0.88 (1 in 114) | 0.91 (1 in 110) | 0.84 (1 in 119) | 0.86 (1 in 116) | 0.9 (1 in 111) | 0.81 (1 in 123) |
| Nigeria | 0.95 (1 in 105) | 1.08 (1 in 93) | 0.84 (1 in 119) | 0.67 (1 in 149) | 0.78 (1 in 128) | 0.57 (1 in 175) |
| Norway | 9.45 (1 in 11) | 10.5 (1 in 10) | 8.52 (1 in 12) | 3.46 (1 in 29) | 4.06 (1 in 25) | 2.93 (1 in 34) |
| Oman | 1.87 (1 in 53) | 1.91 (1 in 52) | 1.78 (1 in 56) | 1.25 (1 in 80) | 1.26 (1 in 79) | 1.22 (1 in 82) |
| Pakistan | 0.68 (1 in 147) | 0.73 (1 in 137) | 0.63 (1 in 159) | 0.57 (1 in 175) | 0.62 (1 in 161) | 0.52 (1 in 192) |
| Panama | 3.45 (1 in 29) | 4.09 (1 in 24) | 2.89 (1 in 35) | 1.78 (1 in 56) | 2.08 (1 in 48) | 1.51 (1 in 66) |
| Papua New Guinea | 2.96 (1 in 34) | 4.8 (1 in 21) | 1.61 (1 in 62) | 2.1 (1 in 48) | 3.69 (1 in 27) | 0.96 (1 in 104) |
| Paraguay | 2.95 (1 in 34) | 3.05 (1 in 33) | 2.84 (1 in 35) | 2 (1 in 50) | 2.09 (1 in 48) | 1.91 (1 in 52) |
| Peru | 3.03 (1 in 33) | 3.3 (1 in 30) | 2.8 (1 in 36) | 1.66 (1 in 60) | 1.92 (1 in 52) | 1.45 (1 in 69) |
| Philippines | 4.06 (1 in 25) | 5.14 (1 in 19) | 3.25 (1 in 31) | 2.83 (1 in 35) | 3.59 (1 in 28) | 2.28 (1 in 44) |
| Poland | 6.4 (1 in 16) | 8.85 (1 in 11) | 4.68 (1 in 21) | 3.93 (1 in 25) | 5.64 (1 in 18) | 2.79 (1 in 36) |
| Portugal | 8.1 (1 in 12) | 11.06 (1 in 9) | 5.74 (1 in 17) | 3.31 (1 in 30) | 4.68 (1 in 21) | 2.28 (1 in 44) |
| Puerto Rico | 5.49 (1 in 18) | 6.9 (1 in 14) | 4.41 (1 in 23) | 2.26 (1 in 44) | 3.07 (1 in 33) | 1.66 (1 in 60) |
| Qatar | 3.41 (1 in 29) | 3.7 (1 in 27) | 2.96 (1 in 34) | 2.55 (1 in 39) | 2.69 (1 in 37) | 2.38 (1 in 42) |
| Republic of Moldova | 6.56 (1 in 15) | 9.27 (1 in 11) | 4.83 (1 in 21) | 4.05 (1 in 25) | 6.02 (1 in 17) | 2.84 (1 in 35) |
| Romania | 5.46 (1 in 18) | 7.57 (1 in 13) | 3.95 (1 in 25) | 3.25 (1 in 31) | 4.65 (1 in 22) | 2.3 (1 in 43) |
| Russian Federation | 5.51 (1 in 18) | 7 (1 in 14) | 4.72 (1 in 21) | 3.48 (1 in 29) | 4.63 (1 in 22) | 2.9 (1 in 34) |
| Rwanda | 3.29 (1 in 30) | 3.15 (1 in 32) | 3.41 (1 in 29) | 2.68 (1 in 37) | 2.7 (1 in 37) | 2.68 (1 in 37) |
| Saint Lucia | 3.53 (1 in 28) | 4.19 (1 in 24) | 3.04 (1 in 33) | 2.25 (1 in 44) | 2.93 (1 in 34) | 1.72 (1 in 58) |
| Samoa | 4.32 (1 in 23) | 5.98 (1 in 17) | 2.89 (1 in 35) | 1.07 (1 in 93) | 1.5 (1 in 67) | 0.76 (1 in 132) |
| Sao Tome and Principe | 0.88 (1 in 114) | 1.33 (1 in 75) | 0.55 (1 in 182) | 0.57 (1 in 175) | 0.96 (1 in 104) | 0.28 (1 in 357) |
| Saudi Arabia | 2.37 (1 in 42) | 2.8 (1 in 36) | 1.85 (1 in 54) | 1.3 (1 in 77) | 1.58 (1 in 63) | 0.99 (1 in 101) |
| Senegal | 1.38 (1 in 72) | 1.42 (1 in 70) | 1.35 (1 in 74) | 1.12 (1 in 89) | 1.22 (1 in 82) | 1.05 (1 in 95) |
| Serbia | 6.64 (1 in 15) | 9.04 (1 in 11) | 4.71 (1 in 21) | 3.84 (1 in 26) | 5.45 (1 in 18) | 2.64 (1 in 38) |
| Sierra Leone | 1.1 (1 in 91) | 0.94 (1 in 106) | 1.24 (1 in 81) | 1.01 (1 in 99) | 0.86 (1 in 116) | 1.15 (1 in 87) |
| Singapore | 8.88 (1 in 11) | 8.9 (1 in 11) | 8.72 (1 in 11) | 4.4 (1 in 23) | 5.11 (1 in 20) | 3.77 (1 in 27) |
| Slovakia | 9.01 (1 in 11) | 12.73 (1 in 8) | 6.44 (1 in 16) | 5.11 (1 in 20) | 7.6 (1 in 13) | 3.57 (1 in 28) |
| Slovenia | 8.49 (1 in 12) | 12.32 (1 in 8) | 5.28 (1 in 19) | 3.23 (1 in 31) | 4.47 (1 in 22) | 2.28 (1 in 44) |
| Solomon Islands | 1.23 (1 in 81) | 1.43 (1 in 70) | 1.03 (1 in 97) | 1.06 (1 in 94) | 1.28 (1 in 78) | 0.84 (1 in 119) |
| Somalia | 1.31 (1 in 76) | 1.52 (1 in 66) | 1.12 (1 in 89) | 1.25 (1 in 80) | 1.47 (1 in 68) | 1.05 (1 in 95) |
| South Africa | 3.12 (1 in 32) | 4.09 (1 in 24) | 2.55 (1 in 39) | 1.84 (1 in 54) | 2.55 (1 in 39) | 1.44 (1 in 69) |
| South Sudan | 1.35 (1 in 74) | 1.49 (1 in 67) | 1.24 (1 in 81) | 1.23 (1 in 81) | 1.37 (1 in 73) | 1.1 (1 in 91) |
| Spain | 7.06 (1 in 14) | 9.74 (1 in 10) | 4.82 (1 in 21) | 3.01 (1 in 33) | 4.33 (1 in 23) | 1.96 (1 in 51) |
| Sri Lanka | 0.93 (1 in 108) | 1.08 (1 in 93) | 0.82 (1 in 122) | 0.68 (1 in 147) | 0.82 (1 in 122) | 0.57 (1 in 175) |
| Sudan | 0.92 (1 in 109) | 1.16 (1 in 86) | 0.72 (1 in 139) | 0.77 (1 in 130) | 1.02 (1 in 98) | 0.57 (1 in 175) |
| Suriname | 3.89 (1 in 26) | 4.88 (1 in 20) | 3.18 (1 in 31) | 2.87 (1 in 35) | 3.39 (1 in 29) | 2.46 (1 in 41) |
| Sweden | 6.03 (1 in 17) | 6.74 (1 in 15) | 5.4 (1 in 19) | 2.77 (1 in 36) | 3.28 (1 in 30) | 2.32 (1 in 43) |
| Switzerland | 5.15 (1 in 19) | 6.3 (1 in 16) | 4.16 (1 in 24) | 2.08 (1 in 48) | 2.64 (1 in 38) | 1.61 (1 in 62) |
| Syrian Arab Republic | 2.87 (1 in 35) | 2.97 (1 in 34) | 2.8 (1 in 36) | 2.11 (1 in 47) | 2.24 (1 in 45) | 2.02 (1 in 50) |
| Tajikistan | 0.69 (1 in 145) | 0.81 (1 in 123) | 0.58 (1 in 172) | 0.58 (1 in 172) | 0.72 (1 in 139) | 0.46 (1 in 217) |
| Tanzania | 2.09 (1 in 48) | 1.7 (1 in 59) | 2.41 (1 in 41) | 1.62 (1 in 62) | 1.38 (1 in 72) | 1.82 (1 in 55) |
