Abstract
The lateral talocalcaneal ligament (LTCL) connects the talus and calcaneus on the lateral side of the hindfoot. Although its function remains has not yet been clearly elucidated, the LTCL is thought to be important for the stabilization of the subtalar joint. Ankle sprains often include not only the talocrural joint but also the subtalar joint; therefore, LTCL injuries occur at a certain rate. Moreover, surgeons often encounter and reluctantly dissect the LTCL during arthroscopic anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL) reconstruction because the LTCL connects to the ATFL at the talus in 42% of people and connects to the CFL at the calcaneus in 18% of people. As a result, LTCL reconstruction might be necessary for those patients. We describe the arthroscopic reconstruction technique of the ATFL, LTCL, and CFL using a triangle-shaped tendon graft (ALC-triangle). This technique provides a possible advantage of an anatomical and stable talocrural joint and subtalar joint.
Introduction (With Video Illustration)
The lateral talocalcaneal ligament (LTCL) connects the talus and the calcaneus on the lateral side of the hindfoot. Its existence rate is reported from 42% to 66%.1, 2, 3 As the LTCL connects to the anterior talofibular ligament (ATFL) at the talar attachment site in 42% of people and combines with the calcaneofibular ligament (CFL) at the calcaneus in 18% of people,3 LTCL injury is likely to be concomitant with ATFL and/or CFL injury.
Several reports of arthroscopic lateral ankle ligament reconstruction for the ATFL,4, 5, 6, 7 CFL,8, 9, 10, 11, 12, 13, 14 and posterior talofibular ligament exist.15 Here, we describe the arthroscopic reconstruction of the ATFL, LTCL, and CFL using a triangle-shaped tendon graft (ALC-triangle). A summary of key steps is provided in Table 1, whereas a summary of the technique is provided in Video 1.
Table 1.
Key Surgical Steps, Pearls, and Pitfalls
| Key Surgical Steps | Pearls | Pitfalls |
|---|---|---|
| Harvesting a hamstring tendon | The harvested tendon usually needs to be longer than 175 mm. A semitendinosus tendon is harvested if the gracilis is too thin or too short. The length is determined by preoperative images. | Too short a tendon will make it difficult to prepare the graft. |
| Creation of the AM portal | The ankle is positioned in neutral position. AM portal is created medial to the anterior tibial tendon. | If the AM portal is created too medially, visualization of the ATFL remnant will be difficult. |
| Creation of the AAL portal | The ankle is dorsiflexed to view the ATFL remnant. Before the AAL portal is created, a needle is inserted into the portal site to confirm accessibility to the ATFL talar footprint. | If the AAL portal is created without confirmation by the needle, the AAL portal position will not be suitable for the talar tunnel creation. |
| Creation of the talar tunnel | A guidewire is inserted through the AAL portal to drill the talus toward the distal end of the medial malleolus. | If a guidewire is directed too posterior, the neurovascular bundle is at risk for damage. If the tunnel is deeper than 20 mm, the risk of the talar penetration may be greater. |
| Creation of the ST portal | The ST portal is created just below the FOT after confirming accessibility to the fibular footprint by needle. | If the ST portal is created too anteriorly, fibular tunnel direction will be distal, and the risk of tunnel fracture will be greater. |
| Creation of the fibular tunnel | Intraoperative fluoroscopy is used to confirm the guidewire position and direction. | If fibular tunnel is created without fluoroscopy assistance, the risk of the tunnel fracture and tunnel malposition may be greater. |
| Dissection of the CFL remnant and the LTCL remnant | The shaver opening can be safely directed toward the calcaneus during the remnant dissection. | If the shaver opening is directed to lateral or distal, the peroneal tendon may be damaged. |
| Creation of the calcaneal tunnel | A 25- to 30-mm deep calcaneal tunnel is overdrilled through the ST portal. The drill should pass gently near the peroneal tendon. | If the tunnel is drilled through the AAL portal, the drill angle to the calcaneal surface will be too sharp and tunnel wall fracture may happen. |
| Placement of the suture anchor to the fibular tunnel | If a drill wire does not reach the opposite cortex, the surgeon can insert it from anterior from anterior edge of the tunnel inlet to the posterior and proximal. | If a drill wire does not reach the opposite cortex, the suture anchor will be placed within the fibula cancellous bone and the graft fixation strength will be weak. |
| Graft fixation | If the screw insertion is too hard in the fibular tunnel, a smaller screw should be chosen, or the suture anchor fixation alone is enough. | If the screw is too big for the fibular tunnel fixation, the tunnel wall fracture will occur. |
AAL, accessory anterolateral; AM, anteromedial; ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; FOT, fibular obscure tubercle; LTCL, lateral talocalcaneal ligament; ST, subtalar.
Surgical Technique
Step 1: Patient Positioning
This surgery is performed with the patient under general anesthesia and in the supine position. A tourniquet is placed on the proximal thigh. The foot is suspended from the distal edge of the bed. The contralateral leg is slightly lowered to provide a wide working space.7,12
Step 2: Graft Preparation
The gracilis tendon is harvested from the pes anserinus and a triangle-shaped graft is prepared. The semitendinosus tendon is used if the gracilis tendon is too thin or too short. An endoscopic harvest technique is recommended for a smaller skin incision scar.16 The allograft tendon is also an alternative.