| Thailand | 3.2 (1 in 31) | 3.71 (1 in 27) | 2.8 (1 in 36) | 1.74 (1 in 57) | 2.07 (1 in 48) | 1.48 (1 in 68) |
| The former Yugoslav Republic of Macedonia | 5.33 (1 in 19) | 5.98 (1 in 17) | 4.81 (1 in 21) | 2.93 (1 in 34) | 3.37 (1 in 30) | 2.59 (1 in 39) |
| The Netherlands | 8.13 (1 in 12) | 9.93 (1 in 10) | 6.51 (1 in 15) | 3.55 (1 in 28) | 4.28 (1 in 23) | 2.92 (1 in 34) |
| The Republic of the Gambia | 0.15 (1 in 667) | 0.21 (1 in 476) | 0.1 (1 in 1000) | 0.15 (1 in 667) | 0.2 (1 in 500) | 0.1 (1 in 1000) |
| Timor-Leste | 1.88 (1 in 53) | 1.86 (1 in 54) | 1.88 (1 in 53) | 1.53 (1 in 65) | 1.52 (1 in 66) | 1.52 (1 in 66) |
| Togo | 1.43 (1 in 70) | 1.38 (1 in 72) | 1.46 (1 in 68) | 1.19 (1 in 84) | 1.19 (1 in 84) | 1.19 (1 in 84) |
| Trinidad and Tobago | 4.12 (1 in 24) | 4.63 (1 in 22) | 3.71 (1 in 27) | 2.22 (1 in 45) | 2.64 (1 in 38) | 1.9 (1 in 53) |
| Tunisia | 2.3 (1 in 43) | 2.55 (1 in 39) | 2.09 (1 in 48) | 1.49 (1 in 67) | 1.68 (1 in 60) | 1.33 (1 in 75) |
| Turkey | 4.27 (1 in 23) | 5.64 (1 in 18) | 3.21 (1 in 31) | 2.43 (1 in 41) | 3.16 (1 in 32) | 1.88 (1 in 53) |
| Turkmenistan | 1.29 (1 in 78) | 1.45 (1 in 69) | 1.18 (1 in 85) | 0.69 (1 in 145) | 0.84 (1 in 119) | 0.58 (1 in 172) |
| Uganda | 1.86 (1 in 54) | 1.75 (1 in 57) | 1.94 (1 in 52) | 1.56 (1 in 64) | 1.48 (1 in 68) | 1.61 (1 in 62) |
| Ukraine | 5.12 (1 in 20) | 6.92 (1 in 14) | 4.12 (1 in 24) | 3.29 (1 in 30) | 4.53 (1 in 22) | 2.61 (1 in 38) |
| United Arab Emirates | 2.93 (1 in 34) | 3.3 (1 in 30) | 2.25 (1 in 44) | 1.72 (1 in 58) | 1.85 (1 in 54) | 1.51 (1 in 66) |
| UK | 6.8 (1 in 15) | 8.17 (1 in 12) | 5.57 (1 in 18) | 2.87 (1 in 35) | 3.48 (1 in 29) | 2.35 (1 in 43) |
| USA | 5.01 (1 in 20) | 5.68 (1 in 18) | 4.44 (1 in 23) | 1.79 (1 in 56) | 2.1 (1 in 48) | 1.53 (1 in 65) |
| Uruguay | 7.54 (1 in 13) | 9.54 (1 in 10) | 6.1 (1 in 16) | 3.73 (1 in 27) | 4.91 (1 in 20) | 2.94 (1 in 34) |
| Uzbekistan | 1.22 (1 in 82) | 1.21 (1 in 83) | 1.22 (1 in 82) | 0.75 (1 in 133) | 1 (1 in 100) | 0.55 (1 in 182) |
| Vanuatu | 0.72 (1 in 139) | 0.64 (1 in 156) | 0.81 (1 in 123) | 0.69 (1 in 145) | 0.64 (1 in 156) | 0.73 (1 in 137) |
| Venezuela, Bolivarian Republic of | 2.85 (1 in 35) | 3.02 (1 in 33) | 2.69 (1 in 37) | 1.66 (1 in 60) | 1.84 (1 in 54) | 1.5 (1 in 67) |
| Viet Nam | 2.51 (1 in 40) | 3.11 (1 in 32) | 2.12 (1 in 47) | 1.55 (1 in 65) | 2 (1 in 50) | 1.28 (1 in 78) |
| World | 4.25 (1 in 24) | 5.15 (1 in 19) | 3.48 (1 in 29) | 2.18 (1 in 46) | 2.69 (1 in 37) | 1.76 (1 in 57) |
| Yemen | 1.86 (1 in 54) | 2.01 (1 in 50) | 1.74 (1 in 57) | 1.55 (1 in 65) | 1.67 (1 in 60) | 1.44 (1 in 69) |
| Zambia | 0.75 (1 in 133) | 0.89 (1 in 112) | 0.66 (1 in 152) | 0.49 (1 in 204) | 0.65 (1 in 154) | 0.38 (1 in 263) |
| Zimbabwe | 2.01 (1 in 50) | 2.35 (1 in 43) | 1.77 (1 in 56) | 1.55 (1 in 65) | 1.85 (1 in 54) | 1.34 (1 in 75) |
Data source: cumulative risk of developing and dying from cancer (before age 85) were procured from GLOBOCAN 2018 and the odds were calculated using the CRC risk. Odds of developing and dying from CRC are presented inside parenthesis.
Discussion
We examined the CRC burden using estimates of incidence and mortality from GLOBOCAN 2018 [11, 17] and examined its association with socioeconomic status measured using HDI. We found that CRC incidence increases with age and has more proclivity towards males than females. While all-age incidence and mortality were the highest in high HDI countries led by China (incidence 521,490 and deaths 247,563), the age-standardized rates were the highest in very high HDI countries led by Hungary (ASIR 51.2/100,000) and South Korea (44.5/100,000); ASMR too was the highest in Hungary (21.5/100,000) followed by Slovakia (20.4/100,000). Due to large population size, East Asia led the world regions in terms of all-age incidence and death counts, whereas ASIR and ASMR were the highest in developed regions, e.g., Northern Europe recorded ASIR of 32.1/100,000 and central and eastern Europe recorded ASMR of 15.2/100,000. Both ASIR and ASMR were lowest in south-central Asia at estimated at 4.9/100,000 and 3.6/100,000, respectively, in 2018. Higher incidence in developed societies has already been documented before [20] and is attributable to a greater percentage of the older population, dietary patterns, and availability of screening procedures [21]. Higher risk of males towards CRC has been documented before and can be possibly attributed to factors such as greater prevalence of risk factors such as alcohol and smoking in males [22–24]. The differences in mortality rates, however, also reflect the role of factors other than alcohol and smoking, though it requires more research to provide conclusive evidence.