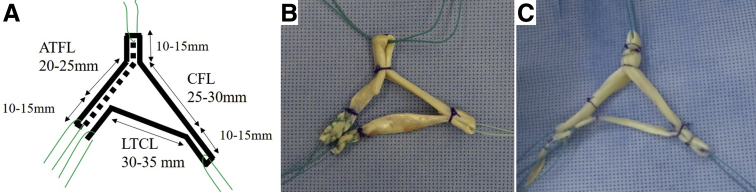
The harvested tendon usually needs to be longer than 175 mm. It is needed for one strand of a 20- to 25-mm long bundle for the ATFL graft, one strand of a 30- to 35-mm long bundle for the LTCL graft, and one strand of 25- to 30-mm long bundle for the CFL graft. The length is determined by a preoperative radiograph and magnetic resonance imaging. The 4 ends form a 10- to 15-mm long loop or free-end to facilitate the attachment of the thread for graft delivery. The talar side ends of the LTCL and the ATFL graft are sutured with the surgeon's preferred method (Fig 1A). If the harvested tendon length is longer than 225 mm, the ATFL graft also can be prepared as a 2-strand bundle for a stronger graft (Fig 1B).12 The diameter of the graft ends of both the ATFL and LTCL is calculated together. The recommended graft diameter is 4.5 to 6.0 mm.
Fig 1.
Graft preparation. (A) A hamstring tendon is harvested from the pes anserinus and a triangle-shaped graft is prepared. An allograft tendon is another alternative. The harvested tendon usually needs to be longer than 175 mm. It contains one strand of a 20- to 25-mm long bundle for the ATFL graft, one strand of a 30- to 35-mm long bundle for the LTCL graft, and one strand of a 25- to 30-mm long bundle for the CFL graft. The length is determined by a preoperative radiograph and MRI. The 4 ends form a 10- to 15-mm long loop or free-end to facilitate attachment of the thread for graft delivery. The talar side ends of the LTCL and the ATFL graft are sutured with the doctor's preferred method, respectively. The diameter of the graft ends of both the ATFL and LTCL is calculated together. The recommended graft diameter is 4.5 to 6.0 mm. If the harvested tendon length is longer than 225 mm, the ATFL graft also can be prepared as a 2-strand bundle for a stronger graft.12 The bold solid line and bold dotted line represent the tendon graft. (B) The graft is a semitendinosus tendon in this picture. It contains one strand bundle for the ATFL graft. The talar side ends of the LTCL and the ATFL graft are sutured with the Krackow method. (C) The graft is a gracilis tendon in this picture. It contains a 2-strand bundle for the ATFL graft. The talar side end of the LTCL is sutured with the rolling hitch method. The talar side end of the ATFL graft is a loop. Panel B is from patient 1. Panel C is from patient 2. (ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; LTCL, lateral talocalcaneal ligament; MRI, magnetic resonance imaging.)
Step 3: Portal Placement of Ankle Arthroscopy
Three portals are created step-by-step: a conventional anteromedial portal (AM portal), an accessory anterolateral portal (AAL portal), and a subtalar portal (ST portal). The ankle is positioned neutrally. The AM portal is created medial to the anterior tibial tendon and slightly proximal to the joint line.7,12,15 A 30° 2.7-mm or 4.0-mm diameter arthroscope is introduced through the AM portal. The ATFL remnant is viewed with the ankle in a dorsiflexed position.
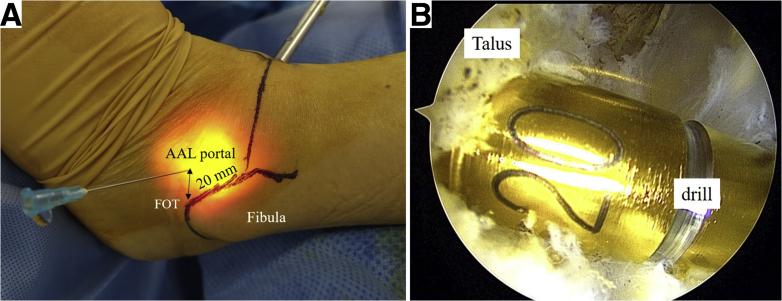
After a needle is inserted into the portal site to confirm accessibility to the ATFL talar footprint, the AAL portal is created. The portal is usually created approximately 20 mm anterior to the anteroinferior tubercle of the distal fibula, known as the fibular obscure tubercle (FOT)17,18 (Fig 2A). The conventional anterolateral portal is created only if necessary, for the treatment to other lesions, e.g. osteochondral lesions.
Fig 2.
Creation of the AAL portal, and the talar tunnel (the left ankle). (A) An arthroscope is introduced through the AM portal. The ankle is dorsiflexed to view the ATFL remnant. Before the AAL portal is created, a needle is inserted into the portal site to confirm accessibility to the ATFL talar footprint. It is usually created at a point approximately 20 mm anterior to the FOT.17,18 (B) A microfracture awl is used to mark the center of the ATFL talar footprint, and a 2.4-mm guidewire is inserted through the AAL portal to drill the talus, from the ATFL footprint toward the distal end of the medial malleolus. The guidewire is then overdrilled, using a drill with the same diameter as the graft end, to create a 20-mm deep talar tunnel. Both panels are from patient 1. (AAL, accessory anterolateral; AM, anteromedial; ATFL, anterior talofibular ligament; FOT, fibular obscure tubercle.)