Ninety percent of CRC incidence and 92% of CRC deaths occurred in 50-plus age group (Fig. 2). As age increases, adenomatous polyps grows slowly from adenoma to frank carcinoma; therefore, CRC deaths can be prevented by the detection and removal of adenomatous polyps through early screening. Although operational screening modalities differ in terms of convenience and cost, mainly two types of screening procedures are currently employed. First is stool based, e.g., fecal occult blood test (FOBT), Guaiac-based FOBT, and fecal immunochemical test (FIT); second involves structural examinations such as flexible sigmoidoscopy and colonoscopy. Colonoscopy is considered to be the gold standard of CRC screening and diagnosis; it has higher specificity and sensitivity than the stool-based methods, the colonoscopy, however, is quite resource-intensive in comparison with stool-based methods [7]. Although different methods vary in terms of efficiency and their implementation varies geographically, randomized control trials have demonstrated that screening methods have been quite effective in early detection of adenomas and colorectal carcinoma, thereby boosting the survival rates [25–29]. There are currently two approaches to screening: population-wide and opportunistic. The population-wide screening is quite prevalent in Western countries, the opportunistic screening, however, had limited success in boosting the take-up rates [30]. As per WHO country survey on cancer control policies, FOBT-based screening procedure was available at public primary level in 82/160 of the responding countries, whereas colonoscopy was present in 70/160 countries (Table 5 of Appendix). Even in those countries where these screening modalities were available, most of the countries belonged to high/very high HDI category. The US Preventive Services Task Force (USPSTF) recommends screening for CRC in the 50–75 age group; those with familial history and other high-risk population are recomended for screening at a comparatively younger age and higher frequency [7]. S A significant percentage of US citizens still had no access to screening in 2010 [31]. Moreover, heterogenous participation rates were observed in developed societies owing to differential socioeconomic status and level of education, thereby resulting in inequalities in the disease outcomes [32].
Table 5.
Country-wise availability of screening modalities
| Population | FOBT | Colonoscopy |
|---|---|---|
| Afghanistan | 0 | 0 |
| Albania | 0 | 0 |
| Algeria | 0 | 0 |
| Angola | ND | ND |
| Argentina | 1 | 1 |
| Armenia | 1 | 0 |
| Australia | 1 | 1 |
| Austria | 1 | 1 |
| Azerbaijan | 1 | 0 |
| Bahamas | 1 | 0 |
| Bahrain | 1 | 1 |
| Bangladesh | 0 | 0 |
| Barbados | 1 | 1 |
| Belarus | ND | ND |
| Belgium | 1 | 1 |
| Belize | 1 | 1 |
| Benin | 0 | 0 |
| Bhutan | 0 | 1 |
| Bolivia | 1 | 0 |
| Bosnia and Herzegovina | ND | ND |
| Botswana | 0 | 0 |
| Brazil | 1 | 1 |
| Brunei | 1 | 1 |
| Bulgaria | 1 | 1 |
| Burkina Faso | 0 | 1 |
| Burundi | 0 | 0 |
| Cabo Verde | ND | ND |
| Cambodia | 0 | DK |
| Cameroon | 1 | 0 |
| Canada | 1 | 1 |
| Central African Republic | 0 | 0 |
| Chad | ND | ND |
| Chile | 1 | 1 |
| China | 1 | 1 |
| Colombia | 1 | 1 |
| Comoros | 1 | 0 |
| Congo | 0 | 1 |
| Costa Rica | 1 | 1 |
| Côte d’Ivoire | 0 | 0 |
| Croatia | 1 | 1 |
| Cuba | 1 | 1 |
| Cyprus | 1 | 1 |
| Czechia | 1 | 1 |
| Democratic Republic of Congo | ND | ND |
| Denmark | 1 | 1 |
| Djibouti | 0 | 0 |
| Dominican Republic | 1 | 0 |
| Ecuador | 1 | 0 |
| Egypt | 1 | 0 |
| El Salvador | 0 | 0 |
| Equatorial Guinea | 0 | 0 |
| Eritrea | 0 | 0 |
| Estonia | 1 | 0 |
| Eswatini | 0 | 0 |
| Ethiopia | ND | ND |
| Fiji | 1 | 1 |
| Finland | 1 | 1 |
| France | 1 | 1 |
| France, Guadeloupe | ||
| France, La Réunion | ||
| France, Martinique | ||
| France, New Caledonia | ||
| French Guyana | ||
| French Polynesia | ||
| Gabon | 1 | 1 |
| Gambia | 0 | 0 |
| Gaza Strip and West Bank | ||
| Georgia | 0 | 0 |
| Germany | 1 | 1 |
| Ghana | 0 | 0 |
| Greece | 1 | 1 |
| Guam | ||
| Guatemala | 0 | 0 |
| Guinea | 0 | 0 |
| Guinea-Bissau | 0 | 0 |
| Guyana | ND | ND |
| Haiti | ND | ND |
| Honduras | 0 | 0 |
| Hungary | 0 | 0 |
| Iceland | 1 | 0 |
| India | 0 | 0 |
| Indonesia | 0 | 0 |
| Iran | 1 | 1 |
| Iraq | 0 | 0 |
| Ireland | 1 | 1 |
| Israel | 1 | 1 |
| Italy | 1 | 1 |
| Jamaica | 1 | 1 |
| Japan | 1 | 1 |
| Jordan | 1 | 0 |
| Kazakhstan | 1 | 1 |
| Kenya | 0 | 0 |
| Kuwait | 0 | 0 |
| Kyrgyzstan | 0 | 0 |
| Lao PDR | DK | 1 |
| Latvia | 1 | 1 |
| Lebanon | 0 | 0 |
| Lesotho | 0 | 0 |
| Liberia | 0 | 0 |
| Libya | 0 | 0 |
| Lithuania | 1 | 1 |
| Luxembourg | 1 | 1 |
| Macedonia FYR | 1 | 1 |
| Madagascar | 0 | 0 |
| Malawi | 0 | 0 |
| Malaysia | 0 | 1 |
| Maldives | 0 | 0 |
| Mali | 0 | 0 |
| Malta | 1 | 1 |
| Mauritania | 0 | 0 |
| Mauritius | ND | ND |
| Mexico | DK | DK |
| Moldova | 1 | 1 |
| Mongolia | 0 | 0 |
| Montenegro | 0 | 0 |
| Morocco | 0 | 1 |
| Mozambique | 0 | 0 |
| Myanmar | 0 | 0 |
| Namibia | 1 | DK |
| Nepal | 0 | 0 |
| Netherlands | 0 | 0 |
| New Zealand | 1 | 0 |
| Nicaragua | 1 | 1 |
| Niger | 0 | 0 |
| Nigeria | 0 | 0 |
| North Korea | 0 | 0 |
| Norway | 1 | 1 |
| Oman | 1 | 1 |
| Pakistan | 0 | 0 |
| Panama | 1 | 0 |
| Papua New Guinea | 1 | 0 |
| Paraguay | 0 | 0 |
| Peru | 0 | 0 |
| Philippines | 0 | 0 |
| Poland | 1 | 1 |
| Portugal | 1 | 1 |
| Puerto Rico | ||
| Qatar | 1 | 0 |
| Romania | 0 | 0 |
| Russian Federation | 1 | 1 |
| Rwanda | 0 | 0 |
| Saint Lucia | 1 | 1 |
| Samoa | 1 | 0 |
| Sao Tome and Principe | 0 | 0 |
| Saudi Arabia | 0 | 0 |
| Senegal | 0 | 1 |
| Serbia | 1 | 1 |
| Sierra Leone | ND | ND |
| Singapore | 1 | 1 |
| Slovakia | 1 | 1 |
| Slovenia | 1 | 1 |
| Solomon Islands | 0 | 0 |
| Somalia | 0 | 0 |
| South Africa | ND | ND |
| South Korea | 1 | 1 |
| South Sudan | ND | ND |
| Spain | 1 | 1 |
| Sri Lanka | 0 | 0 |
| Sudan | 0 | 0 |
| Suriname | 1 | 1 |
| Sweden | 1 | 1 |
| Switzerland | 1 | 1 |
| Syrian Arab Republic | 1 | 1 |
| Tajikistan | NR | NR |
| Tanzania | ND | ND |
| Thailand | 0 | 0 |
| Timor-Leste | ND | ND |
| Togo | 0 | 0 |
| Trinidad and Tobago | 1 | 1 |
| Tunisia | 0 | 0 |
| Turkey | 1 | 1 |
| Turkmenistan | 1 | 1 |
| Uganda | 0 | 0 |
| Ukraine | 0 | 0 |
| United Arab Emirates | 1 | 0 |
| UK | 1 | 0 |
| USA | 1 | 1 |
| Uruguay | 1 | 1 |
| Uzbekistan | 0 | 0 |
| Vanuatu | 0 | 0 |
| Venezuela | 1 | 1 |
| Viet Nam | 0 | 0 |
| Yemen | 0 | 0 |
| Zambia | 0 | 0 |
| Zimbabwe | 0 | 1 |
All the data is procured from WHO Cancer Country Profiles. The answer to the question on screening availability was coded as follows: generally available at the public primary healthcare level (1) and not generally available at the public primary health care level (0). Data was not available for the countries for which no entry is there in the table
DK do not know, ND county did not respond to WHO questionnaire, NR country responded to WHO survey but did not responded to particular question
The modifiable risk factors that are associated with elevated risk of CRC include alcohol [33], smoking [34], red meat [35], obesity [36, 37], and type 2 diabetes [38], whereas fruit and vegetable consumption [39, 40] and physical activity reduce the risk of CRC [41]. The nonmodifiable risk factors of CRC include aging, familial history, preoccurrence of polyps, and inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis [21]. Inflammation has recently been found to be associated with increased incidence of CRC; accordingly, anti-inflammatory drugs like low-dose aspirin has been found to be effective in reducing the CRC incidence [42–44].2
We observed high CRC burden in Asian countries exemplified by high absolute incidence and mortality in China, Japan, India, and South Korea with these four countries accounting for 41.6% (768,755 of 1.85 million) of incident cases and 40.7% (358,325 of 880,792) of global deaths in 2018. Previous studies also reported an increased risk of colorectal carcinoma in Asian populations [3]. The increasing incidence of CRC in these countries is reflective of changing lifestyle and behavior as factors including lack of physical activity and dietary patterns have been shown to be positively associated with high incidence of colorectal neoplasia in developed countries [21, 46]. The first pillar of the PPPM approach advocates for the prevention of CRC via controlling risk factors, the vast majority of which are related to lifestyle [33–41]. Preventable nature of CRC makes it a likely target of PPPM approach to medicine. For targeted therapy and precision medicine envisaged by PPPM, diagnostic, prognostic, and therapeutic markers need to be developed and continually adopted in CRC medicine. Carcinoembryonic antigen (CEA), for instance, has been shown to be a promising prognostic biomarker for CRC [47] and preliminary research has identified few hormones to have prognostic and therapeutic marker properties for CRC, though more research is still needed to explore their full potential [48].