Step 4: Tunnel Creation
The tunnel creation method is the same as has previously been reported.12 The ATFL remnant is dissected by a shaver and a radiofrequency probe. A microfracture awl is used to mark the center of the ATFL talar footprint, and a 2.4-mm guidewire is inserted through the AAL portal to drill the talus from the ATFL footprint toward the distal end of the medial malleolus.19 The guidewire is then overdrilled, using a drill with the same diameter as the graft end, to create a 20-mm deep talar tunnel (Fig 2B).
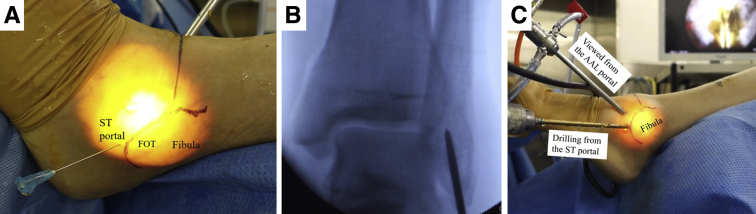
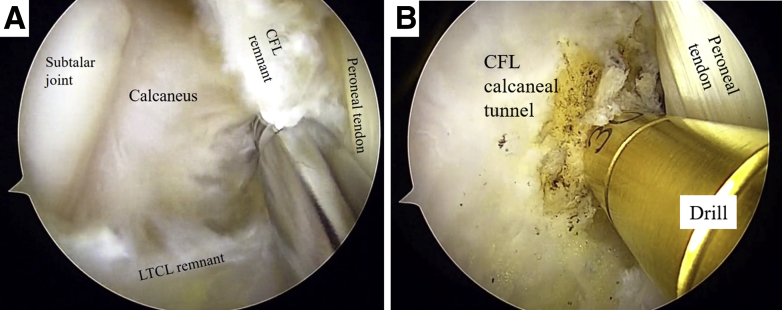
When the ATFL fibular footprint cannot be adequately viewed through the AM portal, surgeons can try to dorsiflex the ankle, change the scope to the 70° arthroscope, or place the scope through the AAL portal. The ST portal is created just below the FOT17 after confirming accessibility to the fibular footprint by a needle (Fig 3A). A guidewire is inserted through the ST portal. Intraoperative fluoroscopy is used to confirm the guidewire position. The insertion point should be below both the articular tip and the FOT.18 The angle between the guidewire direction and the long axis of the fibula on the lateral view is 10° to 30° and almost on the angle bisector of the fibular end on the anteroposterior view (Fig 3B). Viewed from the AAL portal, the guidewire is then overdrilled to create a 20-mm deep fibular tunnel (Fig 3C). The CFL remnant and the LTCL remnant are debrided by a shaver through the ST portal. The surgeon must pay attention to the peroneal tendons, as they run just superficial to the CFL (Fig 4A). The CFL footprint can be observed. A 25- to 30-mm deep calcaneal tunnel is overdrilled after the guidewire is inserted through the ST portal (Fig 4B).
Fig 3.
Creation of the ST portal and the fibular tunnel (the left ankle). (A) The ST portal is created just below the FOT17 after confirming accessibility to the fibular footprint by a needle. (B) A guidewire is inserted through the ST portal. Intraoperative fluoroscopy is used to confirm the guidewire position. The insertion point should be proximal to both the articular tip and the FOT.18 The angle between guidewire direction and the long axis of the fibula on the lateral view is 10° to 30°. The guidewire direction is almost on the angle bisector of the fibular end on the anteroposterior view. (C) Viewed from the AAL portal, the guidewire is overdrilled to create a 20 mm-deep fibular tunnel. All panels are from patient 1. (AAL, accessory anterolateral; AM, anteromedial; FOT, fibular obscure tubercle; ST, subtalar.)
Fig 4.
Creation of the calcaneal tunnel (the left ankle). (A) Viewed from the AAL portal, the CFL remnant and the LTCL remnant are debrided by the shaver through the ST portal. The surgeon must pay attention to the peroneal tendons as they run just superficial to the CFL. (B) A 25- to 30-mm deep calcaneal tunnel for the CFL graft is overdrilled after the guidewire insertion through the ST portal. The subtalar joint is to the left side of the picture. The peroneal tendon is observed on the right side of the drill. Both panels are from patient 1. (AAL, accessory anterolateral; CFL, calcaneofibular ligament; LTCL, lateral talocalcaneal ligament; ST, subtalar.)
Step 5: Tendon Graft Introduction
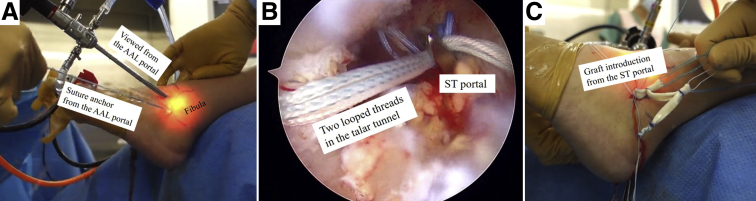
The surgeon then penetrates from the fibula tunnel bottom to the opposite cortex with a 2.9-mm drill wire (Zimmer-Biomet, Warsaw, IN) through the ST portal. If it does not reach the opposite cortex, the drill wire is inserted anteriorly from the anterior edge of the tunnel inlet to the posterior and proximal end to penetrate the posterior cortical wall of the fibula.12 A JuggerKnot Soft Anchor (2.9 mm; Zimmer-Biomet) is placed at the fibula cortex behind the fibular tunnel (Fig 5A). One-strand is sutured to the fibular end of the graft, and the other strand is later pulled to induct it.