The mortality due to CRC reflects the strength of the healthcare system and infrastructure to prevent, diagnose, and treat the disease. The CRC mortality rates were in concordance with incidence rates with ASMR being the highest in Europe (e.g. Hungary (21.5 per 100,000) and Slovakia (20.4 per 100,000)). The lesser developed (low/medium HDI) countries have comparatively lower ASMR because of large population and relatively lower life expectancy, the survival rates (proxied by MIR), however, were lot higher in developed countries (high/very high HDI) as compared to the lesser developed ones. Statistically too, we found that better socioeconomic status of a country measured using HDI has had strong statistically significant negative effect on MIR (a proxy for 5-year survival rate). Low survival rates in lesser developed countries reflect screening prevalence as well as treatment modalities for CRC, which depend critically upon the stage at which malignancy gets detected. While adenomatous polyps or a low-grade tumor detected during screening can be removed by polypectomy, the late-stage tumor, however, can be treated using colectomy (partial or complete removal of colon) in conjunction with adjuvant (neo)chemotherapy and/or radiotherapy. Few of these treatment modalities such as surgery (even if cancer or polyps are detected early) are insufficiently present in less developed countries [49].
Limitations
The accuracy and validity of the estimates of CRC examined in this paper is crucially dependent upon data availability from cancer registries which is far from complete in many of the less developed countries led by Africa. Therefore, the estimates produced for few countries lacking cancer registry mostly reflect estimates from the neighboring countries [11, 17]. Moreover, for the countries lacking coverage and completeness, the GLOBOCAN estimates reported in this paper are expected to be downward biased. Second, the estimates presented in this paper were available only for 1 year (i.e., 2018) which could not be utilized to gauge the temporal patterns of the CRC burden. Third, we employed MIR as a proxy indicator of 5-year survival rate which is not an exact measure of survival rate. This indicator, however, can serve as a useful proxy for the survival rate of colorectal neoplasia in the absence of country-wise exact measure of survival rate.
Conclusion and expert recommendations
High burden of CRC was estimated in developed countries and was correlated positively with HDI and but is also substantially high in Asian countries. It shows that as countries are moving up in the development hierarchy, they are emulating Westernized lifestyle and dietary habits which have manifested in high CRC incidence in these countries. As the vast majority of risk factors are associated with lifestyle and diet, and screening programs are available, the CRC burden can be curtailed to attain the sustainable development goal (SDG 3) of ensuring a healthy and quality life.
Against the rising burden, it is also noteworhty that CRC deaths can be prevented via primary approaches (i.e., control of risk factors) and secondary prevention using cancer screening; both of these approaches are fundamental to the preventive, predictive, and personalized approach to medicine [8–10]. PPPM approach epitomizes the changing philosophy of healthcare from illness to health, from treatment to prevention and from one-size-fits-all to personalized medicine [50]. PPPM approach to medicine requires effective cancer control policies, aware citizens (at-risk population and patient), healthcare infrastructure, and availability and affordability of various technologies (omics technologies etc) to offer personalized medicine [51, 52]. The adoption of the PPPM approach to cancer management, however, is not easy in the context of developing and less-developed countries. This is because the PPPM approach is an integrated approach that combines advantages of individual bio/medical fields through a multi-professional collaboration [9]; such multi-professional collaboration along with multi-omics approach is quite a challenging and costly task for low-resource economies. Additionally, a large percentage of people in low-resource economies are still poor and lacks access to basic healthcare facilities let alone personalized medicine. Therefore, at the policy level, the following strategies must be adopted for cancer management and control in concordance with PPPM approach to disease managment and control. First, prevention must be adopted as the first-line attack on colorectal carcinoma. The major thrust of any policy intervention must be on providing cost-effective screening services and ensure their availability at the broadest possible level. Second, universal health coverage (UHC) can ensure access to basic health services (screening and treatment), which can later be upgraded to provide precision and personalized medicine. Third, through health literacy campaigns, various preventive approaches, behavioral risk factors, and screening programs must be popularized and made available to high-risk populations. Finally, new-age screening devices, omics technologies, and diagnostic and prognostic biomarker panels suiting the low-cost requirements need to be continuously developed and adopted.
Acknowledgments
The authors thank the International Agency for Research on Cancer (IARC) for making available GLOBOCAN 2018 estimates in the public domain.
Appendix
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The research is conducted using data available in the public domain and does not include any human participants and/or animals.
Footnotes
UNDP defines mean number of years of schooling as the number of years of schooling received by people ages 25 and older, and expected years of schooling s defined as number of years of schooling that a child of school entrance age can expect to receive if prevailing patterns of age-specific enrolment rates persist throughout life [12].
US Preventive Services Task Force (US PSTF) recommends the use of low-dose aspirin for the prevention of colorectal cancer in high-risk patients [45].
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, Abbastabar H, Abd-Allah F, Abdela J, Abdelalim A, Abdollahpour I, Abdulkader RS, Abebe HT, Abebe M, Abebe Z, Abejie AN, Abera SF, Abil OZ, Abraha HN, Abrham AR, Abu-Raddad LJ, Accrombessi MMK, Acharya D, Adamu AA, Adebayo OM, Adedoyin RA, Adekanmbi V, Adetokunboh OO, Adhena BM, Adib MG, Admasie A, Afshin A, Agarwal G, Agesa KM, Agrawal A, Agrawal S, Ahmadi A, Ahmadi M, Ahmed MB, Ahmed S, Aichour AN, Aichour I, Aichour MTE, Akbari ME, Akinyemi RO, Akseer N, al-Aly Z, al-Eyadhy A, al-Raddadi RM, Alahdab F, Alam K, Alam T, Alebel A, Alene KA, Alijanzadeh M, Alizadeh-Navaei R, Aljunid SM, Alkerwi A', Alla F, Allebeck P, Alonso J, Altirkawi K, Alvis-Guzman N, Amare AT, Aminde LN, Amini E, Ammar W, Amoako YA, Anber NH, Andrei CL, Androudi S, Animut MD, Anjomshoa M, Ansari H, Ansha MG, Antonio CAT, Anwari P, Aremu O, Ärnlöv J, Arora A, Arora M, Artaman A, Aryal KK, Asayesh H, Asfaw ET, Ataro Z, Atique S, Atre SR, Ausloos M, Avokpaho EFGA, Awasthi A, Quintanilla BPA, Ayele Y, Ayer R, Azzopardi PS, Babazadeh A, Bacha U, Badali H, Badawi A, Bali AG, Ballesteros KE, Banach M, Banerjee K, Bannick MS, Banoub JAM, Barboza MA, Barker-Collo SL, Bärnighausen TW, Barquera S, Barrero LH, Bassat Q, Basu S, Baune BT, Baynes HW, Bazargan-Hejazi S, Bedi N, Beghi E, Behzadifar M, Behzadifar M, Béjot Y, Bekele BB, Belachew AB, Belay E, Belay YA, Bell ML, Bello AK, Bennett DA, Bensenor IM, Berman AE, Bernabe E, Bernstein RS, Bertolacci GJ, Beuran M, Beyranvand T, Bhalla A, Bhattarai S, Bhaumik S, Bhutta ZA, Biadgo B, Biehl MH, Bijani A, Bikbov B, Bilano V, Bililign N, Bin Sayeed MS, Bisanzio D, Biswas T, Blacker BF, Basara BB, Borschmann R, Bosetti C, Bozorgmehr K, Brady OJ, Brant LC, Brayne C, Brazinova A, Breitborde NJK, Brenner H, Briant PS, Britton G, Brugha T, Busse R, Butt ZA, Callender CSKH, Campos-Nonato IR, Campuzano Rincon JC, Cano J, Car M, Cárdenas R, Carreras G, Carrero JJ, Carter A, Carvalho F, Castañeda-Orjuela CA, Castillo Rivas J, Castle CD, Castro C, Castro F, Catalá-López F, Cerin E, Chaiah Y, Chang JC, Charlson FJ, Chaturvedi P, Chiang PPC, Chimed-Ochir O, Chisumpa VH, Chitheer A, Chowdhury R, Christensen H, Christopher DJ, Chung SC, Cicuttini FM, Ciobanu LG, Cirillo M, Cohen AJ, Cooper LT, Cortesi PA, Cortinovis M, Cousin E, Cowie BC, Criqui MH, Cromwell EA, Crowe CS, Crump JA, Cunningham M, Daba AK, Dadi AF, Dandona L, Dandona R, Dang AK, Dargan PI, Daryani A, Das SK, Gupta RD, Neves JD, Dasa TT, Dash AP, Davis AC, Davis Weaver N, Davitoiu DV, Davletov K, de la Hoz FP, de Neve JW, Degefa MG, Degenhardt L, Degfie TT, Deiparine S, Demoz GT, Demtsu BB, Denova-Gutiérrez E, Deribe K, Dervenis N, Des Jarlais DC, Dessie GA, Dey S, Dharmaratne SD, Dicker D, Dinberu MT, Ding EL, Dirac MA, Djalalinia S, Dokova K, Doku DT, Donnelly CA, Dorsey ER, Doshi PP, Douwes-Schultz D, Doyle KE, Driscoll TR, Dubey M, Dubljanin E, Duken EE, Duncan BB, Duraes AR, Ebrahimi H, Ebrahimpour S, Edessa D, Edvardsson D, Eggen AE, el Bcheraoui C, el Sayed Zaki M, el-Khatib Z, Elkout H, Ellingsen CL, Endres M, Endries AY, Er B, Erskine HE, Eshrati B, Eskandarieh S, Esmaeili R, Esteghamati A, Fakhar M, Fakhim H, Faramarzi M, Fareed M, Farhadi F, Farinha CSE, Faro A, Farvid MS, Farzadfar F, Farzaei MH, Feigin VL, Feigl AB, Fentahun N, Fereshtehnejad SM, Fernandes E, Fernandes JC, Ferrari AJ, Feyissa GT, Filip I, Finegold S, Fischer F, Fitzmaurice C, Foigt NA, Foreman KJ, Fornari C, Frank TD, Fukumoto T, Fuller JE, Fullman N, Fürst T, Furtado JM, Futran ND, Gallus S, Garcia-Basteiro AL, Garcia-Gordillo MA, Gardner WM, Gebre AK, Gebrehiwot TT, Gebremedhin AT, Gebremichael B, Gebremichael TG, Gelano TF, Geleijnse JM, Genova-Maleras R, Geramo YCD, Gething PW, Gezae KE, Ghadami MR, Ghadimi R, Ghasemi Falavarjani K, Ghasemi-Kasman M, Ghimire M, Gibney KB, Gill PS, Gill TK, Gillum RF, Ginawi IA, Giroud M, Giussani G, Goenka S, Goldberg EM, Goli S, Gómez-Dantés H, Gona PN, Gopalani SV, Gorman TM, Goto A, Goulart AC, Gnedovskaya EV, Grada A, Grosso G, Gugnani HC, Guimaraes ALS, Guo Y, Gupta PC, Gupta R, Gupta R, Gupta T, Gutiérrez RA, Gyawali B, Haagsma JA, Hafezi-Nejad N, Hagos TB, Hailegiyorgis TT, Hailu GB, Haj-Mirzaian A, Haj-Mirzaian A, Hamadeh RR, Hamidi S, Handal AJ, Hankey GJ, Harb HL, Harikrishnan S, Haro JM, Hasan M, Hassankhani H, Hassen HY, Havmoeller R, Hay RJ, Hay SI, He Y, Hedayatizadeh-Omran A, Hegazy MI, Heibati B, Heidari M, Hendrie D, Henok A, Henry NJ, Herteliu C, Heydarpour F, Heydarpour P, Heydarpour S, Hibstu DT, Hoek HW, Hole MK, Homaie Rad E, Hoogar P, Hosgood HD, Hosseini SM, Hosseinzadeh M, Hostiuc M, Hostiuc S, Hotez PJ, Hoy DG, Hsiao T, Hu G, Huang JJ, Husseini A, Hussen MM, Hutfless S, Idrisov B, Ilesanmi OS, Iqbal U, Irvani SSN, Irvine CMS, Islam N, Islam SMS, Islami F, Jacobsen KH, Jahangiry L, Jahanmehr N, Jain SK, Jakovljevic M, Jalu MT, James SL, Javanbakht M, Jayatilleke AU, Jeemon P, Jenkins KJ, Jha RP, Jha V, Johnson CO, Johnson SC, Jonas JB, Joshi A, Jozwiak JJ, Jungari SB, Jürisson M, Kabir Z, Kadel R, Kahsay A, Kalani R, Karami M, Karami Matin B, Karch A, Karema C, Karimi-Sari H, Kasaeian A, Kassa DH, Kassa GM, Kassa TD, Kassebaum NJ, Katikireddi SV, Kaul A, Kazemi Z, Karyani AK, Kazi DS, Kefale AT, Keiyoro PN, Kemp GR, Kengne AP, Keren A, Kesavachandran CN, Khader YS, Khafaei B, Khafaie MA, Khajavi A, Khalid N, Khalil IA, Khan EA, Khan MS, Khan MA, Khang YH, Khater MM, Khoja AT, Khosravi A, Khosravi MH, Khubchandani J, Kiadaliri AA, Kibret GD, Kidanemariam ZT, Kiirithio DN, Kim D, Kim YE, Kim YJ, Kimokoti RW, Kinfu Y, Kisa A, Kissimova-Skarbek K, Kivimäki M, Knudsen AKS, Kocarnik JM, Kochhar S, Kokubo Y, Kolola T, Kopec JA, Koul PA, Koyanagi A, Kravchenko MA, Krishan K, Kuate Defo B, Kucuk Bicer B, Kumar GA, Kumar M, Kumar P, Kutz MJ, Kuzin I, Kyu HH, Lad DP, Lad SD, Lafranconi A, Lal DK, Lalloo R, Lallukka T, Lam JO, Lami FH, Lansingh VC, Lansky S, Larson HJ, Latifi A, Lau KMM, Lazarus JV, Lebedev G, Lee PH, Leigh J, Leili M, Leshargie CT, Li S, Li Y, Liang J, Lim LL, Lim SS, Limenih MA, Linn S, Liu S, Liu Y, Lodha R, Lonsdale C, Lopez AD, Lorkowski S, Lotufo PA, Lozano R, Lunevicius R, Ma S, Macarayan ERK, Mackay MT, MacLachlan JH, Maddison ER, Madotto F, Magdy Abd el Razek H, Magdy Abd el Razek M, Maghavani DP, Majdan M, Majdzadeh R, Majeed A, Malekzadeh R, Malta DC, Manda