Fig 5.
Tendon graft introduction (the left ankle). (A) Viewed from the AAL portal, surgeon penetrated from the fibula tunnel bottom to the opposite cortex with a 2.9-mm drill wire (Zimmer-Biomet) through the ST portal. A JuggerKnot Soft Anchor-2.9 mm (Zimmer-Biomet) is placed at the fibula cortex behind the fibular tunnel. Passing pins of 1.6 mm (Meira Corporation, Ltd.) are inserted to the talar tunnel through the AAL portal and inserted to the calcaneal tunnel through the ST portal. These pins penetrate the bone and the skin on the opposite side. A looped thread is passed to the eye of each passing pin. The passing pins are completely pulled. By pulling the looped thread in the talar tunnel, 2 looped threads are relayed into the talar tunnel. (B) Viewed from the AM portal, the 2 looped threads in the talar tunnel are led from the AAL portal to the ST portal by the suture retriever. (C) Each looped thread is used to induct of the talar side ends of the ATFL graft and the LTCL graft, respectively. The looped thread in the calcaneal tunnel is connected with the calcaneal graft end. Then, the common looped calcaneal end of the CFL and LTCL is introduced from the ST portal to the calcaneal tunnel by pulling the looped thread. One strand of the suture anchor thread is sutured to the fibular end of the graft, and the other strand is pulled to induct it to the fibula tunnel. Panels A and B are from patient 1. (AAL, accessory anterolateral; AM, anteromedial; ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; LTCL, lateral talocalcaneal ligament; ST, subtalar.)
Then, 1.6-mm passing pins (Meira Corporation, Ltd., Nagoya, Japan) are inserted to the talar tunnel through the AAL portal and inserted into the calcaneal tunnel through the ST portal. These pins penetrate the bone and the skin on the opposite side. A looped thread is passed to the eye of each passing pin. The passing pins are completely pulled. By pulling the looped thread in the talar tunnel, 2 looped threads are relayed into the talar tunnel. These 2 looped threads need to be led from the AAL portal to the ST portal by the suture retriever (Fig 5B) and each looped thread is used to induct the talar side ends of the ATFL graft and the LTCL graft, respectively (Fig 5C). The looped thread in the calcaneal tunnel is connected to the calcaneal graft end. Then, the common looped calcaneal end of the CFL and LTCL is introduced from the ST portal to the calcaneal tunnel by pulling the looped thread. The fibular side end of the tendon graft is introduced to the fibula tunnel by pulling the suture anchor thread as mentioned previously.
Step 6: Tendon Graft Fixation
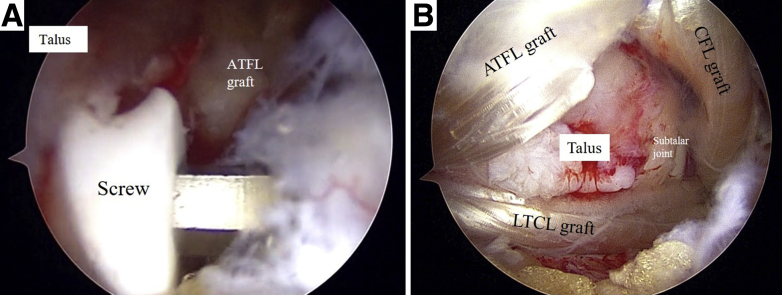
The graft is fixed with an appropriate diameter of 15-mm long bioabsorbable interference screw in the talar tunnel first (Fig 6A). Subsequently, the ATFL graft is tensed by pulling the suture anchor thread at the fibular tunnel. Then, the strands are tied, with the ankle approximately in the 30° to 45° plantar flexion position to avoid postoperative plantar flexion restriction. If the patient is an athlete and wants to start rehabilitation as early as possible, an interference screw fixation is added in the fibular tunnel for stronger initial fixation.12 Finally, the graft is fixed with an interference screw in the calcaneal tunnel, with the ankle in the neutral position. Through this process, the tendon graft finally becomes completely triangle shaped (Fig 6B).
Fig 6.
Tendon graft fixation (the left ankle). (A) Viewed from the AM portal, the graft is fixed with an appropriate-diameter 15-mm long bioabsorbable interference screw in the talar tunnel first. Subsequently, the ATFL graft is tensed by pulling the suture anchor thread at the fibular tunnel. Then, the strands are tied, with the ankle approximately in the 30° to 45° plantar flexion position to avoid postoperative plantar flexion restriction. Finally, the graft is fixed with an interference screw in the calcaneal tunnel, with the ankle in the neutral position. (B) Viewed from the AAL portal, the tendon graft finally becomes the complete triangle-shaped. Both panels are from patient 1. (AAL, accessory anterolateral; AM, anteromedial; ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; LTCL, lateral talocalcaneal ligament.)
Optional Technique when the Screw Is Not Firmly Fixed or Too Big to Insert
If the screw is not firmly fixed, the screw size is changed to a bigger size or the cancellous bone tips are grafted to the space between the tunnel and tendon graft.12 If the screw is too big to insert into the tunnel, a smaller screw should be chosen.
Discussion
Ankle sprains are the most common injuries sustained during sport activities.20,21 The ATFL is most frequently injured in ankle sprains.22 Epidemiologic surveys indicate that the ATFL is the ligament that is injured in 85% of all ankle sprain ligament injuries, whereas the CFL is involved in 35% and the PTFL in 12%.23 Although the existence rate of LTCL rupture in ankle sprains is unclear, 58% of patients with chronic ankle instability have mechanical instability of the subtalar joint.24 The subtalar ligaments include the CFL, the LTCL, the interosseous talocalcaneal ligament, and the cervical ligament.25 Even though anatomical ATFL and CFL reconstruction is performed, 10.5% of patients experience subjective instability.13 The dysfunction of the LTCL or other ligaments might be overlooked in those patients. Moreover, surgeons often encounter and reluctantly dissect the LTCL during the arthroscopic ATFL and CFL reconstruction.12 The present procedure can salvage LTCL function in these cases. Therefore, LTCL reconstruction combined with ATFL and CFL reconstruction is possibly useful for the treatment of the concomitant case of talocrural and subtalar joint instability. As the existence rate of LTCL is from 42% to 66%,1, 2, 3 the repair technique is not always available, and the reconstruction technique using a tendon graft is more reasonable. Open reconstruction techniques may require a longer skin incision and have a greater risk of postoperative skin problems and foot numbness due to the nerve damage. The arthroscopic approach is preferable as the ALC-triangle procedure needs only 3 portals, the same as the arthroscopic ATFL and CFL reconstruction.11,12
The LTCL is classified into 3 types: type I, the LTCL branches from the CFL; type II, the LTCL is independent of the CFL and runs parallel to the calcaneus; and type III, the LTCL is absent.1, 2, 3 Although the function of the LTCL has not been completely elucidated, it is reported that it restricts excessive supination,26 abduction, and adduction27 of the subtalar joint. It may as well regulate the external rotation and medial translation of the calcaneus on the talus in the transvers plane, because the LTCL originates the talar neck and runs posteriorly and distally to the calcaneus on the lateral side of the subtalar joint. Thus, the medial subtalar glide test24 is an alternative method to assess LTCL function. As the talocrural joint is stiffened by bony constraints in the dorsiflexed position, the medial subtalar glide test with a dorsiflexed ankle might be more useful for surgeons to access the subtalar joint stability and consider the indication of LTCL reconstruction.
As the length of the LTCL is approximately 26 mm3,28 and it is difficult to determine the exact length with preoperative images, a 30- to 35-mm long bundle is recommended for the LTCL. If it is too long, it can be adjusted by inducting the graft end deeper into the tunnel. However, if it is too short, additional operative time will be necessary for re-preparation of the tendon graft.
Debate exists regarding the present technique. As type 2 LTCL has an independent calcaneus attachment site of the CFL,1, 2, 3 it might be better to create an independent calcaneal tunnel for the LTCL anterior to the CFL footprint in such cases. However, one common calcaneal tunnel for the LTCL and CFL is an easier, safer, and more reproducible technique. Although the effectiveness of additional LTCL reconstruction is unknown and should be researched in the future, authors believe the ALC-triangle is a useful technique for a certain percentage of chronic ankle instability patients. A summary of advantages and disadvantages is provided in Table 2.
Table 2.
Advantages and Disadvantages
| Advantages |
| Possible improved stability of the subtalar joint and long-term clinical results |
| Salvageable after reluctant LTCL dissection in the arthroscopic ATFL and CFL reconstruction |
| Only 3 portals, the same as the arthroscopic ATFL and CFL reconstruction technique |
| Safe and reproducible tunnel creation |
| Anatomical reconstruction and less postoperative risk of ROM restriction |
| Disadvantages |
| A longer tendon graft is necessary |
| Possible risk of tunnel fracture |
| Necessary for basic arthroscopy skills |
| Use of intraoperative fluoroscopy |
ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; LTCL, lateral talocalcaneal ligament; ROM, range of motion.