AL, Mandarano-Filho LG, Manguerra H, Mansournia MA, Mapoma CC, Marami D, Maravilla JC, Marcenes W, Marczak L, Marks A, Marks GB, Martinez G, Martins-Melo FR, Martopullo I, März W, Marzan MB, Masci JR, Massenburg BB, Mathur MR, Mathur P, Matzopoulos R, Maulik PK, Mazidi M, McAlinden C, McGrath JJ, McKee M, McMahon BJ, Mehata S, Mehndiratta MM, Mehrotra R, Mehta KM, Mehta V, Mekonnen TC, Melese A, Melku M, Memiah PTN, Memish ZA, Mendoza W, Mengistu DT, Mengistu G, Mensah GA, Mereta ST, Meretoja A, Meretoja TJ, Mestrovic T, Mezgebe HB, Miazgowski B, Miazgowski T, Millear AI, Miller TR, Miller-Petrie MK, Mini GK, Mirabi P, Mirarefin M, Mirica A, Mirrakhimov EM, Misganaw AT, Mitiku H, Moazen B, Mohammad KA, Mohammadi M, Mohammadifard N, Mohammed MA, Mohammed S, Mohan V, Mokdad AH, Molokhia M, Monasta L, Moradi G, Moradi-Lakeh M, Moradinazar M, Moraga P, Morawska L, Moreno Velásquez I, Morgado-da-Costa J, Morrison SD, Moschos MM, Mouodi S, Mousavi SM, Muchie KF, Mueller UO, Mukhopadhyay S, Muller K, Mumford JE, Musa J, Musa KI, Mustafa G, Muthupandian S, Nachega JB, Nagel G, Naheed A, Nahvijou A, Naik G, Nair S, Najafi F, Naldi L, Nam HS, Nangia V, Nansseu JR, Nascimento BR, Natarajan G, Neamati N, Negoi I, Negoi RI, Neupane S, Newton CRJ, Ngalesoni FN, Ngunjiri JW, Nguyen AQ, Nguyen G, Nguyen HT, Nguyen HT, Nguyen LH, Nguyen M, Nguyen TH, Nichols E, Ningrum DNA, Nirayo YL, Nixon MR, Nolutshungu N, Nomura S, Norheim OF, Noroozi M, Norrving B, Noubiap JJ, Nouri HR, Nourollahpour Shiadeh M, Nowroozi MR, Nyasulu PS, Odell CM, Ofori-Asenso R, Ogbo FA, Oh IH, Oladimeji O, Olagunju AT, Olivares PR, Olsen HE, Olusanya BO, Olusanya JO, Ong KL, Ong SKS, Oren E, Orpana HM, Ortiz A, Ortiz JR, Otstavnov SS, Øverland S, Owolabi MO, Özdemir R, P A M, Pacella R, Pakhale S, Pakhare AP, Pakpour AH, Pana A, Panda-Jonas S, Pandian JD, Parisi A, Park EK, Parry CDH, Parsian H, Patel S, Pati S, Patton GC, Paturi VR, Paulson KR, Pereira A, Pereira DM, Perico N, Pesudovs K, Petzold M, Phillips MR, Piel FB, Pigott DM, Pillay JD, Pirsaheb M, Pishgar F, Polinder S, Postma MJ, Pourshams A, Poustchi H, Pujar A, Prakash S, Prasad N, Purcell CA, Qorbani M, Quintana H, Quistberg DA, Rade KW, Radfar A, Rafay A, Rafiei A, Rahim F, Rahimi K, Rahimi-Movaghar A, Rahman M, Rahman MHU, Rahman MA, Rai RK, Rajsic S, Ram U, Ranabhat CL, Ranjan P, Rao PC, Rawaf DL, Rawaf S, Razo-García C, Reddy KS, Reiner RC, Reitsma MB, Remuzzi G, Renzaho AMN, Resnikoff S, Rezaei S, Rezaeian S, Rezai MS, Riahi SM, Ribeiro ALP, Rios-Blancas MJ, Roba KT, Roberts NLS, Robinson SR, Roever L, Ronfani L, Roshandel G, Rostami A, Rothenbacher D, Roy A, Rubagotti E, Sachdev PS, Saddik B, Sadeghi E, Safari H, Safdarian M, Safi S, Safiri S, Sagar R, Sahebkar A, Sahraian MA, Salam N, Salama JS, Salamati P, Saldanha RDF, Saleem Z, Salimi Y, Salvi SS, Salz I, Sambala EZ, Samy AM, Sanabria J, Sanchez-Niño MD, Santomauro DF, Santos IS, Santos JV, Milicevic MMS, Sao Jose BP, Sarker AR, Sarmiento-Suárez R, Sarrafzadegan N, Sartorius B, Sarvi S, Sathian B, Satpathy M, Sawant AR, Sawhney M, Saxena S, Sayyah M, Schaeffner E, Schmidt MI, Schneider IJC, Schöttker B, Schutte AE, Schwebel DC, Schwendicke F, Scott JG, Sekerija M, Sepanlou SG, Serván-Mori E, Seyedmousavi S, Shabaninejad H, Shackelford KA, Shafieesabet A, Shahbazi M, Shaheen AA, Shaikh MA, Shams-Beyranvand M, Shamsi M, Shamsizadeh M, Sharafi K, Sharif M, Sharif-Alhoseini M, Sharma R, She J, Sheikh A, Shi P, Shiferaw MS, Shigematsu M, Shiri R, Shirkoohi R, Shiue I, Shokraneh F, Shrime MG, Si S, Siabani S, Siddiqi TJ, Sigfusdottir ID, Sigurvinsdottir R, Silberberg DH, Silva DAS, Silva JP, Silva NTD, Silveira DGA, Singh JA, Singh NP, Singh PK, Singh V, Sinha DN, Sliwa K, Smith M, Sobaih BH, Sobhani S, Sobngwi E, Soneji SS, Soofi M, Sorensen RJD, Soriano JB, Soyiri IN, Sposato LA, Sreeramareddy CT, Srinivasan V, Stanaway JD, Starodubov VI, Stathopoulou V, Stein DJ, Steiner C, Stewart LG, Stokes MA, Subart ML, Sudaryanto A, Sufiyan M'B, Sur PJ, Sutradhar I, Sykes BL, Sylaja PN, Sylte DO, Szoeke CEI, Tabarés-Seisdedos R, Tabuchi T, Tadakamadla SK, Takahashi K, Tandon N, Tassew SG, Taveira N, Tehrani-Banihashemi A, Tekalign TG, Tekle MG, Temsah MH, Temsah O, Terkawi AS, Teshale MY, Tessema B, Tessema GA, Thankappan KR, Thirunavukkarasu S, Thomas N, Thrift AG, Thurston GD, Tilahun B, To QG, Tobe-Gai R, Tonelli M, Topor-Madry R, Torre AE, Tortajada-Girbés M, Touvier M, Tovani-Palone MR, Tran BX, Tran KB, Tripathi S, Troeger CE, Truelsen TC, Truong NT, Tsadik AG, Tsoi D, Tudor Car L, Tuzcu EM, Tyrovolas S, Ukwaja KN, Ullah I, Undurraga EA, Updike RL, Usman MS, Uthman OA, Uzun SB, Vaduganathan M, Vaezi A, Vaidya G, Valdez PR, Varavikova E, Vasankari TJ, Venketasubramanian N, Villafaina S, Violante FS, Vladimirov SK, Vlassov V, Vollset SE, Vos T, Wagner GR, Wagnew FS, Waheed Y, Wallin MT, Walson JL, Wang Y, Wang YP, Wassie MM, Weiderpass E, Weintraub RG, Weldegebreal F, Weldegwergs KG, Werdecker A, Werkneh AA, West TE, Westerman R, Whiteford HA, Widecka J, Wilner LB, Wilson S, Winkler AS, Wiysonge CS, Wolfe CDA, Wu S, Wu YC, Wyper GMA, Xavier D, Xu G, Yadgir S, Yadollahpour A, Yahyazadeh Jabbari SH, Yakob B, Yan LL, Yano Y, Yaseri M, Yasin YJ, Yentür GK, Yeshaneh A, Yimer EM, Yip P, Yirsaw BD, Yisma E, Yonemoto N, Yonga G, Yoon SJ, Yotebieng M, Younis MZ, Yousefifard M, Yu C, Zadnik V, Zaidi Z, Zaman SB, Zamani M, Zare Z, Zeleke AJ, Zenebe ZM, Zhang AL, Zhang K, Zhou M, Zodpey S, Zuhlke LJ, Naghavi M, Murray CJL. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fitzmaurice C, Akinyemiju TF, Al Lami FH, Alam T, Alizadeh-Navaei R, Allen C, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2016: a systematic analysis for the global burden of disease study. JAMA Oncol. 2018;4:1553–68. [DOI] [PMC free article] [PubMed]
- 3.Sung JJ, Lau JY, Goh KL, Leung WK. Increasing incidence of colorectal cancer in Asia: implications for screening. Lancet Oncol. 2005;6:871–876. doi: 10.1016/S1470-2045(05)70422-8. [DOI] [PubMed] [Google Scholar]
- 4.Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–1075. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamilton SR, Bosman FT, Boffetta P, et al. Carcinoma of the colon and rectum. In: In Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO classification of tumours of the digestive system. Lyon: IARC Press; 2010. p. 134–46.