Acknowledgments
We thank Editage (www.editage.jp) for English-language editing.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The video is of patient 1, left ankle. Shown is the surgical technique for arthroscopic reconstruction technique of the ATFL, LTCL, and CFL using a triangle-shaped tendon graft (ALC-triangle). This surgery is performed with the patient under general anesthesia and in the supine position. A tourniquet is placed on the proximal thigh. The foot is suspended from the distal edge of the bed. The contralateral leg is slightly lowered to provide a wide working space.7,12 The semitendinosus tendon is harvested from the pes anserinus, and a triangle-shaped graft is prepared. It contains one strand of a 20-mm long bundle for the ATFL graft, one strand of a 30-mm long bundle for the LTCL graft, and one strand of a 30-mm long bundle for the CFL graft. The length is determined by a preoperative radiograph and MRI. The 4 ends form a 10- to 15-mm long loop or free-end to facilitate the attachment of the thread for graft delivery. The talar side ends of the LTCL and the ATFL graft are sutured with the Krackow method, respectively. The diameter of the graft ends of both ATFL and LTCL is calculated together. The recommended graft diameter is 4.5 to 6.0 mm. Three portals are created step-by-step: a conventional AM portal, an AAL portal, and an ST portal. The ankle is positioned neutrally. The AM portal is created medial to the anterior tibial tendon and slightly proximal to the joint line.7,12,15 A 30° 4.0 mm-diameter arthroscope is introduced through the AM portal. The ATFL remnant is viewed with the ankle dorsiflexed position. After a needle is inserted into the portal site to confirm accessibility to the ATFL talar footprint, the AAL portal is created. The portal is usually created at approximately 20 mm anterior to the anteroinferior tubercle of the distal fibula, which is called the FOT.17,18 The ATFL remnant is dissected. A microfracture awl is used to mark the center of the ATFL talar footprint, and a 2.4-mm guidewire is inserted through the AAL portal to drill the talus from the ATFL footprint towards the distal end of the medial malleolus.19 The guidewire is then overdrilled, using a drill having the same diameter as the graft end, to create a 20-mm deep talar tunnel. The ST portal is created just below the FOT17 after confirming accessibility to the fibular footprint with a needle. A guidewire is inserted through the ST portal. Intraoperative fluoroscopy is used to confirm the guidewire position. The insertion point should be below both the articular tip and the FOT.17 The angle between guidewire direction and the long axis of the fibula on the lateral view is 10° to 30° and almost on the angle bisector of the fibular end on the anteroposterior view. Viewed from the AAL portal, the guidewire is overdrilled to create a 20-mm deep fibular tunnel. The CFL remnant and the LTCL remnant are debrided by a shaver through the ST portal. The CFL footprint can be observed. A 30-mm deep calcaneal tunnel is overdrilled after the guidewire insertion through the ST portal. The surgeon penetrates from the fibula tunnel bottom to the opposite cortex with a 2.9-mm drill wire through the ST portal. A JuggerKnot Soft Anchor-2.9 mm (Zimmer-Biomet) is placed at the fibula cortex behind the fibular tunnel. Then, 1.6-mm passing pins (Meira Corporation, Ltd.) are inserted to the talar tunnel through the AAL portal and inserted into the calcaneal tunnel through the ST portal. These pins penetrate the bone and the skin on the opposite side. A looped thread is passed to the eye of each passing pin. The passing pins are completely pulled. By pulling the looped thread in the talar tunnel, 2 looped threads are relayed into the talar tunnel. These 2 looped threads need to be led from the AAL portal to the ST portal by the suture retriever and each looped thread is then used to induct the talar side ends of the ATFL graft and the LTCL graft, respectively. The looped thread in the calcaneal tunnel is connected with the calcaneal graft end. Then, the common looped calcaneal end of the CFL and LTCL is introduced from the ST portal to the calcaneal tunnel by pulling the looped thread. One-strand of the suture anchor thread is sutured to the fibular end of the graft, and the other strand is pulled to induct it to the fibula tunnel. The graft is fixed with a 15-mm long bioabsorbable interference screw in the talar tunnel first. Subsequently, the ATFL graft is tensed by pulling the suture anchor thread at the fibular tunnel. Then, the strands are tied, with the ankle in the approximately 45° plantar flexion position, to avoid postoperative plantar flexion restriction. Finally, the graft is fixed with an interference screw in the calcaneal tunnel, with the ankle in the neutral position. The tendon graft finally becomes completely triangle-shaped. (AAL, accessory anterolateral; AM, anteromedial; ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; FOT, fibular obscure tubercle; LTCL, lateral talocalcaneal ligament; MRI, magnetic resonance imaging; ST, subtalar.)