- 6.Taylor David P., Burt Randall W., Williams Marc S., Haug Peter J., Cannon–Albright Lisa A. Population-Based Family History–Specific Risks for Colorectal Cancer: A Constellation Approach. Gastroenterology. 2010;138(3):877–885. doi: 10.1053/j.gastro.2009.11.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW, García FA, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2016;315:2564–75. [DOI] [PubMed]
- 8.Grech G, Zhan X, Yoo BC, Bubnov R, Hagan S, Danesi R, Vittadini G, Desiderio DM. EPMA position paper in cancer: current overview and future perspectives. EPMA J. 2015;6:9. doi: 10.1186/s13167-015-0030-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, Krapfenbauer K, Mozaffari MS, Costigliola V. Medicine in the early twenty-first century: paradigm and anticipation - EPMA position paper 2016. EPMA J. 2016;7:23. doi: 10.1186/s13167-016-0072-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Janssens JP, Schuster K, Voss A. Preventive, predictive, and personalized medicine for effective and affordable cancer care. EPMA J. 2018;9:113–123. doi: 10.1007/s13167-018-0130-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 12.UNDP (2018). Human Development Indices and Indicators 2018 Statistical Update. Available at http://hdr.undp.org/sites/default/files/2018_human_development_statistical_update.pdf (Accessed: 3.5.2019).
- 13.Vostakolaei F, Karim-Kos HE, Janssen-Heijnen ML, Visser O, Verbeek AL, Kiemeney LA. The validity of the mortality to incidence ratio as a proxy for site-specific cancer survival. Eur J Pub Health. 2010;21:573–577. doi: 10.1093/eurpub/ckq120. [DOI] [PubMed] [Google Scholar]
- 14.Sunkara V, Hebert JR. The colorectal cancer mortality-to-incidence ratio as an indicator of global cancer screening and care. Cancer. 2015;121:1563–1569. doi: 10.1002/cncr.29228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma R. Breast cancer incidence, mortality and mortality-to-incidence ratio (MIR) are associated with human development, 1990–2016: evidence from Global Burden of Disease Study 2016. Breast Cancer. 2019;26:428–445. doi: 10.1007/s12282-018-00941-4. [DOI] [PubMed] [Google Scholar]
- 16.Sharma R. The burden of prostate cancer is associated with human development index: evidence from 87 countries, 1990–2016. EPMA J. 2019;10:137–152. doi: 10.1007/s13167-019-00169-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, Znaor A, Bray F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144:1941–1953. doi: 10.1002/ijc.31937. [DOI] [PubMed] [Google Scholar]
- 18.Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M et al (2018). Global Cancer Observatory. Lyon, France: International Agency for Research on Cancer. Available from: https://gco.iarc.fr/, accessed [01.05.2019].
- 19.Human Development Database: http://hdr.undp.org/en/data# (Accessed: 3.5.2019).
- 20.Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66:683–691. doi: 10.1136/gutjnl-2015-310912. [DOI] [PubMed] [Google Scholar]
- 21.Haggar FA, Boushey RP. Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg. 2009;22:191–197. doi: 10.1055/s-0029-1242458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Devesa SS, Chow WH. Variation in colorectal cancer incidence in the United States by subsite of origin. Cancer. 1993;71:3819–3826. doi: 10.1002/1097-0142(19930615)71:12<3819::aid-cncr2820711206>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 23.Cheng X, Chen VW, Steele B, Ruiz B, Fulton J, Liu L, Carozza SE, Greenlee R. Subsite-specific incidence rate and stage of disease in colorectal cancer by race, gender, and age group in the United States, 1992–1997. Cancer. 2001;92:2547–2554. doi: 10.1002/1097-0142(20011115)92:10<2547::aid-cncr1606>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 24.Murphy G, Devesa SS, Cross AJ, Inskip PD, McGlynn KA, Cook MB. Sex disparities in colorectal cancer incidence by anatomic subsite, race and age. Int J Cancer. 2011;128:1668–1675. doi: 10.1002/ijc.25481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JM, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010;375:1624–1633. doi: 10.1016/S0140-6736(10)60551-X. [DOI] [PubMed] [Google Scholar]
- 26.Segnan N, Armaroli P, Bonelli L, Risio M, Sciallero S, Zappa M, Andreoni B, Arrigoni A, Bisanti L, Casella C, Crosta C, Falcini F, Ferrero F, Giacomin A, Giuliani O, Santarelli A, Visioli CB, Zanetti R, Atkin WS, Senore C, and the SCORE Working Group Once-only sigmoidoscopy in colorectal cancer screening: follow-up findings of the Italian Randomized Controlled Trial—SCORE. J Natl Cancer Inst. 2011;103:1310–1322. doi: 10.1093/jnci/djr284. [DOI] [PubMed] [Google Scholar]
- 27.Schoen RE, Pinsky PF, Weissfeld JL, Yokochi LA, Church T, Laiyemo AO, Bresalier R, Andriole GL, Buys SS, Crawford ED, Fouad MN, Isaacs C, Johnson CC, Reding DJ, O'Brien B, Carrick DM, Wright P, Riley TL, Purdue MP, Izmirlian G, Kramer BS, Miller AB, Gohagan JK, Prorok PC, Berg CD, PLCO Project Team Colorectal-cancer incidence and mortality with screening flexible sigmoidoscopy. N Engl J Med. 2012;366:2345–2357. doi: 10.1056/NEJMoa1114635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holme Ø, Bretthauer M, Fretheim A, Odgaard-Jensen J, Hoff G. Flexible sigmoidoscopy versus faecal occult blood testing for colorectal cancer screening in asymptomatic individuals. Cochrane Database Syst Rev. 2013;9:CD0009259 [DOI] [PMC free article] [PubMed]
- 29.Holme Øyvind, Løberg Magnus, Kalager Mette, Bretthauer Michael, Hernán Miguel A., Aas Eline, Eide Tor J., Skovlund Eva, Schneede Jørn, Tveit Kjell Magne, Hoff Geir. Effect of Flexible Sigmoidoscopy Screening on Colorectal Cancer Incidence and Mortality. JAMA. 2014;312(6):606. doi: 10.1001/jama.2014.8266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schreuders EH, Ruco A, Rabeneck L, Schoen RE, Sung JJ, Young GP, et al. Colorectal cancer screening: a global overview of existing programmes. Gut. 2015;64:1637–1649. doi: 10.1136/gutjnl-2014-309086. [DOI] [PubMed] [Google Scholar]