References
- 1.Trouilloud P., Dia A., Grammont P., Gelle M.C., Autissier J.M. Variations in the calcaneo-fibular ligament (lig. calcaneofibulare). Application to the kinematics of the ankle. Bull Assoc Anat (Nancy) 1988;72:31–35. [in French] [PubMed] [Google Scholar]
- 2.Wiersma P., Griffioen F., Variations of three lateral ligaments of the ankle A descriptive anatomical study. Foot. 1992;2:218–224. [Google Scholar]
- 3.Edama M., Kageyama I., Kikumoto T. Morphological characteristics of the lateral talocalcaneal ligament: A large-scale anatomical study. Surg Radiol Anat. 2019;41:25–28. doi: 10.1007/s00276-018-2128-8. [DOI] [PubMed] [Google Scholar]
- 4.Higashiyama R., Aikawa J., Iwase D. Arthroscopic anterior talofibular ligament reconstruction using a gracilis tendon. Knee Surg Sports Traumatol Arthrosc. 2014;22:S324–S325. [Google Scholar]
- 5.Song B., Li C., Chen N. All-arthroscopic anatomical reconstruction of anterior talofibular ligament using semitendinosus autografts. Int Orthop. 2017;41:975–982. doi: 10.1007/s00264-017-3410-9. [DOI] [PubMed] [Google Scholar]
- 6.Vila-Rico J., Cabestany-Castella J.M., Cabestany-Perich B., Nunez-Samper C., Ojeda-Thies C. All-inside arthroscopic allograft reconstruction of the anterior talo-fibular ligament using an accesory transfibular portal. Foot Ankle Surg. 2019;25:24–30. doi: 10.1016/j.fas.2017.12.008. [DOI] [PubMed] [Google Scholar]
- 7.Higashiyama R., Sekiguchi H., Takata K., Katagiri A., Inoue G., Takaso M. Anatomical arthroscopic anterior talofibular ligament repair and reconstruction using a free tendon. Arthrosc Tech. 2020;9:e21–e28. doi: 10.1016/j.eats.2019.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lui T.H. Arthroscopic-assisted lateral ligamentous reconstruction in combined ankle and subtalar instability. Arthroscopy. 2007;23:e551–e555. doi: 10.1016/j.arthro.2006.07.038. [DOI] [PubMed] [Google Scholar]
- 9.Guillo S., Archbold P., Perera A., Bauer T., Sonnery-Cottet B. Arthroscopic anatomic reconstruction of the lateral ligaments of the ankle with gracilis autograft. Arthrosc Tech. 2014;3:e593–e598. doi: 10.1016/j.eats.2014.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higashiyama R., Aikawa J., Iwase D. Arthroscopic ATFL and CFL reconstruction using a hamstrings tendon. J Jpn Soc Surg Foot. 2015;36:189–194. [Google Scholar]
- 11.Takao M., Glazebrook M., Stone J., Guillo S. Ankle arthroscopic reconstruction of lateral ligaments (Ankle Anti-ROLL) Arthrosc Tech. 2015;4:e595–e600. doi: 10.1016/j.eats.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higashiyama R., Aikawa J., Iwase D., Takamori Y., Watanabe E., Takaso M. Anatomical arthroscopic anterior talofibular ligament and calcaneofibular ligament reconstruction using an autogenic hamstring tendon: Safe creation of anatomical fibular tunnel. Arthrosc Tech. 2019;8:e215–e222. doi: 10.1016/j.eats.2018.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lopes R., Andrieu M., Cordier G. Arthroscopic treatment of chronic ankle instability: Prospective study of outcomes in 286 patients. Orthop Traumatol Surg Res. 2018;104:S199–S205. doi: 10.1016/j.otsr.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 14.Gui J., Jiang Y., Li Y. All arthroscopic remnant-preserving technique to reconstruct the lateral ankle ligament complex. Arthrosc Tech. 2017;6:e549–e557. doi: 10.1016/j.eats.2016.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Higashiyama R. Arthroscopic reconstruction of the posterior talofibular, anterior talofibular, and calcaneofibular ligaments: Scopic PAC. In: Lui T.H., editor. Arthroscopy and endoscopy of the foot and ankle: Principle & Practice. Springer Singapore; Singapore: 2019. pp. 159–169. [Google Scholar]
- 16.Yeh W.L., Chen J.M., Liu C.H., Tsai P.J., Higashiyama R., Takaso M. Endoscopic harvest of autogenous gracilis and semitendinosus tendons. Arthrosc Tech. 2018;7:e1019–e1024. doi: 10.1016/j.eats.2018.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buzzi R., Todescan G., Brenner E., Segoni F., Inderster A., Aglietti P. Reconstruction of the lateral ligaments of the ankle: An anatomic study with evaluation of isometry. J Sports Traumatol Relat Res. 1993;15:55–74. [Google Scholar]
- 18.Matsui K., Oliva X.M., Takao M. Bony landmarks available for minimally invasive lateral ankle stabilization surgery: A cadaveric anatomical study. Knee Surg Sports Traumatol Arthrosc. 2017;25:1916–1924. doi: 10.1007/s00167-016-4218-7. [DOI] [PubMed] [Google Scholar]
- 19.Michels F., Guillo S., Vanrietvelde F., Brugman E., Stockmans F. How to drill the talar tunnel in ATFL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2016;24:991–997. doi: 10.1007/s00167-016-4018-0. [DOI] [PubMed] [Google Scholar]
- 20.Guillo S., Bauer T., Lee J.W. Consensus in chronic ankle instability: Aetiology, assessment, surgical indications and place for arthroscopy. Orthop Traumatol Surg Res. 2013;99:S411–S419. doi: 10.1016/j.otsr.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 21.Michels F., Pereira H., Calder J. Searching for consensus in the approach to patients with chronic lateral ankle instability: Ask the expert. Knee Surg Sports Traumatol Arthrosc. 2018;26:2095–2102. doi: 10.1007/s00167-017-4556-0. [DOI] [PubMed] [Google Scholar]
- 22.Ferran N.A., Maffulli N. Epidemiology of sprains of the lateral ankle ligament complex. Foot Ankle Clin. 2006;11:659–662. doi: 10.1016/j.fcl.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 23.Swenson D.M., Collins C.L., Fields S.K., Comstock R.D., Epidemiology of U.S High school sports-related ligamentous ankle injuries, 2005/06-2010/11. Clin J Sport Med. 2013;23:190–196. doi: 10.1097/JSM.0b013e31827d21fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hertel J., Denegar C.R., Monroe M.M., Stokes W.L. Talocrural and subtalar joint instability after lateral ankle sprain. Med Sci Sports Exerc. 1999;31:1501–1508. doi: 10.1097/00005768-199911000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Sarrafian S. Sarrafian’s anatomy of the foot and ankle. 3rd ed. Lippincott Williams & Wilkins; Philadelphia: 2011. Syndesmology; pp. 163–222. [Google Scholar]
- 26.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37:364–375. [PMC free article] [PubMed] [Google Scholar]
- 27.Weindel S., Schmidt R., Rammelt S., Claes L., v Campe A., Rein S. Subtalar instability: A biomechanical cadaver study. Arch Orthop Trauma Surg. 2010;130:313–319. doi: 10.1007/s00402-008-0743-2. [DOI] [PubMed] [Google Scholar]
- 28.Burks R.T., Morgan J. Anatomy of the lateral ankle ligaments. Am J Sports Med. 1994;22:72–77. doi: 10.1177/036354659402200113. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The video is of patient 1, left ankle. Shown is the surgical technique for arthroscopic reconstruction technique of the ATFL, LTCL, and CFL using a triangle-shaped tendon graft (ALC-triangle). This surgery is performed with the patient under general anesthesia and in the supine position. A tourniquet is placed on the proximal thigh. The foot is suspended from the distal edge of the bed. The contralateral leg is slightly lowered to provide a wide working space.7,12 The semitendinosus tendon is harvested from the pes anserinus, and a triangle-shaped graft is prepared. It contains one strand of a 20-mm long bundle for the ATFL graft, one strand of a 30-mm long bundle for the LTCL graft, and one strand of a 30-mm long bundle for the CFL graft. The length is determined by a preoperative radiograph and MRI. The 4 ends form a 10- to 15-mm long loop or free-end to facilitate the attachment of the thread for graft delivery. The talar side ends of the LTCL and the ATFL graft are sutured with the Krackow method, respectively. The diameter of the graft ends of both ATFL and LTCL is calculated together. The recommended graft diameter is 4.5 to 6.0 mm. Three portals are created step-by-step: a conventional AM portal, an AAL portal, and an ST portal. The ankle is positioned neutrally. The AM portal is created medial to the anterior tibial tendon and slightly proximal to the joint line.7,12,15 A 30° 4.0 mm-diameter arthroscope is introduced through the AM portal. The ATFL remnant is viewed with the ankle dorsiflexed position. After a needle is inserted into the portal site to confirm accessibility to the ATFL talar footprint, the AAL portal is created. The portal is usually created at approximately 20 mm anterior to the anteroinferior tubercle of the distal fibula, which is called the FOT.17,18 The ATFL remnant is dissected. A microfracture awl is used to mark the center of the ATFL talar footprint, and a 2.4-mm guidewire is inserted through the AAL portal to drill the talus from the ATFL footprint towards the distal end of the medial malleolus.19 The guidewire is then overdrilled, using a drill having the same diameter as the graft end, to create a 20-mm deep talar tunnel. The ST portal is created just below the FOT17 after confirming accessibility to the fibular footprint with a needle. A guidewire is inserted through the ST portal. Intraoperative fluoroscopy is used to confirm the guidewire position. The insertion point should be below both the articular tip and the FOT.17 The angle between guidewire direction and the long axis of the fibula on the lateral view is 10° to 30° and almost on the angle bisector of the fibular end on the anteroposterior view. Viewed from the AAL portal, the guidewire is overdrilled to create a 20-mm deep fibular tunnel. The CFL remnant and the LTCL remnant are debrided by a shaver through the ST portal. The CFL footprint can be observed. A 30-mm deep calcaneal tunnel is overdrilled after the guidewire insertion through the ST portal. The surgeon penetrates from the fibula tunnel bottom to the opposite cortex with a 2.9-mm drill wire through the ST portal. A JuggerKnot Soft Anchor-2.9 mm (Zimmer-Biomet) is placed at the fibula cortex behind the fibular tunnel. Then, 1.6-mm passing pins (Meira Corporation, Ltd.) are inserted to the talar tunnel through the AAL portal and inserted into the calcaneal tunnel through the ST portal. These pins penetrate the bone and the skin on the opposite side. A looped thread is passed to the eye of each passing pin. The passing pins are completely pulled. By pulling the looped thread in the talar tunnel, 2 looped threads are relayed into the talar tunnel. These 2 looped threads need to be led from the AAL portal to the ST portal by the suture retriever and each looped thread is then used to induct the talar side ends of the ATFL graft and the LTCL graft, respectively. The looped thread in the calcaneal tunnel is connected with the calcaneal graft end. Then, the common looped calcaneal end of the CFL and LTCL is introduced from the ST portal to the calcaneal tunnel by pulling the looped thread. One-strand of the suture anchor thread is sutured to the fibular end of the graft, and the other strand is pulled to induct it to the fibula tunnel. The graft is fixed with a 15-mm long bioabsorbable interference screw in the talar tunnel first. Subsequently, the ATFL graft is tensed by pulling the suture anchor thread at the fibular tunnel. Then, the strands are tied, with the ankle in the approximately 45° plantar flexion position, to avoid postoperative plantar flexion restriction. Finally, the graft is fixed with an interference screw in the calcaneal tunnel, with the ankle in the neutral position. The tendon graft finally becomes completely triangle-shaped. (AAL, accessory anterolateral; AM, anteromedial; ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; FOT, fibular obscure tubercle; LTCL, lateral talocalcaneal ligament; MRI, magnetic resonance imaging; ST, subtalar.)