- 31.Shapiro JA, Klabunde CN, Thompson TD, Nadel MR, Seeff LC, White A. Patterns of colorectal cancer test use, including CT colonography, in the 2010 National Health Interview Survey. Cancer Epidemiol Biomark Prev. 2012;21:895–904. doi: 10.1158/1055-9965.EPI-12-0192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Decker KM, Singh H. Reducing inequalities in colorectal cancer screening in North America. J Carcinog. 2014;13:12. doi: 10.4103/1477-3163.144576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fedirko V, Tramacere I, Bagnardi V, Rota M, Scotti L, Islami F. Alcohol drinking and colorectal cancer risk: an overall and dose–response meta-analysis of published studies. Ann Oncol. 2011;22:1958–1972. doi: 10.1093/annonc/mdq653. [DOI] [PubMed] [Google Scholar]
- 34.Botteri Edoardo, Iodice Simona, Bagnardi Vincenzo, Raimondi Sara, Lowenfels Albert B., Maisonneuve Patrick. Smoking and Colorectal Cancer. JAMA. 2008;300(23):2765. doi: 10.1001/jama.2008.839. [DOI] [PubMed] [Google Scholar]
- 35.Demeyer D, Mertens B, De Smet S, Ulens M. Mechanisms linking colorectal cancer to the consumption of (processed) red meat: a review. Crit Rev Food Sci Nutr. 2016;56:2747–2766. doi: 10.1080/10408398.2013.873886. [DOI] [PubMed] [Google Scholar]
- 36.Bardou M, Barkun AN, Martel M. Obesity and colorectal cancer. Gut. 2013;62:933–947. doi: 10.1136/gutjnl-2013-304701. [DOI] [PubMed] [Google Scholar]
- 37.Moghaddam AA, Woodward M, Huxley R. Obesity and risk of colorectal cancer: a meta-analysis of 31 studies with 70,000 events. Cancer Epidemiol Biomark Prev. 2007;16:2533–2547. doi: 10.1158/1055-9965.EPI-07-0708. [DOI] [PubMed] [Google Scholar]
- 38.Peeters PJ, Bazelier MT, Leufkens HG, de Vries F, De Bruin ML. The risk of colorectal cancer in patients with type 2 diabetes: associations with treatment stage and obesity. Diabetes Care. 2015;38:495–502. doi: 10.2337/dc14-1175. [DOI] [PubMed] [Google Scholar]
- 39.Terry P, Giovannucci E, Michels KB, Bergkvist L, Hansen H, Holmberg L, Wolk A. Fruit, vegetables, dietary fiber, and risk of colorectal cancer. J Natl Cancer Inst. 2001;93:525–533. doi: 10.1093/jnci/93.7.525. [DOI] [PubMed] [Google Scholar]
- 40.Van Duijnhoven FJ, Bueno-De-Mesquita HB, Ferrari P, Jenab M, Boshuizen HC, Ros MM, et al. Fruit, vegetables, and colorectal cancer risk: the European Prospective Investigation into Cancer and Nutrition. Am J Clin Nutr. 2009;89:1441–1452. doi: 10.3945/ajcn.2008.27120. [DOI] [PubMed] [Google Scholar]
- 41.Huxley RR, Ansary-Moghaddam A, Clifton P, Czernichow S, Parr CL, Woodward M. The impact of dietary and lifestyle risk factors on risk of colorectal cancer: a quantitative overview of the epidemiological evidence. Int J Cancer. 2009;125:171–180. doi: 10.1002/ijc.24343. [DOI] [PubMed] [Google Scholar]
- 42.Rothwell PM, Wilson M, Elwin CE, Norrving B, Algra A, Warlow CP, Meade TW. Long-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of five randomised trials. Lancet. 2010;376:1741–1750. doi: 10.1016/S0140-6736(10)61543-7. [DOI] [PubMed] [Google Scholar]
- 43.Rothwell PM, Fowkes FG, Belch JF, Ogawa H, Warlow CP, Meade TW. Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials. Lancet. 2011;377:31–41. doi: 10.1016/S0140-6736(10)62110-1. [DOI] [PubMed] [Google Scholar]
- 44.Burn J, Gerdes AM, Macrae F, Mecklin JP, Moeslein G, Olschwang S, Eccles D, Evans DG, Maher ER, Bertario L, Bisgaard ML, Dunlop MG, Ho JWC, Hodgson SV, Lindblom A, Lubinski J, Morrison PJ, Murday V, Ramesar R, Side L, Scott RJ, Thomas HJW, Vasen HF, Barker G, Crawford G, Elliott F, Movahedi M, Pylvanainen K, Wijnen JT, Fodde R, Lynch HT, Mathers JC, Bishop DT. Long-term effect of aspirin on cancer risk in carriers of hereditary colorectal cancer: an analysis from the CAPP2 randomised controlled trial. Lancet. 2011;378:2081–2087. doi: 10.1016/S0140-6736(11)61049-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chubak J, Kamineni A, Buist DSM, Anderson ML & Whitlock EP (2015) Aspirin use for the prevention of colorectal cancer: an updated systematic evidence review for the U.S. Preventive Services Task Force (Agency for Healthcare Research and Quality (US), 2015). [PubMed]
- 46.Gonzalez CA, Riboli E. Diet and cancer prevention: contributions from the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Eur J Cancer. 2010;46:2555–2562. doi: 10.1016/j.ejca.2010.07.025. [DOI] [PubMed] [Google Scholar]
- 47.Thirunavukarasu P, Sukumar S, Sathaiah M, Mahan M, Pragatheeshwar KD, Pingpank JF, Zeh H, Bartels CJ, Lee KKW, Bartlett DL. C-stage in colon cancer: implications of carcinoembryonic antigen biomarker in staging, prognosis, and management. J Natl Cancer Inst. 2011;103:689–697. doi: 10.1093/jnci/djr078. [DOI] [PubMed] [Google Scholar]
- 48.Nikolaou S, Qiu S, Fiorentino F, Rasheed S, Tekkis P, Kontovounisios C. The prognostic and therapeutic role of hormones in colorectal cancer: a review. Mol Biol Rep. 2019:461477–86. [DOI] [PubMed]
- 49.Sullivan R, Alatise OI, Anderson BO, Audisio R, Autier P, Aggarwal A, Balch C, Brennan MF, Dare A, D'Cruz A, Eggermont AMM, Fleming K, Gueye SM, Hagander L, Herrera CA, Holmer H, Ilbawi AM, Jarnheimer A, Ji JF, Kingham TP, Liberman J, Leather AJM, Meara JG, Mukhopadhyay S, Murthy SS, Omar S, Parham GP, Pramesh CS, Riviello R, Rodin D, Santini L, Shrikhande SV, Shrime M, Thomas R, Tsunoda AT, van de Velde C, Veronesi U, Vijaykumar DK, Watters D, Wang S, Wu YL, Zeiton M, Purushotham A. Global cancer surgery: delivering safe, affordable, and timely cancer surgery. Lancet Oncol. 2015;16:1193–1224. doi: 10.1016/S1470-2045(15)00223-5. [DOI] [PubMed] [Google Scholar]
- 50.Lu M, Zhan X. The crucial role of multiomic approach in cancer research and clinically relevant outcomes. EPMA J. 2018;9:77–102. doi: 10.1007/s13167-018-0128-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Horgan RP, Kenny LC. ‘Omic’ technologies: genomics, transcriptomics, proteomics and metabolomics. Obstet Gynaecol. 2011;13:189–195. [Google Scholar]
- 52.Golubnitschaja O, Kinkorova J, Costigliola V. Predictive, preventive and personalized medicine as the hardcore of ‘Horizon 2020’: EPMA position paper. EPMA J. 2014;5:6. doi: 10.1186/1878-5085-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]